Examiner training for the Malaysian anaesthesiology exit level assessment: Factors affecting the effectiveness of a faculty development intervention during the COVID-19 pandemic
Submitted: 30 June 2022
Accepted: 31 October 2022
Published online: 4 July, TAPS 2023, 8(3), 26-34
https://doi.org/10.29060/TAPS.2023-8-3/OA2834
Noorjahan Haneem Md Hashim1, Shairil Rahayu Ruslan1, Ina Ismiarti Shariffuddin1, Woon Lai Lim1, Christina Phoay Lay Tan2 & Vinod Pallath3
1Department of Anaesthesiology, Faculty of Medicine, Universiti Malaya, Malaysia; 2Department of Primary Care Medicine, Faculty of Medicine, Universiti Malaya, Malaysia; 3Medical Education Research & Development Unit, Dean’s Office, Faculty of Medicine, Universiti Malaya, Malaysia
Abstract
Introduction: Examiner training is essential to ensure the trustworthiness of the examination process and results. The Anaesthesiology examiners’ training programme to standardise examination techniques and standards across seniority, subspecialty, and institutions was developed using McLean’s adaptation of Kern’s framework.
Methods: The programme was delivered through an online platform due to pandemic constraints. Key focus areas were Performance Dimension Training (PDT), Form-of-Reference Training (FORT) and factors affecting validity. Training methods included interactive lectures, facilitated discussions and experiential learning sessions using the rubrics created for the viva examination. The programme effectiveness was measured using the Kirkpatrick model for programme evaluation.
Results: Seven out of eleven participants rated the programme content as useful and relevant. Four participants showed improvement in the post-test, when compared to the pre-test. Five participants reported behavioural changes during the examination, either during the preparation or conduct of the examination. Factors that contributed to this intervention’s effectiveness were identified through the MOAC (motivation, opportunities, abilities, and communality) model.
Conclusion: Though not all examiners attended the training session, all were committed to a fairer and transparent examination and motivated to ensure ease of the process. The success of any faculty development programme must be defined and the factors affecting it must be identified to ensure engagement and sustainability of the programme.
Keywords: Medical Education, Health Profession Education, Examiner Training, Faculty Development, Assessment, MOAC Model, Programme Evaluation
Practice Highlights
- A faculty development initiative must be tailored to faculty’s learning needs and context.
- A simple framework of planning, implementing, and evaluating can be used to design a programme.
- Target outcome measures and evaluation plans must be included in the planning process.
- The Kirkpatrick model is a useful tool to use in programme evaluation: to answer if the programme has met its objectives.
- The MOAC model is a useful tool to explain why a programme has met its objective.
I. INTRODUCTION
Anaesthesiology specialist training in Malaysia comprises a 4-year clinical master’s programme. At the time of our workshop, five local public universities offer the programme. The course content is similar in all universities, but the course delivery may differ to align with each university’s rules and regulations. The summative examinations are held as a Conjoint Examination. Examiners include lecturers from all five universities, specialists from the Ministry of Health and external examiners from international Anaesthesiology training programmes. The examination consists of a written and a viva voce examination. The areas examined are the knowledge and cognitive skills in patient management.
A speciality training programme’s exit level assessment is an essential milestone for licensing. In our programme, the exit examination occurs at the end of the training before trainees practise independently in the healthcare system and are eligible for national specialist registration. Therefore, aligning the curriculum and assessment to licensing requirements is necessary.
Examiners play an important role during this high-stakes summative examination, making decisions regarding allowing graduating trainees to work as specialists in the community. Therefore, examiners must understand their role. In recent years, the anaesthesiology training programme providers in Malaysia have been taking measures to improve the validity of the examination. These include a stringent vetting process to ensure examination content reflects the syllabus, questions are unambiguous, and the examiners agree on the criteria for passing. However, previous examinations revealed that although examiners were clear on the aim of the examination, some utilised different assessment approaches, which were possibly coloured by personal and professional experiences, and thus needed constant calibration on the passing criteria. In addition, during examiner discussions, different examiners were found to have different skill levels in constructing focused higher-order questions and were not fully aware of potential cognitive biases that may affect the examination results.
These insights from previous examinations warranted a specific skill training session to ensure the trustworthiness of the examination process and results (Blew et al., 2010; Iqbal et al., 2010; Juul et al., 2019, Chapter 8, pp. 127-140; McLean et al., 2008). The examiners and the Specialty committee were keen to ensure that these issues were addressed with a training programme that complements the current on-the-job examiner training.
II. METHODS
An examiner training module was developed using McLean’s adaptation of Kern’s framework for curriculum development: Planning, Implementation and Evaluation (McLean et al., 2008; Thomas et al., 2015). A conceptual framework for the examiner training programme was drawn up from the programme’s conception stage to the evaluation of its outcome, as illustrated in Figure 1 (Steinert et al., 2016).
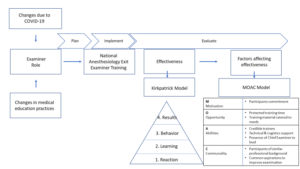
Figure 1: The conceptual framework for the examiner training programme and evaluation of its effectiveness
A. Planning
Three key focus areas were identified for the training programme: (1) Performance Dimension Training (PDT); (2) examiner calibration with Frame-Of-Reference Training (FORT); as well as (3) identifying factors affecting the validity of results and measures that can be taken to prevent them.
1) Performance dimension training (Feldman et al., 2012): The aim was to improve examination validity by reducing examiner errors or biases unrelated to the examinees’ targeted performance behaviours. Finalised marking schemes outlining competencies to be assessed required agreement by all the examiners ahead of time. These needed to be clearly defined and easily understood by all the examiners, and consistency was key to reducing examiner bias.
2) Examiner calibration with Frame-of-Reference Training (FORT) (Newman et al., 2016): Differing levels of experience among all the participants meant that there were differing expectations and performances among them. The examiner training programme needed to assist examiners in resetting expectations and criteria for assessing the candidates’ competencies. This examiner calibration was achieved using pre-recorded simulated viva sessions in which the participants rated candidates’ performances in each simulated viva session and received immediate feedback on their ability and criteria for scoring the candidates.
3) Identifying factors affecting the validity of results (Lineberry, 2019): Factors that may affect the validity of examination results may be related to construct underrepresentation (CU), where the results only reflect one part of an attribute being examined; or construct-irrelevant variance (CIV), where the results are being affected by areas or issues other than the attribute being examined.
An example of CU is sampling issues where only a limited area of the syllabus is examined, or an answer key is limited by the availability of evidence or content expertise.
Examples of CIV include the different ways a concept can be interpreted in different cultures or training centres, ambiguous questions, examiner cognitive biases, examiner fatigue, examinee language abilities, and examinees guessing or cheating. The examiner training programme was designed with the objectives listed in Table 1.
|
Malaysian Anaesthesiology Exit Level Examiner Training Programme |
|
1. Participants should be able to define the purpose and competencies to be assessed in the viva examination. |
|
2. Participants should be able to construct high-order questions (elaborating, probing, and justifying). |
|
3. Participants should be able to agree on anchors on rating scales of examination and narrow the range of ratings for the same encounter everyone observes. |
|
4. Participants should be able to calibrate the scoring of different levels of responses. |
Table 1: Objectives of the Faculty Development Intervention
B. Implementation
The faculty intervention programme was designed as a one-day online programme to be attended by potential examiners for the Anaesthesiology Exit Examination. The programme objectives were prioritised from the needs assessment and designed based on Tekian & Norcini’s recommendations (Tekian & Norcini, 2016). Due to time constraints, training was performed using an online platform closer to the examination dates after obtaining university clearance on confidentiality regarding assessment issues.
The structure and contents of the examiner training programme are outlined in Table 2 and is further elaborated in Appendix A.
|
General content |
Specific content |
|
Lectures |
1. Orientation to the examination regulations, objectives, structure and format of the final examination. |
|
|
2. Ensuring validity of the viva examination: elaborating on the threats present to the process and how to mitigate these concerns. |
|
|
3. Creating high-order questions based on competencies to be assessed and promoting appropriate examiner behaviours through consistency and increasing reliability. |
|
|
4. Utilising marking schemes, anchors and making inferences with:
|
|
Experiential learning sessions |
1. Participants discuss and agree on the competencies to be assessed. 2. Participants work in groups to construct questions based on a given scenario and competencies to be assessed. 3. Participants finalise a rating scale to be used in the examination. 4. Participants observe videos of simulated examination candidates performing at various levels of competencies and rate their performance. The discussion here focused on the similarities and differences between examiners. |
|
Participant feedback and evaluation |
A question-and-answer session is held to iron out any doubts and queries from the participants. |
Table 2: Contents and structure of the examiner training programme
Based on the objectives, the organisers invited a multidisciplinary group of facilitators. The group consisted of anaesthesiologists, medical education experts in assessment and faculty development, and a technical and logistics support team to ensure efficient delivery of the online programme.
A multimodal approach to delivery was adopted to accommodate the diversity of the examiner group (gender, seniority, subspeciality, and examination experience). Explicit ground rules were agreed upon to underpin the safe and respectful learning environment. The educational strategy included interactive lectures, hands-on practice using rubrics created and calibration using video-assisted scenarios. The programme objectives were embedded and reinforced with each strategy. Pre- and post-tests were performed to help participants gauge their learning and assist the programme organisers in evaluating the participants’ learning.
This would be the first time such a programme was held within the local setting. Participants were all anaesthesiologists by profession, were actively involved in clinical duties within a tertiary hospital setting and consented to participate in this programme. As potential examiners, they all had prior experience as observers of the examination process, with the majority having previous experience as examiners as well.
The programme was organised during the peak of the COVID-19 pandemic and was managed on a fully online platform to ensure safety and minimise the time taken away from clinical duties. In addition, participants received protected time for this programme, a necessary luxury as anaesthesiologists were at the forefront of managing the pandemic.
C. Evaluation
The Kirkpatrick model (McLean et al., 2008; Newstrom, 1995;) was used to evaluate the programme’s effectiveness described and elaborated in Figure 2.
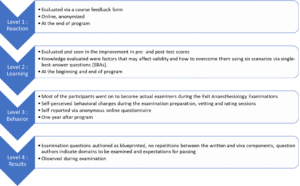
Figure 2: The Kirkpatrick model, elaborated for this programme
The MOAC model (Vollenbroek, 2019), expanded from the MOA (Marin-Garcia & Martinez Tomas, 2016) model by Blumberg & Pringle (Blumberg & Pringle, 1982) was used to examine factors that contributed to the effectiveness of the programme. Motivation, opportunity, ability, and communality are factors that drives action and performance.
III. RESULTS
Eleven participants attended the programme. These participants were examiners for the 2021 examinations from the university training centres and the Ministry of Health, Malaysia. Only one of the participants would be a first-time examiner in the Exit Examination. Four of the would-be examiners could not attend due to service priorities.
A. Level 1: Reaction
Seven of the eleven participants completed the programme evaluation form, which is openly available in Figshare at https://doi.org/10.6084/m9.figshare.20189309.v1 (Tan & Pallath, 2022). All of them rated the programme content as useful and relevant to their examination duties and stated that the content and presentations were pitched at the correct level, with appropriate visual aids and reference materials. The online learning opportunity was also rated as good.
All seven also aimed to make behavioural changes after attending the programme, as indicated below. Some of the excerpts include:
“I am more cognizant of the candidates’ understanding to questions and marking schemes”
“Yes. We definitely need the rubric/marking scheme for standardisation. Will also try to reduce all the possible biases as mentioned in the programme.”
“Yes, as I will be more agreeable to question standardisation in viva examination because it makes it fairer for the candidates.”
The participants also shared their understanding of the importance of standardisation and examiner training and would recommend this programme to be conducted annually. They agreed that the examiner training programme should be made mandatory for all new examiners, with the option of refresher courses for veteran examiners if appropriate.
B. Level 2: Learning
All 11 participants completed the pre-and post-tests. The data supporting these findings of this is openly available in Figshare at https://doi.org/10.6084/m9.figshare.20186582.v1 (Md Hashim, 2021). The participants’ marks in both tests are shown in Appendix B. The areas that showed improvement in scores were identifying why under-sampling is a problem and methods to prevent validity threats. Understanding the source of validity threat from cognitive biases showed a decline in scores (question 2 with scores of 11 to 8 and question 3 with scores of 10 to 8), respectively.
Comparing the post-test scores to pre-test scores, four participants showed improvement, four showed no change (one of the participants answered all questions correctly in both tests) and three participants showed a decline in test scores.
C. Level 3: Behavioural Change
Six participants responded to the follow-up questionnaire, which is openly available in Figshare at https://doi.org/10.6084/m9.figshare.20186591.v2 (Md Hashim, 2022). This questionnaire was administered about a year after the examiner training programme and after the completion of two examinations. Only one respondent did not make any self-perceived behavioural change while preparing the examination questions and conducting the viva examinations. Two respondents did not make any changes while marking or rating candidates.
The specific changes in the three areas of behavioural change that were consciously noted by the respondents were explored. Respondents reported increased awareness and being more systematic in question preparation, making questions more aligned to the curriculum, preparing better quality questions, and being more cognizant of candidates’ understanding of the questions.
They also reported being more objective and guided during marking and rating as the passing criteria were better defined and structured.
Regarding the conduct of the viva examination, respondents shared that they were better prepared during vetting and felt it was easier to rate candidates as the marking schemes and questions were standardised and could ensure candidates could answer all the required questions to pass.
D. Level 4: Results
The examiners who attended the training programme were able to prepare questions as blueprinted and were able to identify areas to be examined and provided recommended criteria for passing each question. This has led to a smooth vetting process and examination.
E. Factors Affecting Effectiveness
Even though the programme was not attended by all the potential examiners, those who did were committed to the idea of a fairer and more transparent examination process. This formed the motivation aspect of the model.
In terms of opportunity, protected training time is important, followed by prioritising the content of the training material according to the most pressing needs.
The ability aspect encompassed the abilities of the facilitators and participants. To emphasise the learning process, credible trainers were invited to this programme to facilitate the lectures and experiential learning sessions. In this aspect, the Faculty Development team comprised an experienced clinician, a basic medical scientist, and an anaesthesiologist, all with medical education qualifications and were vital in ensuring the success of this programme. The whole team was led by the Chief Examiner who focused on the dimensions to be tested and calibrated, while simultaneously managing the expectations of the examiners and their abilities to give and accept feedback. Communication and the skill to be receptive to the proposed changes were also crucial to make the intervention work.
In terms of communality, all the participants were of similar professional backgrounds and shared the common realisation that this training programme was essential and would only yield positive results. Hence this ensured the programme’s overall success.
IV. DISCUSSION
The progressive change seen in this attempt to improve the examination system is aligned with the general progress in medical education. Training of examiners is important (Holmboe et al., 2011), as it is not the tool used for assessment, but rather the person using the tool, that makes the difference. As it is difficult to design the ‘perfect tool’ for performance tests and redesigning a tool only changes 10% of the variance in rating (Holmboe et al., 2011; Williams et al., 2003), educators must now train the faculty in observation and assessment. It is not irrational to extrapolate this effect on written and oral examinations. Holmboe et al. (2011) also share the reasons for a training programme for assessors, which are changing curriculum structure, content and delivery and emerging evidence regarding assessment, building a system reserve, utilising training programmes as opportunities to identify and engage change agents and allow the faculty to form a mental picture of how changes will affect them and improve practice. Enlisting the help and support of a respected faculty member during training will promote the depth and breadth of change.
Khera et al. (2005) described their paediatric examination experiences, in which the Royal College of Paediatrics and Child Health defined examiners’ competencies, selection process and training programme components. The training programme included principles of assessment, examination design, writing questions, interpersonal skills, professional attributes, managing diversity, and assessing the examiners’ skills. They believe these contents will ensure the assessment is valid, reliable, and fair. As Anaesthesiology examiners have different knowledge levels and experiences, it had been crucial to assess their learning needs and provide them with appropriate learning opportunities.
In the emergency brought on by the COVID-19 pandemic, online training was the safest and most feasible platform for conducting this programme. Online faculty development activities have the perceived advantages of being convenient, flexible, and allowing interdisciplinary interaction and providing an experience of being an online student(Cook & Steinert, 2013). Forming the facilitation team together with the dedicated technical and logistics team and creating a chat group prior to conducting the programme were key in anticipating and handling communication and technical issues (Cook & Steinert, 2013).
Though participants were engaged and the results of the workshop were encouraging, the programme delivery and the content will be reviewed based on the feedback received. The convenience of an online activity must be balanced with the participant engagement and facilitator presence of a face-to-face-activity. Since the results of both methods of delivery differs (Arias et al., 2018; Daniel, 2014; Kemp & Grieve, 2014), the best solution may to ask the participants what would best work for them, as they are adult learners and experienced examiners. The programme must be designed with participants involvement, with opportunities to participate and engaging facilitators and support teams that would be able to support the participants’ learning need (Singh et al., 2022).
At the end of the programme, the effectiveness of the programme was measured by referencing the Kirkpatrick model. The Kirkpatrick model (Newstrom, 1995; Steinert et al., 2006) was the most helpful in helping us identify the success of the intervention, which included behavioural change. Measuring behavioural change and impact on the examination results, organisational changes and changes in student learning may be difficult and may not be directly caused by a single intervention (McLean et al., 2008). The key, is perhaps to involve examiners, students and other stakeholders in the evaluation process, using various validated tools, and to ensure that the effort is ongoing, with sustained support, guidance and feedback (McLean et al., 2008).
To explain the overall effectiveness of the programme (with regards to reaction, learning and behavioural change), the MOAC model (Vollenbroek, 2019) expanded from the original MOA model was used. The MOAC model not only describes factors that affect an individual’s performance in a group, but also the group behaviour.
Motivation is an important driving force of action, and members are more motivated when a subject becomes relevant on a personal level, leading to action. The motivation to be informed and to improve has led to active participation in the knowledge sharing session, processing new information presented in the programme and adopting changes learnt during the programme. Presence of a group of motivated individuals with the same goals supported each other’s learning.
Opportunity, especially time, space and resources, must be allocated to reflect the value and relevance of any activity. Work autonomy, allows professionals to engage in what they consider relevant or important, and be accountable for their work outcomes. Facilitating conditions, for example, technology, facilitators, and a platform to practise what is being learnt are also important aspects of opportunity. Allowing protected time with the appropriate facilitating conditions, indicates institutional support and has enabled participants to fully optimise the learning experience.
Ability positively affects knowledge exchange and willingness to participate. Having prior knowledge improves a participant’s ability to absorb and utilise new knowledge. The programme participants, being experienced clinical teachers and examiners are fully aware of their capabilities and are able to process and share important information. Experienced faculty development facilitators who are also clinical teachers and examiners were able to identify areas to focus and provide relevant examples for application.
Communality is the added dimension to the original MOA model. Participants of this programme are members in a complex system, who already know each other. Having shared identity, language and challenges have allowed them to develop trust while pursuing the common goal of improving the system they were working in. This facilitated knowledge sharing and behavioural change.
The limitation in our programme is the small sample size. However, we believe that is important to review the effectiveness of a programme, especially with regards to behavioural change, and to share how other programmes can benefit from using the frameworks we shared. The findings from this programme will also inform how we conduct future faculty development programmes. With pandemic restrictions lifted, we hope to conduct this programme face-to-face, to facilitate engagement and communication.
V. CONCLUSION
For this faculty development programme to succeed, targets for success must first be defined and factors that contribute to its success need to be identified. This will ensure active engagement from the participants and promote the sustainability of the programme.
Notes on Contributors
Noorjahan Haneem Md Hashim designed the programme, assisted in content creation, curation and matching learning activities, moderated the programme, and conceptualised and wrote this manuscript.
Shairil Rahayu Ruslan participated as a committee of the programme, assisted as a simulated candidate during the training sessions, as well as contributed to the conceptualisation, writing, and formatting of this manuscript. She also compiled the bibliography and cross-checked the references for this manuscript.
Ina Ismiarti Shariffuddin created the opportunity for the programme (Specialty board and interdisciplinary buy-in, department funding), prioritised the programme learning outcomes, chaired the programme, and contributed to the writing and review of this manuscript.
Woon Lai Lim participated as a committee member of the programme and contributed to the writing of this manuscript.
Christina Phoay Lay Tan designed and conducted the faculty development training programme, and reviewed and contributed to the writing of this manuscript. She also cross-checked the references for this manuscript.
Vinod Pallath designed and conducted the faculty development training programme, and reviewed and contributed to the writing of this manuscript.
All authors verified and approved the final version of the manuscript.
Ethical Approval
Ethical approval was applied for the follow-up questionnaire that was distributed to the participants, which was approved on the 6th of May 2022 (Reference number: UM.TNC2/UMREC_1879). The programme evaluation and pre- and post-tests are accepted as part of the programme evaluation procedures.
Data Availability
De-identified individual participant data collected are available in the Figshare repository immediately after publication without an end date, as below :
https://doi.org/10.6084/m9.figshare.20189309.v1
https://doi.org/10.6084/m9.figshare.20186582.v1
https://doi.org/10.6084/m9.figshare.20186591.v2
The authors confirm that all data underlying the findings are freely available for view from the Figshare data repository. However, the reuse and resharing of the programme evaluation form, pre- and posttest questions, as well as followup questionnaire, despite being easily accessible from the data repository, should warrant a reasonable request from the corresponding author out of courtesy.
Acknowledgement
The authors would like to acknowledge Dr Selvan Segaran and Dr Siti Nur Jawahir Rosli from the Medical Education, Research and Development Unit (MERDU) for their logistics and technical support in all stages of this programme; Professor Dr Jamuna Vadivelu, Head, MERDU for her insight and support; Dr Nur Azreen Hussain and Dr Wan Aizat Wan Zakaria from the Department of Anaesthesiology, UMMC and UM, for their acting skills in the training videos; and the Visibility and Communication Unit, Faculty of Medicine, Universiti Malaya for their video editing services.
Funding
There is no funding source for this manuscript.
Declaration of Interest
There are no conflicts of interest among the authors of this manuscript.
References
Arias, J. J., Swinton, J., & Anderson, K. (2018). Online vs. face-to-face: A comparison of student outcomes with random assignment. E-Journal of Business Education & Scholarship of Teaching, 12(2), 1–23. https://eric.ed.gov/?id=EJ1193426
Blew, P., Muir, J. G., & Naik, V. N. (2010). The evolving Royal College examination in anesthesiology. Canadian Journal of Anesthesia/Journal canadien d’anesthésie, 57(9), 804-810. https://doi.org/10.1007/s12630-010-9341-1
Blumberg, M., & Pringle, C. D. (1982). The missing opportunity in organizational research: Some implications for a theory of work performance. The Academy of Management Review, 7(4), 560–569. https://doi.org/10.2307/257222
Cook, D. A., & Steinert, Y. (2013). Online learning for faculty development: A review of the literature. Medical Teacher, 35(11), 930–937. https://doi.org/10.3109/0142159X.2013.827328
Daniel, C. M. (2014). Comparing online and face-to-face professional development [Doctoral dissertation, Nova Southeastern University]. https://doi.org/10.13140/2.1.3157.5042
Feldman, M., Lazzara, E. H., Vanderbilt, A. A., & DiazGranados, D. (2012). Rater training to support high-stakes simulation-based assessments. Journal of Continuing Education in the Health Professions, 32(4), 279–286. https://doi.org/10.1002/chp.21156
Holmboe, E. S., Ward, D. S., Reznick, R. K., Katsufrakis, P. J., Leslie, K. M., Patel, V. L., Ray, D. D., & Nelson, E. A. (2011). Faculty development in assessment: The missing link in competency-based medical education. Academic Medicine, 86(4), 460–467. https://doi.org/10.1097/ACM.0b013e31820cb2a7
Iqbal, I., Naqvi, S., Abeysundara, L., & Narula, A. (2010). The value of oral assessments: A review. The Bulletin of the Royal College of Surgeons of England, 92(7), 1–6. https://doi.org/10.1308/147363510×511030
Juul, D., Yudkowsky, R., & Tekian, A. (2019). Oral Examinations. In R. Yudkowsky, Y. S. Park, & S. M. Downing (Eds.), Assessment in Health Professions Education. Routledge. https://doi.org/10.4324/9781315166902-8
Kemp, N., & Grieve, R. (2014). Face-to-face or face-to-screen? Undergraduates’ opinions and test performance in classroom vs. online learning. Frontiers in Psychology, 5. https://doi.org/10.3389/fpsyg.2014.01278
Khera, N., Davies, H., Davies, H., Lissauer, T., Skuse, D., Wakeford, R., & Stroobant, J. (2005). How should paediatric examiners be trained? Archives of Disease in Childhood, 90(1), 43–47. https://doi.org/10.1136/adc.2004.055103
Lineberry, M. (2019). Validity and quality. Assessment in Health Professions Education, 17-32. https://doi.org/10.4324/9781315166902-2
Marin-Garcia, J. A., & Martinez Tomas, J. (2016). Deconstructing AMO framework: A systematic review. Intangible Capital, 12(4), 1040. https://doi.org/10.3926/ic.838
McLean, M., Cilliers, F., & Van Wyk, J. M. (2008). Faculty development: Yesterday, today and tomorrow. Medical Teacher, 30(6), 555–584. https://doi.org/10.1080/01421590802109834
Md Hashim, N. H. (2021). Pre- and Post-test [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.20186582.v1
Md Hashim, N. H. (2022). Followup Questionnaire [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.20186591.v2
Newman, L. R., Brodsky, D., Jones, R. N., Schwartzstein, R. M., Atkins, K. M., & Roberts, D. H. (2016). Frame-of-reference training: Establishing reliable assessment of teaching effectiveness. Journal of Continuing Education in the Health Professions, 36(3), 206–210. https://doi.org/10.1097/CEH.0000000000000086
Newstrom, J. W. (1995). Evaluating training programs: The four levels, by Donald L. Kirkpatrick. (1994). San Francisco: Berrett-Koehler. 229 pp., $32.95 cloth. Human Resource Development Quarterly, 6(3), 317-320. https://doi.org/10.1002/hrdq.3920060310
Singh, J., Evans, E., Reed, A., Karch, L., Qualey, K., Singh, L., & Wiersma, H. (2022). Online, hybrid, and face-to-face learning through the eyes of faculty, students, administrators, and instructional designers: Lessons learned and directions for the post-vaccine and post-pandemic/COVID-19 World. Journal of Educational Technology Systems, 50(3), 301–326. https://doi.org/10.1177/00472395211063754
Steinert, Y., Mann, K., Anderson, B., Barnett, B. M., Centeno, A., Naismith, L., Prideaux, D., Spencer, J., Tullo, E., Viggiano, T., Ward, H., & Dolmans, D. (2016). A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Medical Teacher, 38(8), 769-786. https://doi.org/10.1080/0142159x.2016.1181851
Steinert, Y., Mann, K., Centeno, A., Dolmans, D., Spencer, J., Gelula, M., & Prideaux, D. (2006). A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Medical Teacher, 28(6), 497–526. https://doi.org/10.1080/01421590600902976
Tan, C. P. L., & Pallath, V. (2022). Workshop Evaluation Form [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.20189309.v1
Tekian, A., & Norcini, J. J. (2016). Faculty development in assessment : What the faculty need to know and do. In M. Mentkowski, P.F. Wimmers (Eds.), Assessing Competence in Professional Performance across Disciplines and Professions (1st ed., pp. 355–374). Springer Cham. https://doi.org/10.1007/978-3-319-30064-1
Thomas, P. A., Kern, D. E., Hughes, M. T., & Chen, B. Y. (2015). Curriculum development for medical education : A six-step approach. John Hopkins University Press. https://jhu.pure.elsevier.com/en/publications/curriculum-development-for-medical-education-a-six-step-approach
Vollenbroek, W. B. (2019). Communities of Practice: Beyond the Hype – Analysing the Developments in Communities of Practice at Work [Doctoral dissertation, University of Twente]. https://doi.org/10.3990/1.9789036548205
Williams, R. G., Klamen, D. A., & McGaghie, W. C. (2003). SPECIAL ARTICLE: Cognitive, social and environmental sources of bias in clinical performance ratings. Teaching and Learning in Medicine, 15(4), 270–292. https://doi.org/10.1207/S15328015TLM1504_11
*Shairil Rahayu Ruslan
50604, Kuala Lumpur,
Malaysia
03-79492052 / 012-3291074
Email: shairilrahayu@gmail.com, shairil@ummc.edu.my
Submitted: 23 August 2022
Accepted: 3 January 2023
Published online: 4 July, TAPS 2023, 8(3), 15-25
https://doi.org/10.29060/TAPS.2023-8-3/OA2871
Iroro Enameguolo Yarhere1, Tudor Chinnah2 & Uche Chineze3
1Department of Paediatrics, College of Health Sciences, University of Port Harcourt, Nigeria; 2Department of Anatomy, University of Exeter, United Kingdom; 3Department of Education and Curriculum studies, University of Port Harcourt, Nigeria
Abstract
Introduction: This study aimed to compare the paediatric endocrinology curriculum across Southern Nigeria medical schools, using reports from learners. It also checked the learners’ perceptions about different learning patterns and competency in some expected core skills.
Methods: This mixed (quantitative and qualitative) study was conducted with 7 medical schools in Southern Nigeria. A multi-staged randomized selection of schools and respondents, was adopted for a focus group discussion (FGD), and the information derived was used to develop a semi-structured questionnaire, which 314 doctors submitted. The FGD discussed rotation patterns, completion rates of topics and perceptions for some skills. These themes were included in the forms for general survey, and Likert scale was used to assess competency in skills. Data generated was analysed using statistical package for social sciences, SPSS 24, and p values < 0.05 were considered significant
Results: Lectures and topics had various completion rates, 42.6% – 98%, highest being “diabetes mellitus”. Endocrinology rotation was completed by 58.6% of respondents, and 58 – 78 % perceived competency in growth measurement and charting. Significantly more learners, 46.6% who had staggered posting got correct matching of Tanner staging, versus learners who had block posting, 33.3%, p = 0.018.
Conclusion: Respondents reported high variability in the implementation of the recommended guidelines for paediatric endocrinology curriculum between schools in Southern Nigeria. Variabilities were in the courses’ completion, learners’ skills exposure and how much hands-on were allowed in various skills acquisitions. This variability will hamper the core objectives of human capital development should the trend continue.
Keywords: Paediatric Endocrinology Curriculum, Perception, Compliance, Completion Rate, Learners
Practice Highlights
- Medical and dental council of Nigeria has a recommended benchmark for minimum academic standards in all medical schools to which total compliance is expected.
- Evaluation of paediatric endocrinology curriculum content and training methods was conducted using reports from learners.
- Variability in the content, and training methods of the intended competency were reported across medical schools.
- Compliance rate of the recommended curriculum was less than 50% in some contents and some learners reported low skill performance training.
- The lack of uniformity can prevent achievement of the overarching objective of the curriculum in Nigeria with wide variations in competence among graduating doctors.
I. INTRODUCTION
The primary aim of the Medical and Dental council of Nigeria (MDCN) undergraduate curriculum is “to train doctors and dentists who can work effectively in a health team to provide comprehensive health care to individuals in any community in the nation, and keep up to date on issues of global health” (Federal Ministry of Health of Nigeria, 2012). In Nigeria today, there are 49 federal, 59 states and 111 private universities, and 44 of these have full or partially accredited medical schools and while these schools have a prescribed curriculum, some are not following explicitly (Federal Ministry of Health of Nigeria, 2012). This curriculum advocates for universities to develop syllabus to meet the benchmark for minimum academic standards (BMAS) across schools, however there is no uniform template developed for assessing graduates to know how their competence converge as is applicable in United States of America (USA), Canada and United Kingdom (UK) (Santen et al., 2019; Shah et al., 2020; Sosna et al., 2021). Diabetes mellitus, thyroid disorders, puberty, rickets and growth abnormalities are topics included in the MDCN paediatric curriculum under endocrinology which learners are expected to acquire competence in cognitive and psychomotor skills to diagnose and treat or refer appropriately children presenting with these diseases.
A. Problem
Most deaths from diseases in Nigeria and other resource-limited countries are consequent upon general public ignorance of disease, late presentation to the health care systems, poverty and lack of funds to access healthcare facilities and reduced knowledge of some disease patterns by the healthcare providers (Yarhere & Nte, 2018). Addressing the gaps in reduced knowledge can be done by developing competency-based curriculum for all graduating doctors to have as near-similar competence as possible but achieving this may not be feasible. Training activities are not uniform throughout medical schools in Nigeria and elsewhere, and depend on schools’ vision, mission and objectives, and the structures and processes put in place. There are barriers to positive implementation across schools including but not limited to individual school’s determination of what is relevant in the curriculum, access to the materials needed to teach the curriculum content and getting trainers to use these curriculums (Polikoff, 2018). The lack of uniformity of curriculum across universities may not be contending issues, but when the graduating doctors have varying degree of competencies in skills and cognition, then a template for imparting uniform and up to date knowledge and to evaluate this is needed to find ways of reducing the variability (McManus, 2003; McManus et al., 2020; Rimmer, 2014).
The curriculum uniformity across schools is one way of improving competency and thus, healthcare standards, and there is need to explore this uniformity or diversity within the paediatric undergraduate training. In some countries, there is a uniform board certification examination before doctors can practice and this is also done for doctors immigrating into these countries (Hohmann & Tetsworth, 2018; Puri et al., 2021; Tiffin et al., 2017; van Zanten et al., 2022) but Nigeria is exempt from this uniform exit examination. This uniform exit board examination makes these schools align course contents, and therefore reduces the variabilities between medical schools and undergraduate training.
B. Curriculum Evaluation for Change or Improvement
Curriculum evaluation is a means by which educators understand whether the curriculum used to train learners is working as intended, and whether there is need to change the entire programme or redesign aspects (Burton & McDonald, 2001; Ornstein & Hunkins, 2009). It is also a way of identifying deficiencies in training syllabus across universities, (Rufai et al., 2016) or whether compliance to a curriculum is being achieved (Grant, 2014; Olson et al., 2000). Kirkpatrick’s curriculum evaluation method is widely acceptable in medical education using the 4 steps; learners’ reaction or satisfaction, knowledge, behavioural changes and results or impact, and in Nigeria, for paediatric endocrinology, this has not been done (Alsalamah, 2021; Bates, 2004).
Universities have variabilities in organisation, students’ numbers in classes, duration of specific posting, posting types and whether the courses are elective or core. In medical schools in Nigeria, paediatric postings are undertaken in the 5th or 6th year of a 6-year programme. While some stagger the posting to be done within the last 2 years, others do theirs in the 5th or the 6th year exclusively, and the extent of these variabilities and how they affect the training processes and products has not been evaluated in Nigeria and this can be done using learners’ or graduates’ perceptions.
The aim of this research was to evaluate learners’ report and perception of some aspects of the paediatric endocrinology curriculum contents and learning methods across Southern Nigeria medical schools. Endocrinology was taken from the paediatric course to reduce the volume of information to be analysed.
II. METHODS
This was a cross sectional study design with qualitative and quantitative data analyses, evaluating learners’ report and their perception of the curriculum being used by various medical schools in Southern Nigeria to deliver the MDCN paediatric endocrinology curriculum. Survey was conducted across 10 medical schools in Southern Nigeria that have learners who have either completed their final year, or are doing their internship. Two steps were used to retrieve the information needed; a focus group discussion of sampled learners, and a questionnaire survey sent out to randomly selected respondents and these 2 methods complemented each other. The focus group discussion was used to explore in depth, the minds of the respondents and what they perceived was being done well and what needed to be changed in the syllabus in their respective schools. The questionnaire survey was then used to collect reports and perceptions from a wider set of learners who had completed their paediatric posting within the past 6 – 12 months. Some of these were already doing their internship and others were in their final year in preparation for their final examinations.
Sample size for respondents will be calculated using the formula:
N = (Z score)2 x SD x (1 – SD)
(CI)2
Z score = 1.96, SD (standard deviation of the mean) = estimated at ± 0.5, Confidence interval = 0.05
= 384 respondents, with an attrition rate of 10% will be added 10% of 384 = 38
384 + 38 = 422 respondents.
A. Sampling Technique
Multi-staged sampling technique was used to determine the schools, and respondents that participated in the study. There are 29 Southern Universities with medical / health colleges and 16 of these had more than 50 learners in their final year or had graduated. Ten schools were randomly selected using the excel formula [= rand ()], and a proportionate stratified sampling was done using the matriculation numbers of the students in each school to arrive at 422 respondents. Total number of learners that studied paediatrics in various institutions was 800; Ibadan 150, Port Harcourt, 128, Lagos 128, Niger delta University 69, UNN Enugu 128, University of Benin 128, Others 69. From the total number of learners in each school, selected learners and interns were sent the questionnaire using their email addresses. Selection for the FGD was done using simple random sampling from each school and these were sent separate emails with details for the meeting.
B. Focus Group Discussions Process
Focus group discussion was conducted with the respondents using zoom video platform, and the process lasted for 2 hours, 30 minutes. Ten learners’ representatives from the selected schools were contacted for this FGD, however, 7 (70%) agreed to participate after several email reminders. The interview was semi-structured with a flexible topic guide, which covered issues relating to the respondents’ views and opinions on the curriculum in paediatric endocrinology; description of posting type in each school, whether block, or staggered, topics received and/or completed, perception of their competence in a key psychomotor skill. The focus group interview discussions were recorded in the zoom meeting platform and transcribed verbatim. The data were analysed using the thematic framework content analyses method. The themes generated were categorised into; 1. Lecture contents and completion rate, 2. Types of paediatric rotation and posting, 3. Skill competence acquisition and clinical postings. Their perceptions about these themes were also sought and discussed. The transcription of the groups’ discussions was reviewed by IY and TC to help categorise the data and pull-out important quotes used.
C. Questionnaire Survey
Following thematic analyses of the FGD, the themes generated were converted to questions in a survey for a larger sample population. Themes generated were the type of paediatric posting, rotations through units in the departments and paediatric endocrinology topics, training methods and competency acquired. Demographic characteristics of responders such as level/year of study, age, gender and university of study were collected. The respondents were also asked to select topics from a poll, included in their paediatric endocrinology syllabus, with result in Figure 1, and to state the various methods used to learn growth and growth disorders in their schools. A means of assessing cognitive (recall) skills of the learners was conducted using animated pictures of Tanner staging and matching-type multiple choice, and the responses were crossmatched with the type of posting learners were exposed to, i.e. block posting or staggered posting. Tanner staging was chosen as it cuts across general paediatrics and endocrinology as part of growth and puberty (endocrinology).
Data retrieved were analysed statistically by using chi-square test, and Pearson correlation for categorical variables. The level of competence perceived by learners in height measurement and charting on growth chart was retrieved using 5-point Likert scale (where 1 = not competent; 2 = low competence; 3 = neutral; 4 = competent; and 5 = proficient). The association between level of competence and whether learners rotated through paediatric endocrinology was checked using Pearson’s correlation test. For all statistics, p value < 0.05 was considered significant.
D. Ethics
The research commenced after the Research Ethics committee of the University of Port Harcourt granted approval (UPH/CEREMAD/REC/MM80/056). Verbal informed consent was obtained from the participants during the focus group discussion, who also gave consent for video and recording of the process. Informed consent was also obtained from all participants who filled and submitted the online survey. The focus group discussants received N3,000 ($10) for internet data only as monetary compensation.
