Implicit leadership theories and followership informs understanding of doctors’ professional identity formation: A new model
Published online: 2 May, TAPS 2017, 2(2), 18-23
DOI: https://doi.org/10.29060/TAPS.2017-2-2/OA1022
Judy McKimm, Claire Vogan & Hester Mannion
Swansea University Medical School, Swansea University, United Kingdom
Abstract
Aims: The process of becoming a professional is a lifelong, constantly mediated journey. Professionals work hard to maintain their professional and social identities which are enmeshed in strongly held beliefs relating to ‘selfhood’. The idea of implicit leadership theories (ILT) can be applied to professional identity formation (PIF) and development, including self-efficacy. Recent literature on followership suggests that leaders and followers co-create a dynamic relationship and we suggest this occurs commonly in the clinical setting. The aim of this paper is to describe a new model which utilises ILT and followership theory to inform our understanding of doctors’ PIF.
Methods: Following a literature review, we applied the core concepts of ILT and followership theories to theories underlying PIF by developing a mapping framework. We identified core themes, similarities and differences between the three perspectives and constructed a new model of PIF incorporating elements from ILT and followership. The model can be used to explain and inform understanding of medical practice and leadership situations.
Conclusion: The model offers insight into how concepts such as self-efficacy, prototypicality, implicit theories of self, power, authority and control and cultural competence result in PIF. Bringing together the theoretical frameworks of ILT and followership theory with PIF theories helps us understand and explain the unique dynamic of the clinical environment in a new light; prompting new ways of thinking about teams, interprofessional working, leadership and social identity in medicine. It also offers the potential for new ways of teaching, curriculum design, learning and assessment.
Keywords: Followership; Leadership; Professional Identity; Self Efficacy
Practice Highlights
- Doctors have a deep rooted professional and social identity that is closely connected with notions of leadership.
- New insight into professional identity formation can be achieved by applying the theoretical frameworks of implicit leadership theories, followership, and self efficacy.
- A better understanding of professional identity formation could potentiate new ways of approaching medical education and curriculum design.
I. INTRODUCTION
Doctors’ professional identity formation (PIF) is informed by many factors in the professional environment and is also inextricably linked to social status and personal identity. The professional identity of a doctor is a personal one before it is a group one. The emphasis on personal career progression, competition with peer group and relative autonomy in senior positions starts at medical school, this risks a prevailing attitude amongst physicians that they are ‘lone healers’ (Lee, 2010), causing inevitable problems with team-working. An understanding of how professional identity formation comes about is vital to an understanding of how doctors function in leadership, followership and team-working roles. Our model aligns this for practical developmental purposes with the ‘inbound trajectory’ adapted from the ‘novice to expert model of professional competence’ (Flower, 1999) (see Fig 1).
This model identifies that professional competence develops over time with feedback and reflection. Individuals become part of a ‘community of practice’ as they move along an ‘inbound trajectory’ towards being ‘expert’ (Wenger-Trayner & Wenger-Trayner, 2015). In terms of professional identity formation in ‘becoming a doctor’, a ‘novice’ would not be really aware of the ‘reality’ of medicine, what being a doctor is about or how medicine is positioned vis a vis other professionals. Gradually, through trial and error, observation, conversations and ‘heat experiences’ (significant learning events)(Petrie, 2014), a more rounded and mature professional identity develops so that by the time the doctor is seen as ‘expert’ by others, they also see themselves as proficient, competent professionals distinct from other health workers. The following sections discuss followership theory; implicit leadership theory and implicit theories of the self and conclude by offering suggestions as to how our integrated model of professional identity formation can be used to develop doctors’ leadership, followership and team working skills.
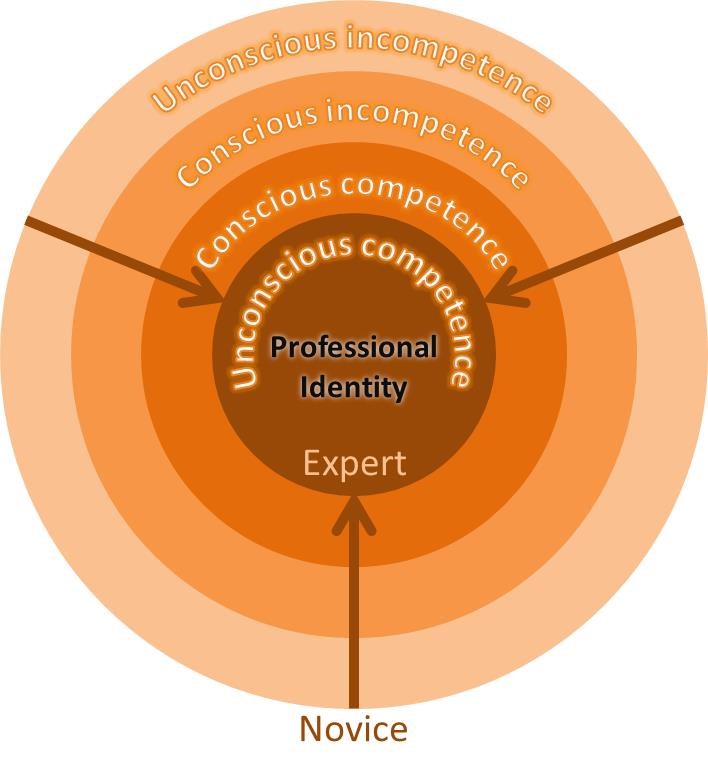 Figure 1. Development of professional identity: A diagrammatic representation of desired inbound trajectory along the ‘novice to expert model of professional competence’ (Flower, 1999).
Figure 1. Development of professional identity: A diagrammatic representation of desired inbound trajectory along the ‘novice to expert model of professional competence’ (Flower, 1999).
II. FOLLOWERSHIP THEORY
Followership theory provides a much needed alternative perspective in a world of leadership-centric models. Leadership, management and followership form an interlinked triad of activities (Till & McKimm, 2016). A consideration of followership informs our understanding of leadership by describing the influence that followers have on their leaders and the process of ‘co-creation’ that occurs as a result of the impact that followers have on leaders and leadership styles (Uhl-Bien, Riggio, Lowe & Carsten, 2014). In leadership-centric thinking, followers are often described in terms of subordination or even derogation. Followership thinking, by contrast, highlights the importance of followership behaviour in facilitating and forming leadership. Followership describes individuals who are more than just those who are ‘not-leading’ or ‘not-leading right now’. Followership practice varies as much as leadership practice, ranging from star-followers who represent an engaged and dynamic influence to those who make effort to be obstructive to team progress and challenge leaders’ authority. Followers can therefore have positive or negative powerful impact on the direction of a team and leadership efficacy. The identity of ‘leader’ and ‘follower’ must be considered fluid, all followers lead and all leaders follow in different contexts.
Doctors who follow are often seen (and see themselves) as ‘leaders in waiting’, ready to move along the ‘inbound trajectory’ by engaging in ‘small ‘l’’ activities (Bohmer, 2012) and moving up the medical hierarchy. Medical schools encourage students to compete with one another, to stand out and win prizes. This continues in the working environment where recognition and reward is for those who can show their personal contribution to service provision and improvement. As a result, it becomes culturally acceptable and desirable to aspire to leadership roles and to place personal career progression over team success, this has profound implications for team working in health services. Real team working in UK hospitals has been described as no more than an ‘illusion’ (West & Lyubovnikova, 2013), with groups of people working in ‘pseudo-teams’. Effective team work requires clear, defined and shared goals, when there is no meaningful team dynamic, quality of patient care must suffer. Although many Medical Councils highlight the importance of team-working in their professional standards, the notion of aspiring to outstanding followership is countercultural in medicine, partly because it is potentially threatening to professional identity.
III. IMPLICIT LEADERSHIP SOCIAL IDENTITY THEORY
One follower-centric approach encompasses the Implicit Leadership Theories (ILTs), which state that followers hold pre-conceived beliefs (almost stereotypes) about what makes a good or a bad leader. The ILTs are often based on a range of generic characteristics (such as height, gender, ethnic or professional background) and played out in practice through unconscious biases. Given the central role that followers play in creating and facilitating leadership, those leaders whose ‘faces don’t fit’ (for whatever reason) may have a difficulty persuading their followership to follow. Those who do not fit the pre-conceived implicit criteria may have to work much harder to gain the trust of a followership, this is regardless of the leader’s expertise and ability to lead. A followership of doctors has deep-seated pre-conceived beliefs about what their clinical leaders should look like. On an individual level these are created by past experiences and personal needs, on a group level these are created by professional culture, which, in turn, creates and is created by professional identity. Celebrated leaders in the world of medicine are usually those who are clinically excellent or high flying researchers, and who have personal charisma (the stereotypical ‘hero leader’), not necessarily those who display exceptional leadership, management and followership qualities in an everyday context. This may be because of the centrality of clinical ability in the professional and personal identity of doctors and may also help explain the relative reluctance of many doctors to move to the ‘dark side’ of healthcare management.
Social identity theory describes followers who identify closely with a leader as ‘high-identifiers’, the extent to which the leader represents the group they lead is referred to as their ‘prototypicality’.
Doctors, who commonly have aspirations to lead, are likely to be ‘high-identifiers’, closely identifying with the leader and the rest of the group, both socially and professionally. High-identifiers are more likely to be affected by group level behaviour but also have high expectations of procedural fairness in their leader and are more likely to be openly critical of leadership decisions. Prototypicality is also very important in clinical leadership, as doctors who follow identify closely with their leaders, they also expect them to look and sound like them, and most importantly they expect them to maintain a successful clinical role. Leaders in health services who do not have a clinical role are often viewed by doctors as an ‘out-group’, a good example of this might be non-clinical managers who are frequently mistrusted and blamed for health service failings. Problems may also arise in multi-disciplinary team settings where doctors, nurses and allied health professionals are required to work closely together. Doctors in this context may struggle to take leadership initiatives from those who are not doctors, however appropriate it is for that person to lead and how ever well qualified they are to do so (Barrow, McKimm & Gasquoine, 2011). Doctors who lead with the full support of their followership may not, therefore, be the most appropriate or able to lead, as their leadership expertise and ability is rarely that which is under scrutiny, rather it is their prototypicality that ensures loyalty. From this perspective, professional identity formation is therefore tied very closely to identifying with prototypical doctors and learning how to be like them. Whilst it can be helpful for individuals who ‘fit’, it can perpetuate a ‘people like us’ mentality and reluctance to welcome people seen as part of an ‘out-group’ into the profession (McKimm & Wilkinson, 2015) or into teams, which runs counter to inclusive leadership and celebration of diverse communities of practice.
IV. IMPLICIT THEORIES OF THE SELF AND SELF-EFFICACY
Implicit theories of the self-relate to domain specific ideas about identity and ability (Molden & Dweck, 2006). This framework divides people into two groups: ‘entity’ theorists who see their professional or social identity as rigid and fixed, and ‘incremental’ theorists who view their professional or social identity as malleable and developmental. In the clinical environment, doctors who hold entity theories regarding their professional identity are likely to find challenges to their professional identity difficult to manage. Such challenges may come in the form of non-doctors taking leadership roles, making a mistake or having a poor clinical outcome. Conversely, a doctor who holds incremental theories regarding professional identity is more likely to embrace and engage with challenges to preconceived identities, whether that is with new ways of working or in looking critically at long established systems. The question of whether doctors are more likely to be entity or incremental theorists in their professional lives is important. The study and practice of medicine can be lucrative and rewarding, but the lengthy training is rigid and prescriptive in many ways. It is reasonable to suggest that there may by a higher percentage of entity theorists amongst doctors than in other professions, not least because of the solid professional and social identity that it conveys. How fixed or fluid a follower feels about their own professional identity will directly impact how fixed or fluid they might feel about their leader, those who hold entity theories about their own professional identity are more likely to have a fixed idea about whether their leaders are fit for the job with little tolerance of those that do not meet their expectations. They are also likely not to appreciate the fluid nature of followership and leadership, with certain ‘types’ being deemed appropriate for simply one or the other.
‘Self-efficacy’ is a domain specific description of self-esteem (which can be understood as global) (Burnette, Pollack & Hoyt, 2010), high self-efficacy in the professional environment implies high professional self-confidence. For doctors with entity theories, high or low self-efficacy will impact their response to their own failings in the clinical environment. For example, those with inflexible entity theories and high self-efficacy (or high professional self-esteem) are likely to view mistakes as somebody else’s fault, alternatively, a doctor with low self-efficacy will be badly affected and possibly debilitated by a mistake. An incremental theorist is more likely to turn their attention to the detail of mistakes made, address them head on without fear and change future practice in light of them. Self-efficacy also effects desired protoypicality. If a doctor has low professional self-efficacy, they will desire leaders who do not look like them, those with high self-efficacy will be a high-identifier and the more prototypical the leader, the more effective they will be perceived to be.
V. AN INTEGRATED MODEL OF PROFESSIONAL IDENTITY FORMATION
So, how do these theories help our understanding of doctors’ professional identity formation in terms of their leadership, followership and team working approaches and skills? The model (Fig 2) maps the theoretical domains discussed in this paper onto the ‘novice to expert model’ which we suggest can be aligned with ‘becoming a doctor’. We have discussed how engagement in a range of activities can help doctors move along the inbound trajectory towards expertise. Such expertise has at its centre a professional identity which is fully aligned with social and self-identity, underpinned by accurate understanding of self-efficacy. These ‘experts’ belong firmly in their community of practice, however that is defined. We suggest also that an explicit focus on specific development activities, underpinned by the theories discussed here, will help develop doctors to function more effectively in multi-cultural and diverse health services and in interprofessional teams. An example of this in undergraduate training would be to give medical students opportunities to work with nursing students early on, this would help both groups to better understand each other and ‘normalize’ interprofessional teamwork at a formative stage.
Specifically, the model provides a framework for educators, supervisors and individuals to plan activities and development opportunities in three key areas of activity: leadership, followership and team working to support students and doctors to become ‘expert professionals’. Whilst some of the techniques are similar to that used in coaching, education or mentoring, the theoretical perspectives described here integrate the literature on team working, followership, leadership, (including implicit leadership theories), theories of self (including self-efficacy) and social and professional identity theory in a unique way. For example, when working with students and doctors in groups and teams (in real or simulated environments), teachers could set activities aimed towards developing shared team goals, ensuring leadership happens and the outcomes are effective. As part of the process, teachers should make explicit reference to and facilitate discussion about team roles, personality preferences and how to take both leadership and followership roles. Educational leaders might facilitate activities that focus on exploring and surfacing unconscious biases about other professional groups, patients or families or by giving and obtaining multi-source feedback on self-efficacy in interprofessional groups and teams. Such activities need to be carefully facilitated in an inclusive environment as much of this work relates directly to people’s views and feelings about ‘self’. This can be quite threatening if not carried out in a safe psychological and physical environment. Using structured debriefs, role modelling inclusive leadership behaviours, sharing appropriate aspects of teachers’ own development, experiences and difficulties will help learners gain self-knowledge and interpersonal skills and reap great benefits for practice.
Within the model, reflective practice plays a key role in challenging unhelpful behaviours and restrictive ways of thinking. As reflection becomes a normal part of training, so might doctors become more comfortable with the process of critically examining choices and learning needs. Universities and post-graduate training programmes can highlight the importance of reflective practice in the development of a well-rounded practitioner by rewarding personal development as well as attainment. Recognizing and rewarding those who show the ability to adapt and evolve will raise the profile of the softer but vital skill of reflection.
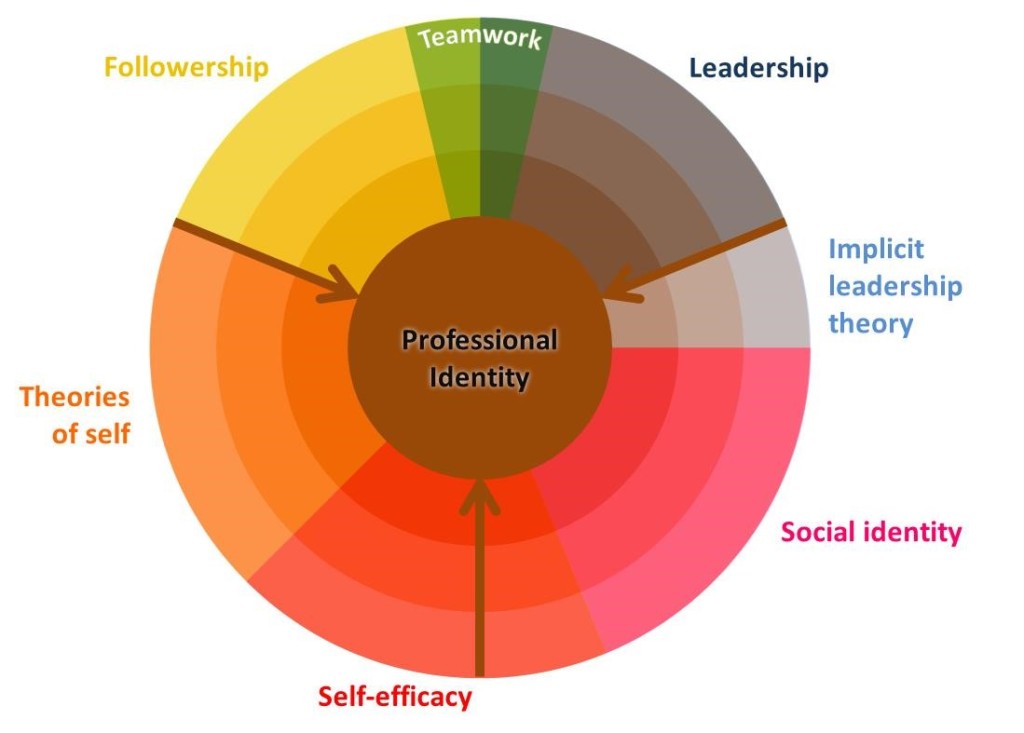 Figure 2. An integrated model that shows the development of a doctors’ professional identity formation, on an inbound trajectory (see Fig 1), through experience and gaining knowledge and understanding of leadership, followership, team working, implicit leadership theory, social identity, self-efficacy and theories of self
Figure 2. An integrated model that shows the development of a doctors’ professional identity formation, on an inbound trajectory (see Fig 1), through experience and gaining knowledge and understanding of leadership, followership, team working, implicit leadership theory, social identity, self-efficacy and theories of self
VI. CONCLUSIONS
Followership, leadership and team-working in medicine are all directly impacted by professional identity formation. Doctors develop as professionals to hold respected positions, to aspire to a degree of autonomous decision making and leadership roles; they are encouraged to compete with their peers and to put their energies in to personal career progression. A better understanding of the culture within medicine and professional identity formation may not only help us to understand the complex dynamic between leaders and followers, but also enable better team working among health professionals. Providing doctors at all stages of training with specific development opportunities designed to enable the acquisition of team working, leadership and followership skills will help more effective team working and improve healthcare. This model provides a structured framework for designing such development activities.
Notes on Contributors
Judy McKimm is Professor of Medical Education, Director of Strategic Educational Development and Director of the MSc in Leadership for the Health Professions at Swansea University. She runs clinical and educational leadership programmes around the world and publishes widely on leadership and education.
Claire Vogan is an Associate Professor at Swansea University Medical School and the Director of Student Support and Guidance for Graduate Entry Medicine. She specialises in the support of students in difficulty and teaches on the Leadership, Medical Education and Graduate Entry Medicine programmes in Swansea.
Hester Mannion graduated from the University of Exeter with a 1st class degree in English Literature and went on to gain a PGCE from King’s College London. She has graduated from Swansea University Medical School in 2016 and now working as a doctor in Wales.
Declaration of Interest
Authors have no conflicts of interest, including no financial, consultant, institutional and other relationships that might lead to bias.
References
Barrow, M., McKimm, J., & Gasquoine, S. (2011). The policy and the practice: Early-career doctors and nurses as leaders and followers in the delivery of health care. Advances in Health Sciences Education, 16(1), 17-29. https://doi.org/10.1007/s10459-010-9239-2.
Bohmer, R. (2012). The instrumental value of medical leadership. White Paper-The King’s Fund, London, England. Retrieved from
http://www.kingsfund.org.uk/sites/files/kf/instrumental-value-medical-leadership-richard-bohmer-leadership-review2012-paper.pdf
Burnette, J. L., Pollack, J. M., & Hoyt, C. L. (2010). Individual differences in implicit theories of leadership ability and self‐efficacy: Predicting responses to stereotype threat. Journal of Leadership Studies, 3(4), 46-56. https://doi.org/10.1002/jls.20138.
Flower, J. (1999). In the Mush. Physician Executive, 25(1), 64–66.
Lee, T.H. (2010). Turning doctors into leaders. Harvard Business Review, 88(4), 50-58.
McKimm, J., & Wilkinson, T. (2015). “Doctors on the move”: Exploring professionalism in the light of cultural transitions. Medical Teacher, 37(9), 837-843. https://doi.org/10.3109/0142159X.2015.1044953.
Molden, D. C., & Dweck, C. S. (2006). Finding “meaning” in psychology: a lay theories approach to self-regulation, social perception, and social development. American Psychologist, 61(3), 192. https://doi.org/10.1037/0003-066X.61.3.192. https://doi.org/10.1037/0003-066X.61.3.192.
Petrie, N. (2014). Future trends in leadership development. Center for Creative Leadership white paper. Retrieved from http://insights.ccl.org/wp-content/uploads/2015/04/futureTrends.pdf
Till, A, & McKimm, J. (2016). Leading from the frontline. BMJ, in press.
Uhl-Bien, M., Riggio, R. E., Lowe, K. B., & Carsten, M. K. (2014). Followership theory: A review and research agenda. The Leadership Quarterly, 25(1), 83-104. https://doi.org/10.1016/j.leaqua.2013.11.007.
Wenger-Trayner, E, & Wenger-Trayner, B. (2015). Communities of practice a brief introduction. Retrieved from http://wenger-trayner.com/introduction-to-communities-of-practice/
West, M. A., & Lyubovnikova, J. (2013). Illusions of team working in health care. Journal of Health Organization and Management, 27(1), 134-142. https://doi.org/10.1108/14777261311311843.
*Judy McKimm
Grove Building, Swansea University
Singleton Park, Swansea, SA2 8PP
Tel: (01792) 606854
Email: j.mckimm@swansea.ac.uk
Published online: 2 May, TAPS 2017, 2(2), 8-17
DOI: https://doi.org/10.29060/TAPS.2017-2-2/OA1004
Wee Shiong Lim1,2, Kar Mun Tham3, Fadzli Baharom Adzahar, Han Yee Neo4, Wei Chin Wong1 & Charlotte Ringsted5
1Department of Geriatric Medicine, Tan Tock Seng Hospital, Singapore; 2Health Outcomes and Medical Education Research, National Healthcare Group, Singapore; 3Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 4Department of Palliative Medicine, Tan Tock Seng Hospital, Singapore; 5Centre for Health Science Education, Faculty of Health, Aarhus University, Denmark
Abstract
Background: Medical education research should aspire to illuminate the field beyond description (“What was done?”) and justification (“Did it work?”) research purposes to clarification studies that address “Why or how did it work?” questions. We aim to determine the frequency of research purpose in both experimental and non-experimental studies, and ascertain the predictors of clarification purpose among medical education studies presented at the 2012 Asia Pacific Medical Education Conference (APMEC).
Methods: We conducted a systematic review of all eligible original research abstracts from APMEC 2012. Abstracts were classified as descriptive, justification or clarification using the framework of Cook 2008. We collected data on research approach (Ringsted et al., 2011), Kirkpatrick’s learner outcomes, statement of study aims, presentation category, study topic, professional group, and number of institutions involved. Significant variables from bivariate analysis were included in logistic regression analyses to ascertain the determinants of clarification studies.
Results: Our final sample comprised 186 abstracts. Description purpose was the most common (65.6%), followed by justification (21.5%) and clarification (12.9%). Clarification studies were more common in non-experimental than experimental studies (18.3% vs 7.5%). In multivariate analyses, the presence of a clear study aim (OR: 5.33, 95% CI 1.17-24.38) and non-descriptive research approach (OR: 4.70, 95% CI 1.50-14.71) but not higher Kirkpatrick’s outcome levels predicted clarification studies.
Conclusion: Only one-eighth of studies have a clarification research purpose. A clear study aim and non-descriptive research approach each confers a five-fold greater likelihood of a clarification purpose, and are potentially remediable areas to advance medical education research in the Asia-Pacific.
Keywords: Research Purpose; Research Approach; Medical Education Research; Asia-Pacific
Practice Highlights
- The hallmark of clarification research is the presence of a conceptual framework or theory that can be affirmed or refuted by the study results.
- We should aspire towards clarification studies that address “Why or how did it work?” questions.
- Only one-eighth of studies have a clarification research purpose.
- A clear study aim and non-descriptive research approach are potentially remediable areas to promote clarification studies.
I. INTRODUCTION
There is much debate about how to ensure that medical education research is not perceived as the poor relation of Biomedical research (Shea, Arnold, & Mann, 2004; Baernstein, Liss, Carney, & Elmore, 2007; Todres, Stephenson, & Jones, 2007).Some have proposed that if medical education were to fulfil its research potential and enjoy academic legitimacy, the discipline must develop a clearer sense of purpose and more rigorously follow the scientific line of enquiry characterized by a cycle of observation; formulation of a model or hypothesis to explain the results; prediction based on the model or hypothesis; and testing of the hypothesis (Cook, Bordage, & Schmidt, 2008a; Bordage, 2009). In particular, medical educators often focus on the first step (observation) and the last step (testing), but omit the intermediate steps (model formulation or theory building, and prediction), and perhaps more importantly, fail to maintain the cycle by building upon previous results. Some authorities attribute this lack of a conceptual framework as a major reason for the paucity of impactful research questions that can illuminate and magnify the body of knowledge to advance the field of medical education (Albert, Hodges, & Regehr, 2007; Cook et al., 2008b; Eva & Lingard, 2008).
Conceptual frameworks represent ways of thinking about an idea, problem, or phenomenon by relating to theories, models, evidence-based best practices or hypotheses (Rees & Monrouxe, 2010; Gibbs, Durning, & Van der Vleuten, 2011). The framework assists in formulating the research question, choosing an appropriate study design, and determining appropriate outcomes to answer the research question. Situating the research question within a conceptual framework elevates and transforms the research purpose from a study which is focused on local issues, into a clarification study of general interest by engendering generalizable knowledge which can be transferable to new settings and future research (Bordage, 2009; Bunniss & Kelly, 2010). Conceptual frameworks are also essential in interpreting the results. Their inter-dependent relationship is underscored by the fact that results are interpreted in light of the existing theories and conversely, existing boundaries of the theoretical framework may limit interpretation of the findings (Wong, 2016). For instance, in the field of observation-based assessments, there is a gradual theoretical shift from a more psychometric (based on large numbers of random elements) to a more expert judgement (based on fewer observation of well-informed opinions) framework (Hodges, 2013)
A. Cook’s Framework of Research Purpose
To better delineate this problem, Cook et al. (2008a) proposed a framework for classifying the purposes of research, namely description, justification and clarification. Description studies focus on the first step in the scientific method (observation) by addressing the question: “What was done?” Justification studies focus on the last step in the scientific method (testing) by asking: “Did it work?” However, without prior model formulation and prediction, the results may have limited application to future research or practice. In contrast, clarification studies seek to answer the question: “Why or how did it work?” The hallmark of clarification research is the presence of a conceptual framework that can be affirmed or refuted by the study results (Cook et al., 2008a; Ringsted, Hodges, & Scherpbier, 2011). Such research is often performed using classic experiments, but non-experimental methods such as correlation research, comparisons among naturally occurring groups, and qualitative research, are also applicable (Shea et al., 2004; Cook et al., 2008a).
Applying this framework in a systematic survey of 850 experimental and non-experimental studies on problem-based learning, Schmidt (2005) reported a paucity of clarification studies (7%) vis-à-vis description (64%) and justification (29%) studies. More recently, García-Durán et al. (2011) reported the predominance of description studies (92.8%) with very few justification (6.8%) studies and just one (0.4%) clarification study among research presentations at a medical education meeting in Mexico. These results are consistent with the seminal study of 105 articles describing education experiments in 6 major journals by Cook et al. (2008a), which noted that clarification studies were uncommon (12%) relative to justification (72%) and description (16%) studies. In this study, inter-rater agreement for these classifications was only moderate at 0.48, with disagreements largely occurring in the classification of less clear-cut single-group pre-test/post-test studies; this discrepancy has since been clarified in the revised definitions.
B. Gaps in Current Knowledge
Cook et al. (2008a) proposed expanding the use of their framework beyond the limited genre of experimental studies to incorporate non-experimental study designs. This input is sorely needed, as studies with a purely descriptive design (which may not qualify as research by some authorities) historically constituted a significant proportion of the literature in medical education (Reed et al., 2008; García-Durán et al., 2011). There is a unifying call for the use of stronger study designs in the field beyond cross-sectional descriptive approaches to enhance the quality of medical education research (Gruppen, 2007; Colliver & McGaghie, 2008).
The opportunity to extend the study of research purpose beyond experimental studies, was afforded by the research compass framework described by Ringsted et al. (2011). Core to the model is the conceptual framework, which is central to any research approach taken. The compass depicts four main quadrants of research approaches in the conduct of medical education research: (1) Explorative studies, aimed at modelling by seeking to identify and explain elements of phenomena and their relationships; (2) Experimental studies, with the main aim of justification to define appropriate interventions and outcomes; (3) Observational studies, aimed at predicting outcomes by the study of natural or static groups of people; and (4) Translational studies, which focus on implementing knowledge and findings from research in complex real-life settings.
Furthermore, predictors of a clarification research purpose in medical education scholarship have hitherto not been studied. Factors that are associated with better quality of medical education research include number of institutions studied (Reed et al., 2007; Reed et al., 2008), outcomes based on the widely-used hierarchy of Kirkpatrick (1967), and the presence of a clear statement of study intent (Cook et al., 2008b). However, the association between these factors with research purpose has not been previously examined.
C. Aims and hypothesis
In recent years, there is a surge of interest in research scholarship in medical education in the Asia-Pacific region. Concomitantly, regional forums such as the Asia-Pacific Medical Education Conference (APMEC) have emerged for the sharing of medical education research, along with ongoing discussions about how to propel the field forwards in conducting meaningful research that can inform educational practice (Gwee, Samarasekera, & Chong, 2012). Determining the prevalence of research purpose of medical education studies from the Asia-Pacific region would be of immediate relevance in ascertaining whether there is a similar lack of clarification studies and research approaches beyond descriptive study designs.
Building upon the earlier work of Cook et al. (2008a) in experimental studies, we developed an empirical operational model that combined the frameworks of Cook and Ringsted to broaden the evaluation of research purpose to include non-experimental studies. The objectives of our study are: (1) to determine the frequency of research purpose in both experimental and non-experimental studies, and (2) to ascertain the predictors of a clarification research purpose among original research abstracts presented at APMEC 2012. In light of the findings in earlier studies of the relative paucity of clarification studies (Schmidt 2005; Cook et al., 2008a; García-Durán et al., 2011), we hypothesize that the proportion of clarification studies would likewise be comparatively lower.
II. METHODS
A. Study setting
This review drew from research abstracts submitted to APMEC 2012. This study is part of a larger piece of work that aims to contribute to the research agenda in the Asia-Pacific region by determining the trends in research purpose and approach in the last 5 years (2008 to 2012). The APMEC is an established regional conference held in Singapore that serves as an accessible “clearinghouse” providing a timely and comprehensive snapshot of research in the Asia Pacific region. The theme for the 9th APMEC in 2012 was “Towards transformative education for healthcare professionals in the 21st century – nurturing lifelong habits of mind, behaviour and action.” The National Healthcare Group Institutional Review Board deemed this study exempt from review.
