Simulation instructional design features with differences in clinical outcomes: A narrative review
Submitted: 18 November 2024
Accepted: 14 May 2025
Published online: 7 October, TAPS 2025, 10(4), 5-25
https://doi.org/10.29060/TAPS.2025-10-4/RA3572
Matthew Jian Wen Low1, Han Ting Jillian Yeo2, Dujeepa D. Samarasekera2, Gene Wai Han Chan1 & Lee Shuh Shing2
1Department of Emergency Medicine, National University Hospital, Singapore; 2Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Effective and actionable instructional design features improve return on investment in Technology enhanced simulation (TES). Previous reviews on instructional design features for TES that improve clinical outcomes covered studies up to 2011, but updated, consolidated guidance has been lacking since then. This review aims to provide such updated guidance to inform educators and researchers.
Methods: A narrative review was conducted on instructional design features in TES in medical education. Original research articles published between 2011 to 2022 that examined outcomes at Kirkpatrick level three and above were included.
Results: A total of 30,491 citations were identified. After screening, 31 articles were included in this review. Most instructional design features had a limited evidence base with only one to four studies each, except 11 studies for simulator modality. Improved outcomes were observed with error management training, distributed practice, dyad training, and in situ training. Mixed results were seen with different simulation modalities, isolated components of mastery learning, just-in-time training, and part versus whole task practice.
Conclusion: There is limited evidence for instructional design features in TES that improve clinical outcomes. Within these limits, error management training, distributed practice, dyad training, and in situ training appear beneficial. Further research is needed to assess the effectiveness and generalisability of these features.
Keywords: Simulation, Instructional Design, Clinical Outcomes, Review
Practice Highlights
- This review pinpoints additional beneficial instructional design features emerging since 2011.
- These include error management training, distributed practice, dyad training, and in situ training.
- Further evidence from diverse task and learner contexts is needed to establish generalisability.
- Current evidence continues to suggest no clear superiority of one simulator modality over the other.
I. INTRODUCTION
Technology enhanced simulation (TES) training has been shown to be effective for skills, behaviour, and patient-related outcomes (Cook et al., 2011; McGaghie et al., 2011). Instructional design features in simulation refer to variations in aspects of simulation design that act as active ingredients or mechanisms that make simulation effective, with examples including distributed practice, mastery learning, and range of difficulty (Cook, Hamstra, et al., 2013). Effective instructional design features for TES are actionable for educators because they offer specific, implementable guidance, and an area of research interest (Issenberg et al., 2005; Nestel et al., 2011; Schaefer et al., 2011), including those that lead to transfer to authentic clinical practice (Frerejean et al., 2023; Zendejas et al., 2013).
While it is acknowledged that conducting a study to establish a causal relationship between an educational intervention and subsequent patient and clinical process outcomes is challenging (Cook & West, 2013), such studies become particularly valuable when appropriately executed (Dauphinee, 2012). These studies represent the apex of impact in Kirkpatrick’s model for program evaluation (Kirkpatrick & Kirkpatrick, 2006), holding the highest clinical significance and representing the ultimate goal of health professions education which is to enhance patient outcomes by equipping the healthcare workforce to effectively address societal needs (Carraccio et al., 2016). Additionally, the examination of clinical outcomes, when coupled with a consideration of costs, contributes to the informed allocation of limited institutional resources to such educational approaches (Lin et al., 2018).
In prior reviews of TES including studies up to 2011, the vast majority of studies examined outcomes at the levels of reaction and learning demonstrated in written or simulation tests, with only a small body of evidence studying outcomes in workplace contexts (Cook, Hamstra, et al., 2013; Nestel et al., 2011; Zendejas et al., 2013) suggesting that clinical variation, multiple learning strategies, and increased time learning are beneficial variations. This limited evidence base for transfer to workplace contexts hinders educators in fully harnessing the potential of TES to improve patient and system outcomes and obtain the best returns on investments in simulation technology. Given the time interval since these prior reviews, further evidence would have accrued regarding these and other instructional design features.
Given the time elapsed since the last comprehensive review of TES instructional design features, the scarcity of prior studies on clinical outcomes, and the importance of these outcomes, we conducted this narrative review. The objective was to provide an updated understanding of the instructional design features in TES that are associated with enhanced clinical outcomes, thereby addressing a significant gap in the existing literature, to guide educators seeking to optimise instructional design, and provide researchers with an overview of the current state of this literature and guide further inquiry.
II. METHODS
We conducted a narrative review based on the framework proposed by Ferrari (2015). We searched MEDLINE, ERIC, Embase, Scopus and Web of Science databases for articles published from 2012 January 01 to 2022 December 06. We translated abstracts and articles not in English into English using Google Translate.
The following search terms were used: (Medical education) AND (Simulation OR Cadaver OR Simulator OR Augmented Reality OR Virtual reality OR Mixed reality).
Studies were included if they were original research articles examining instructional design variations in TES with at least one outcome at Kirkpatrick levels three or above, as described and utilised by the Best Evidence Medical Education Collaboration (Steinert et al., 2006). We included a broad range of TES modalities, such as computer based virtual reality simulators, high fidelity and static mannequins, plastic models, live animals, inert animal products, and human cadavers as stipulated in the review by Cook et al. (2011). We included augmented reality and mixed reality as they satisfied the prior definition of “materials and devices created or adapted to solve practical problems” in simulation established by Cook et al (2011). Studies where TES was utilised together with human patient actors were included. We included studies with observational, experimental, and qualitative designs.
Studies were excluded if they involved only human patient actors as the sole modality of simulation, used simulation outside of health professions education, used simulation for noneducation purposes such as procedural planning or patient education, or only compared simulation with no simulation. We excluded studies involving only nurses given that there are recent and ongoing reviews addressing a similar research question (El Hussein & Cuncannon, 2022; Jackson et al., 2022), but included interprofessional studies. Figure 1 shows the flow of studies through the review and selection process.
Three researchers (MJWL, SSL, JHTY) independently read the full text of articles that met the inclusion criteria and extracted study information including geographical origin, specialty context, type of skill studied, level of the learner, simulation modalities used, instructional design variations studied, and outcomes categorised into the highest Kirkpatrick level studied. Any differences were resolved by a discussion among researchers to arrive at a consensus.
III. RESULTS
A total of 30,491 records were identified using the search strategy. From these, 31 eligible studies were identified and reviewed (Figure 1 and Table 1). Figure 2 summarises basic information on these studies. The number of studies from each geographic region were 13 from North America (42%), 11 from Europe (35%), three from Asia (10%), two from Africa (6%), and one from South America (3%). One study did not clearly state the countries involved.
28 out of 31 (90%) of the studies adopted a quantitative research design focusing on experimental design. Most simulation interventions were conducted among residents/fellows/interns, followed by medical students.
The results reported in the studies are divided into two groups:
- Evidence suggests improved outcomes
- Evidence shows mixed results
A. Improved Outcomes
Error management training was associated with improved obstetric ultrasound skills compared to error avoidance training in novices (Dyre et al., 2017). Frequent brief on-site simulation, at 40 minutes a month and three minutes a week, was associated with reduced infant mortality compared to a single day course (Mduma et al., 2015). Integrating non-technical skills (NTS) training into a colonoscopy skills curriculum with TES, without increasing time spent teaching, improved observed performance during colonoscopies on real patients, although it was unclear whether this was driven by changes in observed NTS only, or both NTS and technical skills (Walsh et al., 2020).
One qualitative study found that in situ training had greater organisational impact and provided more information for practical organisational changes (Sørensen et al., 2015). One qualitative study found that multi-professional training led to improved communication, leadership, and clinical management of post-partum haemorrhage (Egenberg et al., 2017).
1. Dyad Training
In one study of obstetric ultrasound skills (Tolsgaard et al., 2015) a larger proportion of the dyad training group (71%) scored above the criterion referenced pass fail level than the individual training group (30%) on the objective structured assessment of ultrasound skills, though the difference in mean scores on did not reach statistical significance. Other benefits included increased efficiency from greater faculty to learner ratios.
2. Complex Bundles
Three studies found improvements with complex bundles comprising multiple instructional design variations.
Medical students performed the correct sequence of steps for endotracheal intubation measured by a checklist more often when practice with a mannequin was augmented by a 10-question pre-test, hand held tablets containing scenarios, checklists, and learning algorithms, 24-hour access to the simulation laboratory, and remote review of practice recordings with feedback from teachers via email (Mankute et al., 2022).
Residents had improved observed performance in laparoscopic salpingectomy with lectures, videos, reading materials, a box trainer with pre-set proficiency benchmarks, a VR simulator for technical skills, and non-technical skills training with scripted confederates, compared to a conventional curriculum including simulation with minimal further description (Shore et al., 2016).
In one qualitative study of obstetric residents, there was improved transfer of communication and team work skills and situational awareness with simulation aligned to multiple principles including authenticity, psychological fidelity, engineering fidelity, Paivio’s dual coding, feedback, variability, and increasing complexity (de Melo et al., 2018).
B. Mixed Results
1. Simulation Modality
Eleven studies examined whether outcomes differed when different simulation modalities were used. Examples include higher versus lower technological complexity in a physical simulator (DeStephano et al., 2015; Sharara-Chami et al., 2014), cadaveric versus synthetic models (Lal et al., 2022; Tan et al., 2018; Tchorz et al., 2015), virtual reality (VR) versus physical simulators (Daly et al., 2013; Gomez et al., 2015; Orzech et al., 2012; O’Sullivan et al., 2014), and a computer based versus physical simulated operating room for student orientation (Patel et al., 2012).
Overall, there no clear pattern of superiority of a particular type of simulator. Most studies found no difference, with three exceptions: Gomez et al (2012) found that VR alone, and VR with physical simulator, led to superior performance in observed colonoscopic skills in real patients, compared to physical simulator alone; Chunharas et al (2013) found that adding practice on fellow students on top of mannequin practice improved observed performance in subcutaneous and intramuscular injection skills; Patel et al (2012) found that using a physical simulated operating room was superior to an online computer based operating room for training novice medical students in appropriate behaviour in the operating room.
To view Table 1 click here.
Abbreviations. ACS/APDS: American College of Surgeons / Association of Program Directors in Surgery; EAT: Error avoidance training; EMT: Error management training; GAGES-C: Global Assessment of Gastrointestinal Endoscopic Skills-Colonoscopy; GOALS: Global Operative Assessment of Laparoscopic Skills; ISS: In situ simulation; JAG DOPS: Joint Advisory Group Direct Observation of Procedural Skills; JIT: Just in time; OSA-LS: objective structured assessment of laparoscopic salpingectomy; NTS: Non-technical skills. OSAUS: objective structured assessment of ultrasound; OSS: Off-site simulation; PGY: Post graduate year; UK: United Kingdom; USA: United States of America; VR: Virtual reality.
Kirkpatrick levels. 1: Reaction e.g. participants’ views on learning experience; 2a: Learning – Change in attitudes; 2b: Learning – Modification of knowledge or skills; 3: Behaviour – Change in behaviours; 4a: Results – Change in the system/organisational practice; 4b: Results – Change in patient outcomes.
Table 1. List of included studies and skills, instructional design variations and outcomes examined
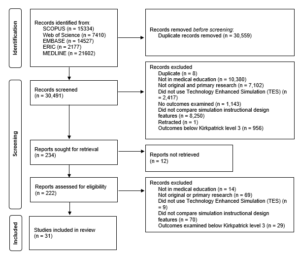
Figure 1. Flow of studies through identification process
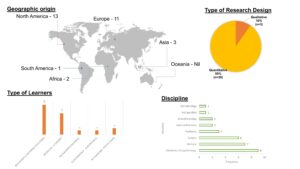
Figure 2. Summary of geographical origin, type of research, type of learners and disciplines studied
2. Components of Mastery Learning
Four studies examined components of mastery learning, such as progressive task difficulty and proficiency-based progression. Progressive task difficulty for TES was associated with improved rater observed colonoscopic performance on real patients (Grover et al., 2017), while the evidence was mixed for proficiency-based progression for TES, with studies finding reduced epidural failure rates (Srinivasan et al., 2018) and fewer adverse events in laparoscopic cholecystectomy (De Win et al., 2016), while another found no difference in operative performance for bowel anastomosis in real patients (Naples et al., 2022).
3. Part Versus Whole Task
Two studies compared part versus whole task training. Both found no difference, in rater observed performance in laparoscopic inguinal hernia repair (Hernández-Irizarry et al., 2016), and intraoperative camera navigation skills (Nilsson et al., 2017), though randomised part task training led to faster skills mastery with greater cost effectiveness compared to whole task training.
4. Increased Time Spent in Simulation Training
Two studies examined amount of time spent in simulation training. One study showed reduced incidence of malpractice claims (Schaffer et al., 2021), while another study found no difference in successful deep biliary cannulation during endoscopic retrograde cholangiopancreatography (Liao et al., 2013).
5. Just in Time (JIT) Training
Overall, there was mostly no benefit seen with JIT training with TES, across three studies. One study examined the addition of JIT video after prior TES (Todsen et al., 2013), and one study compared JIT practice alone, JIT practice with feedback from this practice, and feedback alone derived from baseline testing (Kroft et al., 2017). JIT and just-in-place physical simulator training did not improve first pass lumbar puncture success, but improved mean number of attempts and process measures such as early stylet removal (Kessler et al., 2015).
IV. DISCUSSION
We sought to provide an updated synthesis on effective instructional design features in simulation in medical education, focusing on those that produce higher level outcomes at Kirkpatrick levels three and above. A prior review searching until 2011 identified only 18 studies that examined outcomes at Kirkpatrick level three and above, out of their pool of 10,297 studies. Our review reveals a notable rise in the number of studies over the past ten years, exploring instructional design and clinical outcomes. In the discussion that follows, we synthesise the findings with existing literature and theory to extract valuable insights for medical educators.
A. Implications for Current Practice
This review underscores the necessity of directing resources towards effective instructional design features, emphasising that these need not be strictly tied to specific simulator types, as advocated by Norman. Despite the ongoing evolution and incorporation of an expanding array of TES modalities, including Virtual Reality (VR) in this review, we observed mixed results concerning simulation modality as an instructional design variation. Upon closer examination of interventions outlined in studies comparing simulation modalities, it becomes evident that confounding factors may arise due to variations in the application of training to proficiency criteria (a characteristic of mastery learning) or differences in the quality of measurement.
In the study conducted by Gomez et al (2015), training to proficiency criteria was incorporated in study arms demonstrating benefit (VR and VR plus physical simulator) and not incorporated in the remaining arm (physical simulator alone). Similarly, in the study by Orzech et al (2012) where training until proficiency criteria were reached was a shared feature of both arms, no significant difference between groups was observed. It remains unclear whether observed differences were attributable to the application of training until proficiency criteria were met or to the varied simulation modalities.
Chunharas et al (2013) and Patel et al (2012) also noted outcome differences when comparing different simulation modalities. However, the robustness of these findings is constrained using a checklist observation scale developed for individual studies with minimal validity evidence. Clinical and task variations, recognised as beneficial in prior reviews (Zendejas et al., 2013), may elucidate the advantages identified by Chunharas et al and the VR plus physical simulator arm in the study by Gomez et al.
Components of mastery learning appear mostly effective, although isolated implementation of a component without the whole may erode effectiveness. The inconsistent evidence for effectiveness of components of mastery learning in this review is surprising, given prior evidence for the effectiveness of mastery learning for translational outcomes (Griswold-Theodorson et al., 2015). The difference may lie in piecemeal rather than holistic implementation of mastery learning as a complex intervention, with seven complementary components working together (McGaghie, 2015).
Another difference is that our review only included studies comparing different TES interventions, while the review by Griswold-Theodorson et al included studies that compared mastery learning with a wider range of comparators, including no TES. Notably, a separate systematic review and meta-analysis of mastery learning found only three studies from 1984-2010 comparing mastery learning to other TES interventions for patient outcomes, with no statistically significant benefit overall and substantial heterogeneity (Cook, Brydges, et al., 2013).
Methodological issues may be another contributory factor. Naples et al (2022) postulate in their study the reasons for the lack of observed difference, including a long duration between intervention and outcome assessment, which was longer in the intervention group than the control group, biasing towards the null, and surprisingly high baseline performance with an insufficiently sensitive rater observation tool. This study had only nine participants, limiting statistical power. These represent important methodological considerations for researchers designing educational intervention studies.
The effectiveness of increased time spent in simulation training is associated with incorporation of learning conversations. Discrepancies in outcomes between the two studies assessing the impact of time spent in simulation training may be attributed to the presence of debriefing in the study conducted by Schaffer et al (2021), as opposed to un-coached practice without feedback in the study by Liao et al (2013). It is crucial to note that the advantages derived from extended training periods are not solely attributed to prolonged duration but are also influenced by the integration of learning conversations. These conversations encompass both debriefing and feedback (Tavares et al., 2020), both of which have demonstrated efficacy, as supported by existing research (Cheng et al., 2014; Hattie & Timperley, 2007).
In a systematic review by Hatala and colleagues (Hatala et al., 2014), feedback emerged as moderately effective for procedural skills simulation training. Notably, feedback from multiple sources, including instructors, proved more effective than feedback from a single source.
Distributed practice is preferred over blocked practice for TES. Frequent brief simulation (Mduma et al., 2015) essentially describes distributed rather than blocked practice. The increased effectiveness seen with distributed practice here is consistent with existing literature within (Cecilio-Fernandes et al., 2023) and outside (Dunlosky et al., 2013) of health professions education.
Dyad training is notable for being efficient with similar or better outcomes, and is consistent with existing literature on motor skills learning (Wulf et al., 2010). The optimal group size has not been clearly determined, beyond single versus dyad, and would be a productive avenue of inquiry for evidence-based determination of learner to faculty ratios, accounting for contextual factors such as task complexity and stage of learner’s development.
In situ simulation may be beneficial in generating participant insights that feed into systems-based improvements through quality improvement mechanisms (Calhoun et al., 2024; Nickson et al., 2021). This combines multiple mechanisms by which TES can produce meaningful impact: through changing individual learner behaviour and changing systems processes.
Error management training appears beneficial for transfer outcomes in novices. This is congruent with literature outside of medical education (Keith & Frese, 2008). The limited evidence base within medical education makes this ripe for further study across task and learner types.
In summary, the features mentioned above are predominantly drawn from previous studies, primarily conducted at Kirkpatrick level two. This review contributes by offering an updated synthesis of evidence, outlining the extent to which this evidence can be extrapolated to higher Kirkpatrick levels, and highlighting features that were previously unexplored at clinical process and outcome levels. Collectively, evidence spanning these levels serves as a guide for those designing TES with the goal of achieving educational and clinical impact.
B. Limitations and Implications for Future Research
Studies that examine Kirkpatrick levels three and above continue to constitute a relatively small fraction of the overall research landscape. Furthermore, this limited body of research is dispersed among various instructional design features, with only a small number of studies investigating each specific feature. Consequently, drawing definitive conclusions about effectiveness becomes challenging, representing a primary constraint of this review. Despite these limitations, we have tried to extract valuable insights for health professions educators by synthesising the findings with existing literature and theory.
The limited evidence bases for most individual instructional design features, especially those demonstrating benefits at Kirkpatrick levels three and four, limits the strength of conclusions that can be drawn about their effectiveness. Further studies replicating these results would strengthen the argument that a particular instructional design feature is able to achieve clinical impact. The evidence base is also limited in the variety of task and learner contexts studied for each individual instructional design feature. Determining the generalisability of these findings requires further research applying these features across diverse TES contexts with different skills and learner groups. Future research should also continue to explore novel and promising instructional design features, such as hybrid simulations where mannequins are overlayed with animal tissue or gel-based phantoms (Balakrishnan et al., 2025).
V. CONCLUSION
There is limited evidence for instructional design features in TES that translate to improved clinical outcomes. Within these limits, error management training, distributed practice, dyad training, and in situ training appear beneficial. Given the limited evidence base for these individual features, definitive determination of effectiveness and generalisability requires further research applying promising target features across different task and learner contexts.
Notes on Contributors
Matthew Low is an emergency physician at National University Hospital, Singapore, and adjunct assistant professor at the Yong Loo Lin School of Medicine, National University of Singapore.
Jillian Yeo is a medical educationalist at the Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore.
Dujeepa Samarasekera is senior director at the Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore.
Gene Chan is an emergency physician at National University Hospital, Singapore, and adjunct assistant professor at the Yong Loo Lin School of Medicine, National University of Singapore.
Shuh Shing Lee is a medical educationalist at the Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore.
Matthew Low, Jillian Yeo and Shuh Shing Lee conceived of the work, collected and analysed data, and drafted the work. Gene Chan and Dujeepa Samarasekera conceived of the work and reviewed it critically for important intellectual content. All contributors gave final approval of the version to be published and are agreeable to be accountable for all aspects of the work.
Ethical Approval
Ethical approval was not applicable as this is a review paper.
Funding
There was no funding for this paper.
Declaration of Interest
The authors report no conflicts of interest.
References
Balakrishnan, A., Law, L. S.-C., Areti, A., Burckett-St Laurent, D., Zuercher, R. O., Chin, K.-J., & Ramlogan, R. (2025). Educational outcomes of simulation-based training in regional anaesthesia: A scoping review. British Journal of Anaesthesia, 134(2), 523–534. https://doi.org/10.1016/j.bja.2024.07.037
Calhoun, A. W., Cook, D. A., Genova, G., Motamedi, S. M. K., Waseem, M., Carey, R., Hanson, A., Chan, J. C. K., Camacho, C., Harwayne-Gidansky, I., Walsh, B., White, M., Geis, G., Monachino, A. M., Maa, T., Posner, G., Li, D. L., & Lin, Y. (2024). Educational and patient care impacts of in situ simulation in healthcare: A systematic review. Simulation in Healthcare, 19(1S), S23–S31. https://doi.org/10.1097/SIH.0000000000000773
Carraccio, C., Englander, R., Van Melle, E., Ten Cate, O., Lockyer, J., Chan, M.-K., Frank, J. R., Snell, L. S., & International Competency-Based Medical Education Collaborators. (2016). Advancing competency-based medical education: A charter for clinician-educators. Academic Medicine, 91(5), 645–649. https://doi.org/10.1097/ACM.0000000000001048
Cecilio-Fernandes, D., Patel, R., & Sandars, J. (2023). Using insights from cognitive science for the teaching of clinical skills: AMEE Guide No. 155. Medical Teacher, 45(11), 1214–1223. https://doi.org/10.1080/0142159X.2023.2168528
Cheng, A., Eppich, W., Grant, V., Sherbino, J., Zendejas, B., & Cook, D. A. (2014). Debriefing for technology-enhanced simulation: A systematic review and meta-analysis. Medical Education, 48(7), 657–666. https://doi.org/10.1111/medu.12432
Chunharas, A., Hetrakul, P., Boonyobol, R., Udomkitti, T., Tassanapitikul, T., & Wattanasirichaigoon, D. (2013). Medical students themselves as surrogate patients increased satisfaction, confidence, and performance in practicing injection skill. Medical Teacher, 35(4), 308–313. https://doi.org/10.3109/0142159X.2012.746453
Cook, D. A., Brydges, R., Zendejas, B., Hamstra, S. J., & Hatala, R. (2013). Mastery learning for health professionals using technology-enhanced simulation: A systematic review and meta-analysis. Academic Medicine, 88(8), 1178–1186. https://doi.org/10.1097/ACM.0b013e31829a365d
Cook, D. A., Hamstra, S. J., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., Erwin, P. J., & Hatala, R. (2013). Comparative effectiveness of instructional design features in simulation-based education: Systematic review and meta-analysis. Medical Teacher, 35(1), e867-898. https://doi.org/10.3109/0142159X.2012.714886
Cook, D. A., Hatala, R., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., Erwin, P. J., & Hamstra, S. J. (2011). Technology-enhanced simulation for health professions education: A systematic review and meta-analysis. JAMA, 306(9), 978–988. https://doi.org/10.1001/jama.2011.1234
Cook, D. A., & West, C. P. (2013). Perspective: Reconsidering the focus on “outcomes research” in medical education: A cautionary note. Academic Medicine, 88(2), 162–167. https://doi.org/10.1097/ACM.0b013e31827c3d78
Daly, M. K., Gonzalez, E., Siracuse-Lee, D., & Legutko, P. A. (2013). Efficacy of surgical simulator training versus traditional wet-lab training on operating room performance of ophthalmology residents during the capsulorhexis in cataract surgery. Journal of Cataract and Refractive Surgery, 39(11), 1734–1741. https://doi.org/10.1016/j.jcrs.2013.05.044
Dauphinee, W. D. (2012). Educators must consider patient outcomes when assessing the impact of clinical training. Medical Education, 46(1), 13–20. https://doi.org/10.1111/j.1365-2923.2011.04144.x
de Melo, B. C. P., Rodrigues Falbo, A., Sorensen, J. L., van Merriënboer, J. J. G., & van der Vleuten, C. (2018). Self-perceived long-term transfer of learning after postpartum haemorrhage simulation training. International Journal of Gynaecology and Obstetrics, 141(2), 261–267. https://doi.org/10.1002/ijgo.12442
De Win, G., Van Bruwaene, S., Kulkarni, J., Van Calster, B., Aggarwal, R., Allen, C., Lissens, A., De Ridder, D., & Miserez, M. (2016). An evidence-based laparoscopic simulation curriculum shortens the clinical learning curve and reduces surgical adverse events. Advances in Medical Education and Practice, 7, 357–370. https://doi.org/10.2147/AMEP.S102000
DeStephano, C. C., Chou, B., Patel, S., Slattery, R., & Hueppchen, N. (2015). A randomized controlled trial of birth simulation for medical students. American Journal of Obstetrics and Gynaecology, 213(1), 91.e1-91.e7. https://doi.org/10.1016/j.ajog.2015.03.024
Dunlosky, J., Rawson, K. A., Marsh, E. J., Nathan, M. J., & Willingham, D. T. (2013). Improving students’ learning with effective learning techniques: Promising directions from cognitive and educational psychology. Psychological Science in the Public Interest, 14(1), 4–58. https://doi.org/10.1177/1529100612453266
Dyre, L., Tabor, A., Ringsted, C., & Tolsgaard, M. G. (2017). Imperfect practice makes perfect: Error management training improves transfer of learning. Medical Education, 51(2), 196–206. https://doi.org/10.1111/medu.13208
Egenberg, S., Karlsen, B., Massay, D., Kimaro, H., & Bru, L. E. (2017). “No patient should die of PPH just for the lack of training!” Experiences from multi-professional simulation training on postpartum haemorrhage in northern Tanzania: A qualitative study. BMC Medical Education, 17(1), 119. https://doi.org/10.1186/s12909-017-0957-5
El Hussein, M. T., & Cuncannon, A. (2022). Nursing students’ transfer of learning from simulated clinical experiences into clinical practice: A scoping review. Nurse Education Today, 116, 105449. https://doi.org/10.1016/j.nedt.2022.105449
Ferrari, R. (2015). Writing narrative style literature reviews. Medical Writing, 24(4), 230–235. https://doi.org/10.1179/2047480615Z.000000000329
Frerejean, J., van Merriënboer, J. J. G., Condron, C., Strauch, U., & Eppich, W. (2023). Critical design choices in healthcare simulation education: A 4C/ID perspective on design that leads to transfer. Advances in Simulation (London, England), 8(1), 5. https://doi.org/10.1186/s41077-023-00242-7
Gomez, P. P., Willis, R. E., & Van Sickle, K. (2015). Evaluation of two flexible colonoscopy simulators and transfer of skills into clinical practice. Journal of Surgical Education, 72(2), 220–227. https://doi.org/10.1016/j.jsurg.2014.08.010
Griswold-Theodorson, S., Ponnuru, S., Dong, C., Szyld, D., Reed, T., & McGaghie, W. C. (2015). Beyond the simulation laboratory: A realist synthesis review of clinical outcomes of simulation-based mastery learning. Academic Medicine, 90(11), 1553–1560. https://doi.org/10.1097/ACM.0000000000000938
Grover, S. C., Scaffidi, M. A., Khan, R., Garg, A., Al-Mazroui, A., Alomani, T., Yu, J. J., Plener, I. S., Al-Awamy, M., Yong, E. L., Cino, M., Ravindran, N. C., Zasowski, M., Grantcharov, T. P., & Walsh, C. M. (2017). Progressive learning in endoscopy simulation training improves clinical performance: A blinded randomized trial. Gastrointestinal Endoscopy, 86(5), 881–889. https://doi.org/10.1016/j.gie.2017.03.1529
Hatala, R., Cook, D. A., Zendejas, B., Hamstra, S. J., & Brydges, R. (2014). Feedback for simulation-based procedural skills training: A meta-analysis and critical narrative synthesis. Advances in Health Sciences Education, 19(2), 251–272. https://doi.org/10.1007/s10459-013-9462-8
Hattie, J., & Timperley, H. (2007). The power of feedback. Review of Educational Research, 77(1), 81–112. https://doi.org/10.3102/003465430298487
Hernández-Irizarry, R., Zendejas, B., Ali, S. M., & Farley, D. R. (2016). Optimizing training cost-effectiveness of simulation-based laparoscopic inguinal hernia repairs. American Journal of Surgery, 211(2), 326–335. https://doi.org/10.1016/j.amjsurg.2015.07.027
Issenberg, S. B., McGaghie, W. C., Petrusa, E. R., Lee Gordon, D., & Scalese, R. J. (2005). Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Medical Teacher, 27(1), 10–28. https://doi.org/10.1080/01421590500046924
Jackson, M., McTier, L., Brooks, L. A., & Wynne, R. (2022). The impact of design elements on undergraduate nursing students’ educational outcomes in simulation education: Protocol for a systematic review. Systematic Reviews, 11(1), 52. https://doi.org/10.1186/s13643-022-01926-3
Keith, N., & Frese, M. (2008). Effectiveness of error management training: A meta-analysis. Journal of Applied Psychology, 93(1), 59–69. https://doi.org/10.1037/0021-9010.93.1.59
Kessler, D., Pusic, M., Chang, T. P., Fein, D. M., Grossman, D., Mehta, R., White, M., Jang, J., Whitfill, T., Auerbach, M., & INSPIRE LP investigators. (2015). Impact of just-in-time and just-in-place simulation on intern success with infant lumbar puncture. Pediatrics, 135(5), e1237-1246. https://doi.org/10.1542/peds.2014 -1911
Kirkpatrick, D., & Kirkpatrick, J. (2006). Evaluating training programs: The four levels. Berrett-Koehler Publishers.
Kroft, J., Ordon, M., Po, L., Zwingerman, N., Waters, K., Lee, J. Y., & Pittini, R. (2017). Preoperative practice paired with instructor feedback may not improve obstetrics-gynaecology residents’ operative performance. Journal of Graduate Medical Education, 9(2), 190–194. https://doi.org/10.4300/JGME-D-16-00238.1
Lal, B. K., Cambria, R., Moore, W., Mayorga-Carlin, M., Shutze, W., Stout, C. L., Broussard, H., Garrett, H. E., Nelson, W., Titus, J. M., Macdonald, S., Lake, R., & Sorkin, J. D. (2022). Evaluating the optimal training paradigm for transcarotid artery revascularization based on worldwide experience. Journal of Vascular Surgery, 75(2), 581-589.e1. https://doi.org/10.1016/j.jvs.2021.08.085
Liao, W.-C., Leung, J. W., Wang, H.-P., Chang, W.-H., Chu, C.-H., Lin, J.-T., Wilson, R. E., Lim, B. S., & Leung, F. W. (2013). Coached practice using ERCP mechanical simulator improves trainees’ ERCP performance: A randomized controlled trial. Endoscopy, 45(10), 799–805. https://doi.org/10.1055/s-0033-1344224
Lin, Y., Cheng, A., Hecker, K., Grant, V., & Currie, G. R. (2018). Implementing economic evaluation in simulation-based medical education: Challenges and opportunities. Medical Education, 52(2), 150–160. https://doi.org/10.1111/medu.13411
Mankute, A., Juozapaviciene, L., Stucinskas, J., Dambrauskas, Z., Dobozinskas, P., Sinz, E., Rodgers, D. L., Giedraitis, M., & Vaitkaitis, D. (2022). A novel algorithm-driven hybrid simulation learning method to improve acquisition of endotracheal intubation skills: A randomized controlled study. BMC Anaesthesiology, 22(1), 42. https://doi.org/10.1186/s12871-021-01557-6
McGaghie, W. C. (2015). Mastery learning: It is time for medical education to join the 21st century. Academic Medicine, 90(11), 1438–1441. https://doi.org/10.1097/ACM.0000000000000911
McGaghie, W. C., Issenberg, S. B., Cohen, E. R., Barsuk, J. H., & Wayne, D. B. (2011). Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Academic Medicine, 86(6), 706–711. https://doi.org/10.1097/ACM.0b013e318217e119
Mduma, E., Ersdal, H., Svensen, E., Kidanto, H., Auestad, B., & Perlman, J. (2015). Frequent brief on-site simulation training and reduction in 24-h neonatal mortality—An educational intervention study. Resuscitation, 93, 1–7. https://doi.org/10.1016/j.resuscitation.2015.04.019
Naples, R., French, J. C., Han, A. Y., Lipman, J. M., & Awad, M. M. (2022). The impact of simulation training on operative performance in general surgery: Lessons learned from a prospective randomized trial. Journal of Surgical Research, 270, 513–521. https://doi.org/10.1016/j.jss.2021.10.003
Nestel, D., Groom, J., Eikeland-Husebø, S., & O’Donnell, J. M. (2011). Simulation for learning and teaching procedural skills: The state of the science. Simulation in Healthcare, 6 Suppl, S10-13. https://doi.org/10.1097/SIH.0b013e318227ce96
Nickson, C. P., Petrosoniak, A., Barwick, S., & Brazil, V. (2021). Translational simulation: From description to action. Advances in Simulation (London, England), 6(1), 6. https://doi.org/10.1186/s41077-021-00160-6
Nilsson, C., Sorensen, J. L., Konge, L., Westen, M., Stadeager, M., Ottesen, B., & Bjerrum, F. (2017). Simulation-based camera navigation training in laparoscopy—A randomized trial. Surgical Endoscopy, 31(5), 2131–2139. https://doi.org/10.1007/s00464-016-5210-5
Orzech, N., Palter, V. N., Reznick, R. K., Aggarwal, R., & Grantcharov, T. P. (2012). A comparison of 2 ex vivo training curricula for advanced laparoscopic skills: A randomized controlled trial. Annals of Surgery, 255(5), 833–839. https://doi.org/10.1097/SLA.0b013e31824aca09
O’Sullivan, O., Iohom, G., O’Donnell, B. D., & Shorten, G. D. (2014). The effect of simulation-based training on initial performance of ultrasound-guided axillary brachial plexus blockade in a clinical setting—A pilot study. BMC Anaesthesiology, 14, 110. https://doi.org/10.1186/1471-2253-14-110
Patel, V., Aggarwal, R., Osinibi, E., Taylor, D., Arora, S., & Darzi, A. (2012). Operating room introduction for the novice. American Journal of Surgery, 203(2), 266–275. https://doi.org/10.1016/j.amjsurg.2011.03.003
Schaefer, J. J., Vanderbilt, A. A., Cason, C. L., Bauman, E. B., Glavin, R. J., Lee, F. W., & Navedo, D. D. (2011). Literature review: Instructional design and pedagogy science in healthcare simulation. Simulation in Healthcare, 6 Suppl, S30-41. https://doi.org/10.1097/SIH.0b013e31822237b4
Schaffer, A. C., Babayan, A., Einbinder, J. S., Sato, L., & Gardner, R. (2021). Association of simulation training with rates of medical malpractice claims among obstetrician-gynaecologists. Obstetrics and Gynaecology, 138(2), 246–252. https://doi.org/10.1097/AOG.0000000000004464
Sharara-Chami, R., Taher, S., Kaddoum, R., Tamim, H., & Charafeddine, L. (2014). Simulation training in endotracheal intubation in a paediatric residency. Middle East Journal of Anaesthesiology, 22(5), 477–485.
Shore, E. M., Grantcharov, T. P., Husslein, H., Shirreff, L., Dedy, N. J., McDermott, C. D., & Lefebvre, G. G. (2016). Validating a standardized laparoscopy curriculum for gynaecology residents: A randomized controlled trial. American Journal of Obstetrics and Gynaecology, 215(2), 204.e1-204.e11. https://doi.org/10.1016/j.ajog.2016.04.037
Sørensen, J. L., Navne, L. E., Martin, H. M., Ottesen, B., Albrecthsen, C. K., Pedersen, B. W., Kjærgaard, H., & van der Vleuten, C. (2015). Clarifying the learning experiences of healthcare professionals with in situ and off-site simulation-based medical education: A qualitative study. BMJ Open, 5(10), e008345. https://doi.org/10.1136/bmjopen-2015-008345
Srinivasan, K. K., Gallagher, A., O’Brien, N., Sudir, V., Barrett, N., O’Connor, R., Holt, F., Lee, P., O’Donnell, B., & Shorten, G. (2018). Proficiency-based progression training: An “end to end” model for decreasing error applied to achievement of effective epidural analgesia during labour: A randomised control study. BMJ Open, 8(10), e020099. https://doi.org/10.1136/bmjopen-2017-020099
Steinert, Y., Mann, K., Centeno, A., Dolmans, D., Spencer, J., Gelula, M., & Prideaux, D. (2006). A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Medical Teacher, 28(6), 497–526. https://doi.org/10.1080/01421590600902976
Tan, T. X., Buchanan, P., & Quattromani, E. (2018). Teaching residents chest tubes: Simulation task trainer or cadaver model? Emergency Medicine International, 2018, 9179042. https://doi.org/10.1155/2018/9179042
Tavares, W., Eppich, W., Cheng, A., Miller, S., Teunissen, P. W., Watling, C. J., & Sargeant, J. (2020). Learning conversations: An analysis of the theoretical roots and their manifestations of feedback and debriefing in medical education. Academic Medicine, 95(7), 1020–1025. https://doi.org/10.1097/ACM.0000000000002932
Tchorz, J. P., Brandl, M., Ganter, P. A., Karygianni, L., Polydorou, O., Vach, K., Hellwig, E., & Altenburger, M. J. (2015). Pre-clinical endodontic training with artificial instead of extracted human teeth: Does the type of exercise have an influence on clinical endodontic outcomes? International Endodontic Journal, 48(9), 888–893. https://doi.org/10.1111/iej.12385
Todsen, T., Henriksen, M. V., Kromann, C. B., Konge, L., Eldrup, J., & Ringsted, C. (2013). Short- and long-term transfer of urethral catheterization skills from simulation training to performance on patients. BMC Medical Education, 13, 29. https://doi.org/10.1186/1472-6920-13-29
Tolsgaard, M. G., Madsen, M. E., Ringsted, C., Oxlund, B. S., Oldenburg, A., Sorensen, J. L., Ottesen, B., & Tabor, A. (2015). The effect of dyad versus individual simulation-based ultrasound training on skills transfer. Medical Education, 49(3), 286–295. https://doi.org/10.1111/medu.12624
Walsh, C. M., Scaffidi, M. A., Khan, R., Arora, A., Gimpaya, N., Lin, P., Satchwell, J., Al-Mazroui, A., Zarghom, O., Sharma, S., Kamani, A., Genis, S., Kalaichandran, R., & Grover, S. C. (2020). Non-technical skills curriculum incorporating simulation-based training improves performance in colonoscopy among novice endoscopists: Randomized controlled trial. Digestive Endoscopy, 32(6), 940–948. https://doi.org/10.1111/den.13623
Wulf, G., Shea, C., & Lewthwaite, R. (2010). Motor skill learning and performance: A review of influential factors. Medical Education, 44(1), 75–84. https://doi.org/10.1111/j.1365-2923.2009.03421.x
Zendejas, B., Brydges, R., Wang, A. T., & Cook, D. A. (2013). Patient outcomes in simulation-based medical education: A systematic review. Journal of General Internal Medicine, 28(8), 1078–1089. https://doi.org/10.1007/s11606-012-2264-5
*Matthew Low
Emergency Medicine Department,
National University Hospital
9 Lower Kent Ridge Road, Level 4,
Singapore 119085
Email: mlow@nus.edu.sg
Submitted: 7 April 2024
Accepted: 5 February 2025
Published online: 1 April, TAPS 2025, 10(2), 34-45
https://doi.org/10.29060/TAPS.2025-10-2/RA3272
Jasmin Oezcan1, Marcus A. Henning2 & Craig S. Webster2
1Pediatric Department, Erlangen University Hospital, Erlangen, Germany; 2Centre for Medical and Health Sciences Education, School of Medicine, University of Auckland, New Zealand
Abstract
Introduction: Paediatric practice presents unique challenges for clinical reasoning, including the collection of clinical information from multiple individuals during history taking, often in emotionally charged circumstances, and the variable presentation of signs and symptoms due to the developmental stage of the child. Communication skills are clearly important but the most effective methods of teaching clinical reasoning in paediatrics remains unclear. Our review aimed to examine the existing methods of teaching clinical reasoning in paediatrics, and to consider the evidence for the most effective approaches.
Methods: We performed a scoping review and evidence synthesis drawn from reports found during a systematic search in five major databases. We reviewed 211 reports to include 11.
Results: Students who received explicit training in clinical reasoning showed a significant improvement in their experiential learning, diagnostic ability, and reflective clinical judgement. More specifically, key findings demonstrated frequent student-centered interactive strategies increased awareness of the critical role of communication skills and medical history taking. Real case-based exercises, flipped classrooms, workshops, team-based or/and bed-side teaching, and clinical simulation involving multisource feedback were effective in improving student engagement and performance on multiple outcome measures.
Conclusion: This review provides a structured insight into the advantages of different teaching methods, focusing on the multistep decision process involved in teaching clinical reasoning in paediatrics. Our review demonstrated a relatively small number of studies in paediatrics related to clinical reasoning, underlining the need for further research and curricular developments that may better meet the known unique challenges of the care of paediatric patients.
Keywords: Clinical Reasoning, Paediatrics, Teaching Methods, Medical Students
Practice Highlights
- Clinical reasoning in paediatrics involves unique challenges including the collection of clinical information from multiple people (child, parents and care givers), symptoms that may present differently due to children’s stage of development, and complex pharmacokinetics.
- The efficacy of paediatric training could be increased by combining student-centered methods like flipped-classroom, team-based or bed-side teaching and simulation.
- Low stakes training such as simulation that allows repetition and learning from mistakes is particularly effective and engaging for students.
- Our review demonstrated a relatively small number of studies specifically related to clinical reasoning in paediatrics, underlining the need for further research and curricular developments that may better meet the known unique challenges of the care of paediatric patients.
I. INTRODUCTION
Reflective diagnostic skills, comprising the analyses of symptoms and health issues and the weighing up of alternative explanations, are essential for establishing a correct diagnosis and for successful treatment and patient management. In addition, it is important to acknowledge that conscious and unconscious biases may be associated with human errors underlining clinical decision-making (Croskerry, 2005; Webster, Taylor, et al., 2021). The prevalence of incorrect acute clinical diagnosis has been estimated at 5-15% and emphasises the importance of understanding and minimising reasoning errors (Scott, 2009). It has been estimated that 75% of diagnostic errors may be associated with problems of clinical reasoning, in particular related to failures to elicit, synthesise, decide, or act on clinical information (Graber et al., 2005; Pennaforte et al., 2016).
Clinical reasoning requires a competent and highly developed cognitive process, which can use experiential and formal knowledge to work through a cluster of symptoms to generate a correct diagnosis (Pinnock & Welch, 2014). A general approach should incorporate comprehensive problem-solving and involves the need for clear questioning to discern a set of viable differential diagnoses while remaining mindful of the potential of bias in the decision-making process (Pinnock et al., 2021).
The practice of paediatric medicine, however, presents particular challenges for a careful, question-based process of differential diagnosis. Taking a medical history typically requires the collection of clinical information from multiple individuals, including parents, caregivers and the child themselves, often in emotionally charged circumstances. In addition, symptoms in children and neonates can be subtle and unclear – children often have limited communication abilities, their symptoms may present differently depending on their stage of development, many diagnostic tools and tests are designed for adults and have limited utility in children, and children may have unexpected sensitivities and responses to medications due to having pharmacokinetics that are very different to those of adults (Webster, Anderson, et al., 2021).
Despite these challenges, the teaching and experience of clinical reasoning for trainees in paediatrics is often informal and occurs in an unstructured way throughout clinical attachments. In addition, there is often a lack of opportunity to review performance with an experienced clinician, which hinders the development of insight regarding common causes of errors (Lee et al., 2010; Schmidt & Mamede, 2015). It is well known that quality supervision and feedback leads to better learning in trainees, however, there is often a shortage of appropriately qualified paediatricians able to provide such supervision and feedback (de Jong & Ferguson-Hessler, 1996; Zhang et al., 2019).
The medical curriculum typically focuses on the acquisition of content knowledge, cultivating both theory and practical skills, which culminates in the ability to develop a treatment strategy for the patient (Norman, 2005). Clinical reasoning can be described as a multistep process consisting of: data gathering; the proposal of a diagnosis from a range of possible different hypotheses, and the reevaluation of that proposal in light of new information.
Early approaches to the teaching of diagnostic reasoning included the hypothetico-deductive procedural method that involved establishing a series of hypotheses, which then required the gathering of selective patient data to confirm or rule out the hypotheses being made (Norman, 2005; Schwartz & Elstein, 2008). This approach was intended to promote an understanding of the physical development of a disease or condition, and is also known as the pathophysiological approach, and relies on hypothetico-deductive reasoning and knowledge acquisition (Page et al., 1995). Hence, this approach may not represent the most efficient way to cultivate clinically relevant skills. An alternative approach involves the explanation of an expert’s reasoning as an unconscious and automatic pattern recognition process (Groen & Patel, 1985; Schwartz & Elstein, 2008). This can be linked with the dual-cognition theory (Marcum, 2012). It has been suggested that in 95% of case encounters, expert clinicians use the fast, automatic, and unconscious pattern recognition abilities of system 1, while system 2, which is conscious, slow and effortful, tends to be applied only in unusual and complicated cases (Fabry, 2022; Webster, Taylor, et al., 2021). Studies have underlined that both systems should be used simultaneously to ensure an efficient outcome (Pennaforte et al., 2016). Therefore, the teaching of the awareness of individual unconscious information processing and judgment is a major pedagogical challenge, particularly in potentially difficult practice domains such as paediatrics (Bargh & Chartrand, 1999; Gruppen & Frohna, 2002; Webster et al., 2022).
It takes years to train a qualified paediatrician with accurate perception and judgment, enabling them to work effectively with children and their parents, guardians, or caregivers (Gong et al., 2022). Gathering the medical history appropriately and forming an accurate diagnosis through a reliable clinical reasoning process is a critical professional competency in paediatricians, which may require specific curricular techniques to achieve. Therefore in this review we aimed to examine the existing methods of teaching clinical reasoning and diagnosis in paediatrics, and to consider the evidence for which approaches may be the most effective.
