Medical students use, attitudes towards, and knowledge of complementary and alternative medicine: A scoping review
Submitted: 18 January 2021
Accepted: 19 May 2021
Published online: 5 October, TAPS 2021, 6(4), 107-117
https://doi.org/10.29060/TAPS.2021-6-4/OA2470
Sarah Brown & Justin L C Bilszta
Department of Medical Education, Melbourne Medical School, University of Melbourne, Australia
Abstract
Introduction: Use of complementary and alternative medicine (CAM) is popular in the general population and medical practitioners may not be fully equipped in their knowledge of CAM to advise patients appropriately. The aim of this paper was to perform a scoping review of current literature describing undergraduate medical student use, attitudes, and knowledge of CAM as a means of better understanding the educational needs of these students.
Methods: A systematic search of Medline, PubMed and the Education Resources Information Center (ERIC) databases with keywords related to “complementary and alternative medicine” and “undergraduate medical students” for relevant articles published until August 2020.
Results: Of 131 papers identified, 38 underwent full review. It was found 13-80% of medical students use CAM, and overall have a positive attitude towards CAM therapies. Female medical students and those with religiosity had more positive attitudes towards CAM than their male colleagues and those without a religion. Knowledge of CAM is lacking with approximately only half of students feeling they were knowledgeable about CAM therapies. Popular information resources are the Internet and social media, but students expressed they want more teaching of CAM in the undergraduate medical curriculum.
Conclusion: Evidence suggests high usage of CAM amongst undergraduate medical students, and positive attitudes towards CAM therapies; however, knowledge of CAM is poor, and students want more CAM teaching to upskill them in counselling patients interested in CAM therapies. Further areas for research include a better understanding of resources medical students use for their knowledge and how gender and religiosity influence attitudes towards CAM.
Keywords: Undergraduate Medical Student, Complementary and Alternative Medicine, CAM, Attitude, Knowledge, Use
Practice Highlights
- Medical student’s personal use of CAM is significant, with the most popular therapies being massage, meditation and herbal medicine.
- Medical students have a positive attitude towards CAM but potential differences between attitudes of preclinical and clinical student populations exist.
- Medical student’s knowledge of CAM is lacking, and this impacts their ability to advise patients appropriately.
- Medical students want more CAM teaching integrated into their UGME curriculum, and believe conventional western medicine could benefit from CAM methods and ideas.
- Better integration of the principles of EBM rather than teaching related to specific CAM therapies can provide medical students with the skills to critique claims of CAM efficacy.
I. INTRODUCTION
Complementary and alternative medicine (CAM) encompasses a range of health practices including, but not limited to, acupuncture, naturopathy, chiropractic traditional Chinese medicine (TCM), herbal, vitamin & homeopathic therapies (Zollman & Vickers, 1999). Complementary refers to the practice of something alongside conventional Western medicine, whilst alternative refers to the practice of something instead of conventional Western medicine (Zollman & Vickers, 1999).
In comparison to conventional Western medicine, the eclectic range of CAM is often cited as having a poor-quality evidence-base regarding its efficacy (Australian Medical Association, 2018), yet it remains popular with the general public (Frass et al., 2012). With surveys suggesting 10–76% of the public has used CAM (Ernst, 2000; Harris et al., 2012) the demand for CAM is evident. How knowledgeable medical practitioners are, and their attitudes towards CAM, can influence the advice they might provide to patients who seek information about CAM therapies or want to use CAM in lieu of conventional Western medicine. Janamian et al. (2011) have reported general practitioners feel they do not have the education to appropriately advise patients on CAM (Janamian et al., 2011). This may deter patients from seeking guidance from their healthcare provider and result in a breakdown of communication and lack of congruence over health goals (Xue et al., 2007).
Medical students’ insights into their prevailing attitudes and knowledge of CAM can help determine if CAM teaching within undergraduate medical education (UGME) should be expanded to better meet the needs of growing public demand. The last significant review of medical students’ attitudes and knowledge of CAM was published in 2016 (Joyce et al., 2016), and reported overall medical students believed they lacked knowledge of CAM but were generally positive towards CAM education and thought CAM teaching should be incorporated into UGME. What this review did not explore was the rates of CAM use by medical students, and whether this influenced attitudes towards CAM. Importantly, since the publication of Joyce et al’s review, not only have there been additional studies exploring medical students’ use, attitudes and knowledge of CAM, but the increasing use of the Internet and social media as a source of information means it is timely to re-evaluate the findings of this earlier study and determine whether the results presented remain relevant.
We conducted this scoping review of primary studies to evaluate undergraduate medical student use, attitudes, and knowledge of CAM as a means of better understanding the educational needs of these students. The specific research questions were: 1) what is the usage and knowledge of CAM among medical students?; 2) what are medical students’ attitudes towards CAM?; 3) what factors influence medical students’ attitudes towards CAM, and where do they seek information about CAM? and; 4) what are medical students’ views on the current teaching they receive in UGME about CAM?
II. METHODS
This study adopted the “Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews” (PRISMA-ScR) protocol (Tricco et al., 2018).
A. Search Strategy
Electronic databases Medline (Ovid), PubMed and ERIC were searched for full text articles describing undergraduate medical students use, attitudes, and knowledge of CAM (see Appendix 1). Additional papers were found through a hand search of reference lists of articles identified through the database search. There was no limit on publication date.
B. Selection of Sources
Papers were included if published in English and reported on undergraduate medical students. Papers were excluded if they were not published in English; opinion pieces or review articles; reported on non-undergraduate medical students or; reported on osteopathic medical students. This group was excluded due to the potential bias these students may have due to their medical training including specific CAM teaching.
C. Key Words and Boolean Operators
The search strategy (see Appendix 1) included Boolean operators (AND, NOT, OR), Medical Subject Headings (MeSH) and specific key words.
D. Data Extraction and Charting
Data extraction was performed using a predetermined checklist, and included
- Article details: first author and publication year
- Research aim: purpose of the study
- Method: methods of data collection
- Sample size: number of students invited to participate and the number who responded
- Student CAM use: number of students using CAM, including use of specific therapies and timeframe of use
- Student attitudes/perceptions to CAM: student attitudes to CAM including desire to undertake further education about CAM, beliefs about CAM efficacy, role of CAM in conventional Western medicine and, sources of CAM information
- Influencing factors: factors reported to influence student’s attitudes/perceptions to CAM
- Limitations: identified study limitations
E. Synthesis of Results
Included studies were described by author, publication year, and characteristics described above. Thematic analysis was conducted to identify commonality between included studies. No inferences were made about students’ use, attitudes, or knowledge of CAM if this was not explicitly stated.
Literature searching, title and abstract screening, full text review & data extraction, and charting were undertaken by the 1st author (SB). Where there was uncertainty regarding the aforementioned, these articles were reviewed independently by the 2nd author (JB) and discussed until consensus was reached. The 2nd author also independently reviewed the data extraction and charting results once this process was completed by the 1st author.
III. RESULTS
From the initial search strategy, 131 articles were obtained for screening based on title and abstract. Following screening, 17 duplicate citations were excluded, leaving 114 papers. Abstract and title screening excluded papers focused on pharmacy or nursing students, and those that did not centre on the research questions. Following this, 58 articles underwent full review. Of these, 21 were excluded as they were not in English, did not provide enough detail regarding medical students specifically or focused heavily on medical curricula. The total number of articles included is 38 (see Figure 1); a full version of the outcome harvesting data can be found at https://doi.org/10.6084/m9.figshare.14471250 (Brown & Bilszta, 2021).
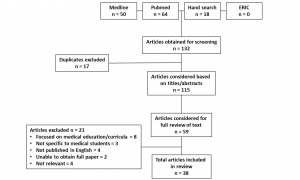
Figure 1: PRISMA Diagram
A. CAM usage
Twenty-two studies assessed CAM usage in medical students (Baugniet et al., 2000; Chaterji et al., 2007; Chez et al., 2001; Ditte et al., 2011; Donald et al., 2010; Flaherty et al., 2015; Frye et al., 2006; Greenfield et al., 2000, 2002; Hegde et al., 2018; Hopper & Cohen, 1998; James et al., 2016; Lie & Boker, 2004, 2006; Nicolao et al., 2010; Oberbaum et al., 2003; Rees et al., 2009; Sadeghi et al., 2016; Samara et al., 2019; Shani-Gershoni et al., 2008; Wong et al., 2006; Yildirim et al., 2010). Rates of usage ranged from 13% to 80% (Chez et al., 2001; Wong et al., 2006). The most common CAM therapy used by medical students was difficult to evaluate due to inconsistent methods of collecting this information with studies either asking students to nominate usage from a predefined list of therapies (Baugniet et al., 2000; Chaterji et al., 2007; Frye et al., 2006; Hegde et al., 2018; James et al., 2016; Lie & Boker, 2004, 2006; Nicolao et al., 2010; Sadeghi et al., 2016; Samara et al., 2019; Shani-Gershoni et al., 2008; Wong et al., 2006; Yildirim et al., 2010); self-report the therapies they had engaged with (Donald et al., 2010; Greenfield et al., 2000, 2002) or; indicating CAM usage without nominating a specific therapy (Chez et al., 2001; Ditte et al., 2011; Flaherty et al., 2015; Hopper & Cohen, 1998; Oberbaum et al., 2003; Rees et al., 2009). The challenge in evaluated CAM usage is highlighted by two separate studies (Lie & Boker, 2004, 2006) which reported a range of practices to be popular including massage, meditation and yoga compared to vitamins, meditation and spirituality, respectively (Lie & Boker, 2004, 2006).
B. CAM perception/attitudes
Overall, the general attitude of medical students towards CAM is positive (Ahmed et al., 2017; Akan et al., 2012; Chaterji et al., 2007; Chez et al., 2001; Ditte et al., 2011; Flaherty et al., 2015; Frye et al., 2006; Furnham & McGill, 2003; Godin et al., 2007; Greenfield et al., 2002, 2006; Hegde et al., 2018; Hopper & Cohen, 1998; James et al., 2016; Lie & Boker, 2004, 2006; Loh et al., 2013; Nicolao et al., 2010; Oberbaum et al., 2003; Perkin et al., 1994; Rees et al., 2009; Sadeghi et al., 2016; Samara et al., 2019; Templeman et al., 2015; Torkelson et al., 2006; Wong et al., 2006; Xie et al., 2020; Yeo et al., 2005) with positive attitudes ranging from 49% to 60% (Ditte et al., 2011; Perkin et al., 1994; Sadeghi et al., 2016). Different methods were used to collect this data including validated measures (for example: (Flaherty et al., 2015; Frye et al., 2006; Rees et al., 2009)), rating scales with various stages of validation (for example: (Ahmed et al., 2017; Oberbaum et al., 2003; Sadeghi et al., 2016; Samara et al., 2019)) or qualitative interviews (for example: (Templeman et al., 2015)).
Differences in the attitude of preclinical and clinical cohorts varied between studies. Akan et al., Furnham & McGill and Syverstad et al. reported preclinical students had a more positive attitude compared to clinical students (Akan et al., 2012; Furnham & McGill, 2003; Syverstad et al., 1999), however others found clinical students were more positive, perhaps due to them receiving more CAM education (Chaterji et al., 2007; Xie et al., 2020). However, multiple studies found no difference between preclinical and clinical cohorts (Ditte et al., 2011; Flaherty et al., 2015; Hopper & Cohen, 1998; Rees et al., 2009). Additionally, all studies bar one (Hübner et al., 2012) asked students to consider attitudes and perceptions in relation to ‘…their clinical practice…’ rather than associated with a specific clinical context or medical condition.
Attitudes towards specific CAM therapies demonstrated acupuncture received consistent positive perceptions ranging from 77% to above 90% (Loh et al., 2013; Torkelson et al., 2006; Yeo et al., 2005). Other therapies with consistent positive perceptions include massage and meditation, with more than 70% of medical students feeling positively towards these practices (Furnham & McGill, 2003; Loh et al., 2013; Torkelson et al., 2006). Conversely, Greenfield et al. and Loh et al. both found homeopathy had the most negative perception from students (Greenfield et al., 2006; Loh et al., 2013). Interestingly, studies indicate ambivalence towards chiropractic practice, with some reporting positive attitudes whilst others reported negative attitudes (Greenfield et al., 2006; Loh et al., 2013). When asked about the integration of CAM with conventional Western medicine, there was overwhelming belief from medical students that benefits may come from applying these practices together. Ahmed et al. and Chez et al. reported a large percentage of their cohorts believed conventional Western medicine could benefit from CAM methods and ideas (67% and 89%, respectively) (Ahmed et al., 2017; Chez et al., 2001). Similar findings have been reported by others, with the percentage of students wanting the integration of CAM and conventional Western medicine ranging from 71% to 92% (Chez et al., 2001; Hopper & Cohen, 1998; Lie & Boker, 2004; Loh et al., 2013; Nicolao et al., 2010; Torkelson et al., 2006; Xie et al., 2020; Yeo et al., 2005).
An important question to consider when evaluating medical student knowledge and attitudes towards CAM is whether they believe CAM works. This question arose frequently in the reviewed literature, with investigators trying to determine if there was congruence between having a positive perception of CAM and belief in its efficacy. When asked if participants found the results of CAM were mainly due to the placebo effect, there were mixed findings with 39-59% of medical students agreeing the CAM efficacy was mainly due to the placebo effect (Baugniet et al., 2000; Nicolao et al., 2010; Yeo et al., 2005; Yildirim et al., 2010). Interestingly, recent studies by Xie et al. and Samara et al. reported only 10% and 35%, respectively, believed CAM efficacy was due to the placebo effect (Samara et al., 2019; Xie et al., 2020). Whether this is simply a cohort effect or a reflection that over time students may be becoming less sceptical of CAM, is unable to be confirmed.
Factors that influence attitudes towards CAM should be considered as they may alter how medical students perceive CAM therapies. The most frequent influence reported was gender, with female medical students overall tending to have a more positive attitude than male colleagues (Akan et al., 2012; Chaterji et al., 2007; Ditte et al., 2011; Donald et al., 2010; Flaherty et al., 2015; Frye et al., 2006; Furnham & McGill, 2003; Godin et al., 2007; Greenfield et al., 2002, 2006; Hübner et al., 2012; Oberbaum et al., 2003; Rees et al., 2009; Schmidt et al., 2005; Xie et al., 2020). Interestingly, Ditte et al. found male medical students feared the social stigma of using CAM more than female students (45% vs 36%) and Donald et al. reported male students were more likely to be more sceptical of CAM than female students (50% vs 44%) (Ditte et al., 2011; Donald et al., 2010).
Religion may also influence attitudes to CAM. Yeo et al. reported nearly two thirds of their cohort believed spiritual/religious beliefs influenced attitudes towards CAM (Yeo et al., 2005). Furnham & McGill reported similar findings as female students and students that rated themselves higher religiously, were more eager for CAM to be on the curriculum compared to males and those who were less religious (Furnham & McGill, 2003). In contrast, Loh et al. reported students with no religion tended to be less interested in CAM (Loh et al., 2013).
C. CAM knowledge
The included studies suggest approximately only half of medical students felt knowledgeable about CAM (Hopper & Cohen, 1998; James et al., 2016; Sadeghi et al., 2016; Shani-Gershoni et al., 2008) and the most common individual therapies students were subjectively knowledgeable in were massage (Baugniet et al., 2000; Chez et al., 2001; Frye et al., 2006; Furnham & McGill, 2003), acupuncture (Akan et al., 2012; Nicolao et al., 2010; Sadeghi et al., 2016; Yeo et al., 2005), chiropractic (Baugniet et al., 2000; Chez et al., 2001; Frye et al., 2006) and herbal medicine (Akan et al., 2012; Baugniet et al., 2000; Chez et al., 2001). It is clear, however, medical students still perceive significant gaps in their knowledge of CAM. Nicolao et al. reported although students indicated acupuncture and homeopathy as their most knowledgeable areas, this was only for a minority of the cohort (34% and 43%, respectively) and the majority of students felt their level of knowledge, and therefore ability to appropriately advise patients, was poor (Nicolao et al., 2010). In one Australian study, investigators found out of ten common CAM therapies (acupuncture, chiropractic, herbal medicine, homeopathy, hypnosis, massage, meditation, naturopathy, reflexology and spiritual healing) 56% of their cohort had no knowledge of any of these therapies (Hopper & Cohen, 1998).
The Internet appears to be a popular avenue for finding CAM information with Lie and Boker reporting 81% of their cohort used online resources as their main information source (Lie & Boker, 2004). Although the specific online resources used were not described, journals, books and health databases were used less frequently in comparison (41%, 38% and 28%, respectively) (Lie & Boker, 2004). A study of Chinese medical students with CAM teaching integrated into their UGME, found their cohort’s main source of information was from teachers, making up 91% with only 2% using the Internet (Xie et al., 2020). Samara et al. reported 73% of their cohort used social media as their main source of information (Samara et al., 2019).
It is clear medical students want more teaching about CAM in their UGME. Flaherty et al. reported just over two thirds of students across all year levels had a desire to study CAM, however, there was a positive correlation between those students who wanted more teaching and a positive attitude towards CAM (Flaherty et al., 2015). Similar findings were reported by Perkins et al. and Frye et al. with approximately 85% of clinical and preclinical students believing they should learn about CAM in UGME (Frye et al., 2006; Perkin et al., 1994). In terms of this would look like in the curriculum, Greenfield et al. reported 67% wanted to study the theory, with Greiner et al. and Yeo et al. finding 72% and 86%, respectively, wanted clinical exposure (Greenfield et al., 2006; Greiner et al., 2000; Yeo et al., 2005). In semi-structured qualitative interviews of Australian medical students, CAM education was considered important regardless of specialisation and CAM literacy was an ethical responsibility (Templeman et al., 2015).
IV. DISCUSSION
In this Discussion, we provide commentary on our findings, consider how these might be applied to the design of UGME curriculum, and suggest areas of further research.
In the current study, we found a significant number of medical students use CAM, however reported rates varied considerably, and our analysis suggests inconsistency in approaches used to assess CAM use may explain the observed differences. As highlighted, data collection was split between those studies that provided a predefined list of specific CAM therapies, with a limited number of response options, and the exact therapies between papers incongruent; those that allowed students to self-report usage and; those indicating CAM usage without nominating a specific therapy (see Table 1). Cultural differences may also explain usage variation; for example, the high use of yoga in Indian medical students (Hegde et al., 2018), TCM in Chinese medical students (Wong et al., 2006) and, traditional Iranian medicine in Iranian medical students (Sadeghi et al., 2016).
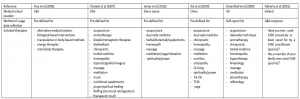
Table 1. Example of the differing methods used to collect student CAM usage data. Data collection of medical student CAM usage was split between those studies that provided a predefined list of specific CAM therapies; those that allowed students to self-report usage and; those indicating CAM usage without nominating a specific therapy. The above examples highlight the inconsistent approaches to collecting this information.
Overall, the general attitude of medical students towards CAM was positive, but differences were noted between preclinical and clinical students, and what exposure students had had to CAM teaching. There is evidence positive attitudes to CAM decline after the preclinical period (Akan et al., 2012; Furnham & McGill, 2003; Syverstad et al., 1999) and this might be due, in part, to the influence of clinical peers, medical school role models or a preference for students new to clinical learning utilizing recently acquired conventional clinical skills. Further work is required to fully elucidate how attitudes to CAM mature as students move from preclinical to clinical learning, are exposed to the application of conventional and CAM practices in different patient encounters and develop skills in the application of evidence-based medicine (EBM).
Two significant factors influencing attitudes to CAM were gender and religion, and these were also identified previously (Joyce et al., 2016).
Whilst medical students as a whole seem to have a positive attitude towards CAM, female students hold more positive attitudes than their male colleagues. There is evidence to suggest this difference is due to higher rates of scepticism around the CAM efficacy in male students (Donald et al., 2010) and fear of social stigma from using CAM (Ditte et al., 2011). There is a noted body of evidence demonstrating similar gender differences in general (Bishop & Lewith, 2010; Kristoffersen et al., 2014) and specific patient populations (Alwhaibi et al., 2019; Alwhaibi & Sambamoorthi, 2016; Barraco et al., 2005; Bell et al., 2006; Jawahar et al., 2012), so it is not surprising this is reflected in medical student cohorts; this is an area for further exploration.
Research within general and specific patient populations into the association between religiosity (the practices of organised religion and the outward expression of belief in a divine being) and spirituality (the personal and emotional expression that arises from searching for a divine being) and CAM utilisation has examined these as a single construct (Heller et al., 2020; McCurdy et al., 2003; Pedersen et al., 2013), or as separate entities (Ben-Arye et al., 2012; Ellison et al., 2012; Hsiao et al., 2008). An added challenge (Ellison et al., 2012; Hsiao et al., 2008) has been attempts to tease out use of religious/spiritual forms of CAM (eg self-prayer, group prayer, or healing rituals) from use of non-religious/nonspiritual forms (eg herbs, supplements, and mind–body techniques). As a result, it remains ambiguous whether religiosity and spiritually are associated with increased CAM utilisation. The results presented here and by others (Joyce et al., 2016) suggests within medical student cohorts an association might be present however the nature remains unclear. What needs to be explored is the intersection between conventional UGME, attitudes to CAM and student’s religious and spiritual beliefs.
Several studies reported most students did not feel knowledgeable about CAM and this impacted their ability to advise patients appropriately (Chaterji et al., 2007; Loh et al., 2013; Torkelson et al., 2006). When evaluating student’s knowledge of CAM, an important limitation is the ways in which knowledge was evaluated. Most studies used self-report, rather than objective, knowledge measures. The only study which attempted to use an objective measure reported the average knowledge of CAM was ‘poor’ (Samara et al., 2019). There is, however, a clear indication medical students want more CAM teaching integrated into UGME. This is relevant as there is evidence CAM users frequently neglect to disclose their usage to their treating health professional (Chao et al., 2008; Davis et al., 2012; Thomson et al., 2012). Foley et al. (2019) identified several factors influencing this including, importantly in this context, perceptions of health professional’s knowledge of CAM and lack of knowledge is considered a barrier to discussions of CAM use during clinical consultations (Foley et al., 2019).
Although medical students believe conventional Western medicine could benefit from CAM methods and ideas, an important caveat to this finding is it does not consider how they feel about specific CAM therapies. For example, would medical students think conventional Western medicine could benefit from integrating herbal medicine or homeopathy approaches, compared to osteopathy or acupuncture? Given the diversity of CAM, it is arguably unfeasible (Wetzel et al., 1998) to teach students about each individual therapy, so an EBM teaching model equipping students with skills needed to critically appraise evidence presents a potential solution, and several medical schools have designed curricular in this way (Bailey et al., 2015; Forjuoh et al., 2003; Hassed, 2004; Jeffries, 2001; Mahapatra et al., 2017; Owen & Lewith, 2001; Perlman & Stagnaro-Green, 2010). This addresses a thematically overwhelming and resource intensive area of medical education where learned knowledge and skills can be adapted for differing CAM therapies.
Only three studies (Lie & Boker, 2004; Samara et al., 2019; Xie et al., 2020) specifically explored how medical students use digital resources to supplement formal CAM teaching, so this is a clear direction for further research. It is important medical students have access to high quality evidence-based information and the skills to determine the validity of evidence presented on digital platforms. Whilst there is evidence to demonstrate resources such as blogs, social networking sites and online support groups are useful platforms for health education, social connection and experience sharing, they are at significant risk of misinformation and mischaracterisation of CAM (Delgado-López & Corrales-García, 2018; Molassiotis & Xu, 2004). Sharma et al. (2016) have underscored the challenges in developing approaches for identifying the reliability of CAM-related information on the Internet, which may not be supported by a reliable evidence-base (Sharma et al., 2016). This means medical students require skills to critique claims related to CAM efficacy for their own education needs, but also so they can appropriately counsel patients. As advocated, an EBM teaching model would provide students with the skills to critique claims of CAM efficacy as well as empower patients to make informed decisions relevant to their health needs.
V. LIMITATIONS OF THE STUDY
As we did not conduct a systematic review of the literature, we are unable to draw any conclusions about the quality of the included studies. We excluded non-English studies, and this potentially creates a gap in the literature and may have altered the findings as CAM use, attitudes and knowledge may be different in non-English speaking countries (for example, the high use of acupuncture or Traditional Chinese medicine in Asian countries). The lack of consistency in data related to medical student use, attitudes and knowledge of CAM therapies is reflected in its heterogeneity. This makes generalisations related to ‘medical students’, even within the same medical school or UGME curriculum, difficult. Despite this significant limitation, the diversity of reported outcomes reflects important contextual differences in medical programs, and medical student cohorts, across the globe.
VI. CONCLUSION
Overall, medical students have a positive attitude towards CAM, with significant influencing factors being gender and religion, and potential differences between preclinical and clinical cohorts. The included literature indicates medical students’ personal use of CAM is significant, with therapies such as massage, meditation and herbal medicine being more popular than others. It is clear medical students’ CAM knowledge is lacking and integration of the principles of EBM may be beneficial in addressing this, ultimately leading to better educated doctors who have better relationships with their patients.
Notes on Contributors
JB: conceptualised the review; JB, SB: designed the search strategy; SB: conducted the search and screened the literature; JB, SB: reviewed the included studies; SB: analysed the data; JB: drafted the manuscript; JB, SB: critically revised the manuscript. All authors had full access to all study data, read and approved the final version of the manuscript.
Ethical Approval
As all the data were retrieved from public databases, this study did not require institutional review board approval.
Data Availability
The data that support the findings of this study are openly available in Figshare repository, https://doi.org/10.6084/m9.figshare.14471250. The data extraction sheet used during the current study is available from the corresponding author on request. All data is based on published studies.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Declaration of Interest
None of the listed authors have financial and personal relationships with organisations or people that could inappropriately influence their work.
References
Ahmed, S. M., Al-Mansour, M. A., Mohamed, E. Y., Medani, K. A., Abdalla, S. M., & Mahmoud, W. S. (2017). Medical Students’ Opinion Toward the Application of Complementary and Alternative Medicine in Healthcare. Saudi Journal of Medicine & Medical Sciences, 5(1), 20-25. https://doi.org/10.4103/1658-631X.194255
Akan, H., Izbirak, G., Kaspar, E. C., Kaya, C. A., Aydin, S., Demircan, N., Bucaktepe, P. G., Ozer, C., Sahin, H. A., & Hayran, O. (2012). Knowledge and attitudes towards complementary and alternative medicine among medical students in Turkey. BMC Complementary & Alternative Medicine, 12, 115. https://doi.org/10.1186/1472-6882-12-115
Alwhaibi, M., AlRuthia, Y., & Meraya, A. (2019). Gender differences in the prevalence of complementary and alternative medicine utilization among adults with arthritis in the United States. Evidence-Based Complementary & Alternative Medicine: eCAM. https://doi.org/10.1155/2019/8739170
Alwhaibi, M., & Sambamoorthi, U. (2016). Sex differences in the use of complementary and alternative medicine among adults with multiple chronic conditions. Evidence-Based Complementary & Alternative Medicine: eCAM. https://doi.org/10.1155/2016/2067095
Australian Medical Association. (2018). AMA Position Statement, Complementary Medicine. https://ama.com.au/position-statement/ama-position-statement-complementary-medicine-2018
Bailey, M. L., Chudgar, S. M., Engle, D. L., Moon, S. D., Grochowski, C. O., & Clay, A. S. (2015). The impact of a mandatory immersion curriculum in integrative medicine for graduating medical students. Explore (NY), 11(5), 394-400. https://doi.org/10.1016/j.explore.2015.07.003
Barraco, D., Valencia, G., Riba, A., Nareddy, S., Draus, C., & Schwartz, S. (2005). Complementary and alternative medicine (CAM) use patterns and disclosure to physicians in acute coronary syndromes patients. Complementary Therapies in Medicine, 13(1), 34-40. https://doi.org/ 10.1016/j.ctim.2005.02.003
Baugniet, J., Boon, H., & Ostbye, T. (2000). Complementary/alternative medicine: comparing the view of medical students with students in other health care professions. Family Medicine, 32(3), 178-184.
Bell, R., Suerken, C., Grzywacz, J., Lang, W., Quandt, S., & Arcury, T. (2006). Complementary and alternative medicine use among adults with diabetes in the United States. Alternative Therapies in Health and Medicine, 12, 16-22.
Ben-Arye, E., Schiff, E., Vintal, H., Agour, O., Preis, L., & Steiner, M. (2012). Integrating complementary medicine and supportive care: Patients’ perspectives toward complementary medicine and spirituality. Journal of Alternative and Complementary Medicine, 18(9), 824-831. https://doi.org/10.1089/acm.2011.0327
Bishop, F., & Lewith, G. (2010). Who uses CAM? A narrative review of demographic characteristics and health factors associated with CAM use. Evidence-Based Complementary & Alternative Medicine: eCAM, 7(1), 11-28. https://doi.org/10.1093/ecam/nen023
Brown, S., & Bilszta, J. L. C. (2021). Medical students use, attitudes towards, and knowledge of complementary and alternative medicine: A scoping review [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14471250
Chao, M., Wade, C., & Kronenberg, F. (2008). Disclosure of complementary and alternative medicine to conventional medical providers: Variation by race/ethnicity and type of CAM. Journal of the National Medical Association, 100(11), 1341-1349. https://doi.org/10.1016/s0027-9684(15)31514-5
Chaterji, R., Tractenberg, R. E., Amri, H., Lumpkin, M., Amorosi, S. B., & Haramati, A. (2007). A large-sample survey of first- and second-year medical student attitudes toward complementary and alternative medicine in the curriculum and in practice. Alternative Therapies in Health & Medicine, 13(1), 30-35.
Chez, R. A., Jonas, W. B., & Crawford, C. (2001). A survey of medical students’ opinions about complementary and alternative medicine. American Journal of Obstetrics and Gynecology, 185(3), 754-757. https://doi.org/10.1067/mob.2001.117484
Davis, E. L., Oh, B., Butow, P. N., Mullan, B. A., & Clarke, S. (2012). Cancer patient disclosure and patient-doctor communication of complementary and alternative medicine use: A systematic review. The Oncologist, 17(11), 1475-1481. https://doi.org/10.1634/theoncologist.2012-0223
Delgado-López, P., & Corrales-García, E. (2018). Influence of Internet and social media in the promotion of alternative oncology, cancer quackery, and the predatory publishing phenomenon. Cureus, 10(5), e2617. https://doi.org/10.7759/cureus.2617
Ditte, D., Schulz, W., Ernst, G., & Schmid-Ott, G. (2011). Attitudes towards complementary and alternative medicine among medical and psychology students. Psychology, Health & Medicine, 16(2), 225-237. https://doi.org/10.1080/13548506.2010.532559
Donald, G. K., Mackereth, P., & Tobin, I. (2010). Medical students and acupuncture: A short sharp placement experience! Acupuncture Medicine, 28(1), 12-15. https://doi.org/10.1136/aim.2009.001602
Ellison, C. G., Bradshaw, M., & Roberts, C. A. (2012). Spiritual and religious identities predict the use of complementary and alternative medicine among US adults. Preventive Medicine, 54(1), 9-12. https://doi.org/10.1016/j.ypmed.2011.08.029
Ernst, E. (2000). Prevalence of use of complementary/alternative medicine: A systematic review. Bulletin of the World Health Organization, 78(2), 252-257.
Flaherty, G., Fitzgibbon, J., & Cantillon, P. (2015). Attitudes of medical students toward the practice and teaching of integrative medicine. Journal of Integrative Medicine, 13(6), 412-415. https://doi.org/10.1016/s2095-4964(15)60206-0
Foley, H., Steel, A., Cramer, H., Wardle, J., & Adams, J. (2019). Disclosure of complementary medicine use to medical providers: A systematic review and meta-analysis. Scientific Reports, 9(1573). https://doi.org/10.1038/s41598-018-38279-8
Forjuoh, S. N., Rascoe, T. G., Symm, B., & Edwards, J. C. (2003). Teaching medical students complementary and alternative medicine using evidence-based principles. The Journal of Alternative & Complementary Medicine, 9(3), 429-439.
Frass, M., Strassl, R. P., Friehs, H., Müllner, M., Kundi, M., & Kaye, A. D. (2012). Use and acceptance of complementary and alternative medicine among the general population and medical personnel: A systematic review. Ochsner Journal, 12(1), 45-56.
Frye, A. W., Sierpina, V. S., Boisaubin, E. V., & Bulik, R. J. (2006). Measuring what medical students think about complementary and alternative medicine (CAM): A pilot study of the complementary and alternative medicine survey. Advances in Health Sciences Education, 11(1), 19-32. https://doi.org/10.1007/s10459-005-1587-y
Furnham, A., & McGill, C. (2003). Medical students’ attitudes about complementary and alternative medicine. The Journal of Alternative & Complementary Medicine, 9(2), 275-284. https://doi.org/10.1089/10755530360623392
Godin, G., Beaulieu, D., Touchette, J. S., Lambert, L. D., & Dodin, S. (2007). Intention to encourage complementary and alternative medicine among general practitioners and medical students. Behavioral Medicine, 33(2), 67-77.
Greenfield, S. M., Brown, R., Dawlatly, S. L., Reynolds, J. A., Roberts, S., & Dawlatly, R. J. (2006). Gender differences among medical students in attitudes to learning about complementary and alternative medicine. Complementary Therapies in Medicine, 14(3), 207-212. https://doi.org/10.1016/j.ctim.2005.12.001
Greenfield, S. M., Innes, M. A., Allan, T. F., & Wearn, A. M. (2002). First year medical students’ perceptions and use of complementary and alternative medicine. Complementary Therapies in Medicine, 10(1), 27-32. https://doi.org/10.1054/ctim.2002.0501
Greenfield, S. M., Wearn, A. M., Hunton, M., & Innes, M. A. (2000). Considering the alternatives: A special study module in complementary therapy. Complementary Therapies in Medicine, 8(1), 15-20.
Greiner, K. A., Murray, J. L., & Kallail, K. J. (2000). Medical student interest in alternative medicine. The Journal of Alternative & Complementary Medicine, 6(3), 231-234. https://doi.org/10.1089/acm.2000.6.231
Harris, P. E., Cooper, K. L., Relton, C., & Thomas, K. J. (2012). Prevalence of complementary and alternative medicine (CAM) use by the general population: A systematic review and update. International Journal of Clinical Practice, 66(10), 924–939. https://doi.org/10.1111/j.1742-1241.2012.02945.x
Hassed, C. S. (2004). Bringing holism into mainstream biomedical education. The Journal of Alternative and Complementary Medicine, 10(2), 405-407. https://doi.org/10.1089/107555304323062428
Hegde, S. V., Rao, S. K., Menezes, R. G., Kotian, S. M., & Shetty, S. (2018). Knowledge, attitude, and practice of yoga in medical students: Assessment of anthropometry and lifestyle factors. International Journal of Yoga Therapy, 28(1), 9-14. https://doi.org/10.17761/2018-00005r1
Heller, T., Kloos, C., Mueller, N., Roemelt, J., Keinki, C., Wolf, G., Mueller, U. A., & Huebner, J. (2020). Complementary and alternative medicine is positively associated with religiousness/ spirituality. Journal of Complementary & Integrative Medicine, Advance online publication. https://doi.org/10.1515/jcim-2018-0023
Hopper, I., & Cohen, M. (1998). Complementary therapies and the medical profession: A study of medical students’ attitudes. Alternative Therapies in Health and Medicine, 4(3), 68-73.
Hsiao, A.-F., Wong, M. D., Miller, M. F., Ambs, A. H., Goldstein, M. S., Smith, A., Ballard-Barbash, R., Becerra, L. S., Cheng, E. M., & Wenger, N. S. (2008). Role of religiosity and spirituality in complementary and alternative medicine use among cancer survivors in California. Integrative Cancer Therapies, 7(3), 139-146. https://doi.org/10.1177/1534735408322847
Hübner, J., Wicker, S., & Münstedt, K. (2012). Survey of students regarding their attitudes toward complementary and alternative medicine in oncology. Forschende Komplementarmedizin, 19(6), 319-321. https://doi.org/10.1159/000345973
James, P. B., Bah, A. J., & Kondorvoh, I. M. (2016). Exploring self-use, attitude and interest to study complementary and alternative medicine (CAM) among final year undergraduate medical, pharmacy and nursing students in Sierra Leone: A comparative study. BMC Complementary & Alternative Medicine, 16, 121. https://doi.org/10.1186/s12906-016-1102-4
Janamian, T., O’Rourke, P., Myers, S. P., & Eastwood, H. (2011). Information resource needs and preference of Queensland general practitioners on complementary medicines: Result of a needs assessment. Evidence-Based Complementary & Alternative Medicine: eCAM, https://doi.org/10.1155/2011/810908
Jawahar, R., Yang, S., Eaton, C. B., McAlindon, T., & Lapane, K. L. (2012). Gender-specific correlates of complementary and alternative medicine use for knee osteoarthritis. Journal of Women’s Health, 21(10), 1091-1099. https://doi.org/10.1089/jwh.2011.3434
Jeffries, W. B. (2001). A fourth-year elective course in alternative medicine. Academic Medicine, 76(5), 525-526. https://doi.org/10.1097/00001888-200105000-00060
Joyce, P., Wardle, J., & Zaslawski, C. (2016). Medical student attitudes towards complementary and alternative medicine (CAM) in medical education: A critical review. Journal of Complementary & Integrative Medicine, 13(4), 333-345. https://doi.org/10.1515/jcim-2014-0053
Kristoffersen, A. E., Stub, T., Salamonsen, A., Musial, F., & Hamberg, K. (2014). Gender differences in prevalence and associations for use of CAM in a large population study. BMC Complementary & Alternative Medicine, 14, 463. https://doi.org/10.1186/1472-6882-14-463
Lie, D., & Boker, J. (2004). Development and validation of the CAM Health Belief Questionnaire (CHBQ) and CAM use and attitudes amongst medical students. BMC Medical Education, 4, 2. https://doi.org/10.1186/1472-6920-4-2
Lie, D. A., & Boker, J. (2006). Comparative survey of Complementary and Alternative Medicine (CAM) attitudes, use, and information-seeking behaviour among medical students, residents & faculty. BMC Medical Education, 6, 58. https://doi.org/10.1186/1472-6920-6-58
Loh, K. P., Ghorab, H., Clarke, E., Conroy, R., & Barlow, J. (2013). Medical students’ knowledge, perceptions, and interest in complementary and alternative medicine. The Journal of Alternative & Complementary Medicine, 19(4), 360-366. https://doi.org/10.1089/acm.2012.0014
Mahapatra, S., Bhagra, A., Fekadu, B., Li, Z., Bauer, B. A., & Wahner-Roedler, D. L. (2017). Incorporation of integrative medicine education into undergraduate medical education: A longitudinal study. Journal of Integrative Medicine, 15(6), 442-449. https://doi.org/10.1016/s2095-4964(17)60367-4
McCurdy, E. A., Spangler, J. G., Wofford, M. M., Chauvenet, A. R., & McLean, T. W. (2003). Religiosity is associated with the use of complementary medical therapies by pediatric oncology patients. Journal of Pediatric Hematology Oncology, 25(2), 125-129.
Molassiotis, A., & Xu, M. (2004). Quality and safety issues of web-based information about herbal medicines in the treatment of cancer. Complementary Therapies in Medicine, 12(4), 217-227. https://doi.org/10.1016/j.ctim.2004.09.005
Nicolao, M., Täuber, M. G., Marian, F., & Heusser, P. (2010). Complementary medicine courses in Swiss medical schools: Actual status and students’ experience. Swiss Medical Weekly, 140(3-4), 44-51.
Oberbaum, M., Notzer, N., Abramowitz, R., & Branski, D. (2003). Attitude of medical students to the introduction of complementary medicine into the medical curriculum in Israel. Israel Medical Association Journal, 5(2), 139-142.
Owen, D., & Lewith, G. T. (2001). Complementary and alternative medicine (CAM) in the undergraduate medical curriculum: the Southampton experience. Medical Education, 35(1), 73-77. https://doi.org/10.1046/j.1365-2923.2001.00762.x
Pedersen, C. G., Christensen, S., Jensen, A. B., & Zachariae, R. (2013). In God and CAM we trust. Religious faith and use of complementary and alternative medicine (CAM) in a nationwide cohort of women treated for early breast cancer. Journal of Religion and Health, 52(3), 991-1013. https://doi.org/10.1007/s10943-012-9569-x
Perkin, M. R., Pearcy, R. M., & Fraser, J. S. (1994). A comparison of the attitudes shown by general practitioners, hospital doctors and medical students towards alternative medicine. Journal of the Royal Society of Medicine, 87(9), 523-525.
Perlman, A., & Stagnaro-Green, A. (2010). Developing a complementary, alternative, and integrative medicine course: One medical school’s experience. Journal of Alternative & Complementary Medicine, 16(5), 601-605. https://doi.org/10.1089/acm.2009.0276
Rees, C. E., Wearn, A. M., Dennis, I., Amri, H., & Greenfield, S. M. (2009). Medical students’ attitudes to complementary and alternative medicine: Further validation of the IMAQ and findings from an international longitudinal study. Medical Teacher, 31(2), 125-132. https://doi.org/10.1080/01421590802139724
Sadeghi, M., Rabiepoor, S., Forough, A. S., Jabbari, S., & Shahabi, S. (2016). A survey of medical students’ knowledge and attitudes toward complementary and alternative medicine in Urmia, Iran. Journal of Evidence-Based Integrative Medicine, 21(4), 306-310. https://doi.org/10.1177/2156587215605751
Samara, A. M., Barabra, E. R., Quzaih, H. N., & Zyoud, S. H. (2019). Use and acceptance of complementary and alternative medicine among medical students: A cross sectional study from Palestine. BMC Complementary & Alternative Medicine, 19(1), 78. https://doi.org/10.1186/s12906-019-2492-x
Schmidt, K., Rees, C., Greenfield, S., Wearn, A. M., Dennis, I., Patil, N. G., Amri, H., & Boon, H. (2005). Multischool, international survey of medical students’ attitudes toward “holism”. Academic Medicine, 80(10), 955-963. https://doi.org/10.1097/00001888-200510000-00017
Shani-Gershoni, Z., Freud, T., Press, Y., & Peleg, R. (2008). Knowledge and attitudes of internists compared to medical students regarding acupuncture. Israel Medical Association Journal, 10(3), 219-223.
Sharma, V., Holmes, J., & Sarkar, I. (2016). Identifying complementary and alternative medicine usage information from internet resources. A systematic review. Methods of Information in Medicine, 55(4), 322-332. https://doi.org/10.3414/ME15-01-0154
Syverstad, D., Norheim, A., & Fonnebo, V. (1999). Changes in medical students’ attitudes toward acupuncture: The possible impact of role models. Education for Health: Change in Learning & Practice, 12(2), 195-210.
Templeman, K., Robinson, A., & McKenna, L. (2015). Student identification of the need for complementary medicine education in Australian medical curricula: A constructivist grounded theory approach. Complementary Therapies in Medicine, 23(2), 257-264. https://doi.org/10.1016/j.ctim.2015.02.002
Thomson, P., Jones, J., Evans, J. M., & Leslie, S. L. (2012). Factors influencing the use of complementary and alternative medicine and whether patients inform their primary care physician. Complementary Therapies in Medicine, 20(1-2), 45-53. https://doi.org/10.1016/j.ctim.2011.10.001
Torkelson, C., Harris, I., & Kreitzer, M. J. (2006). Evaluation of a complementary and alternative medicine rotation in medical school. Alternative Therapies in Health and Medicine, 12(4), 30-34.
