Entrustable Professional Activities implementation in undergraduate allied health therapy programs
Submitted: 24 January 2023
Accepted: 2 August 2023
Published online: 2 January, TAPS 2024, 9(1), 42-48
https://doi.org/10.29060/TAPS.2024-9-1/SC2997
Rahizan Zainuldin1 & Heidi Siew Khoon Tan1,2
1Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore; 2Pre-Professional Education Office, Tan Tock Seng Hospital, Singapore
Abstract
Introduction: Singapore Institute of Technology’s undergraduate (UG) occupational therapy (OT) and physiotherapy (PT) programs are one of the first implementors of Entrustable Professional Activities (EPAs) in the respective allied health professions training. The aim of the paper is to report the outcomes of the first year of EPAs implementation in clinical practice education (CPE) and share next steps refining implementation.
Methods: A quality improvement (QI) study using the Plan-Do-Check-Act (PDCA) cycle was conducted. UG OT Year 2 and Year 3 students, UG PT Year 3 students and their clinical educators (CEs) who experienced the use of EPAs for the first time were surveyed at the end of the clinical block.
Results: There was generally high agreement (>70% agreed or strongly agreed) among all groups in using EPAs to better understand the learning objectives of CPE and practice expectations as future entry-level practitioners at conditional-registration. More than 70% of OT respondents but less than 50% PT respondents found the EPA assessment forms easy to use. Less than 60% of both program CEs did not include colleagues for EPA assessments. 55% of both OT and PT CEs found the EPA training and resources adequate. Overall, PT respondents showed lower agreement than OT respondents in five survey items.
Conclusion: The first implementation cycle of EPA in the undergraduate OT and PT CPE had mixed acceptability to the EPA assessment tools. Three strategic changes were made for the second implementation cycle., i.e., redesign of EPA-based assessment forms, training focus and ‘just-in-time’ training with streamlined resources.
Keywords: Clinical Training, Entrustable Professional Activities, Occupational Therapy, Physiotherapy, Undergraduate, Workplace-based Assessment
I. INTRODUCTION
In 2021, the occupational therapy (OT) and physiotherapy (PT) undergraduate programs at Singapore Institute of Technology (SIT) added a novel assessment, Entrustable Professional Activities (EPAs), to the extant competency-based assessment tools in clinical practice education (CPE). EPAs are units of professional activities entrusted to a learner determined by five levels of supervision, once the learner has demonstrated the required competence (ten Cate & Taylor, 2020). OT EPAs and PT EPAs (Zainuldin & Tan, 2021) were developed and introduced to SIT CPE as part of the Ministry of Health’s review of healthcare professions’ training standards. EPA-based assessments are relevant in CPE where students perform professional activities at workplace, supervised by onsite clinical educators (CEs). Previous CPEs assessed only OT and PT student competencies using the validated Student Practice Evaluation Form-Revised Edition (SPEF-R) (Turpin et al., 2011) and the Clinical Competency and Reasoning Assessment (CCRA), respectively. Conceptually, the pairing of EPAs with SPEF-R or CCRA potentially offer CEs an opportunity to empower students through graduated levels of entrustment supported by appropriate proficiency levels. Operationally, EPA assessment does not add new activities. OT and PT CEs can utilise routine observations of students’ tasks, case discussions and case-notes documentation as sources to inform entrustment levels in EPAs.
No EPA implementation in any OT and PT curricula has been documented. At SIT, EPA implementation in CPE needs evaluation. Recognising that implementing process changes requires an iterative approach, SIT embarked on a quality improvement study using the Plan-Do-Check-Act (PDCA) cycle. This paper reports the results of operationalising EPAs for the first time in OT and PT CPE, including the use of EPA-based assessment forms. The Methods section describes the Plan and Do, followed by the Results section reporting outcomes of the Check and the Discussion section highlighting the Act to improve implementation.
II. METHODS
A. CPE Structure
OT CPE consists of four blocks of seven weeks each and interspersed between academic modules in Years 2, 3 and 4. PT CPE consists of five consequent blocks (four core and one elective) of six weeks each, begins only after all academic modules are completed in Year 3 and continues to Year 4. OT and PT students complete different clinical settings for each CPE block.
B. Participants and Study Design
OT Year 2 and Year 3 students, PT Year 3 students and their CEs who experienced EPA use for the first time were surveyed at the end of a clinical block. An online EPA survey is incorporated with routine post placement feedback for both students and CEs, therefore no consent was required. The QI study was exempt from ethics review (SIT Institutional Review Board, No. 2022122). Survey results were extracted from February to December 2021.
C. PDCA Cycle: Plan-Do
OT and PT have five core EPAs each. EPA-based assessment activities are short practice observations, entrustment-based discussions and case-notes evaluations. These activities serve as sources of information (SOIs), or workplace-based assessments (WBAs) in OT CPE, to inform entrustment decision-making. OT CE assesses EPAs by documenting in a single patient case form with all three WBAs per EPA. PT CE assesses EPAs for every patient case anchored by three different SOI forms with written justifications. OT and PT CEs and students were trained on nuts and bolts of EPAs and on using WBA/SOI forms in CE training workshops and student pre-CPE briefing, respectively.
Each OT EPA requires a total of six patient cases entrusted to students at Level 3 entrustment (indirect supervision) across four CPE blocks. Each PT EPA requires six cases at Level 3 entrustment at each core clinical block, which totals 24 cases by end of the program. Appendix 1 and 2 provides visualisation of EPA implementation across multiple CPE blocks.
The EPA survey has ten items. The first eight items are scored on a 4-point Likert-scale (strongly disagree-strongly agree). The final two questions seek qualitative feedback on benefits and challenges and suggestions for improvements. Unless indicated, items are phrased in the same manner in both student and CE surveys.
D. Data Collection and Analysis
Data were counted as proportions of respondents who agreed (pooled response from ‘agree’ and ‘strongly agree’) and proportions disagreed (pooled from ‘disagree’ and ‘strongly disagree’). The authors grouped the qualitative narrative into benefits and challenges.
III. RESULTS
A. PDCA Cycle: Check
There were 99.0% response rate from OT Year 2 students (105/106), 97.7% from Year 3 OT students (85/87), 93.2% from PT Year 3 students (137/147), 98.5% from OT CEs (199/202) and 92.5% from PT CEs (247/267). Proportion of respondents who agreed with each item statement is shown in Table 1. Data on item scores for each student and CE are available at online repository, http://doi.org/10.6084/m9.figshare.21941288
|
Survey Items |
OT Year 3 students |
OT Year 2 students |
PT Year 3 students |
OT CEs
|
PT CEs
|
|
(n = 85) |
(n = 105) |
(n = 137) |
(n = 199) |
(n = 247) |
|
|
Q1 – Using EPAs in CPE helps me better understand and meet future conditional-registration requirements.
|
90.6 |
98.1 |
75.2 |
89.4 |
71.7 |
|
Q2 – The EPA documents help me to better understand the learning objectives in CPE.
|
84.7 |
98.1 |
72.3 |
75.9 |
71.7 |
|
Q3 – The WBA/SOI forms are easy to use.
|
76.5 |
85.7 |
38.7 |
73.4 |
47.8 |
|
Q4 – CE: The WBA/SOI forms are adequate for me to determine students’ competence and entrustment level. / Student: The WBAs/SOIs help me to better gauge my progress and level of competence.
|
91.8 |
97.1 |
70.1 |
72.9 |
64.6 |
|
Q5 – I understand the connection between OT EPAs and SPEF-R2 competencies or PT EPAs and CCRA.
|
84.7 |
97.1 |
72.3 |
69.8 |
83.0 |
|
Q6 – CE: I use the EPA documents explicitly with students during clinical teaching and assessment. / Student: I use the EPA documents to guide my learning goals during CPE.
|
62.4 |
92.4 |
51.1 |
87.9 |
59.1 |
|
Q7 – CE: I involve other colleagues in doing WBAs/SOIs to calibrate students’ entrustment level. / Student: Besides my CE, I also received feedback from other OTs or other PTs who were involved in my WBAs/SOIs.
|
44.7 |
66.7 |
54.0 |
58.8 |
45.3 |
|
Q8 – I feel the current briefing/training/resources are adequate for me to incorporate the use of EPAs in CPE. |
70.6 |
89.5 |
56.2 |
55.3 |
55.9 |
Table 1. Proportion of OT and PT students and CEs who agree with the EPA survey items
PT CEs and students were almost unanimous that SOI forms were difficult to use (Q3). Common to OT and PT CEs, many did not involve colleagues in EPAs (Q7) and felt that training to understand EPAs was inadequate (Q8).
Qualitatively, both disciplines benefitted from the use of WBA/SOI forms to scaffold learning through structured feedback and action plans when addressing identified competency gaps. Feedback from OT and PT students below closely exemplified the appreciation:
“EPAs allow me to track my progress over the weeks and transfer my reflections into action when given the opportunity to receive objective and qualitative feedback from the EPA form.”
OT Student#45
“The discussions with the CE on what to do if the situation was different made me realise the importance of planning even for the worst-case scenario…enabled me to identify the gaps in knowledge and skills that had to be worked on.”
PT Student#67
However, PT groups cited complicated forms design and copious paperwork from numerous SOIs time-consuming and stressful. Ambivalence on its practicality was best summed by PT CE#31, “As a first-time user of the SOIs, I found it quite difficult to navigate the forms, took me some tries to understand how I can determine the students’ competence and entrustment level. As there were many forms, it was quite confusing, and hence stressful and time-consuming. Otherwise, they are useful tools.”
The most common challenge among OT CEs was assessing certain EPAs, such as planning care transition, in some settings. “Some EPAs are harder to do in some settings, for example, in the hands therapy setting; it is harder to do the handover/discharge EPA as there are less of these patients.” (OT CE#32). Calling for more support, one CE suggested “SIT go through a round of training on the different EPAs and give relevant case examples to help us better understand them.” (OT CE#4).
IV. DISCUSSION
Response rates were excellent. The convergence of high agreement rates with narrative feedback on using EPAs and WBA/SOIs for teaching/learning, understanding the CPE learning objectives and meeting practice expectations as future entry-level practitioners suggest early indication that EPAs may facilitate SIT OT and PT students transit to new practitioners. The positive experience in this regard resonated with other EPA survey on final-year dietetics students and their clinical supervisors in Australia (Bramley et al., 2021). Practical challenges with the SOI forms, resulting in onerous and time-consuming evidence collection; low levels in involving colleagues in EPA assessments; and inadequate EPA training/resources for CEs were identified as key areas for change in both disciplines.
A. PDCA Cycle: Act
First, to reduce assessment burden, WBA and SOI forms were redesigned and harmonised in preparation towards a standardised EPA online assessment system currently developed in-house. Multiple WBA/SOI forms were combined into a single-page checklist form with a small open-ended section. A checklist was similarly suggested for nursing EPAs assessment, citing convenience as a reason (Lau et al., 2020). On the single-page form, CEs tick entrustment levels for each WBA/SOI associated to each EPA with all EPAs on the same page. The only narrative section is where CEs describe key justifications supporting their entrustment decisions, followed by students’ reflections. Second, to bridge assessment expectations among clinicians and increase propensity to share EPA assessments with colleagues, EPA training was refined to emphasise balance of supervision control with autonomy and clearer definitions between entrustment levels 2 (direct supervision) and 3 (indirect supervision) through case examples. Third, ‘just-in-time’ refresher training was added to activate volition in assessing EPAs. Toolkits containing briefing videos and streamlined resources in short bites, such as 3-minute videos, powtoons, form samplers and frequently-asked-questions, were released for OT and PT CEs closer to placement block. PT CEs also received a refresher at early weeks of every placement block.
V. CONCLUSION
The PDCA cycle is used to inform and make iterative adaptations to each cycle of EPA implementation. The Plan-Do stage completed the first implementation cycle of EPA in the undergraduate OT and PT CPE in 2021. The Check stage revealed mixed experiences to EPA use. The lowest agreement was the ease of using SOI forms among PT students and CEs. While EPAs were accepted as teaching and learning tools, CEs did not involve colleagues in EPA assessments. Training on EPA assessment for CEs was inadequate. Consequently, the Act stage yielded changes in form design, training focus and streamlined resources for the next implementation cycle.
Notes on Contributors
Rahizan Zainuldin (RZ) led the design of the quality improvement and implementation of EPAs, submitted the study to SIT IRB, analysed and interpreted both quantitative and qualitative data for the PT CPE, prepared the manuscript, wrote the initial draft and finalised for submission.
Heidi Siew Khoon Tan (HSKT) led the design of the EPA survey, analysed and interpreted both quantitative and qualitative data for the OT CPE, provided a critical review of the manuscript, and concurred on the final version.
Ethical Approval
The QI study was exempt from ethics review (SIT Institutional Review Board, No. 2022122).
Data Availability
Data on item scores for each student and CE are available at online repository, publicly accessed at http://doi.org/ 10.6084/m9.figshare.21941288. While the data is available for readers’ perusal and no permission from the authors is needed, please write an email of intention to use the data for any purposes to the corresponding author.
Acknowledgement
We would like to acknowledge the OT and PT CPE committee members who have contributed in the planning and implementation of the EPA. We would also like to thank Ms Annie Wang Haiyan, Manager, Academic Programmes Administration, SIT, for uploading the survey on and extracting the survey results from the online assessment portal of our Clinical Practice Education portal.
Funding
No funding source is provided.
Declaration of Interest
Rahizan Zainuldin and Heidi Siew Khoon Tan disclose there is no conflict of interest of any form.
References
Bramley, A. L., Thomas, C. J., McKenna, L., & Itsiopoulos, C. (2021). E-portfolios and entrustable professional activities to support competency-based education in dietetics. Nursing and Health Sciences, 23(1), 148-156. https://doi.org/10.1111/nhs.12774
Lau, S. T., Ang, E., Samarasekera, D. D., & Shorey, S. (2020). Evaluation of an undergraduate nursing entrustable professional activities framework: An exploratory qualitative research. Nurse Education Today, 87, Article 104343. https://doi.org/10.1016/j.nedt.2020.104343
ten Cate, O., & Taylor, D. R. (2020). The recommended description of an entrustable professional activity: AMEE Guide No. 140. Medical Teacher 43(10), 1106-1114. https://doi.org/10.1080/0142159X.2020.1838465
Turpin, M., Fitzgerald, C., & Rodger, S. (2011). Development of the Student Practice Evaluation Form Revised Edition Package. Australian Occupational Therapy Journal, 58(2), 67-73. https://doi.org/10.1111/j.1440-1630.2010.00890.x
Zainuldin, R., & Tan, H. Y. (2021). Development of entrustable professional activities for a physiotherapy undergraduate programme in Singapore. Physiotherapy, 112, 64-71. https://doi.org/10.1016/j.physio.2021.03.017
*Rahizan Zainuldin
10 Dover Road,
Singapore 138683
+6596522418
Email: Rahizan.Zainuldin@singaporetech.edu.sg
Submitted: 18 February 2023
Accepted: 28 March 2023
Published online: 3 October, TAPS 2023, 8(4), 40-45
https://doi.org/10.29060/TAPS.2023-8-4/SC3010
Kit Mun Tan1, Chan Choong Foong2, Donnie Adams3, Wei Han Hong2, Yew Kong Lee4 & Vinod Pallath2
1Department of Medicine, Faculty of Medicine, Universiti Malaya, Malaysia; 2Medical Education and Research Development Unit (MERDU), Faculty of Medicine, Universiti Malaya, Malaysia; 3Department of Educational Management, Planning and Policy, Faculty of Education, Universiti Malaya, Malaysia; 4Department of Primary Care, Faculty of Medicine, Universiti Malaya, Malaysia
Abstract
Introduction: The global COVID-19 pandemic had greatly affected the delivery of medical education, where institutions had to convert to remote learning almost immediately. This study aimed to measure undergraduate medical students’ readiness and factors associated with readiness for remote learning.