II. METHODS
A. The Search Process
In consideration of the array and typology of available reviews, we choose the scoping review because it is a useful synthesis approach to create an overview of the salient literature and to identify key findings. A preliminary search identified no published review with an equal or comparable research question as the current work, suggesting that our scoping review may allow priorities for future investigations to be outlined, including potentially informing later systematic reviews (Grant & Booth, 2009). The literature search was conducted during the period of March and April 2023, using five major databases (Pubmed, PsychInfo, Scopus, ERIC, and Google Scholar). We aimed to identify studies, without restriction of type or year of publication, reported in English or German, to capture as much of the Western thought on clinical reasoning in paediatrics as possible and to make the most of the language fluency of the authors. The search employed the PICO (Population, Intervention, Comparison and Outcome) framework and the terms listed in Table 1 (Schardt et al., 2007). These search terms were used according to the following structure, for example: “medical-student” AND “clinical-reasoning” AND “paediatrics”. The search included MeSH terms, truncations, subject headings, word variants and incorporated both American and British spellings.
|
Types of participants |
Types of intervention |
Types of comparison |
Types of outcomes |
|
Medical-students, clinic*ians, experts and teachers. |
Clinical-reasoning, paediatric setting, clinical-rotation, medicine |
Types of educational system, study types and teaching methods.
|
Depending on the study type the comparison of assessment and efficacy. |
Table 1. PICO Framework Components
B. Data Analysis
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) was utilised as an evidence-based guideline for the inclusion and exclusion process, as illustrated in the flow diagram (Figure 1) (Moher et al., 2009). Author JO screened reports initially by title and abstract, with uncertainties being resolved at regular meetings with authors MAH and CSW. Those with suitable titles were placed in a citation management program (Vanhecke, 2008). We included studies that focused on teaching methods in clinical reasoning in paediatrics, in particular approaches that were intended to improve the quality of reasoning and decision making (see Figure 1 for inclusion and exclusion criteria). Author JO subsequently reviewed the references of the publications yielded by the search to identify additional relevant articles. Authors JO, MAH and CSW worked collaboratively to review and categorise each publication in terms of its quality of evidence (Eccles et al., 2001; Moher et al., 2009). The included articles were then summarised with reference to: (1) first study author, year, and country; (2) study design; (3) type of curricula; (4) assessment; and (5) key outcomes related to clinical reasoning (Table 2).

Figure 1. Flow diagram used in search strategy: PRISMA flow chart
III. RESULTS
A. Summary of Search Strategy
The primary literature search generated the most results from Pubmed, Scopus and Google Scholar (Pubmed n=129, Scopus n=28 and Google Scholar n=50). Search results after the first 5 pages on Google Scholar were not considered for inclusion as these pages contained no relevant reports. After the exclusion of duplicates and screening at the title and abstract levels, the application of the inclusion and exclusion criteria upon reading the full text of candidate papers resulted in a further 11 reports being excluded on the basis that they did involve
medical students, clinical contexts or had their full texts available. Eleven studies were admitted to the final scoping review (Figure 1).
Table 2 illustrates an overview of each included study. The curriculum was classified based on the teaching methodology described by Fabry et al. (2022), which entailed dividing the typology into group size and didactic principles, i.e., flipped classroom or bed-side teaching. Due to multifaceted teaching concepts, some studies are included under more than one subheading.
|
First author (year, country) |
Study design |
Type of Curriculum |
Assessment |
Key outcome |
|
Gong et al., (2022) China
|
Randomised-Controlled |
Bedside teaching; team-based learning |
Computer-based case simulation; Mini-CEX; Questionnaire |
Creating a role shift to support and develop awareness of diagnostic steps and team-based mutual critical thinking. Significant improvement of satisfaction, clinical judgement, counseling skills in favor of the intervention group.
|
|
Bye et al., (2009) University of Sydney, Australia |
Randomised-Crossover |
Interactive lecture vs. computerised tutorial. |
Expert Observation; Questionnaire |
Interactive lecture was perceived as being more enjoyable, more effective in teaching clinical reasoning than observation. Face-to-face teaching considered critical to maximising the value of computer-assisted self-learning.
|
|
Yousefichaijan et al., (2016) Amir Kabir Hospital, Iran |
Semi-experimental study |
Workshop |
Clinical-reasoning tests (Diagnostic Thinking Inventory (DTI), Key Features and Clinical Reasoning Problems) |
This study emphasises the lack of teaching concepts of medical data acquisition techniques of reasoning steps. Effective example of repeatedly practicing clinical reasoning as a practical skill by working in small groups on illness scenarios of real medical histories.
|
|
Konopasek et al., (2014) New York-Presbyterian Hospital, Graduate Medical Education, New York, NY, USA
|
Experimental study |
Group Objective Structured Clinical Experience (OSCE); practice of communication skills and Multi- Source Feedback (MSF)
|
Questionnaire |
Studies emphasise the relationship between efficient communication skills, diagnostic accuracy, patient adherence, and positive health outcomes. Additionally this approach used problem-solving exercises based on dual-process theory. Students were instructed to consciously work through their first pattern recognition and second hypothesis-data driven clinical assumptions. Significant improvements of self-efficacy, confidence and learning motivation in the post-training scores.
|
|
Rideout & Raszka (2018) University of Vermont Children’s Hospital, USA |
Comparative studies
|
Simulation Case (Hypovolemic Shock in a Child) |
Questionnaire and Evaluation |
Simulation of rapid critical-illness recognition, diagnostic interpretation, decision-making, management, and procedural skills with the motto: learning from your mistakes. Improvements were noted in clinical judgement in critical situations, procedural and team skills.
|
|
Bhardwaj et al., (2022) University of Florida College of Medicine, USA
|
Longitudinal Survey
|
Script Concordance Test (SCT) |
Written Exam: Comparing the SCT to usual clinical assessments |
Significant correlations between SCT, as ambiguous evolving clinical case scenario, and improved decision-making competency and valid assessment items. The SCT facilitated feedback and meaningful conversation about problem-solving insecurities
|
|
Wright et al., (2019) University of Western Australia |
Retrospective study |
Feedback Learning Opportunities (FLO) |
Multi-source feedback |
Prescence of FLOs in complex cases underlines one problem: insufficient clinical information related to clinical reasoning. Advantages shown for systematic feedback-related advice to handle diagnostic and treatment inaccuracies and the learning of alternatives
|
|
Forbes & Foulds (2023) Department of Pediatrics, University of Alberta, Edmonton, Canada
|
Comparative study |
Team-based learning (TBL) with Key Feature Questions (KFQ) |
Written and oral exam involving KFQ, OSCE and MCQ. Anonymous evaluation |
Significant improvement in KFQ scores. Valuable feedback on team-based approach on KFQ to progress clinical reasoning Ability to experience mistakes and identifying “learning gaps”
|
|
Khera et al., (2020) McGovern Medical School at the University of Texas Health Science Center, USA |
Non-experimental descriptive studies |
Skill session on writing patient assessments
|
Written exam involving Pre- and post-written patient assessments |
Introduction and practice of the efficient usage of semantic qualifiers for key problem summaries. Positive effect demonstrated when practicing the formulation, synthesising, and reviewing of potential differential diagnoses and integration of clinical reasoning.
|
|
Lissinna et al., (2022) Department of Pediatrics, University of Alberta, Edmonton Clinic, Canada
|
Qualitative Study |
Pediatric bootcamp using flipped classroom |
Questionnaire and Evaluation |
Positive effects of pre-readings and virtual interactive illness approach on efficiency of clinical data collection, critical-thinking and new mental approach to learning strategies in low stakes environment. Showed possible benefits from the preclinical-clinical transition. |
|
Schmidt & Grigull (2018) Medizinischen Hochschule Hannover (MHH), Germany |
Qualitative Study |
Interactive Serious Game: “Pedagotchi,” for case-based learning; blended learning |
Questionnaire System Usability Scale (SUS) and User Experience Questionnaire (UEQ) |
Motivational and digital additions to traditional lectures. Improved dialogue, real-time feedback and practice of clinical-reasoning in a low-stakes environment. |
Table 2. Overview of reports included in scoping review
B. Source of Studies and Research Design
Included studies came from 6 countries, in general being conducted at university hospitals. The largest group of included studies (n=4) originated in the USA (Bhardwaj et al., 2022; Khera et al., 2020; Konopasek et al., 2014; Rideout & Raszka, 2018). Two articles came from Australia (Bye et al., 2009; Wright et al., 2019) and Canada (Forbes & Foulds, 2023; Lissinna et al., 2022). Single studies were derived from China (Gong et al., 2022), Germany (Schmidt & Grigull, 2018) and Iran (Yousefichaijan et al., 2016).
We categorised the evidence in each publication based on an established evidence hierarchy (Table 3) (Eccles et al., 2001; Jensen et al., 2004). No reviewed study could be aligned to criterion 1a, i.e., evidence from meta-analysis of randomised controlled trials. Two studies employed a randomised-control design, with Bye et al. conducting a crossover controlled design (Bye et al., 2009; Gong et al., 2022). The method of employing a quasi-experimental study was conducted by two included studies (Konopasek et al., 2014; Yousefichaijan et al., 2016). The majority of included studies could be aligned with category III, i.e., evidence from non-experimental descriptive methods, or more specifically longitudinal surveys (Bhardwaj et al., 2022), retrospective studies (Wright et al., 2019) and qualitative approaches (Forbes & Foulds, 2023; Khera et al., 2020; Lissinna et al., 2022; Rideout & Raszka, 2018; Schmidt & Grigull, 2018).
|
Category of evidence |
Number of studies identified on each rank |
|
Ia: evidence from meta-analysis of randomised controlled trials |
|
|
Ib: evidence from at least one randomised controlled trial |
n=2 Gong et al., 2022; Bye et al., 2009 |
|
IIa: evidence from at least one controlled study without randomisation |
|
|
IIb: evidence from at least one other type of quasi-experimental study |
n=2 quasi-experimental Yousefichaijan et al., 2016; Konopasek et al., 2014 |
|
III: evidence from non-experimental descriptive studies, such as comparative studies, correlation studies |
n=7 Longitudinal survey: Bhardwaj et al., 2022 Qualitative study: Lissinna et al., 2022; Khera et al., 2020; Rideout & Raszka, 2018; Forbes & Foulds, 2023; Schmidt & Grigull, 2018. Retrospective study: Wright et al., 2019 |
|
IV: evidence from expert committee reports or opinions and ⁄ or clinical experience of respected authorities |
|
Table 3. Included studies categorised according to levels of evidence defined by Eccles et al. (2001)
C. Summary based on Type of Evidence
The key outcomes derived from the included studies mostly focused on the principle of problem-based learning and can be framed in reference to experiential learning, such as clinical simulation and the acquisition of theoretical reasoning skills (Fabry, 2022; Jensen et al., 2004).
1) Experiential learning: There is evidence, based on the following studies, indicating that a team-based approach of clinical scenarios, with patients or simulated scenarios facilitate the impartation of clinical skills and critical thinking. The role shift towards student-centered learning increases the motivation to actively participate and overcome passive decision-making (Gong et al., 2022). The randomised study by Gong et al. established a division of bedside tasks (i.e., medical history, physical examination, etc.) amongst the case group students. This facilitated knowledge exchange within the team, and enabled both awareness and practice of reasoning steps. Subsequent assessment using computer-based case simulations and the Mini-CEX (Mini Clinical Evaluation Exercise) detected significant improvements in clinical judgment and counselling skills after bedside team-based learning (Gong et al., 2022). In reference to critical thinking, all of the included studies demonstrated a preference for students to encounter and use real cases involving ambiguity, symptom polymorphisms and the possibility of false leads in the context of paediactric practice (Kassirer, 2010).
Forbes and Foulds (Forbes & Foulds, 2023) found that students’ evaluations of team-based learning showed that positive feedback on the ability to use the experiences of mistakes were linked with significant improvements in assessment scores using the Observed Structured Clinical Exam (OSCE).
Similarly, a survey by Rideout and Raszka (Rideout & Raszka, 2018) highlighted that increased team skills can result from feedback exchange and lead to the improvement of communication skills learnt during simulation, including working in intensive ettings and with distressed parents (Konopasek et al., 2014; Rideout & Raszka, 2018). In addition, improved motivation to learn was related to learning in a low-stakes environment (Lissinna et al., 2022; Rideout & Raszka, 2018; Schmidt & Grigull, 2018). Wright et al. reported that student log entries underlined the advantages of feedback-related advice in handling diagnostic and treatment inaccuracies (Wright et al., 2019).
A technique called the Group Objective Structured Clinical Experience used by Konopasek et al. (Konopasek et al., 2014) showed benefits for the learner-centered method through the practice of communication skills in teams during the process of clinical reasoning. This approach brought together experiential learning, multisource feedback and the perspective of dual-process theory in directing students to begin with their recognition of symptoms, then consider hypotheses based on history taking, and information and feedback from multiple parties (Table 2). In a questionnaire-based evaluation such clinical problem solving demonstrated significant increases in self-efficacy and their motivation to learn data gathering techniques (Konopasek et al., 2014).
A further example, Khera et al. (Khera et al., 2020) focused on written patient information prioritisation by using semantic qualifiers to efficiently summarise key problems. Semantic qualifiers are bipolar descriptions of symptoms linked to distil broad medical histories (Norman, 2005). The comparison of pre- and post-intervention evaluation resulted in statistically significant increases in differential diagnosis assessment scores (Khera et al., 2020).
Furthermore, half of the included studies identified multi-source feedback (student, teacher, patient) as being integral to the development of insight into their reasoning and decision-making processes. Feedback itself can proactively influence students’ awareness about their mistakes allowing a meaningful conversation about areas of confusion.
2) Theoretical reasoning skills: Examples of didactic approaches included the use of short-term workshops, flipped classroom teaching, virtual learning experiences, and script-concordance tests. These teaching methods resulted in improved awareness of theory, development of knowledge structures, data prioritisation, and critical thinking (Yousefichaijan et al., 2016). More specifically, half of the studies acknowledged the incorporation of a medical data acquisition technique as being a useful approach to teaching, since diagnostic inaccuracy can be linked with a lack of accurate data gathering (Bye et al., 2009). In reference to these diagnostic techniques, the workshop of Yousefichaijan et al. is an effective example of repeatedly practicing clinical reasoning as a pragmatic skill (Yousefichaijan et al., 2016). Comparing analyses of the Diagnostic Thinking Inventory (DTI) and Clinical Reasoning Problem (CRP) showed significant advantages of working in small groups on illness scenarios (Yousefichaijan et al., 2016). Lissinna et al. (2022) employed a virtual flipped classroom exercise, and then assessed students’ experiences of pre-reading and their practice of efficient sorting of clinically relevant data via semi-structured interviews. The concept of Blended-Learning, as a combination of digital and traditional teaching, embodies the Serious Game approach of Schmidt et al. (2018). The complementary results of Bye et al.’s comparative study, which focused on interactive versus computerised methods of pedagogy, underlines the advantages of the digital addition in the practice of interactive case-based learning with real-time feedback (Bye et al., 2009). In consideration of the aforementioned aspects, the implementation of the Script-Concordance Test that assesses case training, can reveal several advantageous measurements, related to pedagogical techniques using case-based and feedback methods and thus can be regarded as a valid assessment tool (Bhardwaj et al., 2022).
IV. DISCUSSION
A. Clinical Reasoning – A Complex Practical Skill
The findings from this scoping review affirm that clinical reasoning can be described as the mediatory link influencing a clinician’s cognitive multistep process. This process involves knowledge organisation, efficient data gathering, critical data integration culminating in generating a set of reasonable hypotheses, to finally achieve accurate diagnostic interpretation and reflection (Lissinna et al., 2022; Pennaforte et al., 2016; Pinnock et al., 2021). From a data driven perspective, used by novice learners, teaching these reasoning steps separately would likely impair the effectiveness of the reasoning process (Schmidt & Mamede, 2015). At the moment no peer-reviewed paediatric curricula guidelines focus on active educational experience of clinical reasoning. Additionally, short paediatric rotations only allow limited practice of common paediatric diagnoses (Madduri et al., 2024).
Consistent with Miller’s pyramid of clinical competence learning clinical skills effectively, involves promoting practice by doing, along with frequent repetition (Fabry, 2022; Miller, 1990). In reference to the dual-process model, repetition moves much of the cognitive effort involved in understanding the relevant illness presentation from system 2 to the pattern recognition abilities of system 1 (Yazdani et al., 2017). Considering clinical reasoning as a practical skill, student passivity is the reason why it is relatively difficult to attain a high level of competency (Forbes & Foulds, 2023). Ulfa et al. (2021) used a randomised control trial comparing lecture vs. team-based learning of postpartum hemorrhage of midwifery students. The results indicated the superiority of active team-based methods on the development of independent and effective critical-thinking abilities. This suggests substantial benefits for a paediatric curricula configuration that involves implementation of more active learning experiences starting in the pre-clinical years in the form of mixed teaching strategies (Forbes & Foulds, 2023; Jost et al., 2017; Koenemann et al., 2020). Jost and colleagues observed significantly improved clinical reasoning performance with Team-Based Learning groups in an undergraduate neurology course using key-feature examination (Jost et al., 2017).
B. Mix of Teaching Methods
In reference to this scoping review’s aim, we can identify the advantages of combining different teaching styles. Lectures remain the fundamental method used to convey basic scientific knowledge, which can be an essential precondition for using more practical teaching methods. The findings indicated that improvements of the decision-making process were first identified by theory presentation, i.e., teaching dual-process theory and its links to common cognitive pitfalls and the potentially significant adverse consequences for paediatric clinical reasoning (Schmidt & Mamede, 2015). However, lectures also have didactic disadvantages, which include teacher-centered explanations with less activation and linking of previous knowledge and may create cognitive overload in learners (Fabry, 2022). There are different options to overcome this by promoting active pre-class learning and open discussions about information processing ambiguities (Lissinna et al., 2022). For example, the use of the flipped classroom approach can improve clinical understanding and increase the motivation to learn in contrast to lecture-based approaches (Tang et al., 2017). The crossover study of Tan et al. (Tan et al., 2016) also indicated superior problem-solving ability attributed to team-based learning in comparison with interactive lectures. Similarly, Jackson et al. (Jackson et al., 2020) demonstrated a significant increase in satisfaction when using critical thinking and promoting student self-directed learning when attending an online team-based learning module in a family medicine rotation.
C. Clinical Reasoning and Clinical Cases
The simulation of clinical judgment can be enhanced using an evolving clinical scenario (Fabry, 2022). The focus on improvement of clinical judgment in paediatrics can be justified by a unique interaction of fine perception and empathy of the child’s clinical problem. In particular, the practice of effective communication plays a critical role in the analyses of symptoms when in discussion with parents and children. Since both are overlaid with anxiety, this adds to the diagnostic challenge. This requires experiential learning, for example by the careful student-centered bedside practice of communication with anxious and vulnerable families. This can increase students’ awareness of emotional messages and changes in the patient. The link of promoting empathy by teaching problem-solving plays a critical role in paediatrics (Gong et al., 2022). One example, could be the use of Illness scripts, describing an approach to synthesising patient history into a meaningful flowchart. Levin et al. and Konemann et al. showed students’ motivation working on real complex cases embodying a step-by-step information disclosure approach (Koenemann et al., 2020; Levin et al., 2016). Interestingly, Schmidt and Mamede also described these two opposing ways to present clinical cases, calling them “serial-cue” vs. “whole case” methods (Schmidt & Mamede, 2015). The studies included in this review emphasised students’ challenges with obtaining the correct collection of critical information for a stepwise disclosure in paediatrics.
Furthermore, the randomised trial protocol of Pennaforte et al., embodies an example of combining real-environment patient simulation and iterative discussions (Pennaforte et al., 2016). These discussion protocols appear as reminders at three key moments in time, namely data gathering, integration, and confirmation. The reminder and task verbalisation provide better insight into the dynamic systems, based on the dual-process theory. Debriefing thoughts, in the form of thinking aloud and self-explanation, could promote higher performance of active understanding, more accurate symptom correlations, deliberate reflection and especially detecting pitfalls in the reasoning process (Chamberland et al., 2015; Pennaforte et al., 2016).
Studies revealed the important role of appropriate and timely feedback on the overall improvement of a clinical skill (DeLeon et al., 2018; Fabry, 2022; Wright et al., 2019). Torre et al., identifies the contribution of bedside teaching and multi-source feedback (supervisor, students, and patients) as an essential part of enhancing students’ perceptions and understandings of a meaningful teaching experience (Torre et al., 2005). Feedback allows access to different perspectives, which can promote learning capacity; it is clearly regarded as a positive and proactive influence on the personal development required for successful teamwork (Koenemann et al., 2020).
The constant reference to decision making should not be regarded as relevant only to the clinician’s perspective since effective disease management in paediatric care also depends on decisions being made by the patient and the child’s parents and care givers. Consequently, we also need to focus on shared decision-making and communication skills as a crucial part of such deliberation (Gay et al., 2013). Patient-centered communication includes personal factors, like empathy and authenticity, which are essential when building a trusted and authentic clinician-patient relationship. Additionally, these skills can be seen as a tool for efficiently eliciting information and in the communication of treatment information, including medication information, to parents and children (Konopasek et al., 2014; Yousefichaijan et al., 2016). Effective communication skills of this sort increase patient adherence, especially when treatment strategies are planned in consensus with the patient (Amey et al., 2017).
V. CONCLUSION
Our scoping review illustrated a knowledge gap regarding the teaching of clinical reasoning as a practical skill in paediactric practice. The findings indicate that active student-centered repetition involving experiential learning would likely facilitate more effective learning during clinical reasoning in paediatrics as aligned with the following key steps. Firstly, it would facilitate activation of prior knowledge, supporting clinically relevant knowledge structure and ensuring accurate data gathering techniques. Secondly, the simulation of critical thinking is required to improve the process of reflection to reduce cognitive biases and pitfalls. And thirdly, such an approach would promote efficient communication and the development of feedback skills to overcome diagnostic and treatment inaccuracies. Despite our comprehensive search and the international representation present in the evidence-based studies included in our review, the total number of medical education studies in paediatrics related to clinical reasoning was limited, which underlines the need for further research and curricular development in this domain, particularly given the known unique challenges of the care of paediatric patients.
Notes on Contributors
Dr. Jasmin Oezcan was involved in the conceptualisation of the study, review of the literature, analysis of included reports and in the writing and revision of the manuscript.
Associate Professor Marcus A. Henning was involved in the development of the final list of papers considered for the review and in the writing and revision of the manuscript.
Associate Professor Craig S. Webster was involved in the development of the final list of papers considered for the final review, and in the writing and revision of the manuscript.
All authors have read and approved the final version of the manuscript and agree to be accountable for the work and its findings.
Ethical Approval
This manuscript comprises a scoping review of existing published reports and, therefore did not require approval from institutional review boards.
Data Availability
All relevant quantitative data are within the manuscript.
Acknowledgement
This work was conducted by Dr. Jasmin Oezcan as a visiting scholar at the Centre for Medical and Health Science Education, School of Medicine, University of Auckland, New Zealand. The authors also wish to thank Professor Cameron Grant, Head of the Department of Paediatrics, Child and Youth Health, for helpful insights regarding the development of teaching programs for primary care practitioners in child health and paediatrics in New Zealand.
Funding
There is no external funding involved in this study.
Declaration of Interest
Associate Professor Marcus Henning is an Editor of The Asia Pacific Scholar. Other authors have no conflicts of interest.
References
Amey, L., Donald, K. J., & Teodorczuk, A. (2017). Teaching clinical reasoning to medical students. British Journal of Hospital Medicine, 78(7), 399-401. https://doi.org/10.12968/hmed.2017.78.7.399
Bargh, J. A., & Chartrand, T. L. (1999). The unbearable automaticity of being. American Psychologist, 54(7), 462–479. https://doi.org/10.1037/0003-066X.54.7.462
Bhardwaj, P., Black, E. W., Fantone, J. C., Lopez, M., & Kelly, M. (2022). Script concordance tests for formative clinical reasoning and problem-solving assessment in General Pediatrics. MedEdPORTAL, 18, 11274. https://doi.org/10.15766/mep_2374-8265.11274
Bye, A. M., Connolly, A. M., Farrar, M., Lawson, J. A., & Lonergan, A. (2009). Teaching paediatric epilepsy to medical students: A randomised crossover trial. Journal of Paediatrics and Child Health, 45(12), 727-730. https://doi.org/10.1111/j.1440-1754.2009.01602.x
Chamberland, M., Mamede, S., St-Onge, C., Setrakian, J., Bergeron, L., & Schmidt, H. (2015). Self-explanation in learning clinical reasoning: The added value of examples and prompts. Medical Education, 49(2), 193-202. https://doi.org/10.1111/medu.12623
Croskerry, P. (2005). Diagnostic failure: A cognitive and affective approach. In K. Henriksen, J. B. Battles, E. S. Marks, & D. I. Lewin (Eds.), Advances in Patient Safety: From Research to Implementation (Vol. 2, pp. 241-254). PsycEXTRA Dataset. https://doi.org/10.1037/e448242006-001
de Jong, T., & Ferguson-Hessler, M. G. M. (1996). Types and qualities of knowledge. Educational Psychologist, 31(2), 105-113. https://doi.org/10.1207/s15326985ep3102_2
DeLeon, S., Mothner, B., & Middleman, A. (2018). Improving student documentation using a feedback tool. The Clinical Teacher, 15(1), 48-51. https://doi.org/10.1111/tct.12625
Eccles, M., Freemantle, N., & Mason, J. (2001). Using systematic reviews in clinical guideline development. In M. Egger, G. D. Smith, & D. G. Altman (Eds.), Systematic Reviews in Health Care (pp. 400-409). Wiley Online Library. https://doi.org/10.1002/9780470693926.ch21
Fabry, G. (2022). Medical Didactics- A competence-orientated, practical and scientific-funded education. Hogrefe.
Forbes, K. L., & Foulds, J. L. (2023). A team-based learning approach during pediatric clerkship to promote clinical reasoning. Academic Pediatrics, 23(7), 1459-1464. https://doi.org/10.1016/j.acap.2023.04.002
Gay, S., Bartlett, M., & McKinley, R. (2013). Teaching clinical reasoning to medical students. The Clinical Teacher, 10(5), 308-312. https://doi.org/10.1111/tct.12043
Gong, J., Du, J., Hao, J., & Li, L. (2022). Effects of bedside team-based learning on pediatric clinical practice in Chinese medical students. BMC Medical Education, 22(1), Article 264. https://doi.org/10.1186/s12909-022-03328-4
Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165(13), 1493-1499. https://doi.org/10.1001/archinte.165.13.1493
Grant, M. J., & Booth, A. (2009). A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information & Libraries Journal, 26(2), 91-108. https://doi.org/10.1111/j.1471-1842.2009.00848.x
Groen, G. J., & Patel, V. L. (1985). Medical problem-solving: Some questionable assumptions. Medical Education, 19(2), 95-100. https://doi.org/10.1111/j.1365-2923.1985.tb01148.x
Gruppen, L. D., & Frohna, A. Z. (2002). Clinical Reasoning. In G. R. Norman, C. P. M. van der Vleuten, D. I. Newble, D. H. J. M. Dolmans, K. V. Mann, A. Rothman, & L. Curry (Eds.), International Handbook of Research in Medical Education (pp. 205-230). Springer. https://doi.org/10.1007/978-94-010-0462-6_8
Jackson, L., Otaki, F., Powell, L., Ghiglione, E., & Zary, N. (2020). Study of a COVID-19 induced transition from face-to-face to online team-based learning in undergraduate family medicine. MedEdPublish, 9(1), 232. https://doi.org/10.15694/mep.2020.000232.1
Jensen, L. S., Merry, A. F., Webster, C. S., Weller, J., & Larsson, L. (2004). Evidence-based strategies for preventing drug administration error during anaesthesia. Anaesthesia, 59(5), 493-504. https://doi.org/10.1111/j.1365-2044.2004.03670.x
Jost, M., Brüstle, P., Giesler, M., Rijntjes, M., & Brich, J. (2017). Effects of additional team-based learning on students’ clinical reasoning skills: A pilot study. BMC Research Notes, 10(1), Article 282. https://doi.org/10.1186/s13104-017-2614-9
Kassirer, J. P. (2010). Teaching clinical reasoning: Case-based and coached. Academic Medicine, 85(7), 1118-1124. https://doi.org/10.1097/acm.0b013e3181d5dd0d
Khera, S., Gavvala, S., Parlar-Chun, R., Huh, H., Hsu, J., & Ford, C. (2020). Skill session on writing patient assessments for pediatric clerkship students. MedEdPORTAL, 16. https://doi.org/10.15766/mep_2374-8265.11029
Koenemann, N., Lenzer, B., Zottmann, J. M., Fischer, M. R., & Weidenbusch, M. (2020). Clinical case discussions – A novel, supervised peer-teaching format to promote clinical reasoning in medical students. GMS Journal for Medical Education, 37(5), Doc48. https://doi.org/10.3205/zma001341
Konopasek, L., Kelly, K. V., Bylund, C. L., Wenderoth, S., & Storey-Johnson, C. (2014). The group objective structured clinical experience: building communication skills in the clinical reasoning context. Patient Education and Counseling, 96(1), 79-85. https://doi.org/10.1016/j.pec.2014.04.003
Lee, A., Joynt, G. M., Lee, A. K., Ho, A. M., Groves, M., Vlantis, A. C., Ma, R. C., Fung, C. S., & Aun, C. S. (2010). Using illness scripts to teach clinical reasoning skills to medical students. Family Medicine, 42(4), 255-261.
Levin, M., Cennimo, D., Chen, S., & Lamba, S. (2016). Teaching clinical reasoning to medical students: A case-based illness script worksheet approach. MedEdPORTAL, 12, Article 10445. https://doi.org/10.15766/mep_2374-8265.10445
Lissinna, B., Rashid, M., Foulds, J. L., & Forbes, K. L. (2022). Embracing uncertainty: Medical student perceptions of a pediatric bootcamp developed in response to mandated changes during the pandemic. BMC Medical Education, 22(1), Article 390. https://doi.org/10.1186/s12909-022-03471-y
Madduri, G. B., Torwekar, E. L., Demirel, S., Durham, M., Hauff, K. I., Kaul, R., Nichols, T., Ravid, N. L., Shaner, M. A., & Rassbach, C. E. (2024). CRISP: An inpatient pediatric curriculum for family medicine residents using clinical reasoning and iIllness scripts. MedEdPORTAL, 20, Article 11393. https://doi.org/10.15766/mep_2374-8265.11393
Marcum, J. A. (2012). An integrated model of clinical reasoning: Dual-process theory of cognition and metacognition. Journal of Evaluation in Clinical Practice, 18(5), 954-961. https://doi.org/10.1111/j.1365-2753.2012.01900.x
Miller, G. E. (1990). The assessment of clinical skills/competence/performance. Academic Medicine, 65(9), S63-S67. https://doi.org/10.1097/00001888-199009000-00045
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Norman, G. (2005). Research in clinical reasoning: Past history and current trends. Medical Education, 39(4), 418-427. https://doi.org/10.1111/j.1365-2929.2005.02127.x
Page, G., Bordage, G., & Allen, T. (1995). Developing key-feature problems and examinations to assess clinical decision-making skills. Academic Medicine, 70(3), 194-201. https://doi.org/10.1097/00001888-199503000-00009
Pennaforte, T., Moussa, A., Loye, N., Charlin, B., & Audétat, M. C. (2016). Exploring a new simulation approach to improve clinical reasoning teaching and assessment: Randomised trial protocol. MIR Research Protocols, 5(1), e26. https://doi.org/10.2196/resprot.4938
Pinnock, R., Ritchie, D., Gallagher, S., Henning, M. A., & Webster, C. S. (2021). The efficacy of mindful practice in improving diagnosis in healthcare: A systematic review and evidence synthesis. Advances in Health Sciences Education, 26(3), 785-809. https://doi.org/10.1007/s10459-020-10022-x
Pinnock, R., & Welch, P. (2014). Learning clinical reasoning. Journal of Paediatrics and Child Health, 50(4), 253-257. https://doi.org/10.1111/jpc.12455
Rideout, M., & Raszka, W. (2018). Hypovolemic shock in a child: A pediatric simulation case. MedEdPORTAL, 14, Article 10694. https://doi.org/10.15766/mep_2374-8265.10694
Schardt, C., Adams, M. B., Owens, T., Keitz, S., & Fontelo, P. (2007). Utilisation of the PICO framework to improve searching PubMed for clinical questions. BMC Medical Informatics and Decision Making, 7(1), Article 16. https://doi.org/10.1186/1472-6947-7-1
Schmidt, H. G., & Mamede, S. (2015). How to improve the teaching of clinical reasoning: A narrative review and a proposal. Medical Education, 49(10), 961-973. https://doi.org/10.1111/medu.12775
Schmidt, R., & Grigull, L. (2018). Pedagotchi: Entwicklung einer neuartigen Lernanwendung für die Pädiatrie. Monatsschrift Kinderheilkunde, 166(3), 228-235. https://doi.org/10.1007/s00112-017-0253-9
Schwartz, A., & Elstein, A. (2008). Clinical reasoning in medicine. In J. Higgs, M. Jones, S. Loftus, & N. Christensen (Eds.), Clinical Reasoning in the Health Professions (pp. 223-234). Elsevier.
Scott, I. A. (2009). Errors in clinical reasoning: causes and remedial strategies. BMJ, 338, b1860. https://doi.org/10.1136/bmj.b1860
Tan, N., Tan, K., & Ng, C. (2016). Does team-based learning improve clinical reasoning in neurology? Neurology, 86(16_supplement). https://doi.org/10.1212/wnl.86.16_supplement.p2.373
Tang, F., Chen, C., Zhu, Y., Zuo, C., Zhong, Y., Wang, N., Zhou, L., Zou, Y., & Liang, D. (2017). Comparison between flipped classroom and lecture-based classroom in ophthalmology clerkship. Medical Education Online, 22(1), Article 1395679. https://doi.org/10.1080/10872981.2017.1395679
Torre, D. M., Simpson, D., Sebastian, J. L., & Elnicki, D. M. (2005). Learning/feedback activities and high-quality teaching: Perceptions of third-year medical students during an inpatient rotation. Academic Medicine, 80(10), 950-954. https://doi.org/10.1097/00001888-200510000-00016
Ulfa, Y., Igarashi, Y., Takahata, K., Shishido, E., & Horiuchi, S. (2021). A comparison of team-based learning and lecture-based learning on clinical reasoning and classroom engagement: A cluster randomised controlled trial. BMC Medical Education, 21(1), Article 444. https://doi.org/10.1186/s12909-021-02881-8
Vanhecke, T. E. (2008). Zotero. Journal of the Medical Library Association, 96(3), 275.
Webster, C. S., Anderson, B. J., Stabile, M. J., Mitchell, S., Harris, R., & Merry, A. F. (2021). Improving the safety of pediatric sedation: Human error, technology, and clinical microsystems. In K. P. Mason (Ed.), Pediatric Sedation Outside of the Operating Room, 721–752. https://doi.org/10.1007/978-3-030-58406-1_38
Webster, C. S., Taylor, S., Thomas, C., & Weller, J. M. (2022). Social bias, discrimination and inequity in healthcare: Mechanisms, implications and recommendations. BJA Education, 22(4), 131-137. https://doi.org/10.1016/j.bjae.2021.11.011
Webster, C. S., Taylor, S., & Weller, J. M. (2021). Cognitive biases in diagnosis and decision making during anaesthesia and intensive care. BJA Education, 21(11), 420-425. https://doi.org/10.1016/j.bjae.2021.07.004
Wright, H. M., Maley, M. A. L., Playford, D. E., Nicol, P., & Evans, S. F. (2019). Feedback learning opportunities from medical student logs of paediatric patients. BMC Medical Education, 19(1), Article 107. https://doi.org/10.1186/s12909-019-1533-y
Yazdani, S., Hosseinzadeh, M., & Hosseini, F. (2017). Models of clinical reasoning with a focus on general practice: A critical review. Journal of Advances in Medical Education & Professionalism, 5(4), 177-184.
Yousefichaijan, P., Jafari, F., Kahbazi, M., Rafiei, M., & Pakniyat, A. (2016). The effect of short-term workshop on improving clinical reasoning skill of medical students. Medical Journal of the Islamic Republic of Iran, 30, 396.
Zhang, Y., Huang, L., Zhou, X., Zhang, X., Ke, Z., Wang, Z., Chen, Q., Dong, X., Du, L., Fang, J., Feng, X., Fu, J., He, Z., Huang, G., Huang, S., Ju, X., Gao, L., Li, L., Li, T., … Sun, K. (2019). Characteristics and workload of pediatricians in China. Pediatrics, 144(1), e20183532. https://doi.org/10.1542/peds.2018-3532
*Dr. Jasmin Oezcan
Department of Pediatrics Erlangen
University Hospital Erlangen,
Loschgestraße 15, 91054 Erlangen, Germany,
Email: oezcanj@yahoo.de
Submitted: 5 March 2024
Accepted: 14 October 2024
Published online: 1 April, TAPS 2025, 10(2), 17-33
https://doi.org/10.29060/TAPS.2025-10-2/RA3261
Cheng Li & Gunjeong Lee
School of Nursing, Ewha Womans University, Republic of Korea
Abstract
Introduction: This study aims to explore the development of nurse prescribing and identify nurse prescribing implementation and challenges in China.
Methods: Conducted as a systematic review adhering to the PRISMA, this study involved a comprehensive literature search across various databases. A timeline mapping and a region mapping were conducted.
Results: A total of 28 articles from databases were included in the study. The growth of nursing education and research, the emergence of specialty nurses, and the establishment of nurse-led clinics have contributed to the advancement of nurse prescribing in China. Presently, approximately half of the 34 regions in China are either actively researching or preparing for nurse prescribing involving medication.
Conclusion: Based on the findings, several tasks have been identified for the implementation of nurse prescribing in China. Firstly, it is imperative to elevate the overall level of nursing education and revise the existing curriculum to equip nursing students with the necessary knowledge and skills required for prescribing. Secondly, it is crucial to establish a systematic qualification system for prescribing nurses, defining the roles of specialty nurses and advanced practice nurses. Thirdly, the development of nurse prescribing includes scope of nursing practice and prescribing protocols are essential. Lastly, extension of the geographic reach of legislation and pilot projects is needed to realise the nationwide implementation of nurse prescribing.
Keywords: Nursing, Health Professional, Prescribing
Practice Highlights
- Nurse prescribing is fueled by the emergence of specialty nurses and nurse-led clinics.
- There are regional disparities in readiness for nurse prescribing.
- The key tasks are enhancing nursing education, qualification systems, and prescribing protocols.
I. INTRODUCTION
A. Background
Prescribing is a complex process requires deep understanding of pharmacology and disease, clinical judgement on risks and benefits of a treatment under an unpredictable context (Abuzour et al., 2018). The International Council of Nurses (ICN) stated that prescribing is an evolving process involving information gathering, clinical decision-making, communication, and evaluation which results in the initiation, continuation, or cessation of a medication (International Council of Nurses, 2021).
The extension of prescriptive authority to nurses has taken place for several reasons. First, nurse prescribing contributes to efficient and effective patient care and the quality and continuity of care (Gielen et al., 2014). Second, nurse prescribing accommodates nurses’ professional skills, increases nurses’ autonomy, and minimises unnecessary time waste for medical practitioners and patients (Kilańska et al., 2022). Third, the patient outcome of nurse prescribing is indicated as similar or better compared to the prescribing of other healthcare professionals (Ling et al., 2018; McMenamin et al., 2023).
The legislative expansion of prescriptive authority for nurses has taken place in the 1980s in the USA, 1990s in the UK, at the turn of the 21st Century in Canada, Europe, Australia, New Zealand, some countries of Africa, and Spain. As of 2021, 44 countries were reported to have formal laws or regulations that authorise nurse prescribing (International Council of Nurses, 2021; Maier, 2019).
Nurse prescribing is identified by scholars as sensitive to the country’s context and the healthcare culture, defining and implementing of nurse prescribing follows a distinctive pattern in different countries (International Council of Nurses, 2021; Nissen et al., 2010). The common areas of prescription include medications, therapies and therapeutics, durable medical equipment, appliances and certain dressings, foods designated for specific therapeutic purposes, and electrolytes (International Council of Nurses, 2021). Due to its complexity, the following frameworks and models are formed by scholars and institutions to enhance the understanding of nurse prescribing.
The ICN published the ‘Guidelines on Prescriptive Authority for Nurses’ in 2021, suggesting a framework with five components including education, regulation, authorisation,, scope of practice, and continuing professional development. This guideline adopted a four-category prescribing model (Nissen et al., 2010). This model consists of four categories: independent prescribing, supplementary prescribing (dependent), prescribing via a structured prescribing arrangement (protocol), and prescribing to administer. Each of these four categories in order requires increased skill level, decision-making ability, and accountability of prescriber.
The qualification system of prescribing nurses in different countries and regions is diverse (Maier, 2019). ICN differentiates the post-basic level nurse prescribing from the advanced practice level nurse prescribing. Prescribing nurses at the post-basic level are those who have completed their basic nursing education, and practice nursing as registered nurses (RNs). Prescribing nurses at the advanced practice level are those with a certain period of clinical experience, holding higher credentials such as APN (advanced practice nurse), NP (nurse practitioner) or specialty nurse (International Council of Nurses, 2021).
In China, nurse prescribing is defined as nurses diagnosing and making decisions on diet, psychological health, treatment, disease, and care level of the patients (Ma & Ding, 2018). In 2022, Shenzhen of China passed a medical regulation. This is seen as the first legislation in China that grants prescriptive authority to nurses. The growth of nursing education and research, the emergence of specialty nurses, and the establishment of nurse-led clinics have contributed to the advancement of nurse prescribing in China.
B. Nursing in China
By 2021, the number of registered nurses in China doubled in the last decade and exceeded 5.02 million, nurses fill about 45% of the total number of health professionals and the number of registered nurses per 1,000 population reached 3.56 (National Health Commission of the People’s Republic of China, 2022). The number of RN with a bachelor’s degree or higher has steadily grown for decades, nearly 180,000 in 2010 and 1.36 million in 2020 (National Health Commission of the People’s Republic of China, 2022), 30.4% of whom have received a baccalaureate or higher credential. An increased number of nurses with higher education level accelerates the development of nursing research (Wu, 2022).
Referring to advanced practice nursing in some developed countries, specialty nursing in China umbrellas registered nurses who have received specialised training and been certified by the training institutions, appeared first in the 1990s (Wu, 2022). Oncology, wound ostomy, PICC (Peripherally inserted central catheter), and blood purification are the most common and comparably developed specialties (Wang et al., 2018). Around 8000 nurses participated in specialty nurse (专业护士) training programs run by the Chinese Nursing Association in 2021 (Wu, 2022).
Advanced practice nursing, on the other hand, in 2007, the Guangdong Health Commission worked with the Hong Kong Hospital to prepare 614 APNs of 14 specialties over 4 years (Wong, 2018). To attain an APN credential, nurses are suggested to have a bachelor’s degree, a minimum of 8 years of clinical experience, and 2 years of specialised clinical experience (Wong, 2018). Beijing University in 2017 admitted two candidates to an advanced practice nursing program (Zhang et al., 2022).
A nurse-led clinic is defined as a clinical practice facility where nurses have their own formalised and structured standards to address the healthcare needs of patients and their families (Hatchett, 2003). The common NLCs (护理门诊) of China are run as divisions of outpatients by hospitals. NLCs accommodate specialty nurses and are one of the main settings where pilot nurse prescribing takes place in China (Chen & Peng, 2023; Ling et al., 2018). China first initiated NLCs on maternal health in 1995, psychiatric NLCs in 1997. In 2016, over 900 NLCs in 19 provinces were open, an average number of 2.8 NLCs were operated at each hospital, each NLC accommodated 36 clients a day, and 75.5% of these clinics were PICC NLCs (Gao et al., 2017). 69.3% of the NLC nurses reported that the lack of prescriptive authority is a major challenge they face in NLC nursing (Dong et al., 2022).
Given this global and domestic context, the objective of this study is to examine nurse prescribing in China, offering an overview of its development and implementation, identifying the challenges associated with it.
II. METHODS
The aim of this study is to review, identify, and synthesise the evidence presented in the included literature on nurse prescribing, so to
- Track the development of nurse prescribing in China;
- Describe nurse prescribing implementation in China; &
- Identify challenges faced in nurse prescribing of China
A systematic review was conducted in accordance with the procedure of the PRISMA Statement 2020 (Page et al., 2021). The flow diagram was utilised for the literature search and the checklist was followed as an overall guide of this study.
A. Data Collection
The literature search was conducted on Medline (PubMed), CINAHL, CNKI (China National Knowledge Infrastructure), and Wanfang Data. The records with titles or abstracts containing the terms ‘nurs* prescri*’ (护*处方*)and ‘Chin*’ were expected in this process. The database and document search were conducted from 1 January to 17 June 2023. Articles are included when they present nurse prescribing in China and the full text is available in either Chinese or English. Articles are excluded when the focus is nurse prescribing out of China, or is a single group of a client population or a particular medicine.
B. Data Analysis
A quality assessment was conducted after the screening process, using the Mixed Methods Appraisal Tool 2018 (Hong et al., 2018).
For data analysis, timeline and region mapping were used in former studies to approach nurse prescribing of other countries. In this study, a timeline mapping was conducted to chart the progression of nurse prescribing practices over time. A region mapping was performed focusing on the geographical distribution and implementation of nurse prescribing practices. An overall nurse prescribing profile of China was provided and a discussion on the current practice and indicated challenges was applied.
III. RESULTS
A. Search Outcomes
As a result, a total of 441 studies were taken into the identification process (Figure 1). At the end of the screening, a total number of 28 articles from the databases were included for analysis.