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMAScR): Checklist and explanation. Annals of Internal Medicine, 169, 467-473. https://doi.org/10.7326/M18-0850
Wetzel, M. S., Eisenberg, D. M., & Kaptchuk, T. J. (1998). Courses involving complementary and alternative medicine at US medical schools. Journal of the American Medical Association, 280(9). https://doi.org/10.1001/jama.280.9.784
Wong, W. C., Lee, A., Wong, S. Y., Wu, S. C., & Robinson, N. (2006). Strengths, weaknesses, and development of Traditional Chinese Medicine in the health system of Hong Kong: Through the eyes of future Western doctors. Journal of Alternative & Complementary Medicine, 12(2), 185-189; 191-182. https://doi.org/10.1089/acm.2006.12.185
Xie, H., Sang, T., Li, W., Li, L., Gao, Y., Qiu, W., & Zhou, H. (2020). A survey on perceptions of complementary and alternative medicine among undergraduates in China. Evidence-Based Complementary & Alternative Medicine: eCAM, 2020, 9091051. https://doi.org/10.1155/2020/9091051
Xue, C. C., Zhang, A. L., Lin, V., Da Costa, C., & Story, D. F. (2007). Complementary and alternative medicine use in Australia: A national population-based survey. Journal of Alternative & Complementary Medicine, 13(6), 643-650. https://doi.org/10.1089/acm.2006.6355
Yeo, A. S., Yeo, J. C., Yeo, C., Lee, C. H., Lim, L. F., & Lee, T. L. (2005). Perceptions of complementary and alternative medicine amongst medical students in Singapore – A survey. Acupuncture in Medicine, 23(1), 19-26. https://doi.org/10.1136/aim.23.1.19
Yildirim, Y., Parlar, S., Eyigor, S., Sertoz, O. O., Eyigor, C., Fadiloglu, C., & Uyar, M. (2010). An analysis of nursing and medical students’ attitudes towards and knowledge of complementary and alternative medicine (CAM). Journal of Clinical Nursing, 19(7-8), 1157-1166. https://doi.org/10.1111/j.1365-2702.2009.03188.x
Zollman, C., & Vickers, A. (1999). What is complementary medicine? British Journal of Medicine, 319(7211), 693-696. https://doi.org/10.1136/bmj.319.7211.693
*Justin Bilszta
Department of Medical Education,
Melbourne Medical School,
University of Melbourne, Australia
Parkville, Australia 3052
Tel: +61 3 8344 7826
Fax: +6567775702
Email: jbilszta@unimelb.edu.au
Submitted: 6 November 2020
Accepted: 27 January 2021
Published online: 5 October, TAPS 2021, 6(4), 92-106
https://doi.org/10.29060/TAPS.2021-6-4/OA2459
Ardi Findyartini1,2, Natalia Widiasih Raharjanti3, Nadia Greviana1,2, Gregorius Ben Prajogi4 & Daniar Setyorini2
1Department of Medical Education, Faculty of Medicine Universitas Indonesia, Indonesia; 2Medical Education Center, Indonesian Medical Education and Research Institute (IMERI), Faculty of Medicine, Universitas Indonesia, Indonesia; 3Department of Psychiatry, Faculty of Medicine, Universitas Indonesia, Indonesia; 4Department of Oncology Radiation, Faculty of Medicine, Universitas Indonesia, Indonesia
Abstract
Introduction: E-portfolio may facilitate the entrustment process from supervisors to residents in postgraduate medical education. The present study was aimed at identifying necessary features of an e-portfolio application and to conduct pilot study in a teaching hospital.
Methods: Six programs participated. Eight interviews with education directors and six focus group discussions with residents and supervisors were completed for the needs analysis stage. The application was developed based on the thematic analysis of the needs analysis stage. The mobile-app e-portfolio pilot was conducted for four weeks and a modified version of the System Usability Scale (SUS) was distributed to participants following the pilot program.
Results: Key features of the e-portfolio were identified. A total of 45 supervisors and 66 residents participated in the pilot study. The residents utilised the application according to the clinical activities and supervision level, and the information was fed to the supervisors as per the application design. Challenges during the pilot study in terms of feedback provision and residents’ workload which influence the e-portfolio use for entrustment decisions are discussed.
Conclusion: Current e-portfolio features were created for supervision and are potential to facilitate the entrustment process in Entrustable Professional Activities (EPA) implementation. The pilot study highlighted challenges of the implementation which should be considered for future improvement.
Keywords: Postgraduate Medical Education, E-Portfolio, Entrustable Professional Activities, Supervision, Needs Analysis, Pilot Study
Practice Highlights
- Development of assessment application, including e-portfolio, should consider input from the stakeholders.
- The e-portfolio should further be defined to emphasise the documentation, reflection, and feedback processes.
- Consideration of adequate evidence for EPA should be determined based on the aim of the e-portfolio.
- A robust e-portfolio implementation will potentially support the implementation of EPA.
- Challenges in e-portfolio implementation should be aware of and tackled for future improvement.
I. INTRODUCTION
Supervision is a critical component of postgraduate medical education as it allows residents to have a gradual achievement of competencies while still fulfilling patient safety standards. Patient care conducted by residents under adequate supervision can have results comparable to the care provided by more experienced medical doctors (Farnan et al., 2012). To entrust the resident, a supervisor considers several factors, including incidents experienced during supervision, the resident’s characteristics, the results of assessments, and encountered situations (Cianciolo & Kegg, 2013).
Ten Cate et al. (2015) introduced the Entrustable Professional Activities (EPA) concept to facilitate the implementation of a competency-based curriculum in the workplace (Ten Cate et al., 2015). EPAs are observable and measurable units of work that can correspond to competency milestones, allowing for safe and effective performance (Carraccio et al., 2017). Easily accessible and interpreted information about a resident’s past performance using the EPA concept is, therefore, suggested to facilitate the entrustment process, both for ad-hoc and summative purposes (Hauer et al., 2013; Ten Cate et al., 2015).
Entrustment decision-making refers to a supervisor’s decision to trust a resident to carry outpatient care ‘without supervision’ (Crossley et al., 2011; Ten Cate, 2006; Weller et al., 2014). Given the need for assured patient safety, ‘without supervision’ refers to the reduction of educational supervision and the provision of ‘relational autonomy’, whereby interdependence between the resident, the supervisor, the healthcare team, and the healthcare system becomes critical (Holmboe et al., 2011). However, the amount of data accessible about a resident’s performance should be analysed comprehensively to enable ad-hoc entrustment (Sandhu, 2018).
Logbooks and portfolios have been considered as workplace-based assessment methods that would enable summarising a resident’s performance as well as maintaining assessment results during training (van Tartwijk & Driessen, 2009). Electronic portfolios, or e-portfolios, are believed to increase the accessibility of a portfolio in medical training provided that the purpose of the portfolio development is well defined, such as for learning, assessment, or continuing professional development (Deketelaere et al., 2009, Tepper et al, 2020; van Tartwijk & Driessen, 2009). Generally, an e-portfolio aims to monitor a resident’s competency development and to stimulate the capacity for self-reflection (Meeus et al., 2006).
An e-portfolio may consist of a list of a resident’s performance, the supporting evidence, and the resident’s self-reflection (van der Schaaf, et al., 2017). The content is specific according to the e-portfolio’s purpose and the required activities/competencies for the resident at each level (Mulder et al., 2010). The use of an e-portfolio with a mobile application and updated evidence of residents’ performance potentially enhance informed decision-making in the entrustment process, and hence, it can be embedded in the resident supervision system (Ten Cate et al., 2016). An exploratory study in Australia showed that an EPA-driven e-portfolio model assisted trainees and supervisors in agreeing upon expected trainees’ performance in order to obtain competence level (Bramley et al., 2020).
Implementation of e-portfolio as a supporting system for EPA should consider supporting and hindering factors specific to an institution. Implementation of best practices in this area can be accompanied by an exploration of the most suitable system according to the stakeholders’ needs. Therefore, the current study aimed to explore stakeholders’ needs and develop a mobile-app e-portfolio model in a teaching hospital with various postgraduate medical education programmes located in a resource-limited setting. The study also aims to identify challenges of e-portfolio implementation. The research questions of this study were: (1) What are mobile-app e-portfolio features needed to support EPA implementation in the current teaching hospital? (2) How do stakeholders perceive the use of the developed mobile-app e-portfolio during the pilot study?
II. METHODS
A. Context
Cipto Mangunkusumo General Hospital (CMGH) is the main teaching hospital for the Faculty of Medicine Universitas Indonesia (FMUI) and is located in Jakarta, Indonesia. All 31 study programmes implement a competency-based medical curriculum and EPA approach. CMGH is obliged to have all study programmes participate in clinical activities, which are gradually entrusted to residents in accordance with the resident’s level. The EPA document in form of a matrix is then used to develop supervision system. Supervisors are trained to provide feedback through compulsory clinical teacher training conducted by the faculty. Assessment documentation has been conducted mostly manually in hardcopies for all study programs; consequently, tracking the residents’ performance to provide formative or summative EPA decisions has been challenging in the current setting.
B. Design
This study is participatory action research with a mixed -method approach. The exploration stage was aimed at exploring the needs and features expected from the mobile application. Following the exploration stage, the research team in collaboration with a professional vendor developed the mobile-app e-portfolio according to the results of the exploration stage. The pilot implementation phase aimed to implement and train residents and supervisors in the use of the application. A follow-up evaluation was conducted to assess users’ perception about the use of the e-portfolio application.
C. Respondents
Respondents of this study were education leaders from the medical school and the teaching hospital. Residents, clinical teachers, and administrators from six study programs representing medicine, surgery, and diagnostic: anaesthesiology and intensive care, obstetrics and gynaecology, psychiatry, oncology radiation, radiology, and internal medicine at CMGH/FMUI were recruited with maximum variety sampling method taking into account gender, age, and length of study (residents) or work (clinical teachers). Detailed information of the study was given to all participants who then provided written consents prior to the interviews and completion of the questionnaire.
D. Data Collection
The exploration stage involved interviews with: (1) residency programme directors; (2) education leaders from the medical school and the teaching hospital. Focus group discussions (FGDs) were also conducted with clinical teachers and residents from the six study programmes. The guiding questions of the interviews and FGDs were developed according to e-portfolio and EPA concepts used in medical education, and are shown in Table 1. The data obtained were used as a reference for further development of the application’s content and features. In addition, the EPA document from each study program was also analysed as baseline data for developing the platform.
Following the development of the application, a four-week-long pilot implementation was conducted in November 2018. After week four, the back-end system data were analysed. Supervisors’ and residents’ perceptions of the use of mobile-app e-portfolio for supporting EPA were collected using a modified questionnaire of System Usability Scale (SUS) (Brooke, 1986). Active commentaries were also added in the questionnaire to obtain users’ suggestions:

Table 1. Guiding questions of interviews and focus groups
E. Data Analysis
The transcripts of interviews and FGDs of the need analysis stage were analysed using thematic analysis. The agreed subthemes and themes and the results of the analysis of EPA documents from each study program were then translated into a computational framework to be developed as mobile application e-portfolio’s features, also considering the best practice and theoretical framework of e-portfolio development and EPA practice.
Back-end data of the activities, case variations, and supervisors’ feedback were descriptively analysed using SPSS IBM 22.0. The words submitted on the reflection-on-action section of each activity were counted along with the feedback recorded by the supervisors. Residents’ reflections were categorised into those with descriptions of difficulties (DD), lessons learned (LL), and action plans (AP). The feedback recorded was classified into descriptive (D), constructive (C), and neither descriptive nor constructive (N) categories.
The modified SUS questionnaires were descriptively analysed using chi-square/fisher exact analysis (SPSS 22.0) to compare residents’ and supervisors’ perceptions. The active commentaries in the questionnaire were also thematically analysed to identify areas of improvement in the e-portfolio development.
III. RESULTS
A. Exploration Stage
Eight in-depth interviews were conducted with each residency program director as well as with the leader of FMUI and with teaching hospital director representatives. Two FGDs were conducted, each with three study programmes faculty members. In addition, three FGDs were conducted, each with two study programmes resident representatives. The number and characteristics of the participants are described in Table 2.
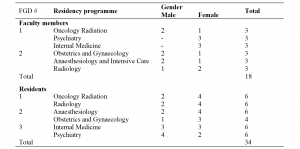
Table 2. Characteristics of Focus Group Discussion (FGD) Participants in Exploration Stage
Four main themes and 22 subthemes were identified during the exploration stage. The main themes identified were (1) resident supervision; (2) current implementation of workplace-based assessments; (3) current implementation of portfolios and logbooks; and (4) development of the mobile application e-portfolio.
|
|
Theme |
Subtheme |
# of Quotes |
Quotations |
|
1 |
Resident supervision |
Constraints in supervision (faculty members, patient/clinical cases) |
59 |
“For example, during the mid-level programme, residents were required to be fully supervised, but when they should be fully supervised was not specifically stated.” (W1, p. 1) |
|
|
|
Form of supervision |
46 |
“…we should report to the supervisor when anything goes wrong to get feedback; otherwise, it will become our fault.” (FGD 2, [R5], p. 2) |
|
|
|
Determination of entrustment (written curriculum, residents and patients factor, workplace, agreement among faculty members) |
42 |
“At some point, we might feel that the resident is eligible to perform the procedure after he/she has observed several times, and then we try to let him/her give it a try, but we are actually risking our trust…” (W7, p. 5) |
|
|
|
Background and determination of supervision (workplace, resident’s educational stage) |
26 |
“Supervision was given hierarchically; the third-year residents attain duty as the chief, supervisor, and the highest form was division of weekly rounds.” (FGD 4, [R1], p. 2) |
|
|
|
Documentation of supervision level |
10 |
“Our logbook contains a very clear explanation about supervision level, such as what cases should be achieved so that we can evaluate and reflect on our progress in one semester.” (FGD 3, [R6], p. 9)
|
|
2 |
The current implementation of workplace-based assessment |
Scheduled WBA |
17 |
“During each rotation, residents and consultants were scheduled with case-based discussions or miniCEX; while for surgical DOPS, [it] is not specifically scheduled because it depends on the availability of the case.” (W3, p. 1) |
|
|
|
WBA as stage step-up procedure |
6 |
“In our programme, there are several cases we need to get done at each level, usually cases written in the logbook.” (FGD 2, [R7], p. 3) |
|
|
|
Based on the written curriculum |
4 |
“In our programme, we arrange evaluation at every level. We evaluate every intern according to the required competency they should achieve.” (FGD 4, [R3], p. 7) |
|
3 |
The current implementation of portfolio and logbook |
Technical portfolio and logbook implementation (as monitoring, communication, and assessment instrument) |
26 |
“On a routine basis, the form was filled in each afternoon, when the patient’s information, such as name, weight, and height, are recorded.” (FGD 2, [R7], p. 4) |
|
|
|
Constraints in portfolio and logbook implementation (lack of ownership, faculty member factor) |
38 |
“Due to the enormous workload every day, such as examining patients, attending division rounds, filling out electronic health records, and receiving so many instructions, they couldn’t complete the logbook routinely. Besides, the supervisor might find it unnecessary to write down their supervision in the log book after discussions, rounds, or treatments.” (W2, p. 10) |
|
|
|
Understanding of portfolio and logbook for residents’ development (clinical, academic, non-academic)
|
24 |
“Portfolio consists of one’s creativity, innovation, and organisation experiences.” (W8, p. 1) |
|
4 |
Development of the mobile application-based e-portfolio |
Residents’ performance and experience (clinical and academic) tracking |
20 |
“We evaluated one intern’s competency in ultrasound, and the result wasn’t quite satisfying. It turned out that this intern lacked of practice that could’ve been done every day since the cases were quite abundant.” (W6, p. 10) |
|
|
|
User-friendliness and real-time access |
18 |
“The application may have to be ‘consultant-friendly,’ so they can finish it in a click.” (FGD 2, [R3], p. 7) |
|
|
|
Feedback documentation |
13 |
“In my opinion, there has to be some immediate feedback.” (FGD 2, [R5], p. 7) |
|
|
|
Accessibility and confidentiality |
11 |
“As they save the record of the treatment that has been checked by the doctor in charge, they can no longer change it because only the supervisor has the authority to change.”(FGD 4, [R4,] p. 19) |
|
|
|
Encompass achievement of competence and modules within the curriculum |
7 |
“We want it to be comprehensive, so it can be evaluated. This is about clinical skills, but then the related academic skill is also important.” (W4, p. 9) |
|
|
|
Ensuring patients were treated by competent and authorised residents |
4 |
“We need to ensure that the patient is treated by competent, authorised, and certified doctors.” (W7, p. 10) |
|
|
|
Reminder and consequences for undocumented activity |
5 |
“There must be something to force the resident to write down his activity so the next day, he can keep up with the new tasks.” (W2, p. 10) |
|
|
|
Paperless attribute, but printable if needed |
6 |
“The record and the format will be the students’ database as well as the supervisors’. Therefore, it needs to be printable for our benefit.” (FGD 2, [R3], p. 7) |
|
|
|
Integrated with service care system |
3 |
“We have to write down the same thing repetitively in so many books and records.” (FGD 3, [R8], p. 12) |
|
|
|
Collect important evidence of accomplishments (cases and complications, image documentation) |
4 |
“Compiling the number of cases is required, and reporting complications in cases is equally important. Let’s say they are in the third level, but complications occurred in most of the procedures they performed.” (W3, p. 7)
|
Table 3. Themes and Subthemes Identified in Exploration Stage
According to the analysis conducted in the exploration stage, stakeholders expected the availability of various features in the mobile application-based e-portfolio. However, it was not possible to accommodate all of the identified features at the implementation stage. The authors identified the key features in order to develop a generic application, taking into consideration the findings related to the current implementation of a workplace-based assessment, portfolios and logbooks, supervision, level of entrustment, and other technical issues. Also considered were the identified basic needs of the teaching hospital, study programmes, faculty members, and residents, along with best practice principles related to application development.
Some of the key features derived from the analysis included in the implementation stage were the following:
1) Supervisors and administrators are allowed to track residents’ performance and achievements.
2) A drop-down menu is used in most form segments for easier and user-friendly data input.
3) Feedback from the clinical supervisor is recorded on each data input.
4) Clinical cases, supervision level, and type of clinical authorities are set according to the residential programme and the resident’s educational stage.
5) Guided self-reflection questions for the resident are mandatory on each data input.
6) Attachment of supporting image as evidence is facilitated for each data input.
The application was divided into two platforms: for residents and supervisors. The menus in the residents’ application included activity list, activity input, report, and profile, among others. While submitting new activity into the platform, residents must fill in the information related to each clinical activity, describe the activity according to the given guided reflection-on-action features, and provide evidence form of photographs (if applicable). The supervisor application had only one main feature for reviewing and providing feedback on activities previously submitted by residents. The figure of the application and its overall process of the application is shown in the appendix.
B. Pilot Implementation Stage
During the four-week-long pilot programme, the residents were encouraged to submit as much evidence as possible related to patient care to the e-portfolio platform. The evidence was automatically sent to assigned faculty members’ platform in order to get feedback. Observations were conducted by evaluating the data input from the application’s backend to obtain data regarding the utilisation frequency and types of cases input in the mobile application in each residency programme. A total of 311 activities were submitted into the application during the four-week-long pilot programme; however, only 98 (31.5%) activities received feedback from clinical supervisors. Table 4 describes the results of the average word count analysis of the residents’ reflection-on-action and the feedback received in the mobile application e-portfolio during the implementation stage.
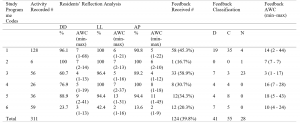
Table 4. Activity Report of the Pilot Programme: Recorded Activity, Residents’ Reflections and Feedback from Supervisors
1: Psychiatry, 2: Internal Medicine, 3: Obstetrics & Gynaecology, 4: Anaesthesiology & Intensive Care, 5: Oncology Radiation, 6: Radiology; DD: description of difficulties
LL: lessons learned, AP: action plan, D: descriptive feedback, C: constructive feedback, N: neither descriptive nor constructive feedback, AWC: average word count
The feedback received covered a wide range of competencies: clinical skills, knowledge, and patient care. The quotations below are completed with codes explaining the details as follows: a. FB which stands for Feedback; b. Number (1-6) which refers to the study programme 1 to 6; and c. Last number (e.g 9, 15) which refers to the list number of feedback comment in the system.
“Spinal USG exercise on new-born infants to improve skills.”
(FB, (5), 9)
“Learn about the differences in fracture due to trauma, metastasis, and infection.”
(FB, (5), 13)
Although most feedback obtained from supervisors was classified as descriptive or “neither descriptive nor constructive”, there was some constructive feedback, describing not only what to do but also how to do it and improve the residents’ performance.
“Volume target determination was excellently and efficiently carried out. Effective and efficient communication could be achieved even by telephone. There were few problems in terms of work efficiency because no confirmation was made about which work had and/or had not been done by the supervisor. However, the overall process and results were excellent.”
(FB, (4), 9)
The users’ evaluations on the mobile application-based e-portfolio were obtained using a modified version of the SUS questionnaire at the end of the pilot programme. The pilot study participants included 45 faculty members and 66 residents. Out of a total of 111 questionnaires distributed, a total of 92 questionnaires were received back: 37 faculty members’ response (84%) and 55 residents’ response (82%). The results showed that the faculty members and residents had similar views regarding most aspects evaluated by the questionnaire. Comparisons between the proportions were conducted using a chi-square test—which showed significant differences between faculty members’ and residents’ perceptions on seven items as shown in Figure 1. The complete result of the SUS questionnaire is provided in Appendix 2.
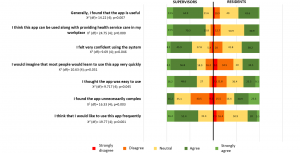
Figure 1. Comparison among supervisors and residents satisfaction on the e-portfolio application
The results of the thematic analysis of the active commentaries in the questionnaire revealed four main themes:
1) Participants believed that the application was user-friendly but needed improvement in some features and interfaces.
“The display can be improved so the most frequent treatment can be put on top. Thus no repeated scrolling down is needed.”
Commentaries- resident-1 (52)
2) Some constraints identified were: the length and number of forms to be filled in the mobile application, the lack of notifications, case grouping according to clinical rotation, as well as the needs for integration with electronic health records and other established applications in each study programme.
“…filling the apps is burdening residents with a bunch of caseload. The interface has to be simplified, with the option to pick certain cases without deeply analysing each case (e.g. there were 50 cases today yet only 2 unique/interesting cases which required special attention, etc.).”
Commentaries-resident-6 (46)
3) Both faculty members and residents similarly noted utilisation of the application to facilitate supervision.
“All supervising needs have been accommodated.”
Commentaries-faculty-1(91)
“Supervisor’s verification system was a good thing.”
Commentaries-residents-3 (8)
4) Lastly, the participants felt that the availability of the feedback feature was positive, despite some identified constraints in giving feedback.
“The most important feature of this, I think is the feedback giving and follow-up plan.”
Commentaries-faculty-5(63)
IV. DISCUSSION
This study highlights the development of an app-based e-portfolio in the teaching hospital of a resource-limited setting. The study was able to identify key features of the e-portfolio based on the stakeholders’ (i.e programme coordinators, supervisors, and residents). Several challenges which should be addressed for future improvement were also identified in the pilot study.
The first stage of the study was able to explore the perceptions of users which informed the e-portfolio. The users identified the need of a portfolio (Crossley et al., 2011) for documenting residents’ achievements over time and for assessing coverage of clinical case management. The use of a portfolio in digital form in this study also aimed to facilitate the process of supervising residents working in the teaching hospital. The supervision system in the current teaching hospital adopted the EPA concept (Carraccio et al., 2017; Ten Cate et al., 2015), which had been in use for the past 2 years in the six study programmes.
The use of an e-portfolio is not particularly new in postgraduate training (Kjaer et al., 2006), but the particular use for facilitating supervision of residents has, to the best of the authors’ knowledge, rarely been reported (van der Schaaf et al., 2017). Reported challenges of e-portfolio are the residents’ burden despite the use of an electronic platform (Birks et al., 2016; Vance et al., 2017), the reliability of a workplace-based assessment portfolio (Castanelli et al., 2019), and the fact that time issues in clinical practice should always be taken into consideration (Binhimd et al., 2017). Heeneman and Driessen hence clarify that it is necessary to determine whether portfolio development by residents is voluntary or compulsory (Heeneman & Driessen, 2017). Based on the framework, the current e-portfolio can be categorised as a combination of a training and personal development portfolio, which comprises mandated required skills and competencies in a fixed format as well as personal reflections of progress (Heeneman & Driessen, 2017). In addition, the use of mobile application was expected to support the use of e-portfolio for residents’ learning in a busy clinical setting (Mok et al., 2019).
An important framework that was adopted in the e-portfolio platform in this study is the EPA. EPA development calls for the consideration of competencies, clinical settings, the entrustment process and stakeholders’ agreements, including those of staff/supervisors and experts (Ten Cate et al., 2015), residents, the teaching hospital and even patients, if applicable (Lundsgaard et al., 2019).
The authors of the present study identified the potential value of a portfolio as a tool to provide ad-hoc supervisor decision-making, based on the study by van der Schaaf et al. (2017). Based on the reflections in the six study programmes, the e-portfolio incorporated residents’ performance, supervisors’ feedback, and evidence of achievement that is in line with the expected level of competencies or EPAs in the curriculum. The evidence is required by supervisors for deciding on a level of entrustment. A study involving experienced obstetrics and gynaecology supervisors in the Netherlands suggests that both formal and informal entrustment processes are used in combination on a daily basis. Informal entrustment is thought to provide more flexibility because it can be adjusted more easily than a formal one (Castanelli et al., 2019).
Based on the analysis in the exploration stage of the present study, the platform was designed to accommodate entries by a resident which were then responded to by a supervisor directly in the clinical setting or indirectly through the application (with the supervisor’s presence according to the EPA and supervision level for particular case managements/procedures). According to van der Schaaf et al. (2017), the current e-portfolio adapted both a student model that provided achievement monitoring and a feedback model that provided personalised feedback. The data visualisation in the current study was not yet used for the supervisors’ entrustment process and is a subject for further development of the application and back-end data analysis.
The e-portfolio application in this study was designed to include a feedback model, which was initiated by reflection by the resident. As described in Table 5, despite the number of recorded activities, only 12.5–45% of them received written feedback from the supervisors. Of these, most of the feedback was descriptive or constructive. Before providing or documenting feedback in the application, the supervisor may verify the case or do so after observing the resident performing the procedure.
Apart from the residents of the Radiology programme, almost all residents documented their reflections on the encountered clinical cases: the difficulties, lessons learned, and action plans (Table 3). The residents’ reflections were considered as one of the key successes of the portfolio implementation (Binhimd et al., 2017), and it is also a best practice in feedback provision in clinical training (Bounds et al., 2013; Kornegay et al, 2017; Ramani & Krackov, 2012). The residents in the pilot study displayed a good habit of feedback-seeking behaviour by initiating their reflections. Given the burden of daily routine in the teaching hospitals, the quality of the written reflections completed by residents was of concern in this study. Further consideration to moderate the frequency of reflections should be incorporated hence the residents can practice more in-depth reflections which are necessary for more meaningful feedback and future actions for improvement.
All reflections and feedback were given in less than 50 words; hence, it is again considered feasible for the users to conduct brief reflection and feedback within the application. The residents’ feedback showed that it was one of the most important features of the application, which supported their learning. Despite this, a rather low amount of feedback with low word counts was given to the residents during the pilot study, raising concerns that despite the feedback training given to supervisors, the use of the application did not necessarily increase the amount and quality of documented feedback. As suggested by Brehaut et al. (2016), the format of feedback delivery matters, and it is preferable to avoid the cognitive overload of the recipients in the use of an electronic platform, as attempted in the current application. The limited amount of feedback documented during the pilot study, however, did not reflect the actual practice of giving feedback in the current setting. The documentation of feedback was expected to facilitate the long-term monitoring of residents’ progress (van der Schaaf et al., 2017), which may prompt supervisors’ summative entrustment decisions. The residents’ feedback in this study also highlighted the need for deeper reflection on the voluntary selection of clinical activities, so that the resident did not have to input all encountered cases. This might increase the user-friendliness of the application, yet it might require further agreement with the supervisors and the study programme coordinators.
The evaluation of the supervisors and residents in the pilot study showed that supervisors perceived more positively the use of the apps, compared to the residents. From the supervisors’ point of views, accessibility of online data on resident’s performance was responded to very positively given current challenge in tracking this in manual documentation. From the residents’ point of views, this might be due to that despite the potential of the current application to enable clinical supervision, submitting data into the application felt like an addition to the residents’ workload, due to redundancy in submitting information into both e-portfolio platform and the e-hospital medical records. The workload of residents in teaching hospitals has been a controversial issue in postgraduate medical education (Nishigori et al., 2015). The stakeholders should agree on which data are compulsory and critical for evaluation and which are voluntary in the e-portfolio, both for training and patient care purposes. In addition, the authors also realised that training on portfolio development and supervision should be supported with a longitudinal mentoring process and an analysis of longitudinal performance (Heeneman & Driessen, 2017).
A. Study Limitations
The study has some limitations. The study was conducted at one teaching hospital and involved a limited number of study programmes. Given that Cipto Mangunkusumo is one of the busiest national referral hospitals, with complex cases and high workloads, the perspectives of key stakeholders explored in this study were critical for consideration in the development of an e-portfolio mobile application. In addition, the study was able to identify the features of an e-portfolio that can potentially support the supervision and entrustment processes. Future versions of the e-portfolio application aimed at enhancing the quality of supervision should consider the analysis of the residents’ longitudinal performance through prompt data analysis in the system, thereby supporting formative and summative entrustments during clinical supervision as well as the integration of an adequate mentoring system.
V. CONCLUSION
The present study explored the stakeholders’ need of an e-portfolio for supervision that enables all parties to monitor learning progress and competency achievement. On top of the implementation of workplace-based assessments and EPA systems in the respective study programmes, the identified key features of an e-portfolio mobile application reflect the needs of residents, faculty/supervisors, the teaching hospital, and the school of medicine.
The pilot implementation showed that the e-portfolio mobile application was feasible and potential for use by residents, supervisors and programme coordinators in monitoring EPAs and competence achievement in the current setting, with highlighted challenges that need to be tackled in the future. The platform’s use in assisting entrustment decisions should be further confirmed with a longitudinal analysis of the residents’ performance and the use of the analysis by the supervisors. The development of such an e-portfolio to support EPA in other settings should consider the dynamics of case complexity, residents’ level of competence and entrustment, workload, the healthcare system, and the education system. Finally, in a resource-limited setting, the involvement of stakeholders from the start to prioritise the e-portfolio features, user-friendliness, and technology feasibility should always be considered.
Notes on Contributors
Ardi Findyartini reviewed the literature, designed the study, conducted interviews and focus group discussions, analysed transcripts and led the manuscript writing.
Natalia Widiasih reviewed the literature, designed the study, conducted interviews and focus group discussions, analysed transcripts and wrote the manuscript.
Nadia Greviana conducted interviews and focus group discussions, analysed transcripts and wrote the manuscript.
Gregorius Ben Prayogi conducted interviews and focus group discussions, analysed transcripts and gave critical feedback in the manuscript writing.
Daniar Setyorini coordinated the e-portfolio development and data collection, analysed transcripts and gave critical feedback in the manuscript writing.
All authors have read and approved the final manuscript.
Ethical Approval
Ethical approval for this study was granted by the Faculty of Medicine Universitas Indonesia – Cipto Mangunkusumo Hospital Research Ethical Review Board (2018) Number: 328/UN2.F1/ETIK/III/2018.
Data Availability
Data will be available upon request to corresponding author due to conditions of consent provided by respondents in this study and that it should abide data sharing policy from the medical school and teaching hospital where the study was completed.
Acknowledgement
The authors would like to thank CMGH, FMUI and IMERI for the organisational supports. The authors would also like to extend gratitude to all six participating study programmes, the programme directors, the residents, and the supervisors. Finally, the authors would like to thank Dr. Sri Puspita, who facilitated data collection for the study.
Funding
This study was funded by Dr. Cipto Mangunkusumo General Hospital Operational Grant 2018.
Declaration of Interest
All authors state no possible conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Binhimd, B., Al-Jifrfee, H. M. A., & Khan, M. A. (2017). Identifying the perceived challenges that affect the use of portfolio as an assessment tool for family medicine residents in Jeddah program. MedEdPublish, 6(2), 1–12. https://doi.org/10.15694/mep.2017.000070
Birks, M., Hartin, P., Woods, C., Emmanuel, E., & Hitchins, M. (2016). Students’ perceptions of the use of eportfolios in nursing and midwifery education. Nurse Education in Practice, 18, 46–51. https://doi.org/10.1016/j.nepr.2016.03.003
Bounds, R., Bush, C., Aghera, A., Rodriguez, N., Stansfield, R. B., Santen, S.A., & MERC at CORD Feedback Study Group (2013). Emergency medicine residents’ self-assessments play a critical role when receiving feedback. Academic Emergency Medicine, 20(10), 1055–1061. https://doi.org/10.1111/acem.12231
Bramley, A. L., Thomas, C. J., & Kenna, L. M. (2020). E-portfolios and entrustable professional activities to support competency-based education in dietetic education. Nursing Health Science, 1-9. https://doi.org/10.1111/nhs.12774
Brehaut, J., Colquhoun, H., Eva, K., Carrol, K., Sales, A., Michie, S., Ivers, N., & Grimshaw, J. M. (2016). Practice feedback interventions: 15 suggestions for optimizing effectiveness. Annals of Internal Medicine, 164(6), 435–461. https://doi.org/10.7326/M15-2248
Brooke, J. (1986). SUS- A quick and dirty usability scale. Digital Equipment Corporation. https://hell.meiert.org/core/pdf/sus.pdf Accessed October 30, 2018
Carraccio, C., Englander, R., Gilhooly, J., Mink, R., Hofkosh, D., Barone, M. A., & Holmboe, E. S. (2017). Building a framework of entrustable professional activities, supported by competencies and milestones, to bridge the educational continuum. Academic Medicine, 92(3), 324–330. https://doi.org/10.1097/ACM.000000000000114
Castanelli, D. J., Moonen-van Loon, J. M. W., Jolly, B., & Weller, J. M. (2019). The reliability of a portfolio of workplace-based assessments in anesthesia training (Fiabilité d’un portfolio d’évaluations sur le lieu de travail dans la formation en anesthésie). Canadian Journal of Anesthesia Can d’anesthésie [Internet], 66(2), 193–200. https://doi.org/10.1007/s12630-018-1251-7
Cianciolo, A. T., & Kegg, J. A. (2013). Behavioral specification of the entrustment process. Journal of Graduate Medical Education, 5(1), 10–12. https://doi.org/10.4300/JGME-D-12-00158.1
Crossley, J., Johnson, G., Booth, J., & Wade, W. (2011). Good questions, good answers: Construct alignment improves the performance of workplace-based assessment scales. Medical Education, 45(6), 560–569. https://doi.org/10.1111/j.1362-2923.2010.03913.x
Deketelaere, A., Degryse, J., De Munter, A., & De Leyn, P. (2009). Twelve tips for successful e-tutoring using electronic portfolios. Medical Teacher, 31(6), 497–501. https://doi.org/10.1080/01421590802572734
Farnan, J. M., Petty, L. A., Georgitis, E., Martin, S., Chiu, E., Prochaska, M., & Arora, V. M. (2012). A systematic review: The effect of clinical supervision on patient and residency education outcomes. Academic Medicine, 87(4), 428–442. http://doi.org/10.1097/ACM.0b013e31824822cc
Hauer, K., Kolwes, J., Cornett, P., Hollander, H., ten Cate, O., Ranji, S. R., Soni, K., Iobst, W., O’Sullivan, P. (2013). Identifying entrustable professional activities in internal medicine training. Journal of Graduate Medical Education, 5(1), 54–59. https://doi.org/10.4300/JGME-D-12-00060.1
Heeneman, S., & Driessen, E. W. (2017). The use of a portfolio in postgraduate medical education – Reflect, assess and account, one for each or all in one? GMS Journal for Medical Education, 34(5). https://doi.org/10.3205/zma001134
Holmboe, E., Ginsburg, S., & Bernabeo, E. (2011). The rotational approach to medical education: time to confront our assumptions? Medical Education, 45(6), 69–80. https://doi.org/10.1111/j.1365-2923.2010.03847.x
Kjaer, N. K., Maagaard, R., & Wied, S. (2006). Using an online portfolio in postgraduate training. Medical Teacher, 28(8), 708–712. https://doi.org/10.1080/01421590601047672
Kornegay, J. G., Kraut, A., Manthey, D., Omron, R., Caretta-Weyer, H., Kuhn, G., Martin, S., & Yarris, L. M. (2017). Feedback in medical education: A critical appraisal. AEM Education and Training, 1(2), 98–109. https://doi.org/10.1002/aet2.10024
Lundsgaard, K. S., Tolsgaard, M. G., Mortensen, O. S., Mylopoulos, M., & Østergaard, D. (2019). Embracing multiple stakeholder perspectives in defining trainee competence. Academic Medicine, 94(6), 838-846. https://doi.org/10.1097/ACM.0000000000002642
Meeus, W., Van Petegem, P., & Van Looy, L. (2006). Portfolio in higher education: Time for a clarificatory framework. International Journal of Teaching and Learning in Higher Education, 17(2), 176–180.
Mok, Z. W., Lee, J. C. S., & Mathur, M. (2019). Harnessing mobile technology to develop a sustainable on the go learning resource for junior doctors. The Asia Pacific Scholar, 4(2), 48-51. https://doi.org/10.29060/TAPS.2019-4-2/SC2070
Mulder, H., Ten Cate, O., Daalder, R., & Berkvens, J. (2010). Building a competency-based workplace curriculum around entrustable professional activities: The case of physician assistant training. Medical Teacher, 32(10), e453-e459. https://doi.org/10.3109/0142159X.2010.513719
Nishigori, H., Deshpande, G. A., Obara, H., Takahashi, O., Busari, J., & Dornan, T. (2015). Beyond work-hour restrictions: A qualitative study of residents’ subjective workload. Perspectives on Medical Education, 4(4), 176–180. https://doi.org/10.1007/s40037-015-0198-4
Ramani, S., & Krackov, S. K. (2012). Twelve tips for giving feedback effectively in the clinical environment. Medical Teacher, 34(10), 787–791. https://doi.org/10.3109/01142159X.2012.684916
Sandhu, D. (2018). Postgraduate medical education – Challenges and innovative solutions. Medical Teacher, 40(6), 607–609. https://doi.org/10.1080/0142159X.2018.1461997
Ten Cate, O. (2006). Trust, competence, and the supervisor’s role in postgraduate training. British Medical Journal, 333(7571), 748–751. https://doi.org/10.1136/bmj.38938.407569.94
Ten Cate, O., Chen, H. C., Hoff, R. G., Peters, H., Bok, H., & van der Schaaf, M. (2015). Curriculum development for the workplace using entrustable professional activities (EPAs): AMEE guide No. 99. Medical Teacher, 37(11), 983–1002. https://doi.org/10.3109/0142159X.2015.1060308
Ten Cate, O., Hart, D., Ankel, F., Busari, J., Englander, R., Glasgow, N., Holmboe, E., Lobst, W., Lovell, E., Snell, L. S., Touchie, C., Van Melle, E., Wycliffe-Jones, K., & International Medical Education Collaborators (2016). Entrustment decision making in clinical training. Academic Medicine, 91(2), 191–198. https://doi.org/10.1097/ACM4.0000000000001044
Tepper, C., Bishop, J., & Forrest, K. (2020). Authentic assessment utilising innovative technology enhanced learning. The Asia Pacific Scholar, 5(1), 70-75. https://doi.org/10.29060/TAPS.2020-5-1/SC2065
Vance, G. H. S., Burford, B., Shapiro, E., & Price, R. (2017). Longitudinal evaluation of a pilot e-portfolio-based supervision programme for final year medical students: Views of students, supervisors and new graduates. BMC Medical Education, 17(1), 1–9. https://doi.org/10.1186/s12909-017-0981-5
van der Schaaf, M., Donkers, J., Slof, B., Moonen-van Loon, J., van Tartjwijk, J., Driessen, E., Badii, A., Serban, O., & Ten Cate, O. (2017). Improving workplace-based assessment and feedback by an e-portfolio enhanced with learning analytics. Educational Technology Research and Development, 65(2), 359–380. https://doi.org/10.1007/s11423-016-9496-8
van Tartwijk, J., & Driessen, E. W. (2009). Portfolios for assessment and learning: AMEE guide no. 45. Medical Teacher, 31(9), 790–801. https://doi.org/10.1080/01421590903139201
Weller, J. M., Misur, M., Nicolson, S., Morris, J., Ure, S., Crossley, J., & Jolly, B. (2014). Can I leave the theatre? A key to more reliable workplace-based assessment. British Journal of Anaesthesia, 112(6), 1083–1091. https://doi.org/10.1093/bja/aeu052
*Ardi Findyartini
Department of Medical Education & Medical Education Center
Indonesia Medical Education Research Institute (IMERI),
Faculty of Medicine Universitas Indonesia,
Jakarta, Indonesia
10430
Email: ardi.findyartini@ui.ac.id
Submitted: 19 October 2020
Accepted: 12 April 2021
Published online: 5 October, TAPS 2021, 6(4), 80-91
https://doi.org/10.29060/TAPS.2021-6-4/OA2456
Balakrishnan Ashokka1,2, Tat Leang Lee1 & Daniëlle M.L. Verstegen3
1Department of Anaesthesia, National University Health System, National University Hospital, Singapore; 2Centre for Medical Education (CenMED), Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Department of Educational Development and Research, Faculty of Health Medicine and Life Sciences, Maastricht University, Netherlands
Abstract
Introduction: There are certain factors in exam preparedness that are not well studied in the postgraduate medical education context. Non-academic predictors have been extensively researched but usually in isolation.
Methods: The study involved a sequential explanatory mixed methods research design. The study was conducted among anaesthesia postgraduates appearing for high-stake nation-wide primary examination. Data obtained by a questionnaire assessing pre-examination attributes were compared with the students’ reflections through focus group discussions (FGD) after the formal declaration of results. The examination had an overall pass rate of 42.9% (18 out of 42).
Results: The study showed that pre-examination questionnaire could identify attributes and study behaviours in the postgraduates who passed. Passers procrastinated three times lesser, pursuing a timetable-based study (conscientiousness); had higher metacognitive self-regulation (p value<0.05) applying concentrated self-directed learning & effective group study and higher self-efficacy compared to those who failed. The focus group discussions affirmed of these attributes in candidates who ‘breeze through exams’. Postgraduate success required better ‘work-study’ balance, self & cross regulation and peer and faculty support.
Conclusion: Implementing a composite tool to assess ‘exam preparedness’, we propose, would help the learners and teachers to skim for non-academic factors (metacognitive self-regulation, self-efficacy, conscientiousness) that influence the chances of success. Understanding & predicting this would help educators to identify the ‘candidates with difficulty’ and delegate personalised faculty attention. This could guide the exam candidates to have a ‘reality check’ to plan and pace their effort with peer learning, consolidated study and goal orientation.
Keywords: Postgraduate Exam Success, Non-Academic Predictors, Self-Regulation
Practice Highlights
- Non-academic attributes impact success in postgraduate examinations.
- Postgraduate exam success necessitates work-study & work-life balance.
- Time on task, self-regulation to task demands is needed when assessments are tougher and high stake.
- Exam preparedness: A collective attribute is proposed with a questionnaire to measure predictability of exam success.
- Shunning away from ‘shame of mock vivas’ spirals down to poor chance of passing.
I. INTRODUCTION
Postgraduate summative examinations have an important role in progress as a medical professional. Success in high-stakes assessments have an impact on societal impressions, career shifts and social strata changes (Hamilton & Brown, 2005; Slavin et al., 2014). Examinations ideally measure the students’ competencies, but there are reasons to think that there are factors other than academic predictors.
Learning strategies and monitoring vary across the age groups (Vermunt, 1996). High school education and learning require mastering declarative knowledge, largely through elaboration and rote memory. College students require advanced learning strategies involving skilful metacognitive knowledge monitoring (MKM) and self-regulatory strategies (SRL) (Isaacson & Fujita, 2006). Metacognition is the higher order mental process of “thinking about one’s thinking”, wherein, there are two aspects, namely the ability to reflect on the quantity & quality of knowledge acquired (MKM) and the operational strategies in pacing and preparing for the challenge ahead (SRL). Educational programs strive to facilitate this transition to become ‘adult learners’ (Ormrod, 2009).
Learning in undergraduate medical education requires ‘critical reasoning’ to assimilate relevant clinical information and deduce differential diagnoses. Postgraduate learners, particularly in the health professions, need self-regulatory skills to pace their self-directed learning in the absence of regular formative assessments. Zimmerman (2008) asserted that postgraduate learners in higher education possibly achieve superior standards of self-regulation and motivation. However, the adaptations in learning strategies or metacognitive regulatory activities are not well described in the context of postgraduate health professions. Soh (2019) described a six-step approach in the pretext of the ‘ownership cycle’ for supporting postgraduate learners with difficulty.