B. Study eligibility
All original research abstracts from APMEC 2012 were considered. Original research was defined as an educational intervention or trial; implementation of evidence based practice or guidelines; curriculum evaluation with subjective or objective outcomes; evaluation of an educational instrument or tool; qualitative research; and systematic reviews. We excluded abstracts from plenary lectures, workshops, special interest group meetings and discussions. Among 210 eligible abstracts, we excluded 24 that were not original research, thus yielding a final sample of 186 abstracts.
C. Data extraction
We performed a pilot study using randomly selected abstracts from APMEC 2011 conference in order to fine-tune definitions of study variables and to refine the data collection form. Four reviewers were involved in data collection. After training and harmonization in the pilot phase, the four raters achieved good to excellent agreement in the coding (overall percentage agreement: 80-87%; ACI-statistic: 0.73 – 0.82) (Gwet, 1991). For the study proper, each abstract was rated independently and in duplicate. Disagreements were resolved by discussion, and if no consensus was reached, via adjudication by a third independent reviewer.
D. Data collection
1) Study design
We classified abstracts into 2 broad categories based upon the “research compass” framework proposed by Ringsted et al. (2011): (1) Experimental, defined as any study in which researchers manipulated a variable (also known as the treatment, intervention or independent variable) to evaluate its impact on other (dependent) variables, including evaluation studies with experimental designs (Fraenkel & Wallen, 2003); and (2) Non-experimental, defined as all other studies that do not meet criteria for (1). Studies using mixed methods (for instance, an experimental design with a qualitative component) were classified according to the methodology that was deemed to be predominant.
Experimental studies were further sub-classified as experimental, quasi-experimental or pre-experimental according to established hierarchies of research designs (Creswell, 2013). We defined experimental studies by the presence of randomization; examples included factorial design, crossover design and randomized controlled trials. In contrast, for quasi-experimental studies, experimental and control groups were selected without random assignment of participants (Colliver & McGaghie, 2008). Pre-experimental studies, namely single group pre-post and post-only designs, did not have a control group for comparison.
Non-experimental studies were further sub-classified as descriptive, qualitative, psychometric, observational (comprising associational, case-control and cohort studies), and translational. Descriptive studies typically provide descriptions of phenomena, new initiatives or activities, such as curriculum design, instructional methods, assessment formats, and evaluation strategies (Ringsted, Hodges, & Scherpbier, 2011). Because pure descriptive study designs may not strictly qualify as research by some authorities, they are ranked by default as lowest in the hierarchy of study designs (Crites et al., 2014). Hence, when two study designs were identified within the same study with one being descriptive, we coded based upon the “higher” non-descriptive study design.
2) Research purpose
Research purpose is classified as description, justification or clarification based upon modified definitions of the Cook framework (Table 1). We further sub-classified clarification studies into whether they relate to theory, model/evidence-based practices, or hypothesis. Because the original definitions pertain only to experimental studies, several modifications were necessary in order to accommodate non-experimental studies in the integrated frameworks of Cook and Ringsted (Table 2). In the process, we were mindful to adhere to the original spirit of the definitions as far as possible. For instance, even though the original definition of justification studies merited a comparison group, we waived this requirement for good quality psychometric studies for which we deemed that there was sufficient rigor in the measures of validity and reliability to answer the question “Does this assessment tool work?” This was motivated by the intention to not “penalize” these studies and spuriously inflate the proportion of description studies in this category. Many validation studies of assessment tools often involve a single group design to determine whether a tool works via implicit comparison with an unknown ‘good enough’ criterion. The dominance of the psychometric views on assessment would also mean that many assessment studies are unlikely to have included an explicit statement of the underlying theoretical (Classical Test Theory, G-theory or Item Response Theory) framework.
Similarly, prompted by the observation that certain categories of approaches would be incongruent with a justification design, such as qualitative and observational studies, we delinked where appropriate the hierarchy of purpose from description to justification. Thus, a well-conducted observational study underpinned by a conceptual framework that explains the relationship between independent and dependent variables, would still qualify as a clarification study. Lastly, in response to difficulties encountered in coding during the pilot phase, we further modified the definition of clarification studies to specify the presence of a conceptual framework that fulfilled 3 crucial elements: 1) A theory, model, or hypothesis that asks “Why or how does it work?” 2) Transferability to new settings and future research; and 3) Confirmed or refuted by the results and/or conclusions of the study.
| A) Description | Describes what was done or presents a new conceptual model. Asks: “What was done?” There is no comparison group. May be a description without assessment of outcomes, or a “single-shot case study” (single-group, post-test only experiment). |
| B) Justification | Makes comparison with another intervention with intent of showing that 1 intervention is better than (or as good as) another. Asks: “Did it work?” (Did the intervention achieve the intended outcome?). Any experimental study with a control group or single-group with pre-post intervention assessment would qualify. Good quality psychometric studies with measures of validity and reliability are exempt from the need for a comparison group, since justification that the tool “works” typically does not involve a comparison group in these studies. Justification studies generally lack a conceptual framework or model that can be confirmed or refuted based on results of the study. |
| C) Clarification | Clarifies the processes that underlie observed effects. Asks: “Why or how did it work?” Often a controlled experiment, but could also use a case–control, cohort or cross-sectional research design. Much qualitative research also falls into this category. Its hallmark is the presence of a conceptual framework that can be transferable to new settings and future research, and which can be confirmed or refuted by the results and/or conclusions of the study. Further sub-classified into whether the conceptual framework pertains to a theory, model/evidence-based practice, or hypothesis. |
Table 1: Definitions of research purposes (modified from Cook et al.5)
| Study Design* | Descriptive | Justification | Clarification |
| (I) Experimental | |||
| – Experimental | Ö | Ö | Ö |
| – Quasi-experimental | Ö | Ö (no randomization) | Ö |
| – Pre-experimental | Ö | Ö (pre-post only) | Ö |
| (II) Non-experimental | |||
| (1) Explorative | |||
| – Descriptive | Ö | X | +/- |
| – Qualitative | Ö | X | Ö |
| – Psychometric | Ö | Ö (validity, reliability) | Ö |
| (2) Observation | |||
| – Associative | Ö | X | Ö |
| – Case control | Ö | X | Ö |
| – Cohort | Ö | X | Ö |
| (3) Translational | |||
| – Knowledge creation | |||
| Narrative | Ö | +/- | X |
| Quantitative review | Ö | Ö | +/- |
| Realist review | Ö | Ö | Ö |
| – Implementation | Ö | Ö | Ö |
| – Efficiency | Ö | Ö | Ö |
Table 2: Conceptual framework for possible classifications of research purpose when analyzed by research approach
*Modified from: Ringsted, C., Hodges, B., & Scherpbier, A. (2011). Medical Teacher, 33(9), 695-709.
3) Other variables
We extracted data on other variables which may affect the quality of medical education research. These included presentation category, topic of medical education addressed, professional group being studied, country of the study population, number of institutions involved, Kirkpatrick’s learner outcomes (if applicable), and statement of study intent. We measured learner outcomes on 4 levels based upon Kirkpatrick’s expanded outcomes typology, namely learner reactions (level 1), modification of attitudes/perceptions (level 2a), modification of knowledge/skills (level 2b), behavioural change (level 3), change in organizational practice (level 4a) and benefits to patients or healthcare outcome (level 4b) (Kirkpatrick, 1967; Reeves, Boet, Zierler, & Kitto, 2015). If a study reported more than one outcome, the rating for the highest-level outcome was recorded, regardless of whether this was a primary or secondary outcome. Although the validity of `hierarchical application of Kirkpatrick’s levels as a standard critical appraisal tool has been questioned, it still remains widely used in assessing the impact of interventions in medical education (Yardley & Donan, 2012). The research question is arguably the most important part of any scholarly activity and is framed as a statement of study intent often in the form of a purpose, objective, goal, aim or hypothesis (Cook et al., 2008b). We therefore collected data on whether there is an explicit statement of study intent, and if present, its quality as judged by correct location in the aims section; representation of study goals as opposed to mere stating of educational objectives; and completeness of information (i.e. whether any important objective was omitted).
E. Data Analysis
Results were summarized using descriptive statistics. Preplanned subgroup analyses were conducted with Chi-square test or Fischer’s exact test using research purpose (description, justification or clarification) as the dependent variable. Significant variables from bivariate analysis (P<.10) were included in logistic regression analysis to ascertain which of these factors were associated with a clarification study purpose. All analyses were performed using SPSS for Windows version 17.0 (SPSS Inc, Chicago, Illinois, USA). Statistical tests were two-tailed and conducted at 5% level of significance.
III. RESULTS
A. Abstract characteristics
Our sample of 186 original research abstracts comprised 38 (20.4%) oral communications, 20 (10.8%) best posters, and 128 (68.8%) poster presentations. All abstracts employed the AMRaC (Aims, Methods, Results and Conclusion) format, with the exception of two unstructured abstracts that were presented in the symposiums. The most common topics covered were in the areas of curriculum (N=54, 29.0%), teaching and learning (N=53, 28.5%), assessment (N=19, 10.2%), and e-learning (N=14, 7.5%). Besides Singapore (N=62, 33.3%), there was a good mix of abstracts from other countries in the South-East Asian region such as Malaysia, Indonesia, Thailand, Philippines and Myanmar (N=19, 10.2%), and other parts of Asia (N=88, 47.3%). Most of the studies involved a single institution (N=169, 90.9%). Kirkpatrick’s learner outcomes were applicable in approximately half (N=94, 50.5%) of the abstracts, with level one (satisfaction, attitudes and opinions of the learners) accounting for 50 (53.2%) of eligible outcomes, followed by knowledge/skills (N=32, 34.0%). An explicit statement of study intent was absent in 29 (15.6%) of abstracts. Among the remaining abstracts with an aims statement, 8 (4.3%) were incorrectly sited in the methods sections, 20 (10.8%) stated educational objectives instead of study goals, and 10 (5.4%) were incomplete.
B. Prevalence of research purpose (Table 3)
Description research purpose was the most common (N=122, 65.6%), followed by justification (N=40, 21.5%) and clarification (N=24, 12.9%). The majority of clarification studies pertain to models (N=20, 83.3%), with the reminder involving theory (N=3, 12.5%) or hypothesis (N=1, 4.2%). The prevalence of clarification studies was higher in non-experimental (N=17, 18.3%) compared with experimental (N=7, 7.5%) studies. Conversely, for justification studies, the prevalence is higher for experimental (N=36, 38.7%) compared with non-experimental (N=4, 4.3%) studies.
| Study | N | Nature of abstracts | Descriptive N(%) | Justification N(%) | Clarification N(%) |
| Lim et al, 2016 | 186 | APMEC 2012 conference abstracts, not limited to particular study type | 122 (65.6) | 40 (21.5) | 24 (12.9)* |
| Experimental | 93 | 50 (53.8) | 36 (38.7) | 7 (7.5) | |
| Non-experimental | 93 | 72 (77.4) | 4 (4.3) | 17 (18.3) | |
| Schmidt, 2005 | 850 | Studies on problem-based learning, not limited to particular study type | 543 (63.9) | 248 (29.2) | 59 (6.9) |
| Cook et al, 2008 | 105 | Experimental studies from 6 major journals published in 2003-4 | 17 (16.2) | 75 (71.4) | 13 (12.4) |
| Garcia-Duran et al, 2011 | 265 | UNAM 2008 and 2010 conference abstracts, not limited to particular study type | 246 (92.8) | 18 (6.8) | 1 (0.4) |
APMEC: Asia-Pacific Medical Education Conference; UNAM: Universidad Nacional Autónoma de México
*Comprises 83.3% Models, 12.5% theory and 4.2% hypothesis.
Table 3. Comparison of research purpose among various studies
C. Relationship of variables with research purpose (Table 4)
There was no significant association between research purpose with research category, professional group, country of study, and number of institutions (Table 4). Learner outcomes of Kirkpatrick’s level 2 and above were more likely to have a justification or clarification research purpose (c2 [4, N=186] = 67.12, p<.001), as were studies with a clear statement of study objectives (c2 [2, N=186] = 10.51, p=.005). Experimental studies were less likely than non-experimental to involve a description purpose (c2 [2, N=186] = 29.26, p=<.001) even though the frequency of clarification studies was comparatively lower (7.5% vs 18.3%). Non-descriptive studies were more likely to have a justification or clarification purpose (c2 [2, N=186] = 71.70, p=<.001).
D. Logistic Regression (Table 5)
We included in the model three independent variables (statement of study intent, Kirkpatrick’s outcome levels and descriptive research approach) which were significant in bivariate analysis. Experimental design was not included due to multicollinearity resulting from high correlation with Kirkpatrick’s levels. The Hosmer-Lemeshow test was non-significant (c2 [5, N=186] = 1.78, p=.881), indicating goodness of fit of the final model. The presence of a clear study aim [Odds ratio (95% CI) = 5.33(1.17 – 24.38)] and non-descriptive research approach [Odds ratio (95% CI) = 4.70(1.50 – 14.71)] but not higher Kirkpatrick’s outcome levels, independently predicted a clarification research purpose.
| Characteristic | Description N (%) | Justification N (%) | Clarification N (%) | P |
| Study category | .765 | |||
| Poster | 88 (68.8) | 25 (19.5) | 15 (11.7) | |
| Best Poster | 12 (60.0) | 5 (25.0) | 3 (15.0) | |
| Orals | 22 (57.9) | 10 (26.3) | 6 (15.8) | |
| Professional Group | .143 | |||
| Postgraduate Medical | 35 (74.5) | 9 (19.1) | 3 (6.4) | |
| Undergraduate Medical, Clinical | 49 (62.0) | 18 (22.8) | 12 (15.2) | |
| Undergraduate Medical, Basic Science | 20 (64.5) | 8 (25.8) | 3 (9.7) | |
| Nursing | 7 (53.8) | 1 (7.7) | 5 (38.5) | |
| Allied Health | 2 (40.0) | 2 (40.0) | 1 (20.0) | |
| Country of study | .492 | |||
| Singapore | 39 (62.9) | 16 (25.8) | 7 (11.3) | |
| South-East Asia, excluding Singapore | 11 (57.9) | 6 (31.6) | 2 (10.5) | |
| Asia, excluding South-East Asia | 61 (69.3) | 14 (15.9) | 13 (14.8) | |
| Europe | 4 (44.4) | 4 (44.4) | 1 (11.1) | |
| North America | 3 (100) | 0 (0) | 0 (0) | |
| Number of institutions studied | .857 | |||
| 1 | 111 (65.7) | 37 (21.9) | 21 (12.4) | |
| 2 | 4 (57.1) | 2 (28.6) | 1 (14.3) | |
| >2 | 7 (70.0) | 1 (10.0) | 2 (20.0) | |
| Kirkpatrick’s learner outcomes | <.001 | |||
| Not applicable | 73 (79.3) | 5 (5.4) | 14 (15.2) | |
| Kirkpatrick’s level 1 | 40 (80.0) | 7 (14.0) | 3 (6.0) | |
| Kirkpatrick’s level 2 and above | 9 (20.5) | 28 (63.6) | 7 (15.9) | |
| Aims statement | .005 | |||
| Absent or unclear | 52 (77.6) | 13 (19.4) | 2 (3.0) | |
| Present, clear aims | 70 (58.8) | 27 (22.7) | 22 (18.5) | |
| Experimental study | <.001 | |||
| Yes | 50 (53.8) | 36 (38.7) | 7 (7.5) | |
| No | 72 (77.4) | 4 (4.3) | 17 (18.3) | |
| Descriptive study | <.001 | |||
| Yes | 94 (92.2) | 3 (2.9) | 5 (4.9) | |
| No | 28 (33.3) | 37 (44.0) | 19 (22.6) |
Table 4. Relationship of variables with research purpose
| b | S.E. | Wald | P | Odds ratio (95% CI) | |
| Clear study aims | 1.67 | .78 | 4.66 | .031* | 5.33
(1.17 – 24.38) |
| No outcomes^ | -.17 | .73 | .06 | .815 | 1.19
(0.29 – 4.94) |
| K2 outcomes and above^ | -.10 | .82 | .02 | .900 | 0.90
(0.18 – 4.52) |
| Non-Descriptive study | 1.55 | .58 | 7.09 | .008** | 4.70
(1.50 – 14.71) |
Table 5. Logistic regression predicting likelihood of clarification research purpose
*P < .05; **P < .01
^Reference group: Kirkpatrick level one outcomes
Nagelkerke R square: 0.197
IV. DISCUSSION
The seminal study by Cook et al. (2008a) ushered in a series of studies that examined research quality through the lenses of research purpose. The underlying premise is that situating the research question and the accompanying study design, methods and analysis within a strong conceptual framework, facilitates the conduct of quality research that transcends the local context, allows transferability of findings, and can lead to new programmes of research (Bordage, 2009; Gill & Griffin, 2009; Beran, Kaba, Caird, & McLaughlin, 2014). By integrating the frameworks of Cook and Ringsted, this systematic review of APMEC 2012 original research abstracts contributes to this conversational turn by extending the Cook framework to include non- experimental studies. The strengths of our study include duplicate review at all stages; standardized definitions of coding categories; clear and detailed description of the methods/procedures involved; and high inter-rater reliability among the coders.
The distribution of research purpose in our study is broadly in line with earlier studies. Only around one-eighth of original research studies have a clarification research purpose. Around two-thirds of studies focused on “What was done?” description purposes which are not readily transferable beyond the immediate context of the individual study. Nonetheless, the relatively higher proportion of clarification purpose in our cohort vis-à-vis the 0.4-12.0% reported in earlier studies (Schmidt, 2005; Cook et al., 2008a; García-Durán et al., 2011) is reassuring (Table 3). Similar to Cook et al. (2008a), experimental studies account for the majority of justification studies. This is unsurprising, given the inherent nature of experimental studies in answering “Does it work?” question. Conversely, because research approaches such as qualitative and observational studies tend to ask “Why?” or “How?” questions, non-experimental designs have a higher proportion of clarification purpose compared with experimental studies (18.3% vs. 7.5%). To promote the further development of medical education scholarship in the Asia-Pacific region, we propose tapping upon regional initiatives like the Asia Pacific Medical Education Network (APME-Net), the Asian Medical Education Association, as well as regional journals such as The Asia-Pacific Scholar, to emphasize clarification studies that promote the wider application of theory which can be affirmed or refuted by the study results.
Our study also highlighted that a non-descriptive study design, in concert with a clear statement of study aims, each predicted a 5-fold increased odds of a clarification research purpose. Similar to developments in outcomes-based research within the field, we advocate a “design-balanced” approach whereby the best study design is one that best answers the research question within a given context (Lim, 2013). While descriptive study designs retain a role in the sharing of innovations and preliminary ideas, we should encourage the greater use of more rigorous non-descriptive study designs where appropriate (Ringsted et al., 2011). For experimental studies, quasi-experimental designs with a control group and true experimental designs characterized by randomization are less likely to overestimate effect size compared with single group pre-/post-test studies (Cook, Levinson, & Garside, 2011). In non-experimental studies, the plurality of non-descriptive approaches includes qualitative, psychometric, observational and translational research designs (Cheong et al., 2015; Ong et al., 2016).
Given the fundamental importance of the research question, it is disconcerting that around one-sixth of abstracts lack an explicit objective statement of study aims, whilst another one-fifth have an aims statement that is either incorrectly sited, confused with educational objectives, or incomplete. This may be indicative of poor reporting quality, or more ominously, the lack of a clear research question underpinning the research study (Cook, 2016). A systematic review that evaluates the quality of abstracts of 110 experimental studies reported that essential elements of an informative abstract were often under-reported, especially in unstructured abstracts (Cook et al., 2007b). There is evidence that structured formats improve the quality of reporting of research abstracts (Taddio et al., 1994; Wong et al., 2005; Cook et al., 2007a). Reporting quality is positively associated with superior methodological quality (Cook et al., 2011), which in turn is associated with funding for medical education research (Reed et al., 2007). There is thus a case to be made for the consistent use of structured abstracts with relevant and thoughtful headings beyond the IMRaD (Introduction, Methods, Results and Discussion) format. Where relevant, separate headings for background and aims would neatly cater to the need for both literature review plus an explicit statement of study objectives. In addition, we propose a separate heading for conceptual framework or study hypothesis to spur the development of higher-order clarification studies, and a “limitations” heading to prompt researchers to think about more rigorous study designs and outcomes through consideration of the limitations of their current research (Cook et al., 2007b).
Some limitations are worth highlighting. Our research is based upon conference abstracts, which has a significant word constraint as compared to full-length papers. The validity of our findings is highly dependent on the reporting quality of the abstracts, such that the quality of a research (as judged by research purpose and approach) may be more a reflection of the reporting quality rather than the actual quality of research. Notwithstanding, evidence affirming the positive relationship between reporting and methodological quality lends credence to the validity of assessing conference abstracts as an indirect quality indicator of research (Cook et al., 2011). Moreover, our research involved fairly objective and essential elements of reporting such as study aims and outcomes. Secondly, we choose to focus on specific aspects of quality rather than a more comprehensive evaluation of methodological quality using validated scales such as the medical education research study quality instrument (MERSQI) (Reed et al., 2007). Our approach is compatible with the ongoing debate about what constitutes quality in medical education research, which highlights the pre-eminence of the conceptual framework in framing meaningful research questions that can advance the field (Eva, 2009; Monrouxe & Rees, 2009).
V. CONCLUSIONS
Taken together, our study identified gaps that will, hopefully, serve to promote further discourse among medical education scholars in the region about the purpose and approach of their research inquiry. To advance the research agenda of the Asia-Pacific region, we should tap upon regional platforms to promote clarification studies that employ more rigorous research approaches beyond cross-sectional descriptive study designs. The thoughtful use of structured abstracts to facilitate ancillary factors such as a clear aims statement that makes explicit the underlying conceptual framework, and study design, can also pave the way towards addressing gaps in research purpose and approach.
Notes on Contributor
W. S. Lim planned and executed the study, performed statistical analysis, and wrote the manuscript. K. M. Tham, F. B. Adzahar, H. Y. Neo, and W. C. Wong contributed to acquisition of data. C. Ringsted contributed to the conception and design of the study. All authors were involved in the critical revision of the paper and approved the final manuscript for publication.
Acknowledgements
The study was supported by an educational research grant from the National Healthcare Group Health Outcomes and Medical Education Research office.
Declaration of Interest
All authors have no potential conflicts of interest.
References
Albert, M., Hodges, B., & Regehr, G. (2007). Research in Medical Education: Balancing Service and Science. Advances in Health Sciences Education, 12(1), 103-115.
Baernstein, A., Liss, H. K., Carney, P. A., & Elmore, J. G. (2007). Trends in study methods used in undergraduate medical education research, 1969-2007. JAMA, 298(9), 1038-1045.
Beran, T. N., Kaba, A., Caird, J., & McLaughlin, K. (2014). The good and bad of group conformity: a call for a new programme of research in medical education. Medical Education, 48(9), 851-859.
Bordage, G. (2009). Conceptual frameworks to illuminate and magnify. Medical Education, 43(4), 312-319.
Bunniss, S., & Kelly, D. R. (2010). Research paradigms in medical education research. Medical Education, 44(4), 358-366.
Cheong, C.Y., Merchant, R.A., Ngiam, N.S.P. & Lim, W.S. (2015). Case-based simulated patient sessions in Mental-State Examination teaching. Med Education, 49(11), 1147-8.
Colliver, J. A., & McGaghie, W. C. (2008). The reputation of medical education research: quasi-experimentation and unresolved threats to validity. Teaching and Learning in Medicine, 20(2), 101-103.
Cook, D. A., Beckman, T. J., & Bordage, G. (2007a). Quality of reporting of experimental studies in medical education: a systematic review. Medical Education, 41(8), 737-745.
Cook, D. A., Beckman, T. J., & Bordage, G. (2007b). A systematic review of titles and abstracts of experimental studies in medical education: Many informative elements missing. Medical Education, 41(11), 1074-1081.
Cook, D. A., Bordage, G., & Schmidt, H. G. (2008a). Description, justification and clarification: a framework for classifying the purposes of research in medical education. Medical Education, 42(2), 128-133.
Cook, D. A., Bowen, J. L., Gerrity, M. S., Kalet, A. L., Kogan, J. R., Spickard, A., & Wayne, D. B. (2008b). Proposed standards for medical education submissions to the Journal of General Internal Medicine. Journal of General Internal Medicine, 23(7), 908-913.
Cook, D. A., Levinson, A. J., & Garside, S. (2011). Method and reporting quality in health professions education research: a systematic review. Medical Education, 45(3), 227-238.
Cook, D. A. (2016). Tips for a great review article: crossing methodological boundaries. Medical Education, 50(4), 384-387.
Creswell, J. W. (2013). Research design: Qualitative, quantitative, and mixed methods approaches. Sage publications.
Crites, G. E., Gaines, J. K., Cottrell, S., Kalishman, S., Gusic, M., Mavis, B., & Durning, S. J. (2014). Medical education scholarship: An introductory guide: AMEE Guide No. 89. Medical Teacher, 36(8), 657-674.
Eva, K. W., & Lingard, L. (2008). What’s next? A guiding question for educators engaged in educational research. Medical Education, 42(8), 752-754.
Eva, K. W. (2009). Broadening the debate about quality in medical education research. Medical education, 43(4), 294-296.
Fraenkel, J.R., & Wallen, N.E. (2003). How to design and evaluate research in education. New York: NY: McGraw-Hill.
García-Durán, R., Morales-López, S., Durante-Montiel, I., Jiménez, M., & Sánchez-Mendiola, M. (2011). Type of research papers in medical education meetings in Mexico: an observational study. Paper presented at the Annual Meeting of the Association for Medical Education in Europe, Vienna, Austria.
Gibbs, T., Durning, S., & Van Der Vleuten, C. (2011). Theories in medical education: Towards creating a union between educational practice and research traditions. Medical teacher, 33(3), 183-187.
Gill, D., & Griffin, A. E. (2009). Reframing medical education research: let’s make the publishable meaningful and the meaningful publishable. Medical Education, 43(10), 933-935.
Gruppen, L.D. (2007). Improving medical education research. Teaching and learning in medicine, 19(4), 331-335.
Gwee, M. C., Samarasekera, D. D., & Chong, Y. (2012). APMEC 2013: In Celebration of Innovation and Scholarship in Medical and Health Professional Education. Medical Education, 46(s2), iii-iii.
Gwet, K. (1991). Handbook of Inter-Rater Reliability. STATAXIS Publishing Company.
Hodges, B. (2013). Assessment in the post-psychometric era: Learning to love the subjective and collective. Medical Teacher, 35(7), 564-568.
Kirkpatrick, D.L. (1967). Evaluation of training. In Training and development handbook, edited by R. L. Craig and L. R. Bittel. New York: McGraw-Hill. Pp. 87-112.
Lim, W. S. (2013). More About the Focus on Outcomes Research in Medical Education. Academic Medicine, 88(8), 1052.
Monrouxe, L.V., & Rees, C. E. (2009). Picking up the gauntlet: constructing medical education as a social science. Medical Education, 43(3), 196-198.
Ong, Y.H., Lim, I., Tan, K.T., Chan, M. & Lim, W.S. (2016). Assessing Shared Leadership in Interprofessional Team Meetings: A Validation Study. The Asia Pacific Scholar, 1(1), 10-21.
Reed, D. A., Cook, D.A., Beckman, T. J., Levine, R. B., Kern, D. E., & Wright, S. M. (2007). Association between funding and quality of published medical education research. JAMA, 298(9), 1002-1009.
Reed, D. A., Beckman, T. J., Wright, S. M., Levine, R. B., Kern, D. E., & Cook, D. A. (2008). Predictive validity evidence for medical education research study quality instrument scores: quality of submissions to JGIM’s Medical Education Special Issue. Journal of General Internal Medicine, 23(7), 903-907.
Rees, C. E., & Monrouxe, L. V. (2010). Theory in medical education research: how do we get there?. Medical Education, 44(4), 334-339.
Ringsted, C., Hodges, B., & Scherpbier, A. (2011). ‘The research compass’: An introduction to research in medical education: AMEE Guide No. 56. Medical Teacher, 33(9), 695-709.
Reeves, S., Boet, S., Zierler, B., & Kitto, S. (2015). Interprofessional Education and Practice Guide No. 3: Evaluating interprofessional education. Journal of interprofessional care, 29(4), 305-312. https://doi.org/10.3109/13561820.2014.1003637.
Schmidt, H.G. (2005). Influence of research in practices in medical education: the case of problem-based learning. Paper presented at the Annual Meeting of the Association for Medical Education in Europe, Amsterdam, The Netherlands.
Shea, J. A., Arnold, L., & Mann, K. V. (2004). A RIME perspective on the quality and relevance of current and future medical education research. Academic Medicine, 79(10), 931-938.
Taddio, A., Pain, T., Fassos, F. F., Boon, H., Ilersich, A. L., & Einarson, T. R. (1994). Quality of nonstructured and structured abstracts of original research articles in the British Medical Journal, the Canadian Medical Association Journal and the Journal of the American Medical Association. CMAJ: Canadian Medical Association Journal, 150(10), 1611.
Todres, M., Stephenson, A., & Jones, R. (2007). Medical education research remains the poor relation. BMJ: British Medical Journal, 335(7615), 333.
Wong, G. (2016). Literature reviews in the health professions: It’s all about the theory. Medical education, 50(4), 380-382.
Wong, H. L., Truong, D., Mahamed, A., Davidian, C., Rana, Z., & Einarson, T. R. (2005). Quality of structured abstracts of original research articles in the British Medical Journal, the Canadian Medical Association Journal and the Journal of the American Medical Association: a 10-year follow-up study. Current Medical Research and Opinion®, 21(4), 467-473.
Yardley, S., & Dornan, T. (2012). Kirkpatrick’s levels and education ‘evidence’. Medical Education, 46(1), 97-106.
*Wee Shiong Lim
Department of Geriatric Medicine
Tan Tock Seng Hospital
11 Jalan Tan Tock Seng, TTSH Annex 2, Level 3
Singapore 308433
Tel: +65 6359 6474
Email: Wee_Shiong_Lim@ttsh.com.sg
Published online: 5 September, TAPS 2017, 2(3), 15-21
DOI: https://doi.org/10.29060/TAPS.2017-2-3/OA1034
Eng-Tat Ang1, Siti Nabihah Binte Abu Talib1, Mark Thong2 & Tze Choong Charn2
1Department of Anatomy, Yong Loo Lin School of Medicine, National University Health System, Singapore; 2Department of Otolaryngology, Sengkang Hospital, Singhealth, Singapore
Abstract
Videos when properly embedded within the curriculum might make learning the basic sciences such as human anatomy much more engaging for medical students. It is unclear how the use of video is advantageous. Possible scientific causations for such an observation include visual and auditory stimulation, coupled with ease of access for the learner. Video usage empowers the medical students to learn in an active manner. However, this cannot happen if motivation for self-directed learning is lacking. This research aims to 1) Elucidate qualitative and quantitative comments on how videos help to enhance anatomy learning. 2) Quantify the level of motivation for self-directedness in order for videos to be impactful amongst medical students. A short video was embedded into selected part of the 1st year anatomy curriculums (pharynx and larynx) for selected medical students (n=100). Separately, all students in the cohort (n=300) were assessed for their attitude towards active learning via a survey on motivation levels. This was done using the modified PRO-SDLS. Results showed that 85% of the participants enjoyed learning the anatomy of the pharynx and larynx with embedded videos (P<0.05). Specifically, they liked the Q&A sessions, the virtual chat platform, and the mode of delivery. Participants perceive it to be clearer, and more structured (P<0.05). Concomitantly, all medical students surveyed exhibited unusually high motivation for self-directed learning (³ agreeing with probe questions in the PRO-SDLS) (P<0.05). This allows videos to be impactful. In conclusion, with videos, medical students appreciated the relevance of basic regional anatomy more in a statistically significant manner compared to controls. However, a threshold motivation is required for active learning to be successful.
Keywords: Video; ENT Anatomy; Feedback; Medical Education
Practice Highlights
- Medical students are generally an intrinsically self-driven group so didactic lectures may not be the optimal way to teach them.
- An appropriate short video embedded in the curriculum will trigger active learning amongst medical students.