Figure 1. Screening Flow Diagram
CINAHL – Cumulative Index to Nursing and Allied Health Literature
CNKI – China National Knowledge Infrastructure
|
No |
Authors |
Origin |
Purpose |
Research design |
Disciplinary home |
Method/ framework |
Major finding |
|
1 |
Chen L. & Peng G. (2023) |
Guangdong |
To describe nurse prescribing at NLCs in Guangdong |
Quantitative |
Nursing |
No |
Detailed nurse prescribing in Guangdong (content focused) |
|
2 |
Wang, X. et al. (2022) |
Shanxi |
To construct general clinical practice training program for drug prescribing applicants of nurses in China |
Qualitative |
Nursing |
Delphi method |
Three-level indexed training program development and comparison with the US, UK and Ireland. |
|
3 |
Zhang, Q. et al. (2022) |
Shanxi |
To interpret ICN guideline to promote common understanding of nurse prescribing in China |
Qualitative |
Nursing |
ICN Guideline |
Analyses nurse prescribing in China providing interpretation of the guide and comparison of other countries |
|
4 |
Han, S. et al. (2022) |
Shanxi |
To review main research results and application on nurse decision making and prescribing |
Qualitative |
Nursing |
No |
Further research and practice in nursing education, APN, nurse prescribing is needed |
|
5 |
Fan, Y. et al. (2022) |
Henan |
To review development of nurse prescribing globally and summarise theory and practice evidence |
Qualitative |
Nursing |
No |
Provides suggestion for the government, nursing institutions and scholars. |
|
6 |
Xing, M. et al. (2022) |
Zhejiang |
To identify nurse prescribing challenges and advantages in China. |
Qualitative |
Nursing |
SWOT analysis |
Summarises internal and external challenges and advantages and provides future strategies. S-O, W-O, S-T, W-T strategies are proposed. |
|
7 |
Han, S. et al. (2021) |
Shanxi |
To further explore nurse prescribing contents |
Qualitative |
Nursing |
Delphi method |
Conducted a list of nurse prescribing medications, suggested forms and training curriculums of nurse prescribing. 348 nurse prescribing medications, 6-unit training |
|
8 |
Wang, L. et al. (2021) |
Zhejiang, Liaoning |
To identify regulatory challenges in nurse prescribing, suggest effort on liability system and institutional mechanism |
Qualitative |
Law |
No |
Redefines nurse prescribing in China, suggests regulatory support and clarification on liability |
|
9 |
Wang, Y. et al. (2021) |
Shanxi |
To construct the general training syllabus for nurses’ prescription right of applicants for prescription right in different clinical specialist nurses |
Qualitative |
Nursing |
Delphi method |
The constructed training syllabus for clinical specialist nurses was reliable, which could provide basis for prescription right training of clinical specialist nurses. A training guide of nurse prescriber is provided. |
|
10 |
Wang, X. et al. (2021) |
Shanxi |
To conduct a global analysis of nurse prescribing training |
Qualitative |
Nursing |
No |
Identifies challenges, provides suggestions on practical training of nurse prescribing |
|
11 |
Hou, X. (2021) |
Sichuan |
To investigate scope and related factors of nurse prescribing in third-level hospitals |
Qualitative |
Nursing |
Phenomenological analysis, Colaizzi |
Nurse prescribing in China is in its infancy. |
|
12 |
Zhong, M. et al. (2020) |
Guangdong |
To understand nurses’ belief in and attitudes towards nurse’s prescription right so as to provide a reference for medical decision makers to formulate relevant policies and expand the scope of nursing service |
Quantitative |
Nursing |
Scale of nurses’ attitudes and belief towards nurse prescribing |
Nurses have positive attitudes and beliefs in nurse’s prescription. A minimum of 10 years’ clinical work experience, a professional title of supervisor nurses and a bachelor’s degree are suggested as entry qualifications for the right |
|
13 |
Wang, Y. et al. (2020) |
Shanxi |
To discuss training in nurse prescribing under global context to provide evidence for domestic application |
Qualitative |
Nursing |
/ |
Standardised trainings to nurses with different education backgrounds are needed |
|
14 |
Wang, S. et al. (2020) |
Shandong |
Discuss the content of the prescription right of nurses and provide references for relevant decision-making |
Qualitative |
Nursing |
Delphi method |
Content table of medical and non-medical nurse prescribing: 27 nursing intervention prescriptions, 15 examination prescriptions, 21 medical device prescriptions and 35 drug prescriptions were identified. |
|
15 |
Wan, Z. & He, Y. (2020) |
Beijing |
To summarise the classification, development data and qualification of nurse prescribing at home and abroad |
Qualitative |
Nursing |
/ |
4 suggestions on nurse prescribing |
|
16 |
Feng, S. et al. (2020) |
Shandong |
To summarise practical exploration and theoretical research of nurse prescribing in China |
Qualitative |
Nursing |
/ |
Stresses both education curriculum and continuing training on prescribing for nurses |
|
17 |
Li, M. (2019) |
Guizhou |
To compare nurse prescribing at home and abroad: the US, Australia, England |
Qualitative |
Medicine |
/ |
Comparison on prescriber qualification, specialization, contents. |
|
18 |
Han, S. & Hou, Y. (2019) |
Shanxi |
Advantages, disadvantages, opportunities and threats of granting prescription rights to clinical nurses in China |
Qualitative |
Nursing |
SWOT analysis |
Construction of nurses team the development of specialist nurses and the training of highly educated personnel in China all should be strengthened |
|
19 |
Tian, Y. et al. (2019) |
Henan |
To investigate the status quo of clinical nurses’ cognition of nurse prescribing |
Quantitative |
Nursing |
/ |
262 nurses lack of knowledge on nurse prescribing while showing a strong will for it. |
|
20 |
Wang, M. et al. (2018) |
Anhui |
To explore attitudes of doctors and nurses towards nurses’ qualification of prescribing |
Quantitative |
Nursing |
/ |
1056 medical staff from 14 hospitals in Anhui |
|
21 |
Li, H. & Ding, P. (2018) |
Anhui |
Overview nurse prescribing under NLC context |
Qualitative |
Nursing |
/ |
NLC nurse prescribing overview and future suggestions |
|
22 |
Ma, D. & Ding, P. (2018) |
Anhui |
To identify the scope of authority on prescription right of nurses in Anhui |
Qualitative |
Nursing |
/ |
Zoom in on Anhui trail |
|
23 |
Cheng, Z. & Xia, H. (2017) |
Shanghai |
To review nurse prescribing in England, Canada, Australia and the US. |
Qualitative |
Nursing |
/ |
Provides details of prescriber qualification, content, format, extension of nurse prescribing, suggests regulations and trials on nurse prescribing in China |
|
24 |
Gong, S. et al. (2016) |
Jilin |
To review nurse prescribing in England, so to provide evidence for domestic application |
Qualitative |
Nursing |
/ |
Provides details of prescriber qualification, content, format, extension of nurse prescribing in England. Identifies 3 challenges of China. |
|
25 |
Wei, X. (2016) |
Gansu |
Explore certain prescriptions that meet nurse’s capability in China |
Qualitative |
Nursing |
/ |
Suggests certain prescriptions nurse should practice within extended prescribing. 11 prescriptions for extended prescribing |
|
26 |
Zhang, G. et al. (2012) |
Shanxi |
To gain opinions on baccalaureate curriculum for nurse prescribing from experts |
Qualitative |
Nursing |
Delphi method |
Provides evidence for baccalaureate curriculum in preparation of nurse prescribing. 3 categories, 11 subjects |
|
27 |
* Zhang, G. et al. (2012) |
Shanxi |
To study on qualification of nurse prescribing applicants |
Qualitative |
Nursing |
Delphi method |
Provides evidence on minimised qualification of nurse prescriber. Baseline of nurse prescribing applicants |
|
28 |
Han, S. & Li, X. (2011) |
Shanxi |
To probe into the promotion factors of nurse prescribing implementation in China |
Qualitative |
Nursing |
Delphi method |
Categorises and lists factors of nurse prescribing in China. 43 promoting factors of nurse prescribing |
Table 1. Summary of included studies
*NLC (Nurse-Led Clinics), Shanxi (山西省), ICN (International Council of Nurses), US (United States), UK (United Kingdom), SWOT (Strengths, Weaknesses, Opportunities, and Threats), AHP (Analytic Hierarchy Process)
The 28 (100%) articles were all in Chinese, published between 2010 and 2023, eleven papers (39.3%) were conducted in the Shanxi (山西) Province. Four (14.3%) studies are designed quantitative and 24 (85.7%) are qualitative. Two articles (7.1%) were conducted in the medicine or law disciplines, the rest 26 (92.9%) were conducted in nursing. Seven studies (25.0%) applied Delphi method and 2 (7.1%) applied SWOT analysis. The studies on nurse prescribing fall mostly into the reviews of nurse prescribing abroad. This research work provides evidence for the qualification of prescribing nurses, the prescription protocols and the challenges in nurse prescribing.
B. Development of Nurse Prescribing in China
Nurse prescribing as well as nurse-led clinic nursing are being practiced since 1996 in Hong Kong (Parker & Hill, 2017; Wong & Chung, 2006). As for the mainland, the realization of nurse prescribing started in 2005 (Han et al., 2022). Research teams formed in 2005 and started research on decision-making in the patient classification system among nurses (Han et al., 2022). In 2007, a research team proposed that nurses should be the decision maker of nursing care, and divided nursing interventions into 16 independent and 11 integrated categories for decision making (Han et al., 2022). In 2020, a list of nurse prescriptions was provided (Wang et al., 2022), it consists of 27 prescriptions for nursing interventions, 15 for tests and examinations, 21 for medical aids and instruments, and 35 for medicine.
For medicine nurse prescribing, starting in 2008, researchers have looked into the contents and forms of prescribing (Han et al., 2022). They identified the contents in 7 acute and 4 chronic illnesses, modified the qualification of prescribing nurses (Han et al., 2022). They also provided a list of nurse prescriptions with 348 medicines and proposed a four-level prescribing model: independent prescribing, supplementary prescribing, extended prescribing, and adjusted prescribing (Han et al., 2022).
As for the qualification of prescribers, prescribing nurses should be those who work at third level hospitals, have bachelor’s degrees in nursing, and have 5 years of clinical work experience after obtaining the intermediate profession rank (Zhang et al., 2012). Researchers also proposed to add courses in nursing education to prepare nurses to prescribe, such as laws and regulations, nursing intervention, dosage calculation and substance abuse (Han et al., 2022).
In July 2017, Anhui Province initiated a trial as the landing of nurse prescribing in China. By the end of 2017, Anhui arranged 78 specialty nurses into 22 community health centers, opened 7 nurse-led clinics, and authorised these nurses limited prescribing (Ma & Ding, 2018). Guangdong Province is known as the first region opened traditional Chinese medicine NLCs in 2006. In 2022, the Shenzhen City of Guangdong Province authorises specialty nurses with the examination, treatment, and external medicine prescribing (Shenzhen Municipal People’s Congress, 2022). A survey conducted in Guangdong indicates 88.54% of the NLC nurses practice independent nurse prescribing (Chen & Peng, 2023).

Figure 2. Nurse Prescribing Timeline in China
*The left presents events in policy and practice, right in education and research.
C. Present Nurse Prescribing in China
Nurses have shown their positive intention in nurse prescribing in several research. A sample of nurses responded with an intermediate to a positive level of faith and attitude toward nurse prescribing (Zhong et al., 2020). The same study also emphasises that higher professional ranking and longer clinical experience led to a stronger intention and faith in nurse prescribing.
In the Anhui trial, the nurse prescribing is limited to non-medicine prescription for hypertension, diabetes, stroke, wound stoma, mental illness, gestational diabetes, and childbirth (Ma & Ding, 2018). Prescribers are limited to a group of nurses who have over 15 years of clinical experience, had received specialty nurse training with certificates, and have advanced communication skills (Ma & Ding, 2018). Prescribers make decisions and provide interventions on dressing changes, general physical examination, health education and consultation, test result and report reading, history taking, and physical or mental examination in chronic diseases (Ma & Ding, 2018).
In Guangdong Province, the NLC nurse prescribing includes medicine, tests and treatments, medical aids and devices, home medical devices, dressings, therapeutic diet prescriptions, and health education (Chen & Peng, 2023). Nurses prescribe several external medicines and limited injected medicines (normal saline solution, heparin injection, peritoneal fluid, etc.) (Chen & Peng, 2023).
In the Shenzhen legislation, specialty nurses are regulated to be the only qualified prescribing nurses, specifically those who have a baccalaureate degree or above in nursing, more than five years of clinical experience and more than two years in relevant specialised departments, meanwhile having intermediate profession ranks or above (Shenzhen Municipal People’s Congress, 2022).
More than half of the 34 provinces run nurse-led clinics and about 70% of nurses at these clinics report independent nursing practice (Gao et al., 2017). Currently, about half of the total 34 regions are recognised in the research or preparation phase for the implementation of nurse prescribing on medicine (Figure 3). Trials and legislative move are seen to take place in regions with intermediate research activity.

Figure 3. Nurse Prescribing Region Mapping of China in 2023
D. Indicated Challenges
Despite the positive intentions, nurses and nursing students lack knowledge of nurse prescribing and lack confidence in it (Hou, 2021; Tian et al., 2019). A percentage 60.7 of registered nurses reported it necessary for nurses to have prescriptive authorization and 58% are willing to have it, but about half, 49.2% of the nurses have not heard about nurse prescribing by the time they were surveyed (Tian et al., 2019). A qualitative study indicates all participated specialty nurses advocated for nurse prescribing (Hou, 2021). Less than 35% of medical and nursing students had heard of nurse prescribing, and less than 5% had heard of the Anhui trial (Tian et al., 2019).
The current nursing education level is a major concern in nurse prescribing (Feng et al., 2020; Y. P. Wang et al., 2020; Zhang et al., 2012). In China, as of 2020 and 2021, respectively, 71.2% and 69.5% of the nurses had credentials below baccalaureate, 28.7% and 30.1% had a baccalaureate degree, 0.2% and 0.3% had a master’s or a higher credential (National Health Commission of the People’s Republic of China, 2022).
For the education curriculum, researchers suggest multi-level prescribing training due to the diversity of current nursing education levels. Researches focus on curriculum design for baccalaureate nursing education (Zhang et al., 2012) or the design for specialty nurse training (Wang et al., 2022), most suggest including pharmacology and related legislation (Zhang et al., 2012).
For the nurse prescribing training, an education program is recommended to reach a performance set standard for the nurse seeking prescriptive authority (International Council of Nurses, 2021). A prescribing-specific training is suggested in some studies (Wang et al., 2021; Wang et al., 2022), most of these studies take the training system of the United Kingdom (UK) as their reference.
The current qualification system for prescribing nurses has been identified as problematic in several studies (Gong et al., 2016; Xing et al., 2022; Zhong et al., 2020). Some studies suggest a combination of a master’s degree and the highest professional rank (Cheng & Xia, 2017). Some suggest specialty nurses (Cheng & Xia, 2017) practice prescribing in their specialties. Some others suggest a baccalaureate degree and 5 years of clinical experience with intermediate profession rank (Wang et al., 2018; Zhang et al., 2012).
The present nurse prescribing implementation is limited within the extended category (Wang et al., 2021) due to the lack of organizational preparation (Han et al., 2022; Hou, 2021). These organizational conditions include the current nursing education level, the lack of systematic qualification of prescribers (Zhang et al., 2012), the clear scope of nursing practice (Fan et al., 2022; Wei, 2016), guidelines and protocols (Han et al., 2021), and solutions on extension and geographic expansion (Wang et al., 2021).
Under the limited pilot practice and the absence of national legislation, current nurse prescribing in China requires both expansion and extension. This session summarised the implementation of nurse prescribing and analysed the indicated challenges. The improvement of nurses’ knowledge of prescribing, the current nursing education level, and the training and qualification of prescribing nurses are indicated as the priorities.
IV. DISCUSSION
Previous studies on nurse prescribing have primarily focused on developed countries, however, it is worth noting that developing countries have shown a slightly higher rate of nurse prescribing authorization, with 38% compared to 31% in developed countries (International Council of Nurses, 2021). This study reviewed the development and implementation of nurse prescribing and identified the challenges China is facing to further practice nursing prescribing.
Unlike other countries that initiated nurse prescribing decades ago, in China, the exploration of nurse prescribing appeared late. Nurse prescribing related regulations can be traced to the 2006 Prescription Administrative Policy, the Article 2 indicates that physicians are the only prescribers of medicine in China. The Nursing Regulation indicates nurses are obliged to implement necessary first aid in emergencies and remain critical on instructions of doctors according to Article 17.
On June 23, 2022, the Municipal People’s Congress of Shenzhen passed the Medical Regulation of Shenzhen Special Economic Zone that came into force on January 1, 2023. This is the first legislation in China that grants prescriptive authority for nurses according to Article 65. It also provides a general qualification guide of specialty nurses, clarified in Article 64.
For the implementation, nurses and nursing students show limited knowledge and confidence in nurse prescribing. This is seen caused by the current nursing education level and the content of the education curriculum. For nursing education level, referring to the nursing education level in the United States, 2016 is reported as the year when all the states in the US practice nurse prescribing. In 2015, an estimated 65% of nurses had obtained a baccalaureate or higher degree (National Council of State Boards of Nursing, 2016). In 2017, the number of RNs with a master’s degree in nursing has increased to 17.1% and 1.1% had a Doctorate in Nursing Practice, 10.0% held an APRN credential (National Council of State Boards of Nursing, 2018).
As for the training of prescribing nurses, the UK applies prescribing-specific training. The training follows a structured framework governed by regulatory bodies such as the Nursing and Midwifery Council (NMC) and involves a combination of theoretical and practical components (Courtenay et al., 2007). The training program typically consists of two parts: the academic component and the clinical component (Nursing and Midwifery Council, 2018).
For qualification of prescribing nurses, thirty-one of the 44 countries authorise nurse prescribing at post-basic levels, to nurses who have completed their basic nursing education; 13 countries at advanced practice levels; 11 countries allow nurses to prescribe at both the post-basic and advanced practice levels (International Council of Nurses, 2021). In the United States by 2016, all 50 states and the District of Columbia authorise certain levels of independent prescribing to APNs (American Nurses Association, 2018). Canada has a broad advanced practice level prescriptive authority for NPs federally and in recent years at a post-basic level for RNs provincially in Alberta and Ontario (Canadian Nurses Association, 2015). In Europe, prescribing by nurses has been recognised legally in 15 countries at a post-basic level (Gielen et al., 2014).
In the UK, the NMC outlines the requirements and standards that nurses must meet to become qualified prescribers. Upon successful completion of an NMC-approved prescribing course delivered by a recognised educational institution, nurses are eligible to apply for the relevant prescribing qualification from the NMC (Nursing and Midwifery Council, 2018). These qualifications determine the scope of prescribing authority for nurses, specifying the range of medications they can prescribe and any limitations or restrictions.
In China, specialty nurses are recognised as prescribing nurses in the Shenzhen legislation. Although prerequisite 2 years of clinical experience, 2 to 3 months training period is seen in most specialty nurse training programs, current evidence shows there is no modified training, qualification, or scope of practice for specialty nurses at a national level (Han & Hou, 2019; Han & Li, 2011).
The confusion in specialty nursing and advanced practice nursing is seen in former studies. The specialty nurse system should be well differentiated from the advanced practice nurse system in China. In a long-term stance either form a linked structure to umbrella both specialty nurses and APNs as equal prescribing nurses or assign respective categories of prescriptive authorities to each group. As a result, the qualifications of prescribing nurses can be modified at a national level.
Evidence on the outcome and evaluation of the current trial practice and the region-specific analysis were rare. The possibility and plan for the expansion of nurse prescribing over the country were not observed in former research. Despite expansion, the extension to other levels of nurse prescribing is needed. In the US, some states allow advanced practice registered nurses (APRNs) to practice independently (independent), some others require APRNs to work within a collaborative agreement with a physician (supplementary), 16 states allow RNs to dispense some medications (protocol) including contraceptives and drugs for sexually transmitted infection care in outpatient settings, such as a health department or a family planning clinic (Guttmacher Institute, 2023).
A. Limitation & Implication
Despite the scarcity of research on nurse prescribing in China and the lack of recent studies addressing the latest updates, this study overviewed nurse prescribing in China through a review of the development, the implementation, and the challenges, provides insights with global relevance. As healthcare systems worldwide face increasing demands and evolving roles for healthcare professionals, understanding diverse implementations of nurse prescribing offers crucial comparative perspectives. This article not only provides evidence on how nurse prescribing is integrated within China’s unique healthcare landscape but also serves as a benchmark for evaluating similar practices across different countries. For researchers and policymakers, these findings contribute to a broader understanding of effective healthcare strategies, policy development, and the global advancement of nursing roles.
As for the limitation, bias might exist in the screening and analysis process as they were conducted by two reviewers. In China, the community healthcare setting is regulated as one of the nurse prescribing settings in the Shenzhen legislation. More investigation on nurse prescribing in community settings seems necessary.
V. CONCLUSION
This systematic review followed the PRISMA 2020 Statement, analysed 28 articles. The 28 articles were assessed by the MMAT 2018 for synthesis. Both a time and a region mapping of nurse prescribing in China were conducted. This study provides an overview of the implementation and challenges of nurse prescribing in China.
Along with the development of specialty nursing, more than half of the province-level regions run hospital-based nurse-led clinics and about 70% of the nurses at these clinics practice independently. As for nurse prescribing, post a long research and preparation period, Anhui Province started a trial in July 2017 and practices non-medicine prescriptions for certain diseases and conditions. In June 2022, the Congress of Shenzhen City passed a medical regulation authorises specialty nurses with examination, treatment, and external medicine such as ointment and dressing prescribing, as the first legislative move in China. About half of the total 34 regions are in research or preparation phase for the implementation of medicine nurse prescribing.
The lack of knowledge and confidence related to nurse prescribing among nurses and nursing students, the current nursing education level and curriculum, and the training and qualification of prescribing nurses are recognised as the major concerns of nurse prescribing in China. Limited research, pilot practice, and legislative move of nurse prescribing are observed.
To meet the growing need for nurse prescribing in China, the following tasks are identified. First, improvement in nursing education level and curriculum is necessary. Second, a systematic qualification system for prescribing nurses should be established based on the clarification of specialty nurses and advanced practice nurses. Third, the scope of nursing practice consists of prescribing and the protocols for prescribing are in need. Fourth, the geographic expansion of legislation and pilot project are expected to reach nurse prescribing implementation at a national level. Last, future research should focus on nurse prescribing in community healthcare settings.
Notes on Contributors
CL performed the literature search and analysis, wrote the original manuscript, prepared the figures and tables, and worked on the review and editing. GJL supervised the conceptualisation and the methodology, provided suggestions on the validation and visualization.
Ethical Approval
As this study is a systematic review, ethical approval and IRB application was not applicable.
Data Availability
Data set that support the findings of this study are openly available in Figshare repository https://doi.org/10.6084/m9.figshare.25310869
Funding
No funding sources are associated with this study.
Declaration of Interest
No conflicts of interest are associated with this paper.
References
Abuzour, A. S., Lewis, P. J., & Tully, M. P. (2018). Practice makes perfect: A systematic review of the expertise development of pharmacist and nurse independent prescribers in the United Kingdom. Research in Social and Administrative Pharmacy, 14(1), 6-17. https://doi.org/10.1016/j.sapharm.2017.02.002
American Nurses Association. (2018). Nursing scope of practice. https://www.nursingworld.org/practice-policy/scope-of-practice/
Canadian Nurses Association. (2015). Framework for Registered Nurse Prescribing in Canada. https://www.cna-aiic.ca/en/nursing/ regulated-nursing-in-canada/rn-prescribing-framework
Chen, L. H., & Peng, G. Y. (2023). Investigation research on nursing outpatient clinics and prescriptive authority for nurses in Guangdong province. Nursing Research, 37(8), 1443-1448. https://doi.org/10.12102/j.issn.1009-6493.2023.08.024
Cheng, Z. H., & Xia, H. O. (2017). Implementation of nurse prescribing rights abroad and its implications for China. Chinese Journal of Nursing, 06, 764-767. http://zh.zhhlzzs.com/CN/Y2017/V52/I6/764
Courtenay, M., Carey, N., & Burke, J. (2007). Independent extended and supplementary nurse prescribing practice in the UK: A national questionnaire survey. International Journal of Nursing Studies, 44(7), 1093-1101. https://doi.org/10.1016/j.ijnurstu. 2006.04.005
Dong, Z., Wei, L., Sun, X., Xiang, J., Hu, Y., Lin, M., & Tan, Y. (2022). Experiences of nurses working in nurse-led clinics in traditional chinese medicine hospitals: A focused ethnographic study. Nursing Open, 10(2), 603-612. https://doi.org/10.1002/nop2.1326
Fan, Y. L., Zhang, Y., Cheng, Q. Y., Zhu, M. Y., Guo, Y. P., Zhao, S. B., & Geng, X. (2022). Management of prescription right of nurses internationally and its application to the practice. Chinese Journal of Nursing Education, 19(02), 187-192. https://doi.org/10.3761/j.issn.1672-9234.2022.02.017
Feng, S. T., Li, X. Z., Li, L., & Zhao, Y. L. (2020). Research progress and advices on nurse prescribing right in China. Chinese Nursing Research, 1, 101-104. https://qikan.cqvip.com/Qikan/Article/Detail?id=7100822761
Gao, F. L., Ding, S., & Huang, J., Dong, L., Wang, S. Q., Lv, Y., Duan, J. M., Li, T. T., Zhang, L. X., & Liu, J. E. (2017). The establishment and advanced nursing practice status of Nurse-Led Clinics in tertiary hospitals in China: findings from a national survey. Chinese Journal of Nursing Management, 17(10), 1297-1302.
Gielen, S. C., Dekker, J., Francke, A. L., Mistiaen, P., & Kroezen, M. (2014). The effects of nurse prescribing: A systematic review. International Journal of Nursing Studies, 51(7), 1048-1061. https://doi.org/10.1016/j.ijnurstu.2013.12.003
Gong, S. S., Lv, J., Wang, S. Y., & Wang, X. (2016). Development of nurse prescribing rights abroad and implementation of nurse prescribing rights in China. Journal of Nursing Continuing Education, 20, 1848-1851. https://doi.org/10.16821/j.cnki.hsjx.2016.20.008
Han, S. F., Duan, Z. G., Han, Q. H., Xue, P., Cheng, J. L., Wang, Y. Q., Zhu, R., Cao, Y., Zhang, Q., Wang, Y., Gao, J., Wang, X., Fan, J., Xue, N., Li, J., Li, X., Han, H., Yang, Y., Zhang, G., … Li, R.(2021). Expert consensus on the scope of nurse prescribing rights for advanced practice nurses in the new era (continuation). Nursing Research, 35(24), 4325-4342. https://doi.org/10.12102/j.issn.1009-6493.2021.24.001
Han, S. F., & Hou, Y. C. (2019). SWOT analysis of granting nurse prescribing rights in China. General Practice Nursing, 17(21), 2574-2578.
Han, S. F., & Li, X. (2011). Application of Delphi method to study the promoting factors of nurse prescribing rights implementation. General Practice Nursing, 19, 1693-1695. https://cqvip.com/doc/journal/967995293
Han, S. F., Zhang, Q., Zhu, R. F., & Cao, Y. (2022). From the decision-making subject of hierarchical nursing to the legislation of nurses’ prescribing authority: A research report. Nursing Research, 36(16), 2821-2826.
Hatchett, R. (2003). The emergence of the modern nurse-led clinic. In R. Hatchett (Ed.), Nurse-led clinics: Practice issues (pp. 1–27). Routledge.
Hong, Q. N., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., Dagenais, P., Gagnon, M., Griffiths, F., Nicolau, B., O’Cathain, A., Rousseau, M., Vedel, I., & Pluye, P. (2018). The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Education for Information, 34(4), 285-291. https://doi.org/10.3233/efi-180221
Hou, X. L. (2021). A qualitative study on the cognition and influence of specialist nurses on the prescription right of Chinese nurses. China Academic Journal Electronic Publishing House, 36(7), 655-659. https://doi.org/10.16821/j.cnki.hsjx.2021.07.019
International Council of Nurses. (2021). Guidelines on prescriptive authority for nurses. https://www.icn.ch/sites/default/files/inline-files/PR_45_%20Nurse%20Prescribing_V1_FINAL.pdf
Kilańska, D., Lipert, A., Guzek, M., Engelseth, P., Marczak, M., Sienkiewicz, K., & Kozłowski, R. (2022). Increased accessibility to primary healthcare due to nurse prescribing of medicines. International Journal of Environmental Research and Public Health, 19(1), 292. https://doi.org/10.3390/ijerph19010292
Ling, D. L., Lyu, C. M., Liu, H., Xiao, X., & Yu, H. J. (2018). The necessity and possibility of implementation of nurse prescribing in China: An international perspective. International Journal of Nursing Sciences, 5(1), 72-80. https://doi.org/10.1016/j.ijnss.2017.12.011
Ma, D. H., & Ding, P. (2018). Practical study on scope of authority on prescription right of nurses in Anhui Province. Chinese Nursing Research, 32(1), 6-12. https://doi.org/10.3969/j.issn.1009-6493.2018.01.002
Maier, C. B. (2019). Nurse prescribing of medicines in 13 European countries. Human Resources for Health, 17(95). https://doi.org/10.1186/s12960-019-0429-6
McMenamin, A., Turi, E., Schlak, A., & Poghosyan, L. (2023). A systematic review of outcomes related to nurse practitioner-delivered primary care for multiple chronic conditions. Medical care research and review: MCRR, 80(6), 563–581. https://doi.org/10.1177/10775587231186720
National Health Commission of the People’s Republic of China. (2022). China health statistics yearbook.
Nissen, L., Kyle, G., Stowasser, D., Lum, E., Jones, A., McLean, C., & Gear, C. (2010). Non-medical prescribing: An exploration of likely nature of, and contingencies for, developing a nationally consistent approach to prescribing by non-medical health professionals-Final Report 1 June 2010. https://eprints.qut.edu.au/204992/1/Non_Medical_Prescribing.pdf
Nursing and Midwifery Council. (2018). Part 3: Standards for prescribing programmes – Nursing and midwifery. Retrieved June 12, 2023, from https://www.nmc.org.uk/globalassets/sitedocuments/education-standards/programme-standards-prescribing.pdf
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., . . . Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
Parker, J. M., & Hill, M. N. (2017). A review of advanced practice nursing in the United States, Canada, Australia and Hong Kong Special Administrative Region (SAR), China. International Journal of Nursing Sciences, 4(2), 196-204. https://doi.org/10.1016/j.ijnss.2017.01.002
Shenzhen Municipal People’s Congress. (2022). Shenzhen Special Economic Zone Medical Regulations. Retrieved from https://www.gd.gov.cn/zwgk/wjk/zcfgk/content/post_2532140.html
National Council of State Boards of Nursing. (2016). The 2015 National Nursing Workforce Survey. Retrieved from https://doi.org/10.1016/S2155-8256(16)31055-9
National Council of State Boards of Nursing. (2018). The 2017 National Nursing Workforce Survey. Retrieved from https://doi.org/10.1016/S2155-8256(18)30131-5
Tian, Y. T., Zhang, Y., Yu, Z. J., Wang, R. H., Zhao, J., Li, H. J., Du, C. C., & Liu, Z. (2019). Survey on nurses’ cognition on prescription right in tertiary hospitals. Chinese Nursing Research, 33(10), 1649-1653. https://doi.org/10.12102/j.issn.1009-6493.2019.10.003
Wang, D., Bo, Y. M., Zhu, J., & Zhong, Q. (2018). Bibliometrics analysis of core competence related literatures of specialist nurses in China. Nursing Research, 32(19), 3107-3110. https://doi.org/10.3969/j.issn.1009-6493.2018.19.030
Wang, L., Kan, K., Shi, Y., & Shi, L. (2021). On legislation on nurse prescribing in China. Journal of Nursing Science, 12, 66-69. http://www.hlxzz.com.cn/hlxzz/article/abstract/20211219
Wang, S. Y., Jiang, W. B., Chen, K., Chen, Q. Q., & Wie, L. L. (2020). Research on the content of the prescription right of nurses based on Delphi method. China Health Standard Management, 11(11), 165-168.https://mqikan.cqvip.com/Article/ArticleDetail?id=7102148196&from=Article_index
Wang, X. J., Han, S. F., Cao, Y., Zhang, Q., & Zhu, R. F. (2022). Construction of general clinical practice training program for drug prescribing applicants of nurses in China. Chinese Nursing Research, 36(23), 4164-4173. https://doi.org/10.12102/j.issn.1009-6493.2022.23.006
Wang, X. J., Han, S. F., Zhang, Q., Zhu, R. F., Wang, Y. P., & Cao, Y. (2021). Current status and implications of clinical practice training for nurse prescribing rights at home and abroad. Nursing Research, 10, 1785-1788. https://doi.org/10.12102/j.issn.10096493.2021.10.016
Wang, Y. P., Han, S. F., Zhu, R. F., Cao, Y., Meng, Y. F., Xu, Z. Y., & Gao, J. P. (2020). Development and enlightenment of education and training of international nurses′ prescription rights. Chinese General Practice Nursing, 18(17), 2069-2073. https://doi.org/10.12104/j.issn.1674-4748.2020.17.005
Wei, X. (2016). Acquisition and content of nurse prescribing rights under specific conditions for clinical nurses. Electronic Journal of Clinical Medical Literature, 40, 8078-8080. https://doi.org/10.16281/j.cnki.jocml.2016.40.132
Wong, F. K. Y., & Chung, L. C. Y. (2006). Establishing a definition for a nurse-led clinic: Structure, process, and outcome. Journal of Advanced Nursing, 53(3), 358-369. https://doi.org/10.1111/j.1365-2648.2006.03730.x
Wong, F. K. Y. (2018). Development of advanced nursing practice in China: Act local and think global. International Journal of Nursing Sciences, 5(2), 101-104. https://doi.org/10.1016/j.ijnss.2018.03.003
Wu, X. J. (2022). Promoting nursing development towards health for all: Overview and prospect of nursing development in China. International Journal of Nursing Sciences, 10(1), 1-4.https://doi.org/10.1016/j.ijnss.2022.12.011
Zhang, G. Z., Han, S. F., & Cheng, J. L., & Wang, Y. J. (2012). Study on expert demonstration for qualification of applicants of nurse prescription right. Chinese Nursing Research, 26(15), 1360-1362.
Zhang, Q., Li, M. Z., Han, S. F., Li, X. P., Zhu, R. F., Wang, X. J., & Zhang, Y. X. (2022). Interpretation of the 2021 International Council of Nurses’ Nurse Prescribing Rights Guidelines. Nursing Research, 16, 2827-2835. https://doi.org/10.12102/j.issn.1009-6493.2022.16.002
Zhong, M. Y., Ling, D. L., Yu, H. J., & Li, W. T. (2020). A survey on nurses’ attitudes towards and belief in nurse’s prescription right. Modern Clinical Nursing, 19(9), 19-25. https://doi.org/10.3969/j.issn.1671-8283.2020.09.004
*Gunjeong Lee
School of Nursing, Ewha Womans University
52, Ewhayeodae-gil, Seodaemun-gu,
Seoul 03760 Republic of Korea
Email: gunjeong@ewha.ac.kr
Submitted: 6 June 2024
Accepted: 3 September 2024
Published online: 7 January, TAPS 2025, 10(1), 10-16
https://doi.org/10.29060/TAPS.2025-10-1/RA3430
Han Ting Jillian Yeo, Dujeepa D. Samarasekera & Shuh Shing Lee
Centre for Medical Education (CenMED), Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Despite significant efforts to address gender equality in medical education, the issue persists. The narrative review aimed to address the research question: What are the strategies implemented to address issues of gender inequality in medical education and what were their outcomes?
Methods: Seven major electronic databases of CINAHL, Embase, ERIC, PsyInfo, PubMed, SCOPUS and Web of Science were reviewed. Search phrases used were (Medical education) AND (Gender equality) OR (Gender bias) OR (Gender diversity) OR (Gender discrimination). Original research articles were included, together with systematic reviews with outcomes reporting on strategies to address gender equality.
Results: Articles unrelated to medical education (e.g. allied health and nursing education) and non-English articles were excluded from the study. A total of 1248 articles were identified, and 23 articles met the inclusion criteria. Training programs (n=14; 60.8%) for medical students and faculty have successfully increased awareness on the issues of gender equality and boost confidence in handling cases on gender inequality, yet implicit bias remains with leadership continuing to be associated more strongly with males.
Conclusion: Leadership bodies in Institutions of Higher Education and policymakers would be in an ideal position to address these issues through shaping policies and provision of training for hiring bodies and faculty.
Keywords: Medical Education, Gender Equality, Strategies
Practice Highlights
- Training programs for medical students and faculty can increase awareness of gender equality.
- Structural and cultural barriers preventing women from attaining leadership roles remain entrenched.
- Targeted training for hiring committees and faculty can help mitigate implicit biases.
I. INTRODUCTION
There has been significant progress in the landscape of medical education since 2000 as women’s representation in health professions has increased steadily across the globe. In 2019, nearly half of all doctors in countries in the Organisation for Economic Co-operation and Development were women (Organisation for Economic Co-operation and Development, 2022). However, beneath the surface of this endeavor lies a persistent and pervasive issue concerning gender equality. The World Health Organisation (WHO) (2007) defines gender equality as the absence of discrimination in the allocation of benefits or resources, access to services, or the provision of opportunities based on a person’s sex, thereby enabling individuals to achieve their full potential. Efforts have been made towards achieving gender equality and inclusivity. Changes in the recruitment processes of residency programs in the United States and Canada have shown an increasing ratio of females among residents and faculty (Jain et al., 2022; Ying et al., 2023). Studies evaluating the assessments of medical students and residents have suggested reduced biases in scorings of examinees based on gender (Hannon et al., 2021; Jacques et al., 2016).
Yet, gender inequality remains prevalent in other aspects of medical education. Sexual harassment in the form of sexist behavior or comments were commonly reported among females in the workplace during residency trainings (DeWane et al., 2020; Ellis et al., 2019; Jackson & Drolet, 2021). Learning opportunities were unequal as female residents performed disproportionately lesser number of procedures (Olson et al., 2023; Sobel et al., 2023) and were given less operative autonomy as compared to their male counterparts hence affecting their preparedness for practice (Joh et al., 2020; Meyerson et al., 2019). The impact of gender inequality is far-reaching. Negative emotions, such as helplessness, and lowered self-esteem, were often described by students or residents who had experienced or observed gender inequality (Kristoffersson et al., 2016; Madeeh Hashmi et al., 2013). Additionally, lowered job satisfaction, feelings of burnout and an increased risk of attrition were reported among those who have experienced or observed gender inequality (Bruce et al., 2015; Ellis et al., 2019; Jackson & Drolet, 2021).
Achieving gender equality in medical education is critical, however, literature highlighted that it continues to persist despite various interventions. Numerous studies have documented progress in gender equality following the implementation of specific interventions, but there is a scarcity of comprehensive reviews consolidating these efforts. Hence, this narrative review aimed to address the research question: What are the strategies implemented to address issues of gender inequality in medical education and what were their outcomes?
II. METHODS
A narrative review was conducted based on the framework proposed by Ferrari (2015). Two researchers (SSL and JYHT) searched seven major electronic databases of CINAHL, Embase, ERIC, PsyInfo, PubMed, SCOPUS and Web of Science for the English-language articles or articles which were translated to English and published between 2013 to 2023. The search terms were broadened using the Boolean operator (“OR/AND”) to search the ‘medical’ subject heading (MeSH) to recognise the significance of the study. As a result, the search phrases were (Medical education) AND (Gender equality) OR (Gender bias) OR (Gender diversity) OR (Gender discrimination).
Original research articles were included into the study, together with systematic reviews with outcomes reporting on strategies to address gender equality. Articles unrelated to medical education (e.g. allied health and nursing education) and non-English articles were excluded from the study. Figure 1 showed a flow chart of the process of literature selection for the narrative review.
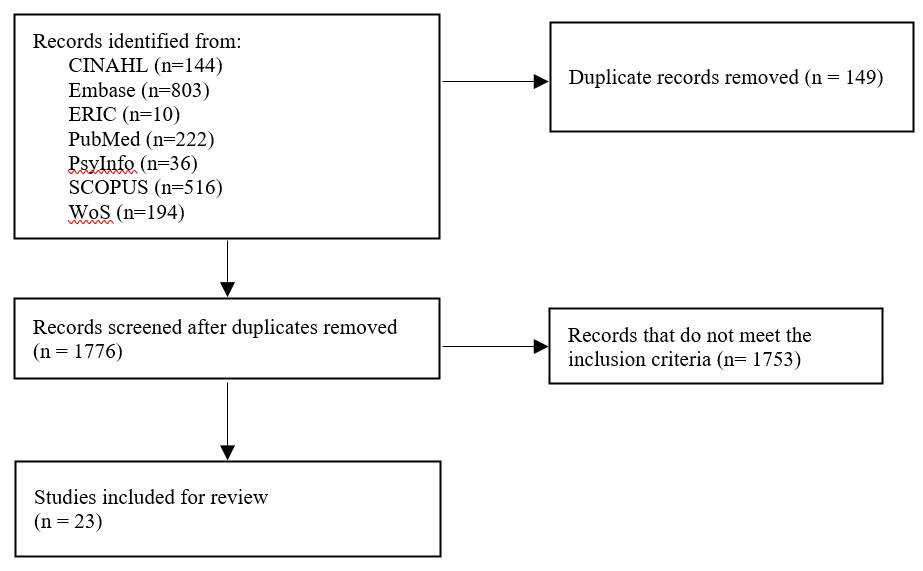
Figure 1. Flow diagram showing the selection of articles
Based on the inclusion and exclusion criteria outlined, both researchers (SSL and JYHT) independently reviewed the title and abstracts of all articles and reviewed the full article when necessary. Articles were categorised based on the types of strategies that were implemented, target audient, method of evaluation and evaluation findings.
III. RESULTS
After removing duplicate articles, a total of 1248 articles were identified through the literature search strategy. Following a thorough examination of the titles and abstracts as well as a review of the articles’ references lists, 23 articles met the review criteria (Table 1). Articles were published between 2015 to 2022. Majority of studies were conducted in the United States (n=16), Canada (n=1), United States and Canada (n=1), Germany (n=1), Sweden (n=1), Switzerland (n=1), Taiwan (n=1), and United Kingdom (n=1).
The findings from this narrative review were divided into two sections: (1) an overview of the interventions implemented to address gender equality and (2) an evaluation of the interventions implemented.
A. Interventions Implemented to Address Gender Equality
Interventions implemented could be divided into micro, meso and macro levels interventions to address gender equality. Micro levels interventions focused on supporting individuals in understanding concepts on gender bias and diversity, its impact on the workplace and strategies to overcome gender bias. These aims could be achieved through training programs for faculty and medical students (n=14; 60.8%). Other micro level interventions described in the articles included giving doctors labelled badges and empowering residents to nominate their chief resident (Olson et al., 2022).
Meso level interventions focused on improving the institutions’ systems, structures, and procedures. Two articles described the formation of task forces in medical societies and higher education institutions (HEIs) to monitor trends and address gender issues (Kandi et al., 2022; Lieberman et al., 2018). Holding a public symposium as a platform to discuss issues on gender equality and enforcing guidelines on writing letter recommendations for medical residency applications were other meso level interventions (Sakowski et al., 2020; Zhang et al., 2021).
Macro level interventions involved shaping policies on a broader, national, or international scale. One study by Chang et al. (2020) shared on three national career developments program aimed at increasing women faculty professional effectiveness. Another macro level intervention involved awarding institutions with Bronze, Silver, and Gold for efforts in addressing gender equity (Caffrey et al., 2016).
The target audience for most interventions were medical students (n=7), these included interventions tailored for women medical students. Other main target audiences included faculty (n=4), residents (n=3) and HEIs (n=2).
B. Addressing Gender Inequality through Training Programs
The duration of the 15 training programmes specified spanned from 15 minutes to 15 weeks long. Seven training programs targeted medical students, 4 training programs targeted faculty, 2 training programs targeted internal medical residents.
Training programs primarily focused on creating an awareness of gender inequality in the workplace through defining terminologies surrounding gender inequality, showing data on gender inequality and its impact on the workplace (Carnes et al., 2015; Driscoll et al., 2019; Farkas et al., 2022; Girod et al., 2016; Jacobs et al., 2022; Kisiel et al., 2020; Lattanza et al., 2016; Sabin et al., 2022). Five programs shared strategies and frameworks to handle situations insinuating gender inequality in the workplace and provided opportunities for practice (Bromberg et al., 2022; Carnes et al., 2015; Farkas et al., 2022; Jacobs et al., 2022; Sabin et al., 2022). Five training programs incorporated elements to guide participants on their career progression through networking opportunities, mentorship programs and leadership training (Chang et al., 2020; Deng et al., 2021; Gaida et al., 2020; Harbold et al., 2021; Lattanza et al., 2016). Training programs developed as part of the Perry’s Initiative for women medical students provided hands-on opportunities to engage in operative procedures to encourage more females to enter the field of orthopaedic surgery (Harbold et al., 2021; Lattanza et al., 2016). Two training programs adopted the approach of engaging in reflexivity with a gendered perspective into one’s own practice and literature materials (Geiser et al., 2022; Liao & Wang, 2020).
C. Evaluation and Findings on the Strategies Implemented
The Kirkpatrick model was adopted to categorise how evaluation of interventions was conducted and the findings.
1) Kirkpatrick Level 1 – Reaction: Participants’ reactions were evaluated for the following strategies: workshops, public symposium, recognition of efforts and empowerment to nominate chief residents (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). Participant satisfaction surveys were the main tool adopted to determine if participants found the strategies useful and identify areas for improvement (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). One qualitative study by Caffrey et al. (2016) used semi-structured interviews. In general, the interventions were perceived positively in all articles (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). However, one study by Caffrey et al. (2016) focusing on recognising institutions which promote gender equity had reported a higher and disproportionate workload on women who were involved in the application process.
2) Kirkpatrick Level 2 – Learning: Participants in 6 studies reported an increased awareness of gender bias after workshops were conducted (Caffrey et al., 2016; Carnes et al., 2015; Deng et al., 2021; Girod et al., 2016; Liao & Wang, 2020; Sabin et al., 2022). Awareness of gender bias can be described in different facets: (1) having an understanding that society has yet to provide equal opportunities for all regardless of their backgrounds; and (2) gaining awareness on the presence of socially constructed gender norms. Two workshops had reported an increase in internal medicine residents’ confidence in responding to incidences related to gender inequality (Bromberg et al., 2022; Farkas et al., 2022).
While strategies had largely positive outcomes with regards to learning, Carnes et al. (2015) and Girod et al. (2016) revealed that workshops on gender bias led to no significant differences in gender/ leadership Implicit Association Test scores suggesting that there remains a persistent association of leadership with males more than females. Gaida, Kujumdshiev and Stengler (2020) shared that low numbers of medical students were able to identify gender sensitive topics despite a week-long elective course on issues of gender equality supported by a mentorship program.
3) Kirkpatrick Level 3 – Behaviour: Reviewed literature revealed conflicting findings on the impact of the interventions on participants’ behaviour. Interventions made to medical assessments (unconscious bias training of examiners, structured interview formats for interviewers and guidelines for writing letter of recommendations) observed no changes in scores and biased language used (Driscoll et al., 2019; Langhan et al., 2022; Zhang et al., 2021).While Olson et al. (2022) had shown a reduction in reported events on gender bias, Kisiel et al. (2020) reported an increase in sexual harassment and gender discrimination events attributing it to an increased awareness in such behaviours.
4) Kirkpatrick Level 4 – Results: Studies which evaluated the overall impact of the interventions on organizational structure showed optimistic results. Articles introducing the Perry’s Initiative to increase women medical students’ exposure to orthopaedic surgery and engineering reported an increased match rates of alumni students to orthopaedics (Harbold et al., 2021; Lattanza et al., 2016). Training of faculty search committee member yielded an increase in number of female candidates throughout the entire hiring process and eventually positions offered to them (Jacobs et al., 2022). Chang et al. (2020) also reported higher rates of promotion for women faculty who had participated in national career development programs.
IV. DISCUSSION
The review highlighted that training programs for students and faculty were not only positively received by students and faculty but were able to create awareness on gender inequality and boost confidence in handling cases on gender inequality. Yet faculty training programs failed to address the implicit bias among faculty who tend to associate leadership with male more than female. This was concurred by more recently published literature reporting that females hold fewer leadership positions in academia or residency programs and hence having potential implications on their career advancement opportunities (Dhingra et al., 2021; Sethi et al., 2022). Achieving gender equality in leadership body is important. The presence of female in any leadership position was correlated with an increase in the number of female faculty or female fellows (Sethi et al., 2022; Sulibhavi et al., 2021). One study also suggested that an increase in the number of female surgical faculty was correlated a decrease in attrition among residents (Saberi et al., 2021).
Macro and meso level interventions via implementation of career development programs and training of recruitment committee showed far reaching impacts on increasing diversity of hires and promotional rates of female faculty. This could serve as a guidance to the leadership bodies in HEIs that the engagement of targeted interventions on training hiring bodies and the provision of faculty development to women faculty can they level the playing field for both genders. Till date few studies reviewed the impact of macro level intervention, and perhaps by sharing the policies in place for training faculty and hiring bodies can the society see an exponential impact on addressing the issues of gender equality.
Lastly, it was evident from the review of selected literature that most research in the areas of gender quality was conducted in the Global North. Given that issues on gender equality tend to be contextual and cultural in nature, there would be a need for medical educators in the Global South to engage in scholarly work in this domain to identify the issues on the ground and identify targeted ways to address the issues on hand.
V. CONCLUSION
While training programs for medical students and faculty have successfully increased awareness of gender equality issues, implicit bias persists, particularly concerning female representation in leadership positions. Despite heightened awareness, the structural and cultural barriers preventing women from attaining leadership roles remain firmly entrenched. Leadership bodies within HEIs and policymakers are uniquely positioned to address these persistent issues. By shaping and implementing equitable policies, they can foster an environment that actively promotes gender diversity. Additionally, targeted training for hiring committees and faculty can help mitigate implicit biases, ensuring a more inclusive and representative leadership. Addressing these challenges requires a multifaceted approach, combining policy reform, education, and continuous evaluation to create lasting change in gender equality within medical education.
