A systematic scoping review of teaching and evaluating communications in the intensive care unit
Submitted: 4 May 2020
Accepted: 3 August 2020
Published online: 5 January, TAPS 2021, 6(1), 3-29
https://doi.org/10.29060/TAPS.2021-6-1/RA2351
Elisha Wan Ying Chia1,2, Huixin Huang1,2, Sherill Goh1,2, Marlyn Tracy Peries1,2, Charlotte Cheuk Yiu Lee2,3, Lorraine Hui En Tan1,2, Michelle Shi Qing Khoo1,2, Kuang Teck Tay1,2, Yun Ting Ong1,2, Wei Qiang Lim1,2, Xiu Hui Tan1,2, Yao Hao Teo1,2, Cheryl Shumin Kow1,2, Annelissa Mien Chew Chin4, Min Chiam5, Jamie Xuelian Zhou2,6,7 & Lalit Kumar Radha Krishna1,2,5,7-10
1Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Division of Supportive and Palliative Care, National Cancer Centre Singapore, Singapore; 3Alice Lee Centre for Nursing Studies, National University of Singapore, Singapore; 4Medical Library, National University of Singapore Libraries, National University of Singapore, Singapore; 5Division of Cancer Education, National Cancer Centre Singapore, Singapore; 6Lien Centre of Palliative Care, Duke-NUS Graduate Medical School, Singapore; 7Duke-NUS Graduate Medical School, Singapore; 8Centre for Biomedical Ethics, National University of Singapore, Singapore; 9Palliative Care Institute Liverpool, Academic Palliative & End of Life Care Centre, University of Liverpool; 10PalC, The Palliative Care Centre for Excellence in Research and Education, Singapore
Abstract
Introduction: Whilst the importance of effective communications in facilitating good clinical decision-making and ensuring effective patient and family-centred outcomes in Intensive Care Units (ICU)s has been underscored amidst the global COVID-19 pandemic, training and assessment of communication skills for healthcare professionals (HCPs) in ICUs remain unstructured
Methods: To enhance the transparency and reproducibility, Krishna’s Systematic Evidenced Based Approach (SEBA) guided Systematic Scoping Review (SSR), is employed to scrutinise what is known about teaching and evaluating communication training programmes for HCPs in the ICU setting. SEBA sees use of a structured search strategy involving eight bibliographic databases, the employ of a team of researchers to tabulate and summarise the included articles and two other teams to carry out content and thematic analysis the included articles and comparison of these independent findings and construction of a framework for the discussion that is overseen by the independent expert team.
Results: 9532 abstracts were identified, 239 articles were reviewed, and 63 articles were included and analysed. Four similar themes and categories were identified. These were strategies employed to teach communication, factors affecting communication training, strategies employed to evaluate communication and outcomes of communication training.
Conclusion: This SEBA guided SSR suggests that ICU communications training must involve a structured, multimodal approach to training. This must be accompanied by robust methods of assessment and personalised timely feedback and support for the trainees. Such an approach will equip HCPs with greater confidence and prepare them for a variety of settings, including that of the evolving COVID-19 pandemic.
Keywords: Communication, Intensive Care Unit, Assessment, Skills Training, Evaluation, COVID-19, Medical Education
Practice Highlights
- The global COVID-19 pandemic has underscored the importance of effective communications in the Intensive Care Unit (ICU).
- ICU communications training should adopt a longitudinal, structured and multimodal approach.
- Robust stepwise evaluation of learner outcomes via Kirkpatrick’s Hierarchy is needed.
- Supportive host organisation and conducive learning environment and are key to successful curricula.
I. INTRODUCTION
The COVID-19 pandemic has placed immense strain on intensive care units (ICU)s with healthcare teams and resources stretched to meet the sudden increased healthcare demands of critically ill patients. To further complicate the situation, ICU teams are called to not only communicate closely with colleagues in a bid to support them but also counsel families confronting acute distress and uneasy waits separated from their loved ones due to restrictions to visiting in an effort to limit the spread of this pandemic (Ministry of Health, 2020; World Health, 2020). From breaking bad news (Blackhall, Erickson, Brashers, Owen, & Thomas, 2014; J. Yuen & Carrington Reid, 2011), to conveying the need for sedation and intubation (Carrillo Izquierdo, Diaz Agea, Jimenez Rodriguez , Leal Costa, & Sanchez Exposito, 2018) and providing progress reports on critically ill patients (Curtis et al., 2005; Curtis, White, Curtis, & White, 2008; Yang et al., 2020), communication skills amongst ICU healthcare professionals (HCPs) are pivotal in reassuring anxious, emotional and stressed patients and families (Ahrens, Yancey, & Kollef, 2003; Foa et al., 2016; Kirchhoff et al., 2002). Good communication in the ICU has also been shown to improve patient-physician relationships (K. G. Anderson & Milic, 2017), patient and family-centred outcomes, quality of care, and patient and family satisfaction (Bloomer, Endacott, Ranse, & Coombs, 2017; Cao et al., 2018; Currey, Oldland, Considine, Glanville, & Story, 2015). Effective communications between HCPs in ICU also enhances clinical decision-making (Kleinpell, 2014), reduces medication and treatment errors (Clark, Squire, Heyme, Mickle, & Petrie, 2009; Happ et al., 2014; Sandahl et al., 2013), decreases physician burnout (Rachwal et al., 2018), and improves staff retention and satisfaction (Hope et al., 2015).
With evidence suggesting that poor communication skills (Downar, Knickle, Granton, & Hawryluck, 2012; Foa et al., 2016) and training (Smith, O’Sullivan, Lo, & Chen, 2013) are likely to increase patients’ (Dithole, Sibanda, Moleki, & Thupayagale ‐ Tshweneagae, 2016) and families’ (Curtis et al., 2008) stress, adversely affect care and recovery (Dithole et al., 2016), and increase healthcare costs (Kalocsai et al., 2018), some authors have suggested that effective communication skills are at least as important (Adams, Mannix, & Harrington, 2017; Cicekci et al., 2017; Van Mol, Boeter, Verharen, & Nijkamp, 2014) to good patient care as clinical acumen (Curtis et al., 2001a). Yet despite evidence of the importance of communication skills in ICU, communication skills training remains inconsistent, variable and not evidence-based in most ICU settings (Adams et al., 2017; Berlacher, Arnold, Reitschuler-Cross, Teuteberg, & Teuteberg, 2017; Bloomer et al., 2017; D. A. Boyle et al., 2017; Miller et al., 2018; Sanchez Exposito et al., 2018).
With this in mind, a systematic scoping review (SSR) is proposed to map current approaches to communications skills training in ICUs (Munn et al., 2018) and potentially guide design of a communications training programme. An SSR allows for systematic extraction and synthesis of actionable and applicable information whilst summarising available literature across a wide range of pedagogies and practice settings employed to understand what is known about teaching and evaluating communication training programmes for HCPs in the ICU setting (Munn et al., 2018).
II. METHODS
To overcome concerns about the transparency and reproducibility of SSR, a novel approach called Krishna’s Systematic Evidenced Based Approach (henceforth SEBA) is proposed (Kow et al., 2020; Krishna et al., 2020; Ngiam et al., 2020). This SEBA guided SSR (henceforth SSRs in SEBA) adopts a constructivist perspective to map this complex topic from multiple angles (Popay et al., 2006) whilst a relativist lens helps account for variability in communication skills training (Crotty, 1998; Ford, Downey, Engelberg, Back, & Curtis, 2012; Pring, 2000; Schick-Makaroff, MacDonald, Plummer, Burgess, & Neander, 2016).
To provide a balanced review, the research team was supported by the medical librarians from the National University of Singapore’s (NUS) Yong Loo Lin School of Medicine (YLLSoM), the National Cancer Centre Singapore (NCCS) and local educational experts and clinicians at the NCCS, the Palliative Care Institute Liverpool, YLLSoM and Duke-NUS Medical School (henceforth the expert team). The research and expert teams adopted an interpretivist approach as they proceeded through the five stages of SEBA (Figure 1).
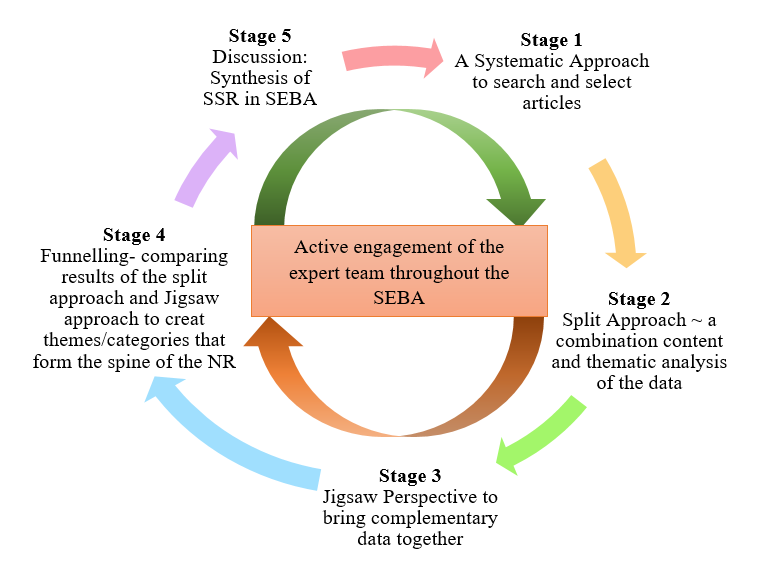
Figure 1. The SEBA Process
A. Stage 1: Systematic Approach
1) Determining the title and research question: The research and expert teams agreed upon the goals, population, context and concept to be evaluated in this SSR. The two teams then agreed that the primary research question should be “What is known about teaching and evaluating communication training programs for HCPs in the ICU setting?” The secondary research questions were “How are communication skills taught and assessed in the ICU setting?” and “How effective have such interventions been as described in the published literature?”
2) Inclusion criteria: A Population, Intervention, Comparison, Outcome, Study Design (PICOS) format was adopted to guide the research process (Peters, Godfrey, Khalil, et al., 2015a; Peters, Godfrey, McInerney, et al., 2015b) (Table 1).
|
PICOS |
Inclusion Criteria |
Exclusion Criteria |
|
Population |
· Undergraduate and postgraduate healthcare providers (e.g. doctors, medical students, nurses, social workers) within ICU setting · ICU settings including medical, surgical, cardiology and neurology ICU · Communication between healthcare providers and patients in the ICU, or between healthcare providers in the ICU and patients’ families · Communication between or within healthcare providers’ teams in the ICU |
· Articles focusing solely on neonatal/ paediatric ICU setting · Articles focusing solely on speech therapy/ physical therapy/ occupational therapy · Non-ICU settings (e.g. general wards, emergency department) · Non-medical professions (e.g. Science, Veterinary, Dentistry) · Communication carried out over technological platforms |
|
Intervention |
· Need for/ importance of interventions to teach communication in ICU setting · Facilitators and barriers to teaching communication in ICU setting · Recommendations, interventions, methods (e.g. tools, simulations, videos), curriculum content and assessments used for teaching communication in ICU setting |
|
|
Comparison |
· Comparisons of various interventions, methods, curricula and evaluation methods used to teach or assess communication in ICU setting and its impact upon patients, healthcare providers, healthcare, and society |
|
|
Outcome |
· Impact of interventions on patients, healthcare providers, healthcare, and society · Evaluation methods to assess interventions, methods, or curriculum used to teach communication |
|
|
Study design |
· Articles in English or translated to English · All study designs including: o Mixed methods research, meta-analyses, systematic reviews, randomised controlled trials, cohort studies, case-control studies, cross-sectional studies, and descriptive papers o Case reports and series, ideas, editorials, and perspectives · Publication dates: 1st January 2000 – 31st December 2019 · Databases: PubMed, ERIC, JSTOR, Embase, CinaHL, Scopus, PsycINFO, Google Scholar |
|
Table 1. PICOS
Nine members of the research team carried out independent searches for articles published between 1st January 2000 – 31st December 2019 in eight bibliographic databases (PubMed, ERIC, JSTOR, Embase, CINAHL, Scopus, Psycinfo and Google Scholar). The searches were carried out between 27th January 2020 and 14th February 2020. The PubMed search strategy can be found in Supplementary Material A. An independent hand search was done to identify key articles.
3) Extracting and charting: Nine members of the research team independently reviewed the titles and abstracts identified and created individual lists of titles to be included which were discussed online. Consensus was achieved on the final list of articles to be included using (Sambunjak, Straus, & Marusic, 2010)’s “negotiated consensual validation” approach through collaborative discussion and negotiation on points of disagreement on online meetings.
B. Stage 2. Split Approach
Working in three independent groups, the reviewers analysed the included articles using the ‘split approach’ (Ng et al., 2020). In one group, four researchers independently reviewed and summarised all the included articles in keeping with according recommendations set out by Wong, Greenhalgh, Westhorp, Buckingham, and Pawson (2013)’s “RAMESES publication standards: meta-narrative reviews” and Popay et al. (2006)’s “Guidance on the conduct of narrative synthesis in systematic reviews”. The four research team members then discussed their individual findings at online meetings and employed ‘negotiated consensual validation’ to achieve consensus on the tabulated summaries (Sambunjak et al., 2010). The tabulated summaries served to highlight key points from the included articles.