Methods: A cross-sectional quantitative study was conducted amongst undergraduate medical students using the Blended Learning Readiness Engagement Questionnaire, during the pandemic where lessons had to be delivered fully online in 2020.
Results: 329 students participated in the study. Mean scores for remote learning readiness were 3.61/4.00 (technology availability), 3.60 (technology skills), 3.50 (technology usage), 3.35 (computer and internet efficacy), and 3.03 (self-directed learning). Male students appeared more ready for remote learning than females, in the dimensions of self-directed learning and computer and internet efficacy. Students in the pre-clinical years showed a lower level of readiness in the technology availability domain compared to clinical students. The lowest score however was in the self-directed learning dimension regardless of the students’ year of studies.
Conclusion: The pandemic had created a paradigm shift in the delivery of the medical program which is likely to remain despite resumption of daily activities post-pandemic. Support for student readiness in transition from instructor-driven learning models to self-directed learning models is crucial and requires attention by institutions of higher learning. Exploring methods to improve self-directed learning and increase availability of technology and conducting sessions to improve computer and internet efficacy can be considered in the early stages of pre-clinical years to ensure equitable access for all students.
Keywords: Remote Learning, Student’s Readiness, Medical Education
I. INTRODUCTION
The COVID-19 pandemic and global emergency from the end of January 2020 had greatly affected the education sector, with many institutions including undergraduate medical schools converting to remote learning within a short timeframe.
Previous studies have shown that e-learning methods were effective and acceptable among medical undergraduate students (Chen et al., 2020). Studies have also suggested that students may struggle in adapting to a self-directed learning process (Vaughan, 2007), prefer traditional face-to-face lectures and possibly lacking the technological skills and infrastructure for a satisfactory remote learning experience.
It is important to determine the remote learning readiness of undergraduate medical students to facilitate the adaptation of these practices to maximise student competencies. Therefore, the primary objective of this study was to determine the readiness for remote learning in undergraduate medical students in a South-East Asian university and the secondary objective was to identify factors associated with their remote learning readiness.
II. METHODS
This was a cross-sectional quantitative study to measure medical students’ readiness towards remote learning using the BLREQ questionnaire. This study was approved by the Research Ethics Committee (Reference UM.TNC2/UMREC-889) of the university.
In the Covid-19 enforced scenario at that time, the physical face-to-face teaching in our institution was moved to online almost immediately, requiring the students to adapt their learning approaches rapidly to suit the needs of a virtual learning environment.
The duration of the study was one month, from the 19th of June to the 19th of July 2020. Our country implemented a national lockdown (and emergency remote learning) due to COVID-19 on the 18th of March 2020. Thus, data collection occurred in the first few months of the remote learning situation and represented students’ experiences and readiness during the early phase of the change.
The students were from all five years of study in the medical undergraduate program. They were contacted via their online educational platform and WhatsApp group chats with details of the study, participant’s consent form, link to the online self-administered questionnaire and weekly reminders to encourage participation. Participation was voluntary and consent was obtained from the students. Data were anonymised and not traceable to a particular individual.
This study utilised Section A and B of the BLREQ questionnaire which is a validated questionnaire on the readiness and engagement of students in blended learning (Adams et al., 2018). Although ‘Blended Learning’ is defined as a combination of e-learning (online) and traditional education (face-to-face) approaches, the BLREQ is appropriate for this study as it primarily measures students’ readiness for remote learning. Section A contained basic demographic questions (i.e., age, gender, year of study). Section B had 37 items in five dimensions which addressed various aspects of students’ readiness for remote learning. A 4-point Likert-type scale ranging from strongly disagree (1) to strongly agree (4) was provided with only one response allowed per item.
The data was analysed using IBM SPSS version 25. The data was non-normally distributed; hence the Mann-Whitney U test was used to test for significant difference in scores between gender and stages of study.
III. RESULTS
There were 329 complete responses out of 734 invited participants (44.8% response rate). Most respondents were aged between 20 to 24 years old (Mean=21.9; SD=1.8). Approximately 59% were female and 59% were clinical students.
The total dimension and individual item mean scores are reported in Table I with the highest and lowest scores of each dimension annotated. The dimensions of remote learning readiness arranged in descending order of total mean score are Technology Availability (3.61+50), Technology Skills (3.60+.43), Technology Usage (3.50+.44), Computer and Internet Efficacy (3.35+.49), and Self-directed Learning (3.03+.51) (Table 1). Research data of this study are available at https://doi.org/10.6084/m9.figshare.21443100
Analysed by gender, the mean scores of male students were significantly higher than female students in the dimensions of Self-directed Learning; 3.13 vs 2.96 (U=10354.5, z=-3.18, p=.001), and Computer and Internet Efficacy; 3.39 vs 3.32 (U=11332.5, z=-2.02, p=.044). Individual items in which male students scored significantly higher in each dimension were [SDL1], [SDL4], [CIE2] and [CIE3].
When comparing between stages of study, the mean score of clinical students was significantly higher than pre-clinical students only in the Technology Availability dimension; 3.65 vs 3.55 (U=11376.0, z=-2.13, p=.034) An individual item which clinical students scored significantly higher in Technology Availability dimension was [TA3].
|
Dimensions and items |
Mean |
SD |
|
[TS] Technology Skills dimension |
3.60 |
.43 |
|
[TS1] I know the basic functions of a computer/laptop and its peripherals like the printer, speaker, keyboard, mouse etc.** |
3.76 |
.45 |
|
[TS2] I know how to save and open documents from a hard disk or other removable storage device. |
3.67 |
.52 |
|
[TS3] I know how to open and send email with file attachments. |
3.72 |
.48 |
|
[TS4] I know how to log on to Wi-Fi |
3.74 |
.46 |
|
[TS5] I know how to navigate web pages (go to next or previous page). |
3.68 |
.50 |
|
[TS6] I know how to download files using browsers (e.g., Google Chrome, Internet Explorer, Firefox) and view them. |
3.67 |
.51 |
|
[TS7] I know how to access an online library or database.* |
3.19 |
.78 |
|
[TS8] I know how to use Word processing software (e.g., Microsoft (MS) Word). |
3.62 |
.53 |
|
[TS9] I know how to use Presentation software (e.g., MS PowerPoint). |
3.60 |
.53 |
|
[TS10] I know how to use Spreadsheet software (e.g., MS Excel). |
3.30 |
.75 |
|
[TS11] I know how to open several applications at the same time and move easily between them. |
3.60 |
.60 |
|
[TU] Technology Usage [TU] dimension |
3.50 |
.44 |
|
[TU1] I often use the internet to find information.** |
3.86 |
.37 |
|
[TU2] I often use e-mail to communicate.* |
2.93 |
.93 |
|
[TU3] I often use office software (e.g., MS Word, PowerPoint, Excel). |
3.62 |
.56 |
|
[TU4] I often use social networking sites to share information (e.g., Facebook, Twitter, Instagram, Snapchat). |
3.39 |
.83 |
|
[TU5] I often use instant messaging (e.g., WhatsApp, Viber, WeChat, Line, Telegram). |
3.72 |
.54 |
|
[TU6] I often use cloud-based file hosting services to store or share documents (e.g., Google Drive, Dropbox, One drive). |
3.44 |
.69 |
|
[TU7] I often use learning management systems (e.g., Blackboard, Moodle). |
3.28 |
.69 |
|
[TU8] I often use mobile technologies (e.g., Smartphone, Tablet) to communicate. |
3.72 |
.51 |
|
[TA] Technology Availability dimension |
3.61 |
.50 |
|
[TA1] I have a computer/laptop with an internet connection.** |
3.74 |
.53 |
|
[TA2] I have a computer/laptop with adequate software for learning (e.g., Microsoft (MS) Office). |
3.63 |
.57 |
|
[TA3] I have speakers for courses with video presentations.* |
3.50 |
.72 |
|
[TA4] I have a computer/laptop and its peripherals like the printer, speaker, keyboard, mouse etc. |
3.57 |
.66 |
|
[SDL] Self-directed Learning dimension |
3.03 |
.51 |
|
[SDL1] I am a highly independent learner. |
3.12 |
.69 |
|
[SDL2] I am able to learn new technologies.** |
3.60 |
.55 |
|
[SDL3] I do not need direct lectures to understand materials.* |
2.36 |
.92 |
|
[SDL4] I would describe myself as a self-starter in learning using technology. |
3.18 |
.79 |
|
[SDL5] I am not distracted by other online activities when learning online (e.g., Facebook, Gaming, Internet surfing). |
2.42 |
1.04 |
|
[SDL6] I can read the online instructional materials on the basis of my needs. |
3.49 |
.58 |
|
[CIE] Computer and Internet Efficacy dimension |
3.35 |
.49 |
|
[CIE1] I feel confident in using online tools (e.g., email, internet chat, instant messenger) to communicate effectively with others. |
3.48 |
.65 |
|
[CIE2] I feel confident in expressing myself (e.g., emotions and humour) in my university’s learning management systems (e.g., Blackboard, Moodle) |
2.89 |
.83 |
|
[CIE3] I feel confident in posting questions in online discussions.* |
2.87 |
.82 |
|
[CIE4] I feel confident in performing the basic functions of Word processing software (e.g., MS Word). |
3.59 |
.55 |
|
[CIE5] I feel confident in performing the basic functions of Presentation software (e.g., MS PowerPoint). |
3.48 |
.62 |
|
[CIE6] I feel confident in performing the basic functions of Spread sheet (e.g., MS Excel). |
3.26 |
.78 |
|
[CIE7] I feel confident in using web browsers (e.g., Google Chrome, Mozilla Firefox) to find or gather information for online learning.** |
3.67 |
.53 |
|
[CIE8] I feel confident in using computer or tablet or mobile phone for online learning. |
3.56 |
.63 |
Table 1. Dimension and individual item mean scores of student readiness to engage in remote learning
** highest score in the dimension
*lowest score in the dimension
IV. DISCUSSION
This study aimed to identify medical students’ readiness for remote learning across five dimensions and to identify factors associated with their readiness during the early months of the COVID-19 online learning transition period. Although there is significant resumption of usual activities post-COVID-19 pandemic, many of the online and self-directed components of learning are likely to remain as the way forward in the medical curriculum. Therefore, we feel that this study still has relevance currently.
All mean scores of the subscales Technology Availability (TA), Technology Skills (TS), Technology Usage (TU), Computer and Internet Efficacy (CIE) and Self-directed Learning (SDL), were above 3 on a scale of 1 to 4. The mean scores in our study were much higher and have less deviation than Adams et al’s study conducted in a similar setting before the COVID-19 pandemic, in which the five dimensions scored lower than 3.00, with SDL scoring the lowest mean in the other study at 1.25+1.55 (Adams et al., 2018). Adams et al’s study also did not show much difference when comparing between medicine, social science, science and engineering students (Adams et al., 2018), indicating that readiness for online learning was much lower overall pre-COVID-19.
Despite the increase compared to Adams et al’s study, SDL still scored the lowest in our study out of the five dimensions. An implication of this is that universities need to help learners transition from facilitator/ instructor-driven learning models to self-directed learning models. This can be done by making training in ‘learning to learn’ (L2L) an essential component of student support. In our setting, this training should address items which scored lowest in SDL as these indicate areas of struggle for students; [SDL3] and [SDL5]. It is also possible that some facilitators are not aware of what SDL is, therefore facilitators can also benefit from training for SDL methods.
Our study demonstrated significantly higher readiness for remote learning among male students in comparison to female students in the domains of SDL and CIE. While some studies indicate no gender differences in e-Learning readiness, other studies also report gender differences such as males having more positive attitudes toward online learning; males being more ready for online learning (Adams et al., 2018) and males using more learning strategies and having better technical skills than females (Alghamdi et al., 2020). In the CIE domain, males scored higher in the items [CIE2] and [CIE3] which are both related to communication through a virtual platform. This resulted in males scoring higher in the CIE domain in general. The gender disparity in remote learning readiness needs to be addressed as female students are increasingly the majority (and therefore primary stakeholders) in medical schools worldwide.
The mean score of clinical students was significantly higher than pre-clinical students only in the Technology Availability domain with clinical students reporting better hardware and infrastructure access compared to pre-clinical students. It is likely that as the learners progress through a course, they become more aware of the technological requirements of the course and invest in better devices and internet access. It is also possible that the students’ socioeconomic status at the beginning of their course may not have been good, for example if they were awaiting scholarships to be processed, which subsequently became available later in their course of study. This may have then enabled the students to purchase better hardware and infrastructure further on in their course, during the clinical years. However, this financial aspect was not included our study. It is still worth considering future programs early in the course, where there could be subsidies for students to purchase necessary technological equipment for their studies.
A. Limitations and Recommendations
One limitation of this study was that it looked at remote learning in general and did not look at clinical elements such as using online simulated patients for history taking classes, or procedural skills videos. The study also only looked at student perspectives, and not faculty perspectives to get a complete picture of the online learning experiences. Future studies should explore student readiness for clinical online learning as this would be a struggle for students even if the transition was under normal circumstances (Vaughan, 2007). The perspectives of faculty members on readiness to move towards online learning also need to be explored. The strength of this study was that it used a previously validated questionnaire which allowed some comparison on students’ remote learning readiness with pre-COVID-19 studies.
V. CONCLUSION
In conclusion, the study explored medical undergraduates’ remote learning readiness in a public medical school in Malaysia during the COVID-19 pandemic. In general, students were found to be ready for remote learning. However, the lowest scores were for the domain of self-directed learning and computer and internet efficacy. Based on our findings, we feel that support for student readiness in transition from instructor-driven learning models to self-directed learning models is crucial and requires attention by institutions of higher learning. Exploring methods to improve self-directed learning and increase availability of technology and conducting sessions to improve computer and internet efficacy can be considered in the early stages of pre-clinical years to ensure equitable access for all students. There should also be efforts to train the educators to develop online learning activities which incorporate the socio-relational aspects of learning into the remote learning experience.
Notes on Contributors
Kit Mun, Tan is the first author and person who initiated the study, contributed to the design of the study, data collection and analysis, writing and approval of the final version of the manuscript.
Chan Choong, Foong contributed to the design of study, data collection and analysis, writing and approval of the final version of the manuscript.
Donnie, Adams is the creator of the original Blended Learning Readiness Questionnaire (BLREQ) and contributed to the design of the study, data collection and analysis, writing and approval of the final version of the manuscript.
Wei Han, Hong contributed to the design of the study, data collection and analysis, writing and approval of the final version of the manuscript.
Yew Kong, Lee contributed to the design of the study, data collection and analysis, writing and approval of the final version of the manuscript.
Vinod, Pallath is the corresponding author and contributed to the design of the study, data collection and analysis, writing and approval of the final version of the manuscript.
Ethical Approval
This study received ethical approval from the Universiti Malaya Ethics Review Committee with the approval number of UM.TNC2/UMREC-889.
Data Availability
Research data of this study are available at https://doi.org/10.6084/m9.figshare.21443100.
Readers may access the anonymised data freely with the above URL. Kindly contact the authors for permission if you wish to use the data for a subsequent study or collaboration.
Acknowledgement
We would like to acknowledge and express gratitude to the undergraduate medical students who took the time to participate in this study.
Funding
There was no external funding for this study.
Declaration of Interest
All the authors do not have a conflict of interest to declare.
References
Adams, D., Sumintono, B., Mohamed, A., & Mohamad Noor, N. S. (2018). E-learning readiness among students of diverse backgrounds in a leading Malaysian higher education institution. Malaysian Journal of Learning and Instruction, 15(2), 227-256. https://doi.org/10.32890/mjli2018.15.2.9
Alghamdi, A., Karpinski, A. C., Lepp, A., & Barkley, J. (2020). Online and face-to-face classroom multitasking and academic performance: Moderated mediation with self-efficacy for self-regulated learning and gender. Computers in Human Behavior, 102, 214-222. https://doi.org/10.1016/j.chb.2019.08.018
Chen, J., Zhou, J., Wang, Y., Qi, G., Xia, C., Mo, G., & Zhang, Z. (2020). Blended learning in basic medical laboratory courses improves medical students’ abilities in self-learning, understanding, and problem solving. Advances in Physiology Education, 44(1), 9-14.