III. RESULTS
There were 314 learners from the 422 calculated sample size, responded to the questionnaire survey, giving a response rate of 74.4%. There were more final year respondents than early career doctors and more of the respondents were in the age bracket 20 – 24 years, with a mean of 25.02 ±2.71 years. The male: female ratio was 1:1.01, and the data that support the findings of this study are available in Figshare at https://doi.org/10.6084 /m9.figshare.20730937.v1 (Yarhere et al., 2022).
|
RESPONDENTS |
Frequency |
Percentage |
|
|
Year of study |
|
|
|
|
Early career doctor (graduate/intern) |
130 |
41.4 |
p = 0.002 |
|
Final year |
184 |
58.6 |
|
|
University attended (calculated cohort) |
|
|
|
|
University of Port Harcourt (63) |
62 |
19.7 |
|
|
Niger Delta University (54) |
54 |
17.2 |
|
|
University of Ibadan (76) |
50 |
15.9 |
|
|
University of Benin (65) |
44 |
14.0 |
|
|
University of Lagos (65) |
40 |
12.7 |
|
|
University of Nigeria (65) |
42 |
13.4 |
|
|
Other western Universities (34) |
22 |
7.0 |
|
|
Age |
|
|
|
|
20-24 |
140 |
44.6 |
|
|
25-29 |
162 |
51.6 |
|
|
>=30 |
12 |
3.8 |
|
|
Mean |
25.02 ± 2.71 |
|
|
|
Gender |
|
|
|
|
Male |
152 |
48.4 |
p = 0.612 |
|
Female |
162 |
51.6 |
|
Table 1. Demographic characteristics of all respondents and the universities attended
A. Evaluating Contents of Lecture Topics and Completion of Lectures
The syllabus lecturers use to teach courses are supposed to be descriptive with all learning outcomes stated in the handbook or in the log books given to them before the start of the academic year. The prescribed topics for paediatric endocrinology as stated below were not completely taught to learners or learners did not attend the lectures. In the discussion, some agreed that they did not have the full complement of lectures suggested by the BMAS. One respondent said she and her group mates did not receive diabetes mellitus lectures in their final paediatric posting. This fact was corroborated in the questionnaire survey as 2% of the respondents revealed not having diabetes mellitus lectures, and more than 40% did not learn genetics in their paediatric endocrinology training as shown in Figure 1.
Diabetes had almost 100% lecture recipient while genetic had the least. In some schools, genetics were placed under endocrine disorders while in others, genetics were left for the pathology and basic medicine classes.
“I was taught, I personally received 4 lectures in Paed Endo including ambiguous genitalia, “CAH” congenital adrenal hyperplasia, hypothyroidism, and puberty.”
Participant 3
“So, you did not get to do calcium and rickets?”
Facilitator
“No, I was not taught calcium and rickets.”
Participant 3
“What about growth and short stature?”
Facilitator
“Yes, I received introductory lectures in my young (sic), junior posting, yes I did in my 400 level, but not in my senior posting and it was not part of endocrinology but general paediatrics.”
Participant 3
“I did not take lectures in diabetes mellitus because it was rescheduled several times until we finally had to sit for our exams. In the end, many of us just took notes from our seniors and other students who had theirs when it was scheduled.”
Participant 2
“Why were the classes rescheduled? I mean what did the lecturer tell you?”
Facilitator
“The lecturer kept traveling or was indisposed most of our time in the senior posting.”
Participant 2
Participant 4 shared:
Dr. xxxxxx taught us diabetes mellitus and the topic was quite extensive. We learnt the different types, pathophysiology, aetiology, DKA, precipitating factors, risk factors, management. Our lecturers even made us do presentations on DKA, we monitored patients that were being managed for DKA, checking their urine samples for ketones, glucose and their blood pressure.
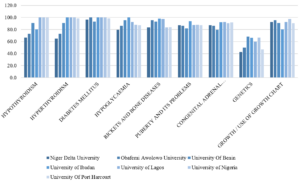
Figure 1: Percentage of learners in various schools who received/attended specific endocrinology lectures in their universities
B. Types of Paediatric Posting and Rotation and Perception of Learners Relating to Task Completion
There were basically 2 modes of paediatric posting in the institutions sampled; 4-months block posting where respondents have a month of didactic lectures and 3 months of clinical rotations through various units in the Paediatric departments, and 4 months of staggered rotations with junior and senior postings in the clinical classes. While some learners rotated through all the units (core and electives) in the departments, some went through core units, emergency and neonatal units, and 2 other units randomly selected for the respondents by the departments.
C. Learners’ Responses to Rotation through Paediatrics and Posting Types
Participant 2 shared:
The way it works in University of xxxx, we rotate through 2 elective postings with core (CHEW and SCBU) postings in the junior and senior postings. These elective postings are randomly selected by the department (meaning heads or coordinators). I did neurology and gastroenterology in my junior posting and haemato-oncology and I really can’t remember the other one in my senior posting.
“Will I be wrong to say you did not see a patient with Diabetic keto acidosis?”
Facilitator
“I saw a child with diabetic keto acidosis in the ward but it wasn’t my unit managing the patient. I only went to the ward to do some other thing.”
Participant 2
“If you were given the opportunity to design a curriculum or programme for your university, will you prefer what is being practiced now, or will you rather have every student go through every unit and get titbits from each unit?”
Facilitator
Participant 2 responded:
Yes, I will prefer that situation where you get to be exposed to every unit in the department but …. emmm, that creates a problem because you may be in a unit for a week, and no patient comes in but the next group rotating to the unit gets to see many patients. I would want to suggest that perhaps, instead of focusing on more of clinical posting, that a unified tutorial class which will expose everyone to the core diseases in the various disciplines.
Table 2 corroborates the information given by the focus group discussants. Testing the competency outcome in either method can give some estimated guess as to which is better, however, there are several confounding factors that will not allow fair comparison (See Table 3).
|
Variable |
Frequency |
Percent (%) |
|
|
Paediatric posting in your university |
|
|
|
|
Staggered posting into Junior and senior paediatrics |
176 |
56.1 |
c2 = 4.59, |
|
Block posting of 4 months total |
138 |
43.9 |
p = 0.032 |
|
Paediatric rotations through various units in universities |
|
|
|
|
I rotated through all units in the department |
162 |
51.6 |
c2 = 0.318, |
|
I rotated through CHEW, neonatal unit, and 2/3 other units |
152 |
48.4 |
p = 0.573 |
|
Rotate through paediatric endocrinology unit in your university |
|
|
|
|
Yes |
184 |
58.6 |
c2 = 7.48, |
|
No |
130 |
41.4 |
p = 0.006 |
Table 2. Paediatric posting and unit rotations in the departments (n=314)
Though there were differences in the mode of paediatric postings where staggered or block, c2 = 4.59, p = 0.032. the difference in proportion of respondents who had core and selected elective posting as against all units posting was not significant, c2 = 0.318, p = 0.573.
|
|
Block posting of 4 months |
Staggered junior and senior paediatrics |
|
|
Correct |
Count |
46 |
82 |
|
% within paediatric posting |
33.3% |
46.6% |
|
|
% of Total |
14.6% |
26.1% |
|
|
Wrong |
Count |
92 |
94 |
|
% within paediatric posting |
66.7% |
53.4% |
|
|
% of Total |
29.3% |
29.9% |
|
|
Total |
Count |
138 |
176 |
|
% within correct response |
43.9% |
56.1% |
|
|
% of Total |
43.9% |
56.1% |
|
Table 3: Comparing correct response to animated picture of Tanner stage (pubic hair) in females, and the type of paediatric rotation learners were exposed to
In the 2×2 table above where recall was tested in the learners based on their paediatric posting type, higher percentage of those who had staggered posting got the correct matching of Tanner stage, and the difference was significant, c2 = 5.630, p = 0.018. However, the total number of respondents with the correct response was low.
D. Perception of Core Competency Skill in Growth Measurement and Charting by Learners
One of the most important courses in paediatrics is growth and development and training future medical doctor to acquire skills and competence in growth and management is a key component of the BMAS. While growth measurement may seem easy to the uninformed, the whole task is daunting especially in children with complex growth abnormalities and malformation, and for more complex skills like arm span. Which of the more complex skills should the learner be expected to be competent in, will be debated in an expert forum of trainers.
“So, did you do anthropometric measures?”
Facilitator
Participant 1 shared:
Yes, anytime we clerk a patient, we must check the weight and height and interpret using age-appropriate charts, but we did not plot them in the charts. We carry the age-appropriate chart and interpreted our patients, as this is a requirement.
Using the chart may not be emphasised by all paediatric lecturers, so learners can be smart to know those lecturers who will request this skill from them during the clerkship period or the unit rotations.
“We did not quite get the concept of mid parental height, height percentile, it was just mentioned in passing. I never saw a severely short child that needed growth hormone. I was only told by a classmate of mine.”
Participant 3
The charting and interpretation of weight and height measurements of children was not done in all schools as shown in Table 4 below, which tells that only 65.8% of total respondents were taught interpretation of measured and charted growth parameters. The level of competence in these tasks will also be varied as seen in Appendix 1. Two hundred and thirty-eight (75.8%) learners perceived they had competency/ proficiency in height measures using stadiometer, and 44.6 % of the learners with these perceptions actually had paediatric endocrinology clinical rotation (Appendix 1).
|
Variable |
Frequency n = 314 |
Percent (%) |
|
How was growth and growth disorders taught in your school (Multiple response applicable) |
|
|
|
Didactic lectures |
272 |
86.6 |
|
Measurement of children using standardised stadiometer |
230 |
73.2 |
|
Charting of growth measurements in CDC/WHO growth charts |
203 |
64.6 |
|
Measurement of children using improvised height rules |
157 |
50.0 |
|
Interpretation of measured and charted growth parameters |
203 |
64.6 |
|
Ward clerkship and presentation |
230 |
73.2 |
|
Measurements of children using bathroom spring balance |
140 |
44.6 |
|
Use of bone age X radiographs |
78 |
24.8 |
|
Use of orchidometer |
90 |
28.6 |
Table 4: Methods used to teach growth and growth disorders in various institutions
Bone age and orchidometers are used to assess skeletal maturation and puberty, which are advanced for the undergraduate learners and certainly not compulsory, but some respondents were taught with the tools showing the variabilities in contents and skills delivery between these schools. From Table 4 above, framers of the syllabus for endocrinology aspect of paediatrics curriculum are unlikely to include use of orchidometer and bone age during the undergraduate paediatric endocrinology rotation as the skill is complex, and not necessary for their level of development.
IV. DISCUSSION
This study has highlighted differences in course contents and training methods across medical schools in Southern Nigeria. While many schools have used the BMAS prescribed by the MDCN, the syllabus used are different and the intended learning outcomes are diverse based on the respondents’ reports. Some learners reported not having diabetes lectures in their school through no fault of theirs, as lecturer rescheduled the lectures and never gave them. While learners have the responsibility to attend lectures, trainers are also obligated to be present at their scheduled lectures or transfer this to their teacher-assistants, or use technologies (Grant, 2014; Ruiz et al., 2006). Some learners had little participation in the Emergency Room, others participated fully in DKA management, learning empathy, specialised skills and communication. The intended competencies to be acquired can be achieved through shadowing and participation, bed-side teaching, and tutorial to improve the cognitive and psychomotor skill, and these opportunities must be created for them in experiential settings (Ryan et al., 2020; Shah et al., 2020).
More learners had staggered postings, going through junior and senior paediatric postings in what may be considered as integrated learning departing from the traditional method (Patel et al., 2005; Watmough et al., 2006, 2009). In the staggered posting type of rotation, we noticed that not all learners went through paediatric endocrinology unit posting, and like one of the discussants said, they would rather everyone went through each unit getting bits of everything and having opportunity to study specific and prevalent diseases in paediatric units rather than leaving them with the possibility of not learning important disorders. As it is not always possible to encounter specific diseases like DKA during entire posting in the schools that use staggered posting types, the likelihood of exposure was higher in schools that had block posting from the FGD conducted, but this did not translate to better retention of skills or cognitions as depicted in the Tanner staging matching question.
Having learners train in all special postings may not be the best approach in undergraduate medicine because the specialised skills may not be utilised in general practice and even in general paediatrics should the learners plan paediatric specialisation (Bindal et al., 2011). While some trainers may argue that all information and skill should be taught to the learners, the time to acquire and achieve mastery may be short for the learners (Jensen et al., 2018; Offiah et al., 2019). This study can be referenced in curriculum designing and implementation so the framers understand what society needs should be filled at any time. The concept of cognitive overload has actually reduced the duration of core specialty in clinical medicine while increasing the duration for others with emphasis on psychomotor, affective skills and professionalism. Some medical schools have core paediatric posting of 7 – 8 weeks, but Nigeria is still fixed with the traditional 3 – 4 months. In some schools in South Africa, the clinical posting is run as modular block for 3 years, with paediatric curriculum running from year 4 through year 6 (Dudley & Rohwer, 2015). With the long duration in the Nigeria curriculum, skills competencies are still deficient, so there is need to revamp the curriculum to make it more competency driven. It is excusable that more sophisticated competence like use of orchidometer were not known by more than half the learners, but if some were taught, the level of confidence in these skills at this stage of their learning should also be assessed as was done for diabetes by George et al. (2008).
Medical schools in Nigeria and other countries will have to continually evolve and produce curricula that are competency based, using problem-based learning, simulations, mannikin training for skills as is done in other countries (Watmough et al., 2006). Diabetes, thyroid, ambiguous genitalia with congenital adrenal hyperplasia, short stature and calcium disorders are common in Nigeria and should be taught in structured and integrated formats. Integrated curriculum where skills are graded from simple to complex can also be tested e g, skills of height measurements and charting using the stadiometer and growth charts can be taught in the 1st clinical year, and then the mid parental heights, target height calculation and bone age may be taught in the 2nd and 3rd clinical years. (Brauer & Ferguson, 2015; Grant, 2014).
A. Strength of the Research
Articulating the perceptions of learners is not always easy as they are varied and subjective, but getting them to come together, discuss and give suggestions on how curriculum can be designed and achieved increases the strength of this research. There was no sense of victimisation of the learners as many had already graduated from their schools, and the discussants admitted to not missing classes, or clinical learning. They spoke freely, with courtesy to others and there was little or no argument among them.
B. Limitations of the Research
As this research is based on past experiences of the cognitive and psychomotor skills achieved during the learners’ training period, the possibility of recall bias is high, and respondents may underestimate or exaggerate their skills. Using respondents who had just concluded their paediatric postings was an attempt at reducing this limitation. The best time to evaluate a programme is usually soon after the programme has been concluded however, as there has been no report of this type of evaluation, there was need to embark on it and make recommendations.
V. CONCLUSION
Respondents reported high variability in the implementation of the recommended guidelines for paediatric endocrinology curriculum between schools in Southern Nigeria. Variabilities were in the courses’ completion, learners’ skills exposure and how much hands-on were allowed in various skills acquisitions. This variability will hamper the core objectives of human capital development should the trend continue.
A. Area of Future Research
Noting the differences exist between schools, curriculum strategists and implementation teams in universities should commission a DELPHI study by experts, where core competencies and objectives for paediatric endocrinology will be agreed on and sent to the regulatory bodies for endorsement and implementation.
Notes on Contributors
IY conceived, designed, planned, executed and conducted interviews and the research. He also collected the data, analysed it and wrote the manuscript.
TC helped in designing the methodology for the data colllection and analyses, and reviewed the manuscript.
CU gave critical appraisal of the manuscript and all authors have approved the final manuscript.
Ethical Approval
The research ethics committee of the Univeristy of Port Harcourt gave ethical approval before the start of the study with the number: UPH/CEREMAD/REC/MM80/056.
Data Availability
The data supporting this research is available for publication purposes, without editing. Data can be shared only with express permission from the corresponding author as deposited in Figshare repository, using the private url:
https://figshare.com/articles/dataset/Copy_of_CURRICULUM_STUDENTS_xls/21154396
Acknowledgement
We acknowledge the early career doctors and final year students who participated in the online survey especially the selected ones who took part in the focus group discussion.
Declaration of Interest
Authors declare that there are no conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
Funding
There was no funding for this survey.
References
Alsalamah, A., & Callinan, C. (2021). Adaptation of Kirkpatrick’s four level model of training criteria to evaluate training programmes for head teachers. Education Science, 11(116), 1-25. https://doi.org/10.3390/educsci11030116
Bates, R. (2004). A critical analysis of evaluation practice: The Kirkpatrick model and the principle of beneficence. Evaluation and Program Planning, 27, 341-347. https://doi.org/10.1016/j.evalprogplan.2004.04.011
Bindal, T., Wall, D., & Goodyear, H. M. (2011). Medical students’ views on selecting paediatrics as a career choice. European Journal of Pediatrics, 170(9), 1193-1199. https://doi.org/10.1007/s00431-011-1467-9
Brauer, D. G., & Ferguson, K. J. (2015). The integrated curriculum in medical education: AMEE Guide No. 96. Medical Teacher, 37(4), 312-322. https://doi.org/10.3109/0142159X.2014.970998
Burton, J. L., & McDonald, S. (2001). Curriculum or syllabus: Which are we reforming? Medical Teacher, 23(2), 187-191. https://doi.org/10.1080/01421590020031110
Dudley, L. D., Young, T. N., Rohwer, A. C., Willems, B., Dramowski, A., Goliath, C., Mukinda, F. K., Marais, F., Mehtar, S., & Cameron, N. A. (2015). Fit for purpose? A review of a medical curriculum and its contribution to strengthening health systems in South Africa. African Journal Health Profession Education, 7(1), 81-84. https://doi.org/10.7196/AJHPE.512
Federal Ministry of Health of Nigeria, Health Systems 20/20Project. (2012). Nigeria undergraduate medical and dental curriculum template. Health systems 20/20 Project, Abt Associates Inc.
George, J. T., Warriner, D. A., Anthony, J., Rozario, K. S., Xavier, S., Jude, E. B., & Mckay, G. A. (2008). Training tomorrow’s doctors in diabetes: Self-reported confidence levels, practice and perceived training needs of post-graduate trainee doctors in the UK. A multi-centre survey. BMC Medical Education, 8, Article 22. https://doi.org/10.1186/1472-6920-8-22
Grant, J. (2014). Principles of curriculum design. In T. Swanwick, K. Forrest, B. C. O’Brien (Eds.), Understanding medical education evidence, theory and practice Sussex, UK: Wiley Blackwell, 31-46.
Hohmann, E., & Tetsworth, K. (2018). Fellowship exit examination in orthopaedic surgery in the commonwealth countries of Australia, UK, South Africa and Canada. Are they comparable and equivalent? A perspective on the requirements for medical migration. Medical Education Online, 23(1), Article 1537429. https://doi.org/10.1080/10872981.2018.1537429
Jensen, J. K., Dyre, L., Jørgensen, M. E., Andreasen, L. A., & Tolsgaard, M. G. (2018). Simulation-based point-of-care ultrasound training: a matter of competency rather than volume. Acta Anaesthesiology Scandanavia, 62(6), 811-819. https://doi.org/10.1111/aas.13083
McManus, I. C. (2003). Medical school differences: beneficial diversity or harmful deviations. BMJ Quality and Safety in Health Care, 12(5), 324-325. https://doi.org/10.1136/qhc.12.5.324
McManus, I. C., Harborne, A. C., Horsfall, H. L., Joseph, T., Smith, D. T., Marshall-Andon, T., Samuels, R., Kearsley, J. W., Abbas, N., Baig, H., Beecham, J., Benons, N., Caird, C., Clark, R., Cope, T., Coultas, J., Debenham, L., Douglas, S., Eldridge, J., . . . Devine, O. P. (2020). Exploring UK medical school differences: the MedDifs study of selection, teaching, student and F1 perceptions, postgraduate outcomes and fitness to practise. BMC Medicine, 18(1), Article 136. https://doi.org/10.1186/s12916-020-01572-3
Offiah, G., Ekpotu, L. P., Murphy, S., Kane, D., Gordon, A., O’Sullivan, M., Sharifuddin, S. F., Hill, A. D. K., & Condron, C. M. (2019). Evaluation of medical student retention of clinical skills following simulation training. BMC Medical Education, 19(1), Article 263. https://doi.org/10.1186/s12909-019-1663-2
Olson, A. L., Woodhead, J., Bekow, R., Kaufman, N., & Marshal, S. (2000). A national general pediatric clerkship curriculum: The process of development and implementation. Pediatrics, 160(S1), 216 -222. https://doi.org/10.1542/peds.106.S1.216
Ornstein A, H. F., & Hunkins, F. P. (2009). Curriculum: Foundations, principles and issues (5th Ed.). Pearson.
Patel, V. L., Arocha, J. F., Chaudhari, S., Karlin, D. R., & Briedis, D. J. (2005). Knowledge integration and reasoning as a function of instruction in a hybrid medical curriculum. Journal of Dental Education, 69(11), 1186-1211. https://www.ncbi.nlm.nih.gov/pubmed/16275683
Polikoff, M. S. (2018). The challenges of curriculum materials as a reform lever Evidence Speaks Reports, 2, 58
Puri, N., McCarthy, M., & Miller, B. (2021). Validity and reliability of pre-matriculation and institutional assessments in predicting USMLE STEP 1 success: Lessons from a traditional 2 x 2 curricular model. Frontiers in Medicine (Lausanne), 8, Article 798876. https://doi.org/10.3389/fmed.2021.798876
Rimmer, A. (2014). GMC will develop single exam for all medical graduates wishing to practise in UK. BMJ, 349, g5896. https://doi.org/10.1136/bmj.g5896
Rufai, S. R., Holland, L. C., Dimovska, E. O., Bing Chuo, C., Tilley, S., & Ellis, H. (2016). A national survey of undergraduate suture and local anesthetic training in the United Kingdom. Journal of Surgical Education, 73(2), 181-184. https://doi.org/10.1016/j.jsurg.2015.09.017
Ruiz, J. G., Mintzer, M. J., & Leipzig, R. M. (2006). The impact of E-learning in medical education. Academic Medicine, 81(3), 207-212. https://doi.org/10.1097/00001888-200603000-00002
Ryan, A., Hatala, R., Brydges, R., & Molloy, E. (2020). Learning with patients, students, and peers: Continuing professional development in the solo practitioner workplace. Journal of Continuing Education in the Health Profession, 40(4), 283-288. https://doi.org/10.1097/CEH.0000000000000307
Santen, S. A., Feldman, M., Weir, S., Blondino, C., Rawls, M., & DiGiovanni, S. (2019). Developing comprehensive strategies to evaluate medical school curricula. Medical Science Educator, 29(1), 291-298. https://doi.org/10.1007/s40670-018-00640-x
Shah, S., McCann, M., & Yu, C. (2020). Developing a national competency-based diabetes curriculum in undergraduate medical education: A Delphi study. Canadian Journal of Diabetes, 44(1), 30-36. https://doi.org/10.1016/j.jcjd.2019.04.019
Sosna, J., Pyatigorskaya, N., Krestin, G., Denton, E., Stanislav, K., Morozov, S., Kumamaru, K. K., Jankharia, B., Mildenberger, P., Forster, B., Schouman-Clayes, E., Bradey, A., Akata, D., Brkljacic, B., Grassi, R., Plako, A., Papanagiotou, H., Maksimović, R., & Lexa, F. (2021). International survey on residency programs in radiology: similarities and differences among 17 countries. Clinical Imaging, 79, 230-234. https://doi.org/10.1016/j.clinimag.2021.05.011
Tiffin, P. A., Paton, L. W., Mwandigha, L. M., McLachlan, J. C., & Illing, J. (2017). Predicting fitness to practise events in international medical graduates who registered as UK doctors via the Professional and Linguistic Assessments Board (PLAB) system: a national cohort study. BMC Medicine, 15(1), Article 66. https://doi.org/10.1186/s12916-017-0829-1
van Zanten, M., Boulet, J. R., & Shiffer, C. D. (2022). Making the grade: licensing examination performance by medical school accreditation status. BMC Medical Education, 22(1), Article 36. https://doi.org/10.1186/s12909-022-03101-7
Watmough, S., Garden, A., & Taylor, D. (2006). Does a new integrated PBL curriculum with specific communication skills classes produce Pre Registration House Officers (PRHOs) with improved communication skills. Medical Teachers, 28(3), 264-269. https://doi.org/10.1080/01421590600605173
Watmough, S., O’Sullivan, H., & Taylor, D. (2009). Graduates from a traditional medical curriculum evaluate the effectiveness of their medical curriculum through interviews. BMC Medical Education, 9, Article 64. https://doi.org/10.1186/1472-6920-9-64
Yarhere, I., Chinnah, T., & Uche, C. (2022). Learners’ report and perception of differences in undergraduate paediatric endocrinology curriculum content and delivery across Southern Nigeria. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.20730937.v1
Yarhere, I. E., & Nte, A. R. (2018) A ten-year review of all cause paediatric mortality in University of Port Harcourt Teaching Hospital, Nigeria (2006–2015). Nigerian Journal of Paediatrics, 45(4), 185-91.
*Iroro Enameguolo Yarhere
East/West Road,
PMB 5323 Choba,
Rivers State, Nigeria
+2347067987148
Email: iroro.yarhere@uniport.edu.ng
Submitted: 16 May 2022
Accepted: 3 January 2023
Published online: 4 July, TAPS 2023, 8(3), 5-14
https://doi.org/10.29060/TAPS.2023-8-3/OA2813
Bikramjit Pal1, Aung Win Thein2, Sook Vui Chong3, Ava Gwak Mui Tay4, Htoo Htoo Kyaw Soe5 & Sudipta Pal6
1Department of Surgery, Manipal University College Malaysia, Melaka, Malaysia; 2Department of Surgery, Manipal University College Malaysia, Melaka, Malaysia; 3Department of Medicine, Manipal University College Malaysia, Melaka, Malaysia; 4Department of Surgery, Manipal University College Malaysia, Melaka, Malaysia; 5Department of Community Medicine, Manipal University College Malaysia, Melaka, Malaysia; 6Department of Community Medicine, Manipal University College Malaysia, Melaka, Malaysia
Abstract
Introduction: The practice of high-fidelity simulation-based medical education has become a popular small-group teaching modality across all spheres of clinical medicine. High-fidelity simulation (HFS) is now being increasingly used in the context of undergraduate medical education, but its superiority over traditional teaching methods is still not established. The main objective of this study was to analyse the effectiveness of HFS-based teaching over video-assisted lecture (VAL)-based teaching in the enhancement of knowledge for the management of tension pneumothorax among undergraduate medical students.
Methods: A cohort of 111 final-year undergraduate medical students were randomised for this study. The efficacy of HFS-based teaching (intervention group) and VAL-based teaching (control group), on the acquisition of knowledge, was assessed by single-best answer multiple choice questions (MCQ) tests in the first and eighth week of their surgery posting. Mean and standard deviation (SD) for the total score of MCQ assessments were used as outcome measures. ANCOVA was used to determine the difference in post-test MCQ marks between groups. The intragroup comparison of the pre-test and post-test MCQ scores was done by using paired t-test. The P-value was set at 0.05.
Results: The mean of post-test MCQ scores were significantly higher than the mean of pre-test MCQ scores in both groups. The mean pre-test and post-test MCQ scores in the intervention group were slightly more than those of the control group but not statistically significant.
Conclusion: There was a statistically significant enhancement of knowledge in both groups but the difference in knowledge enhancement between the groups was insignificant.
Keywords: High-Fidelity Simulation, Video-Assisted Lecture, Simulation-Based Medical Education (SBME), Randomized Controlled Trial (RCT), Medical Education, Pre-test and Post-test Knowledge Assessments
Practice Highlights
- An RCT study to evaluate the effectiveness of HFS over video-assisted lecture teaching method.
- HFS seems to be not superior than VAL-based teaching for knowledge acquisition and retention.
- HFS may be used judiciously when the objectives are mainly knowledge based.
- Further research may determine curricular areas where HFS is superior and worth adopting.
I. INTRODUCTION
High-Fidelity Simulation (HFS) is an innovative healthcare education methodology that involves the use of sophisticated life-like mannequins to create a realistic patient environment. HFS can be considered an innovative teaching method that aids students in translating knowledge and psychomotor skills from the classroom to the actual clinical setting. Kolb’s Experiential Learning Cycle (Kolb, 1984) provides a basis for the integration of active learning of simulation with conventional teaching methods for a comprehensive learning experience in undergraduate medical education. HFS-based education is potentially an efficacious pedagogy that is now available for teaching. The usefulness of HFS has been recognized by the Accreditation Council of Graduate Medical Education (Accreditation Council of Graduate Medical Education [ACGME], 2020). HFS has the added benefit of increasing students’ confidence and their ability to care for the patients at the bedside (Kiernan, 2018). HFS-based education and video-assisted lecture-based teaching are both effective in achieving factual learning. Despite the increasing acceptance of HFS, there are limited studies to compare the usefulness of HFS with conventional teaching methods for factual learning among undergraduate medical students. At present, the different research studies have not provided enough evidence to establish HFS-based teaching’s superiority over traditional educational methods in the acquisition and retention of knowledge. There is inconsistent and variable outcome regarding the effectiveness of HFS on student learning (Yang & Liu, 2016). HFS-based education is both time-consuming and resource intensive. Its long-term merits in retaining knowledge and translating it into enhanced patient care need further research. As educators, we need to systematically evaluate the expensive newer teaching-learning modules like HFPS for their effectiveness by using rigorous research methodology and protocols. This is to ensure that we are providing the best learning opportunities conceivable for the students. Previous studies were mostly done in North America and, therefore, the generalisability of these results is guarded and might not be applicable in the context of Europe and Asia due to many differences in academic and curriculum aspects (Davies, 2008). The purpose of this study was to establish the feasibility of the use of HFS to deliver critical care education to final-year medical students and to find its efficacy in the enhancement of knowledge when compared to video-assisted lectures. The study compared the effectiveness of two methods of teaching pedagogy in the enhancement of knowledge acquisition using pre-test and post-test MCQ. This study was designed to provide insights that may be applied to the future development and improvement of HFS-based education among undergraduate medical students and its possibility of integrating it into course curricula.
II. METHODS
A. Study Design
Randomized Controlled Trial (RCT) with parallel groups and 1:1 allocation. Please see Appendix 1 for the Flow Chart.
B. Sample Size
G*Power software was used to calculate the sample size (Faul et al., 2007). Based on the preliminary RCT study of our institute done with the same protocol in 2018, the calculated sample size was 114 with a power of 0.95 for this study.
C. Inclusion and Exclusion Criteria
All male and female final-year undergraduate medical (MBBS) students in our institute were recruited after obtaining their written informed consent. All final-year students in the institute consented to the study. The participants were between the ages of 22-26 years.
The total number of participants recruited was 123.
The number of participants dropped out was 12 (9.77%).
Out of 111 participants who completed the study, 61 (54.95%) were female and 50 (45.05%) were male.
The study was conducted in the Clinical Skills Simulation Lab of Melaka Manipal Medical College (presently known as Manipal University College Malaysia).
The study period was from March 2019 to February 2020 (12 months).
D. Interventions
1) Description of HFPS-based teaching: It was an interactive session using a high-fidelity patient simulator demonstrating the management of tension pneumothorax by performing Needle Decompression on METIman (Pre-Hospital) following the Advanced Trauma Life Support Manual developed by the American College of Surgeons (ATLS Subcommittee et al., 2013).
2) Description of Hi-fidelity simulator: METIman Pre-Hospital HI-Fidelity Simulator (MMP-0418) was used for the simulation sessions. It was a fully wireless, adult High-Fidelity Patient Simulator (HFPS) with modelled physiology. It comes with extensive clinical features and capabilities designed specifically for learners to practice, gain experience, and develop clinical mastery in a wide range of patient care scenarios.
3) Description of video-assisted lecture-based teaching: It was a small group interactive session delivered face-to-face to the participants using a recorded video clip demonstrating the management of tension pneumothorax by performing Needle Decompression on METIman (Pre-Hospital) following the Advanced Trauma Life Support Manual developed by the American College of Surgeons (ATLS Subcommittee et al., 2013).
E. Outcome
The tool for measurement of knowledge was an identical set of single-best answer A-type MCQs. These MCQs were used for both Pre-test and Post-test knowledge assessments. MCQs were constructed based on the teaching sessions to assess their learning outcome.
The efficacy of HFPS-based teaching when compared to video-assisted lecture-based teaching is enhancement of knowledge for management of tension pneumothorax.
F. Recruitment
The students were recruited in the study during their final year surgical posting.
G. Randomisation
A cohort of 12 to 14 students from each rotation was randomised into intervention (HFPS-based teaching) and control (video-assisted lecture-based teaching) groups following random sequence generation method.
A computer-generated random sequence number was developed from randomizer.org. The independent randomiser was a biostatistician who did not participate in the delivery of interventions. The allocated interventions were then sealed in a sequentially numbered, opaque envelope.
Block randomisation with a block size of two was used to assign the students into intervention and control groups.
H. Implementation
A biostatistician generated the allocation sequence. One independent investigator enrolled the participants, and another independent investigator assigned the participants to interventions. The outcome assessor and the biostatistician were kept blinded to the randomisation.
I. Procedure for Data Collection
The participants who gave consent were enrolled in the study. Each session was conducted with a group of 12 to 14 participants. On the first day, the participants were briefed about the sessions and expected learning outcomes. As part of the briefing process, they were explained the confidentiality of the HFPS, the video-assisted lecture sessions and the ethical issues involved. All the participants were introduced to the high-fidelity patient simulator (METIman) in the clinical lab set-up to make them aware of its functions and familiarise them with the handling of the mannequin. An assurance was given to the students that the training course was not part of the evaluation process for the surgical curriculum. The briefing was followed by the first knowledge assessment (Pre-test MCQ) of all the participants. Pre-test MCQ was designed to collect the score of initial background knowledge about tension pneumothorax and its management following the ATLS protocol. The module for the aetiology, pathophysiology and clinical presentation of tension pneumothorax and its steps of management following the ATLS protocol was part of their final year course curriculum. It was taught before they participated in the study. After the Pre-test MCQ session, they were randomized into intervention and control groups consisting of 6 to 7 participants each. For the intervention group, an independent investigator used the high-fidelity simulator (METIman Pre-hospital) to demonstrate the diagnosis and management of tension pneumothorax (Needle Decompression) in an emergency setting. The demonstration time was 20 minutes followed by hands-on training for another 20 minutes. For the control group, a recorded video clip of the identical facilitated simulation session on the diagnosis and management of tension pneumothorax (Needle Decompression) was shown by another investigator. The video demonstration lasted for 20 minutes. This session was followed by a 20-minute interactive discussion session with the faculty. All the participants in both groups were apprised of the importance of aetiology, pathophysiology and clinical presentation in arriving at the diagnosis and management of tension pneumothorax during these interactive teaching sessions. The participants were encouraged to explore how they would manage the stated clinical situation through discussion. The faculty were instructed to emphasize the teaching points related to the outcome of the study. The total duration for both types of teaching was 40 minutes. There were no more additional hands-on practice or video-assisted lecture sessions for the participants during the course of the research study. In the seventh/eighth week, both the intervention and the control groups again participated in the second knowledge assessment (Delayed Post-test MCQ) to assess their gain and retention of knowledge. Delayed Post-test MCQ assessment may minimise the recall bias and test their retained memory better.
Both Pre-test and Post-test knowledge assessments comprised 20 MCQs which were to be completed in 20 minutes. The single-best answer A-type MCQs with five options of answers were prepared following the guidelines framed by the National Board of Medical Examiners (Case & Swanson, 2001). For each correct response, a score of one point was awarded. No negative marking was awarded for incorrect response. Based on the learning objectives, the MCQs were constructed by 6 experts in the field of Surgery, Medicine and Medical Education who were not part of this research study. The MCQs covered the items on pathophysiology, diagnosis, and management of tension pneumothorax, and assessed for knowledge comprehension and knowledge application. The order of the questions was changed between the Pre-test and the Post-test. The MCQ answer sheets were scanned by Konica Minolta FM (172.17.5.12) scanner and graded by using Optical Mark Recognition (OMR) software (Remark Office OMR, version 9.5, 2014; Gravic Inc., USA). Before the main study, a preliminary study involving 56 students was conducted to explore the time management, feasibility, acceptability, and validation of the MCQs (Pal et al., 2021). In the preliminary study, the Pre-test and the Post-test were administered in the first week and the fourth week respectively to note the short-term retention of knowledge. This study is an extension of the preliminary study with a different cohort of students where the Pre-test and the Delayed Post-test were administered in the first week and the seventh/eighth week respectively to determine the medium-term retention of knowledge. The MCQs were reviewed based on the feedback from the preliminary study on the appropriateness of the content, clarity in wording, and difficulty level. The difficulty index and the bi-serial correlation for item discrimination of all MCQs were checked. The value between 30 and 95 in the difficulty index and the bi-serial correlation value > 0.2 were chosen as the accepted standard for this study.
At the end of the study, the participants in the intervention group were provided with access to the identical video-assisted lecture sessions as designed for the control group. Similarly, the participants in the control group were provided with access to the same HFS sessions. This is to ensure parity between the groups for their professional development of knowledge.
J. Statistical Analysis
SPSS software (version 25) was used for data analysis. The descriptive statistics such as frequency and percentage for categorical data and the mean and standard deviation for the total score of the assessments were calculated. ANCOVA was used to determine the difference in post-test MCQ marks between intervention and control groups with pre-test MCQ marks as a covariate. Intragroup comparison of pre-test and post-test MCQ marks was also done by calculating paired t-test. For intergroup comparison, the effect size – Partial Eta Squared was calculated in ANCOVA. Cohen’s dz was calculated for the comparison of dependent means. The level of significance was set at 0.05 and the null hypothesis was rejected when P < 0.05. We measured the scale-level content validity index (SCVI) and item-level content validity index (ICVI) for the validity and Cronbach alpha for the internal consistency (reliability) of the MCQs. The average values of SCVI and ICVI were 0.94 & 0.89 respectively. The value of Cronbach’s alpha was 0.78.
III. RESULTS
The data that support the findings this RCT study are openly available at https://doi.org/10.6084/m9.figshare.19932053 (Pal et al., 2022).