The four members of the research team also employed the Medical Education Research Study Quality Instrument (MERSQI) (Reed et al., 2008) and the Consolidated Criteria for Reporting Qualitative Studies (COREQ) (Tong, Sainsbury, & Craig, 2007) also evaluated the quality of qualitative and quantitative studies included in this review.
Concurrently, the second group of five researchers analysed all the included articles using (Braun & Clarke, 2006)’s approach to thematic analysis then discussed their individual findings at online meetings and employed ‘negotiated consensual validation’ to achieve consensus on the final themes (Sambunjak et al., 2010). The third group of four researchers employed Hsieh and Shannon (2005)’s approach to directed content analysis to independently analyse all the included articles, discussed their independent findings online and employed ‘negotiated consensual validation’ to achieve consensus on the final themes (Sambunjak et al., 2010). This split approach consisting of the tabulated summaries and concurrent thematic analysis and content analysis enhances the reliability of the analyses. The tabulated summaries also help ensure that important themes are not lost.
1) Thematic analysis: Phase 1 of Braun and Clarke (2006)’s approach saw the team ‘actively’ reading the included articles to find meaning and patterns in the data. In phase 2, ‘codes’ were constructed from the ‘surface’ meaning (Braun & Clarke, 2006; Sawatsky, Parekh, Muula, Mbata, & Bui, 2016; Voloch, Judd, & Sakamoto, 2007) and collated into a code book to code and analyse the rest of the articles using an iterative step-by-step process. As new codes emerged, these were associated with previous codes and concepts (Price & Schofield, 2015). In phase 3, the categories were organised into themes that best depict the data. In phase 4, the themes were refined to best represent the whole data set and discussed. In phase 5, the research team discussed the results of their independent analysis online and at reviewer meetings. “Negotiated consensual validation” was used to determine a final list of themes (Sambunjak et al., 2010).
2) Directed content analysis: Hsieh and Shannon (2005)’s approach to directed content analysis (Hsieh & Shannon, 2005) was employed in three stages.
Using deductive category application (Elo & Kyngäs, 2008; Wagner-Menghin, de Bruin, & van Merriënboer, 2016), the first stage (Mayring, 2004; Wagner-Menghin et al., 2016) saw codes drawn from the article “Enhancing collaborative communication of nurse and physician leadership into two intensive care units” (D. K. Boyle & Kochinda, 2004). Drawing upon Mayring (2004)’s account, each code was defined in the code book that contained “explicit examples, definitions and rules” drawn from the data. The code book served to guide the subsequent coding process.
Stage 2 saw the four reviewers using the ‘code book’ to independently extract and code the relevant data from the included articles. Any relevant data not captured by these codes were assigned a new code that was also described in the code book. In keeping with deductive category application (Wagner-Menghin et al., 2016), coding categories and their definitions were revised. The final codes were compared and discussed with the final author to enhance the reliability of the process (Wagner-Menghin et al., 2016). The final author checked the primary data sources to ensure that the codes made sense and were consistently employed. The reviewers and the final author used “negotiated consensual validation” to resolve any differences in the coding (Sambunjak et al., 2010). The final categories were selected (Neal, Neal, Lawlor, Mills, & McAlindon, 2018) based on whether they appeared in more than 70% of the articles reviewed (Curtis et al., 2001b; Humble, 2009).
The narrative produced was guided by the Best Evidence Medical Education (BEME) Collaboration guide (Haig & Dozier, 2003) and the STORIES (Structured approach to the Reporting In healthcare education of Evidence Synthesis) statement (Gordon & Gibbs, 2014).
III. RESULTS
9532 abstracts were identified from ten databases, 239 articles reviewed, and 63 articles were included as shown in Figure 2 (Moher, Liberati, Tetzlaff, & Altman, 2009).
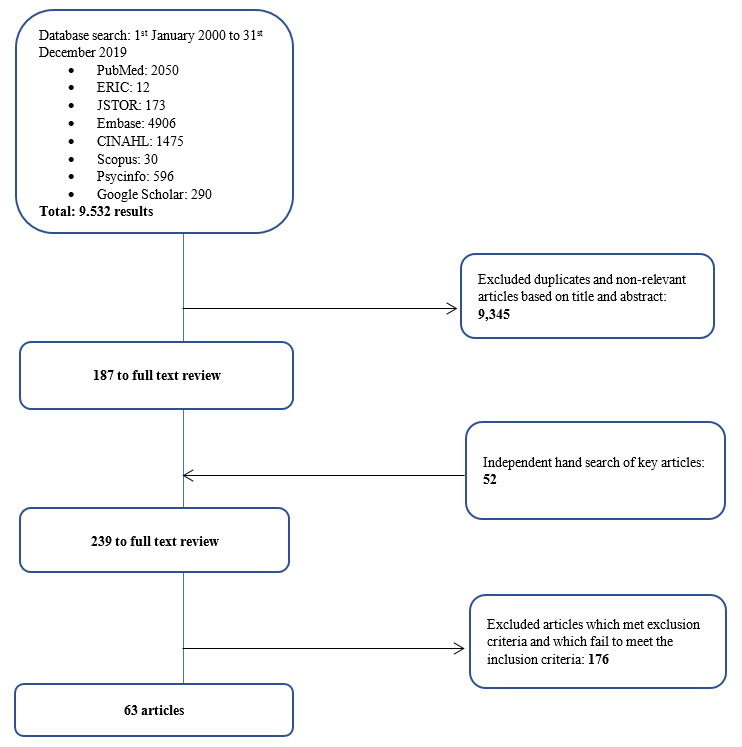
Figure 2. PRISMA Flowchart
3) Comparisons between summaries of the included articles, thematic analysis and directed content analysis: In keeping with SEBA approach the findings of each arm of the split approach was discussed amongst the research and expert teams. The themes identified using Braun and Clarke (2006)’s approach to thematic analysis were how to teach and evaluate communication training in ICU and the factors affecting training.
The categories identified using Hsieh and Shannon (2005)’s approach to directed content analysis were 1) strategies employed to teach communication, 2) factors affecting communication training, 3) strategies employed to evaluate communication, and 4) outcomes of communication training. These categories reflected the major issues identified in the tabulated summaries.
These findings were reviewed with the expert team who agreed that given that the themes identified could be encapsulated by the categories identified, the categories and the themes will be presented together.
a) Strategies employed to teach communication in ICU: 61 articles described various interventions used to teach communication in the ICU. 19 involved ICU physicians, 18 involved ICU nurses, 4 saw participation of ICU physicians and nurses, 13 included the multidisciplinary team in the ICU, 1 was aimed at medical interns, 2 at medical students, 2 at nursing students, and 2 at both medical and nursing students. Given the overlap between teaching strategies, topics taught, and assessment methods employed in ICU communication training for nurses, doctors, nursing and medical students and HCPs in the literature, we discuss and generalise the results across HCPs.
In curriculum design, seven studies (D. K. Boyle & Kochinda, 2004; Hope et al., 2015; Krimshtein et al., 2011; Lorin, Rho, Wisnivesky, & Nierman, 2006; McCallister, Gustin, Wells-Di Gregorio, Way, & Mastronarde, 2015; Miller et al., 2018; Sullivan, Rock, Gadmer, Norwich, & Schwartzstein, 2016) designed a curriculum based on extensive reviews of literature on teaching communication. Brunette and Thibodeau-Jarry (2017) used Kern’s 6-step approach to curriculum development to design a structured curriculum targeted at meeting the needs identified whilst Sullivan et al. (2016) and Lorin et al. (2006) used the authors’ own experiences in tandem with existing literature to guide curriculum design. W. G. Anderson et al. (2017) designed a communication training workshop based on behaviour theories whilst McCallister et al. (2015) based their curriculum on principles of shared decision-making and patient-centred communication. Northam, Hercelinskyj, Grealish, and Mak (2015) conducted a pilot study before implementing their intervention.
Topics included in the curriculum were categorised into “core topics”, or topics essential to the curriculum, and “advanced” which may be useful to incorporate into the curriculum. Core topics were deemed as topics that were most frequently cited in the literature or are crucial across a variety of interactions in the ICU setting such as history taking, relationship skills as well as on common scenarios in the ICU such as breaking bad news and communicating difficult decisions. “Advanced’ topics, though important, are not mentioned as frequently and appeared to be more site specific and sociocultural and ethical issues. These topics are outlined in Table 2 (full table with references found in Supplementary Material B). The methods employed are outlined in Table 3 (full table with references found in Supplementary Material C).
|
|
Curriculum |
|
Core curriculum content |
Communication skills – With families (n=25) – With patients (n=5) – With HCPs (n=12) – General principles |
|
Breaking bad news |
|
|
Understanding/defining goals of care, building therapeutic relationships with families, setting goals and expectations, shared decision making |
|
|
Eliciting understanding and providing information about a patient’s clinical status |
|
|
Relationship skills – Recognising and dealing with strong emotions – Empathy Relationship skills include the “key principles” of esteem, empathy, involvement, sharing, and support |
|
|
Problem solving/conflict management/facing challenges |
|
|
Frameworks for good communication – Ask-Tell-Ask – “Tell Me More” – “SBAR” – Situation, Background, Assessment, Recommendation: to share information obtained in discussions with patients or family members with other HCPs – “3Ws” – What I see, What I’m concerned about, and What I want – Four-Step Assertive Communication Tool – get attention, state the concern (eg, “I’m concerned about…” or “I’m uncomfortable with…”), offer a solution, and get resolution by ending with a question (eg, “Do you agree?”) – “4 C’s” palliative communication model: a. Convening – ensuring necessary communication occurs between the patient, family, and interprofessional team; b. Checking – for understanding; c. Caring – conveying empathy and responding to emotion; and d. Continuing – following up with patients and families after discussions to provide support and clarify information. – ‘‘Communication Strategy of the Week’’ using teaching posters – PACIENTE Interview (Introduce yourself, Listen carefully, Tell you the diagnosis, Advises treatment, Exposes the prognosis, Appoints the bad news introductory phrases, Takes time to comfort empathic, Explains a plan of action involving the family) – Stages of communication (open, clarify, develop, agree, close) – Processes of communication (procedural suggestions, check for understanding) – Explain illness in clear, simple terms – Using a reference manual and pocket reference cards – How HCPs should introduce himself to patients/family members/other HCPs |
|
|
ICU decision making – Survival after CPR – DNR discussions – Prognostication – Legal and ethical issues surrounding life-sustaining treatment decisions – Withdrawing therapies |
|
|
Advanced Topics |
Ethics – Eg. Offering organ donation |
|
Cultural/spirituality/religious issues |
|
|
Leadership |
|
|
Roles and responsibilities in communication with patients and families |
|
|
Discussing patient safety incidents |
|
|
Integration of 5 common behaviour theories: health belief model, theory of planned behaviour, social cognitive theory, an ecological perspective, and transtheoretical model |
|
|
Law |
Table 2. Topics taught
|
Methods Employed |
Number of Studies |
|
Didactic Teaching, which may be employed in conjunction with other methods in a structured programme |
20 |
|
Simulated scenarios with family members/ standardised patients |
17 |
|
Role-play |
12 |
|
Use of simulation technology such as with mannequins |
6 |
|
Group discussions, group reflections and team-based learning |
7 |
|
Case presentations, case discussions and patient care conferences |
4 |
|
Online videos |
3 |
|
Online Powerpoint slides |
3 |
|
Did not specify |
9 |
Table 3. Pedagogy
b) Factors affecting communication training: Identifying facilitators and barriers are critical to the success of communication programmes. Facilitators and barriers to training may be found in Table 4 (full table with references may be found in Supplementary Material D).
|
Facilitators |
Barriers |
|
Longitudinal, structured process with horizontal and vertical integration |
Lack of time |
|
Safe learning environment |
Resource constraints |
|
Clear programme objectives and programme content |
Poor design and a lack of longitudinal support |
|
Funding for training |
Insecurity and awkwardness during simulations |
|
Simulated patients |
Disrupted training |
|
Protected time for training |
Programmes that were not pitched at the right level |
|
Faculty experts helping to plan and review curricula and implement interventions |
Training that is not learner centered |
|
Stakeholders’ engagement to facilitate interprofessional collaboration, as well as debriefing and program feedback |
Training that lacked feedback or debrief sessions |
|
Reflective practice |
Lack of a longitudinal aspect to training |
|
Timely and appropriate feedback |
A lack of a supportive environment in which HCPs can apply the skills learnt |
|
Multidisciplinary learning |
Discordance between physicians’ and nurses’ communication with families |
|
Role modeling |
|
|
Peer support |
Table 4. Facilitators and barriers to training
c) Strategies employed to evaluate communication training: Thirty-nine articles discussed evaluation methods of communication training. The assessment methods are described as follows in Table 5 (full table with references may be found in Supplementary Material E).