Notes on Contributors
Ms. Jillian Yeo was involved in writing the manuscript, conducting the literature search, reviewing the literature retrieved and synthesising the data. Dr Lee Shuh Shing was involved in conducting the literature search, reviewing the literature retrieved and synthesising the data. Dr Dujeepa was involved in the conceptual development of the study and reviewing the manuscript.
Ethical Approval
As this study was a narrative review, ethical approval and IRB application was not required.
Data Availability
The list of articles included in the narrative review can be accessed here:
https://doi.org/10.6084/m9.figshare.25980352.v1 (Yeo, 2024)
Funding
No funding sources are associated with this paper.
Declaration of Interest
There are no conflicts of interests related to the content presented in the paper.
References
Bromberg, G. K., Gay, E. A., Hills-Dunlap, K., & Burnett-Bowie, S. M. (2022). Using a virtual platform to teach residents how to respond to bias. Journal of General Intern Medicine, 37(11), 2871-2872. https://doi.org/10.1007/s11606-021-07156-y
Bruce, A. N., Battista, A., Plankey, M. W., Johnson, L. B., & Marshall, M. B. (2015). Perceptions of gender-based discrimination during surgical training and practice. Med Education Online, 20, 25923. https://doi.org/10.3402/meo.v20.259 23
Caffrey, L., Wyatt, D., Fudge, N., Mattingley, H., Williamson, C., & McKevitt, C. (2016). Gender equity programmes in academic medicine: A realist evaluation approach to Athena SWAN processes. BMJ Open, 6(9), e012090. https://doi.org/10.1136/bmjopen-2016-012090
Carnes, M., Devine, P. G., Baier Manwell, L., Byars-Winston, A., Fine, E., Ford, C. E., Forscher, P., Isaac, C., Kaatz, A., Magua, W., Palta, M., & Sheridan, J. (2015). The effect of an intervention to break the gender bias habit for faculty at one institution: A cluster randomised, controlled trial. Academic Medicine, 90(2), 221-230. https://doi.org/10.1097/acm.0000000000000552
Chang, S., Guindani, M., Morahan, P., Magrane, D., Newbill, S., & Helitzer, D. (2020). Increasing promotion of women faculty in academic medicine: Impact of National Career Development Programs. Journal of Women’s Health (Larchmt), 29(6), 837-846. https://doi.org/10.1089/jwh.2019.8044
Deng, M., Nham, E., Malvea, A., Ramsay, T., Seabrook, C., & Watterson, J. (2021). Exploring the impact of the surgical exploration and discovery (SEAD) program on medical students’ perceptions of gender biases in surgery: A mixed-method evaluation. Journal of Surgical Education, 78(4), 1236-1249. https://doi.org/10.1016/j.jsurg.2020.11.016
DeWane, M. E., Mattessich, S., Wu, R., & Whitaker-Worth, D. (2020). A survey study of resident experiences of sexual harassment during dermatology training. Journal of the American Academy of Dermatology, 83(2), 594-596. https://doi.org/10.1016/j.jaad.2019.07.023
Dhingra, S., Killaspy, H., & Dowling, S. (2021). Gender equality in academic psychiatry in the UK in 2019. BJPsych Bulletin, 45(3), 153-158. https://doi.org/10.1192/bjb.2020.116
Driscoll, S. W., Robinson, L. R., Raddatz, M. M., & Kinney, C. L. (2019). Is there evidence of gender bias in the oral examination for initial certification by the American Board of Physical Medicine & Rehabilitation? American Journal of Physical Medicine & Rehabilitation, 98(6), 512-515. https://doi.org/10.1097/phm.0000000000001126
Ellis, R. J., Hewitt, D. B., Hu, Y. Y., Johnson, J. K., Merkow, R. P., Yang, A. D., Potts, J. R., 3rd, Hoyt, D. B., Buyske, J., & Bilimoria, K. Y. (2019). An empirical national assessment of the learning environment and factors associated with program culture. Annals of Surgery, 270(4), 585-592. https://doi.org/10.1097/sla.0000000000003545
Farkas, A. H., Scholcoff, C., Lamberg, M., Shah, H., Fletcher, K., & Yecies, E. (2022). Preparing residents to respond to incidences of gender discrimination and sexual harassment: An interactive workshop. Southern Medical Journal, 115(10), 740-744. https://doi.org/10.14423/smj.0000000000001459
Ferrari, R. (2015). Writing narrative style literature reviews. Medical Writing, 24(4), 230-235. https://doi.org/10.1179/20474 80615Z.000000000329
Gaida, P., Kujumdshiev, S., & Stengler, K. (2020). Gender sensitivity in career mentoring – A project report from the medical faculty of Leipzig University. GMS Journal for Medical Education, 37(2), Doc24. https://doi.org/10.3205/zma001317
Geiser, E., Schilter, L. V., Carrier, J.-M., Clair, C., & Schwarz, J. (2022). Reflexivity as a tool for medical students to identify and address gender bias in clinical practice: A qualitative study. Patient Education Counselling, 105(12), 3521-3528. https://doi.org/10.10 16/j.pec.2022.08.017
Girod, S., Fassiotto, M., Grewal, D., Ku, M. C., Sriram, N., Nosek, B. A., & Valantine, H. (2016). Reducing implicit gender leadership bias in academic medicine with an educational intervention. Academic Medicine, 91(8), 1143-1150. https://doi.org/10.1097/acm.0000000000001099
Hannon, M., Duffey, K., Bharel, S., Redfield, R., Greidinger, A., Stewart, E., & Diemer, G. (2021). Investigating gender disparities in internal medicine residency awards. The American Journal of Medicine, 134(3), 405-409. https://doi.org/10.1016/j.amjmed.2020.11.003
Harbold, D., Dearolf, L., Buckley, J., & Lattanza, L. (2021). The Perry Initiative’s impact on gender diversity within orthopedic education. Current Reviews in Musculoskeletal Medicine, 14(6), 429-433. https://doi.org/10.1007/s12178-021-09717-4
Jackson, K. R., & Drolet, B. C. (2021). #MedicineToo – Gender bias in medical training: A national survey of residents. Journal of General Internal Medicine, 36(12), 3894-3896. https://doi.org/10.1007/s11606-021-06613-y
Jacobs, N. N., Esquierdo-Leal, J., Smith, G. S., Piasecki, M., & Houmanfar, R. A. (2022). Diversifying academic medicine: One search committee at a time. Front Public Health, 10, 854450. https://doi.org/10.3389/fpubh.2022.854450
Jacques, L., Kaljo, K., Treat, R., Davis, J., Farez, R., & Lund, M. (2016). Intersecting gender, evaluations, and examinations: Averting gender bias in an obstetrics and gynecology clerkship in the United States. Education for Health (Abingdon, England), 29(1), 25-29. https://doi.org/10.4103/1357-6283.178926
Jain, A., Nichols, G., Tarabishy, S., Scomacao, I., & Herrera, F. A. (2022). A comparison of applicant and resident physician demographics among surgical subspecialties from 2009 to 2019: Trends in gender and underrepresented minorities in medicine. Annals of Plastic Surgery, 88(4), 451-459. https://doi.org/10.1097/sap.0000000000003041
Joh, D. B., van der Werf, B., Watson, B. J., French, R., Bann, S., Dennet, E., & Loveday, B. P. T. (2020). Assessment of autonomy in operative procedures among female and male New Zealand general surgery trainees. Journal of the American Medical Association Surgery, 155(11), 1019-1026. https://doi.org/10.1001/jamasurg.2020.3021
Kandi, L. A., Jarvis, T. L., Movtchan, N. V., Hammond, J. B., Teven, C. M., & Rebecca, A. M. (2022). Characterization of national medical societies’ accessible resources to support underrepresented minority and female trainees. Journal of the American Medical Association Network Open, 5(9), Article e2230243. https://doi.org/10.1001/jamanetworkopen.2022.30243
Kisiel, M. A., Kühner, S., Stolare, K., Lampa, E., Wohlin, M., Johnston, N., & Rask-Andersen, A. (2020). Medical students’ self-reported gender discrimination and sexual harassment over time. BioMed Central Medical Education, 20(1), Article 503. https://doi.org/10.1186/s12909-020-02422-9
Klein, R., Law, K., & Koch, J. (2020). Gender representation matters: Intervention to solicit medical resident input to enable equity in leadership in graduate medical education. Academic Medicine, 95(12S), S93-S97. https://doi.org/10.1097/acm.0000000000003698
Kristoffersson, E., Andersson, J., Bengs, C., & Hamberg, K. (2016). Experiences of the gender climate in clinical training – a focus group study among Swedish medical students. BioMed Central Medical Education, 16(1), Article 283. https://doi.org/10.1186/s12909-016-0803-1
Langhan, M. L., Goldman, M. P., & Tiyyagura, G. (2022). Can behavior-based interviews reduce bias in fellowship applicant assessment? Academic Pediatrics, 22(3), 478-485. https://doi.org/10.1016/j.acap.2021.12.017
Lattanza, L. L., Meszaros-Dearolf, L., O’Connor, M. I., Ladd, A., Bucha, A., Trauth-Nare, A., & Buckley, J. M. (2016). The Perry Initiative’s medical student outreach program recruits women into orthopaedic residency. Clinical Orthopaedics and Related Research, 474(9), 1962-1966. https://doi.org/10.1007/s11999-016-4908-y
Liao, H. C., & Wang, Y. H. (2020). Integrating the gender perspective into literature studies to enhance medical university students’ gender awareness and critical thinking. International Journal of Environmental Research and Public Health, 17(24). https://doi.org/10.3390/ijerph17249245
Lieberman, J. A., Ehrhardt, A. A., Simpson, H. B., Arbuckle, M. R., Fyer, A. J., & Essock, S. M. (2018). Eliminating the glass ceiling in academic psychiatry. Academic Psychiatry, 42(4), 523-528. https://doi.org/10.1007/s40596-017-0810-5
Madeeh Hashmi, A., Rehman, A., Butt, Z., Awais Aftab, M., Shahid, A., & Abbas Khan, S. (2013). Gender discrimination among medical students in Pakistan: A cross sectional survey. Pakistan Journal of Medical Sciences, 29(2), 449-453. https://doi.org/10.12669/pjms.292.3256
Meyerson, S. L., Odell, D. D., Zwischenberger, J. B., Schuller, M., Williams, R. G., Bohnen, J. D., Dunnington, G. L., Torbeck, L., Mullen, J. T., Mandell, S. P., Choti, M. A., Foley, E., Are, C., Auyang, E., Chipman, J., Choi, J., Meier, A. H., Smink, D. S., Terhune, K. P., . . . George, B. C. (2019). The effect of gender on operative autonomy in general surgery residents. Surgery, 166(5), 738-743. https://doi.org/10.1016/j.surg.2019.06.006
Organisation for Economic Co-operation and Development. (2022). The proportion of female doctors has increased in all OECD countries over the past two decades. https://www.oecd.org/gender/data/the-proportion-of-female-doctors-hasincreased-in-all-oecd-countries-over-the-past-two-decades.htm
Olson, E. M., Dines, V. A., Ryan, S. M., Halvorsen, A. J., Long, T. R., Price, D. L., Thompson, R. H., Tollefson, M. M., Van Gompel, J. J., & Oxentenko, A. S. (2022). Physician identification badges: A multispecialty quality improvement study to address Professional misidentification and bias. Mayo Clinic Proceedings, 97(4), 658-667. https://doi.org/10.1016/j.mayocp.2022.01.007
Olson, E. M., Sanborn, D. M., Dyster, T. G., Kelm, D. J., Murray, S. G., Santhosh, L., & DesJardin, J. T. (2023). Gender disparities in critical care procedure training of internal medicine residents. American Thoracic Society Scholar, 4(2), 164-176. https://doi.org/10.34197/ats-scholar.2022-0025OC
Saberi, R. A., Herrera Gomez, L. C., Brady, A. C., Sola, J. E., Velazquez, O. C., & Neville, H. L. (2021). AAMC data shows effect of surgery faculty diversity on general surgery resident attrition rate at programs sponsored by LCME-accredited medical schools. Journal of Surgical Education, 78(4), 1123-1126. https://doi.org/10.1016/j.jsurg.2020.11.015
Sabin, J., Guenther, G., Ornelas, I. J., Patterson, D. G., Andrilla, C. H. A., Morales, L., Gurjal, K., & Frogner, B. K. (2022). Brief online implicit bias education increases bias awareness among clinical teaching faculty. Medical Education Online, 27(1), Article 2025307. https://doi.org/10.1080/10872981.2021.2025307
Sakowski, S. A., Feldman, E. L., Jagsi, R., & Singer, K. (2020). Energizing the conversation: How to identify and overcome gender inequalities in academic medicine. Journal of Continuing Education in the Health Professions, 40(4), 274-278. https://doi.org/10.1097/ceh.0000000000000296
Sethi, S., Edwards, J., Webb, A., Mendoza, S., Kumar, A., & Chae, S. (2022). Addressing gender disparity: Increase in female leadership increases gender equality in program director and fellow ranks. Digestive Diseases and Sciences, 67(2), 357-363. https://doi.org/10.1007/s10620-020-06686-5
Sobel, A. D., Lavorgna, T. R., Ames, S. E., Templeton, K. J., & Mulcahey, M. K. (2023). Interpersonal interactions and biases in orthopaedic surgery residency: Do experiences differ based on gender? Clinical Orthopaedics and Related Research, 481(2), 369-378. https://doi.org/10.1097/corr.0000000000002457
Sulibhavi, A., Kaufmann, M. R., Shetty, K. R., Wulu, J. A., Tracy, L. F., & Levi, J. R. (2021). Factors associated with distribution of female otolaryngology residents in United States. Laryngoscope, 131(2), E367-E372. https://doi.org/10.1002/lary.28746
Yeo, J. (2024). Gender equality Data and flow chart.docx (Version 1). Figshare. https://doi.org/10.6084/m9.figshare.25980352.v1
Ying, Y., Dupre, J., & Bhanji, F. (2023). Female surgical trainee recruitment and attrition – A 10-year national retrospective review. The American Journal of Surgery, 225(2), 282-286. https://doi.org/10.1016/j.amjsurg.2022.07.020
Zhang, N., Blissett, S., Anderson, D., O’Sullivan, P., & Qasim, A. (2021). Race and gender bias in internal medicine program director letters of recommendation. Journal of Graduate Medical Education, 13(3), 335-344. https://doi.org/10.4300/jgme-d-20-00929.1
*Han Ting Jillian Yeo
10 Medical Drive,
Singapore 117597
Email: jillyeo@nus.edu.sg
Submitted: 23 November 2021
Accepted: 10 May 2022
Published online: 4 October, TAPS 2022, 7(4), 59-70
https://doi.org/10.29060/TAPS.2022-7-4/OA2714
Deepthi Edussuriya1, Sriyani Perera2, Kosala Marambe3, Yomal Wijesiriwardena1 & Kasun Ekanayake1
1Department of Forensic Medicine, Faculty of Medicine, University of Peradeniya, Sri Lanka; 2Medical Library, University of Peradeniya, Sri Lanka; 3Department of Medical Education, Faculty of Medicine, University of Peradeniya, Sri Lanka
Abstract
Introduction: Emotional Intelligence (EI) is especially important for medical undergraduates due to the long undergraduate period and relatively high demands of the medical course. Determining associates of EI would not only enable identification of those who are most suited for the discipline of medicine but would also help in designing training strategies to target specific groups. However, there is diversity of opinion regarding the associates of EI in medical students. Aim of the study was to determine associates of EI in medical students.
Methods: The databases MEDLINE, CENTRAL, Scopus, EbscoHost, LILAC, IMSEAR and three others were searched. It was followed by hand-searching, cited/citing references and searching through PQDT. All studies on the phenomenon of EI and/or its associates with medical students as participants were retrieved. Studies from all continents of the world, published in English were selected. They were assessed for quality using Q-SSP checklist followed by narrative synthesis on selected studies.
Results: Seven hundred and ninety-two articles were identified of which 29 met inclusion criteria. One article was excluded as its full text was not available. Seven articles found an association between ‘EI and academic performance’, 11 identified an association between ‘EI and mental health’, 11 found an association between ‘EI and Gender’, 6 identified an association between ‘EI and Empathy’ while two have found an association with the learning environment.
Conclusion: Higher EI is associated with better academic performance, better mental health, happiness, learning environment, good sleep quality and less fatigue, female gender and greater empathy.
Keywords: Emotional Intelligence, Associates of Emotional Intelligence, Medical Students, Mental Wellbeing, Empathy
Practice Highlights
- Higher emotional intelligence is associated with better academic performance.
- Higher emotional intelligence is associated with better mental health.
- Higher emotional intelligence is associated with female gender.
- Higher emotional intelligence is associated with greater empathy.
I. INTRODUCTION
Emotional intelligence (EI) is defined as “the ability to perceive emotions accurately, appraise, and express emotion; the ability to assess and/or generate feelings when they facilitate thought; ability to understand emotions and emotional knowledge, and to regulate emotions to promote emotional and intellectual growth” (Mayer & Salovey, 1997). Studies have found that there is a positive effect between EI and academic as well as professional success (Suleman et al., 2019). It has been reported that people and college students with good EI show better social functioning and interpersonal relationship and peers have identified them as less antagonistic and conflictual (Petrovici & Dobrescu, 2014).
Several tests and instruments that have been used to assess the Emotional intelligence of medical students were identified through the literature. These include standard EI tests, modified versions of standard EI tests, and authors’ assessment methods of their own. Schutte self-report EI test, TEIQue questionnaire and Bar-on’s emotional intelligence questionnaire ((EQ-i) 2.0) have been used frequently. Each of these instruments has different advantages and disadvantages of their own.
The Emotional Quotient Inventory (EQ-i) 2.0 is a revision of the EQ-I (Bar-On, 2004). The Emotional Quotient Inventory (EQ-I) 2.0 measures the interaction between an individual and their environment. Since the EQ-i 2.0 is a revision of the original Emotional Quotient Inventory (EQ-I) the standard platform of the EQ-i validation remains intact.
The Schutte Self-Report Emotional Intelligence Test (SSEIT) is a method of measuring general Emotional Intelligence (EI), using four sub-scales: emotion perception, utilising emotions, managing self- relevant emotions, and managing others’ emotions (Schutte et al., 1998). The SSEIT model is closely associated with the EQ-I model of Emotional Intelligence. It has a reliability rating of 0.90. The EI score, overall, is fairly reliable for adults and adolescents. However, the utilising emotions sub-scale has shown poor reliability (Ciarrochi et al., 2001). Also, they report a mediocre correlation of the SSREI with self-estimated EI, the Big Five EI scale, and life satisfaction (Petrides & Furnham, 2000). However, SSREI correlated poorly with well-being and EI criteria.
The Trait Emotional Intelligence Questionnaire (TEIQue), is an openly accessible instrument developed to measure global trait emotional intelligence. Based on the Trait Emotional Intelligence Theory, a significant number of research has been conducted regarding emotional intelligence (EI) (Mikolajczak et al., 2007). The TEIQue is available in long form and short forms. Internal consistency and test-retest both indicated scale reliabilities of 0.71 and 0.76. High correlations between the TEIQue with Shrink’s Emotional Intelligence Scale showed validity in measuring emotional intelligence and the “Big Five” Personality Traits.
Apart from those assessment methods, Genos Emotional Intelligence Assessment, Mayer-Salovey-Caruso Emotional Intelligence Test, TMMS-24 data and DASS-21 scale, Bradbury-Graves’s Emotional Intelligence and Siberia Schering’s Emotional Intelligence Questionnaire have also been used by the authors to assess the EI.
A comprehensive survey in medicine states that EI had a positive contribution in doctor-patient relationship, increased empathy, teamwork, communication skills, stress management, organisational commitment and leadership (Arora et al., 2010). EI is invariably important to medical professionals as it is associated with self-monitoring which would not only ensure adapting to clinical situations appropriately and having desirable interpersonal relations but also result in a favorable outcome for the patient and the wellbeing of the practitioner.
Few studies suggest that EI training can help medical students to build their leadership and empathy skills, as they enter the clinical years (Austin et al., 2005; Dolev et al., 2019). Literature surveys on emotional intelligence and medicine, and physician leadership qualities concludes that EI correlates with many of the competencies that modern medical curricula seek to deliver including leadership (Mintz & Stoller, 2014; Reshetnikov et al., 2020). Other studies indicate that age and gender are associated with emotional intelligence. However, some studies showed that EI at medical school admission could not reliably predict academic success in later years (Reshetnikov et al., 2020). These studies have all looked at the associates in an isolated sense. However, it would also be interesting to reflect on the concept of EI in a broader sense as it is inevitable that there would be an interaction of factors.
The medical course extends over a period of five years as opposed to most undergraduate degrees which are shorter. Medical training involves close interactions with different categories of people including patients, doctors of different grades and the paramedical staff. Training includes long hours of work in stressful environments where some situations could be emotionally challenging. This long undergraduate period and relatively high demands of the medical course would require medical students to possess a high degree of EI. As findings of different studies on EI are sometimes diverse in opinion, it would be useful to conduct a systematic review to identify the associates of EI in order to design training strategies which target specific groups.
Even though EI is considered a trainable trait, the extent of trainability depends on many personal and institutional factors (Mattingly & Kraiger, 2019). Völker (2020) expresses that trainability in emotional intelligence is subjected to acquired knowledge which is situational and may depend on accumulating relevant experience.
In the Sri Lankan context, the sole criteria for selection of students to a medical course is the academic excellence at the Advanced level examination, which alone may not reflect their suitability to follow a profession like medicine (University Grants Commission, 2022).
However, since EI is an essential trait especially for medical practice many universities worldwide use different tools to assess EI in their applicants. Furthermore, different universities adopt varying techniques to develop EI of their students throughout the course. It is envisaged that this review would not only help determine what additional factors could be considered in the selection of applicants for a medical course but would also help teachers design training strategies to target specific groups of students and also ensure a more enjoyable and productive learning experience for the students as a whole. There is no doubt that these selection and intervention programs would produce doctors with more favourable qualities which would not only produce greater benefits to the patient but would prevent burn out among doctors.
A. Objective
The objective of this study is to find out, the associates of Emotional Intelligence in Medical students based on available literature in English from 2015 to 2020.
II. MATERIALS AND METHODS
The research question was defined based on the PICOS (Population, Intervention, Comparison, Outcomes and Setting) format. The review protocol was developed according to PRISMA-P 2015 (Preferred reporting items for systematic review and meta-analysis protocols) statement (Moher et al. 2015) by all three authors DE, KM and SP and was registered in the PROSPERO Registry (CRD42021227877). The methodology for the systematic review (SR) followed the guidelines and standards of IOM (Institute of Medicine) (Eden et al., 2011) and PRISMA-2015 for reporting.
A. Search Strategy
A Systematic and comprehensive search was conducted by SP in April 2020 and references were managed using the software Mendeley. The search explicitly aimed to identify all published and unpublished relevant studies in order to limit bias in the searching process. The key search terms were identified with the aid of a search-term-harvesting table by KM and DE. A combination of relevant medical subject headings and search terms tagged with other appropriate search fields were used in the literature search. The following databases were searched:
CDSR (Cochrane Database of Systematic Reviews), DARE (The Database of Abstracts of Reviews of Effects), MEDLINE (1950- 2020) via Pubmed (See supplemental Appendix 1 for search strategy), CENTRAL (The Cochrane Central Register of Controlled Trials, 1948 – 2020), Scopus, EbscoHost, LILAC, IMSEAR (Index Medicus for South East Asian region) and WHO International Clinical Trials Registry Platform (ICTRP). In addition to electronic searches, two key journals (2015-2020) were hand-searched, and cited & citing references of all included studies were screened for further relevant articles. Searches were limited to studies published between the years 2015-2020. Searching other resources included grey literature such as PQDT (ProQuest Dissertations and Thesis database) and Global health (via WHO).
B. Selection Criteria
After removal of duplicates from the retrieved articles, the remaining articles with abstracts were uploaded to the Web application, Rayyan (Quzzani et al., 2016) for the purpose of screening. The criteria for selection of articles were based on the PICOS elements. The studies were from all continents of the world and limited to those published in English. All studies focusing on the phenomenon of EI and/or its associates with medical students as participants were considered for inclusion in the review.
The authors DE, KM, SP and KE independently screened the uploaded articles in Rayyan, using the above eligibility criteria. In the first phase, title and abstract of each article were reviewed by any of the two authors independently for its candidacy. Following this initial evaluation, the full text of all those selected articles were retrieved and further examined by KM and DE independently (second phase), for the final verification before inclusion in the review. Any disagreements regarding eligibility of studies were resolved by consulting a third author (SP). Reviews, systematic reviews, editorials, letters and comments were removed. Articles which met the eligibility criteria were selected for inclusion in the review. Excluded studies were marked with the ‘reason’ in Rayyan.
C. Data Extraction and Quality Assessment
Data from all included studies were extracted by the review authors YW and KM using a data extraction table developed for the purpose of this review (Appendix 2). Data extracted were cross-checked by SP for any errors. Information recorded included: study details (author, year, country of origin), participants (number of participants, gender, level of undergrad program, etc.), methods (study aim, design, total study duration, tools used), study type (phenomenon /context studied) and outcomes (all relevant findings related to primary and secondary outcomes).
SP and YW independently assessed the quality of those selected studies using Quality Assessment Checklist for Survey Studies in Psychology (Q-SSP) (Protogerou & Hagger, 2020) Results of the quality assessments were compared (Appendix 3); any disagreements were resolved by consensus. Articles which met the required quality criteria were selected for inclusion in the review.
D. Strategy for Data Synthesis
Due to the heterogeneity between the included studies, a quantitative synthesis was not considered. A narrative synthesis of the findings from individual included studies was carried out by DE, based on the characteristics of the targeted populations and the type of outcome such as association/correlation of EI with academic performance, professional success, social functioning, interpersonal relationship, empathy, teamwork spirit, communication skills, stress management, organizational commitment, leadership quality, self-monitoring, mental health and emotional well-being.
III. RESULTS
A total of 792 articles were retrieved during the literature search. After removing the duplicates, 752 articles were considered for screening using the eligibility criteria. Initial evaluation of articles through title and abstract resulted in only 29 articles meeting the selection criteria. During the full-text evaluation, one article (Parijitham, 2018) was removed, as its full-text article could not be found even after contacting the author. The data that support the findings of this study are openly available at https://doi.org/10.6084/m9.figshare.15564210 (Edussuriya et al., 2021). Twenty-eight articles were finally selected for quality assessment. Flow diagram of the selection of studies is shown in Figure 1.
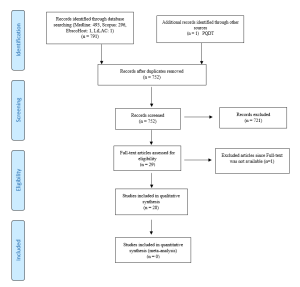
Figure 1. Flow diagram illustrating included and excluded studies in the systematic review
The study design of the selected studies comprised of 26 cross sectional (majority), one longitudinal and one quasi-experimental. However, all studies used standard validated survey questionnaires to collect data. Therefore, to assess the quality of selected studies, Quality Assessment Checklist for Survey Studies in Psychology (Q-SSP) was selected as the best, ‘applicable to all’ tool in this review, considering its relevance also to the trait emotional intelligence since emotions, thoughts and mental processes are aspects of psychology. The quality of the studies was determined by the extent to which the items on above checklist were met by each of the articles. There were 20 checklist items in the tool out of which one item (item-19 – Debriefing participants at the end of data collection) could be justifiably waived; one reason being none of the included studies used it in the methodology. Thus 19 items were considered to be applicable in this review (Appendix 4).
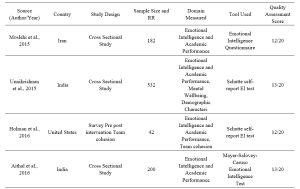



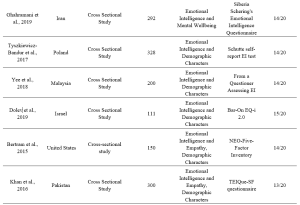

Table 1. Characteristics of included studies
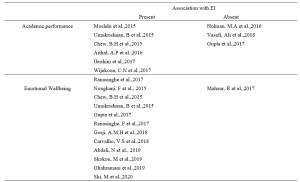

Table 2. Categorisation of findings of the studies
A. Findings of Studies and Data Analysis
1) EI and academic performance: According to studies, a positive correlation was identified between EI and academic performance (Aithal, et al., 2016, Ibrahim et al. 2017; Moslehi et al., 2015, Wijekoon et al., 2017) while (Ranasinghe et al., 2017; Unnikrishnan et al., 2015) also found a significant association between EI and academic performance. These studies indicated that students with higher EI intend to perform better in their academic work. A cross-sectional study done by Chew et al. (2015) showed that medical students with less emotional intelligence were largely unaware of their anxiety, which was associated with lower academic performance. According to studies done by Holman et al., 2016, Gupta et al., 2017 and Vasefi et al., 2018 there was no correlation of EI with academic performance. A study by Othman et al., 2020 revealed that EI showed a significant positive effect on intuitive decision-making style and a negative effect on avoidant and dependent decision-making styles which may explain better academic performance of medical students with high EI.
2) EI and mental health (emotional wellbeing): A direct relationship between EI and academic satisfaction was found in studies done by Rouhani et al., 2015, Unnikrishnan et al., 2015 and Carvalho et al., 2018. Further, Carvalho et al., 2018 reported that a positive relationship was observed between EI and academic-related well-being which accounts for both academic performance and mental health. It was seen that medical students with less emotional intelligence were largely unaware of their anxiety (Chew et al., 2015) and those with higher emotional intelligence perceived lesser stress (Gupta et al., 2017 and Ranasinghe et al., 2017). Shi and Du (2020) found that EI was strongly and negatively associated with Personal Distress. Heidari Gorji et al. (2018) identified a direct relationship between emotional intelligence and mental health while a study done by Mahaur et al. (2017) did not find a significant relationship between the two. Ghahramani et al. (2019) identified a significant positive relationship of EI with happiness while Abdali et al. (2019) showed a positive correlation with sleep quality and a negative correlation with general fatigue.
3) EI and demographic characters: Higher EI in females compared to males was found (Aithal et al., 2016, Bertram et al., 2015, Ibrahim et al., 2017, Khan et al., 2016, Raut & Gupta, 2019 Sundararajan and Gopichandran, 2018, Tyszkiewicz-Bandur et al., 2017, Unnikrishnan et al., 2015 and Wijekoon et al., 2017). Irfan et al. (2019) suggests that female medical students had significantly higher empathic behavior and emotional intelligence than male students. However, Skokou et al. (2019) did not find any difference in EI in males and females. Vasefi et al. (2018) and Abe et al. (2018) too did not find a significant relationship between EI and gender. However, Abe et al. (2018) revealed that females showed significantly higher Neuroticism, Agreeableness and Empathy scores than males. According to Ibrahim et al. (2017) increasing age resulted in higher EI. However, Yee et al. (2018) did not find a significant association of EI with age. According to Yee et al. (2018) there was no significant association of EI with ethnicity.
4) EI and empathy: Significant correlation between EI and Empathy was identified (Bertram et al., 2015, Irfan et al., 2019 Khan et al., 2016; Sundararajan & Gopichandran, 2018). Shi and Du (2020) suggests that EI helps medical professionals to establish a better association with the patient.
5) Learning environment: Relationship between EI and academic background was identified by both Irfan et al. (2019) and Sundararajan and Gopichandran (2018). According to Sundararajan and Gopichandran (2018), students who attended government schools for high school education had greater emotional intelligence than students from private schools. But Irfan et al. (2019) suggests that medical students of private medical schools showed higher level of empathy as compared to public medical schools. Dolev et al. (2019) reveals that there are no differences in EI levels between first-year and sixth-year medical students.
IV. DISCUSSION
The review included studies conducted in South and Southeast Asian, European, Arabian, North American and South American countries. Majority of studies on Asian students revealed a high association between EI and academic performance. However, two studies on Asian students and one on US students failed to observe such associations. The impact of EI on academic performance may be explained by the fact that being aware of one’s anxiety relieved stress and those with high EI experienced greater mental wellbeing and satisfaction with their programs; which may contribute to better academic performance. Furthermore, the fact that EI showed a positive correlation with better mental health/wellbeing, less perceived stress/distress, happiness, good sleep quality and less fatigue may account for the better academic performance of students with high EI.
Empathy is an important aspect in the delivery of high-quality healthcare. Several researchers from different regions of the world reported strong association between empathy and high EI scores. Therefore, assessment of EI may be useful in admitting students for medical degrees. However, since EI is considered as a “trainable trait”, the role that EI plays in admitting students to medical schools is debatable. Therefore, all efforts must be taken by medical schools to include activities that enhance EI, during the medical course, irrespective of the EI levels of students on admission. The fact that EI did not improve with seniority does not purely support the fact that EI is not trainable but it maybe those students were not exposed to and not sensitised to activities which enhance EI.
Evidence indicated a positive association between high EI scores and female gender. It maybe postulated that the “nurturing and caring” role assigned by society to the females influence their upbringing. Thereby improving their emotional intelligence.
In conclusion it must be stated that since a majority of studies revealed that higher EI is associated with better academic performance, better mental health and greater empathy and since EI is considered a trainable trait, curricular need to be developed with a view to improving EI.
In order to develop EI, curricular should contain programs on general leadership development, self-care/ wellness and burn-out prevention (Monroe & English, 2013). Small-group experiential learning activities and meeting with trained mentors throughout the years would be helpful. Debriefing sessions and maintaining a journal are some other techniques that need to be considered. It may be helpful to discuss change management and quality improvement with students (Audra et al., 2020). Exposure of students to skills of self-awareness and self-management through discussion, exposure to theories of conflict management, mindfulness practice, leadership training, discussions on learning styles, discussions on power and influence, identification of team dynamics, exposure to high-functioning inter-professional teams, peer coaching, health care leader interview and shadowing of experienced clinicians are some techniques that could be adopted in attempting to develop EI among students (Kozlowski & Ilgen, 2006). It would be beneficial to evaluate acquisition based on completion of an EI inventory, feedback from peers and staff, project presentations, reflective writing, measurement of achievement of professional and personal development benchmarks and milestones, performance on simulated scenarios and small-group exercises (Pan & Allison, 2010).
During the study it was observed that there is paucity of longitudinal studies on Associates of EI. Therefor it would be beneficial to conduct longitudinal studies which may help identify some aspects with regard to the trainability of EI in medical students.
V. CONCLUSION
Through this review it was revealed that higher EI is associated with
- better academic performance,
- better mental health including less perception of stress and distress, happiness, good sleep quality and less fatigue,
- female gender, and
- greater empathy.
No significant association was found between age, ethnicity, and seniority in the medical course, and emotional intelligence. No conclusions could be made about the association between the nature of the educational institute (private or state) and emotional intelligence.
A. Limitations
In this review, it was found that authors of included studies which used several different tools to assess the EI of medical students. Each of these tools have their own advantages and disadvantages which cause comparison difficult. It could not be assumed that, each and every one of these methods provide results in the same level.
B. Recommendation
Since high EI has shown a positive correlation with academic performance and better mental wellbeing of students and since it has been identified as a “trainable trait” all efforts should be made to enhance EI of medical students during their undergraduate training.
Notes on Contributors
Edussuriya D.H (DE) was the Principal Investigator of the study. Protocol drafting, study selection, analysis and interpretation of data, synthesis of findings of individual studies and the drafting of manuscript was done by the author.
Perera S. (SP) facilitated the methodology, involved in drafting the protocol and retrieved selected articles, since the author has previous experience in conducting systematic reviews. Reference management in Mendeley and Rayyan, cross-checking the extracted data, assessed quality of selected studies and final review of draft was also done by the author.
Marambe K.N (KM) was involved in drafting the protocol, involved in article selection and extracted data from the selected articles.
Wijesiriwardena W.M.S.Y (YW) extracted data from selected articles, assessed the quality of selected articles and finalised the manuscript.
Ekanayake E.M.K.B (KE) has screened the uploaded articles in Rayyan.
Ethical Approval
The review is registered in PROSPERO – The International Prospective Register of Systematic Reviews under the registration number CRD42021227877 for the systematic review.
Data Availability
Data set that support the findings of this study are openly available in Figshare repository https://doi.org/10.6084/ m9.figshare.15564210
Acknowledgement
The authors acknowledge Information Officers of National Science Library and Resources Center, National Science Foundation, Sri Lanka for support in Scopus searches and staff of Medical Library of Faculty of Medicine, University of Peradeniya for the assistance in finding full text articles of the included studies in the review.
Funding
No funding sources are associated with this study.
Declaration of Interest
No conflicts of interest are associated with this paper.
References
Abdali, N., Nobahar, M., & Ghorbani, R. (2019). Evaluation of emotional intelligence, sleep quality, and fatigue among Iranian medical, nursing, and paramedical students: A cross-sectional study. Qatar Medical Journal, 2019(3), 15. https://doi.org/10.5339/qmj.2019.15
Abe, K., Niwa, M., Fujisaki, K., & Suzuki, Y. (2018). Associations between emotional intelligence, empathy and personality in Japanese medical students. BMC Medical Education, 18, Article 47. https://doi.org/10.1186/s12909-018-1165-7
Aithal, A. P., Kumar, N., Gunasegeran, P., Sundaram, S. M., Rong, L. Z., & Prabhu, S. P. (2016). A survey-based study of emotional intelligence as it relates to gender and academic performance of medical students. Education for Health, 29(3), 255–258.
Arora, S., Ashrafian, H., Davis, R., Athanasiou, T., Darzi, A., & Sevdalis, N. (2010). Emotional intelligence in medicine: A systematic review through the context of the ACGME competencies. Medical education, 44(8), 749–764. https://doi.org/10.1111/j.1365-2923.2010.03709.x
Audra, V. W., O’Brien, T. C., Varvayanis, S., Alder, J., Greenier, J., Layton, R. L., Stayart,C. A., Wefes, I., & Brady, A. E. (2020). Applying experiential learning to career development training for biomedical graduate students and postdocs: Perspectives on program development and design. CBE—Life Sciences Education, 19(3), 1-12. https://doi.org/10.1187/cbe.19-12-0270
Austin, E. J., Evans, P., Goldwater, R., & Potter, V. (2005). A preliminary study of emotional intelligence, empathy and exam performance in first year medical students. Personality and Individual Differences, 39(8), 1395-1405. https://doi.org/10.1016/j.paid.2005.04.014
Bar-On, R. (2004). The Bar-On Emotional Quotient Inventory (EQ-i): Rationale, description and summary of psychometric properties. In G. Geher (Ed.), Measuring Emotional Intelligence: Common Ground and Controversy (pp. 115–145). Nova Science Publishers.
Bertram, K., Randazzo, J., Alabi, N., Levenson, J., Doucette, J. T., & Barbosa, P. (2016). Strong correlations between empathy, emotional intelligence, and personality traits among podiatric medical students: A cross-sectional study. Education for Health (Abingdon), 29(3), 186–194.
Carvalho, V. S., Guerrero, E., & Chambel, M. J. (2018). Emotional intelligence and health students’ well-being: A two-wave study with students of medicine, physiotherapy and nursing. Nurse Education Today, 63, 35–42. https://doi.org/10.1016/j.nedt.2018.01.010
Chew, B. H., Hassan, F., & Zain, A. M. (2015). Medical students with higher emotional intelligence were more aware of self-anxiety and scored higher in continuous assessment: A cross-sectional study. Medical Science Educator, 25(4), 421-430. https://doi.org/10.1007/s40670-015-0168-9
Ciarrochi, J., Chan, A. Y., & Bajgar, J. (2001). Measuring emotional intelligence in adolescents. Personality and Individual Differences, 31(7), 1105-1119. https://doi.org/10.1016/S0191-8869(00)00207-5.
Dolev, N., Goldental, N., Reuven-Lelong, A., & Tadmor, T. (2019). The evaluation of emotional intelligence among medical students and its links with non-cognitive acceptance measures to medical school. Rambam Maimonides Medical Journal, 10(2), e0010. https://doi.org/10.5041/RMMJ.10365
Eden, J., Levit, L., Berg, A., & Morton. S. (2011). Finding what works in health care: Standards for systematic reviews. National Academies Press. https://doi.org/10.17226/13059
Edussuriya, D., Perera, S., Marambe, K., Wijesiriwardena, Y., & Ekanayake, K. (2021). Emotional intelligence systematic review (Version 3) [Data Set]. Figshare. https://doi.org/10.6084/m9.figshare.15564210.v3
Ghahramani, S., Jahromi, A. T., Khoshsoroor, D., Seifooripour, R., & Sepehrpoor, M. (2019). The relationship between emotional intelligence and happiness in medical students. Korean Journal of Medical Education, 31(1), 29–38. https://doi.org/10.3946/kjme.2019.116
Gupta, R., Singh, N., & Kumar, R. (2017). Longitudinal predictive validity of emotional intelligence on first year medical students perceived stress. BMC Medical Education, 17(1), 139. https://doi.org/10.1186/s12909-017-0979-z
Heidari Gorji, A. M., Shafizad, M., Soleimani, A., Darabinia, M., Goudarzian, A. H. (2018) Path analysis of self-efficacy, critical thinking skills and emotional intelligence for mental health of medical students. Iranian Journal of Psychiatry and Behavioral Sciences. 12(4), e59487. https://doi.org/10.5812/ijpbs.59487
Holman, M. A., Porter, S. G., Pawlina, W., Juskewitch, J. E., & Lachman, N. (2016). Does emotional intelligence change during medical school gross anatomy course? Correlations with students’ performance and team cohesion. Anatomical Sciences Education, 9(2), 143–149. https://doi.org/10.1002/ase.1541
Ibrahim, N. K., Algethmi, W. A., Binshihon, S. M., Almahyawi, R. A., Alahmadi, R. F., & Baabdullah, M. Y. (2017). Predictors and correlations of emotional intelligence among medical students at King Abdulaziz University, Jeddah. Pakistan Journal of Medical Sciences, 33(5), 1080–1085. https://doi.org/10.12669/pjms.335.13157
Irfan, M., Saleem, U., Sethi, M. R., & Abdullah, A. S. (2019). Do we need to care: emotional intelligence and empathy of medical and dental students. Journal of Ayub Medical College, Abbottabad: JAMC, 31(1), 76–81.
Khan, M. A., Niazi, I. M., & Rashdi, A. (2016). Emotional intelligence predictor of empathy in medical students. Rawal Medical Journal, 41(1), 121-124.
Kozlowski, SWJ., & Ilgen. D.R. (2006). Enhancing the effectiveness of work groups and teams. Psychological Science in the Public Interest, 7(3), 77-124. https://doi.org/10.1111/j.1529-1006.2006.00030.x
Mahaur, R., Jain, P., & Jain, A. K. (2017). Association of mental health to emotional intelligence in medical undergraduate students: Are there gender differences? Indian Journal of Physiology and Pharmacology, 61(4), 383-391.
Mattingly, V., & Kraiger, K. (2019). Can emotional intelligence be trained? A meta-analytical investigation. Human Resource Management Review, 29(2), 140-155. https://doi.org/10.1016/j.hrmr.2018.03.002
Mayer, J. D., & Salovey, P. (1997). What is emotional intelligence? Emotional development and emotional intelligence: Educational implications (pp. 3-31). Basic Books.
Mikolajczak, M., Luminet, O., Leroy, C., & Roy, E. (2007). Psychometric properties of the Trait Emotional Intelligence Questionnaire: Factor structure, reliability, construct, and incremental validity in a French-speaking population. Journal of Personality Assessment, 88(3), 338–353. https://doi.org/10.1080/00223890701333431
Mintz, L. J., & Stoller, J. K. (2014). A systematic review of physician leadership and emotional intelligence. Journal of Graduate Medical Education, 6(1), 21–31. https://doi.org/10.4300/JGME-D-13-00012.1
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., Stewart, L. A., & PRISMA-P Group (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), Article 1. https://doi.org/10.1186/2046-4053-4-1
Monroe, A. D., & English, A. (2013). Fostering emotional intelligence in medical training: The SELECT program. AMA Journal of Ethics, 13(6), 509-513. https://doi.org/10.1001/virtualmentor.2013.15.6.medu1-1306
Moslehi, M., Samouei, R., Tayebani, T., & Kolahduz, S. (2015). A study of the academic performance of medical students in the comprehensive examination of the basic sciences according to the indices of emotional intelligence and educational status. Journal of Education and Health Promotion, 4, 66. https://doi.org/10.4103/2277-9531.162387
Noughani, F., Bayat, R. M., Ghorbani, Z., & Ramim, T. (2015). Correlation between emotional intelligence and educational consent of students of Tehran University of Medical Students. Tehran University Medical Journal, 73(2), 110-116.
Othman, R., El Othman, R., Hallit, R., Obeid, S., & Hallit, S. (2020). Personality traits, emotional intelligence and decision-making styles in Lebanese universities medical students. BMC Psychology, 8(1), Article 46. https://doi.org/10.1186/s40359-020-00406-4
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan- A web and mobile app for systematic reviews. Systematic Reviews, 5(1), Article 210. https://doi.org/10.1186/s13643-016-0384-4
Petrides, K., & Furnham, A. (2000). On the dimensional structure of emotional intelligence. Personality and Individual Differences, 29(2), 313-320. https://doi.org/10.1016/S0191-8869(99)00195-6
Petrovici, A., & Dobrescu, T. (2014). The role of emotional intelligence in building interpersonal communication skills. Procedia-Social and Behavioral Sciences, 116, 1405-1410. https://doi.org/10.1016/j.sbspro.2014.01.406
Protogerou, C., & Hagger, M. S. (2020). A checklist to assess the quality of survey studies in psychology. Methods in Psychology, 3, 100031. https://doi.org/10.31234/osf.io/uqak8
Ranasinghe, P., Wathurapatha, W. S., Mathangasinghe, Y., & Ponnamperuma, G. (2017). Emotional intelligence, perceived stress and academic performance of Sri Lankan medical undergraduates. BMC Medical Education, 17(1), Article 41. https://doi.org/10.1186/s12909-017-0884-5
Raut, A. V., & Gupta, S. S. (2019). Reflection and peer feedback for augmenting emotional intelligence among undergraduate students: A quasi-experimental study from a rural medical college in central India. Education for Health (Abingdon, England), 32(1), 3–10. https://doi.org/10.4103/efh.EfH_31_17
Reshetnikov, V. A., Tvorogova, N. D., Hersonskiy, I. I., Sokolov, N. A., Petrunin, A. D., & Drobyshev, D. A. (2020). Leadership and emotional intelligence: current trends in public health professionals training. Frontiers in Public Health, 7, 413. https://doi.org/10.3389/fpubh.2019.00413
Schutte, N. S., Malouff, J. M., Hall, L. E., Haggerty, D. J., Cooper, J. T., Golden, C. J., & Dornheim, L. (1998). Development and validation of a measure of emotional intelligence. Personality and Individual Differences, 25(2), 167–177. https://doi.org/10.1016/S0191-8869(98)00001-4
Shi, M., & Du, T. (2020). Associations of emotional intelligence and gratitude with empathy in medical students. BMC Medical Education, 20(1), Article 116. https://doi.org/10.1186/s12909-020-02041-4
Skokou, M., Sakellaropoulos, G., Zairi, N. A., Gourzis, P., & Andreopoulou, O. (2019). An exploratory study of trait emotional intelligence and mental health in freshmen Greek medical students. Current Psychology, 40, 6057–6066. https://doi.org/10.1007/s12144-019-00535-z
Suleman, Q., Hussain, I., Syed, M. A., Parveen, R., Lodhi, I. S., & Mahmood, Z. (2019). Association between emotional intelligence and academic success among undergraduates: A cross-sectional study in KUST, Pakistan. PloS one, 14(7), e0219468. https://doi.org/10.1371/journal.pone.0219468
Sundararajan, S., & Gopichandran, V. (2018). Emotional intelligence among medical students: A mixed methods study from Chennai, India. BMC Medical Education, 18(1), Article 97. https://doi.org/10.1186/s12909-018-1213-3
Tyszkiewicz-Bandur M., Walkiewicz M, Tartas M, Bankiewicz-Nakielska J. (2017). Emotional intelligence, attachment styles and medical education. Family Medicine & Primary Care Review, 19(4), 404–407. https://doi.org/10.5114/fmpcr.2017.70127
University Grants Commission, Sri Lanka. (2022). University Admissions. Retrieved April 21, 2022, from https://www.ugc.ac.lk/index.php?option=com_content&view=article&id=25&Itemid=11&lang=en
Unnikrishnan, B., Darshan, B., Kulkarni, V., Thapar, R., Mithra, P., Kumar, N., Holla, R., Kumar, A., Sriram, R., Nair, N., Juanna, Rai, S., & Najiza, H. (2015). Association of emotional intelligence with academic performance among medical students in South India. Asian Journal of Pharmaceutical and Clinical Research, 8(2), 300-302.