Vaughan, N. (2007). Perspectives on blended learning in higher education. International Journal on E-Learning, 6(1), 81-94. https://www.learntechlib.org/primary/p/6310/
*Associate Professor Dr Vinod Pallath
Medical Education Research and Development Unit,
Faculty of Medicine, Universiti Malaya,
50603 Kuala Lumpur
Email: vinodpallath@um.edu.my
Submitted: 9 February 2023
Accepted: 22 March 2023
Published online: 3 October, TAPS 2023, 8(4), 36-39
https://doi.org/10.29060/TAPS.2023-8-4/SC3000
Komson Wannasai1, Wisanu Rottuntikarn1, Atiporn Sae-ung2, Kwankamol Limsopatham2, Wiyada Dankai1
1Department of Pathology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 2Department of Parasitology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Abstract
Introduction: Global medical and healthcare education systems are increasingly adopting team-based learning (TBL). TBL is an interactive teaching programme for improving the performance, clinical knowledge, and communication skills of students. The aim of this study is to report the learning experience and satisfaction of participants with the TBL programme in the preclinical years of the Faculty of Medicine, Chiang Mai University.
Methods: Following the implementation of TBL in the academic year 2022, we asked 387 preclinical medical students, consisting of 222 Year 2 and 165 Year 3 medical students who attended the TBL class to voluntarily complete a self-assessment survey.
Results: Overall, 95.35% of the students were satisfied with the structure of the TBL course and agreed to attend the next TBL class. The overall satisfaction score was also high (4.44 ± 0.627). In addition, the students strongly agreed that the TBL programme improved their communication skills (4.50 ± 0.796), learning improvement (4.41 ± 0.781), and enthusiasm for learning (4.46 ± 0.795).
Conclusion: The survey findings indicated that students valued TBL-based learning since it enabled them to collaborate and embrace learning while perhaps enhancing their study abilities. However, since this is a pilot study, further investigations are warranted.
Keywords: Team-based Learning, Small Group Interaction, Medical Education, Implementation
I. INTRODUCTION
Team-based learning (TBL) is a form of small-group teaching which can improve student performance, clinical knowledge, and communication skills. It has been employed in medical and healthcare education in the US, Australia, Austria, Japan, South Korea, and Singapore (Burgess et al., 2014; Michaelsen & Sweet, 2008). Since 2000s, this model has been used in medical education to foster deep learning across a variety of subjects and educational contexts, benefiting teachers and helping academically weak and strong students achieve the same or better results than with conventional methods (Parmelee et al., 2012). In addition, it is more effective for engaging students than lecturing in a large class with few teachers (Burgess et al., 2020b).
The key elements of TBL include pre-class preparation to encourage self-study, teamwork, and instant feedback. These key elements promote active learning and critical thinking (Burgess et al., 2020a; Parmelee et al., 2012). The steps in TBL include pre-class preparation, individual readiness assurance test (iRAT), team readiness assurance test (tRAT), feedback, and team application (Burgess et al., 2014). In the tRAT and team application phase, students work in small groups to demonstrate the use of teamwork for problem-solving. Clinical problem-solving exercises by students lead to class discussions and instructor comments (Burgess et al., 2020a; Michaelsen & Sweet, 2008). The teacher’s feedback can help clarify students’ responses by discussing their answers. In the academic year 2022, TBL was implemented on second- and third-year medical students in the Faculty of Medicine, Chiang Mai University, and self-assessment questionnaires were used to assess students’ satisfaction with the TBL model. This research aims to examine the impact of team-based learning on whether or not students were able to build their own learning processes, as well as to measure student satisfaction with teaching and learning in the TBL paradigm in order to improve further TBL classrooms in the faculty.
II. METHODS
A. Sampling and Participants
In 2022, 387 pre-clinic medical students from Chiang Mai University’s Faculty of Medicine were studied (222 from Year 2 and 165 from Year 3). Year 2 medical students studied human skin and the connective tissue system, while Year 3 medical students studied human haematology. Each TBL class consisted of 50 teams of mixed-gender and grades. Each team contained five members.
B. Structure and Components of TBL
The TBL programme was first implemented in the 2022 academic year, covering preclinical academic Years 2 and 3 at the Faculty of Medicine, Chiang Mai University. The TBL structure comprised two major phases: pre-class and in-class. The TBL topics included automated haematology and venomous snakes for Year 3 medical students. The skin infection topic was selected for Year 2 medical students.
After TBL, the non-researcher academic team informed medical students about the study and sought volunteers to avoid a conflict of interest between the instructors and the medical students. The non-researchers urged students interested in the experiment to complete a Google Forms questionnaire outlining the study’s relevance, including an explanation of the topic, data gathering, and the pros and cons of participation. If participants agreed to answer the questionnaire, they could complete the Google Form to consent and submit the questionnaire, with their personal information remaining anonymous.
For validity, a questionnaire to explore students’ views on TBL was prepared via a literature study, student review (two students), peer review (faculty members from two departments), and expert opinion (a TBL expert). It also examined students’ perceptions of teams and their beliefs and values in collaboration. The outcomes of the different years of student were then compared.
C. Data Collection and Analysis
Upon completing the TBL class, participant students were invited to voluntarily take the self-assessment survey to explore their thoughts on the assertions made in the TBL literature. The questionnaire was in Thai and we used a five-point Likert scale (1 = strongly dissatisfied, 2 = unsatisfied, 3 = neither satisfied nor dissatisfied, 4 = satisfied, 5 = strongly satisfied). Students were asked about the preparation for the TBL class, including student material, classroom, teaching content, self-preparation, orientation programme, class material, and the overall programme. The self-assessment survey also asked about promoting self-understanding, including communication skills, learning improvement, and enthusiasm in learning using a five-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree).
The TBL self-assessment survey data were analysed according to mean and standard deviation (SD) using STATA version 16 (STATA Corp., Texas, USA). The Pearson’s Chi-square test was used to analyze the difference between second- and third-year medical students’ percentages of satisfaction or agreement in each aspect. Statistical significance was accepted at p < 0.05. The reliability of the questionnaire was calculated using Cronbach’s alpha.
III. RESULTS
In years 2 and 3, Cronbach’s alpha of the medical students’ questionnaire was 0.869. In total, 369/387 (95.35%) participants appreciated the course structure and agreed to attend the next TBL session. Students rated the TBL class 4.44 ± 0.627 on a five-point Likert scale, with 1 being severely dissatisfied and 5 very pleased. Students also liked the classroom (4.48 ± 0.738), TBL structure (4.41 ± 0.771), and self-preparation (4.28 ± 0.780). The orientation programme, instructional material, pre-recorded video, and handouts were also well-received. Most students (69.25%, 268/387) spent 1–2 days self-preparing before the TBL class, followed by 3–4 days (24.55%, 95/387) and 5–7 days (5.43%, 21/387), while 0.78% (3/387) did not self-prepare.
On a five-point Likert scale from 1 to 5, students assessed their self-understanding progress, stating that TBL increased their communication, learning, and enthusiasm (4.50 ± 0.796, 4.41 ± 0.781, 4.46 ± 0.795).
The student t-tests revealed no significant differences between students in years 2 and 3. Except time for preparation (Pearson’s Chi-square test; p < 0.005), medical students in years 2 and 3 had similar self-assessment survey scores. In addition, Year 3 medical students also scored better in enthusiasm for studying than Year 2 medical students in increasing self-understanding (Student t-test; p = 0.023) (Table 1).
|
|
Year 2 |
Year 3 |
p-value |
|
Student satisfaction towards the TBL class |
|||
|
Agree to attend the next TBL class: % (n) |
95.95% (213/222) |
94.55% (156/165) |
0.519 |
|
Classroom: mean (SD) |
4.49 (0.671) |
4.47 (0.823) |
0.903 |
|
TBL structure: mean (SD) |
4.38 (0.73) |
4.45 (0.822) |
0.377 |
|
Orientation programme: mean (SD) |
4.46 (0.628) |
4.40 (0.810) |
0.417 |
|
Teaching material: mean (SD) |
4.67 (0.568) |
4.56 (0.578) |
0.064 |
|
Student preparation time: mean (SD) |
4.20 (0.788) |
4.40 (0.755) |
0.012 |
|
Time for preparation: % (n) 1–2 days 3–4 days 5–7 days No preparation |
80.18% (178/222) 14.41% (32/222) 4.50% (10/222) 0.90% (2/222) |
54.55% (90/165) 38.18% (63/165) 6.67% (11/165) 0.61% (1/165) |
< 0.005 |
|
Promotion of learning skills |
|||
|
Communication skills: mean (SD) |
4.46 (0.734) |
4.56 (0.674) |
0.154 |
|
Understanding of the topics: mean (SD) |
4.36 (0.729) |
4.47 (0.845) |
0.180 |
|
Enthusiasm for learning: mean (SD) |
4.38 (0.797) |
4.56 (0.783) |
0.023 |
|
Cronbach’s alpha |
0.869 |
0.869 |
|
Table 1. Comparison between the satisfaction of medical students in years 2 and 3 towards the TBL class and agreement to the promotion of self-understanding
IV. DISCUSSION
TBL changes how students learn by encouraging them to become more accountable by preparing for the team assurance test and application exercise (Burgess et al., 2020a). Teacher-directed pre-class preparation for advanced tasks may involve reading textbooks, reference articles, or instructor-created material while the readiness assurance test enhances students’ enthusiasm for TBL (Parmelee et al., 2012). However, students may resist TBL or active learning because it varies from passive lecture-based learning. Teachers must be aware of this and advocate TBL-style learning to improve ability and encourage students to be more prepared. This research examines the attitudes of medical students towards the two courses post-TBL and provides valuable input on TBL strategies, regardless of the course schedule.
Student feedback can improve teaching and student satisfaction. Students agreed that TBL can improve communication, learning, and passion. Second-year medical students were less motivated than third-year (p = 0.023), implying they need to focus on the core content of the preclinical module rather than TBL preparation, while third years have more time management experience for pre-class self-study. Students liked the teaching material because, in addition to textbooks, the instructors prepared PowerPoint presentations, recorded VDOs, and documentation, allowing those with different learning styles to make the appropriate choice.
Interestingly, both classes found the TBL structure and location less satisfying, possibly because first-time students could not comprehend group activities. Students can further grasp the TBL framework and enjoy the structured process with a revamped instructional layout and additional classes. As for the classroom, the seat layout may prevent suitable group conversations, with a small-group or smart classroom being more appropriate for TBL.
The preparation time satisfaction results are significantly difference, with Year 2 students being considerably less satisfied than Year 3 (p = 0.012). Most second-year medical students spent one to two days planning, and third years one to four (p = 0.005), primarily because the third-year course was longer. Second-year medical students attended a two-week course on human skin and the connective tissue system with a TBL class in the second week, whereas third years took a five-week haematological system course with a TBL class in the fourth week. Both classes received course material on Mondays, while the TBL was on Fridays in the same week. Second-year medical students may need to study the basic science aspects and be unable to independently assess the pre-class material, whereas third-year students had more time. Accordingly, a TBL course should last at least three to four weeks to allow medical students to understand the basic TBL instructional material and independently assess it.
This study has limitations. The questionnaire was expert-evaluated without instructor facilitation. In addition, our study focused on students’ satisfaction with TBL, hence we didn’t include academic outcomes to prove the value of TBL.
V. CONCLUSION
The survey showed that students appreciated TBL-based learning since it helped them to work together and embrace learning, while potentially improving their study skills. A diversity of pre-class material allows students to choose learning tactics depending on their individual abilities. Students found the activity venue inadequate and classroom improvements would boost their satisfaction level.
Notes on Contributors
KW reviewed the literature, designed the study, analysed data, co-wrote the manuscript, critically reviewed and edited the manuscript, and then read it through prior to final approval.
WD reviewed the literature, analysed the data, co-wrote the manuscript, and critically reviewed and edited the manuscript.
WR gave critical feedback on the writing of the manuscript.
AS and KL provided scientific insight and advice, and critically reviewed and edited the manuscript.
Ethical Approval
This research was approved by the institutional ethics committee of the Faculty of Medicine at Chiang Mai University (Study code: PAT-2565-09243).
Data Availability
On reasonable request, the corresponding author will provide data to support the conclusions of this study. Due to privacy and ethical considerations, the data cannot be made public.
Acknowledgement
The authors wish to express their sincere appreciation to Ms. Naorn Sriwangdang for assisting with the preparation of the research proposal.
Funding
This study was supported by the Faculty of Medicine, Chiang Mai University, grant no. 062-2566.
Declaration of Interest
The authors confirm they have no potential conflicts of interest.
References
Burgess, A., Bleasel, J., Hickson, J., Guler, C., Kalman, E., & Haq, I. (2020a). Team-based learning replaces problem-based learning at a large medical school. BMC Medical Education, 20, Article 492. https://doi.org/10.1186/s12909-020-02362-4
Burgess, A., van Diggele, C., Roberts, C., & Mellis, C. (2020b). Team-based learning: Design, facilitation and participation. BMC Medical Education, 20(Suppl 2), Article 461. https://doi.org/10.1186/s12909-020-02287-y
Burgess, A. W., McGregor, D. M., & Mellis, C. M. (2014). Applying established guidelines to team-based learning programs in medical schools: A systematic review. Academic Medicine, 89(4), 678–688. https://doi.org/10.1097/ACM.0000000000000162
Michaelsen, L. K., & Sweet, M. (2008). The essential elements of team-based learning. New Directions for Teaching and Learning, 2008(116), 7–27. https://doi.org/10.1002/tl.330
Parmelee, D., Michaelsen, L. K., Cook, S., & Hudes, P. D. (2012). Team-based learning: A practical guide: AMEE Guide No. 65. Medical Teacher, 34(5), e275–e287. https://doi.org/10.3109/0142159X.2012.651179
*Komson Wannasai
Department of Pathology,
Faculty of Medicine,
Chiang Mai University,
110 Inthavaroros road, Sriphume
Meaung, Chiang Mai, 50200
+6653935442
Email: komson.wanna@gmail.com
Submitted: 11 September 2021
Accepted: 22 March 2023
Published online: 4 July, TAPS 2023, 8(3), 58-61
https://doi.org/10.29060/TAPS.2023-8-3/SC2694
Maria Isabel Atienza & Noel Atienza
San Beda University College of Medicine, Philippines
Abstract
Introduction: An evaluation of the online medical course was conducted to assess student readiness, engagement, and satisfaction at the San Beda University College of Medicine in Manila during the COVID-19 pandemic.
Methodology: A convergent mixed methods approach was done with a quantitative online survey and a qualitative thematic analysis of focus group discussions (FGD) with medical students. A total of 440 students participated in the survey while 20 students participated in the FGDs.
Results: The medical students were sufficiently equipped with computers and internet connections that allowed them to access the online medical course from their homes. The 5 themes identified during the study that were relevant to education were: Student readiness for online learning, Learning Management System (LMS) and internet connectivity, teaching and learning activities, the value of engagements, and teaching effectiveness of the faculty. The combined quantitative and qualitative analysis revealed vital issues that affect student learning. This included the need for students to interact with fellow students and to be engaged with their faculty. The issues that affect teaching included the need for continuing faculty training and management skills in delivering the full online course.
Conclusion: The success of online education rests heavily on the interactions of the students, the teachers, and the knowledge. Student interactions, managerial and skills training for the faculty, and providing students with a mix of synchronous and asynchronous activities are the most effective means to ensure the effective delivery of online medical courses.
Keywords: Medical Curricular Revision, Formative Evaluation, Student Engagement, Synchronous and Asynchronous Online Learning, Cognitive Overload
I. INTRODUCTION
The COVID-19 pandemic necessitated a shift to online teaching and a revision of the medical curriculum with synchronous and asynchronous online activities. Medical schools worldwide adapted teaching strategies utilising Video Conferencing and Learning Management Systems.