|
Method |
|
|
Self-assessment |
|
|
1 |
Quantitative and qualitative surveys were administered to learners to assess their knowledge, experience in the programme, and perceived preparedness, comfort and confidence in communicating |
|
1.1 |
Some programmes only used post-intervention assessments |
|
1.2 |
Others used a combination of pre- and post-intervention assessments of learners |
|
1.3 |
Some programmes adapted existing tools to conduct post-intervention surveys to evaluate learners’ experiences and skills learnt |
|
Feedback from Others |
|
|
2 |
patients, family members, peers and simulated patients was obtained through a combination of surveys and interviews that assessed their level of satisfaction with learners’ communication skills |
|
Observation |
|
|
3 |
Direct observation of HCPs’ communication skills to ascertain the frequency, quality, success and ease of communication post-intervention. This was done through the use of modified communication tools and feedback forms |
|
Debriefing Sessions |
|
|
4 |
One study used debriefing sessions to understand shared experiences of learners. |
Table 5. Assessment Methods
d) Outcomes of communication training: The outcomes of communication training may be mapped to 5 levels of the Adapted Kirkpatrick’s Hierarchy (Jamieson, Palermo, Hay, & Gibson, 2019; Littlewood et al., 2005; Roland, 2015) allowing outcome measures used were also identified. Majority of the programmes achieved Level 2a and Level 2b outcomes as shown in Table 6 (full table with references may be found in Supplementary Material F). 40 articles described successes and three articles described variable outcomes of teaching communications.
|
Adapted Kirkpatrick’s Hierarchy |
Items evaluated |
|
Level 1 (participation) |
Experience in the programme |
|
Assessment of programme’s effectiveness |
|
|
Trainee satisfaction |
|
|
Programme completion |
|
|
Level 2a (attitudes and perception) |
Attitudes towards/ experience with communication |
|
Self-rated confidence/ preparedness in communication |
|
|
Colleagues’ satisfaction with communication |
|
|
Trainees’ views on training programme (e.g. satisfaction, perceived effectiveness) |
|
|
Self-perceived job stress/ job satisfaction |
|
|
Level 2b (knowledge and skills) |
Self-rated skill level using Likert scales |
|
Form asking trainees to list/ indicates skills they learnt during the programme |
|
|
Self-rated knowledge level using Likert scales |
|
|
Self-evaluation of communication skills using validated tools |
|
|
Evaluation of trainees’ knowledge by faculty/ experts |
|
|
Evaluation of trainees’ communication skills by faculty/ experts |
|
|
Level 3 (behavioural change) |
Feedback from peers and facilitators on interactions with actors |
|
Records of ICU rounds |
|
|
Notes from colleagues documenting supportive environment and involvement in communication |
|
|
Frequency of usage of communication skills taught |
|
|
Workplace observations |
|
|
Evaluation of trainees’ communication skills in clinical setting by patients and colleagues |
|
|
Level 4a (increased interprofessional collaboration) |
Workplace observations |
|
Level 4b (patient benefits) |
Self-perceived quality of care |
|
Patient and family satisfaction with communication |
|
|
Family satisfaction with communication |
Table 6. Outcome Measures mapped onto Adapted Kirkpatrick’s Hierarchy
Three studies compared outcomes with non-intervention arms and reported improved patient satisfaction and self-rated and third party reported improvements in communication (Awdish et al., 2017; Happ et al., 2014; McCallister et al., 2015).
C. Stage 3: Jigsaw Perspective
The jigsaw perspective builds upon Moss and Haertel’s (2016) concept of methodological pluralism and sees data from different methodological approaches as pieces of a jigsaw providing a partial picture of the area of interest. The Jigsaw perspective brings data from complementary pieces of the training process in order to paint a cohesive picture of ICU communication training. As a result, related aspects of the training structure and the working culture were studied together so as to better understand the influences each of the aforementioned have on the other.
D.Stage 4. An Iterative Process
Whilst there was consensus on the themes/categories identified, the expert team and stakeholders raised concerns that data from grey literature which is neither quality assessed nor necessarily evidenced based could bias the discussion. To address this concern, the research team thematically analysed the data from grey literature and non-research-based pieces such as letters, opinion and perspective pieces, commentaries and editorials drawn from the bibliographic databases separately and compared these themes against themes drawn from peer reviewed evidenced based data. This analysis revealed the same themes with an additional tool (PACIENTE tool) identified in the grey literature to enhance communication with patients’ families (Pabon et al., 2014).
IV. DISCUSSION
E. Stage 5. Synthesis of Systematic Scoping Review in SEBA
This SSR in SEBA reaffirms the importance of communications training in ICU and suggests that a combination of training techniques is required (Akgun & Siegel, 2012; Chiarchiaro et al., 2015; Happ et al., 2010; Happ et al., 2015; Hope et al., 2015; Lorin et al., 2006; Miller et al., 2018; Roze des Ordons, Doig, Couillard, & Lord, 2017; Sandahl, et al., 2013; D. J. Shaw, Davidson, Smilde, Sondoozi, & Agan, 2014).
A framework for the design of a competency-based approach to ICU communications training (W. G. Anderson et al., 2017; Berkenstadt et al., 2013; D. Boyle et al., 2016; Brown, Durve, Singh, Park, & Clark, 2017; Chiarchiaro et al., 2015; Fins & Solomon, 2001; Happ et al., 2010; Hope et al., 2015; Karlsen, Gabrielsen, Falch, & Stubberud, 2017; Pabon et al., 2014; Roze des Ordons et al., 2017; Tamerius, 2013; J. Yuen & Carrington Reid, 2011) may be found in Figure 3 below.
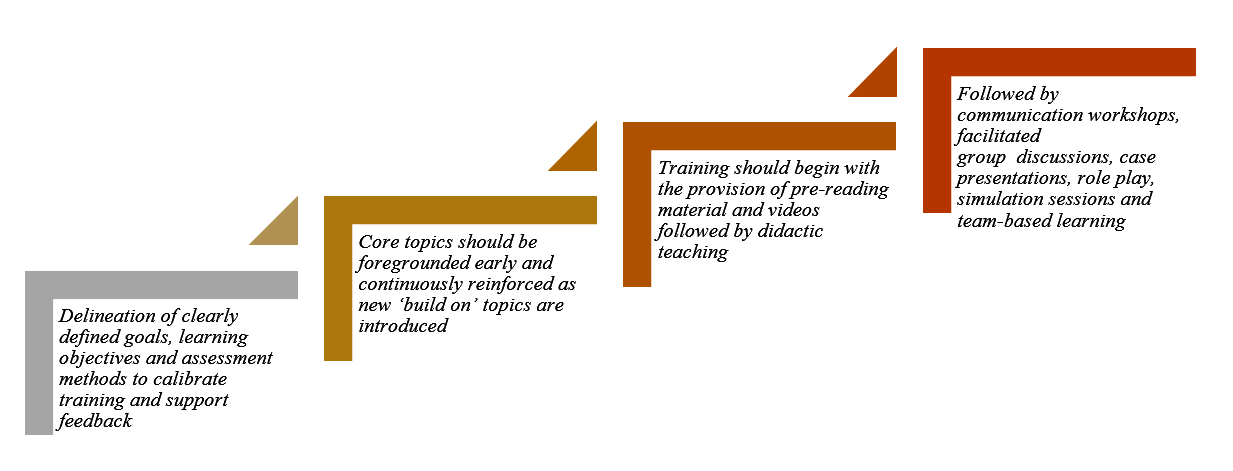
Figure 3. Framework for Competency-based Approach to ICU Communication Skills Training
These findings resonate with Kirkpatrick’s Hierarchy (Jamieson et al., 2019; Littlewood et al., 2005; Roland, 2015) where each level builds upon the next and the learner moves from “peripheral participation” to active “doing and internalising” in real clinical practice.
Such a competency-based programme necessitates a structured approach to holistic and longitudinal assessments of the learner’s progress. Such a structured approach must be horizontally and vertically integrated into other forms of clinical training as cogent communication is a fundamental skillset across all practice and specialties (Akgun & Siegel, 2012; Roze des Ordons et al., 2017).
Whilst Kirkpatrick’s Hierarchy offers a viable framework for assessing trainees’ progress (Boothby, Gropelli, & Succheralli, 2018; Roze des Ordons et al., 2017), ICU training programmes may also keep in mind the various outcomes measures listed previously in Table 3 when designing assessment tools. These tools should conscientiously account for perspectives offered by trainers, standardised patients and family members involved in the evaluation process and should consider benefits and repercussions of their communication abilities to patients, families and the ICU multidisciplinary team(Aslakson, Randall Curtis, & Nelson, 2014; Awdish et al., 2017; Blackhall et al., 2014; D. A. Boyle et al., 2017; DeMartino, Kelm, Srivali, & Ramar, 2016; Happ et al., 2014; Happ et al., 2015; Hope et al., 2015; Miller et al., 2018; Sanchez Exposito et al., 2018; Sullivan et al., 2016; Turkelson, Aebersold, Redman, & Tschannen, 2017).
With flexibility within training programmes highlighted as essential (Ernecoff et al., 2016), this flexibility should also extend to cover remediation and provision of additional support in areas jointly identified and agreed upon by trainees and trainers to be paramount for targeted improvement. As it is worrying that no studies have focused on the effects of remediation on ICU communication skills training thus far, this should be a critical area for future research considering its importance (Steinert, 2013).
Likewise, it is pivotal that trainers should undergo rigorous training (Berlacher et al., 2017; Roze des Ordons et al., 2017) and are granted protected time for this undertaking (Boothby et al., 2018; Happ et al., 2010; Roze des Ordons et al., 2017). In order to ensure that quality and up-to-date skills and knowledge are transferred down the line, it is posited that trainers should also be holistically and longitudinally assessed alongside their charges (Roze des Ordons et al., 2017). Whilst trainers should ideally nurture a safe, collaborative, learning environment for all (Hales & Hawryluck, 2008; Milic et al., 2015; Roze des Ordons et al., 2017; Sandahl, et al., 2013), it is clear that this can only be achieved through sustained administrative and financial support, according learners and trainers sufficient time and resources to foster cordial relationships open to mutual and honest feedback (Akgun & Siegel, 2012; Miller et al., 2018).
V. LIMITATIONS
The SSR in SEBA approach is robust, reproducible and transparent addressing many of the concerns about inconsistencies in SSR methodology and structure arising from diverse epistemological lenses and lack of cogency in weaving together context-sensitive medical education programmes. Through a reiterative step-by-step process, the hallmark ‘Split Approach’ which saw concurrent and independent analyses and tabulated summaries by separate teams of researchers allowed for a holistic picture of prevailing ICU communications training programmes without loss of any conflicting data. Consultations with experts every step of the way also significantly curtailed researcher bias and enhanced the accountability and coherency of the data.
Yet it must be acknowledged that this SSR focused on articles published in English or with English translations. Hence, much of the data comes from North American and European countries, potentially skewing perspectives and raising questions as to the applicability of these findings in the setting of other cultures. Moreover, whilst databases used were selected by the expert team and the team utilised independent selection processes, critical papers may still have been unintentionally omitted. Whilst use of thematic analysis to review the impact of the grey literature greatly improves transparency of the review, inclusion of grey literature-based themes may nonetheless bias results and provide these opinion-based views with a ‘veneer of respectability’ despite a lack of evidence to support it.
VI. CONCLUSION
In the absence of a standardised evidence-based communication training programme for HCPs in ICUs, many HCPs are left in the hope that clinical experience alone will be sufficient to ensure their proficiency in communication. This SSR provides guidance on how to effectively develop and structure a communications training programme for HCPs in ICUs and suggests that communications training in ICU must involve a structured multimodal approach to training carried out in a supportive learning environment. This must be accompanied by robust methods of assessment and personalised and timely feedback and support of the trainees. Such an approach will equip HCPs with greater confidence and preparedness in a variety of situations, including that of the evolving COVID-19 pandemic.
To effectively institute change in communication training within ICUs, further studies should look into the desired characteristics of trainers and trainees, the context and settings as well as the case scenarios used. The design of an effective tool to evaluate learners’ communication skills longitudinally, holistically, and in different settings should be amongst the primary concerns for future research.
Notes on Contributors
Dr EWYC recently graduated from Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms HH is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms SG is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms MTP is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms CCYL is a nursing student at Alice Lee Centre for Nursing Studies, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms LHET is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Dr MSQK recently graduated from Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Dr KTT recently graduated from Yong Loo Lin School of Medicine, National University of Singapore. He was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms YTO is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Mr WQL is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. He was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms XHT is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Mr YHT is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. He was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms CSK is a medical student at Yong Loo Lin School of Medicine, National University of Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms AMCC is a senior librarian from Medical Library, National University of Singapore Libraries, National University of Singapore, Singapore. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ms MC is a researcher at the Division of Cancer Education, NCCS. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Dr JXZ is a Consultant at the Division of Supportive and Palliative Care, NCCS. She was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Professor LKRK is a Senior Consultant at the Division of Supportive and Palliative Care, NCCS. He was involved in research design and planning, data collection and processing, data analysis, results synthesis, manuscript writing and review and administrative work for journal submission.
Ethical Approval
This is a systematic scoping review study which does not require ethical approval.
Acknowledgement
This work was carried out as part of the Palliative Medicine Initiative run by the Department of Supportive and Palliative Care at the National Cancer Centre Singapore. The authors would like to dedicate this paper to the late Dr S Radha Krishna whose advice and ideas were integral to the success of this study.
Funding
There is no funding for the paper.
Declaration of Interest
The authors declare that they have no competing interests.