Vasefi, A., Dehghani, M., & Mirzaaghapoor, M. (2018). Emotional intelligence of medical students of Shiraz University of Medical Sciences cross sectional study. Annals of Medicine and Surgery, 32, 26–31. https://doi.org/10.1016/j.amsu.2018.07.005
Völker, J. (2020). An examination of ability emotional intelligence and its relationships with fluid and crystallized abilities in a student sample. Journal of Intelligence, 8(2), 18. https://doi.org/10.3390/jintelligence8020018
Wei, P., & Joseph, A. (2011). Implementing and evaluating the integration of critical thinking into problem based learning in environmental building. Journal for Education in the Built Environment, 6(2), 93-115. https://doi.org/10.11120/jebe.2011.06020093
Wijekoon, C. N., Amaratunge, H., de Silva, Y., Senanayake, S., Jayawardane, P., & Senarath, U. (2017). Emotional intelligence and academic performance of medical undergraduates: A cross-sectional study in a selected university in Sri Lanka. BMC Medical Education, 17(1), Article 176. https://doi.org/10.1186/s12909-017-1018-9
Yee, K. T., Yi, M. S., Aung, K. C., Lwin, M. M., & Myint, W. W. (2018). Emotional intelligence level of year one and two medical students of University Malaysia Sarawak: Association with demographic data. Malaysian Applied Biology, 47(1), 203-208.
*Edussuriya D.H
Department of Forensic Medicine, Faculty of Medicine,
University of Peradeniya, Sri Lanka, 20400
+94711698916
Email: deepthi.edussuriya@med.pdn.ac.lk
Submitted: 19 May 2021
Accepted: 7 October 2021
Published online: 4 January, TAPS 2022, 7(1), 21-32
https://doi.org/10.29060/TAPS.2022-7-1/RA2537
Kirsty J Freeman1, Sandra E Carr2, Brid Phillips2, Farah Noya3 & Debra Nestel4,5
1Office of Education, Duke NUS Medical School, Singapore, Singapore; 2Division of Health Professions Education, The University of Western Australia, Perth, Australia; 3Faculty of Medicine, Pattimura University, Ambon, Indonesia; 4School of Clinical Sciences, Monash University, Clayton, Australia; 5Austin Precinct, Department of Surgery, University of Melbourne, Heidelberg, Australia
Abstract
Introduction: As healthcare educators undergo a career transition from providing care to providing education, their professional identity can also transition accompanied by significant threat. Given their qualifications are usually clinical in nature, healthcare educators’ knowledge and skills in education and other relevant theories are often minimal, making them vulnerable to feeling fraudulent in the healthcare educator role. This threat and vulnerability is described as the impostor phenomenon. The aim of this study was to examine and map the concepts of professional identity and the influence of impostor phenomenon in healthcare educators.
Methods: The authors conducted a scoping review of health professions literature. Six databases were searched, identifying 121 relevant articles, eight meeting our inclusion criteria. Two researchers independently extracted data, collating and summarising the results.
Results: Clinicians who become healthcare educators experience identity ambiguity. Gaps exist in the incidence and influence of impostor phenomenon in healthcare educators. Creating communities of practice, where opportunities exist for formal and informal interactions with both peers and experts, has a positive impact on professional identity construction. Faculty development activities that incorporate the beliefs, values and attributes of the professional role of a healthcare educator can be effective in establishing a new professional identity.
Conclusion: This review describes the professional identity ambiguity experienced by clinicians as they take on the role of healthcare educator and solutions to ensure a sustainable healthcare education workforce.
Keywords: Professional Identity, Impostor Phenomenon, Healthcare Educators, Health Professions Education, Scoping Review
Practice Highlights
- Professional identity ambiguity experienced when a clinician transitions to the role of healthcare educator is understudied relative to other professions.
- Professional identity ambiguity experienced when a clinician transitions to the role of healthcare educator is understudied relative to other professions.
- Creating communities of practice, whereby healthcare educators can interact with peers and experts, in both formal and informal settings, has a positive impact on professional identity construction.
- Faculty development activities that incorporate the beliefs, values and attributes of the professional role of a healthcare educator are effective in establishing a new professional identity or aligning multiple professional identities.
I. INTRODUCTION
Educating the current and future healthcare workforce relies on clinicians sharing their knowledge, skills and experience by teaching others. Some clinicians have a passion to educate and seek out this role. For others it is often their high level of clinical expertise that results in requests to take on an education role. This may result in an expansion of their current role as a clinician, or a transition from one role to another. There are many terms used to describe those teaching in healthcare including educator, teacher, and faculty. The term healthcare educators is used throughout this paper to describe clinicians educating in any environment. Changes in work roles can pose a threat to an individual’s identity (Barbulescu & Ibarra, 2008; Becker & Carper, 1956), as this requires the individual to develop a new sense of self (Conroy & O’Leary-Kelly, 2014). With this change in role comes a transition in professional identity.
Professional identity is defined as “the relatively stable and enduring constellation of attributes, beliefs, values, motives, and experiences in terms of which people define themselves in a professional role” (Ibarra, 1999, pp. 764). The formation of professional identity is centred on how an individual perceives themselves as a professional, their relationship with the profession, and how their knowledge, skills and attitudes align with the norms and culture of that profession (Sethi et al., 2018). Within healthcare there has been a call for professional identity formation to be explicitly addressed in the curriculum of future healthcare professionals, addressing both what it is to think, act and feel like a healthcare professional, and the processes by which that identity is formed (Cruess et al., 2019).
Individuals manage numerous identities during their lifespan, across personal, vocational, social and professional spheres. Van Gennep’s theory of rites of passage, where-by an individual transitions through three phases 1) ‘separation’ – letting go of the old self, 2) ‘liminality’ – middle phase, and 3) ‘aggregation’ – establishing a new identity, has been cited in the literature to describe career transition and formation of a new identity (Kulkarni, 2019; Mayrhofer & Iellatchitch, 2005; Petersen, 2017). It is in this middle phase of liminality where a clinician taking on the role of a healthcare educator may experience identity ambiguity. Given that literature from other industries show that professional identity can influence job satisfaction, feelings of accomplishment, and employment retention (Canrinus et al., 2012; Hutchins et al., 2018), it is essential that the formation of professional identity and potential identity ambiguity in healthcare educators is examined.
The term impostor phenomenon, also known as impostor syndrome, is used to describe negative feelings an individual experiences, despite achieving a level of competence, and the fear of being ‘found out’ by those around them (Clark et al., 2014). The concept of being exposed as a ‘fraud’ was coined impostor phenomenon by clinical psychologists Clance and Imes (1978). Literature suggests that despite external evidence of their competence, those exhibiting the phenomenon remain convinced that they are frauds and do not deserve the success they have achieved (Leonhardt et al., 2017; Neureiter & Traut-Mattausch, 2016; Vergauwe et al., 2015).
In their seminal work from the late 1970’s, Clance and Imes (1978) reported that impostor phenomenon is more prevalent in specific female populations. Recent studies however have shown that impostor phenomenon impacts individual regardless of gender, and occurs in a variety of contexts (Bernard et al., 2018; Chae et al., 1995). Prominent among high performing individuals, impostor phenomenon is experienced on a continuum from the occasional concern that the individual is not up to the task, to an extreme fear of being ‘found out’ as a fraud (Hibberd, 2019). Studies suggest that impostor phenomenon can have significant negative effects including an increase in work-family conflict (Crawford et al., 2016), and decreased job satisfaction (Cowman & Ferrari, 2002), with studies also reporting a link between impostor phenomenon and burnout (Villwock et al., 2016).
With impostor phenomenon well described in professions outside of healthcare, most literature published on impostor phenomenon within the healthcare professions has focused on students transitioning from study to the workplace (Aubeeluck et al., 2016; Dudău, 2014; Robinson-Walker, 2011), with very few studies examining current working professionals (Gottlieb et al., 2019; Hutchins et al., 2018). The aim of this study was to examine and map the concepts of professional identity and implications of impostor phenomenon in healthcare educators. By furthering our understanding of impostor phenomenon in healthcare educators and how it impacts professional identity, both individuals and organisations will be able to implement strategies that will assist in the development of a sustainable healthcare education workforce, addressing workforce capability, capacity, resilience and culture.
II. METHODS
The aim of a scoping review is to examine evidence, identify gaps in the literature, and clarify key concepts (The Joanna Briggs Institute, 2017). The objective of this scoping review is to examine and map the concepts of professional identity and impostor phenomenon in healthcare educators.
A. Review Questions
The primary review question was ‘how is professional identity and impostor phenomenon described in the literature about healthcare educators?’, with the secondary review question being ‘how is professional identity of healthcare educators influenced by imposter phenomenon?’. Tricco et al. (2016) identified 25 knowledge synthesis methods used across the health fields. We selected a scoping review methodology as it is the most appropriate to address our aim to map and summarise the literature, clarify working definitions and identify gaps. The framework that will guide the process is the five-step approach proposed by Arksey and O’Malley (2005). The steps are 1) identify the research question; 2) identify the relevant articles; 3) select the articles; 4) chart the data; and 5) collate and summarise the results.
B. Identifying Relevant Articles
Adopting the population, concept, and context (PCC) framework (Peters et al., 2020) informed the development of the search strategy as demonstrated in Table 1.
|
|
Main concepts |
|
|
|
|||
|
|
Population |
Concept 1 |
Concept 2 |
Context |
|||
|
|
Healthcare educators |
Professional identity |
Impostor phenomenon |
Healthcare education |
|||
|
Search Terms |
“healthcare educator.ti,ab,kw.” “nursing educator.ti,ab,kw.” “medical educator.ti,ab,kw.” “allied health educator.ti,ab,kw” “faculty.ti,ab,kw.” “facilitator.ti,ab,kw.” “educator.ti,ab,kw.” “*faculty, medical/ or *faculty, nursing/ or *health educators/” “clinical educator.ti,ab,kw.” “clinical teacher.ti,ab,kw.” |
“Professional identity.ti,ab,kw.” “Professional role*.ti,ab,kw.” “Professional competence.ti,ab,kw.” “Professional sociali*ation.ti,ab,kw.” “Professional identity formation.ti,ab,kw.” “*Professional Competence/” “*Professional Role/” “*Professionalism/” |
“impostor.ti,ab,kw.” “imposter.ti,ab,kw.” “fraud.ti,ab,kw.” “fake.ti,ab,kw.” “impost*rism.ti,ab,kw.” “intellectual fraud*.ti,ab,kw.” “(impost*r adj3 syndrome).ti,ab,kw.” “(impost*r adj3 phenomenon).ti,ab,kw.” “*Adaptation, Psychological/” “*Self Concept/” “*social identification/” “Self concept.ti,ab,kw.” |
“education, medical/ or *education, medical, continuing/ or *education, medical, graduate/ or *education, medical, undergraduate/” “*Education, Nursing/” “*Education, Allied Health/” “*Education, Clinical/” “education, medical/ or education, nursing/ or education, pharmacy/ or education, public health professional/” |
|||
Table 1: Key search terms
Note: ti = title; ab = abstract; kw = keyword
To identify potentially relevant articles, a literature search of six online databases was conducted on the November 6, 2020. These included MEDLINE, EMBASE, Joanna Briggs Institute EBP Database, CINAHL, PsycINFO, and ERIC. The search strategies were drafted in collaboration with an experienced librarian and further refined by the researchers. The search strategy conducted in MEDLINE is detailed in Table 2. The final search results were exported into Covidence systematic review software, a screening and data extraction tool (Covidence Systematic Review Software, 2019).
|
# |
Searches |
Results |
|
1 |
healthcare educator.ti,ab,kw. |
5 |
|
2 |
nursing educator.ti,ab,kw. |
51 |
|
3 |
medical educator.ti,ab,kw. |
164 |
|
4 |
allied health educator.ti,ab,kw. |
7 |
|
5 |
faculty.ti,ab,kw. |
46912 |
|
6 |
facilitator.ti,ab,kw. |
6518 |
|
7 |
educator.ti,ab,kw. |
5586 |
|
8 |
*faculty, medical/ or *faculty, nursing/ or *health educators/ |
14624 |
|
9 |
clinical educator.ti,ab,kw. |
119 |
|
10 |
clinical teacher.ti,ab,kw. |
279 |
|
11 |
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 |
66130 |
|
12 |
Professional identity.ti,ab,kw. |
1917 |
|
13 |
Professional role*.ti,ab,kw. |
2643 |
|
14 |
Professional competence.ti,ab,kw. |
1267 |
|
15 |
Professional sociali*ation.ti,ab,kw. |
376 |
|
16 |
Professional identity formation.ti,ab,kw. |
241 |
|
17 |
*Professional Competence/ |
11751 |
|
18 |
*Professional Role/ |
6495 |
|
19 |
*Professionalism/ |
836 |
|
20 |
12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 |
24196 |
|
21 |
impostor.ti,ab,kw. |
169 |
|
22 |
imposter.ti,ab,kw. |
148 |
|
23 |
fraud.ti,ab,kw. |
4102 |
|
24 |
fake.ti,ab,kw. |
1772 |
|
25 |
impost*rism.ti,ab,kw. |
16 |
|
26 |
intellectual fraud*.ti,ab,kw. |
7 |
|
27 |
(impost*r adj3 syndrome).ti,ab,kw. |
57 |
|
28 |
(impost*r adj3 phenomenon).ti,ab,kw. |
63 |
|
29 |
*Adaptation, Psychological/ |
43405 |
|
30 |
*Self Concept/ |
25641 |
|
31 |
*social identification/ |
5255 |
|
32 |
Self concept.ti,ab,kw. |
5240 |
|
33 |
21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 |
80945 |
|
34 |
20 and 33 |
597 |
|
35 |
education, medical/ or *education, medical, continuing/ or *education, medical, graduate/ or *education, medical, undergraduate/ |
108815 |
|
36 |
*Education, Nursing/ |
24454 |
|
37 |
*Education, Allied Health/ |
0 |
|
38 |
*Education, Clinical/ |
0 |
|
39 |
education, medical/ or education, nursing/ or education, pharmacy/ or education, public health professional/ |
96076 |
|
40 |
35 or 36 or 37 or 38 or 39 |
147396 |
|
41 |
11 and 34 and 40 |
17 |
Table 2: Search strategy conducted in Ovid MEDLINE on November 6, 2020
C. Eligibility Criteria
To be eligible for inclusion in the study, articles were required to satisfy the following criteria:
1. Population: This scoping review will consider literature that included educators within the healthcare context. Educators can include those of any age, gender, culture or geography.
2. Concept: There are two concepts that will be examined in this review, transition in professional identity and impostor phenomenon. This review will include the definition of the concepts, the theoretical, conceptual and the measurement of both concepts.
3. Context: This review will consider literature written in English, from any healthcare context with no restrictions on geographical location, or cultural factors.
D. Selection of Articles
One hundred and twenty-one articles were collated and citations, title and abstract were retrieved. An initial check identified one duplicate, which was removed. Titles and abstracts of the 120 articles were screened by three independent reviewers (KF, FN, BP) for assessment against the inclusion criteria for the review. Thirty-three articles were found to meet the inclusion criteria and progressed to full text review. Two researchers (KF, BP) conducted a full text review, recording reasons for exclusion. Disagreements were resolved through discussion, and consensus. Based on the Joanna Briggs Institute recommendations on scoping review methods, no critical appraisal of methodological quality was undertaken (The Joanna Briggs Institute, 2017).
E. Charting the Data
A data-charting form to determine which data to extract was jointly developed by two researchers (KF, SC). Two researchers (KF, BP) independently charted the data, then discussed the results and edited the data-charting form as required. A third researcher (FN) verified the data.
F. Collating, Summarising and Reporting the Data
Data was abstracted on article characteristics including country of publication, population of interest, study aim, sample size, study design, data collection methods, and findings related to the concepts of professional identity and impostor phenomenon.
III. RESULTS
One hundred and twenty-one abstracts were identified from six databases, 33 full text articles were reviewed, and 8 full text articles were analysed (See Figure 1). Of the included articles five were conducted in the USA (Cranmer et al., 2018; Heinrich, 1997; O’Sullivan & Irby, 2014; Stone et al., 2002; Talisman et al., 2015), and one in each of Australia (Higgs & McAllister, 2007), Canada (Lieff et al., 2012), and the United Kingdom (Andrew et al., 2009) (Table 3). In relation to the population of healthcare educators, four articles involved those working in medicine (Cranmer et al., 2018; O’Sullivan & Irby, 2014; Stone et al., 2002; Talisman et al., 2015), two in nursing (Andrew et al., 2009; Heinrich, 1997), one in speech pathology (Higgs & McAllister, 2007), and one involving healthcare educators from multiple professions (Lieff et al., 2012). Five studies adopted a qualitative approach, such as interviews or narrative responses, (Andrew et al., 2009; Higgs & McAllister, 2007; Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002), one employing a quantitative approach (Cranmer et al., 2018), one mixed methods (Talisman et al., 2015), and one article was a program description (Heinrich, 1997).

Figure 1: PRISMA flow diagram
|
Article |
Country |
Population |
Study aim |
Sample size (n) |
Study design |
Data collection method |
Findings |
|
Andrew et al. (2009) |
UK |
Nursing |
To explore online communities for novice educators to develop professional identity |
14 |
Qualitative content analysis |
Web blog |
Communities of practice can help in the development of professional identity |
|
Talisman et al. (2015) |
USA |
Medicine |
To explore the impact of teaching the mind-body medicine course on course facilitator’s professional identity |
50 |
Mixed Methods cross sectional design |
Survey including the FMI & PSS tools, & open-ended questions |
Participation as a facilitator in a mind-body medicine program has tangible positive outcomes for the professional identity of facilitators through improved communication, connection, empathy, and self-confidence. |
|
Stone et al. (2002) |
USA |
Medicine |
To examine factors that preceptors perceive as important to their identity as teachers |
10 |
Qualitative |
Semi-structured interviews |
Preceptors associate strong feelings with their identity as teacher. Four aspects of teacher identity are as follows: humanitarianism; adult learning principles; benefits and drawbacks, and image of self as teacher. Teacher identity was not associated with student learning. Faculty development can foster preceptor identity as teacher. |
|
O’Sullivan and Irby (2014) |
USA |
Medicine |
To examine identity formation of part time faculty developers |
29 |
Qualitative |
Semi-structured interviews |
Professional identity is fluid, and evolves over time. Faculty development, particularly developing others has a direct impact on this. |
|
Lieff et al. (2012) |
Canada |
Multiple professions |
To understand the factors that relate to the formation and growth of academic identity |
43 |
Qualitative case study approach |
Reflective paper and focus groups |
Academic identity formation is influenced by personal, relational and contextual factors, and that this identity the motivation, satisfaction, and productivity of health professional educators. |
|
Higgs and McAllister (2007) |
Australia |
Speech Pathology |
To examine the preparation and professional development of clinical educators based on research into the experiences of being a clinical educator |
5 |
Qualitative approach using hermeneutic phenomenology and narrative inquiry |
Interviews |
The model of The Experience of Being a Clinical Educator, emphasising six dimensions: a sense of self, of self-identity; a sense of relationship with others; a sense of being a clinical educator; a sense of agency or purposeful action; dynamic self-congruence; and the experience of growth and change, can be used as the basis for helping clinical educators to reflect on what it means to be a clinical educator Faculty development activities that include reflective strategies can assist the educator transition from novice to expert. |
|
Heinrich (1997) |
USA |
Nursing |
To describe an educational interventional designed to assist nurses who experience impostor phenomenon as they negotiate professional transitions |
Not stated |
Program description |
Faculty/author observation |
Impostor phenomenon is prevalent among nurses as they negotiate professional identity transformation, and that the use of metaphors in faculty development programs can be effective in aiding this transition. |
|
Cranmer et al. (2018) |
USA |
Medicine |
To describe the impact of a faculty mentoring program on the retention, promotion and professional fulfilment of junior faculty members |
23 |
Quantitative |
Survey |
Participation in a mentoring program has a positive effect on confidence, self-efficacy and skills, and that participation can assist new academic s develop their academic role and achieve professional fulfilment by fostering strong collegial and social relationships, ultimately leading to career satisfaction. |
Table 3. Summary of extracted data from the included articles
Articles identified several key influences when describing the professional identity of healthcare educators (Figure 2). Seven articles describe the healthcare educator’s interaction with others as having a positive influence on professional identity (Andrew et al., 2009; Heinrich, 1997; Higgs & McAllister, 2007; Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002; Talisman et al., 2015). Interactions with peers was identified as being key to clinicians successfully adopting an educator professional identity. One study found that by providing opportunities for informal discussions and social interactions amongst peers, healthcare educators reported a sense of belonging which was found to be essential in identity formation (Lieff et al., 2012). These findings were supported by Andrew et al. (2009) who found that online communities of practice were effective in supporting new educators in developing their professional identity.
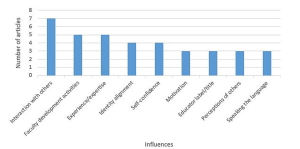
Figure 2. Key influences of professional identity
Interactions between the novice and expert educators were reported to have both a positive and negative influence on healthcare educators as they construct their educator identity. Two studies described the positive impact of formal mentoring programs, one as a means of maintaining a link to their clinical identity (Andrew et al., 2009), and the other as a tool to successfully negotiate the role transition (Cranmer et al., 2018). Lieff et al. (2012) reported that whilst certain individuals are motivated by experts, seeing them as role models, others were intimidated, discouraged, and overwhelmed by the interaction with the expert. Comparing oneself to others has the potential to reinforce or inhibit the development of the healthcare educator identity (Lieff et al., 2012).
The role of faculty development activities on educator professional identity was reported by five studies (Cranmer et al., 2018; Heinrich, 1997; Higgs & McAllister, 2007; Lieff et al., 2012; Stone et al., 2002). Three studies recommended that faculty development programs include content on fostering the development of identity as a healthcare educator (Higgs & McAllister, 2007; O’Sullivan & Irby, 2014; Stone et al., 2002). One study recommended using faculty development activities to remind clinicians of their existing role as educators to patients as a means of increasing their confidence and enhance educator identity (Stone et al., 2002). Another study identified the importance of faculty development programs in facilitating interactions with other healthcare educators with varying levels of expertise, that foster a sense of belonging (Lieff et al., 2012).
The perceptions of others was found to have an influence on professional identity (Andrew et al., 2009; Lieff et al., 2012; O’Sullivan & Irby, 2014). One study reported that an evolving identity can be strengthened when the educator was seen by others as an educator, validating the new identity. The opposite was also found to be true where the perceptions of others that one is an educator could place a high level of anxiety on the emerging identity not yet fully embraced (Lieff et al., 2012). The influence which holding the title of healthcare educator had on an emerging identity is also linked to the perceptions of others. When labelled and referred to by others as an educator two studies found that professional identity as an educator was reinforced (Lieff et al., 2012; Stone et al., 2002).
Three studies found that the ability to learn and speak the language of the healthcare educator influenced how individuals developed their professional identity (Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002). O’Sullivan and Irby (2014) found that sharing a common healthcare educator language increased deeper relationship between educators, with Lieff et al. (2012) reporting that acquiring the right language provided credibility and legitimacy. A strong sense of professional identity was linked to motivation to educate, with one study suggesting that a desire to teach correlated with satisfaction in the role (Stone et al., 2002).
Aspects of identity alignment was found to be key in a healthcare educator’s professional identity formation (Andrew et al., 2009; Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002). One study of novice nurse educators described the tension experienced when managing the dual identities of clinician and educator, and the stress that maintaining dual roles places on these nurses (Andrew et al., 2009). Another study looking at multiple healthcare professions highlighted this struggle, with participants facing the dilemma of how they can excel in both identities simultaneously (Lieff et al., 2012). Exploring physician educators, the study by Stone et al. (2002) found that the identities of clinician and educator were interwoven.
Four studies reported that as self-confidence developed so too did professional identity (Cranmer et al., 2018; Heinrich, 1997; Lieff et al., 2012; Talisman et al., 2015). Data from the study by Lieff et al. (2012) revealed that just as self-confidence ebbed and flowed during a healthcare educator’s role transition, so too did their identity, resulting in feeling like an impostor. Talisman et al. (2015) found that as self-confidence grew fear of rejection by colleagues became less, and that self-confidence in ones’ professional identity opened up opportunities to develop as a healthcare educator.
Only one study (Heinrich, 1997) made specific reference to the concept of impostor phenomenon, describing an educational program using metaphors as a corrective tool for those who experience feeling like a fraud. The authors do not provide any data on the prevalence of impostor phenomenon in the population of healthcare educators, nor do they provide any results on the impact of the educational program described.
IV. DISCUSSION
Healthcare educators manage multiple identities, from social and cultural, to gender and religious, however professional identity tends to contribute a large part of an individual’s overall identity. A change in professional identity brings with it inconsistencies between the old and the new, producing anxiety and discomfort, as the individual navigates this transition phase through which identity is reconstructed (Beech, 2010). In answering the review question, ‘How is professional identity and impostor phenomenon described in the literature about healthcare educators?’ the findings indicate that in relation to professional identity, clinicians who become educators experience identity ambiguity, in line with the theory of rites of passage described by Van Gennep (Kulkarni, 2019; Petersen, 2017). Characteristics of impostor phenomenon include anxiety, lack of self-confidence, depression, and frustration (Heinrich, 1997; Hibberd, 2019). While the literature describes the experiences of healthcare educators as they strive to solidify their professional identities, this review suggests that despite impostor phenomenon being described since the 1970’s, the reporting of the phenomenon in the healthcare literature has only occurred in recent years, impostor phenomenon is not being measured amongst healthcare educators.
For the secondary question in this review ‘How is professional identity of healthcare educators influenced by imposter phenomenon?’ we found that there are key influences (Figure 2) that can be harnessed, through faculty development activities, to assist individual’s transition to Van Gennep’s third phase, aggregation, which is the final step in transitioning to a new career and establishing a new professional identity.
Creating opportunities for interactions with others, both peers and experts, through formal and informal interactions, has a positive impact on professional identity construction (Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002). A community of practice has been described as a collection of individuals who have a shared interest and who wish to deepen their knowledge, where participation provides members an opportunity to learn from one another (Wenger, 2010). The opportunity to engage in a community of practice enables the novice healthcare educator to construct their identity by comparing themselves with others, “boosting their confidence and solidifying their identities as educators” (Lieff et al., 2012; Wenger, 2010).
Communities of practice have been used in the healthcare sector in a variety of forms and with varying purposes (Dickinson et al., 2020; Ranmuthugala et al., 2011). Elements of social cognitive theory (Bandura, 1986) and social comparison theory (Bonifield & Cole, 2008) underpin the outcomes that result from participating in a community of practice, whereby members learn through observing the behaviour of others. If the purpose of a community of practice is to assist in professional identity formation, membership needs to be carefully cultivated as the findings of this study acknowledge the potential negative influence ‘experts’ can have, as other members compare themselves, possibly viewing themselves as inadequate (Lieff et al., 2012).
The formation of single-disciplinary communities of practice should be considered given that this study has revealed healthcare educators from nursing and medicine experience their identity alignment differently. Nurses were reported as struggling with managing the dual identities of clinician and educator (Andrew et al., 2009), whereas the physicians viewed them as interwoven (Stone et al., 2002).
Faculty development activities traditionally focus on providing healthcare educators with the knowledge and skill required to perform a new role. Adopting a new professional identity as a healthcare educator involves more than acquiring new skills, but also new behaviours and attitudes (Ibarra, 1999). The findings of this review support the addition of a specific focus on fostering professional identity as part of any faculty development program for new healthcare educators (O’Sullivan et al., 2021). Such inclusions to faculty development activities could be used to emphasize the skills that clinicians have as educators, skills that are transferable to their role in teaching emerging or current clinicians (Stone et al., 2002).
This review has revealed the tension that healthcare educators may experience as they transition from one professional identity to another, as well as the struggles in balancing dual identities. The impact of this identity misalignment on the individual could result in levels of stress that see the individual reverting to their clinical professional identity and withdrawing from the healthcare educator workforce. Healthcare training organisations need to ensure that strategies such as developing communities of practice and faculty development activities are engaged to support healthcare educators on their rite of passage to developing their healthcare educator identity.
Whilst several tools to measure impostor phenomenon exist, including the Clance Impostor Phenomenon Scale (CIPS), Harvey Impostor Scale, Perceived Fraudulence Scale and Leary Impostor Scale, Mak et al. (2019) report that no scales have been validated for use with healthcare educators, a finding supported by this review.
Our findings indicate a paucity of articles on the influence of impostor phenomenon on healthcare educators as they align their clinical and educator identities. This review has described the influences on professional identity that can be harnessed to address identity ambiguity, resulting in improved job satisfaction, employment retention, ensuring a sustainable healthcare education workforce.
A. Limitations of the Review
Six databases across health and education were included; it is possible that additional articles may have been identified if different databases were searched. We did not comprehensively search the gray literature beyond conference abstracts, protocols, and dissertations. By limiting our coverage of articles only published in English we may have missed important studies published in other languages, potentially resulting in a regional bias. As no critical appraisal of methodological quality was undertaken the reliability of some findings may be limited. With the ever-changing use of language the search terms selected related to the concepts of professional identity and impostor phenomenon may not be exhaustive.
V. CONCLUSION
The influence of impostor phenomenon on the professional identity alignment in healthcare educators has the potential to negatively impact the education of the current and future healthcare workforce. This review is a starting point for individuals and organisations involved in health professions education, and faculty development. It offers insight to the under examined understudied but potentially important prevalence and impact of impostor phenomenon in healthcare educators and the professional identity ambiguity experienced by clinicians as they take on the role of healthcare educator. This review highlights the need for further research into the prevalence of impostor phenomenon in healthcare educators across different settings, as well as exploring the experience and influence of impostor phenomenon on professional identity.
Notes on Contributors
KF led the design and conceptualisation of this work, drafted the protocol, developed the search strategy, and conducted the search, data extraction, analysis, discussion and conclusion. SC and DN were involved in the conceptualisation of the review design, specifically in establishing the review question as well as the inclusion and exclusion criteria, provided feedback on the manuscript. BP, FN and SC guided the conceptualisation and design of the study and participated in data analyses and have revised all drafts of the manuscript. All authors approve the publishing of this manuscript.
Ethical Approval
Ethics approval was granted by The University of Western Australia Human Research Ethics Committee: RA/4/20/5061.
Data Availability
All relevant quantitative data are within the manuscript.
Acknowledgement
The authors would like to acknowledge Terena Solomons, Faculty Librarian, for her support and guidance in the development of the search strategy.
Funding
This work has not received any external funding.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Andrew, N., Ferguson, D., Wilkie, G., Corcoran, T., & Simpson, L. (2009). Developing professional identity in nursing academics: The role of communities of practice. Nurse Education Today, 29(6), 607-611. https://doi.org/https://dx.doi.org/10.1016/j.nedt.2009.01.012
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methods, 8, 19-32. https://doi.org/10.1080/136455703200011961
Aubeeluck, A., Stacey, G., & Stupple, E. J. N. (2016). Do graduate entry nursing student’s experience ‘Imposter Phenomenon’?: An issue for debate. Nurse Education in Practice, 19, 104-106. https://doi.org/https://doi.org/10.1016/j.nepr.2016.06.003
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Prentice-Hall.
Barbulescu, R., & Ibarra, H. (2008). Identity as narrative: Overcoming identity gaps during work role transitions. INSEAD Working Papers Collection, 27, 1-39.
Becker, H. S., & Carper, J. W. (1956). The development of identification with an occupation. The American Journal of Sociology, 61(4), 289-298. https://doi.org/10.1086/221759
Beech, N. (2010). Liminality and the practices of identity reconstruction. Human relations (New York), 64(2), 285-302. https://doi.org/10.1177/0018726710371235
Bernard, D. L., Hoggard, L. S., & Neblett, E. W. (2018). Racial discrimination, racial identity, and impostor phenomenon: A profile approach. Cultural Diversity and Ethnic Minority Psychology, 24(1), 51-61. https://doi.org/10.1037/cdp0000161
Bonifield, C., & Cole, C. A. (2008). Better him than me: Social comparison theory and service recovery. Journal of The Academy of Marketing Science, 36(4), 565-577. https://doi.org/10.1007/s11747-008-0109-x
Canrinus, E. T., Helms-Lorenz, M., Beijaard, D., Buitink, J., & Hofman, A. (2012). Self-efficacy, job satisfaction, motivation and commitment: Exploring the relationships between indicators of teachers’ professional identity. European Journal of Psychology of Education, 27(1), 115-132. https://doi.org/10.1007/s10212-011-0069-2
Chae, J. H., Piedmont, R. L., Estadt, B. K., & Wicks, R. J. (1995). Personological evaluation of Clance’s imposter phenomenon scale in a Korean sample. Journal of personality assessment, 65(3), 468-485. https://doi.org/10.1207/s15327752jpa6503_
Clance, P. R., & Imes, S. A. (1978). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention. Psychotherapy, 15(3), 241-247. https://doi.org/10.1037/h0086006
Clark, M., Vardeman, K., & Barba, S. (2014). Perceived inadequacy: A study of impostor phenomenon among college and research librarians. College & Research Libraries, 75(3), 255-271. https://doi.org/10.5860/crl12-423
Conroy, S. A., & O’Leary-Kelly, A. M. (2014). Letting go and moving on: Work-related identity loss and recovery. The Academy of Management review, 39(1), 67-87. https://doi.org/10.5465/amr.2011.0396
Covidence Systematic Review Software. (2019). Veritas Health Innovation. https://covidence.org
Cowman, S. E., & Ferrari, J. R. (2002). “Am I for real?” Predicting impostor tendencies from self-handicapping and affective components. Social Behavior and Personality, 30(2), 119-125. https://doi.org/10.2224/sbp.2002.30.2.119
Cranmer, J. M., Scurlock, A. M., Hale, R. B., Ward, W. L., Prodhan, P., Weber, J. L., Casey, P. H., & Jacobs, R. F. (2018). An adaptable pediatrics faculty mentoring model. Pediatrics, 141(5), Article e20173202. https://doi.org/10.1542/peds.2017-3202
Crawford, W. S., Shanine, K. K., Whitman, M. V., & Kacmar, K. M. (2016). Examining the impostor phenomenon and work–family conflict. Journal of Managerial Psychology, 31(2), 375-390. https://doi.org/10.1108/JMP-12-2013-0409
Cruess, S. R., Cruess, R. L., & Steinert, Y. (2019). Supporting the development of a professional identity: General principles. Medical Teacher, 41(6), 641-649. https://doi.org/10.1080/0142159X.2018.153626
Dickinson, B., Chen, Z. X., & Haramati, A. (2020). Supporting medical science educators: A matter of self-esteem, identity, and promotion opportunities. The Asia Pacific Scholar, 5(3), 1-4. https://doi.org/10.29060/TAPS.2020-5-3/PV2164
Dudău, D. P. (2014). The relation between perfectionism and impostor phenomenon. Procedia – Social and Behavioral Sciences, 127, 129-133. https://doi.org/10.1016/j.sbspro.2014.03.226
Gottlieb, M., Chung, A., Battaglioli, N., Sebok‐Syer, S. S., & Kalantari, A. (2019). Impostor syndrome among physicians and physicians in training: A scoping review. Medical Education, 54(2), 116-124. https://doi.org/10.1111/medu.13956
Heinrich, K. T. (1997). Transforming impostors into heroes. Metaphors for innovative nursing education. Nurse educator, 22(3), 45-50. https://doi.org/10.1097/00006223-199705000-00018
Hibberd, J. (2019). The Imposter Cure: How to stop feeling like a fraud and escape the mind-trap of imposter syndrome. Aster.
Higgs, J., & McAllister, L. (2007). Educating clinical educators: Using a model of the experience of being a clinical educator. Medical Teacher, 29(2-3), e51-e57. https://doi.org/10.1080/01421590601046088
Hutchins, H. M., Penney, L. M., & Sublett, L. W. (2018). What imposters risk at work: Exploring imposter phenomenon, stress coping, and job outcomes. Human Resource Development Quarterly, 29(1), 31-48. https://doi.org/10.1002/hrdq.21304
Ibarra, H. (1999). Provisional selves: Experimenting with image and identity in professional adaptation. Administrative Science Quarterly, 44(4), 764-791. https://doi.org/10.2307/2667055
Kulkarni, M. (2019). Holding on to let go: Identity work in discontinuous and involuntary career transitions. Human Relations, 73(10), 1415-1438. https://doi.org/10.1177/0018726719871087
Leonhardt, M., Bechtoldt, M. N., & Rohrmann, S. (2017). All impostors aren’t alike – Differentiating the impostor phenomenon. Frontiers in Psychology, 8, 1505. https://doi.org/10.3389/fpsyg.2017.01505
Lieff, S., Baker, L., Mori, B., Egan-Lee, E., Chin, K., & Reeves, S. (2012). Who am I? Key influences on the formation of academic identity within a faculty development program. Medical Teacher, 34(3), e208-215. https://doi.org/10.3109/0142159x.2012.642827
Mak, K. K. L., Kleitman, S., & Abbott, M. J. (2019). Impostor phenomenon measurement scales: A systematic review. Frontiers in Psychology, 10, 671. https://doi.org/10.3389/fpsyg.2019.00671
Mayrhofer, W., & Iellatchitch, A. (2005). Rites, right? The value of rites de passage for dealing with today’s career transitions. Career Development International, 10(1), 52-66. https://doi.org/10.1108/13620430510577628
Neureiter, M., & Traut-Mattausch, E. (2016). Inspecting the dangers of feeling like a fake: An empirical investigation of the impostor phenomenon in the world of work. Frontiers in Psychology, 7, 1445. https://doi.org/10.3389/fpsyg.2016.01445
O’Sullivan, P. S., & Irby, D. M. (2014). Identity formation of occasional faculty developers in medical education: A qualitative study. Academic Medicine, 89(11), 1467-1473. https://doi.org/10.1097/ACM.0000000000000374
O’Sullivan, P. S., Steinert, Y., & Irby, D. M. (2021). A faculty development workshop to support educator identity formation. Medical Teacher, 43(8), 916-917. https://doi.org/10.1080/0142159X.2021.1921135
Peters, M. D. J., Godfrey, C., McInerney, P., Munn, Z., Tricco, A. C., & Khalil, H. (2020). Scoping Reviews. In E. Aromataris., & Z. Munn (Eds.), JBI Manual for Evidence Synthesis, JBI. https://doi.org/10.46658/JBIMES-20-12
Petersen, N. (2017). The liminality of new foundation phase teachers: Transitioning from university into the teaching profession. South African Journal of Education, 37(2), 1-9. https://doi.org/10.15700/saje.v37n2a1361
Ranmuthugala, G., Plumb, J. J., Cunningham, F. C., Georgiou, A., Westbrook, J. I., & Braithwaite, J. (2011). How and why are communities of practice established in the healthcare sector? A systematic review of the literature. BMC Health Services Research, 11, 273. https://doi.org/10.1186/1472-6963-11-273
Robinson-Walker, C. (2011). The imposter syndrome. Nurse Leader, 9(4), 12-13. https://doi.org/https://doi.org/10.1016/j.mnl.2011.05.003
Sethi, A., Schofield, S., McAleer, S., & Ajjawi, R. (2018). The influence of postgraduate qualifications on educational identity formation of healthcare professionals. Advances in Health Sciences Education, 23(3), 567-585. https://doi.org/10.1007/s10459-018-9814-5
Stone, S., Ellers, B., Holmes, D., Orgren, R., Qualters, D., & Thompson, J. (2002). Identifying oneself as a teacher: The perceptions of preceptors. Medical Education, 36(2), 180-185. https://doi.org/10.1046/j.1365-2923.2002.01064.x
Talisman, N., Harazduk, N., Rush, C., Graves, K., & Haramati, A. (2015). The impact of mind-body medicine facilitation on affirming and enhancing professional identity in health care professions faculty. Academic Medicine, 90(6), 780-784. https://doi.org/10.1097/acm.0000000000000720
The Joanna Briggs Institute (Ed.). (2017). Joanna Briggs Institute Reviewer’s Manual. https://reviewersmanual.joannabriggs.org/
Tricco, A. C., Soobiah, C., Antony, J., Cogo, E., MacDonald, H., Lillie, E., Tran, J., D’Souza, J., Hui, W., Perrier, L., Welch, V., Horsley, T., Straus, S. E., & Kastner, M. (2016). A scoping review identifies multiple emerging knowledge synthesis methods, but few studies operationalize the method. Journal of Clinical Epidemiology, 73, 19–28. https://doi.org/10.1016/j.jclinepi.2015.08.030
Vergauwe, J., Wille, B., Feys, M., De Fruyt, F., & Anseel, F. (2015). Fear of being exposed: The trait-relatedness of the impostor phenomenon and its relevance in the work context. Journal of Business and Psychology, 30(3), 565-581. https://doi.org/10.1007/s10869-014-9382-5
Villwock, J. A., Sobin, L. B., Koester, L. A., & Harris, T. M. (2016). Impostor syndrome and burnout among American medical students: A pilot study. International Journal of Medical Education, 7, 364-369. https://dx.doi.org/10.5116%2Fijme.5801.eac4
Wenger, E. (2010). Communities of practice and Social Learning Systems: The career of a concept. In C. Blackmore (Ed.), Social Learning Systems and Communities of Practice (pp. 179-198). Springer. https://doi.org/10.1007/978-1-84996-133-2_11
*Kirsty J Freeman
Duke-NUS Medical School
8 College Road,
Singapore 169857
Tel: +65 89219676
Email: kirsty.freeman@duke-nus.edu.sg
Submitted: 1 March 2021
Accepted: 13 September 2021
Published online: 4 January, TAPS 2022, 7(1), 9-20
https://doi.org/10.29060/TAPS.2022-7-1/RA2460
Cindy Shiqi Zhu1, Ryan Kye Feng Yap2,3, Samuel Yong Siang Lim2,3, Ying Pin Toh2,4 & Victor Weng Keong Loh1,2
1Department of Family Medicine, National University Health System, Singapore; 2Division of Family Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Ministry of Health Holdings, Singapore; 4HCA Hospice, Singapore
Abstract
Introduction: Humanistic values lie at the heart of medicine. In the wake of professional breaches among health care professionals, the place of humanistic values in medical training has been the subject of much debate and development in the literature. This scoping review aims to map the current understanding of how humanism in the Asian socio-cultural context may be understood and applied, and how the strengthening of humanistic values may be further integrated into medical schools in Asia.
Methods: Arksey and O’Malley’s approach to scoping reviews was used to guide the study protocol. Databases PubMed, ERIC, EMBASE, Scopus, CINAHL, and Web of Science were searched for articles on humanism and medical education in Asia. Data charting and thematic analysis were performed on the final articles selected.
Results: Three hundred and six abstracts were retrieved, 93 full-text articles were analysed, and 48 articles were selected. Thematic analysis revealed four themes on the need to strengthen humanistic values, the challenge of finding a common framework and definition, opportunities in medical school for curriculum design and training, and the need for validated tools in program evaluation in Asia.
Conclusion: Themes highlighted in this review show an increasing recognition amongst Asian medical educators of the importance of inculcating humanistic values into medical training. Further research and ongoing discussion are needed to develop culturally relevant, effective, and integrative curricula in order to promote humanistic attitudes and behaviours among medical students and physicians in Asia.
Keywords: Humanism, Asia, Medical Education, Medical Students, Admission, Curriculum, Mentorship, Assessment, Medical Humanities, Humanistic Values
Practice Highlights
- This review maps how medical schools in Asia impart humanistic values.
- There is a pressing need to strengthen humanistic values among medical students in Asia.
- The outcomes of current strategies are varied; mentorship and reflection on experience are crucial.
- There is much scope for further research in culturally relevant pedagogy that may impart humanism.
- Validated tools need to be developed for evaluating interventions to impart humanism in healthcare.
I. INTRODUCTION
Humanistic values lie at the heart of medicine. Humanism in health care has been defined as “an intrinsic set of deep-seated convictions about one’s obligations toward others”, and “devotion to human welfare”, characterised by a respectful and compassionate relationship between physicians, their patients, and other members of the healthcare team (Cohen, 2007; Gold, 2018).
Recent increased interest in the development of humanism in medical education (Maheux et al., 2000; Moyer et al., 2010; Wald et al., 2015) may be in response to concerns regarding the erosion of humanistic qualities among medical professionals (Haque & Waytz, 2012; Thibault, 2019). The push for medical humanism gained momentum through various advocacy movements, such as the Arnold P. Gold foundation in the United States, where the ‘IECARES’ framework was created to facilitate systematic discourse and study of humanism (Gold, 2018).
Medical educators in Asia have long recognised that humanistic traits are key to the art of medicine. They recognise that humanistic values have a positive effect on the patient-physician relationship, correlate positively with patient satisfaction, positively influence treatment outcome and adherence, and help maintain harmony in the working environment (Asai et al., 2007; Chiu et al., 2009; Saw, 2018; Song et al., 2017; Tokuda et al., 2008). Training in humanistic attitudes may therefore provide ballast to the thorny relationships sometimes seen in medical practice. In China, for example, more than 70% of doctors have experienced medical violence in hospitals, and strengthening humanistic values during medical training has been proposed as an urgent and important strategy to counteract this phenomenon (Hu, 2016).
Published studies from Asian medical training contexts that examine the perception, pedagogy, and assessment of humanistic values, and how humanism education frameworks derived from Western sociocultural contexts resonate with the cultural values, social history, and healthcare infrastructure in Asia are however relatively scarce.
As a social construct (Cohen, 2007; Kelly & Dornan, 2016; Rios, 2016), the discourse on humanism in Asian medical education and medical practice must consider cultural and contextual distinction from the main body of current literature that stems mainly from the West (Claramita et al., 2013; Schouten & Meeuwesen, 2006; Tsai, 2001). This study aims to explore how humanism has been understood and applied in medical education in the Asian sociocultural context by scoping current knowledge and evidence.
II. METHODS
A preliminary literature review revealed that existing literature on humanism in medical education in Asia was heterogeneous and limited. As such, a scoping review methodology was selected (Thomas et al., 2017). Arksey and O’Malley’s approach to scoping reviews was used to guide the study protocol (Arksey & O’Malley, 2005). Ethics approval was not required for this study, as it does not involve human subjects or data.
A. Identifying the Research Question and Relevant Studies
This study aims to provide an overview of the current knowledge on humanism in Asian medical education, identify successes and deficiencies in current practice, and guide further research.