- A certain threshold for Self-directedness (motivation) must be present for videos to be impactful.
I. INTRODUCTION
The use of video is fast becoming popular within medical education (Baldwin et al., 2016; Dong & Goh, 2015). In the larger scheme of academic medicine, the advent of media such as YouTube and Dailymotion coupled with ease of access to electronic gadgets and the internet is threatening the traditional way of learning (Egle, Smeenge, Kassem, & Mittal, 2015; Hansen et al., 2016; Pusz & Brietzke, 2012). Furthermore, expectations of millennial medical students, and the teaching-learning environments in general, are slowly but surely evolving (Lim & Seet, 2008; Youm & Wiechmann, 2015). More importantly, the learning and resource gathering habits of medical students and residents are also changing, as they depend increasingly on audio-visuals to score better in examinations (Ahmad, Sleiman, Thomas, Kashani, & Ditmyer, 2016). Specifically in the context of anatomy education, millennials often resort to YouTube videos to further enhance their learning (Barry et al., 2016). Taken together, medical education as we once know is under considerable pressure to change. In the face of these developments, teachers need to adopt newer teaching-learning techniques and delivery methods. One such modality is the usage of videos. So what does it take to make this endeavour really successful? The scientific basis for this observation is unclear. It could be the result of an array of factors but was recently explained using the science of learning (Mayer, 2010). All things considered, it is crucial that faculty members reinvent themselves to stay on top of the challenges, and to customise their institution´s curriculum to match and complement student´s needs. This will ensure accurate and proper dissemination of relevant knowledge, as well as scholarly information (Egle et al., 2015; Pusz & Brietzke, 2012; Volsky, Baldassari, Mushti, & Derkay, 2012). Traditionally, at the Yong Loo Lin School of Medicine (YLLSoM), National University of Singapore (NUS), medical students have learnt human anatomy from a well-wrought system of lectures, practical classes and small group tutorials (Ang et al., 2012). In recent times, due to curricular reforms, lecture times are proposed to be shortened, and in place of it, more interactive sessions. One initiative is the use of videos to trigger active learning, leaving more time for interactions, questions and answers (Q&A), and for reflections. A quick literature review shows that the use of multimedia (videos) to achieve such aims has been attempted in other parts of the world, with fairly convincing outcomes (Catling, Williams, & Baker, 2014; Soh, Reed, Poulos, & Brennan, 2013). These include drug prescriptions, detecting radiological lesions, and in general pathology education (Thakore & McMahon, 2006). We hope to emulate this pedagogy to teach medical students basic anatomy of the ear, nose, and throat (ENT) in a clinically-orientated manner at this institution. We believe this endeavour will help medical students in their anatomy education, and to help teachers understand the values of videos, and to further encourage buy-ins from key stake holders (Calaman et al., 2016; Choi-Lundberg, Low, Patman, Turner, & Sinha, 2016). We hypothesize that students will enjoy learning from videos in class, and its success hinges on having a high level of self-directedness (motivation) in learning.
II. METHODS
The entire first year medical students cohort (M1) from the YLLSoM (n=300) was recruited for the research, and surveyed using the Personal Responsibility Orientation to Self-Direction in Learning Scale (PRO-SDLS) (Stockdale & Brockett, 2011). This is to ascertain, and assess the level of baseline self-directedness/ motivation in their daily learning. They were polled on how much they agree with a list of statements provided in the modified scale (See Appendix). The responses are categorised by a Likert scale involving 5 options – “Strongly agree”, “Agree”, “Sometimes”, “Disagree” and “Strongly disagree” (Komorita, 1963). This is to quantify the 4 domains, namely: 1) Initiatives; 2) Control; 3) Self-efficacy; 4) Motivation.
A. Participants
In the research, selected medical students from the M1 cohort (n = 100; equal number of males and females; 19-21 years old) were asked to provide qualitative and quantitative feedback with regards to videos in ENT anatomy education. As a pre-requisite, it is assumed that these students would have also already attended all lectures and practical classes pertaining to the anatomy of the pharynx and larynx.
1) Without video: All students in the cohort were educated through a system of lectures, practical classes, and tutorials based on a prescribed list of objectives outlined at the beginning of the class. The lecture was covered in a didactic manner, and the tutorials manned by different tutors (n=16) using varying techniques in engaging these students. However, there was no active learning using any prescribed videos.
2) With video: The following links were provided for these students:
(1)http://vidcast.nus.edu.sg/camtasiarelay/Pharynx_Larynx_-_20150211_183654_26.html
A video was embedded into the tutorial teaching the head and neck anatomy (Dr. Ang’s group), and students were instructed to view them before coming to class. Controls for the intervention were the rest of the cohorts. The video (~15 minutes duration), features an introduction, learning objectives, demonstrations, self-tests using plastic anatomical models, clinical anatomy via endoscopy and fluoroscopy images. After tackling the questions individually, the group received feedback, and was given the opportunity to raise questions via an electronic bulletin board. During the class, participants were further directed to other learning resources in the Internet. To consolidate the learning, students were allowed to review the videos ad libitum, interact with classmates, and post questions to their tutor via the bulletin board. Both qualitative and quantitative feedback were obtained and tabulated from the surveys and observations based on best practice (Kelley, Clark, Brown, & Sitzia, 2003; Tai & Ajjawi, 2016), and this was carried out before and at the end of the intervention. At the end of session, all participants need to fill up the post-PRO-SDLS survey.
B. Data Analysis
The PRO-SDLS data from the entire cohort was collected via SurveyMonkey® (online). Further analysis, descriptive statistics and graphs were generated using the SPSS 24 with ad hoc consultation with the faculty Biostatistician. Whenever possible, the non-parametric Mann Whitney test was carried out to test any significant difference between participants’ perception towards the use of the video versus the control. In instances when there were 2 or more categories, the ANOVA test was used. Next, the binary logistic regression model (see Fig.1) was used to estimate and further predict the amount of self-directedness (motivation) required for videos to be impactful in medical education, all in the context of ENT anatomy education. Approval for the study was granted by the NUS institutional review board (NUS IRB B-15-186).
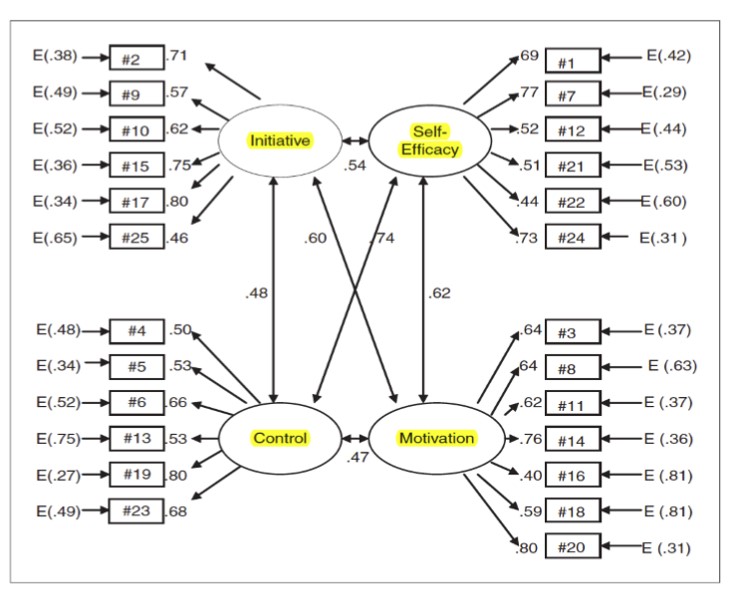 Note: Bidirectional arrows denote interrelation. E = Error. Figure 1. The PRO-SDLS allows the investigators to gauge the levels of initiative, self-efficacy, control and motivation in the participants. These domains have been proven to be important in the learning process for adults (Stockdale & Brockett, 2011).
Note: Bidirectional arrows denote interrelation. E = Error. Figure 1. The PRO-SDLS allows the investigators to gauge the levels of initiative, self-efficacy, control and motivation in the participants. These domains have been proven to be important in the learning process for adults (Stockdale & Brockett, 2011).
III. RESULTS
A. Modified PRO-SDLS survey
The online response rate for the pre-PRO-SDLS survey was a dismay 5-15% of the cohort. However, in the corresponding author’s groups, the responses were 100% for both pre- and post-PRO-SDLS respectively. The results demonstrated some statistical differences in trends across the 25 questions, and the 4 considered domains with video as an intervention. Specifically designed to measure self-directedness, the pre-modified PRO-SDLS revealed that medical students exhibited “Initiative” (≥85% responding agreed or strongly agreed), “Control” (≥80% responding agreed or strongly agreed), “Self-efficacy” (≥80% agreed or strongly agreed) and “Motivation” (≥75% agreed or strongly agreed). With regression modelling, it was further estimated that when “Initiative”, “Control” and “Self-efficacy” were increased, motivation was likely to be increased further, and hence more active learning.
1) Qualitative comments: Based on the feedback, participants like embedded videos during tutorial because it empowered them to learn at their own pace. In addition, the audio-visuals facilitated their learning. This was evidently expressed by some students when they articulated: “…We could pause and replay certain segments whenever in doubt…” and “….The images and audio aided our understanding of the subject matter…..”. Furthermore, the pre-video and post-video tests were very much appreciated by the students as it generated opportunities for discussion with peers and real opportunities to see if one has really understood the subject. This was opined by some students as follows: “ ……..The Q&A helps to make it interactive and helps to clear doubts……….” and “……….I found that the pedagogy (pre-test + video + interactive session) helped me learn the content better” and “……I was given an opportunity to participate actively in discussion with my classmates…….” Generally, students did not perceive the usage of technology as disruptive to their learning process. This was apparent when some students expressed the following: “…….the usage of “Pigeonhole” helped me to interact more effectively with the teacher……..” and “……using the “keypad” helped me learn more efficiently…….”. It appears that the embedded video in the tutorial was beneficial to the student’s learning process, and the use of technology was not getting into the way of learning as some have suggested otherwise.
2) Quantitative comments: As shown in Fig.2, when polled (A) “The video adequately helped me learn the anatomy”, participants mostly agreed (53%) or strongly agreed (31%) that it did so but some indicated disagreement (13%); (B) “Learning with video promoted more interaction”, the responses were largely positive, strongly agreed (26%) and agreed (44%) while the rest disagreed; (C) “The bulletin helped me to answer my queries”, the responses were strongly agreed (46%) and agreed (37%) while some disagreed (17%). It appears that the participants appreciated learning ENT anatomy better in this manner (all p < 0.05, ANOVA). Moreover, they mostly agreed that the mode of delivery using anatomical models was clinically relevant for their learning but this did not reach statistical significance (p > 0.05). It was also discovered that traits like “Self-efficacy” and “Control” were negatively correlated with the affinity for video learning. However, “Motivation” and “Initiative” were determined to be positively correlated with wanting to learn from videos (p < 0.05) (see Fig.3).
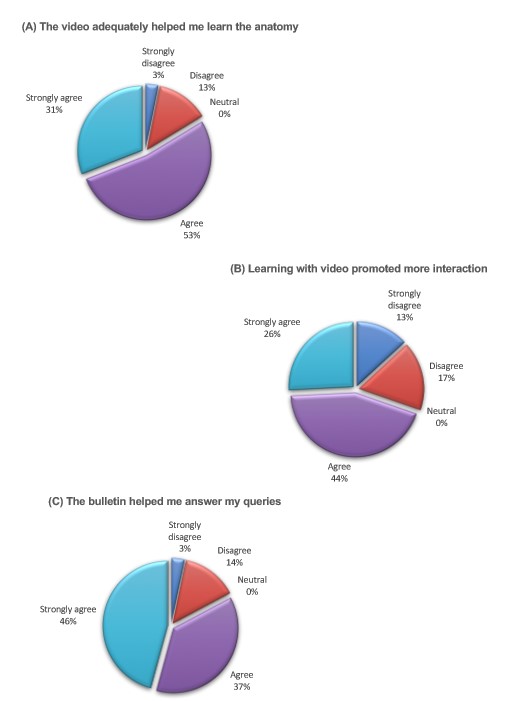
Figure 2. Quantitative results of student’s attitude towards video usage.
Pie charts illustrating the degree of agreement to: (A) The video adequately helped me learn the anatomy. (B) Learning with video promoted more interaction. (C) The bulletin helped me answer my queries.
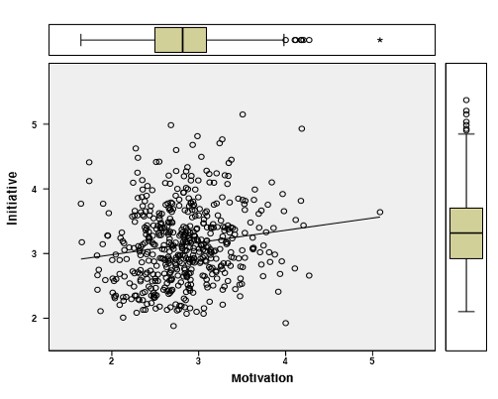
Figure 3. Regression modelling: Using other independent variables in PRO-SDLS to predict and estimate the level of dependent variable “Motivation” required to achieve active learning of ENT anatomy in medical students. “Initiative” and “Motivation” was positively correlated with wanting to learn from videos.
IV. DISCUSSION
Previous studies have described benefits associated with the blended approach of studying to a variety of subject matters, including human anatomy (Catling et al., 2014; Durham, Brettell, Summerside, & McHanwell, 2009; Pereira et al., 2007). In fact, participants in one of the research project definitively outperformed those in the traditional curriculum (Pereira et al., 2007). Specifically, videos have been shown to be just as effective, if not better than conventional histology classes (Rosenberg et al., 2006). This clearly demonstrated the ability of videos to engage students, and to inculcate active learning of the subject matter. All things considered, because of the many independent variables involved (different teachers, presentation formats, and depth of coverage), it remains a challenge to categorically say with absolute certainty, that the use of videos actually enhance the learning process. Indeed, very often, such benefits were simply students’ opinions about the use of such a modality (participants might like it but their academic performance was not improved). We gathered from this research that participants generally appreciated the video presentations for ENT anatomy education, especially the endoscopic segment (Yanagisawa, 1994), as it helped them to understand and apply the knowledge (Mayfield, Ohara, & O’Sullivan, 2013) in a clinically relevant context. Importantly, it allows participants to appreciate anatomy from an “inside” perspective. This would have been impossible in a traditional class using dissected specimens. The participants also enjoyed the opportunity to interact with their peers during, and after the session compared to a conventional class whereby interaction was lacking. Interestingly, some would like the video to be even longer, and with more details included (Egle et al., 2015). They also reported that the pre-tests and post-tests stimulated them to apply, and retain their knowledge more effectively.
To further understand how the use of videos triggered active learning, we decided to use the modified PRO-SDLS to measure the 4 critical domains in behavioural sciences. These were namely: 1) Initiatives 2) Control 3) Self-efficacy 4) Motivation. On careful analysis, there were differences between the 4 domains after the video intervention (p< 0.05). We believed that the visuals and audios inherent of the video, possibly could have enhanced self-directed drive, in a manner that is time and teacher independent (Mayer, 2010). However, it should be noted that there are still inherent controversies regarding the use of such a scale (PRO-SDLS versus other scales) to validate the many variables (Hoban, Lawson, Mazmanian, Best, & Seibel, 2005; McBride, 1987), so any strict interpretation should be avoided, bearing in mind possible caveats (Hoban et al., 2005) (e.g. subjectivity amongst interpreters). Nonetheless, we were energised by this form of blended teaching (video). In the next phase of our research, we would like to collect and analysed the academic results of participants exposed to video and compare this to the rest of the cohort.
In all honesty, there were some who resisted the use of videos in class (<5% of participants). Here, we need to understand and interpret these outliers carefully. Individual tutors conduct their classes differently, and therefore the degree of interactions varies considerably. We are aware that didactic classes have their benefits, but we opined that videos would encourage more interactions and active learning. Students enjoyed the privilege to review the contents at their own pace, with the possibility to revise pertinent sections. They also felt that the interactions with their tutor, and fellow classmates would further enhance their learning of the subject matter. In essence, it was unanimously agreed that an effective education should not be a didactic monologue, but instead a dialogue between teachers and students.
Both faculty and students are aware that technology certainly could impact their education, but it has to be done in a non-disruptive manner. For instance, all students could view the content together on the projector as a group so that there would be better synergy and dynamics. The Q&A was particularly welcomed by the participants, and helped to reinforce the key issues. Collectively, most of these comments were in line with an earlier study (Mayfield et al., 2013), presenting clinical scenarios appeared to aid students in their contextual learning so that there was less rote memorisation involved. Students appeared very receptive and excited about the application of anatomy to ENT settings.
From the tutor’s perspective, the use of technology to enhance teaching continues to be a love-hate relationship as there would be a reduction in didactic teaching time with the students. However, this could be compensated by more thought provoking interactions during the Q&A session. There was informal consensus amongst tutors (personal communication) that using new technological platform to deliver contents, involves a huge investment of time, energy, and resources. This is indeed very real for the presenter in the video, as he struggled with initial conceptualisation, work flow, and how to engage the students via this approach. While it is true that all teaching involves much deliberate planning, teaching also involves spontaneity and “thinking on the spot”. In this regard, technology and pre-recorded videos may very well inhibit this.
A) Limitations and recommendations
A significant limitation of this project is the lack of direct correlation between exposure to videos and examination outcome, hence there is no way to determine its superiority. Furthermore, one needs to be mindful that the competence of the teachers versus the rest of the colleagues teaching the cohort, should be taken into consideration. We also assume that participants in the study responded in a faithful and thoughtful manner. There were reports suggesting that students do not take surveys seriously (Slade & McConville, 2006). It will be good if future version of such videos could include the following: 1) More interactive quizzes with feedback scores and answers, 2) Case scenarios to strengthen anatomical knowledge, 3) Practice board examination questions.
On a separate note, the outreach of the internet is unquestionable but there were recent alarming reports suggesting that the information found in it may be inaccurate to varying degrees (Egle et al., 2015; Pusz & Brietzke, 2012; Volsky et al., 2012). Students and residents should therefore be more discerning when consulting the internet, during their learning of basic and clinical subjects, and patient management subsequently (Pusz & Brietzke, 2012).
B) Conclusions
We have shown there are value-adding benefits associated with embedded videos in medical teachings, and especially so in anatomy education. Medical students have expressed interest in the use of videos but one has to explore avenues to incorporate it to maximise its benefits (Chan & Robbins, 2006). In addition, we have alluded that a threshold of self-directedness, curiosity and intrinsic motivation must be present in the students in order for videos to be impactful, as pointed out by others (Oudeyer, Gottlieb, & Lopes, 2016). Faculty members should be ready to embrace modalities such as video to enhance their teaching. They should be cognisant that students’ learning behaviours have changed since their own experience some decades ago.
Notes on Contributors
Eng-Tat Ang designed the study, collected and analysed the data, and wrote the first draft of this manuscript. Siti Nabihah Binte Abu Talib contributed ideas, collected and analyzed the data. Tze Choong Charn and Mark Thong acted as clinical consultants to this project. Dr Charn provided critical multimedia files that were embedded into the videos. He also revised the manuscript and provided helpful comments. All authors approved the version submitted for review.
Acknowledgements
The authors are grateful to Mr Yeo Su Ping (CenMed, NUS), Ms Caroline (EduTech, YLLSoM) and Ms Wong Hung Chew (Biostatistician) for their input and technical assistance.
Declaration of Interest
The authors declare no conflict of interest.
References
Ahmad, M., Sleiman, N. H., Thomas, M., Kashani, N., & Ditmyer, M. M. (2016). Use of High-Definition Audiovisual Technology in a Gross Anatomy Laboratory: Effect on Dental Students’ Learning Outcomes and Satisfaction. Journal of Dental Education, 80(2), 128-132.
Ang, E. T., Sugand, K., Hartman, M., Seow, C. S., Bay, B. H., & Abrahams, P. (2012). Singapore’s anatomical future: quo vadis? Anatomical Sciences Education, 5(4), 234-240.
Baldwin, A. C., Mallidi, H. R., Baldwin, J. C., Sandoval, E., Cohn, W. E., Frazier, O. H., & Singh, S. K. (2016). Through the Looking Glass: Real-Time Video Using ‘Smart’ Technology Provides Enhanced Intraoperative Logistics. World Journal of Surgery, 40(1), 242-244.
Barry, D. S., Marzouk, F., Chulak-Oglu, K., Bennett, D., Tierney, P., & O’Keeffe, G. W. (2016). Anatomy education for the YouTube generation. Anatomical Sciences Education, 9(1), 90-96.
Calaman, S., Hepps, J. H., Bismilla, Z., Carraccio, C., Englander, R., Feraco, A., . . . Committee, I. P. S. E. E. (2016). The Creation of Standard-Setting Videos to Support Faculty Observations of Learner Performance and Entrustment Decisions. Academic Medicine, 91(2), 204-209.
Catling, F., Williams, J., & Baker, R. (2014). A prescribing e-tutorial for medical students. Clinical Teacher, 11(1), 33-37.
Chan, C. H., & Robbins, L. I. (2006). E-Learning systems: promises and pitfalls. Academic Psychiatry, 30(6), 491-497.
Choi-Lundberg, D. L., Low, T. F., Patman, P., Turner, P., & Sinha, S. N. (2016). Medical student preferences for self-directed study resources in gross anatomy. Anatomical Sciences Education, 9(2), 150-160.
Dong, C., & Goh, P. S. (2015). Twelve tips for the effective use of videos in medical education. Medical Teacher, 37(2), 140-145.
Durham, J. A., Brettell, S., Summerside, C., & McHanwell, S. (2009). Evaluation of a virtual anatomy course for clinical undergraduates. European Journal of Dental Education, 13(2), 100-109.
Egle, J. P., Smeenge, D. M., Kassem, K. M., & Mittal, V. K. (2015). The Internet School of Medicine: Use of Electronic Resources by Medical Trainees and the Reliability of those Resources. Journal of Surgical Education, 72(2), 316-320.
Hansen, C., Interrante, J. D., Ailes, E. C., Frey, M. T., Broussard, C. S., Godoshian, V. J., . . . Gilboa, S. M. (2016). Assessment of YouTube videos as a source of information on medication use in pregnancy. Pharmacoepidemiology Drug Safety, 25(1), 35-44.
Hoban, J. D., Lawson, S. R., Mazmanian, P. E., Best, A. M., & Seibel, H. R. (2005). The Self-Directed Learning Readiness Scale: a factor analysis study. Medical Education, 39(4), 370-379.
Kelley, K., Clark, B., Brown, V., & Sitzia, J. (2003). Good practice in the conduct and reporting of survey research. International Journal for Quality in Health Care, 15(3), 261-266.
Komorita, S. S. (1963). Attitude Content, Intensity, and the Neutral Point on a Likert Scale. Journal of Social Psychology, 61, 327-334.
Lim, E. C., & Seet, R. C. (2008). In-house medical education: redefining tele-education. Teaching and Learning in Medicine, 20(2), 193-195.
Mayer, R. E. (2010). Applying the science of learning to medical education. Medical Education, 44(6), 543-549.
Mayfield, C. H., Ohara, P. T., & O’Sullivan, P. S. (2013). Perceptions of a mobile technology on learning strategies in the anatomy laboratory. Anatomical Sciences Education, 6(2), 81-89.
McBride, S. (1987). Validation of an instrument to measure exercise of self-care agency. Research in Nursing & Health, 10(5), 311-316.
Oudeyer, P. Y., Gottlieb, J., & Lopes, M. (2016). Intrinsic motivation, curiosity, and learning: Theory and applications in educational technologies. Progress in Brain Research, 229, 257-284.
Pereira, J. A., Pleguezuelos, E., Meri, A., Molina-Ros, A., Molina-Tomas, M. C., & Masdeu, C. (2007). Effectiveness of using blended learning strategies for teaching and learning human anatomy. Medical Education, 41(2), 189-195.
Pusz, M. D., & Brietzke, S. E. (2012). How good is Google? The quality of otolaryngology information on the internet. Otolaryngology-Head and Neck Surgery, 147(3), 462-465.
Rosenberg, H., Kermalli, J., Freeman, E., Tenenbaum, H., Locker, D., & Cohen, H. (2006). Effectiveness of an electronic histology tutorial for first-year dental students and improvement in “normalized” test scores. Journal of Dental Education, 70(12), 1339-1345.
Slade & McConville (2006) Student Evaluation of Teaching. International Journal for Educational Integrity 2(2), 43-59
Soh, B. P., Reed, W. M., Poulos, A., & Brennan, P. C. (2013). E-tutorial improves students’ ability to detect lesions. Radiologic Technology, 85(1), 17-26.
Stockdale, S. L., & Brockett, R. G. (2011). Development of the PRO-SDLS: A Measure of Self-Direction in Learning Based on the Personal Responsibility Orientation Model. Adult Education Quarterly, 61(2), 161-180.
Tai, J., & Ajjawi, R. (2016). Undertaking and reporting qualitative research. Clinical Teacher, 13(3), 175-182.
Thakore, H., & McMahon, T. (2006). An interactive e-tutorial in pathology. Medical Education, 40(11), 1135.
Volsky, P. G., Baldassari, C. M., Mushti, S., & Derkay, C. S. (2012). Quality of Internet information in pediatric otolaryngology: a comparison of three most referenced websites. International Journal Pediatric Otorhinolaryngology, 76(9), 1312-1316.
Yanagisawa, E. (1994). The use of video in ENT endoscopy: its value in teaching. Ear Nose Throat Journal, 73(10), 754-763.
Youm, J., & Wiechmann, W. (2015). The Med AppJam: a model for an interprofessional student-centered mHealth app competition. Journal of Medical Systems, 39(3), 34.
*Dr. Eng-Tat Ang
Department of Anatomy
Yong Loo Lin School of Medicine
MD10, National University of Singapore
Singapore 117599
Tel: 65168110
Fax: 67787643
Email: antaet@nus.edu.sg
Published online: 5 September, TAPS 2017, 2(3), 8-15
DOI: https://doi.org/10.29060/TAPS.2017-2-3/OA1023
Hashmet P Ghouse, Fazean IH Idris, Zaw Wint & Tayyab Hasan
Universiti Brunei Darussalam, Brunei Darussalam
Abstract
Introduction: With the growing trend and importance towards producing holistically groomed medical graduates as discussed in Tomorrow’s Doctors, we introduced a community oriented Special Study Module 3 (SSM3) in the Year 3 undergraduate medicine program in the Institute of Health Sciences, Universiti Brunei Darussalam. This module incorporates the principles of Community Oriented Medical Education (COME) to facilitate Holistic development and Team-based learning.
Method: A descriptive cross sectional survey design using a self- designed 18 item questionnaire to explore the overall organization, benefits and skills learnt from this module, was sent to the emails of all students in the three cohorts. Questionnaire was piloted on a small group of nursing students who accomplished a community based project. Cronbach’s Alpha analysis was done to establish the reliability of survey.
Result: Questionnaire was sent to 47 students and got a 74% response rate. Most of the students found the project very interesting and useful in learning various skills and enhancing self-development. Cronbach’s Alpha of more than 0.70 suggested strong internal reliability. Discussion: Students perception strongly suggests that all the objectives of SSM3 module have been achieved. This approach facilitated multifaceted learning including leadership, teamwork, communication skills, managerial and organizational skills by working with the community members to identify and address their health risks.
Conclusion: Community oriented medical education approach can be used to enhance multifaceted learning in real life environment as small group students led projects.
Keywords: Undergraduate Medical Education; Community Oriented Medical Education; Holistic Health Professionals
Practice Highlights
- Community Oriented Medical Education (COME) approach is useful in enhancing multifaceted learning in undergraduate medical students if applied properly.
- Students value activities that let them know more about community and its health related issues.
- Students perceive that small group student led field projects are beneficial in developing teamwork, communication and organizational skills.
- Time allocated and credits awarded for modules should match with the workload and the intended impact.
- COME can be used in a wider scope such as to promote IPE, sustainable health promotion in communities, community engagement towards healthy living.
I. INTRODUCTION
In order to produce holistically groomed medical graduates as described in Tomorrow’s Doctors (General Medical Council Education Committee, 2009), medical curriculum needs to provide a teaching environment where students get the opportunity for multifaceted learning. In addition, Declaration of Alma-Ata (1978) released in International Conference on Primary Health Care identified the role of primary health care in promoting health for all, demands undergraduate medical students to be exposed to community so they can understand various non-biological determinants of health in addition to biological and therefore can contribute in preventive medicine practices as part of primary health care team. NHS also recommends increasing community oriented undergraduate medical education to increase the understanding of patients’ needs that may promote a more holistic medical practice (Habbick & Leeder, 1996; Schroeder, Zones & Showstack, 1989). Health organizations and policy makers have realized the need of moving medical education focus from the patient to the community, along with developing educational programs designed to measure and improve the health of the community (General Medical Council Education Committee, 2009; Henderson, 1989; World Health Organization, 1987).
Literature describes some instances of the use of educational approaches applied in community settings to teach social and environmental determinants of health (Davison et al., 1999; Kirk, 1994; Kisil & Chaves, 1994; Kulig & Wilde, 1996; McKnight & Van Dover, 1994).
In view of the current trends and demands of medical education in 21st century, we reviewed our modules and changed one of the Special Study Modules. During their first three years of medical education in the university, students are well supported to take three Special Study Modules (SSM) one in each year namely SSM 1, SSM 2 and SSM 3. We introduced a COMMUNITY ORIENTED multifaceted learning approach as Special Study Module 3 (SSM3), in the third year of our under-graduate medicine program. This module incorporates the principles of Community Oriented Medical Education (COME) where in addition to students, the teachers, members of the community, and representatives of other government and non-government sectors are actively involved throughout the educational process.
COME is an education which is ‘focused on population groups and individual persons taking into account the health needs of the community concerned’ (Schmidt, 1991; World Health Organization, 2011). It is different from Community-based learning activity, where learning takes place in some primary or secondary health care facility in the community. Learning activities taken place in tertiary care settings like hospitals or large scale specialized medical facilities are not considered as community-based activities (World Health Organisation, 1987). The major difference between these two approaches is that in Community-based education learning activities take place in a particular setting in the community but these activities may or may not be directly relevant to that particular community health needs (Magzoub & Schmidt, 2000).While Community oriented education refers to learning activities that have direct relevance with regard to the priority health problems of that particular community (Hamad, 1991).
This SSM 3 module is based on developing projects that requires community involvement in participating in the planning, organization, operation and control of primary health care as highlighted in Declaration of Alma-Ata (1978). The module incorporate many important concepts that already have set the trend in medical education all around the world for example,
- Holistic healthcare to cover not only the biological aspects but also the psychological, social and spiritual aspects of health and illness.
- Team-based learning and practice, Inter-professional education is gaining popularity in most of the medical education institutions and it is believed that working as a team enhances performances and patient care.
- Social Determinants of Health (SDH), World health organization (WHO) and Centres for disease control and prevention (CDC) has recognized various social determinants of health and understanding of these determinants is crucial for a holistic healthcare provider.
- Transforming ‘Theory into Practice’, according to Bloom’s taxonomy the higher levels of learning need application, analysis, synthesis and evaluation and students should be able to apply all their knowledge and learning into real life situations.
The main objectives of this module include:
- To identify health related issues associated with various social and non-biological determinants of health.
- To be able to analyse health status or a health related problem in a community.
- To plan a solution for the problems with the involvement of relevant community, government and/or non-governmental agencies
- To demonstrate leadership, teamwork and management skills
- To develop community oriented approach to healthy living and preventive medicine
The module contains a team-based, small group, student-centred approach to undertake group projects developed by students with consultation of supervisors and finally approved by SSM 3 committee.