References
Adams, A. M. N., Mannix, T., & Harrington, A. (2017). Nurses’ communication with families in the intensive care unit – A literature review. Nursing in Critical Care, 22(2), 70-80. https://doi.org/10.1111/nicc.12141
Ahrens, T., Yancey, V., & Kollef, M. (2003). Improving family communications at the end of life: implications for length of stay in the intensive care unit and resource use. American Journal of Critical Care, 12(4), 317-323. https://doi.org/10.4037/ajcc2003.12.4.317
Akgun, K. M., & Siegel, M. D. (2012). Using standardized family members to teach end-of-life skills to critical care trainees. Critical Care Medicine, 40(6), 1978-1980. https://doi.org/10.1097/CCM.0b013e3182536cd1
Anderson, K. G., & Milic, M. (2017). Doctor know thyself: Improving patient communication through modeling and self-analysis. Journal of General Internal Medicine, 32(2), S670-S671.
Anderson, W. G., Puntillo, K., Cimino, J., Noort, J., Pearson, D., Boyle, D., . . . Pantilat, S. Z. (2017). Palliative care professional development for critical care nurses: A multicenter program. American Journal of Critical Care, 26(5), 361-371. https://doi.org/10.4037/ajcc2017336
Anstey, M. (2013). Communication training in the ICU: Room for improvement? Critical Care Medicine, 41(12), A179. https://doi.org/10.1097/01.ccm.0000439963.49763.f2
Aslakson, R. A., Curtis, J. R., & Nelson, J. E. (2014). The changing role of palliative care in the ICU. Critical Care Medicine, 42(11), 2418-2428. https://doi.org/10.1097/CCM.0000000000000573
Awdish, R. L., Buick, D., Kokas, M., Berlin, H., Jackman, C., Williamson, C., . . . Chasteen, K. (2017). A communications bundle to improve satisfaction for critically ill patients and their families: A prospective, cohort pilot study. Journal of Pain and Symptom Management, 53(3), 644-649. https://doi.org/10.1016/j.jpainsymman.2016.08.024
Barbour, S., Puntillo, K., Cimino, J., & Anderson, W. (2016). Integrating multidisciplinary palliative care into the ICU (impact-ICU) project: A multi-center nurse education quality improvement initiative. Journal of Pain and Symptom Management, 51(2), 355. https://doi.org/10.1016/j.jpainsymman.2015.12.203
Barth, M., Kaffine, K., Bannon, M., Connelly, E., Tescher, A., Boyle, C., … Ballinger, B. (2013). 827: Goals of care conversations: A collaborative approach to the process in a Surgical/Trauma ICU. Critical Care Medicine, 41(12), A206. https://doi.org/10.1097/01.ccm.0000440065.45453.3f
Berkenstadt, H., Perlson, D., Shalomson, O., Tuval, A., Haviv-Yadid, Y., & Ziv, A. (2013). Simulation-based intervention to improve anesthesiology residents communication with families of critically ill patients–preliminary prospective evaluation. Harefuah, 152(8), 453-456, 500, 499.
Berlacher, K., Arnold, R. M., Reitschuler-Cross, E., Teuteberg, J., & Teuteberg, W. (2017). The Impact of Communication Skills Training on Cardiology Fellows’ and Attending Physicians’ Perceived Comfort with Difficult Conversations. Journal of Palliative Medicine, 20(7), 767-769. https://doi.org/10.1089/jpm.2016.0509
Blackhall, L. J., Erickson, J., Brashers, V., Owen, J., & Thomas, S. (2014). Development and validation of a collaborative behaviors objective assessment tool for end-of-life communication. Journal of Palliative Medicine, 17(1), 68-74. https://doi.org/10.1089/jpm.2013.0262
Bloomer, M. J., Endacott, R., Ranse, K., & Coombs, M. A. (2017). Navigating communication with families during withdrawal of life-sustaining treatment in intensive care: a qualitative descriptive study in Australia and New Zealand. Journal of Clinical Nursing, 26(5-6), 690-697. https://doi.org/10.1111/jocn.13585
Boothby, J., Gropelli, T., & Succheralli, L. (2018). An Innovative Teaching Model Using Intraprofessional Simulations. Nursing Education Perspectives. https://doi.org/10.1097/01.Nep.0000000000000340
Boyle, D., Grywalski, M., Noort, J., Cain, J., Herman, H., & Anderson, W. (2016). Enhancing bedside nurses’ palliative communication skill competency: An exemplar from the University of California academic Hospitals’ qualiy improvement collaborative. Supportive Care in Cancer, 24(1), S25. https://doi.org/10.1007/s00520-016-3209-z
Boyle, D. A., & Anderson, W. G. (2015). Enhancing the communication skills of critical care nurses: Focus on prognosis and goals of care discussions. Journal of Clinical Outcomes Management, 22(12), 543-549.
Boyle, D. A., Barbour, S., Anderson, W., Noort, J., Grywalski, M., Myer, J., & Hermann, H. (2017). Palliative Care Communication in the ICU: Implications for an Oncology-Critical Care Nursing Partnership. Seminars in Oncology Nursing, 33(5), 544-554. https://doi.org/10.1016/j.soncn.2017.10.003
Boyle, D. K., & Kochinda, C. (2004). Enhancing collaborative communication of nurse and physician leadership in two intensive care units. Journal of Nursing Administration, 34(2), 60-70.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
Brown, S., Durve, M. V., Singh, N., Park, W. H. E., & Clark, B. (2017). Experience of ‘parallel communications’ training, a novel communication skills workshop, in 50 critical care nurses in a UK Hospital. Intensive Care Medicine Experimental, 5(2). https://doi.org/10.1186/s40635-017-0151-4
Brunette, V., & Thibodeau-Jarry, N. (2017). Simulation as a Tool to Ensure Competency and Quality of Care in the Cardiac Critical Care Unit. Canadian Journal of Cardiology, 33(1), 119-127. https://doi.org/10.1016/j.cjca.2016.10.015
Cameron, K. (2017). Bridging the Gaps: An Experiential Commentary on Building Capacity for Interdisciplinary Communication in the Cardiac Intensive Care Unit (CICU). Canadian Journal of Critical Care Nursing, 28(2), 53-54.
Cao, V., Tan, L. D., Horn, F., Bland, D., Giri, P., Maken, K., … Nguyen, H. B. (2018). Patient-Centered Structured Interdisciplinary Bedside Rounds in the Medical ICU. Critical Care Medicine, 46(1), 85-92. https://doi.org/10.1097/ccm.0000000000002807
Centofanti, J., Duan, E., Hoad, N., Swinton, M., Perri, D., Waugh, L., . . . Cook, D. (2015). Improving an ICU daily goals checklist: Integrated and end-of-grant knowledge translation. Canadian Respiratory Journal, 22(2), 80.
Centofanti, J., Duan, E., Hoad, N., Waugh, L., & Perri, D. (2012). Residents’ perspectives on a daily goals checklist: A mixed-methods study. Critical Care Medicine, 40(12), 150. https://doi.org/10.1097/01.ccm.0000425605.04623.4b
Chiarchiaro, J., Schuster, R. A., Ernecoff, N. C., Barnato, A. E., Arnold, R. M., & White, D. B. (2015). Developing a simulation to study conflict in intensive care units. Annals of the American Thoracic Society, 12(4), 526-532. https://doi.org/10.1513/AnnalsATS.201411-495OC
Cicekci, F., Duran, N., Ayhan, B., Arican, S., Ilban, O., Kara, I., … Kara, I. (2017). The communication between patient relatives and physicians in intensive care units. BMC Anesthesiology, 17(1), 97. https://doi.org/10.1186/s12871-017-0388-1
Clark, E., Squire, S., Heyme, A., Mickle, M. E., & Petrie, E. (2009). The PACT Project: Improving communication at handover. Medical Journal of Australia, 190(S11), S125-S127. https://doi.org/10.5694/j.1326-5377.2009.tb02618.x
Crotty, M. (1998). The Foundations of Social Research: Meaning and Perspective in the Research Process. Thousand Oaks, United States: Sage Publications Inc.
Currey, J., Oldland, E., Considine, J., Glanville, D., & Story, I. (2015). Evaluation of postgraduate critical care nursing students’ attitudes to, and engagement with, Team-Based Learning: A descriptive study. Intensive Critical Care Nursing, 31(1), 19-28. https://doi.org/10.1016/j.iccn.2014.09.003
Curtis, J. R., Engelberg, R. A., Wenrich, M. D., Shannon, S. E., Treece, P. D., & Rubenfeld, G. D. (2005). Missed opportunities during family conferences about end-of-life care in the intensive care unit. American Journal of Respiratory & Critical Care Medicine, 171(8), 844-849. https://doi.org/ 10.1164/rccm.200409-1267OC
Curtis, J. R., Patrick, D. L., Shannon, S. E., Treece, P. D., Engelberg, R. A., & Rubenfeld, G. D. (2001a). The family conference as a focus to improve communication about end-of-life care in the intensive care unit: Opportunities for improvement. Critical Care Medicine, 29(2 Suppl), N26-33.
Curtis, J. R., Wenrich, M. D., Carline, J. D., Shannon, S. E., Ambrozy, D. M., & Ramsey, P. G. (2001b). Understanding physicians’ skills at providing end‐of‐life care: Perspectives of patients, families, and health care workers. Journal of General Internal Medicine, 16(1), 41-49. https://doi.org/10.1111/j.1525-1497.2001.00333.x
Curtis, J. R., White, D. B., Curtis, J. R., & White, D. B. (2008). Practical guidance for evidence-based ICU family conferences. CHEST, 134(4), 835-843. https://doi.org/10.1378/chest.08-0235
DeMartino, E. S., Kelm, D. J., Srivali, N., & Ramar, K. (2016). Education considerations: Communication curricula, simulated resuscitation, and duty hour restrictions. American Journal of Respiratory and Critical Care Medicine, 193(7), 801-803. https://doi.org/10.1164/rccm.201510-2012RR
Dithole, K. S., Sibanda, S., Moleki, M. M., & Thupayagale ‐ Tshweneagae, G. (2016). Nurses’ communication with patients who are mechanically ventilated in intensive care: the Botswana experience. International Nursing Review, 63(3), 415-421. https://doi.org/10.1111/inr.12262
Dorner, L., Schwarzkopf, D., Skupin, H., Philipp, S., Gugel, K., Meissner, W., … Hartog, C. S. (2015). Teaching medical students to talk about death and dying in the ICU: Feasibility of a peer-tutored workshop. Intensive Care Medicine, 41(1), 162-163. https://doi.org/10.1007/s00134-014-3541-z
Downar, J., Knickle, K., Granton, J. T., & Hawryluck, L. (2012). Using standardized family members to teach communication skills and ethical principles to critical care trainees. Critical Care Medicine, 40(6), 1814-1819. https://doi.org/10.1097/CCM.0b013e31824e0fb7
Elo, S., & Kyngäs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107-115. https://doi.org/10.1111/j.1365-2648.2007.04569.x
Ernecoff, N. C., Witteman, H. O., Chon, K., Buddadhumaruk, P., Chiarchiaro, J., Shotsberger, K. J., … & Lo, B. (2016). Key stakeholders’ perceptions of the acceptability and usefulness of a tablet-based tool to improve communication and shared decision making in ICUs. Journal of Critical Care, 33, 19-25. https://doi.org/10.1016/j.jcrc.2016.01.030
Fins, J. J., & Solomon, M. Z. (2001). Communication in intensive care settings: The challenge of futility disputes. Critical Care Medicine, 29(2 Suppl), N10-N15.
Foa, C., Cavalli, L., Maltoni, A., Tosello, N., Sangilles, C., Maron, I., … Artioli, G. (2016). Communications and relationships between patient and nurse in Intensive Care Unit: Knowledge, knowledge of the work, knowledge of the emotional state. Acta Bio-medica: Atenei Parmensis, 87(4-s), 71-82.
Ford, D. W., Downey, L., Engelberg, R., Back, A. L., & Curtis, J. R. (2012). Discussing religion and spirituality is an advanced communication skill: An exploratory structural equation model of physician trainee self-ratings. Journal of Palliative Medicine, 15(1), 63-70. https://doi.org/10.1089/jpm.2011.0168
Gordon, M., & Gibbs, T. (2014). STORIES statement: Publication standards for healthcare education evidence synthesis. BMC medicine, 12(1), 143.