The PICOS format was used to structure the research question for the literature search (Table 1). While alternate frameworks of humanism such as the Interactive Heart and Head model (Montgomery et al., 2017) and the outcome-oriented approach (Ferry-Danini, 2018) were considered, the authors decided that the Gold Foundation’s IECARES framework which knit together different strands of the humanism construct into a meaningful cohesive unit was most suited as a scaffold for our search terms. We thus included studies of any design on humanism and its core characteristics (Integrity, Excellence, Compassion & Collaboration, Altruism, Respect & Resilience, Empathy, and Service) as defined by the Gold Foundation’s IECARES framework), among medical students and educators in Asia. We excluded articles in foreign languages, on non-Asian populations, and allied health professionals (e.g. dentistry, pharmacy, nursing students). The search strategy was formulated through discussions between the authors and a medical librarian (A.C). Comprehensive search terms were constructed to expansively identify studies containing any synonyms or variation of three key concepts: humanism, medical education, and Asian countries and regions as defined by the United Nations Statistical Division (United Nations Statistics Division, n.d.). Six databases – PubMed, ERIC, EMBASE, Scopus, CINAHL, and Web of Science were searched.
|
PICOS Table |
Inclusion Criteria |
Exclusion Criteria |
|
Population |
Medical students and practising physicians including residents in Asia |
Allied health specialities such as nursing, pharmacy and physiotherapy. Non-medical specialities such as dentistry. Studies from non-Asian countries and regions |
|
Intervention |
Studies on humanism and its core characteristics (integrity, excellence, compassion, altruism, respect, empathy, and service) as defined by the GOLD foundation |
|
|
Comparison |
N/A |
N/A |
|
Outcome |
Definition of humanism Similarities and differences between Asian and Western concepts of humanism Perceptions on the integration of humanism as a subject/concept in medical education Methods of teaching humanism Assessment of humanistic characteristics and behaviour Suggested time point in training for teaching humanism |
|
|
Study Design |
All study designs and article types were included (observation studies, cross-sectional studies, nominal group studies, Delphi study, literature review, and scoping review) |
Studies published in a non-English language |
Table 1: PICOS Table of Inclusion and Exclusion Criteria
B. Study Selection
The selection process for articles is summarised in the PRISMA format (Moher et al., 2015) in Figure 1. Three hundred and six abstracts were identified through the initial search and reviewed after the removal of duplicates. Ninety-three full-text articles were examined to determine suitability for inclusion according to the selection criteria. Forty-eight full-text articles were included in the final review for thematic analysis.
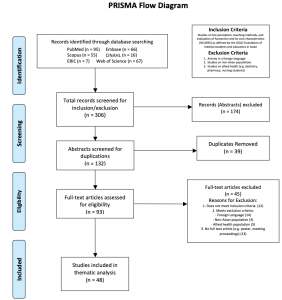
Figure 1. PRISMA Flowchart
C. Data Charting
Braun and Clarke’s inductive approach to reflective thematic analysis was utilised (Braun & Clarke, 2013, pp. 248-273). Two researchers (CZ and RY) independently reviewed the studies. Articles were read and analysed in detail, and key ideas were recorded into a data abstraction coding sheet (Zhu et al., 2021a). Frequently discussed ideas were identified and generated into a list of initial themes, which were added to a data extraction form (Zhu et al., 2021b). The researchers iteratively reviewed the independently extracted themes for agreement. This entailed a familiarisation with the depth and breadth of current knowledge through literature review and immersion in the derived data. The researchers subsequently ensured consistency in data extraction by applying the same coding sheet and data extraction forms on the entire data set, forming a template that included all the key ideas that were coded. Sessions for peer debriefing were set up to discuss more complex ideas by discussing each researchers’ interpretation all the while ensuring relevance to the research question.
D. Collating, Summarising, and Reporting Results
Codes and initial themes from the data abstraction sheet were reviewed and summarised into four final themes based on semantic and conceptual similarity. The themes were refined during the abstraction phase, and multiple discussions were conducted amongst all authors to achieve consensus on their definition and content. The results are reported in figures and narrative form below.
III. RESULTS
The final articles included in this review consisted mainly of cross-sectional studies of survey-based quantitative or mixed-method design and commentaries/essays by medical educators. There were a smaller number of nominal group studies, literature reviews, one Delphi study, and one scoping review on medical professionalism (Figure 2). East Asian studies (China, Taiwan, Japan, and Korea) comprised 58.33% of the articles included, South Asian (India, Pakistan, and Bangladesh) studies accounted for 16.7%, while studies from West Asia (Israel, Lebanon, Saudi Arabia) and Southeast Asia (Malaysia, Singapore, and Thailand) each accounted for 12.5% (Figure 3). The articles ranged in publication date from 1995 to 2018. Notably, there was a steady increase in the number of articles over this period (Figure 4). Thematic analysis revealed the following themes on humanism in Asian medical education (Zhu et al., 2021a, 2021b).

Figure 2. Graphical representation of article types included in the current review
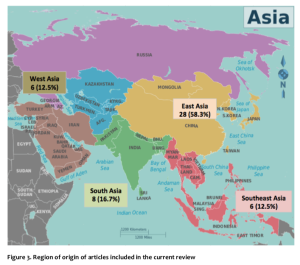
Figure 3. Region of origin of articles included in the current review
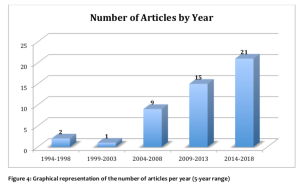
A. Training in Humanistic Values: A Pressing Need in Asian Medical Schools
The common refrain of concern for the current state of medical students’ and physicians’ humanistic qualities was highlighted in many articles from several Asian countries and regions. Issues related to breaches of professional and ethical behaviour among medical students and young physicians were widespread and of serious concern to medical educators and the general public in Japan (Tokuda et al., 2008). Taiwanese educators lamented a lack of dedication and personal commitment among young Taiwanese physicians compared to their predecessors (Chiu et al., 2010). In Pakistan, concerns regarding the deterioration of humanism and professional values in medicine were raised, with students overestimating the self-rated quality of their bedside manner compared to objective assessments (Farooq et al., 2013). Bhatia et al from India indicated that humanistic traits such as empathy, caring, altruism, and compassion were often underdeveloped in medical students and doctors (Bhatia et al., 2013). In China, medical students were described to be lacking in humanistic concerns, humanistic knowledge (cultural, geographical, historical), and awareness of the importance of humanism education (Liu & Li, 2012). A cross-sectional study of emergency physicians in Singapore found that they were perceived to be weak in humanistic traits including patient communication, holistic management, and professional relationship with colleagues (Fones et al., 1998). There was a clear and pressing need to foster humanistic values in medical training in Asian medical schools (Asai et al., 2007; Chiu et al., 2009; Hu, 2016; Saw, 2018; Song et al., 2017; Tokuda et al., 2008).
B. “Seeking the Welfare of the Other”: Unity Amidst Diversity of Meanings of Humanistic Values
Studies on Asian medical humanism adopted definitions and frameworks from the West, such as the Gold Foundation’s IECARES framework, and ABIM’s charter of physician professionalism (Chiu et al., 2009; Tsai et al., 2007). However, the direct application of these definitions and frameworks in Asia has been questioned (Chiu et al., 2009; Wang et al., 2016){Chiu, 2009 #53}. It has been recognised that the interpretations of medical humanism may vary due to the influence of local cultural, religious and philosophical systems, as well as difficulties in translating abstract concepts such as “ethics” that have been derived from a Western context (Ho et al., 2014; Pan et al., 2013; Qian et al., 2018; Zhang & Cheng, 2000).
While Western notions of humanism dichotomised physicians’ professional and personal lives, studies found that the collectivism imbued in East Asian physicians underpinned by Confucian cultural traditions blurred the lines between one’s personal and societal roles (Ho et al., 2014). Pan et al. (2013) commented that healthcare professionals in China considered the Western-derived term of “ethics” as being external to the individual, and thus ranked it low on the list of desired professional values in deference to “moral character” which was perceived to be more innate. The Confucian collectivistic slant could further be gleaned in concepts such as guanxi – the fostering of social relationships through the mutual exchange of favours, renai – “humane love” and gongxin or “public-spiritedness”. Traditional Chinese medical ethics, while influenced by two other major traditions – Taoism which leaned toward the pursuit of longevity, and Buddhism whose goal was the transcendence of the endless cycles of rebirth through non-attachment and garnering of merit, nonetheless had Confucianism as its core position (Zhang & Cheng, 2000).
While Jiang and Liu from mainland China proposed a narrative definition of humanistic medicine as “an interdisciplinary science that synthesizes knowledge concerning medical philosophy, medical ethics, medical law, medical history, medical sociology, medical logic, and doctor-patient communication” (Jiang & Liu, 2014), Wong from Taiwan has proposed the same to be “[a service environment where] patient welfare, patient autonomy, and social justice take primacy, and [practitioners] offer charitable and dignified treatment” (Wong et al., 2012). Among Asians of the Muslim tradition, Al-Eraky et al. (2014) described a four-gates model that pointed to four relationships the Muslim-Arab medical professional did well to align him/herself with; these include right relationships with the self – self-awareness, with the task-at-hand – excellence and reflective practice, with others – respect of patients and team members, and with God – self-awareness and right relationship with the Divine (Al-Eraky et al., 2014). Meanwhile, the perspective of patients in Singapore and Israel while highlighting the importance of moral-humanistic traits such as empathy highly, nonetheless ranked professional expertise above all other traits (Fones et al., 1998; Schattner et al., 2004).
Amid the broad differences in individual differences in how humanistic values were articulated regionally – for instance, the reference to collectivism in the East Asian context, and the reference to the divine in the Arab-Muslim context – these expressed how each sociocultural context sought that common humanistic goal of “seeking the welfare of the other.” We propose that the universal attributes of the IECARES framework (Gold, 2018) arguably encompasses these values.
C. Humanistic Values in Medical Training
1) Select for humanistic values:
For medical admissions to successfully select candidates that would become humanistic and competent medical professionals at the end of training, any process for entry into medical school based narrowly on academic criteria was inadequate. Authors argued that in addition to academic performance, medical admissions processes should include involvement in community work, extra-curricular activities, and the consideration of recommendation letters to better reflect the humanistic attributes of candidates that academic performance alone would not capture (Chiu et al., 2009; Lee & Ahn, 2004; Tokuda et al., 2008)
2) An afterthought in planning:
As a non-traditional curricular item, the introduction of humanism learning activities into already heavily packed curricula would often be met with resistance and/or inertia, be ranked lower in priority (Rao & Rao, 2007; Tokuda et al., 2008) and thereby poorly integrated into Asian medical school curricula (Liu & Li, 2012; Rao & Rao, 2007). When these existed in the curriculum, humanism courses were usually of short duration, offered as an elective (Liu & Li, 2012; Qian et al., 2018; Wang et al., 2016), and scheduled at unfavourable time slots (Kosik et al., 2014; Notzer et al., 2005). Students were often hard-to-manage and poorly motivated (Tsai et al., 2007; Woratanarat, 2014), and faculty would often have variable credentials (Liu & Li, 2012). Compounding this was the common experience of observing humanistic values being sidelined by busy healthcare providers on entering the workforce (Tsai et al., 2007).
Caught where holistic care is valued. Humanistic values would be best caught in specialities that prioritised the holistic care of individuals and families such as Family Medicine. Authors lamented how paternalistic medical cultures (Farooq et al., 2013) prioritised the draw of cutting-edge technologies and hospital specialities in the curriculum (Akhund et al., 2014) over disciplines where humanistic biopsychosocial (Engel, 1977) care was explicitly valued (Biderman, 2003; Iqbal, 2010; Rao & Rao, 2007).
3) Begin early, continue longitudinally:
Asian medical educators generally agreed that learning humanistic values should start early, and continue into post-graduate education, with contextualisation of how these could be applied at different workplace settings (Biderman, 2003; Karunakaran et al., 2017; Kosik et al., 2014; Qian et al., 2018; Singh & Talwar, 2013; Wang et al., 2016). The Medical Council of India recommended that humanistic values be introduced in the early pre-clinical years to students who often harboured ideals and a sense of duty to their home communities before these sentiments waned with further training (Karunakaran et al., 2017). These learning opportunities should then extend longitudinally into post-graduate years when values may be challenged in the face of real-world challenges in clinical practice (Biderman, 2003; Singh & Talwar, 2013; Wang et al., 2016).
4) Learning methods: Experiences and reflection:
A range of teaching methods has been tried in the attempt to impart humanistic values in Asia. In addition to lecture-based learning, it was recommended that interactive experiential learning activities where humanistic attributes were practised should be designed into the curriculum (Wang et al., 2016). The Silent Mentor Program where students met and interacted with the families of human cadaver donors, listened to their narratives, and respectfully participated in culturally and religiously appropriate ceremonies, was an example of a successful program where students learnt to integrate humanistic values as they learnt about human anatomy (Karunakaran et al., 2017; Rao & Rao, 2007; Saw, 2018). Other teaching activities include the use of art in Hong Kong to prompt self-awareness and empathy (Potash & Chen, 2014), the use of film and photography (Kosik et al., 2014; Lee & Ahn, 2004; Nakayama, 2009; Woratanarat, 2014), and training in communications skills that integrated interpersonal- and clinical- skills training (Biderman, 2003; Kaga & Asakage, 2007; Yazigi et al., 2006), narrative medicine (Chiu et al., 2009) and community humanitarian work (Chen & Chou, 2015; Wang et al., 2016). Courses in the humanities and social sciences, such as history, literature, ethics, law, and medical social studies have also become part of some medical curricula; they provide insight into the human condition and have been successfully used to foster humanistic qualities in medical students (Fones et al., 1998; Lee & Ahn, 2004; Liu & Li, 2012; Song & Tang, 2017). The co-design and co-facilitation of medical humanities course of home-faculty based basic scientists or clinicians with social scientist colleagues as opposed to having social scientists running a programme solo was a promising curriculum strategy that legitimised and contextualised the importance of learning the medical humanities (Rider et al., 2014; Singh & Talwar, 2013).
5) Mentorship and role-modelling crucial:
Fostering strong and dedicated mentor-mentee relationships is crucial for the development of humanistic traits through positive role-modeling (Bhatia et al., 2013; Islam et al., 2014). Positive attributes in mentors motivated learners to model their humanistic behaviour (Bhatia et al., 2013; Chiu et al., 2009; Farooq et al., 2013; Islam et al., 2014; Singh & Talwar, 2013), whereas negative behaviours in the informal and hidden curriculum constituted a formidable counter-influence (Akhund et al., 2014; Salam et al., 2012; Wong et al., 2012). Authors highlighted the importance of faculty development where faculty learnt to internalise their responsibility as role models; strengthened awareness of their learner’s needs, expectations, and feelings; and recognised how as mentors they unwittingly enabled or hindered the positive development of humanistic attitudes among learners (Biderman, 2003; Liu & Cheng, 2017; Notzer et al., 2005; Rao & Rao, 2007).
D. Program Evaluation: Need for Validated Tools
A small number of articles in this review examined how humanism was evaluated in Asian medical schools. Most used self-assessment tools developed in Western contexts. For example, the Jefferson Scale of Physician Empathy (JSPE) has been validated in several Asian cultures and languages and has a version for medical students (Mostafa et al., 2014). Taiwanese educators have translated and applied a 32-item self-administered questionnaire reflecting students’ perception of seven characteristics of professionalism defined by the American Board of Internal Medicine, many of which overlap with humanistic traits (Tsai et al., 2007). A novel instrument to measure students’ perception of personal attributes including honesty, respectfulness, and compassion was developed and validated by Malaysian educators, which included both a Likert scale and open-ended questions (Salam et al., 2012).
Few observer-rated and arguably more objective methods of humanistic behaviours were identified in this review. In a limited number of studies, the 360-degree peer evaluation was well received for evaluation of humanistic skills among physician trainees and residents (Tham, 2007; Wang et al., 2016), whereas the Defining Issues Test (DIT) may be a better tool for medical students with little working experience (Wang et al., 2016).
The need to develop validated methods to assess humanistic attributes was recognised, both to evaluate the effectiveness of teaching at the programmatic level (Tsai et al., 2007), as well as to identify students who required remediation and guidance in their professional development (Liu & Cheng, 2017).
IV. DISCUSSION
The current article presents a scoping review of peer-reviewed publications on humanism in Asian medical education. The four themes identified include the need to strengthen humanistic values among Asian medical students and physicians; the challenge of finding a common conceptual framework for operationalising humanistic values in Asia; opportunities in medical school to foster humanistic values at admissions, in curriculum planning, implementation within disciplines which teach holistic care, the use of different pedagogies, the role of mentorship, and fourthly the need for validated tools in program evaluation.
This review encompassed a diversity of types of articles and broad geographical representation.
Several findings of this review resonate with international literature. Both Western and Asian literature highlighted the importance of imparting humanistic values in medical training (Bombeke et al., 2010; Rios, 2016; Wald et al., 2015).
There was a lack of a common definition of humanistic medicine in this review, and that it was often conflated with other education concepts such as professionalism (Cohen, 2007; Hauck et al., 1990; Thibault, 2019; Tsai et al., 2007). We found nonetheless that the Gold foundation’s IECARES framework provided a broad enough scaffold to encompass the key notions of humanistic values in the Asian context. One of the key discrepancies between Asian and Western notions of humanism that surfaced in this review was that while humanistic medicine in the Western context often referred to a set of physician attributes, most commonly compassion, respect, and empathy toward patients, the therapeutic relationship in Asia may have distinct priorities. This would include the role of the patient in relation to his/her family, community, and society given the more collectivistic stance of the Asian patient. In addition, the notion of physician expertise may need to be more explicitly articulated (Fones et al., 1998; Ho et al., 2014; Schattner et al., 2004). In addition, the notion of relationship with self and the divine was highlighted in the West Asian four doors framework that is not explicitly mentioned in IECARES.
Much like educators in the West, Asian educators in this review describe the challenges associated with teaching humanism alongside the existing rigorous medical curricula for acquiring scientific and clinical skills, which often overshadows the humanistic aspect of medical education (Doran, 1983; Mostafa et al., 2014; Singh & Talwar, 2013). Nevertheless, some of the current methods used to impart humanism in Asian medical schools show promise in improving students’ humanistic attitudes. For example, medical-themed films were rated highly by students in their ability to enable understanding of humanistic and social aspects of medicine (Lee & Ahn, 2004), art-mediate learning increased students’ empathy on the State Empathy Scale (Potash & Chen, 2014), and the Silent Mentor Program nurtured the sense of responsibility and compassion within students as shown in their personal reflections (Lin et al., 2009). It remains a challenge for both Asian and Western medical educators to develop tools to objectively evaluate humanistic attitudes and behaviours (Buck et al., 2015; Shrank et al., 2004; Wang et al., 2016), which would be valuable in both assessing the effectiveness of teaching methods as well as motivate trainees to foster an active learning attitude (Pacifico et al., 2020).
Furthermore, methods to impart humanism must evolve along with students’ level of medical training. A qualitative study conducted in Singaporean found that medical trainees at different stages of their training valued different types of teachers, preferring a didactic approach in their earlier years, in contrast to more role-modelling and feedback once they step into clinical practice (Ooi et al., 2021).
This study has several limitations. Firstly, the term “humanism” and its conjugations were used in our search strategy to identify articles on humanistic attitudes and behaviours as a collective concept rather than its parts. However, there may be articles focused on one or more aspects of humanism education, such as empathy or compassion alone, which may not have been identified in the search. Furthermore, the inclusion criteria were constructed using Gold Foundation’s ‘IECARES’ framework, while it was later revealed through inductive thematic analysis that culturally relevant definitions should be developed to explore humanism in Asian medical education. Secondly, only English language databases were searched, and foreign language articles were excluded for practical purposes. Thirdly, there were notable intra-continental differences between various Asian countries represented, and there were a larger proportion of articles from East Asia in this review with Confucianism-based cultural origins. As such, conclusions drawn from these regions may be internally similar but require further adaptation for regions with differing religious or cultural origins.
V. CONCLUSION
Though Asia has been the cradle of many humanistic traditions since the dawn of civilisation, the explicit introduction of humanism education into the discourse of Asian medical schools is a recent phenomenon. This scoping review unveiled themes on key contentions around why, when, and how humanism should be integrated into the curriculum, and how this may impact the professional development of students, physicians and their relationship with their patients. Many of these topics are exciting areas of research that deserves greater attention.
Culturally validated frameworks and definitions of Asian medical humanism are lacking, and the agreed-upon frameworks may need to consider the sociocultural contexts of the different regions. What is clearly agreed upon is that the humanistic qualities of Asian medical students and physicians are in pressing need of improvement. Progress has been stifled by a slow start, the inertia from existing traditions that constrain changes, and differing opinions regarding the need for change. Various approaches to teaching humanism have been devised, such as elective humanities courses, participatory learning, mentorship, and the hidden curriculum. Authors called for improved quantity and quality of humanities courses, learning experiences outside of the classroom, and positive role-modeling in a longitudinal manner with constant integration back to the learner’s evolving clinical setting.
The current review presents an exciting growing body of literature advocating for the development of medical humanism in Asia. Further research, especially longitudinal studies, is needed to evaluate medical school admission processes, teaching and evaluation strategies in the instillation of humanistic medicine in Asia.
Notes on Contributors
TYP and VL designed and conceived the study. CZ and SL constructed search terms. CZ and RY conducted the literature review. CZ wrote the draft of the manuscript. CZ and VL co-edited the final draft. All authors have reviewed and approved the manuscript.
Ethical Approval
Ethics approval is not application for this review, as it does not involve human subjects or data.
Data Availability
The manuscript’s data is available at Figshare and may be accessed via the following public digital object identifier:
- Coding Sheet https://doi.org/10.6084/m9.figshare.14245850.v1
- Data Abstraction Sheet https://doi.org/10.6084/m9.figshare.14245991.v1
Acknowledgement
The authors wish to thank Ms. Annelissa Chin Mien Chew for her assistance with search terms and database search.
Funding
This research received no specific grant or funding from any agency in the public, commercial, or not-for-profit sectors.
Declaration of Interest
All authors certify that they have no affiliations with any organisation or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
References
Akhund, S., Shaikh, Z. A., & Ali, S. A. (2014). Attitudes of Pakistani and Pakistani heritage medical students regarding professionalism at a medical college in Karachi, Pakistan. BMC Research Notes, 7, 150. https://doi.org/10.1186/1756-0500-7-150
Al-Eraky, M. M., Donkers, J., Wajid, G., & van Merrienboer, J. J. G. (2014). A Delphi study of medical professionalism in Arabian countries: The Four-Gates model. Medical Teacher, 36 (Suppl 1), S8-S16. https://doi.org/10.3109/0142159X.2014.886013
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19-32. https://doi.org/10.1080/1364557032000119616
Asai, A., Ohnishi, M., Bito, S., Furutani, N., Ino, T., Kimura, K., Imura, H., Hayashi, A., & Fukui, T. (2007). Humanistic qualities of physicians: A view of Japanese residents. Medical Teacher, 29(4), 414. https://doi.org/10.1080/01421590701288523
Bhatia, A., Singh, N., & Dhaliwal, U. (2013). Mentoring for first year medical students: Humanising medical education. Indian Journal of Medical Ethics, 10(2), 100-103. https://doi.org/10.20529/IJME.2013.030
Biderman, A. (2003). Family medicine as a frame for humanized medicine in education and clinical practice. Public Health Reviews, 31(1), 23-26.
Bombeke, K., Symons, L., Debaene, L., De Winter, B., Schol, S., & Van Royen, P. (2010). Help, I’m losing patient-centredness! Experiences of medical students and their teachers. Medical Education, 44(7), 662-673. https://doi.org/10.1111/j.1365-2923.2010.03627.x
Braun, V., & Clarke, V. (2013). Successful Qualitative Research: A practical guide for beginners. SAGE.
Buck, E., Holden, M., & Szauter, K. (2015). A methodological review of the assessment of humanism in medical students. Academic Medicine, 90(11 Suppl), S14-S23. https://doi.org/10.1097/ACM.0000000000000910
Chen, S.-S., & Chou, P. (2015). The implication of integrated training program for medical history education. Biomedical Journal, 38(1), 90-94. https://doi.org/10.4103/2319-4170.132885
Chiu, C.-H., Arrigo, L. G., & Tsai, D. (2009). Historical context for the growth of medical professionalism and curriculum reform in Taiwan. Kaohsiung Journal of Medical Sciences, 25(9), 510-514. https://doi.org/10.1016/S1607-551X(09)70558-3
Chiu, C.-H., Lu, H.-Y., Arrigo, L. G., Wei, C.-J., & Tsai, D. (2010). A professionalism survey of medical students in Taiwan. Journal of Experimental & Clinical Medicine, 2(1), 35-42. https://doi.org/10.1016/S1878-3317(10)60006-X
Claramita, M., Nugraheni, M. D. F., van Dalen, J., & van der Vleuten, C. (2013). Doctor-patient communication in Southeast Asia: A different culture? Advances in Health Sciences Education, 18(1), 15-31. https://doi.org/10.1007/s10459-012-9352-5
Cohen, J. J. (2007). Viewpoint: Linking professionalism to humanism: What it means, why it matters. Academic Medicine, 82(11), 1029-1032. https://doi.org/10.1097/01.ACM.0000285307.17430.74
Doran, G. A. (1983). Scientism vs humanism in medical education. Social Science & Medicine, 17(23), 1831-1835. https://doi.org/10.1016/0277-9536(83)90159-4
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129-136. https://doi.org/10.1126/science.847460
Farooq, Z., Mustaf, T., Akram, A., Khan, M., Amjad, R., Naveed, M., Azhar, A., Chaudhry, A. M., Khan, M. A. Z., & Rafiq, F. (2013). Bedside manners: Do we care? Journal Ayub Medical College Abbottabad, 25(1-2), 179-182.
Ferry-Danini, J. (2018). A new path for humanistic medicine. Theoretical Medicine and Bioethics, 39(1), 57-77. https://doi.org/10.1007/s11017-018-9433-4
Fones, C., Heok, K. E., & Gan, G. L. (1998). What makes a good doctor: Defining the ideal end-product of medical education. Academic Medicine, 73(5), 571-572. https://doi.org/10.1097/00001888-199805000-00029
Gold, A. P. (2018). Definition of humanism. Gold Foundation. Retrieved September 21, 2021, from https://www.gold-foundation.org/definition-of-humanism/
Haque, O. S., & Waytz, A. (2012). Dehumanization in Medicine: Causes, solutions, and functions. Perspectives on Psychological Science, 7(2), 176-186. https://doi.org/10.1177/1745691611429706
Hauck, F. R., Zyzanski, S. J., Alemagno, S. A., & Medalie, J. H. (1990). Patient perceptions of humanism in physicians: Effects on positive health behaviors. Family Medicine, 22(6), 447-452.
Ho, M.-J., Yu, K.-H., Pan, H., Norris, J. L., Liang, Y.-S., Li, J.-N., & Hirsh, D. (2014). A tale of two cities: Understanding the differences in medical professionalism between two Chinese cultural contexts. Academic Medicine, 89(6), 944-950. https://doi.org/10.1097/ACM.0000000000000240
Hu, X. (2016). Education as a starting point for preventing medical violence: Implications for medical violence in China. A commentary on Tan MF et al.” Nursing management of aggression in a Singapore emergency department: A qualitative study” Nursing & Health Sciences, 18(4), 539.
Iqbal, S. P. (2010). Family medicine in undergraduate medical curriculum: A cost-effective approach to health care in Pakistan. Journal Ayub Medical College Abbottabad, 22(4), 207-209.
Islam, M. Z., Salam, A., Helali, A. M., Rahman, Z., Wan, W. P. E., Ismail, S., Rahman, N. I. A., & Haque, M. (2014). Comparative study of professionalism of future medical doctors between Malaysia and Bangladesh. Journal of Applied Pharmaceutical Science, 4(4), 66-71.
Jiang, B., & Liu, H. (2014). Constructing the discipline of humanistic medicine on Mainland China. Chinese Education & Society, 47(3), 70-73.
Kaga, K., & Asakage, T. (2007). Medical education by bedside learning – Helping medical students to interact with patients who have head and neck cancer. Acta Oto-Laryngologica, 127(4), 408-410. https://doi.org/10.1080/00016480601011485
Karunakaran, I., Thirumalaikolundusubramanian, P., & Nalinakumari, S. D. (2017). A preliminary survey of professionalism teaching practices in anatomy education among Indian Medical Colleges. Anattomical Sciences Education, 10(5), 433-443. https://doi.org/10.1002/ase.1679
Kelly, M., & Dornan, T. (2016). Mapping the landscape or exploring the terrain? Progressing humanism in medical education. Medical Education, 50(3), 273-275. https://doi.org/10.1111/medu.12967
Kosik, R. O., Huang, L., Cai, Q., Xu, G.-T., Zhao, X., Guo, L., Tang, W., Chen, Q., & Fan, A. P.-C. (2014). The current state of medical education in Chinese Medical Schools: Humanities and medical ethics. Chinese Education & Society, 47(3), 74-87. https://doi.org/10.2753/CED1061-1932470308
Lee, Y.-M., & Ahn, D.-S. (2004). Medical-themed film and literature course for premedical students. Medical Teacher, 26(6), 534-539. https://doi.org/10.1080/01421590412331282318
Lin, S. C., Hsu, J., & Fan, V. Y. (2009). “Silent virtuous teachers”: Anatomical dissection in Taiwan. BMJ, 339(b5001). https://doi.org/10.1136/bmj.b5001
Liu, S., & Li, Y. (2012). Analysis of the status quo of humanistic quality-oriented education in medical colleges and universities. International Education Studies, 5(1), 216-220. https://doi.org/10.5539/ies.v5n1p216
Liu, Y., & Cheng, X. (2017). An upcoming program for medical humanities education in Fudan University’s School of Basic Medical Sciences. BioScience Trends, 11(2), 152-153. https://doi.org/10.5582/bst.2017.01094
Maheux, B., Beaudoin, C., Berkson, L., Côté, L., Des Marchais, J., & Jean, P. (2000). Medical faculty as humanistic physicians and teachers: The perceptions of students at innovative and traditional medical schools. Medical Education, 34(8), 630-634. https://doi.org/10.1046/j.1365-2923.2000.00543.x
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., Stewart, L. A., & PRISMA-P Group (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4, 1. https://doi.org/10.1186/2046-4053-4-1
Montgomery, L., Loue, S., & Stange, K. C. (2017). Linking the heart and the head: Humanism and professionalism in medical education and practice. Family Medicine, 49(5), 378-383.
Mostafa, A., Hoque, R., Mostafa, M., Rana, M. M., & Mostafa, F. (2014). Empathy in undergraduate medical students of bangladesh: Psychometric analysis and differences by gender, academic year, and specialty preferences. ISRN Psychiatry, 2014, 375439. https://doi.org/10.1155/2014/375439
Moyer, C. A., Arnold, L., Quaintance, J., Braddock, C., Spickard, A., Wilson, D., Rominski, S., & Stern, D. T. (2010). What factors create a humanistic doctor? A nationwide survey of fourth-year medical students. Academic Medicine, 85(11), 1800-1807. https://doi.org/10.1097/ACM.0b013e3181f526af
Nakayama, D. K. (2009). Professionalism in Kurosawa’s medical dramas. Journal of Surgical Education, 66(6), 395-398. https://doi.org/10.1016/j.jsurg.2009.06.001
Notzer, N., Abramovitch, H., Dado-harari, R., Abramovitz, R., & Rudnick, A. (2005). Medical students’ ethical, legal and cross-cultural experiences during their clinical studies. Israel Medical Association Journal, 7(1), 58-61.
Ooi, S. B. S., Tan, C. W. T., & Frambach, J. M. (2021). Who is an effective clinical teacher from the perspectives of medical students and residents? The Asia Pacific Scholar, 6(1), 40-48. https://doi.org/10.29060/TAPS.2021-6-1/OA2227
Pacifico, J. L., Villanueva, J. A. S., Heeneman, S., & van der Vleuten, C. (2020). How perceptions of residents toward assessment influence learning: A qualitative study. The Asia Pacific Scholar, 5(1), 46-53. https://doi.org/10.29060/TAPS.2020-5-1/OA2080
Pan, H., Norris, J. L., Liang, Y.-S., Li, J.-N., & Ho, M.-J. (2013). Building a professionalism framework for healthcare providers in China: A nominal group technique study. Medical Teacher, 35(10), e1531-e1536. https://doi.org/10.3109/0142159X.2013.802299
Potash, J., & Chen, J. (2014). Art-mediated peer-to-peer learning of empathy. The Clinical Teacher, 11(5), 327-331. https://doi.org/10.1111/tct.12157
Qian, Y., Han, Q., Yuan, W., & Fan, C. (2018). Insights into medical humanities education in China and the West. Journal of International Medical Research, 46(9), 3507-3517. https://doi.org/10.1177/0300060518790415
Rao, K. H., & Rao, R. H. (2007). Perspectives in medical education 5. Implementing a more integrated, interactive and interesting curriculum to improve Japanese medical education. Keio Journal of Medicine, 56(3), 75-84. https://doi.org/10.2302/kjm.56.75
Rider, E. A., Kurtz, S., Slade, D., Longmaid, E., Ho, M.-J., Pun, J. K., Eggins, S., & Branch, W. T. (2014). The international charter for human values in healthcare: An interprofessional global collaboration to enhance values and communication in healthcare. Patient Education and Counseling, 96(3), 273-280. https://doi.org/10.1016/j.pec.2014.06.017
Rios, I. C. (2016). The contemporary culture in medical school and its influence on training doctors in ethics and humanistic attitude to the clinical practice. International Journal of Ethics Education, 1(1), 173-182. https://doi.org/10.1007/s40889-016-0012-0
Salam, A., Chew, O. S., Mazlan, N. F., Hassin, H., Lim, S. L., & Abdullah, M. H. (2012). Professionalism of future medical professionals in universiti kebangsaan Malaysia (ukm) medical centre. International Medical Journal, 19(3), 224-228.
Saw, A. (2018). A new approach to body donation for medical education: The silent mentor programme. Malaysian Orthopaedic Journal, 12(2), 68-72. https://doi.org/10.5704/MOJ.1807.015
Schattner, A., Rudin, D., & Jellin, N. (2004). Good physicians from the perspective of their patients. BMC Health Services Research, 4(1), 26. https://doi.org/10.1186/1472-6963-4-26
Schouten, B. C., & Meeuwesen, L. (2006). Cultural differences in medical communication: A review of the literature. Patient Education and Counselling, 64(1-3), 21-34. https://doi.org/10.1016/j.pec.2005.11.014
Shrank, W. H., Reed, V. A., & Jernstedt, C. (2004). Fostering professionalism in medical education: A call for improved assessment and meaningful incentives. Journal of General Internal Medicine, 19(8), 887-892. https://doi.org/10.1111/j.1525-1497.2004.30635.x
Singh, M., & Talwar, K. K. (2013). Putting the humanities back into medicine: Some suggestions. Indian Journal of Medical Ethics, 10(1), 54-55. https://doi.org/10.20529/IJME.2013.013
Song, P., Jin, C., & Tang, W. (2017). New medical education reform in China: Towards healthy China 2030. BioScience Trends, 11(4), 366-369. https://doi.org/10.5582/bst.2017.01198
Song, P., & Tang, W. (2017). Emphasizing humanities in medical education: Promoting the integration of medical scientific spirit and medical humanistic spirit. Bioscience Trends, 11(2), 128-133. https://doi.org/10.5582/bst.2017.01092
Tham, K.-Y. (2007). 360 Degrees feedback for emergency physicians in Singapore. Emergency Medicine Journal, 24(8), 574-575. https://doi.org/10.1136/emj.2007.047530
Thibault, G. E. (2019). Humanism in Medicine: What does it mean and why is it more important than ever? Academic Medicine, 94(8), 1074-1077. https://doi.org/10.1097/ACM.0000000000002796
Thomas, A., Lubarsky, S., Durning, S. J., & Young, M. E. (2017). Knowledge syntheses in medical education: Demystifying scoping reviews. Academic Medicine, 92(2), 161-166. https://doi.org/10.1097/ACM.0000000000001452
Tokuda, Y., Hinohara, S., & Fukui, T. (2008). Introducing a new medical school system into Japan. Annals of the Academy of Medicine Singapore, 37(9), 800-802.
Tsai, D. F.-C. (2001). How should doctors approach patients? A Confucian reflection on personhood. Journal of Medical Ethics, 27(1), 44-50. https://doi.org/10.1136/jme.27.1.44
Tsai, T.-C., Lin, C.-H., Harasym, P. H., & Violato, C. (2007). Students’ perception on medical professionalism: The psychometric perspective. Medical Teacher, 29(2-3), 128-134. https://doi.org/10.1080/01421590701310889
United Nations Statistics Division. (n.d.). UNSD — Methodology. United Nations. Retrieved September 23, 2021, from https://unstats.un.org/unsd/methodology/m49/
Wald, H. S., Anthony, D., Hutchinson, T. A., Liben, S., Smilovitch, M., & Donato, A. A. (2015). Professional identity formation in medical education for humanistic, resilient physicians: Pedagogic strategies for bridging theory to practice. Academic Medicine, 90(6), 753-760. https://doi.org/10.1097/ACM.0000000000000725
Wang, X., Shih, J., Kuo, F.-J., & Ho, M.-J. (2016). A scoping review of medical professionalism research published in the Chinese language. BMC Medical Education, 16(1), 300. https://doi.org/10.1186/s12909-016-0818-7
Wong, Y. F., Lin, S. J., Cheng, H. C., Hsieh, T. H., Hsiue, T. R., Chung, H. S., Tsai, M. Y., & Wang, M. R. (2012). The formation and performance of medical humanities by interns in a clinical setting. Tzu Chi Medical Journal, 24(1), 5-11.
Woratanarat, T. (2014). Higher satisfaction with ethnographic edutainment using YouTube among medical students in Thailand. Journal of Educational Evaluation for Health Professions, 11. https://doi.org/10.3352/jeehp.2014.11.13
Yazigi, A., Nasr, M., Sleilaty, G., & Nemr, E. (2006). Clinical teachers as role models: Perceptions of interns and residents in a Lebanese medical school. Medical Education, 40(7), 654-661. https://doi.org/10.1111/j.1365-2929.2006.02502.x
Zhang, D., & Cheng, Z. (2000). Medicine is a humane art. The basic principles of professional ethics in Chinese medicine. The Hastings Center Report, 30(4), S8-S12.
Zhu, C., Yap, R., Lim, S., Toh, Y., & Loh, V. (2021a). Coding sheet (Humanism in Medical Education – A Scoping Review) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14245850.v1
Zhu, C., Yap, R., Lim, S., Toh, Y., & Loh, V. (2021b). Data Abstraction Sheet for Thematic Analysis (Humanism in Medical Education – A Scoping Review) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14245991.v1
*Cindy Shiqi Zhu
National University Health System,
1E Kent Ridge Road,
Singapore 119228
Email: Shi_Qi_ZHU@nuhs.edu.sg
Submitted: 25 May 2020
Accepted: 30 December 2020
Published online: 13 July, TAPS 2021, 6(3), 24-31
https://doi.org/10.29060/TAPS.2021-6-3/RA2314
Maria Isabel Atienza
Curriculum and Instruction, College of Medicine, San Beda University, Philippines
Institute of Pediatrics & Child Health, St. Luke’s Medical Center, Global City, Philippines
Abstract
Introduction: The prevailing consensus is that medical professionalism must be formally included as a programme in the undergraduate medical curriculum.
Methods: A literature search was conducted to identify institutions that can serve as models for incorporating professionalism in medical education. Differences and similarities were highlighted based on a framework for the comparison which included the following features: Definition of professionalism, curricular design, student selection, teaching and learning innovations, role modelling and methods of assessment.
Results: Four models for integrating professionalism in medical education were chosen: Vanderbilt University School of Medicine (VUSM), University of Washington School of Medicine (UWSOM), University of Queensland (UQ) School of Medicine, and Mayo Clinic and Mayo Medical School. The task of preparing a programme on medical professionalism requires a well-described definition to set the direction for planning, implementing, and institutionalising professionalism. The programmes are best woven in all levels of medical education from the pre-clinical to the clinical years. The faculty physicians and the rest of the institution’s staff must also undergo a similar programme for professionalism.
Conclusion: The development of all scopes of professionalism requires constant planning, feedback and remediation. The students’ ability to handle professionalism challenges are related to how much learning situations the students encounter during medical school. The learning situations must be adjusted according to the level of responsibilities given to students. The goal of learning is to enable students to grow from a novice to a competent level and afterwards to a proficient and expert level handling professionalism challenges in medicine.
Keywords: Medical Professionalism, Medical Curriculum, Role Modelling in Medical Education, Culture of Medical Professionalism
Practice Highlights
- A programme on medical professionalism in education starts with a working definition of the term.
- The culture of professionalism must be articulated in the school’s vision and mission.
- The professionalism programme must be woven through the four years of medical education.
- Role models are essential in teaching medical professionalism.
- For teaching medical professionalism, a nurturing environment is preferable over punitive actions.
I. INTRODUCTION
There is a prevailing sentiment that professionalism must be taught formally and explicitly in all medical schools (Cruess & Cruess, 2006). This review aims to highlight some exceptional models for incorporating professionalism in the curriculum of medical education. The models were chosen based on the consensus among medical educators that medical schools need to respond to the following observations and recommendations from the vast literature on this subject:
1. Society expects physicians to act professionally (Lynch et al., 2004; Mueller, 2009; O’Sullivan et al., 2012).
2. There is a link between unprofessional behaviour in medical school and subsequent practice (Mueller, 2009; O’Sullivan et al., 2012; Parker et al., 2008).
3. Professionalism is associated with improved medical outcomes (Mueller, 2009).
4. Professionalism needs to be taught in the undergraduate medical institutions (O’Sullivan et al., 2012).
5. The teaching and learning must be coupled with a carefully constructed means of assessment of professionalism and professional behaviour (O’Sullivan et al., 2012).
6.Students must be supported in developing the skills for continuing professional development throughout their career (O’Sullivan et al., 2012).
This review aims to utilise these assumptions as a framework for reviewing and comparing models for the incorporation of medical professionalism in the curriculum of medical schools. This paper aims to provide answers to this question: Among medical schools that have incorporated professionalism in the medical curriculum, what are the salient features of the programmes that may be adopted by other institutions in need of such curricular innovations?
II. METHODOLOGY
A literature search was conducted to search for relevant institutions that have established a programme for incorporating professionalism in their medical schools. There was no attempt to review all published reports but to focus on the schools that can serve as models for other institutions in need of such curricular innovations. All information concerning the programmes were taken from the published journal articles which were authored by the faculty members in charge of the respective programmes on professionalism. An independent appraisal was done using a framework adopted from a systematic review by Passi and co-workers which included the following criteria: institutional definition of professionalism, curricular design, student selection, teaching and learning innovations, role modelling and assessment (Passi et al., 2010).
III. RESULTS
The review of literature on undergraduate medical programmes on professionalism revealed four notable models that describe how their institutions have integrated the teaching and assessment of professionalism among medical students, namely, Vanderbilt University School of Medicine (VUSM), University of Washington School of Medicine (UWSOM), University of Queensland (UQ) School of Medicine, and Mayo Clinic School of Medicine.
A. Vanderbilt University School of Medicine (VUSM)
A model applied at the VUSM focused on an Academic Leadership Programme (ALP) established to address unprofessional and disruptive behaviours of students (Hickson et al., 2007). The ALP is a programme designed for leaders and administrators tasked to identify and tackle unprofessional behaviours. A four-level graduated intervention programme was designed to deal with the incident cases occurring in the school. The tenets of professionalism are introduced to the medical students through a discussion of case vignettes dealing with unprofessional behaviour. The faculty are also asked to sign a creed and a commitment to be role models of professional behaviour for graduates and medical students.
A so-called “disruptive behaviour pyramid” serves as a guide for identifying and assessing variable degrees of unprofessional behaviour with their corresponding intervention. Surveillance systems have also been put in place to detect unprofessional behaviour of students and physicians from patients, visitors, and health care team members (Hickson et al., 2007).
B. University of Washington School of Medicine (UWSOM)
The UWSOM introduced their professionalism curriculum through the development of the Colleges programme for the preclinical medical students. Outstanding faculty-clinicians are selected and trained to teach and model clinical skills with small groups of students at the bedside from the second-year level until the time of their graduation. The institution recognises these faculty as role model physicians working closely with students in the care of patients (Goldstein et al., 2006).
The school promotes an “ecology of professionalism” in the campus and provides an environment for group discussions, role modelling and reflection among the different year levels of medical education. Professionalism is an institution wide concern such that both students and the faculty are required to undergo training on professionalism. In order to make the programme more meaningful, the institution added the “Patients as Teachers” project whereby the patients are asked to provide feedback and to offer advice to the medical students. The loop of learning involving the faculty, the students, and the patient is deemed as a “safe” and respectful educational environment that encourages professionalism as an institutional-wide responsibility (Goldstein et al., 2006).
C. University of Queensland (UQ) School of Medicine
The programme of the University of Queensland integrates medical ethics, law and the professionalism curriculum with a “Personal and Professional Development” process (Parker et al., 2008). Throughout the four-year levels of undergraduate medical education, topics of ethics and professional development are taught and assessed through written tests and objective structured clinical examinations. A document called “Commitment to Professionalism” is signed by every student at the start of their first-year level to reinforce the principles and their acceptance of the expectations of the school, including attendance.
A “Pyramid of Professionalism” serves as a model to identify the students that require supervision and eventually pass or fail the programme. Students are assessed at several levels with a committee providing support, feedback and remediation. Professional conduct ultimately affects the student’s promotion to the next year level (Parker et al., 2008).
D. Mayo Clinic School of Medicine
The Mayo Clinic incorporated professionalism into medical education by first articulating its culture through a statement of the institution’s primary value: “The needs of the patient come first”. Their mission statement declares that “Mayo will provide the best care to every patient every day through integrated clinical practice, education, and research.” This culture is expressed in all the institution’s policies and procedures (Mueller, 2009).
Mayo has adopted a framework for professionalism which places clinical competence, communication skills and sound understanding of ethics at its foundation (Mueller, 2015). Built on this foundation are the pillars or the key attributes of accountability, altruism, excellence and humanism. With this framework and the culture that Mayo promotes, professionalism teaching and assessment programmes have been implemented involving all levels of learners of the Mayo Clinic School of Medicine. An intensive bioethics courses and a leadership and professionalism course is given to the first-year medical students. For the second-year level, the “Advance Doctoring” professionalism reflective writing programme is given. For the third-year level, the “Safe Harbor” professionalism programme and an intensive bioethics course is applied (Mueller, 2009; Mueller, 2015).
More professionalism and ethics teaching are incorporated into different courses and clinical rotations throughout the four-year curriculum. Other interesting features include an elective course in Professionalism and Ethics related to the students’ career interest. Professionalism assessments are carried out by way of formative and summative feedback and professionalism “portfolios” which are summarized for their future applications for further training (Mueller, 2009; Mueller, 2015).
The Mayo Clinic faculty physicians also have their share of professionalism modules. The new physician staff are required to attend a complete series of professionalism courses. All faculty physicians have to take a complete web-based, interactive module on professionalism in order to maintain their status as practicing physicians. They also undergo a 360-degree review to identify and address lapses in professionalism. The non-physician allied healthcare staff of the institution also have their own professionalism programme to support Mayo’s service philosophy (Mueller, 2009; Mueller, 2015).
The core value of professionalism continues to guide the clinic in its leadership practices and management strategies. The value-based culture serves as a positive hidden curriculum that promotes the achievement of desired educational outcomes among the health care professionals (Viggiano et al., 2007).
E. Institutional Definitions of Medical Professionalism
The lack of a universal definition of medical professionalism has resulted in medical schools formulating what is suitable to their context (O’Sullivan et al., 2012). Among the four curricular models, Mayo clearly expounded on their definition of medical professionalism. This institution defined professionalism by embracing seven patient care-related and seven practice environment-related attributes as summarised in the Mayo Clinic Model of Care (Mueller, 2009).