A. General Data Analysis
There was no difference in the highest Pre-test scores achieved by the participants in both intervention and control groups. The lowest scores recorded in the intervention group were better than the control group in both Pre-test and Post-test. There was a negligible difference between the highest Post-test scores among control and intervention groups (See Table 1).
|
Test score |
Intervention |
Control |
|
PRE-TEST |
||
|
Mean (SE) |
12.31 (0.34) |
12.23 (0.36) |
|
95% CI for Mean |
11.64 – 12.98 |
11.50 – 12.96 |
|
Min – Max |
6.0 – 18.0 |
6.0 – 18.0 |
|
POST-TEST |
||
|
Mean (SE) |
13.65 (0.27) |
13.60 (0.30) |
|
95% CI for Mean |
13.12 – 14.19 |
12.98 – 14.20 |
|
Min – Max |
8.0 – 18.0 |
7.0 – 17.0 |
|
Table 1. Highest, lowest and unadjusted mean MCQ scores among intervention and control groups |
||
|
SE – Standard Error CI – Confidence Interval Min – Minimum Max – Maximum |
||
B. Statistical Data Analysis
ANCOVA was used to determine the difference in Post-test MCQ scores among control and intervention groups after adjusting pre-test MCQ scores. There was a linear relationship between Pre-test and Post-test MCQ scores for each group, as determined by visual inspection of the scatterplot. The homogeneity of regression slopes was noted as the interaction term was not statistically significant, F (1, 107) = 0.889, P = 0.348. When assessed by Shapiro-Wilk’s test, standardized residuals were normally distributed (P > 0.05) in the intervention group, but not normally distributed in the control group (P < 0.05). Both homoscedasticity and homogeneity of variance were noted, as assessed by visual inspection of a scatterplot and Levene’s test of homogeneity of variance (P = 0.531), respectively. Data were adjusted with mean ± standard error unless otherwise stated. The effect size, Partial Eta Squared (Partial η2) was calculated in ANCOVA. A partial η2 value of 0.01 or less was considered to be small. For the comparison of dependent means, the effect size, Cohen’s dz was calculated; where the effect size of 0.5-0.8 was considered to be moderate (Ellis, 2010). Post-test MCQ score was higher in the intervention group but after adjustment for pre-test MCQ scores, there was no statistically significant difference in post-test MCQ scores between the control and intervention groups. The effect size was small (See Table 2).
|
Variable |
n |
Post-test MCQ score Mean (SE) |
Mean difference (95% CI) |
P-value |
Partial η2 |
|
Intervention |
55 |
13.65 (0.27) |
0.04 (-0.69, 0.77) |
0.917 |
0.0001 |
|
Control |
56 |
13.60 (0.30) |
|||
|
Table 2. Intergroup comparison of post-test MCQ scores between intervention and control groups after adjusting pre-test MCQ marks (ANCOVA) |
|||||
|
n: number of students SE: Standard error 95% CI: 95% confidence interval Partial η2: Partial Eta Squared |
|||||
There was a statistically significant difference between pre-test and post-test MCQ scores among the intervention and control groups. The mean of post-test MCQ scores was significantly higher than the mean of pre-test MCQ scores in both intervention and control groups. The effect size was moderate in both groups (See Table 3).
|
Variable |
n |
Mean (SD) |
Mean difference (95% CI) |
t (df) |
P-value |
Dz |
|
|
Pre-test MCQ scores |
Post-test MCQ scores |
||||||
|
Intervention |
55 |
12.31 (2.49) |
13.65 (1.99) |
1.34 (0.64, 2.05) |
3.841 (54) |
* < 0.001 |
0.518 |
|
Control |
56 |
12.23 (2.72) |
13.60 (2.26) |
1.36 (0.68, 2.04) |
3.998 (55) |
* < 0.001 |
0.534 |
|
Table 3. Intragroup comparison of pre and post MCQ scores among intervention and control groups (Paired t-test) |
|||||||
|
n: number of students * Significant SD: Standard deviation 95% CI: 95% confidence interval dz: Cohen’s dz |
|||||||
IV. DISCUSSION
Multiple studies have revealed slight to the modest enhancement of knowledge in simulation-based medical education (SBME) when compared to other instructional teaching methods (Cook et al., 2012; Gordon et al., 2006; Lo et al., 2011; Ray et al., 2012; Ten Eyck et al., 2009). Notwithstanding the increasing popularity of SBME, there is little evidence to conclude that it is superior to other small-group teaching modalities for the acquisition of knowledge (Alluri et al., 2016). The common perception is that knowledge lies at the lowest level of competence in Miller’s model of clinical acumen (Miller, 1990), but it is also important to note that knowledge is the basic foundation of competence and proficiency (Norman, 2009). Theoretically, SBME is advantageous for assessment of both knowledge and skills but there are few studies which directly evaluated the effectiveness of HFS in the assessment of knowledge (McGaghie et al., 2009; Rogers, 2008).
The mean scores of both Pre-test and the Post-test were higher in the intervention group in this study. In comparison, our preliminary study demonstrated that the control group had higher mean MCQ marks than the intervention group in Pre-test whereas at Post-test, the intervention group had higher mean MCQ marks than the control group (Pal et al., 2021).
In our study, there is significant enhancement of knowledge (P < 0.001) in both modes of teaching which corroborates the findings of Alluri et al. (2016). Their RCT study demonstrated that the participants in both the simulation and lecture groups had improved post-test scores (p < 0.05). The comparison of Pre-test and Post-test MCQ scores in our preliminary study also revealed significant higher mean MCQ scores at Post-test than Pre-test in both intervention and control groups (Pal et al., 2021). A study by Couto et al. (2015) showed improved post-test scores in both methods. Similar results were noted in the studies by Chen et al. (2017) and Vijayaraghavan et al. (2019). The finding of a study by Hall (2013) showed a slight increase in post-test scores in both the HFPS and control groups.
A systematic review by La Cerra et al. (2019) revealed that HFS was superior to other teaching methods in improving knowledge and performance. Significant higher scores for participants in the HFS group in the studies by Larsen et al. (2020) and Solymos et al. (2015) demonstrated that HFS may be superior to conventional teaching methods for factual learning. In another study by Bartlett et al. (2021), HFS showed a significant long-term gain in knowledge over traditional teaching methods, but short-term knowledge gain was insignificant. Our study revealed that the Post-test MCQ score was higher in the HFS group but after adjustment of pre-test scores, there was no significant difference in knowledge gain between the control and intervention groups. The findings were similar in our preliminary study where the intervention group had higher mean change score of MCQ scores than the control group but it was not statistically significant (Pal et al., 2021).
On the other hand, there was no significant knowledge improvement in both simulation and traditional teaching methods as observed in the studies (Corbridge et al., 2010; Kerr et al., 2013; Moadel et al., 2017). The findings of Alluri et al. (2016) also showed no difference in knowledge gain between simulation and lecture-based teaching. The studies by Morgan et al. (2002) and Tan et al. (2008), demonstrated equal efficacy between simulation and conventional lectures. The findings of a study by Kerr et al. (2013) demonstrated that SBME was not beneficial in acquisition and retention of knowledge. There was no significant improvement in knowledge after simulation-based education as revealed by the findings of three RCTs (Cavaleiro et al., 2009; Cherry et al., 2007; Kim et al., 2002).
Despite simulation being effective in acquisition of knowledge, it may not be the most efficient modality when compared to other traditional educational methods (Bordage et al., 2009). There is ample evidence that SBME usually leads to enhancement of knowledge and skills among undergraduate students but its superiority over other conventional teaching methods is yet to be defined (Nestel et al., 2015).
A. Limitations
There is a possibility of potential biases in the form of design, recruitment, sample populations and data analysis that could have influenced the findings. Due to randomization in blocks of two, the allocation of participants may be predictable which may result in selection bias. The confounding factors such as communication between the different groups of students prior to the second MCQ assessment, participants’ recall memory and preparation for the post-test after 7 – 8 weeks need to be considered. As it was a single-centre study which included final-year medical students only, the validity of the findings may not be applicable to other settings.
V. CONCLUSION
Conventional teaching modalities and HFS, when used in conjunction with bedside teaching, may complement clinical practice, leading to higher retention of knowledge. Therefore, more studies are required to measure the efficacy of simulation for a better understanding of the differences that it can make in the acquisition of knowledge. Our study revealed that the efficacy of high-fidelity simulation-based teaching was not superior to video-assisted lecture-based teaching in terms of knowledge acquisition and retention. The substantially higher cost and maintenance associated with HFS need to be considered before planning a teaching-learning activity. It may be used judiciously with conventional teaching when the objectives are mainly knowledge-based. More studies are required to determine its effectiveness and further evaluation as a teaching-learning tool in medical education.
Notes on Contributors
Bikramjit Pal was involved in Conceptualization, Formal Analysis, Literature Review, Methodology, Project administration & Supervision, Data Analysis and Writing (original draft & editing).
Aung Win Thein was involved in Formal Analysis, Literature Review, Methodology, Supervision and Writing (review & editing).
Sook Vui Chong was involved in Literature Review, Methodology, Supervision and Writing (review & editing).
Ava Gwak Mui Tay was involved in Formal Analysis, Literature Review, Supervision and Writing (review & editing).
Htoo Htoo Kyaw Soe was involved in Formal Analysis, Methodology, Data curation, Statistical Analysis and Validation.
Sudipta Pal was involved in Literature Review, Methodology, Formal Analysis, Data curation and Writing (review & editing).
Ethical Approval
Ethical approval was duly obtained from the Ethical Committee / IRB of Manipal University College Malaysia. Informed consent was taken from all the participants. All information about the participants was kept confidential.
Approval number: MMMC/FOM/Research Ethics Committee – 11/2018.
Data Availability
The data that supports the findings of this RCT study are openly available at Figshare repository, https://doi.org/10.6084/m9.figshare.19932053.v2 (Pal et al., 2022).
Acknowledgement
The authors would like to acknowledge the final year MBBS students of Manipal University College Malaysia who had participated in this research project, the faculty of the Department of Surgery, the lab assistants and technicians of Clinical Skills Lab and the Management of Manipal University College Malaysia.
Funding
The researchers had not received any funding or benefits from industry or elsewhere to conduct this study.
Declaration of Interest
The researchers had no conflicts of interest.
References
Accreditation Council for Graduate Medical Education. (2020, July 1). Program requirements for graduate medical education in general surgery. https://www.acgme.org/globalassets/pfassets/programrequirements/440_generalsurgery_2020.pdf.
Alluri, R. K., Tsing, P., Lee, E., & Napolitano, J. (2016). A randomized controlled trial of high-fidelity simulation versus lecture-based education in preclinical medical students. Medical Teacher, 38(4), 404–409. https://doi.org/10.3109/0142159X.2015.1031734
ATLS Subcommittee, American College of Surgeons’ Committee on Trauma, & International ATLS working group. (2013). Advanced trauma life support (ATLS®): The ninth edition. Journal of Trauma and Acute Care Surgery, 74(5), 1363–1366. https://doi.org/10.1097/TA.0b013e31828b82f5
Bartlett, R. S., Bruecker, S., & Eccleston, B. (2021). High-fidelity simulation improves long-term knowledge of clinical swallow evaluation. American Journal of Speech-Language Pathology, 30(2), 673–686.
Bordage, G., Carlin, B., Mazmanian, P. E., & American College of Chest Physicians Health and Science Policy Committee (2009). Continuing medical education effect on physician knowledge: Effectiveness of continuing medical education: American College of Chest Physicians evidence-based educational guidelines. Chest, 135(3 Suppl), 29S–36S. https://doi.org/10.1378/chest.08-2515
Case, S. M., & Swanson, D. B. (2001). Constructing written test questions for the basic and clinical sciences. 3rd ed. Philadelphia: National Board of Medical Examiners.
Cavaleiro, A. P., Guimarães, H., & Calheiros, F. (2009). Training neonatal skills with simulators? Acta Paediatrica, 98(4), 636–639.
Chen, T., Stapleton, S., Ledford, M., & Frallicciardi, A. (2017). Comparison of high-fidelity simulation versus case-based discussion on fourth- year medical student performance. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 18(5.1). https://escholarship.org/uc/item/5k73f4qc
Cherry, R. A., Williams, J., George, J., & Ali, J. (2007). The effectiveness of a human patient simulator in the ATLS shock skills station. Journal of Surgical Research, 139(2), 229–235. https://doi.org/10.1016/j.jss.2006.08.010
Cook, D. A., Brydges, R., Hamstra, S. J., Zendejas, B., Szostek, J. H., Wang, A. T., Erwin, P. J., & Hatala, R. (2012). Comparative effectiveness of technology-enhanced simulation versus other instructional methods: A systematic review and meta-analysis. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, 7(5), 308–320. https://doi.org/10.1097/SIH.0b013e3182614f95
Corbridge, S. J., Robinson, F. P., Tiffen, J., & Corbridge, T. C. (2010). Online learning versus simulation for teaching principles of mechanical ventilation to nurse practitioner students. International Journal of Nursing Education Scholarship, 7(1), Article 12. https://doi.org/10.2202/1548-923X.1976
Couto, T. B., Farhat, S. C., Geis, G. L., Olsen, O., & Schvartsman, C. (2015). High-fidelity simulation versus case-based discussion for teaching medical students in Brazil about pediatric emergencies. Clinics (Sao Paulo, Brazil), 70(6), 393–399. https://doi.org/10.6061/clinics/2015(06)02
Davies, R. (2008). The Bologna process: the quiet revolution in nursing higher education. Nurse Education Today, 28(8), 935–942. https://doi.org/10.1016/j.nedt.2008.05.008
Ellis, P. (2010). The essential guide to effect sizes: Statistical power, meta-analysis, and the interpretation of research results. Cambridge University Press. https://doi.org/10.1017/CBO9780511761676
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/bf03193146
Gordon, J. A., Shaffer, D. W., Raemer, D. B., Pawlowski, J., Hurford, W. E., & Cooper, J. B. (2006). A randomized controlled trial of simulation-based teaching versus traditional instruction in medicine: A pilot study among clinical medical students. Advances in Health Sciences Education , 11(1), 33–39. https://doi.org/10.1007/s10459-004-7346-7
Hall, R. M. (2013). Effects of high fidelity simulation on knowledge acquisition, self-confidence, and satisfaction with baccalaureate nursing students using the solomon-four research design [Doctoral dissertation, East Tennessee State University]. East Tennessee State University Higher Education Commons. https://dc.etsu.edu/etd/2281
Kerr, B., Hawkins, T. L., Herman, R., Barnes, S., Kaufmann, S., Fraser, K., & Ma, I. W. (2013). Feasibility of scenario-based simulation training versus traditional workshops in continuing medical education: a randomized controlled trial. Medical Education Online, 18(1), Article 21312. https://doi.org/10.3402/meo.v18i0.21312
Kiernan, L. C. (2018). Evaluating competence and confidence using simulation technology. Nursing, 48(10), 45–52. https://doi.org/10.1097/01.NURSE.0000545022.36908.f3
Kim, J. H., Kim, W. O., Min, K. T., Yang, J. Y., & Nam, Y. T. (2002). Learning by computer simulation does not lead to better test performance on advanced cardiac life support than textbook study. The Journal of Education in Perioperative Medicine, 4(1), Article E019.
Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development. Prentice Hall.
La Cerra, C., Dante, A., Caponnetto, V., Franconi, I., Gaxhja, E., Petrucci, C., Alfes, C. M., & Lancia, L. (2019). Effects of high-fidelity simulation based on life-threatening clinical condition scenarios on learning outcomes of undergraduate and postgraduate nursing students: A systematic review and meta-analysis. BMJ Open, 9(2), Article e025306. https://doi.org/10.1136/bmjopen-2018-025306
Larsen, T., Jackson, N., & Napolitano, J. (2020). A comparison of simulation-based education and problem-based learning in pre-clinical medical undergraduates. MedEdPublish, 9(1), Article 172.
Lo, B. M., Devine, A. S., Evans, D. P., Byars, D. V., Lamm, O. Y., Lee, R. J., Lowe, S. M., & Walker, L. L. (2011). Comparison of traditional versus high-fidelity simulation in the retention of ACLS knowledge. Resuscitation, 82(11), 1440–1443. https://doi.org/10.1016/j.resuscitation.2011.06.017
McGaghie, W. C., Siddall, V. J., Mazmanian, P. E., Myers, J., & American College of Chest Physicians Health and Science Policy Committee (2009). Lessons for continuing medical education from simulation research in undergraduate and graduate medical education: Effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest, 135(3 Suppl), 62S–68S. https://doi.org/10.1378/chest.08-2521
Miller, G. E. (1990). The assessment of clinical skills/competence/performance. Academic Medicine, 65(9), S63–S67. https://doi.org/10.1097/00001888-199009000-00045
Moadel, T., Varga, S., & Hile, D. (2017). A prospective randomized controlled trial comparing simulation, lecture and discussion-based education of sepsis to emergency medicine residents. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 18(5.1). https://escholarship.org/uc/item/0132981t
Morgan, P. J., Cleave-Hogg, D., McIlroy, J., & Devitt, J. H. (2002). Simulation technology: A comparison of experiential and visual learning for undergraduate medical students. Anesthesiology, 96, 10–16. https://doi.org/10.1097/00000542-200201000-00008
Nestel, D., Harlim, J., Smith, C., Krogh, K., & Bearman, M. (2015). Simulated learning technologies in undergraduate curricula: An evidence check review for HETI.
Norman, G. (2009). The American College of Chest Physicians evidence-based educational guidelines for continuing medical education interventions: a critical review of evidence-based educational guidelines. Chest, 135(3), 834–837. https://doi.org/10.1378/chest.09-0036
Pal, B., Chong, S. V., Thein, A. W., Tay, A. G., Soe, H. H., & Pal, S. (2021). Is high-fidelity patient simulation-based teaching superior to video-assisted lecture-based teaching in enhancing knowledge and skills among undergraduate medical students? Journal of Health and Translational Medicine, 24(1), 83-90. https://doi.org/10.22452/jummec.vol24no1.14
Pal, B., Thein, A. W., Chong, S. V., Tay, A., Htoo, H., & Pal, S. (2022). A randomized controlled trial study to compare the effectiveness of high-fidelity based teaching with video-assisted based lecture teaching in enhancing knowledge [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.19932053
Ray, S. M., Wylie, D. R., Shaun Rowe, A., Heidel, E., & Franks, A. S. (2012). Pharmacy student knowledge retention after completing either a simulated or written patient case. American Journal of Pharmaceutical Education, 76(5), 86. https://doi.org/10.5688/ajpe76586
Rogers, D. A. (2008). The role of simulation in surgical continuing medical education. Seminars in Colon and Rectal Surgery, 19(2), 108-114. https://doi.org/10.1053/j.scrs.2008.02.007
Solymos, O., O’Kelly, P., & Walshe, C. M. (2015). Pilot study comparing simulation-based and didactic lecture-based critical care teaching for final-year medical students. BMC Anesthesiology, 15, Article 153. https://doi.org/10.1186/s12871-015-0109-6
Tan, G. M., Ti, L. K., Tan, K., & Lee, T. (2008). A comparison of screen-based simulation and conventional lectures for undergraduate teaching of crisis management. Anaesthesia and Intensive Care, 36(4), 565–569.
Ten Eyck, R. P., Tews, M., & Ballester, J. M. (2009). Improved medical student satisfaction and test performance with a simulation-based emergency medicine curriculum: a randomized controlled trial. Annals of Emergency Medicine, 54(5), 684–691. https://doi.org/10.1016/j.annemergmed.2009.03.025
Vijayaraghavan, S., Rishipathak, P., & Hinduja, A. (2019). High-fidelity simulation versus case-based discussion for teaching bradyarrhythmia to emergency medical services students. Journal of Emergencies, Trauma, and Shock, 12(3), 176–178. https://doi.org/10.4103/JETS.JETS_115_18
Yang, Y., & Liu, H. P. (2016). Systematic evaluation influence of high-fidelity simulation teaching on clinical competence of nursing students. Chinese Nursing Research, 30(7), 809–814. https://caod.oriprobe.com/articles/47628779/Systematic_evaluation_influence_of_high_fidelity_s.htm
*Bikramjit Pal
RCSI & UCD Malaysia Campus (RUMC),
4 Jalan Sepoy Lines,
Georgetown, Penang, 10450, Malaysia
+6042171908-1908 (Ext)
Email: bikramjit.pal@rcsiucd.edu.my
Submitted: 16 March 2022
Accepted: 26 May 2022
Published online: 4 April, TAPS 2023, 8(2), 57-65
https://doi.org/10.29060/TAPS.2023-8-2/OA2778
Vijay Kautilya Dayanidhi1, Arijit Datta2, Shruti P Hegde3 & Preeti Tiwari4
1Department of Forensic Medicine, Medicine, Manipal Tata Medical College, MAHE, India; 2Department of Forensic Medicine, Medicine, Pramukhswamy Medical college, India; 3Department of Ophthalmology, Medicine, Manipal Tata Medical College, MAHE, India; 4Department of Community Medicine, Medicine, Pramukhswamy Medical college, India
Abstract
Introduction: Summative assessments play a major role in shaping the student’s learning. There is little literature available on validity of summative assessment question papers in Forensic Medicine & Toxicology. This study analyses 30 question papers from 6 reputed universities for content validity.
Methods: A retrospective cross-sectional record-based observational study was conducted where 30 university summative question papers in Forensic Medicine & Toxicology from 6 universities across India were evaluated for content validity. The learning domain assessed, the type of questions asked, and sampling of the content was compared and presented in the results.
Results: From the results of the study, it was noted that 80% weightage was allotted to recall in most papers and only one paper tested for application. 70 to 80% of the marks were allotted to Forensic Pathology leading to disproportionate sampling. Core areas in Toxicology and Medical Jurisprudence were sparsely assessed.
Conclusion: The content validity of the summative question papers in Forensic Medicine and Toxicology was unsatisfactory, emphasising the need for evaluation of the clarity and efficacy of the blueprints being used by the universities. Faculty training to motivate and influence a change in the mindset is necessary to bring about a course correction.
Keywords: Forensic Medicine & Toxicology, Summative Assessments, University Assessments, Blueprint, Content Validity, Learning Domains
Practice Highlights
- Content validity of the Forensic Medicine & Toxicology university exam question papers form six universities was studied.
- It was observed that certain subtopics like Forensic Pathology over time have been over value (80% Weightage).
- Core areas in Medical Jurisprudence and toxicology like substance abuse, environmental toxicology, and pharmaceutical toxicity have been undervalued.
- None of the QPs analysed tested for application. Most items in the assessment tested only recall.
- The blueprints for the paper setters, considering the competencies to be assessed must be designed and validated.
I. INTRODUCTION
Reflecting on our learning experience during MBBS, we realised that we have always had issues with the examination system. The questions are vague and clustered around few important topics. Undergraduate students look up to previous examination question papers as references to decide the stake to be allotted to the topics while preparing for examination. Invariable all students attempt to predict the examination pattern and allot appropriate time and efforts to different subjects, skills, and topics. This reiterates George E Miller’s quote “Assessment drives Learning”. Summative assessments need to be planned appropriately as medicine has high stakes (Amin et al., 2006). Properly designed and executed assessments are known to have a “positive steering effect on the student’s learning. They are also needed to evaluate the programs. Improper assessments can drive a hidden curriculum leading to a completely unintended outcomes (Amin & Khoo, 2003, pp. 260).
Competency Based Medical Education (CBME) model being adopted in India as per the new Graduate Medical Education Regulations 2019, has attempted to bring about a radical change in the educational process. Undergraduate examinations in India are shifting towards a criteria-based process (Aggarwal & Agarwal., 2017; Bhattacharya et al., 2017; Mehta & Kikani, 2019). Outcome based education demands that the examinations be designed to sample and evaluate specific competencies prescribed. The success of these models strongly depended on the validity of the examination process. Summative assessments require that the assessment tool be validated. Key outcomes need to be tested (Amin & Khoo, 2003, pp. 260; McAleer, 2001). Content validity and construct validity are two very important aspect that support the effectiveness of an assessment. Content validity tests the representativeness of the learning objectives in the assessment tool and construct validity represents the congruence of the assessment tool with the intended purpose (Amin & Khoo, 2003, pp. 260).
Forensic Medicine and Toxicology in India, trains the undergraduate to apply their knowledge gained in Medicine for the benefit of law. It is a culmination of Forensic Pathology, Medical Jurisprudence and Toxicology put together. Its key objective is to empower Indian Medical Graduates in handling Medical Legal issues and critically apply their medical skills in delivering justice. Emphasis is also placed on training in etiology, identification, and management of Poisoning ( Sharma et al., 2005). Studies on student perception suggest that teaching is significantly teacher centric and theory oriented. Skill training in Medical Jurisprudence and Toxicology is significantly neglected. Students allege though they value the subject, they spend less time as only select concepts are emphasised (Gupta et al., 2017; Parmar, 2018; Sharma et al., 2005; Sudhan & Raj, 2019). As the new CBME UG curriculum 2019 is being rolled out it is necessary that deficiencies in the traditional curriculum be identified in order to deliver an efficient and effective Forensic Medicine & Toxicology curriculum (National Medical Commission, 2018).
Summative theory exams inherently have a challenge with distribution of the items being tested (Aggarwal & Agarwal, 2017; Amin et al., 2006; Amin & Khoo, 2003, pp. 260; Bhattacharya et al., 2017). Validity of the content being tested in examination is always in question. Selecting appropriate questions, question types and domain can make all the difference in the validity of the examination (Amin et al., 2006; Amin & Khoo, 2003, pp. 260; McAleer, 2001). Particularly in Forensic Medicine which is purely application-based course, testing critical thinking and synthesis is necessary. This is found wanting in the traditional curriculum (Parmar, 2018; Sharma et al., 2005; Sudhan & Raj, 2019). Published literature on systematic analysis of summative assessment question papers in Forensic Medicine & Toxicology are sparsely available. In this study, we have analysed and compared undergraduate summative examination question papers of Forensic Medicine & Toxicology from six reputed universities all over India for the distribution of content tested, Domain of learning and Construct of the question.
II. METHODS
A retrospective cross-sectional record-based observational study was conduct at Government Medical College, Bharatpur after obtaining ethical approval from the Institutional Ethics Committee between October to December 2020. For the study, 30 summative exam question papers from six reputed medical universities were selected based on the availability of the University question papers in public domain. The last five-year (2016-20) undergraduate question papers in Forensic Medicine & Toxicology were collected from the university websites and the college records from constituent colleges after thorough web search. The names of the universities have been kept anonymous during the analysis of results. All the data was collected form sources in public domain hence explicit consent was not taken. Two of the selected universities were based in North India and four universities were based in South India. The identity of the Medical Universities was kept confidential during the analysis of the question papers.
The Summative theory examination in Forensic Medicine & Toxicology as per the Medical Council of India (MCI) regulations consists of one theory paper of minimum 40 marks. The question paper consists of essay type questions and objective questions like very short answer questions or Multiple-choice questions depending on the universities (National Medical Commission, 2018).
For analysis, the questions were categorised based on the question type as LEQ (Long Essay Question), SAQ (Short Answer Question) & VSAQ (Very Short Answer Question including MCQs). The Questions were also categorised based on the domain of learning as Recall Based, Comprehension Based and Application Based Questions.
The Topics in Forensic Medicine & Toxicology can be broadly subdivided into Medical Jurisprudence, Forensic Pathology and Toxicology. These were further subdivided as Six Categories as Legal Procedure, Medical jurisprudence, Forensic Pathology, Forensic Psychiatry, Lab Technique, emerging trends, and Toxicology (Medical Council of India, 1997). Percentage of marks allotted to each of these topics was analysed in each of the papers.
Further, Forensic Pathology was Sub divided into Subtopics like Identification, Postmortem Changes, Mechanical Injuries, Mechanical Asphyxia, Thermal Deaths, Sexual Offences and Medico Legal issues related to Pregnancy, Delivery, Abortion. Toxicology was Sub divided into General Toxicology, Chemical Toxicology, Drug, Pharmacy & Substance abuse Toxicology, Bio toxicology (Medical Council of India, 1997). Percentage allotment of Marks in each of the question papers was analysed for each of the subtopics.
The data thus collected was tabulated in an Excel Sheet and the percentage distribution of marks in various subtopics noted. The SPSS Statistical Software (IBM SPSS Statistics for Windows, Version 23.0) was used to analyse the data. Radar Graphs and line graphs were plotted to represent and compare pattern of distribution of marks in various topics in each question paper. The type of questions asked, the weightage allotted to the subtopics were compared keeping in mind the expected outcomes in the Forensic Medicine & Toxicology curriculum proposed by National Medical Commission and Medical Council of India for content validity (Medical Council of India, 1997; National Medical Commission, 2018). The learning domain targeted in the questions was compared for construct validity of the question papers.
III. RESULTS
In this study, five question papers(n=30) from each university(n=6) were analysed and compared. The data that supports the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.Fig share.19367864 (Kautilya et al., 2022).
As regulated the university Summative examination in Forensic Medicine & Toxicology consists of one theory assessment and one practical assessment (Medical Council of India, 1997; National Medical Commission, 2018). The theory paper is allotted a minimum of 40 marks. Five universities conducted exam for 40 marks and one university paper was of 100 marks. All question papers had three types of questions, namely Essay questions (Long Answer Questions-LAQs) of 8 to 10 marks each, short essays (Short Answer questions-SAQs) of 3-5 marks each and Objective questions (like Multiple choice questions-MCQs or Very short answer questions- VSAQs) of 1-2 marks each. Table 1 presents the percentage distribution of the marks allotted to each question type.
|
University
|
% Marks LAQ |
% Marks SAQ |
% Marks VSAQ/ MCQ |
|
U1 |
43 |
49.5 |
7.5 |
|
U2 |
25 |
50 |
25 |
|
U3 |
20.4 |
51.2 |
28.4 |
|
U4 |
25 |
50 |
25 |
|
U5 |
25 |
56 |
19 |
|
U6 |
42 |
40.5 |
17.5 |
Table 1. University vice distribution marks in the question papers based on the type of questions
Nearly 50% of the marks in all universities is allotted to Short Essay or Short Answer question types. This was followed by Long Answer questions and very short answer questions respectively. Relative to the number of marks allotted to each question type the university question papers consisted of 11 to 22 items or questions in every question paper.
A. Domain of the Learning Tested
Theory questions papers attempt to test the knowledge/ cognition of the students. Limiting the questions to just recall type affects the quality of the question paper. Medicine and Forensic Medicine, requires application of knowledge. Testing of higher order cognition is necessary for the assessment to be Valid. To evaluate this the questions were categorised into Recall type, Comprehension type and application type. The percentage distribution of marks in each question paper was also analysed and presented in the Line graph (Figure 1).
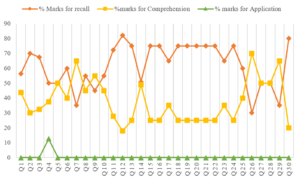
Figure 1. Comparison of percentage mark distribution based on the domain of learning
B. Distribution of Marks Based on the Subtopics
The Graduate Medical education regulation- 2019 further divide the subject of Forensic Medicine and Toxicology into Forensic Pathology, General Information and legal procedures, medical jurisprudence, Forensic Psychiatry, Toxicology, Lab investigations and general trends. The question papers were further analysed for the percentage distribution of marks among these six subtopics and presented in a radar graph in Figure 2.
Figure 2. Topic wise distribution of marks (%) in the question papers
From the graph it is noted that Forensic Pathology receives the most attention in almost all the question papers from all the universities. Forensic pathology can further be divided into seven subtopics. From the total marks allotted in each paper for forensic Pathology, percentage marks allotted for each of these subtopics was calculated and presented as a separate radar graph in Figure 3.
Figure 3. Percentage distribution of marks in Forensic Pathology in the question papers
Toxicology can further be divided into subtopics like General Toxicology dealing with management of poisons, Chemical Toxicology, drug-pharmacy, and substance abuse dealing with pharmaceutical agents and banned substances, Bio and environmental toxicology dealing with snakebite, venomous stings, mushrooms, Food poisoning and plant toxicology etc. From the total marks allotted to toxicology, the percentage distribution of marks allotted to each of these subtopics was analysed and presented in Figure 4.
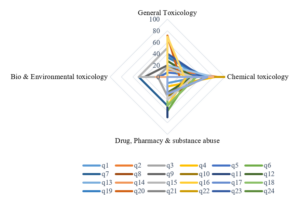
Figure 4. Percentage distribution of marks in Toxicology in the question papers
IV. DISCUSSION
The undergraduate medical education curriculum has been governed by the Graduate Medical Education Rule- GMR 1997 (Medical Council of India, 1997) framed by the Medical Council of India over the last two decades and in 2019, the National Medical Commission adopted a competency-based training model to revamp the medical education in India. The National Medical Commission in its series of reports and documents has attempted to identify the lacuna in the old curriculum. To be able to successfully implement this radically new proposal it is necessary that we understand the limitations of the current curriculum. The Graduate Medical Education Rules 1997, like the newer GMER 2019 provides a clear framework of the Undergraduate curriculum. It lays down guidelines on the standards of implementation. The curriculum framework is designed in a manner that there is significant room for the colleges and the Universities to plan and implement the same as they deem best suits them. This however is not the case always. It has been observed in various previous studies that universities and colleges sometimes fall short of the expectations (Medical Council of India, 1997; National Medical Commission, 2018; Sharma et al., 2005).
Previous studies attempting to gauge the student’s perception on the implementation of Forensic Medicine and Toxicology curriculum have raised serious doubts among the academicians. Kumar et al. (2018) in their study of student’s perception revealed that 20% of the students felt that autopsy was a mere formality and 64% felt the need for student involvement during the autopsy training. Mardikar and Kasulkar (2015) revealed that 89% of the Interns and 41% of the residents didn’t have any exposure to handling medico-legal cases. It was noted that only 14% of the Interns and 21% of the residents were aware of the proper preservatives to be used for body fluids in poisoning. Only 32% of the interns and 46% of the residents were aware of Medical Indemnity Insurance. Only 13% of the interns were aware of the consumer protection act. There is a serious disconnect between the proposed and the implemented curriculum in forensic medicine.
As per the guidelines framed by the Medical Council of India in the GMER-1997, a variety of essay questions and short answer questions are permitted. Objective question like Very Short Answer questions and MCQs are permitted to the extent of 20 % only (Medical Council of India, 1997). Most of the question papers analysed in this study conformed to this regulation. From the Table 1 it can be noted that nearly 50% of the marks were allotted for short essay/Answer questions (SAQ) requiring a descriptive answer. Long Answer Questions (LAQ) requiring an elaborate explanation of the concepts represented about 20% to 42 % of the question paper. The total marks allotted for the individual questions also varied with the LAQs being allotted between 8 to 10 marks each, SAQs being allotted 3 to 5 marks and VSAQs being allotted 1- 2 marks each. Thus, the Number of Items included in each question paper ranged from 11 to 22. This distribution is similar to the analysis published in papers of other subjects like microbiology, Pharmacology, anatomy, Physiology etc (Aggarwal & Agarwal , 2017; Ayub et al., 2013; Bhattacharya et al., 2017; Choudhary et al., 2012; Chowdhury et al., 2017; Mehta & Kikani, 2019; Pichholiya et al., 2021).
With the number of items being limited the chance of certain areas being missed increases. This has a profound influence on the sampling while making the blueprint (Raymond & Grande, 2019). In papers with only 11 Items, there is a definite probability of certain topics being left out compared to papers having 22 items. As Forensic Medicine and Toxicology has only one paper compared to other subjects which have two papers in the second year MBBS, some key topics get left out, adversely effecting its content validity.
A. Analysis of the Domain of Learning Tested
From the Figure No 1, it can be observed that in about 10 of the 30 papers, more than 75% of the questions/ Items tested recall. In only 7 of the 30 papers, more than 50% of the marks were allotted to comprehension. In only one paper the application was assessed to an extant of 12.5%. This is similar studies done in Anatomy, Physiology, Pharmacology, and microbiology (Aggarwal & Agarwal., 2017; Bhattacharya et al., 2017; Choudhary et al., 2012; Chowdhury et al., 2017; Mehta & Kikani, 2019).
This raises a serious doubt on the construct validity of the question papers. Forensic Medicine and Toxicology, an application-based course requires that higher order cognition like application is tested. The current papers fall short of assessing the right competency domains. The Regulations prescribed by the GMER-1997 require that the at least one long answer question (LAQ) of 10 marks (i.e., 25% of the Marks) testing application is asked in the theory question paper (Medical Council of India, 1997). The newer Competency based medical education Regulations prescribed in the GMER- 2019 document also reiterate this fact and in addition suggest that an application based question including Attitude, Ethics and communication skills module be included in every paper (National Medical Commission, 2018). This needs serious introspection in the times to come.
B. Content Validity of the Question Papers
The content validity of a test depends strongly on how well the sample is spread across the syllabus. From the analysis of the percentage distribution of marks allotted to different subtopics presented in figure no 2, it is very clear that in majority of the question papers the bulk of the questions asked are from forensic pathology. There is distinct skewing of the graph toward forensic pathology with an average allocation of 60% of the marks.
This is like studies in physiology with over 42% of the marks being allotted to Cardiovascular system. The observations in the figure no 2 classically suggest that the forensic medicine and toxicology curriculum is a victim of “Carcinoma of the Curriculum” (Abrahamson, 1978). Over a period, certain section of the curriculum takes precedence and are valued more than other equally relevant sections. Core areas like Toxicology and Medical Jurisprudence which are clinically more relevant to the undergraduate students, considering their role as a physician of the first contact, seem to have been blatantly missed and neglected. Faculty should reflect on the factors that might have caused this drift which over time has led to this dangerous disease of the curriculum.
The New Competency based UG curriculum being implemented by the National Medical Commission wonderfully provides a framework of competencies in forensic medicine and toxicology (National Medical Commission, 2018). They serve as guiding milestones to reorient and redistribute the weightage, time and value allotted to certain topics.
From the Percentage marks allotted to each of these subtopics in forensic pathology in Figure no 3 it clearly shows that over 60 to 70% of the marks allotted were distributed among just 3 key topics i.e., Post-Mortem Changes, Mechanical Injuries and Asphyxia. The source of the error in the assessment is this high value allotted to theoretical aspects related to Autopsy and Medical examination. The faculty and the student’s attention have shifted towards the conduct of postmortem examination which is generally a high stakes scenario. But only a handful of undergraduates end up doing autopsies in their career. The ability to do autopsy is no doubt an important competency for the Undergraduates but the competencies related to Medical Jurisprudence and Toxicology are equally Important. The competencies related to handling Medico- legal issues related to patient care are encountered more frequently by an undergraduate thus requiring additional attention in the undergraduate curriculum than Forensic Pathology which is a rare or chance encounter for an MBBS graduate in India (Kumar et al., 2018; Medical Council of India, 1997; National Medical Commission, 2018; Sharma et al., 2005).
An Indian Medical graduate needs to make accurate observation, logical deductions and take critical decisions applying medical ethics in patient care. He should be able to diagnose and manage the common cases of poisoning as a physician of the first contact (Kumar et al., 2018; Medical Council of India, 1997; National Medical Commission, 2018; Sharma et al., 2005).
Most of the competencies in Toxicology are covered in the Forensic Medicine curriculum rather than in General Medicine. Hence, the percentage marks allotted for various subtopics of toxicology was also analysed in figure no 4. From figure no 2 it can be noted that about 20% of the marks were allotted to toxicology. Further considering figure no 4 it can be observed that 60-80% of the marks for toxicology was allotted to general toxicology and chemical toxicology showing a skewing in the distribution of marks.
Assessments must complement the roles of the undergraduate after completion of the course. Snake bite, an occupational disease in India, is an emergency frequently encountered by physicians of first contact (Vijay & Hegde, 2019). Substance abuse and pharmaceutical toxicity are also some of the most encountered cases in clinical practice following pesticide abuse (Basu & Mattoo, 1999). As a curriculum planner it is imperative that these factors considered as core in the curriculum (Amin et al., 2006; Amin & Khoo, 2003, pp. 260; McAleer, 2001). The current UG curriculum is deficient as certain areas have been undervalued leading to poor perception about the subject. Students undervalue the subject as the core competencies tested are not relevant considering their role as physician of the first contact. Students allot little time to study as most assessments cover few topics leading deterioration in the quality of teaching and learning in the course (Sharma et al., 2005).
Adult learners value learning bases on its immediate applicability and its use in problem solving. Curriculum must value topic and skill that complement the roles the learner after the training. Medical jurisprudence and toxicology have not been sufficiently assessed in this curriculum.
V. CONCLUSION
From the above discussion, it is reiterated that the university assessments in Forensic Medicine and Toxicology need to be realigned with the curricular needs. Certain subtopics like Forensic Pathology have been over valued compared to Medical Jurisprudence and Toxicology which have been undervalued. The sampling in Forensic Medicine and Toxicology assessment is not ideal. Application must be tested instead of just recall.
Universities need to periodically Assess their question papers for validity and chalk down clear guidelines for the paper setters. The current blueprints being used must be revalidated to check if there is clarity and scope of improvement. Most importantly, training the faculty and the question paper setters to use the blueprint and value the competencies mandated by the Curriculum lies at the heart of the solution to this problem. Overtime, this curricular malignancy observed, has had a profound effect on the mindsets of the faculty trainers. Faculty Developments activities to motivate and influence these mindsets to bring change is indispensable. The Application centered regulations prescribed by the National Medical Commission provides an excellent opportunity to motivate positive changes leading to the required course correction.
Notes on Contributors
Dr Vijay Kautilya was instrumental in conseptualising the idea, designing the study, data collection, data analysis, drafting and reviewing the manuscript.
Dr Arijit Datta contributed in designing the study, data collection, data analysis, drafting and reviewing the manuscript.
Dr Shruti P Hegde was instrumental in designing the study, data analysis, drafting and reviewing portions of the manuscript.
Dr Preethi Tiwari, contributed in data collection, data analysis, drafting and reviewing portions of the manuscript.