Haig, A., & Dozier, M. (2003). BEME Guide no 3: Systematic searching for evidence in medical education–Part 1: Sources of information. Medical Teacher, 25(4), 352-363. https://doi.org/ 10.1080/0142159031000136815
Hales, B. M., & Hawryluck, L. (2008). An interactive educational workshop to improve end of life communication skills. Journal of Continuing Education in the Health Professions, 28(4), 241-248; quiz 249-255. https://doi.org/10.1002/chp.191
Happ, M. B., Baumann, B. M., Sawicki, J., Tate, J. A., George, E. L., & Barnato, A. E. (2010). SPEACS-2: intensive care unit “communication rounds” with speech language pathology. Geriatric Nursing, 31(3), 170-177. https://doi.org/10.1016/j.gerinurse.2010.03.004
Happ, M. B., Garrett, K. L., Tate, J. A., DiVirgilio, D., Houze, M. P., Demirci, J. R., … Sereika, S. M. (2014). Effect of a multi-level intervention on nurse–patient communication in the intensive care unit: Results of the SPEACS trial. Heart & Lung: The Journal of Critical Care, 43(2), 89-98. https://doi.org/10.1016/j.hrtlng.2013.11.010
Happ, M. B., Sereika, S. M., Houze, M. P., Seaman, J. B., Tate, J. A., Nilsen, M. L., … Barnato, A. E. (2015). Quality of care and resource use among mechanically ventilated patients before and after an intervention to assist nurse-nonvocal patient communication. Heart & Lung: The Journal of Critical Care, 44(5), 408-415.e402. https://doi.org/10.1016/j.hrtlng.2015.07.001
Havrilla-Smithburger, P., Kane-Gill, S., & Seybert, A. (2012). Use of high fidelity simulation for interprofessional education in an ICU environment. Critical Care Medicine, 40(12), 148. https://doi.org/10.1097/01.ccm.0000425605.04623.4b
Hope, A. A., Hsieh, S. J., Howes, J. M., Keene, A. B., Fausto, J. A., Pinto, P. A., & Gong, M. N. (2015). Let’s talk critical: Development and evaluation of a communication skills training programme for critical care fellows. Annals of the American Thoracic Society, 12(4), 505-511. https://doi.org/10.1513/AnnalsATS.201501-040OC
Hsieh, H.-F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277-1288. https://doi.org/10.1177/1049732305276687
Hughes, E. A. (2010). Crucial conversations: Perceptions of staff and patients’ families of communication in an intensive care unit. Dissertation Abstracts International, 71(5-A), 1548.
Humble, Á. M. (2009). Technique triangulation for validation in directed content analysis. International Journal of Qualitative Methods, 8(3), 34-51. https://doi.org/10.1177/160940690900800305
Jamieson, J., Palermo, C., Hay, M., & Gibson, S. (2019). Assessment practices for dietetics trainees: A systematic review. Journal of the Academy of Nutrition and Dietetics, 119(2), 272-292. e223. https://doi.org/10.1016/j.jand.2018.09.010
Kalocsai, C., Amaral, A., Piquette, D., Walter, G., Dev, S. P., Taylor, P., . . . Gotlib Conn, L. (2018). “It’s better to have three brains working instead of one”: a qualitative study of building therapeutic alliance with family members of critically ill patients. BMC health services research, 18(1), 533. https://doi.org/10.1186/s12913-018-3341-1
Karlsen, M.-M. W., Gabrielsen, A. K., Falch, A. L., & Stubberud, D.-G. (2017). Intensive care nursing students’ perceptions of simulation for learning confirming communication skills: A descriptive qualitative study. Intensive and Critical Care Nursing, 42, 97-104. https://doi.org/http://dx.doi.org/10.1016/j.iccn.2017.04.005
Kirchhoff, K. T., Walker, L., Hutton, A., Spuhler, V., Cole, B. V., & Clemmer, T. (2002). The vortex: Families’ experiences with death in the intensive care unit. American Journal of Critical Care, 11(3), 200-209. https://doi.org/10.4037/ajcc2002.11.3.200
Kleinpell, R. M. (2014). Improving communication in the ICU. Heart and Lung: The Journal of Acute and Critical Care, 43(2), 87. https://doi.org/10.1016/j.hrtlng.2014.01.008
Kow, C. S., Teo, Y. H., Teo, Y. N., Chua, K. Z. Y., Quah, E. L. Y., Kamal, N. H. B. A., . . . Tay, K. T. J. B. M. E. (2020). A systematic scoping review of ethical issues in mentoring in medical schools. BMC Medical Education, 20(1), 1-10. https://doi.org/10.1186/s12909-020-02169-3
Krimshtein, N. S., Luhrs, C. A., Puntillo, K. A., Cortez, T. B., Livote, E. E., Penrod, J. D., & Nelson, J. E. (2011). Training nurses for interdisciplinary communication with families in the intensive care unit: An intervention. Journal of Palliative Medicine, 14(12), 1325-1332. https://doi.org/10.1089/jpm.2011.0225
Krishna, L. K. R., Tan, L. H. E., Ong, Y. T., Tay, K. T., Hee, J. M., Chiam, M., … & Kow, C. S. (2020). Enhancing mentoring in palliative pare: An evidence based mentoring Framework. Journal of Medical Education and Curricular Development, 7, 2382120520957649. https://doi.org/10.1177/2382120520957649
Littlewood, S., Ypinazar, V., Margolis, S. A., Scherpbier, A., Spencer, J., & Dornan, T. (2005). Early practical experience and the social responsiveness of clinical education: Systematic review. The BMJ, 331(7513), 387-391. https://doi.org/ 10.1136/bmj.331.7513.387
Lorin, S., Rho, L., Wisnivesky, J. P., & Nierman, D. M. (2006). Improving medical student intensive care unit communication skills: A novel educational initiative using standardized family members. Critical Care Medicine, 34(9), 2386-2391. https://doi.org/10.1097/01.Ccm.0000230239.04781.Bd
Mayring, P. (2004). Qualitative content analysis. A companion to qualitative research, 1(2004), 159-176.
McCallister, J. W., Gustin, J. L., Wells-Di Gregorio, S., Way, D. P., & Mastronarde, J. G. (2015). Communication skills training curriculum for pulmonary and critical care fellows. Annals of the American Thoracic Society, 12(4), 520-525. https://doi.org/10.1513/AnnalsATS.201501-039OC
Milic, M. M., Puntillo, K., Turner, K., Joseph, D., Peters, N., Ryan, R., … Anderson, W. G. (2015). Communicating with patients’ families and physicians about prognosis and goals of care. American Journal of Critical Care, 24(4), e56-64. https://doi.org/10.4037/ajcc2015855
Miller, D. C., Sullivan, A. M., Soffler, M., Armstrong, B., Anandaiah, A., Rock, L., … Hayes, M. M. (2018). Teaching residents how to talk about death and dying: A mixed-methods analysis of barriers and randomized educational intervention. The American Journal of Hospice & Palliative Care, 35(9), 1221-1226. https://doi.org/10.1177/1049909118769674
Ministry of Health, Singapore. (2020). Updates on COVID-19 (Coronavirus disease 2019) local situation. Retrieved from https://www.moh.gov.sg/covid-19.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine, 151(4), 264-269.
Moss, P. A., & Haertel, E. H. (2016). Engaging methodological pluralism. In Drew H. Gitomer & Courtney A. Bell (Eds) Handbook of Research on Teaching (5th ed., pp. 127-247). Washington, D.C: American Educational Research Association
Motta, M., Ryder, T., Blaber, B., Bautista, M., & Lim-Hing, K. (2018). Multimodal communication enhances family engagement in the neurocritical care unit. Critical Care Medicine, 46, 409. https://doi.org/10.1097/01.ccm.0000528859.01109.0f
Munn, Z., Peters, M. D., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC medical research methodology, 18(1), 143. https://doi.org/10.1186/s12874-018-0611-x
Neal, J. W., Neal, Z. P., Lawlor, J. A., Mills, K. J., & McAlindon, K. (2018). What makes research useful for public school educators? Administration and Policy in Mental Health and Mental Health Services Research, 45(3), 432-446.
Ng, Y. X., Koh, Z. Y. K., Yap, H. W., Tay, K. T., Tan, X. H., Ong, Y. T., … Shivananda, S. J. P. o. (2020). Assessing mentoring: A scoping review of mentoring assessment tools in internal medicine between 1990 and 2019. PLOS One, 15(5), e0232511. https://doi.org/10.1371/journal.pone.0232511
Ngiam, L. X. L., Ong, Y. T., Ng, J. X., Kuek, J. T. Y., Chia, J. L., Chan, N. P. X., … & Ng, C. H. (2020). Impact of caring for terminally ill children on physicians: A systematic scoping review. American Journal of Hospice and Palliative Medicine, 1049909120950301. https://doi.org/10.1177/1049909120950301
Northam, H. L., Hercelinskyj, G., Grealish, L., & Mak, A. S. (2015). Developing graduate student competency in providing culturally sensitive end of life care in critical care environments – A pilot study of a teaching innovation. Australian Critical Care, 28(4), 189-195. https://doi.org/10.1016/j.aucc.2014.12.003
Pabon, M. C., Roldan, V. C., Insuasty, A., Buritica, L. S., Taboada, H., & Mendez, L. U. (2014). Paciente a semi-structured interview enhances family communication in the ICU. Cirtical Care Medicine, 42(12), A1507. https://doi.org/10.1097/01.ccm.0000458108.38450.38
Pantilat, S., Anderson, W., Puntillo, K., & Cimino, J. (2014). Palliative care in university of California intensive care units. Journal of Palliative Medicine, 17(3), A15. https://doi.org/10.1089/jpm.2014.9449
Peters, M. D., Godfrey, C. M., Khalil, H., McInerney, P., Parker, D., & Soares, C. B. (2015a). Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare, 13(3), 141-146. https://doi.org/10.1097/XEB.0000000000000050
Peters, M., Godfrey, C., McInerney, P., Soares, C., Khalil, H., & Parker, D. (2015b). The Joanna Briggs Institute reviewers’ manual 2015: Methodology for JBI scoping reviews. Adelaide, SA: The Joanna Briggs Institute.
Popay, J., Roberts, H., Sowden, A., Petticrew, M., Arai, L., Rodgers, M., … Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme. Version, 1, b92.
Price, S., & Schofield, S. (2015). How do junior doctors in the UK learn to provide end of life care: A qualitative evaluation of postgraduate education. BMC Palliative Care, 14, 45. https://doi.org/10.1186/s12904-015-0039-6
Pring, R. (2000). The ‘False Dualism’ of educational research. Journal of Philosophy of Education, 34(2), 247-260. https://doi.org/10.1111/1467-9752.00171
Rachwal, C. M., Langer, T., Trainor, B. P., Bell, M. A., Browning, D. M., & Meyer, E. C. (2018). Navigating communication challenges in clinical practice: A new approach to team education. Critical Care Nurse, 38(6), 15-22. https://doi.org/10.4037/ccn201874
Reed, D. A., Beckman, T. J., Wright, S. M., Levine, R. B., Kern, D. E., & Cook, D. A. (2008). Predictive validity evidence for medical education research study quality instrument scores: quality of submissions to JGIM’s Medical Education Special Issue. Journal of General Internal Medicine, 23(7), 903-907. https://doi.org/10.1007/s11606-008-0664-3
Roland, D. (2015). Proposal of a linear rather than hierarchical evaluation of educational initiatives: The 7Is framework. Journal of Educational Evaluation for Health Professions, 12. https://doi.org/10.3352/jeehp.2015.12.35
Roze des Ordons, A. L., Doig, C. J., Couillard, P., & Lord, J. (2017). From communication skills to skillful communication: A longitudinal integrated curriculum for critical care medicine fellows. Academic Medicine : Journal of the Association of American Medical Colleges, 92(4), 501-505. https://doi.org/10.1097/ACM.0000000000001420
Roze Des Ordons, A. L., Lockyer, J., Hartwick, M., Sarti, A., & Ajjawi, R. (2016). An exploration of contextual dimensions impacting goals of care conversations in postgraduate medical education. BMC Palliative Care, 15(1). https://doi.org/10.1186/s12904-016-0107-6
Sambunjak, D., Straus, S. E., & Marusic, A. (2010). A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. Journal of General Internal Medicine, 25(1), 72-78. https://doi.org/10.1007/s11606-009-1165-8
Sanchez Exposito, J., Leal Costa, C., Diaz Agea, J. L., Carrillo Izquierdo, M. D., & Jimenez Rodriguez, D. (2018). Ensuring relational competency in critical care: Importance of nursing students’ communication skills. Intensive and Critical Care Nursing, 44, 85-91. https://doi.org/10.1016/j.iccn.2017.08.010
Sandahl, C., Gustafsson, H., Wallin, C. J., Meurling, L., Ovretveit, J., Brommels, M., & Hansson, J. (2013). Simulation team training for improved teamwork in an intensive care unit. International Journal of Health Care Quality Assurance, 26(2), 174-188. https://doi.org/10.1108/09526861311297361
Sawatsky, A. P., Parekh, N., Muula, A. S., Mbata, I., & Bui, T. (2016). Cultural implications of mentoring in sub-Saharan Africa: A qualitative study. Medical Education, 50(6), 657-669. https://doi.org/10.1111/medu.12999
Schick-Makaroff, K., MacDonald, M., Plummer, M., Burgess, J., & Neander, W. (2016). What synthesis methodology should I use? A review and analysis of approaches to research synthesis. AIMS Public Health, 3(1), 172. https://doi.org/10.3934/publichealth.2016.1.172
Shannon, S. E., Long-Sutehall, T., & Coombs, M. (2011). Conversations in end-of-life care: Communication tools for critical care practitioners. Nursing Critical Care, 16(3), 124-130. https://doi.org/10.1111/j.1478-5153.2011.00456.x
Shaw, D., Davidson, J., Smilde, R., & Sondoozi, T. (2012). Interdisciplinary team training for family conferences in the intensive care unit. Critical Care Medicine, 40(12), 226. https://doi.org/10.1097/01.ccm.0000425605.04623.4b
Shaw, D. J., Davidson, J. E., Smilde, R. I., Sondoozi, T., & Agan, D. (2014). Multidisciplinary team training to enhance family communication in the ICU. Critical Care Medicine, 42(2), 265-271. https://doi.org/10.1097/CCM.0b013e3182a26ea5
Smith, L., O’Sullivan, P., Lo, B., & Chen, H. (2013). An educational intervention to improve resident comfort with communication at the end of life. Journal of Palliative Medicine, 16(1), 54-59. https://doi.org/10.1089/jpm.2012.0173
Steinert, Y. J. M. t. (2013). The “problem” learner: Whose problem is it? AMEE Guide No. 76. 35(4), e1035-e1045. https://doi.org/10.3109/0142159X.2013.774082
Sullivan, A. M., Rock, L. K., Gadmer, N. M., Norwich, D. E., & Schwartzstein, R. M. (2016). The impact of resident training on communication with families in the intensive care unit resident and family outcomes. Annals of the American Thoracic Society, 13(4), 512-521. https://doi.org/10.1513/AnnalsATS.201508-495OC
Tamerius, N. (2013). Palliative care in the ICU: Improving patient outcomes. Journal of Palliative Medicine, 16(4), A19. https://doi.org/10.1089/jpm.2013.9516
Thomson, N., Tan, M., Hellings, S., & Frys, L. (2016). Integrating regular multidisciplinary ‘insitu’ simulation into the education program of a critical care unit. How we do it. Journal of the Intensive Care Society, 17(4), 73-74. https://doi.org/10.1177/1751143717708966
Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349-357. https://doi.org/10.1093/intqhc/mzm042
Turkelson, C., Aebersold, M., Redman, R., & Tschannen, D. (2017). Improving nursing communication skills in an intensive care unit using simulation and nursing crew resource management strategies: An implementation project. Journal of Nursing Care Quality, 32(4), 331-339. https://doi.org/10.1097/NCQ.0000000000000241
Van Mol, M., Boeter, T., Verharen, L., & Nijkamp, M. (2014). To communicate with relatives; An evaluation of interventions in the intensive care unit. Critical Care Medicine, 42(12), A1506-A1507. https://doi.org/10.1097/01.ccm.0000458107.38450.dc
Voloch, K. A., Judd, N., & Sakamoto, K. (2007). An innovative mentoring program for Imi Ho’ola Post-Baccalaureate students at the University of Hawai’i John A. Burns School of Medicine. Hawaii Medical Journal, 66(4), 102-103.