Students are given protected time of 6 weeks in semester 1 of year 3 to complete this module. They explore available material, resources, and literature to understand the background of relevant health issues and their importance. The possible issues may be related to (though not limited to) healthy life-style, environmental pollution/hazards, and belief, culture, knowledge, attitudes and practice of community related to health. Students, as a group, implement the project in a selected community with consultation and full involvement of the community and its leaders. The health issues or problems are identified, analysed, and the group plan and carry out an appropriate intervention with the full involvement of community. At the end, students write a project report and present their experience and intervention to share what they have learnt during the project. Two assessors assessed report, presentation and the expected impact of intervention. Each project report is assessed on pre-set criteria. Marks are awarded as:
a) Group Marks (Written project report & oral Presentation) — 50% and
b) Individual Marks (Peer assessment and 2 SSM3 committee members assessment based on information from 2 community representatives) – 50%
The purpose of this survey was to assess the overall organization and benefits obtained from SSM3 module.
II. METHODS
A descriptive cross sectional survey was designed to get perception from the three cohorts of medical undergraduates, who had undergone this new module and completed it successfully, by reflecting on their experiences about the effectiveness of this student-led learning experience. Survey included a self- designed 18 item questionnaire to explore the effectiveness, benefits and overall organization of SSM3 module using a 5 point Likert scale response option from 1 = ‘Strongly disagree’ to 5 = ‘Strongly agree’. Items I to 9, 11, 15 and 18 explore the overall organization of SSM3 module while items 10, 12, 13, 14, 16 and 17 explore the perceived benefits and skills learnt. Cronbach’s Alpha analysis was done to establish internal reliability for these two sets of items. Items 19 and 20 explore any other learning experiences and suggestions to improve this module. Face and content validity was maintained by carefully selecting the questions to cover the area of interest.
Questionnaire was piloted on a small group of nursing students who accomplished a community based project to confirm the clarity of questions. It was sent via email to all students in the three cohorts including a reminder email 2 weeks later. The survey was uploaded on a free online software available in public domain and answers were collected anonymously. Students were informed about the voluntary nature of participation. Completion and submission of the form indicated their consent for participating in this survey. Ethical approval was not needed as this activity is part of routine module and course evaluation based on students’ feedback.
III. RESULTS
Questionnaire was sent to 47 students, 35 of them responded with completed surveys (74% response rate). Some students sent incomplete forms and few could not submit the survey online and sent their response in word document format. These incomplete and word format responses were not included in the analysis because of missing data and lack of anonymity which can influence the validity and reliability. For open questions, 21 responded for question 19 and 19 responded for question 20.
IBM SPSS Statistics version 21 was used to do descriptive analysis of responses in the form of frequency distribution and to establish the internal reliability by Cronbach`s Alpha analysis (Tables 1 and 2). Based on SPSS analysis, a Microsoft Excel Worksheet was created to show the summary of all results. Responses to items 1 to 18 are summarized in Table 3 as percentage distribution of responses for each item. Question 19 and 20 were analysed manually for the emerging themes and are summarised in Table 4.
Cronbach’s Alpha for the set of questions to assess overall organization of SSM3 module (Q1 – 9, 11, 15 and 18) is .974 (Table 1) and for set of questions assessing benefits and skills learnt (Q10, 12,13,14,16 and 17) .968 (Table 2). Both values are more than .70 and indicate strong internal consistency in terms of items under each set. This can be interpreted as having good internal reliability for the survey.
| Reliability Statistics | ||
| Cronbach’s Alpha | Cronbach’s Alpha Based on Standardized Items | N of Items |
| .974 | .978 | 12 |
Table 1. Reliability for overall organization of module (Q1 – 9, 11, 15 and 18)
| Reliability Statistics | ||
| Cronbach’s Alpha | Cronbach’s Alpha Based on Standardized Items | N of Items |
| .968 | .972 | 6 |
Table 2. Internal reliability for benefits and skills learnt (Q10, 12,13,14,16 and 17)
More than 90% students replied as ‘agree’ or ‘strongly agree’ for 15 out of 18 questions while for the remaining 3 questions the responses were: ‘the learning objectives for the SSM 3 COMMUNITY OUTREACH PROGRAMME projects were clear’ (87.5%), ‘the time allocated for the project was sufficient to complete it’ (76.4%) and ‘the credits earned for the project equates the time spent to complete it’ (57%).
The highest response rate for ‘strongly agree’ option include questions about team working e.g. ‘Good Team work is necessary for the project completion’ (76.4%) and ‘the project is a good tool to learn and enhance team building skills’ (76.4%).
The response ‘strongly disagree’ was selected for only one question on ‘Project ideas were solely generated by students’ (2.1%). Similarly, the response ‘disagree’ was selected for one question on ‘The credits earned for the project equates the time spent to complete it’ (10.4). This question also has the lowest agreement with a cumulative percentage for ‘agree’ and ‘strongly agree’ as 57%.
There were 4 questions where students were very decisive and didn’t select ‘neither agree nor disagree’ option e.g. ‘Good Team work is necessary for the project completion’, ‘the project is a good tool to learn and enhance team building skills’, ‘the project is a good tool to learn and enhance organizing skills’ and ‘conducting the project is a worthwhile personal experience’. In all these 4 questions the cumulative percentage for responses as ‘agree’ and ‘strongly agree’ was 100%.
For question 19, the most frequent themes emerged were communication skills (07), teamwork and managerial skills (05) and community knowledge (04). Students also mentioned about learning other skills as shown in Table 4. For question 20, majority suggested to provide more time and funding/sponsorship (07), early introduction of Module (03) and guidelines for getting funds from private organizations and sponsors (02). In addition, overseas exposure to carry out community projects and a smooth process for getting permission letters to carry out their projects were also suggested. One interesting suggestion was to focus more on studies then this type of projects.
| No. | Items | Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree |
| Theme | Organisation of the SSM3 | |||||
| Q1 | The learning objectives for the SSM 3 COMMUNITY OUTREACH PROGRAMME projects were clear. | 0 | 0 | 12.5 | 52.8 | 34.7 |
| Q2 | Project ideas were solely generated by students. | 2.1 | 0 | 4.2 | 34 | 59.7 |
| Q3 | Your supervisors provided enough good support and direction. | 0 | 0 | 6.3 | 39.6 | 54.2 |
| Q4 | Your supervisors were readily available for constructive feedback. | 0 | 0 | 8.3 | 40.3 | 51.4 |
| Q5 | The time allocated for the project was sufficient to complete it. | 0 | 0 | 23.6 | 52.1 | 24.3 |
| Q6 | The credits earned for the project equates the time spent to complete it. | 0 | 10.4 | 32.6 | 39.6 | 17.4 |
| Theme | Community awareness and personal bonding | |||||
| Q7 | This project activity is useful to the community. | 0 | 0 | 6.3 | 31.3 | 62.5 |
| Q8 | This project made you more aware of health issues in the community. | 0 | 0 | 8.3 | 40.3 | 51.4 |
| Q9 | The project is a good learning experience | 0 | 0 | 4.2 | 27.8 | 68.1 |
| Q15 | Conducting the project is a worthwhile personal experience. | 0 | 0 | 0 | 34.7 | 65.3 |
| Q18 | The project activities were enjoyable. | 0 | 0 | 4.2 | 27.8 | 68.1 |
| Theme | Benefits and skills learnt | |||||
| Q10 | The project activities enhances teamwork. | 0 | 0 | 8.3 | 20.8 | 70.8 |
| Q11 | Good teamwork is necessary for the project completion. | 0 | 0 | 0 | 23.6 | 76.4 |
| Q12 | The project is a good tool to learn and enhance team building skills. | 0 | 0 | 0 | 23.6 | 76.4 |
| Q13 | The project is a good tool to learn and enhance organizing skills. | 0 | 0 | 0 | 29.2 | 70.8 |
| Q14 | The project is a good tool to learn and enhance communication skills? | 0 | 0 | 4.2 | 25 | 70.8 |
| Q16 | The project is a good tool to learn and enhance bonding with the community? | 0 | 0 | 4.2 | 38.9 | 56.9 |
| Q17 | The project is a good tool to foster bonding with teammates. | 0 | 0 | 6.3 | 25.7 | 68.1 |
Table 3. Percentage distribution of responses
| Question No.
|
Themes emerged from open responses
|
Total responses | Top 3 themes | Total responses |
| Q19: In your own words what else did you learn from this project?
(21 responses)
|
Communication skills
Leadership skills Time management Team work Organizational skills Community knowledge Planning Critical thinking Finance management Trust Self-control Self-exploration Administration Problem solving |
7
3 3 5 5 4 2 2 2 1 1 1 1 1 |
1. Communication skills
2. Team work and Organizational skills
3. Community knowledge |
7
5
4 |
| Q20: Do you have any suggestions or comments about this project could be improved?
(19 responses)
|
More time
Funding/sponsorship Early introduction Guidelines for getting funds Overseas exposure More focus on studies than SSM3 Permission letters |
7
7 3 2 1 1 1 |
1. More Time and Funding/sponsorship
2. Early introduction
3. Guidelines for getting funds |
7
3
2 |
Table 4. Responses to open questions
IV. DISCUSSION
We would like to cite a few examples of the community projects undertaken during this six weeks module which clearly points to a student community involvement and education outcome envisaged by the COME principles in this module. One of the most impressive programmes was an outreach BREAST CANCER AWARENESS PROGRAMME. Students started with approaching the Ketua Kampong or Headman of a remote village for permission to meet the women in that village between the ages of 18-50years. They then organised a meet and greet session whereby they spoke about the prevalence of breast cancer and how Breast Self -Examination (BSE) is a simple way of screening oneself regularly. They employed the help of their classmates and ran a session on teaching BSE to the gathered women and finally ran a fun quiz to assess how much the participants remembered their take home messages. Another example was a small endeavour to help initiate a HEALTHY FOOD CHOICES IN PRIMARY SCHOOL CHILDREN. Here it was completely left to the students to obtain permission to conduct this programme, from the school Principal and the parents of these primary school children. They chose one PE session time to invite parents and children to learn and draw common local fruits and vegetables after a talk on the nutrition value of some common fruits and vegetables. The programme ended in a quiz competition for the children who were answering questions on caloric values and benefits of the local fruits and vegetables and prizes were in the form of fruits and vegetables. Students’ overall perception about SSM3 Module suggests that community oriented medical education approach can be used effectively to enhance multifaceted learning in undergraduate medical education. Results show that the overall organization of SSM3 module was well accepted by students and this module motivated them to learn about community health problems, their reasons and to develop appropriate strategies to solve these issues.
This study shows that students were clear about the learning objectives of this module (Q1) and projects were developed by students themselves (Q2), only a small fraction (2.1%) strongly disagree with this. The reason may be that in one or two groups, supervisors interfered or dictated the project to students but majority of the projects were developed by students. Results also show that supervisors` role were well acknowledged as supportive and constructive (Q3 and Q4). Students also realized the usefulness of this module and approach not only for the communities (Q7) but also for students understanding of community health issues (Q8). Results endorses the value of this approach in enhancing learning experience by students by showing 95.9% students from 3 different cohorts either strongly agree or agree to this statement (Q 9) and at the same time 100% students consider this module worthwhile personal experience (Q15) and 95.9% consider it enjoyable (Q18). This module is conducted as small group activity and 100% students agree that good teamwork is mandatory for completing this type of projects (Q11). A 6 week protected time was provided for completion of this module and project but only 76.4% students agree that it’s enough time (Q5), a significant number of students (23.6%) are not sure if this allocated time is enough to complete their projects. Considering this fact, it might be useful to modify the time allocated for this module. One option may be to offer this module throughout the semester or even over two semesters. This will provide enough time for students to explore community, identify health issues and plan and develop a good project with more efficient interventions for a bigger and long lasting impact. SSM3 module is a Pass/Fail module and adds only 1 grade point towards cGPA. Only 57% Students agree that the credit earned for the project equates the time spent to complete it (Q6), 10.4% disagree and another 32.6% are undecided if they agree or disagree. This raises the concern about re-thinking module’s grade point. One way is to convert it from pass/fail to graded module so the time and efforts spent will have more value in terms of grade points and cGPA. The reason it was not graded was concern from faculty members about the quality and reliability of assessment system. In SSM3 students are awarded marks based on group work and from that individual marks are obtained. In addition, peer assessment and assessment by supervisors also contribute to individual marks. After 3 years of assessment without any issues, this 360o nature of assessment can help in making this a graded module.
This study also highlights the perception of students in achieving multifaceted learning. Students perceived that this module helped them in learning teamwork (91.6%), developing team building skills (100%) and fostering bonding among team members (93.8%) in Q10, Q12 and Q17. In addition, 100% students agreed that they learn about organizational skills (Q13), 95.8% about communication skills (Q14) and 95.8% about learning and enhancing bonding with the community (Q16).
On exploring further regarding students’ learning experience in Q19, new scopes even beyond the objectives of SSM3 were identified by students, for example, students indicated various aspects of communication skills including written communication, communication with community leaders, governmental and non-governmental organizations. Students also mentioned acquiring effective leadership skills (03), time management, teamwork, organizational skills, community knowledge, planning, critical thinking, finance management, trust development, self-control, self-exploration, administration and problem solving skills.
Students also provided some suggestions to further improve the project success and to increase the scope of their projects in Q20. Students strongly feel that more time should be provided to complete the project and this will help them in understanding the community needs more effectively. With more time they can develop better and long lasting interventions to solve community health issues. In order to organize events and activities in communities, students need funds and currently University is not providing any funding for SSM3 projects. Students find it difficult to get sponsors or funds to organize big scale events and attract more members of the community. They strongly suggest that institution should provide some funding to support their educational projects. Some students suggested to at least provide some formal guidelines on how to approach private organizations and sponsors to support their activities. Students also suggested having early introduction of this module so they are well prepared and developing their projects before the start of SSM3 six week period for better planning and activities. Other students indicated issues related with getting permission letters from institution to carry out activities in various communities or from various agencies, they suggest to have some proper procedure to get these letters quickly so time is not wasted while just waiting for letters. One student suggested widening the scope of this project and allowing students to do community work in other countries. Another student indicated that these activities are good but students should focus more on their studies. This suggestion indicates that some students may not be clear about the need of learning various other skills important to work as a doctor in future. This issue can be addressed by more explicit description of the benefits of having this type of modules in module handbook.
Overall, the result of this survey shows that SSM3 module is well accepted by students in terms of their interest, enthusiasm, motivation and participation. Students enjoy working on their own in community with various agencies to identify health related issues. They are very keen to work together with community representatives and leaders to implement the solutions designed in solving problems in a particular community. Students also agree that this community oriented medical education approach is helpful in multifaceted learning and skill developments they need to work as a good doctor in future.
Community Oriented Medical Education (COME) approach in SSM3 module can also be extended to other health professions and may be useful in facilitating ‘Inter-Professional Education (IPE)’ concepts among undergraduate health professionals.
The limitation of this study is small number of participants and lack of focus group discussion to elaborate the benefits of this module in depth. Community and supervisors feedback may help in evaluating this module. Future studies should focus on mixed method approach with descriptive survey and qualitative exploration of issues from various stakeholders for triangulation to increase reliability.
V. CONCLUSION
Undergraduate medical students perceive Community Oriented Medical Education (COME) approach in SSM3 module as an effective method to enhance multifaceted learning in real life environment. This approach is useful in developing various skills especially teamwork, leadership, organizational, managerial and communication skills. COME also helps in enhancing knowledge and understanding about communities and their health related issues with fostering bonding with community. SSM3 type small group students led projects may be useful in developing teamwork skills at various levels.
Notes on Contributors
Ghouse H.P is General practitioner and Senior lecturer clinical academia, Coordinator of MSC PHC and Coordinator of SSM3 Programme for BHSc medicine at the PAPRSB Institute of health sciences, Brunei Darussalam. The author has also an active role in the MRCGP int exams in the university.
Idris F.I is General practitioner and Senior lecturer clinical academia, Programme Leader for the BHSc medicine programme at the PAPRSB Institute of health sciences, Brunei Darussalam. Brunei Coordinator for the MRCGP int exams in the university.
Wint Z is Director, Office of Planning and Development, Universiti Brunei Darussalam and Senior Lecturer at PAPRSB Institute of health sciences.
Hasan T. Is General practitioner and Lecturer clinical academia, Ex Programme leader for the BHSc medicine programme at the PAPRSB Institute of health sciences, Brunei Darussalam. The author has also an active role in the teaching and coordinating of the undergraduate medicine programme.
Declaration of Interest
This is an unfunded study. All authors have no potential conflicts of interest.
References
Davison, H., Capewell, S., Macnaughton, J., Murray, S., Hanlon, P., & McEwen, J. (1999). Community‐oriented medical education in Glasgow: developing a community diagnosis exercise. Medical Education, 33(1), 55-62.
Declaration of Alma-Ata (1978). International Conference on Primary Health Care, Alma-Ata, USSR, 6-12 September 1978. Retrieved from: http://www.who.int/social_determinants/tools/multimedia/alma_ata/en/
General Medical Council Education Committee (2009). Tomorrow’s Doctors. Retrieved from: http://www.gmc.uk.org/Tomorrow_s_Doctors_1214.pdf_48905759.pdf
Habbick, B. F., & Leeder, S. R. (1996). Orienting medical education to community need: A review. Medical Education, 30(3), 163-71.
Hamad, B. (1991). Community-oriented medical education: What is it? Medical Education, 25(1), 16-22.
Henderson, D. A. (1989). Defining global medical education needs. Academic Medicine, 64(5), S9-12.
Kirk G. D. (1994). Medical students, community join in Cherokee model to prevent child injury. Public Health Report, 109(2173), 4.
Kisil, M., & Chaves, M. (1994). Linking the university with the community and its health system. Medical Education, 28(5), 343-349.
Kulig, J. C., & Wilde, I. (1996). Collaboration between communities and universities completion of a community needs assessment. Public Health Nursing, 13(2), 112-119.
McKnight, J., & Van Dover, L. (1994). Community as client: a challenge for nurse education. Public Health Nursing, 11(1), 12-16.
Magzoub, M. E. M.., & Schmidt, H. G. (2000). A Taxonomy of Community-based Medical Education. Academic Medicine, 75(7), 699–707.
Schmidt, H. G., Neufeld, V. R., Nooman, Z. M., & Ogunbode, T. (1991). Network of community-oriented educational institutions for the health sciences. Academic Medicine, 66(5), 259-263.
Schroeder, S. A., Zones, J. S., & Showstack, J. A. (1989). Academic medicine as a public trust. Journal American Medical Association, 262(6), 803-812.
World Health Organisation (1987). WHO study group on Community-based Education of Health Personnel. Retrieved from http://apps.who.int/iris/handle/10665/41714
World Health Organization (2011). Innov8 approach for reviewing national health programmes to leave no one behind. Retrieved from http://www.who.int/social_determinants/en/
*Dr. Hashmet Parveen
PAPRSB Institute of Health Sciences
Universiti Brunei Darussalam
Tel: 6738818424
Email: parveenbrunei@gmail.com
Published online: 5 September, TAPS 2017, 2(3), 1-7
DOI: https://doi.org/10.29060/TAPS.2017-2-3/OA1033
Junji Haruta1, Kiyoshi Kitamura2 & Hiroshi Nishigori3
1Department of General Medicine and Primary Care, University of Tsukuba Hospital, Japan; 2International Research Center for Medical Education, Graduate School of Medicine, The University of Tokyo, Japan; 3Center for Medical Education, Kyoto University, Japan
Abstract
Lay people without a body of specialty knowledge, like the professionals, have not been able to partake in interprofessional education (IPE). Transprofessional education (TPE), which was defined as IPE with non-professionals /lay people, is an important extension of (IPE). A TPE programme was developed to explore how health professionals and lay people learn with, from and about each other in a Japanese community. The present study was conducted in a hospital and the surrounding community in Japan. An ethnographic study design was adopted, and the study participants were six lay individuals from the community and five professionals working in the community-based hospital. During the health education classes, the first author acted as a facilitator and an observer. On reviewing interview data and field notes using a thematic analysis approach, findings showed that healthcare professionals and lay participants progressed through uniprofessional and interprofessional before achieving transprofessional learning. Both type of participants became to transcend boundaries after sharing their viewpoints in a series of classes and recognized that they were important partners in their local community step by step, which increased their sense of belonging to the community. The transformation was driven by dynamic interaction of the following four factors: reflection, dialogue, reinforcement of ties, and expanding roles. We believe this process led both groups to come to feel collective efficacy and inspire healthcare professionals to reflect on their transprofessional learning. We clarified how healthcare professionals and lay people achieved transprofessional learning in a TPE programme where participants advanced through uniprofessional, interprofessional stage before achieving transprofessional learning.
Keywords: Interprofessional Education; Transprofessional Education; Ethnography; Health Education
Practice Highlights
- Healthcare professionals and lay participants became to transcend boundaries and recognized their sense of belonging to their community in a TPE program.
- The transformation was driven by dynamic interaction of the following four factors: reflection, dialogue, reinforcement of ties, and expanding roles.
- Both type of participants proceeded through uniprofessional and interprofessional learning before transprofessionally.
I. INTRODUCTION
In recent years, the need for interprofessional education (IPE) has been underscored by challenges associated with expanding medical knowledge and technologies, such as the compartmentalization of medical specialties, increased need for ensuring patient safety, and assurance of healthcare quality (Frenk et al., 2010). In 2010, the World Health Organization (WHO) emphasized the importance of IPE to mitigate the global workforce crisis and identified mechanisms for shaping successful collaborative teamwork, presenting possible action steps that policy-makers could take in their respective health systems. IPE is undoubtedly essential for promoting collaborative practice (Gilbert, Yan, & Hoffman, 2010).
Increasing emphasis has also been placed on patient involvement in the education of healthcare professionals, based on the concept that “patients are experts on their own personal and cultural context and their own stories of illness” (Centre For The Advancement Of Interprofessional Education, 2002). “Patient involvement” has a great potential to promote the learning of patient-centred practice, interprofessional collaboration, community involvement, shared decision making and how to support self-care (Towle et al., 2010). In this vein, Frenk et al. suggested that teamwork involving non-professional health workers, administrators and leaders of the local community, was vital to the smooth running of complex health systems (Frenk et al., 2010). In the field of interprofessional education, however, lay people without a body of specialty knowledge, like the professionals, have not been able to partake in IPE, as the term “interprofessional” might lead to the exclusion of lay people from active collaborative care (Vyt, Pahor, & Tervaskanto-Maentausta, 2015). They argued that transprofessional education (TPE), defined as IPE transcend traditional discipline boundaries (Stepans, Thompson, & Buchanan, 2002), was an important model that should be promoted as vigorously as IPE (Frenk et al., 2010), as it leads boundaries between professionals and lay people/patients to be blurred or vanish (Paul & Peterson, 2002). To encourage involvement of lay people beyond IPE, we developed a TPE programme, the details of which are described and explained herein.
Through this programme, we explored how lay people and multi-health professionals learned. Our research question was how healthcare professionals and lay people in a community learned with, from, and about each other in a TPE programme.
II. METHODS
A. Health education programme
In 2010, a TPE programme for lay people and healthcare professionals was developed and delivered to a hospital in Tokyo, Japan, as well as to the local community residing within easy visiting distance of the hospital. The first author (JH), an academic general practitioner, organized this TPE programme consisting of seven health education classes adapting social interdependence theory (Bruffee, 1998; Deutsch, 1949; Deutsch, 1962; Johnson, 2003). The term “health education” is used in accordance with the WHO definition: “any combination of learning experiences designed to help individuals and communities improve their health, by increasing their knowledge or influencing their attitudes” (World Health Organization, 2014).
Five healthcare professionals working in the hospital and six lay people living in the local area participated in this programme which was developed based on Harden’s 10-step approach (Harden & Davis, 1995). The learning outcome was first set to deliver information about well-being to lay people in the community. We hoped both lay and healthcare professional participants work and learn interactively through developing a series of health education class. Learning contents and methods were established through discussion between both groups.
Each health education class in our TPE programme was delivered in the following cycle, based on the Kolb’s experiential learning style theory (Kolb, 1984) and active learning theory (Graffam, 2007): pre-meeting, public bulletin, session, and two debriefing meetings. In the pre-meeting, healthcare professionals participants decided on session contents with lay participants, who then drafted an advertising leaflet about the session and distributed it to the community to recruit other community members to the class. Approximately 10 lay people participated in each session and were engaged in simulation (e.g. participants cut nails on clay fingers) or small group discussion (e.g. about their end-of-life plans). Debriefing meetings to share participants’ perspectives and values were organized a few days after each session, the conduct of which was facilitated by JH. Through these iterative cycles of developing each health education class, we incorporated both lay and healthcare professional participants’ interactions. We conducted the reflection session after completing six health education classes. The TPE programme is described in full in Table 1.
| Date | Main instructor | Session’s theme | Leaning methods | |
| 1 | June 9, 2010
2 hours |
First author (JH) (Physician) | Communication for connection
|
Interactive lecture and workshop |
| 2 | July 25, 2010
2 hours |
Nurse | Nail care
– Tinea pedis and ingrown nails |
Interactive lecture and simulation |
| 3 | August 29, 2010
2 hours |
Physical therapist | How to select the right shoes and how to walk correctly | Interactive lecture and demonstration |
| 4
|
November 23, 2010
2 hours |
Physician | End-of-life care | Narrative session and workshop |
| 5 | December 12, 2010
2hours |
|||
| 6 | February 6, 2011
3 hours |
Pharmacist, dietician | Efficacy of supplements and complementary foods | Interactive lecture and workshop |
| 7 | March 5, 2011 2 hours | All lay participants and health professionals | Reflection session | Small-group work |
Table 1: A Summary of the TPE Programme
B. Study participants
Lay candidates who lived within easy visiting distance of the hospital and healthcare professionals from the hospital were recruited to the TPE programme using convenience sampling (Babbie, 2007). The backgrounds of lay candidates varied; some had worked as nursery school teachers before, while others had been housewives. Some had chronic disease, and others had experienced being admitted to the hospital. JH then sent these candidates letters to confirm their willingness to participate in the study. The healthcare professional candidates were selected from each professional section (e.g. pharmacy section) using convenience sampling. JH sent them letters to confirm their willingness to participate in the study.
C. Methodology
We used ethnography as the methodology for this study. Ethnography is a social research methodology “occurring in natural settings characterized by learning the culture of the group under study and experiencing their way of life before attempting to derive explanations of their attitudes or behaviour” (Goodson & Vassar, 2011). Ethnography is usually used in a single setting, and data collection is mainly conducted through participant observation and interviews (Atkinson & Pugsley, 2005). In our study, we conducted participant observation during the health education classes and in clinical settings as well as focus group interviews (FGIs) over the course of 2 years to clarify participants’ behaviour and understanding in regard to the health education classes. (Figure 1)
D. Data collection
JH observed participants by recording the class events, participants’ dialogues, responses to the health education sessions, and group interactions in each health education session. JH took field notes during the classes and then asked the healthcare professional participants through e-mail whether or not they thought the data were credible. The field notes were modified or supplemented as necessary based on the healthcare professional participants’ responses. In addition, after completion of the programme, we conducted a 90-minute FGI session for the 6 lay participants and a 120-minute FGI session for the 5 healthcare professional participants in January and February 2011, respectively. In the FGIs, participants were asked about their behavioural changes subsequent to the class.
JH continued to observe participants’ behaviours in the hospital and in the community until March 2012, and he also conducted monthly FGIs for the healthcare professional participants from August 2011 to January 2012. In the FGIs, we asked how participants’ behaviours had changed after completion of the TPE programme and how they perceived these changes. The FGIs were terminated in January 2012 on recognition that data had been saturated (Morse, 1994). In addition, we asked the participating nurse to write a reflective document that we also used as data, since she had not attended most of the FGIs. (Figure 1)
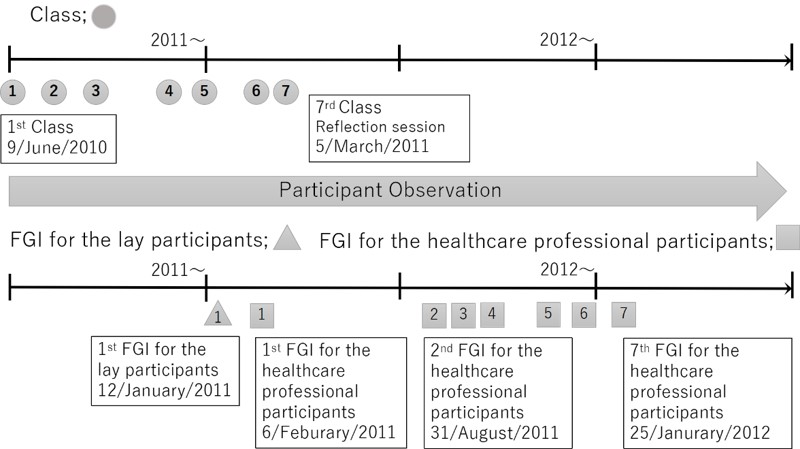
Figure 1: The flow of data collection
E. Analysis
All of the FGIs were audiotaped and transcribed verbatim by JH. A thematic analysis method was used to analyse the interview data and field notes, in which the data were iteratively read and coded for emergent themes (Braun & Clarke, 2006). First, JH and the last author (HN) read the transcripts separately. Second, the data were coded deductively based on the research questions, and inductive codes were created by JH. HN checked the inductive codes and modified as necessary. Third, JH and HN cooperatively identified and discussed the themes together from January 2011 to October 2014 for over 100 hours. This process was adopted to achieve richer interpretation of the data.
This study was reviewed and approved by the ethical committee of the hospital, which considered sampling, informed consent, and the confidentiality of participants. All participants provided written informed consent for the observation and FGIs.
III. RESULTS
The lay participants who agreed to participate in this study were six females between 60 and 80 years of age; we suspect that only females agreed to participate because women tend to stay home whereas men tend to work outside of the home in Japan. The healthcare professional participants were five 24- to 30-year-old females’ healthcare professionals (a physician, a nurse, a pharmacist, a dietician, and a physical therapist) working in the hospital.
Analysing the themes and subthemes emerged by the thematic analysis, we found that healthcare professionals and lay participants needed to progress through two stages—uniprofessional and interprofessional stages—before learning transprofessionally. Participants displayed enhanced mutual understanding only in the interprofessional and transprofessional stages. Representative data of each stage are described below. Of note, once healthcare professionals and lay participants reached the transprofessional stage, they became advocates of inter/transprofessional learning within and beyond their community.
A. Uniprofessional stage
1) Healthcare professionals:
Healthcare professionals were used to working within their professions and did not even fully understand what the other healthcare professionals did. This lack of understanding was a typical uniprofessional perspective.
“I thought nurses and doctors would know more about pharmacists.” (Pharmacist)
“Nurses looked stern, so I did not feel able to ask questions.” (Dietician)
“I thought only doctors did health education, not us.” (Nurse)
[Healthcare professional participants felt annoyed because they were not used to dealing with questions that were difficult to understand, asked suddenly, or not contextualized.](Participant observation August 2010)
2) Lay participants:
Lay participants were used to paternalistic relationships with healthcare professionals. The lay participants, who had not known one another before the programme, had hierarchical relationships or else had no connections within their own group, so a few participants led the group while the rest followed. Their perspectives might be similar to the uniprofessional perspective observed among healthcare professionals.
[When the lay participants were asked by the researcher (as a participant observer) what they wanted to do (learn), no one answered anything. They said, “We would like YOU to tell us what you want to do, then we will consider how we can help.” A few led the group of lay participants, and others just followed.] (Participant observation in May 2010)
[We could not identify the needs of lay participants through questions. However, when the author gave examples, the lay participants started to show interest by nodding in response to the author’s comments. Although the lay participants had latent needs, these were not yet tangible or the lay participants were unable to verbalize them.](Participant observation May 2010)
B. Interprofessional stage
1) Healthcare professionals:
Discussion of specialty-boundary themes in the health education classes, where multiple specialties intersect, enhanced mutual learning between professionals, which helped them to understand their own speciality and their roles within the organization. In this stage, professionals learned with, from, and about each other to improve collaboration. Discovering perceptions of their profession by other professionals also strengthened their own professional roles.