This program evaluation of the online medical course aimed to evaluate the effectiveness of instruction using the various components of online learning. The study centered on the perspectives of students using a mixed methods design (Fitzpatrick et al., 2011). The study focused on the interplay of digital capabilities, students’ perceptions and satisfaction with the interactions and engagements during the online course.
II. METHODS
The mixed methods research protocol was approved by the Institutional Ethics Board of San Beda University. The study utilised a convergent mixed method design with a quantitative online survey that was conducted on 440 respondent students representing each of the four-year levels of the medical school. Six focus group discussion (FGD) sessions were conducted on 20 students. All student participants provided a signed informed consent form to participate in the survey and in the FGDs. The 25-item online survey questionnaire included a 5-point Likert scale for items on readiness for the online course, overall satisfaction, and engagement. The online FGD sessions were conducted using an open-ended questionnaire guide on student capabilities for the online course, student satisfaction, and student engagement.
The FGD recordings were transcribed and subjected to thematic analysis to identify major themes. Quantitative and qualitative data were analysed simultaneously through a joint display of the two sets of results. A joint display using pillar integration was done to demonstrate the themes where the data corroborated or validated each other. The conceptual framework, data collection tools, the data results, and the pillar integration table are posted in a data repository file for this study can be accessed through a repository at: https://doi.org/10.6084/m9.figshare.16682569.v2 (Atienza & Atienza, 2021).
III. RESULTS
The survey revealed that students were adequately equipped with the necessary computers and smartphones needed to access the online course. Only 50% of the students were taking the online course from their homes within the same city as the medical school. While 72% encountered internet connectivity problems, 88% of students were successful in the use of the LMS and the videoconferencing platform to access the course and take online examinations.
Seventy-eight percent of students found online student-to-student and faculty-to-class interactions to be beneficial to student learning. Among the synchronous activities, 63% of students preferred live online lectures. Among the asynchronous activities, 52% of students preferred uploaded video lectures. Overall, around 52% of students experienced being overloaded with study requirements while 48% of students felt there was sufficient time for independent study.
The results of the survey and the thematic analysis of the FGDs were organised into themes and subthemes. These themes were generated from the integration of the quantitative and qualitative data. The schematic diagram (Figure 1) demonstrates how the themes are related to the effectiveness of learning based on the perspective of the students.
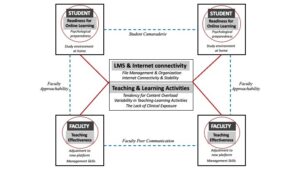
Figure 1. Schematic diagram of themes and subthemes identified in a mixed methods analysis of a fully online medical course at SBU-COM during the COVID pandemic
A. Student Readiness
The first theme that surfaced from the results was Student Readiness to engage in online learning. Students found their readiness to be dependent on two subthemes:
1) Study environment at home: Students expressed that the sudden shift to studying from home required that they designate sufficient time and space for studying. Students recognised that responsibilities at home and to the family could be distractions if not managed properly.
2) Psychological preparedness: The students also expressed the value of psychological preparedness as essential in dealing with stress and fatigue resulting from the unexpected shift to the online learning mode.
B. LMS and Internet Connectivity
The second theme highlights the importance of having computers and a stable internet connection as major determinants of student satisfaction with the online course. The introduction of an LMS for the medical course required immediate training for both the students and the faculty. While 81% of the students had the necessary gadgets and a good internet signal, 17% experienced major connection problems that disrupted up to 50% of live lectures and offline recorded videos. Student satisfaction with online learning was dependent on how timely and how organised the learning materials were uploaded into the LMS.
C. Teaching and Learning Activities
The third theme refers to the blend of online and offline activities for the different courses. The major subthemes included cognitive overload, variability of teaching and learning activities across courses, and the lack of clinical exposure.
1) Cognitive overload: Students had a perception of being overloaded by the volume of information delivered through the online course. The introduction of new forms of assessments such as video assignments, group reports, and research outputs contributed to the perceived cognitive overload.
2) Variability of teaching and learning activities: The variability in the blend of online and offline activities across the different courses required varying degrees of adjustments from the students. The students expressed their preference for live or recorded lectures over small group discussions and live laboratory demonstrations.
3) Lack of clinical exposure: Students in the 3rd and 4th year levels were apprehensive about the lack of clinical exposure in the actual medical environment due to the restrictions brought about by the pandemic. They recognise that they may not have the necessary skills training needed for internship.
D. The Value of Engagements
Unexpectedly, the fourth theme that students found important in the shift to online learning was the value of engagements.
1) Student-to-student online interactions: Up to 78% of students found support through interactions with other students. These interactions were useful not only for sharing the academic workload but also for mental and emotional support highlighting the value of student camaraderie despite being limited to virtual interactions.
2) Faculty-to-class interactions: Up to 80% of students expressed appreciation for the efforts of the faculty to get student feedback, answer clarificatory questions, and provide explanations when necessary. The students also expressed greater satisfaction with courses delivered online. Both faculty interactions with the class and with individual students were recognised as faculty approachability.
E. Teaching Effectiveness of The Faculty
The fifth theme Teaching pertains to the ability of the faculty to manage the online platform for teaching.
1) Faculty management skills: Teaching effectiveness is facilitated by the ease by which the faculty manages virtual teaching.
2) Faculty peer communication: Students recommend that the faculty within and across different courses coordinate their activities so that students can more easily manage their time and learning.
IV. DISCUSSION
The experience of delivering the medical course online has been very limited in the past. The teaching and learning strategies for medical courses to be delivered fully online require extensive preparation of the three main points in the transaction of learning: the learners, the teachers, and the course content. Learner readiness entails a clear delineation of the study environment in terms of time and space for study. Proper orientation to the online learning environment and psychological support should be made available to the students before the course begins. An inventory of the students’ computers and internet connectivity should also be done to ensure readiness for the course.
Delivering the course online necessitates faculty training on teaching and learning strategies for synchronous and asynchronous delivery as well as the proper navigation of the LMS and its available features. The faculty must maximise the benefits of technology as well as pedagogy in the online learning environment.
This study showed that in the shift of medical education to an online mode during the pandemic, student learning relies heavily on interactions between the learners, the teachers, and the course content. In an online course that relies so much on technology as a means of course delivery and integration, teaching and learning success depends on how well the interactions are established among these three points (Ifinedo & Rikala, 2019).
The design of courses must facilitate student-to-student interactions while faculty-to-class interactions using both synchronous and asynchronous activities would provide a good learning experience for students (Rhim & Han, 2020; Seymour-Walsh et al., 2020).
V. CONCLUSION
To succeed in the delivery of the online medical course, sufficient time must be given for faculty-to-student interactions during synchronous sessions and after the online classes. The faculty must demonstrate approachability by being open to continuing interactions with students outside the synchronous sessions. The coordination of faculty members within and across different courses must be enhanced to reflect efficiency in delivering their respective courses.
This study was performed during the early phase after the shift to full online delivery of the medical course. While the study is based on the perceptions of the students, the results of this study may be valuable in planning for continuing the online delivery of the medical course. The results of this study may be more robust with the inclusion of faculty perceptions and indicators of student academic performance.
Notes on Contributors
Dr. Maria Isabel Atienza conceptualised, designed, and implemented this study. She conducted the focus group discussions, prepared the thematic analysis, and wrote the manuscript for this study.
Dr. Noel Atienza helped in the design and conduct of the online survey and was involved in the data processing and data analysis of the survey. He was also involved in the preparation and editing of the final manuscript.
Ethical Approval
The research protocol SBU-REB # 2020-028 for this study was reviewed and approved by the San Beda University Research Ethics Board on November 28, 2020.
Data Availability
Data collection tools and research data are available and can be accessed by any interested reader through a repository at: https://doi.org/10.6084/m9.figshare.16682569.v2. The data in the repository may not be copied or cited without written permission from the authors.
Acknowledgment
The authors would like to acknowledge the support provided by the Alumni of San Beda and their commitment to promoting faculty research activities.
Funding
This study was funded by the Jesus P. Francisco Distinguished Professorial Chair Research Grant from the San Beda College Alumni Foundation, Inc.
Declaration of Interest
There are no conflicts of interest in this study.
References
Atienza, M., & Atienza, N. (2021). An online medical course during the COVID-19 pandemic: A mixed methods analysis. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.16682569.v2
Fitzpatrick, J., Sanders, J., & Worthen, B. (2011). Program evaluation: Alternative approaches and practical guidelines 4th Edition. Pearson Education, Inc.
Ifinedo, E., & Rikala, J. (2019). TPACK and educational interactions: Pillars of successful technology integration. World Conference on E-Learning. Association for the Advancement of Computing in Education, 295-305. https://www.learntechlib.org/primary/p/211094/
Rhim, H., & Han, H. (2020). Teaching online: Foundational concepts of online learning and practical guidelines. Korean Journal of Medical Education, 32(3), 175-183. https://doi.org/10.3946/kjme.2020.171
Seymour-Walsh, A., Bell, A., Weber, A., & Smith, T. (2020). Adapting to a new reality: COVID-19 coronavirus and online education in the health professions. Rural and Remote Health, 20, 6000. https://doi.org/10.22605/RRH6000
*Maria Isabel Maniego Atienza
San Beda University, Mendiola Street,
Barangay San Miguel,
City of Manila, Philippines
+639178668751
Email: mimatienza@yahoo.com
Submitted: 15 August 2022
Accepted: 20 December 2022
Published online: 4 July, TAPS 2023, 8(3), 54-57
https://doi.org/10.29060/TAPS.2023-8-3/SC2867
Seow Chong Lee & Foong May Yeong
Department of Biochemistry, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: In the first weeks of medical school, students learn fundamental cell biology in a series of lectures taught by five lecturers, followed by a mass tutorial session. In this exploratory study, we examined students’ perceptions of the mass tutorial session over two academic years to find out if they viewed the tutorials differently after minor tweaks were introduced.
Methods: Reflective questions were posted to the undergraduate Year 1 Medical students at the end of each mass tutorial session in 2019 and 2020. Content analysis was conducted on students’ anonymous responses, using each response as the unit of analysis. The responses were categorised under the learning objectives, with responses coded under multiple categories where appropriate. The distribution of the counts from responses in 2019 and 2020 was compared, and the tutorial slides used over the two years were reviewed in conjunction with students’ perceptions to identify changes.
Results: In 2019, we collected 122 responses which coded into 127 unique counts, while in 2020, 119 responses coded into 143 unique counts. Compared to 2019, we noted increases in the percentage of counts under “Link concepts” and “Apply knowledge”, with concomitant decreases in percentage of counts in “Recall contents”. We also found that the 2020 tutorial contained additional slides, including a summary slide and lecture slides in their explanations of answers to the tutorial questions.
Conclusion: Minor tweaks in the tutorial presentation could improve students’ perceptions of our mass tutorials.
Keywords: Mass Tutorials, Students’ Reflections, Apply Knowledge, Link Concepts, Minor Tweaks
I. INTRODUCTION
In the first few weeks of medical school, students learn about cell biology which is fundamental to what they need to know about tissues, organs, and the whole body in a series of lectures co-taught by five lecturers. In the lectures, efforts are made to highlight basic cellular processes, and illustrate how these are inter-connected in a cell. Where appropriate, how knowledge in the biomedical sciences underpins applications in clinical settings is also illustrated by the lecturers. At the end of the series of lectures, the lecturers will co-facilitate a mass tutorial session aimed at summing up the topics.
The mass tutorial session has several learning objectives. These include basic levels of learning such as recalling concepts, preparing for assessments, and building knowledge on topics, to higher levels of learning such as applying concepts to solve real life problems, and linking concepts between topics. Being the only teaching and learning activity that all lecturers co-teach, the mass tutorial provides the best opportunity to demonstrate links and apply the consolidated knowledge learnt during the different lectures.
Once the teaching and learning activities are completed, the coordinator of the lectures Foong May Yeong (YFM) reviews the curriculum to ensure that the teaching and learning activities delivered the intended learning objectives. Such reviews include students’ experiences of the curriculum (Erickson et al., 2008), which the coordinator (YFM) routinely collect through posting reflective questions at the end of the tutorial. In this exploratory study, we analysed students’ reflections from 2019 and 2020, and categorised them under different learning objectives of the tutorial. We noted an increase in percentage counts under “Apply knowledge” and “Link concepts” in 2020 compared to 2019. A review of the tutorial slides revealed the addition of summary and lecture slides in 2020. Our results suggest that minor tweaks to the tutorial presentation are sufficient to help students see the intended usefulness and relevance of tutorials.
II. METHODS
A. Format of Mass Tutorials
The mass tutorial was conducted after completion of the cell lectures. For 2019, this was a face-to-face session. For 2020, due to the COVID-19 pandemic, the tutorial was conducted online via Microsoft Teams. The class size was 281 for 2019, and 280 for 2020. Four out of five lecturers taught the same topics for both years. For both years, during the mass tutorial, each lecturer used Poll Everywhere to pose a mix of five to six recall and application questions linked to their topic. Identical questions were used in 2019 and 2020. Students discussed among themselves before answering these questions. The class responses were then revealed, after which the lecturer explained the solutions to their questions. The cycle was repeated until all the lecturers completed their parts.
B. Collection of Student Reflections
After each tutorial, the coordinator (YFM) posted two reflection questions on Poll Everywhere. The two questions were: 1. “What were the key points you learned in this session?”, 2. “Any questions?”. Answering these reflection questions were voluntary and anonymous. A waiver of informed consent was approved by Yong Loo Lin School of Medicine Medical Sciences Departmental Ethics Review Committee. The responses to question 1 obtained from students in 2019 and 2020 were analysed in this study.
C. Content Analysis
The responses to question 1 were coded and categorized into the different learning objectives of the mass tutorial, using each response as a unit of analysis. Each response could be coded into multiple categories when appropriate. The counts under each category were represented as a percentage of all counts coded from the responses. The tutorial slides used in 2019 and 2020 were also reviewed to understand students’ perceptions.
III. RESULTS
In 2019, we collected 122 responses which were coded into 127 unique counts. In 2020, we collected 119 responses which were coded into 143 unique counts. The number of responses and unique counts coded were largely similar between the two years. The unique counts were categorised into the five learning objectives and their percentage counts were presented in Figure 1. Supplemental data containing an overview of the categories and samples of students’ responses, as well as the counts under each category, are openly available in Tables 1 and 2 shared at Figshare at http://doi.org/10.6084/m9.figshare.20484498 (Lee & Yeong, 2022). The distribution of the counts differed between the two years. In 2019, majority of the counts were categorized to “Recall contents” (37.0%), with low numbers categorized as “Apply knowledge” and “Link concepts” (15.0% and 3.1% respectively). In comparison, in 2020, we observed a decrease in percentage of counts in “Recall contents” (to 21.0%), with an increased percentage in counts in “Apply knowledge” and “Link concepts” (to 22.4% and 15.4% respectively). Overall, there is a shift in distribution of counts, from a skewed distribution in 2019, to an even distribution in 2020.
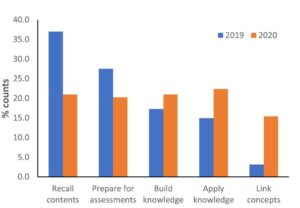
Figure 1. Categorisation of students’ responses into the learning objectives
Given that tutorial questions used in the two years were largely identical, we reviewed the tutorial slides used in these two years to look for possible differences. In 2020, firstly, a summary slide detailing the different aspects of the cell was added to the start of the tutorial slides. Secondly, lecture slides were included in the tutorial slides to explain the answers to the tutorial questions. The lecture slides could come from the lecturer teaching the topic of interest, or from other lecturers if connections across topics were important. These additions could have altered students’ perceptions of the mass tutorial session in 2020.