Ethical Approval
Institutional Ethics committee approval was received from the IEC, Government Medical College, Bharatpur where the study was conducted (GMCB/IEC/2020/009 dated 26th September 2020).
Data Availability
Datasets generated and/or analysed during the current study are available from the following DOI.
https://doi.org/10.6084/m9.figshare.19367864
Acknowledgement
We wish to acknowledge the Faculty of Forensic Medicine and Toxicology at MTMC, Jamshedpur for assisting in procurement of the question papers.
Funding
No external funding was received for the conduct of this study.
Declaration of Interest
There is no conflict of Interests to the best of our knowledge.
References
Abrahamson, S. (1978). Diseases of the curriculum. Academic Medicine, 53(12), 951-957. https://doi.org/10.1097/00001888-197812000-00001
Aggarwal, M., & Agarwal, S. (2017). Analysis of undergraduate pharmacology annual written examination papers at Pt. B. D. Sharma University of health sciences Rohtak. National Journal of Physiology, Pharmacy and Pharmacology, 7(5), 509. https://doi.org/10.5455/njppp.2017.7.1236224012017
Amin, Z., Chong, Y. S., & Khoo, H. E. (2006). Practical guide to medical student assessment. World Scientific. https://doi.org/10.1142/6109
Amin, Z., & Khoo, H. E. (2003). Basics in Medical Education. World Scientific.
Ayub, M., Habib, M., Huq, A., Manara, A., Begum, N., & Hossain, S. (2013). Trends in covering different aspects of anatomy in written undergraduate MBBS course. Journal of Armed Forces Medical College, Bangladesh, 9(1), 75-83. https://doi.org/10.3329/jafmc.v9i1.18729
Basu, D., & Mattoo, S. K. (1999). Epidemiology of substance abuse in India: Methodological issues and future perspectives. Indian Journal of Psychiatry, 41(2), 145-153.
Bhattacharya, S., Wagh, R., Malgaonkar, A., & Kartikeyan, S. (2017). Analysis of content of theory question papers in preliminary examinations and marks obtained by first-year MBBS students in physiology. International Journal of Physiology, Nutrition and Physical Education, 2(2), 856-868.
Choudhary, R., Chawla, V. K., Choudhary, K., Choudhary, S., & Choudhary, U. (2012). Content validity of first MBBS Physiology examinations and its comparison with teaching hours devoted for different sub-divisions of physiology. Journal of Physiology and Pathophysiology, 3(1), 8-11.
Chowdhury, D. K., Saha, D., Talukder, M. H., Habib, M. A., Islam, A. S., Ahmad, M. R., & Hossin, M. I. (2017). Evaluation of pharmacology written question papers of MBBS professional examinations. Bangladesh Journal of Medical Education, 8(2), 12-17. https://doi.org/10.3329/bjme.v8i2.33331
Gupta, S., Parekh, U. N., & Ganjiwale, J. D. (2017). Student’s perception about innovative teaching learning practices in forensic medicine. Journal of Forensic and Legal Medicine, 52, 137-142. https://doi.org/10.1016/j.jflm.2017.09.007
Kumar, A., Kumar, S., Goel, N., Ranjan, S. K., Prasad, M., & Kumari, P. (2018). Attitude of undergraduate medical students towards medico-legal autopsies at IGIMS, Patna, Bihar. International Journal of Medical Research Professionals, 4(6), 132-135.
Kautilya, D. V., Datta, A., Hegde, S. P., & Tiwari, P. (2022). Evaluating the content validity of the undergraduate summative exam question papers of forensic medicine & toxicology from 6 medical universities in India. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.19367864
Mardikar, P. A., & Kasulkar, A. A. (2015). To assess the need of medicolegal education in interns and residents in medical institution. Journal of Evolution of Medical and Dental Sciences, 4(17), 2885-2889. https://doi.org/10.14260/jemds/2015/417
McAleer, S. (2001). Formative and Sumative assessment. In J. A. Dent, & R. M. Harden, A Practical Guide to Medical teachers (pp. 293-302). Edinbergh Churchill Livingstone.
Medical Council of India. (1997). Regulations on Graduate medical education, 1997. https://www.nmc.org.in/wp-content/uploads/2017/10/GME_REGULATIONS-1.pdf
Mehta, S., & Kikani, K. (2019). Descriptive analysis of II – MBBS university question papers of microbiology subject. Journal of Education Technology in Health Sciences, 6(2), 44-47. https://doi.org/10.18231/j.jeths.2019.011
National Medical Commission. (2018). Competency based undergraduate curriculum for the indian medical graduate. https://www.nmc.org.in/information-desk/for-colleges/ug-curriculum/
Parmar, P. (2018). Study of students’ perceptions towards case based learning in forensic medicine. Indian Journal of Forensic Medicine & Toxicology, 12(1), 154-160.
Pichholiya, M., Yadav, A., Gupta, S., Kamlekar, S., & Singh, S. (2021). Blueprint for summative theory assessment in pharmacology – A tool to increase the validity as per the new competency based medical education. National Journal of Physiology, Pharmacy and Pharmacology, 11(12), 1345-1355. https://doi.org/10.5455/njppp.2021.11.06170202107072021
Raymond, M. R., & Grande, J. P. (2019). A practical guide to test blueprinting. Medical Teacher, 41(8), 854-861. https://doi.org/10.1080/0142159x.2019.1595556
Sharma, B., Harish, D., & Chavali, S. (2005). Teaching, training and practice of forensic medicine in India-An overview. Indian Journal of Forensic medicine & Toxicology 27(4), 247-251.
Sudhan, S. M., & Raj, M. N. (2019). Current status of knowledge, attitude and awareness of medical students on forensic autopsy in Tumkur district of Karnataka. Indian Journal of Forensic Medicine & Toxicology, 13(1), 131-141.
Vijay, D. K., & Hegde, S. P. (2019). Study of snake bite and factors influencing snake bite among the rural population of Kancheepuram district. Journal of Punjab Academy of Forensic Medicine & Toxicology, 19(2), 142-146.
*Vijay Kautilya D
Kadani Road, Baridih,
Jamshedpur-831017
Jharkhand, India.
+919448651848
Email: kautilya.dacroo@gmail.com
Submitted: 19 August 2022
Accepted: 5 December 2022
Published online: 4 April, TAPS 2023, 8(2), 47-56
https://doi.org/10.29060/TAPS.2023-8-2/OA2869
Edyta Truskowska1, Yvonne Emmett2 & Allys Guerandel1
1Department of Psychiatry, Faculty of Medicine, University College Dublin, Ireland; 2National College of Ireland, Ireland
Abstract
Introduction: Digital Badges have emerged as an alternative credentialing mechanism in higher education. They have data embedded in them and can be displayed online. Research in education suggests that they can facilitate student motivation and engagement. The authors introduced digital badges in a Psychiatry module in an Irish University. Completion of clinical tasks during the student’s clinical placements, which were previously recorded on a paper logbook, now triggers digital badges. The hope was to increase students’ engagement with the learning and assessment requirements of the module.
Methods: The badges – gold, silver and bronze level – were acquired on completion of specific clinical tasks and an MCQ. This was done online and student progress was monitored remotely. Data was collected from the students at the end of the module using a questionnaire adapted from validated questionnaires used in educational research.
Results: The response rate was 68%. 64% of students reported that badges helped them achieve learning outcomes. 68% agreed that digital badges helped them to meet the assessment requirements. 61% thought badges helped them to understand their performance. 61% were in favour of the continuing use of badges. Qualitative comments suggested that badges should contribute to a higher proportion of the summative mark, and identified that badges helped students to structure their work.
Conclusions: The findings are in keeping with the literature in that engagement and motivation have been facilitated. Further evaluation is required but the use of badges as an educational tool is promising.
Keywords: Medical Education, Digital Badges, Students’ Engagement, Continuous Assessment Gamification, Health Profession Education
Practice Highlights
- Digital badges may enhance student engagement.
- Digital badges may promote motivation for learning.
- Evaluation of digital badges using a questionnaire with ordinal analysis of data and coding of free comments.
- Majority of students reported working harder than in a non-gamified module.
- Digital badges provided structure and direction to the student’s learning.
I. INTRODUCTION
Educational research recognises student engagement as valuable and as having significant impact on their learning (Mandernach, 2015). While searching for tools impacting on engagement, educators observed that games have been good at engaging players for decades, through their ability to sustain players’ attention and keep them motivated throughout the games (Przybylski et al., 2010). This level of engagement is desirable to both students and educators. This achievable level of engagement in gaming strategies has led to the exploration of its use in education. Elements from game design applied in non-game contexts to influence, engage and motivate individuals and groups have resulted in the development of a new field known as gamification (Deterding et al., 2011).
Digital badges are common tools of gamification (Barata et al., 2013). They are frequently used by game designers and in recent years also by educators. A digital badge used in education can be a validated symbol of academic achievement, accomplishment, skill, quality or interest (HASTAC, n.d.). Digital badges are digital images obtained through the completion of some pre-specified goals that are annotated with metadata and that can be displayed online (Hensiek et al., 2017). In higher education badges have been used to recognise a student’s participation in a learning activity, to help students explicitly and visually capture and monitor progress made on learning tasks, to recognise the achievement of skills and competencies and to serve as a means of certifying these achievements. They are reported to have a positive effect on the learners’ motivation if they are considered as awards or if they trigger competition among peers (Yildirim et al., 2016).
It appears that the value of digital badges depends on their design (when awarded, for what, and what they mean). For example, the use of badges as credentials only, has been criticised for focusing exclusively on extrinsic motivating factors, which have less impact on engagement than intrinsic ones (Seaborn & Fels, 2015). This is why combining the use of badges, as credentials as well as using them within the assessment process appears to be a better idea. Considering, that assessment has proven to have the most impact on effective learning, the use of badges during structured assessment has been favoured by educators (Abramovich, 2016; Rolfe & McPherson, 1995). The assessments that have potential to generate formative and summative feedback are presented as particularly useful (Armour-Thomas & Gordon, 2013). Digital Badges represent a viable alternative to existing methods of assessment in educational institutions and in the work environment (Dowling-Hetherington & Glowatz, 2017). It was also noted that access to regular feedback (broadly available in games) is helpful to learners. Students that are given opportunities to complete a task and learn from their mistakes do better in overall assessment. Games are a great example of the design where a player learns through feedback, gets better and eventually becomes successful (McGonigal, 2011). Similarly, the literature states that the use of badges has potential to offer a sort of “covert assessment”, meaning that students can approach a task as if it was a game. This helps to maintain the benefits of assessment while minimizing the potential for unhelpful levels of test anxiety (McGonigal, 2011) (Abramovich et al., 2013).
Another advantage given for the use of digital badges is their potential for remote monitoring of students’ progress and their difficulties by instructors and tutors (Huang & Soman, 2013). There is a growing momentum for the use of digital badges as an innovative instruction and credentialling strategy in higher education (Noyes et al., 2020).
In our University, Psychiatry is taught as a 10-credit module to both undergraduate and graduate entry students in the final stage of their degree in medicine. Typically, approximately 240 students are taught the module in four different groups: two groups in the spring and two groups in autumn, for six weeks at a time. Face to face teaching is centralized on Mondays and Fridays. Clinical teaching is delivered during the rest of the week and takes place in multiple different clinical centres. The overall assessment of this module comprised a continuous assessment with specific formative and summative tasks recorded in a paper logbook. The summative tasks were worth 20% of their overall assessment.
Standardising the student clinical experience, engaging them in their clinical placements and monitoring their attendance and progress can be challenging. The paper logbook/portfolio we were using was inadequate in that it did not allow for central monitoring of progress and often the difficulties students were encountering came to the attention of the teaching staff only when the logbook was handed over at the end of the module. Provision of feedback on progress was also limited. We felt that, in particular, students that were slow to progress were missing potential remediation before the summative assessments. We also encountered practical difficulties such as lost logbooks that affected the continuous assessment process.
We felt that digital badges offered a way of monitoring attendance and participation in tasks remotely, providing feedback, facilitating remediation and allowing students’ gauge how they are doing in relation to their peers while optimizing engagement in the clinical placements and structuring the learning to sustain progress through the module. We introduced and piloted the use of digital badges in the Psychiatry module as part of the continuous assessment. We carried out a descriptive study to appraise the potential usefulness of digital badges as part of our teaching strategy.
II. METHODS
A. Course Design
Students taking the 6-week Psychiatry module start their clinical placement on day 2 of the Module. Each week, students participate in their continuous assessment in order to collect their weekly badge. To acquire a badge, they need to complete and upload specific clinical tasks including formative clinical cases scheduled for them, to upload a Clinical Placement Form signed by the consultant on the team they are attached to and do an online multiple-choice question test at the end of the week. As all of this is done online their progress can be monitored remotely by the teaching team independent of the location of their clinical placement. Collecting their weekly badges provides them with 5% of their continuous assessment mark. The other marks for continuous assessment come from a summative clinical case (90%) and a reflective assignment (5%). Continuous assessment contributes to 20% of overall assessment mark.
B. Badges Design
Tutors in Psychiatry in conjunction with the University’s Teaching and Learning Department created Badges. It was part of an institution-wide digital badging pilot project (UCD Teaching and learning, 2017). It was agreed that there would be three types of badges -bronze, silver and gold – obtained and displayed on the university’s virtual learning environment (currently, Brightspace). As noted above students receive a digital badge on completion of assigned tasks, which are part of their continuous assessment. The type of badge awarded depends on the MCQ score and it is displayed on the student’s Blackboard profile. Figure 1 depicts the process. It shows that all badges are contributing to 5% of the module continuous assessment. Every week students receive information as to what percentage of the group has acquired a bronze, silver or gold badge so they have an idea of their performance in relation to that of the rest of the group.
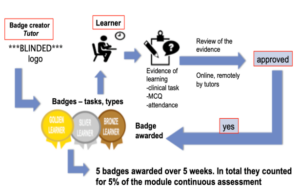
Figure 1. Step-by-step the process of getting/awarding a badge
C. Questionnaire
The ‘Digital Badges Experience Survey’ questionnaire was designed based on previously described surveys: the ARCS Badge Motivation Survey (Foli et al., 2016) and the Badge Opinion Survey (Abramovich et al., 2013) with some additional questions suggested by the literature on digital badges. The authors and faculty members identified and agreed on the following constructs as being relevant to our teaching delivery and our study: previous knowledge of digital badges (items 1 & 2), their meaning and relevance to students (items 22, 13, 14, 12, 8 & 5) motivation and engagement (items 3, 4 & 23), relevance to assessment and feedback (items 11, 9, 10, 24, 18 & 19), their use in structuring learning (items 15, 6, 7 & 16), self-efficacy (items 17, 20, 21 & 25), social context implication (items 26, 27 & 28). Under each construct, items from the above questionnaires were discussed and agreement reached on the ones to be used, altered or added assessing relevance and acceptability for our aims and teaching context.
Our survey consisted of 30 items with answers displayed on a seven-point Likert Scale. The 31st (final) question required dichotomous (yes/no) answer with space for respondents to explain their reasons for it. We also provided for free commenting from students (Questionnaire is available in Table 1).
Please rate your agreement with each of the statements using the following scale:
|
Strongly Agree |
Agree |
Somewhat Agree |
Neutral |
Somewhat Disagree |
Disagree |
Strongly Disagree |
||
|
+3 |
+2 |
+1 |
0 |
– 1 |
-2 |
-3 |
||
|
Please circle one number for each statement |
Strongly Agree |
|
|
Strongly Disagree |
||||
|
1. I knew what digital badges were before I began this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
2. I have earned digital badges before beginning this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
3. I felt motivated to complete the module because I was earning digital badges. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
4. Compared to other modules on my programme, the digital badges motivated me to work harder. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
5. The digital badges helped me to understand the learning outcomes for this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
6. The digital badges helped me to achieve the learning outcomes for this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
7. The badge helped draw my attention to the clinical seminars. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
8. The digital badges helped me to understand the content of this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
9. The digital badges helped me to understand the assessment requirements for this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
10. I was more aware of the module continuous assessment requirements because I would be earning digital badges. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
11. Because I was earning digital badges, I knew the continuous assessment requirements were important. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
12. Earning digital badges made a difference in how I viewed completing the continuous assessment requirements. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
13. Earning badges made the assignments more significant to me. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
14. The badges increased how relevant the assignments were. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
15. The digital badges helped me to structure my work in this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
16. The digital badges helped me to meet the assessment requirements of this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
17. The badges increased my confidence that I could demonstrate the content of my knowledge. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
18. The digital badges helped me to understand my performance in this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
19. The digital badges helped me to understand my progress through the module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
20. The badges were symbols that I had mastered content. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
21. The badges increased my overall level of satisfaction with completing the continuous assessment requirements. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
22. By earning the badges I was more fulfilled as a student by completing the assessment requirements. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
23. The digital badges made me want to keep on working. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
24. I understand why I earned all of my badges. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
25. The badges I earned represent what I learned on this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
26. I talked to others about the badges I earned. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
27. I compared the badges I earned with others’ on the module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
28. The potential to earn digital badges at gold, silver and bronze levels made me feel competitive. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
29. I think digital badges are a good addition to the programme. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
30. I would like to earn digital badges in other modules on my programme. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
31. I think the badges are helpful and should be used in the coming years: tick as appropriate and give 3 reasons why |
Yes ☐ |
No ☐ |
||||||
|
32. Any other comments |
||||||||
Thank you for your participation
Table 1. Digital Badges Experience Survey
D. Participants
The questionnaires were distributed to all the students of final year of Medicine in our university at the beginning of the final or sixth week of the module and collected by their tutors. Informed verbal consent was obtained from study participants. As described above, the course was run four times in one academic year, and we collected data from all four groups of students: two in the spring and two in the autumn.
E. Data Collection and Analysis
As noted above, questionnaires were distributed and collected by tutors at the beginning of the sixth (last) week of the Psychiatry Course. The level of student’s agreement with various statements was marked on the 7-point Likert-type scale. Those data were uploaded to Excel. Data from Likert scales can be analysed as ordinal as well as interval data (Sullivan & Artino 2013), (Norman, G. 2010) and we have considered both options. We concluded that using descriptive statistics such as the mean in relation to students’ opinions had limited value (Sullivan & Artino 2013), (Knapp 1990). This is why we decided to analyse our data as ordinal. To simplify the answers, we organised them into three groups: “agreed”, “neutral”, “disagreed”.
Students’ comments were entered into an excel sheet and analysed by two independent researchers. The comments relating to the use of badges in teaching of Psychiatry were coded according to topics, which were identified and agreed upon by the two independent researchers (Johnson & LaMontagne, 1993), (Sundler et al., 2019). Topics were further codified as positive or negative. This way of coding is described and performed in more details in other studies (Quesenberry et al., 2011).
III. RESULTS
A. Demographics
161 out of 237 students completed questionnaires giving a 68% response rate. The response rate was 75% in the first half (from springtime) of the students and 61% in the second (autumn rotation).
B. Analysis of Answers
65% of students had no previous knowledge of digital badges and 93% had never earned a badge before the module as per items 1 & 2 of questionnaire.
1) Meaning and relevance: Item 22: 48% of respondents agreed that by earning the badges they felt more fulfilled as a student when completing the assessment requirements. 31% disagreed. 45% agreed and 39% disagreed that earning badges made the assignments more significant to them (item 13) and similarly only 42% felt the badges increased the sense of how relevant the assignments were, while 40 % disagreed with this view as per item 14.
Earning digital badges made a difference in how 59% of students viewed completing the continuous assessment requirements, (item 12). 29% disagreed with this. 68% students felt that the digital badges helped them to understand the content of this module and 18% disagreed, (item 8). 66% students agreed and 24% disagreed about the fact that digital badges helped them to understand the learning outcomes for this module (item 5).
2) Motivation and engagement: 51% of students that responded felt motivated to complete the module because they earned a digital badge (item 3). 33% did not agree with this. The possibility of earning a digital badge motivated 43% of respondents to work harder (item 4). 39% disagreed with this. The digital badges made 45% of students want to keep on working, while 29% were not impacted (item 23).
3) Assessment and feedback: Item 11: 50% felt that because they were earning digital badges, they knew that the continuous assessment requirements were important. 36% disagreed. The digital badges also helped 69% respondents to understand the assessment requirements for this module but not so for the 15% respondents (item 9). Out of all respondents, 78% were more aware of the module continuous assessment requirements because of the digital badges, and only 15% disagreed with that (item 10). Item 24: As many as 74% of all respondents did and 14% did not understand why they earned their badges. The digital badges helped 61% of students to understand their performance in this module (item18). 27% did not find that badges helped in that way. Similarly, the digital badges helped 61% of students to understand their progress through the module. 22% disagreed with this (item 19).
4) Structure: Out of all respondents 50% agreed and 33% disagreed that the digital badges helped them to structure their work in the module (item 15). 64% of respondents agreed and 21% disagreed that the digital badges helped them to achieve the learning outcomes for this module (item 6). Similarly, the badge helped draw attention to the clinical seminars for 57% of respondents, but not so for 25%. 68% of students (vs 19% who have disagreed) felt that the digital badges helped them to meet the assessment requirements of this module (item 16).
5) Self-efficacy: Item 17: 48% of students agreed (vs 33% who disagreed) that earning the digital badges made them more confident that they could demonstrate the content of their knowledge. Item 20: 41% of all respondents agreed that the badges were symbols of mastering the content of the module. A similar number (40%) of students disagreed and 17% stayed neutral. 59% found the badges increased their overall level of satisfaction with completing the continuous assessment requirements (item 21). 27% disagreed with this. 44% of students agreed and 41% disagreed with the statement that the badges they earned represented their learning in the module (item 25).
6) Social context and competitiveness: 42% of students did and 44% did not talk to others about the badges they earned (item 26). The potential to earn digital badges at gold, silver and bronze levels made 49% of students more competitive (item 28). 39% disagreed with this. 29% of students did and 56% did not compare the badges they earned with others on the module (item 27).
7) Overall: 56% agreed that digital badges were a good addition to the program. 61% of students found digital badges helpful and felt that they should be used in the future. 31% did not agree with the statement and 8% did not answer.
Students’ opinions: 136 students did and 25 students did not write any comment. Students’ comments related either to one or to several topics. Students were positive about the use of badges (in various topics) 134 times (See Figure 1) and negative/critical 106 times (See Figure 2). It is important to note however that as many as 67 out of the 106 negative comments related to the low value of the badges.
Figure 2 depicts information about positive topics included in students’ comments. 50 students liked the structure and focus that the badge system provided. Twenty-eight students found badges motivating and 24 valued feedback they received in the process. A number of students found the whole process enjoyable, rewarding and fun (See Figure 2). Figure 3 indicates the negative opinions. The most frequent topic of all was repeated 67 times as was related to the value of badges (See Figure 3). Figure 4 shows some comments made by students in the free comment box provided on the survey (See Figure 4).
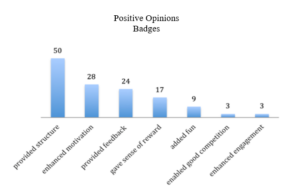
Figure 2. Frequency of positive comment grouped by topic
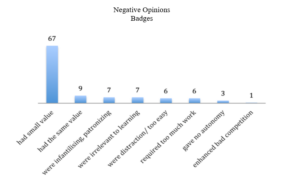
Figure 3. Frequency of negative comment grouped by topic
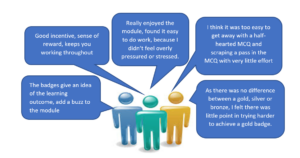
Figure 4. Comments written by students
In summary, the majority of the students liked the way Digital Badges were used in the teaching of Psychiatry, however both groups (those that liked and those that dislike badges) criticized them for their low value of the overall assessment.
IV. DISCUSSION
Students met digital Badges piloted in the teaching of Psychiatry to Medical Students of our university originally with apprehension. The majority of the students had never heard of digital badges and have never earned a digital badge before this module. However, data from the study looking at students’ perception of the use of digital badges in medical education provided encouraging results.
A. Sense of Reward
Students found badges rewarding yet complained about the small value of the badges. This reflected our design intention in which we wanted to support and engage students rather than focus on extrinsic motivating factors such as sense of reward.
As mentioned above the badge was awarded for completion of weekly tasks, and the acquisition of a badge was functioning more as a method of feedback to students rather than for grading. However, a number of students complained about this, and reported a sense of frustration and a lack of motivation to try harder when the assessment value of the badge was so low.
Nevertheless, our design was supported by other studies. One such study concluded that achievement of badges could influence students’ behaviour even if they do not interfere with grading (Hakulinen & Auvinen, 2014). It seems that competitiveness was triggered in those who wanted to do better anyway.
We were pleased to see learners’ comments about reduced stress during the module. We wanted our award system to potentiate a sense of safety around assessment, giving participants freedom to learn from their mistakes without influencing their final grade. This is a well-recognized principle in gamification as a facilitator of students’ engagement (De Byl & Hooper, 2013).
In addition, our design was guided by the fact that the best use of badges was linked with the recognition of already occurred learning, therefore more viewed as an assessment tool, providing feedback and possibly self-reflection (Reid et al., 2015).
B. Impact on Structure, Assessment and Feedback
We were pleased to note that students in our study felt that digital badges provided direction and structure to their learning. This was also reflected in their comments: students mentioned how badges impacted on their study structure, helping them to focus attention on important aspects of the seminars. These findings are consistent with a study that reported that students who enjoyed badges, found them helpful in giving them the direction they needed to work in (Abramovich et al., 2013). These students also praised the alignment between badge topics and course content (Abramovich et al., 2013).
We were also hoping that badges designed, as part of an assessment that generates formative feedback would help students know if they are progressing enough to meet the requirements of their class (HASTAC n.d.). Based on responses to items 24, 18 and 19 it appeared that students benefited somewhat from the potential guidance and feedback provided by the digital badges system.
It is important to remember that students were asked about the badges at their review seminar and few days prior to their exams. This timing could have influenced their answers. For example, students’ opinion was divided on the statement that earning a badge gave them a sense that they have mastered the course content. Similarly, opinion was divided on whether badges increased students’ confidence that they could demonstrate their knowledge, nevertheless more students felt that they had an impact. It would be interesting to see if students’ responses had been different after their exams. We know gamification has already been described as a powerful strategy that can help achieve learning objectives by affecting the way students behave (Huang & Soman, 2013).
C. Impact on Motivation and Engagement
In our study, a majority of students responded that they worked harder in this module compared to non-gamified modules. Similarly, about 30% more students stated that they were more motivated to work harder through the module because they were earning digital badges. Interestingly when they were given space to provide free comment, many have noted that they did feel more motivated, and a few felt more engaged. Previous studies also reported that students were more likely to engage in the game-like tasks providing rapid feedback (Thamvichai & Supanakorn-Davila, 2012). In other publications students also considered gamified courses to be more motivating, interesting and easier to learn as compared to other courses (Barata et al., 2013), (Dicheva et al., 2015), (Hakulinen & Auvinen, 2014). It is suggested that badges are most valued by learners who are extrinsically motivated and value external validation (Foli et al., 2016).
D. Impact on Outcomes
We did not compare outcomes in overall performance in assessment between students before and after implementation of badges. Having considered this, we decided against it. We felt there were too many variables influencing students’ performance and it would be difficult to definitely attribute potential change to the implementation of digital badges.
E. View of Badges and Learner Type
The impact of an educational tool could also depend on characteristics of the student as a learner. It is reported that students with high expectation for learning and those that value their learning tasks may view the badge as validating if designed as a performance assessment (having impact on intrinsic motivation), but it may devalue their learning if it was viewed as an external reward (Reid et al., 2015). On the other hand, badges used as an assessment model can have a negative impact on students with low expectancy values (Reid et al., 2015). Another study concluded that engagement in the gamified classroom was dependent on students’ playfulness (De Byl & Hooper, 2013). In this study, we have not addressed the learner types and other such specifications of the individuals in our group of students.
In a systematic review of digital badges in health care education, it is mentioned that digital badges represent an innovative approach to learning and assessment and evidence in further education literature demonstrates that their use increases knowledge, retention and motivation to learn. However, they also report a lack of empirical research investigating digital badges within the health care education context (Noyes et al., 2020).
F. Limitations
Our study is limited by the lack of demographic data from all participants. This reduces the potential for comparison between genders and undergraduate vs postgraduate students. As mentioned above, we have not addressed learner characteristics and types (intrinsic versus extrinsic motivation, playfulness). The timing of the data collection (students completed questionnaires before their exams, rather than after) may also be limiting factors. It is also important to remember that this study allowed only for assessment of subjective impact (via students’ opinions and experience) of the badges on students learning and did not perform objective measures of students’ overall performance.
V. CONCLUSION
This study was performed at the start of the implementation of the digital badges in the module and at the time, it was the only module with elements of gamification throughout the whole undergraduate medical curriculum in our university. Like most changes in the assessment process, the students greeted this with a level of apprehension. It would be interesting to see if students’ opinion has evolved after a few years of digital badges being integrated in the module and when other modules are using them. Nevertheless, our data shows that our group of students felt, that they benefited from the learning structure provided by the digital badges. The online process of obtaining the badges enabled tutors to provide timely feedback and monitor students’ progress. In addition, our findings are in keeping with the literature in that engagement and motivation have been facilitated by introducing the digital badges and as such, they indicate that the use of digital badges is a promising tool in education.
The use of digital badges in Medical Education is only starting and would benefit from more research in its judicious integration in higher education curriculum as appropriate.
Notes on Contributors
Dr Edyta Truszkowska did the literature search, collected and analysed the data and gave feedback on methodology and questionaire developed and wrote paper.
Dr Yvonne Emmett designed the methodology and developed questionaire. She gave feedback on the data analysis and edited the writing of the paper.
Prof Allys Guerandel suggested the implementation of digital badges and research project. She gave feedback on data analysis and wrting of paper making revisions to same.
All three authors have read and approved the final manuscript.
Ethical Approval
Our project has been exempted by ethics committee of our institution Human Research Ethics Committee – Sciences (Exemption number LS-E-17-56).
Data Availability
Data is available on reasonable request and data is shared in the institution.
Acknowledgement
We would like to acknowledge our institution psychiatry teaching team for their support in the implementation of the digital badges.
Funding
There are no sources of funding.
Declaration of Interest
There is no conflict of interest for any of the authors.
References
Abramovich, S. (2016). Understanding digital badges in higher education through assessment. On the Horizon, 24(1), 126-131. https://doi.org/10.1108/OTH-08-2015-0044
Abramovich, S., Schunn, C., & Higashi, R. M. (2013). Are badges useful in education? It depends upon the type of badge and expertise of learner. Educational Technology Research and Development, 61(2), 217-232. https://doi.org/10.1007/s11423-013-9289-2
Armour-Thomas, E., & Gordon, E. (2013). Toward an Understanding of Assessment as a Dynamic Component of Pedagogy. https://www.ets.org/Media/Research/pdf/armour_thomas_gordon_understanding_assessment.pdf
Barata, G., Gama, S., Jorge, J., & Gonçalves, D. (2013, September). Engaging engineering students with gamification. In 2013 5th International Conference on Games and Virtual Worlds for Serious Applications IEEE, UK (VS-GAMES) (pp. 1-8). https://doi.org/10.1109/VS-GAMES.2013.6624228
De Byl, P., & Hooper, J. (2013). Key attributes of engagement in a gamified learning environment. In ASCILITE-Australian Society for Computers in Learning in Tertiary Education Annual Conference, Australia (221-230). https://www.learntechlib.org/p/171232/
Deterding, S., Dixon, D., Khaled, R., & Nacke, L. (2011, September). From game design elements to gamefulness: defining” gamification”. In Proceedings of the 15th international academic MindTrek conference: Envisioning future media environments (pp. 9-15). https://doi.org/10.1145/2181037.2181040
Dicheva, D., Dichev, C., Agre, G., & Angelova, G. (2015). Gamification in education: A systematic mapping study. Journal of Educational Technology & Society, 18(3), 75-88. https://www.jstor.org/stable/jeductechsoci.18.3.75
Dowling-Hetherington, L., & Glowatz, M. (2017). The usefulness of digital badges in higher education: Exploring the student perspectives. Irish Journal of Academic Practice, 6(1), 1-28. https://researchrepository.ucd.ie/handle/10197/9691
Foli, K. J., Karagory, P., & Kirby, K. (2016). An exploratory study of undergraduate nursing students’ perceptions of digital badges. Journal of Nursing Education, 55(11), 640-644. https://doi.org/10.3928/01484834-20161011-06
Hakulinen, L., & Auvinen, T. (2014, April). The effect of gamification on students with different achievement goal orientations. In 2014 international conference on teaching and learning in computing and engineering, Malaysia (pp. 9-16). IEEE. https://doi.org/10.1109/LaTiCE.2014.10
HASTAC. (n.d.). Digital Badges. http://www.hastac.org/digital-badges
Hensiek, S., DeKorver, B. K., Harwood, C. J., Fish, J., O’Shea, K., & Towns, M. (2017). Digital badges in science: A novel approach to the assessment of student learning. Journal of College Science Teaching, 46(3), 28. https://www.proquest.com/scholarly-journals/digital-badges-science-novel-approach-assessment/docview/1854234735/se-2
Huang, W. H. Y., & Soman, D. (2013). Gamification of education. Report Series: Behavioural Economics in Action, 29, 11 -12.
Johnson, L. J., & LaMontagne, M. J. (1993). Research methods using content analysis to examine the verbal or written communication of stakeholders within early intervention. Journal of Early Intervention, 17(1), 73-79.
Knapp, T. R. (1990). Treating ordinal scales as interval scales: An attempt to resolve the controversy. Nursing Research, 39(2), 121-123.
Mandernach, B. J. (2015). Assessment of student engagement in higher education: A synthesis of literature and assessment tools. International Journal of Learning, Teaching and Educational Research, 12(2), 1-14.
McGonigal, J. (2011). Reality is broken: Why games make us better and how they can change the world. Penguin.
Norman, G. (2010). Likert scales, levels of measurement and the “laws” of statistics. Advances in health sciences education, 15(5), 625-632.
Noyes, J. A., Welch, P. A., Johnson, J. W., & Carbonneau, K. J. (2020). A systematic review of digital badges in health care education Medical Education, 54(7), 600-615. https://doi.org/10.1111/medu.14060
Przybylski, A. K., Rigby, C. S., & Ryan, R. M. (2010). A motivational model of video game engagement. Review of General Psychology, 14(2), 154. https://doi.org/10.1037/a0019440
Quesenberry, A. C., Hemmeter, M. L., & Ostrosky, M. M. (2011). Addressing challenging behaviors in Head Start: A closer look at program policies and procedures. Topics in Early Childhood Special Education, 30(4), 209-220. https://doi.org/10.1177/0271121410371985
Reid, A. J., Paster, D., & Abramovich, S. (2015). Digital Badges in undergraduate composition courses: effects on intrinsic motivation. Journal of Computers in Education, 2(4), 377-98. https://doi.org/10.1007/s40692-015-0042-1
Rolfe, I., & McPherson, J. (1995). Formative assessment: How am I doing? The Lancet, 345(8953), 837-839. https://doi.org/10.1016/S0140-6736(95)92968-1
Seaborn, K., & Fels, D. I. (2015). Gamification in theory and action: A survey. International Journal of Human Computer Studies, 1(74), 14-31. https://doi.org/10.1016/j.ijhcs.2014.09.006
Sullivan, G. M., & Artino, A. R. (2013). Analyzing and interpreting data from likert-type scales. Journal of Graduate Medical Education, 5(4), 541-542 https://doi.org/10.4300/JGME-5-4-18
Sundler, A. J., Lindberg, E., Nilssonn, C., & Palmer, L. (2019). Qualitative thematic analysis based on descriptive phenomenology. Nursing Open, 6(3), 733-739. https://doi.org/10.1002/nop2.275
Thamvichai, R., & Supanakorn-Davila, S. (2012). A pilot study: Motivating students to engage in programming using game-like instruction. Proceedings of Active Learning in Engineering Education. St Cloud University. https://nms.asee.org/wp-content/uploads/sites/47/2020/02/St_Cloud_2012_Conference_Proceedings.pdf#page=18
UCD Teaching and learning. (2017). UCD digital/open badges pilot 2016/2017. Implementation and evaluation report. UCD Teaching and Learning, 1-23. https://www.ucd.ie/t4cms/UCD%20Digital%20Badges%20Pilot%20Report.pdf
Yildirim, S., Kaban, A., Yildirim, G., & Celik, E. (2016). The effect of digital badges specialization level of the subject on the achievement, satisfaction and motivation levels of the students. Turkish Online Journal of Educational Technology- TOJET, 15(3), 169-182. https://eric.ed.gov/?id=EJ1106420
*Allys Guerandel
University College Dublin,
School of Medicine and Medical Sciences,
Belfield, Dublin 4, Ireland D04V1W8.
00353868590063
Email: allys.guerandel@ucd.ie
Submitted: 1 August 2022
Accepted: 1 November 2022
Published online: 4 April, TAPS 2023, 8(2), 36-46
https://doi.org/10.29060/TAPS.2023-8-2/OA2855
Marina C. Jenkins1, Caroline R. Paul2, Shobhina Chheda1 & Janice L. Hanson3
1School of Medicine and Public Health, University of Wisconsin-Madison, United States; 2Langone Health, Grossman School of Medicine, New York University, United States; 3School of Medicine, Washington University in St. Louis, United States
Abstract
Introduction: Increases in vaccine hesitancy continue to threaten the landscape of public health. Literature provides recommendations for vaccine communication and highlights the importance of patient trust, yet few studies have examined medical student perspectives on vaccine hesitancy in clinical settings. Therefore, we aimed to explore medical student experiences encountering vaccine hesitancy, mistrust, and personal biases, with the goal of informing medical student education.
Methods: A health disparities course including simulated clinical scenarios required students to complete a written reflection. We sorted reflections written in 2014-2016 to identify common topics and used inductive thematic analysis to identify themes relevant to vaccine hesitancy by group consensus.
Results: Our sample included 84 de-identified essays sorted into three non-exclusive topics: vaccine hesitancy (n=42), mistrust (n=34), and personal bias (n=39). We identified four themes within medical students’ reflections: 1) Building a Relationship, including emphasis on patient-centred approaches; 2) Preparedness and Need to Prepare for Future Encounters, including highlighting gaps in medical education; 3) Reactions to Encountering Hesitant Patients, including frustration; 4) Insights for Providing Information and Developing a Plan with Hesitant Patients, including approaches to presenting knowledge.
Conclusion: Reflections in the context of simulated encounters and discussion are useful in students identifying their preparedness for vaccine discussion with patients. Student reflections can assist educators in identifying missing educational frameworks for particular scenarios such as vaccine hesitancy. Without a structured framework regarding addressing vaccine hesitancy, students draw upon other skills that may contradict recommended practices.
Keywords: Medical Education, Vaccine Hesitancy, Reflective Writing, Bias, Mistrust
Practice Highlights
- Reflective writing can be a useful tool in medical education toward addressing vaccine hesitancy.
- Medical student reflective writing can be used to demonstrate curricular gaps.
- Medical students expressed feeling unprepared to care for vaccine hesitant patients.
- Without a framework for vaccine communication, students may draw on other inappropriate skills.
I. INTRODUCTION
Increases in vaccine hesitancy and refusal threaten public health (He et al., 2022; Hough-Telford et al., 2016; Kempe et al., 2020; Santibanez et al., 2020), especially with the COVID-19 pandemic introducing a need for quick and widespread uptake of a new vaccine (Hamel et al., 2022; Ognyanova et al., 2022). Patients, especially parents, are increasingly seeking alternative forms of health information, such as online sources that can include misinformation (Broniatowski et al., 2018; Hara & Sanfilippo, 2016; Jenkins & Moreno, 2020; Meleo-Erwin et al., 2017). Patient trust in their clinician and the health care system delivering the vaccine strongly influence vaccination decisions (Goldenberg, 2016; Kennedy et al., 2011; Larson, 2016). Trust remains the most important barrier to acceptance and uptake of the COVID-19 vaccine, with mistrust of government, medicine, and science presenting major barriers to vaccine uptake (Ognyanova et al., 2022). Vaccine hesitant patients may bring preconceptions and concerns from their own research to in-clinic vaccine communication. Thus, it is important for clinicians to be well-prepared to work with vaccine-hesitant patients and parents.