O’Connor and Paunonen (2007) urged researchers to ‘use multiple predictors beyond intelligence, such as personality, motivation, and study habits when predicting academic achievement’ (Ray & Brown, 2015). We set to explore how we can improve on the understanding of attributes that could be collectively stated as ‘exam preparedness’ (Appendix 1). We proposed to define ‘exam preparedness’ as:
“ability of the learner to inculcate educational situation awareness, to gauge task difficulty, assess self-efficacy, modify one’s own learning behaviour, manage self and moderate it with resources and personal capabilities, so as to plan and operationalise a scheme/ construct in exam taking aptitude & skills, resulting in comprehensive exam success”.
It is known from literature that testwiseness, “a subject’s capacity to utilise the characteristics and formats of the test and/or the test taking situation” could impact the outcomes of the examinations (Millman et al., 1965; Sarnacki, 1981; Wahlstrom & Boersma, 1968; Watling & Ginsburg, 2019). Our proposition of understanding ‘exam preparedness’ is more than coachable test-taking strategy of testwiseness, but on a broader holistic front that looks at emotive, behavioural, self-regulatory perspectives and preparedness for a task in anticipation.
II. RELEVANCE OF THE STUDY
We need ways to measure ‘exam preparedness’ because, first, it could help the postgraduate learners to identify major deficiencies in being task focussed and hone self-regulatory strategies. Second, it would help teachers to enhance support or ‘scaffolding’ that suits the needs of individual students. The concept ‘exam preparedness’ is not well constructed or described in literature. In the context of this research, we identify ‘exam preparedness’ to be everything but the student’s level of knowledge or competence. The cognitive determinants, like grade point average (GPA), are strong predictors of college success (Conard, 2006; Sladek et al., 2016; Zhou et al., 2014). In the postgraduate medical education context, where the academic capabilities are comparable and are well matched during their selection into residency, there are other non-academic attributes that could predict exam success.
The prediction of exam performance by factors such as achievement goal orientation, self-regulation, (Lucieer et al., 2016) conscientiousness (Brazdău & Mihai, 2011; Colthart et al., 2008), metacognition and meta-comprehension have been well described (Cook et al., 2011; Dunlosky & Lipko, 2007; Pintrich & De Groot, 1990; Zimmerman, 2000). The inter-relationships among these attributes are complex and not well studied. Our work was designed to help understand postgraduate students’ metacognitive, self-regulation, conscientiousness, and self-efficacy perceptions to aid in their learning.
III. METHODOLOGY
A. Study Design
The study involved a sequential explanatory mixed methods research design (McKim, 2017). The attribute of ‘exam preparedness’ was explored using existing predictors of academic success such as metacognition, self-regulation, self-efficacy and conscientiousness quotient. Data obtained by a questionnaire assessing pre-examination attributes were compared with the students’ reflections through focus group discussions, after the formal declaration of results. The mixed methods design consisted of ‘sequential approach’ where the questionnaire data collected prior to the high-stake examination provided inputs for quantitative analysis of the predictors of exam outcomes. This was followed by qualitative exploration of themes that emerged through focus group discussions. The themes summarised from the first focus group discussions were used to enhance the richness of second focus group discussion (Hennink, 2013).
B. Procedure
Anaesthesia postgraduate learners who appeared for the primary anaesthesia examinations were invited for participation in the study. These were high-stake summative examinations and mandatory for all postgraduates, limiting progression to senior years in residency and subsequent accreditation to a specialist. Informed consent was obtained for voluntary participation and confidentiality was ascertained for information on participant profiles and sensitivity of information about personal learning attributes. After approval by the institute review board, a pilot study was conducted to enhance validity of the questionnaire.
All the study participants who consented (30 out of 42 who appeared for exams) filled the pre-examination questionnaire, one month before the examinations. After completion of examinations and declaration of results, focus group interviews were conducted among students who passed the exam to explore further insights. Candidates who had not passed the examinations were excluded from the second part of study (as per Institutional Review Board (IRB) stipulations). The ‘passers’ were allocated into two sub-groups: the first-time passers or the ‘acers’, who succeeded in their first attempt and the ‘non-acers’, who were postgraduates with previous unsuccessful attempt(s) and have passed the examinations in this attempt (Figure 1).
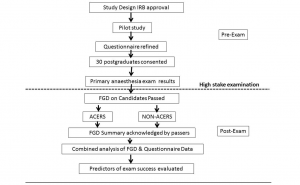
Figure 1. Procedure of the study in chronological order
After completion of focus group discussions, the results were summarised and sent back to the participants for authenticity and approval of the content (member checking). Data analysis with mixing of the quantitative and qualitative data was conducted to appraise pre-examination attributes evaluated through the questionnaire with themes that emerged from the post-examination focus group discussions.
C. Instrument
A 50-point questionnaire was designed to understand the pre-examination attributes of the postgraduate residents when they had to face a high-stake assessment. The chief themes (Table 1) that were explored included the self-regulatory aspects of cognition, motivation/affect, behaviour and context that were adopted from the Motivated Strategies of Learning Questionnaire (MSLQ) (Credé & Phillips, 2011; Pintrich & De Groot, 1990; Pintrich, 2000).
|
Themes/ Attributes |
Definition |
Existing scales/ comments |
Simple meaning |
|
Metacognition & Self-regulation |
‘the people’s knowledge of their own learning and cognitive processes, as well as their regulation of those processes to enhance learning and memory’ (Ormrod, 2009) |
MSLQ (Motivated strategies for learning questionnaire, 81 items) (Pintrich & De Groot, 1990)
MAI (Metacognitive awareness inventory, 52items) (Schraw & Dennison, 1994) |
Metacognition= thinking about one’s thinking
Self-regulation= ability to pace one’s own efforts to task
|
|
Self-efficacy |
‘personal judgments of one’s capabilities to organise and execute courses of action to attain designated goals’ (Colthart et al., 2008) |
SES (Self-efficacy survey, 150 items) (Zimmerman, 2000, 2008) |
Self-perception of effectiveness |
|
Conscientiousness |
‘a broad domain encompassing individual differences in the propensity to follow socially prescribed norms for impulse control; to be goal directed, planful, to be able to delay gratification and to follow norms and rules’ (Roberts, et al., 2009). |
CQI (Conscientiousness quotient inventory,62 items) (Brazdău & Mihai, 2011)
|
Self-disciplined planful and perseverant
Conscientiousness is one of the big 5 personality traits with well validated proven predictors of academic performance |
Table 1. Major themes in pre-examination questionnaire
Note: Table showing the basic themes of the questionnaire and the existing published scales used for measurement of each of the attributes from which the questionnaire was developed.
The sections A-B of the questionnaire addressed time on task, study strategy, goal orientation and task preparedness. These were complemented with questions exploring students’ approach to learning in sections C-D (Pintrich, 2004). Personality traits and themes appraising the proven predictors such as conscientiousness were deduced from the Conscientiousness Quotient Inventory (CQI) (Brazdău & Mihai, 2011). In Section F, the questionnaire addressed the postgraduates’ reflection on how they handled the situation with ‘work-study’ and ‘work-life’ balance, through subsections on procrastination, handling distractions and rejuvenation (taking time off). Metacognition and self-efficacy were appraised in sections E & G with questions adopted from metacognitive awareness inventory (MAI) and self-efficacy scale (SES) (Coutinho & Neuman, 2008; Schraw & Dennison, 1994). These included questions on the residents’ own regulations of their learning such as choice of study resources, environment, effective study group dynamics, self-rated confidence, preparedness and understanding of impact of high stakes of the examination. The questionnaire was constructed with subsections that had reliability value of more than 0.7 in prediction of academic performance.
D. Purposive Sampling: Focus Group Discussions
The focus group discussions were conducted with semi-structured interview guides that were designed from the pre-examination questionnaire results. The questions were designed to be ‘open-ended’ and to understand ‘exam preparedness’. The interviewing faculty were carefully chosen to be neither the exam-trainers nor the exam-assessors, to minimise ‘observer biases’ and to remove confounding from ‘power’ relationships. The focus group structure included the investigator as the primary interviewer, while the information and discussions were captured through field notes by an assistant present inside the room. Audio or video recording were not permitted by the IRB for this study. To understand the perspectives of ‘failing’ and ‘what it takes to bounce back and succeed’, the ‘non-acers’ focus group was designed. These included students who had the experience of failing in previous examinations and have now succeeded in the present effort.
E. Analysis
For the questionnaire data, descriptive statistics were computed with SPSS 20 (IBM, Armont, NY, USA). The data analyses were carried out in three stages. First, the pre-exam questionnaire data of the passers were compared with the questionnaire data from the failed candidates to obtain any common patterns or contrasts. Unpaired t tests were performed to obtain the statistical significance of the questionnaire data comparing the two groups. Owing to limited size of the sample (n<60), no formal logistic regression could be performed.
Next, the focus group reflections of the candidates were compared between the sub-group of passers into ‘acers’ and ‘non-acers’. Thematic analysis was performed with initial codes applied during preliminary analysis and further confirmed as themes that consistently emerged in the subsequent focus group discussions.
In the final stage, the focus group discussion data were compared with pre-exam questionnaire attributes of the candidates for understanding the predictors of exam success and to strengthen the construct of ‘exam preparedness’.
F. Ethics
National University of Singapore institutional review board approved of the study (IRB:13-276) and focus group discussions were permitted only with candidates who passed the exams. The study was voluntary, and participants were empowered to opt out at any phase of the study.
III. RESULTS
Forty-two candidates appeared for the primary anaesthesia examinations. Of the 42 primary anaesthesia examination candidates, 30 (n=30) gave consent for the study and filled the pre-examination questionnaire (70% response rate). The overall pass rate was 42.9% (18 out of 42 who appeared for the examinations). 18 out of the 30 candidates who filled the questionnaire passed the exam. One candidate who had appeared for two concurrent primary exams (United Kingdom & Singapore) was excluded from the analyses as she might have received additional exam support. Hence, total number of study participants who passed the examination were 17, of which, 12 had passed the exam in first attempt (acers) and five had succeeded after previous attempts (non-acers). Of those who passed the exam, eight students participated in focus group discussions in two groups (acers and non-acers) of four each. The pass and fail groups were compared based on the various themes of the questionnaire such as study strategy, study time, goal orientation, self-regulation, metacognition and conscientiousness (Table 2).
|
Attributes |
Feature assessed |
Passers Subgroups |
Passers (17/29) %(n) |
Failed (12/29) %(n) |
|
|
Acers % (n=12) |
Non-Acers % (n=5) |
||||
|
Study Time |
Average weekday study time <2 hours / day |
25(3) |
20(1) |
23.5(4) |
83.3(10) |
|
Average weekend study time >6 hours in total |
75(9) |
80(4) |
76.5(13) |
33.3(4) |
|
|
Study strategy |
Timetable-based pattern of study |
41.7(5) |
60(3) |
47.1(8) |
16.7(2) |
|
Weekly Review of timetable |
50(6) |
60(3) |
52.9(9) |
33.3(4) |
|
|
Revisions for exam >= 2 times |
66.7(8) |
80(4) |
70.6(12) |
41.7(5) |
|
|
Goal Orientation |
Mock SAQ exam set rehearsals (Atleast once) |
91.7(11) |
80(4) |
88.2(15) |
50(6) |
|
Self-regulation |
Insufficient material covered <50 % only |
9.1(1) |
0* |
5.9(1) |
41.7(5) |
|
Conscientiousness |
Set Targets achieved <50 % only (procrastination) |
16.7(2) |
0* |
11.8(2) |
41.7(5) |
|
How prepared: feels <50% only |
33.3(4) |
20(1) |
29.4(5) |
41.7(5) |
|
|
Rejuvenate >= 2 times/ week |
33.3(4) |
60(3) |
41.2 (7) |
50(6) |
|
|
Self-efficacy |
> 50 % Confidence to face exams |
41.7(5) |
80(4)* |
52.9(9) |
41.7(5) |
|
Metacognition |
Study location: home |
33.3(4) |
80(4) |
47.1(8) |
75(9) |
|
Study with: solitude |
58.3(7) |
60(3) |
58.8 (10) |
83.3(10) |
|
|
Demographics |
Marital status: single |
83.3(10) |
20(1) |
64.7(11) |
66.7(8) |
|
Gender: Male |
33.3(4) |
60(3) |
41.2(7) |
50(6) |
|
Table 2. Subgroup comparison within passers and with failed candidates
Note: Table showing questionnaire data demonstrating differences between the two groups of passers and their comparison with the ‘failed group’ of candidates. Acers=first time passers; Non-acers=candidates who failed before but have succeeded in this attempt. The percentages are calculated in relation to the column header on top of respective rows. (* denotes statistical significance with p value<0.05)
A. Time on Task & Self-Regulation
The passers spent more weekend hours for study (average > 6 hours, 76.5% vs 33.3%) and far more of them planned their study using a timetable (47.1 % vs 16.7 %) (p value 0.036). Where they were timetable-based, passers reviewed their study plans weekly (52.9% vs 33.3%). Passers revised the study materials more often than those who failed (70.6% vs 41.7%). Passers perceived that they covered more study material sufficiently (5.9% lapses to cover in passers vs 41.7% in failure group, p value 0.05). The focus group discussions revealed that postgraduates who passed had higher self-regulation, covering larger volumes of sufficient material required. This was more prominent in the ‘non-acers’ who had failed before. The focus group discussions showed that the candidates rated the attribute of self-regulation as the most important quality to succeed in exams. The candidates felt that ‘diligently apportioning time, effort & resources, knowing to map what examiners want and selectively consolidating preparation’ (effort regulation), were predictive of exam success.
B. Self-Efficacy
Passers procrastinated less (perceived self-assessment of set targets achieved) with their study plans (11.8% vs 41.7%, p value 0.057). The focus group discussion showed that group study and external support through peers and seniors were vital in providing individualised attention & feedback to stay focused on track. They asserted that ‘being planful, persevering to achieve more than 50% schedule, pushing one another in striving to achieve that goal’ helped to pass.
C. Conscientiousness
The non-acers scored higher (p value<0.05) on conscientiousness (lesser procrastination) when compared to the failed candidates. Both groups took similar efforts to rejuvenate and recuperate, showing no difference (with p value >0.05), with no specific patterns in how postgraduates prepared for the high-stake assessments.
D. Additional Themes
Social factors like marital commitments (64.7% passers-single) and gender (41.2% passers-male vs 52.9% female) showed little difference (p value 0.335) in overall exam outcomes. Yet, subgroup analysis showed that among the passers, 83.3% of first-time passers were single and only 20% of those who were married passed in first attempt (Table 2). The study environment and study in solitude vs groups were comparable. On further elaboration in focus group discussion, the residents affirmed that not all the study-time with peers involved discussion, but the fact they all studied together helped them to ‘stick together and push each other to the very end’ (Table 3). The ‘non-acers’ study strategies were comparable to the ‘acers’ and they tend to study longer and plan their study ‘more timetable-based’ and reviewed it more often.
|
Themes |
Acers |
Non-Acers |
Common features |
|
The Primary Exam: general impressions |
Internalised factors: need deliberate effort, sacrifice, push on to end, set aside time, less social life |
Externalised issues: exam not structured, mark allocation not clear, no syllabus, no guidance, prep time not enough; requires senior guidance |
Work study balance difficult Primary exams a hindrance to progress in career |
|
Level of task difficulty |
Toughest of exams, difficult content to recall/ remember |
Need to know relevant knowledge (not a lot), Technique: structure/ how to answer is vital |
Task difficulty same throughout prep stages |
|
Difference from past success |
More deliberate effort; perseverance & discipline; not spoon fed like in UG |
More applied sciences content involved |
Work study balance needed |
|
Adaptations when facing exams |
Not to chance a failure; adapting study style to exams; perseverance |
Failure is a possibility; lots of practice; stay back post call to study; Technique: direct answers, open ended, forth coming answers |
Group study: push each other, enjoy same things, reinforces prep External / senior help: personalised attention, helps focus and formulate |
|
What went well as planned? |
Being in groups; Study material completion |
Exam goal-oriented selective study; more viva practice |
Study plan: timetable based; efficient completion; cover 50-75% plan; not giving up |
|
Perceived reasons for failure |
Not being ready in many ways |
Bad luck; unsupportive hostile examiners |
Gross lack of knowledge |
|
What to improve if rewind to 6 months before exam? |
Unpreparedness is an issue to avoid; minimise luck factor; get resources that answers / on syllabus on what examiners want |
Do past year questions to know the areas of focus; study leave at least two weeks |
Start earlier; push timetable better; syllabus-oriented prep; learn examiner mapping & prepare / practice so |
|
Exam preparedness: predictable qualities |
Knows weak & strong spots; knows a bare min of everything; consolidates prep to what examiners want |
Not fumble under pressure |
Know well what examiners want; smartly choosing enough material; technique/ way to answer exam question |
|
Breezing through exams: qualities |
Being in tune with recent exam patterns; not giving up |
Strong memory in foundational sciences- chemistry physics; enough material not lots of it |
Structured diligent exam-oriented prep Flexibly tied in plans Expressive in viva Delivers the wanted |
|
Advice for future candidates |
Minimise luck factor Stick to study plan Handling burn outs to avoid study plan disruptions |
Having good social exam taking attributes Small textbooks are useful more resources |
Not to shy away from shame of mock viva. Know examiner needs. Know syllabus well & Plan the study and technique |
Table 3: Focus group discussions summary
The main themes emerging from the two focus groups are summarised in Table 3. All focus group discussion candidates agreed that failure was chiefly a result of ‘gross lack in knowledge’ and ‘un-preparedness in many ways’. The focus group discussions concluded with the passers’ advice for success of future candidates and stated that:
“adhering to syllabus & plan of study, technique suited to examiner needs and not shying away from shame of mock exams, minimizing luck factor, possessing good social attributes (viva skills), persevering with study plans and timing of rejuvenation was the key to success”.
The focus group discussions supported this concept that ‘the best way of passing the exam was to dare the shame of practice viva’ and not to shun away from faculty feedback on performance in mock exams. The ‘passers’ had spent twice the time and effort in practice exams and revisions when compared to the ‘fail’ group (self-regulation).
IV. DISCUSSION
Our study showed that the candidates who passed, monitored their learning well by choosing to stay in groups and ‘stuck together’ by helping one another. The focus group discussions showed that they opted to adopt this mode of studying because the task was difficult and required constant motivation and peer support. This is in accordance with literature that claims the usefulness of peer support and feedback (de la Cruz et al., 2015; Dochy et al., 1999; Lerchenfeldt et al., 2019). What is vital was the ability of the candidates to assess what components of the exam content requires concentrated self-learning, like memorization, and differentiate it from study materials that require learning in groups and further elaboration.
Our study showed that the ‘passers’ were mindful of how they took time off to study or rejuvenate. The ‘passers’ tend to procrastinate three times lesser than the ones who failed. More so, a subgroup analysis showed that the ‘non-acers’ or the previous failed candidates never put away their schedules and stayed pursuing a timetable-based study (0% procrastination). The focus group discussions reinforced the fact that the ‘passers’ felt that there were loads of enormously difficult basic science content to be covered, such as applied physics and pharmacology, and time was limited, requiring further organisation and seamless execution of the study plan.
Self-efficacy evaluations showed no clear difference when comparing the groups of ‘passers’ and ‘failed’ candidates. However, the subgroups analysis showed that the ‘non-acers’ were twice as confident as the rest. The focus group discussions confirmed that the non-acers, having had the experience of failing before, ‘had a clear understanding of the difficulty of task and had commenced their study early in a programmed timetable-based manner with specific feedback and personalised attention from faculty supporting them’.
Cilliers et al., (2012) modelled the pre-assessment learning effects of high-stakes assessments and postulated ‘efficacy’ as an adaptation in the learner in anticipation of the task. Our ‘non-acers’ had been through the actual task difficulty, having failed earlier, had higher self-efficacy and now programmed their study well, expending more time on task. The lower self-efficacy might mean that this is an important lead for the faculty, in how they counselled and supported future candidates that are to be trained for high-stakes examinations (Lucieer et al., 2016).
A. ‘The Exam Ready Candidate’
Our study showed that passers had higher degree of self-regulation, conscientiousness, and metacognition. The focus group discussions further affirmed the information about the relationship between the various attributes and the students’ perceptions of ‘exam preparedness’. They felt that the candidates who ‘breeze through exams’, in other words, the exam ready, ‘possessed exam oriented (goal oriented) flexibly tied into study plans (metacognition), were expressive in viva (self-efficacy), delivered the necessary content well (conscientiousness)’ in addition to ‘diligently apportioning time, effort & resources (effort regulation), knowing to map what examiners want & selectively consolidating preparations (study strategy)’.
B. Understanding the High Failure Rates
The anaesthesia postgraduate primary examinations had a dismal 42.9% pass rate while undergraduate examinations had more than 90% pass rates. This is intriguing and highlights the complex relationships between the poor predictability of undergraduate academic scores and the influences of other paradigms in postgraduate exam performances (Division of Graduate Medical Studies [DGMS], 2013). The focus group discussions helped us understand this phenomenon better. The residents felt that ‘unlike undergraduate exams, the postgraduate examinations required lot more application of work-study balance and work-life balance’. During the undergraduate years, the students felt that the sole focus was to learn and perform in examinations, with lot more protected time during the day and all the weekends were dedicated to study. Although they require a particular level of academic competence to become a postgraduate, there is more to explore when it comes to exam success such as ‘work-life’ and ‘work-study’ balance (Klomegah & Yao, 2007; Rau & Durand, 2000).
C. Practical Implications
Through this study, we identify the presence of attributes such as metacognitive self-regulation, conscientiousness, and self-efficacy. We now know that candidates who score well in these component-attributes tend to pass the examinations. We propose that achieving an element of predictability will be a good lead for:
1. The educators to identify the ‘candidates with difficulty’ and delegate special care and personalised attention to them, while it is feasible and not too late.
2. The exam candidates themselves to have a ‘reality check’ on where they stand and what would be the best way ahead: peer learning, consolidated study, goal orientation etc.
D. Scoring Exam Preparedness and Planning Scaffolding
Candidates with ‘poor conscientiousness score’ could be scheduled to ‘receive more structured assistance through study groups, frequent deadlines, shorter assignments, group assignments and clearly defined learning goals’ (Kappe & Van Der Flier, 2012). This was put to light in our focus group discussions when one of the candidates who was unsuccessful earlier, but passed this time (non-acer) stated that:
“what made all the difference in this exam was that faculty and peers sat next to me in a quiet room, gave me a short study topic, made me do a SAQ, then a short viva on it, then gave me a critical feedback on how to improve. This was very encouraging, and I felt the intention of the faculty and peers were to help me and not to embarrass me on how unprepared I was. This inspired me to pass this ordeal this time…”
Implementing a composite tool to assess ‘exam preparedness’, we propose, would help the learners and teachers to skim for predictable factors that influence the chances of success. Incorporating a system of ‘scaffolding’ would help in early guided learning towards exam success. This, we feel, is particularly imperative when educational programs deploy high-stakes single summative exams. Self-efficacy Survey (SES) was described as a measure for identifying disability in adaptive attitudes and disfunctionality (Panc et al., 2012). Using such a measure could identify ‘trainees with difficulty’ and guide us to channelise our efforts and resources for those who need it the most. Kandaswamy and Anbarasi (2014) suggested early identification of ‘gifted under achievers’ and successfully devised a structured program for psychological support, demonstrating a reduction of dropouts for dental undergraduates.
E. Limitations & Reflections
The chief limitation our study was the aspect that attributes like metacognitive self-regulation, conscientiousness and self-efficacy have considerable overlapping concepts and it was difficult to compartmentalise these themes when interpreting the qualities of a learner. Our study population was limited to anaesthesia postgraduates’ primary examination results from one country. A fair comparison of other specialty postgraduate examinations could not be accomplished in our context owing to variation in exam task difficulty, timings, and patterns of assessments.
Of the 42 who appeared for exams only 30 consented to fill the questionnaire. Only one among the 12 students who chose not to fill the questionnaire passed the exam. This could have been another area of rich information. Did the learners know that they were not prepared at all or was the title labelling students “exam smart” made them to excuse themselves off the study? It is possible that respondents gave ‘socially acceptable answers’ when the questionnaire was given, especially so when our study is titled to explore how ‘prepared/ ready’ they were or predicting their chance to pass.
There are possibilities that testwiseness could have contributed to exam success and were not explored in the focus group discussions (Millman et al., 1965; Sarnacki, 1981; Wahlstrom & Boersma, 1968; Watling & Ginsburg, 2019). Though the present study involved short answer questions and viva-based examinations that tend to report less of testwiseness, as compared to multiple choice questions, future research could appraise this concept and consider ways to address that in the methodology.
1) Validating a questionnaire for ‘exam preparedness’- A lead for the future: Our model of ‘exam preparedness’ was proposed to address the complex learning and myriad of factors that impact postgraduate academic performance (Appendix 1). A well validated composite score or scale on ‘exam preparedness’ can be a yardstick for ‘assessment for exam-readiness’, thereby planning the allocation of resources and faculty time and effort. Future studies could evaluate when it would be an appropriate time for evaluating the score (1 or 3 or 6 months before exams). It should not be too near to the examinations, lest it could be too late for any usefulness of its predictability.
V. CONCLUSION
There were similarities in attributes that characterise passing such as time scheduling, plan of study, group and peer support, goal oriented selective mastery learning and effort regulation to task difficulty. The two groups of passers also identified that the chief cause of failure to be ‘gross lack of knowledge’ and ‘unpreparedness’. Implementing a composite tool to assess ‘exam preparedness’ we propose, would help the learners and teachers to skim for predictable factors (metacognitive self-regulation, self-efficacy, conscientiousness) that influence the chances of success.
As teachers, we would agree that the students who are relatively more prepared, tend to seek and receive more faculty support, while those who are trailing, continue to distance themselves with the divide getting more distinct nearer to the examinations. Identifying this discrepancy early, while predicting and preventing failure in high-stakes examinations, we propose, needs in-depth understanding of ‘exam preparedness’. Using the ‘exam preparedness’ scale might help to identify the postgraduates with academic difficulty, thereby offering a support system, wherein we don’t lose some ‘Good Samaritans’ who are just not ‘exam ready’.
Notes on Contributors
Dr Balakrishnan Ashokka is an Anaesthesiologist & Educationalist with special interest in Simulation-based postgraduate education at National University Health System, Singapore. He conceived the idea of the study, performed literature search, conducted the study, and drafted the manuscript of the study. He agrees fully to the final version of manuscript.
Prof Lee Tat Leang has been involved in Undergraduate and Postgraduate teaching and examination processes over 30 years at the National University of Singapore. He provided support during conceptualisation, discussion of results and creation of the manuscript. He fully agrees to the final version of the manuscript.
Dr Daniëlle M.L. Verstegen has a background in Cognitive Science and Instructional Science. She currently leads an e-learning group in the Department of Educational Development and Research, FHML, Maastricht University. She supervised the conduct of the entire study, qualitative analysis and agrees fully to the final version of the manuscript.
Ethical Approval
The National University of Singapore, Institute Review Board (NUS-IRB) provided the ethics committee approval for the conduct of study on passers of the examination (NUS-IRB approval number NUS 1946, reference code 13-276). No audio or video recording or discussions with failed students was permitted as per the directorate’s policy of research on exam candidates.
Data Availability
The study data with summarised, deidentified data synthesis is provided in tables 1-3 in this manuscript. The NUS-IRB and DGMS had provided approval for the study with a clause for private storage of study data with authors’ password-protected workstation. No permission was granted for open access platforms, as the data contained sensitive information about failed candidates.
Acknowledgement
The authors acknowledge the anaesthesia postgraduates who participated in this study, offering their valuable time and effort.
Funding
No funding was received for the conduct of the study.
Declaration of Interest
The authors declare that there are no financial or non- financial competing conflicts of interests.
References
Brazdău, O., & Mihai, C. (2011). The consciousness quotient: A new predictor of the students’ academic performance. Procedia-Social and Behavioral Sciences, 11, 245-250. https://doi.org/10.1016/j.sbspro.2011.01.070
Cilliers, F. J., Schuwirth, L. W., & Van der Vleuten, C. P. (2012). Modelling the pre‐assessment learning effects of assessment: Evidence in the validity chain. Medical Education, 46(11), 1087-1098. https://doi.org/10.1111/j.1365-2923.2012.04334.x
Colthart, I., Bagnall, G., Evans, A., Allbutt, H., Haig, A., Illing, J., & McKinstry, B. (2008). The effectiveness of self-assessment on the identification of learner needs, learner activity, and impact on clinical practice: BEME Guide no. 10. Medical Teacher, 30(2), 124-145. https://doi.org/10.1080/01421590701881699
Conard, M. A. (2006). Aptitude is not enough: How personality and behavior predict academic performance. Journal of Research in Personality, 40(3), 339-346. https://doi.org/10.1016/j.jrp.2004.10.003
Cook, D. A., Thompson, W. G., & Thomas, K. G. (2011). The motivated strategies for learning questionnaire: Score validity among medicine residents. Medical Education, 45(12), 1230-1240.
Coutinho, S. A., & Neuman, G. (2008). A model of metacognition, achievement goal orientation, learning style and self-efficacy. Learning Environments Research, 11(2), 131-151.
Credé, M., & Phillips, L. A. (2011). A meta-analytic review of the motivated strategies for learning questionnaire. Learning and Individual Differences, 21(4), 337-346. https://doi.org/10.1016/j.lindif.2011.03.002
de la Cruz, M. S. D., Kopec, M. T., & Wimsatt, L. A. (2015). Resident perceptions of giving and receiving peer-to-peer feedback. Journal of Graduate Medical Education, 7(2), 208.
Dunlosky, J., & Lipko, A. R. (2007). Metacomprehension: A brief history and how to improve its accuracy. Current Directions in Psychological Science, 16(4), 228-232. https://doi.org/10.1111/j.1467-8721.2007.00509.x
Division of Graduate Medical Studies. (2013). The primary anaesthesia MMed examinations. https://medicine.nus.edu.sg/dgms/anaesthesiology.htm
Dochy, F. J. R. C., Segers, M., & Sluijsmans, D. (1999). The use of self-, peer and co-assessment in higher education: A review. Studies in Higher education, 24(3), 331-350.
Hamilton, L., & Brown, J. (2005). ‘Judgement day is coming!’: young people and the examination process in Scotland. Improving Schools, 8(1), 47-57. https://doi.org/10.1177/1365480205049339
Hennink, M. M. (2013). Focus group discussions. Oxford University Press.
Isaacson, R., & Fujita, F. (2006). Metacognitive knowledge monitoring and self-regulated learning. Journal of the Scholarship of Teaching and Learning, 6(1), 39-55.
Kandaswamy, D., & Anbarasi, K. (2014). Gifted underachievers in dental education- An action research report. Medical Education, 48(s2), 1-19. Abstract number 49. https://doi.org/10.1111/medu.12579
Kappe, R., & Van Der Flier, H. (2012). Predicting academic success in higher education: What’s more important than being smart?. European Journal of Psychology of Education, 27(4), 605-619. https://doi.org/10.1007/s10212-011-0099-9
Klomegah, R. Y. (2007). Predictors of academic performance of university students: An application of the goal efficacy model. College Student Journal, 41(2), 407-415.
Lerchenfeldt, S., Mi, M., & Eng, M. (2019). The utilization of peer feedback during collaborative learning in undergraduate medical education: A systematic review. BMC Medical Education, 19(1), 1-10.
Lucieer, S. M., Jonker, L., Visscher, C., Rikers, R. M. J. P., & Themmen, A. P. N. (2016). Self-regulated learning and academic performance in medical education. Medical Teacher, 36(6), 585-593. https://doi.org/10.3109/0142159X.2015.1073240
McKim, C. A. (2017). The value of mixed methods research: A mixed methods study. Journal of Mixed Methods Research, 11(2), 202-222.
Millman, J., Bishop, C. H., & Ebel, R. (1965). An analysis of test-wiseness. Educational and Psychological Measurement, 25(3), 707-726.
O’Connor, M. C., & Paunonen, S. V. (2007). Big Five personality predictors of post-secondary academic performance. Personality and Individual Differences, 43(5), 971-990. https://doi.org/10.1016/j.paid.2007.03.017
Ormrod, J. E. (2009). Human Learning. (5th ed) Chapter 12. Upper Saddle River, NJ: Pearson Education.
Panc, T., Mihalcea, A., & Panc, I. (2012). Self-efficacy survey: A new assessment tool. Procedia-Social and Behavioral Sciences, 33, 880-884. https://doi.org/10.1016/j.sbspro.2012.01.248
Pintrich, P. R. (2000). Multiple goals, multiple pathways: The role of goal orientation in learning and achievement. Journal of Educational Psychology, 92(3), 544.
Pintrich, P R. (2004). A Conceptual Framework for Assessing Motivation and Self-Regulated Learning in College Students. Educational Psychology Review, 16(4), 385-407. http://hdl.handle.net/2027.42/44454
Pintrich, P. R., & De Groot, E. V. (1990). Motivational and self-regulated learning components of classroom academic performance. Journal of Educational Psychology, 82(1), 33.
Rau, W., & Durand, A. (2000). The academic ethic and college grades: Does hard work help students to “make the grade”? Sociology of Education, 73(1) 19-38. https://doi.org/10.2307/2673197
Ray, R., & Brown, J. (2015). Reassessing student potential for medical school success: Distance travelled, grit, and hardiness. Military Medicine, 180(4, Suppl), 138-141.
Roberts, B. W., Jackson, J. J., Fayard, J. V., Edmonds, G., & Meints, J. (2009). Conscientiousness. In M. R. Leary & R. H. Hoyle (Eds.), Handbook of individual differences in social behavior (p. 369–381). The Guilford Press.
Sarnacki, R. E. (1981). The effects of test-wiseness in medical education. Evaluation & the Health Professions, 4(2), 207-221.
Schraw, G., & Dennison, R. S. (1994). Assessing metacognitive awareness. Contemporary Educational Psychology, 19(4), 460-475.
Soh, J. Y. (2019). The ownership cycle and self-regulated learning. The Asia Pacific Scholar, 4(1), 65-68. https://doi.org/10.29060/TAPS.2019-4-1/CS2047
Sladek, R. M., Bond, M. J., Frost, L. K., & Prior, K. N. (2016). Predicting success in medical school: A longitudinal study of common Australian student selection tools. BMC Medical Education, 16(1), 1-7.
Slavin, S. J., Schindler, D. L., & Chibnall, J. T. (2014). Medical student mental health 3.0: Improving student wellness through curricular changes. Academic Medicine, 89(4), 573.
Vermunt, J. D. (1996). Metacognitive, cognitive and affective aspects of learning styles and strategies: A phenomenographic analysis. Higher Education, 31(1), 25-50.
Wahlstrom, M., & Boersma, F. J. (1968). The influence of test-wiseness upon achievement. Educational and Psychological Measurement, 28(2), 413-420.
Watling, C. J., & Ginsburg, S. (2019). Assessment, feedback and the alchemy of learning. Medical Education, 53(1), 76-85.
Zhou, Y. X., Zhao, Z. T., Li, L., Wan, C. S., Peng, C. H., Yang, J., & Ou, C. Q. (2014). Predictors of first-year GPA of medical students: A longitudinal study of 1285 matriculates in China. BMC Medical Education, 14(1), 1-9.
Zimmerman, B. J. (2000). Self-efficacy: An essential motive to learn. Contemporary Educational Psychology, 25(1), 82-91.
Zimmerman, B. J. (2008). Investigating self-regulation and motivation: Historical background, methodological developments, and future prospects. American Educational Research Journal, 45(1), 166-183. https://doi.org/10.3102/0002831207312909
*Dr Balakrishnan Ashokka
Department of Anaesthesia,
National University Hospital,
5 Lower Kent Ridge Road
Singapore 119074.
Tel: +6597118855
Fax: +6567775702
Email: ashokkab@gmail.com
Submitted: 16 January 2021
Accepted: 17 May 2021
Published online: 5 October, TAPS 2021, 6(4), 65-79
https://doi.org/10.29060/TAPS.2021-6-4/OA2447
Yee Cheun Chan1, Chi Hsien Tan1 & Jeroen Donkers2
1Department of Medicine, National University Health System, Singapore; 2Department of Educational Development and Research, Faculty of Health, Medicine and Life Sciences, Maastricht University, Netherlands
Abstract
Introduction: Reflection is a critical component of learning and improvement. It remains unclear as to how it can be effectively developed. We studied the impact of reflective writing in promoting deep reflection in the context of learning Accreditation Council for Graduate Medical Education (ACGME) competencies among residents in an Internal Medicine Residency programme.
Methods: We used a convergent parallel mixed-methods design for this study in 2018. We analysed reflective writings for categories and frequencies of ACGME competencies covered and graded them for levels of reflection. We collected recently graduated residents’ perceptions of the value of reflective writings via individual semi-structured interviews.
Results: We interviewed nine (out of 27) (33%) participants and analysed 35 reflective writings. 30 (86%) of the writings showed a deep level (grade A or B) of reflection. Participants reflected on all six ACGME competencies, especially ‘patient care’. Participants were reluctant to write but found benefits of increased understanding, self-awareness and ability to deal with similar future situations, facilitation of self-evaluation and emotional regulation. Supervisors’ guidance and feedback were lacking.
Conclusion: We found that a reflective writing programme within an Internal Medicine Residency programme promoted deep reflection. Participants especially used self-reflection to enhance their skills in patient care. We recognised the important role of mentor guidance and feedback in enhancing reflective learning.
Keywords: Reflective Writing, ACGME Competencies, Internal Medicine, Residency
Practice Highlights
- Reflection is a critical component of learning and improvement.
- Written reflections offer theoretical advantages over other forms of reflections in requiring more commitment and ownership of experience, promoting critical thinking and offering more opportunities for feedback.
- Written reflections can be a record for mentored reflection, included in a portfolio, used in ongoing self-assessment and longitudinal integration of learning.
- Practitioners reported benefits of increased understanding, self-awareness and ability to deal with similar future situations, facilitation of self-evaluation and emotional regulation.
- Supervisors’ guidance and feedback are important for enhancing reflective learning.
I. INTRODUCTION
Medical competencies are developed through experience and application, not just knowledge acquisition (Frank et al., 2010). Kolb (1984) conceptualises experiential learning in a four-stage cyclical process. An experience triggers a reflection on that experience that leads to the formation of abstract concepts and generalisations. These are then tested in future situations, resulting in new experiences. Reflection is an essential aspect of the learning experience. It remains unclear how it can be developed most effectively.
Reflection is a complex concept that has been defined in several ways. One definition describes it as the process of engaging self in attentive, critical, exploratory, and iterative interactions with one’s thoughts and actions, and their underlying conceptual frame, with a view on the change itself (Nguyen et al., 2014). Thus, reflection has an iterative dimension which describes a cyclic process with phases triggered by experience, which produces new understanding, and then an intention to act differently in future encounters of similar experience (Mann et al., 2009). There is also a vertical dimension correlating to the depth of reflection. The surface levels are more descriptive and less analytical than the deeper levels. For example, Boud et al. (1985) described iterative phases of returning to experience, attending to feelings, re-evaluation of experience and outcome/resolution. Mezirow (1991) described increasing depth of reflection as habitual action, thoughtful action/understanding, reflection, critical reflection. Evidence suggests that deeper levels of reflections are associated with deep approaches to learning (Leung & Kember, 2003).
Reflective writing is a commonly utilised method in developing reflective learning but evidence for its value remains limited. Theoretically, written reflections offer advantages over other types of reflections e.g. verbal discussions. Creating an artefact by writing involves a commitment to learning, ownership of experience, promotes critical thinking and offers more opportunities for feedback (Aronson, 2011). The writings can be a record for mentored reflection, included in a portfolio, used in ongoing self-assessment and longitudinal integration of learning. A systematic review (Winkel et al., 2017) looking at the impact of reflection in graduate medical education found only three studies (Epner & Baile, 2014; Levine et al., 2008; Winkel et al., 2010) that involved reflective writings. Levine et al. (2008) found that the process of narrative writings encouraged deepening of reflection leading to reconsideration of core values and priorities, improved self-awareness, provided an emotional outlet and motivation to improve. However, the study did not formally gauge the depth of reflections in the writings.
We aimed to further study the impact of reflective writing in promoting reflection and the learning of medical competencies. Better understanding this will guide the development of reflective learning skills in training programmes for medical trainees.
A. Research Question
Does reflective writing promote deep reflection in the context of learning core competencies defined by the Accreditation Council for Graduate Medical Education (ACGME) (Accreditation Council for Graduate Medical Education, 2013)?
II. METHODS
A. Research Paradigm and Design
Our study adopted a phenomenological approach. We used a convergent parallel mixed-methods design (Figure 1). Quantitative data included the tabulation of the categories of ACGME competencies and the frequency they were covered in the reflective writings. Quantitative scoring of levels of reflections in the reflective writings was done using two grading scales. Qualitative data included graduates’ perceptions of the value and effects of reflective writings on learning ACGME competencies. The quantitative and qualitative data were analysed, compared and related together to answer the research question.
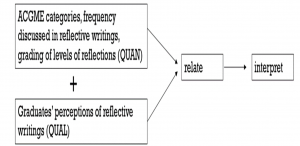
Figure 1. Convergent parallel mixed-methods design to study the role of reflective writing in promoting reflective learning of ACGME competencies
B. Study Setting and Subjects
The study setting was the Internal Medicine Residency of a single tertiary university hospital in 2018. We have used reflective writing as a tool for developing reflective learning and practice in our Internal Medicine Residency. Our programme has a competency-based curriculum using the ACGME framework. Residents are encouraged to write their reflections on how an encounter or situation helped them develop one or more of the competencies. They are required to include at least two such reflective writings in their portfolio each year. The reflective writings are not graded but are read by the residents’ supervisors as part of their portfolio’s content during regular reviews and by the competency review committee during 6-monthly meetings. They provide insight into the residents’ competencies development.
We invited all past residents (27) who graduated from the programme one year earlier to participate. We used a convenience sampling method. We determined the final number of participants after data saturation was reached in the analysis of the collected qualitative data.
The study was approved by the National Healthcare Group Domain Specific Review Board (NHG DSRB) (Reference number: 2017/01219). We obtained informed consent from each participant.
C. Data Collection
We collected and analysed reflective writings from the participants’ three years of residency. We used individual semi-structured interviews to gather participants’ perceptions to avoid bias from others’ opinions. One researcher (YCC) conducted, recorded and transcribed the interviews. Box 1 shows the main questions that were asked. An interactive approach was used, and interviews conducted till thematic saturation was reached.

Box 1. Main questions asked during interviews
D. Data Analysis
Reflective writings from participants were analysed for the categories as well as frequencies of ACGME competencies covered. They were graded for levels of reflection using grading rubrics. To reduce possible interpretation bias or conflicts related to confidentiality and power relationships, grading was done by an ‘external’ co-researcher (CHT) who was a faculty member of the Neurology residency programme. Two grading scales were used. The first (Box 2) had a simple grading scale from A to F (Moon, 2004). The other grading rubric provided more categorical details and was based on that used by Tsingos et al. (2015) (Supplementary Table 1). The rubric graded the reflective writings on seven stages of reflection based on the model by Boud et al. (1985) and categories of non-reflector, reflector or critical reflector according to Mezirow’s model (Mezirow, 1991). The co-researcher read through each reflective writing and first determined if stages of ‘returning to experience’, ‘attending to feelings’, ‘association’, ‘integration’, ‘validation’, ‘appropriation’ and ‘outcomes of reflection’ were present. He then assessed if the written content related to these stages fit the descriptors for non-reflector, reflector or critical reflector as given in the rubric. Finally, he graded the reflective writing on the simple grading scale of A to F according to the descriptors given (Box 2).