IV. DISCUSSION
In this study, we examined students’ reflections collected across two academic years to understand their perceptions of the mass tutorial sessions that capped the teaching of cell biology. One of the intentions of the lecturers when designing the tutorial questions was to demonstrate links across topics, and illustrate how questions can be solved using connections across topics. The decrease in percentage of counts under “Recall contents” in 2020 suggested an increase in students’ awareness of the usefulness and relevance of the tutorial sessions when minor changes were made in the presentation of the overview of the cell biology topic and the answers to the tutorial questions.
Both lecture and summary slides likely promoted links in different ways. The lecture slides represent theoretical knowledge for each topic, and also add visuals to the explanations of tutorial questions. Inclusion of lecture slides allow students to use both visual and audio channels to process the explanations, instead of using only the audio channel to listen to explanations when they were delivered verbally without visuals (Mayer, 2014). Using both channels could lower the cognitive load for students to learn and construct meaningful frameworks to solve problems. Summary slides juxtaposed different topics within a slide, allowing students to visualize connections between topics in the proper functioning of a cell (Bae & Watson, 2014). Adding these slides require little effort from the lecturers as the slides are readily available. Such small changes in improving the instructional approach could result in improvements in student learning (Lang, 2016).
There are several limitations to our study. Firstly, we only reviewed the tutorial slides, which covers part of the enacted curriculum. Secondly, the tutorial in 2019 was conducted face-to-face while the one in 2020 was conducted online. Online learning normally is not something students view positively, hence the improvements in student perceptions was surprising. Students prefer the social aspects of learning, which is abundant in face-to-face learning but greatly diminished in online learning (Siah et al., 2022). However, the diminished opportunities for peer-learning in online environment might contribute to increased attention diverted to lecturers for explanations.
V. CONCLUSION
Surveying and analysing students’ reflections at the end of mass tutorial proved to be informative in evaluating and improving our tutorials. In our preliminary analysis, a change in students’ perceptions of the tutorial from recalling of concepts to application of knowledge and linking concepts corresponded to minor tweaks in our tutorial presentation slides. Such minor tweaks, requiring little time, but yet are effective in helping students see the usefulness and relevance of tutorials, is an approach that even busy academics can do.
Notes on Contributors
Seow Chong Lee contributed to the analysis and interpretation of data, drafting and revising of the manuscript.
Foong May Yeong contributed to the conception and design of the study, interpretation of data, drafting and revising of the manuscript.
Ethical Approval
Ethics approval was obtained from Yong Loo Lin School of Medicine Medical Sciences Departmental Ethics Review Committee (Reference code: MSDERC-2022-006).
Data Availability
An overview of the categorization of responses into categories and samples of students’ responses, as well as the counts under each category are openly available in Figshare at https://doi.org/10.6084/m9.figshare.20484498.
Funding
This paper receives no funding from outside sources.
Declaration of Interest
The authors have no conflict of interest to declare.
References
Bae, J., & Watson, B. (2014). Toward a better understanding and application of the principles of visual communication. In W. Huang (Ed.), Handbook of Human Centric Visualization (pp. 179-201). Springer. https://doi.org/10.1007/978-1-4614-7485-2_7
Erickson, F., Bagrodia, R., Gook-Sather, A., Espinoza, M., Jurow, S., Shultz, J. J., & Spencer, J. (2008). Students’ experience of school curriculum: the everyday circumstances of granting and withholding assent to learn. In F. M. Connelly, M. F. He, & J. Phillion. (Eds.), The SAGE Handbook of Curriculum and Instruction (pp. 198-218). https://doi.org/10.4135/9781412976572.n10
Lang, J. M. (2016). Small Teaching: Everyday Lessons from the Science of Learning (1st ed.). Jossey-Bass.
Lee, S. C., & Yeong, F. M. (2022). Minor tweaks to tutorial presentation improved students’ perceptions of our mass tutorial. https://doi.org/10.6084/m9.figshare.20484498
Mayer, R. E. (2014). Multimedia instruction. In M. Spector, D. Merrill, J. Elen, & M. J. Bishop (Eds.), Handbook of Research on Educational Communications and Technology (pp. 385-399). https://doi.org/10.1007/978-1-4614-3185-5_31
Siah, C. R., Huang, C. M., Poon, Y. S. R., & Koh, S. S. (2022). Nursing students’ perceptions of online learning and its impact on knowledge level. Nurse Education Today, 112, Article 105327. https://doi.org/10.1016/j.nedt.2022.105327
*Foong May Yeong
MD4, 5 Science Drive 2,
S117545
+65 6516 8866
Email: bchyfm@nus.edu.sg
Submitted: 28 April 2022
Accepted: 9 February 2023
Published online: 4 July, TAPS 2023, 8(3), 50-53
https://doi.org/10.29060/TAPS.2023-8-3/SC2798
Olivia MY Ngan1,2, Jasmine YN Hui3 & Sihan Sun4
1Medical Ethics and Humanities Unit, School of Clinical Medicine, LKS Faculty of Medicine, The University of Hong Kong, HKSAR; 2Centre for Medical Ethics and Law, Faculty of Law and LKS School of Medicine, The University of Hong Kong; 3Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR; 4CUHK Centre for Bioethics, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR
Abstract
Introduction: Didactic pedagogy and passive learning in bioethics and medical humanities teaching are ineffective in engaging students and gauging learning interests. As a result, medical students are unaware of why and how bioethics and medical humanities relate to their learning and thus prioritising acquiring clinical knowledge in their medical education.
Methods: This project involves a teacher-student collaboration to develop a teaching approach, which bridges historical events and contemporary issues, acknowledging how ethics and humanities are interwoven in clinical and everyday life. The objectives are to (1) highlight landmark historical events in bioethics and medical humanities and (2) recognise the evolving nature of values and social norms that inform current practice.
Results: The three activities include the use of historical narratives, annual newsletter publications, and social media to augment didactic classroom teaching and learning. Video narratives of landmark events in bioethics were developed to strengthen historical knowledge and encourage self-reflection. The newsletter invited students to write about any topic in bioethics and medical humanities and enabled them to experience a peer-review process. It allowed students to critically appraise everyday issues. Social media engagement via Instagram offered a flexible and informal medium to diversify the traditional bioethics content taught in the classroom. The advantages and obstacles of each element are discussed.
Conclusion: A holistic approach using historical narratives, newsletters, and social media engages students’ learning and allows students to become conscious of how past events shape the present.
Keywords: Bioethics, Medical Ethics, Medical Humanities, Education, History, Curriculum Development, Social Media, Student as Partner, Newsletter
I. INTRODUCTION
With modern bioethics taking shape in the late 1960s, the introduction of formal bioethics teaching in medical schools developed slowly in Europe and Northern America over the subsequent decades. It was recognised that professional ability not only encompassed scientific knowledge and clinical skills, but also embodied a high standard of professional ethics, values, and moral conduct. A paradigm shift in how medical education shaped students’ moral compasses and holistic decision-making abilities was needed. In 1987, the Liaison Committee on Medical Education stated that medical schools must incorporate bioethics and medical humanities teaching into their curricula (Carrese et al., 2015). In 1993, the British General Medical Council published a white paper, Tomorrow’s Doctors, which outlined a blueprint for reforming the curriculum and affirmed that teaching ethics and law was an integral part of medical education (Mattick & Bligh, 2006).
Bioethics teaching started relatively late in Asia-Pacific and is strategically less developed in its teaching content, methodology, and assessment (Qian et al., 2018; Sim et al., 2019). There is little discussion on how to best deliver bioethics education through a multidisciplinary lens, as the disciplines of humanities (e.g., philosophy, history, and law), social sciences (e.g., anthropology and sociology), and arts (e.g., literature) are extensive. Our team recognised that passive learning using conventional pedagogy (e.g., didactic lectures and tutorials) had significant drawbacks. Earlier studies showed that teachers adopting these methods struggled to engage and stimulate students’ reception to ethics learning (Ganguly et al., 2022; Ngan & Sim, 2021). They were unaware of why and how bioethics and medical humanities were related to their science background, called them “soft” subject, and thus prioritised acquiring clinical knowledge (Leo & Eagen, 2008).
This paper describes a new teaching approach that draws reference from the philosophy of history teaching, using the past to understand and predict present and future actions. We describe three activities, including using historical narratives, annual newsletter publications, and social media to augment classroom teaching and learning in hopes of promoting ethical sensitivity to students’ clinical and everyday life experiences. Our learners are medical students undertaking a six-year undergraduate medical degree programme. These activities were implemented to support pre-clinical year teaching, though also applicable to clinical year students.
II. DESCRIPTIONS OF THREE TEACHING ACTIVITIES
A. Historical Narratives
The adoption of historical narratives in bioethics teaching draws reference from the philosophy of history teaching, using the past to appreciate the present and the future. But its history is often neglected in the curriculum due to time constraints. Students perceived a disconnection between themselves and unethical events, struggling to understand the significance and effects specific past events may have had on present society (Ngan & Sim, 2021). Gerald L. Gutek (1995), History Educator, advocated that “[teaching] should illuminate the past in order to provide the perspective in time and place that we need to make reflective decisions on the [medical] education choices that face us today. Understanding the importance of bioethics history reminds ourselves about the wrongdoings in science, either due to procedural insensitivity or limited guidelines, and may also improve individual behaviour and organisational culture, re-enforcing a high standard of professional conduct. The video narratives reinforce historical knowledge and the ability to discern and scrutinize the similarities and differences between the past and present.
In this pilot project supported by the faculty’s teaching development grant, landmark historical events were developed as short video narratives that complemented the teaching curriculum topic. Table 1 is a non-exhaustive list of examples describing key events in ethics and how they relate to contemporary issues. In our experience, the video productions were well-received by students’ feedback evaluation. The high cost, however, would be a concern. Should the video improve students’ sensitivity towards bioethics, a comprehensive development of bioethics history video should be invested as an educational media to support teaching.
|
Historical Events |
Related Ethical Concerns |
Contemporary Issues |
|
Eugenics measures in the United States (1896- 1940), Germany (1933-45), and Japan (1948-1996) |
Eugenics |
Emerging technologies (e.g., gene-editing technologies, preimplantation diagnosis, and prenatal diagnosis) |
|
The “God” Committee: Rationing dialysis machines (1961) |
Equity, fair allocation approach, transplantation ethics |
Allocation of scarce resources (e.g., vaccine, ICU bed, funds) |
|
Tuskegee Syphilis Study, (1972) |
Research ethics (e.g., informed consent, exploitation of vulnerable populations) |
Research involving vulnerable populations (e.g., homeless, inmates) |
|
Stanford Prison Experiment (1971)
Milgram’s “destructive obedience” Study (1974) |
Unethical research conduct was uncovered (e.g., psychological harms, deception) |
Social and behaviour research illuminates the need for participant protection beyond the scope of biomedical studies. |
|
Table 1. Implications of Landmark Events on Present-day |
||
B. Bioethics Newsletter
In this pilot project, our team incepted a student-led bioethics newsletter aiming to draw ethical sensitivity in everyday life. Medical students were invited to contribute and write a commentary based on a topical issue of their interest; stimuli may have ranged from the news, movies, dramas, documentaries, plays, clinical ward experiences, and overseas observations. The opportunity provided students with a platform to voice and elucidate their opinions. It also allowed students to be more receptive to opposing ideas, developing a greater awareness of ethical dilemmas.
We published three annual newsletters and reflected on our experience. In the first issue, there was no peer-review process. We felt that the absence of a communication medium between the student writers and student editors hindered the quality of submissions. A peer-review process was implemented starting from the second issue, which was perceived to be beneficial as students were able to receive feedback and enhance intellectual rigour. More importantly, students were also exposed to the peer-reviewing process, which is useful for their future professional career development in academia.
Several obstacles relating to the submission process and the future sustainability of the newsletter were also met. In the first issue, interest was generated primarily through word-of-mouth and promotion on social media. In the second issue, prize incentives were given to best-written submissions. Participation gained momentum in the second and third issues, where we saw an average of 15-20 submissions. Sustainability was also a concern in terms of reader engagement and recruiting altruistic junior students to take over the project. To encourage multidisciplinary engagement, we aim to call for submissions in both written Chinese and English and accept entries from all students within the medicine faculty. We have a long-term goal of fostering a multidisciplinary collaboration across the Faculties.
C. Social Media
Given the generational influx of physicians and medical educators, the use of social media in medical education has seen rising popularity in recent years. Platforms like Twitter, Instagram, YouTube, and LinkedIn are easily accessible, user-friendly and encourage users’ interaction in a local and international setting. The flexibility of social media may also promote active learning pedagogies and personalised education, allowing students to build upon the knowledge they perceive to be interesting.
We started an Instagram page (IG: cubioethics) in June 2020 and curated content on a monthly basis. Content covered a broad range of bioethical topics, including several themed series: a news roundup named “Ethics in the News” and a series based on biotechnology seen in the sci-fi television series, Black Mirror. Each post consisted of a short synopsis on the topic and multiple discussion points were raised to incite critical thinking and reflection.
The flexibility and informal nature of Instagram allowed us to diversify the traditional bioethics content taught in the classroom. For example, it offered an experimental opportunity to teach through television and film. Moreover, the Instagram page allowed us to connect with students and professionals from local and international institutes. Engagement was reflected in post shares, likes, comments, and page follows. As the bioethics community on Instagram remains relatively small, it was easy to establish rapport. This community was able to help expand our audience via mutual post sharing and furthered the ethical debate raised in our posts.
Maintaining an Instagram page was not easy – content creation, the design process, and engaging with readers required careful planning and time. Also, from a cultural standpoint, it seemed as if there was a stronger tendency for international users to publicly participate in the conversation by commenting rather than local students. This may be due to worries about online criticism or the pervasive nature of social media and how it may no longer be viewed as a “safe space” for controversial discourse.
III. CONCLUSION
We reflected on our experience refining traditional didactic pedagogy by adopting three activities: historical narratives, newsletters, and social media. Each component presents unique educational benefits (e.g., recounting the evolution of today’s achievements, exposing students to peer-review publishing experience, cultivating sensitivities to everyday life) and operational barriers (e.g., budget constraints, altruistic students’ recruitment, time- and labour-intensive). Our teaching pedagogy may also be adopted in bioethics teaching in other disciplines, including biomedical and life sciences.
Notes on Contributors
OMYN conceived the study, developed the narration scripts, facilitated the newsletter peer-review as a teacher editor, reviewed the literature, and drafted the intellectual content of the manuscript.
JYNH led the newsletter peer-review as a student editor, managed the social media platform, and drafted the intellectual content of the manuscript.
SS reviewed newsletter entries and critically revised the manuscript for intellectual content. All authors are accountable for all aspects of the work and approve the final manuscript.
Ethical Approval
This study involves a theoretical discussion only and does not require ethical approval.
Data Availability
The data that support the findings of this study are openly available in the Figshare repository. http://doi.org/10.6084/m9.figshare.19768264
Funding
The study is supported by the Teaching Development and Language Enhancement Grant (TDLEG) for the 2019-22 Triennium. The funders had no role in the content review of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Carrese, J. A., Malek, J., Watson, K., Lehmann, L. S., Green, M. J., McCullough, L. B., Geller, G., Braddock III, C. H., & Doukas, D. J. (2015). The essential role of medical ethics education in achieving professionalism: The Romanell Report. Academic Medicine, 90(6), 744–752. http://doi.org/10.1097/ACM.0000000000000715
Ganguly, B., D’Souza, R., & Nunes, R. (2022). Challenges in the teaching–learning process of the newly implemented module on bioethics in the undergraduate medical curriculum in India. Asian Bioethics Review. https://doi.org/10.1007/s41649-022-00225-2
Gutek, G. L. (1995). A history of the western educational experience (2nd ed.). Waveland Press, Inc.