“As I was listening to the pharmacist explaining the difference between acetaminophen and NSAIDs, I came to understand why a certain painkiller was used for a certain patient, and now I understand my patients more.” (Physiotherapist)
“For the first time, I understood that terms I thought of as standard (as a professional in my field) were unfamiliar to other professionals when they asked me what a word meant.” (Physiotherapist)
“Through discussion, we should record information in clearly understandable terms to share with other professionals, as many healthcare professionals are involved in patient care.” (Pharmacist)
2) Lay participants:
The lay participants discovered unique characteristics of their local community through the health education classes, which helped them to recognize their own roles and responsibilities in their community. In addition, they played a role as health advocates for the community by reporting discussion about health-related topics that they encountered in their daily lives with those who did not participate in health education classes. These classes provided opportunities for the participants to engage with other lay people and strengthened the relationships among them. They learned together how to improve their quality of life.
“When I was handing out an advertising leaflet for health education class, I found a unit of an apartment building smelling awful. I called the police, and they found one elderly person dead and another starving.” (Interview with lay participants)
[Lay participants shared their own understanding about the community with other participants after the event <in which they found an elderly person dead>. I felt that this prompted them to consider their role and responsibility in their community in order to avoid dying alone.] (Participant observation in January 2011)
“I have seen someone teaching his friend how to clip nails properly. The impact of the classes seems to have spread among the participants.” (Interview with lay participants)
“(First) it was hard to encourage others to attend a health education classes, but as we continued, people came to sessions regularly. As the number of attendees increased, trust was nurtured, which led to more attendees.” (Interview with lay participants)
C. Transprofessional Stage
Through the debriefing meetings in each health education class, the healthcare professionals came to view the lay people’s problems like their own affairs as if their boundaries was blurred, and the lay participants began noticing the healthcare professionals’ roles in their own community. In the seventh health education class (reflection session) in particular, the participants shared their perspectives and understanding of each other’s roles, values, positions, and problems. Through the interactions in these health education classes, they came to feel a partnership and an emotional attachment with each other. At this stage, they could transcend traditional disciplinary, and their boundaries be blurred. That is transprofessional learning. They also came to advocate for interprofessional and transprofessional learning within and beyond their community.
1) Healthcare professionals:
“[Lay participants] wanted to solve the issues and change our community. So, together, we made it happen.” (Interview with healthcare professionals)
“Attending a health education class for healthy individuals was a good experience, as I was able to learn about things I did not think of before, such as what lay participants are interested in or what they want to know.” (Nurse’s report)
“These classes stimulated both the lay participants and [healthcare professions] to be more energetic” (Interview with healthcare professionals)
[The healthcare professionals set up an IPE committee in their hospital as a hub of people in different professions which served as to promote collaboration.] (Participant observation after TPE programme)
[The physicians and pharmacists actively participated in academic conferences to publicize this programme. The nurse wrote articles (about their activities).] (Participant observation after TPE programme)
2) Lay participants:
“We would not have achieved such (work) without [the healthcare professionals’] cooperation. We worked together.” (Interview with lay participants)
“We felt very close to [the healthcare professionals]. When we saw some [of them] on other occasions, we felt like cheering.” (Participant observation in the reflection session)
[Since then, lay people have actively participated in a series of classes. They gave their opinions about not only the contents but also the order of the sessions.] (Participant observation November 2010)
[To let other people know about the programme, the lay participants made a poster presentation at a local networking event and published community papers (about their activities), which helped to enhance their sense of self-efficacy.] (Participant observation after TPE programme)
IV. DISCUSSION
In the present study, we clarified how healthcare professionals and lay people achieved transprofessional learning in a TPE programme where participants advanced through uniprofessional, interprofessional stage before achieving transprofessional learning.
In the uniprofessional stage, participants tended to reflect positively on groups they belonged to (in-group favouritism) and negatively on external groups (prejudice by selective perception) (Paradis et al., 2014). In our study, little to no interaction between these groups of participants meant they lacked tangible ties, as the previous study revealed (Granovetter, 1973). Participants had limited perspectives and had not categorized themselves as belonging to their own group, which hindered recognition of problems within their own groups.
In the interprofessional stage, healthcare professional participants came to have greater understanding of other professional roles and overcame the lack of interprofessional collaboration through dialogue. Lay participants expanded their perspectives by interacting among themselves and sharing the health-related topics discussed in health education classes. This interaction might strengthen ties among participants and increase feelings of equality among members within each group. In this stage, both groups of participants began learning beyond their uniprofessional outlook.
After previous two stages, participants transcended boundaries after sharing their viewpoints in a series of classes; step-by-step, participants learned more interactively. Healthcare professionals enriched their understanding of lay people’s problems, which they had not recognized before the programme. In addition, both types of participants recognized that they were important partners in their local community, which increased their sense of belonging to the community. They developed strong ties with each other that constituted a base of trust. In this transprofessional stage, participants learned with, from, and about each other beyond the viewpoints of the interprofessional stage.
Several aspects of the transformation between stages of learning warrant mention. First, we found that reflection was key to promoting transprofessional learning. Many participants clarified their agendas by sharing their experiences mainly in the reflection sessions, and this process allowed all participants to learn interactively. Second, we identified that participants became aware of other professional and lay perspectives through dialogue. Some participants compared their perspective with others, recognized differences, and came to respect others. This encouraged participants to explore new possible selves and integrate alternative perspectives, which could be explained as transformative learning by Mezirow (Freire, 2013; Mezirow, 1991) Third, the participants’ learning experiences strengthened the ties among healthcare professionals and lay participants. Their strong ties also motivated them to band together and contribute to their own community (Krackhardt, 1992). Finally, we recognized that both types of participants expanded their roles in our programme. This experience gave them confidence and motivation, which in turn strengthened them to promote transprofessional learning (e.g. from IPE to TPE).
Thus we argued that the transprofessional learning in this programme was driven by dynamic interaction of the following four factors: reflection, dialogue, reinforcement of ties, and expanding roles. Through this process, both groups came to feel collective efficacy, which is a group’s shared belief in its joint capabilities to organize and execute the courses of action required to produce given attainments (Bandura, 1997). They thus came to share the burden of responsibility for their community across boundaries and advocated for transprofessional learning.
One strength of the present study was the involvement of non-professionals in the education of healthcare professionals. As noted in the introduction, TPE is a theme in the field of medical education that merits further research. Another strength of the study was asking, as Cook suggested, not only “Did it work?” but clarifying “How did it work?” (Cook, Bordage, & Schmidt, 2008). We described the process of how healthcare professionals and lay people learn together through ethnography. However, several limitations to the present study also warrant mention. First, the data were obtained from a single programme implemented in a single region in Japan with a relatively small population. A multi-centred study with a larger population is therefore warranted. Second, the data were collected only for two years. Studies examining the long-term effects of such a programme should be conducted. Third, the author’s role (JH) as a facilitator might have influenced participants’ responses.
V. CONCLUSION
In this study, we clarified how healthcare professionals and lay people in a community learned interactively in a TPE programme. Our participants proceeded first through uniprofessional and interprofessional stages before being able to learn transprofessionally. We described an example of how healthcare professionals and lay people promoted collaborative learning. We hope that our study will encourage healthcare practitioners involved in transprofessional education to reflect on and improve their programmes.
Notes on Contributors
Junji Haruta is an Assistant Professor in Department of General Medicine and Primary Care, University of Tsukuba Hospital, Japan. He holds PhD of Medical Education in the University of Tokyo. His areas of interest and research are in the interprofessional and transprofessional education /collaboration. He formalized in his PhD (2011-2015) on this subject.
Kiyoshi Kitamura is a Professor in International Research Center for Medical Education, Graduate School of Medicine, the University of Tokyo, Japan.
Hiroshi Nishigori is an Associate Professor in Center for Medical Education, Kyoto University, Japan.
Acknowledgements
The authors wish to thank Dr. Helena Law for reviewing the manuscript. This work was supported by JSPS KAKENHI Grant Number 2459062 Grant-in-Aid for Scientific Research (C).
Ethical Approval
This study was reviewed and approved by the ethical committee of the hospital, which considered sampling, informed consent, and the confidentiality of participants. All participants provided written informed consent for the observation and FGIs.
Declaration of Interest
The all authors have no declarations of interest.
References
Atkinson, P., & Pugsley, L. (2005). Making sense of ethnography and medical education. Medical Education, 39(2), 228–34.
Babbie, E. (2007). The Ethics and Politics of Social Research. In E. Babbie (Ed.), The Practice of Social Research. Thomson Wadsworth.
Bandura, A. (1997). Self-Efficacy: The Exercise of Control. (W.H.Freeman, Ed.). New york: Worth Publishers.
Braun, V., & Clarke, V. (2006). Using Thematica Analysis in Psychology. Qualitative Research in Psychology, 3(2), 77–101.
Bruffee, K. A. (1998). Collaborative Learning: Higher Education, Interdependence, and the Authority of Knowledge (2nd ed.). London: Johns Hopkins University Press.
Centre for the Advancement of Interprofessional Education. (2002). CAIPE. Retrieved from http://caipe.org.uk/resources/defining-ipe/
Cook, D. A., Bordage, G., & Schmidt, H. G. (2008). Description, justification and clarification: a framework for classifying the purposes of research in medical education. Medical Education, 42(2), 128–133.
Deutsch, M. (1949). A Theory of Co-operation and Competition. Human Relations, 2(2), 129–152.
Deutsch, M. (1962). Cooperation and trust: Some theoretical notes. In I. M. R. .Jones (Ed.), Nebraska symposium on motivation (pp. 275–319). Lincoln, NE:University of Nebraska Press.
Freire, P. (2013). Education for Critical Consciousness (Bloomsbury Revelations). Bloomsbury Academic.
Frenk, J., Chen, L., Bhutta, Z. A., Cohen, J., Crisp, N., Evans, T., … Zurayk, H. (2010). Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The Lancet, 376(9756), 1923–1958.
Gilbert, J. H. V, Yan, J., & Hoffman, S. J. (2010). A WHO Report: Framework for Action on Interprofessional Education and Collaborative Practice. Journal of Allied Health, 39, 196–197.
Goodson, L., & Vassar, M. (2011). An overview of ethnography in healthcare and medical education research. Journal of Educational Evaluation for Health Professions, 8(4).
Graffam, B. (2007). Active learning in medical education: strategies for beginning implementation. Medical Teacher, 29(1), 38–42.
Granovetter, M. S. (1973). The Strength of Weak Ties. American Jounal of Sociology, 78(6), 1360–1380.
Harden, R. M., & Davis, M. H. (1995). AMEE Medical Education Guide No. 5. The core curriculum with options or special study modules. Medical Teacher, 17(2), 125–148.
Johnson, D. W. (2003). Social interdependence: interrelationships among theory, research, and practice. The American Psychologist, 58(11), 934–45.
Kolb, D. A. (1984). Experiential learning: experience as the source of learning and development.
Krackhardt, D. (1992). The Strength of Strong Ties: The Importance of Philos in Organizations. In N. Nohria & R. Eccles (eds.), Networks and Organizations: Structure, Form, and Action. Boston, MA: Harvard Business School Press.
Mezirow, J. (1991). Transformative Dimensions of Adult learning (1st ed.). San Francisco: Jossey-Bass.
Morse, J. M. (1994). Designing funded qualitative research. In Y. S. Lincoln (Ed.), Handbook of qualitative research (2nd ed., p. 220–235.). Denzin, New York: Thousand Oaks, Sage.
Paradis, E., Reeves, S., Leslie, M., Aboumatar, H., Chesluk, B., Clark, P., … Kitto, S. (2014). Exploring the nature of interprofessional collaboration and family member involvement in an intensive care context. Journal of Interprofessional Care, 28(1), 74–5.
Paul, S., & Peterson, C. Q. (2002). Interprofessional collaboration: issues for practice and research. Occupational Therapy in Health Care, 15(3–4), 1–12.
Stepans, M. B., Thompson, C. L., & Buchanan, M. L. (2002). The role of the nurse on a transdisciplinary early intervention assessment team. Public Health Nursing (Boston, Mass.), 19(4), 238–45.
Towle, A., Bainbridge, L., Godolphin, W., Katz, A., Kline, C., Lown, B., … Thistlethwaite, J. (2010). Active patient involvement in the education of health professionals. Medical Education, 44(1), 64–74.
Vyt, A., Pahor, M., & Tervaskanto-Maentausta, T. (2015). Interprofessional education in Europe: Policy and practice. Garant Uitgevers N V.
World Health Organization (2014). Health education. Retrieved from http://www.who.int/topics/health_education/en/
*Junji Haruta
2-1-1 Amakubo Tsukuba Ibaraki
Japan
Tel: +81-29-853-3189
Fax: +81-29-853-3189
Email: junharujp@gmail.com
Published online: 2 January, TAPS 2018, 3(1), 27-37
DOI: https://doi.org/10.29060/TAPS.2018-3-1/OA1064
Pei Se Wong1, Syed Shahzad Hasan1, Jinly Ooi2, Lawrence, S. H. Lim3 and Vishna Devi Nadarajah1
1International Medical University (IMU), Malaysia; 2Hospital Kulim, Malaysia; 3Penang General Hospital, Malaysia
Abstract
Inter-professional education (IPE) contributes to the development of an ‘inter-professional, collaborative and practice-ready’ healthcare workforce that is well prepared to respond to local healthcare needs. Little is known about the extent, to which health professional students who are nearing graduation understand the competencies of diverse health professions. The aim of this study was to investigate the perception of final-year undergraduate students’ towards interprofessional team working and their knowledge of the competencies of 6 health professions. This study evaluated the final-year health professional students’ from six (6) health professions programmes namely medical, dental, nursing, pharmacy, dietetics and biomedical sciences programmes. Attitudes towards Health Care Team Scale (ATHCTS) was used to measure students’ attitudes towards teamwork while a checklist was used measure students’ knowledge of 6 health professionals competencies. Construct validity was ascertain and findings from ATHCTS showed mean scores ranges from 48.57 to 54.23 indicating positive attitudes toward working within interprofessional health care teams. While the ACTHS findings were positive, the competencies checklist showed mixed findings in that students correctly identified some competencies and had misconceptions for others. For example, the majority of students regarded physicians as competent in ‘assessment and evaluation’ and ‘medication management’ while less than 50% of participants recognised the importance of assessment of patient’s health-illness as a competency for dieticians. Gaps identified in final year students’ knowledge of the roles and competencies of health professions has an impact on future interprofessional collaborative practice suggesting a need to further improve curriculum design and delivery of IPE.
Keywords: Allied health, Inter-professional, Learning, Inter-professional education
Practice Highlights
- Little is known about the extent, to which health professional students who are nearing graduation understand the competencies of diverse health professions.
- The findings indicated the final-year health professional students from six (6) health professions programmes namely medical, dental, nursing, pharmacy, dietetics and biomedical sciences programmes have positive attitudes toward working within interprofessional health care teams.
- There were mixed findings in students’ perceptions of competencies of health professions.
- Gaps identified in final year students’ knowledge of the roles and competencies of health professions suggesting a need to enhance curriculum design and delivery of IPE.
I. INTRODUCTION
Interprofessional collaborative practice (IPC) in health care has been widely recognised as a potential solution to improve healthcare delivery. IPC has been linked with improved service provision, health outcomes, patient safety (Lemieux-Charles & McGuire, 2006; Mickan, 2005), and reduced mortality and hospitalisation (Malone, Marriott, Newton-Howes, Simmonds, & Tyrer, 2007; McAlister, Stewart, Ferrua, & McMurray, 2004). Awareness and understanding of one’s own and others’ professional roles, responsibilities and value in patient care is an important prerequisite for IPC to occur (Suter, 2009).
Interprofessional education (IPE) is viewed as the means to prepare an inter-professional health workforce that can better respond to local healthcare needs. The World Health Organisation describes IPE as a learning event when students from two or more professions learn about, from, and with each other to enable effective collaboration and improve health outcomes (World Health Organization, 2010). The ultimate goal of IPE is to prepare students for Interprofessional Collaboration (IPC), by becoming collaborative interprofessional team members who display respect and positive attitudes towards each other as well as focusing on shared and positive patient outcomes. IPE is also expected to enhance students with interpersonal skills needed for liaison and communication.
A systematic review performed by Hammick, Freeth, Koppel, Reeves and Barr (2007) identified, organised and synthesised the best available contemporary evidence from the strongest evaluations of IPE evidence involving health professional students at the undergraduate level. The findings suggested that IPE is more effective in relation to ‘reaction’ and ‘learning’, with much less evidence of impact on ‘behaviour’ and ‘results’. It has also been postulated that to achieve positive effect of IPE, validity and customization as well as legitimacy of IPE is required (Hammick et al., 2007).
Much international literature has discussed the promotion of IPE in terms of when it should take place, how it should be managed, who will be involved, and what should be taught (Thistlethwaite 2012). In the discussion of what should be taught, little is mentioned about how each other’s responsibilities could be collaboratively optimised in the healthcare setting. Less is also known about students’ perceptions of the roles and competencies of other health professions which could affect their future collaborative work. In addition to that, there are lesser publications on IPE for some of the allied health sciences programmes such as dietetics, biomedical science and pharmacy. This can be seen from majority of the IPE publications, which are done within professions of medicine, dentistry and nursing (Curran, Sharpe, Forristall, and Flynn, 2008; Heinemann, Schmitt, Farrell, and Brallier, 1999; Spence & Weston, 1995).
IPE initiatives need to account for differences in perceptions of what IPC is and how it can be achieved in practice. Yet little is known about how much health professional students who are nearing graduation understand roles and responsibilities of the different health professions. This study evaluated final-year health professional students from six (6) health professions programmes on their perceptions towards interprofessional team working and their knowledge of the roles and competencies of health professions.
II. METHODS
A. Study design
This cross-sectional study was conducted at a medical and health sciences university (International Medical University), located in Kuala Lumpur, Malaysia to assess students’ perceptions on interprofessional team working and understanding of roles and competencies of different health professions. All final-year students pursuing medical, dental, pharmacy, nursing, dietetic, and biomedical sciences programmes were invited to participate in this study. Students who provided the consent and completed the study instrument were included in the study sample. Ethics approval was received from International Medical University, Research and Ethics Joint Committee (Project ID BPI-01-11(50)2014).
B. Data collection tool
The data collection tool used in this study was divided into three parts. The first part covered the socio-demographic characteristics of the study participants. The second part of the questionnaire collected data on students’ agreement on team working using the Attitudes towards Health Care Team Scale (ATHCTS). A 14-item Attitudes Toward Health Care Teams (ATHCT), adapted from Heinemann, Schmitt and Farrell (2002) was used to measure attitudes towards working on interprofessional healthcare teams. In the ATHCT scale (Heinemann et al., 1999), the authors identified three main factors namely quality of care, costs of team care and physician centrality, having 14, 7 and 6 items, respectively. For the purpose of our study, we followed Curran et al. (2008) approach and selected 11 items from the quality of care factor and 3 items from the costs of team care factor. As described by Curran et al. (2008), selected items are appropriate and relevant for undergraduate health science students who would have little or no experience with items relating to physician centrality (factor 3). Responses were scored on a five-point Likert scale ranging from one (strongly disagree) to five (strongly agree). Three items which were related to time constraints were reverse coded because they were negative statements. Higher scores indicate more positive attitudes toward interprofessional health care teams.
The last part was a self-developed form to collected data on students’ perception and understanding of health professions roles and competencies in patient care. Responses were scored on a five-point Likert scale ranging from one (highly competent) to five (least competent). A total of 15 items consisting of the roles and competencies of health professionals in patient care was included. These 15 items covered three broad areas of assessment and evaluation, provision of care and medication management.
C. Sampling procedure
During the data collection phase, researchers approached final-year cohorts of medicine, dentistry, pharmacy, nursing, dietetics, and biomedical sciences students at IMU to provide information about the study. Questionnaires were provided with a copy of participant information sheets and consent forms. Convenience sampling was used to enrol all the eligible respondents during the study period. Participants were briefed by the researchers before completing the questionnaire. Participation was anonymous and voluntary, with no reward for participation. Researchers were there in person to clarify any doubts from students. The participants were approached after major teaching and learning sessions to obtain higher response rate. Responses from final-year students were collected within 6 month prior to completion of the programmes. The content and the teaching methods remained stable over the period in which the information was collected.
D. Statistical analysis
Both descriptive and inferential data analyses were performed using SPSS® version 22 with 0.05 as the level of significance. Descriptive statistics was used to generate summary estimates on the participants by programme. Frequencies, percentages, mean, and standard deviations were also calculated. Since ATHCTS has not been previously used in Malaysia, we conducted a Principal Component Analysis (PCA) to examine the underlying components of ATHCTS in Malaysian students. The sample size was 301, which is sufficient to perform factor analysis. Kaiser-Meyer-Olkin test (KMO) was performed to measure sampling adequacy of >0.7. Bartlett’s test of sphericity was used to measure significant correlations between variables. The corrected item-total score correlations were also examined. Internal consistency was analysed using Cronbach’s alpha. Independent T-test and one-way analyses of variance (ANOVA) including post hoc tests were computed to examine differences in scores related to gender, age, and programme. Chi-square test for association and Pearson test for correlation were also applied.
III. RESULTS
A. Participants’ Demographics
Of 443 students approached, 301 accepted and completed with an overall response rate of 67.9%. These 301 respondents represented more than 50% of the final year medical, dentistry, pharmacy, dietetics, nursing, and biomedical sciences students. Final-year nursing students had the lowest population due to small cohort size as shown in Table 1. The mean age of participating students was 23.17 with a standard deviation of 1.42. Majority of the students were females (67.5%), aged between 23 and 25 years (63.6%) and enrolled in Medicine (37.5%) and Pharmacy (27.2%) programmes. Table 1 summarizes the demographic data of the participants.
B. The construct and reliability of ATHCTS
The adapted ATHCTS (Curran et al., 2008) consists of 14 items that measure attitudes toward inter-professional health care teams was employed in this study. Table 2 summarizes the assessment of reliability and validity of the adapted ATHCTS using the 301 final-year health professional students in this current study.
Factor loadings of all items were above 0.40, and item 13 had the strongest factor loading of 0.778. Internal consistency of the ATHCTS was good at 0.93. Using exploratory factor analysis, the authors identified two factors: quality of care and time constraint. The quality of care subscale (Items 1–11) showed good internal consistency (alpha: 0.83), whereas Cronbach’s alpha for time constraints (Items 12–14) was very low (alpha: 0.54).
| Items | N | % |
| Age (mean, SD) | 23.27 (1.42) | |
| Age groups | ||
| 20-22 | 96 | 31.8 |
| 23-25 | 192 | 63.6 |
| 26 and above | 14 | 4.6 |
| Gender | ||
| Female | 204 | 67.5 |
| Male | 97 | 32.1 |
| School | ||
| Medical | 113 | 37.5 |
| Dentistry | 36 | 12.0 |
| Nursing | 14 | 4.7 |
| Pharmacy | 82 | 27.2 |
| Biomedical | 23 | 7.6 |
| Dietetics | 33 | 11.0 |
Table 1. Demographic characteristics of the study participants (n=301)
| No | Items (sequence in scale) | Rotated Factor Coefficients | |
| Quality of Care
(Factor 1) |
Time Constraints (Factor 2) | ||
| 1 | The inter-professional approach improves the quality of care to patients/clients (2). | 0.661 | – |
| 2 | The inter-professional approach permits health professionals to meet the needs of family caregivers as well as patients (17). | 0.668 | – |
| 3 | Having to report observations to a team helps team members better understand the work of other health professionals (18). | 0.641 | – |
| 4 | The inter-professional approach makes the delivery of care more efficient (16). | 0.652 | – |
| 5 | Hospital patients who receive inter-professional team care are better prepared for discharge than other patients (15). | 0.576 | – |
| 6 | Team meetings foster communication among team members from different professions or disciplines (3). | 0.598 | – |
| 7 | The give and take among team members helps them make better patient/client care decisions (12). | 0.565 | – |
| 8 | Patients/clients receiving inter-professional care are more likely than others to be treated as whole persons (4). | 0.631 | – |
| 9 | Health professionals working as teams are more responsive than others to the emotional and financial needs of patients/clients (9). | 0.563 | – |
| 10 | Working in an inter-professional environment keeps most health professionals enthusiastic and interested in their jobs (5). | 0.613 | – |
| 11 | Developing a patient/client care plan with other team members avoids errors in delivering care (7). | 0.436 | – |
| 12 | *Working in an inter-professional manner unnecessarily complicates things most of the time (1). | – | 0.538 |
| 13 | *In most instances, the time required for inter-professional consultations could be better spent in other ways (13). | – | 0.778 |
| 14 | *Developing an inter-professional patient/client care plan is excessively time-consuming (10). | – | 0.748 |
| Cronbach’s alpha | 0.83 | 0.54 | |
| Percent of variance (%) | 30.51 | 11.30 | |
*Denotes reverse coded items.
Table 2. Factor Analysis and corrected item-total score correlations of the ATHCTS
| No | Items | Factor Loadings | |||
| Curran et al. (2008) | Hayashi et al.
(2012) |
Kim et al. (2014) | Present (2016) | ||
| 1 | The inter-professional approach improves the quality of care to patients/clients. | 0.68 | 0.51 | 0.61 | 0.66 |
| 2 | The inter-professional approach permits health professionals to meet the needs of family caregivers as well as patients. | 0.64 | 0.63 | 0.72 | 0.67 |
| 3 | Having to report observations to a team helps team members better understand the work of other health professionals. | 0.63 | 0.56 | 0.66 | 0.64 |
| 4 | The inter-professional approach makes the delivery of care more efficient. | 0.61 | 0.44 | 0.71 | 0.65 |
| 5 | Hospital patients who receive inter-professional team care are better prepared for discharge than other patients. | 0.61 | 0.54 | 0.79 | 0.58 |
| 6 | Team meetings foster communication among team members from different professions or disciplines. | 0.60 | 0.76 | 0.70 | 0.59 |
| 7 | The give and take among team members helps them make better patient/client care decisions. | 0.54 | 0.60 | 0.76 | 0.56 |
| 8 | Patients/clients receiving inter-professional care are more likely than others to be treated as whole persons. | 0.52 | 0.32 | 0.70 | 0.63 |
| 9 | Health professionals working as teams are more responsive than others to the emotional and financial needs of patients/clients. | 0.51 | 0.74 | 0.68 | 0.56 |
| 10 | Working in an inter-professional environment keeps most health professionals enthusiastic and interested in their jobs. | 0.51 | 0.36 | 0.55 | 0.61 |
| 11 | Developing a patient/client care plan with other team members avoids errors in delivering care. | 0.49 | 0.27 | 0.62 | 0.44 |
| 12 | *Working in an inter-professional manner unnecessarily complicates things most of the time. | 0.65 | 0.36 | 0.80 | 0.54 |
| 13 | *In most instances, the time required for inter-professional consultations could be better spent in other ways. | 0.59 | 0.24 | 0.88 | 0.78 |
| 14 | *Developing an inter-professional patient/client care plan is excessively time-consuming. | 0.42 | 0.79 | 0.76 | 0.75 |
| Cronbach’s alpha for Quality of Care | 0.82 | – | 0.92 | 0.83 | |
| Cronbach’s alpha for Time Constraints | 0.56 | – | 0.86 | 0.54 | |
| N | 1179 | 285 | 288 | 301 | |
| Disciplines | UG Health Sciences | UG Health Sciences | G Health professionals | UG Health Sciences | |
Note: UG = Undergraduate, G = Graduate
Table 3. Comparison of factor loadings among Curran et al. (2008), Hayashi et al. (2012), Kim et al. (2014) and present study.
| Item | Categories |
Mean |
SD |
Overall |
| Gender | Female | 51.32 | 5.44 | t = 0.963 |
| Male | 52.00 | 6.22 | ||
| Age | 20 – 22 | 51.13 | 5.17 | F = 8.312
p = 0.001 |
| 23 – 25 | 50.78 | 5.94 | ||
| > 25 | 54.23 | 5.25 | ||
| Discipline | Medical (n=113) | 53.14 | 5.92 | F = 4.901
p = 0.001 |
| Dentistry (n=36) | 51.69 | 6.10 | ||
| Nursing (n=14) | 49.64 | 5.81 | ||
| Pharmacy (n=82) | 50.10 | 5.47 | ||
| Dietitics (n=33) | 52.42 | 4.15 | ||
| Biomedical (33) | 48.57 | 3.96 |
*. The mean difference is significant at the 0.05 level. Scale: 1 (strongly disagree) to 70 (strongly agree)
Table 4. Mean score of ATHCTS questionnaire, by participants’ gender, age and discipline
| Items | Nurse | Dentist | Physician | Pharmacist | Biotechnologist/
Biomedical Scientist |
Dietician
|
| Assessment and Evaluation | ||||||
| 1. Assesses patient’s health-illness. | 68.5 | 69.5 | 95.7* | 55.6 | 20.5 | 48.7 |
| 2. Obtains and records the patient’s and family’s health history. | 71.5 | 78.5 | 92.7* | 65.2 | 22.5 | 59.6 |
| 3. Performs a physical examination. | 48.0 | 68.5 | 97.4* | 22.2 | 10.9 | 26.5 |
| 4. Orders routine laboratory investigations. | 25.2 | 64.6 | 87.4* | 36.1 | 38.7 | 22.2 |
| Provision of Care | ||||||
| 5. Performs laboratory investigations. | 12.3 | 29.1 | 35.8 | 19.2 | 74.8* | 11.9 |
| 6. Provides care that encompasses the physical, psychosocial, developmental, cultural, & spiritual levels. | 72.5 | 53.6 | 73.2* | 47.4 | 14.6 | 48.7 |
| 7. Provides health education to patient and family. | 72.2 | 72.8 | 88.7* | 73.2 | 21.5 | 68.5 |
| 8. Provides advice on strategies to adopt a healthy caloric plan | 31.8 | 25.5 | 53.0 | 33.4 | 10.9 | 86.8* |
| 9. Initiates treatment and therapeutic regimens. | 28.5 | 70.9 | 94.4* | 63.6 | 8.9 | 26.2 |
| 10. Advises on referrals to other health professionals if necessary. | 39.4 | 76.2 | 92.7* | 60.9 | 28.8 | 51.7 |
| Medication Management | ||||||
| 11. Prescribes medications. | 19.2 | 67.5 | 93.0* | 83.8 | 6.3 | 9.9 |
| 12. Administers medications. | 78.1 | 72.5 | 86.8* | 74.5 | 10.6 | 14.2 |
| 13. Makes adjustment to medications. | 17.2 | 66.6 | 92.4* | 82.1 | 8.6 | 22.5 |
| 14. Provides counselling regarding the medications to individuals and families. | 47.0 | 62.3 | 84.1 | 85.8* | 15.6 | 34.1 |
| 15. Evaluates progress of patient with medications. | 57.0 | 64.2 | 90.7* | 70.9 | 9.9 | 30.1 |
*Denotes healthcare professions who are perceived as most competent
Table 5. Proportion (%) of participating students who considered healthcare professionals as competent or highly competent for specific roles and competencies.
Table 3 shows the factor structure found in this study is similar to the previous studies (Kim & Ko, 2014; Curran et al., 2008) except Hayashi et al. (2012) confirming the construct validity of ATHCTS tool in current study using undergraduate health profession students. Hayashi et al. (2012) identified three factors within the list of 14 items using an exploratory factor analysis: quality of care delivery, patient-centered care and team efficiency. They identified an additional subscale consisting of 4 items, which is different from the two-factor solution yielded by other three studies.
C. Attitudes towards team working
Table 4 summarizes the attitudes of participants towards working on interprofessional healthcare team according to gender, age and programme. All mean scores ranges from 48.57 to 54.23 indicating positive attitudes toward working on interprofessional health care teams.
Male students and students aged above 25 years were found to have higher mean scores compared with female and students aged 25 years and below. Medical students had the highest mean score compared to the rest, followed by dietetic and dental students.