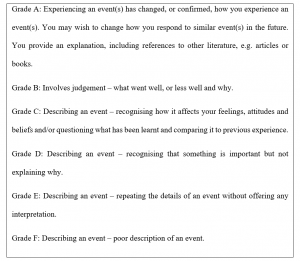
Qualitative data from interviews were transcribed in full, coded and thematically analysed (Braun & Clarke, 2006). Coding and analysis were independently done by two researchers (YCC, CHT) before discussions to reach consensus. Each interview was analysed after its completion and before subsequent interviews. Thematic saturation was determined by the absence of any new themes emerging from the analysis of the previous three interviews. This was reached after six interviews. Three further interviews were conducted after that. The participants were asked if the results of the thematic analysis were a fair interpretation of the discussions. Peer debriefing processes were employed to enhance the validity of the study. Validity was enhanced by triangulation of quantitative and qualitative data.
III. RESULTS
A. Demographic Data
There were nine participants in the study. This represented 33% of the study population (27). There were five males and four females. Five were Singaporean. The other four were from Sri Lanka, Malaysia, Hong Kong in China and Myanmar. Five attended undergraduate medical school in Singapore, two in Australia, one in the United Kingdom and one in Myanmar. One participant, age 45, was more than ten years older than the others. The mean age of the other eight participants was 29.4 years, with ages ranging from 27 to 32. Apart from the oldest participant, the others were between four to seven years post medical school graduation. The gender ratio of the participants is similar to that of the study population while the proportion of international graduates among the participants was higher (44% vs 30%).
B. Grading of the Reflective Writings
35 reflective writings were reviewed, with a range of 2 to 8 writings from each participant. The number of writings was less than the expected minimum number of 6 for some participants because of ‘exemptions’ made for various reasons at certain points in the course of the 3 years of residency. These included periods away on electives or ‘substitution’ with audits, quality improvement projects etc.
On the grading scale of A to F (Box 2), 30 (86%) of the writings were graded A or B. 4 (11%) were graded C while 1 (3%) was graded D. 13 (81%) of writings done in the first year of residency were graded A or B. For those written in the second and third year of residency, the corresponding numbers were 7 (88%) and 10 (91%) respectively. With only one exception, all writings involved all seven phases of reflection based on the model by Boud et al. (1985). The exceptional piece did not include the phase of ‘association’. The results are described in Table 1.


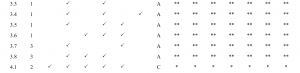

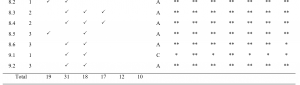
![]()
Table 1. Tabulation of competencies covered and grading of reflection level in writings
The writings covered all six ACGME competencies. Patient care was discussed in 31 (89%) of the writings. Medical knowledge, professionalism and communications were discussed in 19 (54%), 18 (51%) and 17 (49%) of the writings respectively while system-based practice and problem-based learning and improvement were discussed in 12 (34%) and 10 (29%) of the writings respectively.
C. Thematic Analysis of Interviews
Thematic analysis of the interviews revealed five themes relevant to the research question: (1) effect of the writings in motivating reflections on practice, (2) did the writings facilitate feedback or other learning activities, (3) perceived value of the writings, (4) limitations of the writing programme and (5) possible improvements or alternatives for the writing programme. These are discussed below. The anonymised interview transcripts are available on Figshare (Chan, 2021).
1) Effect of the writings in motivating reflections on practice: All residents conveyed that the main reason they did the writings was because it was a requirement that needed to be fulfilled (Supplementary table 2, A1). All, except one, did the writings just before the six-monthly deadlines (Supplementary Table 2, A2). The one exception usually wrote learning encounter diaries (LEDs) soon after significant events. Though reluctant, most residents were not resentful towards writing as it was deemed not difficult to do and they recognise, to varying extent, some value in doing it (Supplementary Table 2, A3).
Residents described having written on a wide variety of topics. These included reflections about patient care; diagnostic and management dilemmas, ethical issues, communication difficulties, professionalism, safety or inefficiencies in system practices and audit or quality improvement projects. All chose events or encounters that were atypical or non-routine. They used words like ‘special’, ‘interesting’, ‘stand out’, ‘struck my mind’, ‘memorable’, ‘stuck in my mind’ to describe such events or encounters (Supplementary Table 2, A4). Some of these events or encounters affected their emotions and were described as ‘emotionally-tied’, ‘traumatising’ or induced a sense of ‘helplessness’ (Supplementary Table 2, A5).
One was candid in expressing disinterest in the whole exercise (Supplementary Table 2, A6). A few residents felt that the writings involved only recollection of events (Supplementary Table 2, A7). However, most participants believed that the process of writing LEDs promoted additional reflections.
2) Did the writings facilitate feedback or other learning activities: The LEDs were part of the documents reviewed during formal 6-monthly progress review meetings between residents and supervisors. The amount of time spent discussing the contents of the LEDs, as well as residents’ value perception of such discussions varied. However, in general, they were considered of limited value, due to lack of time, supervisors’ disinterest, poor appreciation of or lack of connection with the events. Discussions at a proximate time to the event occurrence and feedback by peers or seniors involved in or familiar with the events or encounters were deemed more useful (Supplementary Table 2, B1).
Apart from reviewing the LEDs with supervisors, there was little that occurred after or as a result of the writings. One remembered that the writings triggered emotions. Another remembered an instance where he was prompted to research and learn more about the topic he wrote about after the writing. It was not common for residents to re-read the LEDs after writing them. In the few instances where this occurred, residents reported that there were some self-evaluation of change and progress in the time elapsed (Supplementary Table 2, B2).
3) Perceived value of the writings: Many residents said reflective writings helped increased self-awareness, recollection, reorganisation and consolidation of thoughts. The writings also served as records for facilitating self-evaluation and references for informing future actions (Supplementary Table 2, C1). A few also spoke about the writing being therapeutic, providing ‘emotional release’ and ‘closure’ to traumatising experiences (Supplementary Table 2, C2).
One resident offered that the LEDs provided him with a good means of communication with his supervisors. As he found it easier to write than to verbally describe, writing the LEDs helped him elicit feedback from his supervisor about the scenarios that he experienced (Supplementary Table 2, C3).
4) Limitations of the writing programme: Several residents pointed out limitations of the writing programme. There may be reluctance to share honestly in the writings for fear of embarrassment or creating a ‘bad impression’. A few felt that reflections can take place without the need for writing. Another opined that reflecting on unpleasant experiences may trigger unwanted emotions (Supplementary Table 2, D1).
5) Possible improvements or alternatives for the writing programme: Residents understood that potential benefits can only be fully realised if reflective writings become ‘routine process’, or ‘habit’ (Supplementary Table 2, E1). Residents also believed that discussions with and feedback from seniors enhance the value of self-reflection in reflective writing or may even replace the need for reflective writings. For such discussions to be useful, they need to occur soon after the events. Sufficient time, interest in participation and trust of confidentiality are also necessary (Supplementary Table 2, E2).
Instead of writing with pen and paper, reflections and discussions on digital platforms; blogging and group discussions online through a portal were suggested by some residents (Supplementary Table 2, E3).
IV. DISCUSSION
In our study, participants demonstrated deep levels of reflection in their writings, despite being reluctant with the task. They wrote on encounters they considered meaningful and covered all of the ACGME competencies. Evidence from the interviews suggested that the writings may not have taken place if they were not mandated. It was also likely that reflections on the topics written about would then not reach similar levels of depth. The percentage of writings with high grades (A and B) for the level of reflection was higher for writings done in year 3 than in year 1 (91% vs 81%) but the numbers were too small for any meaningful comparison to see if reflection depth improved in individuals over the years.
Given the freedom to choose what they write reflections on, our participants reflected most about patient care in their writings. System-based practice and problem-based learning and improvement were covered only in less than a third of the writings. This may reflect differential emphasis that the residents put on the different competencies. At the same time, there is evidence that diagnostic reasoning of complex and unusual cases can be improved by reflection (Mamede & Schmidt, 2017). Our residents may have intuitively recognised this and chose to reflect mainly on diagnostic and management dilemmas in patient care: ‘patients who are a little bit more special, either in terms of their presentations not being the most obvious, or patients who present with a diagnostic or management dilemma.’ (R1), ‘either difficult scenarios I’ve seen or interesting medical scenarios’ (R3). It is possible that our participants wrote less about system-based practice and problem-based learning and improvement because there were many alternative learning activities such as root-cause analysis discussions or participating in quality improvement projects.
The participants reported that the writings resulted in better understanding and increased ability to deal with similar encounters in the future. They also expressed other benefits such as increased self-awareness, facilitation of self-evaluation and having served as a method of coping with emotionally-charged encounters.
We had not provided specific training or detailed instructions on reflective writing for our residents. There was only general guidance that they should review prior experiences in order to learn from them. Nevertheless, our residents did not express difficulty in doing the reflective writings. There were a few possible reasons for this. Firstly, it was likely that the concept of reflective learning had been taught during undergraduate medical education. Secondly, the presence of the three sections with ‘prompt title/questions’: ‘scenario’, ‘what I have learnt from this’ and ‘what would I do differently in future’ provided some guidance. Thirdly, the residents were working in an environment where reflective learning and practice was part of daily practice and likely learned aspects of these in the process; they participated in root-cause analyses for incidents of medical error or adverse events and attended courses that teach clinical practice improvement methodology.
Reflective writing involves mainly self-reflection after an event. Learning is limited if the written self-reflection is not accompanied by discussion and feedback from peers or mentors (Sandars, 2009). Our study found that there was little guidance from supervisors on reflective techniques and limited feedback for the content of reflective writings. Several reasons emerged. Time was limited during scheduled supervisor-resident meetings and the reflective writings were only part of several documents reviewed by the supervisors. Supervisors were generally not involved in the events described and unfamiliar with the situational contexts. Residents’ interest in feedback on the events had also declined due to the lapse of time since the occurrences.
Literature shows that self-assessment is often inaccurate (Eva & Regehr, 2008). Feedback from others can provide multiple perspectives on experience, support integration of affective and cognitive experience and discourage uncritical acceptance of experience. Feedback from supervisors is not limited to the content of a reflection but should include the resident’s reflective skills as well. There had not been emphasis placed on teaching reflective techniques to residents. Supervisors can point out assumptions in the reflections, offer alternative interpretations and ask for clarifications of reasoning, omissions and conclusions. Faculty training for supervisors would be necessary to enable them to do these well.
Other limiting factors were discussed during the interviews. One participant expressed a reluctance to write honestly about incidents that showed one’s deficiencies for fear of giving a ‘bad impression’. This may reflect the resident’s goal orientation towards performance rather than mastery, the lack of a formative learning environment or inadequate trust towards a supervisor. Another participant pointed out the potential for reflection on events to trigger unwanted emotions. This highlighted the need for establishing in advance a plan for appropriate actions to ensure privacy and support for distressed residents.
A. Limitations of this Study
Our study described the outcomes from a programme of reflective writings in one institution. Differences in contextual factors may limit the transferability of our experience to settings elsewhere. Voluntary participation in this study may have resulted in a small, self-selected group of participants with strong opinions towards reflective writings. With graduates of the residency as participants, obtained opinions were based on memories that may have been altered by time and circumstances. Even though the writings were not included for any summative assessments, some participants may not have written accurate accounts of their thoughts and emotions due to concerns of creating a ‘bad impression’.
V. CONCLUSION
Our study found that a programme of reflective writings promoted deep reflection, with participants focusing especially on self-reflection to enhance their diagnostic and management skills in patient care. In general, the writings led to increased understanding, self-awareness and ability to deal with similar future situations. It also facilitated self-evaluation and emotional regulation. The important role of supervisor guidance and feedback in enhancing reflective learning was recognised. Providing this would require investment in faculty training, time resources and commitment of supervisors.
Notes on Contributors
YCC reviewed the literature, designed the study, conducted interviews, analysed interview transcripts and wrote the manuscript. CHT analysed and graded the reflective writings, analysed interview transcripts and developed the manuscript. JD advised on the design of the study and developed the manuscript. All the authors have read and approved the final manuscript.
Ethical Approval
The study was approved by the National Healthcare Group Domain Specific Review Board (NHG DSRB) (Reference number: 2017/01219).
Data Availability
The anonymised interview transcripts are available on Figshare (Chan, 2021). To protect the confidentiality of the participants, the reflective writings cannot be shared.
Acknowledgements
We thank Ms Jocelyn Chan and Ms Alicia Chan for their assistance in transcribing the interviews.
Funding
No funding was received for this research study.
Declaration of Interest
YCC is a core faculty member of the Internal Medicine Residency Programme. To reduce possible bias or conflicts related to confidentiality and power relationships, grading of reflective writings was done by CHT, who is not a faculty member of the programme. There are no other conflicts of interest.
References
Accreditation Council for Graduate Medical Education. (2013, April 24). Implementing milestones and clinical competency committees. Retrieved December 16, 2016, from http://www.acgme.org/acgmeweb/Portals/0/PDFs/ACGMEMilestones-CCC-AssesmentWebinar.pdf
Aronson, L. (2011). Twelve tips for teaching reflection at all levels of medical education. Medical Teacher, 33(3), 200-205. https://doi.org/10.3109/0142159X.2010.507714
Boud, D., Keogh, R., & Walker, D. (1985). Reflection: Turning experience into learning. Kogan Page.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
Chan, Y. C. (2021). Impact of Reflective Writings data [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14069369.v1
Epner, D. E., & Baile, W. F. (2014). Difficult conversations: Teaching medical oncology trainees communication skills one hour at a time. Academic Medicine, 89(4), 578-584. https://doi.org/10.1097/ACM.0000000000000177
Eva, K. W., & Regehr, G. (2008). “I’ll never play professional football” and other fallacies of self-assessment. Journal of Continuing Education in the Health Professions, 28(1), 14-19. https://doi.org/10.1002/chp.150
Frank, J. R., Snell, L. S., Cate, O. T., Holmboe, E. S., Carraccio, C., Swing, S. R., Harris, P., Glasgow, N. J., Campbell, C., Dath, D., Harden, R. M., Iobst, W., Long, D. M., Mungroo, R., Richardson, D. L., Sherbino, J., Silver, I., Taber, S., Talbot, M., & Harris, K. A. (2010). Competency-based medical education: Theory to practice. Medical Teacher, 32(8), 638–645. https://doi.org/10.3109/0142159X.2010.501190
Kolb, D. (1984). Experiential learning. Prentice-Hall.
Leung, D. Y. P., & Kember, D. (2003). The relationship between approaches to learning and reflection upon practice. Educational Psychology, 23(1), 61-71. https://doi.org/10.1080/01443410303221
Levine, R. B., Kern, D. E., & Wright, S. M. (2008). The impact of prompted narrative writing during internship on reflective practice: A qualitative study. Advanced Health Science Education Theory Practice, 13(5),723-733. https://doi.org/10.1007/s10459-007-9079-x
Mamede, S., & Schmidt, H. G. (2017). Reflection in Medical Diagnosis: A Literature Review. Health Professions Education, 3(1), 15-25. https://doi.org/10.1016/j.hpe.2017.01.003
Mann, K., Gordon, J., & MacLeod, A. (2009). Reflection and reflective practice in health professions education: A systematic review. Advanced Health Science Education Theory Practice, 14(4), 595-621. https://doi.org/10.1007/s10459-007-9090-2
Mezirow, J. (1991). Transformative Dimensions of Adult Learning. Jossey-Bass.
Moon, J. A. (2004). A handbook of reflective and experiential learning: Theory and practice. Routledge Falmer.
Nguyen, Q. D., Fernandez, N., Karsenti, T., & Charlin, B. (2014). What is reflection? A conceptual analysis of major definitions and a proposal of a five-component model. Medical Education, 48(12), 1176-1189. https://doi.org/10.1111/medu.12583
Sandars, J. (2009). The use of reflection in medical education: AMEE Guide No. 44. Medical Teacher, 31(8), 685-95. https://doi.org/10.1080/01421590903050374
Tsingos, C., Bosnic-Anticevich, S., Lonie, J. M., & Smith, L. (2015). A Model for Assessing Reflective Practices in Pharmacy Education. American Journal of Pharmaceutical Education, 79(8), 124. https://doi.org/10.5688/ajpe798124
Winkel, A. F., Hermann, N., Graham, M. J., & Ratan, R. B. (2010). No time to think: Making room for reflection in obstetrics and gynecology residency. Journal of Graduate Medical Education, 2(4), 610-615. https://doi.org/10.4300/JGME-D-10-00019.1
Winkel, A. F., Yingling, S., Jones, A. A., & Nicholson, J. (2017). Reflection as a Learning Tool in Graduate Medical Education: A Systematic Review. Journal of Graduate Medical Education, 9(4), 430-439. https://doi.org/10.4300/JGME-D-16-00500.1
*Chan Yee Cheun
1E Kent Ridge Road
NUHS Tower Block, Level 10
Singapore 119228
Tel: +65 67795555
Email: yee_cheun_chan@nuhs.edu.sg
Submitted: 1 December 2020
Accepted: 5 April 2021
Published online: 5 October, TAPS 2021, 6(4), 49-64
https://doi.org/10.29060/TAPS.2021-6-4/OA2443
Yasushi Matsuyama1, Hitoaki Okazaki1, Kazuhiko Kotani2, Yoshikazu Asada3, Shizukiyo Ishikawa1, Adam Jon Lebowitz4, Jimmie Leppink5 & Cees van der Vleuten6
1Medical Education Center, Jichi Medical University, Japan; 2Center for Community Medicine, Jichi Medical University, Japan; 3Center for Information, Jichi Medical University, Japan; 4Department of General Education, Jichi Medical University, Japan; 5Hull York Medical School, University of York, United Kingdom; 6School of Health Professions Education, Maastricht University, The Netherlands
Abstract
Introduction: Previous studies indicate that professional identity formation (PIF), the formation of a self-identity with the internalised values and norms of professionalism, may influence self-regulated learning (SRL). However, it remains unclear whether a PIF-oriented intervention can improve SRL in clinical education. The aim of this study was to explore whether a PIF-oriented mentoring platform improves SRL in a clinical clerkship.
Methods: A mixed-methods study was conducted. Forty-one students in a community-based clinical clerkship (CBCC) used a PIF-oriented mentoring platform. They articulated the values and norms of professionalism in a professional identity essay, elaborated on future professional self-image, and reflected on their current compared to future selves. They made a study plan while referring to PIF-based self-reflection and completed it. The control group of 41 students completed CBCC without the PIF-oriented mentoring platform. Changes in SRL between the two groups were quantitatively compared using the Motivated Strategies for Learning Questionnaire. We explore how PIF elements in the platform affected SRL by qualitative analysis of questionnaire and interview data.
Results: A moderate improvement in intrinsic goal orientation (p = 0.005, ε2 = 0.096) and a mild improvement in critical thinking (p = 0.041, ε2 = 0.051) were observed in the PIF-oriented platform group. Qualitative analysis revealed that the PIF-oriented platform fostered professional responsibility as a key to expanding learning goals. Gaining authentic knowledge professionally fostered critical thinking, and students began to elaborate knowledge in line with professional task processes.
Conclusion: A PIF-oriented mentoring platform helped students improve SRL during a clinical clerkship.
Keywords: Self-Regulated Learning, Professional Identity Formation, Clinical Clerkship
Practice Highlights
- Encourage students to verbalise their future self-image as a medical professional.
- Encourage students to reflect on their current selves compared with their perceived future ones.
- Promote in-depth communication between students and role models to foster self-regulated learning.
- Train mentors to become professional role models as self-regulated learners.
I. INTRODUCTION
Rapid advances in clinical knowledge require medical professionals to update their knowledge autonomously throughout their practice. Self-regulation in life-long learning has therefore become an important competency, and competency-based undergraduate medical education has emphasised students’ self-regulated learning (SRL) (Berkhout et al., 2018; Brydges & Butler, 2012; Frank, 2005; Sandars & Cleary, 2011). SRL is defined as learners’ active participation in their own learning processes from metacognitive, motivational, and behavioural perspectives (Zimmerman, 1989). In undergraduate education, SRL has been related to academic achievements (Artino, Cleary et al., 2014; Artino, Dong et al., 2012; Song et al., 2011; Turan & Konan, 2012), clinical skills (Cleary & Sandars, 2011) and emotional management (van Nguyen et al., 2015).
Several reports have claimed that drastic changes in learning context, from structured learning in preclinical years to less-structured and complex learning in clinical clerkships, may be too challenging for students and lead to insufficient learning (Berkhout et al., 2015, 2018; Cho et al., 2017; van Houten-Schat et al., 2018). This question appears more serious in East Asian countries, including Japan, where strong teacher instruction in pre-university education and teacher-centred curricula are the norm (Iwata & Doi, 2017; Lam & Lam, 2009; Tagawa, 2008). In order to make the typically limited clinical clerkship period a fruitful learning opportunity, remediation for struggling students from the perspective of SRL might be important (Durning et al., 2011; van Houten-Schat et al., 2018).
Several reports have shown that individualised mentoring intervention is effective in fostering SRL in clinical practice. For example, Aho et al. (2015) found that mentor-assisted SRL for surgical habits of residents led to more frequent practice and improved skills compared to peers. In Stuart et al. (2005), individualised guidance on strategies and learning plans raised students’ awareness of the learning process. However, the educational interventions undertaken in this study will focus on another contextual characteristic that may facilitate SRL – Professional Identity Formation (PIF) – defined according to Cruess et al. (2014, p.1447) as “a representation of self, achieved in stages over time during which the characteristics, values, and norms of the medical profession are internalised”.
In response to advances in medical science and the increasingly diverse needs of society, “professional” attributes such as autonomy, self-regulation, and social responsibility have been emphasised, in addition to traditional moral and ethical education emphasising healer roles (Cruess & Cruess, 1997, 2019). Furthermore, formation of professional identity can result in individuals thinking, acting, and feeling like physicians (Cruess et al., 2014; Cruess & Cruess, 2019). During the formation of professional identity, medical students begin to perceive belonging to a professional community and increase attention to role models (Jarvis-Selinger et al., 2012; Kalet, Buckvar-Keltz, Harnik et al., 2017; Kalet, Buckvar-Keltz, Monson et al., 2018). Emulation of role models’ self-regulation in learning behaviour is also expected.
People are more likely to interpret difficult experiences as task important when an accessible identity feels congruent to the task (Oyserman et al., 2017). In the context of this study, growing professional identity as a ‘physician-to-be’ might strengthen the perceived importance of engaging in challenges during clinical clerkships, and in self-regulating learning behaviours. In addition, when physicians perceive their identity as professionals, they begin to view daily learning tasks as high-stakes, and to self-regulate learning behaviours as coping strategies (Matsuyama et al., 2018). Another study has suggested that an explicit future professional self-image in medical students leads to self-reflection, increased attention to learning strategies of professional role models, and diversification of learning strategies (Matsuyama et al., 2019). Given that PIF is associated with motivational states, self-reflection, and diversified learning strategies, SRL may be facilitated by introduction of a PIF-oriented intervention.
This study specifically focused on PIF as a facilitating factor for SRL, because previous studies have suggested possible benefits of PIF-oriented education even for East Asian medical students, who are generally considered to have less SRL due to influence of pre-university education, with its strong faculty instruction and in-university teacher-centred curricula (Matsuyama et al., 2018, 2019).
The purpose of this study was to examine whether SRL during clinical training can be fostered using a mentorship tool emphasising PIF, in addition to conventional mentorship by faculty members. In the pre- and post-clinical clerkship mentorship, students were asked to elaborate on their future self-image as professionals and compare their current and future selves to strengthen self-reflection under mentor support. Learners were aided in articulating their values and norms of medical professionalism by using the Professional Identity Essay (PIE) (Kalet, Buckvar-Keltz, Harnik et al., 2017; Kalet, Buckvar-Keltz, Monson et al., 2018), a self-administered questionnaire with 9 questions relevant to PIF. This encouraged mentors to understand the developmental stage of each learner’s professionalism and to provide individualised feedback on PIE and their future self-image. The feedback was also aimed at remediation for those whose self-images showed underdeveloped professionalism (low developmental stages in PIE). Study plans in the clinical clerkship were developed with reference to PIE-based self-images. We have named this platform ‘PIF-oriented mentoring platform for SRL (PIF-SRL)’. An overview of PIF-SRL is provided in Figure 1.
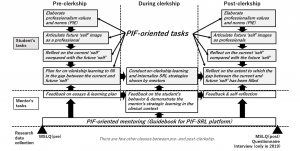
Figure 1. Overview of the PIF-SRL and research data collection
This studied centred on two research questions:
- Does PIF-SRL improve SRL during the period around the clinical clerkship?
- If so, how does the PIF-oriented elements in PIF-SRL improve SRL?
This study was approved by the ethics committee of Jichi Medical University (reference number: 19-001).
II. METHODS
A. Settings
1) Community-based clinical clerkship in Jichi Medical University: The mission of Jichi Medical University (JMU) is to educate students to become general practitioners competent in rural settings. Students are accepted per a quota system from each of Japan’s 47 prefectures. In the current curriculum at JMU, students complete lectures on almost every basic and clinical medicine area before the end of Year 3. From Year 4 to Year 6, students are permitted to participate in a clinical clerkship during which they receive training centred on taking patient histories and providing physical examination. Previously, most ward placements took place at the University’s affiliated hospital providing little opportunity for in-depth communication with role models in rural settings.
The community-based clinical clerkship (CBCC) was introduced in 1998 (Okayama & Kajii, 2011). For 2 weeks from late August to early September in Year 5, CBCC students stay at a community hospital or clinic in their home prefecture where JMU graduates work. Every year, two to five JMU graduates per prefecture are appointed to be CBCC mentors based on their motivation to teach in their prefectural communities. JMU faculty ensures the instructional quality of mentors by conducting annual face-to-face faculty development sessions. In addition, standards for learning activities are proposed, including ambulatory care, home care, hospital care, placement in mobile clinics, on-call work, rehabilitation, health education, health check-ups, vaccination, day services, and placement in welfare facilities (welfare institutions or nursing homes for the aged) (Okayama & Kajii, 2011).
Prior to the regular CBCC without PIF-SRL, students had several opportunities to communicate with mentors by telephone or e-mail. However, these communications did not provide sufficient opportunity for students to develop an image of future professionalism. We therefore felt that the communication framework in the regular CBCC did not fulfil its potential to stimulate PIF.
2) PIF-SRL for the CBCC: The PIF-SRL platform (Matsuyama et al., 2021) used an online communication platform, Google Forms. Before the CBCC began, mentors were briefed multiple times in writing and verbally on the purpose of the PIF-SRL to ensure their mentorship was PIF-oriented. They were also asked to read a manual which provided specific step-by-step responses from their first interaction with medical students on Google Forms in mid-July to their post-practice reflection in early to mid-September (Figure 1).
In the pre-clerkship phase, participants were asked to write their reflexive PIE. We used PIE because it is useful for helping learners articulate their own values and norms of medical professionalism, and for teachers providing feedback with rubrics based on Kegan’s constructive developmental theory (Kalet, Buckvar-Keltz, Harnik et al., 2017; Kalet, Buckvar-Keltz, Monson et al., 2018; Kegan, 1994). The present study used a Japanese version of the original English-language PIE form. Translation to Japanese was conducted by the main author (YM). To validate the translation accuracy, back-translation to English was conducted by a co-author (AJL), an American professor living in Japan who is literate in both English and Japanese. In accordance with in-depth talks based on PIE contents, students were encouraged to verbalise their future self-image and reflect on their current selves compared with their perceived future ones. The Question 6 of PART 2 in the PIF-SRL asked alumni mentors to describe their present self-image (Matsuyama et al., 2021). Students in PIF-SRL can also refer to this information when verbalising their future self-image.
Additionally, students in PIF-SRL were asked to create study plans for CBCC based on gaps between their current and future selves, and identify one or more learning goals. Referring to these plans, alumni mentors observed students and gave just-in-time feedback. Also, mentors provided students with learning strategies to help them overcome potential future challenges. Apart from these instructions, mentors were essentially independent in their education of the medical students. After the two-week clerkship, students were asked to re-articulate their own future image and received feedback from their mentors by Google Forms (Figure 1).
B. Subjects
First, PIF-SRL mentors were selected. In 2018 and 2019, 94 JMU graduates registered as attending rural physicians for the CBCC. Among them, 20 candidates for PIF-SRL mentors in 2018 and 2019 were randomly selected and informed consent for their contribution to PIF-SRL in this study was requested. Eventually, 17 and 13 JMU alumni agreed to participate in 2018 and 2019, respectively, 8 of whom participated in both years.
Independent of this study, the JMU Center for Community Medicine matched one alumnus with one to three students for the CBCC. The 30 PIF-SRL alumni-mentors were paired with 1 to 3 students each before informed consent was obtained. In this study, students paired with the 30 PIF-SRL alumni were chosen as candidates for the PIF-SRL group subjects. There were 22 and 20 candidates in 2018 and 2019, respectively. One candidate in 2019 declined participation. Eventually, 41 students were registered as subjects in the PIF-SRL group. Simultaneously, 41 control subjects were chosen from the same school year cohort and informed consent to participate was obtained. Control subjects experienced the regular CBCC mentorship without PIF-SRL. Because previous studies have shown that gender (Ray et al., 2003) and academic performance (Lucieer et al., 2016) might independently influence SRL development, participants in both groups were paired by gender and academic ranking from the previous year (Year 4).
C. Procedures
A convergent mixed method was chosen for the first research question ‘Does PIF-SRL improve SRL during the period around the clinical clerkship?’ to identify common data between quantitative and qualitative results (Creswell & Clark, 2017). Next, an explanatory mixed method was used to address the second research question ‘How does the PIF-oriented elements in PIF-SRL improve SRL?’. A rationale for this method is that follow-up qualitative approaches can explain quantitative results (Creswell & Clark, 2017). We conducted this mixed method study in the paradigm of pragmatism, which emphasises solutions to research questions and integrates qualitative and quantitative research results to obtain general findings (Shannon-Baker, 2016).
1) Quantitative approach: Learner SRL levels were measured with a Japanese-language version of the Motivated Strategies for Learning Questionnaire (MSLQ-J) before (mid-July) and after (mid-September) subjects participated in CBCC with or without PIF-SRL. The MSLQ (Pintrich et al., 1991) is composed of 81 items with seven-point Likert scales quantifying levels of 9 types of SRL strategy (rehearsal, elaboration, organisation, critical thinking, metacognitive self-regulation, time and study environment, effort regulation, peer learning, and help seeking), and 6 variables of motivation states (intrinsic goal orientation, extrinsic goal orientation, task value, control of learning beliefs, self-efficacy for learning and performance, and test anxiety). All 81 items of the MSLQ were used as done previously in a medical school context (Cho et al., 2017) because it was believed the 15 SRL-related categories could multi-dimensionally identify differences between the PIF-SRL group and control group. Translation to Japanese was conducted by the main author (YM) and back-translation to English by a co-author (AJL). For the MSLQ validation, the Cronbach alpha and McDonald omega were measured for 15 categories (Matsuyama et al., 2021).
2) Qualitative approach: To explore changes in motivation, strategies and reflective behaviours from self-reflection and study during the clinical clerkship, we created a questionnaire composed of seven questions (Matsuyama et al., 2021). All participants answered the questionnaire within two weeks after post-CBCC PIF-SRL mentoring. In late September 2019, one-on-one interviews were also conducted after intensive qualitative data analysis of the questionnaire from 41 participants in 2018 and 2019. Three interviewers familiar with the CBCC but not engaged in the assessment of Year 5 students conducted interviews in order to encourage interviewees to openly articulate their own perceptions. Twelve students in the 2019 PIF-SRL group consented to participate in interviews conducted in a semi-structured manner using an interview form with similar questions to those in the questionnaire (Matsuyama et al., 2021). The interviewers were instructed beforehand by the main author (YM) to obtain data about changes in perception regarding motivation, strategies and reflective behaviours after experiencing PIF-SRL. After collecting interview data from 10 students, the two main authors (YM and HO) found no additional meaningful codes emerging and, concluding that data saturation had been reached (Hennink et al., 2017), and stopped further interview data collection.
D. Analysis
1) Quantitative approach: The 15 MSLQ-J pre-intervention subcategory scores of the PIF-SRL group and control group were compared using Kruskal-Wallis one-way analysis of variance (ANOVA). After confirming that there were no statistically significant differences between the two groups, subtracted (post-pre) scores in the 15 MSLQ-J subcategories were compared between the two groups using Kruskal-Wallis one-way ANOVA. This non-parametric method was used because of considerable skewness in distribution in the scales of several items and outliers in other scales in MSLQ-J. A p-value < 0.05 was considered statistically significant. The effect sizes for comparisons were also calculated using ε2 values, wherein small effect sizes ranged from 0.01 to <0.08, medium effect sizes ranged from 0.08 to <0.26 and large effect sizes ranged from ≥0.26. We used JAMOVI version 1.0.7.0 for statistical analysis.
2) Qualitative approach: Qualitative data from PIE, the questionnaire and interviews were analysed using thematic analysis. Anonymised qualitative data were analysed in accordance with the six phases proposed by Braun and Clarke (2006). Initial coding was conducted by the two Japanese researchers (YM and HO). YM, the lead author, was involved in the development of PIF-SRL and has previous experience with qualitative studies relevant to SRL. HO was not directly engaged in PIF-SRL but has had experience in qualitative studies relevant to SRL. The transcripts were thoroughly analysed using an inductive coding approach until agreement on coding was achieved through repetitive face-to-face meetings between the pair.
The focus was on changes in SRL (motivation, learning strategies, and reflective behaviours), and student opinion of the effects of PIF-SRL on SRL. Representative codes and statements were translated into English by an American professor literate in both English and Japanese (AJL). In the final phase, two other authors (JL and CV; education psychologists familiar with SRL) joined the discussion, and a higher-level synthesis of the codes was developed.
III. RESULTS
A. Quantitative Data
Mean averages, standard deviations, and median averages for fifteen MSLQ-J categories plus gender and academic rank data at pre-intervention are shown in Table 1. No categories significantly differed between the PIF-SRL and control groups.
The subtracted (post- minus pre-intervention) between-group scores in the 15 MSLQ-J categories are shown in Table 2. Improvements in 1. Intrinsic goal orientation and 10. Critical thinking were significantly better in the PIF-SRL group than the control group with ε2 values 0.096 (p = .005) and 0.051 (p = .041), respectively. The quantitative data used in this study are accessible (Matsuyama et al., 2021).
|
|
|
PIF-SRL (N=41) |
Control (N=41) |
p value |
|
Gender |
Male/Female |
30/11 |
30/11 |
|
|
Academic rank in the previous school year |
Mean±SD |
43.7±33.0 |
45.3±32.4 |
0.79 |
|
Median |
36 |
37 |
||
|
1. Intrinsic goal orientation |
Mean±SD |
4.07±1.18 |
4.23±1.16 |
0.42 |
|
Median |
4.00 |
4.25 |
||
|
2. Extrinsic goal orientation |
Mean±SD |
3.67±1.46 |
3.69±1.44 |
0.95 |
|
Median |
3.75 |
3.75 |
||
|
3. Task value |
Mean±SD |
5.12±0.95 |
4.85±1.17 |
0.34 |
|
Median |
5.33 |
4.83 |
||
|
4. Control beliefs |
Mean±SD |
4.92±0.92 |
4.69±0.98 |
0.09 |
|
Median |
4.75 |
4.50 |
||
|
5. Self-efficacy |
Mean±SD |
3.52±1.11 |
3.36±1.23 |
0.72 |
|
Median |
3.38 |
3.50 |
||
|
6. Test anxiety |
Mean±SD |
3.94±1.17 |
4.35±1.03 |
0.12 |
|
Median |
4.20 |
4.40 |
||
|
7. Rehearsal |
Mean±SD |
4.38±1.07 |
4.23±0.91 |
0.81 |
|
Median |
4.25 |
4.25 |
||
|
8. Elaboration |
Mean±SD |
4.46±1.00 |
4.32±1.13 |
0.86 |
|
Median |
4.50 |
4.50 |
||
|
9. Organisation |
Mean±SD |
4.45±1.35 |
4.27±1.30 |
0.66 |
|
Median |
4.50 |
4.50 |
||
|
10. Critical thinking |
Mean±SD |
4.11±1.10 |
4.30±1.21 |
0.36 |
|
Median |
4.20 |
4.40 |
||
|
11. Metacognitive regulation |
Mean±SD |
4.23±0.70 |
4.18±0.82 |
0.89 |
|
Median |
4.25 |
4.17 |
||
|
12. Time and environment |
Mean±SD |
4.63±0.85 |
4.44±0.87 |
0.38 |
|
Median |
4.50 |
4.25 |
||
|
13. Effort management |
Mean±SD |
3.92±1.07 |
3.91±0.96 |
0.83 |
|
Median |
4.00 |
4.00 |
||
|
14. Peer learning |
Mean±SD |
4.70±1.24 |
4.40±1.24 |
0.36 |
|
Median |
4.67 |
4.67 |
||
|
15. Help seeking |
Mean±SD |
4.46±0.97 |
4.37±0.96 |
0.34 |
|
Median |
4.50 |
4.25 |
Table 1. Pre-intervention scores for the 15 categories of the Motivated Strategies for Learning Questionnaire-J and descriptive gender and academic rank data
|
|
|
PIF-SRL (N=41) |
Control (N=41) |
p value |
ε2 value |
|
1. Intrinsic goal orientation |
Mean±SD |
0.48±1.02 |
-0.26±1.17 |
0.005 |
0.096 |
|
Median |
0.50 |
-0.25 |
|||
|
2. Extrinsic goal orientation |
Mean±SD |
0.31±1.36 |
-0.05±1.04 |
0.200 |
0.020 |
|
Median |
0.25 |
0.00 |
|||
|
3. Task value |
Mean±SD |
0.12±1.08 |
-0.02±1.08 |
0.587 |
0.004 |
|
Median |
0.00 |
0.00 |
|||
|
4. Control beliefs |
Mean±SD |
0.04±1.07 |
0.02±1.16 |
0.665 |
0.002 |
|
Median |
0.00 |
0.25 |
|||
|
5. Self-efficacy |
Mean±SD |
0.49±1.20 |
0.10±0.82 |
0.210 |
0.019 |
|
Median |
0.25 |
0.00 |
|||
|
6. Test anxiety |
Mean±SD |
0.30±1.07 |
-0.11±1.07 |
0.152 |
0.025 |
|
Median |
0.20 |
0.00 |
|||
|
7. Rehearsal |
Mean±SD |
0.23±1.23 |
-0.02±1.14 |
0.500 |
0.006 |
|
Median |
0.25 |
0.00 |
|||
|
8. Elaboration |
Mean±SD |
0.30±1.23 |
0.13±1.03 |
0.083 |
0.037 |
|
Median |
0.50 |
0.00 |
|||
|
9. Organisation |
Mean±SD |
0.08±1.48 |
-0.04±1.08 |
0.915 |
<0.001 |
|
Median |
0.00 |
0.00 |
|||
|
10. Critical thinking |
Mean±SD |
0.48±1.08 |
-0.06±1.21 |
0.041 |
0.051 |
|
Median |
0.60 |
0.00 |
|||
|
11. Metacognitive regulation |
Mean±SD |
0.31±0.80 |
-0.07±0.69 |
0.060 |
0.043 |
|
Median |
0.16 |
0.00 |
|||
|
12. Time and environment |
Mean±SD |
0.02±1.28 |
0.02±1.03 |
0.700 |
0.002 |
|
Median |
0.00 |
0.00 |
|||
|
13. Effort management |
Mean±SD |
0.41±0.89 |
0.10±0.85 |
0.092 |
0.035 |
|
Median |
0.25 |
0.00 |
|||
|
14. Peer learning |
Mean±SD |
0.03±1.28 |
0.03±1.03 |
0.978 |
<0.001 |
|
Median |
0.00 |
0.00 |
|||
|
15. Help seeking |
Mean±SD |
0.04±1.27 |
0.04±0.84 |
0.819 |
<0.001 |
|
Median |
0.00 |
-0.25 |
Table 2. Subtracted (post- minus pre-intervention) scores in the 15 categories of the Motivated Strategies for Learning Questionnaire-J
A higher-level synthesis of the codes eventually resulted in three major themes corresponding to the second research question, ‘How does the PIF-oriented elements in PIF-SRL improve SRL?’
1) Active expansion of learning goals based on professional responsibility: The first theme consisted of subthemes which included learning motivated from responsibility, clear learning goals based on explicit self-images, and wider learning goals based on wider perceptions of professional roles.
Students viewed in-depth communication with mentors through the PIF-SRL platform with PIE helpful for imagining their future professional responsibilities in a positive and objective manner.
‘A lot of opening questions were, for example, what do you expect from work, what is the worst that can happen if you failed to live up to the expectations you have set for yourself, that’s the situation you’re working under when you’re a doctor, and the first time I really felt this was the time I really should be aware of this, it was positive, and actually although I was still just a student, I could objectively assess what I was thinking…’
(Interview, 1D-10)
During PIF-SRL mentoring, they were able to realise that knowledge beyond what they were currently learning in the curriculum was required of them as professionals. They were actively trying to set learning goals that they could connect to what they would need to learn in the future.
‘Knowing what skills and knowledge the region expects of you, you can create a working image of your future situation, and this becomes motivation to learn about new areas you weren’t aware of before.’
(Questionnaire, 2019-19)
Aside from the expansion of perceived learning goals, students also began to see that self-study was required to ensure the authenticity of medical knowledge applicable to their future professional work. This was linked to Theme 3.
‘What I got was that incomplete understanding or recall wasn’t going to cut it when actually applying knowledge in the clinic. I began to train with the awareness that I wouldn’t be useful there if I didn’t understand and remember all I learned about disease.’
(Questionnaire, 2018-21)
2) Elaboration by linking future professional task processes to daily self-study contents: The second theme was comprised of subthemes which included focus on the task processes of role models and relating daily self-study content to future roles.
After PIF-SRL, students began to imagine what they would do as professionals in future medical practice at a task process-based level. Because their vivid future professional image helped them identify deep responsibilities for their professional tasks, they began to carefully observe mentors’ complete professional tasks in the clinical clerkship and articulate task processes. This in turn encouraged students to select learning strategies which linked information in daily self-study materials (e.g. textbooks) to professional task processes, which is referred to as ‘elaboration’ in MSLQ.
‘I started to learn in terms of what I would do if it were me. I also started to think about the details and not just the general flow of things, and to apply them as much as possible to reality.’
(Questionnaire, 2018-8)
‘Since the clerkship, I’ve been able to relate and recall what I actually encountered in the clinical clerkship, and when I was actually reading textbooks in self-study, I was able to align it with my future work content, and if there were things that applied, I would emphasise them… The study method that I use to impress upon myself was strengthened in the mentoring and clerkship…’
(Interview, 1D-3)
3) Critical thinking based on the pursuit of authentic medical knowledge: The third theme was comprised of subthemes which included realisation of the significance of authenticity pursuit, access to a wide variety of educational materials, and critical reflection.
Because they began to perceive that what they were learning would affect the lives of individual patients, they recognised the significance of gaining authentic knowledge that could be applied to each patient, differentiated from textbook-based universal knowledge.
‘It’s really important to learn about disease by studying the texts and gaining comprehensive knowledge, but since that tertiary material is insufficient for responding to clinical questions and individual patient backgrounds, I’m not sure that knowledge is useful in clinical practice. For that, what’s most meaningful are secondary materials like UpToDate, or if you still have doubts then primary material research papers.
(Questionnaire, 2019-1)
After beginning to pursue authenticity of medical knowledge, students found diversity and inconsistency in information from learning materials. To deal with this, they began to formulate inquiries focusing on self-study, a variety of information resources, and different viewpoints. Through this strategic shift, critical thinking emerged in an intrinsic manner.
‘I’ve come to think opinions are going to diverge to some extent as you get down to actually asking opinions of several different doctors, and these are choices you have to make, the stages you go through when studying.’
(Interview, 1C-7)
‘Having the ability to doubt, and because it’s science not taking everything at face value, becoming sceptical, I think that’s necessary.’
(Interview, 3C-14)
IV. DISCUSSION
Regarding the first research question ‘Does PIF-SRL improve SRL during the period around the clinical clerkship?’, our findings of a moderate improvement in intrinsic goal orientation and a mild improvement in critical thinking in the PIF-SRL group compared with the control group suggested that PIF-SRL promotes SRL. The qualitative analysis supports the MSLQ-J results. With regard to intrinsic goal orientation, students’ recognition of their future ‘professional responsibility’ was a key to fostering this. Further, recognition of professional responsibility led to critical thinking — critical evaluation of learning materials or their interpretation — as a means of pursuing authenticity of information for professional task processes. The consistency between quantitative and qualitative data was notable in understanding the outcomes of the PIF-oriented mentoring on SRL.