Existing recommendations for clinicians encountering vaccine hesitancy emphasise centring patient views and voice instead of a medical, academic perspective (Holt et al., 2016; Koski et al., 2019). Approaches including motivational interviewing, presumptive language around vaccine recommendations, and persistent vaccine reminders without pressuring or dismissing patients have been shown to be effective in addressing vaccine hesitancy in medical practice (Dempsey et al., 2018; Gagneur et al., 2018; Hofstetter et al., 2017), while correcting misinformation and offering evidence to patients have been found to be counterproductive (Holt et al., 2016; Koski et al., 2019). These pre-COVID recommendations remain the same for addressing COVID-19 vaccine hesitancy, and lack of physician preparedness for encountering these patients is still an important issue (Centres for Disease Control and Prevention, 2021). Physicians may have misconceptions about patients’ reasons for vaccine hesitancy, often assuming lack of understanding or information on the safety, effectiveness, and necessity of vaccines (Hough-Telford et al., 2016), rather than recognising the more central roles of trust and validation of concerns. If physicians do not learn approaches for centring patient voices in vaccine communication, these pre-conceived biases may present a barrier to vaccine uptake and patient-physician trust.
While valuable recommendations for addressing vaccine hesitancy in the clinical setting exist, current efforts center around informing practicing clinicians on these approaches and providing more educational resources to patients (Centres for Disease Control and Prevention, 2021). These may not represent a sufficient, long-term solution. Furthermore, resources available for healthcare workers may be inaccessible or overwhelming for physicians independently seeking tools (Karras et al., 2019). Incorporating vaccine hesitancy-centred curriculum into medical education may be the optimal, long-term solution to the lack of physician preparedness for these encounters, especially in the face of future pandemics and introduction of new vaccines. With curriculum renewal efforts incorporating early clinical experiences, students could encounter patients for whom vaccines are recommended, including vaccine hesitant patients, early in medical school. It would provide a better educational experience for students and a better health care experience for patients if students receive education to prepare them for these conversations. However, few studies have examined medical student perspectives on vaccine hesitancy in the clinical setting. Existing studies have found mixed findings around medical students’ reflections on their preparedness for encountering vaccine hesitant patients and highlight the need for expansion of related curriculum in medical education (Brown et al., 2017; Kernéis et al., 2017). While COVID vaccine hesitancy literature lacks exploration of medical student perspectives and preparedness, recent studies have highlighted an additional barrier of vaccine hesitancy among medical students in some settings (Lucia et al., 2021). These findings provide additional motivation for including vaccine hesitancy-specific curriculum in medical education.
Understanding medical students’ reactions to vaccine hesitancy is critical in preparing students to address vaccine hesitancy while maintaining patient trust. In the present study, which used a scholarship-of-teaching approach, we aimed to expand on existing research on medical student preparedness for encountering vaccine hesitancy to examine written reflections on mistrust and personal bias in clinical encounters more broadly and use a larger sample of student narratives. We analysed students’ structured reflections regarding assigned reading, simulated patient encounters, peer discussions, and faculty-facilitated discussions to evaluate medical students’ learning during a health disparities curriculum. Structured reflection on simulated encounters has been shown to be a useful tool for understanding student perspectives (Koski et al., 2018); this approach can inform development of medical curriculum for addressing vaccine hesitancy and may be a useful teaching tool as well for students to practice, discuss, and reflect on their own biases in an educational setting. Therefore, the purpose of this study was to explore medical student reflections on encountering vaccine hesitancy, patient mistrust, and personal biases, with the goal of informing medical student education.
II. METHODS
In this qualitative study, we analysed written reflections from a third-year medical student Skills to Impact Health Disparities course, to evaluate their learning about interacting with vaccine-hesitant patients and parents. This study was determined to be exempt by the relevant institutional review boards, including a waiver of informed consent.
From 2006-2018, a medical school at a U.S., Midwestern university required a one-day core session with the goal of developing learner skills to impact health disparities. Small groups of approximately six students went through five to six standardized patient scenarios, each designed to generate discussion and reflection about clinician bias that can unintentionally influence patient care. During the learning activity, each student spent 3-5 minutes interacting with a standardized patient who presented a challenge designed to provoke a level of discomfort in the learners to allow for discussion and reflection. One of these six scenarios included a parent with a history of vaccine refusal for their child expressing concerns about a recommended vaccine.
Following each case, students engaged in a 15-minute, non-facilitated discussion based on a list of focused questions. After all cases, students joined another group of six students for a 75-minute faculty-facilitated debrief. In addition, students were required to complete a brief critical reflection based on a theme of the core day activity using the LeAP framework (Aronson et al., 2012). This framework is modelled on a clinical framework, the SOAP note (Chief complaint, Subjective, Objective, Assessment, and Plan). Students were asked to consider a specific experience that led to concern or questions; describe the experience as fully as possible; reconsider the experience by getting other perspectives; synthesize learning; and make a plan to address future similar challenges. Students could choose to reflect on simulated or real clinical experiences.
Written reflective essays were available for analysis from years 2014-2016, providing qualitative data about students’ observations and experiences with health disparities and health equity. All available essays (n=292) from 2014, 2015, and 2016 that were submitted as a course requirement for the Skills to Impact Health Disparities Core Day required course were de-identified and organized by year.
To ascertain the topics that the students addressed, three investigators (two involved in this study and one from another study using the larger set of all essays) read all essays. Each investigator then designated each essay to a topic from a jointly-developed list of non-exclusive topics derived from the data. After individually assigning topics for a sample of essays, the investigators met to compare their sorting and reconcile any differences before they went on to sort through another set of essays. This process continued until all essays were assigned to one or more topics. Most topic labels matched topics of the simulated scenarios that the students encountered in the course, while others related to broader issues highlighted across scenarios. With the goal of selecting reflections relevant to the issue of vaccine hesitancy, all reflections designated under the topics of vaccine hesitancy, mistrust, and personal bias were gathered for qualitative data analysis. Literature review and initial reading of essays suggested essays on encountering mistrust and bias relate to students’ experiences when encountering vaccine hesitant patients, despite not all essays relating directly to vaccine hesitancy. Each essay was assigned an identifier with cohort year and an essay number. Individual essays were excluded based on group consensus on lack of relevance to vaccine hesitancy.
Inductive thematic analysis was used to identify codes and themes in the reflection data using a semantic, realist approach to identify explicit reactions from students grounded in clinical experiences to identify themes that could be directly applied to clinical practice (Braun & Clarke, 2006). Four investigators, including two involved in topic assignment (CRP, SC) and two additional investigators (MCJ, JLH), read and discussed six essays to develop a preliminary codebook, applied these codes to the same six essays, then met to discuss and revise the codebook. Subsequently, investigators coded the remaining essays in pairs using the revised codebook through four rounds of coding, making further iterative changes to the codebook and reconciling differences within pairs. The full team then met to discuss the coding, revise code descriptions, refine the grouping of the codes, and agree on descriptions of the groups. Any changes made to the codebook during the analysis process were retrospectively updated in all previous coding, so that all coding data reflected the final version of the codebook. Data were organized with qualitative analysis software (HyperResearch version 4.5.4). After all data were coded, investigators discussed and reached consensus on the themes.
III. RESULTS
A total of 90 reflections were collected from the Skills to Impact Health Disparities course across three cohorts of third-year medical students from 2014-2016 at one U.S., Midwestern university. Based on investigator consensus on lack of content relevance, six reflections were excluded from our study sample. Our final study sample included 84 de-identified reflections across three, non-exclusive topics: 42 categorized as relating to vaccine hesitancy, 34 as mistrust, and 39 as personal bias. We identified four major themes in medical students’ reflections on encountering vaccine hesitancy, mistrust and personal bias: 1) Building a Relationship, 2) Preparedness and Need to Prepare for Future Encounters, 3) Reactions to Encountering Hesitant Patients, and 4) Insights for Providing Information and Developing a Plan with Hesitant Patients. Representative quotes for each theme can be found in Table 1. Supplemental Table 1 lists each theme with the codes that informed the theme.
A. Building a Relationship
In our first theme, medical students recognized the importance of Building a Relationship with hesitant parents or patients as the foundation for discussions about vaccines or other care about which patients expressed hesitance. They focused on approaches such as building rapport, centring the parent/patient’s views during the discussion, acknowledging their efforts to gather information about their health decisions, expressing empathy, and avoiding direct confrontation of the patient’s viewpoint during the discussion. Many of these observations occurred during the core day experience. For example, one student wrote:
“I learned the importance of letting the patient try to teach the doctor what they know rather than the doctor jumping in and lecturing to the patient. In the future I will try to talk less and let the patient explain more about why they oppose vaccinations to better gauge what they understand about the literature before I try to explain why vaccinations are important and the facts about vaccinations.”
[Year3_61]
The students saw the importance of finding points of commonality between their perspectives and those of the patient and moving the conversation toward establishing goals that they could work together with the patient to accomplish.
One student described, “I learned that a big part of approaching this difficult conversation is establishing the correct approach: common goal, shared decision making.”
[Year3_65]
B. Preparedness and Need to Prepare for Future Encounters
Another major theme identified in medical student reflections on encountering hesitant patients was Preparedness and Need to Prepare for Future Encounters. This theme included discussion of whether the student expressed feeling ready for the encounter or whether they thought it was successful, as well as specific plans for preparing for similar encounters in the future. One way that students discussed their own feelings of preparedness was by recognizing their own biases upon reflection of the encounter. For example, one student wrote:
“I realized my own prejudices influenced my care of my patients more than I would have liked. … It was an eye opener that I am not as impartial as I would like to be and that it takes a lot more self-reflection and awareness to be the best care provider I can be.
[Year3_16]
When discussing a need to prepare for future encounters, many students referenced plans to independently seek additional resources, especially those referenced by patients in encounters.
Other students mentioned plans to practice patient interactions related to the reflection encounter; including, “For me, practicing acknowledging a patient’s views and concerns without endorsing or validating false information is paramount.”
[Year1_07]
Some students also referenced plans to request feedback or advice from more senior clinicians. Additionally, several students identified gaps in their medical school curriculum that contributed to their lack of preparedness or that needed to be filled to support future preparedness. Students specifically referred to needing more resources, support, and training for encountering hesitant patients. They sometimes called for system-wide changes to address this gap in knowledge.
C. Reactions to Encountering Hesitant Patients
One of the themes identified in the students’ self-reflection was related to their own and others’ Reactions to Encountering Hesitant Patients. While some students expressed frustration with patients/parents who expressed hesitance about vaccines, they acknowledged that they can be passionate about the topic of vaccines in their patient care, but ultimately, patients and parents make their own decisions.
One student shared, “I have always found it quite distressing when an otherwise healthy child goes unvaccinated, given the enormous amount of evidence in favour of vaccination efficacy and its effect on public health.”
[Year2_86]
Another student shared, “I knew I could not force the patient, and I knew that she ultimately was in control of what she would do.”
[Year3_78]
In some reflections patient and parents were labelled, for example, as “anti-vaxxers.” Some reflections described parents’ and patients’ bias towards the physician or clear messaging of a desire for a different doctor. In encountering standardized patients in our scenarios or in reflecting on patients seen in clinical settings, students acknowledged that these conversations were difficult, and they were able to self-assess their level of comfort with conversations.
This was well-summarized in one reflection: “It was remarkable to me how such a strong reaction from this patient’s mother elicited an equally strong reaction in me.”
[Year2_34]
At times students recognized a point where these difficult conversations could reach a dead end. One student stated, “No matter how hard I would try, nothing seemed to work.”
[Year2_03]
Especially in this context, students reflected ambivalence towards the patient’s decision. For example:
“I personally feel that providers allowing for healthy children on their patient panels to remain unvaccinated indirectly reinforces non-vaccination as being acceptable by the medical establishment. That said, I also see and appreciate that turning a child away from one’s practice because their parents refuse to vaccinate them not only does not solve the problem at hand, but it also leaves a child at a very critical developmental age with no health care at all until an alternative provider can be found. Ultimately, I found attempting to reconcile these seemingly incompatible sides of the issue of dealing with anti-vaccination quite confusing and uncomfortable.”
[Year2_86]
D. Insights for Providing Information and Developing a Plan with Hesitant Patients
A fourth theme centred on students’ insights regarding how to provide information appropriately to patients and how to create a plan with patients who were hesitant regarding the medical recommendations given to them. Medical students suggested a variety of ways to provide information to patients who were hesitant. They noted the importance of contributing relevant facts and evidence, stressing that such information and knowledge in general needed to be presented in an understandable manner.
As one student described, “Finding the appropriate words to use in such conversations with a patient is essential.”
[Year1_44]
Students often wrote that they needed to provide reputable information to inform the patient’s decision-making. Some suggested strategies for how to present information to patients, including the sharing of stories and the use of scary information to convey the level of seriousness of the medical recommendation and advice.
One student referenced storytelling in the literature, “…the use of storytelling, the same method used by the anti-vaccination movement, [can be] a way to counteract the barrage of misinformation regarding vaccines.”
[Year1_90]
Sharing these insights about how to present information, students also moved towards how to develop a plan with their patients with some deliberate suggestions. Some students felt they needed to be persistent in their recommendations for vaccines. Some students explained how intentional discussions on the risks and benefits of their recommendations can help in their negotiation about a care plan with their patients.
One student noted, “This draws along the line of patient autonomy, and as long as we are clear about the risks and benefits with the patient, then ultimately, it’s up to the patient to make the decision about which medications she will take.”
[Year1_52]
|
Medical Students’ Experiences with Vaccine Hesitancy, Mistrust, and Bias |
|
|
Themes |
Exemplar Quotes |
|
Building a relationship |
“I felt it was most important that I listen to his story as much as I possibly could, before I spoke. So I let him talk. I said, ‘tell me your concerns.’” [Year3_18] “My feelings during this situation were somewhat of frustration but more of just desire for the patient to feel as though I was there to care for her child above all else and to come alongside her rather than combat with her.” [Year3_03] “One suggestion that my classmate said was to start out the conversation by validating how they are feeling more and that you understand that they are a good parent rather than jumping into facts about vaccinations which caused the patient to become defensive.” [Year3_61] |
|
Preparedness and need to prepare for future encounters
|
“I need more tools for dealing with these situations in the future.” [Year1_04] “My plan is to educate myself more on the materials available for parents regarding immunizations.” [Year3_03] “Ultimately it would be nice to see EMRs advance to the point where they can track a patient’s problem, not just on a list, but through stages of management and onto completion, with a provider responsible for follow-up.” [Year2_33] “I will seek feedback from my attendings and residents so that I can improve my motivational interviewing skills.” [Year3_81] |
|
Reactions to encounter-ing hesitant patients |
“Ultimately this is a decision of the parent and I can only offer my professional advice…I learned that this topic did elicit some emotion which I was surprised about.” [Year3_79] “I learned that I need to work on my bluntness (what I consider to be honesty), as well as increasing affirmation of patients’ fears, since telling someone they are wrong (in any facet of life) typically doesn’t work out that well.” [Year2_34] “I felt uncomfortable and offended at times during the conversation. The patient clearly was not interested in negotiating vaccination, and when I tried to discuss the validity of some of the studies and articles she had read, she became very defensive.” [Year2_82] “I dealt with a mother who had embraced the anti-vaccination movement. This is an issue that I have thought about a lot but despite my reflections, it is an issue that I do not know how to address well. This filled me with fear because I honestly didn’t know what the best approach was.” [Year1_90] |
|
Insights for providing information and creating a plan with hesitant patients
|
“From the debriefing session I learned that a promising approach for the anti-vaccine population is to continue to offer the vaccines at each well-child check-up without intensive counsel on the risks/benefits of vaccines.” [Year1_13] “I also learned about using pictures to get a visceral response from the parent which hopefully would change their mind about not getting a vaccine.” [Year3_69] “When I encounter this scenario in the future, as I’m sure I will, I will begin by teasing out whether the patient is interested in more information, in which case I can have resources and studies available, or if they have already made up their mind and at that point I need to negotiate the visit to ensure that they continue to see me for whatever care they are willing to receive, even if that doesn’t include all the preventive measures I would like.” [Year2_82] |
Table 1. Medical students’ experiences with vaccine hesitancy, mistrust, and bias—Themes and exemplar quotes
IV. DISCUSSION
In this qualitative study of a curricular activity designed to build medical students’ skills for interacting with patients toward reducing health disparities, we explored medical student reflections on real and simulated patient care encounters related to vaccine hesitancy, mistrust and personal bias, with the overall goal of informing medical student education. This allowed for evaluation of the utility of this curriculum framework, as well as highlighting gaps in medical curriculum around addressing vaccine hesitancy. Our analysis supports that medical student reflections across the areas of vaccine hesitancy, mistrust and personal bias share thematic structure and implications for informing medical curriculum regarding encounters with patients who resist medical advice, as well as recommendations for teaching approaches to communication with patients and parents who express hesitancy about vaccines.
This study highlights the benefits of reflections on simulated clinical encounters in the context of a Skills to Impact Health Disparities course. Reflections in the context of simulated encounters and discussion were successful in encouraging students assess their preparedness for vaccine discussions with patients. Review of written reflections, like those analysed in this study, can assist educators in identifying missing educational frameworks for particular patient care scenarios such as vaccine hesitancy. While efforts are growing to incorporate vaccine hesitancy information into medical curricula, especially now, in response to the COVID-19 pandemic (Kelekar et al., 2022; Onello et al., 2020; Real et al., 2017; Schnaith et al., 2018), there is little focus on recommending or evaluating these efforts on a large scale in the U.S. However, recent efforts to establish innovative curriculum of this kind have shown it to be feasible and effective for improving medical student preparedness in addressing vaccine hesitancy (Kelekar et al., 2022; Onello et al., 2020; Real et al., 2017; Schnaith et al., 2018). The curriculum structure assessed in this study may offer a strong approach to teach students valuable lessons related to vaccine hesitancy and evaluate existing progress in this area.
Findings from this study also highlight gaps in existing medical curriculum for preparing students to encounter hesitant patients. We found that without a structured and deliberate learning framework for addressing vaccine hesitancy, students will draw upon other skills that may not be appropriate and may be counterproductive. Students in this study often expressed feeling unprepared, aligning with prior studies (Brown et al., 2017; Kernéis et al., 2017). However, we found that using a structured framework for reflection encouraged planning future preparation for similar encounters. This included calling for system-wide changes to curriculum and availability of resources. Additionally, discussion with peers and reflection were cited as helping students to feel more prepared for future encounters with hesitant patients.
While discussion with peers as a learning strategy was widely recognized as helpful, outcomes of these discussions varied greatly and were directly related to the student’s overall reflection and plan for future preparation. This sometimes led to misguided solutions, highlighting the need for aligning education and training around similar encounters with evidence-informed recommendations. Many students referenced using an approach of centring patient views, either during the clinical encounter or after peer discussion and reflection, which aligns with recommendations (Centres for Disease Control and Prevention, 2021; Holt et al., 2016; Jarrett et al., 2015; Koski et al., 2019). However, many others referenced using only facts to correct knowledge, which is advised against in the vaccine hesitancy literature (Holt et al., 2016; Koski et al., 2019). In the context of these reflections, there would not be a space for students who came to misguided conclusions about approaching vaccine hesitancy to have this knowledge corrected based on recommended practices. Additional support and curriculum around vaccine hesitancy should be implemented alongside this framework of practice, peer discussion and reflection.
Previous research has shown that written reflections provide an effective tool for students to acknowledge their biases and the potential impact on patient care, as was seen in this study (Ross & Lypson, 2014). Physician biases related to perceptions of patient education, lifestyle, and identity have been documented and found to impact patient care and rapport (Forhan & Salas, 2013; Franz et al., 2021; Verbrugge & Steiner, 1981; Walls et al., 2015). There are concerns of physicians’ dismissal of patients expressing vaccine hesitancy from their care and physicians’ beliefs that patient hesitancy is due to lack of reliable information (Hough-Telford et al., 2016). Physician frustration may contribute to lack of willingness to bridge communication with hesitant patients; this has been seen even at the student-level, in this study and in previous research (Koski et al., 2018). Preparing students for these types of encounters by promoting reflection on frustrations and biases is important for addressing vaccine hesitancy.
Limitations of this study include that data were collected from a single institution. However, detailed, written reflections allowed for in-depth thematic analysis that may transfer to medical students more broadly. Additionally, reflections were from a course required for all medical students at the institution from cohorts over three years. Students’ reflections were written in 2014-2016, prior to the COVID-19 pandemic. However, vaccine hesitancy is an even more relevant topic now and reasons for vaccine hesitancy as well as strategies for addressing it are largely unchanged (Centres for Disease Control and Prevention, 2021). Indeed, vaccine hesitancy to the COVID-19 vaccine highlights the need for deliberate curricular efforts. Another limitation is that our sample only includes students who chose to discuss vaccine hesitancy, mistrust and bias in their reflections. However, this allowed us to analyse a fairly large sample of student reflections for a qualitative study, aiding in robust thematic saturation and providing insights that are relevant beyond vaccine hesitancy cases.
V. CONCLUSION
There are several meaningful implications of this study for medical education. Our findings illustrate benefits of learner reflection to build insights about communicating and building relationships to address vaccine hesitancy in medical education. Students found encounters with vaccine hesitant patients challenging, in part due to lack of preparedness, highlighting a gap in curriculum. Findings demonstrate varied familiarity with existing recommendations for addressing vaccine hesitancy, emphasizing the need to incorporate specific training into medical curriculum regarding specific skills gaps such as with communication. By focusing on mistrust and personal bias beyond vaccine hesitancy-specific cases, medical curriculum can better prepare students to approach these underlying issues with vaccine hesitant patients and patients expressing hesitancy to other medical recommendations in their future clinical practice. Finally, comprehensive efforts to improve vaccine hesitancy preparedness amongst learners are needed in our current climate of medical mistrust, given the prominence of vaccine hesitancy not just in paediatrics but also throughout clinical care in the context of the current COVID-19 pandemic. To improve vaccine confidence and decrease mistrust in the physician-patient relationship, medical educators must address medical student preparedness for encounters with vaccine-hesitant patients and parents through intentional learning strategies incorporated into medical school curriculum. We recommend that medical schools explore incorporating simulated patient encounters or role-play scenarios with structured reflection and discussion activities in response to encounters with hesitant patients, alongside didactic curriculum on evidence-based vaccine communication strategies, as research continues to evaluate best practices for preparing medical students to encounter vaccine hesitancy.
Notes on Contributors
Marina C. Jenkins BA was involved in the conceptual development of this qualitative analysis; analysis of reflective writings for development of themes; writing of introduction, results, methods and discussion and editing all sections and final approval of the manuscript.
Caroline R. Paul MD was involved in the original curriculum, the original sorting process of student reflective writing; the conceptual development of this qualitative analysis; analysis of reflective writings for development of themes; writing of results section and editing of all sections and final approval of the manuscript.
Shobhina Chheda MD MPH was involved in the original curriculum, the original sorting process of student reflective writing; analysis of reflective writings for development of themes; writing of results section and editing of all sections and final approval of the manuscript.
Janice L. Hanson PhD EdS MH was lead in the conceptual development of this qualitative analysis and organization of qualitative data; analysis of reflective writing; writing of results; writing of methods; and primary mentor to first author on writing of introduction and discussion; editing of all sections and final approval.
Ethical Approval
This study received exemption status from the Institutional Review Boards from the University of Wisconsin-Madison and the Washington University in St. Louis.
Data Availability
We do not have IRB permission to share our data in a data repository. The data are essays written by medical students during a required university course. While the essays are de-identified, it could be possible for someone who wrote an essay or participated in discussion groups with those who wrote the essays to identify an individual who wrote an essay.
Acknowledgement
We would like to acknowledge Andrea Maser, MS for her assistance in de-identifying student reflections and organization of student reflections from various student cohorts.
We would like to acknowledge Roberta Rusch, MPH for assistance in the original sorting of student reflections.
Funding
There is no funding source for this study.
Declaration of Interest
The authors have no conflicts of interest to disclose.
References
Aronson, L., Kruidering, M., Niehaus, B., & O’Sullivan, P. (2012). UCSF LEaP (Learning from your experiences as a professional): guidelines for critical reflection. MedEdPORTAL, 8, 9073. https://doi.org/10.15766/mep_2374-8265.9073
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
Broniatowski, D. A., Jamison, A. M., Qi, S. H., AlKulaib, L., Chen, T., Benton, A., Quinn, S. C., & Dredze, M. (2018). Weaponized health communication: Twitter bots and russian trolls amplify the vaccine debate. American Journal of Public Health, 108(10), 1378-1384. https://doi.org/10.2105/ajph.2018.304567
Brown, A. E. C., Suryadevara, M., Welch, T. R., & Botash, A. S. (2017). “Being persistent without being pushy”: Student reflections on vaccine hesitancy. Narrative Inquiry in Bioethics, 7(1), 59-70. https://doi.org/10.1353/nib.2017.0018
Centres for Disease Control and Prevention. (2021). COVID-19 vaccination field guide: 12 strategies for your community. United States Department of Health and Human Services. https://www.cdc.gov/vaccines/covid-19/downloads/vaccination-strategies.pdf.
Dempsey, A. F., Pyrznawoski, J., Lockhart, S., Barnard, J., Campagna, E. J., Garrett, K., Fisher, A., Dickinson, L. M., & O’Leary, S. T. (2018). Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination: A cluster randomized clinical trial. JAMA Pediatrics, 172(5), e180016. https://doi.org/10.1001/jamapediatrics.2018.0016
Forhan, M., & Salas, X. R. (2013). Inequities in healthcare: A review of bias and discrimination in obesity treatment. Canadian Journal of Diabetes, 37(3), 205-209. https://doi.org/10.1016/j.jcjd.2013.03.362
Franz, B., Dhanani, L. Y., & Miller, W. C. (2021). Rural-urban differences in physician bias toward patients with opioid use disorder. Psychiatric services, 72(8), 874-879. https://doi.org/10.1176/appi.ps.202000529
Gagneur, A., Gosselin, V., & Dubé, È. (2018). Motivational interviewing: A promising tool to address vaccine hesitancy. Vaccine, 36(44), 6553-6555. https://doi.org/10.1016/j.vaccine.2017.10.049
Goldenberg, M. J. (2016). Public misunderstanding of science? Reframing the problem of vaccine hesitancy. Perspectives on Science, 24(5), 552-581. https://doi-org/10.1162/POSC_a_00223
Hamel, L., Sparks, G., Lopes, L., Stokes, M., & Brodie, M. (2022). KFF COVID-19 Vaccine Monitor: January 2022 Parents And Kids Update. K. F. Foundation. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-january-2022-parents-and-kids-update/
Hara, N., & Sanfilippo, M. R. (2016). Co-constructing controversy: Content analysis of collaborative knowledge negotiation in online communities. Information Communication & Society, 19(11), 1587-1604. https://doi.org/10.1080/1369118x.2016.1142595
He, K., Mack, W. J., Neely, M., Lewis, L., & Anand, V. (2022). Parental perspectives on immunizations: Impact of the COVID-19 pandemic on childhood vaccine hesitancy. Journal of Community Health, 47(1), 39-52. https://doi.org/10.1007/s10900-021-01017-9
Hofstetter, A. M., Robinson, J. D., Lepere, K., Cunningham, M., Etsekson, N., & Opel, D. J. (2017). Clinician-parent discussions about influenza vaccination of children and their association with vaccine acceptance. Vaccine, 35(20), 2709-2715. https://doi.org/10.1016/j.vaccine.2017.03.077
Holt, D., Bouder, F., Elemuwa, C., Gaedicke, G., Khamesipour, A., Kisler, B., Kochhar, S., Kutalek, R., Maurer, W., Obermeier, P., & Seeber, L. (2016). The importance of the patient voice in vaccination and vaccine safety—Are we listening? Clinical Microbiology and Infection, 22, S146-S153. https://doi.org/10.1016/j.cmi.2016.09.027
Hough-Telford, C., Kimberlin, D. W., Aban, I., Hitchcock, W. P., Almquist, J., Kratz, R., & O’Connor, K. G. (2016). Vaccine delays, refusals, and patient dismissals: A survey of pediatricians. Pediatrics, 138(3), 9, Article e20162127.https://doi.org/10.1542/peds.2016-2127
Jarrett, C., Wilson, R., O’Leary, M., Eckersberger, E., & Larson, H. J. (2015). Strategies for addressing vaccine hesitancy–A systematic review. Vaccine, 33(34), 4180-4190. https://doi.org/10.1016/j.vaccine.2015.04.040
Jenkins, M. C., & Moreno, M. A. (2020). Vaccination discussion among parents on social media: A content analysis of comments on parenting blogs. Journal of Health Communication, 25(3), 232-242. https://doi.org/10.1080/10810730.2020.1737761
Karras, J., Dubé, E., Danchin, M., Kaufman, J., & Seale, H. (2019). A scoping review examining the availability of dialogue-based resources to support healthcare providers engagement with vaccine hesitant individuals. Vaccine, 37(44), 6594-6600. https://doi.org/10.1016/j.vaccine.2019.09.039
Kelekar, A., Rubino, I., Kavanagh, M., Lewis-Bedz, R., LeClerc, G., Pedell, L., & Afonso, N. (2022). Vaccine hesitancy counseling—an educational intervention to teach a critical skill to preclinical medical students. Medical Science Educator, 32(1), 141-147. https://doi.org/10.1007/s40670-021-01495-5
Kempe, A., Saville, A. W., Albertin, C., Zimet, G., Breck, A., Helmkamp, L., Vangala, S., Dickinson, L. M., Rand, C., & Humiston, S. (2020). Parental hesitancy about routine childhood and influenza vaccinations: A national survey. Pediatrics, 146(1). https://doi.org/10.1542/peds.2019-3852
Kennedy, A., LaVail, K., Nowak, G., Basket, M., & Landry, S. (2011). Confidence about vaccines in the United States: Understanding parents’ perceptions. Health Affairs, 30(6), 1151-1159. https://doi.org/10.1377/hltaff.2011.0396
Kernéis, S., Jacquet, C., Bannay, A., May, T., Launay, O., Verger, P., Pulcini, C., Abgueguen, P., Ansart, S., Bani-Sadr, F., Bannay, A., Bernard, L., Botelho-Nevers, E., Boutoille, D., Cassir, N., Cazanave, C., Demonchy, E., Epaulard, O., Etienne, M., & Wyplosz, B. (2017). Vaccine education of medical students: A nationwide cross-sectional survey. American Journal of Preventive Medicine, 53(3), e97-e104. https://doi.org/10.1016/j.amepre.2017.01.014
Koski, K., Lehto, J. T., & Hakkarainen, K. (2018). Simulated encounters with vaccine-hesitant parents: Arts-based video scenario and a writing exercise. Journal of Medical Education and Curricular Development, 5, 2382120518790257. https://doi.org/10.1177/2382120518790257
Koski, K., Lehto, J. T., & Hakkarainen, K. (2019). Physician self-disclosure and vaccine-critical parents׳ trust: Preparing medical students for parents׳ difficult questions. Health Professions Education, 5(3), 253-258. https://doi.org/10.1016/j.hpe.2018.09.005
Larson, H. J. (2016). Vaccine trust and the limits of information. Science, 353(6305), 1207-1208. https://doi.org/10.1126/science.aah6190
Lucia, V. C., Kelekar, A., & Afonso, N. M. (2021). COVID-19 vaccine hesitancy among medical students. Journal of Public Health, 43(3), 445-449. https://doi.org/10.1093/pubmed/fdaa230
Meleo-Erwin, Z., Basch, C., MacLean, S. A., Scheibner, C., & Cadorett, V. (2017). “To each his own”: Discussions of vaccine decision-making in top parenting blogs. Human Vaccines & Immunotherapeutics, 13(8), 1895-1901. https://doi.org/10.1080/21645515.2017.1321182
Ognyanova, K., Lazer, D., Baum, M., Perlis, R. H., Druckman, J., Santillana, M., Qu, H., Trujillo, K. L., Safarpour, A., Uslu, A., Quintana, A., Green, J., Pippert, C. H., & Shere, A. (2022). The COVID States Project# 82: COVID-19 vaccine misinformation trends, awareness of expert consensus, and trust in social institutions. Open Science Framework. https://doi.org/10.31219/osf.io/9ua2x
Onello, E., Friedrichsen, S., Krafts, K., Simmons, G., Jr., & Diebel, K. (2020). First year allopathic medical student attitudes about vaccination and vaccine hesitancy. Vaccine, 38(4), 808-814. https://doi.org/10.1016/j.vaccine.2019.10.094
Real, F. J., DeBlasio, D., Beck, A. F., Ollberding, N. J., Davis, D., Cruse, B., Samaan, Z., McLinden, D., & Klein, M. D. (2017). A virtual reality curriculum for pediatric residents decreases rates of influenza vaccine refusal. Academic Pediatrics, 17(4), 431-435. https://doi.org/10.1016/j.acap.2017.01.01
Ross, P. T., & Lypson, M. L. (2014). Using artistic-narrative to stimulate reflection on physician bias. Teaching and Learning in Medicine, 26(4), 344-349. https://doi.org/10.1080/10401334.2014.945032
Santibanez, T. A., Nguyen, K. H., Greby, S. M., Fisher, A., Scanlon, P., Bhatt, A., Srivastav, A., & Singleton, J. A. (2020). Parental vaccine hesitancy and childhood influenza vaccination. Pediatrics, 146(6), Article e2020007609. https://doi.org/10.1542/peds.2020-007609
Schnaith, A. M., Evans, E. M., Vogt, C., Tinsay, A. M., Schmidt, T. E., Tessier, K. M., & Erickson, B. K. (2018). An innovative medical school curriculum to address human papillomavirus vaccine hesitancy. Vaccine, 36(26), 3830-3835. https://doi.org/10.1016/j.vaccine.2018.05.014
Verbrugge, L. M., & Steiner, R. P. (1981). Physician treatment of men and women patients: Sex bias or appropriate care? Medical Care, 19(6), 609-632. https://doi.org/10.1097/00005650-198106000-00005
Walls, M. L., Gonzalez, J., Gladney, T., & Onello, E. (2015). Unconscious biases: Racial microaggressions in American Indian health care. The Journal of the American Board of Family Medicine, 28(2), 231-239. https://doi.org/10.3122/jabfm.2015.02.140194
*Marina C. Jenkins
Department of Paediatrics
University of Wisconsin-Madison
2870 University Ave., Suite 200
Madison, WI 53703
Email address: mcjenkins@wisc.edu
Submitted: 11 March 2022
Accepted: 28 June 2022
Published online: 4 April, TAPS 2023, 8(2), 14-35
https://doi.org/10.29060/TAPS.2023-8-2/OA2762
Sayaka Oikawa1, Ruri Ashida2 & Satoshi Takeda3
1Center for Medical Education and Career Development, Fukushima Medical University, Fukushima, Japan; 2Center for International Education and Research, Tokyo Medical University, Tokyo, Japan; 3Department of Emergency Medicine, The Jikei University School of Medicine, Tokyo, Japan
Abstract
Introduction: There are various difficulties in treating foreign patients; however, the existing educational programs are still insufficient for addressing this issue. The purpose of this study is to investigate what difficulties are encountered in the treatment of foreigners in emergency departments, and to create scenarios for simulation-based education using real-life cases.
Methods: A cross-sectional anonymous survey to 457 emergency departments was conducted in 2018. Additionally, we conducted a survey of 46 foreign residents who had visited hospitals for treatment in Japan. The data was analysed quantitatively, and the narrative responses were thematically analysed.
Results: Of the 141 hospitals that responded (response rate: 30.9%), 136 (96.5%) answered that they had treated foreign patients. There were 51 and 66 cases with cultural and linguistic difficulties, respectively. In the qualitative analysis, different ideas/beliefs towards treatments or examinations (51.0%) and communication with non-English speaking patients (65.2%) were most common categories in the cases with cultural and linguistic difficulties, respectively. The survey of 46 foreign residents on the surprising aspects of Japanese healthcare showed, 14% mentioned difference in treatment plans between own country and Japan, 12% each mentioned a lack of explanation by medical staff, and a lack of privacy in the examination room. Based on the survey results, we created 2 scenarios of simulation.
Conclusions: Scenarios of simulation-based education using real-life cases may be effective materials for cultivating cultural awareness of medical staff.
Keywords: Cultural Awareness, Cultural Humility, Emergency Department, Foreign Patients, Simulation-based Education
I. INTRODUCTION
According to the Japan Tourism Agency (JTA), the number of foreign visitors to Japan was increasing every year in the midst of the recent rapid globalisation (Japan Tourism Agency, 2021). Although it is currently on the decline due to COVID-19 infection, a survey of foreign visitors to Japan conducted by the JTA in 2018 revealed that 5% of 3,000 visitors had suffered injuries or illnesses while visiting Japan (Japan Tourism Agency, 2019). When visiting a medical institution in an unfamiliar country, patients have anxiety due to language and cultural differences. Various measures are being taken around the world to prevent patients with different cultural backgrounds from being disadvantaged in medical care (NHS England, 2016; Office of Disease Prevention and Health Promotion, 2021), such as training medical staff to recognise factors impeding cultural awareness (Hobgood et al., 2006).
Due to its nature, prompt treatment is required in emergency departments (EDs). Previous reports showed that among 97 EDs in Japan, 84 had some difficulties in treating foreign patients (Kubo et al., 2014), and medical staff faced complex cultural and social problems with foreign patients (Osegawa et al., 2002). According to the reports of Japanese government, health care institutions in Japan organise English conversation training or lectures on cultural differences by foreign lecturers for medical staff to improve treatment of foreign patients (Japan Ministry of Economy, Trade and Industry, 2019; Japan Ministry of Health, Labour and Welfare, 2021). However, a training for cultivating cultural awareness among medical staff who take care of foreign patients is still insufficient (Osegawa et al., 2002; Serizawa, 2007).
Simulation-based education (SBE) is a practical learning method which enables mastery learning (Kelly et al., 2018; Motola et al., 2013), and in Japan, English-speaking simulated patients are increasingly introduced in medical education (Ashida & Otaki, 2022). Simulated patients enhance reflective learning which improves cultural awareness of learners (Leake et al., 2010; Paroz et al., 2016). However, according to a survey of emergency training programs, less than 10% of the programs used SBE as a training method for cultivating cultural awareness (Mechanic et al., 2017).
The purposes of this study were to investigate what difficulties are encountered in the treatment of foreigners in EDs, and to create scenarios of SBE using real-life cases.
II. METHODS
In January 2018, we sent a questionnaire to 457 EDs of residency training hospitals in the top 10 prefectures with the highest number of foreign visitors, Hokkaido, Chiba, Tokyo, Kanagawa, Shizuoka, Aichi, Kyoto, Osaka, Fukuoka, and Okinawa (Japan Tourism Agency, 2016), by postal mail. In an anonymous survey, we asked about the hospital readiness for treating foreign patients and about difficult cases of foreign patients with linguistic or cultural differences in medical care (Appendix 1). The questions about readiness on treating foreign patients were analysed by simple percentages, and descriptive statistics were used for the questions about number of patients visiting ED per day. The narrative responses were collated and thematic analysis was performed. First, two authors created codes, generated several categories based on the codes, and sorted each case into categories independently as an investigator triangulation. Following that, we merged categories that were similar and revised categories that were different in interpretation through discussion. We repeated the member checking until we built our consensus, and the final categorisation was confirmed by all authors. The number of cases in each category was also calculated.