Leo, T., & Eagen, K. (2008). Professionalism education: The medical student response. Perspectives in Biology and Medicine, 51(4), 508–516. https://doi.org/10.1353/pbm.0.0058
Mattick, K., & Bligh, J. (2006). Teaching and assessing medical ethics: Where are we now? Journal of Medical Ethics, 32(3), 181–185. http://doi.org/10.1136/jme.2005.014597
Ngan, O. M. Y., & Sim, J. H. (2021). Evolution of bioethics education in the medical programme: A tale of two medical schools. International Journal of Ethics Education, 6, 37–50. https://doi.org/10.1007/s40889-020-00112-0
Qian, Y., Han, Q., Yuan, W., & Fan, C. (2018). Insights into medical humanities education in China and the West. Journal of International Medical Research, 46(9), 3507–3517.
Sim, J. H., Ngan, O. M. Y., & Ng, H. K. (2019). Bioethics education in the medical programme among Malaysian medical schools: Where are we now? Journal of Medical Education and Curricular Development, 6.
*Olivia M.Y Ngan
Medical Ethics and Humanities Unit,
School of Clinical Medicine,
Li Ka Shing Faculty of Medicine,
The University of Hong Kong, Pokfulam,
Hong Kong Island, Hong Kong SAR
Email: olivian1@hku.hk
Submitted: 30 Nov 2022
Accepted: 30 Jan 2023
Published online: 4 July, TAPS 2023, 8(3), 45-49
https://doi.org/10.29060/TAPS.2023-8-3/SC2921
Sasikala Devi Amirthalingam1, Shamala Ramasamy2 & Sharifah Sulaiha Hj Syed Aznal3
1Department of Family Medicine, International Medical University, Kuala Lumpur, Malaysia; 2Department for Psychology, International Medical University, Kuala Lumpur, Malaysia; 3Department of Obstetrics and Gynaecology, International Medical University, Kuala Lumpur, Malaysia
Abstract
Introduction: Introduction to Health Profession (IHP) was designed to teach first-year medical students the importance of self-directed learning, accountability, and teamwork in healthcare. Due to the COVID 19 pandemic, the course was delivered virtually, incorporating elements of gamification.
Methods: Gamification features included collaborative teamwork to simulate and record the roleplay for assignments based on crisis management scenarios. The syllabus involves knowledge checks to promote self-directed learning and personal accountability as well as online questionnaires to identify personality traits followed by discussion. Games like Chinese whispers and charades were introduced to identify listening skills. Additional gamification features include progress mechanics for collecting badges upon successful completion of knowledge checks / assessments and completing collaborative teamwork activities.
Results: Results from the descriptive study on the educational usefulness of the IHP module was found to be satisfactory. The feedback was encouraging as >95% of students gave positive feedback that the IHP activities enabled them to understand the value of teamwork, effective communication, professional behavior and enabled them to be resilient and adaptable. 92% agreed that the IHP activities helped to make connections and network with their peers during the pandemic
Conclusion: Gamification of IHP course was successful in terms of practicality and usefulness in promoting communication, collaborative work, experiential learning, and teamwork. Students were empowered to take charge of their own learning of both content and development of interpersonal skills and teamwork through gamification. The isolation caused by the pandemic was alleviated by the networking that occurred during collaborative group activities.
Keywords: Gamification, Self-directed Learning, Collaborative Learning
I. INTRODUCTION
Introduction to Health Profession (IHP) course was initiated during Covid-19 pandemic and conducted at the beginning of our medical program enrolment to introduce freshmen to the real world and value systems of health professional. The learning activities were designed to provide real life experiences, exposing to communication skills within the community and peers, professionalism including teamwork and ethics, and the value of self-reflecting practice. The isolation caused by the pandemic was alleviated by networking that occurred during collaborative group activities and online interactive discussion with invited speakers of health professionals. The group activities were gamified to make learning fun, memorable, engaging and motivating. It is designed to promote a sense of accomplishment while learning through discovery and during the social interaction.
Gamification in education has existed since time immemorial but with the advent of wireless technology, it has given rise to unique ways to improve student engagement (Dodson, 2021) in learning. Gamification is defined as “the craft of deriving all the fun and addicting elements found in games and applying them to real-world or productive activities” (Chou, 2012). There is growing evidence for gamification in a wider pedagogical context and the concept is gaining traction within the medical education community. These “fun and addicting elements” include progress mechanics such as badges, narrative structure and immediate feedback. The gamification features introduced in the IHP module are badges, immediate feedback, challenges in the form of knowledge checks and roleplay in virtual reality in crisis management scenarios.
II. METHODS
Collaborative group activities were conducted by dividing 171 first year students into 16 small groups. Activities were carried out using synchronous and asynchronous virtual platforms to accommodate about 40 % of international students who were still in their home countries. Lessons in IHP consisted of recognising personality traits, application of communication skills, ethics and professionalism and recognising teamwork as intrinsic requirements for delivery of effective healthcare.
Asynchronous sessions required students to individually go through the prepared learning materials followed by knowledge checks. Test repetition without penalty is allowed within an allotted time frame until learners reach a satisfactory result. Following successful completion of knowledge check, students would earn their badge of completion.
Activities like ‘discovering personality traits’ are conducted as online synchronous workshops and facilitated by a group of psychologists. Self-administered questionnaire was administered to determine personality traits, followed by a psychologist-led group discussion to share feedback and reflection. Having the session on a virtual platform provided the students with a degree of anonymity, which enabled them to share profound reflections and feedback. Through the questionnaire responses, the psychologists were able to identify red flags and reach out to the students.
During the online ‘communication skills’ workshop, games such as Chinese whispers and charades were used to cultivate active listening skills and understand nonverbal communication. Students were assigned to group works comprising of preparing oral presentations on scenarios involving ethics and professionalism. In addition, they were tasked to solve issues in selected crisis management scenarios using role-plays and virtual reality. Creativity is highly encouraged and weighted with high percentage. This encourages social interaction and influences learning by creating a subjective sense of presence to facilitate virtual experiential learning.
Upon completion of the IHP activities, students are required to complete a self-administered questionnaire to feedback on the efficacy of the module, hence implied consent is given. The questionnaire measured whether the gamification of IHP achieved the learning outcomes of enabling the understanding of the value of teamwork, effective communication, professional behaviour and to be adaptable and resilient. In addition, the questionnaire inquired if participation in IHP activities helped them create contacts and network with their peers. Open comments are sought after for thematic analysis.
III. RESULTS
51.4% of the cohort responded to the self-administered online questionnaire. Feedback was encouraging as >95% of students gave positive feedback. They felt IHP activities enabled them to understand the value of teamwork, effective communication, professional behaviour and being resilient and adaptable. Most agreed IHP activities helped to make connections and network with peers during the pandemic. Many agreed they developed some insight about themselves during IHP activities. Several themes were drawn from the collected feedback. The primary theme is teamwork where students demonstrate co-operation in working together in teams to attain mutual goals and learn leadership qualities. Majority felt they developed skills in active listening, organisation, patience, self-confidence, and showing empathy. Other characteristics learnt were resilience building, controlling emotions, adaptation, overcoming challenges, professionalism and ethical behaviour.
Common comments on areas to improve are their lack of confidence and discomfort in expressing one’s thoughts. Both being too rigid and overly flexible were commented. Other comments were not feeling at ease with working in a team, becoming overwhelmed, paying excessive attention to detail, and becoming frustrated. Being shy and quiet as well as not being assertive were among the constructive feedback (See Table 1). A copy of the survey questions and the additional tables of survey results are openly available at https://doi.org/10.6084/m9.figshare.21656864.
|
Student Feedback for the Introduction to Health Profession (IHP) module Total number of respondents: 88 |
|||
|
NO. |
THEMES |
OPEN FEEDBACK FROM STUDENTS |
|
|
Majority of the positive responses are as follows: |
Common comments on areas to improve self: |
||
|
1 |
Teamwork |
|
|
|
2 |
Effective Communication |
|
|
|
3 |
Professional Behavior |
|
|
|
4 |
Adaptability and resilience |
|
|
|
5 |
Making connections and networking with peers |
|
|
|
6 |
Insight to self |
|
|
|
Table 1. Student Feedback from IHP Cohort ME121 |
|||
IV. DISCUSSION
IHP is a new course with the objectives of introducing students to the real world and value systems of the health professional, focusing on communication skills, medical ethics, teamwork, and the importance of self-reflective practice. The learning is mainly facilitated by group work and formative assessment through immediate provision of feedback and self-reflection. Due to pandemic-related restrictions, the initial plans for real life experience and exposure in IHP course had to be converted to the online platform. An instructional method such as gamification was selected to help retain student engagement and encourage participation (Chou, 2012). Applying the design elements and principles found in games to education was useful in sparking student interest and motivation (Chou, 2012).
Knowledge checks challenged the minds, improved cognition and knowledge retention (Singhal et al., 2019). Progress mechanics in the form of earning ‘a badge on completion’ of assigned activities, going through the provided learning material and completing the knowledge check to an acceptable level, promoted self-directed learning, created a sense of achievement and retained student engagement. This reward system fosters student participation, as it is a tangible reward (Dodson, 2021).
The seclusion from real life interaction is feared to mentally and psychologically affect students. A study in Switzerland has shown a significant impact on the mental health of learners due to the lockdown in 2020 (Elmer et al., 2020). In another study, social interaction is recognised as an important factor for enhancing learning especially in areas of critical thinking and problem solving (Hurst et al., 2013). The group works in the IHP course, though set virtually, have assisted students in networking and socialising during the pandemic. This was agreed by majority of the students who participated in IHP activities.
Effective leadership is essential in delivering high standards of clinical practice. The students learnt leadership skills through organising group work, delegating roles and responsibilities among team members. Among the examples of group work are problem- solving scenarios like managing a fire in CCU or multiple vehicle accident on the highway. The instructional content was related to the teamwork and roles and responsibilities of the different health professionals involved in managing the crisis and it was gamified by adding elements of game fiction such as the different themes, settings and characters. As students had to self- produce scripts after some brief research of relevant contents, they had some autonomy over the depth and breadth of their learning. Working in teams towards common goals lead to improved productivity and self-esteem and created supportive relationships during the collaborative learning (Singhal et al., 2019). Narrative synthesis and role playing in scenarios managing crisis situations stimulated reflective practice whilst integration of cause and effect enabled experiential learning.
Overall feedback was encouraging as almost all students enjoyed the activities and found them both educational and engaging. They discovered characteristics in themselves that helped them to improve team spirit and communication. The groupwork on the various projects developed learning communities and promoted interpersonal skills, integrating diverse learner types with a wide range of knowledge, skills, past experiences and personal attributes. This was effectively utilized in the groupwork and collaborative learning.
Some setbacks occurred when both the faculty and students were unfamiliar with online gamification. The synchronous sessions with international students in different time zones, made group discussions challenging. Support from the Information Technology team is valuable but poses an exorbitant cost. Students having expectations of medical school learning to be more didactive, instead had to adapt to being adult learners, for more extensive self- directed learning and reflective practice.
V. CONCLUSION
In conclusion, gamification of IHP module encouraged student engagement, teamwork and collaborative learning. IHP course was accessible virtually, which was a boon for our international students who could interact virtually with peers and access and take part in the lessons. The gamification features used were reproducible. Gamification is useful in medical education and can be pursued as a method to deliver lessons and engage students. It is a tool to allow learning in depth and for experiential learning on the virtual platform.
Notes on Contributors
Dr Sasikala Devi Amirthalingam is the first author, contributing to the abstract, introduction, discussion and literature review. She agrees to be accountable for all aspects of the work.
Dr Shamala Ramasamy is the second author, contributing to methodology, results and literature review. She agrees to be accountable for all aspects of the work.
Prof Sharifah Sulaiha Hj Syed Aznal is the third author, contributing to abstract, introduction, discussion and revising it critically for important intellectual content. She agrees to be accountable for all aspects of the work.
Ethical Approval
The dean of School of Medicine, International Medical University has given a letter to say that there is no objection to sharing of findings for educational purpose.
Data Availability
The data that support the finding are openly available in the Figshare repository. https://doi.org/10.6084/m9.figshare.21656864
Acknowledgement
We would like to acknowledge Fareeza Marican Bt Abu Backer and Norhasliza Binti Hashim from E Learning Department from International Medical University for the technical assistance in the gamification features to the module.
Funding
There is no financial support or any financial relationships that may pose a conflict of interest.
Declaration of Interest
There is no conflicting interest to any parties concerned.
References
Chou, Y. K. (2012). What is gamification. Yukai Chou: Gamification and Behavioral Design. https://yukaichou.com/gamification-examples/what-is-gamification/
Dodson, K. R. (2021). Can gamification drive increased student engagement? Educause Review. https://er.educause.edu/articles/sponsored/2021/10/can-gamification-drive-increased-student-engagement
Elmer, T., Mepham, K., & Stadtfeld, C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE, 15(7), Article e0236337. https://doi.org/10.1371/journal.pone.0236337
Hurst, B., Wallace, R., & Nixon, S. B. (2013). The impact of social interaction on student learning. Reading Horizons: A Journal of Literacy and Language Arts, 52(4), Article 5. https://scholarworks.wmich.edu/reading_horizons/vol52/iss4/5
Singhal, S., Hough, J., & Cripps, D. (2019). Twelve tips for incorporating gamification into medical education. MedEdPublish, 8(3), Article 216.
*Sasikala Devi Amirthalingam
International Medical University,
Kuala Lumpur, Malaysia
+60133513435
Email: SasikalaDevi@imu.edu.my
Submitted: 5 August 2022
Accepted: 2 November 2022
Published online: 4 April, TAPS 2023, 8(2), 76-79
https://doi.org/10.29060/TAPS.2023-8-2/SC2861
Poh-Sun Goh1 & Elisabeth Frieda Maria Schlegel2
1Department of Diagnostic Radiology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Science Education, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hofstra University, United States
Abstract
Introduction: The aim of this short communication is to examine the journey of scholarship in health professions education (HPE).
Methods: We will focus on tangible small steps to start, sustain, and succeed along this journey. Through a proposed innovation in scholarship – micro-scholarship – we will describe how this is similar to and an extension of bite-size or micro-learning, and workplace micro-practice related to just-in-time (JiT) learning settings.
Results: We will demonstrate how the small steps for generating and engaging with micro-content can be similarly applied to micro-scholarship. Then, progressive and iterative refinement of output and practice of micro-scholarship can be combined and result in macro-scholarship after cycles of public engagement for final digital or print publication. This stepwise approach creates an accessible, sustainable strategy to achieve success as a scholar in HPE. We will elaborate on micro, macro, and meta matters and celebrate how these small steps encourage and allow broad participation in the creation, critique, and progressive refinement of scholarship.
Conclusion: Small, sustainable, steps leads to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Keywords: Micro-Scholarship, Micro-Learning, Just-In-Time (JiT) Learning, Community of Practice (CoP), Technology, Network Effects, Post-Publication Peer Review (PPPR)
I. INTRODUCTION
Modern changes in the pace and way we conduct and experience teaching and learning have resulted in production and consumption of smaller chunks of content. Succinct, bite-size content is easier to remember and consumes less cognitive bandwidth with reduced cognitive load. In addition, it is also significantly easier to share and engage with within a professional community of practice (CoP). Compact modular, bite-size content is also ideal for just-in-time (JiT) micro-learning and workplace micro-practice (Yilmaz et al., 2022), or on-demand learning and practice, with which we are all familiar. In this paper, we will extend this idea of micro-learning and micro-practice to scholarship, by examining the “new” idea of micro-scholarship – defined as “the process of making visible the smallest accessible and assessable steps that document a scholarly journey, which can then be assembled and presented as an outcome of academic scholarship” (Goh et al., 2021). Mobile technology tools and platforms support open display, access to, and iterative engagement with this content by a community of practice (CoP), both in learning and scholarship (Goh et al., 2021; Goh & Sandars, 2020; Schlegel, 2021).