Wagner-Menghin, M., de Bruin, A., & van Merriënboer, J. J. (2016). Monitoring communication with patients: Analyzing judgments of satisfaction (JOS). Advances in Health Sciences Education, 21(3), 523-540. https://doi.org/10.1007/s10459-015-9642-9
Wong, G., Greenhalgh, T., Westhorp, G., Buckingham, J., & Pawson, R. (2013). RAMESES publication standards: Meta-narrative reviews. BMC medicine, 11(1), 20. https://doi.org/ 10.1186/1741-7015-11-20
World Health, O. (2020). Coronavirus disease 2019 (COVID-19) Situation Report. Retrieved from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200330-sitrep-70-covid-19.pdf?sfvrsn=7e0fe3f8_2
Yang, X., Yu, Y., Xu, J., Shu, H., Liu, H., Wu, Y., … Yu, T. (2020). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. The Lancet Respiratory Medicine. https://doi.org/10.1016/S2213-2600(20)30079-5
Yuen, J., & Carrington Reid, M. (2011). Development of an innovative workshop to teach communication skills in goals-of-care discussions in the ICU. Jounral of General Internal Medicine, 26, S605. https://doi.org/10.1007/s11606-011-1730-9
Yuen, J. K., Mehta, S. S., Roberts, J. E., Cooke, J. T., & Reid, M. C. (2013). A brief educational intervention to teach residents shared decision making in the intensive care unit. Journal of Palliative Medicine, 16(5), 531-536. https://doi.org/10.1089/jpm.2012.0356
*Ong Yun Ting
1E Kent Ridge Road,
NUHS Tower Block, Level 11,
Singapore 119228
Tel: +65 6227 3737
Email: e0326040@u.nus.edu
Published online: 7 January, TAPS 2020, 5(1), 8-15
DOI: https://doi.org/10.29060/TAPS.2020-5-1/RA2087
Justin Bilszta1, Jayne Lysk1, Ardi Findyartini2 & Diantha Soemantri2
1Department of Medical Education, Melbourne Medical School, University of Melbourne, Australia; 2Department of Medical Education, Faculty of Medicine, Universitas Indonesia, Indonesia
Abstract
Transnational collaborations in faculty development aim to tackle challenges in resource and financial constraints, as well as to increase the quality of programs by collaborating expertise and best evidence from different centres and countries. Many challenges exist to establishing such collaborations, as well as to long-term sustainability once the collaboration ceases. Using the experiences of researchers from medical schools in Indonesia and Australia, this paper provides insights into establishing and sustaining a transnational collaboration to create a faculty development initiative (FDI) to improve clinical teacher practice. Viewed through the lens of the experiences of those involved, the authors describe their learnings from pathways of reciprocal learning, and a synergistic approach to designing and implementing a culturally resonant FDI. The importance of activities such as needs assessment and curriculum blueprinting as ways of establishing collaborative processes and the bilateral exchange of educational expertise, rather than as a mechanism of curriculum control, is highlighted. The relevance of activities that actively foster cultural intelligence is explored as is the importance of local curriculum champions and their role as active contributors to the collaborative process.
Keywords: Faculty Development, Transnational, Collaboration, Clinical Teacher
Practice Highlights
- Successful transnational collaborative FDI requires genuine collaboration and partnership.
- Curriculum blueprinting with the awareness of cultural nuances is important for a collaborative FDI.
- Long-term sustainability needs to be considered and planned in light of the resource challenges.
I. INTRODUCTION
The opportunities to develop and foster collaborative partnerships across the globe in the field of higher education are growing. There are many forms of transnational collaboration in education; however, the majority of university collaborations are symbolised by ‘providers and buyers’, with buying countries being developing nations and provider countries based in developed ones (Nhan & Nguyen, 2018). This contrasts with non-economically driven forms of transnational collaboration which generally include partnerships looking to expand areas of research, knowledge or working on international curriculum (Carciun & Orosz, 2018), Regardless of the form, research into collaborative international partnerships reveal common challenges including issues of joint decision making, the different learning cultures and hierarchical structures, and sustainability of program outcomes (Allen, 2014; Caniglia et al., 2017; Kim, Lee, Park, & Shin, 2017; Sullivan, Forrester, & Al-Makhamreh, 2010; Yoon et al., 2016). This has implications for any new or emerging form of international collaboration and its continuing success.
One expanding area of non-economically driven transnational collaborations in higher education has been faculty development. These partnerships have been flourishing in many different disciplines and similar challenges concerning the establishment and long term sustainability have been identified. This paper contributes to the study of transnational collaborations in higher education by focusing specifically on faculty development in the field of medical education. It firstly reviews the challenges associated with international collaborations involved in faculty development. The authors then critically reflect on an example of an international collaboration between researchers from medical schools in Indonesia and Australia through the lens of the experiences of those involved.
Faculty development initiatives (FDIs) in medical schools are an inseparable part of the internationalisation of medical education (Harden, 2006). In this era of globalisation, medical faculty should be prepared to teach in a cross-cultural environment (Deardorff, 2009). International collaboration in FDIs aim to tackle challenges in resource and financial constraints as well as to increase the quality of programs by drawing on expertise and best evidence from different centres and countries (Burdick, Amaral, Campos, & Norcini, 2011; Burdick et al., 2010; Harden, 2006; Kim et al., 2015; Yoon et al., 2016). Despite the push to develop international collaborations in FDIs many countries, particularly those in developing nations, find this especially challenging (Kim et al., 2017; Sherman & Chappell, 2018) and there are several reasons for this. The first relates to the dominant model of foreign ownership and control. Whitehead et al. in their recent commentary on this issue highlighted the trend for educational collaborations to flow in one direction – Europe and North American to other parts of the world – with control of the curriculum and academic structures resting with the ‘foreign expert’ (Whitehead, Wondimagegn, Baheretibeb, & Brian, 2018). The second challenge centres around the limitations on the opportunities for faculty development because of heavy teaching loads, a lack of a well-trained faculty who can provide professional training, limited infrastructure and competing demands for research and clinical services (Alkan, 2000). The World Health Organization has recognised this critical problem for faculty development and its long term impact on creating a healthcare workforce fit for purpose in the 21st century (Buchan & Campbell, 2013). As clinical education changes health provider practice, it can have wide-ranging effects on the health of a population, especially in underdeveloped countries (Boulet, Bede, McKinley, & Norcini, 2007). Thus, FDIs must reflect the contexts and requirements of developing countries if they are to surmount these challenges.
Southeast Asia has its specific challenges that need to be recognised. Although in some countries it is heavily modelled on Western education systems, the medical education culture has innumerable adaptations and innovations with identified socio-economic, cultural and institutional barriers (Amin, 2004; Majumder, 2004). Cultural and community needs differ vastly and with one of the smallest number of medical schools per million population (Boulet et al., 2007), the lack of human and institutional capacity to satisfactorily address the healthcare needs of populations in this region is stark (Kanchanachitra et al., 2011). Although there are international FDIs provided by developed countries for academic institutions in Southeast Asia there is limited evidence as to their effectiveness and benefits to teaching practice gained by participants (Phuong, Duong, & McLean, 2015; Steinert et al., 2006). Other commonly cited challenges for FDI development include: a divide between the education contexts and expectations of Asian and Western countries (T. P. Lam & Y. Y. B. Lam, 2009); a lack of English ability which adversely impacts on establishing an effective international collaboration as well as in delivery of the FDI content to participants (Ferry et al., 2006); and where countries in Southeast Asia have tried to develop and implement their own FDIs (World Health Organization, 2013) insufficient resources and shortage of qualified educators result in significant limitations in achieving self-sufficiency.
II. CONTEXT
The Faculty of Medicine Universitas Indonesia (FMUI) and the Cipto Mangunkusumo Hospital, are committed to supporting the role of clinical teachers. An introductory FDI–Clinical Teacher Course (CTC)–has been available since 2008 to clinical teachers wanting to develop their teaching practice. The CTC is designed to support clinicians in the practical delivery of teaching and primarily focuses on the principles and techniques of teaching and supervising in clinical settings, the development of clinical reasoning skills, teaching procedural skills, and assessment practices in clinical settings. Training materials have been developed by the Department of Medical Education FMUI and the trainers are teaching staff from the Universitas Indonesia Academic Health System community. The CTC meets the provision of a minimum of 40 hours of training as regulated by the Directorate General of Higher Education, Ministry of Research and Higher Education and Universitas Indonesia.
In 2015, a formal collaboration (Partnerships in Clinical Education) between FMUI and the University of Melbourne (UoM) Medical School’s Excellence in Clinical Teaching (EXCITE) program was established. EXCITE is a series of linked award courses for clinical teachers from all health-related disciplines, that supports them in the practical delivery of teaching into the clinical workplace and provides a deeper understanding of the theories underpinning clinical education. A key aim of the FMUI–UoM collaboration was to develop an innovative and culturally relevant teaching program for clinical teachers from FMUI, that leveraged pedagogical strengths of the CTC and EXCITE programs and their teaching staff. The impetus for this collaboration was the long-standing professional relationships between academics from UoM and FMUI and was borne from FMUI recognising the need to develop, not just the practical delivery of teaching to their medical students, but opportunities for their clinical teachers to be exposed to cutting-edge clinical education practice. Importantly, any educational initiative needed to consider Indonesian academic and cultural traditions and be developed specifically for Indonesian clinical teachers, rather than simply transplanting or imposing an external (i.e. Western) teaching program ill-suited to the Indonesian context (Bleakley, Brice, & Bligh, 2008; Hodges, Maniate, Martimianakis, Alsuwaidan, & Segouin, 2009; Waterval, Frambach, Driessen, & Scherpbier, 2014).
III. AIMS AND OBJECTIVES
Much of the research into transnational collaborations have focused on the issue pertaining to quality assurance, regulation and accreditation of educational programs; translocation of curriculum and intercultural understanding; institutional and management strategic decision making; and student choice and academic mobility (Kosmützky & Putty, 2015). However, few studies have evaluated the critical factors for the success or failure of sustainable partnerships (Waterval, Driessen, Scherpbier, & Frambach, 2018; Waterval et al., 2014) particularly from the perspective of those who have negotiated the challenges of establishing such a transnational partnership. In this light, the focus of this paper is to provide the reader with insights on how to facilitate transnational collaboration viewed through the lens of the experiences of those involved. Its aim is not to provide a step-by-step process for the development of an FDI but critically reflect on the process by which the collaboration was established, and management of both the partnership and differences in context between medical schools in Indonesia and Australia. When read in conjunction with the companion paper published in the previous issue (Findyartini, Bilszta, Lysk, & Soemantri, 2019), we hope that the reader will gain an appreciation of better ways to foster transnational collaborations to drive educational reform.