D. Knowledge of roles and competencies
Table 5 summarizes the proportion of participants who considered health professionals as competent or highly competent, according to roles and competencies needed for patient care. A list of 15 items consisting of common roles and competencies of various health care professionals, were provided to participating students. The participating students were instructed to indicate “highly competent” to “least competent” for each item. The healthcare professions who are perceived as most competent had the highest scores for both the ‘highly competent’ and ‘competent’ in each of items.
Physicians were regarded as the most competent in all items related to ‘patient assessment’ (ranging from 87.4% to 97.4%), except for three items. In terms of ‘performing laboratory investigations’, biotechnologists and biomedical scientist were regarded to be most competent (74.8%), while dieticians were most competent in providing advice on strategies to adopt a healthy caloric plan (86.8%). Most students also perceived physicians to be competent/highly competent in providing care related to physical, psychosocial, developmental, cultural and spiritual matters (73.2%), providing health education to patient and family (88.7%), initiating treatment and therapeutic regimens (94.44%), and advise on referrals (92.7%). Dentists were second to physicians with regards roles and competencies related assessment and evaluation of patients and providing referrals. Nurses on the other hand, received higher scores compared to other professions (except physicians) for provision of care related to physical and psychosocial factors and in health education.
Majority of the students also perceived physicians to be competent/highly competent in most areas of ‘medication management’ (ranging 86.8% to 93%) except medication counseling. Pharmacist were regarded as the second to physicians with competent/highly competent skills in medication prescribing (83.8%), making adjustment to medication (82.1%) and evaluate patient progression with medication (70.9%).
IV. DISCUSSION
The main objectives of this study were to evaluate attitudes toward working in interprofessional health teams and determine the perception and understanding of final year health professional students on roles and competencies of health professions. The ability to work with professionals from other professions to provide effective healthcare is an important element of professional practice requiring the right attitude towards team working and a specific set of competencies. While there are studies evaluating attitudes toward working in interprofessional health teams among medical, pharmacy, dentistry and nursing students, attitudes towards other allied health professional programmes and of dietetics and biomedical sciences students were less reviewed. Lesser known though is final year students’ perception and understanding of the role and competencies of health professions that they will interact with, both in the early years after graduation and later in practice. The findings of this study which is across 6 health professions programme will provide broader understanding for encouraging IPC and serves as a baseline for more extensive studies.
The ACTHS instrument was found to be valid and reliable for the context of our study and was comparable to previous reports. Overall findings from our study are congruent with results from previous studies (Hojat et al., 1999; Leipzig et al., 2002), indicating that attitudes towards team working are generally positive among health professional students. There are few possible reasons for the positive scores. It is plausible that the emphasis on the importance of IPC approaches in education has encouraged the positive attitude towards IPC. The university (IMU) since 2012 has initiated efforts to integrate and embed collaborative learning sessions into the undergraduate health professional programmes. Although the delivery method of collaborative learning each programme varies, all programmes have graduate outcomes, which are related to core competencies of IPC within the programme. For example, collaborative learning requires communication skills and teamwork. The student learning outcomes related communication skills and team working are delivered through Problem Based Learning, community service projects and research projects, group presentations and assignments from year 1 to the final year.
As the participants of this study were final-year students who have been exposed to the real clinical practice via experiential learning, it is also possible that the interaction and observation of different level of collaborative practice in primary or secondary care settings could have promoted the positive attitudes towards team working (Lai, Sivalingam, & Ramesh, 2007; Tunstall-Pedoe, Rink, & Hilton, 2003). It has been recognised that the ideal interprofessional clinical learning experience involves students from several disciplines in experiential learning via practice-based settings (Lapkin, Levett-Jones, & Gilligan, 2012). One such learning environment is a “training ward”, in which preregistration health professional students work in interprofessional teams, under supervision, to manage the care of patients (Morphet et al., 2014). Successful training ward programmes not only engaged students in interprofessional patient care, but also reported to have positive student and patient outcomes (Hasan et al., 2013; Ericson, Masiello & Bolinder, 2012; Lindblom, Scheja, Torell, Astrand, & Felländer-Tsai, 2007; Tanaka & Yokode, 2005; Freeth et al., 2001).
Studies have highlighted that understanding of one’s own and others’ professional roles, responsibilities and value in patient care is an important prerequisite for collaboration to occur (Orchard, Curran & Kabene, 2005; Suter et al., 2009). In this study, we evaluated the final-year students’ perception and understanding of the roles and competencies of 6 health professions including their own. While the ACTHS findings were positive, the roles and competencies checklist showed mixed findings in that students correctly identified some competencies and had misconceptions for others.
For example, physician is regarded by the majority of students as the competent profession for these responsibilities ranging from ‘assessment and evaluation’, ‘the provision of patient care’ and ‘medication management’. Although patient assessment is considered as one of the core competencies in undergraduate health professional programmes, it is of concern that less than 50% of participants recognised the importance of assessment of patient’s health-illness as a competency for dieticians. The finding indicates that the need to increase awareness of the dieticians’ responsibilities in patients’ assessment in the curriculum of the respective programmes. A recent study by Darlow et al. (2015), which introduced an IPE initiative across 4 health professional programmes including dieticians, suggests improved attitudes towards interprofessional teams and learning, as well as self-reported ability to function within an interprofessional team, and ability to manage people with long-term conditions. Biomedical scientist and biotechnologist on the other hand is rightly recognised to be competent in performing laboratory investigation. This probably due to unique roles of biomedical scientist/biotechnologist and the lesser opportunities for contact or collaboration the other health professions have with them for direct patient care.
Majority of participants correctly identified physicians as competent or highly competent in prescribing medication while only 67.5 % considered dentist to be competent in prescribing medications. This figure is quite low compared to 84% for pharmacists, who are only authorised to prescribe selected group of medications (mostly over the counter products and non-prescription medication). This perhaps indicates lack of awareness that licensed dentists are also considered legal prescribers for medicines in Malaysia and other countries, similarly to physicians. Another reason could be due to the limited range of dental prescription from general dental practitioners. Dental prescription generally comprises of analgesics and antibiotics (Dar-Odeh, Ryalat, Shayyab, and Abu-Hammad 2008; Mendonca et al., 2010). It is also worth noting that the misconception or lack of understanding of professional roles has been observed for the nursing profession too. Previous studies found that medical students were less clear about competencies important for nursing than nursing students were in their perceptions of competencies important for doctors (Rudland & Mires, 2005; Spence & Weston, 1995). Given that majority of the students in this study are from medicine and pharmacy, attention is needed to close the gap on understanding nurses’ roles as both these professions especially physicians will work closely with them in various clinical and community settings. Although the need for IPE to improve knowledge of different healthcare roles has been suggested for more than 20 years, the findings reported in this study and others suggest undergraduate IPE can still be improved at the undergraduate level (Fagin, 1992; McCahan, 1986).
In terms of roles and competencies related to medication, pharmacist was recognised to be the second most competent professional in medication prescribing and adjustment. The finding seems surprising as pharmacists’ roles in prescribing in limited to non-prescription medication. Pharmacists have the limited rights to prescribe medication. Nevertheless, there is increasing evidences of expanding roles of pharmacist in medication management. One such example is the introduction of Medication Therapy Adherence Clinic (MTAC) and home medication reviews. In provision of these services, pharmacists’ roles include medication review as well as making recommendations on dosage adjustment (Aidit, Shaharuddin, Neoh, & Ming, 2015; Lim & Lim, 2010; Saleem, Hassali, & Chow, 2015). Although not yet a model in Malaysia, the expanded pharmacist prescribing role is also emerging internationally (Hoti, Hughes, & Sunderland, 2011). In United Kingdom, the movement has led to introduction of supplementary and independent models of prescribing (Cooper et al., 2008).
The gaps or misconception regarding roles and competencies identified amongst the health professional final year students are a cause for reflection on curriculum delivery. Although there is an awareness of the importance of interprofessional curriculum and providing opportunities for students to learn in interprofessional groups, individual programme needs may take priority in curriculum delivery and assessment resulting in challenges for IPE. This includes developing learning outcomes, scheduling teaching learning activities, class size, blue printing of assessments, as well as skill development based on individual health professional roles, competencies and needs. Hence it is possible that the learning environments within the professional groups differ significantly (Pollard, Miers, & Gilchrist, 2005). Furthermore, it has been pointed that if students do not observe IPC being role modelled in practice or have opportunities to engage with other health professions in practice, it will difficult for them to recognize the roles and competencies important for health professionals. Universities and health care institutions should work together to unite the theory and practice, allowing learning to be supported with “real practice” (Jackson et al., 2016).
There are several limitations encountered in this study. Firstly, this study was cross-sectional in design and not longitudinal in nature. Thus, it does not reveal the actual development of interprofessional team working behaviour in the student cohorts. Secondly, the scores reported for roles and competencies were derived from measures obtained with a self-reported instrument which was not supplemented with observational measurements. Therefore, the assessment was of students’ orientation to IPP and may not accurately reflect the true learning behaviour and experiences. Thirdly, the finding may somewhat limited in general ability owing to their derivation from only one institution. This study however does provide useful insights on graduating health professionals’ perceptions toward IPP as the attitudes toward team working and understanding of the roles and competencies of 6 different health professions was elucidated. Future directions for research should continue with implementing IPE activities with goals on improving understanding on the roles and competencies of health professionals. The long-term effect of these initiatives on interprofessional practice as well as attitudes toward interprofessional teamwork and knowledge of health professionals’ roles and competencies should be evaluated.
V. CONCLUSION
Final year health professional students have positive attitudes toward interprofessional team working. However, this study also identified gaps in understanding the roles and competencies of 6 different health professions amongst the final year students. The understanding of one’s own and others’ professional roles, responsibilities and value in patient care is critical in a collaborative environment. The findings of this study will be helpful in making informed decisions for curriculum design and delivery of IPE programmes. In relation to this study, the gaps identified in final year students’ perception of the roles of above mentioned health professionals has been highlighted to the respective programme coordinators for their further action.
Notes on Contributors
Vishna Devi V Nadarajah (VDN), Pei Se Wong (PSW), Syed Shahzad Hasan (SSH), Jinly Ooi (JLO) and Lawrence Hsien Sheng Lim (LL) were involved in conception and design of the work, drafting the research proposal, data analysis and manuscript writing. VDN and PSW were involved in conception and design of work, JLO and LL collected the data, and together with VDN, PSW and SSH contributed on the data analysis and interpretation. PSW, VDN and SSH contributed on critical revision of the article; and writing of final approval of the version to be published.
Ethical Approval
Ethics approval was received from International Medical University, Research and Ethics Joint Committee (Project ID BPI-01-11(50)2014).
Acknowledgements
The authors would like to acknowledge final-year students who had participated in this study. The authors are also thankful to the International Medical University for the study approval and funding.
Declaration of Interest
This study was supported by International Medical University, Kuala Lumpur. Ethics approval was received from International Medical University, Research and Ethics Joint Committee (Project ID BPI-01-11(50)2014). All authors have no potential conflicts of interest.
References
Aidit, S., Shaharuddin. S., Neoh, C. F., & Ming, L. C. (2015). Evolvement of warfarin medication therapy adherence clinic in Malaysia and its impact on international normalized ratio control over time. Journal of Pharmacy Practice and Research, 45, 431–432.
Cooper, R. J., Anderson, C., Avery, T., Bissell, P., Guillaume, L., Hutchinson, A., … Ward, P. (2008). Health Policy. 85(3), 277-92.
Curran, V.R., Sharpe, D., Forristall, J., & Flynn, K. (2008). Attitudes of health sciences students towards interprofessional teamwork and education. Learning in Health and Social Care, 7(3), 146–156.
Dar-Odeh, N., Ryalat, S., Shayyab, M., & Abu-Hammad, O. (2008). Analysis of clinical records of dental patients attending Jordan University Hospital: Documentation of drug prescription and local anaesthetic injections. Therapeutics and Clinical Risk Management, 4, 1111-1117.
Darlow, B., Coleman, K., McKinlay, E., Donovan, S., Beckingsale, L., Gray, B., … Pullon, S. (2015). The positive impact of interprofessional education: a controlled trial to evaluate a programme for health professional students. BMC Medical Education, 98. doi: 015-0385-3/s12909-015-0385-3.
Ericson, A., Masiello, I., & Bolinder, G. (2012). Interprofessional clinical training for undergraduate students in an emergency department setting. Journal of Interprofessional Care, 26(4), 319–325.
Fagin, C. (1992). Collaboration between nurses and physicians: no longer a choice. Nursing and Health Care, 13, 354–363.
Freeth, D., Reeves, S., Goreham, C., Parker, P., Haynes, S., & Pearson, S. (2001). ‘Real life’ clinical learning on an interprofessional training ward. Nurse Education Today, 21(5), 366–372.
Hammick, M., Freeth, D., Koppel, I., Reeves, S., & Barr, H. (2007). A best evidence systematic review of interprofessinal education: BEME Guide no. 9. Medical Teacher, 29(8), 735-751.
Hayashi, T., Shinozaki, H., Makino, T., Ogawara, H., Asakawa, Y., Iwasaki, K., … Watanabe, H (2012). Changes in attitudes toward interprofessional health care teams and education in the first-and third-year undergraduate students. Journal of Interprofessional Care, 26(2),100–107. doi: 10.3109/13561820.2011.644355.
Hasan, S.S., Wong, P.S., Ahmed, S.I., Chong, D.W.K., Mai, C.W., Pook, P., & Kairuz, T. (2013) Perceived impact of clinical placements on students’ preparedness to provide patient-centered care in Malaysia. Currents in Pharmacy Teaching and Learning, 5(4), 303-310.
Heinemann, G.D., Schmitt, M.H., Farrell, M.P. & Brallier, S.A. (1999). Development of an attitudes toward health care teams scale. Evaluation and the Health Professions, 22, 123–142.
Heinemann, G.D., Schmitt, M.H., & Farrell, M.P. (2002). Attitudes toward health care teams. In G.D. Heinemann & A.M. Zeiss (Eds.), Team Performance in Health Care: Assessment and Development. (pp. 155–159). New York: Kluwer Academic/Plenum Publishers.
Hojat, M., Fields, S., Veloski, J.J., Griffiths, M., Cohen, M., & Plumb, J. (1999). Psychometric properties of an attitude scale measuring physician-nurse collaboration. Evaluation & the Health Professions, 22(2), 208-20.
Hoti, K., Hughes, J., & Sunderland, B. (2011). An expanded prescribing role for pharmacists – an Australian perspective. Australasian Medical Journal, 4(4), 236-242.
Jackson, M., Pelone, F., Reeves, S., Hassenkamp, A.M., Emery, C., Titmarsh, K., & Greenwood, N. (2016) Interprofessional education in the care of people diagnosed with dementia and their carers: a systematic review. BMJ Open, 16(6):e010948. doi:10.1136/bmjopen-2015-010948.
Kim, K. & Ko, J. (2014). Attitudes toward interprofessional health care teams scale: a confirmatory factor analysis. Journal of Interprofessional Care, 28(2), 149–154.
Lai, N.M., Sivalingam, N., & Ramesh, J.C. (2007) Medical students in their final six months of training: progress in self-perceived clinical competence, and relationship between experience and confidence in practical skills. Singapore Medical Journal, 48 (11), 1018-1027.
Lapkin, S., Levett-Jones, T., & Gilligan, C. (2012). A cross-sectional survey examining the extent to which interprofessional education is used to teach nursing, pharmacy and medical students in Australian and New Zealand universities. Journal of Interprofessional Care, 26 (5), 390–396.
Leipzig, R., Hyer, K., Ek, K., Wallenstein, S., Vezina, M.L., Fairchild, S., …C.K., Howe, J.L.(2002). Attitudes toward working on interdisciplinary healthcare teams: a comparison by discipline. Journal of the American Geriatrics Society, 50, 1141–1148.
Lemieux-Charle, L. & McGuire, W.L. (2006). What do we know about health care team effectiveness? A review of the literature. Medical Care Research and Review, 63, 263-300.
Lim, P.C. & Lim, K. (2010). Evaluation of a pharmacist-managed diabetes medication therapy adherence clinic. Pharmacy Practice, 8(4),250-254. doi: 10.4321/S1886-36552010000400008.
Lindblom, P., Scheja, M., Torell, E., Astrand, P., & Felländer-Tsai, L. (2007). Learning orthopaedics: assessing medical students’ experiences of interprofessional training in an orthopaedic clinical education ward. Journal of Interprofessional Care, 21(4), 413-423.
Malone, D., Marriott, S., Newton-Howes, G., Simmonds, S., & Tyrer, P. (2007). Community mental health teams (CMHTs) for people with severe mental illnesses and disordered personality. Cochrane Database of Systematic Reviews, Issue 2. doi:10.1002/14651858.CD000270.pub2.
McAlister, F.A., Stewart, S., Ferrua. S., & McMurray, J.J. (2004). Multidisciplinary strategies for the management of heart failure patients at high risk for admission. Journal of the American College of Cardiology, 44, 810–819.
McCahan, J. (1986). Education in medicine. In J. Steel (Eds), Issues in Collaborative Practice (pp. 129–138). Orlando, Florida: Grune & Stratton.
Mendonca, J.M., Lyra, D.P., Rabelo, J.S., Siqueira, J.S., Balisa-Rocha, B.J., Gimenes F.R.E., & Bonjardim, L.R. (2010) Analysis and detection of dental prescribing errors at primary health care units in Brazil. Pharmacy World & Science, 32, 30-35.
Mickan, S.M. (2005). Evaluating the effectiveness of health care teams. Australian Health Review, 29(2), 211-217.
Morphet, J., Hood, K., Cant, R., Baulch, J., Gilbee, A., & Sandry, K. (2014) Teaching teamwork: an evaluation of an interprofessional training ward placement for health care students. Advances in Medical Education and Practice, 5, 197-204. doi: 10.2147/AMEP.S61189.
Orchard, C.A., Curran, V., & Kabene, S. (2005) Creating a culture of interdisciplinary. Medical Education Online [serial online], 10(11). Retrieved from https://www.researchgate.net/publication/239823451_Creating_a_Culture_for_Interdisciplinary_Collaborative_Professional_Practice.
Pollard, K., Miers, M., & Gilchrist, M. (2005). Second year scepticism: pre-qualifying health and social care students’ midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working, Journal of Interprofessional Care, 19(3): 251-268.
Rudland, J. & Mires, G. (2005). Characteristics of doctors and nurses as perceived by students entering medical school: Implications for shared teaching. Medical Education, 39, 448–455.
Saleem, F., Hassali, M.A., & Chow, E.P. (2015). Home Medication Review in Improving Patient Medication Adherence and Minimizing Medication Wastage among Type 2 Diabetes Patients. Health Economics & Outcome Research: Open Access. Retrieved from https://www.omicsonline.org/open-access/home-medication-review-in-improving-patient-medication-adherence-andminimizing-medication-wastage-among-type-2-diabetes-patients-heor-1000104.pdf.
Spence, L.H. & Weston, W. (1995). Role perceptions of freshman and senior nursing and medical students and attitudes toward collaborative decision making. Journal of Professional Nursing, 11, 119-128.
Suter, E., Arndt, J., Arthur, N., Parboosingh, J., Taylor, E., & Deutschlander, S. (2009) Role understanding and effective communication as core competencies for collaborative practice. Journal of Interprofessional Care, 23, 41-51.
Tanaka, M. & Yokode, M. (2005) Attitudes of medical students and residents toward multidisciplinary team approach. Medical Education, 39, 1255–1256.
Thistlethwaite, J. (2012). Interprofessional education: A review of context, learning and the research agenda. Medical Education, 46, 58-70.
Tunstall-Pedoe, S., Rink, E. & Hilton, S. (2003). Student attitudes to undergraduate interprofessional education. Journal of Interprofessional Care, 17(2), 161-172.
World Health Organization. (2010). WHO: Framework for action on interprofessional education and collaborative practice. Retrieved from http://apps.who.int/iris/bitstream/10665/70185/1/WHO_HRH_HPN_10.3_eng.pdf.
*Pei Se Wong
School of Pharmacy
International Medical University (IMU)
26, Jln Jalil Perkasa 19,
57000 Bukit Jalil,
Kuala Lumpur, Malaysia
Tel: +60 3-8656 7228
Fax: +60 3 8656 7229
Email: peise_wong@imu.edu.my
Published online: 2 January, TAPS 2018, 3(1), 15-26
DOI: https://doi.org/10.29060/TAPS.2018-3-1/OA1048
Yuen Teng Choo1, Mui-Ling Tan1, Cheong Hian Goh2 & Wai-Ping Yau1
1Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore, 2Health Products Regulation Group, Health Sciences Authority, Singapore
Abstract
Aim: To assess the importance of compounding training in today’s pharmacy education in Singapore, this study examined the perception of final year National University of Singapore (NUS) pharmacy undergraduates on compounding training in pharmacy education and their awareness of compounding services in Singapore in relation to compounding pharmacists’ perception, practice and role of pharmacy compounding in Singapore.
Methods: A cross-sectional survey was carried out between November 2013 and January 2014. It comprised of a questionnaire survey conducted on 134 final year pharmacy undergraduates, and face-to-face interviews conducted on 7 retail compounding pharmacists. Questionnaire responses were analysed using descriptive statistics, while the interviews were transcribed verbatim and analysed by thematic coding.
Results: Less than 40% of final year pharmacy undergraduates were aware of compounding activities and compounding pharmacies in Singapore. Nonetheless, majority agreed that compounding should be included in the pharmacy curriculum (83.6%) as it is an important part of pharmacy education (78.3%) and pharmacy profession (61.2%). All the interviewed compounding pharmacists felt that compounding in pharmacy education has provided them with the basics to build on knowledge and skills at work. Compounded medications were also viewed as necessary by 71.4% of the pharmacists in fulfilling the needs of certain patient populations.
Conclusion: Compounding training is necessary in pharmacy education. Pharmacy compounding has evolved from its traditional role into a professional speciality of customizing medications to meet different patient needs today. Hence, knowledge and skills in pharmacy compounding remain a relevant foundation for practising pharmacists to enhance pharmaceutical care at work.
Keywords: Pharmacy compounding; Pharmacy education; Pharmacy students; Compounding pharmacists; Perceptions; Survey
Practice Highlights
- Majority of the pharmacy undergraduates and retail compounding pharmacists surveyed considered compounding as an important part of pharmacy education and also an integral aspect of the pharmacy profession.
- Most of the retail compounding pharmacists felt that there was a place for compounding as a specialised service in Singapore to meet the needs of special populations and for individualised patient care.
- Students were more confident at preparing oral liquid preparations than topical preparations, but the latter were reported by retail compounding pharmacists as being more frequently compounded in practice.
- There is a need to build students’ confidence in compounding and to better prepare them to meet the needs of the compounding industry.
- Compounding training is necessary in pharmacy education.
I. INTRODUCTION
Pharmacy compounding is defined as the preparation of a patient-specific medication by a pharmacist in response to an individual prescription from a medical practitioner (Cauthon, Bowman, & Gurney, 2013). Traditionally, compounded medications are prepared for various reasons, from individual ingredients or by reformulating a medicinal product (Giam, McLachlan, & Krass, 2011). This includes instances where a product is made in response to a patient’s needs, e.g. allergy, or a more appropriate dosage form of the medicine formulated for improved patient compliance and administration. Over the years, the rise of mass drug manufacturing by the pharmaceutical industry has resulted in a drop in compounding of medications (Cauthon et al., 2013; Giam, McLachlan, & Krass, 2012). However, though demand was low, pharmacy compounding persisted especially when not all patients’ needs were met by manufactured medications, such as the non-suitability of manufactured products for certain patient groups and the unavailability of certain products in the market (Cauthon et al., 2013; Eley & Birnie, 2006; Mullarkey, 2009; Pegues, 2006).
Today, there appears to be resurgence in pharmacy compounding as a specialised service offered in more pharmacies, especially in Australia and the United States (U.S.) where pharmacy compounding accounts for about 1% of the prescription needs (Cauthon et al., 2013; Giam et al., 2012; Wilson, Blythe, & Sharfstein, 2012). It has been suggested that an increasing trend in the provision of compounding services by pharmacies was linked to the greater role that pharmacists can now play in the therapy of patients with the use of compounded medications (Giam et al., 2012; Maine, 2008). This resulted in improved communication and collaboration between pharmacists, and both doctors and patients, leading to greater professional satisfaction of pharmacists who provide this specialised service (Giam et al., 2012; Maine, 2008).
Compounding is incorporated in the curriculum of pharmacy schools in many countries (Aspden et al., 2011). In Singapore, formal training on compounding also remains by and large an integral aspect of the pharmacy curriculum. However, little is known about the compounding scene, such as the demand for compounded products in Singapore, or the relevance for pharmacists to be equipped with such skills in pharmacist professional training. Nonetheless, pharmacists are the only healthcare professionals with formal training in the knowledge and skills of compounding, and pharmacy compounding still remains an inherent part of the profession (Eley & Birnie, 2006; Mullarkey, 2009; Shrewsbury et al., 2012).
In order to assess the importance of compounding training in today’s pharmacy education in Singapore, the perspectives of both undergraduates in the pharmacy course as well as pharmacists working in compounding pharmacies need to be considered. This study thus examined the perception of final year National University of Singapore (NUS) pharmacy undergraduates on compounding training in pharmacy education and their awareness of compounding services in Singapore in relation to compounding pharmacists’ perception, practice and role of pharmacy compounding in Singapore. By gathering the views of graduating pharmacy students and practising pharmacists, the course content in pharmacy education can be tailored to meet the needs of the compounding industry in Singapore.
II. METHODS
A. Study Design
A cross-sectional study, comprising of a self-administered questionnaire survey and a face-to-face interview, was conducted from November 2013 to January 2014.
B. Questionnaire Survey
1) Study population: The target group was final year pharmacy undergraduates in NUS, which is the only university providing professional pharmacy education in Singapore. These students had completed all compounding modules in the curriculum, and with prior pharmacy practice experience (i.e. completed 6-week preceptorship programme in retail and hospital settings, respectively). Based on a 95% confidence level, proportion of 0.5 and a ±5% precision level, the minimum sample size targeted was 109 students out of the class size of 150.
2) Survey instrument: A self-designed questionnaire with 16 closed- and open-ended questions was used to gather information on students’ experience in compounding outside of the curriculum, as well as their awareness of compounding services and opinions on compounding in pharmacy education in Singapore. The questionnaire was first pilot-tested on three registered/pre-registration pharmacists who completed the questionnaires and provided feedback to improve the ease of understanding the questions. Results from the pilot test were not included in the final analysis.
3) Questionnaire administration: The voluntary, anonymous survey questionnaire was self-administered by final year NUS pharmacy undergraduates at the end of a pharmacy lecture. Questionnaires were completed and collected back on the spot.
C. Interview Survey
1) Study population: The target group was compounding pharmacists who worked in retail pharmacies whose mainstay of the business was compounding. These pharmacists were included as their job scope was primarily on pharmacy compounding. Pharmacists who carried out some compounding activities in hospitals and pharmaceutical companies were excluded.
Potential pharmacies that largely provided compounding services were identified from an online search on the open access Infosearch portal of the Health Sciences Authority of Singapore (http://eservice.hsa.gov.sg/prism/common/enquirepublic/SearchPharmacy.do?action=load). Retail compounding pharmacies were included after confirmation of their provision of compounding service through phone calls. All 11 pharmacists working at these included pharmacies were then approached in person and invited to participate in this study.
2) Survey instrument: Interviews with the pharmacists were conducted using a 16-question semi-structured interview guide that centred on pharmacy compounding. It was adapted with slight modification from a previous study (Giam et al., 2012) to obtain information on retail compounding pharmacists’ education, career, challenges, motivations and opinions, and their pharmacy operations. The interview guide was first pilot-tested on three registered/pre-registration pharmacists who were interviewed and provided feedback to improve the ease of understanding the questions. Results from the pilot test were not included in the final analysis.
3) Conduct of interview: For consistency, all the interviews were conducted by one trained investigator (YTC). Face-to-face interviews with the pharmacists were conducted at their retail compounding pharmacies during non-peak hours. Field notes were taken during the interviews and the interviews were also audio-recorded for pharmacists who consented to recording. Written informed consent was obtained from the interviewed pharmacists for participation in the interview and audio-recording, respectively.
D. Data Analysis
Data was analysed using IBM SPSS Statistics software (version 21). Descriptive statistics and chi-square tests were conducted. Statistical significance was set at p<0.05. Data from the interviews were transcribed verbatim and analysed by thematic coding.
III. RESULTS
A. Questionnaire Survey
1) Demographics of respondents surveyed: 139 final year pharmacy undergraduates were issued the questionnaire, out of which 134 completed questionnaires were received (response rate: 96.4%). The respondents have all participated in some form of pharmacy-related activities through either the pharmacy preceptorship programme or via their own work or internship experiences (Table 1).
2) Awareness of compounding activities and compounding pharmacies: Overall, most students (73.1%) were unaware of the existence of compounding pharmacies in Singapore. Only 38.1% (n=51) came across compounding activities in pharmacies, which were mainly during their hospital preceptorship programme (41/51, 80.4%). It is also interesting to note that most (84.3%) were unaware of contemporary issues in compounding, specifically the fungal meningitis outbreak associated with the use of contaminated compounded medication in the U.S. (Wilson et al., 2012).
3) Opinions on compounding in pharmacy education and practice: 83.6% of the students felt that compounding should be included in the pharmacy curriculum, with the top 2 reasons mentioned being that compounding is a traditional and exclusive specialised skill of pharmacists and that compounding skills will be useful when practising as a pharmacist (Table 2). Most also agreed that compounding is an important part of pharmacy education (78.3%) and pharmacy profession (61.2%) (Figure 1A).
Most students indicated that the time devoted to teaching compounding (67.9%), the breadth (76.9%) and depth (63.4%) of content taught in compounding, as well as the compounding knowledge (70.1%) and skills (68.7%) acquired, were just right in the NUS pharmacy curriculum (Table 3). Majority indicated that they understood the benefits (82.9%) and risks (80.6%) associated with compounded medications (Figure 1A). In addition, more than half of the respondents agreed that they have the knowledge (53.7%) and skills (60.4%) needed to compound medications (Figure 1A). Nonetheless only a minority felt that they were able to compound medications of good quality (32.1%) and ensure their compounded medications are free from contamination (17.9%) (Figure 1A).
Of the compounded formulations learnt in the NUS pharmacy curriculum, most respondents felt that suspensions (91.8%), solutions (87.3%) and extemporaneous preparations using commercially available products (79.9%) were relevant in pharmacy practice (Figure 1B). While most felt confident in compounding solutions (84.3%) and suspensions (79.1%), comparatively fewer students were confident in compounding extemporaneous preparations using commercially available products (64.1%) (Figure 1C). It is also interesting to note that although 70.9% of pharmacy undergraduates did feel that skin preparations, such as creams, gels and lotions, were relevant in pharmacy practice (Figure 1B), only around 60% have the confidence to compound them (Figure 1C). In addition, while more than half of the respondents (53.8%) felt that sterile preparations were relevant in pharmacy practice (Figure 1B), only 24.6% indicated that they were confident in compounding sterile preparations (Figure 1C).
When asked if the respondents would be interested in taking an advanced elective course in compounding if available, only slightly less than half (47.0%) were interested (Table 2). Those who felt that the time spent teaching compounding and that the breadth and depth of compounding taught were too little tend to express interest in taking this advanced elective course in compounding (p<0.05) (Table 3). Among those who were not interested in an advanced elective compounding course, the top 3 reasons mentioned were that it may not be relevant to future practice, they had other interests, and compounding taught in current pharmacy curriculum is sufficient (Table 2).