II. MICRO-MATTERS
Just as a musical composition is made up of individual notes, a construction from its individual parts, and a meal of its individual ingredients, commonly accepted and acknowledged finished works of scholarship in HPE are composed of its individual parts. A conference presentation or journal paper, peer reviewed, read by and engaged with by a CoP, contains core components – e.g., the title (which includes key ideas); key words (which are defined and illustrated in the presentation or paper); and cited published work by earlier authors (from a review of the field, including takeaways from the author(s) that are relevant and that the authors intend to discuss, elaborate, and build upon). However, a close examination and reflection of these core parts of finished works of scholarship show that they not only form the ingredients of the final work, but that they also fall within the categories of scholarship proposed by Boyer, with evaluation criteria described by Hutchings and Shulman; (Goh et al., 2021; Goh & Sandars, 2020). Boyer’s model for scholarship includes (1) integration, (2) application, (3) teaching and learning, and (4) discovery.
Innovative JiT micro-content on mobile platforms is easily accessible for members of a CoP to engage with, evaluate, critique, and build upon. All online content, including, e.g., on Twitter, blogs, or modular courses, is subject to creative reader collectives, which post comments, repost, reshare, and create new meaning and value from individual posts of content, contributing to group engagement, which has many of the characteristics of scholarship (Schlegel & Primacio, 2021). We propose that these artefacts and activities illustrate examples of Boyer’s Scholarship categories, including demonstrating the Scholarship of Teaching and Learning SoTL. Digital and online content and platforms support and scale our efforts as learners and scholars, no different yet more facile as compared to in-person activities, with increased importance placed on being a public professional, and respecting intellectual property, shown by proper citation of digital content, and use of this content with permission where applicable, followed by data-driven dissemination (Arrington & Cohen, 2015; Kern et al., 2015). This public reaction and appraisal of content compares to wide audience post-publication peer review (PPPR) with the added value of a feedback-loop through responses on comments. Just as developing bite-size, short format, JiT digital, online content, has transformed and continues to transform our educational and professional practices, a similar process can now facilitate and support granular, open digital display and engagement of both our initial and subsequent steps when engaging in scholarship in HPE, similar to and an extension of micro-learning. Practicing micro-scholarship involves encountering a “new idea”; researching its meaning; adding relevance to specific discussion themes and takeaways; discovering key published and presented work; and then both taking note of and making notes on these findings during reflection and discussions within a local CoP. This micro-scholarship is subsequently made open and visible to a global readership or a CoP, through private, semi-private, and public engagement platforms. Micro-scholarship content gets progressively refined through iterative engagement with members of a CoP, through discussion, feedback, critique, and personal reflection. The relevance and usefulness of this content, as well as confidence in the authors of this micro- scholarship content, is progressively enhanced. We also learn how and where this content is best disseminated and presented, and best ways this might be combined and stacked. The iterative in- person and scalable digital conversations amplifying the spread and engagement with this material to create meaning, in step-by-step fashion, form the core practices of both micro-scholarship (Goh et al., 2021) and bite-size engagement with material (Schlegel, 2021). After refinement, these pieces can be combined into larger pieces of finished work of macro-scholarship. Thus, activities undertaken as part of micro-learning or micro-scholarship are accessible, independent, and sustainable small, step-wise efforts that can and do add-up. Progression along the developmental path of a scholar will include a variety of conversations within a CoP, such as the supportive networks of peers, senior practitioners, mentors and coaches, including collaborative (team)work and initially supervised instruction as part of a successful scholar’s journey. Conversations and engagement within a CoP do range from positive and helpful to (those that are or perceived to be) occasionally provocative and challenging. However, professional and good-natured discussion generally guide scholarly development similar to trial and error, and progressive improvement and iterative steps enable learning and growth.
III. MACRO-MATTERS
Simply put, a finished larger work is made up small pieces that have been selected and refined, through an iterative process of reflection and feedback, by engaging with a CoP or specialised collective of readers. Open (digital) practice from an early stage, the platforms (places and readers) we engage in, and our active participation in professional CoP of global specialised readers provide both “informed” and “critical” feedback – and review of these “early” and “small” or “micro” pieces of work – from a (much wider) audience. The key distinction is who engages with this work, from as wide a spectrum of professional practice, experience, and expertise as possible, and from a diversity of points of view. Digital tools and practices facilitate and scale this process. This is similar to the work of artists, who engage in open sketching, including showcasing early drafts and ideas, prototyping, drawing, and artistic creation in open studios. When members of a CoP engage through digital platforms the impact from their individual and collective input can scale exponentially through network effects (Azhar, 2021).
IV. META-MATTERS
The process of scholarship mirrors the stepwise, sequential, cumulative process of learning, and training for proficiency and mastery in any area of practice. Our roles as practitioners, educators and scholars are all informed by learning science. Digital devices, tools, platforms, and practices exponentially scale up the impact of our efforts through applied network theory and interactions. Ultimately, we live and practice professionally within our CoP, which provides both the audience and peer reviewers of our public work, thus driving a fruitful evolution of our profession. Our ultimate aim is to engage a CoP in conversations, including broader participation in the production, refinement, and consumption of products of scholarship, in form and format, and through processes accessible for all. Micro-scholarship is a starting point that allows wider participation and engagement in the process of scholarship. The components of micro-scholarship, when refined and confidently presented, are contained within published finished macro-scholarship outputs. Then, micro-scholarship and macro-scholarship add collaboration and value within a larger scholarship ecosystem and professional CoP, a meta-level practice or meta-system, within which micro- and macro- level activities occur. An explicit example of the outputs and process of moving from micro, through macro, to meta practice illustrated https://www.slideshare.net/dnrgohps/illustrated-stacked-microscholarship-steps-along-academic-path-of-educational-scholar.
Another example of enhancing scholarship of teaching and learning SoTL across different levels might include, e.g. a remote consultation with members of scholarly project teams, prompting to publish a themed blog post, which, in return, becomes now a generalizable, transferrable offering to the global CoP, moving from the meta-system to the macro-level, as evidenced by comments from different institutions and subsequent implementation of ideas (Arrington & Cohen, 2015).
V. CONCLUSION
In this paper, we have examined, showcased, and celebrated the small sustainable steps to success as a scholar in HPE, describing micro, macro, and meta matters and illustrating how combining small components of scholarship is an effective strategy for dissemination, access, engagement, conversation and collaboration within a CoP in HPE.
Notes on Contributors
Poh-Sun Goh pitched initial idea, was involved in active discussion and brainstormed with co-author iterative refinement of core message(s), wrote first draft, and actively revised series of subsequent drafts, and submitted final draft. This manuscript built on previous collaborative work, cited in article on Micro-Scholarship and Digital Scholarship.
Elisabeth Schlegel was involved in active discussion and brainstormed with co-author iterative refinement of core message(s), and actively revised series of subsequent drafts, and including and approving final draft. This manuscript built on previous work, cited in article including on bite-sized learning.
Ethical Approval
As this manuscript is a description of an innovative approach to scholarship, ethical approval and IRB application was not required.
Data Availability
There is no additional data separate from available in cited references.
Acknowledgement
No technical help and/or financial and material support or contributions was received in preparation of this manuscript.
Funding
Both authors have no funding source to declare.
Declaration of Interest
Both authors declare that there are no possible conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Arrington, N. M., & Cohen, A. L. (2015). Enhancing scholarship of teaching and learning through micro-level collaboration across two disciplines. International Journal of Teaching and Learning in Higher Education, 27(2), 194.
Azhar, A. (2021). The exponential age: How accelerating technology is transforming business, politics and society. Diversion Books.
Goh, P. S., Roberts-Lieb, S., & Sandars, J. (2021). Definition of Micro-Scholarship. https://microscholarship.blogspot.com/
Goh, P. S., & Sandars, J. (2020). Rethinking scholarship in medical education during the era of the COVID-19 pandemic. MedEdPublish, 9(97). https://doi.org/10.15694/mep.2020.000097.1
Kern, B., Mettetal, G., Dixson, M., & Morgan, R. K. (2015). The role of SoTL in the academy: Upon the 25th anniversary of Boyer’s scholarship reconsidered. Journal of the Scholarship of Teaching and Learning, 15(3), 1-14. https://doi.org/10.14434/josotl.v15i3.13623
Schlegel, E. (2021). (Not only) for medical students: Get involved in medical education research & scholarship. https://elisabeth-fm-schlegel.weebly.com/elearning-bites/not-only-for-medical-students-get-involved-in-medical-education-research-scholarship
Schlegel, E., & Primacio, J. (2021). Blogging for the continuum of medical education: Engaging diverse communities of learners. MedEdPublish, 10, Article 136. https://doi.org/10.15694/mep.2021.000136.1
Yilmaz, Y., Papanagnou, D., Fornari, A., & Chan, T. M. (2022). The learning loop: Conceptualizing Just-in-Time faculty development. AEM Education and Training, 6(1), e10722. https://doi.org/10.1002/aet2.10722
*Poh-Sun Goh
Department of Diagnostic Radiology
National University Hospital,
Main Building, Lobby F, Level 4
#04-398, DDI Library
5 Lower Kent Ridge Road, Singapore 119074
+6567724211
Email: dnrgohps@nus.edu.sg
Submitted: 28 April 2022
Accepted: 19 August 2022
Published online: 4 April, TAPS 2023, 8(2), 70-75
https://doi.org/10.29060/TAPS.2023-8-2/SC2802
Sok Mui Lim, Ramesh Shahdadpuri & Ching Yee Pua
Centre for Learning Environment and Assessment Development (CoLEAD), Singapore Institute of Technology, Singapore
Abstract
Introduction: Coaching has gained acceptance in the education field as a way to enable learners to achieve their fullest potential. In the endeavor to set up a coaching ecosystem in our university, we started by equipping our educators with fundamental coaching skills and techniques. Our training workshop, Coaching As An SIT Educator, covers the key coaching competencies and is highly practice focused. Participants get hands-on skills practice using contextualised scenarios that are based on realistic academic, workplace and clinical placement settings.
Methods: To address concerns on time-effectiveness, we adopt a solution-focused approach to coaching. We want to create a mindset shift for educators, from subject experts providing advice and solutions, to coaches asking powerful coaching questions that help students make discoveries and work towards their goals. We encourage our educators to engage students holistically by finding coachable moments in their daily student interactions.
Results: Competency-based assessments are conducted to determine achievement of the learning outcomes, articulated by the knowledge, attitude, and demonstration of coaching skills with students. Assessments consist of a reflection, multiple-choice question (MCQ) quiz, and scenario-based coaching role plays. Participants achieved the learning outcomes as demonstrated from the assessments.
Conclusion: The coach training workshop is the major pillar of our coaching initiative. Beyond the workshop, ongoing coaching development is supported through other activities and resources, including community of practice, coaching circle and knowledge repository. Opportunities for continuous learning and conversation platforms for sharing coaching experiences are part of the growing coaching ecosystem at SIT.
Keywords: Assessments, Coaching Competencies, Coaching Conversations, Coaching Ecosystem, Coachable Moments, Faculty Development, Feedback, Holistic Development, Solution-Focused
I. INTRODUCTION
Coaching has gained greater awareness and wider acceptance in the education field in the past decade, led by the efforts of innovative educators and more evidence-based research. Coaching has been described as a very powerful approach that facilitates personal and professional change through deep level listening, questioning, setting the right challenges and providing support along the process (Griffiths, 2005). More specifically, academic coaching is defined as individualised practice of asking students reflective, motivation-based questions, providing opportunities for formal self-assessment, sharing effective strategies, and co-creating a tangible plan that promotes accountability (Deiorio et al., 2017).
In traditional educational settings, communication tends to be mostly directive, where the educator is the subject expert who gives instructions, solutions or advice to students. From this “telling” or “pushing” stance where the focus is on problem solving and advice giving, shifting to coaching conversations requires an “asking” or “pulling” communication approach. Engaging in coaching conversations involves the educator coaching students through powerful questioning, active listening and guiding them to explore possibilities so as to discover new ideas and find solutions for themselves.
In 2020, Singapore Institute of Technology (SIT) introduced internal coach training for all academic staff with the aim to build educators’ capability to work with students at a deeper level. This highly contextualised academic coaching training was made mandatory for all educators. This was essential for the creation of a strong coaching ecosystem in the university and adopting coaching practices across a variety of learning contexts, such as providing assignment feedback, consultations on projects and supervising students at the workplace. In working with students towards their preferred futures, SIT educators can help the students develop confidence and self-efficacy, enabling them to achieve their fullest potential.
II. METHODS
This section highlights the critical elements of the faculty development programme.
A. Solution-focused Approach
One of the top concerns of many educators is time. There are underlying concerns on whether coaching students will take up too much time, and what happens if they uncover student issues that they cannot deal with. A solution-focused coaching approach alleviates some of these concerns. The basic principle of the solution-focused approach is to help coachees reflect and design their solutions, rather than go down the path of root cause analysis. Its forward-oriented solution approach contrasts with other traditional psychological techniques, which tend to look back at the past or are problem-focused (Grant & Gerrard, 2020).
The solution-focused approach is known for its simplicity, attention to language and time effectiveness. The conversation is steered to a preferred future of the issue at hand without dwelling on the troubled past. The coach encourages the coachee to focus on their strengths and positive resources, to think about their resourceful past, and to draw on positive lessons from when they have been at their best. After identifying their desired outcomes and considering their options in the context of present realities, the coach guides the coachee to think about the next steps to progress towards their preferred future.
B. Mindset Shift
In higher education, many coachable opportunities outside the formal contact hours can be easily missed. For example, instead of merely deducting marks for repeated late submissions of assignments, the educator could coach the student on improving time management. In clinical fieldwork, when a student complains about limited interaction with the busy clinical educator, the university supervisor can coach the student on how best to schedule time for feedback. Our daily encounters and interactions with students present many coachable moments that offer just-in-time and authentic learning opportunities to support students in their development to become work-ready graduates.
Students may initially find coaching sessions difficult as it is easier to just ask for solutions than to discover solutions for oneself. However, with time, students will realise the value of coaching as they witness their progress. In an Asian context, where many students are respectful and value advice from authoritative figures, such as professors, coaching can require a mindset shift for both students and faculty (Lim, 2021).
C. Tailoring the Coaching Training to Education Context
The Coaching As An SIT Educator workshop is an in-house designed 2-day program. It is highly contextualised for the needs of SIT academic staff, to equip them to be versatile and agile educators, performing the role of Teacher-Coach-Mentor. The workshop covers the key coaching fundamentals and is highly practice-oriented. The programme design was intended for participants to develop hands-on coaching skills with contextualised role play scenarios (see Appendix A for an example), so that they can apply what they have learnt with their students immediately after the workshop.
While we do not intend to train credentialed professional coaches, the key International Coaching Federation (ICF) coaching competencies were referenced to guide the design of the SIT workshop. The GROW model (Whitmore, 2019) was introduced as a framework for the participants to organise and manage the flow of the coaching conversation. Drawing on inputs from academic staff, realistic student-centric scenarios were created for class discussions and role plays. The coaching practice sessions are conducted in dyad, triad, and hot seat formats. The workshop design and facilitation ensure that there is psychological safety, providing a trusting space for constructive debriefing, feedback sharing and open questions and answers to take place.
To manage the workshop time and resources effectively, e-learning content was developed in-house, specifically to complement the interactive classroom session. A week before the start of the workshop, the participants can access materials in the form of an asynchronous pre-recorded webinar. The webinar consists of five micromodules, covering topics such as Mindset, Motivation, Emotional Intelligence, and Feedback Skills (refer to Appendix B for more details). As many participants may already be familiar with these topics, this self-learning component serves as a good refresher to prepare participants for the coaching workshop.