There was no statistical significance in the difference between the PIF-SRL and the control groups regarding elaboration in MSLQ-J data. However, qualitative analysis illuminated that PIF-SRL students’ attention to professional task processes triggered a strategy toward elaboration of knowledge in accordance with their future professional task processes. Reasons for this discrepancy might include the number of participants and sensitivity of the outcome measurement (Tonkin-Crine et al., 2016). Further research is needed to address these issues. However, we believe that in order to remediate learning strategies necessary for professional tasks or professionalism, it is useful to reflect on daily self-learning in accordance with the process of professional work shown by role models.
Recent research pertaining to educational intervention for SRL emphasises analysing the learning process of a particular task in detail and remediating the individual process (Artino et al., 2014; Durning et al., 2011; Gandomkar et al., 2016). While we generally concur with this, learning tasks that take place in clinical practice are limitless, so it would be beneficial to explore a foundational intervention applicable to a variety of tasks in clinical settings. The PIF-oriented mentoring in this study is presented as a foundational SRL intervention for a variety of clinical settings wherein learners can recognise professional identities and role models can suggest learning strategies.
The major strength of this study is that the subjects were Japanese students, who are considered to engage less in self-regulation than their Western counterparts (Iwata & Doi, 2017; Matsuyama et al., 2018; Tagawa, 2008). We believe that our study can provide educators with evidence that PIF-oriented educational schemes promote better learning behaviours in institutions desiring to promote undergraduate SRL. Another strength is that there were few formal classes or training programmes – i.e., intervening confounders — except for PIF-SRL and CBCCs between pre- and post-data collection (Figure 1). We believe the study schedule, without other educational interventions, optimised learning comparison outcomes between the two groups. For instance, changes in accessing learning materials for critical thinking (e.g. UpToDate) can be attributed mostly to the experiences in PIF-oriented mentoring and the subsequent CBCCs.
This study also has some limitations. First, we did not collect one-on-one interview data from 2018 cohort. Second, we did not examine student SRL changes from the mentor’s perspective, despite the fact that mentors’ perceptions of changes in students’ SRL would be as useful as, or more useful than students’ self-administered data. Third, reference to mentors’ self-images in the PIF-SRL could help students in PIF-SRL construct their professional self-image more clearly; however, this may cause bias student statements in the PIF-SRL form regardless of their real professionalism. Future research needs to measure PIF and SRL in more multifaceted and objective manners. Lastly, we do not have long-term outcomes of PIF-SRL. According to previous studies (Cruess et al., 2014; Cruess & Cruess, 2019; Kalet et al., 2017; Oyserman et al., 2017), identity is flexibly attuned to immediate situations rather than fixed in memory. Plus, frequently and fluently cued identities form stable ones. Accordingly, we speculate that the repetitive use of PIF-SRL could strengthen learners’ SRL. Validation of this notion would require a longitudinal cohort study.
Evaluation of these results suggests that the ability of PIF-SRL to work effectively requires that the quality of mentors be guaranteed. One reason for the success of the relatively random combination of students and mentors in this PIF-SRL group is that all are future rural physicians, and their mentors are also alumni of JMU in rural practice. On the other hand, for medical students from other universities who can follow diverse specialties and career paths, use of the PIF-SRL will require pairing medical students with appropriate mentors who can respond to students’ identities or future images. Also, it is important to pair students not only by their interest in future expertise, but also by looking at the mental and physical traits of individual students as they relate to motivation and student career choices (Henning et al., 2017). Moreover, in-depth conversations that would foster professionalism might not be done only through text messages in the PIF-SRL platform, but also through video calls and in-person meetings that would convey the participants’ voices, facial expressions, and mood. We think it is important for mentors to actively provide opportunities for direct dialogue with students. In light of this challenge, the present study supports PIF-oriented intervention as a method for improvement in SRL.
V. CONCLUSION
Allowing for these limitations and the need for further research, this study indicated that PIF-oriented education in a clinical clerkship with alumni mentors increased immediate intrinsic goal orientation and promoted a shift to SRL. Their SRL was characterised as task process-based elaboration, with critical thinking emerging from the pursuit of authenticity in medical practice.
Notes on Contributors
Yasushi Matsuyama reviewed the literature, designed the study, conducted both quantitative and qualitative data analysis, and wrote the manuscript.
Hitoaki Okazaki conducted qualitative data analysis.
Kazuhiko Kotani designed the study, and collected both quantitative and qualitative data.
Yoshikazu Asada collected both quantitative and qualitative data.
Shizukiyo Ishikawa collected both quantitative and qualitative data.
Adam Jon Lebowitz contributed to Japanese-English translation of data collection tools and qualitative data from questionnaire and interviews.
Jimmie Leppink reviewed the literature, designed the study, conducted both quantitative and qualitative data analysis, and wrote the manuscript.
Cees van der Vleuten reviewed the literature, designed the study, conducted both quantitative and qualitative data analysis, and wrote the manuscript.
All the authors have read and approved the final manuscript.
Ethical Approval
This study was approved by the ethics committee of Jichi Medical University (Reference number: 19-001). Consent was obtained from all participants for the research study.
Acknowledgements
We would like to express our sincere gratitude to Dr. Adina Kalet and Dr. Verna Monson for their consultation and provision of supplementary materials. We would also like to thank Drs. Yasuko Aoyama, Yoshitaka Maeda, and Maiko Watanabe for their support in conducting one-on-one interviews. We would also like to thank Ms. Akemi Watanabe and Yasuko Koguchi for their helpful assistance.
Funding
This work was supported by JSPS KAKENHI [Grant number JP17K08924].
Declaration of Interest
The authors report no conflicts of interest.
Data availability
The quantitative data used in this study, Supplemental files are available at https://doi.org/10.6084/m9.figshare.14312507
Representative qualitative data translated into English are shown in the Result section (Matsuyama et al., 2021). All qualitative data written in Japanese are available from the corresponding author on reasonable request.
A preprint of the previous version of our manuscript, which is not peer-reviewed, is available at https://www.researchsquare.com/article/rs-12667/v1
References
Aho, J. M., Ruparel, R. K., Graham, E., Zendejas-Mummert, B., Heller, S. F., Farley, D. R., & Bingener, J. (2015). Mentor-guided self-directed learning affects resident practice. Journal of Surgical Education, 72(4), 674–679. https://doi.org/10.1016/j.jsurg.2015.01.008o
Artino, A. R., Jr., Cleary, T. J., Dong, T., Hemmer, P. A., & Durning, S. J. (2014). Exploring clinical reasoning in novices: A self-regulated learning microanalytic assessment approach. Medical Education, 48(3), 280–291. https://doi.org/10.1111/medu.12303
Artino, A. R., Jr., Dong, T., DeZee, K. J., Gilliland, W. R., Waechter, D. M., Cruess, D., & Durning, S. J. (2012). Achievement goal structures and self-regulated learning: Relationships and changes in medical school. Academic Medicine, 87(10), 1375–1381. https://doi.org/10.1097/ACM.0b013e3182676b55
Berkhout, J. J., Helmich, E., Teunissen, P. W., van den Berg, J. W., van der Vleuten, C. P., & Jaarsma, A. D. (2015). Exploring the factors influencing clinical students’ self-regulated learning. Medical Education, 49(6), 589–600. https://doi.org/10.1111/medu.12671
Berkhout, J. J., Helmich, E., Teunissen, P. W., van der Vleuten, C., & Jaarsma, A. (2018). Context matters when striving to promote active and lifelong learning in medical education. Medical Education, 52(1), 34–44. https://doi.org/10.1111/medu.13463
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
Brydges, R., & Butler, D. (2012). A reflective analysis of medical education research on self-regulation in learning and practice. Medical Education, 46(1), 71–79. https://doi.org/10.1111/j.1365-2923.2011.04100.x
Cho, K. K., Marjadi, B., Langendyk, V., & Hu, W. (2017). Medical student changes in self-regulated learning during the transition to the clinical environment. BMC Medical Education, 17(1), 59. https://doi.org/10.1186/s12909-017-0902-7
Cleary, T. J., & Sandars, J. (2011). Assessing self-regulatory processes during clinical skill performance: A pilot study. Medical Teacher, 33(7), e368–e374. https://doi.org/10.3109/0142159X.2011.577464
Creswell, J. W., & Clark, V. L. P. (2017). Designing and conducting mixed methods research. SAGE Publications.
Cruess, R. L., & Cruess, S. R. (1997). Teaching medicine as a profession in the service of healing. Academic Medicine, 72(11), 941–952. https://doi.org/10.1097/00001888-199711000-00009
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2014). Reframing medical education to support professional identity formation. Academic Medicine, 89(11), 1446–1451. https://doi.org/10.1097/ACM.0000000000000427
Cruess, S. R., & Cruess, R. L. (2019). The development of professional identity. In T. Swanwick., K. Forrest., B. C. O’Brein (Eds.), Understanding medical education; Evidence, theory, and practice (3rd ed., pp. 239–254). https://doi.org/10.1002/9781119373780.ch17
Durning, S. J., Cleary, T. J., Sandars, J., Hemmer, P., Kokotailo, P., & Artino, A. R. (2011). Perspective: Viewing “strugglers” through a different lens: How a self-regulated learning perspective can help medical educators with assessment and remediation. Academic Medicine, 86(4), 488–495. https://doi.org/10.1097/ACM.0b013e31820dc384
Frank, J. R. (2005). The CanMEDS 2005 physician competency framework. Better standards. Better physicians. Better care. The Royal College of Physicians and Surgeons of Canada.
Gandomkar, R., Mirzazadeh, A., Jalili, M., Yazdani, K., Fata, L., & Sandars, J. (2016). Self-regulated learning processes of medical students during an academic learning task. Medical Education, 50(10), 1065–1074. https://doi.org/10.1111/medu.12975
Henning, M. A., Krägeloh, C. U., Booth, R., Hill, E. M., Chen, J., & Webster, C. S. (2017). Profiling potential medical students and exploring determinants of career choice. The Asia Pacific Scholar, 2(1), 7-15. https://doi.org/10.29060/TAPS.2017-2-1/OA1019
Hennink, M. M., Kaiser, B. N., & Marconi, V. C. (2017). Code saturation versus meaning saturation: How many interviews are enough? Qualitative Health Research, 27(4), 591–608. https://doi.org/10.1177/1049732316665344
Iwata, K., & Doi, A. (2017). Can hybrid educational activities of team and problem based learning program be effective for Japanese medical students? International Journal of Medical Education, 8, 176–178. https://doi.org/10.5116/ijme.591b.2bc8
Jarvis-Selinger, S., Pratt, D. D., & Regehr, G. (2012). Competency is not enough: Integrating identity formation into the medical education discourse. Academic Medicine, 87(9), 1185–1190. https://doi.org/10.1097/ACM.0b013e3182604968
Kalet, A., Buckvar-Keltz, L., Harnik, V., Monson, V., Hubbard, S., Crowe, R., Song, H. S., & Yingling, S. (2017). Measuring professional identity formation early in medical school. Medical Teacher, 39(3), 255–261. https://doi.org/10.1080/0142159X.2017.1270437
Kalet, A., Buckvar-Keltz, L., Monson, V., Harnik, V., Hubbard, S., Crowe, R., Ark, T. K., Hyuksoon, Song, H. S., & Yingling, S. (2018). Professional Identity Formation in medical school: One measure reflects changes during pre-clerkship training. MedEdPublish, 7(1), 41. https://doi.org/10.15694/mep.2018.0000041.1
Kegan, R. (1994). In over our heads: The mental demands of modern life. Harvard University Press.
Lam, T. P., & Lam, Y. Y. (2009). Medical education reform: The Asian experience. Academic Medicine, 84(9), 1313–1317. https://doi.org/10.1097/ACM.0b013e3181b18189
Lucieer, S. M., Jonker, L., Visscher, C., Rikers, R. M. J. P., & Themmen, A. P. N. (2016). Self-regulated learning and academic performance in medical education. Medical Teacher, 38(6), 585–593. https://doi.org/10.3109/0142159X.2015.1073240
Matsuyama, Y., Nakaya, M., Okazaki, H., Leppink, J., & van der Vleuten, C. (2018). Contextual attributes promote or hinder self-regulated learning: A qualitative study contrasting rural physicians with undergraduate learners in Japan. Medical Teacher, 40(3), 285–295. https://doi.org/10.1080/0142159X.2017.1406074
Matsuyama, Y., Nakaya, M., Okazaki, H., Lebowitz, A. J., Leppink, J., & van der Vleuten, C. (2019). Does changing from a teacher-centered to a learner-centered context promote self-regulated learning: A qualitative study in a Japanese undergraduate setting. BMC Medical Education, 19(1), 152. https://doi.org/10.1186/s12909-019-1550-x
Matsuyama, Y., Okazaki, H., Kotani, K., Asada, Y., Ishikawa, S., Lebowitz, A. J., Leppink, J., & van der Vleuten, C. (2021). Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14312507
Matsuyama, Y., Okazaki, H., Kotani, K., Asada, Y., Ishikawa, S., Lebowitz, A. J., Leppink, J., & van der Vleuten, C. (2020). Education in professional identity formation enhances self-regulated learning: A mixed-method exploratory study from a community-based clinical clerkship in Japan. [Preprint]. Research Square. January 28, 2020. [cited June 10, 2020] Available from: https://doi.org/10.21203/rs.2.22088/v1
Okayama, M., & Kajii, E. (2011). Does community-based education increase students’ motivation to practice community health care? A cross sectional study. BMC Medical Education, 11(1), 19. https://doi.org/10.1186/1472-6920-11-19
Oyserman, D., Lewis, Jr., N. A., Yan, V. X., Fisher, O., O’Donnell, S. C., & Horowitz, E. (2017). An identity-based motivation framework for self-regulation. Psychological Inquiry, 28(2-3), 139-147. http://doi.org/10.1080/1047840X.2017.1337406
Pintrich, P. R., Smith, D. A. F., Garcia, T., & McKeachie, W. J. (1991). A manual for the use of the Motivated Strategies for Learning Questionnaire (Technical Report 91-B-004). The Regents of the University of Michigan. https://files.eric.ed.gov/fulltext/ED338122.pdf
Ray, M. W., Garavalia, L. S., & Gredler, M. E. (2003, April 21-25). Gender differences in self-regulated learning, task value, and achievement in developmental college students. Annual Meeting of the American Educational Research Association. https://files.eric.ed.gov/fulltext/ED476176.pdf
Sandars, J., & Cleary, T. J. (2011). Self-regulation theory: Applications to medical education: AMEE Guide No. 58. Medical Teacher, 33(11), 875–886. https://doi.org/10.3109/0142159X.2011.595434
Shannon-Baker, P. (2016). Making paradigms meaningful in mixed methods research. Journal of Mixed Methods Research, 10(4), 319-334. https://doi.org/10.1177/1558689815575861
Song, H. S., Kalet, A. L., & Plass, J. L. (2011). Assessing medical students’ self-regulation as aptitude in computer-based learning. Advances in Health Sciences Education: Theory and Practice, 16(1), 97–107. https://doi.org/10.1007/s10459-010-9248-1
Stuart, E., Sectish, T. C., & Huffman, L. C. (2005). Are residents ready for self-directed learning? A pilot program of individualized learning plans in continuity clinic. Ambulatory Pediatrics, 5(5), 298–301. https://doi.org/10.1367/A04-091R.1
Tagawa, M. (2008). Physician self-directed learning and education. The Kaohsiung Journal of Medical Sciences, 24(7), 380–385. https://doi.org/10.1016/S1607-551X(08)70136-0
Tonkin-Crine, S., Anthierens, S., Hood, K., Yardley, L., Cals, J. W., Francis, N. A., Coenen, S., van der Velden, A. W., Godycki-Cwirko, M., Llor, C., Butler, C. C., Verheij, T. J., Goossens, H., Little, P., & GRACE INTRO/CHAMP consortium (2016). Discrepancies between qualitative and quantitative evaluation of randomised controlled trial results: Achieving clarity through mixed methods triangulation. Implementation Science, 11, 66. https://doi.org/10.1186/s13012-016-0436-0
Turan, S., & Konan, A. (2012). Self-regulated learning strategies used in surgical clerkship and the relationship with clinical achievement. Journal of Surgical Education, 69(2), 218–225. https://doi.org/10.1016/j.jsurg.2011.09.003
van Houten-Schat, M. A., Berkhout, J. J., van Dijk, N., Endedijk, M. D., Jaarsma, A. D. C., & Diemers, A. D. (2018). Self-regulated learning in the clinical context: A systematic review. Medical Education, 52(10), 1008–1015. https://doi.org/10.1111/medu.13615
Van Nguyen, H., Laohasiriwong, W., Saengsuwan, J., Thinkhamrop, B., & Wright, P. (2015). The relationships between the use of self-regulated learning strategies and depression among medical students: An accelerated prospective cohort study. Psychology, Health & Medicine, 20(1), 59–70. https://doi.org/10.1080/13548506.2014.894640
Zimmerman, B. J. (1989). A social cognitive view of self-regulated academic learning. Journal of Educational Psychology, 81(3), 329.
*Yasushi Matsuyama
3311-1
Yakushiji, Shimotsuke,
Tochigi, 329-0498
Email: yasushim@jichi.ac.jp
Submitted: 2 November 2020
Accepted: 8 February 2021
Published online: 5 October, TAPS 2021, 6(4), 37-48
https://doi.org/10.29060/TAPS.2021-6-4/OA2425
Stephen Bradley1, Aaron Ooi2, Kerry Stafford3, Shuvayon Mukherjee1 & Marcus A. Henning4
1Department of Paediatrics, Lakes District Health Board, New Zealand; 2Department of Paediatrics, Waikato District Health Board, New Zealand; 3Department of Paediatrics, Christchurch Hospital, New Zealand; 4Centre for Medical and Health Sciences Education, University of Auckland, New Zealand
Abstract
Introduction: The paediatric team handover process is a crucial workplace practice and comprises the transfer of patient information from one shift to another involving medical professionals and students. A qualitative study was performed to analyse the feasibility, functionality, benefits and limitations of the dramaturgical approach when applied to examining a handover session.
Methods: Data relating to one handover were collected and analysed from video and audio recordings, notes created by two independent observers and a de-identified copy of the handover sheet.
Results: The dramaturgical constructs and subsequent findings allowed us to make informed inferences about the dynamics of the handover procedure. The directors/lead actors consisted of a consultant and a registrar. One consultant was transitory and the remaining 12 attendees were either major support, support or bit actors. The students (bit actors/audience) were included when a learning point was emphasised. The script was informal and improvised as the discussion emphasised certain facets of patient care or accentuated learning points. The staging involved the seating arrangement, a whiteboard, computer screen and ongoing data presentation. The performance suggested a handover of two halves: one emphasising learning and the other allocation of patient care responsibility.
Conclusion: We concluded that the real-life drama occurring within a handover was feasibly analysed, with its functionality demonstrated, using the dramaturgical investigative system. The multifaceted recordings enabled researchers to review the ‘authentic’ handover system without censorship. These findings have implications for educational and organisational research.
Keywords: Dramaturgical, Handover, Paediatric, Methodology
Practice Highlights
- Dramaturgical methodology provided a unique, authentic and detailed analysis of the handover.
- The dramaturgical research methodology used to evaluate the handover was feasible and functional.
- This research methodology can be used to analyse education within similar team based settings.
- This research methodology can be applied to the team handovers and other complex health meetings.
- This research methodology identifies important clinical/educational roles and dynamics within teams.
I. INTRODUCTION
Hospital team handovers involve effective transfer of information and responsibility from one health professional to another, ensuring continuity of patient care (Australian Medical Association Limited, 2006; Hilligoss & Cohen, 2011). The level of communication needs to be comprehensive, unambiguous and coherent so that patient information is easily understood, thus optimising patient care through the meaningful and efficient transfer of patient information (Fujikawa et al., 2021). This is crucial given the ramifications for optimising patient care and minimising potential treatment error, including miscued transfer of knowledge, insertion of faulty or misleading information, treatment delay, and poor patient outcomes (Arora et al., 2005; Bomba & Prakash, 2005). To explore the nuances occurring in handover practice from organisational behaviour and educational perspectives, different methodological approaches need to be developed.
In this paper, we propose that the dramaturgical approach can optimally analyse handover dynamics, as it is an integrated, pragmatic and multidimensional approach. This approach uses multi-source feedback from video and audio recordings, observer records, and transcripts of analysis. The dramaturgical approach argues that the individuals present in the activity assume different roles that influence the way they communicate and behave (Canary et al., 2008; Goffman, 1959; Henderson, 2005). Using this approach, the handover activity can be analysed much like a drama or element of theatre. The dramaturgical approach has the potential to offer insights into the clinical and educational handover components, much like the insights drawn when applying this approach to analysing healthcare simulations (Crea, 2017), decision-making aspects of an emergency department triage (Forde, 2014), and behaviour of radiographers and their patients (Murphy, 2009). This analytical approach enables the researcher to be present at the moment of the occurrence, rather than relying on retrospective data obtained when subsequently interviewing participants. Interviews can be a powerful means of obtaining information, but require participants to accurately retell their experiences of the activity (DiCicco‐Bloom & Crabtree, 2006). The dramaturgical approach tells it for what it is, and allows researchers the ability to see and hear the authentic process of communication (Goffman, 1959; Murphy, 2009). We surmised that the dramaturgical approach would be a more comprehensive evaluative system and thus well suited for collecting observational data that could inform training and development initiatives within hospital systems.
The research aim of this study was to explore the feasibility and functionality of the dramaturgical methodological system of analysis not yet applied to the handover procedure.
The research questions driving this study include:
- How can the dramaturgical approach feasibly be applied to the handover system?
- How does the dramaturgical approach describe the functional dynamics of the handover procedure?
- What are the benefits and limitations associated with applying this research methodology?
II. METHODS
A. Phenomenon of Interest
Feasibility, functionality and quality were informed by examples taken from one handover involving team discussion regarding patients admitted to a general paediatric ward (20 beds) and a Special Care Baby Unit (8 cots) in a New Zealand secondary-level hospital (Hensher et al., 2006).
B. Sample/Participants
All the health professionals and medical students involved in one handover were asked to volunteer for the study, with eligibility determined by consent and approval from hospital management. Informed consent was obtained after eligible participants read a detailed information sheet, provided by an administrator, followed by a consent form that they then signed.
C. Data Collection
Data were obtained from several sources.
- Five video cameras were situated in the handover room to obtain multiple angles of the handover. Two audio recorders were placed in the room and served as the primary sources of data for transcription.
- The final transcription of events was checked by all authors using data from the cameras.
- Notes on the salient aspects of handover interactions were made by two present ‘unknown’ observers (i.e., one medical student and one medical educationalist).
A diagram of the seating positions of each participant was constructed (see Figure 1).
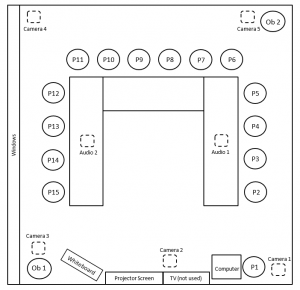
Figure 1: Handover room layout depicting seating arrangements, participants (P1-P15, with original position participants sat in), 2 observers (Ob1 and Ob2) and equipment.
D. Ethical Considerations
Confidentiality of the key informants was maintained by the following criteria:
- All participants were given an anonymised label (P1 to P15).
- All patients discussed within the handover were anonymised (labelled 1 to 36) and identifiable information was deleted from patient reports.
- Several hospital employees involved in the study were not present at the handover and transcription was conducted by an uninvolved third party.
-
-
E. Data Analysis
To test the feasibility of the dramaturgical approach, a framework was adapted exploring the perspectives of the actors and audience, the script, the staging and the overall performance (Canary et al., 2008; Crea, 2017; Henderson, 2005). Delineation of roles within the handover (Preves & Stephenson, 2009; Schell, 2016) identified the following ‘actors’: lead, major support, support, and bit actors. The perceived director was involved in the leading and facilitation of the handover (Goffman, 1959). The audience was defined as observers or those actors minimally involved in the main discussion (Canary et al., 2008; Hays & Weinert, 2006). Other factors considered in the analysis included scripting, staging, and performance analysis (Hays & Weinert, 2006).
We scrutinised the data using a deductive thematic content analysis based on dramaturgy criteria (Elo & Kyngäs, 2008). The usefulness of voice-occupied time (VOT) was appraised and VOT was defined as the total time a participant spoke during the entire handover divided by the total duration of the handover, expressed as a percentage. The utility of a timeline considered the dynamics connected to scene development. Lastly, the trustworthiness of the qualitative data analysis protocol was audited (Elo et al., 2014).
III. RESULTS
The following data were used to assess the feasibility, functionality and quality of the dramaturgical process. For full data details, please refer to Figshare (2020).
A. Actors and Audience
The handover involved 15 participants (Table 1).

Table 1: Roles and number of participants and observers present in handover.
The VOT analysis (see Table 2) was useful in quantifying participation as aligned with perceived roles. The participant with the highest VOT was deemed to be the lead actor, while the second highest VOT was classified as the major supporting actor. Participants with VOTs of greater than 5% were defined as supporting actors, and participants who had VOTs of less than 5% were judged to be bit actors and audience. Accordingly, the lead consultant (the initial director) (P13) and the senior registrar (P3), who each had more than 15% of the VOT, were judged to be the lead and major support actors respectively. Eight (53%) of the participants were identified to be present as bit actors or audience.
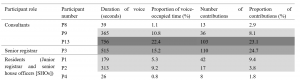
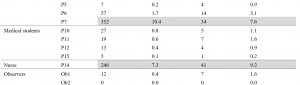

Table 2: Percentage of voice occupied time (VOT) and number of contributions per participant.
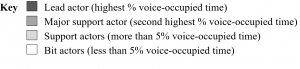
A separate analysis was conducted counting the number of contributions (clearly-heard comments) each handover participant made, with a total of 446 contributions quantified during the handover. This was correlated with the VOT and provided a point of comparison to identify crucial facets of the handover drama.
B. Roles
The utility of the dramaturgical approach was also demonstrated in identifying the roles of handover members. It was ascertained that the three consultants had distinct roles. The lead actor (P13) was the consultant on the ward that week. She led the beginning of the handover, directed the flow of discussion and took on a major teaching role. The second consultant (P9), who had been on call overnight, contributed important information and was involved in teaching. The third consultant (P8) sought information about suitable patients for teaching, but contributed little to the discussions.
A further key role identified was the senior registrar (P3), who contributed little to the handover until the dramatic time when a phone call interrupted the handover. After the departure of the lead consultant (P13), she acquired the major support actor role, but did so in a very business-like manner to ensure that all patients were discussed and a safe plan established.
Roles were highlighted participants’ costumes. The doctors and students in the handover wore smart-casual attire. Several clearly had available stethoscopes, whilst the nurse wore a uniform.
C. Script
The script was found to be a useful informal source of information. Whilst close attention was given to the handover sheet containing patient details, it was clear that participants improvised. The dramaturgical analysis established that the patients cared for by the paediatric team were the subjects of the performance. Patients were referred to respectfully, and the discussion was focused on their daily requirements.
D. Staging
The room (Figure 1) was notable for the horseshoe-shaped arrangement of tables and chairs, which enabled the researchers to evaluate visibility of participants and their access to technological equipment. The notion of staging also enabled researchers to establish the activities that occurred within the room (on-stage) as opposed to those outside the room (off-stage).
E. Props
The most significant prop was the handover sheet (or script) listing the patients’ names, demographic data, their medical issues, and initiated investigations and plan.
F. Performance
1) Scenes: The scenes could be classified as follows. These were the prologue, three acts, and an epilogue represented as 14 distinct scenes (Table 3). We were able to identify each new scene arising at the point of a significant incident in the handover discussion.
|
Act |
Scene number |
Scene name |
Major theme of scene |
Description of scene |
Actors with VOT within scene |
|
Prologue. |
1 |
“Nice to meet you.” |
Setting the scene. |
First four handover members arrive (P3, P12, P13, P14). New SHO arrives (P6) and receives brief orientation. Remaining handover members arrive (P1, P2, P4, P5, P7, P9, P10, P11). Meet member of research team (Ob 1). |
P3, P6, P12, P13, P14, Ob 1 |
|
Act 1 – The beginning of handover. |
2 |
“Can we just get going?” |
Introductions. |
Each member of team states their name and role. |
P1, P2, P3, P4, P5, P6, P7, P9, P10, P11, P12, P13, P14 |
|
3 |
“Fire away!” |
Start of night handover. |
Lead consultant (P13) initiates handover. Night SHO (P2) utilises handover sheet as a prompt to discuss cases encountered during the night. P8 enters room. |
P2, P8, P13 |
|
|
4 |
“Patient 21, a baby.” |
Focus on a sick child. |
Case of specific child who deteriorated during the night presented, becoming a significant aspect of discussion. Four most senior members of the team (P3, P8, P9, P13) contribute to this discussion. P15 enters room. P2 completes handover of relevant patients, exits thereafter. |
P1, P2, P3, P8, P9, P13 |
|
|
Act 2 – Educational moments and the climax.
|
5 |
“Can I just interrupt?” |
Planning for assessment. |
Consultant (P8) requests patients for examination purposes (principal reason for P8 attending handover), exits thereafter. |
P8, P13 |
|
6 |
“What other things would you like to tell us?” |
Educational moment arising from handover. |
Consultant (P9) presents case of a specific child with alleged non accidental injury, with subsequent educational moment (P13 and P9 acting as prompts for discussion and sources of information respectively). |
P1, P4, P9, P13, P14 |
|
|
7 |
“Is there any learning for us from that one?” |
Further educational moment. |
Lengthy discussion focussed around a ‘difficult’ case. Consultant (P13) uses words “And herein is the learning”, stands up and uses whiteboard to discuss differentials and poses questions to individual team members. P9 serves as a source of clinical information. On-call SHO phone rings and SHO (P5) exits room, followed by senior registrar (P3) from whom help is sought. P9 exits room. |
P1, P3, P4, P5, P6, P7, P9, P10, P11, P12, P13, P14, P15 |
|
|
8 |
“I will need to divide them up.” |
Focus on workload for patients on inpatient ward. |
Resumption of systematically working through inpatients on the handover sheet to generate management plans, with input obtained from residents and students who had seen children the previous day. |
P1, P3, P7, P13 |
|
|
9 |
“Just been phoned from ED!” |
Dramatic intervention – a sick child in the Emergency Department (ED). |
Interruption of handover to discuss a seriously unwell child who requires specialist attention in ED (climax). P13 states: “Emergent patient care always takes priority”. Lead consultant (P13) exits with on-call SHO (P5). |
P1, P3, P5, P13, P14 |
|
|
Act 3 – The business end of handover. |
10 |
“So, shall we go back up to …?” |
Focus on workload for patients on inpatient ward. |
Resumption of systematically working through inpatients on the handover sheet to generate management plans, with input obtained from residents and students who had seen children the previous day. Senior registrar (P3) now leads the handover discussion with regular, brief contributions. |
P1, P3, P7, P11, P14 |
|
11 |
“OK. Umm and SCBU…” |
Focus on workload for neonates in the Special Care Baby Unit (SCBU). |
Systematic working through SCBU patients on the handover sheet to generate management plans, with input obtained from residents and students who had seen children the previous day. |
P3, P7, P14 |
|
|
12 |
“And then… chase results.” |
Focus on chasing up outstanding laboratory results. |
Systematic working through patients on handover sheet who have outstanding laboratory results to be followed up. |
P1, P3, P7, P14 |
|
|
Epilogue. |
13 |
“So, what are you doing now?” |
Discussion about participants’ day plans. |
Senior registrar (P3) checks with members of team their understanding of their roles for the day. |
P1, P3, P4, P6, P7 |
|
14 |
“Yeah, sweet… done!” |
Conclusion. |
Completion of handover as evidenced by verbal and body language cues as members of team exit the room. |
P3 |
Table 3: Acts and scenes within the handover
2) Entrances and exits: Easily demarcated entrance and exit points of the handover were identified. P1 arrived 5 minutes before the handover commenced, prepared the computer, and then left and returned with the remainder of the handover team. This initial entrance represented the entire group arriving, with a prologue consisting of set up and early introductions (Scene 1).
An example of a dramatic exit and re-entrance of two doctors (P3, P5) was noted during Scenes 7 and 9, which proved to be a major incident, as the phone call off-stage notified them of a critical case. Following this, the lead consultant (P13) exited with a SHO (P5) and the director role was handed to the senior registrar (P3). This altered the handover significantly and came at a time when the handover had moved from a largely educational milieu to a more work-like role.
See Figure 2 for a time-line regarding the Handover.
Figure 2: Timeline of acts, scenes and selected events
3) Additional observations: Multiple data collection methods enhanced the dramaturgical method, through clarifying inaudible audio data. Entrances and exits did not always prompt comments on the audio recording, but were noted from the video recordings. A critical incident occurred when the lead consultant established an educational role and used the whiteboard for teaching – the impact of this would not have been so apparent without a video recording.
IV. DISCUSSION
The studied handover was attended by multiple professionals and students, and had several purposes, focussing on the safe exchange of knowledge and responsibility for a group of patients with variable clinical conditions and acuity (Australian Medical Association Limited, 2006; Hilligoss & Cohen, 2011). We argued that the dramaturgical approach would be a valuable method for analysing the dynamics of this handover. To evaluate the effectiveness of this research approach, we focussed on the feasibility, functionality and quality of the dramaturgy approach.
A. Feasibility
The dramaturgical perspective argues that individuals “play different roles as ‘actors’ and engage in ‘performances’ in order to shape their ‘definition of the situation’” (Canary et al., 2008, p. 155). We applied the metaphor of ‘life as drama’ to this handover. The findings and information gleaned from this handover demonstrated that a dramaturgy approach embedded within a case study methodology can be applied to a complex team handover.
Obtaining consent from all handover attendees in a manner that did not impact on the handover itself required significant pre-planning by the research team and cooperation from the department. In their systematic review, Flory and Emanuel (2004) examined methods for improving the consent process and for increasing participant understanding. One recommendation centred on employing significant person-to-person contact as an optimal method to improve understanding. To avoid undue power dynamics, a senior consultant at this hospital involved in the study was not involved in the administrative process, and this prevented any direct involvement in the recruitment and data collection processes, thus minimising inducement and conflict of interest.
Patients are often particularly vulnerable in this type of research, as they may not fully understand their legal or ethical rights (Sankar et al., 2003). We were cognisant of this when considering our research design. To maintain confidentiality of patients, we de-identified patient details, using a numbering system and only referred to patients by their number code to minimise release of personal medical information.
We established that the dramaturgical approach was able to feasibly capture both verbal and non-verbal elements of the discourse. To capture this wide range of information, we used multiple methods of data collection creating greater accuracy of the handover. Other studies have used different research approaches. Using grounded theory and content analysis, Behara et al. (2005) studied five North American Emergency Departments using ethnographic observations, and emphasised the active participation of handover members in co-construction of their understanding about the patients who were considered in the handover. The use of ethnographic observation has some resonance with this study, although, in this study, we created an ‘a priori’ framework for analysis using the dramaturgical components. The dramaturgical method allowed us to structure our analysis. Several researchers (Donnelly et al., 2019; Ooi et al., 2020) have used inductive techniques to analyse semi-structured interview data, and these studies provided useful perceptions of team handovers in New Zealand hospitals. The advantage of using interviews is that professionals interviewed have time to reflect on the salient aspects of the handover; however, a disadvantage is that the interviewees can censor and forget key elements of the process.
B. Functionality
In this section, we address the second research question focussed on describing the functional dynamics of the handover.
We found that dramaturgical methods provided a useful lens to analyse the way the actors and their roles interacted with the staging. For example, the handover was clearly orchestrated by designated and perceived roles of the lead actor (P13) and the major support actor (P3). Our method of utilising VOT allowed us to evaluate the reasons why some actors within the handover participated more or less, with findings clearly showing that the handover was directed by P13, until she left the room and then P3 became the dominant driver of the performance. This finding is consistent with the work of Donnelly, who described the critical nature of the team handover leader’s role in ensuring safe and equitable outcomes for patients by “running meetings smoothly and respectfully” (Donnelly et al., 2019, p. 611).
The interruption caused by the critical case in Scene 9 highlighted the importance of patient safety and care in handover function (Australian Medical Association Limited, 2006), which took priority over ensuring equal voice contribution of the handover attendees. The impact of handover members having differing levels of clinical experience within a team has been noted as an important contributor to handover dynamics (Behara et al., 2005; Hilligoss & Cohen, 2011). We documented a degree of audience segregation (Canary et al., 2008; Murphy, 2009) within the handover, in that, within specific scenes, some actors were markedly involved, whilst others, particularly the bit actors, were effectively the audience and were relatively uninvolved unless prompted by the director or major support actor.
The video analysis permitted us to regard this handover as more akin to an unscripted improvisation (Sawyer, 2004; Schryer et al., 2003) based on the handover sheet. Hilligoss and Cohen (2011, p. 95) have described handovers as “routines grounded in human memory for habits”, and the handover sheet provided a routine document to be worked through. The dramaturgical framework allowed us to visually consider the layout of the room (or stage) (Goffman, 1959; Murphy, 2009). Kinahan (2017), in her qualitative analysis of seating positions within an educational context, reported that different seating positions likely yield different outcomes. The horseshoe-formation structure used in this handover likely promoted more participant engagement.
Lastly, the dramaturgical approach allowed us to segment the analysis in terms of acts and scenes (Henderson, 2005). This was useful as it allowed us to determine if there were specific activity patterns or key events arising within this handover. Hilligoss and Cohen (2011, p. 95) stated that research “examines how micro patterns of activity in [handover] are embedded in, shaped by, and ultimately produce effects on the larger system of hospital activities”. The handover had a prologue in which members had a brief period of social contact, an important element of handover (Hilligoss & Cohen, 2011; Nugus et al., 2017) which initiates formalising the community of practice (Bradley et al., 2018; Egan & Jaye, 2009).
The functionality of the dramaturgical approach can be easily demonstrated within Acts 2 and 3. Act 2 centred on discussion regarding two patients who presented diagnostic uncertainty, and provided the platform for opportunistic teaching, with significant emphasis and time spent on these patients. However, it was clear from our analysis that these teaching moments resulted in a single focus when all team members were effectively engaged through use of directed questioning. The importance of learning within handover has been described (Hilligoss & Cohen, 2011; Ooi et al., 2020; Paradis & Sutkin, 2017). Specifically, the use of brief opportunistic learning related to appropriate patients has been suggested as a useful strategy within handover (Bradley et al., 2018; Ooi et al., 2020). Nonetheless, it was unclear to the researchers whether the teaching initiatives seen in this handover represent typical behaviour, or whether participant activity may have been influenced by the study itself (Paradis & Sutkin, 2017). Act 2 revealed a subsequent shift from a focus on education to patient care, demonstrating that patients continued to receive emergency treatment when required. This reflected an understanding that the participation of the team at handover did not compromise the ongoing provision of medical care for other patients (Australian Medical Association Limited, 2006).
A further change in focus was observed in Act 3, with a focus on the requirement to discuss briefly the remaining 28 patients on the sheet. Our analysis demonstrated a shift to much briefer discussions, reflecting the need to work in a timely manner. This suggested a shift in the handover from a community of practice with at least partly an educational focus to that of a formal work group (Egan & Jaye, 2009; Wenger & Snyder, 1999). The need to pace the handover and to balance the conflicting functions has been noted in other studies (Donnelly et al., 2019; Horsky et al., 2015).
C. Quality Appraisal of the Research Methodology
The dramaturgical approach created a formalised structure from which authentic workplace activity could be identified. In comparison to other qualitative methods, the advantages were the rich, untainted data obtained. The findings of semi structured interviews conducted with the participants involved in this handover are published in a further report (Ooi et al., 2020) and builds on other existing findings published to date within other specialties (Donnelly et al., 2019). The findings of the Ooi et al study were informative as they allowed probing, using semi-structured interviews, into the perceptions of the handover participants after the handover had taken place. These findings are useful in the understanding participants’ views on team dynamics, modes of communication, and the opportunities for learning. Similarly using an interview approach to gathering data, Bradley et al. (2018) was able to develop a set of themes that could be used to describe the handover process, namely informal learning (comprising opportunistic learning, implicit learning, and reflective learning) and formal and deliberative learning. Gathering data using the interview approach enables a deliberative process whereby the participants have time to reflect on their educational and clinical experience associated with the handover. Nevertheless, as aforementioned, it also allows participants to censor their thoughts and memories of the handover (Knox & Burkard, 2009) and may not capture the authoritative complexity of what has occurred in a multifaceted meeting. Therefore, the dramaturgical process could be viewed as authentic ‘in the moment’ research whilst an interview perspective is memory driven, retrospective and reflective.
The optimal approach is to use the dramaturgical system to capture the objective evidence of what actually happened in the handover, and then to use interview data to consider how the participants frame their reflections of what happened. Using both systems would be highly informative in terms of illustrating congruity or incongruity between what happened, what participants thought had happened, and participants’ consequential deliberations regarding their educational and clinical experiences. Using both research systems would benefit handovers, as they would complement each other. To gather data from a larger sample source, using a self-report questionnaire may be valuable once the theoretical domains are established. However, it is acknowledged that designing and developing a questionnaire that is fit for purpose takes careful planning and a rigorous research process (Rattray & Jones, 2007).
A major limitation of the dramaturgical approach taken was the presence of the observers, cameras and audio recording devices and the knowledge of being observed. The Hawthorne effect has been noted as an important aspect of studies as it infers that the perception of special attention may influence behaviour (Paradis & Sutkin, 2017). The research team was uncertain whether the strong emphasis within this handover on teaching reflected the usual practice of the paediatricians involved, but acknowledged that some of the handover participants were aware that two of the researchers were involved in previous research in this area (Ooi et al., 2020), which could have contributed to conciliatory behaviour. One further area of concern was conflict of interest or undue influence. The handover we studied occurred within a hospital at which one of the researchers is both Clinical Director and a paediatrician, and where two others are previous or current members of the paediatric team. None of these three doctors was present in the room during the study, but we acknowledge a potential conflict of interest, which could have altered participants’ behaviour. However, we felt that we had instigated safeguards to minimise this influence, such as having two independent observers within the handover and asking an administrator to contact handover participants with regards to participation and consent. In addition, we also believe in the professionalism of the participants as their main concern in the handover was the authentic transfer of patient information to ensure optimal patient care. It is likely that a mixed-methods approach would be the optimal method for describing the explicit and implicit nature of the handover process.
Our system of analysis created a triangulation method drawing information from the video and audio recordings taken from differing angles, the subsequent transcription of the audio recording, and the notes from two independent observers (medical student and medical educationalist). We were also able to collect data on the room layout (Figure 1) and the handover sheet. We found the data from the video source invaluable in identifying which participants were speaking and in detecting dialogue that was not clearly audible from the audio recording. Once the transcript was agreed on, we found analysis of the video sources and the recordings of the two observers critical to understanding the dynamics within the handover. The video allowed us to identify non-verbal behaviours such as the entrances and exits of staff where this was not otherwise referenced in the audio recording. An entire sequence of teaching occurred when one participant used the whiteboard, and this would not have been appreciated from use of the audio source only. Rees et al., 2013) used video and audio recordings to collect data relating to bedside teaching of medical students, but did not use a structured method of analysis; nonetheless, they found the video useful in capturing linguistic and para-linguistic information, although they noted the difficulty in capturing subtle non‐verbal communication (e.g. smiles).
V. CONCLUSION
This feasibility study has demonstrated that a dramaturgical method had immense utility when analysing the complexity of a paediatric handover meeting. A discussion as to its functionality, benefits and limitations is also provided and we believe that this approach has generated a deep understanding of this handover’s dynamics and highlighted key aspects of the handover’s function, with implications for educational and organisational research.
Further studies could be designed relating to the dramaturgical method. These could be directed to other team handovers in either paediatric or other specialties, and in different health systems to broaden the understanding of processes that occur within these complex meetings. Examples of other such meetings are Multi-Disciplinary patient related meetings, ward rounds, radiology meetings and educational meetings such as Grand Rounds and workshops. Further research could be broadened to include semi-structured interviews of handover participants to gain further understanding of handover members’ reactions to the handovers they have participated in.