4) Place for compounding as a specialised service: 44.8% of the respondents felt that there is a place for compounding as a specialised service in Singapore, mainly because they saw the benefits of having compounded medications for special populations or for individualised patient care (Table 2). In contrast, among the 55.2% who felt that there was no place for compounding as a specialised service in Singapore, their main reason was that most products are commercially available or can be manufactured or prepared using machines in advance (Table 2).
| Demographics | n | (%) |
| Final year pharmacy undergraduates (n=134): | ||
| Gender | ||
| Male | 58 | (43.3) |
| Female | 76 | (56.7) |
| Participation in pharmacy-related activitiesa | ||
| Preceptorship I (Retail pharmacy)
Preceptorship I (Polyclinic pharmacy) Preceptorship II (Hospital pharmacy) Overseas work experience in a pharmacy Internship in industry |
115
20 123 13 12 4 |
(85.8)
(14.9) (91.8) (9.7) b (9.0) c (3.0) |
| Retail compounding pharmacists (n=7): | ||
| Gender | ||
| Male | 2 | (28.6) |
| Female | 5 | (71.4) |
| Age | ||
| ≤ 40 years | 5 | (71.4) |
| > 40 years | 2 | (28.6) |
| Pharmacy training | ||
| Locally trained | 6 | (85.7) |
| Foreign trained | 1 | (14.3) |
| Length of pharmacy course underwent | ||
| 3 years | 2 | (28.6) |
| 4 years | 5 | (71.4) |
| Years of working experience, median (range) | 11 | (4 – 47) |
| Previous work experience | ||
| Retail only | 2 | (28.6) |
| Retail and polyclinic | 1 | (14.3) |
| Retail and hospital | 1 | (14.3) |
| Retail and industry | 1 | (14.3) |
| Retail, hospital and industry | 2 | (28.6) |
a Each respondent could indicate more than one category from this list.
b Hospital pharmacy: 11 (8.2%); Retail pharmacy: 1 (0.7%); Charity organisation: 1 (0.7%)
c Taiwan: 7 (5.2%); United States: 3 (2.2%); Canada: 1 (0.7%); Not specified: 1 (0.7%)
Table 1. Demographics of final year pharmacy undergraduates surveyed (n=134) and retail compounding pharmacists interviewed (n=7)
B. Interview Survey
1) Demographics of respondents interviewed: Of the 11 retail compounding pharmacists approached, 7 accepted the interview (response rate: 63.6%). The other four pharmacists declined to participate as they were too busy (n=3) or not comfortable with sharing proprietary information of the pharmacy in an interview (n=1). Of the pharmacists interviewed, their years of working experience varied widely from 4 to 47 years (median=11 years) (Table 1). All pharmacists had previous work experience in retail pharmacies.
2) Compounding training in pharmacy education: All 7 pharmacists believed that pharmacy education provided them with the basics in compounding (Table 4): ‘…it sets a foundation… if I were not in pharmacy school, you wouldn’t know the properties of chemicals, what they do and how, so basically you can’t compound things or make things in terms of any way I want to.’ (Pharmacist 3). 71.4% also felt that compounding was a specialised skill that pharmacists were trained in.
While it is generally agreed that compounding is an integral aspect of pharmacy education, there were differences in opinions among the responses on how well pharmacy education has prepared them for compounding in pharmacy practice (Table 4). The depth of content taught in compounding or the time devoted to teaching compounding was insufficient to some pharmacists (28.6%) but just right to other pharmacists (28.6%). 42.9% of the respondents also felt that the clinical aspect of pharmacy was viewed as more important presently and more focused on compared with compounding training in pharmacy education (Table 4).
| n | (%) | |
| Do you think compounding should be included in the pharmacy curriculum? Why? | ||
| Yes (n=112; 83.6%) | ||
| · A traditional, exclusive specialised skill of pharmacists. | 33 | (29.5) |
| · Compounding skills may/ will be useful someday when practising as a pharmacist. | 32 | (28.6) |
| · Compounding knowledge and/ or skills are essential/ important/ good to know as part of pharmacy education. | 27 | (24.1) |
| · There are benefits of having compounded medications (e.g. for special populations, for individualised patient care). | 18 | (16.1) |
| · Interesting/ fun. | 16 | (14.3) |
| No (n=22; 16.4%) | ||
| · Most products are/ can be manufactured or prepared using machines in advance. | 7 | (31.8) |
| · Compounding appears to be uncommon in Singapore. | 5 | (22.7) |
| · Time-consuming/ inefficient. | 5 | (22.7) |
| · Can be trained at work. | 1 | (4.5) |
| · Compounding in the pharmacy curriculum is not necessary. | 1 | (4.5) |
| · Manufacturing, rather than compounding, can ensure products of good quality. | 1 | (4.5) |
| · There could be risk of contamination with compounded medications. | 1 | (4.5) |
| If an elective to provide students with a more advanced course in compounding is available, will you be interested in taking the module? Why? | ||
| Yes (n=63; 47.0%) | ||
| · Sounds interesting and/ or fun. | 34 | (54.0) |
| · Aids professional development/ enrichment through improving knowledge and honing skills in compounding. | 18 | (28.6) |
| · Provides compounding skills that may/ will be needed someday when practising as a pharmacist. | 12 | (19.0) |
| · Compounding is an important part of pharmacy education. | 2 | (3.2) |
| No (n=71; 53.0%) | ||
| · Compounding does not seem relevant/ applicable/ important to future practice. | 19 | (26.8) |
| · Not interested in taking advanced course in compounding/ have other interests that do not involve compounding/ pharmacy. | 17 | (23.9) |
| · Compounding taught in current pharmacy curriculum is sufficient. | 13 | (18.3) |
| · The current workload in school is too heavy/ takes up too much time already. | 7 | (9.9) |
| · Not a hands-on person. | 4 | (5.6) |
| · Not interested in pursuing compounding in future career. | 4 | (5.6) |
| · Taking this advanced elective course may affect academic results. | 3 | (4.2) |
| Do you think there is a place for compounding as a specialised service in pharmacy practice in Singapore? Why? | ||
| Yes (n=60; 44.8%) | ||
| · There are benefits of having compounded medications (e.g. for special populations, for individualised patient care). | 22 | (36.7) |
| · It is a specialised skill that pharmacists are trained in. | 10 | (16.7) |
| · It is a niche market with potential. | 9 | (15.0) |
| · Have seen compounding as a specialised service in Singapore. | 5 | (8.3) |
| · Compounding skills may/ will be useful someday when practising as a pharmacist. | 4 | (6.7) |
| No (n=74; 55.2%) | ||
| · Most products are commercially available/ can be manufactured or prepared using machines in advance. | 28 | (37.8) |
| · Demand for compounding service is low. | 13 | (17.6) |
| · Compounding is time-consuming/ inefficient/ technically challenging. | 8 | (10.8) |
| · Compounding appears to be uncommon/ not widely used in Singapore. | 7 | (9.5) |
| · Compounding is outsourced to companies or carried out by pharmacy technicians instead of pharmacists now. | 3 | (4.1) |
| · There are other areas of pharmacy that are more important these days and should be focused on. | 3 | (4.1) |
| · Manufacturing, rather than compounding, can ensure products of good quality and efficacy. | 2 | (2.7) |
| · Pharmacists not interested in compounding. | 1 | (1.4) |
a For each question, some respondents provided more than one reason while some did not indicate specific reasons(s).
Table 2. Identified reasons for opinions provided by final year pharmacy undergraduates (n=134) on compounding in pharmacy education and practicea
| Statements | Interested in taking advanced elective course in compounding if available | ||||||
| Overall | Yes | No | |||||
| (n=134) | (n=63) | (n=71) | |||||
| n | (%) | n | (%) | n | (%) | p value | |
| Time devoted to teaching compounding | < 0.0005* | ||||||
| Too little | 22 | (16.4) | 20 | (31.7) | 2 | (2.8) | |
| Just right | 91 | (67.9) | 41 | (65.1) | 50 | (70.4) | |
| Too much | 21 | (15.7) | 2 | (3.2) | 19 | (26.8) | |
| Breadth of content taught in compounding | 0.007* | ||||||
| Too little | 19 | (14.2) | 14 | (22.2) | 5 | (7.0) | |
| Just right | 103 | (76.9) | 47 | (74.6) | 56 | (78.9) | |
| Too much | 12 | (9.0) | 2 | (3.2) | 10 | (14.1) | |
| Depth of content taught in compounding | 0.005* | ||||||
| Too little | 40 | (29.9) | 27 | (42.9) | 13 | (18.3) | |
| Just right | 85 | (63.4) | 34 | (54.0) | 51 | (71.8) | |
| Too much | 9 | (6.7) | 2 | (3.2) | 7 | (9.9) | |
| Compounding knowledge acquired | 0.149 | ||||||
| Too little | 31 | (23.1) | 18 | (28.6) | 13 | (18.3) | |
| Just right | 94 | (70.1) | 43 | (68.3) | 51 | (71.8) | |
| Too much | 9 | (6.7) | 2 | (3.2) | 7 | (9.9) | |
| Compounding skill set acquired | 0.151 | ||||||
| Too little | 35 | (26.1) | 21 | (33.3) | 14 | (19.7) | |
| Just right | 92 | (68.7) | 40 | (63.5) | 52 | (73.2) | |
| Too much | 7 | (5.2) | 2 | (3.2) | 5 | (7.0) | |
* p < 0.05: results are statistically significant.
Table 3. Opinions of final year pharmacy undergraduates (n=134) on compounding in the NUS pharmacy curriculum in relation to their interest in taking an advanced elective course in compounding if available
(A)
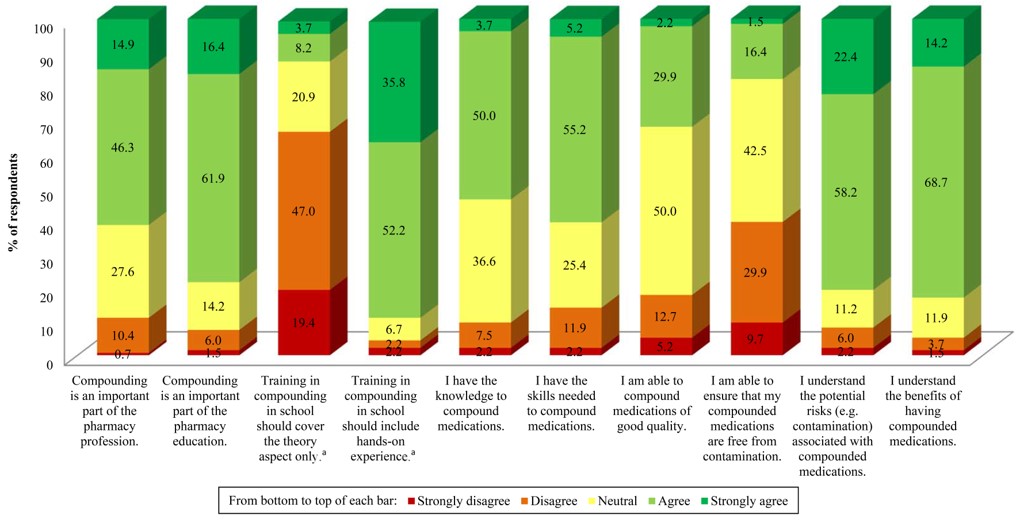
a Numbers do not add up to 100% due to non-response of participants.
(B)
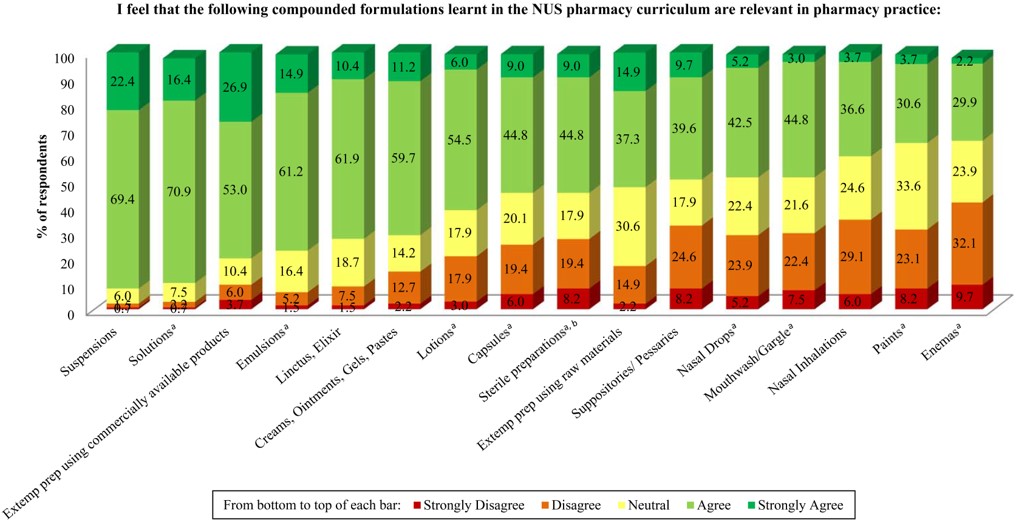
a Numbers do not add up to 100% due to non-response of participants.
b Examples provided in questionnaire: Aseptic solution preparation in ampoules, ophthalmic solutions
(C)
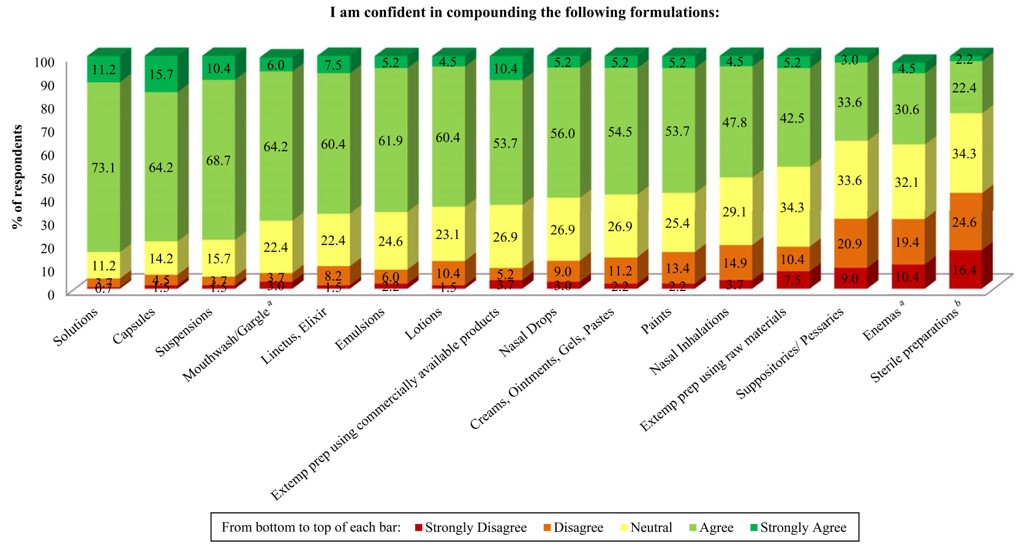
a Numbers do not add up to 100% due to non-response of participants.
b Examples provided in questionnaire: Aseptic solution preparation in ampoules, ophthalmic solutions
Figure 1. Opinions of final year pharmacy undergraduates (n=134) on: (A) statements related to compounding in pharmacy education, (B) the relevance of compounded formulations learnt in the NUS pharmacy curriculum to pharmacy practice, and (C) their confidence in compounding different formulations learnt in the NUS pharmacy curriculum.
| Themes | Responses | n | (%) |
| Compounding training in pharmacy education | · Compounding taught in school set the basics/ formed a foundation. | 7 | (100.0) |
| · It is a specialised skill that pharmacists are trained in. | 5 | (71.4) | |
| · Clinical aspect of pharmacy was deemed more important these days and more focused on than compounding. | 3 | (42.9) | |
| · Compounding in school prepared me well. | 3 | (42.9) | |
| · Compounding in school prepared me minimally. | 2 | (28.6) | |
| Knowledge of compounding in pharmacy practice | · Acquired compounding knowledge and skills outside school from: | ||
| o Experiences/ on-the-job | 7 | (100.0) | |
| o References/ resources | 5 | (71.4) | |
| o Other pharmacists at work | 4 | (57.1) | |
| o External training | 2 | (28.6) | |
| o Customers’ feedback | 1 | (14.3) | |
| o Suppliers of ingredients | 1 | (14.3) | |
| · Knowledge gained in school is lost after years without/ having no avenues for application. | 5 | (71.4) | |
| Motivations in choosing compounding as an area of specialty | · Interesting. | 4 | (57.1) |
| · Ability to customise medications for patients’ needs. | 3 | (42.9) | |
| · Compounding is a traditional and exclusive role of pharmacists. | 3 | (42.9) | |
| · A hands-on type of person. | 1 | (14.3) | |
| · Niche market. | 1 | (14.3) | |
| Challenges faced | · Meeting expectations of patients and doctors. | 5 | (71.4) |
| · A lot of time required to make the preparations. | 4 | (57.1) | |
| · Building up vast amount of knowledge in compounding. | 4 | (57.1) | |
| · Obtaining raw materials. | 2 | (28.6) | |
| · Creating awareness/ interest in compounding services. | 2 | (28.6) | |
| Compounding operations and practices | · Checking and counterchecking by pharmacists during compounding. | 7 | (100.0) |
| · Average shelf-life of compounded products is 6 months. | 7 | (100.0) | |
| · Compounding is a very manual process. | 6 | (85.7) | |
| · Low volume of sales of commercially available medications. | 6 | (85.7) | |
| · Standard practices in place to maintain adequate hygiene levels. | 6 | (85.7) | |
| · Specialisation of products compounded: | |||
| o Skin care | 4 | (57.1) | |
| o Bio-identical hormones | 2 | (28.6) | |
| Common dosage forms compounded | · Skin preparations (e.g. creams, gels, lotions). | 7 | (100.0) |
| · Capsules. | 3 | (42.9) | |
| · Oral liquid preparations (e.g. solutions). | 1 | (14.3) | |
| · Inhalations. | 1 | (14.3) | |
| · Troche. | 1 | (14.3) | |
| Place for compounding as a specialised service in Singapore | · Compounding as a specialised service in Singapore: | ||
| o There is a place for compounding as a specialised service. | 5 | (71.4) | |
| o There is no place for compounding as a specialised service. | 2 | (28.6) | |
| · Demand and awareness for compounding service is low among doctors and patients. | 6 | (85.7) | |
| · There are benefits of having compounded medications (e.g. for special populations, for individualised patient care). | 5 | (71.4) | |
| · Doctors must want compounded medications for patients/ doctors make the final decision. | 4 | (57.1) | |
| · Compounding appears to be uncommon in Singapore. | 4 | (57.1) | |
| · Potential for compounding in skin care to take off. | 3 |
(42.9) |
Table 4. Responses of retail compounding pharmacists interviewed (n=7)
3) Compounding in pharmacy practice: After graduation, the main method of acquiring compounding knowledge and skills for these pharmacists was through on-the-job training to gain more experience (Table 4). On the initial challenges faced when first working in pharmacy compounding, 71.4% of the pharmacists (n=5, all were less than 40 years old) expressed that the compounding knowledge gained in school was mostly forgotten, as they had not applied the knowledge for years since graduation: ‘…after like a few years later and ask you to do a cream and I suddenly forget like how do I start doing it.’ (Pharmacist 4). On the other hand, the pharmacists who were more than 40 years old (n=2) and had the opportunities to compound right after graduation mentioned that the knowledge and skills of compounding did not pose a challenge to them initially. The more senior pharmacists further commented that compounding was part and parcel of their competence as a pharmacist.
Within the operations of the pharmacies, checking and counterchecking during the process of compounding was an integral aspect of the practice of all compounding pharmacists interviewed (Table 4). Compounding was generally described as a very manual process in many of the pharmacies (85.7%).
The most common dosage forms compounded by all the pharmacists interviewed were mainly creams and topical preparations (Table 4): ‘I used to have some mixtures but not anymore. Now is mostly external.’ (Pharmacist 5). Oral liquid dosage forms such as solutions were only mentioned by one (14.3%) pharmacist. No sterile compounding was said to be carried out at all of their facilities: ‘We do not have sterile facilities so we do not make ophthalmic preparations. No injections too.’ (Pharmacist 7). On a side note, 85.7% of the pharmacists mentioned that their pharmacies handled low volume of sales of commercially available medications.
4) Place for compounding as a specialised service: 71.4% of the pharmacists felt that there was a place for compounding as a specialised service in Singapore as compounded medications can provide for the individual and specific needs of patients (Table 4). While 85.7% felt that the demand and awareness of compounding service was low, its relevance was nonetheless highlighted: ‘I think it is here to stay although it would not be so big like compounding pharmacies everywhere. It is still viable; there are still people who have the needs for it.’ (Pharmacist 6).
IV. DISCUSSION
In Singapore, only licensed retail pharmacies can compound medications in accordance to a doctor’s prescription. Pharmacy compounding is traditionally a manual process, and it is important to understand the training of pharmacists in these operations. In this study, pharmacy students and compounding pharmacists provided useful feedback on their academic training and knowledge in pharmacy compounding. It is interesting to note that final year NUS pharmacy undergraduates and retail compounding pharmacists share common views regarding compounding training in pharmacy education and pharmacy practice, as well as whether there is a place for compounding as a specialised service in Singapore.
A. Compounding in Pharmacy Education and Practice
In this study, most final year pharmacy undergraduates and retail compounding pharmacists considered compounding as an important part of pharmacy education and also an integral aspect of the pharmacy profession as it is a specialised skill that pharmacists were trained in. This is in agreement with the results in an Arizona study where 95% of 412 pharmacists surveyed agreed that compounding is an important part of the pharmacy profession and 99% indicated that some aspects of compounding should be taught in pharmacy school (Cauthon et al., 2013).
Over the years, with a switch in the approach in pharmacy education and practice from product-focused to patient-centred care, clinical knowledge appeared to have a more important position in education (Maine, 2008; Ryan et al., 2008), as commented by some surveyed pharmacists and undergraduates. Despite this, compounding itself was reported to lead to greater patient-centred care as opposed to using commercial products for reasons such as the ability to provide individualised medications and develop stronger professional relationship with patients (Cauthon et al., 2013; McPherson & Fontane, 2010). Indeed, compounding skills are still considered important to be imparted to pharmacy students in many pharmacy schools globally (Aspden et al., 2011). From an American Association of Colleges of Pharmacy (AACP) survey study that evaluated compounding education within the curriculum of its member institutions, all 137 respondents unanimously supported the inclusion of compounding education as part of the curriculum in pharmacy school (Shrewsbury et al., 2012), showing the importance of imparting compounding knowledge and skills to pharmacy students.
The AACP study reported that compounding education was included at an average of 2.2 semesters (range: 0-6 semesters) in the pharmacy curriculum of the respondents’ institutions, with the time spent on a single compounding laboratory exercise ranging from ≤2.5 hours to ≥6 hours (Shrewsbury et al., 2012). In the NUS undergraduate pharmacy curriculum at the point of this study, compounding education was included in 6 semesters in total in the 4-year pharmacy curriculum in NUS (i.e. 6 out of 8 semesters), with a 3-hour laboratory session per week for around 6 weeks spent on compounding exercises for most modules. Hands-on compounding laboratory sessions were incorporated in Pharmacy Practice I and III, Pharmacy Law, and Dosage Form Design I, II and III modules. In this regard, most undergraduates surveyed generally agreed that the amount of time devoted to compounding and the content of compounding taught in the NUS curriculum is just right. The component of compounding training has continued to be included in the revamped NUS undergraduate pharmacy curriculum starting August 2014.
While school provided the basics in compounding, all the interviewed pharmacists gained the knowledge and skills they needed through experience at work and learning on the job. Nonetheless, the knowledge and skills from pharmacy education was still important to the pharmacists interviewed. It served as a starting point to allow them to take up compounding at work: ‘Of course pharmacy education prepared me before I can do all this.’ (Pharmacist 3). The knowledge gained on the job mainly served to supplement what was taught to pharmacy undergraduates to improve their knowledge and skills in compounding: ‘The basic skills like I said, was from my time in school, but NUS course is very basic. For more advanced skills, it’s mainly on the job…’ (Pharmacist 6). Indeed, 71.4% of the pharmacists also stated that compounding knowledge gained in school is lost when not used for many years after graduation. This was also shown in some studies whereby pharmacy students do not retain all the compounding knowledge and skills they learnt over the course (Eley & Birnie, 2006), and often after graduation, additional training is required during actual practice at work (Kairuz, Noble, & Shaw, 2010). However with sufficient time, the knowledge and skills can be easily recalled once again: ‘…not very familiar with this skill because we have not touched them for a very long time but after a while it’s still quite okay.’ (Pharmacist 4), clearly highlighting the importance of building a foundation in compounding in school.
In our study, both undergraduate students and practising pharmacists perceived compounding to be interesting and can provide for patients’ needs, and in line with the traditional role of pharmacists in compounding. These motivations to compound were largely similar with studies in Australia and the U.S., which also encompassed aspects of developing a stronger professional relationship with the patients and the professional satisfaction derivable by the pharmacists providing the service (Giam et al., 2011, 2012; McPherson & Fontane, 2010).
Our undergraduate students were most confident in compounding oral liquid dosage forms, such as suspensions and solutions, which they felt were most relevant in practice. These were also the most commonly compounded preparations in pharmacy schools in the U.S. (Shrewsbury et al., 2012). In practice, however, the pharmacists interviewed in our study indicated that skin preparations, especially creams, were more commonly compounded instead. Similarly, community pharmacists providing compounding services in the U.S. reported that the most common preparations compounded were first and foremost also dermatological preparations for localised effects (ointments, creams and gels) (90.7%), followed by oral solutions (73.2%) and suspensions (70.4%) (Martin et al., 2009).
In terms of sterile compounding in the curriculum, at least half of the pharmacy undergraduates felt that sterile preparations were relevant to pharmacy practice, even though not all were equally confident in compounding these preparations. This may be due to the range of sterile preparations compounded within the NUS pharmacy curriculum which was not as comprehensive as that in the curriculum of U.S. pharmacy schools. The latter included compounding of a wide range of sterile preparations including intravenous solutions (both small and large volume parenterals), ophthalmic and otic solutions, and chemotherapy in biological safety hood as part of their required course (Shrewsbury et al., 2012). While sterile compounding may not apply in the retail setting as mentioned by the pharmacists interviewed, such skills remain relevant to the compounding industry, especially in hospitals and specialized institutions. Indeed, the AACP study has stressed on the importance of sufficiently training students in sterile compounding within the pharmacy curriculum (Shrewsbury et al., 2012).
B. Place for Compounding
Based on the students’ and practising pharmacists’ perspectives, compounding does not appear to be common in Singapore. According to the pharmacists interviewed, it seems that the demand and awareness for compounding services is low among the doctors and patients. Nonetheless, majority of the pharmacists felt that there was a place for compounding as a specialised service in Singapore to meet the requirements of specific patients. This underscores the need to create greater awareness among doctors and patients, and even pharmacy undergraduates, that there are compounding pharmacists who are capable of compounding alternative options for patients’ therapy apart from commercially available products.
C. Significance of Findings
Our study revealed two findings that are significant to the educational institution. Nearly 30% of students reported to feeling only minimally prepared to compounding and they were more confident at preparing oral liquid preparations (e.g. solutions) than topical preparations (e.g. creams), but the latter were reported by retail compounding pharmacists as being preparations that are more likely to be compounded in practice. These findings serve as feedback to assist with curriculum design. There is a need to build students’ confidence in compounding and to better prepare them to meet the needs of the compounding industry.
D. Strengths and Limitations
As our study focused on retail compounding pharmacists, the results may not be generalizable to the entire compounding industry in Singapore, which extends to the hospitals as well. In addition, the interview was limited by the small sample size due to the inherent small number of pharmacists practising in retail compounding pharmacies. Nonetheless, the study does capture a representative view of the pharmacists from retail compounding pharmacies, with a total response rate of 63.6%. In addition, having the opinions of the undergraduates help supplement that of the pharmacists to provide a more comprehensive evaluation of the importance and relevance of compounding training in pharmacist professional education.
V. CONCLUSION
Compounding in pharmacy education provides pharmacists with the basic skills needed for future careers in compounding. Such training is still emphasized in many pharmacy schools around the world, albeit dedicating different content and depth in the curriculum time.
Like other aspects of pharmacist professional training, the knowledge and skills in compounding may be honed on-the-job as pharmacists gain experiences in compounding in their career. However, without the basics to start them off on, they would not know where to begin. Even if they thought they had forgotten most of what they learnt in school when they started working in the compounding pharmacies, they were still able to recall with time and pick up the knowledge and skills again. The findings in this study strongly reiterate the need for the continued role of compounding training in the curriculum of pharmacist professional education.
The basics imparted have allowed the pharmacists to move on to advance their knowledge and skills to enhance pharmaceutical care at work. Compounding does not belong to the past. While the true potential of compounding in Singapore seems unclear, doctors continue to work with pharmacists to seek alternatives to commercialised products for their patients. Compounded medications continue to fulfil different patient needs today and pharmacists must be adequately trained and competent to provide this specialised service. Indeed, there is a place for compounding training in pharmacy education in Singapore.
Notes on Contributors
Ms. Yuen Teng Choo, BSc (Pharm) (Hons), is currently a pharmacist at Ng Teng Fong General Hospital. She conducted this research study while she was an Honours year undergraduate student with the Department of Pharmacy at the National University of Singapore.
Ms. Mui-Ling Tan, MSc (Healthcare Management), is a Senior Lecturer at the Department of Pharmacy, National University of Singapore, and a registered pharmacist in Singapore. She teaches pharmacy professional skills and pharmacy law. As coordinator for professional placement, she also manages the pre-employment clinical training (PECT) programme for pharmacy undergraduates.
Dr. Cheong Hian Goh, PhD, is a registered pharmacist in Singapore and is currently Deputy Director of the GDP Unit at the Audit and Licensing Division of the Health Products Regulation Group of Health Sciences Authority (HSA), Singapore. He is also a preceptor to pharmacy undergraduates undergoing PECT at HSA.
Dr. Wai-Ping Yau, PhD, is a Lecturer at the Department of Pharmacy, National University of Singapore, and a registered pharmacist in Singapore. She teaches pharmacokinetics, pharmacostatistics and research methodology. She is also a member of the committee overseeing the pharmacy experiential program in service-oriented undergraduate learning (SOUL) for pharmacy students.
Ethical Approval
The study protocol was approved by the NUS Institutional Review Board.
Acknowledgements
This work was supported by the National University of Singapore Department of Pharmacy (Project Grant C-148-000-003-001).
Declaration of Interest
Authors have no conflicts of interest, including no financial, consultant, institutional and other relationships that might lead to bias.
References
Aspden, T. J., Anderson, C., Rew, A., Tan, J., Woodrow, R., & Zheng, Y. (2011). An investigation into the teaching of extemporaneous compounding skills to pharmacy students in schools of pharmacy in Australia, Canada, New Zealand, South Africa and the United Kingdom. Paper presented at the 9th International Conference: Life Long Learning in Pharmacy, Rotorua, New Zealand.
Cauthon, K. A., Bowman, B. J., & Gurney, M. K. (2013). Compounding practices and beliefs of Arizona pharmacists. International Journal of Pharmaceutical Compounding, 17(2), 154-161.
Eley, J. G., & Birnie, C. (2006). Retention of compounding skills among pharmacy students. American Journal of Pharmaceutical Education, 70(6), 132.
Giam, J. A., McLachlan, A. J., & Krass, I. (2011). Community pharmacy compounding–impact on professional status. International Journal of Clinical Pharmacy, 33(2), 177-182.
Giam, J. A., McLachlan, A. J., & Krass, I. (2012). Characterizing specialized compounding in community pharmacies. Research in Social & Administrative Pharmacy, 8(3), 240-252.
Kairuz, T., Noble, C., & Shaw, J. (2010). Preceptors, interns, and newly registered pharmacists’ perceptions of New Zealand pharmacy graduates’ preparedness to practice. American Journal of Pharmaceutical Education, 74(6), 108.
Maine, L. L. (2008). A Contemporary Perspective on Compounding Education. International Journal of Pharmaceutical Compounding, 12(3), 279.
Martin, K. S., McPherson, T. B., Fontane, P. E., Berry, T., Chereson, R., & Bilger, R. (2009). Independent community pharmacists’ perspectives on compounding in contemporary pharmacy education. American Journal of Pharmaceutical Education, 73(3), 54.