In the case of UQ, while no clear-cut definition of professionalism was described in the journal article, the institution instead presented a list of topics of medical ethics and professional development for formal training and instruction. A review of the UQ listing shows that most of the elements of professionalism covered were related to the theme of public or societal professionalism, such as Medical Practice and the Law, Accountability and Self-Regulation, Inappropriate Practice and Medical Over servicing, and Commercialization of Medicine (Parker et al., 2008).
A second list of elements of professionalism was prepared by the UQ faculty, and this list contained attributes related to intrapersonal and interpersonal professionalism. This list served as their guide to identify students who required support, feedback or remediation through the process called the Pyramid of Professionalism (Parker et al., 2008).
The VUSM also did not state the elements of professionalism in their model. Instead, the institution focused on defining the unprofessional or disruptive behaviours that required case discussions in particular year levels of medical education. These were the same unacceptable behaviours that were used to identify students who needed immediate intervention ranging from non-punitive interventions up to the imposition of disciplinary processes if needed (Hickson et al., 2007).
The UWSOM developed a list of elements of professionalism that served as benchmarks for preclinical students, namely, the principles of altruism, honour and integrity, compassion, communication, respect, accountability and responsibility, scholarship, excellence and leadership. Despite this listing, the faculty received feedback from the students that the idea of professionalism and cultural competency remained unclear to them. This feedback came with a request from the students that the teaching of professionalism should be “more specific, clinically relevant, and challenging” (Goldstein et al., 2006).
F. Comparison of Programme Implementation
A systematic review (Passi et al., 2010) was done with the aim to summarise the evidence on methods used by medical schools to promote medical professionalism. Five main strategic areas to promote the development of professionalism in medical education were identified from the review: Curriculum design, student selection, teaching and learning methods, role modelling and assessment methods. These five areas can be used as guideposts in reviewing school programmes on professionalism. Table 1 shows a comparison of the four models presented earlier.
G. Similar Features in the Four Models
These are the features common to all four models: (1) Commitment of the leadership of the institution to embark on integrating professionalism into the curriculum, (2) Built-in programme for training of faculty for teaching and modelling of clinical skills, and (3) Vertical integration of the programme of professionalism from preclinical to clinical years.
These features are significant means to heighten the attention of both students and faculty to the need for growth in the area of professionalism. This will also help institutionalize professionalism. The journals on the models did not mention any policy regarding the screening for unprofessional behaviour during the student selection process.
H. Differences in the Four Models
Major differences are evident in the approach to teaching professionalism in the four curricular models.
1) The formal teaching and learning experience of the students of the four schools were varied in terms of duration and delivery of instruction: UWSOM and Mayo incorporates a formal course throughout the four years of medical education. In Mayo, all faculty physicians are trained and involved in the training of students for professionalism. UWSOM, on the other hand, has a select group of thirty faculty assigned for this purpose. UQ described a formal course on professionalism in the first two years of medical education. After the first 2 years, UQ proceeds to the clinical years of medical education using the personal and professional development (PPD) process of identifying personal and professional shortcomings among the students.
The approach taken by VUSM is more interventional in nature. Although short problem-based discussions are provided in the four-year levels of medical education, the main thrust of the programme is on identifying and rectifying incident cases of unprofessional behaviour. Its basis rests on the idea that “failing to address unprofessional behaviour simply promotes more of it.” The VUSM model mentions four graduated interventions as a disciplinary measure to address unprofessional behaviour.
2) The four schools also differed in their assessment methods: VUSM focuses on immediate recognition and grading using the “disruptive behaviour pyramid” to determine the appropriate intervention. UWSOM uses reflection and feedback in the preclinical years followed by a “closed loop” system of obtaining feedback from patients and faculty. Deficiencies in professional behaviour are identified so that remediation may be provided to ensure that only students who are ready will graduate or advance to the next year (Hickson et al., 2007).
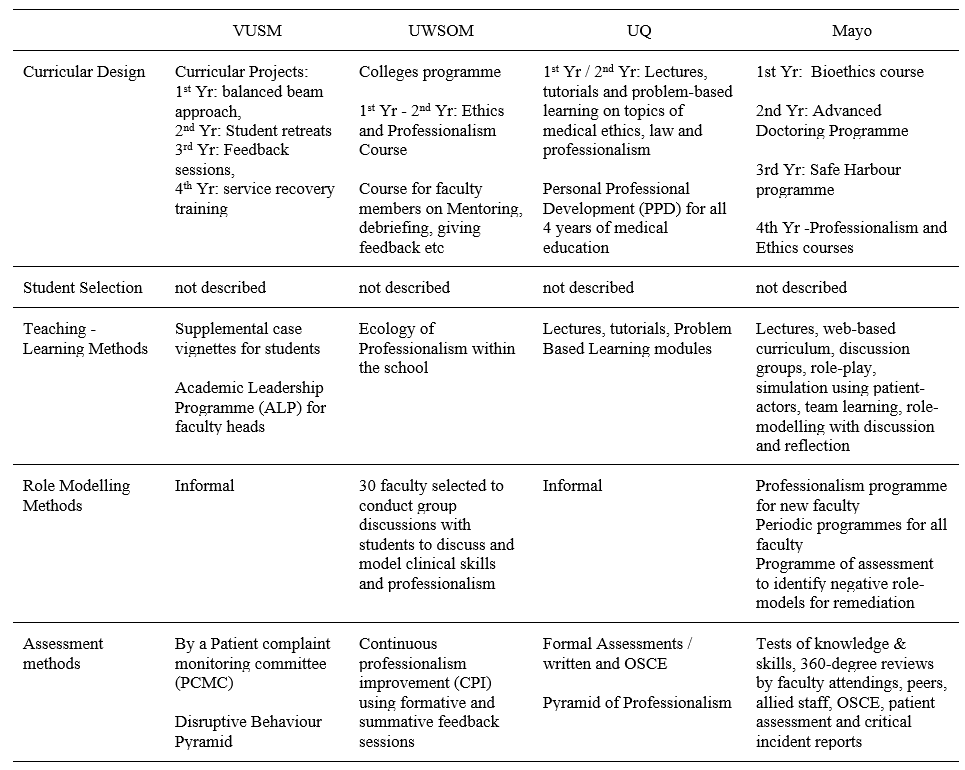
(Goldstein et al., 2006; Hickson et al., 2007; Mueller, 2009; Mueller, 2015; Parker et al., 2008)Table 1. Comparative Summary of Four Models of Educational Programme for Teaching Medical Professionalism
UQ focuses more on written tests and objective structured clinical examinations (OSCE) in the preclinical years. Because the school recognises that these assessment methods may not necessarily measure actual attitudes, the personal and professional development (PPD) process serves as a means directed towards identifying students with problems who are then referred to a committee for support and remediation (Parker et al., 2008).
Mayo has a more comprehensive assessment method by including a 360-degree review from faculty attendings, peers, allied staff and patients to complement the written tests and OSCE (Mueller, 2009).
3) Role modelling: On the area of role modelling, UWSOM has developed a formal programme to train select faculty members to promote role modelling as a means of teaching students. The programme to promote an “ecology of professionalism” within the institution is unique to UWSOM. This is the school’s way of making professionalism an institution-wide responsibility and yet maintains a “safe” educational environment for learning and improvement (Goldstein et al., 2006).
Mayo, on the other hand, has required all faculty and staff physicians to attend and successfully complete a series of modules on professionalism, physician-patient communication, self-awareness, and diversity. Maintaining the culture of professionalism in the Mayo Clinic is a result of a continuing process of allowing ethics and professionalism to be woven into the courses and clinical rotations (Mueller, 2009).
I. Professionalism in Medical Education in the Future
Much progress has been attained in the last decade when various models for incorporating professionalism in medical education have been disseminated in various journals. The Bioethics Core Curriculum introduced by the UNESCO also declared that bioethical principles and human rights must be taught early to medical students and that Medical Ethics, which is a branch of Bioethics, must be taught in all levels of education (United Nations Educational, Scientific and Cultural Organization, 2008).
The Medical Ethics Manual released by the World Medical Association (WMA) provided a basic and universally used curriculum for the teaching of medical ethics. The WMA curriculum includes professionalism as a key component needed for the inclusion of Medical Ethics and Human Rights as an obligatory course for medical schools worldwide (Williams, 2015).
It has been observed that professionalism taught through time-based training might not be sufficient to address the changing healthcare environment and new learners. For the current generation of learners, specialty training must now be aligned with global standards such as that of Accreditation Council for Graduate Medical Education (ACGME). The ACGME standards incorporates professionalism and system-based practice as core components of the curriculum that begins with acquisition of medical knowledge and clinical skills.
Moving forward to the future necessitates the development of methods of assessment of professionalism as a means to successfully teach these professional behaviours (Chay, 2019).
Another key step in the future includes the teaching of professionalism as part of health professions education. Future academic health centres will need more medical educators who can pursue further education and help foster an environment that supports educator development. This key step will help in the attainment of long-term goals and to adapt to the changes in medical education (Dickinson et al., 2020).
Providing doctors with professional models as they move from novice to expert in their professional career will be instrumental as a framework for education. One clear example is the professional identity model that incorporated leadership, followership and team-working roles A more rounded and mature professional identity eventually develops that would set these doctors as models of professionalism for other health workers (McKimm et al., 2017).
IV. CONCLUSION
The unresolved definition of medical professionalism has made the incorporation of programmes on professionalism quite challenging. Any programme that will be implemented must be well thought of and tailored to the needs of the institution and all stakeholders. Analysing unique contexts of the curricular programme will be the key to keep any programme on professionalism relevant and viable.
The fact is that there are few curricular models for the incorporation of medical professionalism into the medical curriculum. This process is not an easy task and needs a strong institutional commitment and resolve for it to be successfully implemented. The four models were amazing attempts to incorporate professionalism in medical education. No formal evaluation has been published concerning this. Based on the comparative analysis of the four models, certain aspects should be highlighted so that we could possibly learn from them:
1. The task of preparing a programme on medical professionalism would be more systematic if the institution starts with a working definition of professionalism. This was seen in Mayo where a well-described definition set the direction for planning, implementing and institutionalising professionalism.
2. The culture of professionalism needs to be articulated institutionally and incorporated in the institution’s vision, mission, goals and policies. Mayo’s declaration of its primary value that “the needs of the patient come first” sets the stage for an atmosphere that is conducive to serving with professionalism.
UWSOM also opened its door to a culture of professionalism by declaring an “ecology of professionalism”. However, its implementation may have been limited when the Colleges programme for the purpose of institutionalising professionalism was limited to thirty designated faculty and role models.
3. The professionalism programme must be woven in all levels of medical education from the pre-clinical to the clinical years. Just like any competency, acquiring the values and skills and putting it into practice requires constant learning and reinforcement throughout the years of education.
Mayo and VUSM have prepared programmes for all the four years of medical education. Both institutions have crafted programmes for the pre-clinical years and have provided teaching and learning activities such as lectures, problem-based learning, small group discussions and feedback. Mayo engaged their students in the clinical years in elective experiences in professionalism and ethics and a “professionalism portfolio” for all students. VUSM designed a programme for the clinical year that was limited to a service recovery training for the purpose of addressing actual patient complaints.
4. Role models are essential in teaching professionalism because they can greatly influence attitudes and behaviours. Unprofessional physician behaviours such as disrespect and abuse of medical personnel, and refusal to complete duties must be corrected. If left unchecked, the observing medical students may consider such behaviours as normal (Mueller, 2009). These are among the ill effects of a hidden curriculum that occurs when an institution lacks role models. For a programme on professionalism to be successful, the faculty physicians and the rest of the healthcare team and institution’s staff need to undergo professionalism programmes applicable to their needs and roles.
In the case of UWSOM, a group of 30 selected faculty underwent training while in Mayo, all faculty underwent a professionalism programme.
5. Based on the curricular models described, it appears that a nurturing environment is preferable over punitive actions. The development of all scopes of professionalism from the intrapersonal to interpersonal to societal professionalism requires constant discussion, feedback and remediation. Although repetitive unprofessional behaviours may have consequences, the medical trainee will need to go through the nurturing process in order to fully imbibe the heart and soul of a medical professional.
6. The ability to handle professionalism challenges follows a learning curve as well. The levels of difficulty of professionalism challenges are related to how much learning situations a student may have encountered. The goal is to move from novice to competent to proficient and hopefully to an expert level of handling professionalism challenges just like all other aspects of learning in medicine.
The ability of the future generation of physicians to serve society ultimately rests on how professionalism has been woven into the curriculum in medical education. How to incorporate professionalism will be a continuing challenge for all medical educators.
Note on Contributor
Dr. Maria Isabel M. Atienza, Professor, San Beda University College of Medicine, Philippines and Head, Institute of Pediatrics & Child Health, St. Luke’s Medical Center, Global City developed the methodological framework for the study and performed data collection and data analysis as part of her PhD research, and wrote and approved the manuscript.
Ethical Approval
This review article was not submitted for IRB/ethical approval.
Acknowledgement
The author would like to acknowledge the insightful suggestions of the Vice Dean of San Beda University College of Medicine: Dr Noel Atienza.
Funding
This review article did not receive any funding.
Declaration of Interest
There are no conflicts of interest to declare.
References
Chay, O. M. (2019). Transformation of medical education over the years – A personal view. The Asia Pacific Scholar, 4(1), 59-61. https://doi.org/10.29060/taps.2019-4-1/pv1076
Cruess, R. L., & Cruess, S. R. (2006). Teaching professionalism: General principles. Medical Teacher, 28(3), 205-208. https://doi.org/10.1080/01421590600643653
Dickinson, B. L., Chen, Z. X., & Haramati, A. (2020). Supporting medical science educators: A matter of self-esteem, identity, and promotion opportunities. The Asia Pacific Scholar, 5(3), 1-4. https://doi.org/10.29060/taps.2020-5-3/pv2164
Goldstein, E. A., Maestas, R. R., Fryer-Edwards, K., Wenrich, M. D., Oelschlager, A.-M. A., Baernstein, A., & Kimball, H. R. (2006). Professionalism in medical education: An institutional challenge. Academic Medicine, 81(10), 871-876. https://doi.org/10.1097/01.acm.0000238199.37217.68
Hickson, G. B., Pichert, J. W., Webb, L. E., & Gabbe, S. G. (2007). A complementary approach to promoting professionalism: Identifying, measuring, and addressing unprofessional behaviors. Academic Medicine, 82(11), 1040-1048. https://doi.org/10.1097/acm.0b013e3185761ee
Lynch, D. C., Surdyk, P. M., & Eiser, A. R. (2004). Assessing professionalism: A review of literature. Medical Teacher, 26(4), 366-373. https://doi.org/10.1080/01421590410001696434
McKimm, J., Vogan, C., & Mannion, H. (2017). Implicit leadership theories and followership informs understanding of doctors’ professional identity formation: A new model. The Asia Pacific Scholar, 2(2), 18-23. https://doi.org/10.29060/taps.2017-2-2/oa1022
Mueller, P. S. (2009). Incorporating professionalism into medical education: The Mayo clinic experience. The Keio Journal of Medicine, 58(3), 133-143. https://doi.org/10.2302/kjm.58.133
Mueller, P. S. (2015). Teaching and assessing professionalism in medical learners and practicing physicians. Ramban Maimonides Medical Journal, 6(2), e0011. https://doi.org/10.5041/rmmj.10195
O’Sullivan, H., van Mook, W., Fewtrell, R., & Wass, V. (2012). Integrating professionalism into the curriculum. Medical Teacher, 34(2), 155-157. https://doi.org/10/3109/0142159x.2011.595600
Parker, M., Luke, H., Zhang, J., Wilkinson, D., Peterson, R., & Ozolins, I. (2008). The pyramid of professionalism: Seven years of experience with an integrated program of teaching, developing, and assessing professionalism among medical students. Academic Medicine, 83(8), 733–741. https://doi.org/10.1097/acm.0b013e31817ec5e4
Passi, V., Doug, M., Peile, E., Thistlewaite, J., & Johnson, N. (2010). Developing medical professionalism in future doctors: A systematic review. International Journal of Medical Education, 1, 19-29. https://doi.org/10.5116/ijme.4bda.ca2a
United Nations Educational, Scientific and Cultural Organization. (2008). Bioethics core curriculum. Syllabus section 1: Ethics education programme. UNESCO. http://www.unesco-chair-bioethics.org/?mbt_book=bioethics-core-curriculum
Viggiano, T. R., Pawlina, W., Lindor, K. D., Olsen, K. D., & Cortese, D. A. (2007). Putting the needs of the patient first: Mayo clinic’s core value, institutional culture, and professionalism covenant. Academic Medicine, 82(11), 1089-93. https://doi.org/10.1097/acm.0b013e3181575dcd
Williams, J. R. (2015). Medical ethics manual (3rd ed.). World Medical Association. https://www.wma.net/what-we-do/education/medical-ethics-manual/
*Maria Isabel Maniego Atienza
San Beda University
College of Medicine,
Mendiola Street,
City of Manila,
Philippines 1005
Tel: 6329178668751
Email: mmatienza@sanbeda.edu.ph
Submitted: 20 July 2020
Accepted: 6 November 2020
Published online: 13 July, TAPS 2021, 6(3), 14-23
https://doi.org/10.29060/TAPS.2021-6-3/RA2346
Claude Jeffrey Renaud1, Zhi Xiong Chen2,6, Heng-Wai Yuen3, Lay Ling Tan4, Terry Ling Te Pan5 & Dujeepa D. Samarasekera6
1Department of Medicine, Khoo Teck Puat Hospital, Singapore; 2Department of Physiology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Department of Otorhinolaryngology-Head & Neck Surgery, Changi General Hospital, Singapore; 4Department of Psychological Medicine, Changi General Hospital, Singapore; 5Department of Anaesthesiology, National University Health System, Singapore; 6Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: The Coronavirus-19 pandemic has had profound effects on health professions education (HPE) posing serious challenges to the continued provision and implementation of undergraduate, postgraduate and continuing medical education (CME). Across these HPE domains, the major disruptions included the exclusion of undergraduate learners from clinical learning environments, restricted intra-, inter-institutional and overseas movement of medical professionals, termination of face-to-face learner-educator interactions, deployment of postgraduate learners into non-scope service settings, and CME postponement.
Methods: In this review we report on how in Singapore various adaptive measures were instituted across the 3 HPE domains at institutional and national level to maintain adequate resources at the frontline to meet service exigencies, promote healthcare professionals’ wellbeing and safety as well as mitigate the spread of the pandemic.
Results: We identified several strategies and contingencies developed to address these challenges. These involved the use of online learning platforms, distributed and asynchronous learning, an undergraduate Pathway Programme, and use of innovative hands-on technology like simulation. Robust, well pre-planned pandemic preparedness, effective communication, as well as provision of psychological support resources ensured maintenance of service and academic continuity, trust and resilience within HPE. However, several challenges remain, namely the timing and manner of conducting formative and summative assessments, cybersecurity, and the indispensable hands-on, in-person experiential learning for surgical training.
Conclusion: Strong leadership with vision and planning, good communication, prioritising learners’ and educators’ wellbeing and safety, and harnessing existing and emerging online learning technologies are crucial elements for effective contingencies for HPE disruption during pandemics.
Keywords: Pandemic Preparedness, COVID-19, Curriculum Development, Online Learning and Assessment, Learner Wellbeing and Safety, Health Profession Education
Practice Highlights
- COVID-19 pandemic has caused profound disruption to medical education and Singapore is no exception.
- Health professions education community (undergraduate, residency and continuous professional development) had to rethink traditional learning approaches.
- There is a need for contingencies that integrate service and academic continuity and safety.
- Implementing contingencies requires coordinated national and institutional pandemic pre-preparedness.
- There remain uncertainties as to the long-term effectiveness of these contingencies on learning.
I. INTRODUCTION
Singapore had its first case of Coronavirus 19 (COVID-19) on 23rd January 2020 and scaled up its response from DORSCON (Disease Outbreak Response System Condition) Yellow to Orange 2 weeks later as the crisis evolved to pandemic proportion (Ashokka et al., 2020; J.E.L. Wong et al., 2020). This involved setting up a suite of strategies aimed at containing community transmission (Lee et al., 2020).
At the healthcare service and health profession education (HPE) level, these strategies centred on mobilising adequate resources at the frontline, mandating use of personal protective equipment (PPE) in high-risk areas and restricting healthcare workers’ movement (Ashokka et al., 2020; Lee et al., 2020; Liang et al., 2020; C. Wong et al., 2020; J.E.L. Wong et al., 2020). In addition, undergraduate medical education put a stop to clinical clerkships and large and small on-campus learning and restructured formative and summative assessments.
As the very stakeholders and resources required for HPE were diverted to fighting the pandemic, HPE faced extraordinary disruption. Educators and learners had to delicately balance service continuity, patients’ and learners’ wellbeing and safety versus maintaining a business-as-usual approach to learning. Moreso, the entire HPE community had to critically relook at the applicability of competency-based learning which is traditionally predicated on the principles of authentic supervised patient experience, programmatic assessment, learners as part of a community of practice and continuous professional development (CPD) (Harris et al., 2010; Iobst et al., 2010).
Previous public health emergencies like Severe Acute Respiratory Syndrome (SARS) have taught that such disruptions can provide unique opportunities for contingency planning in HPE especially when there is little time for wholesale programme redesign (Lim et al., 2009; Patil & Yan, 2003). This report thus describes the experience of 3 HPE domains in Singapore in mitigating the dissonance between optimal pandemic preparedness, unconstrained academic continuity and learners’ and educators’ well-being.
II. METHODS
A comprehensive review of the adaptive contingency strategies adopted at 1 undergraduate (Yong Loo Lin School of Medicine), Singapore residency programmes and across the CPD was made by looking at institutional and governmental programmes during the early phase of the pandemic and prevalent COVID-19 related literature on HPE. As this research is a description of events that have already happened and did not involve HPE stakeholders’ directly and interventionally, participants’ informed consent and internal review board approval were not required for its conduct.
III. RESULTS
Herein, is a detailed outline of the contingencies implemented across the 3 HPE domains which are also summarised in Table 1.
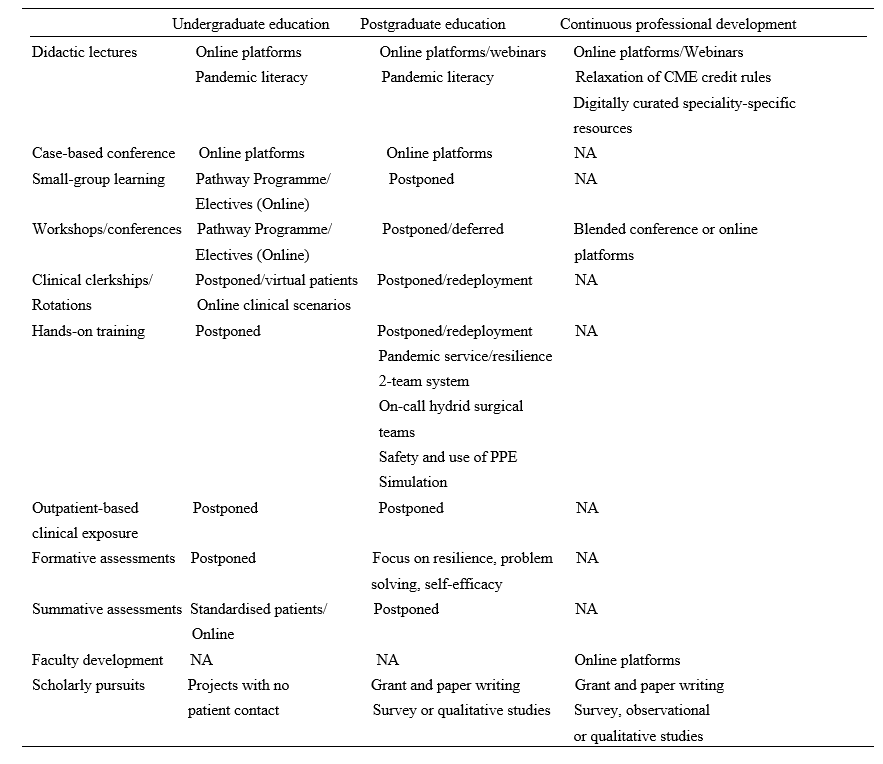
Table 1. Summary of disruptions and contingences across the health profession education spectrum during COVID-19 pandemic in Singapore.
Note: NA=not applicable; PPE= personal protective equipment
A. Contingencies in Undergraduate Medical Education: Experience of Yong Loo Lin School of Medicine
At the Yong Loo Lin School of Medicine which is the largest of the three medical schools in Singapore, the Education Team led by the Vice Dean (Education) started preparing in February 2020 for the possibility of loss of clinical teaching. Those most affected would be Phase 3 and 4 (Year 3 and 4) medical students. Phase 5 (Year 5) students were preparing for their Final Professional Examinations even though assessment was significantly disrupted across all Phases. Phase 1 and 2 (Year 1 and 2) students have relatively less clinical learning exposure and assessments, and were finishing their curricula and preparing for exams. Focusing on the Phase 3 and 4 students, first, their vacation and elective periods were brought forward respectively. Next, to give students meaningful learning opportunities that do not require patient contact, the Pathway Programme which had been launched before the pandemic was paced up (National University Singapore, Yong Yoo Lin School of Medicine, 2020).
The Pathway Programme consists of six Pathways. They are Health and Humanity, Health Informatics, Inquiry and Thinking, Medical Education and Medical Innovation and Entrepreneurship all led by a team of trained educationists. In addition, a non-Pathway initiative called Education Innovation completed the suite of new education offerings for the students. The sixth Pathway Behavioural and Implementation Science was partially offered under Inquiry and Thinking through a series of lectures on Health Economics. Below we describe what each Pathway is about.
1) Behavioral and implementation science: This pathway exposes medical students to principles of behavioural and implementation science, and applies this knowledge to effectively design and deliver healthcare in real-world settings, and lays the foundation for them to become active agents of change in clinical practice.
2) Health and humanity: This pathway aims to nurture emotionally resilient, socially conscious and globally minded health leaders through rekindling one’s love for medicine and humanity. Through experiential activities, inspirational workshops and hands-on project work in the community, students develop critical thinking skills in global health, teamwork and leadership skills to inspire health for all.
3) Health informatics: This pathway aims to enable students to gather and critically evaluate research and health informatics data, equipping them with the skills necessary to apply the principles of health informatics, summarise and visualise datasets to perform basic analyses, so they become data-science competent clinicians who can identify and analyse medical data to address clinical issues.
4) Inquiry and thinking: This pathway aims to inspire and motivate our medical students to develop a sense of curiosity so as to foster a habit of inquiry that is able to dynamically utilise a range of thinking methods, processes and skillsets to tackle questions and problems. The end goal of this pathway is to groom a pipeline of thinking doctors who can advance healthcare in any aspect they desire.
5) Medical education: This pathway exposes medical students to concepts and principles in HPE, to equip them with foundational skills in HPE, with a focus on educational innovation and scholarship of teaching and learning, so as to groom future clinical educators.
6) Medical innovation and entrepreneurship: This pathway aims to nurture medical students with the 6Cs attributes: Curiosity, Creativity, Compassion, Collegiality, Collaboration, and Commercial Intelligence. The programme gradually exposes medical students to concepts and principles in innovation, and the selective elements equip students with foundational skills in innovation and entrepreneurship.
With the elective period brought forward, Phase 4 students were exposed to the Pathway Programme from early-March to early-May 2020 through two weeks of front-loading online lectures, followed by four to eight weeks of projects. Most Pathways followed the general structure with slight variations between them. For Phase 3 students, they enjoyed an early vacation before encountering a shortened Pathway Programme from early-April to early-May 2020, comprising of 2 weeks of front-loading online lectures and 2 weeks of projects, which students had the option of continuing into Phase 4.
Using Inquiry and Thinking Pathway as an example, topics of front-loading online lectures included ‘Complexity and Systems Thinking’, ‘Habits of Inquiry and Critical Thinking’ and ‘Evidence-based Medicine and Search Methods’. More than 80 projects were offered by prospective supervisors with more than 70 students getting involved in projects. Each student was guided in the project by the supervisor as well as engaged in a one to two-hour weekly reflection sessions with a separate mentor or the supervisor who doubled up as a mentor. Students were required to submit a weekly reflection write-up of 50 words or more. At the end of the Pathway Programme, students submitted a single slide of their projects for evaluation. Top two projects from each Pathway were selected to present and compete in a Grand Finale on 8 May 2020 before the School’s leadership, a panel of judges, their peers and overseas observers. The Grand Finale attracted over 200 participants. Single slides of all projects were compiled into an e-book to be shared with students and faculty members.
B. Postgraduate Training: Experience of Residency Programmes across Singapore Three Sponsoring Institutions (SIs)
Since SARS, Singapore has steadily been bolstering critical resource reserves and expertise in pandemic preparedness, culminating in the setup of the 330-bed purpose-built National Centre for Infectious Diseases (NCID) at the National Healthcare Group (NHG) Novena campus (Lee et al., 2020; Seah, 2020). Concurrently, postgraduate medical education underwent significant transformation with the adoption of Accreditation Council for Graduate Medical Education (ACGME) styled competency-based learning, culminating in the setup of three residency SIs of which NHG is one (Huggan et al., 2012; Khoo et al., 2014). Thus during the build-up to COVID-19 pandemic, NCID, residents and faculty at NHG 27 residency programmes formed the initial frontliners in managing the pandemic before being later joined by the other two SIs (C. Wong et al., 2020).
Care delivery and learning had to be restructured so that adequate manpower could be redeployed at screening centres, emergency departments, outbreak wards and critical care units. Frontline residents had to endure long and exhausting shifts wearing PPEs and prolonged time away from family, not to mention postponed leaves. Residents and faculty also had to be segregated into independent two-team system with phased two-weekly rotations to avoid manpower attrition and service disruption as a result of staff infection, quarantine or burnout. Elective surgeries, continuity clinics, grand rounds, face-to-face case conferences, cross-institutional elective rotations, in-person programme selection interviews as well as summative assessment had to be deferred. Postgraduate specialty conferences, courses and workshops, whether local or international, also had to be postponed or cancelled due to travel restrictions, further limiting opportunities for learning.
As a result of these changes several resourceful strategies were implemented to balance the palpable tensions between service, wellbeing and learning.
The first was maintaining open and transparent communication between institutional and academic leaders, faculty and residents so that the rationale for a pandemic-mode centralised command-control leadership model could be accepted. This allowed residents to grasp the real sense of urgency brought in by COVID-19, thus facilitating speedier buy-in and compliance to ever changing human resource and education policies. In addition, this strategy helped build up trust in the institutional support structure and contain the spread of parallel distracting infodemics, allowing residents to focus on service delivery, learning and well-being.
The second strategy was the promotion of residents’ physical and psychological safety and wellbeing. This entailed ensuring all residents had adequate orientation to the proper use of PPEs and could easily access them. Well-being and resilience support resources like in-person or anonymous virtual outreach psychological crisis intervention counselling and peer support through online debriefing and feedback were put in place across all hospitals under the three SIs. The ancillary effect was that residents felt their safety, their families’ and patients’ was valued and that there was fair and equitable work and rest allocation. Further, ACGME cancelled all accreditation and Clinical Learning Environment Review site visits and took steps to reframe and relax some accreditation criteria (Nasca, 2020). This went a long way in allaying residents’ anxieties regarding clinical progression.
The third strategy was leveraging existing online tools to maintain some element of learning continuity without the need to invest in significantly expensive technologies, curricular redesign or faculty re-development. Programmes transferred their core didactic lectures, journal clubs and case-based discussions onto distributed learning platforms such as Zoom, Go to meeting, Google meet or WebEx for synchronous learning. Access to Webinars had the added advantage of providing opportunities for asynchronous learning. Zoom teleconferencing in particular, remains the most popular due to its affordable subscription, large participant capacity and easier accessible collaborative interface and a breakout feature that enables mounting learning models like team-based learning.
Residents from surgical residency programmes who rely on direct-patient encounter and hands-on experience for learning were more significantly impacted. Importantly, because non-emergency visits to hospitals were halted, elective procedures and surgeries were postponed or cancelled and, the number of patients and learning opportunities was thus greatly reduced. This was further aggravated by the shift of many training institutions and teaching hospitals to pandemic service (Liang et al., 2020). In many instances, surgical residents were redeployed to frontline areas, like screening centres, which are beyond their usual scope of practice (C. Wong et al., 2020).
Curriculum development contingencies thus went beyond online didactic content dissemination to embrace enhanced distributed learning approaches like videos, podcasts, virtual reality and simulated learning (C. Wong et al., 2020). Some programmes improvised by forming on-call hybrid surgical teams, which allowed surgical residents some measure of hands-on exposure to generic emergency or semi-elective cases during on calls but not necessarily within the scope of their area of interest.
C. Contingencies for Continuous Professional Development (CPD)
The disruption brought on by closure of higher educational institutions, scaling down of healthcare organisations and travel restrictions, compelled educators and health care professionals to adapt and embrace curricular changes and transition to virtual learning and use of technology for simulated learning.
Continuing medical education (CME) and CPD are integral parts of the development of a healthcare professional in providing optimal clinical care for his/her patient. CME is aimed at maintaining or updating the requisite knowledge, skills, professional performance and relationships and crucially, is a requirement for maintenance of certification in the discipline or specialty of the healthcare profession (Davis et al., 2008). CPD on the other hand caters to a broader range of competencies that reflect the healthcare profession attitudes towards learning and learning needs (Filipe et al., 2018). Every specialty and governing medical body has its stipulated requirements. In Singapore, the Singapore Medical Council (SMC) states that all fully and conditionally registered doctors are required to meet the compulsory CME requirements of 50 core points for the qualifying period before their practising certificate can be renewed (Singapore Medical Council, 2020a). While most CME activities involve attendance at local, regional or international scientific meetings or conferences, self-study, review and authorship of articles are also considered core CME points. Most hospitals hold regular Grand Ward Rounds, journal clubs and peer review learning sessions at departmental and institutional levels, which also contribute towards core CME points.
However, with Singapore moving to DORSCON Orange, many of these learning activities were immediately suspended as staff scrambled to reorganise clinical services amidst the pandemic imperative for team separation and safe distancing. Thus, traditional face-to-face meetings were replaced by online meetings and webinars facilitated by virtual platforms mentioned previously. In tandem the SMC relaxed requirements for CME credits by allowing healthcare professionals to log in attendance to online sessions, including webinars (Singapore Medical Council, 2020b). There was also an increase in allocation of CME credits for self-study (e.g., reading of referenced journals listed in PubMed). COVID-19-related CME activities were also considered core points for all doctors (Singapore Medical Council, 2020b).
While, much of the recent global CME content has primarily focused on increasing understanding of COVID-19 and its infectious nature across various medical disciplines, there has been lesser emphasis on its medical and psychological impact to health. It has nonetheless enabled healthcare professionals to better provide optimal care for patients while adopting best available evidenced practice relating to all aspects of this rapidly contagious disease. Thus, online information dissemination has been at an unprecedented high with multiple local, regional and international webinars and resource websites being made readily accessible. Professional societies have also made available to their members regularly curated digital speciality-specific resources on best practices pertaining to COVID-19 management (Academy of Medicine Singapore, 2020).
In addition to CME, healthcare professionals have traditionally relied on annual live face-to-face local, regional and international scientific conferences, symposiums, and educational workshops to network as a learning community and keep abreast of domain-specific advances. With strict travel restrictions these have been cancelled, postponed or moved online as webinars, interactive content, forums and chats.
Some conference organisers decided to still proceed to issue notices of acceptance of abstract submissions as ‘proof’ of scholarly work or allowed online presentation. Other creative ways of continuing with international conferences have included a “blended conference” approach with a mix of face-to-face and online content to support those attending onsite and online (Nadarajah et al., 2020). With careful attention paid to safe distancing for onsite participants, such “blended conferences” provide the all-important human face-to-face interactions which online webinars and conferences, though functional in most parts, sorely lack. They also provide the best of both worlds and may indeed be the new normal in the foreseeable future as COVID-19 further changes the HPE landscape relating to international travel and social interaction.
Similarly, Singapore’s three medical school curriculum development centres rapidly transited in-person to virtual faculty development sessions. This allowed educators openly dispersed by social distancing and clinical exigencies to continue tapping on the best pedagogic practices, interact and engage in interprofessional learning.
IV. DISCUSSION
The COVID-19 pandemic disruptions have reinforced the need for agency and adaptation in HPE. We have shown that through well-coordinated, multisectoral efforts, solutions can be harnessed to minimise their negative impact on learning. However COVID-19, unlike other recent coronavirus epidemics like SARS and Middle East Respiratory Syndrome (MERS) seems a more formidable crisis (Jones, 2020; Peeri et al., 2020). It may not go away quickly without the advent of effective vaccines and sustained infection control measures. These contingencies are therefore aimed at promoting service and academic continuity, safety and resilience. Whilst they are useful blueprints for pandemic preparedness and responsiveness in the short term, they may not be applicable in all contexts or in a crisis of attrition. Further, they have their own strengths and limitations.
A major strength is institutional and academic leaders’ sense of long-term planning and commitment to educators’ and learners’ safety through effective communication, being visible and providing programme and system support. In a rapidly evolving disruptive environment, this is crucial, as stakeholders remain engaged and trusting without having to anguish over under-resourcing or abandonment. Recent publications have alluded to the social capital returns of such an “integrative resilience approach” that amplifies individual and system wellbeing and minimises burn-out and contagion (Neufeld & Malin, 2020; Samarasekera et al., 2020; Schwartz et al., 2020; Wald, 2020).
Another strength is the adoption of adaptive online technologies which not only ensures academic continuity but also allows a smooth and rapid quarantine and pandemic curriculum development. Large virtual communities of learners can thus be rapidly mobilised without fundamentally affecting content, quality and institutional bottom lines. Indeed, this may have had the unintended consequences of unprecedentedly boosting attendance rates in medical schools, residency programmes and CPD sessions. Online migration also facilitates quick and mass standardised training and deployment of untrained or returning retired healthcare professionals in general and critical care medicine, allowing healthcare institutions to boost capacity in those critical areas during pandemics (Brunner et al., 2020; Li et al., 2020). More so, these emergent technologies hold a lot of promise for post-pandemic medical education and replication of authentic patient experiences. It is envisioned that they can be interfaced onto learning management systems (LMS) and into areas like virtual patient consults, telemedicine, adaptive learning and extended reality or avatar-like high fidelity simulation (Goh & Sandars, 2020). They are also important as a source of asynchronous learning whereby learners who are too busy with clinical duties or for surgical residents when there is a lack of critical hands- on training (Tolu et al., 2020).
A third strength, is that such crisis can open unintended opportunities for learners to develop competencies outside the core curricular knowledge and procedural skills sphere. For instance, the mere exposure of undergraduate learners not directly involved in patient care to pandemic-related content, volunteering in contact tracing or public awareness centres or restructuring of learning experiences like the Pathway Programme can nurture professional identity, pandemic literacy and doctor-ready qualities like service prioritisation, altruism and resilience (Bauchner & Sharfstein, 2020; Rose, 2020; Stetson et al., 2020). Indeed, the Pathway Programme succeeded in meaningfully engaging medical students at a time when clinical teaching and clinical elective opportunities were frozen. It gave time for the medical school to work out a safe and calibrated approach to resume clinical training in consultation with the relevant government bodies. The fact that it was conceptualised pre-pandemic demonstrates an extraordinary sense of prescience by the academic leadership. The advent of COVID-19 served to accelerate its implementation. It thus not only helped undergraduate medical education to cope with the pandemic but enrich the medical curriculum by catering to the diverse strengths and interests of each learner in order to nurture future-ready doctors for a post-COVID world.
As to residents’ learning, negotiating challenging pandemic duty rosters, making personal choices and sacrifices, navigating processes like resource allocation and public health measures and being deployed into non-core areas, can be just-in-time learning platforms for more nuanced ACGME competencies like professionalism, interpersonal and communication skills, system-based practice and practice-based learning (Hall et al., 2020; Nasca, 2020; Schwartz et al., 2020; Tolu et al., 2020; C. Wong et al., 2020). For surgical residents, there is also an added learning and safety benefit when hitherto straightforward surgical procedures like tracheostomy suddenly come with a myriad of precautions, criteria, and protocols (Givi et al., 2020). Clinic and elective surgery postponement can provide ample opportunities for self-directed learning, exit exams preparation and scholarly pursuits like grant, research ventures and quality improvement projects writing (Schwartz et al., 2020; Tolu et al., 2020). Additionally, prioritisation of public health emergency response training across the HPE spectrum can render healthcare institutions better prepared at handling future pandemics and burn-out (Yang et al., 2020).
Nevertheless, these contingencies have a number of limitations. Namely, moving medical education from the bedside to the ‘web-side’ cannot replace the real patient-centred clinical experience and case-mix learners derive from ward rounds, grand rounds and continuity clinics. Even the Pathway Programme was not without its challenges. With Singapore entering into Circuit Breaker phase of DORSCON Orange on 3rd April 2020, some projects were disrupted as access and movement became more limited (Ministry of Health Singapore, 2020).
Secondly, the utility of online learning is very much predicated on the vagaries of internet penetration and connectivity which makes this approach not always transferable to all socio-economic contexts (Cecilio-Fernandes et al., 2020). More so, for surgical residents, online learning or high-fidelity simulation cannot substitute for in-person learning. The technical skills, haptic feedback, the realism of live surgery, the experiential and contextual learning of ‘being there’ in a surgical team, and the non-cognitive domain skills like collaboration and resilience can be hard to simulate. Reduced contact time between residents and faculty also impacts adversely on opportunities for mentoring, role modelling and supervision. There is also always a danger of breaching learning principles such as cognitive overload when online content design is outside the hands of curriculum developers and programme directors (Kachra & Ma, 2020). As to health professionals, most of these online CME resources represent rather an amalgam of available information that may not have been well curated and pre-approved by accreditation organisations for relevancy.
Thirdly, the contingencies fail to address the enormous challenges in conducting clinical workplace-based assessments, without compromising their validity, reliability, defensibility and educational impact. Although high-stakes OSCE can be successfully conducted in a pandemic environment, its implementation comes with tremendous logistical and political manoeuvring to ensure students’, examiners’ and patients’ safety and assessment integrity are preserved (Boursicot et al., 2020). Cancelling both formative and summative assessments can delay learners’ progression or completion unless adjustments are made to previously established competency criteria. Undergraduates may fail to graduate on time to join the vital pool of medical workforce and residents may not be able to practise as independent practitioners. This can create anxiety and concern to both learners and educators about how to catch up post-pandemic with piling assessment and case and portfolio backlogs.
Lastly, reliance on third party software entities for online content dissemination contrary to institution-designed LMS or whole-sale programme information technology infrastructure redesign carries cybersecurity, privacy and data ownership risks (Fawns et al., 2020; Sandars et al., 2020). Not all faculty are tech savvy to handle the technical intricacies and the many options in the market. Predatory providers may thus seek to peddle behaviourist tactics onto users for their own corporate gains.
V. CONCLUSION
In summary, the COVID-19 pandemic has been a major threat to HPE in Singapore but it has also created opportunities for adaptive and flexible contingencies so that learning goes on safely with minimum constraints. While there is a need to celebrate these early successes, it is also imperative that we assess and learn from their limitations so that we can further refine and more successfully, collaboratively and iteratively apply them in a prolonged crisis. Furthermore, these experiences can serve as templates for adaptive and value-added learning at both regional and international HPE settings beset by larger service and academic disruption. But most importantly they foreshadow the resilience, reimagining and resourcefulness that are expected of HPE as it transits from the new normal of pandemic crisis management to the post-pandemic next normal of innovative technology-based learning.
Notes on Contributors
Adj Associate Professor Claude J Renaud is a senior consultant nephrologist at Khoo Teck Puat hospital Singapre and Associate Programme Director at the National Healthcare Group Renal Residency Programme. He conceptualised, drafted and revised article and wrote introduction, postgraduate medical education (PGME), discussion and conclusion sections.
Dr Zhi Xiong Chen is a Senior Lecturer in Physiology and Assistant Dean for Education at Yong Loo Lin School of Medicine, National University of Singapore. He conceptualised article and wrote the undergraduate medical education section.
Adj Associate Professor Heng Wai Yuen is senior consultant in the Department of Otorhinolaryngology-Head & Neck Surgery, Changi General Hospital, Singapore and Campus Director, SingHealth Duke-NUS Institute for Medical Simulation (SIMS). He wrote abstract and post graduate medical education sections and revised article.
Adj Associate Professor Tan Lay Ling is senior consultant in the Department of Psychological Medicine, Psychogeriatric Service, at Changi General Hospital (CGH). She wrote the section on continuous professional development and revised article overall.
Dr Terry Ling Te Pan is a Senior Consultant, Department of Anaesthesia, National University Hospital and Advisor, Education Technology Unit, Yong Loo Lin School of Medicine, National University of Singapore. He co-wrote the section on continuous professional development and revised article overall.
Dr Dujeepa D. Samarasekera, director at Centre for Medical Education (CenMED) Yong Loo Lin School of Medicine, National University of Singapore. conceptualised and revised article.
Ethical Approval
This study is a description of events and practices and therefore did not require approval from institutional review boards.
Funding
There is no external funding involved in this study.
Declaration of Interest
Other than Dr Dujeepa D Samarasekera who is Editor of TAPS, all authors have no conflict of interest, including financial, consultant, institutional and other relationships that might lead to bias.
References
Academy of Medicine Singapore (AMS) (2020, June 2). Resource site on COVID-19. https://www.ams.edu.sg/policy-advocacy/covid-19-resource-page
Ashokka, B., Ong, S. Y., Tay, K. H., Loh, N. H. W., Gee, C. F., & Samarasekera, D. D. (2020). Coordinated responses of academic medical centres to pandemics: Sustaining medical education during COVID-19. Medical Teacher, 42(7), 717-720. https://doi.org/10.1080/0142159X.2020.1757634
Bauchner, H., & Sharfstein, J. (2020). A bold response to the COVID-19 pandemic: Medical students, national service, and public health. The Journal of the American Medical Association, 323(18), 1790-1791, https://doi.org/10.1001/jama.2020.6166
Boursicot, K., Kemp, S., Ong, T. H., Wijaya, L., Goh, S. H., Freeman, K., & Curran, I. (2020). Conducting a high-stakes OSCE in a COVID-19 environment. MedEdPublish, 9(1), 54. https://doi.org/10.15694/mep.2020.000054.1
Brunner, M., Vogelman, B., & Smith, J. (2020). Rapid development of an outpatient‐to‐inpatient crash curriculum for COVID providers. Medical Education. Advanced online publication. https://doi.org/10.1111/medu.14244
Cecilio-Fernandes, D., Parisi, M. C. R., Santos, T. M., & Sandars, J. (2020). The COVID-19 pandemic and the challenge of using technology for medical education in low and middle income countries. MedEdPublish, 9(1), 74. https://doi.org/10.15694/mep.2020.000074.1
Davis, N., Davis, D., & Bloch, R. (2008). Continuing medical education: AMEE education guide No 35. Medical Teacher, 30(7), 652–666. https://doi.org/10.1080/01421590802108323
Fawns, T., Jones, D., & Aitken, G. (2020). Challenging assumptions about “moving online” in response to COVID-19, and some practical advice. MedEdPublish, 9(1), 83. https://doi.org/10.15694/mep.2020.000083.1
Filipe, H. P., Golnik, K. C., & Mack, H. G. (2018). CPD? What happened to CME? CME and beyond. Medical Teacher, 40(9), 914–916. https://doi.org/10.1080/0142159X.2018.1471200
Givi, B., Schiff, B. A., Chinn, S. B., Clayburgh, D., Iyer, N. G., Jalisi, S., Moore, M. G., Nathan, C. A., Orloff, L. A., O’Neill, J. P., Parker, N., Zender, C., Morris, L., & Davies, L. (2020). Safety Recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. The Journal of the American Medical Association Otolaryngology-Head & Neck Surgery, 146(6),579-584. https://doi:10.1001/jamaoto.2020.0780
Goh, P. S., & Sandars, J. (2020). A vision of the use of technology in medical education after the COVID-19 pandemic. MedEdPublish, 9(1), 49. https://doi.org/10.15694/mep.2020.000049.1
Hall, A. K., Nousiainen, M. T., Campisi, P., Dagnone, J. D., Frank, J. R., Kroeker, K. I., Brzezina, S., Purdy, E., & Oswald, A. (2020). Training disrupted: Practical tips for supporting competency-based medical education during the COVID-19 pandemic. Medical Teacher, 42(7), 756-761. https://doi.org/10.1080/0142159X.2020.1766669
Harris, P., Snell, L., Talbot, M., & Harden, R. M. (2010). Competency-based medical education: Implications for undergraduate programs. Medical Teacher, 32(8), 646–650. https://doi.org/10.3109/0142159X.2010.500703
Huggan, P. J., Samarasekara, D. D., Archuleta, S., Khoo, S. M., Sim, J. H. J., Sin, C. S. P., & Ooi, S. B. S. (2012). The successful, rapid transition to a new model of graduate medical education in Singapore: Academic Medicine, 87(9), 1268–1273. https://doi.org/10.1097/ACM.0b013e3182621aec
Iobst, W. F., Sherbino, J., Cate, O. T., Richardson, D. L., Dath, D., Swing, S. R., Harris, P., Mungroo, R., Holmboe, E. S., & Frank, J. R. (2010). Competency-based medical education in postgraduate medical education. Medical Teacher, 32(8), 651–656. https://doi.org/10.3109/0142159X.2010.500709
Jones, D. S. (2020). History in a crisis—Lessons for Covid-19. New England Journal of Medicine, 382(18), 1681–1683. https://doi.org/10.1056/NEJMp2004361
Kachra, R., & Ma, I. W. Y. (2020). Practical tips for faculty development workforce training under pressure in the time of COVID-19 pandemic. MedEdPublish, 9(1), 81. https://doi.org/10.15694/mep.2020.000081.1
Khoo, S. M., Lahiri, M., Huggan, P. J., Archuleta, S., Olszyna, D. P., Goh, W. P., Chua, S. W., & Ho, K. Y. (2014). When traditional model meets competencies in Singapore: Beyond conflict resolution. Annals of the Academy of Medicine Singapore, 43, 544–549.