Notes on Contributors
Stephen Bradly is a consultant paediatrician (MBChB, FRACP, MClinEd), Clinical Lead, Medical Education, Lakes District Health Board, New Zealand. He reviewed the literature, co-designed the study, analysed the transcripts and co-wrote the manuscript.
Aaron Ooi is a registrar and teaching fellow (MBChB, DipPaed, PGDipClinEd), Waikato District Health Board, New Zealand. He reviewed the literature, co-designed the study, analysed the transcripts and co-wrote the manuscript.
Kerry Stafford is a senior house officer (BMBS), Department of Paediatrics, Christchurch Hospital, Canterbury District Health Board, New Zealand. She reviewed the literature, co-designed the study, analysed the transcripts and contributed to the manuscript.
Shuvayon Mukherjee was a fifth year medical student (BSc) at the time of the study, University of Auckland, New Zealand and on clinical attachment at the Department of Paediatrics, Rotorua Hospital, Lakes District Health Board. He reviewed the literature, co-designed the study, conducted the interviews, analysed the transcripts and contributed to the manuscript.
Marcus A. Henning is an associate professor (BA, MA, MBus, PhD), Centre for Medical and Health Sciences Education, University of Auckland, New Zealand. He reviewed the literature, co-designed the study, conducted the interviews, analysed the transcripts and co-wrote the manuscript. He is the corresponding author for this manuscript*.
Ethical Approval
Ethics approval was obtained from the University of Auckland Human Participants Ethics Committee (UAHPEC) on 26 June 2018. The reference protocol number is 121483.
Data Availability
The anonymised data set is available on https://figshare.com/s/2985a2e3047594816d88 Figshare (2020), with URL details below.
Due to the nature of the video and audio recording containing identifying information, these have not been made public. Requests for these can be directed to the corresponding author if required.
Acknowledgement
We wish to thank the participants in the handover that we studied, who graciously allowed our observation of them working hard to provide excellent care for their patients. We are also grateful to Brenda Flood, who efficiently and capably transcribed the handover.
Funding
A grant to meet the cost of transcription was received from the Stolwyk Trust, Lakes District Health Board.
Declaration of Interest
The authors declare no conflicts of interest.
References
Arora, V., Johnson, J., Lovinger, D., Humphrey, H., & Meltzer, D. (2005). Communication failures in patient sign-out and suggestions for improvement: A critical incident analysis. BMJ Quality & Safety, 14(6), 401-407. https://doi.org/10.1136/qshc.2005.015107
Australian Medical Association Limited. (2006). Safe handover: Safe patients. Guidance on clinical handover for clinicians and managers. http://ama.com.au/sites/default/files/documents/Clinical_Handover_0.pdf
Behara, R., Wears, R. L., Perry, S. J., Eisenberg, E., Murphy, L., Vanderhoef, M., Shapiro, M., Beach, C., Croskerry, P., & Cosby, K. (2005). A conceptual framework for studying the safety of transitions in emergency care. In K. Henricksen, J. Balttles, & E. Marks (Eds.), Advances in patient safety: From research to implementation (Vol. 2, pp. 309-321). Agency for Healthcare Research and Quality.
Bomba, D. T., & Prakash, R. (2005). A description of handover processes in an Australian public hospital. Australian Health Review, 29(1), 68-79. https://doi.org/10.1071/AH050068
Bradley, S. K., Egan, J., & Henning, M. A. (2018). Paediatric team handover: A time to learn? New Zealand Medical Journal, 131(1476), 70-80. https://assets-global.website-files.com/5e332a62c703f653182faf47/5e332a62c703f63e992fd3f5_Bradley-FINAL.pdf
Canary, D. J., Cody, M. J., & Manusov, V. L. (2008). Interpersonal communication: A goals based approach. Bedford/St. Martin’s.
Crea, T. (2017). Narrative dramaturgy and sense making in healthcare simulation. In D. Nestel, B. Jolly, M. Kelly, & M. Watson (Eds.), Healthcare Simulation Education: Evidence, Theory and Practice (pp. 54-59). John Wiley and Sons.
DiCicco‐Bloom, B., & Crabtree, B. F. (2006). The qualitative research interview. Medical Education, 40(4), 314-321. https://doi.org/10.1111/j.1365-2929.2006.02418.x
Donnelly, S., Dinesh, D., Dew, K., & Stubbe, M. (2019). The handover room: A qualitative enquiry into the experience of morning clinical handover for acute medical teams. Internal medicine journal, 49(5), 607-614. https://doi.org/10.1111/imj.14142
Egan, T., & Jaye, C. (2009). Communities of clinical practice: The social organization of clinical learning. Health, 13(1), 107-125. https://doi.org/10.1177/1363459308097363
Elo, S., Kääriäinen, M., Kanste, O., Pölkki, T., Utriainen, K., & Kyngäs, H. (2014). Qualitative content analysis: A focus on trustworthiness. SAGE Open, 4(1), 2158244014522633. https://doi.org/10.1177/2158244014522633
Elo, S., & Kyngäs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107-115. https://doi.org/10.1111/j.1365-2648.2007.04569.x
Figshare. (2020). Handover notes – Observer 1 (Anonymised).docx. https://figshare.com/s/2985a2e3047594816d88
Flory, J., & Emanuel, E. (2004). Interventions to improve research participants’ understanding in informed consent for research: A systematic review. Journal of the American Medical Association, 292(13), 1593-1601. https://doi.org/10.1001/jama.292.13.1593
Forde, C. A. (2014). Emergency medicine triage as the intersection of storytelling, decision-making, and dramaturgy. University of South Florida. https://scholarcommons.usf.edu/etd/5354/
Fujikawa, H., Son, D., & Eto, M. (2021). Are residents learners or workers? A historical perspective in Japan. The Asia Pacific Scholar, 6(1), 122-124. https://doi.org/10.29060/TAPS.2021-6-1/PV2339
Goffman, E. (1959). The Presentation of Self in Everyday Life. Anchor Books.
Hays, M. M., & Weinert, C. (2006). A dramaturgical analysis of shift report patterns with cost implications: A case study. Nursing Economics, 24(5), 253.
Henderson, A. (2005). The value of integrating interpretive research approaches in the exposition of healthcare context. Journal of Advanced Nursing, 52(5), 554-560. https://doi.org/10.1111/j.1365-2648.2005.03622.x
Hensher, M., Price, M., & Adomakoh, S. (2006). Referral hospitals. In D. T. Jamison, J. G. Breman, A. R. Measham, G. Alleyne, M. Claeson, D. B. Evans, P. J. Mills, & P. Musgrove (Eds.), Disease control priorities in developing countries (2nd ed., pp. 1229-1243). Oxford University Press.
Hilligoss, B., & Cohen, M. D. (2011). Hospital handoffs as multifunctional situated routines: Implications for researchers and administrators. In L. H. Friedman, J. Goes, & G. T. Savage (Eds.), Biennial review of health care management (Vol. 11, pp. 91-132). Emerald Group Publishing Limited. https://doi.org//10.1108/S1474-8231(2011)0000011008
Horsky, J., Suh, E. H., Sayan, O., & Patel, V. (2015). Uncertainty, case complexity and the content of verbal handoffs at the emergency department. AMIA Annual Symposium Proceedings.
Kinahan, M. P. (2017). Teachers and seating arrangements and assignments: A qualitative study [Doctoral thesis, Northeastern University]. https://repository.library.northeastern.edu/files/neu:cj82q019x/fulltext.pdf
Knox, S., & Burkard, A. W. (2009). Qualitative research interviews. Psychotherapy research, 19(4-5), 566-575. https://doi.org/10.1080/10503300802702105
Murphy, F. (2009). Act, scene, agency: The drama of medical imaging. Radiography, 15(1), 34-39. https://doi.org/10.1016/j.radi.2007.09.006
Nugus, P., McCarthy, S., Holdgate, A., Braithwaite, J., Schoenmakers, A., & Wagner, C. (2017). Packaging patients and handing them over: Communication context and persuasion in the emergency department. Annals of Emergency Medicine, 69(2), 210-217. e212. https://doi.org/10.1016/j.annemergmed.2016.08.456
Ooi, A., Bradley, S., Mukherjee, S., Stafford, K., & Henning, M. A. (2020). Facilitating educational experiences in a paediatric handover: A qualitative case study. Journal of Paediatrics Child Health, 56(9), 1426-1431. https://doi.org/10.1111/jpc.14964
Paradis, E., & Sutkin, G. (2017). Beyond a good story: from hawthorne effect to reactivity in health professions education research. Medical Education, 51(1), 31-39. https://doi.org/10.1111/medu.13122
Preves, S., & Stephenson, D. (2009). The classroom as stage: Impression management in collaborative teaching. Teaching Sociology, 37(3), 245-256. https://doi.org/10.1177/0092055X0903700303
Rattray, J., & Jones, M. C. (2007). Essential elements of questionnaire design and development. Journal of Clinical Nursing, 16(2), 234-243. https://doi.org/10.1111/j.1365-2702.2006.01573.x
Rees, C. E., Ajjawi, R., & Monrouxe, L. V. (2013). The construction of power in family medicine bedside teaching: A video observation study. Medical Education, 47(2), 154-165. https://doi.org/10.1111/medu.12055
Sankar, P., Mora, S., Merz, J. F., & Jones, N. L. (2003). Patient perspectives of medical confidentiality: A review of the literature. Journal of General Internal Medicine, 18(8), 659-669. https://doi.org/10.1046/j.1525-1497.2003.20823.x
Sawyer, R. K. (2004). Creative teaching: Collaborative discussion as disciplined improvisation. Educational Researcher, 33(2), 12-20. https://doi.org/10.3102/0013189X033002012
Schell, H. (2016). Casting revealed: A guide for film directors. Routledge.
Schryer, C. F., Lingard, L., Spafford, M., & Garwood, K. (2003). Structure and agency in medical case presentations. In B. C & R. D (Eds.), Writing selves/writing societies: Research from activity perspectives (pp. 62-96). The WAC Clearing House. https://wac.colostate.edu/books/selves_societies/schryer/schryer.pdf
Wenger, E. C., & Snyder, W. M. (2000). Communities of practice: The organizational frontier. Retrieved June 22, 2019, from https://hbr.org/2000/01/communities-of-practice-the-organizational-frontier
*Marcus A. Henning
The University of Auckland,
Private Bag 92019,
Auckland 1142,
New Zealand,
Contact No: 0064 923 7392
Email: m.henning@auckland.ac.nz
Submitted: 17 October 2020
Accepted: 12 April 2021
Published online: 5 October, TAPS 2021, 6(4), 26-36
https://doi.org/10.29060/TAPS.2021-6-4/OA2420
Chee Yang Chin1, Si Qi Tan2, Swee Leng Kui1,2, Kurugulasigamoney Gunasegaran1 & Jill Cheng Sim Lee3
1Department of Cardiovascular Medicine, National Heart Centre Singapore, Singapore; 2Ministry of Health Holdings, Singapore; 3Department of Obstetrics and Gynaecology, KK Women’s and Children’s Hospital, Singapore
Abstract
Introduction: Sleep deprivation impacts clinical performance. However, literature is conflicting, with insufficient focus on patient outcomes. The aim of this study was to assess if patient satisfaction and prescription errors in outpatient clinics were adversely affected when consulting post-call versus non-post-call registrars.
Methods: This prospective, quantitative study was set in a large teaching hospital in Singapore. Between November 2015 and February 2016, patients from clinics run by a registrar after 24-hour shift were recruited to post-call group. Patients from non-post-call clinics run by the same registrar were controls. Outcome measures were patient satisfaction, using 5-item 4-point Likert scale questionnaire, and prescribing error rate, defined as number of errors over number of orders. Differences were analysed using chi-squared test.
Results: 103 of 106 (97%) patients in 9 post-call clinics and 93 of 105 (90%) patients in 9 non-post-call clinics were recruited. Questionnaire completion rate was 99%. 536 and 526 prescriptions were ordered in post-call and non-post-call groups, respectively. Percentage of top-box responses (greatest satisfaction) was higher in post-call group overall (79.3% versus 62.4%, p<0.001), and for each questionnaire item. There was no significant difference in prescribing errors (1.31% versus 2.28%, p=0.23).
Conclusion: Patient satisfaction and prescribing error rates in outpatient clinics were not detrimentally affected. This provides some objective evidence that patients may safely consult post-call registrars. True impacts of sleep deprivation remain poorly understood, and larger, longer term, multicentre studies would inform generalisability. Qualitative studies of fatigue may shed light on complex interactions of emotions that compensate for tiredness.
Practice Highlights
- Studies of sleep deprivation and work-hour restrictions are conflicting, with few on patient outcome.
- We compared patient satisfaction and prescribing errors of clinics post-call, versus non-post-call.
- We demonstrate quantitative evidence that patients may safely consult post-call registrars in clinic.
- Impairment may be mitigated by adaptive effort to be conscientious and post call euphoria.
- No recommendations were made to change the current practice of registrars running post-call clinics.
I. INTRODUCTION
Sleep deprivation and fatigue are thought to have detrimental effects on trainee doctors’ performance. It was previously shown that the Epworth Sleepiness Scale score in junior doctors was equivalent to that of patients with sleep apnoea and narcolepsy (Mustafa et al., 2005). Indeed, cognitive psychomotor performance after 24 hours of sustained wakefulness was found to be equivalent to a blood alcohol concentration twice the prohibited level of alcohol intoxication (Dawson & Reid, 1997). The performance and safety to practise of fatigued trainee doctors, especially at the end of a long shift, is thus of utmost concern.
Increasing awareness of fatigue-related medical errors has led to reforms in trainee doctor working hours. Work hours were limited by the Accreditation Council for Graduate Medical Education (ACGME) in the USA in 2003 to 80 hours per week, and by the European Working Time Directive (EWTD) in 2009 to 48 hours per week. A subsequent ACGME stipulation in 2017 further restricted work periods to 24 consecutive hours for first‐year residents (Rosenbaum & Lamas, 2012). Still, doubts remain as to the clinical impact of these restrictions (Baldwin et al., 2011; Fletcher et al., 2005). A systematic review of ACGME’s 2011 work hour restrictions found no improvements in patient care or resident well-being, and in fact revealed unintended negative impacts on resident education (Bolster & Rourke, 2015). Indeed, low job satisfaction was found to be associated with a higher rate of attrition from training (Lee et al., 2019). Thus, the optimal working hours and working patterns for trainee doctors remain ill-defined.
Studies on the impact of sleep deprivation and fatigue on trainee doctors’ performance and wellbeing have yielded mixed results. Chronic sleep deprivation was shown to be particularly detrimental to tasks requiring sustained concentration (Bertram, 1988). After an extended night shift, intensive care unit physicians made 36% more serious medical errors (Landrigan et al., 2004), were 61% more likely to suffer a percutaneous injury (Ayas et al., 2006) and 2.3 times more likely to have a motor vehicle collision (Barger et al., 2005). Hostility and anger in trainee doctors were also more prevalent after a night’s sleep loss (Saadat et al., 2016; Samkoff & Jacques, 1991). Cardiologists were particularly prone to sleep deprivation due to frequent call coverage responsibilities, and in a recent 2019 survey of 481 cardiologists, 46% felt work performance hindrance and 8.6% described sleep-deprivation related adverse events (Lobo et al., 2019).
Yet, other studies have not observed a similar impairment of ability amongst fatigued trainee doctors. There were fewer errors in cognitive tests and cardiopulmonary resuscitation (CPR) manoeuvres in residents after on-call duty (Domínguez et al., 2009; Hamui-Sutton et al., 2013), and psychomotor performance and acquisition of laparoscopic and robotic simulator skills in post-call trainee doctors were also found to be no different from non-post-call trainee doctors (Robison et al., 2018; Yi et al., 2013).
Notably, the outcome measures in the vast majority of these published studies were either subjective through interviews with the trainee doctors themselves, which introduces bias in results, or based on performance on robotic surgical simulators, which is not reflective of true patient contact. Few studies focused on actual patient outcome measures.
Trainee doctors (“registrars”) at our institution, a high volume tertiary referral centre for cardiovascular medicine in Singapore, may be expected to run busy outpatient clinics after a 24-hour continuous in-hospital shift. Typically, up to 20 patients are seen within 4 hours in these clinics. Concerns linger regarding the suitability of post-call registrars running these high-intensity clinics, both in terms of psychomotor ability as well as proneness to error.
With the lack of published literature on the impact of fatigue on trainee doctor performance in outpatient clinics, we aimed to study for ourselves whether patient outcomes were adversely affected if they consulted a post-call registrar, versus a non-post-call registrar. To achieve this, we decided on two practical and measurable outcomes: patient satisfaction and prescribing error rates. Quantifying patient satisfaction allowed an assessment of the registrars’ ability to communicate and show empathy despite their fatigued state. Prescribing error rates allowed an objective evaluation of patient safety. Using two very different outcome measures was a means to allow some triangulation of results and to reduce bias.
Our hypothesis was that both patient outcome measures – patient satisfaction and prescribing error rate – would be worse off in the clinics run by registrars when they were post-call versus when they were not post-call.
II. METHODS
A. Study Setting and Population Design
This study was set in a high volume, specialised Cardiology clinic in a large teaching hospital in Singapore. Registrars, who are trainee doctors in the final stages of training prior to specialist accreditation, work overnight in-hospital shifts as part of service and training commitments. “On-call” duties last from 7am to 1pm the following day (30 continuous hours), during which they are responsible for all urgent inpatient and Emergency department Cardiology referrals. “Post-call” refers to the last 6 hours of the continuous 30-hour shift, during which they may be posted to run busy outpatient clinics.
B. Patient Recruitment
Between November 2015 and February 2016, all patients who attended clinics run by a post-call registrar were recruited to the post-call group. Patients who attended clinics run by the same registrar on a non-post-call day were recruited as controls into the non-post-call group. This provided internal control by comparing performances by the same registrar post-call and non-post call. Patients were approached for participation after their clinic consultation so as not to bias the consultation. They were informed of the purpose of the study but not informed whether the registrar they had just consulted was post-call or not, so as not to bias their responses. All patients, whether new or established, were approached.
C. Patient Satisfaction Questionnaire
Patient satisfaction was evaluated using a 5 item questionnaire (Appendix A). These questions were adapted from the Hospital Consumer Assessment of Healthcare Providers And Systems (HCAHPS), a well-established standardised instrument for the measurement of patient perspectives on hospital care (Giordano et al., 2009; Goldstein et al., 2005).
1) During today’s consultation, did the doctor treat you with courtesy and respect?
2) During today’s consultation, did you feel the doctor listened carefully to you?
3) During today’s consultation, were you given the opportunity to ask your questions?
4) During today’s consultation, did the doctor explain things in a way you could understand?
5) How would you rate your overall satisfaction with today’s consultation?
For each item, as per the HCAHPS questionnaire format, patients were asked to rate responses on a 4-point Likert scale. Smiley faces were incorporated to provide visual representations. The questionnaire was in English and Chinese text, which would have been understood by the vast majority of the patient population. Relevant translations in Chinese, Malay or Tamil languages were provided by research assistants for illiterate patients or those who required further clarification, with care not to influence the patients’ responses. Only fully completed questionnaires were included in the data analysis.
D. Prescribing Error Rates
All prescription orders entered electronically were logged. As is standard procedure for our outpatient clinics, all prescriptions are reviewed by the Pharmacy Department prior to dispensing. All suspected prescription errors will be verified via a phone call to the prescribing doctor, who will confirm whether that prescription was intended or if it truly was an error. All verified prescription errors, including medication name, dose or frequency, or omission of a necessary drug, were recorded regardless of severity. The Pharmacy Department conducts regular internal audits to ensure that this process is accurate and consistent.
The total number of medications ordered and total number of errors were retrospectively summed. Prescribing error rate was calculated by dividing total number of prescribing errors by total number of medications ordered.
E. Consent and Ethics
In accordance with local Institutional Review Board (IRB) guidelines, the study protocol was exempted from full IRB review as it was non-interventional and intended primarily for medical education. All recruited patients provided informed consent to participate. All data were anonymised, with no personal identifiers recorded.
F. Data Analysis
For the patient satisfaction questionnaire, the “top-box” response was defined as the most positive response on the Likert scale (for example “all of the time” or “very satisfied”). The proportions of “top-box” responses were calculated and reported for each questionnaire item and overall items. Only “top-box” responses were sought, to target a higher quality of performance.
For both patient satisfaction and prescribing error outcomes, comparisons between post-call and non-post-call groups were tested for statistical significance with p<0.05 using the chi-squared test. All statistical analyses were reviewed by a biostatistician.
III. RESULTS
The recruitment period consisted of 9 outpatient clinics run by 8 post-call registrars. Two of these clinics were run by the same registrar who was post-call on separate days. We then identified a further 9 clinics run by the same registrars during days when they were not post-call. Thus, 7 registrars had one post-call clinic and one non-post-call clinic studied, while 1 registrar had two post-call clinics and two non-post-call clinics studied.
All patients seen were invited to participate. 103 of 106 (97%) patients in the post-call group and 93 of 105 (90%) in the non-post-call group consented. The number of patients seen per clinic ranged from 7 to 20 (median 11) in the post-call group, and 7 to 17 (median 10) in the non-post-call group.
Basic demographic data on the registrars and the distribution of patients in these clinics were summarised in Table 1.
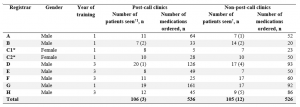
Table 1: Basic demographic data of registrars and distribution of patients seen and number of medications ordered per clinic.
Note: [1] †Numbers in brackets indicate number of patients who declined participation. *C1 and C2 refer to the same registrar, who had 2 post-call and 2 non-post-call clinics from whom patients were recruited for the study.
A. Patient Satisfaction Questionnaire
Questionnaire completion rate was 99% in both groups. Percentages of top-box responses were higher in the post-call group as compared with non-post-call group for item 1 (86% versus 65%, p<0.001), item 2 (82% versus 64%, p=0.003), item 3 (81% versus 65%, p=0.012) and item 4 (79% versus 63%, p=0.01). There was no statistical difference in the percentage of top-box responses for item 5 (64% versus 54%, p=0.184). Overall, percentage of top-box responses was higher in the post-call group compared to non-post-call group (79.3% versus 62.4%, p<0.001).
Percentages of top-box responses for each questionnaire item were illustrated in Figure 1. Individual registrars’ ratings were shown in Appendix B.
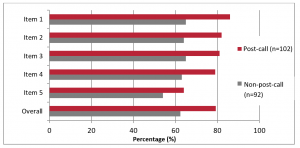
Figure 1: Summary of patient questionnaire responses according to registrars’ post-call status. Questionnaire items were shown on the y-axis and percentage of top-box responses were shown on the x-axis.
B. Prescribing Error Rates
536 and 526 medications were ordered in the post-call and non-post-call group respectively. Seven prescribing errors were made in the post-call group and 12 in the non-post-call group (Table 2).
Overall, there was no significant difference in prescribing error rates (1.31% versus 2.28%, p=0.231).

Table 2: Distribution of medications ordered and prescribing errors made according to registrar.
IV. DISCUSSION
To our knowledge, this is one of very few studies on post-call trainee doctor performance in the context of a realistic outpatient setting, centred on patient outcomes. In our study, the results of both patient satisfaction and prescription errors were congruent in demonstrating that these measurable patient outcomes were not adversely affected when patients were seen by a post-call registrar in an outpatient clinic setting.
A. Patient Satisfaction
Patient satisfaction is an important measure as it demonstrates a doctor’s ability to communicate, which is a key element of any patient-doctor encounter. Fatigue leading to increased stress levels and hostility could have negatively influenced this.
In our study, rather than create a novel and unvalidated questionnaire, we adapted the HCAHPS, a well-established standardised instrument for the measurement of patient perspectives on hospital care (Giordano et al., 2009; Goldstein et al., 2005). As per HCAHPS, only the proportions of top-box responses (i.e., the percentage of patients who rated a particular questionnaire item the most positively) were taken into account in the analysis. This was a means of assessing and aiming for the highest quality of care possible.
The results from overall and individual item top-box responses in our questionnaire demonstrated that patient satisfaction was statistically significantly (p-value <0.001) higher in the post-call group. Indeed, 6 out of 8 registrars had higher percentages of overall top-box responses when post-call, adding consistency to this finding. Nonetheless, given the small cohort of registrars surveyed, there were still the likelihood that this was a chance finding, and previous studies in this area had shown only subtle differences in patient satisfaction (Hoellein et al., 2004; Liu & Wissow, 2011). The key take away point was that patient satisfaction in our study was not adversely affected when patients saw a post-call registrar.
There were two other studies examining post-call trainee doctors in outpatient clinics. In Liu and Wissow’s study (2011), 170 pre-recorded paediatric clinic consultations were analysed to reveal that parents were twice as likely to request a post-call doctor to repeat explanations, both post-call doctors and parents used paraphrasing more frequently to check that they understood each other, and trainee doctors were perceived as less willing to help the patient accomplish their goals during the visit. This suggested that communication was less effective when trainee doctors were post-call. The earlier study by Hoellein et al. (2004), using a 7-item 10-point Likert scale questionnaire, found that patients were significantly less satisfied (mean score 8.99) when seen by a post-call trainee doctor than when seen by a non-post-call trainee doctor (mean score 9.31). Differences in study design and clinic setup could explain the discrepancy between our findings and those of these 2 previous studies. In these 2 studies, patient volume was low at 3 to 7 per clinic, trainee doctors and patients were aware that they were being recorded, and some clinics surveyed were the trainee doctors’ “continuity clinics” where visits were more likely returning patients with already established rapport. In our clinic setting, patient volumes were higher, patients were only approached after the consultation, and none of the clinics were “continuity clinics”.
Another possible explanation for the lack of reduction in patient satisfaction in our study was the phenomenon of “post-call euphoria”, where trainee doctors experience an upbeat mood associated with being able to look forward to the end of a long 30-hour shift and finishing work earlier than usual, at 1 p.m. instead of at 6 p.m. They may be emotionally less stressed in clinic than if they had a long day of work ahead, particularly if they were just starting an on-call shift. In Liu and Wissow’s study (2011), trainee doctors reported more anxiety and frustration when running morning clinics when they still had the rest of the day’s work ahead of them. Additionally, they described themselves as tired, but not more unhappy, when they were post-call as opposed to when they had left on time the day before. Furthermore, post-call trainee doctors made attempts to cope with their fatigue, adaptively or maladaptively, and were seemingly able to compensate for compromised abilities. This counter-intuitive psychological effect warrants further study.
B. Prescribing Error Rates
Prescribing errors were evaluated as a marker of patient safety. Errors have been shown to be provoked by situations of high workload, stress and fatigue (Keers et al., 2013; Tully et al., 2009). Overall case volume in particular was associated with increased rate of major diagnostic discrepancies for junior residents (Hanna et al., 2016), which is relevant to our high-volume clinic setting. The questionnaire among anaesthesiologists from Santa Catarina by Erdmann et al. (2016) revealed that most respondents committed more than one error in drug administration, with distraction and fatigue being the highest contributing factor of 64.9%. Interns made substantially more serious medical errors in the intensive care unit when they worked frequent shifts of 24 hours or more, than when they worked shorter shifts (Landrigan et al., 2004). There was only one other study that dealt specifically with medication errors in the post-call setting. In a retrospective study of 8,195 inpatient prescriptions, trainee doctors were found to be significantly more likely to commit an error on-call and post-call, than when they were off-call, by 2.16%, with odds ratio 1.44 (Hendey et al., 2005).
Our study in the outpatient setting revealed no statistically significant difference in prescribing error rates between patients who had seen a post-call registrar (1.31%) and those who had seen a non-post-call registrar (2.28%) across 536 and 526 prescriptions respectively. The overall prescribing error rate seen in our study was comparable to that of Hendey et al. (2005) (1.79% versus 2.16%, respectively), supporting the validity of our results. Importantly, prescribing error rates were low in both groups, providing reassurance for patient safety.
Previous studies on the impact of fatigue on clinical performance show mixed results. Surgical trainees awake the previous night made 20% more errors in stimulators (Taffinder et al., 1998). Gastroenterologists who performed emergent procedures the previous night had a significant 24% decrease in adenoma detection rates on colonoscopies performed post-call (Benson et al., 2014). While long work hours may contribute to mistakes, the lack of supervision, faulty handovers and large patient caseloads were important factors that further compounded these errors.
Yet, other studies have observed that performance was no worse amongst fatigued trainee doctors. Yi et al. (2013) found no significant difference in psychomotor performance of general surgery residents performing laparoscopic simulator tasks after a 24-hour call work shift versus a 12-hour night-float shift. Robison et al. (2018) reported no significant difference in acquisition of robotic simulator skills between pre-call and post-call general surgery residents despite higher levels of fatigue, and Domínguez et al. (2009) and Hamui-Sutton et al. (2013) observed fewer errors in cognitive tests and CPR manoeuvres in residents after on-call duty. This paradox of improved execution might be explained by an increased motivation to execute tasks as efficiently as possible, even if cognitive processes were theoretically impaired by sleep deprivation (Ayas et al., 2006; Barger et al., 2005; Taffinder et al., 1998).
Additionally, it was postulated that alertness and task performance were impaired immediately in the first 2 hours of awakening due to sleep inertia, but these detrimental effects dissipate with time (Jewett et al., 1999). Post-call residents in our study might therefore have had a chance to recover by the time clinic started.
C. Strengths and Limitations
A particular strength of our study was that registrars who had post-call clinics surveyed also had a non-post-call clinic surveyed. This enabled them to act as controls for themselves and reduced potential bias that may be introduced as a result of differences in registrar demographics, such as age, gender and training experience. Second, there was a high patient participation rate in both the post-call group (97%) and non-post-call group (90%), with a high questionnaire return rate (99% in both groups). This increased the validity of our findings. Third, our study measured two different patient outcomes as a means of triangulation, and both were congruent in showing better outcomes in the post-call group. Fourth, we approached patients for their participation only after their clinic consultation, so as not to have influenced their interaction with the doctor. Fifth, patients were not informed if the registrar that they had just consulted was post-call or not, so as not to influence their questionnaire responses.
Nonetheless, being a single-centre study, caution should be exercised when attempting to generalise these findings to other healthcare settings. Second, only 8 of 18 eligible registrars in the department had clinics surveyed during the study period; thus the findings may not be reflective of the entire cohort. Third, there may have been factors outside the doctor-patient encounter that affected overall patient satisfaction, such as waiting times. Fourth, we did not quantify how busy each registrar’s on-call shift was and what amount of rest they obtained; the results might have been influenced by the amount of rest obtained. Fifth, we could not control for the complexity of the patients seen in the clinics; it is perceivable that a clinic with more straightforward patients would have been more easily managed by a fatigued registrar and vice versa.
For future studies, increasing cohort size of registrars over a longer period of time, and at more categories of call status (such as post-call, on-call and neither post- nor on-call) could improve the generalisability of the findings and reveal influences of call status on performance. In addition, incorporating qualitative data on registrars’ emotions and perceptions of their own performances in clinic would improve understanding of potential factors that may influence performance.
V. CONCLUSION
Our study showed that patient satisfaction and prescription error rates were not adversely affected when patients consulted a post-call registrar versus a non-post-call registrar in an outpatient clinic. This provides reassurance that the current practice of post-call trainee doctors running clinics is not harmful to patients. Complex interactions of associated positive and negative emotional factors could possibly compensate for any physical and mental tiredness. Impairment may be mitigated by adaptive effort to be conscientious. In our institution, no recommendations were made to change the current practice of registrars running post-call clinics. Ultimately, the relationship between being post-call with physician performance and patient outcomes remains poorly understood.
Notes on Contributors
Dr. Chin Chee Yang is a Consultant in Cardiology at the National Heart Centre Singapore and Clinical Assistant Professor at Duke-NUS Medical School. He has a Master of Science in Clinical Education. CCY designed and directed the study, implemented the research, data analysis and writing of the manuscript.
Dr. Tan Si Qi is a Medical Officer with the Ministry of Health Holdings, Singapore. TSQ contributed to the data analysis and writing of the manuscript.
Dr. Kui Swee Leng is a senior resident in Cardiology at Singhealth. She is an Adjunct Research Fellow with Singhealth Duke-NUS Cardiovascular Sciences Academic Clinical Programme (ACP) and Singhealth Associate in Education. KSL contributed to design and implementation of the research.
Assistant Professor Kurugulasigamoney Gunasegaran is a Senior Consultant at the National Heart Centre Singapore. KG contributed to the design and overall supervision of the research.
Dr. Jill Cheng Sim Lee is a Consultant in Obstetrics and Gynaecology and Associate Programme Director to the SingHealth Obstetrics and Gynaecology Residency Programme. She has a Master of Science in Clinical Education. JCSL contributed to the design of the research and writing of the manuscript.
All authors have read and approved the final manuscript.
Ethical Approval
The study was categorised as an educational study hence formal Institutional Board Review (IRB) was exempted. We have attached the Local IRB Exception waiver document.
Funding
No funding source was utilised in this study.
Declaration of Interest
Authors report no declaration of interest.
Data Availability
In our study, all raw data from questionnaires was collected on hard copies and not scanned into a repository. All other data are presented in the direct manuscript.
References
Ayas, N. T., Barger, L. K., Cade, B. E., Hashimoto, D. M., Rosner, B., Cronin, J. W., Speizer, F. E., & Czeisler, C. A. (2006). Extended work duration and the risk of self-reported percutaneous injuries in interns. Journal of the American Medical Association, 296(9), 1055–1062. https://doi.org/10.1001/jama.296.9.1055
Baldwin, K., Namdari, S., Donegan, D., Kamath, A. F., & Mehta, S. (2011). Early effects of resident work-hour restrictions on patient safety: A Systematic review and plea for improved studies. The Journal of Bone and Joint Surgery-American Volume, 93(2), e5(1)-e5(9). https://doi.org/10.2106/JBJS.J.00367
Barger, L. K., Cade, B. E., Ayas, N. T., Cronin, J. W., Rosner, B., Speizer, F. E., & Czeisler, C. A. (2005). Extended work shifts and the risk of motor vehicle crashes among interns. New England Journal of Medicine, 352(2), 125–134. https://doi.org/10.1056/NEJMoa041401
Benson, M., Grimes, I., Gopal, D., Reichelderfer, M., Soni, A., Benson, H., Austin, K., & Pfau, P. (2014). Influence of previous night call and sleep deprivation on screening colonoscopy quality. The American Journal of Gastroenterology, 109(8), 1133–1137. https://doi.org/10.1038/ajg.2014.28
Bertram, D. A. (1988). Characteristics of shifts and second-year resident performance in an emergency department. New York State Journal of Medicine, 88(1), 10–14.
Bolster, L., & Rourke, L. (2015). The Effect of Restricting Residents’ Duty hours on patient safety, resident well-being, and resident education: An updated systematic review. Journal of Graduate Medical Education, 7(3), 349–363. https://doi.org/10.4300/JGME-D-14-00612.1
Dawson, D., & Reid, K. (1997). Fatigue, alcohol and performance impairment. Nature, 388(6639), 235–235. https://doi.org/10.1038/40775
Domínguez, P., Grosso, M. L., Pagotto, B., Taliercio, V., & Allegri, R. (2009). Efectos de la privación de sueño en el desempeño de los médicos residentes de pediatría [Effects of sleep deprivation on medical performance of pediatric residents]. Archivos Argentinos De Pediatria, 107(3), 241–245.
Erdmann, T. R., Garcia, J. H. S., Loureiro, M. L., Monteiro, M. P., & Brunharo, G. M. (2016). Profile of drug administration errors in anesthesia among anesthesiologists from Santa Catarina. Brazilian Journal of Anesthesiology (Elsevier), 66(1), 105–110. https://doi.org/10.1016/j.bjane.2014.06.011
Fletcher, K. E., Underwood, W., Davis, S. Q., Mangrulkar, R. S., McMahon, L. F., & Saint, S. (2005). Effects of work hour reduction on residents’ lives: A systematic review. Journal of the American Medical Association, 294(9), 1088–1100. https://doi.org/10.1001/jama.294.9.1088
Giordano, L. A., Elliott, M. N., Goldstein, E., Lehrman, W. G., & Spencer, P. A. (2009). Development, implementation, and public reporting of the HCAHPS survey. Medical Care Research and Review, 67(1), 27–37. https://doi.org/10.1177/1077558709341065
Goldstein, E., Farquhar, M., Crofton, C., Darby, C., & Garfinkel, S. (2005). Measuring hospital care from the patients’ perspective: An overview of the CAHPS® hospital survey development process: Measuring hospital care from the patients’ perspective. Health Services Research, 40(6p2), 1977–1995. https://doi.org/10.1111/j.1475-6773.2005.00477.x
Hamui-Sutton, L., Barragán-Pérez, V., Fuentes-García, R., Monsalvo-Obregón, E. C., & Fouilloux-Morales, C. (2013). Efectos de la privación de sueño en las habilidades cognitivas, psicomotoras y su relación con las características personales de los médicos residentes [Sleep deprivation effects on cognitive, psychomotor skills and its relationship with personal characteristics of resident doctors]. Cirugia Y Cirujanos, 81(4), 317–327.
Hanna, T. N., Loehfelm, T., Khosa, F., Rohatgi, S., & Johnson, J. (2016). Overnight shift work: factors contributing to diagnostic discrepancies. Emergency Radiology, 23(1), 41-47. https://doi.org/10.1007/s10140-015-1355-0
Hendey, G. W., Barth, B. E., & Soliz, T. (2005). Overnight and postcall errors in medication orders. Academic Emergency Medicine, 12(7), 629–634. https://doi.org/10.1197/j.aem.2005.02.009
Hoellein, A. R., Feddock, C. A., Griffith, C. H., Wilson, J. F., Barnett, D. R., Bass, P. F., & Caudill, T. S. (2004). Are continuity clinic patients less satisfied when the resident is postcall? Journal of General Internal Medicine, 19(5p2), 562–565. https://doi.org/10.1111/j.1525-1497.2004.30165.x
Jewett, M. E., Wyatt, J. K., Ritz-De Cecco, A., Khalsa, S. B., Dijk, D. J., & Czeisler, C. A. (1999). Time course of sleep inertia dissipation in human performance and alertness. Journal of Sleep Research, 8(1), 1–8. https://doi.org/10.1111/j.1365-2869.1999.00128.x
Keers, R. N., Williams, S. D., Cooke, J., & Ashcroft, D. M. (2013). Prevalence and nature of medication administration errors in health care settings: A Systematic review of direct observational evidence. Annals of Pharmacotherapy, 47(2), 237–256. https://doi.org/10.1345/aph.1R147
Landrigan, C. P., Rothschild, J. M., Cronin, J. W., Kaushal, R., Burdick, E., Katz, J. T., Lilly, C. M., Stone, P. H., Lockley, S. W., Bates, D. W., & Czeisler, C. A. (2004). Effect of reducing interns’ work hours on serious medical errors in intensive care units. New England Journal of Medicine, 351(18), 1838–1848. https://doi.org/10.1056/NEJMoa041406
Lee, J. C. S., Kee, X. L. J., Wiener-Ogilvie, S., Chern, B. S. M., & Chin, C. Y. (2019). What drives attrition amongst obstetrics and gynaecology residents in Singapore. The Asia Pacific Scholar, 4(1), 34–41. https://doi.org/10.29060/TAPS.2019-4-1/OA2005
Liu, C.-C., & Wissow, L. (2011). How post-call resident doctors perform, feel and are perceived in out-patient clinics: Post-call residents seeing outpatients. Medical Education, 45(7), 669–677. https://doi.org/10.1111/j.1365-2923.2010.03912.x
Lobo, A. S., Sandoval, Y., Burke, M. N., Sorajja, P., Mooney, M., Traverse, J., Henry, T. D., Chavez, I., Gössl, M., Lips, D. L., Bradley, S. M., Poulose, A., Wang, Y., & Brilakis, E. S. (2019). Sleep deprivation in cardiology: A multidisciplinary survey. The Journal of Invasive Cardiology, 31(6), 195–198.
Mustafa, M., Erokwu, N., Ebose, I., & Strohl, K. (2005). Sleep problems and the risk for sleep disorders in an outpatient veteran population. Sleep and Breathing, 9(2), 57–63. https://doi.org/10.1007/s11325-005-0016-z
Robison, W., Patel, S. K., Mehta, A., Senkowski, T., Allen, J., Shaw, E., & Senkowski, C. K. (2018). Can fatigue affect acquisition of new surgical skills? A prospective trial of pre- and post-call general surgery residents using the da Vinci surgical skills simulator. Surgical Endoscopy, 32(3), 1389–1396. https://doi.org/10.1007/s00464-017-5820-6
Rosenbaum, L., & Lamas, D. (2012). Residents’ Duty hours — Toward an empirical narrative. New England Journal of Medicine, 367(21), 2044–2049. https://doi.org/10.1056/NEJMsr1210160
Saadat, H., Bissonnette, B., Tumin, D., Thung, A., Rice, J., Barry, N., & Tobias, J. (2016). Time to talk about work-hour impact on anesthesiologists: The effects of sleep deprivation on Profile of Mood States and cognitive tasks. Pediatric Anesthesia, 26(1), 66–71. https://doi.org/10.1111/pan.12809
Samkoff, J. S., & Jacques, C. H. (1991). A review of studies concerning effects of sleep deprivation and fatigue on residents’ performance. Academic Medicine, 66(11), 687–693. https://doi.org/10.1097/00001888-199111000-00013
Taffinder, N., McManus, I., Gul, Y., Russell, R., & Darzi, A. (1998). Effect of sleep deprivation on surgeons’ dexterity on laparoscopy simulator. The Lancet, 352(9135), 1191. https://doi.org/10.1016/S0140-6736(98)00034-8
Tully, M. P., Ashcroft, D. M., Dornan, T., Lewis, P. J., Taylor, D., & Wass, V. (2009). The causes of and factors associated with prescribing errors in hospital inpatients: A Systematic Review. Drug Safety, 32(10), 819–836. https://doi.org/10.2165/11316560-000000000-00000
Yi, W. S., Hafiz, S., & Sava, J. A. (2013). Effects of night-float and 24-h call on resident psychomotor performance. Journal of Surgical Research, 184(1), 49–53. https://doi.org/10.1016/j.jss.2013.03.029
*Chin Chee Yang
National Heart Centre Singapore
5 Hospital Drive, Singapore 169609
Tel: +65 6704 8962
E-mail: chin.chee.yang@singhealth.com.sg
Submitted: 18 October 2020
Accepted: 1 March 2021
Published online: 5 October, TAPS 2021, 6(4), 17-25
https://doi.org/10.29060/TAPS.2021-6-4/OA2418
Xin Rong Goh1, Chee Wai Ku2,4, Rajeswari Kathirvel1,2,4,5 & Kok Hian Tan1,3,4
1Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore; 2Department of Obstetrics and Gynaecology, KK Women’s & Children’s Hospital, Singapore; 3Department of Maternal Fetal Medicine, KK Women’s & Children’s Hospital, Singapore; 4Duke-NUS Medical School, Singapore; 5Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Disease outbreaks (DO) result in unprecedented changes to the healthcare industry with far-reaching implications for medical education. The need to adapt to the fluidity during DO requires the delivery of the clinical medical curriculum to be flexible and effective. There is a lack of well-established guidelines on how medical education should be delivered during DO. This study aimed to explore the efficacy of teleconferencing-based platforms (TBP) as a teaching modality to overcome the challenges of clinical year medical education amidst a global pandemic and possibility of its use when there are no disease outbreaks (NDO).
Methods: A cross-sectional survey amongst 144 undergraduate clinical year students from a medical school in Singapore was conducted from May to June 2020, to explore their perspectives on TBP compared to physical venue-based platforms (PVBP). The survey consisted 5-point Likert scale and open-ended questions. Statistical and thematic analyses were performed.
Results: TBP provides greater convenience in travelling, note-taking and ability to overcome administrative challenges. Students strongly recommended its use in DO and NDO. However, students faced increased distractibility, decreased engagement and ease of raising questions, with a lower efficacy in content delivery. The above is dependent on the type of lessons delivered – clinical skills-based or didactic sessions.
Conclusion: TBP is a promising teaching modality for DO with promising possibility of extending its use to NDO. We propose a tri-faceted approach to target improvement in content delivery on TBP, mainly with measures to target propensity for decreased engagement and increased distractibility and to address the technology-related concerns.