As a sub study, we also conducted a survey of 46 foreigners who were residing in Japan and had visited the hospital for treatment in Japan (hereafter foreign residents) to find patients’ perspectives on medical care in Japan (Appendix 2). The questionnaire was initially sent to those who were recruited by the authors via email using Google form from January to May in 2018, and data were collected by snowball sampling. The data were analysed by simple percentages, and for narrative responses, we created codes and sorted the responses into categories. The number of responses in each category was also calculated. Both questionnaires stated that the participants’ responses would be considered as their consent to the study, and the answers would be used anonymously for educational research.
Following the survey analysis, we selected cases suitable for scenario creation from an educational perspective with focus on the following points: 1) cases which were noted by multiple facilities, 2) difficulties that can be demonstrated by simulated patients; and 3) cases which had teaching points for multiple professions. The scenarios were composed following the Scenario Folder Sections by Seropian (2003) and included case description, manual for simulated patients, and teaching guide for the instructors. The scenarios were reviewed by an experienced medical English communication teacher from a linguistic and cultural standpoint, and by 2 experienced emergency medicine physicians from a medical standpoint. All 3 experts co-reviewed the final scenarios.
III. RESULTS
A. Survey of the EDs
1) Characteristics of the responding EDs: We received responses to the questionnaire from 141 EDs (response rate: 30.9%). Of these, 136 (96.5%) answered that they had accepted foreign patients, 116 (82.3%) had English-speaking staff, and 76 (53.9%) used translation tools or manuals. On the other hand, only 13 (9.2%) answered that they had a full-time English interpreter, and 27 (19.1%) had a website in English. The median number of overall outpatients visiting the ED per day was 30 (1–135), and the median number of foreign patients visiting the ED per day was 0.5 (0–8.3) (Table 1). As for translation method, a variety of methods were used. Of the 76 EDs, 36 (47.4%) answered that they used translation applications on tablet/PC or smartphone (Appendix 3).
|
Total Responded Hospitals |
141 |
|
|
|
|
Readiness on treating foreign patients |
n |
( % ) |
||
|
Have accepted foreign patients |
136 |
( |
96.5 |
) |
|
Have an English-speaking staff |
116 |
( |
82.3 |
) |
|
Use translation tools or manuals |
76 |
( |
53.9 |
) |
|
Have English medical history forms |
52 |
( |
36.9 |
) |
|
Have English medical certificates |
50 |
( |
35.5 |
) |
|
Have English signs for patients |
46 |
( |
32.6 |
) |
|
Have English medical explanation / consent forms |
27 |
( |
19.1 |
) |
|
Have a hospital website in English |
27 |
( |
19.1 |
) |
|
Have a full-time English interpreter |
13 |
( |
9.2 |
) |
|
No. of patients visiting emergency department per day |
Median |
|
Range |
|
|
Total |
30 |
( |
1-135 |
) |
|
Foreign patients |
0.5 |
( |
0-8.3 |
) |
Table 1: Characteristics of the responding hospitals.
2) Cases with cultural / linguistic difficulties: Cultural difficulties were encountered in 51 cases, and linguistic difficulties were encountered in 66 cases. In the thematic analysis, the cultural difficulties were classified into 4 categories: different ideas/beliefs towards treatments or examinations, medical fees, patients’ lifestyle, and others. The linguistic difficulties were classified into 4 categories: communication with non-English-speaking patients, communication with English-speaking patients, communication with interpreters or using translation tools, and others. Different ideas/beliefs towards treatments or examinations (51.0%), and communication with non-English-speaking patients (65.2%) were the most common, respectively. Case examples in each category and how the hospital handled to the cases are shown in Table 2.
|
Cases with cultural difficulties (51 cases) |
|||
|
Categories |
n (%) |
Examples and ways they were handled |
|
|
1 |
Different ideas/beliefs towards treatments or examinations |
26 (51.0) |
The patient’s husband requested that only female medical staff be allowed to examine the patient. -Initially, the doctor in charge was a male, but he was switched to a female doctor. |
|
2 |
Medical fees |
10 (19.6) |
The patient’s credit card was over its limit and he/she could not pay for the hospitalisation. -They asked the embassy of his/her country to handle the international money transfer.
|
|
3
|
Patients’ lifestyle
|
7 (13.7)
|
The patient complained about the predominantly rice-based diet during his/her hospitalisation. -They changed his/her diet to the bread-based one during the hospitalisation. |
|
4 |
Others |
8 (15.7) |
The patient had a low threshold for pain and was very assertive about the pain. -They confirmed that the complaint was due to pain and prescribed adequate painkillers.
|
|
Cases with linguistic difficulties (66 cases) |
|||
|
Categories |
n (%) |
Examples and ways they were handled |
|
|
1 |
Communication with non-English-speaking patients |
43 (65.2) |
The medical staff could not communicate with the patient in either English or Japanese. -They used a translation tool to communicate. |
|
2 |
Communication with English-speaking patients |
10 (15.2) |
The medical staff could understand ordinary conversation, but it was difficult for them to explain medical terms in English. -The English-speaking staff helped them. |
|
3 |
Communication with interpreters or translation tools |
9 (13.6) |
The patient brought in an interpreter, but it was unclear if the interpreter was able to understand the details. -They asked an interpreter to support. |
|
4 |
Others |
4 (6.1) |
The patient asked to provide a medical certificate in his/her native language. -They could not provide a medical certificate in the patient’s native language, so we provided one in English. |
Table 2: Categories of cultural and linguistic difficulties, their examples and ways handled
B. A Survey of the Foreign Residents
As regards the questionnaire sent to the foreign residents, we received 46 responses. Of those, 11 (23.9%) had lived in Japan for more than 30 years. In the multiple-answer questions regarding the reasons for visiting the hospital, 11 (8.2%) answered acute illness treated in the ED (The demographic data of foreigners responded to the survey is shown in Appendix 4). In terms of interpretation in the hospital, 10 (21.7%) answered that they have had some means of interpretation. For the question “What aspects of your medical care in Japan were most surprising or different from those in your country?”, of a total of 50 responses with multiple answers, 7 (14%) answered “difference in treatment plans between own country and Japan ” while 6 respondents (12%) each answered “a lack of explanation by medical staff” and “a lack of privacy in the examination room” (Table 3).
|
Questions about the medical care/staff |
Answer |
No. (%) in total respondents |
|||||
|
Q1 |
Did you have any means of interpretation in the hospital? |
Yes |
10 (21.7) |
||||
|
No |
36 (78.3) |
||||||
|
Q2 |
Could you tell the doctor/nurse about your concerns in history taking? |
Yes |
27 (58.7) |
||||
|
Somewhat |
18 (39.1) |
||||||
|
No |
1 (2.2) |
||||||
|
|
|||||||
|
Q3 |
Did you feel the doctor/nurse really cared for your ideas and culture during the history taking? |
Yes |
23 (50.0) |
||||
|
Somewhat |
17 (37.0) |
||||||
|
No |
6 (13.0) |
||||||
|
Q4 |
Did you feel that you were sincerely cared for during the physical exam? |
Yes |
29 (63.0) |
||||
|
Somewhat |
16 (34.8) |
||||||
|
No |
1 (2.2) |
||||||
|
Q5 |
Could you tell the doctor/nurse about your true concerns about treatment? |
Yes |
29 (63.0) |
||||
|
Somewhat |
12 (26.1) |
||||||
|
No |
5 (10.9) |
||||||
|
Q6 |
Did the doctor/nurse explain the diagnosis and treatment plan clearly? |
Yes |
29 (63.0) |
||||
|
Somewhat |
12 (26.1) |
||||||
|
No |
5 (10.9) |
||||||
|
|
|
|
|||||
|
Q7 |
Were you satisfied with the medical care you received? |
Yes |
32 (69.6) |
||||
|
Somewhat |
12 (26.1) |
||||||
|
No |
2 (4.3) |
||||||
|
Questions about surprising points |
|||||||
|
Q8 |
What aspects of your medical care in Japan was most surprising or different from your country? |
Top 3 Answers |
No. (%) |
||||
|
|
Different treatment plan |
7 (14.0) |
|||||
|
|
Lack of explanation by medical staffs |
6 (12.0) |
|||||
|
|
No privacy in the examination room |
6 (12.0) |
|||||
Table 3: Result of the survey of foreign residents
C. Scenario Development
Based on the survey results, we decided the main topic of the scenarios based on the contents overlapped in multiple cases. “Gender restriction of doctors who treated patients” and “communication difficulty in languages other than Japanese or English” were the most frequent topics in cultural and linguistic difficulties respectively. Following the selection of topics, we synthesised the similar responses to create a scenario that could occur in any size of ED setting. We developed the settings including patient age, sex, language, and backgrounds, regarding that the patient characteristics can be demonstrated by simulated patients. As a result, we developed two scenarios: a scenario of abdominal pain in a Muslim female patient and a scenario of forearm fracture in a Chinese male patient (Appendices 5 and 6). In the abdominal pain scenario, no female doctor was available, and a learner, a male doctor, had to examine and treat a simulated patient who refused to be seen by a male doctor. In the forearm fracture scenario, no interpreter was available, and a learner had to communicate with a simulated patient who spoke Chinese only. The learning objective for the learners was to communicate appropriately with patients with different cultural and linguistic backgrounds. Based on the results of the survey for foreign residents, we indicated the importance of listening to the patient’s concerns carefully as a teaching point. Also, we reflected the survey results of how each hospital handled the cases on the information for instructors and teaching points.
IV. DISCUSSION
At the time of writing this paper, 96.5% of the EDs had accepted foreign patients; and 82.3% had English-speaking staff. However, only 32.6% of the EDs had multilingual signs for patients, which is listed as actions to be taken in the manual for treating foreign patients (Japan Ministry of Health, Labour and Welfare, 2021).
In the present study, most of the EDs used translation tools when treating foreign patients. Various types of translation methods were found to be used in the EDs, the use of which is consistent with the manual for treating foreign patients (Japan Ministry of Health, Labour and Welfare, 2021). However, we found that the EDs still encountered a significant number of cases with linguistic difficulties. This suggests that even though the EDs own the translation tools, medical staff are not able to utilise them in communicating with foreign patients. According to our survey result, it was revealed that more than half of the cases with linguistic difficulties were of non-English speaking patients. To overcome the linguistic difficulties, medical staff need to be capable of using them enough to communicate with patients of various native languages. In addition to the use of translation tools, multilingual medical explanation/consent forms or signs in hospitals may be effectively used in the aim of communication with foreign patients.
Regarding culturally difficult cases, our survey showed the various issues caused by differences of religious background, lifestyles, and ideas and beliefs on treatment and testing between medical staff and patients. This result is consistent with the reports which elaborated difficulties in treating foreign patients in Japan (Tatsumi et al., 2016). Our study showed that different ideas/beliefs towards treatments or examinations was most common theme in the cases with cultural difficulties in EDs. Knowing beliefs of other culture is one of individual’s capabilities to manage effectively in culturally diverse settings (Ang et al., 2007), and a report on psychiatric hospitals showed that medical staff adapted to hospitalised foreign patients’ culture and religion as they built the relationships with the patients over a long period of time (Kobayashi et al., 2014). Whereas, it is difficult to build relationships with foreign patients in the acute ED setting. Thus, we realised that practical training of communication with foreign patients provide knowledge about their cultures and religions in limited time and is critically important for medical staff in EDs.
SBE is an effective educational format which makes learners’ unconscious incompetence to conscious incompetence (Morell et al., 2002), in other words, medical staff may be able to recognise their unconscious biases towards foreign patients by participating in SBE. As consistent with the previous survey by the MHLW (2021), the culturally difficult cases included complicated issues that require the cooperation of administrative staff and full-time English interpreters in the hospital. In the present study, we created the two scenarios targeting medical staff as learners based on the real-life cases with the many responses in the survey. However, we need to create more varieties of scenarios that can involve other professions than health care professionals. Furthermore, the acquisition and retention of learners’ skills in a single training session of SBE is limited (Legoux et al., 2021). SBE aimed at cultivating cultural awareness cannot be completed in a single session but in continuous sessions with multiple scenarios.
The results of our survey of foreign residents showed that they had been surprised at the differences in treatment plans between their country and Japan, a lack of explanation by medical staff, and a lack of privacy in the examination room. We found that it is important to investigate the opinions of those who receive medical care in a country different from their home because their perspectives allow us to recognise the things taken for granted among medical staff. Medical staff’s unconscious biases about patients of different cultural backgrounds or national origins influence their decision-making (Tervalon & Murray-Garcia, 1998), and implicit bias can contribute to miscommunication (Bartlett et al., 2019). Therefore, listening to the concerns of foreign patients is important in order to avoid providing treatment based solely on medical staff’s biases. Furthermore, in creating scenarios, referring to the survey results of multiple stakeholders made the contents more multi-dimensional and relevant. This study was conducted in the contexts of EDs in Japan, however, scenarios created with perspectives of both medical staff and patients who have various cultural backgrounds may effectively address to the real-life problems triggered by unconscious biases, even in other contexts.
In Emergency situations, we often focus on the patients’ cultural backgrounds, national origins, languages, and religious background in order to provide effective treatments. However, recognising our own bias is not achieved by only focusing on the patients’ culture. Self-reflection is necessary to recognise one’s own cultural biases. The process of self-reflection of our own culture is important for cultivating cultural awareness. Furthermore, the importance of cultural humility – discovering one’s own values toward other cultures through continuous self-reflection and becoming aware of one’s own relationship to the world – has been recently noted in medical education (Chang et al., 2012). As a further research, the development of scenarios that include the study guide which ensure the learners’ self-reflection is required for SBE in emergency settings.
There are several limitations in this study. The response rate of a survey for EDs was 30.9%, which is unable to deny sampling bias. We conducted a survey for EDs with a focus on English, however, it is necessary to conduct surveys on languages other than English. In addition, the survey was only for the EDs of training hospitals in the top 10 prefectures with the most foreign tourists. We may consider expanding the number of hospitals to collect more information about difficulties they encounter in treating foreign patients. For the sub study, the snowball sampling had a methodological limitation in calculating total number the survey sent. As a further research, impacts of SBE using these scenarios on the treatment of foreign patients is less clear. To assess whether foreign patients’ satisfaction of medical care will change, and whether unconscious bias towards foreign patients among medical staff will decrease by conducting these scenarios are necessary.
V. CONCLUSION
In the current study, we were able to clarify linguistic and cultural difficulties in treating foreign patients in the EDs. We developed the scenarios for SBE using the real-life difficult cases of foreign patients with linguistic or cultural differences in medical care in Japan. The simulation training using these scenarios may be useful for promoting cultural awareness of medical staff in EDs. In future, more varieties of scenarios of SBE need to be created and shared in order to treat foreign patients safely and adequately.
Notes on Contributors
SO contributed to the design of the study and conducted data collection and analysis. RA devised the project, the main conceptual ideas, and conducted data collection and analysis. ST contributed to the design of the study and the interpretation of the data.
Ethical Approval
This study was approved by the Institutional Review Board of The Jikei University School of Medicine Japan (Approval No. 28-211(8454), 28-276(8519)). An informed consent was obtained from all the participants responded to the survey.
Data Availability
The data that support the findings of this study are not openly available due to privacy. The materials are available from the corresponding author on reasonable request.
Acknowledgement
The authors would like to acknowledge the respondents at the EDs of training hospitals, the foreigners living in Japan, and the young clinicians at The Jikei University School of Medicine for their cooperation in the study.
Funding
This work has been supported by JSPS KAKENHI, grant number 16K08883.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content of the article.
References
Ang, S., Van Dyne, L., Koh, C., Ng, K. Y., Templer, K. J., Tay, C., & Chandrasekar, N. A. (2007). Cultural intelligence: Its measurement and effects on cultural judgment and decision making, cultural adaptation and task performance. Management and Organization Review, 3(3), 335-371. https://doi.org/10.1111/j.1740-8784.2007.00082.x
Ashida, R., & Otaki, J. (2022). Survey of Japanese medical schools on involvement of English-speaking simulated patients to improve students’ patient communication skills. Teaching and Learning in Medicine, 34(1), 13-20. https://doi.org/10.1080/10401334.2021.1915789
Bartlett, K., Strelitz, P., Hawley, J., Sloane, R., & Staples, B. (2019). Explicitly addressing implicit bias in a cultural competence curriculum for pediatric trainees. MedEdPublish, 8. https://doi.org/10.15694/mep.2019.000102.1
Chang, E. S., Simon, M., & Dong, X. (2012). Integrating cultural humility into health care professional education and training. Advances in Health Sciences Education, 17(2), 269–278. https://doi.org/10.1007/s10459-010-9264-1
Hobgood, C., Sawning, S., Bowen, J., & Savage, K. (2006). Teaching culturally appropriate care: a review of educational models and methods. Academic Emergency Medicine, 13(12), 1288-1295. https://doi.org/10.1197/j.aem.2006.07.031
Japan Ministry of Economy, Trade and Industry. (2019, January). Kokunai iryokikan ni okeru gaikokujin kanja no ukeire jittai chosa [Survey on the actual conditions of foreign patients accepted at domestic medical institutions in Japan]. https://www.meti.go.jp/policy/mono_info_service/healthcare/iryou/inbound/activity/survey_report.html
Japan Ministry of Health, Labour and Welfare. (2021, March). Gaikokujin kanja no ukeire no tameno iryokikan muke manyuaru [A manual for medical institutions to accept foreign patients]. https://www.mhlw.go.jp/content/10800000/000795505.pdf
Japan Tourism Agency. (2018, February). Shukuhakuryoko tokeichosa hokokusho [Report on the survey of accommodations and travel statistics]. Ministry of Land, Infrastructure, Transport and Tourism. https://www.mlit.go.jp/common/001220398.pdf
Japan Tourism Agency. (2019, March). Honichi gaikokujin ryokosha no iryo ni kansuru jittaichosa ukeire kankyo no seibikyoka wo okonaimashita [Conducted a survey on the actual conditions of medical care for foreign visitors to Japan and strengthened the development of the receiving environment]. Ministry of Land, Infrastructure, Transport and Tourism. https://www.mlit.go.jp/kankocho/news08_000272.html
Japan Tourism Agency. (2021, June). Shukuhakuryoko tokeichosa [Survey of accommodations and travel statistics]. Ministry of Land, Infrastructure, Transport and Tourism. https://www.mlit.go.jp/kankocho/siryou/toukei/content/001413644.pdf
Kelly, M. A., Balakrishnan, A., & Naren, K. (2018). Cultural considerations in simulation-based education. The Asia Pacific Scholar, 3(3), 1-4. https://doi.org/10.29060/TAPS.2018-3-3/GP10 70
Kobayashi, Y., Yoshimitsu, Y., & Kato, S. (2014). Super kyukyu ni okeru kangoshi no gaikokujinkanja nitaishite ninshiki suru mondai to taio no jissai [Nurses’ perceptions of and responses to foreign patients in a super emergency hospitals]. Nihon Seishinka Kango Gakujutsu Shukaishi [The Japanese Psychiatric Nursing Society], 57(3), 379 383.
Kubo, Y., Takaki, S., Nomoto, Y., Maeno, Y., & Kawaguchi, Y. (2014). Nihon no byoin ni okeru kyukyugairai deno gaikokujinkanja heno kango no genjo ni kansuru chosa. [A survey on the current status of nursing care for foreign patients in emergency departments in Japanese jospitals]. Kosei no shihyo [Journal of Health and Welfare Statistics], 61(1), 17-25.
Leake, R., Holt, K., Potter, C., & Ortega, D. M. (2010). Using simulation training to improve culturally responsive child welfare practice. Journal of Public Child Welfare, 4(3), 325-346. https://doi.org/10.1080/15548732.2010.496080
Legoux, C., Gerein, R., Boutis, K., Barrowman, N., & Plint, A. (2021). Retention of critical procedural skills after simulation training: a systematic review. AEM Education and Training, 5(3), e10536. https://doi.org/10.1002/aet2.10536
Mechanic, O. J., Dubosh, N. M., Rosen, C. L., & Landry, A. M. (2017). Cultural competency training in emergency medicine. The Journal of Emergency Medicine, 53(3), 391-396. https://doi.org/10.1016/j.jemermed.2017.04.019
Morell, V. W., Sharp, P. C., & Crandall, S. J. (2002). Creating student awareness to improve cultural competence: creating the critical incident. Medical Teacher, 24(5), 532-534. https://doi.org/10.1080/0142159021000012577
Motola, I., Devine, L. A., Chung, H. S., Sullivan, J. E., & Issenberg, S. B. (2013). Simulation in healthcare education: a best evidence practical guide. AMEE Guide No. 82. Medical Teacher, 35(10), e1511-e1530. https://doi.org/10.3109/0142159X.2013.818632
NHS England. (2016). NHS England response to the specific duties of the Equality Act. Equality information relating to public facing functions. https://www.england.nhs.uk/wp-content/uploads/2016/02/nhse-specific-duties-equality-act.pdf
Office of Disease Prevention and Health Promotion. (2021, August). Disparities. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities
Osegawa, M., Morio, H., Nomoto, K., Nishizawa, M., & Sadahiro, T. (2002). Present medical practice and problems in emergency disease in foreign travelers requiring hospital admission. Nihon Kyukyu Igakukai Zasshi [Journal of Japanese Association for Acute Medicine], 13(11), 703-710. https://doi.org/10.3893/jjaam.13.703
Paroz, S., Daele, A., Viret, F., Vadot, S., Bonvin, R., & Bodenmann, P. (2016). Cultural competence and simulated patients. The Clinical Teacher, 13(5), 369-373. https://doi.org/10.1111/tct.12466
Serizawa, A. (2007). Developing a culturally competent health care workforce in Japan: implications for education. Nursing education perspectives, 28(3), 140-144.
Seropian, M. A. (2003). General concepts in full scale simulation: getting started. Anesthesia & Analgesia, 97(6), 1695-1705. https://doi.org/10.1213/01.ane.0000090152.91261.d9
Tatsumi, Y., Sasaki-Otomaru, A., & Kanoya, Y. (2016). The actual situation and issues of emergency medical services for foreigners staying in Japan extracted by systematic review. Nihon Kenko Igakukai Zasshi [Journal of Japan Health Medicine Association], 25(2), 91-97.
Tervalon, M., & Murray-Garcia, J. (1998). Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. Journal of Health Care for the Poor and Underserved, 9(2), 117-125. https://doi.org/10.1353/hpu.2010.0233
*Sayaka Oikawa
Center for Medical Education and Career Development,
Fukushima Medical University,
1 Hikarigaoka, Fukushima, 960-1295, Japan
Email: sayaka9@fmu.ac.jp
Submitted: 11 February 2022
Accepted: 21 July 2022
Published online: 4 April, TAPS 2023, 8(2), 4-13
https://doi.org/10.29060/TAPS.2023-8-2/OA2755
Tri Nur Kristina1, Fatikhu Yatuni Asmara2, Sudaryanto Sudaryanto1, Nuryanto Nuryanto3 & Saekhol Bakri1
1Department of Medicine, Faculty of Medicine, Universitas Diponegoro, Indonesia; 2Department of Nursing, Faculty of Medicine, Universitas Diponegoro, Indonesia; 3Department of Nutrition, Faculty of Medicine, Universitas Diponegoro, Indonesia
Abstract
Introduction: This study aimed to examine the usefulness of Community Based-Education (CBE) and Interprofessional Education (IPE) to community health outcomes.
Methods: The design was a mixed-method study. Each small group worked together to identify family health problems, implement interventions, and evaluate the results. The Readiness for Interprofessional Learning Scale (RIPLS) questionnaire was applied to compare students’ perceptions before and after the implementation. In addition, qualitative data were acquired from students’ comments on the questionnaire, interviews with community representatives, and FGDs with instructors at the end of the program.
Results: Three hundred and sixty-seven out of 465 students returned the completed paired questionnaire (78.9 % response rate). Paired t-test showed that student perception of responsibility slightly increased, whereas teamwork and collaboration, negative and positive professional identity decreased somewhat. However, most pre-post students’ responses already trended to the positive side (scales 4 and 5). Moreover, the Chi-square test showed that pre-post students’ confidence levels significantly increased. Most small groups of students successfully empowered the community to solve health problems. Students, instructors, and representatives of community members appreciated the program. However, several students felt their instructors were not motivated to mentor their tasks, and sometimes they had difficulty conducting home visits together.
Conclusion: This study showed that the combination of CBE-IPE contributes to more favourable community health outcomes. However, it was challenging in several aspects of preparation, including highly motivated instructors. Nevertheless, pre and post-implementation students’ attitudes are still positive.
Keywords: Interprofessional Education (IPE), Community Based Education (CBE), Health Profession Students, Readiness
I. INTRODUCTION
Community-based education (CBE) programs for medical and other health professionals expose students to community health problems, in which they will work in the future as health professionals. However, the CBE program is usually implemented within a single discipline, whereas community health problems must be solved collaboratively among a health care team (Housley et al., 2018).
Interprofessional Education (IPE) has been identified as a valuable method of learning experiences to increase the collaboration and communication of health professionals in healthcare settings. Several studies have reported positive student perceptions of IPE, including improved patient and community outcomes (Dynes et al., 2013). For example, the Leicester Model of IPE demonstrated that students and healthcare professionals gain valuable insights into the balance task of patient-related issues and offer clarity about the effectiveness of collaborative opportunities in addressing patients’ needs (Lennox & Anderson, 2012). Carr (2015) also reported that after the IPE experience, students perceived strong confidence in communication with other professions, increased knowledge of the importance of teamwork and collaboration, learning professional roles, respecting other professional points of view, and improved communication skills.
The goal of undergraduate education for students in the health professions is mainly to produce graduates who can solve community health problems and increase community health, particularly in primary health care. Moreover, community health problems should be solved collaboratively. Thus, Community Based Education (CBE) combined with IPE is needed to be implemented in health professions schools. Several studies have implemented IPE in the community and positively affected students. For example, a study in the Philippines showed the usefulness of the IPE in the community, such as: learning about collaboration, appreciation of roles, holistic care, service to the community, and unique learning experience (Opina-Tan, 2013). A qualitative study in Australia also concluded that students who were voluntarily involved in an IPE program appreciate the opportunity to have direct practice experience in a community context and see this as a valuable way of engaging in interprofessional learning (Stewart et al., 2015). Furthermore, Wagner et al. (2011) stated that IPE in the community improved teamwork.
However, the IPE implementation in community-setting in Indonesia is not yet promising. Lestari et al. (2020) reported that communication and mutual support were problems faced by students. Furthermore, Randita et al. (2019) also stated that collaborative patient-centred competence has a moderate effect when IPE is implemented in the community setting. Therefore, IPE in Indonesia needs further exploration, especially when it is implemented in the community setting with a large number of students who are not volunteers but are obliged to be involved in such programs. In addition, it is anticipated that a learning model combining CBE and IPE will have additional benefits in supporting community health. Thus, the research question of this study was, is the combination of CBE-IPE valuable on community health outcomes, and what are the students’ attitudes and perceptions towards the new program?
II. METHODS
A. The Combination CBE-IPE Model
Before implementation, we matched the curricula of three health professions study programs (Medicine, Nursing, and Nutrition) at the Faculty of Medicine Universitas Diponegoro (a government medical school in Semarang, Indonesia). Based on the acquired competencies and timing possibility, we agreed that the new CBE-IPE program should be implemented for students in the 6th semester. In the 6th semester, all 465 health professions students (212 medical students, 127 nursing students, and 126 nutrition students) participated in this program during one semester.
Before implementation, we discussed with the head of the district health office and the director of the community health centre (CHC) to receive suggestions related to this program, especially in conjunction with the population health situation. As a result, we agreed that students should be assigned to families with pregnant women to support the local government health program in reducing maternal mortality. Thirty-six cadres (voluntary community members) were requested to participate in the project by the director of the CHC and agreed to help them in the program implementation. All cadres had been trained to conduct simple health promotion by the CHC.
A total of 465 health professions students were divided into 126 small groups consisting of 1-2 medical and nursing students and one nutrition student. One small group was attached to one family with a pregnant woman. To have experiences with a continuum of care, small groups of students added one other family if the first family had no children or elderly. Students had to work together to measure the health status of all family members, identify health problems, and propose a solution for identified health problems in discussions with their instructors. Based on those discussions, the students worked collaboratively with the cadres to implement collaborative interventions and eventually evaluated the result of their interventions. During this implementation, groups of students presented their work three times in seminars attended by all instructors and coordinators from three departments. The head of CHC received final reports for follow-up.
B. Study Design and Subjects
The design of this study was a mixed-method study to combine quantitative and qualitative data, in which the qualitative data was used to enrich the quantitative ones. Quantitative data was acquired by asking all students (465 health professions students) to fill out questionnaires before and after implementing the CBE-IPE program. We used the Readiness for Interprofessional Learning Scale (RIPLS) to evaluate students’ perceptions. This questionnaire has been widely used to collect students’ attitudes and perceptions to measure the readiness of healthcare professional students to undertake shared learning activities (Hertweck et al., 2012; Parsell & Bligh, 1999). Negative professional identity items represented negative statements regarding the value of working with other healthcare students. Therefore, this study reversed scored items so that high scores indicated IPE readiness (McFadyen et al., 2006). We used RIPLS in the Indonesian language version, which was developed by Tyastuti et al. (2014). It used exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The EFA accounted for 59.9% of the total variance, while the alpha coefficient of CFA was > 0.7. Furthermore, construct validity was acceptable goodness of fit. Thus, the RIPLS in the Indonesian language version is a valid tool to assess students’ attitudes toward IPE.
The qualitative data were gained by collecting student comments in the questionnaire by asking: “Please write your words regarding this new program.” Moreover, TNK conducted interviews one by one with representatives of community members: two housewives and three cadres. At the end of the program, we conducted a workshop, including two times FGD conducted by TNK, FYA, and SB with 16 instructor’s representatives. Verbatim of all qualitative data was completed by TNK. The result of students’ intervention for patients and families was identified from students’ reports.
C. Data Analyses
We described the student’s characteristics and the result of student intervention on community outcomes. Paired-sample t-tests were used to compare the pre-post students’ responses to RIPLS. In addition, students’ perceptions related to self-confidence before and after the implementation were compared using chi-square. SPSS v22 was used to analyse the quantitative data. The students’ comments and interviews with community member representatives and instructors were analysed using content analysis according to Braun and Clarke (2006). First, keywords were identified as codes, and we used a matrix consisted three columns, namely keywords, categories, and themes. TNK and FYA conducted qualitative data analysis. Different coding was discussed to reach a consensus.
D. Ethical Consideration
We verbally explained this study to all participants before collecting the data. Especially for students, we guaranteed that their perceptions would not affect their scores. Then, we asked for participants’ agreement to join this study by signing the informed consent. The author would confidentially keep their identity.
III. RESULTS
Three hundred and sixty-seven out of 465 students returned the completed paired questionnaire (78.9 % response rate). Table 1 shows the subject’s characteristics of this study.
|
No |
Subject’s characteristics |
Categories |
Quantity |
Percentage |
|
1. |
Students (n= 367) |
|||
|
The study program |
Medicine |
167 |
45.4 |
|
|
Nursing |
100 |
27.3 |
||
|
Nutrition |
100 |
27.3 |
||
|
Gender |
Male |
73 |
20 |
|
|
Female |
294 |
80 |
||
|
2. |
Instructors (n: 16) |
|||
|
The study program |
Medicine |
6 |
38 |
|
|
Nursing |
5 |
31 |
||
|
Nutrition |
5 |
31 |
||
|
Gender |
Male |
4 |
25 |
|
|
Female |
12 |
75 |
||
|
Age |
31-40 |
6 |
37 |
|
|
41-50 |
10 |
63 |
||
|
3 |
Representative of community members |
|||
|
Age |
30-40 |
3 |
60 |
|
|
41-50 |
2 |
40 |
||
|
Gender |
Male |
0 |
0 |
|
|
Female |
5 |
100 |
||
Table 1. Characteristics of study subjects
A. The Result of Students’ Intervention in the Community Outcomes
Various health problems were identified and successfully managed by the students in collaboration with cadres (Table 2 and 3). Students also recognised that most families with low social-economic status and little education did not have health insurance. The head of the CHC agreed to follow up on some parts of the identified health problems, such as visiting pregnant women with high risk to ensure that they will deliver in the hospital, giving intervention for malnutrition toddlers, and vitalizing the post-health for the elderly.
|
No |
Problems identified |
Students’ interventions |
Results
|
|
1 |
One pregnant woman with an abortion |
Students and cadre provided education and accompanied the mother to the hospital. |
a. The mother should be curettage by the doctor in the hospital. b. The mother healthy and agrees to postpone the next pregnancy. |
|
2 |
Only 20% of pregnant women without risk factors who follow gymnastic program in CHC |
Motivation to follow gymnastic for pregnant women |
Moderate-high compliance
|
|
3 |
About 40% of pregnant women have low knowledge about monitoring of pregnancy and low compliance with routine ANC |
Direct education and gave motivation |
Increasing knowledge and compliance for ANC |
|
4 |
25.4% of pregnant women with risk factors according to the standard of WHO and 0.04% with high risk |
Motivation to routinely ANC and monitoring |
High compliance |
|
5 |
42.1% of pregnant women do not have health insurance |
Education to apply government health insurance |
25% have insured key person agrees to follow up |
|
6 |
Social and cultural problem (do not want to eat fish) |
Direct education |
Moderate-high compliance |
|
7 |
83.3% of pregnant women not enough nutrition in their daily diet (2 days recall) |
Gave leaflet and an example of healthy food |
Moderate-high compliance |
|
8 |
20% of pregnant women with anemia)
|
Gave Fe from CHC or midwives. |
Low compliance (reason: not good taste and felt nausea) |
Table 2. Students’ work-related pregnant women in the community
|
No |
Problems identified |
Students’ interventions |
Results
|
|
Baby and Toddlers |
|||
|
1 |
10% with malnutrition |
Education to mother and giving an example of healthy food |
Head of CHC followed up based on student’s report |
|
2 |
Acute Respiratory Infection |
Education and Suggested to CHC |
Cured |
|
3 |
Diarrhoea |
Education and Suggested to CHC |
Cured |
|
4 |
Motoric low development |
Education and Suggested to CHC |
Still to be followed up |
|
5 |
Difficult to eat, low knowledge of mother about healthy food |
Education to mother and give an example of healthy food |
Increasing knowledge |
|
6 |
One child with hydrocephalus |
Motivation to go to the hospital and finding the agency of hydrocephalus |
Has been tackled by the agency of hydrocephalus |
|
Puberty |
|||
|
1 |
Low knowledge about reproductive health |
Direct education |
Increasing knowledge and Head of CHC agree to follow up |
|
2 |
Smoking habit & Narcotic consumption |
Direct education |
|
|
3 |
Anemia among girl |
Direct education |
|
|
Adult |
|||
|
1 |
Low knowledge of occupational accident |
Direct education |
Increasing knowledge |
|
2 |
Low knowledge about family planning |
Direct education |
Increasing knowledge |
|
Elderly |
|||
|
1 |
Hypertension, Knee osteoarthritis, DM type II, Low Back Pain, Stroke, Low quality of life due to osteoarthritis and LBP |
Education and Suggestion to routinely to CHC |
Have been followed up by CHC
|
|
2 |
Only 15% routinely come to the integrative post health for elderly |
Education and Motivation |
Low compliance
|
Table 3. Students’ work with other family members
B. Pre-post Comparison of Students’ Perceptions
Students’ perceptions using RIPLS (5-point Likert scale) from all study programs showed a slight decrease in team collaboration, professional identity, and the cumulative sub-scale. Only student perception of responsibility slightly increased (Table 4). However, most pre-post students’ responses to the RIPLS questionnaire already trended to the positive side (scales 4 and 5). Comparison of pre-post students’ self-assessment of their confidence level significantly increased (Table 5).
|
No |
Subscale |
Pre Mean ± SD |
Post Mean ± SD |
P |
|
1 |
Teamwork & Collaboration |
38.96 ± 3.2 |
36.93 ± 4.0 |
< 0.001* |
|
2 |
Negative professional identity |
6.01 ± 2.4 |
5.29 ± 1.9 |
< 0.001* |
|
3 |
Positive Professional identity |
20.91 ± 1.9 |
20.23 ± 2.5 |
< 0.001* |
|
4 |
Role of responsibility |
5.38 ± 1.3 |
5.56 ± 1.5 |
0.07 |
|
5 |
Total subscale |
70.57 ± 5.0 |
68.74 ± 5.9 |
< 0.001* |
Table 4. Comparison of all students’ perception using RIPLS pre and post implementation (n: 367)
*Significance (p < 0.05) with paired t test
|
No |
Level of Confidence |
Pre |
Post |
Sig |
|
1 |
Not so confident |
69 (18.8%) |
3 (0.8%) |
< 0.00* |
|
2 |
Confident |
272 (74.1%) |
281 (76.6%) |
|
|
3 |
Very confident |
26 (7.1%) |
83 (22.6%) |
Table 5. Level of students’ Confidence (N: 367)
*Significance (p < 0.05) with chi-square test
C. Students’ Comments
Only 141/367 (38%) students wrote their comments in the questionnaire. However, most students (94% of 141 students) appreciated this program and suggested it be continued.
“The program is good; it can help community member to solve their health problem”
F23Nurs
“I agree if the program will be continued”
F50Nurs
Positive aspects raised by the students were:
- Opportunity to have direct communication with the community member (68%),
“I have the opportunity to communicate directly with patients and family, which is difficult to do when I’m only studying in the class”
M13Med
- Understanding each other when exploring and sharing knowledge to solve the identified health problems (32%),
“I feel amazed that each of us has our roles in solving health problems”
F67Med
- Learning about health team collaboration in the actual situation (40%),
“I learn a lot about how to collaborate with other health students in the real situation”
F90Nut
- Feeling proud that they had the opportunity to contribute to managing community health problems (69%).
“This program gives me an opportunity to collaborate with other professions to solve community health problems”
F44Nurs
The student’s complaints were as follows:
- Their task of working with a continuum of care was too heavy and exhausting.
“Focus on one family problem for one small team would be more useful.”
F57Med
- Several students (13%) also felt that their instructors were not motivated to mentor their tasks.
“It is difficult to make an appointment with the instructors, so we don’t have enough time to get feedback from him”
F21Med
- They had difficulty conducting home visits together (73%).
“Our biggest problem is matching the schedule to do a home visit.”
M98Nut
D. Interviews with Representatives of Community Members (two housewives, three cadres)
Both housewives and cadres appreciated the students’ work. They believed the students already had enough competencies to help their health problems. Cadres were still committed to participating in the following program and working with the students to implement, monitor, and evaluate the intervention.
“We are so happy that students help us a lot to identify and to solve our health problems”
F01HW
“Yes, of course, we will help students to communicate with the family as well as report the result of students’ intervention to Community Health Centre”
F03C
Community members thought they were not receiving enough information about the students’ purpose for visiting their house. They suggested that the cadre should have explained to them this program. However, they welcomed the students and told them to make an appointment before the home visit.
“There was no information from cadres of CHC that students will come to our house, but we still welcoming the students because it gives many benefits for us”
FHW02
E. FGD with Instructors at the End of the Program
Most instructors (94,5%) appreciated the value of this program. However, they needed more detailed information about the program, especially assessing students. They also thought it was too hard for students to add one family after already concentrating on one family’s health problem. They agreed that a tiny group should only be attached to one family with a pregnant woman. To strengthen collaboration competencies, all groups of students should implement a “collaborative intervention” that involves all disciplines.
“Sometimes students implemented their intervention within a single discipline that they thought more appropriate to solve the specified health problem.”
F05Inst
The instructors suggested that the assessment include peer assessment to increase students’ attitudes toward valuing each other. It was finally agreed that in the next implementation, various types of assessment would be implemented, namely students’ activities, presentation and discussion, peer assessment, and students’ assessment by the family members.