Lee, V. J., Chiew, C. J., & Khong, W. X. (2020). Interrupting transmission of COVID-19: Lessons from containment efforts in Singapore. Journal of Travel Medicine, 27(3), 1-5. https://doi.org/10.1093/jtm/taaa039
Li, L., Xv, Q., & Yan, J. (2020). COVID-19: The need for continuous medical education and training. The Lancet Respiratory Medicine, 8(4), e23. https://doi.org/10.1016/S2213-2600(20)30125-9
Liang, Z. C., Ooi, S. B. S., & Wang, W. (2020). Pandemics and their impact on medical training: Lessons from Singapore. Academic Medicine, 95(9), 1359-1361. https://doi.org/10.1097/ACM.0000000000003441
Lim, E. C., Oh, V. M., Koh, D. R., & Seet, R. C. (2009). The challenges of “continuing medical education” in a pandemic era. Annals of the Academy of Medicine, Singapore, 38(8), 724–726.
Ministry of Health Singapore. (2020, June 1). Circuit breaker to minimise further spread of COVID-19. https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19
Nadarajah, V. D., Er, H. M., & Lilley, P. (2020). Turning around a medical education conference: Ottawa 2020 in the time of COVID‐19. Medical Education, 54(8), 760-67. https://doi.org/10.1111/medu.14197
Nasca, T. J. (2020). ACGME’s early adaptation to the COVID-19 pandemic: Principles and lessons learned. Journal of Graduate Medical Education, 12(3), 375-378. https://doi.org/10.4300/JGME-D-20-00302.1
National University of Singapore, Yong Yoo Lin School of Medicine. (2020, June 30). Curriculum structure and requirements. https://www.nus.edu.sg/nusbulletin/yong-loo-lin-school-of-medicine/undergraduate-education/degree-requirements/bachelor-of-medicine-and-bachelor-of-surgery-m-b-b-s/curriculum-structure-and-requirements
Neufeld, A., & Malin, G. (2020). Twelve tips to combat ill-being during the COVID-19 pandemic: A guide for health professionals & educators. MedEdPublish, 9(1), 70. https://doi.org/10.15694/mep.2020.000070.1
Patil, N. G., & Yan, Y. C. H. (2003). SARS and its effect on medical education in Hong Kong. Medical Education, 37(12), 1127–1128. https://doi.org/10.1046/j.1365-2923.2003.01723.x
Peeri, N. C., Shrestha, N., Rahman, M. S., Zaki, R., Tan, Z., Bibi, S., Baghbanzadeh, M., Aghamohammadi, N., Zhang, W., & Haque, U. (2020). The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? International Journal of Epidemiolology, 49(3), 717-720. https://doi.org/10.1093/ije/dyaa033
Rose, S. (2020). Medical student education in the time of COVID-19. The Journal of the American Medical Association, 323(21), 2131-2132. https://doi.org/10.1001/jama.2020.5227
Samarasekera, D. D., Goh, D., & Lau, T. C. (2020). Medical school approach to manage the current COVID-19 crisis. Academic Medicine: Journal of the Association of American Medical Colleges, 95(8), 1126–1127. https://doi.org/10.1097/ACM.0000000000003425
Sandars, J., Correia, R., Dankbaar, M., de Jong, P., Goh, P. S., Hege, I., Masters, K., Oh, S.-Y., Patel, R., Premkumar, K., Webb, A., & Pusic, M. (2020). Twelve tips for rapidly migrating to online learning during the COVID-19 pandemic. MedEdPublish, 9(1), 82. https://doi.org/10.15694/mep.2020.000082.1
Schwartz, A. M., Wilson, J. M., Boden, S. D., Moore, T. J., Bradbury, T. L., & Fletcher, N. D. (2020). Managing resident workforce and education during the COVID-19 pandemic: Evolving strategies and lessons learned. Journal of Bone & Joint Surgery Open Access, 5(2), 1-5. https://doi.org/10.2106/JBJS.OA.20.00045
Seah, I. (2020). Striving as a nation to become an academic leader in the COVID-19 crisis. Singapore Medical Journal, 61(7), 370-372. https://doi.org/10.11622/smedj.2020059
Singapore Medical Council (2020a, May 29). Continuing medical education (CME) for doctors. https://www.healthprofessionals.gov.sg/smc/continuing-medical-education-(cme)-for-doctors
Singapore Medical Council (SMC) (2020b, May 29). Fulfilling continuing medical education (CME) requirements via online platforms. https://www.healthprofessionals.gov.sg/docs/librariesprovider2/continuing-medical-education-(cme)-for-doctors/circular—fulfilling-cme-requirements-via-online-platforms.pdf
Stetson, G. V., Kryzhanovskaya, I. V., Lomen‐Hoerth, C., & Hauer, K. E. (2020). Professional identity formation in disorienting times. Medical Education, 54(8), 765-766. https://doi.org/10.1111/medu.14202
Tolu, L. B., Feyissa, G. T., Ezeh, A., & Gudu, W. (2020). Managing Resident Workforce and residency training during COVID-19 pandemic: Scoping review of adaptive approaches. Advances in Medical Education and Practice, 11, 527–535. https://doi.org/10.3171/2020.4.JNS201012
Wald, H. S. (2020). Optimizing resilience and wellbeing for healthcare professions trainees and healthcare professionals during public health crises—Practical tips for an ‘integrative resilience’ approach. Medical Teacher, 42(7), 744-755. https://doi.org/10.1080/0142159X.2020.1768230
Wong, C., Tay, W., Hap, X., & Chia, F. (2020). Love in the time of coronavirus: Training and service during COVID-19. Singapore Medical Journal, 61(7), 384-386. https://doi.org/10.11622/smedj.2020053
Wong, J. E. L., Leo, Y. S., & Tan, C. C. (2020). COVID-19 in Singapore—current experience: Critical global issues that require attention and action. The Journal of the American Medical Association, 323(13), 1243. https://doi.org/10.1001/jama.2020.2467
Yang, D.-Y., Cheng, S.-Y., Wang, S.-Z., Wang, J.-S., Kuang, M., Wang, T.-H., & Xiao, H.-P. (2020). Preparedness of medical education in China: Lessons from the COVID-19 outbreak. Medical Teacher, 42(7), 787-790. https://doi.org/10.1080/0142159X.2020.1770713
*Claude J Renaud
Department of Medicine,
Division of Renal Medicine,
Khoo Teck Puat Hospital,
90 Yishun Central, Singapore 768828
Email: jeffrey.renaud@ktph.com.sg
Submitted: 4 August 2020
Accepted: 14 October 2020
Published online: 4 May, TAPS 2021, 6(2), 1-8
https://doi.org/10.29060/TAPS.2021-6-2/RA2370
Tow Keang Lim
Department of Medicine, National University Hospital, Singapore
Abstract
Introduction: Clinical diagnosis is a pivotal and highly valued skill in medical practice. Most current interventions for teaching and improving diagnostic reasoning are based on the dual process model of cognition. Recent studies which have applied the popular dual process model to improve diagnostic performance by “Cognitive De-biasing” in clinicians have yielded disappointing results. Thus, it may be appropriate to also consider alternative models of cognitive processing in the teaching and practice of clinical reasoning.
Methods: This is critical-narrative review of the predictive brain model.
Results: The theory of predictive brains is a general, unified and integrated model of cognitive processing based on recent advances in the neurosciences. The predictive brain is characterised as an adaptive, generative, energy-frugal, context-sensitive action-orientated, probabilistic, predictive engine. It responds only to predictive errors and learns by iterative predictive error management, processing and hierarchical neural coding.
Conclusion: The default cognitive mode of predictive processing may account for the failure of de-biasing since it is not thermodynamically frugal and thus, may not be sustainable in routine practice. Exploiting predictive brains by employing language to optimise metacognition may be a way forward.
Keywords: Diagnosis, Bias, Dual Process Theory, Predictive Brains
Practice Highlights
- According to the dual process model of cognition diagnostic errors are caused by bias reasoning.
- Interventions to improve diagnosis based on “Cognitive De-biasing” methods report disappointing results.
- The predict brain is a unified model of cognition which accounts for diagnostic errors, the failure of “Cognitive De-biasing” and may point to effective solutions.
- Using appropriate language as simple rules or thumb, to fine-tune predictive processing meta-cognitively may be a practical strategy to improve diagnostic problem solving.
I. INTRODUCTION
Clinical diagnostic expertise is a critical, highly valued, and admired skill (Montgomery, 2006). However, diagnostic errors are common and important adverse events which merit research and effective prevention (Gupta et al., 2017; Singh et al., 2014; Skinner et al., 2016). Thus, it is now widely acknowledged and recognized that concerted efforts are required to improve the research, training and practice of clinical reasoning in improving diagnosis (Simpkin et al., 2017; Singh & Graber, 2015; Zwaan et al., 2013). The consensus among practitioners, researchers and preceptors is that most preventable diagnostic errors are associated with bias reasoning during rapid, non-analytical, default cognitive processing of clinical information (Croskerry, 2013). The most widely held theory which accounts for this observation is the dual process model of cognition (B. Djulbegovic et al., 2012; Evans, 2008; Schuwirth, 2017). It posits that most diagnostic errors reside in intuitive, non-analytical or systems 1 thinking (Croskerry, 2009). Thus, the logical, practical and common sense implication which follows from this assumption is that we should activate and apply analytical or system 2 thinking to counter-check or “De-bias” system 1 errors (Croskerry, 2009). This is a popular notion and it has facilitated the emergence of many schools of clinical reasoning based on training methods designed to deliberately understand, recognise, categorise and avoid specific diagnostic errors arising from system thinking 1 or cognitive bias (Reilly et al., 2013; Rencic et al., 2017; Restrepo et al., 2020). However, careful research on the merits of these interventions under controlled conditions do not show consistent nor clear benefits (G. Norman et al., 2014; G. R. Norman et al., 2017; O’Sullivan & Schofield, 2019; Sherbino et al., 2014; Sibbald et al., 2019; J. N. Walsh et al., 2017). Moreover, even the recognition and categorization of these cognitive error events themselves are deeply confounded by hindsight bias itself (Zwaan et al., 2016). Perhaps, at this juncture, it might be appropriate to consider alternative models of cognition based on advances in multi-disciplinary neuroscience research which have expanded greatly in recent years (Monteiro et al., 2020).
Over the past decade the theory of predictive brains has emerged as an ambitious, unified, convergent and integrated model of cognitive processing from research in a large variety of core domains in cognition which include philosophy, meta-physics, cellular physics, thermodynamics, Associative Learning theory, Bayesian-probability theory, Information theory, machine learning, artificial intelligence, behavioural science, neuro-cognition, neuro-imaging, constructed emotions and psychiatry (Bar, 2011; Barrett, 2017a; Barrett, 2017b; Clark, 2016; Friston, 2010; Hohwy, 2013; Seligman, 2016; Teufel & Fletcher, 2020). It may have profound and practical implications on how we live, work and learn. However, to my knowledge, there is almost no discussion of this novel proposition in either medical education pedagogy or research. Thus, in this presentation I will review recent developments in the predictive brain model of cognition, map its key elements which impacts on pedagogy and research in medical education and propose an application in the training of diagnostic reasoning based on it.
An early version of this work had been presented as an abstract (Lim & Teoh, 2018).
II. METHODS
This is a critical-narrative review of the predictive brain model from Friston’s “The free energy principle” proposition a decade ago to more recent critical examination of the emerging supportive evidence based on neurophysiological studies over the past 5 years (Friston, 2010; K. S. Walsh et al., 2020).
III. RESULTS
A. The Brain is a Frugal Predictive Engine
The Brain Is A Frugal Predictive Engine (General references (Bar, 2011; Barrett, 2017a; Barrett, 2017b; Clark, 2013; Clark, 2016; Friston, 2010; Gilbert & Wilson, 2007; Hohwy, 2013; Seligman, 2016; Seth et al., 2011; Sterling, 2012).
In contrast with traditional top-down, feed-forward models of cognition, the predictive brain model reverses and inverts this process. Perception is characterised as an entirely inferential rapidly adaptive, generative, energy-frugal, context-sensitive action-orientated, probabilistic, predictive process (Tschantz et al., 2020). This system is governed by the need to respond rapidly to ever changing demands from the external environmental and our body’s internal physiological signals (intero-ception) and yet minimise free energy expenditure (or waste) (Friston, 2010; Kleckner et al., 2017; Sterling, 2012). Thus, it is not passive and reactive to new information but predictive and continuously proactive. From very early, elemental and sparse cues it is continuously generating predictive representations based on remembered similar experiences in the past which may include simulations. It performs iterative matching of top down prior representations with bottom up signals and cues in a hierarchy of categories of abstractions and content specificity over scales of space and time (Clark, 2013; Friston & Kiebel, 2009; Spratling, 2017a). This matching process is also sensitive to variations in context and thus enable us to make sense of rapidly changing and complex situations (Clark, 2016).
Cognitive resource, in terms of allocating attention, is only focused on the management of errors in prediction or the mismatch between prior representations and new emergent information. It seeks to minimise prediction errors (PEs) and there is repetitive, recognition-expectation-based signal suppression when this is achieved. Thus, this is a system which only responds to the unfamiliar situation or what it considers as news worthy. This is analogous to Claude Shannons’s classic analysis of “surprisals” in information theory (Shannon et al., 1993). Learning is based on the generation and neural coding of a new predictive representations in memory. The most direct and powerful evidence for this process comes from optogenetic experiments with their exquisitely high degree of resolution in the monitoring and manipulations over space-time of neuronal signalling and behaviour in freely forging rats which show causal linkages between PE, dopamine neurons and learning (Nasser et al., 2017; Steinberg et al., 2013).
The brain intrinsically generates representations of the world in which it finds itself from past experience which is refined by sensory data. New sensory information is represented and inferred in terms of these known causes. Determining which combination of the many possible causes best fits the current sensory data is achieved through a process of minimising the error between the sensory data and the sensory inputs predicted by the expected causes, i.e. the PE. In the service of PE reduction, the brain will also generate motor actions such as saccadic eye movement and foraging behaviour. The prediction arises from a process of “backwards thinking” or inferential Bayesian best guess or approximation based simultaneously on sensory data and prior experience (Chater & Oaksford, 2008; Kersten et al., 2004; Kwisthout et al., 2017a; Kwisthout et al., 2017b; Ting et al., 2015). It is a hierarchical predictive coding process, reflecting the serial organization of the neuronal architecture of cerebral cortex; higher levels are abstract, whereas the lowest level amounts to a prediction of the incoming sensory data (Kolossa et al., 2015; Shipp, 2016; Ting et al., 2015). The actual sensory data is compared to the predicted sensory data, and it is the discrepancies, or ‘error’ that ascends up the hierarchy to refine all higher levels of abstraction in the model. Thus, this is a learning process whereby, with each iteration, the model representations are optimised and encoded in long term memory as the PEs minimise (Friston, FitzGerald, Rigoli et al., 2017; Spratling, 2017b).
This system of neural responses is regulated and fine-tuned by varying the gains on the weightage of the reliability (or precision) of the PE estimate itself. In other words, it is the level of confidence (versus uncertainty) in the PE which determines the intensity of attention allocated to it and strength of coding in memory following its resolution (Clark, 2013; Clark, 2016; Feldman & Friston, 2010; Hohwy, 2013). This regulatory, neuro-modulatory process is impacted by the continuous cascade of action relevant information which is sensitive to both external context and internal interoceptive (i.e. from perception of our own physiological responses) and affective signals (Clark, 2016). This metacognitive capacity to effectively manipulate and re-calibrate the precision of PE itself may be a critical aspect of decision making, problem solving behaviour and learning. (Hohwy, 2013; Picard & Friston, 2014).
B. Clinical Reasoning is Predictive Error Processing and Learning is Predictive Coding
The core processes of the predictive brain which are engaged during diagnostic reasoning are summarised in Table 1 and Figure 1.
|
Core features of the predictive brain model |
Clinical reasoning features and processes |
|
The frugal brain and free energy principle(Friston, 2010) |
Cognitive load in problem solving (Young et al., 2014)
|
|
Iterative matching of top down priors Vs bottom up signals |
Inductive foraging (Donner-Banzhoff & Hertwig, 2014; Donner-Banzhoff et al., 2017) |
|
Predictive error processing |
Pattern recognition in diagnosis |
|
Recognition-expectation-based signal suppression |
Premature closure (Blissett & Sibbald, 2017; Melo et al., 2017) |
|
Hierarchical predictive error coding as learning |
Development of illness scripts (Custers, 2014) |
|
Probabilistic-Bayesian inferential approximations |
Bayesian inference in clinical reasoning |
|
Context sensitivity |
Contextual factors in diagnostic errors(Durning et al., 2010) |
|
Action orientation |
Foraging behaviour in clinical diagnosis (Donner-Banzhoff & Hertwig, 2014; Donner-Banzhoff et al., 2017) |
|
Interoception and affect in prediction error management |
Gut feel and regret (metacognition) |
|
The precision(reliability/uncertainty) of prediction errors |
Clinical uncertainty (metacognition) (Bhise et al., 2017; Simpkin & Schwartzstein, 2016) |
Table 1: Core features of the predictive brain model of cognition manifested as clinical reasoning processes
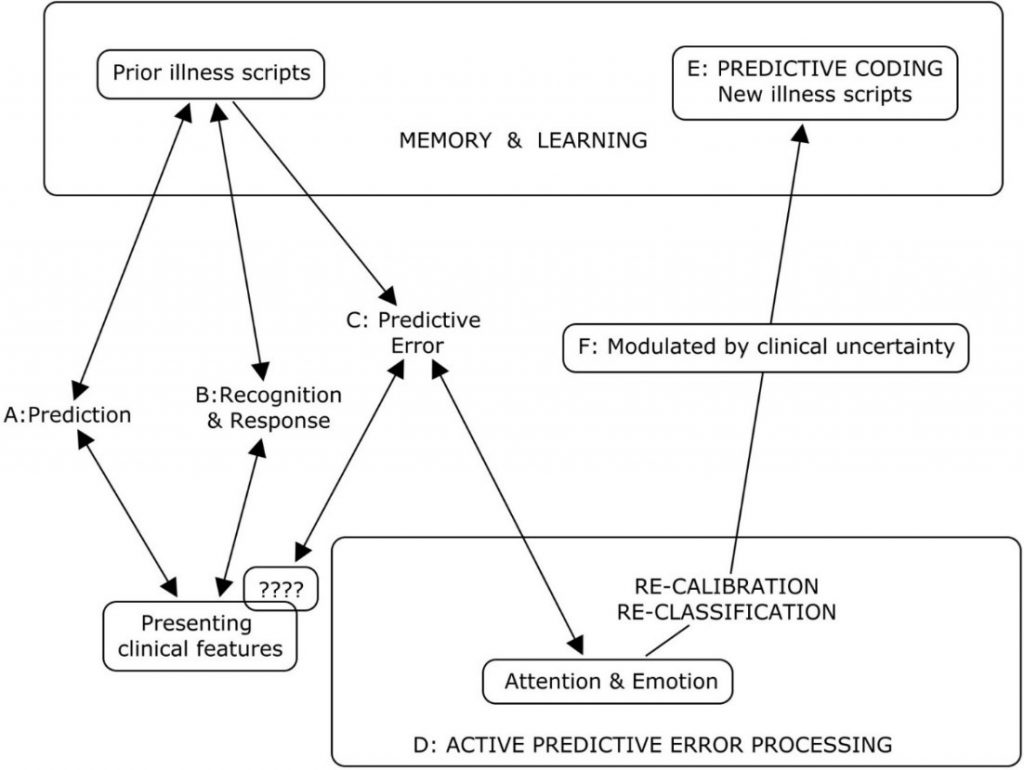
Legend to Figure 1
A summary of the cognitive processes engaged by the predict brain model during clinical diagnosis
A: Active search for diagnostic clues based on prior experience of similar patients in similar situations.
B: Recognition of key features will activate a series of familiar illness script from long term memory to match with the new case. If this is successful, a diagnosis made and any prediction error signals are rapidly silenced.
C & D: When the illness scripts do not match the presenting features (????), cognition slows down, attention is heightened and further searches are made for additional matching clues and illness scripts. This is iterated until a satisfactory match is found or a new illness script is generated to account for the mismatch.
E: A new variation in the presenting features for that disease is then encoded in memory as a new illness script in memory and thus, a valuable learning moment.
F: The degree of uncertainty or level of confidence in matching key presenting features to a diagnosis is a meta-cognitive skill and a critical expertise in clinical diagnosis. This corresponds to the precision or gain/weightage of prediction errors (Meta cognition) in the predictive brain model.
Figure 1: A summary of the cognitive processes engaged by the predict brain model during clinical diagnosis
Thermodynamic frugality is a central feature of the predictive brain model and in this system, the primacy of attending only to surprises or PEs is pivotal (Friston, 2010). This might be regard as an energy efficient strategy in coping with cognitive load which has been long recognised as an important consideration in clinical problem solving and learning (Young et al., 2014; Van Merrienboer & Sweller, 2010).
From the first moments of a diagnostic encounter the clinician is alert to clues which might point to the diagnosis and begins to generate possible diagnosis scenarios and simulations based upon her prior experience of similar patients and situations (Donner-Banzhoff & Hertwig, 2014). This is iterative and, from a scanty set of presenting features, a plausible diagnosis may be considered within a few seconds to minutes (Donner-Banzhoff & Hertwig, 2014; Donner-Banzhoff et al., 2017). Thus, a familiar illness script is activated from long term memory to match with the new case (Custers, 2014). If this is successful, a particular diagnosis is recognised and any PE signal is rapidly silenced. Functional MRI studies of clinicians during this process showed that highly salient diagnostic information, reducing uncertainty about the diagnosis, rapidly decreased monitoring activity in the frontoparietal attentional network and may contribute to premature diagnostic closure, an important cause of diagnostic errors (Melo et al., 2017). This may be considered a form of diagnosis or recognition related PE signal suppression analogous to the well know phenomenon of repetitive suppression (Blissett & Sibbald, 2017; Bunzeck & Thiel, 2016; Krupat et al., 2017).
In cases where the illness scripts do not match the presenting features, a PE event is encountered, cognition slows down, attention is heightened and further searches are made for additional matching clues and illness scripts (Custers, 2014). This is iterated until a satisfactory match is found or a new illness script is generated to account for the mismatch. This is then encoded in memory as a new variation in the presenting features for that disease and thus, a valuable learning moment. Bayesian inference is a fundamental feature of both clinical diagnostic reasoning and the predictive brain model (Chater & Oaksford, 2008).
As in the predictive brain model, external contextual factors and internal emotional and physiological responses such as gut feeling and regret, exert profound effects on clinical decision making (M. Djulbegovic et al., 2015; Durning et al., 2010; Stolper & van de Wiel, 2014; Stolper et al., 2014). Also active inductive foraging behaviour in searching for diagnostic clues described in experienced primary physicians is analogous to behaviour directed at reducing PEs (Donner-Banzhoff & Hertwig, 2014; Donner-Banzhoff et al., 2017). The precision or gain/weightage of PEs is manifested metacognitively as uncertainties or levels of confidence in clinical reasoning (Sandved-Smith et al., 2020). Metacognition is a critical capacity and expertise in effective decision making. (Bhise et al., 2017; Fleming & Frith, 2014; Simpkin & Schwartzstein, 2016).
C. Why Applying the Dual Process Model May Not Improve Clinical Reasoning
Recent studies which have applied the popular dual process model to improve diagnostic performance by “cognitive de-biasing” in clinicians have yielded disappointing results (G. R. Norman et al., 2017). Cognitive processing of the predictive brain as the dominant default network mode of operation may account for this setback since de-biasing is not naturistic, requires retrospective “off line” processing after the monitoring salience network has already shut off (Krupat et al., 2017; Melo et al., 2017). It is not thermodynamically frugal and thus, may not be sustainable in routine practice (Friston, 2010; Young et al., 2014). Even Daniel Kahneman himself admits that, despite decades of research in cognitive bias he is unable to exert agency of the moment and de-bias himself (Kahneman, 2013). This will be more so in novice diagnosticians in the training phase who have scanty illness scripts and limited tolerance of any further cognitive loading (Young et al., 2014). The failure to even identify cognitive biases reliably by clinicians due to hindsight bias itself suggests that this intervention will be the least effective one in improving diagnostic reasoning (Zwaan et al., 2016).
D. Using Words to Fine Tune the Precision of Diagnostic Prediction Error
Daniel Kahneman, the foremost expert on cognitive bias, cautions that, contrary to what some experts in medical education advice, avoiding bias is ineffective in improving decision making under uncertainty (Restrepo et al., 2020). By contrast he suggested that we apply simple, common sense, rules of thumb (Kahneman et al., 2016). I hypothesise that instructing clinical trainees to use appropriate words to self in the diagnostic setting during active, naturalistic PE processing before the diagnosis is made and not as a retrospective counter check to cognition afterwards may be a way forward (Betz et al., 2019; Clark, 2016; Lupyan, 2017). In a multi-center, iterative thematic content analysis of over 2,000 cases of diagnostic errors with a structured taxonomy, Schiff and colleagues identified a limited number of pitfall themes which were overlooked and predisposed physicians to reasoning errors (Reyes Nieva H et al., 2017). These pitfall themes included three which are of particular interest in relation to naturalistic PE processing namely: (1) counter diagnostic cues, (2) things that do not fit and (3) red flags (Reyes Nieva H et al., 2017). Thus, we instructed our student interns and internal medicine residents to pay particular attend to these three diagnostic pitfalls during review of new patients and clinical problems (Lim & Teoh, 2018). They were required to append the following sub-headings to their clerking impression in the patient’s electronic health record (eHR): (a) Counter diagnostic features; (b) Things that do not fit; (c) Red flags. This template was added after the resident had entered his or her numerated list of diagnoses or issues. “Counter diagnostic features” was defined as symptoms, signs or investigations which were inconsistent with the proposed primary diagnosis. “Things that do not fit” was defined as any finding that could not be reasonably accounted for taking into account the main and differential diagnoses. “Red flags” were defined as findings which raised the possibility of a more serious underlying illness requiring early diagnosis or intervention. The attending physicians were required, during bedside rounds, to give feedback on these points and make amendments to the eHR as appropriate. This exercise may give us an opportunity to see if we can improve diagnostic accuracy by using pivotal words-to-self in the appropriate setting to maintain cognitive openness, flexibility and thus, avoid premature (Krupat et al., 2017). It is also a valuable critical, metacognitive thinking habit to inculcate in tyro diagnosticians (Carpenter et al., 2019).
IV. CONCLUSION
The theory of predictive brains has emerged as a major narrative in the understanding of how our mind works. It may account for the limitations of interventions designed to improve diagnostic problem solving which are based on the dual process theory of cognition. Exploiting predictive brains by employing language to optimise metacognition may be a way forward.
Note on Contributor
Lim designed the paper, reviewed the literature, drafted and revised it.
Ethical Approval
There is no ethical approval associated with this paper.
Funding
No funding sources are associated with this paper.
Declaration of Interest
No conflicts of interest are associated with this paper.
References
Bar, M. (2011). Predictions in the brain using our past to generate a future (pp. xiv, 383 p. ill. (some col.) 327 cm.).
Barrett, L. F. (2017a). How emotions are made: the secret life of the brain. Houghton Mifflin Harcourt.
Barrett, L. F. (2017b). The theory of constructed emotion: An active inference account of interoception and categorization. Social Cognitive and Affective Neuroscience, 12(1), 1-23. https://doi.org/10.1093/scan/nsw154
Betz, N., Hoemann, K., & Barrett, L. F. (2019). Words are a context for mental inference. Emotion, 19(8), 1463-1477. https://doi.org/10.1037/emo0000510
Bhise, V., Rajan, S. S., Sittig, D. F., Morgan, R. O., Chaudhary, P., & Singh, H. (2017). Defining and measuring diagnostic uncertainty in medicine: A systematic review. Journal of General Internal Medicine 33, 103–115. https://doi.org/10.1007/s11606-017-4164-1
Blissett, S., & Sibbald, M. (2017). Closing in on premature closure bias. Medical Education, 51(11), 1095-1096. https://doi.org/10.1111/medu.13452
Bunzeck, N., & Thiel, C. (2016). Neurochemical modulation of repetition suppression and novelty signals in the human brain. Cortex, 80, 161-173. https://doi.org/10.1016/j.cortex.2015.10.013
Carpenter, J., Sherman, M. T., Kievit, R. A., Seth, A. K., Lau, H., & Fleming, S. M. (2019). Domain-general enhancements of metacognitive ability through adaptive training. Journal of Experimental Psychology. General, 148(1), 51-64. https://doi.org/10.1037/xge0000505
Chater, N., & Oaksford, M. (2008). The probabilistic mind : prospects for Bayesian cognitive science. Oxford University Press.
Clark, A. (2013). Whatever next? Predictive brains, situated agents, and the future of cognitive science. The Behavioral and Brain Sciences, 36(3), 181–204. https://doi.org/10.1017/S0140525X12000477
Clark, A. (2016). Surfing uncertainty : Prediction, action, and the embodied mind: Oxford University Press.
Croskerry, P. (2009). Clinical cognition and diagnostic error: Applications of a dual process model of reasoning. Advances in Health Sciences Education : Theory and Practice, 14 Suppl 1, 27–35. https://doi.org/10.1007/s10459-009-9182-2
Croskerry, P. (2013). From mindless to mindful practice–cognitive bias and clinical decision making. The New England Journal of Medicine, 368(26), 2445–2448. https://doi.org/10.1056/NEJMp1303712
Custers, E. J. (2014). Thirty years of illness scripts: Theoretical origins and practical applications. Medical Teacher, 1-6. https://doi.org/10.3109/0142159X.2014.956052
Djulbegovic, B., Hozo, I., Beckstead, J., Tsalatsanis, A., & Pauker, S. G. (2012). Dual processing model of medical decision-making. BMC Medical Informatics and Decision Making, 12, 94. https://doi.org/10.1186/1472-6947-12-94
Djulbegovic, M., Beckstead, J., Elqayam, S., Reljic, T., Kumar, A., Paidas, C., & Djulbegovic, B. (2015). Thinking styles and regret in physicians. Public Library of Science One, 10(8), e0134038. https://doi.org/10.1371/journal.pone.0134038
Donner-Banzhoff, N., & Hertwig, R. (2014). Inductive foraging: Improving the diagnostic yield of primary care consultations. European Journal of General Practice, 20(1), 69–73. https://doi.org/10.3109/13814788.2013.805197
Donner-Banzhoff, N., Seidel, J., Sikeler, A. M., Bosner, S., Vogelmeier, M., Westram, A., & Gigerenzer, G. (2017). The phenomenology of the diagnostic process: A primary care-based survey. Medical Decision Making, 37(1), 27-34. https://doi.org/10.1177/0272989X16653401
Durning, S. J., Artino, A. R., Jr., Pangaro, L. N., van der Vleuten, C., & Schuwirth, L. (2010). Perspective: redefining context in the clinical encounter: Implications for research and training in medical education. Academic Medicine: Journal of the Association of American Medical Colleges, 85(5), 894–901. https://doi.org/10.1097/ACM.0b013e3181d7427c
Evans, J. S. (2008). Dual-processing accounts of reasoning, judgment, and social cognition. Annual Review of Psychology, 59, 255–278. https://doi.org/10.1146/annurev.psych.59.103006.093629
Feldman, H., & Friston, K. J. (2010). Attention, uncertainty, and free-energy. Frontiers in Human Neuroscience, 4, 215. https://doi.org/10.3389/fnhum.2010.00215
Fleming, S. M., & Frith, C. D. (2014). The cognitive neuroscience of metacognition. Springer.
Friston, K. (2010). The free-energy principle: A unified brain theory? Nature Reviews. Neuroscience, 11(2), 127–138. https://doi.org/10.1038/nrn2787
Friston, K., FitzGerald, T., Rigoli, F., Schwartenbeck, P., & Pezzulo, G. (2017). Active inference: A process theory. Neural Computation, 29(1), 1–49. https://doi.org/10.1162/NECO_a_00912
Friston, K., & Kiebel, S. (2009). Predictive coding under the free-energy principle. Philosophical Transactions of the Royal Society of London. Series B, Biological sciences, 364(1521), 1211–1221. https://doi.org/10.1098/rstb.2008.0300
Gilbert, D. T., & Wilson, T. D. (2007). Prospection: Experiencing the future. Science, 317(5843), 1351-1354. https://doi.org/10.1126/science.1144161
Gupta, A., Snyder, A., Kachalia, A., Flanders, S., Saint, S., & Chopra, V. (2017). Malpractice claims related to diagnostic errors in the hospital. BMJ Quality and Safety, 27(1), 53-60. https://doi.org/10.1136/bmjqs-2017-006774
Hohwy, J. (2013). The predictive mind. Oxford University Press..
Kahneman, D. (2013). Thinking, fast and slow (1st pbk. ed.). Farrar, Straus and Giroux.
Kahneman, D., Rosenfield, A. M., Gandhi, L., & Blaser, T. O. M. (2016). NOISE: How to overcome the high, hidden cost of inconsistent decision making. (cover story). Harvard Business Review, 94(10), 38-46. Retrieved from http://libproxy1.nus.edu.sg/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=buh&AN=118307773&site=ehost-live
Kersten, D., Mamassian, P., & Yuille, A. (2004). Object perception as bayesian inference. Annual Review of Psychology, 55, 271–304. https://doi.org/10.1146/annurev.psych.55.090902.142005
Kleckner, I. R., Zhang, J., Touroutoglou, A., Chanes, L., Xia, C., Simmons, W. K., & Feldman Barrett, L. (2017). Evidence for a large-scale brain system supporting allostasis and interoception in humans. Nature Human Behaviour, 1, 0069. https://doi.org/10.1038/s41562-017-0069
Kolossa, A., Kopp, B., & Fingscheidt, T. (2015). A computational analysis of the neural bases of Bayesian inference. Neuroimage, 106, 222-237. https://doi.org/10.1016/j.neuroimage.2014.11.007
Krupat, E., Wormwood, J., Schwartzstein, R. M., & Richards, J. B. (2017). Avoiding premature closure and reaching diagnostic accuracy: Some key predictive factors. Medical Education, 51(11), 1127-1137. https://doi.org/10.1111/medu.13382
Kwisthout, J., Bekkering, H., & van Rooij, I. (2017a). To be precise, the details don’t matter: On predictive processing, precision, and level of detail of predictions. Brain and Cognition, 112, 84–91. https://doi.org/10.1016/j.bandc.2016.02.008
Kwisthout, J., Phillips, W. A., Seth, A. K., van Rooij, I., & Clark, A. (2017b). Editorial to the special issue on perspectives on human probabilistic inference and the ‘Bayesian brain’. Brain and Cognition, 112, 1-2. https://doi.org/10.1016/j.bandc.2016.12.002
Lim T.K., & Teoh, C. M. (2018). Exploiting predictive brains for better diagnosis. Diagnosis (Berl), 5(3), eA40. Retrieved from https://www.degruyter.com/view/journals/dx/5/3/article-peA1.xml
Lupyan, G. (2017). Changing what you see by changing what you know: The role of attention. Frontiers in Psychology, 8, 553. https://doi.org/10.3389/fpsyg.2017.00553
Melo, M., Gusso, G. D. F., Levites, M., Amaro, E., Jr., Massad, E., Lotufo, P. A., & Friston, K. J. (2017). How doctors diagnose diseases and prescribe treatments: An fMRI study of diagnostic salience. Scientific Reports, 7(1), 1304. http://observatorio.fm.usp.br/handle/OPI/19951
Monteiro, S., Sherbino, J., Sibbald, M., & Norman, G. (2020). Critical thinking, biases and dual processing: The enduring myth of generalisable skills. Medical Education, 54(1), 66-73. https://doi.org/10.1111/medu.13872
Montgomery, K. (2006). How doctors think: Clinical judgement and the practice of medicine. Oxford University Press.
Nasser, H. M., Calu, D. J., Schoenbaum, G., & Sharpe, M. J. (2017). The dopamine prediction error: Contributions to associative models of reward learning. Frontiers in Psychology, 8, 244. https://doi.org/10.3389/fpsyg.2017.00244
Norman, G., Sherbino, J., Dore, K., Wood, T., Young, M., Gaissmaier, W., & Monteiro, S. (2014). The etiology of diagnostic errors: A controlled trial of system 1 versus system 2 reasoning. Academic Medicine: Journal of the Association of American Medical Colleges, 89(2), 277–284. https://doi.org/10.1097/ACM.0000000000000105
Norman, G. R., Monteiro, S. D., Sherbino, J., Ilgen, J. S., Schmidt, H. G., & Mamede, S. (2017). The Causes of Errors in Clinical Reasoning: Cognitive Biases, Knowledge Deficits, and Dual Process Thinking. Academic Medicine: Journal of the Association of American Medical Colleges, 92(1), 23–30. https://doi.org/10.1097/ACM.0000000000001421
O’Sullivan, E. D., & Schofield, S. J. (2019). A cognitive forcing tool to mitigate cognitive bias – A randomised control trial. BMC Medical Education, 19(1), 12. https://doi.org/10.1186/s12909-018-1444-3
Picard, F., & Friston, K. (2014). Predictions, perception, and a sense of self. Neurology, 83(12), 1112-1118. https://doi.org/10.1212/WNL.0000000000000798
Reilly, J. B., Ogdie, A. R., Von Feldt, J. M., & Myers, J. S. (2013). Teaching about how doctors think: A longitudinal curriculum in cognitive bias and diagnostic error for residents. BMJ Quality & Safety, 22(12), 1044–1050. https://doi.org/10.1136/bmjqs-2013-001987
Rencic, J., Trowbridge, R. L., Jr., Fagan, M., Szauter, K., & Durning, S. (2017). Clinical reasoning education at us medical schools: Results from a national survey of internal medicine clerkship directors. Journal of General Internal Medicine, 32(11), 1242–1246. https://doi.org/10.1007/s11606-017-4159-y
Restrepo, D., Armstrong, K. A., & Metlay, J. P. (2020). Annals Clinical Decision Making: Avoiding Cognitive Errors in Clinical Decision Making. Annals of Internal Medicine, 172(11), 747–751. https://doi.org/10.7326/M19-3692
Reyes Nieva H., V. M., Wright A, Singh H, Ruan E, Schiff G. (2017). Diagnostic Pitfalls: A New Approach to Understand and Prevent Diagnostic Error. In Diagnosis (Vol. 4, pp. eA1). https://www.degruyter.com/view/journals/dx/5/4/article-peA59.xml
Sandved-Smith, L., Hesp, C., Lutz, A., Mattout, J., Friston, K., & Ramstead, M. (2020, June 10). Towards a formal neurophenomenology of metacognition: Modelling meta-awareness, mental action, and attentional control with deep active inference. https://doi.org/10.31234/osf.io/5jh3c
Schuwirth, L. (2017). When I say … dual-processing theory. Medical Education, 51(9), 888–889. https://doi.org/10.1111/medu.13249
Seligman, M. E. P. (2016). Homo Prospectus. Oxford University Pres.
Seth, A. K., Suzuki, K., & Critchley, H. D. (2011). An interoceptive predictive coding model of conscious presence. Frontiers in Psychology, 2, 395. https://doi.org/10.3389/fpsyg.2011.00395
Shannon, C. E., Sloane, N. J. A., Wyner, A. D., & IEEE Information Theory Society. (1993). Claude Elwood Shannon : Collected Papers. IEEE Press.
Sherbino, J., Kulasegaram, K., Howey, E., & Norman, G. (2014). Ineffectiveness of cognitive forcing strategies to reduce biases in diagnostic reasoning: A controlled trial. Canadian Journal of Emergency Medicine, 16(1), 34–40. https://doi.org/10.2310/8000.2013.130860
Shipp, S. (2016). Neural Elements for Predictive Coding. Frontiers in Psychology, 7, 1792. https://doi.org/10.3389/fpsyg.2016.01792
Sibbald, M., Sherbino, J., Ilgen, J. S., Zwaan, L., Blissett, S., Monteiro, S., & Norman, G. (2019). Debiasing versus knowledge retrieval checklists to reduce diagnostic error in ECG interpretation. Advances in Health Sciences Education: Theory and Practice, 24(3), 427–440. https://doi.org/10.1007/s10459-019-09875-8
Simpkin, A. L., & Schwartzstein, R. M. (2016). Tolerating uncertainty – The next medical revolution? The New England Journal of Medicine, 375(18), 1713–1715. https://doi.org/10.1056/NEJMp1606402
Simpkin, A. L., Vyas, J. M., & Armstrong, K. A. (2017). Diagnostic Reasoning: An endangered competency in internal medicine training. Annals of Internal Medicine, 167(7), 507–508. https://doi.org/10.7326/M17-0163
Singh, H., & Graber, M. L. (2015). Improving diagnosis in health care- The next imperative for patient safety. The New England Journal of Medicine, 373(26), 2493–2495. https://doi.org/10.1056/NEJMp1512241
Singh, H., Meyer, A. N., & Thomas, E. J. (2014). The frequency of diagnostic errors in outpatient care: Estimations from three large observational studies involving US adult populations. BMJ Quality & Safety, 23(9), 727–731. https://doi.org/10.1136/bmjqs-2013-002627
Skinner, T. R., Scott, I. A., & Martin, J. H. (2016). Diagnostic errors in older patients: A systematic review of incidence and potential causes in seven prevalent diseases. International Journal of General Medicine, 9, 137–146. https://doi.org/10.2147/IJGM.S96741
Spratling, M. W. (2017a). A hierarchical predictive coding model of object recognition in natural images. Cognitive Computation, 9(2), 151–167. https://doi.org/10.1007/s12559-016-9445-1
Spratling, M. W. (2017b). A review of predictive coding algorithms. Brain and Cognition, 112, 92–97. https://doi.org/10.1016/j.bandc.2015.11.003
Steinberg, E. E., Keiflin, R., Boivin, J. R., Witten, I. B., Deisseroth, K., & Janak, P. H. (2013). A causal link between prediction errors, dopamine neurons and learning. Nature Neuroscience, 16(7), 966–973. https://doi.org/10.1038/nn.3413
Sterling, P. (2012). Allostasis: A model of predictive regulation. Physiology & Behavior, 106(1), 5–15. https://doi.org/10.1016/j.physbeh.2011.06.0044
Stolper, C. F., & van de Wiel, M. W. (2014). EBM and gut feelings. Medical Teacher, 36(1), 87-88. https://doi.org/10.3109/0142159X.2013.835390
Stolper, C. F., Van de Wiel, M. W., Hendriks, R. H., Van Royen, P., Van Bokhoven, M. A., Van der Weijden, T., & Dinant, G. J. (2014). How do gut feelings feature in tutorial dialogues on diagnostic reasoning in GP traineeship? Advances in Health Sciences Education: Theory and Practice, 20(2), 499–513. https://doi.org/10.1007/s10459-014-9543-3
Teufel, C., & Fletcher, P. C. (2020). Forms of prediction in the nervous system. Nature Reviews Neuroscience, 21(4), 231–242. https://doi.org/10.1038/s41583-020-0275-5
Ting, C. C., Yu, C. C., Maloney, L. T., & Wu, S. W. (2015). Neural mechanisms for integrating prior knowledge and likelihood in value-based probabilistic inference. The Journal of Neuroscience : The Official Journal of the Society for Neuroscience, 35(4), 1792–1805. https://doi.org/10.1523/JNEUROSCI.3161-14.2015
Tschantz, A., Seth, A. K., & Buckley, C. L. (2020). Learning action-oriented models through active inference. PLoS Computational Biology, 16(4), e1007805. https://doi.org/10.1371/journal.pcbi.1007805
Van Merrienboer, J. J., & Sweller, J. (2010). Cognitive load theory in health professional education: Design principles and strategies. Medical Education, 44(1), 85-93. https://doi.org/10.1111/j.1365-2923.2009.03498.x
Walsh, J. N., Knight, M., & Lee, A. J. (2017). Diagnostic errors: Impact of an educational intervention on pediatric primary care. Journal of Pediatric Health Care : Official Publication of National Association of Pediatric Nurse Associates & Practitioners, 32(1), 53–62. https://doi.org/10.1016/j.pedhc.2017.07.004
Walsh, K. S., McGovern, D. P., Clark, A., & O’Connell, R. G. (2020). Evaluating the neurophysiological evidence for predictive processing as a model of perception. Annals of the New York Academy of Sciences, 1464(1), 242–268. https://doi.org/10.1111/nyas.14321
Young, J. Q., Van Merrienboer, J., Durning, S., & Ten Cate, O. (2014). Cognitive load theory: Implications for medical education: AMEE Guide No. 86. Medical Teacher, 36(5), 371-384. https://doi.org/10.3109/0142159X.2014.889290
Zwaan, L., Monteiro, S., Sherbino, J., Ilgen, J., Howey, B., & Norman, G. (2016). Is bias in the eye of the beholder? A vignette study to assess recognition of cognitive biases in clinical case workups. BMJ Quality & Safety. 26(2), 104–110. https://doi.org/10.1136/bmjqs-2015-005014
Zwaan, L., Schiff, G. D., & Singh, H. (2013). Advancing the research agenda for diagnostic error reduction. BMJ Quality & Safety, 22 Suppl 2, ii52-ii57. https://doi.org/10.1136/bmjqs-2012-001624
*Lim Tow Keang
Department of Medicine
National University Hospital
5 Lower Kent Ridge Rd
Singapore 119074
Email: mdclimtk@nus.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