IV. INSIGHTS
A. Insight 1 – Actively Foster Genuine Collaboration
Collaboration is a process of working together, which involves not only cooperation and communication, but also trust, respect and understanding, in order to establish an interdependent relationship that will augment the contributions of each party involved (Pike et al., 1993). As outlined, a key focus of the FMUI–UoM collaboration was to consider Indonesian academic and cultural traditions to develop an FDI specifically for Indonesian clinical teachers, rather than simply transplanting or imposing an external (i.e. Western) teaching model.
Research into successful international education partnerships has identified several key elements to ensure success with the most important of these being communication, mutual respect, humility and trust (Tupe, Kern, Salvant, & Talero, 2015). The relevance of a trusting relationship to collaborative performance has been repeatedly emphasised (Bachmann, 2001; Das & Teng, 2001; Fryxell, Dooley, & Vryza, 2002) and Bovill, Jordan, and Watters (2014) have highlighted that partners need to share a sense of mutual responsibility and benefit from a project, contribute expertise, effort and resource equally and for this contribution is to be recognised by the other partner (Bovill et al., 2015).
To ensure that externally the FMUI–UoM partnership was perceived as a genuine collaborative process, one of the very first initiatives undertaken was a needs assessment activity involving a broad mix of clinical teachers from FMUI. This activity was facilitated by staff from the FMUI Department of Medical Education with staff from UoM as active observers. This activity resulted in a mutual sharing of ideas and perspectives thereby allowing clinical teachers from FMUI to 1) share information on the current status of clinical teacher training at FMUI; 2) identify internal and external factors that influence the introduction and efficacy of FDIs at FMUI; 3) reach a consensus on practical visions of future health professions education at FUMI and; 4) discuss methods of delivering FDIs and the pros and cons of each format.
Whilst the focus of the needs assessment was to inform the development of the FDI, the learning for the research team was the importance of active engagement with clinical teaching leaders and a greater understanding for the UoM team of the cultural and academic context in which FMUI clinical teachers deliver their teaching activities. This led to a recognition of the cultural importance of negotiation and discussion when proposing change and of spending time in person and in location with those impacted by change (Tupe et al., 2015; Zhang & Huxham, 2009). Of significance, this activity emphasised the bilateral exchange of educational expertise and experiences rather than a unilateral flow of ideas, materials, and experts from one context (UoM) to another (FMUI) as well as the process of developing the collaborative partnership rather than concentrating merely on the educational product (Keay, May, & O’Mahony, 2014).
Importantly, a small but significant part of actively maintaining a collaborative mindset and approach was regular contact between the researchers, through both formal (e.g. email and exchanging documentation) and informal (e.g. social media) means. These methods of collaboration, whether scheduled or unscheduled, contributed to building and maintaining rapport which then enhanced mutual respect and co-construction of strategies and approaches to achieving the collaborative project goals.
B. Insight 2 – Utilise Curriculum Blueprinting as a Means Rather Than an End
There are three well-documented barriers to curriculum delivery in international partnerships–that a shared curriculum will inevitably result in a ‘variability in expectations, decision-making, and academic performance’ (Coleman, 2003, p. 359); content knowledge and delivery, and teaching skills, will differ between academic contexts (Heffernan & Poole, 2005; Shams & Huisman, 2012); and the inherent weakness of relying only on documents when engaging in curriculum mapping processes as these maps only describe what is intended to take place in the learning environment, not necessarily what does take place (Hays, 2016) and why.
To overcome these barriers a three-step process was undertaken using the paradigm of the designed-delivered-experienced curriculum (Prideaux, 2003): 1) a formalised curriculum blueprinting exercise comparing the CTC and EXCITE program at the Graduate Certificate level (i.e. the designed curriculum); 2) the curriculum map was then supplemented with experiences of the research team who had delivered into their respective FDIs (i.e. the delivered curriculum); and 3) acknowledging the experiences of participants of both FDIs (i.e. the experienced curriculum). This blueprinting activity highlighted areas of pedagogical similarities (e.g. the characteristics of providing effective feedback to students; using OSCEs to assess student performance in the clinical setting) and differences (e.g. engaging peers in a process of peer feedback of teaching) and provided a trigger for frank discussion and reflection, with both groups of researchers freely and honestly questioning the pedagogical decisions made for their individual FDIs. It was through this iterative process of challenge and reflexivity, rather than the blueprinting activity itself, that meant that decisions on the pedagogical framework and selection of teaching and learning activities and education resources was a collaborative and shared process.
Visualising the curriculum and making visible the structure of both programs made decisions related to modifying pedagogical approaches self-evident and consequently, the goals and objectives of the FDI become more important in guiding planning and development, rather than control of the content, and recognition that content can be represented and interpreted from multiple perspectives. Through this process, the curriculum blueprint represented the collaborative thought process used to establish the FDI. The presence of the document encouraged dynamic discussions among the researchers in attempting to create an evidence-based, best practice FDI while still considering the characteristics of those who would be participating.
C. Insight 3 – Awareness of Cultural Nuances is Vital
Successful international collaborations necessarily involve multiple interwoven dimensions of leadership, organisation, collaboration, and personal growth, the relevance of which is inseparable from society and social frameworks (Eldridge & Cranston, 2009). In the context of this project, not only did societal cultural differences have to be considered but also the different academic and clinical medicine and teaching cultures of Australia and Indonesia. When undertaking transnational teaching projects in other countries, it is important that the assumptions made about one’s own and others’ cultures are both questioned (Maher, Sicchia, & Stein, 2003). But this itself provides an opportunity to compare and contrast both cultures, thereby fostering greater understanding, and appreciation of, the nuances of both.
Although the researchers had well established professional and personal relationships and extensive knowledge of both countries and cultures, there was still a need–especially on the side of the UoM team–to observe the Indonesian academic culture in vivo and the interaction and relationships between faculty members from different clinical disciplines. This then needed to be overlayed with an understanding of the social structures which govern Indonesian life and the influences of factors such as age, gender and religious background on how individuals and communities of practice interact. As others have highlighted (Yudhi, Nanere, & Nsubuga-Kyobe, 2006) difficulties in negotiation between Indonesia and Australia can be avoided by having a better cultural understanding of each other.
The aforementioned needs analysis activity was an important lens through which the UoM researchers could observe how clinical teachers as individuals within FMUI interact, as well as how FMUI as an educational organisation functions. This was developed further when the FMUI researchers had the opportunity to audit the EXCITE Graduate Certificate in Clinical Teaching program. This allowed the FMUI researchers to observe the Australian context within the same paradigms as the UoM researchers had the Indonesian context. An outcome of this was the opportunity to compare, contrast and challenge perceptions about teaching and learning in both settings and how this is influenced by social and cultural norms. Extensive discussion within, and between, both teams of researchers were vitally important to explicitly examine, and challenge, established assumptions (Bleakley et al., 2008) around teaching in the clinical environment and the pedagogical structure of an FDI. Early and Ang’s (2003) model of cultural intelligence − cognition (‘do I know what is going on?), motivation (‘am I motivated to act?’ which the research teams re-visualised as ‘what needs to be changed?’) and behaviour (‘can I act appropriately and effectively?’ which again was re-visualised as ‘can I make change appropriately and effectively?’) − provided a framework for these discussions and led to a better understanding of the working context of both partners. As observed by others, the need for genuine respect for complex contexts, practices, and paradigms of thinking, as an integral part of developing cultural competence among the researches, cannot be overemphasised (Mertens, 2009).
D. Insight 4 – Actively Engage and Empower Colleagues to Champion the Work of the Transnational Collaboration
Developing collaborative partnerships based on sustainable equitable relationships in which sociocultural and power differences are acknowledged, demanded participation and a shared vision at every stage of the project (Heron & Reason, 2001). From the outset, both FMUI and UoM had an agreed goal to provide a pathway for FMUI clinical teachers to further develop their teaching practice including articulation into a higher degree program at UoM and/or advanced study in clinical teaching and clinical leadership delivered locally.
Success required, not just a program built on a sold and justifiable pedagogy but ‘buy-in’ from senior clinical teaching leaders who not only share a passion for teaching themselves, but also recognise the need to support the development of junior teachers by exposing them to innovative and best practice methods of teaching training; and long term sustainability through training a pool of FMUI education leaders who could not only deliver the FDI as designed but also make changes in response to feedback from both participants and local needs. Importantly, the collaborative partnership needed to acknowledge the hierarchical nature of academic culture in Indonesia. This type of academic culture has been recognised as a potential impediment to the selection of participants for FDIs as this can restrict the pool of participants because of screening by senior academics and administrators (Kim et al., 2017).
The 1st Advanced Clinical Teacher Training and Training on Trainers Workshop was an important step in ensuring senior clinical teaching/education leaders were involved in the process of developing the FDI, thereby becoming de facto members of the research team, and took ownership of the program structure and curriculum objectives. Importantly, these ‘champions’ were able to describe to their teaching colleagues that rather than a transplanted, imposed and/or culturally misaligned program, the newly developed FDI grew out of a shared desire to create a program developed specifically for Indonesian clinical teachers. At all times the researchers were aware of the risk of education imperialism (Bleakley et al., 2008) and the perception that the UoM approach was the only way to deliver an FDI. The ideas of Bruning, Schraw, and Ronning (1999) and Hodges et al. (2009) resonated with our thinking: that learning is highly dependent on individual and social context and activity (Bruning et al., 1999) and therefore by whose criteria should ‘standards…and other culturally specific constructions associated with the practice of medicine’ (Hodges et al., 2009, p. 916) be applied. It is only through having conversations that acknowledge and address these issues – with clinical teaching/education leaders as both participants of the FDI, as well future program leaders – are the seeds of long-term viability planted. These ‘champions’ become co-creators and owners of the program through active contribution, rather than simply passive recipients of learning.
The companion paper published in this issue explores in detail the experiences of participants from the Training on Trainers Workshop (Findyartini et al., 2019).
E. Insight 5 – Identify Resource Challenges to Implementation and Sustainability
Identifying challenges that impact on, and developing strategies to effectively utilise financial, institutional, and human resources, are vital to developing transnational collaborations that are sustainable (Wiek et al., 2013) and successfully capitalise on intercultural, linguistic, and national differences (Pashby & de Oliveira Andreotti, 2016). Caniglia et al. (2017) in their review of factors that influence sustainability in high education collaborations have identified resource allocation as an important consideration for the implementation of a transitional collaboration.
We would agree, but also argue that resource allocation is important for ensuring sustainability. One of the crucial aspects to the success of this project was the funding from the Australian-Indonesia Institute which allowed the research team to meet regularly face-to-face and attend activities in both countries. However, this grant was limited to costs associated with travel and accommodation and consequently much in-kind support was required from both institutions; for example, none of the costs associated with delivery of the Training the Trainer workshop was covered by the Australia–Indonesia Institute grant and expenses such as room hire, catering and photocopying were provided in-kind by FMUI senior management. Another factor which soon became evident was that much of the success of the collaboration depended on the researchers allocating time from other academic activities which could not be backfilled by other staff. This meant much of the time spent working on this project was after-hours or on the weekend. Further, the involvement of administrative staff from both institutions was limited for similar reasons which meant most of the organisational workload also fell back on the researchers.
Although there is an acknowledgment that goodwill from senior management and a commitment to the partnership are important factors ensuring the success of transnational collaborations, very few studies have formally looked at this and to our knowledge, only one (Caniglia et al., 2017) has attempted to systematically evaluate challenges (such as those described above) and strategies related to financial, institutional, and human resources in relation to implementation and sustainability. Given our experiences of having to find the capacity to undertake tasks peripheral to, but important for the success of, the partnership described in this paper, we see an opportunity for further work in this area.
V. CONCLUSION
The approaches that were undertaken in this project actively sought to develop a non-economically driven partnership between universities from Indonesia and Australia. This focus on expanding knowledge and best-practice teaching training, rather than ‘selling of a product’, resulted in pathways of reciprocal learning, the development of new ways of thinking about clinical teacher training and a synergistic approach to designing and implementing a culturally resonant FDI. As a transnational collaboration, the context and requirements of the Indonesian partner were central to the quality of the FDI, and its sustainability. Shared experiences among the researchers and flexibility to implement the best evidence, with adaptation to local needs and values – often referred to as glocalisation – was a key to success. This, in conjunction with a constructivist approach to curriculum mapping, and negotiation over the pedagogical content of the curriculum, mitigated several challenges identified with establishing successful transnational educational collaborations.
Notes on Contributors
Dr Justin Bilszta is a Senior Lecturer in Medical Education, Department of Medical Education, Melbourne Medical School University of Melbourne.
Dr. Jayne Lysk is a Lecturer in Clinical Education, Department of Medical Education, Melbourne Medical School University of Melbourne.
Dr Ardi Findyartini is a Senior Lecturer in Medical Education, currently the Head of Department of Medical Education and Head of Medical Education Unit, Faculty of Medicine Universitas Indonesia.
Dr Diantha Soemantri is a Senior Lecturer in the Department of Medical Education and currently the Vice Director (Medical Education) of the Indonesian Medical Education and Research Institute (IMERI), Faculty of Medicine Universitas Indonesia.
Ethical Approval
Ethical approval is not required for a program evaluation type of study as employed in this paper.
Acknowledgements
The authors would like to thank the Faculty of Medicine, Universitas Indonesia and the Department of Medical Education, Melbourne Medical School, University of Melbourne for this support of this collaboration.