“Various assessment methods are preferable to capture students’ performance from the different side”
M09Inst
IV. DISCUSSION
This study aimed to examine the impact of implementing the CBE-IPE model on the outcomes of student intervention in the community and students’ attitudes and perceptions towards the new program. Within the CBE-IPE program, the health professions students successfully worked together to empower the community to solve most community health problems. The CBE-IPE program aims to give health profession students direct experiences in working as a health team in dealing with community health problems that might correlate with the social and economic backgrounds of community members. In this study, students identified several health problems in the family with low financial status, low education, and did not have any health insurance. Hence, the health profession students within this program also had an opportunity to learn several principles, including the level of education and economic aspects when implementing their interventions. It is in line with the study by Ngo et al. (2021), who reported that hypertension and cardiovascular risk could be identified by conducting CBE-IPE in homeless adults.
We implemented the CBE-IPE program without any serious obstacles due to the support from the local health government and the director of CHC. Cadres and representatives of community members also commented that the students’ presence and work were beneficial. They stated that they would be involved in the program and work with students to implement, monitor, and evaluate the result. It is important to involve cadres in this program because they will handle the follow-up under the supervision of CHC. Some studies also involved non-health workers in IPE implementation, such as Akter et al. (2016), who involved lay health workers, and Dynes et al. (2013), that involved health extension workers and community health promoters in improving maternal and neonatal health outcomes.
A. Students’ Attitudes and Perceptions Toward the CBE-IPE Program
This study showed that students’ attitudes and perceptions toward this program have improved, especially regarding the role of responsibility and confidence level. In this study, students have tasks to implement health intervention after discussing health problems identified with their instructor, which might increase their commitment and confidence. Tan et al. (2021) also demonstrated the importance of feedback and discussion, in which IPE participants noted that the debriefing process improves their compliance and teamwork.
Students’ perceptions as assessed by the RIPLS in aspects of team collaboration and interprofessional identity were slightly lower, although statistically significant. These statistically significant differences might result from the large sample size of this study. Several studies have shown that one-time IPE implementation is unlikely to change attitudes, whereas multiple or longitudinal IPE experiences elicit attitudinal change with a more positive response (Hammick et al., 2007; Pollard et al., 2006). Hind et al. (2003) reported little to no change in the health professions students’ perception of the RIPLS between pre-and post-implementation. Schreiber et al. (2014) also reported a slight increase and no statistically significant differences in the pre-post response to the RIPLS because the students already had positive attitudes toward IPE. Torsvik et al. (2021) reported that RIPLS tends to have a ceiling effect. Therefore, RIPLS no longer seems suitable for measuring and evaluating the impact of interprofessional learning. In this study, “most pre-post students’ responses to the RIPLS questionnaire already trended to the positive side.” Thus, the RIPLS also possibly has a ceiling effect in this study.
B. Wrapped up CBE-IPE Program Evaluation
Evaluation of this initial program demonstrates that students felt favourable toward the CBE-IPE program and felt more confident when dealing with community health problems. In line with Wong et al. (2018) study, the final students of six health programs have a positive attitude towards working together in an interprofessional health care team.
Nevertheless, students also complained that their tasks in working within a continuum of care were too heavy. As a result, they felt exhausted and less motivated to identify other health problems in another family. This complaint was in line with the instructors’ opinion. It concurred that students could learn from each other when they presented and discussed their work in the seminar. The recommendations included an adjustment in the tasks, scheduling, and improvements in the communication and quality of supervision. Therefore, the students’ tasks must be adjusted to accommodate these suggestions in the following implementation. Sunguya et al. (2014) reported that curriculum is an essential challenge in implementing IPE, which is in line with the study conducted by Thistlethwaite (2012) and Herath et al. (2017), which states that teaching methods and learning activities can be problems faced when implementing IPE. Furthermore, scheduling is one of the problems faced by faculty who implement the IPE program (Ngabonzima et al., 2020)
The instructors mentioned that the students’ interventions were not always “collaborative disciplines” since sometimes only a single discipline intervention for some health problems, and very little content was contributed by the other students in the specified group. Therefore, these circumstances might influence the lower perception of negative professional identity after the program implementation (Hind et al., 2003). Milot et al. (2015) also reported that it could sometimes be challenging to combine heterogeneous student teams during the learning together phase, where every discipline should be represented.
Understanding the attitudes of health professional students and the factors that influence their perceptions, including the situation they face during implementation, may help implement the program in several stages. There are four levels for the students to join the interprofessional collaborative practice. These include level 1: intra-professional education: the foundation of group skills, level 2: introduction to interprofessional education and collaboration: exposure to the healthcare team, level 3: interprofessional collaboration, and level 4: becoming an influential member of the healthcare team (Salfi et al., 2012).
C. Limitations
This study’s limitation lies in the type of data collection that only uses a closed-ended questionnaire and asks the students to write their comments on the program. Although the students raised several positive attributes, this study did not obtain sufficient information about what happened during the implementation and what was behind the students’ rated aspects. Therefore, FGDs with students are still needed to understand program implementation in-depth. Further, direct participation in program implementation might identify obstacles regarding when students should collaborate in their intervention program. Additionally, limitations in this study are acknowledged as data were collected from less than 80% of students participating in the program. Finally, no formal feedback was collected from the community members, although verbal input in the interview was positive. A collection of more detailed data would have provided a deeper understanding of the program’s impact on community perceptions.
We realize that implementing the CBE-IPE program in the community, which involves many students, was challenging and needed more careful preparation. Moreover, the lecturers’ motivation might be increased by encouraging and facilitating them to include field epidemiology research in the same area, with research funding from the faculty. Several changes should be made based on this evaluation, including more detailed guidance for the students and instructors.
V. CONCLUSION
This study revealed that the combination of CBE-IPE for 6th-semester health profession students had been perceived as a valuable learning experience to build community health. Nevertheless, it was challenging for many students in several aspects of the preparation. Moreover, highly motivated lecturers are required, which might be increased by encouraging and facilitating field epidemiology research in the same area. Finally, further research is needed to explore students’ experiences during implementation, primarily how they work as a team and their belief in professional identity. It is also important to identify the result of a combination of CBE-IPE implementation in terms of the satisfaction of students, instructors, and family members.
Notes on Contributors
Tri Nur Kristina conceptualised and designed the research, participated in the analysis and intepretation of data, drafted and revised the manuscript, and giving final approval of the version to be published.
Fatikhu Yatuni Asmara conceptualised of the program implementation, participated in the data collection, and revised the manuscript.
Sudaryanto conceptualised of the program implementation.
Nuryanto conceptualised of the program implementation and participated in the data collection.
Saekhol Bakri conception of the program implementation and participated in the data collection.
Ethical Approval
The Medical and Health Research Ethics Committee (MHREC), Faculty of Medicine Diponegoro University-Dr. Kariadi General Hospital had approved this study (No. 519/EC/FK/2020).
Data Availability
Author could not share the data of this study widely because of its privacy. It also contains qualitative data.
Acknowledgement
The authors would like to thank the Faculty of Medicine Universitas Diponegoro for providing the funding for this study.
Funding
This work supported by Faculty of Medicine Universitas Diponegoro (Grant number: 233-71/UN7.6.1/PP/2020).
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
Akter, T., Sibbritt, D., & Dawson, A. (2016). Workforce interventions to deliver postnatal care to improve neonatal outcomes in low- and lower-middle-income countries: A narrative synthesis. Asia-Pacific Journal of Public Health, 28(8), 659–681. https://doi.org/10.1177/1010539516656435
Braun, V., & Clarke, V. (2006). Qualitative research in psychology using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101.
Carr, S. (2015). Examining health professional students’ attitudes on interprofessional education. (Publication no. 309) [Doctoral Dissertations, University of Rhode Island]. DigitalCommons@URI. http://digitalcommons.uri.edu/oa_diss/309
Dynes, M., Buffington, S. T., Carpenter, M., Handley, A., Kelley, M., Tadesse, L., Beyene, H. T., & Sibley, L. (2013). Strengthening maternal and newborn health in rural Ethiopia: Early results from frontline health worker community maternal and newborn health training. Midwifery, 29(3), 251–259. https://doi.org/10.1016/j.midw.2012.01.006
Hammick, M., Freeth, D., Koppel, I., Reeves, S., & Barr, H. A. (2007). A best evidence systematic review of interprofessional education. BEME guide no.9. Medical Teacher, 29(8), 735-751. https://doi.org/10.1080/01421590701682576
Herath, C., Zhou, Y., Gan, Y., Nakandawire, N., Gong, Y., & Lu, Z. (2017). A comparative study of interprofessional education in global health care: A systematic review. Medicine, 96(38), 1-7. https://doi.org/10.1097/MD.0000000000007336
Hertweck, M., Hawkins, S., Bednarek, M., Goreczny, A., Schreiber, J., & Sterrett, S. (2012). Attitudes towards interprofessional education: Comparing physician assistant and other health care professions students. The Journal of Physician Assistant Education, 23(2), 8-15.
Hind, M., Norman, I., Cooper, S., Gill, E., Hilton, R., Judd, P., & Jones, S. (2003). Interprofessional perceptions of health care students. Journal of Interprofessional Care, 17(1), 21-34. https://doi.org/10.1080/1356182021000044120
Housley, C. L., Neill, K. K., White, L. S., Tedder, A. T., & Castleberry, A. N. (2018). An evaluation of an interprofessional practice-based learning environment using student reflections. Journal of Interprofessional Care, 32(1), 108–110. http://doi.org/10.1080/13561820.2017.1356808
Lennox, A., & Anderson, E. S. (2012). Delivering quality improvements in patient care: the application of the Leicester Model of interprofessional education. Quality in Primary Care, 20(3), 219–226.
Lestari, E., Scherpbier, A., & Stalmeijer, R. (2020). Stimulating students’ interprofessional teamwork skills through community-based education: A mixed methods evaluation. Journal of Multidisciplinary Healthcare, 13, 1143–1155. http://doi.org/10.2147/JMDH.S267732
McFadyen, A. K., Webster, V. S., & Maclaren, W. M. (2006). The test-retest reliability of a revised version of the Readiness for Interprofessional Learning Scale (RIPLS). Journal of Interprofessional Care, 20(6), 633-639. https://doi.org/10.1080/13561820600991181
Milot, E., Dumont, S., Aubin, M., Bourdeau, G., Azizah, G. M., Picard, L., & St‑Germain, D. (2015). Building an interfaculty interprofessional education curriculum: What can we learn from the Université Laval Experience? Education for Health, 28(1), 58-63. https://doi.org/10.4103/1357-6283.161896
Ngabonzima, A., Kenyon, C., Hategeka, C., Utuza, A. J., Banguti, P. R., Luginaah, I., & F Cechetto, D. (2020). Developing and implementing a novel mentorship model (4+1) for maternal, newborn and child health in Rwanda. BMC Health Services Research, 20(1), Article 924. https://doi.org/10.1186/s12913-020-05789-z
Ngo, A. N., Islam, M. A., Aoyagi, J., Sandor, Z., & Sandor, S. (2021). Prevalence of hypertension in homeless adults: An interprofessional education community-based health fairs cross-sectional study in urban long beach, California. High Blood Pressure and Cardiovascular Prevention, 28(1), 63-68. https://doi.org/ doi: 10.1007/s40292-020-00424-8
Opina-Tan, L. A. (2013). A pilot implementation of interprofessional education in a community‑academy partnership in the Philippines. Education for Health, 26(3), 164-171. https://doi.org/10.4103/1357-6283.125992
Parsell, G., & Bligh, J. (1999). The development of a questionnaire to assess the readiness of healthcare students for interprofessional learning (RIPLS). Medical Education, 33(2), 95-100. https://doi.org/10.1046/j.1365-2923.1999.00298.x
Pollard, K. C., Miers, M. E., Gilchrist, M., & Sayers, A. (2006). A comparison of interprofessional perception and working relationship among health and social care students: The results of a 3-year intervention. Health and Social Care in the Community, 14(6), 541-552. https://doi.org/10.1111/j.1365-2524.2006.00642.x
Randita, A. B. T., Widyandana, W., & Claramita, M. (2019). IPE-COM: A pilot study on interprofessional learning design for medical and midwifery students. Journal of Multidiscipline Health Care, 12, 767–775. http://doi.org/10.2147/JMDH.S202522
Salfi, J., Solomon, P., Allen, D., Mohaupt, J., & Patterson, C. (2012). Overcoming all obstacles: A framework for embedding interprofessional education into a large, multisite bachelor of science nursing program. Journal of Nursing Education, 51(2), 106-110. https://doi.org/10.3928/01484834-20111230-05
Schreiber, J., Goreczny, A., Bednarek, M. L., Hawkins, S. R., Hertweck, M. L., & Sterret, S. E. (2014). The effects of single event interprofessional education (IPE) experience on occupational therapy students’ attitude toward IPE. The Internet Journal of Allied Health Sciences and Practice, 12(1), 1-8. https://doi.org/10.46743/1540-580X/2014.1467
Stewart, V., Betts, H., Chee, P., & Ingamells, A. (2015). Interprofessional learning: Health and allied health students in a community context. Advance in Social Work & Welfare Education, 17(2), 70-85.
Sunguya, B. F., Hinthong, W., Jimba, M., & Yasuoka, J. (2014). Interprofessional education for whom? – Challenges and lessons learned from its implementation in developed countries and their application to developing countries: A systematic review. PLoS ONE, 9(5), e96724. https://doi.org/10.1371/journal.pone.0096724
Tan, K. W., Ong, H. K., & Mok, U. S. (2021). Using simulation and inter-professional education to teach infection prevention during resuscitation. The Asia Pacific Scholar, 6(1), 93-108. https://doi.org/10.29060/TAPS.2021-6-1/OA2229
Thistlethwaite, J. (2012). Interprofessional education: a review of context, learning and the research agenda. Medical Education, 46(1), 58–70. https://doi.org/10.1111/j.1365-2923.2011.04143.x
Torsvik, M., Johnsen, H. C., Lillebo, B., Reinaas, L. O., & Vaag, J. R. (2021). Has “the ceiling” rendered the readiness for interprofessional learning scale (RIPLS) outdated? Journal of Multidisciplinary Healthcare, 14, 523–531. https://doi.org/10.2147/JMDH.S296418
Tyastuti, D., Onishi, H., Ekayanti, F., & Kitamura, K. (2014). Psychometric item analysis and validation of the Indonesian version of the Readiness for Interprofessional Learning Scale (RIPLS). Journal of Interprofessional Care, 28(5), 426-432. https://doi.org/10.3109/13561820.2014.907778
Wagner, J., Liston, B., & Miller, J. (2011). Developing interprofessional communication skills. Teaching and Learning in Nursing, 6(3), 97-101. https://doi.org/10.1016/j.teln.2010.12.003
Wong, P. S., Hasan, S. S., Ooi, J., Lim, L. S. H., & Nadarajah, V. D. (2018). Assessment of attitude for interprofessional team working and knowledge of health professions competencies for final year health professional students. The Asia Pacific Scholar, 3(1), 27-37. https://doi.org/10.29060/TAPS.2018-3-1/OA1064
*Fatikhu Yatuni Asmara
Department of Nursing, Faculty Medicine,
Universitas Diponegoro
Jl. Prof Soedarto, SH, Tembalang,
Semarang, Indonesia
+6281229495962
Email: f.y.asmara@fk.undip.ac.id
Submitted: 28 July 2022
Accepted: 12 October 2022
Published online: 3 January, TAPS 2023, 8(1), 25-32
https://doi.org/10.29060/TAPS.2023-8-1/OA2850
Choon Peng Jeremy Wee1, Mingwei Ng1 & Pim W. Teunissen2
1Department of Emergency Medicine, Singapore General Hospital, Singapore; 2School of Health Professions Education (SHE), Faculty of Health Medicine and Life Sciences, Maastricht University, Maastricht, The Netherlands
Abstract
Introduction: This study was performed to understand how fixed clinical teams affected informal learning in Emergency Medicine Residents. Better understanding the effects of team dynamics on informal learning may help to optimise learning and improve performance.
Methods: From 8th February 2020 till 27th September 2020, the Singapore General Hospital Emergency Department adopted a fixed team system. Zoom interviews were carried out amongst Emergency Medicine Residents who worked in the fixed team system using a semi-structured iterative interview guide. A qualitative content analysis was used for this exploratory study. The interviews were transcribed verbatim, anonymised and coding via template analysis performed. Data collection and analysis were performed until data sufficiency.
Results: The themes identified centred around relationship dynamics, team composition and motivation for learning. The first was how improved relationships led to improved trust, communications and camaraderie among team members. This improved peer learning and clinical supervision and provided a more personalised learning experience. A balanced team composition allowed learners to be exposed to experts in various subspecialties. Finally, there was an initial increase in motivation, followed by a decrease with time.
Conclusion: In postgraduate medical education, working in a fixed team system with balanced members had positive effects on informal learning by strengthening relationships and communications.
Keywords: Informal Learning, Workplace Learning, Fixed Teams, Medical Education, Postgraduate
Practice Highlights
- Fixed teams can strengthen relationships between members through better trust, familiarity and communication.
- A balanced fixed team with members having different areas of expertise allows a variety of perspectives.
- Rotation of team members may achieve a balance between the stronger relationship and familiarity of the members of fixed teams and the greater variance in perspectives from a non-fixed team system.
I. INTRODUCTION
Fixed teams (FT) and non-fixed teams (NFT) exist in medicine because of differing service requirements and manpower resources. Examples of FTs can exist in ward round teams and operating surgical teams (Eddy et al., 2016; Stepaniak et al., 2012) where personnel stay within the same work team for long periods. In other areas of healthcare like the Emergency Departments (ED), a NFT system is usually employed where teams are formed according to the personnel rostered to work on that shift and team members change every shift. This allows a more flexible system for the team members as they can request off days and leave according to their personal schedule and yet allows for 24-hour coverage in the ED.
High levels of performance are required of medical teams, both fixed and non-fixed, to achieve good patient outcomes. Therefore, team members should learn how to work effectively together to deliver the best patient care. There are studies, both within healthcare and other industries, which showed mixed results when FT were compared with NFT with regards to team performance. A systematic review on minimal invasive surgical teams found that the FTs had better teamwork and had reduced rates of technical mistakes compared to NFTs (Gjeraa et al., 2016). However, an aviation study showed that FTs made more minor errors compared to NFTs due to FT members being too familiar with each other and overlooking errors (Barker et al., 1996). Although it is unclear how transferable specific research findings from non-healthcare domains are, what is clear is that FTs and NFTs are different in the way teams were formed and the amount of time team members spend working together. There is a lack of understanding if and how these differences affect the way learning takes place in FT and NFTs; which could translate to the performance of the team and its members.
Workplace learning occurs through informal learning by experiencing work challenges and via interpersonal relationships. Informal learning can be supported through learner engagement by encouraging active participation in work activities and aligning learners’ interests with that of the organisation’s objectives towards improving the individuals’ and organisation’s capabilities (Billett, 2007). Informal learning is now widely accepted as a form of workplace learning that occurs out of a formal planned teaching program. It usually occurs during work activities which are not primarily aimed towards education, with learning objectives not planned beforehand (Callanan et al., 2011; Rogoff et al., 2016; Watkins et al., 2018). Although informal learning had been studied, there are very few studies looking at how being in FTs affects informal learning. A review on the involvement of employees in workplace learning (Kyndt & Baert, 2013) revealed that there was a paucity of literature on whether any team system improves the involvement of employees in informal learning. Thus, it remains to be studied what effects working in a FT system has on informal learning especially of the more junior team members.
An integrative literature review on informal learning found that some of the important components of informal learning within members of a team and between teams included interpersonal relationships, feedback, networking and leadership (Jeong et al., 2018). Therefore, there may be differences in interpersonal relationships and feedback between the different team systems. It is known that good interpersonal relationships include good supervisor and peer support and both affect whether what is learnt is applied at the workplace (Burke & Hutchins, 2016), there was little published data on whether supervisor and peer support or even the supervisory relationship were affected by the amount of time spent together. Within some healthcare systems both FTs and NFTs consists of members with varying levels of experience, differing expertise and roles. In a FT, the learners are only supervised by supervisors within that team; therefore, each learner’s supervised time is divided within a small group of supervisors as compared to a NFT system where each learner’s supervised time is spread amongst a larger number of supervisors. Thus, despite this increased time spent together in a FT, it is not clear if working in a FT impacts supervisory or interpersonal relationship.
Having a good trusted learner-supervisor relationship can result in the establishment of an “Educational Alliance” (Telio et al., 2015). This is because feedback from a credible trusted source was more readily accepted and feedback is another important component of effective informal learning within a team (Jeong et al., 2018).
Furthermore, a study among social work students and their supervisors in a rotational placement model, found that the longer the amount of time they spent with each other the greater the trust between them (Vassos et al., 2017). On the other hand, being in a FT could restrict networking and socialisation to a smaller group of people as contact with other teams’ members could be reduced however it is not known how this could affect informal learning.
Understanding how informal learning takes place within FT and NFT may allow optimisation of learning within each and perhaps even configure teams to enhance learning and thus ultimately improve performance. Our study aimed to fill this gap in the literature by exploring how fixed clinical teams affected the experience of informal learning for Emergency Medicine (EM) Residents. By doing so we hope to understand how informal learning can be supported via the appropriate implementation of team systems especially where high performance is expected from the teams.
II. METHODS
To study how being in fixed clinical teams affected the experience of informal learning for EM Residents we conducted an exploratory qualitative study based on a constructivism research paradigm using content analysis of individual interviews. This is because informal learning could not be quantified with specific learning outcomes.
A. Setting
EDs teams manage a large number of critically ill patients who may need time sensitive interventions. These teams would comprise of experienced Emergency Physicians (EPs) and more junior Medical Officers (MOs) and Residents. The Residents are postgraduate doctors who are training to graduate as EPs; therefore, informal workplace learning is a crucial part of their training. Hence the residents would be good study subjects to investigate the effect of team systems on informal learning.
The Singapore General Hospital (SGH) ED functioned via NFTs where the composition and number of members in the team differed with each 8 hour shifts accordingly to the anticipated patient load. The COVID-19 pandemic provided a naturalistic setting where the effect of a FT system can be compared to a NFT system which had existed before hand. After COVID-19 was declared a pandemic by the World Health Organisation (WHO) on the 11th March 2020 (World Health Organisation, 2020). There was an emphasis on infection control to contain the pandemic. Many countries had instituted social distancing measures which included curfew-like measures and travel restrictions (Lake, 2020). Similarly, the Singapore government had instituted legislative measures to limit face-to-face interactions. In the ED of SGH, measures were put in place to limit the spread of COVID-19.
Thus, from 8th February till 27th September 2020, as part of infection control measures, doctors were organised into 5 FTs, each having between 5-7 Consultants, 3-5 EM Senior Residents, 2-3 EM Junior Residents and 7-9 non-EM Medical Officers (MO) (Liu et al., 2020; Quah et al., 2020). The Senior Emergency Physicians (SEPs) consisted of certified specialists in EM (Associate Consultants, Consultants and Senior Consultants); they played supervisory and educational roles to the junior doctors (JD) which included MOs, Junior Residents and Senior Residents. Each FT worked 12-hour shifts. Interactions between teams were kept to a minimum and members from different teams were not allowed to mingle. Thus, the residents were only supervised by their team’s SEPs. Informal learning would now occur within these FTs.
Formal learning was converted to a remote online platform because of infection control measures. Lectures and tutorials were held and recorded using software which enabled online asynchronous access e.g. Zoom (Zoom, 2016) as not all residents could be given protected learning time together. Sessions which could not be transferred onto an online platform (e.g. hands on simulation and procedure skills training) were cancelled. Formal summative examinations were also cancelled.
B. Interviews
Interviews were conducted and recorded via Zoom (Zoom, 2016) to maintain social distancing. The primary investigator performed 11 interviews and a coinvestigator performed the remaining 4 out of a total of 15 interviews. A semi-structured iterative interview guide was developed based on Eraut’s typology on informal learning which included team activities, tasks and enabling/disabling factors (Eraut, 2010) was used, and the interviews were audio-recorded and transcribed verbatim and anonymised. The interviews allowed positive and negative aspects to be explored and being semi structured the questions asked varied according to the interviewees’ responses. This helped to focus the interviewees to what informal learning was with examples when it could occur within team activities. The guide was iteratively amended with each interview to enhance clarity which helped to obtain more in-depth data in later interviews.
C. Participants
Twenty-four ED residents were working in the FT system in the ED of SGH during COVID-19. Fifteen were Junior Residents and 9 were Senior Residents. Purposive sampling was carried out with at least two Residents from each team being sampled. This is to ensure that there was good representation for all of the fixed clinical teams. All 24 residents were invited to participate via email and WhatsApp messaging platform with written consent being obtained. Fifteen individual interviews were conducted before data sufficiency was achieved where no new data would change the outcome of the study, thus no further interviews were conducted beyond data sufficiency (Varpio et al., 2017). Eleven interviewees were Junior Residents (4 females and 7 males) and 4 were Senior Residents (3 females and 1 male).
D. Data Analysis
Data analysis was performed via template analysis by the primary and coinvestigator independently (Brooks et al., 2015). Eraut’s typology developed from his research on informal learning was used as a priori themes in the initial coding template (Eraut, 2010). Coding template modifications were made as the analysis of the transcripts continued. Themes were categorised into hierarchical clusters and relationships between them were studied and defined. After final modifications, the coding template was applied to the entire data set. Coding themes were compared and discussed between the primary investigator and the coinvestigator until consensus was reached.
E. Ethics
Waiver for approval was granted by the Singhealth Institutional Ethics Board. The primary investigator was a core faculty within the Singhealth Emergency Medicine Residency Program and although the interview was conducted among EM residents the primary investigator did not conduct the interviews when the interviewees were from the same team as the primary investigator. These were conducted by the coinvestigator. The coinvestigator was an EM Senior Resident who was not involved in the FT system. A reflexivity diary was kept, and peer debrief was done.
III. RESULTS
Three main themes emerged on how working in FTs affected informal learning amongst our participants (Figure 1). These included changes in relationship dynamics between members, effect of FT composition on informal learning of the participants and influence on motivation.
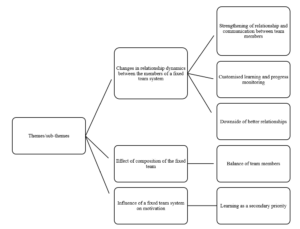
Figure 1. Themes and sub-themes
Theme 1: Changes in Relationship Dynamics between FT Members
From the interviews, the participants felt that the FT system resulted in more familiarity, trust, teamwork and improved communications between team members including SEPs, Residents and MOs. Interviewees felt that this strengthened the relationship dynamics between FT members as compared to a NFT. This meant that FT members were able to coordinate and exchange information better. It led to an increase in familiarity in knowing each member’s style of practice and way of thinking. The team members could understand each other better and how they reasoned.
The strengthened relationship between residents and SEPs changed with dynamics. Having a “closer rapport” and “deeper bond” allowed the residents to “tag along” with SEPs “more often” and gave the residents more insight as to why the SEPs behaved in a certain way as to “how they had practiced medicine” and the rationale behind each step was “more easily communicated to the residents who were tagging along” (Resident A), resulting in residents having a deeper understanding of why things were done in addition to how things were done. This strengthened relationship was also present between the residents and their peers. Therefore, peer learning improved within the FTs as junior residents reported feeling less reservation in asking each other questions.
Resident D felt that peer learning was better within FTs because of the improved relationship, there were less reservations which had prevented him from asking his peers questions in a NFT setting.
He elaborated:
“Fixed team [was] definitely better for peer learning. For the same reasons, because you know each other better, you’re more familiar. We don’t only talk to each other about work… after a while, when you go for meals together… or rather like resting together and no cases around you sit and talk. So there’s a lot more familiarity with the person you’re working with, and… you’re just more comfortable with asking questions… you don’t feel like this is somebody who’s going to judge you if [you] asked a stupid question”
This was not just amongst the residents but also with SEPs. Resident G felt that it was easier for the residents to speak to the SEPs because of familiarity and resulted in less workplace stress:
“Over the time as we knew each other better … the workplace stress was much lower… so I could… work with less stress at workplace… Because if you didn’t really know the consultant you tend to be afraid to talk to them; then of course your stress levels will be higher. But if you know that consultant and you know what kind of person, he or she is then you could be more comfortable to talk to them…”
“…It is more comfortable to… approach the senior because you know every day… we have a fixed team so naturally we feel that our relationship is closer…”
“… so, I won’t be too afraid to speak out or to talk to them to discuss with them.”
Contributing to additional ways of informal learning, communication within FTs even during work took on a more “friendly [and] social” form with greater congeniality and via more “communication platforms” (WhatsApp and Tiger Text) which continued even “outside of work” (Resident H). These platforms were also used as learning tools to facilitate case discussions, share learning points and experiences. This was not previously present in the NFTs. The residents felt that learning was more customised because of the change in relationship dynamics. In FTs, there was closer supervision of residents by SEPs. The residents “spent more time” with the same group of supervisors, thus the supervisors were able to better “assess both strengths, weaknesses and address any particular loopholes” of the residents (Resident A).
However, there were some adverse effects of this change in relationship dynamics. Some residents felt that with a closer relationship between team members, supervisors sometimes were more tolerant of the learners’ shortcomings and be less likely to point it out because of not wanting to affect the relationship. This closer relationship could result in residents taking “shortcuts” and “flying under the radar” because they knew the SEPs could tolerate or would not scrutinise the learners closely once “trust” was established (Resident L). Resident H gave an example of how familiarity could lead to less critical thinking by the learner:
“If… the senior always does like… [Rapid Sequence Intubation] … even though I question the first time I saw him do that… subsequently … every time I work with him I will do [it] this way. I won’t really think does the patient really need this way [of management] or will the patient benefit in a different way… if you are working with different bosses then every case you need to restart your thinking…”
Theme 2: Effect of Composition of the FT
All interviewees felt that the composition of the FT had affected informal learning, and that having a balanced team in terms of a wide range of years of practice amongst both the SEPs as well as the JDs would help improve informal learning. Having a team where the JDs were of differing seniorities of practice could help with peer learning because the senior ones could help the junior ones more. This also applied to the SEPs as that provided a wider perspective to clinical issues due to having different clinical experience and expertise in different subspecialties. Furthermore, if the JDs in a FT were of a similar level of practice, Resident C expressed that they could be “competing with each other for cases and procedures” which adversely affected informal learning with fewer opportunities to perform procedures. In a NFT the members would be constantly changing and it would be unlikely its JD would be always of the same level of practice.
The interviewees expressed concern that within a FT system that, although residents had close contact with a fixed group of supervisors, they lacked contact with the other teams’ SEPs. Many residents felt that this had adversely impacted informal learning because the SEPs were experts in different subspecialties (e.g., Trauma, Toxicology, Ultrasound, etc). By not interacting with many SEPs, residents were unable to learn from them. Furthermore, different supervisors had different perspectives and approaches to patients which the residents may not be exposed to if they were not in the same team as these seniors. However, this was mitigated by having a team with a balanced variation in the areas of specialty of the seniors. Resident F summarised this:
“…a team with… people from different seniorities are essential… (even) juniors can teach seniors… the way that my team was composed… it was a good mix… there are people from different… specialties… from different seniorities even within the juniors … like first posting to… [senior post graduate years]… offers different perspectives, learning of different things… people from different [subspecialties] can offer insight into the systems-based learning or component from other parts of the institution…”
Theme 3: Influence of a FT System on Motivation
Many residents felt that having FTs increased their motivation to learn. This resulted from their supervisors being able to inspire them and follow up with their learning progress more closely. Resident M was motivated to learn because his “friends (FT members) were very motivating” and “enthusiastic”; this encouraged him to learn more. Furthermore, resident C felt more motivated to learn in a FT because he “always sees the same senior” and this more frequent contact results in him being “more likely to take their feedback and opinion more seriously and work harder”
However, “after some time everyone is comfortable with each other” and some participants feared that their motivation “might go down” (Resident N). This was because there was a feeling of complacency as time went on within a FT, hence the motivation to learn started to dwindle after an initial increase.
Other reasons for this decline were related to COVID-19, the focus was more on facing the threat rather than learning and the priority to learn was secondary. The motivation to learn “was a bit less” as “the mood was more to survive than to learn”; Resident L was “less driven to learn” because there was a “general bleakness in the whole situation of [COVID-19] which made his “inner desire to learn… wane a bit”
IV. DISCUSSION
This study explored how working in fixed clinical teams affected informal learning for EM Residents. There are many pros and cons to fixed team rostering however the focus of this study is on informal learning. The findings highlighted the importance of having a balanced team composition where team members were able to establish trust and a strong bidirectional relationship because of the longer time spent working together. Motivation to learn increased initially; however after some time, some felt a decrease. This was consistent with prior work which highlighted team dynamics and commitment and that feedback which was given often and in a socially interactive environment were factors which helped to enable effective work-based learning (Attenborough et al., 2019; Jeong et al., 2018; Kyndt et al., 2016). Unlike in Attenborough’s work where team leadership was one of the factors identified; our respondents did not mention the effect of team leadership on informal learning. Their focus was more on the relationships between the different team members. From this study the predominant factors which positively affected informal learning included teamwork, collaborative task performance, where good communication was needed between different people, and personal development especially in building interpersonal relationships and group decision making.
Limited studies were done on how FTs affect informal learning. Our study found that FTs resulted in more (informal) communication channels (e.g. WhatsApp) being formed which was not present in NFTs, resulting in more learning activities including sharing ideas, resources and experiences. These sharing activities were some of the major forms of informal learning activities identified in the literature (Lohman, 2006). FTs resulted in open communication and quality feedback which was well received, and were found to be beneficial towards informal learning (Jeong et al., 2018). Our study showed that working in a FTs led to more customised learning. Findings of improved communications and strengthened relationships in a bidirectional manner involving teacher and learner alike, supports a shift from a predominantly teacher to learner type of dynamics to a team learning dynamics where all team members can learn with and from one another. This is important because informal learning takes place effectively when learning from past mistakes and feedback exchange occurs, involving both cognitive and social interactions (Jeong et al., 2018).
FTs had negative effects on informal learning as well. Familiarity resulted in supervisors being more tolerant of shortcomings and FTs limited learners’ contact with other teams’ supervisors and adversely affected informal learning. This was because informal learning also takes place when there is sharing of ideas, expertise and experience (Lohman, 2006) and limiting the number of supervisors limits the variance of shared viewpoints.
Our study has limitations. Firstly, interviewee recall bias was possible because 6 months had passed after the FT system was stopped before the interviews. Therefore, some details may not have been accurately recalled given this period which could affect the trustworthiness of results. Secondly, the participants were likely to be comparing their experiences in the FT system during COVID-19 to a NFT system without a pandemic. Thus, some of the experienced changes may be because of the pandemic rather than purely due to the FT system. Thirdly, there are many pros and cons to FTs however the focus of this study is on informal learning thus other factors not investigated with this study may affect the feasibility of FT. Lastly there could be power differential effects between the interviewers and the interviewees because the interviewers performed supervisory and roles to the residents. However, to mitigate this, a reflexivity diary was kept, and peer debrief between the two interviewers was performed. Furthermore, the interviewers did not interview members who had been in the same team as them.
V. CONCLUSION
In conclusion, FTs impact informal learning by building strong relationships with improved team communications and adding a social dimension for learning. A balance of team members as well as rotating the residents across different FTs may be beneficial for improving informal learning for EM Residents.
Notes on Contributors
Dr Wee Choon Peng Jeremy submitted the CIRB application, (with the help of the last author) conceptualised the study and its design. He performed the literature review, recruited and interviewed the participants, collected and transcribed the data, performed the thematic analysis of the data and wrote the manuscript.
Dr Ng Mingwei helped to recruit and interview some of the participants, transcribed and collected the data. Dr Ng helped perform the thematic analysis of the data and helped edit the manuscript.
Prof. Dr. Pim Teunissen was central to the conceptualisation of the study, advised on the design of the study and gave critical feedback to the writing of the manuscript and edited the manuscript extensively
All the authors have read and approved the final manuscript.
Ethical Approval
We have included the letter for waiver of CIRB via email. Ethics approval for waiver of written informed consent was obtained from the Singhealth Institutional Review Board (CIRB Ref: 2020/3114).
Data Availability
As the data set is qualitative in nature, we are not able to upload that in any public repository.
Funding
There is no funding for this paper/study.
Declaration of Interest
The authors report there are no competing interests to declare.
References
Attenborough, J., Abbott, S., Brook, J., & Knight, R. A. (2019). Everywhere and nowhere: Work-based learning in healthcare education. Nurse Education in Practice, 36, 132-138. https://doi.org/10.1016/j.nepr.2019.03.004
Barker, J. M., Clothier, C. C., Woody, J. R., McKinney, E. H., Jr., & Brown, J. L. (1996). Crew resource management: A simulator study comparing fixed versus formed aircrews. Aviation, Space, and Environmental Medicine, 67(1), 3-7.
Billett, S. (2007). Constituting the workplace curriculum. Journal of Curriculum Studies, 38(1), 31-48. https://doi.org/10.1080/00220270500153781
Brooks, J., McCluskey, S., Turley, E., & King, N. (2015). The utility of template analysis in qualitative psychology research. Qualitative Research in Psychology, 12(2), 202-222. https://doi.org/10.1080/14780887.2014.955224
Burke, L. A., & Hutchins, H. M. (2016). Training transfer: An integrative literature review. Human Resource Development Review, 6(3), 263-296. https://doi.org/10.1177/1534484307303035
Callanan, M., Cervantes, C., & Loomis, M. (2011). Informal learning. Wiley Interdisciplinary Reviews Cognitive Science, 2(6), 646-655. https://doi.org/10.1002/wcs.143
Eddy, K., Jordan, Z., & Stephenson, M. (2016). Health professionals’ experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. JBI Database of Systematic Reviews Implementation Reports, 14(4), 96-137. https://doi.org/10.11124/JBISRIR-2016-1843
Eraut, M. (2010). Informal learning in the workplace. Studies in continuing education, 26(2), 247-273. https://doi.org/10.1080/158037042000225245
Gjeraa, K., Spanager, L., Konge, L., Petersen, R. H., & Ostergaard, D. (2016). Non-technical skills in minimally invasive surgery teams: A systematic review, Surgical Endoscopy, 30(12), 5185-5199. https://doi.org/10.1007/s00464-016-4890-1
Jeong, S., Han, S. J., Lee, J., Sunalai, S., & Yoon, S. W. (2018). Integrative literature review on informal learning: Antecedents, conceptualizations, and future directions. Human Resource Development Review, 17(2), 128-152. https://doi.org/10.1177/1534484318772242
Kyndt, E., & Baert, H. (2013). Antecedents of employees’ involvement in work-related learning. Review of Educational Research, 83(2), 273-313. https://doi.org/10.3102/0034654313478021
Kyndt, E., Vermeire, E., & Cabus, S. (2016). Informal workplace learning among nurses. Journal of Workplace Learning, 28(7), 435-450. https://doi.org/10.1108/JWL-06-2015-0052
Lake, M. A. (2020). What we know so far: COVID-19 current clinical knowledge and research. Clinical Medicine, 20(2), 124-127. https://doi.org/10.7861/clinmed.2019-coron
Liu, Z., Teo, T. L., Lim, M. J., Nadarajan, G. D., Segaram, S. S. C., Thangarajoo, S., Wee, L. E., Wee, J. C. P., & Tan, K. B. K. (2020). Dynamic emergency department response to the evolving COVID-19 pandemic: The experience of a tertiary hospital in Singapore. Journal of the American College of Emergency Physicians Open, 1(6),1395-1403. https://doi.org/10.1002/emp2.12264
Lohman, M. C. (2006). Factors influencing teachers’ engagement in informal learning activities. Journal of Workplace Learning, 18(3), 141-156. https://doi.org/10.1108/13665620610654577
Quah, L. J. J., Tan, B. K. K., Fua, T. P., Wee, C. P. J., Lim, C. S., Nadarajan, G., Zakaria, N. D., Chan, S. J., Wan, P. W., Teo, L. T., Chua, Y. Y., Wong, E., & Venkataraman, A. (2020). Reorganising the emergency department to manage the COVID-19 outbreak. International Journal of Emergency Medicine, 13(1), Article 32. https://doi.org/10.1186/s12245-020-00294-w
Rogoff, B., Callanan, M., Gutiérrez, K. D., & Erickson, F. (2016). The organization of informal learning. Review of Research in Education, 40(1), 356-401. https://doi.org/10.3102/0091732×16680994
Stepaniak, P. S., Heij, C., Buise, M. P., Mannaerts, G. H., Smulders, J. F., & Nienhuijs, S. W. (2012). Bariatric surgery with operating room teams that stayed fixed during the day: A multicenter study analyzing the effects on patient outcomes, teamwork and safety climate, and procedure duration. Anesthesia and Analgesia, 115(6), 1384-1392. https://doi.org/10.1213/ANE.0b013e31826c7fa6
Telio, S., Ajjawi, R., & Regehr, G. (2015). The “Educational Alliance” as a framework for reconceptualizing feedback in medical education. Academic Medicine, 90(5), 609-614. https://doi.org/10.1097/ACM.0000000000000560
Varpio, L., Ajjawi, R., Monrouxe, L. V., O’Brien, B. C., & Rees, C. E. (2017). Shedding the cobra effect: Problematising thematic emergence, triangulation, saturation and member checking. Medical Education, 51(1), 40-50. https://doi.org/10.1111/medu.13124
Vassos, S., Harms, L., & Rose, D. (2017). Supervision and social work students: Relationships in a team-based rotation placement model. Social Work Education, 37(3), 328-341. https://doi.org/10.1080/02615479.2017.1406466
Watkins, K. E., Marsick, V. J., Wofford, M. G., & Ellinger, A. D. (2018). The evolving Marsick and Watkins (1990) theory of informal and incidental learning. New Directions for Adult and Continuing Education, 2018(159), 21-36. https://doi.org/10.1002/ace.20285
World Health Organisation. (2020). World Health Organisation emergencies press conference on coronavirus disease outbreak – 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
Zoom. (2016). Security guide. Zoom Video Communications Inc.