Please refer to Table 1 for details of the Coaching as An SIT Educator workshop.
|
Workshop: Coaching As An SIT Educator |
|
|
Learning Outcomes By the end of this course, participants will be able to:
|
|
|
Topics Covered |
|
|
Pre-Workshop: eLearning
|
Workshop Day 1:
Workshop Day 2:
|
|
Assessments (Day 2) |
|
|
Role Plays: Standardised Students & Assessors Scenarios (each – 20 minutes):
|
Quiz: Multiple Choice Questions (MCQs)
|
Table 1. Coaching As An SIT Educator Workshop
III. EVALUATION OF COACHING COMPETENCY
To assess the attainment of the learning outcomes and development of the participants’ coaching competence (knowledge, skills, attitude), assessments and reflection exercises are incorporated into the workshop. As this is not a certification program, assessments are formative in nature, with focus on providing the educators quality feedback. Coaching knowledge is assessed through a multiple-choice question (MCQ) quiz. Attitude and mindset shift is evaluated through pre- and post- workshop surveys, and reflection questions.
Coaching skills are assessed via role plays (with standardised students). The role play format involves two 20-minute coaching sessions with the participant (playing the role of an educator) having a coaching conversation with standardised students (who act as coachees) and are conducted virtually in real time over the Zoom platform, using breakout rooms. The role plays that are based on common scenarios in university and workplace supervision settings. An invaluable part of the learning in this assessment comes from the feedback conversation between the participant (coach) and assessor, who observes the coaching conversation. Many participants regard the skills assessment and individualised feedback on their coaching skills as the highlight of the training programme.
IV. DISCUSSION
Many readily available coaching materials or vendor-run workshops are geared towards executive or corporate scenarios. While the skills of coaching may be transferable, it is difficult for educators to draw relevance to student engagement. Therefore, Coaching As An SIT Educator workshop focuses on case studies of university scenarios, and supervision for work-integrated learning (e.g., internship, clinical placement). Participants get to work with fellow learners in group work and discussions, to engage in personal reflection, and takeaway practical knowledge and skills on their learnings in a safe space.
For a sustained effort to practice coaching and build an on-going coaching culture, a mandatory workshop is inadequate. Other coaching resources are available to support coaching practice and promote continuous learning in SIT:
- Community of Practice: Coaching Conversations @SIT (offered to any interested academic staff)
- Coaching Circle (offered to all alumni of the coaching workshop)
- Coach Academy (knowledge repository with academic and coaching industry resources).
V. CONCLUSION
In coaching, there lies great potential for students to be developed holistically if we tap on coachable moments in higher education. A contextualised, well-developed coaching development programme is an enabler for this potential to be fulfilled. Drawing on evidence-based research from academia and professional practice, a practice-oriented programme which focuses on developing hands-on coaching skills will be impactful, as educators can put these skills into action in their interaction with students.
Notes on Contributors
Associate Professor Lim Sok Mui (May) led the Center for Learning Environment and Assessment Development (CoLEAD) and spearheaded the coaching initiative in the university, contributed to the conception, drafted and critically revised the manuscript.
Ramesh Shahdadpuri is the senior educational developer in CoLEAD and plays the role of the coaching trainer for the faculty training program. reviewed the literature, contributed to the conception and assisted in revising the manuscript.
Pua Ching Yee is the learning analyst in CoLEAD and plays the role of coordinating the coaching training and assessment of the participants. She assisted in critically reviewing, revising and formatting the manuscript.
All authors gave their final approval and agree to be accountable for all aspects of the work.
Ethical Approval
This is a narrative review related to coaching training program with no data presented and no ethical approval is required.
Data Availability
This paper is a narrative review with no data analysis.
Acknowledgement
The authors would like to thank Miss Cherine Foo for her significant contribution of the coaching program.
Funding
There is no funding involved in the preparation of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Deiorio, N. M., Skye, E., & Sheu, L. (2017). Introduction and definition of academic coaching. In N. M. Deiorio & M. M. Hammoud (Eds.), Coaching in medical education: A faculty handbook (pp. 1-5). American Medical Association.
Grant, A. M., & Gerrard, B. (2020). Comparing problem-focused, solution-focused and combined problem-focused/solution-focused coaching approach: solution-focused coaching questions mitigate the negative impact of dysfunctional attitudes. Coaching: An International Journal of Theory, Research and Practice, 13(1), 61-77. https://doi.org/10.1080/17521882.2019.1599030
Griffiths, K. (2005). Personal coaching: A model for effective learning. Journal of Learning Design, 1(2), 55–65. http://dx.doi.org/10.5204/jld.v1i2.17
Lim, S. M. (2021, May 27). The answer is not always the solution: using coaching in higher education. Times Higher Education. https://www.timeshighereducation.com/campus/answer-not-always-solution-using-coaching-higher-education
Whitmore, J. (2019). Coaching for performance: The principles and practice of coaching and leadership (5th ed.). Nicholas Brealey Publishing.
*Lim Sok Mui
Singapore Institute of Technology,
10 Dover Drive, Singapore 138683
+65 65921171
Email: may.lim@singaporetech.edu.sg
Submitted: 4 October 2022
Accepted: 5 December 2022
Published online: 4 April, TAPS 2023, 8(2), 66-69
https://doi.org/10.29060/TAPS.2023-8-2/SC2894
Simon Field1, Pat Croskerry2, Susan Love3, & Peggy Alexiadis Brown4
1Undergraduate Medical Education and Emergency Medicine, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada; 2Critical Thinking Program, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada; 3Faculty Development, Continuing Professional Development, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada; 4Dalhousie Medicine New Brunswick, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada
Abstract
Introduction: For all clinical providers in healthcare, decision-making is a critical feature of everything they do. Every day physicians engage in clinical decision-making where knowledge, evidence, experience, and interpretation of clinical data are used to produce decisions, yet, it is fair to say that most do not have an explicit insight or understanding of this complex process. In particular, few will have training in teaching and assessing the cognitive and affective factors that underlie clinical decision-making.
Methods: To foster an increased awareness and understanding of these factors, the Dalhousie Critical Thinking Program was established with the mandate to develop and deliver curriculum for critical thinking in the 4-year undergraduate program. To assist teaching faculty with the goal and objectives of the program, the Teaching and Assessing Critical Thinking Program (TACT) was introduced.
Results: Using the dual process model as a platform for decision-making, this program introduces general principles of critical thinking and provides tools to teach learners how to strengthen their critical thinking skills. To offer flexible learning, an online approach was chosen for delivery of the program.
Conclusion: To date, we have offered eleven iterations of Part 1 to a total of 261 participants and six iterations of Part 2 to a total of 89 participants. Evaluations show the online approach to content delivery was well received and the content to be of practical use.
Keywords: Critical Thinking, Clinical Decision-Making, Faculty Development, Asynchronous Learning
I. INTRODUCTION
This paper provides a review of a two-part Teaching and Assessing Critical Thinking (TACT) program which was developed to help faculty understand vulnerability to bias and the role of metacognitive processes in clinical decision-making. The objective of the TACT program is to better prepare faculty to teach learners these important skills. In this paper, we describe how it was implemented, how participants perceived the program, and what changes were needed to address this important hidden ‘soft’ skill within the clinical setting.
II. METHODS
Physicians are constantly required to interpret information when they interact with patients, communicate with colleagues, review medical histories and laboratory reports, conduct physical exams, review the medical literature, and attend rounds. All of these clinical activities demand a sustained level of accuracy, clarity, and especially rationality. Critical thinking (CT) does not guarantee rationality but is one of its more important features and is essential for the role of physician.
Reliable and accurate diagnosis is the barometer of good clinical decision-making and will have a direct impact on treatment outcomes and patient safety. One in 20 (or roughly 12 million) American adult outpatients are affected by diagnostic errors every year. The overall number of fatalities associated with diagnostic failure is not known, but it is estimated that 40,000 – 80,000 deaths occur annually in hospitalised patients in the USA due to diagnostic failure.
A number of studies have shown that training in the development of CT skills in undergraduate students is effective. (Abrami et al., 2015) However, given that most faculty in medical schools today will not have had explicit CT training, specific initiatives in teaching it seem appropriate, not only for the faculty themselves but, importantly, for the students they teach.
To better prepare learners, Dalhousie’s Faculty of Medicine established the Critical Thinking Program in 2012. The program incorporated principles from the Foundation for Critical Thinking into a general model of clinical reasoning (Croskerry, 2018). The Dalhousie critical thinking curriculum reflects a consensus in the current medical literature that the dual process model (System 1 and System 2) is the most appropriate platform for reviewing the clinical decision-making process (See Figure 1).
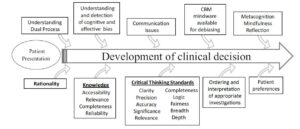
Figure 1. The Dalhousie University model for clinical decision making. (Reproduced with Permission)
A key component in the delivery of this curriculum is helping faculty develop the skills they will need to teach and mentor critical thinking in the clinical environment. Most educators have limited understanding of the advances in medical decision-making and how to best teach critical thinking and clinical reasoning.
The TACT Program comprises two distinct courses: TACT 1 and TACT 2. The program is structured to develop a sound knowledge of critical thinking principles in TACT 1, followed by a focus on teaching and learning in TACT 2. TACT 1 centres on three main themes: How Physicians Make Decisions, Cognitive and Affective Biases, and Cognitive Debiasing Strategies. TACT 2 centres on two main themes: Fundamentals of Medical Education and Strategies for Teaching and Assessing CT. In TACT 2, participants choose one of four elective options: Evidence Based Medicine, Competency Based Medical Education, Medical Humanities, or Curriculum Development.
The TACT Program uses an asynchronous online approach to reach Dalhousie faculty who are distributed across the Canadian Maritime Provinces. This approach mediates potential barriers for participation such as distance and time constraints and allows for individualised learning experiences while building an interactive online community of practice experience (Cook & Steinert, 2013). We use a combination of curricular tools including online didactic lectures, independent study activities, webinars, and discussion boards.
To date (Winter 2022), we have held 11 iterations of TACT 1 and 6 iterations of TACT 2, with 163 of 261 participants completing TACT 1 and 78 of 89 registrants completing TACT 2.
Of those who completed TACT 1, 55 % went on to enrol in TACT 2.
We initially developed the TACT Program for Dalhousie faculty (primarily physicians); however, due to growing interest in the topic, we have opened enrolment to include participants from around the world, including the United States, Mexico, United Kingdom, Australia, New Zealand, Turkey and Brazil. We also opened enrolment to participants from a variety of health professions and other fields of study. By opening the program to participants with diverse backgrounds in practice and location we have increased the diversity of perspectives and the richness of reflections posted to the discussion boards.
Prior to starting the TACT Program, we asked participants to complete a survey measuring their current knowledge of teaching and assessing CT, and motivation for taking the course.
Participants reported little satisfaction with previous knowledge in CT (Mean: 2.67 ± 0.84 on a Likert Scale of 1 (not at all satisfied) to 5 (very satisfied)). The following themes were identified as motivators for taking the TACT Program — a desire to: learn, improve clinical reasoning by increasing knowledge, understand the impact of critical thinking, provide better clinical care, decrease diagnostic error, and become a better educator.
We administered a summative evaluation following both TACT 1 and TACT 2. For TACT 1, 75% (121/162) completed the final evaluation and for TACT 2, 90% (63/70). In the summative evaluation, we asked participants to rate their course in a number of areas from course delivery to the effectiveness of increasing their knowledge and comfort in teaching critical thinking. Consent to data collection was implied as part of the administration of the evaluation. We found that participants were very satisfied with delivery methods.
III. RESULTS
A. What Did We Learn about the Participants?
All participants taking the TACT Program shared a similar motivation: the intent to improve their critical thinking skills and to teaching others. Steinert et al. (2002) found that faculty are more likely to enrol in an online program if they believe it would meet a perceived need. Our participants identified a desire to improve their own practice, confidence and awareness, to make the unconscious conscious, and to develop the language to name, identify and act on cognitive biases and those circumstances that create biases. This enabled them to better teach and mentor CT.
Participants also identified the value of communicating with others who offered a different perspective on clinical work and life experiences.
Physicians may not readily share/disclose mistakes they make in the clinical setting. In medical training environments, overconfidence and reluctance to admit mistakes are often the norm, which may work against fostering a culture of reflection (Brezis et al., 2016). Due to the confidentiality of the discussion boards, our participants could freely reflect on what factors contribute to errors they have made/seen and share those lessons with peers without fear of loss of reputation and embarrassment.
B. What Did We Learn about the Delivery?
We found that the online delivery was successful in reaching a broad base of participants. Some participants appreciated the mode of delivery as well.
A benefit of online courses is the ease with which faculty can control their pace of instruction. When asked, we found that 97.4% of respondents identified they would do more faculty development programs online.
When we reviewed the online tracking statistics, we found that our participants were accessing materials at all hours. Participants, each with their own learning style, appreciated the mix of interactivity and self-study the online format offered.
IV. DISCUSSION
Ideally, we would like to know how effectively participants in the TACT program incorporated the teaching principles into their own practices in the real clinical world. However, it is very challenging methodologically to do this, and it appears the best we can do is to ask about participant impressions and insight into their experience.
It appeared that the TACT program provided a rich opportunity for participants to interact and share their quest to understand and refine the metacognitive aspects associated with their clinical decision-making and critical thinking processes. It also provided our participants with the language to describe and teach these processes to trainees.
V. CONCLUSION
In summary, the TACT program shows promise in engaging distributed faculty to further their curiosity and interest in how to improve, teach and foster critical thinking skills within medical education and in their own practice. We recognise that although this online asynchronous mode of delivery may not be appropriate to meet the diverse learning styles of all potential participants, the favourable reviews we have received from our program graduates highlighted that the flexible interactivity with the content contributed to the success of the TACT program.
Notes on Contributor
Simon Field assisted in the initial development of the TACT program and contributed to the data analysis and writing of the article.
Pat Croskerry was a founding member of the Critical Thinking Advisory Group, and contributed to the development of the TACT program and to the writing of the article.
Susan Love has been an active contributor to the running of the TACT program, designed the survey tools, collected and analyzed qualitative and quantitative data from the program evaluation, and contributed to the writing of the article.
Peggy Alexiadis Brown collected and analyzed qualitative and quantitative data from the program evaluation survey tools, and contributed to the writing of the article.
All authors have reviewed and approved the final manuscript.
Ethical Approval
The data gathered for this article was collected anonymously as part of Program Evaluation, and a written waiver has been obtained stating that it is exempt from full institutional Research Ethics approval.
Acknowledgement
We acknowledge the valuable support and contribution of Deirdre Harvey and other members of the Critical Thinking Advisory Group. For further information on how to implement a similar program in your region, please feel free to contact us.
Funding
There is no funding associated with this project.
Declaration of Interest
None of the authors have any conflicts of interest to declare, and they do not receive any financial assistance or funding for their participation in the TACT program.
References
Abrami, P. C., Bernard, R. M., Borokhovski, E., Waddington, D. I., Wade, C. A., & Persson, T. (2015). Strategies for teaching students to think critically: A meta-analysis. Review of Educational Research, 85(2), 275-314. https://doi.org/10.3102%2F0034654314551063
Brezis, M., Orkin-Bedolach, Y., Fink, D., & Kiderman, A. (2016). Does physician’s training induce overconfidence that hampers disclosing errors? Journal of Patient Safety, 15(4) 296-298. https://doi.org/10.1097/pts.0000000000000255
Cook, D. A., & Steinert, Y. (2013). Online learning for faculty development: a review of the literature. Medical Teacher, 35(11), 930-937. https://doi.org/10.3109/0142159X.2013.827328
Croskerry, P. (2018). A model for clinical decision-making in medicine. Medical Science Educator, 27(Suppl 1), S9-S13. https://doi.org/10.1007/s40670-017-0499-9
Steinert, Y. L., McLeod, P. J., Conochie, L., & Nasmith, L. (2002). An online discussion for medical faculty: An experiment that failed. Academic Medicine., 77(9), 939-940. https://doi.org/10.1097/00001888-200209000-00046
*Simon Field
Dept of Emergency Medicine,
Dalhousie University, Halifax,
Nova Scotia, Canada
Email: simonfield@dal.ca
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