Keywords: Medical Education, Teleconferencing, Teaching Modalities, Medical Students, COVID-19, Disease Outbreaks, Pandemics
Practice Highlights
- TBP was strongly recommended as substitute teaching modality during disease outbreaks.
- Students recommended TBP as a supplement for teaching even when there are no disease outbreaks.
- TBP enabled more convenience in travelling, note-taking and overcoming administrative challenges.
- Decreased engagement and increased distractibility noted when sessions are conducted on TBP.
- TBP can be improved via use of teaching aids and contextualising it to the lesson type.
I. INTRODUCTION
Singapore has experienced the escalation of its Disease Outbreak Response System Condition (DORSCON) status to ‘Orange’ due to COVID-19 outbreak on 7th February 2020. This has had significant implications in multiple sectors of the healthcare industry, including that of medical education (Samarasekera, Goh & Lau, 2020). It called for the rapid remodelling of the delivery of the medical education curriculum during a time when social containment and avoidance of large groups gatherings were enforced (Samarasekera & Gwee, 2021). In particular, to contain and prevent the spread of COVID-19, clinical rotations in healthcare institutions were temporarily suspended during the DORSCON Orange period (Chandratre, 2020; Samarasekera, Goh, Yeo et al., 2020).
Many institutions had since employed teleconferencing-based platforms (TBP) to deliver curriculum (Kanneganti et al., 2020; Srinivasan, 2020). TBP is defined as an avenue of e-learning that is ‘internet and local-networking based’ (Al-Shorbaji et al., 2015), enabling the provision of ‘synchronous’ (Dhir et al., 2017) real time audio-visual online interactions across different locations (Lamba, 2011). The literature exploring the use of TBP during DO is limited. Most studies on TBP focused on its use when there are no disease outbreaks (NDO). They described its facilitation of direct teacher-student engagement with quieter students (Fox, 2004) and raised its comparable effectiveness in fulfilling learning outcomes to traditional face-to-face lectures (Bertsch et al., 2007). TBP nonetheless faces deterrents to its implementation, including those of financial implications (Lim et al., 2009) and technical difficulties (Boatin et al., 2015; Lamba, 2011). During DO, it had helped to overcome concerns of social distancing and allowed the continuation of medical training (Kanneganti et al., 2020; Lim et al., 2009).
In spite of the above, it should be recognised that the temporary suspension of clinical rotations represent the absence of a cornerstone in delivery of the medical curriculum (Govindarajan et al., 2018; Jacobs & Samarasekera, 2012; Lim et al., 2009; Rawekar et al., 2016). This study thus chose to specifically focus on the clinical year students owing to the potential application of these findings to post-graduate clinical trainings. Furthermore, the different content and focus during the pre-clinical years (e.g. lack of clinical rotations, presence of anatomy and science practical) would likely raise concerns that are unique and non-generalisable to students in the clinical years. Pre-clinical students were therefor excluded from the current study.
While the use of TBP is largely commended (Fatani, 2020), it is pertinent to compare its efficacy to traditional physical venues-based platforms (PVBP) as a potential replacement or supplement for the delivery of the clinical curriculum during DO. This study aims to understand the ground-up perspective of clinical year students on TBP as an education tool during DO, as compared to PVBP. It also explored TBP’s suitability and effectiveness for the delivery of the undergraduate medical education when there are no disease outbreaks (NDO).
II. METHODS
A. Ethics Review
The following study was approved by NTU Institutional Review Board (IRB Reference number: 2020-05-003) with an exempt status.
B. Survey Design and Study Population
All undergraduate clinical year medical students from the Lee Kong Chian School of Medicine who had used teleconferencing as a part of their curriculum were invited to participate in an online survey via email and social-messaging platform that included an explanation of the study’s details. Informed consent was implied when the participant accessed the online survey administered via SurveyMonkeyÓ platform. Personal identifiers were not collected.
The cross-sectional survey consisted of a mix of 5-point Likert scale questions and open-ended questions. It was anticipated to be completed in 10 minutes. The questions were designed to evaluate their familiarity with teleconferencing and their opinions on teleconferencing as an educational tool as compared to physical venue-based sessions, e.g. traditional lectures, bedside and small group tutorials, and team-based learning. Their willingness to extend teleconferencing as a supplementary delivery tool for medical education in both DO and NDO situations were also explored.
The survey questions were developed de-novo with reference to the existing literature. The themes of platform accessibility and ease of raising questions were adapted from Al-Neklawy (2017) while that of engagement and distractibility were adapted from the Danielson’s Framework for Teaching – The classroom environment (Alvarez & Anderson-Ketchmark, 2011). The survey was then piloted amongst a group of medical students and faculty to assess content and face validity.
C. Statistical Analysis
Self-reported estimates on the number of prior use of teleconferencing were divided by 52 to determine weekly usage. Numerical values were awarded for the 5-point Likert scale as follows: Strongly agree (5), agree (4), neutral (3), disagree (2) and strongly disagree (1).
Paired 2 tailed T test was performed to determine the significance of difference in subjective efficacy of PVBP and TBP. To compare effect of gender on subjective efficacy for the two platforms and recommendations for TBP, independent T test and Fisher’s exact test were performed respectively. Pearson Correlation testing was performed to look for correlations between the variables. Kruskal-Wallis H test was used to study the effect of year of study on the responses. A p value of < 0.05 indicated statistical significance. Data analysis was performed using SPSSTM software (V.24.0).
D. Qualitative Analysis
Thematic analysis was performed for the elaborations and justifications provided by survey respondents. Concepts that were similar were used to guide the development of themes.
III. RESULTS
A. Sociodemographic Characteristics
A total of 144 out of 315 clinical year medical students completed the survey over a 3-week period from May to June 2020 (Year 3: n = 51; Year 4: n = 64; Year 5: n = 29). The survey response rate was 45.7%. Majority of students who responded were female (58.3%) and Year 4 (44.4%).
B. Teleconferencing Usage Patterns
Majority (73.6%) of students had used a teleconferencing platform, for educational and non-education purposes, in the past year prior to declaration of DORSCON Orange. The top three teleconferencing platforms by corrected mean weekly usage prior to DORSCON orange were Skype© (0.2), FaceTime© (0.2) and ZOOM© (0.1). During DOSRCON orange, the top three platforms for educational purposes by corrected mean weekly usage were ZOOM© (4.0), Skype© (0.3), Facetime© (0.1). (Table 1)
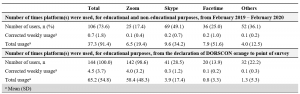
Table 1. Use of teleconferencing-based platforms by medical students
Corrected weekly usage was calculated as follows: (A) Total usage divided by 52, (B) Total usage divided by number of weeks from declaration of DOSRSCON orange to point of survey (For example: 1 week + 1 day would be considered as 2 weeks)
Others included: Whatsapp©, Microsoft Teams©, Google Hangouts©, WebEx©, Discord©, Houseparty©
C. Physical-Venue Based (PVBP) vs Teleconferencing-Based (TBP) Platforms
Students felt PVBP had significant engagement (mean = 4.0) and less distractibility (mean = 2.7). TBP had notable convenience (mean = 4.6), with negligible concerns on its safety (mean = 2.3) on a 5-point Likert scale. (Table 2)
When comparing TBP to PVBP, there was a significant increase in convenience (mean = 4.6 vs 3.8; p <0.001) with TBP. However, this was faced with increased distractibility (mean = 3.7 vs 2.7; p <0.001), decreased engagement (mean = 3.5 vs 4.0; p <0.001), ease of raising questions (mean: 3.4 vs 3.7; p =0.008) and efficacy in the delivery of content (mean: 4.0 vs 3.8; p =0.001). (Table 2)
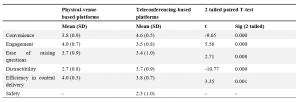
Table 2: Comparison of subjective efficacy of physical venue-based vs teleconferencing based platforms by clinical year medical students surveyed from May to June 2020 on a 5-point Likert Scale
Numerical values were assigned as follows: Strongly disagree (1), Disagree (2), Neutral (3), Agree (4), Strongly agree (5)
D. Correlations Between Responses
Based on Pearson’s correlation, students who were engaged on PVBP, tend to be more comfortable in raising questions (r = 0.301, p <0.001) and less distracted (r = -0.337, p <0.001) with PVBP. Similarly, students who felt engaged on TBP tend to feel comfortable in raising questions on TBP (r = 0.301, p <0.001), less distracted (r = – 0.353, p <0.001) and agree on its efficacy in content delivery (r = 0.570, p <0.001). Students who felt more distracted on PVBP tend to also be more distracted on TBP (r = 0.176, p <0.05). No significant correlations were found between prior teleconferencing experience on self-reported rating of PVBP and TBP.
Kruskal-Wallis H test showed a statistically significant difference in rating of convenience for TBP between different years of study (χ2 (2) = 18.1, p <0.001, mean (Year 3) 87.1, (Year 4) 69.8, (Year 5) 53.0). There were no statistically significant effects of gender on the responses.
E. Recommendations of Teleconferencing Platform
An overwhelming majority of students recommended use of TBP in DO (n = 143, 99.3%), 54.9% (n = 79) recommended it as a substitute, and 44.4% (n = 64) as a supplement for learning, whereas one student did not recommend it at all. A significant proportion continued to favour its use even during NDO (n = 121, 84.0%), although there was a slight shift in preference for it to be used as a supplement (Supplement: n = 108, 75%; Substitute: n = 13, 9.0%). (Table 3A)
There were no statistically significant effects of gender or year of study on the responses.
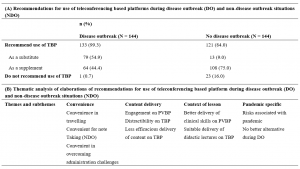
Table 3. Recommendations and suggested improvements for use of teleconferencing platforms during disease and non-disease outbreak situations by clinical year medical students surveyed from May to June 2020
N refers to the total number of elaborations provided for each type of recommendations, of which percentage (%) calculated reflects the percentage of respondents who raised a particular theme in their elaborations. n refers to the number of times the theme appeared per respondent.
Representative elaborations were quoted and tagged by the respondent’s demographic (Recommendation, Year of Study, Gender)
F. Qualitative Analysis
Thematic analyses revealed 10 main areas of discussion. These were categorised into three main themes that were common for both DO and NDO: convenience, content delivery and context of lesson (Table 3B). For the analysis for DO recommendations, a new theme materialised: Pandemic-specific considerations. Suggestions for improvements of TBP mainly fell into 3 categories – enhanced use of TBP teaching aids, ZOOM© fatigue and connectivity and technological concerns.
1) Convenience: Students indicated that TBP reduced their need to travel to teaching destinations, thereby saving on expenditure and time. This was especially useful when they were scheduled with a full day of lectures that did not require any clinical setting training, and during the exam period. For example, one student reported, “I value the time saved on travelling… more than the increased concentration and engagement of a face-to-face tutorial, given that exams are looming.” (Year 4, Female)
The ability to stream these sessions from home was advantageous as students could take additional measures to help sustain their attention, including the ease of taking refreshment breaks. Students valued the ease of taking notes as elaborated by one student as “easier to take screenshots of the slides so we don’t waste time copying the points.” (Year 5, Female)
Students noted TBP to be more convenient in arranging lectures across institutions. Specific to NDO, TBP was suggested as a potential mean to allow “teaching very large groups of people… combined stream classes” (Year 3, Male) and across medical schools. TBP also offered flexible scheduling arrangements. Examples included situations where participants are “feeling unwell but are worried about missing class” (Year 3, Female), “tutors with very busy or unpredictable schedules… which would require students to meet at odd or inconvenient timings” (Year 4, Male), hence minimising need for students to “stay back” (Year 5, Female) in the late evening.
2) Content delivery: Students discussed how triadic interactions between tutors and students, and amongst themselves were better afforded on PVBP. Nuances of social cues like facial expressions were cited as potentially beneficial for tutors to gauge students’ engagements. One student shared that “the tutor can gauge whether or not the content is appropriate based on the body language/facial expressions of the students which may be hard to do so on an online platform.” (Year 5, Female) Students also noted how TBP changed the nature of social interactions, making participants “less likely to speak up or participate… [with] the tutor [feeling] more distant.” (Year 4, Female)
The interactions between students as a reinforcement for learning surfaced as a crucial component. As one student shared, PVBP gave the “chance for the team to meet and learn from each other… quizzing each other, clarifying doubts, or sharing fun facts and important information [that]… cannot be done over teleconferencing.” (Year 3, Female)
Students reported that it was harder to stay focused during TBP sessions as one was in a “more comfortable location with no one monitoring your movements and actions” (Year 3, Male), unable to see the tutor in person and may have concomitant activities surrounding them. The implications of such distractibility were noted that TBP made it easier “to hide away and therefore not be present.” (Year 4, Female)
3) Context of lesson: Students felt their subjective assessment of TBP versus PVBP should factor in the type of lessons being delivered. It was unanimous that clinical-based teachings required use of PVBP to develop soft skills and appreciate clinical signs. To illustrate, one student shared, “medicine is an apprenticeship – there are many skills that cannot be learnt theoretically but must be observed in a clinical setting… Physical sessions are still very important to teach such skills, and should proceed with adequate safety measures in place. Otherwise, we will become doctors with good theoretical knowledge but poor practical/people skills” (Year 5, Female). However, many agreed that didactic lectures which involved pure unidirectional delivery of content could be suitably delivered over TBP as “lecturer… can still speak and present slides as usual.” (Year 3, Male)
4) Pandemic specific considerations: Students acknowledged the risk-benefit ratio of disease transmission and accommodation for the schedule of clinical tutors. One student summarised, “Additional benefits gained through physical venue-based outweighed by risks of disease transmission due to physical interaction.” (Year 3, Male) TBP was hence considered to be a safe and only suitable alternative to ensure continuity of curriculum delivery during DO.
5) Identified areas of improvement: Students raised suggestions to overcome the drawbacks of TBP in 3 main domains. Firstly, they recommended the enhanced used of teaching aids to increase engagement peer-peer interactions. Secondly, they raised the phenomenon of “ZOOM© fatigue” and the need to manage scheduling of tutorials. For example, one student shared, “People seem to think that online lectures are less mentally taxing since you’re at home, and proceed to pack the entire day full of lectures for couple weeks on end… there is no time to consolidate knowledge especially in the absence of opportunity to apply in a clinical setting.” (Year 4, Male) Hence, students suggested tutors to avoid “bombarding students with back-to-back tutorials, leading to information overload” (Year 4, Female) and decrease the maximum time per day to less than 4-5 hours. The inclusion of breaks between sessions as a mental break since tutors who are “swapping in… would not know if students are still engaged or fatigued.” (Year 4, Male)
Lastly, presence of poor connectivity contributed to streaming lags, with negative implications on students “concentration and ability to follow the lecture.” (Year 4, Female) The possibility of increasing tutors’ familiarity with the platform was cited to have facilitated a smoother conduct of lessons.
IV. DISCUSSION
A. Summary of Results
An overwhelming majority of students recommended the continued use of TBP during both DO and NDO. This is most likely due to the increased convenience in travelling, taking down notes, overcoming administrative challenges, and its suitable replacement for didactic lectures. The student’s perception of convenience of TBP correlated to the year of study, with the earlier clinical year students finding it more convenient than the final year students. Nevertheless, this should be evaluated against the background that end users range from enthusiastic ‘technophiles’ to ‘technophobes’, which influences the receptiveness towards e-learning platforms (Bruce, 1997; Fox, 2004).
Specifically during DO, it was viewed to be the best available alternative when considering the disease transmission risk and the busy schedules of the clinical tutors as they may have new responsibilities as front-liners in pandemics (Branch et al., 1997; Cook, 2006; Goh, 2020; Harden & Crosby, 2000; Ramani & Leinster, 2008).
The shift in preference of use of TBP as a substitute to supplement during NDO was noticeable. This can be due to many factors. There is a decreased engagement due to the reduced ability of tutors to assess nuances of social cues (Fox, 2004), greater distractibility and decreased ease of raising questions on TBP. Notably, peer-peer interaction is lost over TBP. Each student’s interaction is multidirectional: student with resource materials, with educator, and between students (Dhir et al., 2017). The value of such interactions and study groups in medical education should be duly taken into consideration (Burgess et al., 2014). Poorer engagement were further compounded by challenges with technology-related concerns and risks of “ZOOM© fatigue”.
Distractibility on TBP could be due to learning in a non-classroom environment (Fox, 2004) with a device that could also be used for non-educational purposes (Walsh, 2015). “ZOOM© fatigue” was likely due to lack of pre-fixed maximal time duration and the tendency for tutors to over-deliver and pile extra study materials (Fox, 2004) causing student’s to “feel tired and restless” (Srinivasan, 2020).
Interestingly, students’ innate personality and learning attitudes potentially influenced their perceptions of PVBP and TBP. Students who were more engaged on a platform, also felt more comfortable raising questions, were less distracted and believed that the platform was efficacious in delivering content. This demonstrates the difference between the “active and engaged learners” and the majority who are “silent lurkers (Fox, 2004). Similarly, students who felt more distracted on PVBP appeared to also be more distracted on TBP.
B. Recommendations
TBP as a teaching modality has an indisputable role during both DO and NDO. It is well-established that medical students experience significant psychological impact during DO (AlAteeq et al., 2020; Ullah & Amin, 2020), possibly related concerns on the impact of their studies (Lyons et al., 2020). Hence with the increased use of TBP, it is imperative that medical educators develop a deeper understanding on the potential short-comings of the platform and how best to maximise its utility as a teaching modality.
Nonetheless, it is vital to recognise that the efficacy of any new education tool depends on both educators and students. It would be better facilitated if the end user is familiar with the platform. It should be considered in light of its application and configuration (Cook, 2006) and ideally be managed and monitored by trained staff (Dhir et al., 2017; Harden, 2018). Moving forward, we recommend a tri-faceted approach to improve the content delivery of TBP during both DO and NDO (Figure 1).

Figure 1. Correlation of domains assessed for efficacy of teleconferencing-based platforms (TBP) with themes identified and suggestions to improve content delivery on TBP
1) Domain 1: Contextual use of TBP: Disease outbreak situations:
- Where physical appreciation of clinical skills through bedside tutorial or real-life clinical interactions might not be feasible, consider use of media and standardised patients to simulate clinical exposure.
- The supplemental use of standardised patients (Peters & Thrien, 2020) hones student’s clinical competence while facilitating the training of relevant skills needed for future practice (Khoo et al., 2020), a notable example in these evolving recent times also includes that of telemedicine (Williams & Song, 2016).
No disease outbreak situations
- TBP should mainly be used for didactic or team-based learning sessions, large group teaching sessions and for students who are unable to physically attend the lecture.
2) Domain 2: Targeting decreased engagement and increased distractibility:
- Use of multi-modal teaching aids, e.g. virtual quizzes, breakout rooms for small group engagement, drawing functions to better visually illustrate explanations.
- Monitoring of students’ current fatigue level in session via live polls at regular hourly intervals.
- Engagement of a central coordinator to regulate the maximum hours of online sessions per day, with considerations of suitable breaks between sessions.
- Prior assessment of student’s learning attitudes and class dynamics to enable tailored use of teaching aids.
3) Domain 3: Smoothening transition to TBP:
- Engagement of central coordinator to brief tutors on the functionality of TBP of choice to minimise technology unfamiliarity and maximise its utility in conducting sessions.
- Educational institutions to consider providing infrastructural support to students and educators, including dedicated spaces, electronic devices with internet connections, and easy access to technical support. These would help minimise network connectivity challenges and providing a conducive study environment for those who might face difficulties accessing TBP off-campus.
- Selective use of TBP as a supplement during NDO to increase both students and educator’s familiarity with the platform and as a learning tool, thereby enabling a smoother transition during DO.
C. Limitations
Our study has few limitations. We surveyed clinical year students from a single medical school and therefore, our study may not reflect the views of students from other medical schools with different teaching pedagogies and those of pre-clinical year students. Future studies should consider exploring the opinions of clinical tutors on PVBP and TBP and their perspective as educators in delivering such curriculum. In addition, given our limited sample size, some statistically significant sub-group patterns may not have been evident.
V. CONCLUSION
TBP is an important teaching modality during DO and NDO, especially with its increased convenience. However, it has certain issues including context-specific use, decreased engagement, increased distractibility and technological challenges. Our proposed potential interventions may help to maximise its utility and facilitate transition of its use in subsequent DO.
Notes on Contributors
Xin Rong Goh designed the study, recruited the participants, administered the survey, analysed the data and wrote the first and subsequent drafts of the manuscript. Rajeswari Kathirvel and Chee Wai Ku contributed to analysis of the data and writing of the manuscript. Kok Hian Tan contributed to the study design and reviewed the manuscript. All authors have read and approved the final manuscript.
Ethical Approval
The following study was approved by NTU Institutional Review Board (IRB Reference number: 2020-05-003) with an exempt status.
Data Availability
The ethical approval by NTU Institutional Review Board was based on the conditions that while the data is deidentified data, only study team members will have access to the raw data that will be stored on a password protected PC. The data could thus not be uploaded on a public data sharing platform.
Acknowledgement
The authors acknowledge Dr Joel Shi Quan Tan, Yong Loo Lin School of Medicine, National University of Singapore, for his contribution to the statistical analysis of the paper.
Funding
No funding sources was used for this research study.
Declaration of Interest
The authors have no conflicts of interest to declare.
References
AlAteeq, D. A., Aljhani, S., & AlEesa, D. (2020). Perceived stress among students in virtual classrooms during the COVID-19 outbreak in KSA. Journal of Taibah University Medical Sciences, 15(5), 398–403. https://doi.org/10.1016/j.jtumed.2020.07.004
Al-Neklawy, A. F. (2017). Online embryology teaching using learning management systems appears to be a successful additional learning tool among Egyptian medical students. Annals of Anatomy, 214, 9–14. https://doi.org/10.1016/j.aanat.2017.07.001
Al-Shorbaji, N., Atun, R., Car, J., Majeed, A., & Wheeler, E. (2015). eLearning health professional for undergraduate education. World Health Organistion. https://www.who.int/hrh/documents/14126-eLearningReport.pdf
Alvarez, M. E., & Anderson-Ketchmark, C. (2011). Danielson’s framework for teaching. Children and Schools, 33(1), 61–63. https://doi.org/10.1093/cs/33.1.61
Bertsch, T. F., Callas, P. W., Rubin, A., Caputo, M. P., & Ricci, M. A. (2007). Applied research: Effectiveness of lectures attended via interactive video conferencing versus in-person in preparing third-year internal medicine clerkship students for clinical practice examinations (CPX). Teaching and Learning in Medicine, 19(1), 4–8. https://doi.org/10.1080/10401330709336616
Boatin, A., Ngonzi, J., Bradford, L., Wylie, B., & Goodman, A. (2015). Teaching by teleconference: A model for distance medical education across two continents HHS public access. Open Journal of Obstetrics and Gynecology, 5(13), 754–761. https://doi.org/10.4236/ojog.2015.513106
Branch, W. T., Kroenke, K., & Levinson, W. (1997). The clinician-educator – Present and future roles. Journal of General Internal Medicine, 12(Suppl. 2), 1–4. https://doi.org/10.1046/j.1525-1497.12.s2.16.x
Bruce, B. C. (1997). Literacy technologies: What stance should we take? Journal of Literacy Research, 29(2), 289–309.
Burgess, A., McGregor, D., & Mellis, C. (2014). Medical students as peer tutors: A systematic review. BMC Medical Education, 14,115. https://doi.org/10.1186/1472-6920-14-115
Chandratre, S. (2020). Medical students and COVID-19: Challenges and supportive strategies. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520935059
Cook, D. A. (2006). Where are we with web-based learning in medical education? Medical Teacher, 28(7), 594–598. https://doi.org/10.1080/01421590601028854
Dhir, S. K., Verma, D., Batta, M., & Mishra, D. (2017). E-learning in medical education in India. Indian Pediatrics, 54(10), 871–877. https://doi.org/10.1007/s13312-017-1152-9
Fatani, T. H. (2020). Student satisfaction with videoconferencing teaching quality during the COVID-19 pandemic. BMC Medical Education, 20(1), 396. https://doi.org/10.1186/s12909-020-02310-2
Fox, R. (2004, December). SARS epidemic: Teachers’ experiences using ICTs. In R. Atkinson., C. McBeath., D. Jonas-Dwyer. & R. Phillips (Eds.), Beyond the comfort zone: Proceedings of the 21st Annual Conference of the Australasian Society for Computers in Learning in Tertiary Education (ASCILITE) (pp. 319-327). Australasian Society for Computers in Learning in Tertiary Education. http://www.ascilite.org.au/conferences/perth04/procs/fox.html
Goh, C. T. (2020, May 3). COVID-19: Guarding against burnout, compassion fatigue and trauma in frontline healthcare workers. Channel News Asia. https://www.channelnewsasia.com/news/singapore/covid-19-guarding-against-burnout-trauma-ttsh-ncid-frontline-12669280
Govindarajan, S., Vasanth, G., Kumar, P. A., Priyadarshini, C., Radhakrishnan, S. S., Kanagaraj, V., Balasubramanian, N., Kumar, P. N., Divya, T. J., & Aishwarya, C. N. (2018). Impact of a comprehensive early clinical exposure program for preclinical year medical students. Health Professions Education, 4(2), 133–138. https://doi.org/10.1016/j.hpe.2017.06.002
Harden, R. M. (2018). Medical teacher E-learning-caged bird or soaring eagle? Medical Teacher, 30(1), 1–4. https://doi.org/10.1080/01421590801938878
Harden, R. M., & Crosby, J. (2000). AMEE guide no 20: The good teacher is more than a lecturer – The twelve roles of the teacher. Medical Teacher, 22(4), 334–347. https://doi.org/10.1080/014215900409429
Jacobs, J. L., & Samarasekera, D. D. (2012). How we put into practice the principles of embedding medical students into healthcare teams. Medical Teacher, 34(12), 1008–1011. https://doi.org/10.3109/0142159X.2012.731097
Kanneganti, A., Sia, C.-H., Ashokka, B., & Ooi, S. B. S. (2020). Continuing medical education during a pandemic: An academic institution’s experience. Postgraduate Medical Journal, 96, 384- 386. https://doi.org/10.1136/postgradmedj-2020-137840
Khoo, S. A., Aswin, W., Shen, G. Q. Y., Haq, H. M., Junaidah, B., Yiew, J. L., Abiramy, M., & Sashikumar, G. (2020). Improving provider-patient communication skills among doctors and nurses in the children’s emergency department. The Asia Pacific Scholar, 5(3), 28–41. https://doi.org/10.29060/TAPS.2020-5-3/OA2160
Lim, E. C. H., Oh, V. M. S., Koh, D. R., & Seet, R. C. S. (2009). The challenges of “continuing medical education” in a pandemic era. Annals of the Academy of Medicine Singapore, 38(8), 724–726.
Lyons, Z., Wilcox, H., Leung, L., & Dearsley, O. (2020). COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australasian Psychiatry, 28(6), 649–652. https://doi.org/10.1177/1039856220947945
Lamba, P. (2011). Teleconferencing in medical education: A useful tool. Australasian Medical Journal, 4(8), 442–447. https://doi.org/10.4066/AMJ.2011.823
Peters, T., & Thrien, C. (2020). The digital use of simulated patients in times of the corona pandemic – Considerations and proposals. GMS Journal for Medical Education, 37(7), Doc 93. https://doi.org/10.3205/zma001386
Ramani, S., & Leinster, S. (2008). AMEE guide no. 34: Teaching in the clinical environment. Medical Teacher, 30(4), 347–364. https://doi.org/10.1080/01421590802061613
Rawekar, A., Jagzape, A., Srivastava, T., & Gotarkar, S. (2016). Skill learning through early clinical exposure: An experience of Indian medical school. Journal of Clinical and Diagnostic Research, 10(1), JC01–JC04. https://doi.org/10.7860/JCDR/2016/17101.7022
Samarasekera, D. D., Goh, D. L. M., & Lau, T. C. (2020). Medical school approach to manage the current COVID-19 crisis. Academic Medicine, 95(8), 1126–1127. https://doi.org/10.1097/ACM.0000000000003425
Samarasekera, D. D., Goh, D. L. M., Yeo, S. P., Ngiam, N. S. P., Aw, M. M., Lim, M. M., Pillai, S., Lee, S. S., Mahadevan, M., Kow, A., Chong, Y. S., & Lau, T. C. (2020). Response and lessons learnt managing the covid-19 crisis by school of medicine, National University of Singapore. MedEdPublish, 9(1), 92, https://doi.org/10.15694/mep.2020.000092.1
Samarasekera, D. D., & Gwee, M. C. E. (2021). Adapting to change during challenging times. The Asia Pacific Scholar, 6(1), 1-2. https://doi.org/10.29060/TAPS.2021-6-1/EV6N1
Srinivasan, D. K. (2020). Medical students’ perceptions and an anatomy teacher’s personal crisis experience using an e-learning platform for tutorials during the Covid-19 crisis. Anatomical Sciences Education, 13(3), 318-319. https://doi.org/10.1002/ase.1970
Ullah, R., & Amin, S. (2020). The psychological impact of COVID-19 on medical students [Letter]. Psychiatry Research, 288, 113020. https://doi.org/10.1016/j.psychres.2020.113020
Walsh, K. (2015). Mobile learning in medical education: Review. Ethiopian Journal of Health Sciences, 25(4), 363–366. https://doi.org/10.4314/ejhs.v25i4.10
Williams, B., & Song, J. J. Y. (2016). Are simulated patients effective in facilitating development of clinical competence for healthcare students? A scoping review. Advances in Simulation (London, England), 1, 6. https://doi.org/10.1186/s41077-016-0006-1
*Goh Xin Rong
11 Mandalay Road,
Singapore 308232
Email: xinronggoh@yahoo.com.sg
Submitted: 26 September 2020
Accepted: 1 March 2021
Published online: 5 October, TAPS 2021, 6(4), 7-16
https://doi.org/10.29060/TAPS.2021-6-4/OA2415
Rasika Manori Jayasinghe1, Indika Priyanthi Thilakumara1, Bandara Dhanushka Leuke2, Gishan Edirisinghe3, Manil Christopher Nishan Fonseka3, Manjula Attygalla4 & Ruwan Duminda Jayasinghe2
1Department of Prosthetic Dentistry, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka; 2Department of Oral Medicine and Periodontology, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka; 3Department of Restorative Dentistry, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka; 4Department of Oral Surgery, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka
Abstract
Introduction: E-learning resulted in a revolution in dental education with continuous educational experiences. General objective of this study was to assess the perspective of undergraduate dental students on effectiveness of e-learning in the Bachelor of Dental Surgery (BDS) programme. Specific objectives were to identify students’ opinion on the factors that promote e-learning, awareness on the effectiveness of using different platforms and social media, barriers imposed and suggestions for the improvement of e-learning in the BDS programme.
Methods: This was a cross sectional descriptive study among undergraduate dental students of the Faculty of Dental Sciences, University of Peradeniya, Sri Lanka using a self-administered pre-tested questionnaire administered via a web-based survey form. Frequencies and percentages were obtained for categorical data and Chi-square test was used to determine the association between variables.
Results: The majority received the e-learning experience well. Fifty-four percent of the participants felt it was better compared to traditional face-to-face learning and the difference between the semesters (p=0.000) and genders was statistically significant (p=0.000). Difference in overall satisfaction on e-learning material across the different semesters was statistically significant. Students felt that e-learning should be used as a supplementary tool mainly by means of procedural videos during delivery of the skill component. Fifty percent participants felt that conducting assessments online is fair for all the students.
Conclusion: A positive learning experience was achieved through the e-learning modalities in comparison to traditional face-to-face learning though in terms of skills training, e-learning modalities should only be considered as a supplementary tool.
Keywords: E-Learning, Perspective, Dental Undergraduates, Dental Education
Practice Highlights
- Majority felt e-learning was better compared to traditional face-to-face learning.
- Majority were satisfied with interactions with teachers and teacher responses to clarifications.
- Students felt that e-learning used as a supplementary tool during delivery of the skill component.
I. INTRODUCTION
E-learning has resulted in a revolutionising dental education to an extent that more interactive and intuitive e-learning options have evolved which provide students with an enjoyable and meaningful continuum to their educational experience. During the current COVID-19 pandemic electronic learning tools have been invaluable in the delivery of knowledge in many higher education institutions (Li & Lalani, 2020). One of the great advantages of e-learning is the possibility of transferring knowledge and skills to a large number of recipients irrespective of the time of delivery of knowledge (Asiry, 2017). In addition, students can repeatedly peruse the material and follow it in their own pace at a relatively low cost. This is considered an excellent method of overcoming certain difficulties faced with the traditional system of teaching such as the lack of space especially within the lecture halls and a shortage of human resources (Asiry, 2017). However, socio-economic factors play an important role in deciding the type of teaching. Students in the developed countries prefer e-learning modalities while students in the developing countries prefer it as a supplementary method (Schlenz et al., 2020). A study by Asiry (2017) identified e-learning as a helpful supplementary learning method among Saudi Arabian dental students rather than a replacement for traditional teaching methods. According to authors’ experience, though there was much resistance in adopting to e-learning at its infancy, it has now been universally accepted as a learning modality not only by teachers but also by the students. Many are of the view that assimilation of knowledge could be best achieved purely through e-learning modalities where as it should be supplementary in nature in skills acquisition. The popularity of books and hard copies of journals have seen a steady decline due to the availability of e-learning resources and even publishers have realised this trend and supply both hard and electronic versions of their publications which in future may progressively be replaced by electronic educational materials.
The success of e-learning is dependent on a multitude of factors. Computer literacy, availability of appropriate technology, accessibility and having a good high bandwidth internet connection are some of the key factors (Asiry, 2017; Linjawi & Alfadda, 2018). According to a study by Gunawardane and Wijekoon (2017), it was revealed that dental students in the Faculty of Dental Sciences, University of Peradeniya, Sri Lanka had adequate computer literacy and facilities. Although Linjawi and Alfadda (2018) identified that the perceived impact of e-learning and readiness for e-learning though popular and satisfactory among Saudi Arabian dental students, declined as they proceeded to higher semesters. Imparting the skills component has been identified as a major challenge in using e-learning and students were in need of more support in the skills domain (Linjawi & Alfadda, 2018). Students have been shown to have better skills and motivation for use of online tools for personal or non-educational purposes than for learning purposes. Thus, this should be carefully considered when developing a successful strategy to motivate them for e-learning (Linjawi & Alfadda, 2018). Apart from the above mentioned factors, student characteristics, cognitive factors (performance expectations) and the social environment (learning climate) are considered as some predictors of the perceived satisfaction among students (Venkatesh et al., 2019). Most of the students prefer a combined approach comprising traditional and e-learning methods than relying on e-learning methods alone. Some of the preferred methods of delivery of e-learning resources for pre-clinical dental undergraduates were online flash lectures and procedural videos (Asiry, 2017). Video demonstrations enabled students to reflect on their predominant learning approaches, which emphasise self-directed learning and avoid surface learning techniques (Chonkar et al., 2019). Some dental schools in the developed countries have introduced tools such as Technology Enhanced Learning (TEL) in both pre-clinical and clinical courses with the development of innovative learning platforms and they further assess and monitor student performance in relation to the new approach (Wong et al., 2020). Further, Faculty of Dentistry, National University of Singapore has implemented a multi-stage framework for the academic staff to grasp technology in various aspects such as reflecting teaching practice, designing new technology options and identifying learner impact with changes on teaching methods.
However, not everyone is in agreement with the benefits of e-learning. University administrators and experts in information technology working in universities have varying opinion (ranging from majority of teaching on traditional classroom mode to predominant e-learning mode) regarding the need of administrational change created by e-learning, generation of resources, impact on enrolment, responsibility for course design and content and the impact on the mission of the university. However, there is a general agreement on challenges such as the requirement of resources and cost of maintenance, need for motivating the teachers to keep abreast with the latest technology and the necessity for cooperation to improve e-learning (Hillenburg et al., 2006).
The COVID-19 pandemic has made it necessary to impart changers in the modalities of education all over the world. Since schools and universities have been closed to prevent the spread of infection, conducting e-learning sessions has become the prime mode of teaching. The situation in Sri Lanka was without exception. Most programmes including the Bachelor of Dental Surgery had to comply with this requirement in order to provide the students a continuous educational experience during the pandemic situation. E-learning has been used in a very primitive level in the Faculty of Dental Sciences, University of Peradeniya for a long time but had not been utilised to its full potential. As dentistry is mostly a skill based professional degree programme, delivering course content online was a challenge. In addition, resistance to change was evident among the staff due to the fact that they were comfortable with the traditional time tested methods. However, with the new norms, e-learning platforms such as Zoom, Google Meet and WhatsApp discussions were used at the Faculty of Dental Sciences for the learning along with narrated PowerPoint presentations, video demonstrations and online quizzes uploaded onto the existing e-learning platform Dent Moodle. Due to this novel experience, it was considered important to analyse the students’ opinion on e-learning, the difficulties faced by them and expectations to improve e-learning in the field of dentistry. Further, it would be beneficial to identify barriers of e-learning when designing and revising the dental undergraduate curriculum in the future.
II. OBJECTIVES
General objective of the study was to assess the undergraduate dental students’ perception on the effectiveness of e-learning utilised in the Bachelor of Dental Surgery (BDS) programme. The specific objectives were to identify students’ opinion on the factors that promote e-learning, awareness on the effectiveness of using different platforms and social media, barriers imposed and suggestions for the improvement of e-learning in the BDS study programme.
III. MATERIALS AND METHODS
A cross sectional descriptive study was carried out on a sample comprising of undergraduate dental students of the Faculty of Dental Sciences, University of Peradeniya who had enrolled and followed all online lectures and assignments based on the content taught via e-learning in the first, third, fifth and seventh semesters. A self-administered and pre-tested (25 students representing all batches for the pilot and their responses were excluded from the study sample) questionnaire was administered via a web-based survey form. A covering letter, information sheet and consent form were also annexed to this form. Those respondents who gave the informed consent were able to fill the questionnaire. The survey link was disseminated among the dental students via the email by the faculty administration unit. The questionnaire used in this study comprised of 23 close-ended questions which consisted of demographic data and specific questions on awareness, attitude and practice of e-learning. Examples of e-learning platform stated in the questionnaire were live Zoom presentations, Google Meet, Power Point presentations with voice narrations and supplementary material such as web links, video demonstrations and YouTube and other video links.
Confidentiality and anonymity of the data provided were assured by keeping the questionnaire anonymous. No identification details were included in the questionnaire. Data management and statistical analysis was performed using the statistical software SPSS version 21.0. Frequencies and percentages were obtained for categorical data and Chi-square test was used to determine the association between variables. Ethical clearance was obtained from the Ethics Review Committee of the Faculty of Dental Sciences, University of Peradeniya (ERC/ FDS/UOP/I/2020/21).
IV. RESULTS
The response rate was 82% (250 participants out of 305 of all undergraduates). The sample comprised 19% from the first semester, nearly 25% from the third semester, 26% from the fifth semester and nearly 30% from the seventh semesters of the Bachelor of Dental Surgery (BDS) programme. Seventy-two percent (72%) were females. Approximately 41% claimed that they have either very good or excellent literacy on information technology (IT). Fifty-four percent of the respondents claimed that their English language literacy is very good or excellent. A majority of the population accessed e-learning content using their mobile devices. Half of the sample had experienced some kind of interruptions during e-learning.
A. Satisfaction on E-learning
Seventy-one percent (71%) responded that they were either satisfied or highly satisfied about e-learning materials they received. More than one third of the respondents (39%) felt encouraged to collaborate and interact with their teachers during e-learning time compared to the in-class teaching sessions. A similar percentage of respondents felt that they were more encouraged to work on course materials compared to the traditional learning sessions received at the university. Around 74% of the students felt that the teachers were friendly during e-learning sessions. Moreover, 62% of them were either satisfied or highly satisfied with the provision to ask questions during e-learning sessions. Sixty percent (60%) of respondents was satisfied or highly satisfied with the answers received for the clarifications they requested. Seventy percent (70%) of the students claimed that the interactions between the lecturers and students during question and answer sessions, case scenarios and case discussions were essential for the success of e-learning experience. Fifty-five percent (55%) of them were satisfied with the interactions they experienced during e-learning sessions in their study period. Interestingly, more than one third of the respondents were of the opinion that online lectures were more effective than traditional live lectures. Moreover, 54% of the sample felt that the overall e-learning experiences was better than the traditional learning opportunities they received in the university and the possibility of following the coursework at their own pace (14.8%) was chosen as the main reason for this response.
Females had better overall e-learning experiences than the learning opportunities they received at the university compared to male students and this difference was statistically significant (p=0.000) (Table 1).
Surprisingly, only 1% of the respondents had identified social media as a positive influence on e-learning.
Table 1 describes participants’ response to the questionnaire according to their gender.
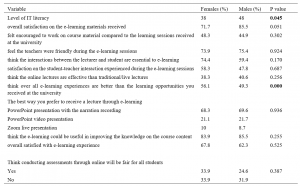
Table 1. Comparison of participants’ response according to their gender (in percentages)
B. Preference on Methods of E-learning
Sixty-four percent (64%) of the participants were familiar with Zoom as an e-learning platform. Majority of the students preferred PowerPoint presentations with narrations (68%) to receive lectures. In addition, 69% felt that e-learning materials had helped them to improve their knowledge on the course content specified in the Intended Learning Outcomes (ILOs). Around 34% had identified video demonstrations as an important tool in imparting skills training to achieve the course ILOs. Over 70% rated it as highly useful when students’ opinion is taken in consideration in improving knowledge on the course content.
Sixty-four percent (64%) felt that that e-learning material should be used as supplementary materials for in-class learning within the skills domain. The e-learning materials considered appropriate were video demonstrations, procedural steps described in text documents, YouTube links and case discussions. Majority of the courses in the first semester (Anatomy, Dental Anatomy and Physiology related), third semester (Tooth morphology and occlusion, Human Diseases, Dental Biomaterials), fifth semester (Operative Dentistry, Population Oral Health, Clinical and Diagnostic Oral Sciences [CDOS1] and Child and Adolescent Oral Health [CAOH1]) and seventh semester (Adult Oral Health, CDOS2 and CAOH2) were rated as suitable for e-learning activities.
C. Opinion on Assessment via E-Learning Platforms
The Multiple Choice Questions (MCQ) and Short Answer Questions (SAQ) were the more common forms of assessments provided to the participants. However, some students (9%) had experience with essays too. These assessments were formative in nature whereby the questions were posted after each learning session in order to assess the effectiveness of the learning process. These questions were marked by the teachers or self-marked by the students. Sixty-nine percent (69%) felt that conducting assessments online is fair.
D. Opinion on Barriers Identified in E-Learning
Though the majority of first semester students had identified inadequate opportunities to work with other batch mates as a stumbling block, the majority of the seventh semester had identified technical difficulties in accessing the e-learning resources as the major barrier in e-learning. However, there was no significant difference in the responses between the genders and the semester of study of the student.
E. Suggestions to Improve E-Learning
When the students were requested to suggest ways to use the e-learning to improve the required skills, approximately half (52%) of the respondents preferred video demonstrations on clinical and lab procedures. Furthermore, multiple choice questions, use of charts to explain presentations, discussion forums, quizzes, assignments, web links and supplementary reading material were other ways of improving the learning experience as suggested by the participants. However, 3% of the students had clearly mentioned that e-learning could not be used to improve the required skills in dentistry.
There were multiple suggestions by the majority to improve the overall effectiveness of their e-learning experience. Some of the suggestions were uploading of lectures coupled with assignments, video demonstrations especially for practical scenarios, lectures followed by discussions and lectures on Zoom followed by case discussions. However, the statistical significance could not be assessed between genders or semesters as the number of responses for each option was small.
F. Analysis of Results According to the Respondents’ Current Semester
When the results were assessed according to the current semester, a majority of the first, third and seventh semesters students preferred video demonstrations for e-learning sessions. However, a majority of the fifth semester students preferred a combination of video demonstrations and a text document describing procedural steps or video demonstrations combined with YouTube links and discussion forums. Respondents from first semester had the highest overall satisfaction on e-learning materials they received and the difference between the semesters was statistically significant. (p=0.002). Over two-thirds of the seventh semester students (being the students who were exposed to conventional classroom learning experience for more than three years) confirmed that their overall e-learning experiences were better than the traditional classroom learning opportunities they received at the university and the difference was statistically significant (p=0.000) (Table 2). Further, students’ rating of e-learning materials received from teachers (p=0.002) (Figure 1) and encouragement to work on course material compared to the learning sessions received at the university (p=0.015) (Figure 2) were statistically significant when the semester of study were considered.