*Wee Choon Peng Jeremy
Outram Road,
Singapore 169608
Email: jeremy.wee.c.p@singhealth.com.sg
Submitted: 26 November 2021
Accepted: 21 July 2022
Published online: 3 January, TAPS 2023, 8(1), 33-42
https://doi.org/10.29060/TAPS.2023-8-1/OA2712
Jaime Maria Tan1, Junaidah Binte Badron1 & Sashikumar Ganapathy1,2
1Department of Emergency Medicine, KK Women’s & Children’s Hospital, Singapore; 2Duke-NUS Medical School, Singapore
Abstract
Introduction: Perceptions towards the working and learning environment as well as coping mechanisms have been studied across different healthcare sectors. They have shown to reduce stress and burnout. However, perceptions of the work environment in the Emergency Department (ED) setting have not been studied in depth. The literature surrounding coping mechanisms also mostly focuses on their impacts rather than the mechanisms utilised. In addition, these were often investigated using surveys. This study aimed to use a phenomenological approach to explore the perceptions and coping strategies of junior doctors working in a paediatric ED.
Methods: Sixteen junior doctors working in the Paediatric ED were recruited. Semi-structured interviews were conducted after conducting literature reviews. Data was collected until saturation point. All interviews were recorded and transcribed verbatim manually and subsequently analysed.
Results: The greatest fears of junior doctors starting their paediatric emergency posting were lack of knowledge due to inexperience in the subspecialty; fear of the work environment due to unfamiliarity as well as workload and the intrinsic high-stress environment. The main coping strategies were ensuring clinical safety, obtaining psychosocial support from loved ones and colleagues, and placing focus on spirituality and wellbeing.
Conclusion: In this study, the perceptions and coping strategies of the junior doctors in the Paediatric ED were explored. The findings from this study will help to structure and improve the support given to future junior doctors who rotate to the department as well as better orientate them to allay their pre-conceived notions.
Keywords: Coping Behaviours, Perceptions, Paediatric Emergency Department, Stressors, Interviews
Practice Highlights
- Participants worried about knowledge, workload and responsibilities prior to starting their posting.
- Perceptions were mostly of an anticipatory nature, influenced by seniors’ past experiences.
- In work, support from senior staff was helpful in allaying their fears and increasing patient safety.
- Participants felt psychosocial support, spirituality and wellness were useful coping strategies.
- Maladpative coping strategies did not come up as a main theme in our study.
I. INTRODUCTION
Perceptions toward the work and learning environment can strongly impact experiences and even lead to large amounts of stress (Chan et al., 2016). A poorer perception of the learning environment is also associated with greater levels of burnout (Chew et al., 2019; Sum et al., 2019). Conversely, a positive perception of the work environment helps to alleviate stress (Abraham et al., 2018). Workers’ perception of their work environment contributes significantly to their overall experiences.
Main factors contributing to stress in the ED include heavy workload and critically ill patients. Workplace violence, trauma, abuse and morbidity also add to the stress and burnout experienced (Burbeck et al., 2002; Copeland & Henry, 2018; Healy & Tyrrell, 2011; Xu et al., 2019). In the paediatric setting, added stressors include dealing with sexual abuse and non-accidental injury as well as death and the inability to provide optimal care for children (Alomari et al., 2021; Basu et al., 2016; Durand et al., 2019; Greenslade et al., 2019; Shanafelt et al., 2012; Watson et al., 2019).
Given these significant stressors, individuals utilise different coping mechanisms to mediate these experiences (Howlett et al., 2015).
Some coping strategies discussed in previous studies include socialising with friends and family (Gribben et al., 2019). Focusing on physical wellbeing, clinical variety, reflectivity, and organizational activities were also helpful in alleviating burnout in other areas of healthcare (Barham et al., 2019; Koh et al., 2015).
Several studies also found that the use of maladaptive coping mechanisms, such as alcohol use and self-blame increased with the frequency of burnout (Jackson et al., 2016; Oreskovich et al., 2015; Ryali et al., 2018; Talih et al., 2018).
While many studies studied stressors and the effectiveness of the coping mechanisms used, the actual components of coping mechanisms were not well studied. In studies that did look at coping mechanisms and their effectiveness, these studies were also often done via the survey method and were only evaluated on the surface.
Most studies looked at healthcare workers in general. Few studies looked solely at the doctor population. This makes conclusively evaluating the doctor component of coping mechanisms and their effects difficult.
While other studies looked at an adult emergency perspective, there were also few studies looking at the paediatric ED. It has been reported that dealing with paediatric emergencies causes more stress compared to their adult equivalents. Some of the contributing factors are related to the nature of working with children. These, in itself, are unmodifiable (Guise et al., 2017). Therefore, it is important to study how the paediatric context can affect the experiences of the doctors who care for them.
In our study, we studied the perceptions of junior doctors at the beginning of their posting. We subsequently explored their coping mechanisms in the Singaporean context.
The element of stress in the ED among junior doctors is significant as the ED is often part of many specialist training pathways (Mason et al., 2015). During the time of training, the doctors are still learning and developing. Hence, many doctors experience sharp learning curves during their postings. This brings about more stress (McPherson et al., 2003). In some cases, the stress can even lead to doctors thinking about leaving clinical practice altogether (Degen et al., 2014).
In the Singaporean context, paediatric emergency postings are part and parcel of speciality training for junior doctors (especially for those in emergency medicine and family medicine training). Because of this, junior doctors spend the majority of their paediatric postings in the paediatric emergency. As such, a Singapore-specific context would give light on the challenges of this sizable group.
The nature of the healthcare system in Singapore is unique. Up to 60% of the consultations in the paediatric ED were for nonurgent conditions due to the overall perception of the severity of symptoms and parental preference towards paediatric specialist facilities (Ganapathy et al., 2015). This would lead to an increased workload for the paediatric ED. The distribution in workload may also differ compared to a global perspective, with the load of severe paediatric trauma in Singapore being low (Pek et al., 2019).
These subtleties in the paediatric ED in Singapore can influence the experiences of junior doctors differently. With these key differences in mind, we aimed to investigate the perceptions of junior doctors towards their paediatric ED posting in Singapore and how they subsequently coped with the challenges faced.
II. METHODS
A. Design
In this study, we examined the experiences of doctors in their paediatric ED rotation and how their thoughts and actions influenced their stress during their rotation. We deemed the phenomenological approach to be the most appropriate for this study. Phenomenology is defined as the study of how individuals see and experience a phenomenon and what this means to the individuals in their own experience (Neubauer et al., 2019; Smith, 2021).
The approach we chose was that of an interpretive phenomenological analysis in which we aimed to investigate the experience through the participants’ own experiences and perceptions. With the help of the various participants’ accounts, themes and ideas bound by their experiences were explored (Tuffour, 2017).
B. Methods
The members of the study performed a preliminary literature review on the topic and explored plausible methods of data collection. The study team decided on semi-structured interviews as it promotes sharing and would allow for sufficient privacy.
The team members included a senior consultant, a staff physician and a medical officer. Together, after discussions about concepts that the team was keen to explore, an interview guide was drawn up.
Subsequently, a proposal was submitted to the Hospital Centralised Institutional Review Board for approval.
One-on-one interviews were conducted with the participants by investigator A, a medical officer who was rotating within the department at the time of the study. This was done to reduce the power differential. Interviews were conducted at a location and time convenient to the participant.
Prior to the interviews, consent was sought and all interviews were recorded and subsequently transcribed verbatim. The interviews were conducted over a 1-month period in December 2019.
Questions were open-ended and allowed participants to share ideas that they were keen to raise with no restrictions to the topics brought up. Interview questions were tweaked alongside subsequent interviews so that they were easier to understand and would encourage sharing. Additional questioning in subsequent interviews was adopted to improve clarity. For example, one of the questions that featured early in the interviews was ‘What are some of the coping mechanisms you use?’ During subsequent interviews we noticed some participants utilised coping mechanisms before work to prepare themselves, some used other strategies during work to cope with the stress, while others dealt with their stressors after getting off work. We tweaked the question to include ‘during the shift or outside of the shift’ to help participants widen their perspective about certain coping methods they may have used but were not immediately conscious of when answering the questions. No new questions referring to particular themes were inserted although interviewers were aware of the themes that had been highlighted in previous interviews. This was done in addition to the initial interview guide and ensured the broad nature of questioning was not compromised and the breadth of interviews was maintained.
Themes were identified from the interviews until data saturation was reached. Data saturation was noted at the 12th interview. The team continued to learn from subsequent interviews, with interviews contributing additional depth to the issues explored. Further interviews were conducted to confirm that no new theme was being identified.
The interviews were then transcribed and de-identified. They were subsequently reviewed by 2 reviewers (Investigator A and Investigator B). Data was analysed using a step-by-step thematic analysis method (Braun & Clarke, 2006). Investigators A and B independently analysed the transcripts, identified themes and later reported the common themes. These themes were discussed for concurrence. When any differences in opinion arose, these would be reviewed by investigator C to resolve any disagreement.
C. Setting
The research was conducted within the Paediatric ED in KK Women’s and Children’s Hospital, a tertiary paediatric hospital.
The Children’s Emergency of KK Women’s and Children’s Hospital is the largest paediatric emergency unit in Singapore. During the time of the interviews, the department treated over 400 patients daily. The Children’s Emergency sees all children under the age of 18 years for all medical complaints.
The department is staffed by over 60 junior doctors at a single time. These junior doctors come from various backgrounds and pass through the department for varying amounts of time. Thus, their experience can be very heterogeneous.
The job scope and responsibilities of all the junior doctors are primarily the same despite the different levels of experience. They are expected to treat the patients that present to the ED. These doctors can seek advice from the senior doctors who are on the ground. However, for the majority of the time, they would be tasked to treat patients on their own.
D. Participants
Participants were recruited through an email that was circulated to all junior doctors in the department. Participation in the study was voluntary and participants were not remunerated.
A total of 16 junior doctors were recruited and interviewed over a 1-month period. Due to the busyness of the ED and the limited time frame in which the interviews were conducted, only 16 interviews were conducted. Convenience sampling was chosen for the sampling method. The first 16 volunteers who had volunteered were interviewed. However, it was noted that saturation point was reached prior to the conclusion of the interview process.
The variety within the ED was well represented. The details of participant breakdown are elaborated on in Table 1.
|
Experience & Training Information |
|
|
|
|
|
Mean post-graduate year, 3.6 (2-6)* |
|
|
|
|
|
|
Emergency Medicine |
Family Medicine |
Paediatric Medicine |
Not in a training program at time of study |
|
Training Program (n=16) |
5 |
2 |
1 |
8 |
|
Epidemiological Data |
|
|
|
|
|
|
Chinese |
|
Indian |
|
|
Race (n=16) |
13 |
|
3 |
|
|
|
Male |
|
Female |
|
|
Gender (n=16) |
6 |
|
10 |
|
Table 1: Characteristics of Participants
*Mean (Range)
E. Analysis
All transcripts were reviewed by JT and SG. Coding was done manually using Microsoft Word. During the process, themes were identified and substantiating quotes were recorded. Iterative data analysis was done so that interviewers were aware of themes that were previously mentioned. However, the themes were not specifically explored unless brought up by the subsequent interviews.
III. RESULTS
Through the interviews, we collected information about the experiences within the ED. Interview transcripts collected as a part of this study are openly available on Figshare at http://doi.org./10.6084/m9.figshare.19204761 (Tan et al., 2022). From the interviews conducted, the experience was divided into the initial perceptions and coping mechanisms.
A. Perceptions
The perceptions of the paediatric emergency rotation in the ED were largely contributed by the experiences of the individuals who had previously worked in the department. This was achieved through consultation with friends or colleagues prior to starting the posting to find out more about the rotation.
“Before I started doing the posting, I asked some people who have done or were currently doing the posting…to find out what I was getting myself into”
(P7)
The broad themes elicited about the perceptions and inherent worries of the incoming medical officers were that of being unprepared due to ‘inadequate knowledge’ or ‘unfamiliarity’, as well as the impending ‘work load’ and ‘work factors’.
1) Fear of subject matter: Participants who were not familiar with the paediatric content were worried about their competency and adequacy in treating children. Oftentimes, participants cited that exposure to the paediatric subject matter may have been inadequate or dated and as a result, resulted in fears of being unprepared or being unsafe.
“I’ve not done any paediatric postings before as a doctor so that was a bit worrying.”
(P4)
“I’ve never dealt with paediatrics before so it was quite scary to come onto the posting”
(P14)
In participants who did however have some background in paediatrics, additional fears of specialised emergency knowledge also emerged with participants feeling nervous about the posting.
“Some of the things included technical skills such as doing back slabs, manipulation and reduction, and I guess managing trauma and more complicated acute conditions such as diabetic ketoacidosis and haemophilia and oncological and metabolic related conditions.”
(P11)
“When I started I learnt about resuscitation cases which I felt was a bit nerve-wracking to start with”
(P12)
2) Unfamiliarity: Even though participants may have been at different time points in their careers during the posting, they were all expected to perform mostly the same duties and responsibilities. As a result, a section of the participants cited worries about adjusting to the roles and environment that they may have been new to. These included concerns about being new to the system used. These added to the worries that participants often had about starting a new posting and made participants even more fearful.
“Coming from the UK, this was my first job in Singapore as a MO and thus had close to 0 experience of working in Singapore”
(P8)
“I was also not very familiar with the system. It added to the fear and unpreparedness before starting the posting.”
(P9)
3) Work factors: As a place with high turnover and workload, the picture painted to many of the participants was that it may be difficult to cope with the high workload. This would result in participants being overloaded and overwhelmed. A level of uncertainty was also described. Many participants were left feeling fearful, apprehensive and unsure of what to expect during the upcoming posting. Some were also worried about the expectations they may have to live up to and the nature of the environment being extremely stressful.
“I just heard that it can be quite busy with many patients and at the beginning, it can feel a bit of a throw into the deep end as we often don’t know what to expect and the learning curve can be quite steep”
(P12)
“I was also a bit apprehensive as I heard how busy the posting could get”
(P10)
“It’s quite a stressful working environment because the seniors have a certain working expectation and if you can’t live up to the expectations.”
(P16)
Practically, participants were also worried about the potential to get sufficient rest. Many participants heard that manpower may be tight and would result in having fewer or insufficient off days and would run the risk of feeling tired and burnt out.
“I heard that it was also difficult to get leave that you want and that you would also be really tired during the posting”
(P13)
B. Coping Mechanisms
We then explored the different ways the participants utilised to cope with their experiences in the ED. Participants used a variety of means that we broadly classified into broad themes of ensuring clinical safety, psychosocial support and spirituality.
1) Clinical safety: Participants were inevitably worried about competency and had inherent fears of patient safety in their practice. Coping strategies in this realm could be divided into preparation, senior supervision and collegial opinion.
Preparation was often seen in speaking to doctors who had previously rotated through the posting to allow junior doctors to prepare themselves mentally.
“I asked around and tried to mentally prepare myself for what people told me to expect”
(P3)
In addition, the perceived knowledge gaps and lack of experience were dealt with by many participants through studying and reading up to cover these gaps as well as to prevent them from feeling out of depth.
“I had actually read the guidelines prior especially for the things that I was not familiar with.”
(P10)
On the ground, participants found the availability and approachability of help and support from senior colleagues helpful in easing the worry and anxiety experienced in the emergency department. This also helped participants feel more safe and secure in their practices in the emergency department.
“I appreciate the nice seniors. Most of the seniors are approachable and they treat us like fellow colleagues. They respect our opinions and try to keep it in mind”
(P10)
“I feel very safe at work and very well supported by the seniors. In general, it is easy to ask for help from most of the seniors.”
(P8)
In addition, many participants also felt that their fellow medical officer colleagues were also important in ensuring safety in their practice. With different levels of experience, they could bounce ideas off each other and get a second opinion from their peers. Furthermore, their colleagues also helped to pick up the workload when they felt overwhelmed.
“Everyone is willing to help out when you get stuck. Help is useful and it is easy to come by”
(P1)
“I feel like I have a good relationship with them (peers) and that helps me and I can also get second opinions from them if I’m unsure.”
(P9)
2) Psychosocial support: In the high-strung environment of the emergency department, there is a lot of stress and emotions that come with the job. We found that many participants shared about the social component involved in unpacking these emotions and relieving their stress. The components of the collegial environment and support from loved ones appeared to be crucial coping mechanisms that helped participants.
The work climate was cited to be collegial and relationships between co-colleagues were described as friendly. Many participants felt comfortable with their co-colleagues such that they could ventilate their emotions and experiences with one another. These helped participants process and debrief their experiences.
“We generally laugh about the situation together and it gets better. Sometimes they give advice based on what they have seen and how to avoid such circumstances and we try and help each other.”
(P7)
“It’s useful amongst colleagues because we go through the same things and we get to exchange ideas and I feel we get to debrief this way as well. That helps because we don’t feel like we go through it alone because we have similar experiences.”
(P8)
Apart from the work environment, supportive loved ones and close friends also helped participants cope with difficult days. Participants cited that out of work encounters helped them to get through tough days and relieve their stress.
“Sometimes I also talk about it with someone. Usually that helps and my stress doesn’t usually last beyond the same day.”
(P6)
“I guess these 3 things, my family, friends and colleagues help me with tough days.”
(P7)
3) Spirituality and wellness: Spirituality and wellbeing were also important in dealing with the experiences and stressors the participants faced. Apart from dealing with the clinical stressors and unpacking the experiences with others, participants also spoke about coming to terms with their experiences and emotions on their own. This involved components of religion and reflexivity. Participants also spoke about the role of maintaining their wellbeing with leisure and self-care activities.
Participants spoke about reflecting and reviewing the good as well as the bad moments at work. These helped the participants make sense of their experiences and as a result, helped them improve and learn.
“I usually pray and reflect on my day and think about what are the good points I can get out of the day.”
(P9)
Religion also featured as a means of coping with emotions in the sometimes chaotic environment seen in the ED. These helped participants work better and feel more focused at work.
“I feel like I’m stable when I pray … and I think more thoughts are more ordered. That helps me.”
(P15)
Focusing on physical wellbeing also helped to reduce the stress experienced. Participants cited different activities – food, sleep, exercise, self-care and hobbies that helped them take their minds off work and help them get rejuvenated before the next working day.
“Eating and relaxing help me after a tough day”
(P4)
“I find exercising is helpful, and it helps me feel fresher and less sleepy”
(P3)
“Listening to music and watching videos and just going about non-work related normal daily life.”
(P11)
“I ensure that I have a good work-life balance… I go for a massage, go for a buffet, watch a movie and enjoy myself.”
(P13)
“I draw, I paint. I learn languages. Sometimes I travel. These things help me relax and cope with stress.”
(P16)
IV. DISCUSSION
We sought to understand the perceptions of junior doctors starting out in the emergency department as well as the subsequent coping strategies they undertook for challenges that they faced. During the process, we interviewed sixteen junior doctors who spoke in detail about their experiences.
The perceptions that the junior doctors in our study described consisted mainly of their worries and concerns prior to the start of the posting. Most of the perceptions and worries were centred on knowledge, workload and responsibilities that came with the posting.
A large proportion of participants expressed worry regarding competency and personal comfort levels in managing children. As the ED is a broad one and knowledge is inexhaustible, the concerns in lack of competency are seen in the other elements of emergency care and not strictly paediatric emergency (Jelinek et al., 2013; Kennelly et al., 2012; Yong & Ng, 2016).
Many of the worries described by the participants were of an anticipatory nature, from hearing their predecessors’ experiences. Anticipation of negative experiences can lead to anxiety and stress in individuals (Carlson et al., 2010; Grupe & Nitschke, 2013). Participants had anxiety about the workload and certain work factors prior to the start of the posting. While predecessors’ recounts are helpful in preparing doctors for their upcoming experience, the anxiety that comes with this preparation may not be. Positive effects can also be seen when a positive picture is painted of the upcoming experience (Gangwal et al., 2014; Luo et al., 2018). As it is difficult to balance the negative anxiety and the positive effects of preparation, it may be helpful for junior doctors to receive a formal handover from existing doctors who themselves have had a positive experience so as to prevent excessive anxiety.
We next explored the coping strategies involved to help the participants through the difficult parts of their experiences.
In areas of safety, participants commented on how the support from the senior staff helped allay their fears and increase patient safety at work. Other studies showed similar themes with HCWs expressing the desire for support, professional help and preventive action in the ED (Mikkola et al., 2019; Povedano-Jimenez et al., 2020; Ruotsalainen et al., 2015). In situations where support was provided, these corresponded to higher levels of satisfaction at work (Hunsaker et al., 2015). This is especially so in HCWs who were exposed to traumatic situations (Zhao et al., 2015).
Social support is an important factor in dealing with stressful situations (Gribben et al., 2019). In our cohort, our participants also engaged in social interactions with family, friends and colleagues in an attempt to deal with stressors in the ED. The collegial environment was also beneficial in dealing with stress and helping participants better process their experiences (Povedano-Jimenez et al., 2020).
Apart from expressing emotions and stressors, participants also sought to ensure mental and physical wellness of oneself. This was done by focusing on their spirituality as well as physical wellness and self-care. These strategies utilised were similar to those seen in other studies (Gribben et al., 2019; Hoonpongsimanont et al., 2013; McPherson et al., 2003; Palmer Kelly et al., 2020; Xu et al., 2019).
Maladaptive coping strategies did not come up as a main theme in our interviews.
A. Limitations
The study was conducted in a single ED at a single time point. Efforts were taken to diversify the population interviewed with participants experiencing different durations within the department. However, interviews of participants who had experienced the ED at different time points could have brought about different views and themes.
The primary investigator was also working within the same department during the time of the study. As the investigator was also a junior doctor during the study, a power dynamic effect was minimised.
The setting was limited to a single centre in the Singapore setting and thus, was extremely specific. Singapore is a city-state with easy access to healthcare. In addition, due to strict legislation, violence is minimal compared to other areas. As such, the patient load and patient type may differ from other ED and may raise the question of applicability in a different setting.
In addition, this study was conducted prior to the COVID-19 pandemic and the findings were representative of the climate at that time. The pandemic has led to multiple changes in workflow and work culture in the paediatric ED, and these may affect the applicability of our findings.
B. Future Research and Practical Implications
The study is the first qualitative in-depth study looking at perceptions and coping strategies in a paediatric emergency setting among junior doctors in a single centre. It is the first study to explore the individual perceptions and coping mechanisms of doctors, with a focus on the subset of junior doctors. The group was relatively small and conducted at a single time point. As such, the study can be expanded to include a larger group of participants across different time points and centres to illustrate a bigger picture.
Many of the participants also talked about the challenges they experienced in the paediatric emergency. They also raised possible improvements that could be made to help with stressors and challenges in the ED. This could be studied further and future research could focus on how we could target these factors and how effective these adjustments can be.
The findings of this research echoed the findings of prior studies. This study also sheds light and gives us more depth in terms of the early perceptions prior to the start of the postings and the coping strategies that were used.
These findings can also help future doctors rotating through the ED picture the experience. This would give doctors an opportunity to decide how best to prepare themselves. It could also help the doctors feel united with their current colleagues and predecessors in their challenges. And that they are not alone in their experiences.
V. CONCLUSION
In this study, the perceptions of junior doctors and coping strategies of junior doctors in an Asian Paediatric ED were studied. We looked at the perceptions and coping strategies utilised. Many factors were established in contributing to the experience. Improvements and suggestions to improve the experience were also brought up. Other HCWs can also understand how to best work with the junior doctors to facilitate an effective and pleasant working environment.
Notes on Contributors
Jaime Tan undertook literature reviews, conducted and analysed interviews and drafted the manuscript. Junaidah Badron reviewed the interviews and drafted and reviewed the manuscript. Sashikumar Ganapathy conceived the idea of the study, reviewed and analysed interview transcripts and advised the manuscript design. All authors have read and approved the final manuscript.
Ethical Approval
This project was submitted to the Centralised Institutional Review Board for approval (CIRB Ref 2019.2772). All participants consented to the research study.
Data Availability
All data collected in this study are openly available on Figshare repository, http://doi.org/10.6084/m9.figshare.19204761
Acknowledgement
We would like to thank all participants for volunteering their time and agreeing to participate in this study.
Funding
No funding was involved in this study.
Declaration of Interest
The authors declare that they have no conflicts of interest.
References
Abraham, L. J., Thom, O., Greenslade, J. H., Wallis, M., Johnston, A. N., Carlström, E., Mills, D., & Crilly, J. (2018). Morale, stress and coping strategies of staff working in the emergency department: A comparison of two different-sized departments. Emergency Medicine Australasia, 30(3), 375-381. https://doi.org/10.1111/1742-6723.12895
Alomari, A. H., Collison, J., Hunt, L., & Wilson, N. J. (2021). Stressors for emergency department nurses: Insights from a cross‐sectional survey. Journal of Clinical Nursing, 30(7-8), 975-985. https://doi.org10.1111/jocn.15641
Barham, D., De Beer, W., & Clark, H. (2019). The role of professional supervision for palliative care doctors in New Zealand: A quantitative survey of attitudes and experiences. The New Zealand Medical Journal, 132(1501), 10–20.
Basu, S., Yap, C., & Mason, S. (2016). Examining the sources of occupational stress in an emergency department. Occupational Medicine, 66(9), 737–742. https://doi.org/10.1093/occmed/kqw155
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
Burbeck, R., Coomber, S., Robinson, S. M., & Todd, C. (2002). Occupational stress in consultants in accident and emergency medicine: A national survey of levels of stress at work. Emergency Medicine Journal, 19(3), 234–238. https://doi.org/10.1136/emj.19.3.234
Carlson, J. M., Greenberg, T., Rubin, D., & Mujica-Parodi, L. R. (2010). Feeling anxious: Anticipatory amygdalo-insular response predicts the feeling of anxious anticipation. Social Cognitive and Affective Neuroscience, 6(1), 74–81. https://doi.org/10.1093/scan/nsq017
Chan, C. Y. W., Sum, M. Y., Lim, W. S., Chew, N. W. M., Samarasekera, D. D., & Sim, K. (2016). Adoption and correlates of Postgraduate Hospital Educational Environment Measure (PHEEM) in the evaluation of learning environments – A systematic review. Medical Teacher, 38(12), 1248–1255. https://doi.org/10.1080/0142159x.2016.1210108
Chew, Q. H., Ang, L. P., Tan, L. L., Chan, H. N., Ong, S. H., Cheng, A., Lai, Y. M., Tan, M. Y., Tor, P. C., Gwee, K. P., & Sim, K. (2019). A cross-sectional study of burnout and its associations with learning environment and learner factors among psychiatry residents within a National Psychiatry Residency Programme. BMJ Open, 9(8), e030619. https://doi.org/10.1136/bmjopen-2019-030619
Copeland, D., & Henry, M. (2018). The relationship between workplace violence, perceptions of safety, and professional quality of life among emergency department staff members in a Level 1 Trauma Centre. International Emergency Nursing, 39, 26–32. https://doi.org/10.1016/j.ienj.2018.01.006
Degen, C., Weigl, M., Glaser, J., Li, J., & Angerer, P. (2014). The impact of training and working conditions on junior doctors’ intention to leave clinical practice. BMC Medical Education, 14(1). https://doi.org/10.1186/1472-6920-14-119
Durand, A. C., Bompard, C., Sportiello, J., Michelet, P., & Gentile, S. (2019). Stress and burnout among professionals working in the emergency department in a French university hospital: Prevalence and associated factors. Work, 63(1), 57–67. https://doi.org/10.3233/wor-192908
Ganapathy, S., Lim, S. Y., Kua, J. P., & Ng, K. C. (2015). Non-urgent paediatric emergency department visits: Why are they so common? A Singapore perspective. Annals of the Academy of Medicine, Singapore, 44(7), 269–271. https://doi.org/10.47102/annals-acadmedsg.v44n7p269
Gangwal, R. R., Rameshchandra Badjatia, S., & Harish Dave, B. (2014). Effect of exposure to positive images of dentistry on dental anxiety among 7 to 12 years old children. International Journal of Clinical Pediatric Dentistry, 7(3), 176–179. https://doi.org/10.5005/jp-journals-10005-1260
Greenslade, J. H., Wallis, M., Johnston, A. N. B., Carlström, E., Wilhelms, D. B., & Crilly, J. (2019). Key occupational stressors in the ED: an international comparison. Emergency Medicine Journal, 37(2), 106–111. https://doi.org/10.1136/emermed-2018-208390
Gribben, J. L., Kase, S. M., Waldman, E. D., & Weintraub, A. S. (2019). A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in paediatric critical care physicians in the United States*. Paediatric Critical Care Medicine, 20(3), 213–222. https://doi.org/10.1097/pcc.0000000000001803
Grupe, D. W., & Nitschke, J. B. (2013). Uncertainty and anticipation in anxiety: An integrated neurobiological and psychological perspective. Nature Reviews Neuroscience, 14(7), 488–501. https://doi.org/10.1038/nrn3524
Guise, J. M., Hansen, M., O’Brien, K., Dickinson, C., Meckler, G., Engle, P., Lambert, W., & Jui, J. (2017). Emergency medical services responders’ perceptions of the effect of stress and anxiety on patient safety in the out-of-hospital emergency care of children: A qualitative study. BMJ Open, 7(2), e014057. https://doi.org/10.1136/bmjopen-2016-014057
Healy, S., & Tyrrell, M. (2011). Stress in emergency departments: Experiences of nurses and doctors. Emergency Nurse, 19(4), 31–37. https://doi.org/10.7748/en2011.07.19.4.31.c8611
Hoonpongsimanont, W., Murphy, M., Kim, C. H., Nasir, D., & Compton, S. (2013). Emergency medicine resident well-being: Stress and satisfaction. Occupational Medicine, 64(1), 45–48. https://doi.org/10.1093/occmed/kqt139
Howlett, M., Doody, K., Murray, J., LeBlanc-Duchin, D., Fraser, J., & Atkinson, P. (2015). Burnout in emergency department healthcare professionals is associated with coping style: A cross-sectional survey. Emergency Medicine Journal, 32(9), 722–727. https://doi.org/10.1136/emermed-2014-203750
Hunsaker, S., Chen, H. C., Maughan, D., & Heaston, S. (2015). Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. Journal of Nursing Scholarship, 47(2), 186–194. https://doi.org/10.1111/jnu.12122
Jackson, E. R., Shanafelt, T. D., Hasan, O., Satele, D. V., & Dyrbye, L. N. (2016). Burnout and alcohol abuse/dependence among U.S. medical students. Academic Medicine, 91(9), 1251–1256. https://doi.org/10.1097/acm.0000000000001138
Jelinek, G. A., Weiland, T. J., Mackinlay, C., Gerdtz, M., & Hill, N. (2013). Knowledge and confidence of Australian emergency department clinicians in managing patients with mental health-related presentations: Findings from a national qualitative study. International Journal of Emergency Medicine, 6, Article 2. https://doi.org/10.1186/1865-1380-6-2
Kennelly, S. P., Morley, D., Coughlan, T., Collins, R., Rochford, M., & O’Neill, D. (2012). Knowledge, skills and attitudes of doctors towards assessing cognition in older patients in the emergency department. Postgraduate Medical Journal, 89(1049), 137–141. https://doi.org/10.1136/postgradmedj-2012-131226
Koh, M. Y. H., Chong, P. H., Neo, P. S. H., Ong, Y. J., Yong, W. C., Ong, W. Y., Shen, M. L. J., & Hum, A. Y. M. (2015). Burnout, psychological morbidity and use of coping mechanisms among palliative care practitioners: A multi-centre cross-sectional study. Palliative Medicine, 29(7), 633–642. https://doi.org/10.1177/0269216315575850
Luo, Y., Chen, X., Qi, S., You, X., & Huang, X. (2018). Well-being and anticipation for future positive events: Evidences from an fMRI Study. Frontiers in Psychology, 8. https://doi.org/10.3389/fpsyg.2017.02199
Mason, S., O’Keeffe, C., Carter, A., & Stride, C. (2015). A longitudinal study of well-being, confidence and competence in junior doctors and the impact of emergency medicine placements. Emergency Medicine Journal, 33(2), 91–98. https://doi.org/10.1136/emermed-2014-204514
McPherson, S., Hale, R., Richardson, P., & Obholzer, A. (2003). Stress and coping in accident and emergency senior house officers. Emergency Medicine Journal, 20(3), 230–231. https://doi.org/10.1136/emj.20.3.230
Mikkola, R., Huhtala, H., & Paavilainen, E. (2019). Development of a coping model for work‐related fear among staff working in emergency department in Finland – Study for nursing and medical staff. Scandinavian Journal of Caring Sciences, 33(3), 651–660. https://doi.org/10.1111/scs.12658
Neubauer, B. E., Witkop, C. T., & Varpio, L. (2019). How phenomenology can help us learn from the experiences of others. Perspectives on Medical Education, 8(2), 90–97. https://doi.org/10.1007/s40037-019-0509-2
Oreskovich, M. R., Shanafelt, T., Dyrbye, L. N., Tan, L., Sotile, W., Satele, D., West, C. P., Sloan, J., & Boone, S. (2015). The prevalence of substance use disorders in American physicians. The American Journal on Addictions, 24(1), 30–38. https://doi.org/10.1111/ajad.12173
Palmer Kelly, E., Hyer, M., Payne, N., & Pawlik, T. M. (2020). A mixed-methods approach to understanding the role of religion and spirituality in healthcare provider well-being. Psychology of Religion and Spirituality, 12(4), 487–493. https://doi.org/10.1037/rel0000297
Pek, J. H., Ong, Y. K. G., Quek, E. C. S., Feng, X. Y. J., Allen, J. C., Jr., & Chong, S. L. (2019). Evaluation of the criteria for trauma activation in the paediatric emergency department. Emergency Medicine Journal, 36(9), 529–534. https://doi.org/10.1136/emermed-2018-207857
Povedano-Jimenez, M., Granados-Gamez, G., & Garcia-Caro, M. P. (2020). Work environment factors in coping with patient death among Spanish nurses: A cross-sectional survey. Revista Latino-Americana de Enfermagem, 28. https://doi.org/10.1590/1518-8345.3279.3234
Ruotsalainen, J., Verbeek, J., Mariné, A., & Serra, C. (2015). Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews, 2015(4), CD002892. https://doi.org/10.1002/14651858.cd002892.pub5
Ryali, V. S. R., Sreelatha, P., & Premlal, L. (2018). Burnout and coping strategies among residents of a private medical college in South India: A cross-sectional study. Industrial Psychiatry Journal, 27(2), 213-218. https://doi.org/10.4103/ipj.ipj_53_18
Shanafelt, T. D., Boone, S., Tan, L., Dyrbye, L. N., Sotile, W., Satele, D., West, C. P., Sloan, J., & Oreskovich, M. R. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377-1385. https://doi.org/10.1001/archinternmed.2012.3199
Smith, D. W. (2021). Stanford Encyclopaedia of Philosophy. https://plato.stanford.edu.
Sum, M. Y., Chew, Q. H., & Sim, K. (2019). Perceptions of the learning environment on the relationship between stress and burnout for residents in an ACGME-I accredited national psychiatry residency program. Journal of Graduate Medical Education, 11(4s), 85–90. https://doi.org/10.4300/jgme-d-18-00795
Talih, F., Daher, M., Daou, D., & Ajaltouni, J. (2018). Examining burnout, depression, and attitudes regarding drug use among Lebanese medical students during the 4 years of medical school. Academic Psychiatry, 42(2), 288–296. https://doi.org/10.1007/s40596-017-0879-x
Tan, M. Y., Ng, N. B. H., Aw, M. M., & Lin, J. B. (2022). Perceived stress & sentiments of housemen starting work during the COVID-19 Pandemic in Singapore. The Asia Pacific Scholar, 7(2), 56–60. https://doi.org/10.29060/taps.2022-7-2/sc2686
Tuffour, I. (2017). A critical overview of interpretative phenomenological analysis: A contemporary qualitative research approach. Journal of Healthcare Communications, 2(4). https://doi.org/10.4172/2472-1654.10009
Watson, A. G., Saggar, V., MacDowell, C., & McCoy, J. V. (2019). Self-reported modifying effects of resilience factors on perceptions of workload, patient outcomes, and burnout in physician-attendees of an international emergency medicine conference. Psychology, Health & Medicine, 24(10), 1220–1234. https://doi.org/10.1080/13548506.2019.1619785
Xu, H. G., Johnston, A. N., Greenslade, J. H., Wallis, M., Elder, E., Abraham, L., Thom, O., Carlström, E., & Crilly, J. (2019). Stressors and coping strategies of emergency department nurses and doctors: A cross-sectional study. Australasian Emergency Care, 22(3), 180–186. https://doi.org/10.1016/j.auec.2018.10.005
Yong, A. M. Y., & Ng, J. (2016). Assessing the level of knowledge of emergency department physicians in recognition of common skin lesions. Annals of Clinical and Laboratory Research, 4(1). https://doi.org/10.21767/2386-5180.100073
Zhao, S., Liu, H., Ma, H., Jiao, M., Li, Y., Hao, Y., Sun, Y., Gao, L., Hong, S., Kang, Z., Wu, Q., & Qiao, H. (2015). Coping with Workplace Violence in Healthcare Settings: Social Support and Strategies. International Journal of Environmental Research and Public Health, 12(11), 14429–14444. https://doi.org/10.3390/ijerph121114429
*Jaime Maria Tan
KK Women’s and Children’s Hospital,
100 Bukit Timah Road,
Singapore 229899
+6590303124
Email: jaime.tan@mohh.com.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