Funding
This project was supported by the Commonwealth of Australia through the Australia-Indonesia Institute of the Department of Foreign Affairs and Trade (Application No: AII00004 of AII Grant Round 1 2014). Generous in-kind support was provided by Faculty of Medicine, Universitas Indonesia and the Department of Medical Education, Melbourne Medical School, University of Melbourne.
Declaration of Interest
The authors declare that they have no conflict of interest.
References
Alkan, M. L. (2000). The global medical school, 2020. Medical Teacher, 22(5), 527-530.
https://doi.org/10.1080/01421590050110821
Allen, J. F. (2014). Investigating transnational collaboration of faculty development and learning: An argument for making learning culturally relevant. International Journal for the Scholarship of Teaching and Learning, 8(2), Article 17. https://doi.org/10.20429/ijsotl.2014.080217
Amin, Z. (2004). Medical education in Asia: Is it a time for optimism? ANNALS Academy of Medicine Singapore, 33(2), 264-266.
Bachmann, R. (2001). Trust, power and control in trans-organizational relations. Organization Studies, 22(2), 337-365. https://doi.org/10.1177/0170840601222007
Bleakley, A., Brice, J., & Bligh, J. (2008). Thinking the post-colonial in medical education. Medical Education, 42(3), 266-270. https://doi.org/10.1111/j.1365-2923.2007.02991.x
Boulet, J., Bede, C., McKinley, D., & Norcini, J. (2007). An overview of the world’s medical schools. Medical Teacher, 29(1), 20-26. https://doi.org/10.1080/01421590601131823
Bovill, C., Jordan, L., & Watters, N. (2015). Transnational approaches to teaching and learning in higher education: Challenges and possible guiding principles. Teaching in Higher Education, 20(1), 12-23. https:/doi.org/10.1080/13562517.2014.945162
Bruning, R. H., Schraw, G. J., & Ronning, R. R. (1999). Cognitive psychology and instruction. Upper Saddle River, NJ: Prentice Hall.
Buchan, J., & Campbell, J. (2013). Challenges posed by the global crisis in the health workforce. British Medical Journal, 347, f6201-f6201. https://doi.org/10.1136/bmj.f6201
Burdick, W., Amaral, E., Campos, H., & Norcini, J. (2011). A model for linkage between health professions education and health: FAIMER international faculty development initiatives. Medical Teacher, 33(8), 632-637. https://doi.org/10.3109/0142159X.2011.590250
Burdick, W. P., Diserens, D., Friedman, S. R., Morahan, P. S., Kalishman, S., Eklund, M. A., . . . Norcini, J. J. (2010). Measuring the effects of an international health professions faculty development fellowship: The FAIMER Institute. Medical Teacher, 32(5), 414-421. https://doi.org/10.3109/01421590903394587
Caniglia, G., Luederitz, C., Groß, M., Muhr, M., John, B., Keeler, L. W., . . . Lang, D. (2017). Transnational collaboration for sustainability in higher education: Lessons from a systematic review. Journal of Cleaner Production, 168, 764-779. https://doi.org/10.1016/j.jclepro.2017.07.256
Carciun, D., & Orosz, K. (2018). Benefits and costs of transnatioanl collaborative partnerships in higher education. European Expert Network on Economics of Education (EENEE) Analytical Report No 36. Retrieved from http://www.eenee.de/eeneeHome/EENEE/Analytical-Reports.html
Coleman, D. (2003). Quality assurance in transnational education. Journal of Studies in International Education, 7(4), 354-378. https://doi.org/10.1177/1028315303255597
Das, T. K., & Teng, B.-S. (2001). Trust, control and risk in strategic alliances: An integrated framework. Organization Studies, 22(2), 251-283. https://doi.org/10.1177/0170840601222004
Deardorff, D. K. (Ed.) (2009). The SAGE Handbook of Intercultural Competence. Thousand Oaks, CA: SAGE Publications Inc.
Early, P. C., & Ang, S. (2003). Cultural intelligence: Individual interactions across cultures. Stanford, CA: Stanford University Press.
Eldridge, K., & Cranston, N. (2009). Managing transnational education: Does national culture really matter? Journal of Higher Education Policy and Management, 31(1), 67-79. https://doi.org/10.1080/13600800802559286
Ferry, L. H., Job, J., Knutsen, S., Montgomery, S., Petersen, F., Rudatsikira, E., & Singh, P. (2006). Mentoring Cambodian and Lao health professionals in tobacco control leadership and research skills. Tobacco Control, 15(Suppl 1), i42-i47. http://dx.doi.org/10.1136/tc.2005.015008
Findyartini, A., Bilszta, J., Lysk, J., & Soemantri, D. (2019). Transnational clinical teacher training: Lessons learned and cross-cultural implications. The Asia Pacific Scholar, 4(3), 79-90. https://doi.org/10.29060/TAPS.2019-4-3/OA2088
Fryxell, G. E., Dooley, R. S., & Vryza, M. (2002). After the ink dries: The interaction of trust and control in US‐based international joint ventures. Journal of Management Studies, 39(6), 865-886. https://doi.org/10.1111/1467-6486.00315
Harden, R. M. (2006). International medical education and future directions: A global perspective. Academic Medicine, 81(12), S22-29. https://doi.org/10.1097/01.ACM.0000243411.19573.58
Hays, R. (2016). How to review a medical curriculum. The Asia Pacific Scholar, 1(1), 25-28. https://doi.org/10.29060/TAPS.2016-1-1/SC1009
Heffernan, T., & Poole, D. (2005). In search of ‘‘the vibe’’: Creating effective international education partnerships. Higher Education, 50(2), 223-245. https://doi.org/10.1007/s10734-004-6352-2
Heron, J., & Reason, P. (2001). The practice of co-operative inquiry: Research ‘with’ rather than ‘on’ people. In P. Reason & H. Bradbury (Eds.), Handbook of action research: Participative inquiry and practice (pp. 179-188). London: Sage Publications.
Hodges, B. D., Maniate, J.M., Martimianakis, M. A. (Tina), Alsuwaidan, M., & Segouin, C. (2009). Cracks and crevices: Globalization discourse and medical education. Medical Teacher, 31(10), 910-917.
https://doi.org/10.3109/01421590802534932
Kanchanachitra, C., Lindelow, M., Johnston, T., Hanvoravongchai, P., Lorenzo, F. M., Huong, N. L., . . . dela Rosa, J. F. (2011). Human resources for health in southeast Asia: Shortages, distributional challenges, and international trade in health services. The Lancet, 377(9767), 769-781. https://doi.org/10.1016/S0140-6736(10)62035-1
Keay, J., May, H., & O’Mahony, J. (2014). Improving learning and teaching in transnational education: can communities of practice help? Journal of Education for Teaching, 40(3), 251-266.
https://doi.org/10.1080/02607476.2014.903025
Kim, D.-H., Lee, J.-H., Park, J., & Shin, J.-S. (2017). Process-oriented evaluation of an international faculty development program for Asian developing countries: A qualitative study. BMC Medical Education, 17(1), 260.
https://doi.org/10.1186/s12909-017-1101-2
Kim, D.-H., Yoon, H. B., Sung, M., Yoo, D.-M., Hwang, J., Kim, E. J., . . . Shij, J.-S. (2015). Evaluation of an international faculty development program for developing countries in Asia: The Seoul Intensive Course for Medical Educators. BMC Medical Education, 15(1), 224. https://doi.org/10.1186/s12909-015-0518-8
Kosmützky, A., & Putty, R. (2015). Transcending borders and traversing boundaries: A systematic review of the literature on transnational, offshore, cross-border, and borderless higher education. Journal of Studies in International Education, 20(1), 8-33. https://doi.org/10.1177/1028315315604719
Lam, T. P., & Lam, Y. Y. B. (2009). Medical education reform: The Asian experience. Academic Medicine, 84(9), 1313-1317. https://doi.org/10.1097/ACM.0b013e3181b18189
Maher, J., Sicchia, S., & Stein, L. G. (2003). Learning the culture of partnership: A case study in collaboration between a Canadian university and its Costa Rican partner. Canadian Journal of Development Studies/Revue Canadienne d’etudes Du Developpement, 24(1), 107-118. https://doi.org/10.1080/02255189.2003.9668899
Majumder, M. A. A. (2004). Issues and priorities of medical education research in Asia. ANNALS Academy of Medicine Singapore, 33(2), 257-263.
Mertens, D. M. (2009). Transformative research and evaluation. New York, NY: Guilford Press.
Nhan, T. T., & Nguyen, H. C. (2018). Quality challenges in transnational higher education under profit-driven motives: The Vietnamese experience. Issues in Educational Research, 28(1), 138-152.
Pashby, K., & de Oliveira Andreotti, V. (2016). Ethical internationalisation in higher education: Interfaces with international development and sustainability. Environmental Education Research, 22(6), 771-787.
https://doi.org/10.1080/13504622.2016.1201789
Phuong, T. T., Duong, H. B., & McLean, G. N. (2015). Faculty development in Southeast Asian higher education: A review of literature. Asia Pacific Education Review, 16(1), 107-117. https://doi.org/10.1007/s12564-015-9353-1
Pike, A., McHug, M., Canney, K. C., Miller, N. E., Reiley, P., & Seibert, C. (1993). A new architecture for quality assurance: Nurse-physician collaboration. Journal of Nursing Care Quality, 7(3), 1-8.
Prideaux, D. (2003). ABC of learning and teaching in medicine: Curriculum design. British Medical Journal, 326(7383), 268-270. https://doi.org/10.1136/bmj.326.7383.268
Shams, F., & Huisman, J. (2012). Managing offshore branch campuses: An analytical framework for institutional strategies. Journal of Studies in International Education, 16(2), 106-127. https://doi.org/10.1177/1028315311413470
Sherman, L. T., & Chappell, K. B. (2018). Global perspective on continuing professional development. The Asia Pacific Scholar, 3(2), 1-5. https://doi.org/10.29060/TAPS.2018-3-2/GP1074
Steinert, Y., Mann, K., Centeno, A., Dolmans, D., Spencer, J., Gelula, M., & Prideaux, D. (2006). A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Medical Teacher, 28(6), 497-526. https://doi.org/10.1080/01421590600902976
Sullivan, M. P., Forrester, D., & Al-Makhamreh, S. (2010). Transnational collaboration: Evaluation of a social work training workshop in Jordan. International Social Work, 53(2), 217-232. https://doi.org/10.1177/0020872809355387
Tupe, D. A., Kern, S. B., Salvant, S., & Talero, P. (2015). Building international sustainable partnerships in occupational therapy: A case study. Occupational Therapy International, 22(3), 131-140. https://doi.org/10.1002/oti.1407
Waterval, D. G. J., Driessen, E. W., Scherpbier, A. J. J. A., & Frambach, J. M. (2018). Twelve tips for crossborder curriculum partnerships in medical education. Medical Teacher, 40(5), 514-519.
https://doi.org/10.1080/0142159X.2018.1429585
Waterval, D. G. J., Frambach, J. M., Driessen, E. W., & Scherpbier, A. J. J. A. (2014). Copy but not paste: A literature review of crossborder curriculum partnerships. Journal of Studies in International Education, 19(1), 65-85.
https://doi.org/10.1177/1028315314533608
Whitehead, C., Wondimagegn, D., Baheretibeb, Y., & Brian, B. H. (2018). The International partner as invited guest: Beyond colonial and import-export models of medical education. Academic Medicine, 93(12), 1760-1763. https://doi.org/10.1097/ACM.0000000000002268
World Health Organisation. (2013). Implementation of the Human Resources for Health Strategy in the Western Pacific Region: A analytical review. Manila: World Health Organisation Regional Office for the Western Pacific. Retrieved August 22, 2019, from
http://www.wpro.who.int/hrh/documents/publications/implementation_of_hrh_strategy_upload.pdf
Wiek, A., Bernstein, M., Laubichler, M., Caniglia, G., Minteer, B., & Lang, D. (2013). A global classroom for international sustainability education. Creative Education, 4(4), 19-28. https://doi.org/10.4236/ce.2013.44A004
Yoon, H., Shin, J., Lee, S., Kim, D., Sung, M., Amgalan, N., & Chinzorig, T. (2016). Transnational collaboration for faculty development in health professions education in Mongolia. Korean Journal of Medical Education, 28(4), 381-390. https://doi.org/10.3946/kjme.2016.43
Yudhi, W. S., Nanere, M. G., & Nsubuga-Kyobe, A. (2006). A comparative study of negotiation styles of education managers in Australia and Indonesia. In Proceedings of the Asian Forum on Business Education. Retrieved August 22, 2019, from http://www.seameo.org/vl/library/dlwelcome/publications/paper/ABFE06/AFBE06.htm
Zhang, Y., & Huxham, C. (2009). Identity construction and trust building in developing international collaborations. The Journal of Applied Behavioral Science, 45(2), 186-211. https://doi.org/10.1177/0021886309333327
*Diantha Soemantri
Department of Medical Education,
Faculty of Medicine, Universitas Indonesia,
Salemba 6 Central Jakarta,
DKI Jakarta, Indonesia 10430
Email: diantha.soemantri@ui.ac.id
dianthasoemantri@yahoo.com
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