Table 2 describes participants’ response to the questionnaire according to their semester of study.
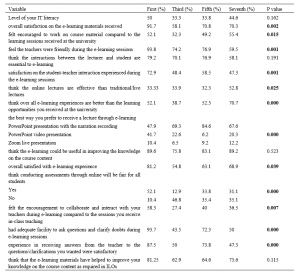
Table 2. Variations of participants’ response according to their semester of study (in percentages)
Figure 1 shows students’ rating of e-learning materials received from teachers according to their semester of study.
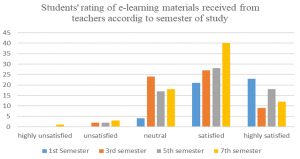
Figure 1. Students’ rating of e-learning materials received from teachers according to their semester of study
Figure 2 shows students’ feeling of encouragement to work on course material compared to conventional learning sessions received at the university.
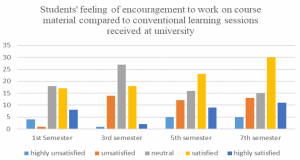
Figure 2. Students’ feeling of encouragement to work on course material compared to conventional learning sessions received at the university according to their semester of study
When the results were analysed according to theory based courses (Anatomy, Oral Biology, Human Diseases, Tooth morphology and Occlusion, Dental Biomaterials) against practical, lab based and clinical training courses (Adult Oral Health, Population Oral Health, Clinical and Diagnostic Oral Sciences, Child and Adolescent Oral Health), the participants’ overall e-learning experience in theory based courses was significantly higher than practical and clinical courses (p= 0.03).
All data are available at https://figshare.com/s/c6c7b8f1d5cfd0076808.
V. DISCUSSION
E-learning is a broad term which encompasses the use of software applications to support learning, whether online or offline (Piccoli et al., 2001). The efficacy of an e-learning experience is dependent on many factors such as availability of devices, access to internet, knowledge on IT and uninterrupted internet connectivity (Asiry, 2017; Linjawi & Alfadda, 2018).
In the present study, half of the sample experienced some interruption during the e-learning sessions. It has been demonstrated in previous studies that students generally have a positive outlook to e-learning in spite of technical problems and related stresses (Brumini et al., 2014). Other studies have also highlighted positive experiences in isolated dental specialties (Bains et al., 2011; Gonzalez & Gadbury-Amyot, 2016; Qi et al., 2013; Reissmann et al., 2015). Our results revealed that students had a better learning experience with e-learning in comparison to traditional methods which was compatible with the findings of similar studies (Turkyilmaz et al., 2019). A study in Germany involving undergraduate dental students stated that participation in online learning was higher compared to “face-to-face” courses which was similar to the findings of the present study (Schlenz et al., 2020). Reasons for popularity of e-learning material over face-to-face learning are that it not only provides flexibility in the learning process (p=0.003) but also saves time (p = 0.012) (Anwar et al., 2021).
When the students’ perception on e-learning resources were analysed, males showed better IT literacy in comparison to female students. Even though the female students were not as confident as male students, a majority of them expressed that the overall e-learning experience was better than the conventional learning. These findings endorse the observations of Linjawi and Alfadda (2018) where the students claimed that they had better skills and motivation for e-learning than conventional learning activities. The identification of social media platforms for e-learning opportunities by a very few students in our study corroborate the fact that formal modalities of delivering e-learning resources should be implemented rather than relying on generic platforms.
Participants’ overall e-learning experience in theory based courses were significantly higher than practical and clinical courses due to the need of hands on experience, simulator training and working with patients for the practical and clinical courses than listening, reading and writing practice. This fact should be carefully considered when developing and planning the modes of content delivery as the knowledge and skills domains should be separately considered. More theory could be delivered through e-learning modalities and this time saved could be utilised for the face to face delivery of practical and clinical procedural teaching in predominantly skills based courses such as the Bachelor of Dental Surgery. However, the findings contradict the previous belief of the faculty that e-learning should only be used as a supplementary tool. There is a possibility to incorporate classroom and e-learning as a blended learning experience when imparting theory components in the future to save time, improve efficient use of limited infrastructure and to focus more on much needed skill development in dentistry. Incorporation of e-learning facilities to the maximum possible level should also be considered in future planning of the state universities in the delivery of undergraduate education in countries such as in Sri Lanka to enhance the quality of learning using the minimal physical and human resources available. Reports from experience in other countries highlight that e-learning processes are also cost effective, due to the availability of low cost or free online tools and platforms which can be used by teachers with a sound background of pedagogical knowledge (Goh, 2018).
First semester had the highest overall satisfaction on e-learning. This group consisted of students who hardly had any noteworthy face-to-face learning experience in the Faculty of Dental Sciences due to the abrupt closure during pandemic situation. Therefore, it seems that they could not effectively compare the two learning methods. Though less than first semester, more than 50% of the seventh semester students had a positive attitude towards e-learning experience. Our finding is in agreement with the findings of a previous study where it was shown that the perceived impact of e-learning and readiness for e-learning became less acceptable as students became mature (Linjawi & Alfadda, 2018).
Positive feedback regarding e-learning experience showed statistically significant differences between students of different semesters in relation to overall satisfaction on the e-learning materials received; encouragement to work on course materials; feeling that the teachers were friendly during the e-learning sessions; satisfaction on the student-teacher interaction during e-learning sessions. These findings should be considered when modes of learning for different components are planned by the Faculty of Dental Sciences during future revisions to the curriculum. Similarly, a recent report on undergraduate dental education during the COVID-19 pandemic has described that e-learning has been appreciated not only by students and teachers, but also in relation to the teacher-student interaction (Bennardo et al., 2020).
A majority of the students felt that the best way to receive the theory component was through PowerPoint presentation with voice narrations. This was statistically significant when compared among different semesters. This is in contrast with the preferred e-learning method among the Saudi Arabian dental students whereby online flash lectures were the most preferred method (Asiry, 2017).
Similar to our findings, a study on health care students belonging to 11 countries among the developed and developing nations also identified that 60% agreed that clinical and practical skills are best learned in clinics and laboratories (Abbasi et al., 2020). Another study involving over 3000 medical students of all years from over 13 schools in Libya has revealed only 21% agreed that e-learning could be used for clinical aspects, as compared with 55% who disagreed with this statement and 24% who were neutral (Alsoufi et al., 2020). The students ‘most preferred mode to learn skills as prescribed in the ILOs was through the use of procedural videos. A previous study carried out in the same institute to investigate the efficacy of procedural video versus live demonstrations revealed that that there was no appreciable difference in the development of skills in dental laboratory technology procedures (Thilakumara et al., 2018). This outcome could be applied to our findings that e-learning sessions, if followed by discussion forums with the teachers, as suggested by the participants would dramatically improve the e-learning experience.
E-learning with its virtual learning environment also requires different skills and a positive attitude from instructors. The positive attitude of the instructors towards technology, the interactive teaching style, and control over the technology were found to have an important influence on students’ reactions to the learning environment (Piccoli et al., 2001). This highlights the importance of professional development in two main aspects; technical and e-pedagogical areas (Conole & Oliver, 2002). The significance of institutional support should be highlighted. Therefore, the need of training for the teachers in the use of efficient methods for e-learning is emphasised. Furthermore, the faculty needs to have a long-term plan to encourage learning facilities through the use of different platforms, use of web links and production of supplementary video for demonstrations in order to encourage students towards a lifelong learning experience. Investment in more user-friendly and versatile software and resources to improve e-learning activities should be prioritised in order to make this endeavour more effective, interactive and receptive to the end users.
A. Limitations of the Study
Our study was performed in a single country and in a single institution as the country has only one dental school. Therefore, the results may not be generalised to other countries and to the region. The results must be validated through further multi-centre studies in order to obtain an overall opinion. Multi-national studies would provide a better understanding on how e-learning could replace the bulk of conventional dental undergraduate clinical learning and provide cost effective solutions for the developing countries with limited physical and human resources to avoid disruption of clinical training during difficult times such as the present COVID-19 pandemic. Another limitation is the cross-sectional nature of the study design, which limited our ability to identify causal associations.
VI. CONCLUSION
A positive learning experience was achieved through the e-learning modalities by the undergraduate dental students in comparison to traditional face-to-face learning. In terms of skills training, e-learning should only be considered as a supplementary tool. These findings will be useful when designing the study courses as a major part of theory component via e-learning mode and skill component with combined e-learning and conventional modes in the future.
We recommend adapting interactive e-learning platforms by using highly sophisticated technologies along with virtual clinical experience with combined clinical scenarios and assessments based on discussions of patient cases. Cost-effective solutions are needed to reduce disruption of undergraduate dental education especially in developing countries in the region like Sri Lanka and there should be new collective effort by the countries in the South Asian region in planning and sharing less expensive e-learning solutions in order to overcome financial issues. Such measures may vary from learning theory and virtual clinical and lab-based experience, followed by limited hands-on experience on live patients in a safe environment during difficult times of this nature.
Notes on Contributors
Principal and corresponding author (Rasika Jayasinghe) conceptualised the research and edited the initial draft and wrote the results after analysis. She also did the final approval of the version to be published and agreed to be accountable for all aspects of the work.
Manjula Attygalla edited the initial draft of the manuscript and supported in modification of the questionnaire. He also did the final approval of the version to be published and agreed to be accountable for all aspects of the work.
Manil Fonseka supported planning of the study, edited the research proposal and manuscript. He also did final editing and approval of the version to be published and agreed to be accountable for all aspects of the work.
Dhanushka Leuke Bandara supported planning of the study, designed the Google form, carried out the survey and entered the data in addition to editing of the manuscript. She also did final approval of the version to be published and agreed to be accountable for all aspects of the work.
Gishan Edirisinghe carried out the literature survey and did the final approval of the version to be published and agreed to be accountable for all aspects of the work.
Ruwan Jayasinghe supported planning of the study, prepared the initial draft of the research proposal and edited the final draft of the manuscript. He did the final approval of the version to be published and agreed to be accountable for all aspects of the work.
Indika Thilakumara supported planning of the study, edited the first draft and wrote the discussion. She did the final approval of the version to be published and agreed to be accountable for all aspects of the work.
Ethical Approval
Ethical clearance has been granted by Ethics Review Committee, Faculty of Dental Sciences, University of Peradeniya. (ERC/FDS/UOP/I/2020/21).
Data Availability
All data are available at https://figshare.com/s/c6c7b8f1d5cfd0076808 and can be accessed on request and approval from the corresponding author.
Funding
No funding sources are associated with this study.
Declaration of Interest
Authors declare that they do not have possible conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Abbasi, M. S., Ahmed, N., Sajjad, B., Alshahrani, A., Saeed, S., Sarfaraz, S., Alhamdan, R. S., Vohra, F., & Abduljabbar, T. E. (2020). E-Learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work, 67(3), 549-556. https://doi.org/10.3233/WOR-203308
Alsoufi, A., Alsuyihili, A., Msherghi, A., Elhadi, A., Atiyah, H., Ashini, A., Ashwieb, A., Ghula, M., Hasan, H. B., Abudabuos, S., Alameen, H., Abokhdhir, T., Anaiba, M., Nagib, T., Shuwayyah, A., Benothman, R., Arrefae, G., Alkhwayildi, A., Alhadi, A., … Elhadi, M. (2020). Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLOS ONE, 15(11), e0242905. https://doi.org/10.1371/journal.pone.0242905
Anwar, A., Mansoor, H., Faisal, D., & Khan, H. S. (2021). E-learning amid the COVID-19 lockdown: Standpoint of medical and dental undergraduates. Pakistani Journal of Medical Sciences, 37 (1), 217-222. https://doi.org/10.12669/pjms.37.1.3124
Asiry, M. A. (2017). Dental students’ perceptions of an online learning. The Saudi Dental Journal, 29(4), 167–170. https://doi.org/10.1016/j.sdentj.2017.03.005
Bains, M., Reynolds, P. A., McDonald, F., & Sherriff, M. (2011). Effectiveness and acceptability of face-to-face, blended and e-learning: A randomised trial of orthodontic undergraduates. European Journal of Dental Education, 15(2), 110–117. https://doi.org/10.1111/j.1600-0579.2010.00651.x
Bennardo, F., Buffone, C., Fortunato, L., & Giudice, A. (2020). COVID-19 is a challenge for dental education—A commentary. European Journal of Dental Education, 24(4), 822-824. https://doi.org/10.1111/eje.12555
Brumini, G., Špalj, S., Mavrinac, M., Biočina-Lukenda, D., Strujić, M., & Brumini, M. (2014). Attitudes towards e-learning amongst dental students at the universities in Croatia. European Journal of Dental Education, 18(1), 15-23. https://doi.org/10.1111/eje.12068
Chonkar, S. P., Qi, H. L. C., Ha, T. C., Lim, M., Ng, M. J., & Tan, K. H. (2019). Can digital media affect the learning approach of medical students? The Asia Pacific Scholar, 4(1), 13- 23. https://doi.org/10.29060/TAPS.2019-4-1/OA1058
Conole, G. C., & Oliver, M. (2002). Embedding theory into learning technology practice with toolkits. Journal of Interactive Media in Education (8), 2- 3. https://doi.org/10.5334/2002-8
Goh, P. S. (2018). eLearning in medical education – Costs and value add. The Asia Pacific Scholar, 3(2), 58- 60. https://doi.org/10.29060/TAPS.2018-3-2/PV1073
Gonzalez, S. M., & Gadbury-Amyot, C. C. (2016). Using Twitter for teaching and learning in an oral and maxillofacial radiology course. Journal Dental Education, 80(2), 149–155. https://doi.org/10.1002/j.0022-0337.2016.80.2.tb06070.x
Gunawardane, S., & Wijekoon, P. (2017). Changes in perceived computer use and knowledge in Sri Lankan dental students in the last ten years. Scholars Journal of Dental Sciences, 4(5), 216-219.
Hillenburg, K. L., Cederberg, R. A., Gray, S. A., Hurst, C. L., Johnson, G. K., & Potter, B. J. (2006). E-learning and the future of dental education: Opinions of administrators and information technology specialists. European Journal of Dental Education, 10, 169–177. https://doi.org/10.1111/j.1600-0579.2006.00413.x
Li, C., & Lalani, F. (2020). The COVID-19 pandemic has changed education forever. This is how. World Economic Forum. https://www.weforum.org/agenda/2020/04/coronavirus-education-global-covid19-online-digital-learning
Linjawi, A. I., & Alfadda, L. S. (2018). Students’ perception, attitudes, and readiness toward online learning in dental education in Saudi Arabia: A cohort study. Advances in Medical Education and Practice, 9, 855–863. https://doi.org/10.2147/AMEP.S175395
Piccoli, G., Ahmed, R., & Ives, B. (2001). Web-based virtual learning environments: A research framework and a preliminary assessment of effectiveness in basic IT skills training. MIS Quarterly, 25(4), 401-426. https://doi.org/10.2307/3250989
Qi, S., Yan, Y., Li, R., & Hu, J. (2013). The impact of active versus passive use of 3D technology: A study of dental students at Wuhan University, China. Journal of Dental Education, 77(11), 1536–1542.
Reissmann, D. R., Sierwald, I., Berger, F., & Heydecke, G. (2015). A model of blended learning in a preclinical course in prosthetic dentistry. Journal of Dental Education, 79(2), 157–165. https://doi.org/10.1002/j.0022-0337.2015.79.2.tb05870.x
Schlenz, M. A., Michel, K., Wegner, K., Schmidt, A., Rehmann, P., & Wöstmann, B. (2020). Undergraduate dental students’ perspective on the implementation of digital dentistry in the preclinical curriculum: A questionnaire survey. BMC Oral Health, 20, 78. https://doi.org/10.1186/s12903-020-01071-0
Thilakumara, I. P., Jayasinghe, R. M., Rasnayaka, S. K., Jayasinghe, V. P., & Abeysundara, S. (2018). Effectiveness of procedural video verses live demonstrations in teaching laboratory techniques to dental students. Journal of Dental Education; 82(8), 898-904. https://doi.org/ 10.21815/JDE.018.086
Turkyilmaz, I., Hariri, N. H., & Jahangiri, L. (2019). Student’s perception of the impact of e-learning on dental education. Journal of Contemporary Dental Practice, 20(5), 616-621.
Venkatesh, S., Rao, Y. K., Nagaraja, H., Woolley, T., Alele, F. O., Bunmi, S., & Malau-Aduli, B. S. (2019). Factors influencing medical students’ experiences and satisfaction with blended integrated e-learning. Medical Principles and Practice, 29, 296-402. https://doi.org/10.1159/000505210
Wong, M. L., Lee, T. W. O., Allen, P. F., & Foong, K. W. C. (2020). Dental education in Singapore: A journey of 90 years and beyond. The Asia Pacific Scholar, 5(1), 3- 7. https://doi.org/10.29060/TAPS.2020-5-1/GP1086
*RM Jayasinghe
Department of Prosthetic Dentistry,
Faculty of Dental Sciences,
University of Peradeniya
Tel: +94777806314
Email: manorija@pdn.ac.lk/ manoripathiraja@yahoo.com
Submitted: 19 July 2020
Accepted: 7 October 2020
Published online: 13 July, TAPS 2021, 6(3), 67-74
https://doi.org/10.29060/TAPS.2021-6-3/OA2347
Tess Lin Teo, Jia Hao Lim, Choon Peng Jeremy Wee & Evelyn Wong
Department of Emergency Medicine, Singapore General Hospital, Singapore
Abstract
Introduction: Singapore experienced the COVID-19 outbreak from January 2020 and Emergency Departments (ED) were at the forefront of healthcare activity during this time. Medical students who were attached to the EDs had their clinical training affected.
Methods: We surveyed teaching faculty in a tertiary teaching hospital in Singapore to assess if they would consider delivering clinical teaching to medical students during the outbreak and conducted a thematic analysis of their responses.
Results: 53.6% felt that medical students should not undergo clinical teaching in the ED and 60.7% did not wish to teach medical students during the outbreak. Three themes arose during the analysis of the data – Cognitive Overload of Clinical Teachers, Prioritisation of Clinical Staff Welfare versus Medical Students, and Risk of Viral Exposure versus Clinical Education.
Conclusion: During a pandemic, a balance needs to be sought between clinical service and education, and faculty attitudes towards teaching in high-risk environments can shift their priorities in favour of providing the former over the latter.
Keywords: Disease Outbreak, Pandemic, Faculty, Medical Students, Attitudes, Clinical Teaching, Emergency Medicine
Practice Highlights
- In a pandemic, a balance needs to be sought between clinical education and risking learner exposure to the virus.
- A crisis situation can affect educators’ priorities and attitudes towards the provision of clinical education, in favour of providing crucial clinical services.
I. INTRODUCTION
Since the first reported cases of COVID-19 infections in Wuhan, in December 2019, the month of January 2020 saw Singapore’s Ministry of Health (MOH) issue guidelines and implement a series of calibrated defensive measures to reduce the risk of imported cases and community transmission (Lin et al., 2020; WHO, 2020). Singapore has a Disease Outbreak Response System Condition (DORSCON) framework, which guides the nation’s response to various emerging infectious diseases outbreaks. The four-level colour-coded system of Green, Yellow, Orange and Red, describes the increasing severity of the outbreak in the community (Quah et al., 2020).
The Department of Emergency Medicine (DEM) of Singapore General Hospital saw 130 000 visits in 2019 (SGH, 2019). It hosted 158 medical students (MS) through the year. Aside from some elective students, the majority were in their second year of clinical postings. Formal clerkships consisted of four weeks of clinical exposure in which they were expected to clerk and present cases to teaching faculty and perform minor procedures such as intravenous cannulation and insertion of bladder catheters etc., with about nine hours of classroom tutorials.
In early January 2020, DORSCON yellow was declared, indicating either a severe outbreak outside Singapore or that the disease was contained locally with no significant community spread (Quah et al., 2020). All DEM staff were required to wear personal protective equipment (PPE). Hospital elective surgeries were postponed. Other outbreak measures included setting up new isolation areas for patients. DEM staff had their leave embargoed to ensure that there was adequate manpower to staff these areas in anticipation of a gradually worsening outbreak (Chua et al., 2020).
On 7 February 2020, the outbreak alert rose to DORSCON Orange (DO) as there were cases of community transmissions (Quah et al., 2020). Based on previous experience managing the Severe Acute Respiratory Syndrome (SARS) outbreak 17 years prior, the DEM transitioned to an Outbreak Response Roster, where physicians and nurses of the DEM were split into teams that worked 12 hour shifts, with no overlapping shifts, hence limiting staff contact to only those within their teams (Chua et al., 2020). With DO in effect, the department needed to come to a rapid decision about whether or not to accept MS in the ED. A group of 12 MS that the DEM was supposed to host this April already had their clerkship cancelled due to concerns of breaching infection control and safe distancing measures. There have been no studies to date on faculty attitudes towards clinical teaching of MS during a pandemic, although papers have been published about students’ attitudes towards clinical training during disease outbreaks. The Clerkship Director conducted a short and focused survey amongst the faculty between the 27th-29th of March, amidst rising public concerns that the country might soon be locked down, to explore their attitudes on having MS clerkships during the COVID-19 pandemic. The results of this survey allowed the Director to quickly understand the sentiments of the faculty and thus decided that an entirely remote, online teaching program would be created instead. 9 days after the survey, on the 7th of April, the Singapore government officially announced the implementation of a lockdown, known locally as a ‘circuit breaker’ (Quah et al., 2020).
II. METHODS
Clinical teachers of the DEM were issued an anonymous survey over a period of three days via an online survey tool, SurveyMonkey (www.surveymonkey.com). Participants were informed prior to completing the survey that it was anonymous, and by proceeding with the survey they consented to the results being used for research purposes. The data collected included their professional appointments in the department and two yes/no questions: “Do you think medical students should be performing their EM clerkship during DO?” and “Are you keen on teaching MS clinically during DO?”. Participants answering “No” to the latter were asked to elaborate. All participants were asked to write about any concerns they had about having MS in the emergency department (ED) during DO. No other personal identifying information was sought. The survey was deliberately kept short and easy to answer to promote staff participation within the short timeframe the DEM had to make the decision about accepting students. Informed consent was waived as per the Institutional Review Board (IRB).
A simple descriptive quantitative analysis of responses to the 1st two yes-no questions identified the overarching sentiment of the department towards hosting MS during DO and was followed by a thematic analysis of the free-text answers to the last two open-ended questions (Braun & Clarke, 2006).
As many participants used the last question (‘any other comments?’) to emphasise or elaborate on the preceding question (‘why aren’t you keen to teach?’), the majority of the qualitative data gathered pertains to the issues of having MS in the department during DO. There was a paucity of data detailing why participants were in favour of teaching MS, as the survey did not specifically ask this. Hence, the authors chose to focus on analysing the responses of participants who were not keen to teach during this time. This analysis yielded three different themes. However, a small number of respondents supportive of MS felt strongly about teaching and volunteered their reasons in response to the last question. While this data is insufficient to support a robust thematic analysis, a small section is included at the end in order to present as complete a discussion as possible.
III. RESULTS
A. Participant Background
Participants consisted of Emergency Medicine (EM) specialists, permanent registrars or middle grade staff and EM senior residents. These groups were chosen because they each hold significant roles, such as being named supervisors or clinical instructors of MS, and have considerably more contact time with MS in the DEM as opposed to nursing staff or junior doctors.
B. Quantitative Results
A total of 28 out of 45 (62.3%) responses were recorded. Except for two individuals, all other respondents in favour of hosting MS in the ED during DO (46.4%) were also keen to teach them. About two-thirds of the participants (60.7%) were not keen to teach MS during DO. However, of this latter group, 23.5% of respondents offered (without prompting) a compromise – where they proposed teaching only during the relatively less busy night shifts, in their response to ‘Any other comments?’ Table 1 shows the breakdown of responses.
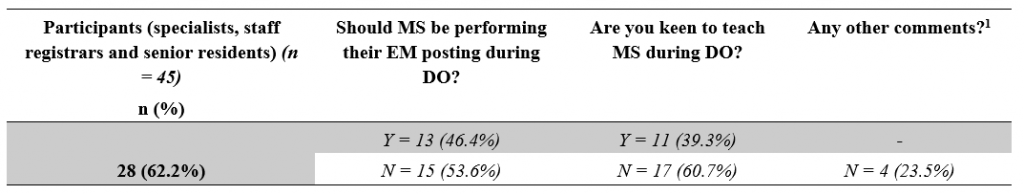
Table 1: Responses broken down by question.
[1]Number of participants who offered the compromise of teaching during the relatively less busy night shifts despite indicating they were not keen to teach MS.
C. Qualitative Results – Reasons Against
Each of the three themes presented here begins with a short paragraph that describes the situational context in which this survey took place, followed by a series of selected statements, and ends with a general summary and discussion of the responses within the respective theme. In order to maintain the authenticity of the data, each response is reproduced verbatim, sometimes in Singlish, the local colloquial variety of Standard Singaporean English (Bokhorst-Heng, 2005). Any edits to the text for clarification purposes have been clearly identified.
1) First theme: Cognitive overload of clinical teachers– There is only so much one can handle: Emergency physicians are no strangers to high stress environments, and are aware that as frontline workers they will be at the forefront in dealing with any emerging infectious disease. The move into DO represented the shifting of the local virus epidemiology from predominantly imported cases that could be easily identified and isolated, into the community-at-large. With this shift came changes to existing workflows and the re-arrangement of department space to form isolation areas for treating potential infectious cases. The implementation of a strict team-based roster described earlier meant that almost half the entire department would not physically meet the other half, and a surge in manpower requirements saw many junior doctors from other departments being rotated into the ED to help tackle the increased clinical load. Being new to the DEM, these new doctors required more supervision and assistance in adapting to the unfamiliar work environment. Responses that supported this theme include:
“High clinical load, long hours. Already cognitively overloaded. Not conducive for teaching. New [junior doctors] need to be taught also.”
Participant #6, Specialist
“Focus on daily evolving challenge first.” and in response to the last question “Please no.”
Participant #2, Senior Resident
“During DORSCON ORANGE we are in stress, if clinical teaching sessions start then other [doctors’] stress and workload level will increase.”
Participant #25, Staff registrar
“May be more a hassle if we have to look after the new [junior doctors] rotating and students [as well].”
Participant #4, Specialist
“We are also in a 12-hour outbreak roster which is physically, emotionally and mentally draining. Teaching students in this environment is far from ideal” and in response to the last question “Am fairly strongly against this idea”.
Participant #8, Specialist
“Day shifts no bandwidth to teach […] also can’t pay attention to [medical students] during day shifts, too tiring and too busy […] but I feel I can’t do [medical students] justice because I can’t debrief after a shift either, too tired.”
Participant #17, Specialist
Many of these responses conveyed a sense of exhaustion, reflecting the toll that constant workflow changes, longer work hours and relative social isolation was taking on the faculty. Teaching and supervising MS appeared to be viewed as a “hassle” or “extra work”, an additional drain to a clinical faculty’s energy during a busy and stressful shift.
This brought the department to a discussion on the provision of clinical services versus clinical education – whether teaching the next generation of future doctors was as important as treating the patient in front of us. One school of thought held that as clinician educators, physicians should – as the name implies – be clinicians first before educators. However, the interplay between these two roles is likely dependent on the faculty’s attitudes towards learners, as will be described later. Being cognitively overloaded naturally results in a shuffling of One’s priorities, which is seen next.
2) Second theme: Prioritisation of staff welfare – whose welfare is more important, staff or students? : It is well known that mental health can be adversely affected in crisis situations, and as the COVID-19 situation unfolded, boosting morale and maintaining the welfare of all staff became an important consideration (Matsuishi et al., 2012; McAlonan et al., 2007). At the forefront of this effort was the need to provide the staff with a supply of good quality personal protective equipment (PPE) so the staff would feel safe and confident in existing infection control measures. Although Singapore had yet to experience a shortage of PPE, there was still a concerted effort made by all hospitals to conserve these resources. Staff wellness was a theme seen in several responses:
“[I] can’t do the [junior doctors] justice because having a [medical student] attached to them is another stressor in an already stressful shift.”
Participant #17, Specialist
“Having to keep our doctors and nurses safe takes up a lot of energy. Students are young and naïve and will require even more time and resources to ensure they are safe.”
Participant #22, Specialist
“Furthermore, they will need to use PPE and again this should be conserved during the period of the outbreak.”
Participant #27, Specialist
“Medical students are important for future but I feel staff currently working in the department should be look after well.”
Participant #25, Staff registrar
“Waste PPE.”
Participant #20, Specialist
The importance of conserving PPE during a pandemic is undisputed and the concern that MS would use them up is valid. It was interesting to note in these responses hints of an “us-versus-them” mentality, where MS were seen as competition for the limited resources of PPE, time, and energy. Students were not viewed as part of the DEM team and perceived more as “stressors”, who required attention because they were “young and naïve”, and their use of PPE was viewed as a “waste”. This identification of an “in-group” of staff and an “out-group” of students led to a prioritisation or favouring of the former over the latter. This behaviour can be explained by the Social Identity Theory (SIT), which states that part of an individual’s self-image or self-concept is derived from the social groups to which they perceive themselves to belong to (Hogg & Reid, 2006; Tajfel & Turner, 1979). Thus, in order to maintain a positive self-image, there is a tendency for people to favour the in-group and discriminate against the out-group. This phenomenon was famously demonstrated by Tajfel et al in their Minimal Group Paradigm studies, which essentially showed that the mere perception of belonging to one of two distinct groups was enough to trigger social discrimination between the groups (Tajfel et al., 1971). Behaviour like this is indicative that a significant number of the department hold the belief that there is a distinct divide between students and staff, rather than seeing MS as belonging to the wider group of the medical fraternity. Creating such a divide between staff and student is problematic because it hinders effective teaching, especially because MS will eventually transition from the “out-group” of students to the “in-group” of staff upon graduation, and clinician educators are responsible for providing a safe environment for them to learn in. However, beyond this discussion of intergroup competition, there were concerns amongst the faculty with regards to the appropriateness of siting clinical learning in the high-risk, front-line location of the ED in a pandemic, as discussed in the next theme.
3) Third Theme: Risk of viral exposure vs clinical education – What is the price to pay and who pays it?: During the initial period of DO, medical schools pulled MS out of the clinical environment and moved to online learning, with the aim of protecting them from unnecessary exposure to the virus and for safe distancing. However, when they proposed that students be allowed back into the hospitals after undergoing PPE training, this risk of exposure had not changed, as the number of positive cases was rising daily still. Responses that reflected this theme included:
“Don’t think it’s appropriate to have students around in a high-risk environment.”
Participant #4, Specialist
“Having medical students around not only will expose them to infection it will also compromise the rest of the staff in the event of a breach in infection [protocols]. Also, them just hanging around & not allowed to have hands-on [participation] in the procedures, clerking, [patient] contact etc will not be of any benefit [to them] at this time.”
Participant #7, Senior Resident
“Student safety issue. No minder to ensure students’ adherence to strict PPE as Doctors and Nurses will be busy with clinical service.”
Participant #11, Specialist
“I think medical students are not providing clinical care to patients and having them in the ED increases risk to patients (without the attendant benefits) and increases risk to themselves (without the moral obligation to do so as doctors) and their family.”
Participant #27, Specialist
“Can students be [held] responsible for their own health? Or the school or the department? As doctors, we know it as our duty and occupational hazard. But as students – their duty is to learn (best done in a safe environment), not put their health at risk.”
Participant #6, Specialist
Responses that addressed the risk of virus exposure in the ED could be divided into two groups –those that were predominantly concerned about the students themselves catching the virus, and those that were more concerned about the consequences of such an event. The risk of catching the virus was seen as too high a cost – one that was borne not only by the individual student but by the patients and the staff as well. The benefits of clinical bedside instruction were called into question, as students’ movements would be restricted to low or medium-risk areas only. More than one participant raised the potential issue of students breaching infection control protocol or needing supervision in donning their PPE, despite reassurances given that schools would send MS for PPE training. This reflected a lack of trust in MS – themselves adult learners – who could be reasonably expected to understand the importance of infection control protocols. It begs the question of how big a role the educator plays in the personal safety of a MS and that of the patients and staff they interact with.
D. Qualitative Results – Reasons For
The survey design did not specifically ask responders about their reasons for supporting teaching MS during this pandemic. However, some participants felt strongly enough about this to advocate for clinical postings. Their reasons are shared below.
1) Theme: For the sake of tomorrow – In defence of teaching amidst a crisis:
“I feel we can still provide a meaningful learning experience for these students. We just need to lay out clear instructions and precautions for them to follow. It is a good opportunity to show to students how emergency medicine is adaptive, versatile, and for them to appreciate how quickly workflows can change, or how triage works in a disaster setting.”
Participant # 15, Specialist
“The way it is done has to be different […] the traditional method of teaching, where the students look to the seniors and may expect some form of spoon feeding […] Only when this mind-set is removed, will the tutors […] look at them as part of the team and incorporate them […], and will students see […] themselves as Drs to be [sic], practice safe habits from the very start and protect themselves as the patient’s doctor. This sense of ownership, accountability, professionalism can be started from that stage as a medical student. This is the perfect opportunity to state that this is what is expected and groom them likewise.”
Participant #19, Specialist
“I feel that the teaching should as much as possible be a simulation of working life and that working in high-risk areas such as these gives a semblance of pressure which cultivates good habits such as mindfulness of hand hygiene, donning of PPE etc.”
Participant #26, Senior Resident
The responses share a commonality of seeing the pandemic as an opportunity for modelling positive attitudes that would benefit the student in the future. This point of view advocates for the acknowledgement of the realities of being a doctor and assumes that students are already part of the “in-group” of the medical team rather than the “out-group” as seen in the earlier discussion.
IV. DISCUSSION
A. Limitations
This study has its limitations, chiefly being the lack of qualitative data representing the opinions of those who were keen to teach MS as the initial survey was conducted with the purpose of gauging whether or not the department would be open to receiving MS during DO. This lack of data meant that this study is at best a one-sided representation of the department’s opinion.
Additionally, all four of the authors have a keen interest in the education of MS and two of the authors are actively involved in faculty development. They were all both participants in the study as well as its evaluators. Prior to evaluation of results, the authors themselves suspected that majority of the faculty would be too overwhelmed with the changes the pandemic wrought to want to teach students, which may have contributed to confirmation bias in the analysis of the data. However, throughout the analysis, every attempt was made to ensure that the themes uncovered remained true to the data, and much of the original data was reproduced here faithfully to maintain transparency, such that the reader may draw their own conclusions.
Another limitation of the study was that the survey was unable to measure shifts in the attitudes of faculty as the pandemic evolved, which would have allowed us to understand the amplitude of the effect of the pandemic itself more clearly.
B. New Insights
It was worth noting that nearly two-thirds of the department did not want to teach MS during DO, despite each participant having taught MS routinely prior to this pandemic. Initial analysis of the reasons given for this refusal revealed three distinct themes of Cognitive Overload of Teachers, the need to Prioritise Staff Welfare and the Risk of Viral Exposure to Students – themes that are transferrable to many departments involved in pandemic response, regardless of locality.
Expounding further on this topic, it can be seen in some of the responses detailed under the themes of Cognitive Overload and Prioritising Staff Welfare, that there was a perceived increase in the need to supervise the new junior doctors rotating into the department on short notice (as opposed to the junior doctors who were already in the middle of their rotation and thus more familiar with the department’s protocols). This supervision is an important component of the continuing clinical education of junior doctors, which in itself is part of a larger debate surrounding the competing aims of clinical service versus clinical education that has been ongoing for many years (Woods, 1980). It is often the case in EM that when overwhelmed with patients, clinical education is sacrificed for clinical service without much short-term complications. Indeed, even amongst EM residents, more research is needed to define the optimal balance between service and education (Quinn & Brunett, 2009). However, a pandemic presents a rather unique situation in that most junior doctors will not have worked in a pandemic before. Thus, the need to educate junior doctors on both pandemic response and the importance of personal safety – with its direct impact on patient safety – now cannot be sacrificed without directly affecting the provision of clinical service.
It is beyond the scope of this paper to comment on whether educating MS on pandemics through clinical immersion programs during a pandemic better prepares them for future outbreaks, or in the broader sense, whether the clinical education of today’s MS by immersive learning can bolster the clinical service of tomorrow’s junior doctors. In fact, it seems almost premature to consider this question given the paternalistic attitude many of our faculty appeared to have towards students, perceiving them as learners to be looked after – to the extent that they could not even be trusted with their own safety and that of the patients and staff they interact with. Interestingly, this view seems to be shared by MS themselves – an electronic survey conducted at one of Singapore’s medical schools showed that a third of currently enrolled MS were concerned that they might introduce possible risks to the patient should they return to the clinical setting (Compton et al., 2020). These findings are indicative of a more deeply rooted mindset in which the social hierarchy draws a clear line between Teacher and Student. This becomes clearer when one considers that in Confucian Heritage Cultures such as Singapore (Biggs, 1998), the teacher holds great authority and students brought up in such cultures tend to defer to such authority as a matter of course (Ho, 2020). Given the multiple factors that contribute to this debate, it is unlikely that we will be able to arrive at a clear answer without further research, but what is certain is that medical students are not essential workers and, in a pandemic, medical schools need to balance their educational needs and ethical obligations to keep students safe (Menon et al., 2020).
Within our paper, it is heartening that many participants who were not keen to teach still tried to offer a compromise of teaching during the relatively less busy night shifts instead, and that 46% of our department were willing to accept MS during this period. COVID-19 allowed us to uncover some of the underlying attitudes towards MS and to consider them in the context of Singapore’s cultural heritage. These attitudes are important for us to address if we are to improve the delivery of medical education in the ED and we would like to invite the reader to consider whether the same uncovering has occurred in their respective departments.
V. CONCLUSION
The balance between clinical service and clinical education is a precarious one that appears to shift quickly in favour of the former in the high-risk environment of an evolving pandemic, which presents significant challenges even for experienced educators to overcome. As seen in our paper, cognitive overload of educators and the need to prioritise the welfare of junior staff inexperienced in pandemic response takes clear precedence over the education of MS. The paternalistic view that majority of our faculty hold leads to doubts about the ability of MS to keep themselves and their patients safe from virus exposure, doubts that are surprisingly shared by MS as well, and is indicative of the social hierarchy deeply ingrained in Confucian Heritage Cultures such as Singapore and surrounding countries in the region, where students tend to defer to authority as a matter of course. In order to improve as medical educators, we must place further effort into uncovering the underlying attitudes of both faculty and MS and address them in ways specific to our cultural heritage.
Notes on Contributors
Author Teo TL analysed the transcripts, conducted the primary thematic analysis and wrote the manuscript. Author Lim JH co-wrote the manuscript. Author Wee JCP conducted the literature review and developed the manuscript. Author Wong E designed and conducted the study, performed the data collection and developed the manuscript. All the authors have read and approved the final manuscript.
Ethical Approval
IRB approval for this study was obtained (SingHealth CRIB reference number 2020/2134).
Acknowledgement
The authors would like to acknowledge all participants of the survey.
Funding
No funding sources are associated with this study.
Declaration of Interest
All authors work in SGH DEM and answered the survey as participants.
References
Biggs, J. (1998). Learning from the confucian heritage: So size doesn’t matter? International Journal of Educational Research, 29(8), 723–738. https://doi.org/10.1016/S0883-0355(98)00060-3
Bokhorst-Heng, W. D. (2005). Debating singlish. Multilingua, 24(3), 185–209. https://doi.org/10.1515/mult.2005.24.3.185
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Chua, W. L. T., Quah, L. J. J., Shen, Y., Zakaria, D., Wan, P. W., Tan, K., & Wong, E. (2020). Emergency department ‘outbreak rostering’ to meet challenges of COVID-19. Emergency Medicine Journal, 37(7), 407–410. https://doi.org/10.1136/emermed-2020-209614
Compton, S., Sarraf-Yazdi, S., Rustandy, F., & Radha Krishna, L. K. (2020). Medical students’ preference for returning to the clinical setting during the COVID-19 pandemic. Medical Education, 54(10), 943–950. https://doi.org/10.1111/medu.14268
Ho, S. (2020). Culture and learning: Confucian heritage learners, social-oriented achievement, and innovative pedagogies. In C. Sanger & N. Gleason (Eds.), Diversity and inclusion in global higher education (pp. 117–159). Palgrave Macmillan. https://doi.org/10.1007/978-981-15-1628-3
Hogg, M. A., & Reid, S. A. (2006). Social identity, self-categorization, and the communication of group norms. Communication Theory, 16(1), 7–30. https://doi.org/10.1111/j.1468-2885.2006.00003.x
Lin, R. J., Lee, T. H., & Lye, D. C. B. (2020). From SARS to COVID-19: The Singapore journey. The Medical Journal of Australia, 212(11), 497-502.e1. https://doi.org/10.5694/mja2.50623
Matsuishi, K., Kawazoe, A., Imai, H., Ito, A., Mouri, K., Kitamura, N., Miyake, K., Mino, K., Isobe, M., Takamiya, S., Hitokoto, H., & Mita, T. (2012). Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry and Clinical Neurosciences, 66(4), 353–360. https://doi.org/10.1111/j.1440-1819.2012.02336.x
McAlonan, G. M., Lee, A. M., Cheung, V., Cheung, C., Tsang, K. W. T., Sham, P. C., Chua, S. E., & Wong, J. G. W. S. (2007). Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Canadian Journal of Psychiatry, 52(4), 241–247. https://doi.org/10.1177/070674370705200406
Menon, A., Klein, E. J., Kollars, K., & Kleinhenz, A. L. W. (2020). Medical students are not essential workers: Examining institutional responsibility during the COVID-19 pandemic. Academic Medicine, 95(8), 1149–1151. https://doi.org/10.1097/ACM.0000000000003478
Quah, L. J. J., Tan, B. K. K., Fua, T. P., Wee, C. P. J., Lim, C. S., Nadarajan, G., Zakaria, N. D., Chan, S. J., Wan, P. W., Teo, L. T., Chua, Y. Y., Wong, E., & Venkataraman, A. (2020). Reorganising the emergency department to manage the COVID-19 outbreak. International Journal of Emergency Medicine, 13(1), 32. https://doi.org/10.1186/s12245-020-00294-w
Quinn, A., & Brunett, P. (2009). Service versus education: Finding the right balance: A consensus statement from the council of emergency medicine residency directors 2009 academic assembly “Question 19” working group. Academic Emergency Medicine, 16(SUPPL. 2), 15–18. https://doi.org/10.1111/j.1553-2712.2009.00599.x
SGH. (2019). Hospital Overview – Singapore General Hospital. Retrieved August 17, 2020, from https://www.sgh.com.sg/about-us/corporate-profile/Pages/hospital-overview.aspx
COVID-19 (Temporary Measures) Act 2020. (2020). https://sso.agc.gov.sg/Act/COVID19TMA2020
Tajfel, H., Billig, M. G., Bundy, R. P., & Flament, C. (1971). Social categorization and intergroup behaviour. European Journal of Social Psychology, 1(2), 149–178. https://doi.org/10.1002/ejsp.2420010202
Tajfel, H., & Turner, J. C. (1979). An integrative theory of intergroup conflict. In W. G. Austin & S. Worchel (Eds.), The social psychology of intergroup relations (pp. 33–47). Brooks/Cole.
WHO. (2020). IHR emergency committee for pneumonia due to the novel coronavirus 2019-nCoV transcript of a pressing briefing. Retrived January 30, 2020, from https://www.who.int/docs/default-source/coronaviruse/transcripts/ihr-emergency-committee-for-pneumonia-due-to-the-novel-coronavirus-2019-ncov-press-briefing-transcript-30012020.pdf?sfvrsn=c9463ac1_2
Woods, D. (1980). Service and education in residency programs. A question of balance. Canadian Medical Association Journal, 123(1), 44.
*Evelyn Wong
Department of Emergency Medicine,
Singapore General Hospital
Outram Road
Singapore 169608
Email: evelyn.wong@singhealth.com.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