McPherson, T., & Fontane, P. (2010). Patient-centered care in the community-based compounding practice setting. Journal of the American Pharmacists Association, 50(1), 37-44.
Mullarkey, T. (2009). Pharmacy compounding of high-risk level products and patient safety. American Journal of Health-System Pharmacy, 66(17 Suppl 5), S4-S13.
Pegues, D. A. (2006). Improving and enforcing compounding pharmacy practices to protect patients. Clinical Infectious Diseases, 43(7), 838-840.
Ryan, M., Shao, H., Yang, L., Nie, X. Y., Zhai, S. D., Shi, L. W., & Lubawy, W. C. (2008). Clinical pharmacy education in China. American Journal of Pharmaceutical Education, 72(6), 129.
Shrewsbury, R., Augustine, S., Birnie, C., Nagel, K., Ray, D., Ruble, J., Scolaro, K., & Athay Adams, J. (2012). Assessment and recommendations of compounding education in AACP member institutions. American Journal of Pharmaceutical Education, 76(7), S9.
Wilson, L. E., Blythe, D., & Sharfstein, J. M. (2012). Fungal meningitis from injection of contaminated steroids: A compounding problem. JAMA, 308(23), 2461-2462.
* Wai-Ping Yau
Department of Pharmacy
Faculty of Science
National University of Singapore
18 Science Drive 4
Singapore 117543, Singapore
Tel: 6516 8913
Fax: 6779 1554
Email: phaywp@nus.edu.sg
Published online: 2 January, TAPS 2018, 3(1), 6-14
DOI: https://doi.org/10.29060/TAPS.2018-3-1/OA1050
Ryne W. Dougherty1, Cody C. Wyles2, Wojciech Pawlina3 & Nirusha Lachman3
1Department of Radiology, University of Michigan, United States; 2Department of Orthopaedic Surgery, Mayo School of Graduate Medical Education, Mayo Clinic, United States; 3Department of Anatomy, Mayo Clinic College of Medicine and Science, Mayo Clinic, United States
Abstract
In the current healthcare environment, team-based models in the teaching and practice of medicine have become more a norm than a preference. Renewed focus on team-based practice discloses the effect that poorly functioning teams may have on successful outcomes in team-based delivery of patient care. Team incompetence compromises learning and work performance for all members; an outcome often rooted in poor communication and understanding of role responsibilities within the team. Business schools have been innovative and proactive in recognizing this problem and have instituted team charters to align team expectations and norms through discussion and consensus. Team charters were introduced in Block 2 Microscopic Anatomy and Block 3 Human Structure courses at Mayo Medical School in the first year curriculum. Teams were oriented on the concept of the team-charter and given the opportunity to create individual team charters to suit each team’s work ethos. Teams were encouraged to revisit their charters midway through the course to maintain a dynamic contract. Students took time to reflect on and adapt their strategy in order to facilitate better team cohesiveness, communication, interaction and ultimate performance. Qualitative student feedback indicated that the exercise fostered better group dynamic and improved communication within the team. Students were empowered to take responsibility for their own learning, professional identity formation, performance, academic development and their impact on total performance of the team.
Keywords: Gross anatomy education; Medical education; Team-based learning; Team charters; Assessment
Practice Highlights
- Concept of team charters adopted from business schools can be used to facilitate team-based learning strategies in basic science courses in medical curriculum.
- Team charters help engage students in development of non-traditional discipline-independent skills within the team setting.
- Team charters are the most effective when they are adopted and valued among team members
- Process of designing custom team charters reinforces student’s sense of accountability for their own learning and provides a welcomed infrastructure for internal management of team dynamics and productivity.
I. INTRODUCTION
The notion that the “team is more than just the sum of its parts” (Siassakos et al., 2010) has never been more pertinent than in the current healthcare environment where team-based models in the teaching and practice of medicine are now more a norm than a preference, (Siassakos et al., 2010). Renewed focus on team-based practice discloses the effect that poorly functioning teams may have on successful outcomes in team-based delivery of patient care. Team incompetence compromises learning and work performance for all members an outcome often rooted in the lack of clarity in communication and role responsibilities within the team, (Sutcliff, Lewton, & Rosenthal, 2004).
To align with the goals of healthcare delivery, medical educators have acknowledged the importance of teamwork and modern day curricula tend to build student learning environments within structured team-based models, (Dodge, Sherwood, & Shomaker, 2012; Pershing & Fuchs, 2013; Snyderman, Eibling, & Johnson, 2011. While the Accreditation Council for Graduate Medical Education (ACGME) lists “interpersonal skills and communication skills” and “system-based practice” as two of the six core competencies that are widely accepted in medical school curricula, the importance of teamwork, while not officially listed, has gained increasing attention with a drive to integrate this concept into the framework of curricular educational models. In both 2011 and 2012, Academic Medicine’s Question of the Year focused on promoting team behaviour in medical school so they can be utilized in the new practice settings (Dodge et al., 2012; Snyderman et al., 2011).
Historically, curricular improvements were aimed at improving two different ACGME core competencies, “professionalism” and “medical knowledge.” Professionalism has been promoted through active management of the hidden curriculum of medical schools and careful selection of role models (Derstine, 2002; Elliott et al., 2009; Hafferty, 1998; Maudsley, 2001; Wiseman, Bradwejn, & Westbroek, 2014). While professionalism remains difficult to define, there have been frameworks created with specific behaviours and actions to promote among students (Arnold, Blank, Race, & Cipparrone, 1998; Jones, Hanson, & Longacre, 2004). Basic science educators and in particular, anatomists, have taken an active role in fostering professional development of students during undergraduate medical training (Escobar-Poni & Poni, 2006; Pawlina, 2006). Through a focus on acquisition and development of non-traditional discipline-independent skills (also called non-technical skills in clinical disciplines, which includes teamwork, communication, leadership skills) along with peer and faculty feedback, “professionalism”, has been effectively promoted as a core competency in many anatomy classes (Camp et al., 2010; Evans & Pawlina, 2015). Similarly for “medical knowledge” competencies anatomists have been progressive by directing learning innovations toward more active student learning initiatives and participation through technology (audience response systems), increased imaging access, and utilization of near-peer teachers (Alexander, Crescini, Juskewitch, Lachman, & Pawlina, 2009; Bulte, Betts, Garner, & Durning, 2007; Drake & Pawlina, 2014; Lachman, Christensen, & Pawlina, 2013; Solomon & Crowe, 2001; Vasan, DeFouw, & Holland, 2008).
However, while anatomy programs have been successful in including assessments of non-traditional discipline-independent skills into their grading systems, they have not as yet been successful in providing students with effective guidance on how to facilitate these skills for their own growth and for that of their peers. Near-peer teachers have long held the reputation of being particularly effective in relating to their junior counterparts since both TAs and students enjoy positive growth shared experience of medical knowledge and professionalism (Erie, Starkman, Pawlina, Lachman, 2013; Evans & Cuffe, 2009). The perspectives gained from more senior students who have been through the same course have become an invaluable resource in determining implementations for improvement in course delivery. Anatomy faculty striving to incorporate ACGME requirements into the curriculum are often challenged by limited opportunity to provide meaningful instruction on development of non-traditional discipline-independent skills (Evans & Pawlina, 2015). While this challenge is felt by faculty, the impact of this limitation is more strongly felt by the student who is being evaluated not only by faculty, but also by peers and themselves; and without a bar by which to support their perceptions and expectations, students are left challenged by their inability to reconcile the outcome of their performance.
Difficulties with varying norms are encountered frequently in business relations and thus have been the subject of extensive research. Traditionally, the business world has made significant contributes to medical education including the audience response system and the team-based learning approach (Collins, 2008; Michaelsen, Fink, & Knight, 1997). Most business research utilizes classical Tuckman’s team development framework (Tuckman, 1965). Tuckman asserts that teams grow through the following steps:
- Forming: Team members avoid conflict as they establish a routine;
- Storming: Conflicts emerge within the team as members grapple for position and acceptance of their ideas;
- Norming: Members agree on roles and standards; and
- Performing: Team focuses on completing the task.
Following a review of this framework in late 1970s, a fifth stage, “adjourning,” was added to address the final phase of group disengagement, separation and termination (Tuckman & Jensen, 1977). The last stage of group dismantling after task is completed may trigger insecurity and anxiety related to separation and often contains elements of self-reflection by members of the group (Lacoursiere, 1974; Spitz & Sadock, 1973). Team performance decreases during the storming phase, but recovers during the norming phase to ultimately peak in the performing phase (Kozlowski & Bell, 2013; Tuckman, 1965). Unfortunately, it is known that not all teams completely progress through these steps and can become derailed in the storming stage. In addition, some individual members of the team are prone to use less effort on a task if they are in a team versus when they work alone. This effect refers to as “social-loafing” and has been identified across teams and in different work populations (Kozlowski & Bell, 2013). There are known interventions (i.e., implementing transparency in identifying each team member individual contributions, or providing clear performance standards) that significantly decrease tendency to engage in social loafing (Kozlowski & Bell, 2013; Latané, Williams, & Harkins, 1979; Liden, Wayne, Jaworski, & Bennett, 2004). Many of the factors that eliminate social loafing also serve to enhance team performance, a process known as “social facilitation” (Bond & Titus, 1983). The decrease in team performance is particularly concerning in short educational courses, such as the current trend for condensed / reduced hours, basic science courses where team development needs to occur quickly, a problem that extends into medical practice as fluctuating personal often creates short-lived teams centred on patients.
As a possible solution to such problems, in addition to approaches for social facilitation, research in the business field proposes the strategy of using a “team charter”. A “team charter” is a document developed by all team members to outline team-specific norms on tangible manifestations of professionalism and teamwork (e.g., attendance, tardiness, participation), (Cox & Bobrowski, 2000; Mathieu & Rapp, 2009). Recently, the Harvard Business Review provided guidance on specific characteristics of great teams (Pentland, 2012). These include equal brief contributions by all team members, maintaining high energy, interpersonal relationships between all team members and their interaction with other teams (Pentland, 2012). At Mayo Medical School, basic science courses are delivered primarily within a team-based environment where non-traditional discipline-independent skills are emphasized through evaluation of team performance. As part of our commitment to quality improvement, course evaluations from the previous year are reviewed and discussed with upcoming teaching assistants (TAs) during the Student-as-Teacher program which prepares TAs for their teaching responsibilities (Erie et al., 2013; Lachman et al., 2013). Input of near peers (upcoming TAs) provides a more informed and authentic needs assessment of issues identified in students’ evaluations. Anatomy teaching faculty decided to engage students in taking ownership for their learning experience and concomitant development of non-traditional discipline-independent skills by developing custom created “team charters” to guide their team-based experience. The aim of this paper is to present a method for implementing team charters in a first year medical school team-based anatomy course.
II. METHODS
The Block 2 Histology and Block 3 Human Structure (Gross Anatomy) courses within the Mayo Medical School curriculum, employs an exclusively team-based learning approach in facilitation of the course objectives. The courses themselves are delivered by a team of core faculty and TAs in the Department of Anatomy (Erie et al., 2013; Lachman et al., 2013).
By providing students the opportunity to establish norms on common areas of contention and define characteristics of what they viewed as an effective team, faculty hoped to improve students experience of team-work and appreciation of team dynamics during 13 weeks of working within the same team. Based on a review of the approaches used in the business field to improve team interaction, the concept of the “team-charter” was introduced prior to the start of the course (Block 2-Histology) with its perceived benefits of guiding students in their pursuit of assuming ownership for their learning experience.
Class size consisted of a total of 52 students divided into 13 groups of 4 students each. In order to maintain at best, a fair distribution and balance of academic merit and social factors, teams of four were structured using criteria that included academic performance scores, college background, home-town, previous experience with course content, gender, under-representative minority and curricular track (MD or MD/PhD). The design and finalization of the teams were conducted by the core teaching faculty without input from TAs.
Expectations for team-based learning were highlighted to students as follows:
- Understanding that teams differ fundamentally from working groups because they require both individual and mutual accountability.
- Understanding that teams rely on more than group discussion, debate, decision and on more than just sharing information and performance on formative feedback based activities.
- Understanding that team’s performance and outcomes (e.g., assignments, bed-side presentations, autopsy report, embryology brochure) are achieved through the joint contributions of all their members.
- Understanding that the role of the assigned team leader is to facilitate team activities and direct the team in maximizing the talents of individuals within the team.
- Understanding that providing and receiving feedback for personal and team enhancement is a responsibility of every individual within the team.
Evaluation criteria for successful completion of the course were highlighted in Table 1 as follows:
| Component of the final grade | Percentage (%) of value | Type of assessment | Description |
| Written assessments in the classroom | |||
| Written examination | 30 | Individual | Course examination based on course assignments |
| NBME® subject examination | 10 | Individual | Standardized board subject examination on Gross Anatomy and Embryology |
| Audience response system quizzes | 10 | Mixed (individual and group) | Daily sessions that consist of clinical questions that explore clinical reasoning based on acquired anatomy knowledge |
| Embryology brochure | 5% | Group | Embryology brochure for lay public information produced by a team is assessed by course faculty and member of public education department. |
| Practical assessments in the laboratory | |||
| Practical examination | 20 | Individual | Identification of tagged structures with second and third order questions. |
| Quality of dissection | 2.5 | Group | Weekly evaluation of assigned dissection by faculty and teaching assistants |
| Bed side presentations | 2.5 | Group | Assessment of presentation related to dissected cadaver evaluated by faculty and teaching assistants. |
| Peer and Faculty evaluations | |||
| Peer evaluation | 10 | Individual | Score is provided by the team members based on overall teammate contribution to the learning process of peer evaluator. |
| Faculty evaluation | 10 | Individual | Derived from debriefing session of faculty and teaching assistants |
Table 1. Summary of final grade calculation for block 3 human structure anatomy course.
- Anatomy Written Assessments (40%): written examination includes material from assigned self-directed learning, briefing sessions, laboratory exercises, discussions, peer teaching, embryology, radiology, Ultrasound Mini Institute (Smither, Bhagra, Lachman, & Pawlina, 2014), and other assignments during the block. This category also includes standardized National Board of Medical Examiners® (NBME®) Gross Anatomy and Embryology Subject Examination (10%) score.
- Laboratory Practical Examination (30%): includes tagged structures and radiologic images (ultrasound, CT, x-rays). In addition, a result from a daily audience response quizzes which include clinical questions related to the dissected region in the laboratory (10%).
- Quality of dissection evaluations (2.5%): structure identification and subjective quality. Six structures are to be identifiable to TAs/faculty each week. These structures should be visible through adequate dissection. Quality of dissection is evaluated in a subjective manner by TAs and faculty according to a 4-point scale (Nwachukwu, Lachman, & Pawlina, 2015).
- Group projects (7.5%): include both the patient education embryology pamphlet (5%) and the bed-side presentation (2.5%). Goals for these assignments align with the goals for Improving the Public Health Block (Chock, Lachman, Havyer, & Pawlina, 2014) and patient communication skills (Lachman & Pawlina, 2015). The cadaver is presented as a patient in the hospital, while on internal medicine rounds. The goal of this assignment is to get the team accustomed to presenting a patient with a specific chief complaint, an underlying medical condition, and different comorbidities. The embryology brochure is prepared with guidance from Mayo Clinic Patient Education Department to present scientific material in lay language in order to improve doctor-patient communication skills (Evans, 2008).
- Peer and faculty evaluations (20%): include laboratory peer assessment score (based on Michaelsen’s method), which represents the average percent value calculated from the sum of points assigned by each team member (Levine, 2008). For 10% of the score, students are expected to assign a score to teammates based on their own assessment how their teammates contributed to their own learning and to overall team performance during the course. Students are asked to distribute a total of 60 points among their peers with differentiation among their ratings. Evaluation is subjective and includes qualitative feedback and justification for highest and lowest ratings. Faculty assessment is provided on a 5-point scale (where 5 = exceeds expectation and 1 = needs improvement) which is based on faculty and teaching assistants assessments of professionalism, leadership, teamwork, and other non-technical skills.
Evaluation criteria for non-traditional discipline-independent skills were highlighted as follows:
The following standards were applied to the format for all evaluation data collected through peer evaluation, leadership evaluation, self-evaluation and faculty evaluation (Lachman & Pawlina, 2015).
- Respect: Demonstration of personal commitment to honouring the choices and rights of others.
- Integrity: Demonstration of commitment to honesty and trustworthiness in evaluating and demonstrating own skills and abilities.
- Responsibility: Demonstration of the ability to accept responsibility for own actions and decisions without blaming others.
- Compassion: Demonstration of adequate appreciation of other person’s special needs for comfort and provides support without overt emotional involvement.
- Commitment to Excellence: Demonstration of adequate commitment to the pursuit of excellence and continuous quality improvement.
III. RESULTS
A. Defining the team charter for anatomy teams
In order to orientate students on the guiding principles for the construction of a team charter, the following guidelines for the formulation of a framework were presented during outlines of the objectives for team based learning (Table 2).
B. Timeline for Formulation and Implementation of Team Charter
- STEP 1
Introduction and creation of team charter: Two weeks before the commencement of Block 2, the course, a short presentation was given explaining the purpose of the team charter and highlighting the areas where students should focus their discussions.
- STEP 2
Student Meeting: Students met in their assigned teams (made available to them at the start of the academic year) and developed their charters before the start of Block 2 Histology course. Team Charters were emailed to the instructors in order to increase accountability.
- STEP 3
Creation of team charter framework: To guide discussion toward positive behaviours and previous areas of contention, a framework (Table 2) was provided for each individual team to develop and customized for its own needs. This framework included elements from “Characteristics of Successful Teams”, exit interviews from previous students, and faculty experience (Pentland, 2012). There were eight main categories including: goals, norms, decision making, participation, attendance, interruptions, team socialization and conflicts.
- STEP 4
Implementation of team charter: The course appoints a rotating team leader who was primarily responsible for implementing the charter. Near-peer teachers and peers evaluated the leaders on their ability to promote the team-specific policies. At the end of the leadership block, leaders were given specific feedback on their success in promoting or how to better promote the charter. During near peer lead feedback sessions, leaders were able to reflect on these results with their instructors.
- STEP 5
Revision of team charter: A mid-block review of the team charter was encouraged with a re-alignment of expectations at the point of transition from Block 2 to Block 3. Teams were required to meet and revise their charter based on their experience of team interaction and usefulness of their charter as they proceeded into the next block where the expectations for team-based productivity were higher.
According to course evaluation qualitative metrics, the team charter concept, was recognized as largely “helpful in guiding team expectations” by many students. However, it was also perceived unfavourably by some as “adding more paperwork” to their already heavy workload.
| Key Principles | Guidelines |
| Goals | What are the team’s goals (academic performance, dissection time, lab reviews) and objectives? How will the team keep members motivated during the block? How will the team reward itself (and individual members) for a job well done? |
| Norms | What behaviours are permissible?
How do we deal with inappropriate humour? How do we deal with people who dominate, resist, are too quiet or noisy, etc.? How will we monitor our progress? What important roles need to be assumed by team members during the fall? How will these roles (dissection leader, radiology liaison, clean up leader) be assigned? |
| Decision Making | How do we make decisions?
What decisions must be agreed to by all? What does consensus mean? Who will ask when we get stuck (another team, TA, professor, first available)? |
| Participation | What do we mean by participation?
How do we encourage equal participation? Are there group norms that we can establish to encourage participation? |
| Attendance:
|
How often should we meet?
How we address flat contributions? How long should our meetings be? When is it OK to miss a meeting? How will be responsible when we do not complete a dissection to return and complete it? Since team meetings should start on time, how do we deal with lateness? What does “on time” mean? |
| Interruptions:
|
How do we deal with interruptions?
What is allowed? Phone calls? Messages? |
| Team socializing:
|
Do we have food or coffee?
Who cleans up? How many breaks should we have? How much socializing is permissible? |
| Conflict:
|
How will the team encourage positive/creative conflict and discourage negative/dysfunctional conflict?
How can the team encourage and manage differences of opinion and different perspectives? |
Table 2. Framework for the development of team charters
IV. DISCUSSION
A. Perspectives and Experience on Implementation of Team Charters
Student feedback at the end of the course suggested that the introduction of team charters made a positive impact on teamwork experience within the first year gross anatomy course. The revision of the charter was critical for team functioning and teams that did not take the time to consciously review their charters appeared to face challenges in team productivity during Block 2, when the course demands and student expectations were greater.
Scholarly contributions from the field of business education reinforce that effective team performance requires more than simply bringing students together to accomplish common goals (Hunsaker, Pavett, & Hunsaker, 2011; Mathieu & Rapp, 2009). Even though students, and in particular, medical students may have the capacity to accomplish tasks individually, effective execution as a team requires additional organizational skill.
According to Mathieu & Rapp (2009) team effectiveness is dependent on a team member’s ability to manage “two major tracks of activities: task work and teamwork”. Both “what” students are doing and “how” students are accomplishing goals translates to effective teamwork. In the current anatomy curriculum, these skills are imperative for ensuring that students stay on task in a fast paced educational delivery format. Teams who are unable to complete dissection goals for the day, often end up having to dedicate many more hours after class, creating imbalance in other shared academic responsibilities. When team charters are used effectively, a sense of accountability amongst team members provides an important source of motivation for achieving team goals.
As anticipated, the course was not without its challenges and faculty intervention was instituted for groups that required additional support in alleviating their discordance. However, based on our impression of the dynamic within the overall team-based learning environment, we believe that the accountability that came with creation of the team charter may have played a role in decreasing the need for faculty intervention in team performance measures during the gross anatomy course. Business practitioners and business education specialists, consider the use of team charters as a valuable exercise for establishing norms and a foundation for teamwork. When used appropriately within the educational setting team charters empower partnerships and fosters shared decision making, responsibility and identification of individual strengths, essential to meeting designated milestones in curricular competencies (Aaron, McDowell, & Herdman, 2014).
Effectiveness of the team charter in improving team dynamic, communication skills, effort, mutual support, cohesion, and bringing clarity to team expectations needs to be quantitatively measured through establishing any correlation that might exist between successful charter implementation and revision with other measurable outcomes of learning and team dynamics (Aaron et al., 2014).
Student and TA feedback have been helpful in understanding student comfort level with creation and implementation of the team charter. By maintaining a dynamic charter students were able to reflect on behaviours and performance strategies within the safety of their team environment. Open communication improves team’s conversational capacity by promoting balanced, candid, non-defensive dialogue about difficult to approach situations. According to Weber (2013), a team with high conversational capacity is known to perform well, maintaining focus even through the uncertainty of unanticipated events. The ownership for facilitation of team charters is a best suited responsibility for the near peer teacher who is able to meet the student at the level of comfort needed to encourage open communication. Near peer feedback is also a valuable and essential tool in helping students recognize their own strengths and areas for improvement as they relate to their near peers own past experience of the course. Facilitating non-technical skills in basic science education remains one of the more challenging objectives. Small interventions aimed at providing benchmarks to implement better understanding of what these skills are and how to recognize them will inadvertently provide students with capacity to enhance them.
B. Limitations
This paper is not based on any quantitative measure of effectiveness of implementing team charters in the gross anatomy course. The practice of creating a team charter was instituted as a means of providing students with a document of accountability for team interaction and responsibilities. Future studies may be designed to measure use of the team charter against overall team performance both on cognitive and non-technical levels. Additionally, as we continue to use the team charter student feedback will be used to improve student orientation and expectations. As a next step, team charters may be used to provide more structured student-near peer interaction time for feedback and debriefing.
V. CONCLUSION
The team charters initiative provided a novel framework for facilitating team-based learning in basic science courses. While we acknowledge that student reaction to this task was both positive and challenging for some, we believe that the process of designing custom team charters reinforced student’s sense of accountability for their own learning and provided a welcomed infrastructure for internal management of team dynamics and productivity.
Notes on Contributors
Ryne W. Dougherty, MD is a second year-resident of interventional radiology in the Department of Radiology at University of Michigan, Ann Arbor, MI, United States. He was instrumental in introducing team charter concept into Human Anatomy didactic block.
Cody C. Wyles, MD is the second-year resident of orthopaedics in the Department of Orthopaedic Surgery at Mayo School of Graduate Medical Education, Mayo Clinic, Rochester, MN, United States.
Wojciech Pawlina, MD is a professor of anatomy and medical education and Chair of the Department of Anatomy at Mayo Clinic College of Medicine and Science, Mayo Clinic, Rochester, MN, United States. He teaches anatomy and histology to first-year medical students, residents and fellows.
Nirusha Lachman, PhD is a professor of anatomy in the Department of Anatomy at Mayo Clinic College of Medicine and Science, Mayo Clinic, Rochester, MN, United States. She teaches histology and anatomy to first-year medical students, residents, and fellows and is course director for the Surgical First Assistant Anatomy course.
Ethical Approval
This study was considered exempt by the Mayo Clinic Institutional Review Board (protocol number 14-005364).
Acknowledgements
The authors have no additional acknowledgements
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
Aaron, J. R., McDowell, W. C., & Herdman, A. O. (2014). The effects of a team charter on student team behaviors. Journal of Education for Business, 89, 90–97.
Alexander, C. J., Crescini, W. M., Juskewitch, J. E., Lachman, N., & Pawlina, W. (2009). Assessing the integration of audience response system technology in teaching of anatomical sciences. Anatomical Sciences Education, 2, 160–166.
Arnold, E. L., Blank, L. L., Race, K. E., & Cipparrone, N. (1998). Can professionalism be measured? The development of a scale for use in the medical environment. Academic Medicine, 73, 1119–1121.
Bond, C. F., & Titus, L. J. (1983). Social facilitation: A meta-analysis of 241 studies. Psychological Bulletin, 94, 265–292.
Bulte, C., Betts, A., Garner, K., & Durning, S. (2007). Student teaching: Views of student near-peer teachers and learners. Medical Teacher 29, 583–590.
Camp, C. L., Gregory, J. K., Lachman, N., Chen, L. P., Juskewitch, J. E., & Pawlina, W. (2010). Comparative efficacy of group and individual feedback in gross anatomy for promoting medical student professionalism. Anatomical Sciences Education, 3, 64–72.
Chock, M., Lachman, N., Havyer, R., & Pawlina, W. (2014). The anatomy of public health: Integrating population health in the anatomy lab. FASEB Journal 28, S536.14.
Collins, J. (2008). Audience response systems: Technology to engage learners. Journal of the American College of Radiology, 5, 993–1000.
Cox, P. L., & Bobrowski, P. E. (2000). The team charter assignment: Improving the effectiveness of classroom teams. Journal of Behavioral and Applied Management, 1, 92–103.
Derstine, P. L. (2002). Implementing goals for non-cognitive outcomes within a basic science course. Academic Medicine, 77, 931–932.
Dodge, C., Sherwood, E. J., & Shomaker, T. S. (2012). Organizational performance and teamwork: Achieving interactive excellence. Academic Medicine, 87, 1474.
Drake, R. L., & Pawlina, W. (2014). Multimodal education in anatomy: The perfect opportunity. Anatomical Sciences Education, 7, 1–2.
Elliott, D. D., May, W., Schaff, P. B., Nyquist, J. G., Trial, J., Reilly, J. M., & Lattore, P. (2009). Shaping professionalism in pre-clinical medical students: Professionalism and the practice of medicine. Medical Teacher, 31, e295–e302.
Erie, A. J., Starkman, S. J., Pawlina, W., & Lachman, N. (2013). Developing medical students as teachers: An anatomy-based Student-as-Teacher program with emphasis on core teaching competencies. Anatomical Sciences Education, 6, 385–392.
Escobar-Poni, B., & Poni, E. S. (2006). The role of gross anatomy in promoting professionalism: A neglected opportunity! Clinical Anatomy, 19, 461–467.
Evans, D. J. (2008). Designing patient-focused information: An opportunity for communicating anatomically related information. Anatomical Sciences Education, 1, 41–45.
Evans, D. J., & Cuffe, T. (2009). Near-peer teaching in anatomy: An approach for deeper learning. Anatomical Sciences Education, 2, 227–233.
Evans, D. J., & Pawlina, W. (2015). The role of the anatomist in teaching of nontraditional discipline-independent skills. In L. K. Chan & W. Pawlina W (Eds). Teaching Anatomy: A Practical Guide (pp 319–329). New York, NY: Springer International Publishing.
Hafferty, F. W. (1998). Beyond curriculum reform: Confronting medicine’s hidden curriculum. Academic Medicine, 73, 403–407.
Hunsaker, P., Pavett, C., & Hunsaker, J. (2011). Increasing student-learning team effectiveness with team charters. Journal of Education for Business, 86, 127–139.
Jones, W. S., Hanson, J. L., & Longacre, J. L. (2004). An intentional modeling process to teach professional behavior: Students’ clinical observations of preceptors. Teaching and Learning in Medicine, 16, 264–269.
Kozlowski, S. W., & Bell, B. S. (2013). Work groups and teams in organizations: Review update. In N. W. Schmitt , S. Highhouse, I. B. Weiner (Eds). Handbook of Psychology: Vol. 12. Industrial and Organizational Psychology (pp 412–469). Hoboken, NJ: John Wiley & Sons, Inc.
Lachman, N., Christensen, K. N., & Pawlina, W. (2013). Anatomy teaching assistants: Facilitating teaching skills for medical students through apprenticeship and mentoring. Medical Teacher, 35, e919–e925.
Lachman, N., & Pawlina, W. (2015). Peer and faculty assessment of nontraditional discipline-independent skills in gross anatomy. In L. K. Chan & W. Pawlina W (Eds). Teaching Anatomy: A Practical Guide (pp 299–309). New York, NY: Springer International Publishing.
Lacoursiere, R. (1974). A group method to facilitate learning during the stages of a psychiatric affiliation. International Journal of Group Psychotherapy, 24, 342–351.
Latané, B., Williams, K., & Harkins, S. (1979). Many hands make light work: The causes and consequences of social loafing. Journal of Personality and Social Psychology, 37, 822–832.
Levine, R.E. (2008). Peer Evaluation in team-based learning. In L. K. Michaelsen, D. X. Parmelee, K. K. McMahon, & R. E. Levine (Eds). Team-Based Learning for Health Professions Education: A Guide to Using Small Groups for Improving Learning (pp. 103–116). Sterling, VA: Stylus Publishing, LLC.
Liden, R., Wayne, S. J., Jaworski, R. A., & Bennett, N. (2004). Social loafing: A field investigation. Journal of Management, 30, 285–311.
Mathieu, J. E., & Rapp, T. L. (2009). Laying the foundation for successful team performance trajectories: The roles of team charters and performance strategies. Journal of Applied Psychology, 94, 90–103.
Maudsley, R.F. (2001). Role models and the learning environment: Essential elements in effective medical education. Academic Medicine, 76, 432–434.
Michaelsen, L. K., Fink, L. D., & Knight, A. (1997). Designing effective group activities: Lessons for classroom teaching and faculty development. To Improve the Academy, 16, 373-397.
Nwachukwu, C., Lachman, N., & Pawlina, W. (2015). Evaluating dissection in the gross anatomy course: Correlation between quality of laboratory dissection and students outcomes. Anatomical Sciences Education, 8, 45–52.
Pawlina, W. (2006). Professionalism and anatomy: How do these two terms define our role? Clinical Anatomy, 19, 391–392.
Pentland, A. (2012). The new science of building great teams. Harvard Business Review, 90, 60–69.
Pershing, S., & Fuchs, V. R. (2013). Restructuring medical education to meet current and future health care needs. Academic Medicine, 88, 1798–1801.
Siassakos, D., Draycott, T. J., Crofts, J. F., Hunt, L. P., Winter, C., & Fox, R. (2010). More to teamwork than knowledge, skill and attitude. International Journal of Obstetrics & Gynaecology, 117, 1262–1269.
Smither, F., Bhagra, A., Lachman, N., & Pawlina, W. (2014). The mini ultrasound institute: Does incorporating ultrasound in the anatomy curriculum increase students’ understanding of living anatomy and comfort with new technology? FASEB Journal 28, S211.4.
Snyderman, C. H., Eibling, D. E., & Johnson, J. T. (2011). The physician as team leader: New job skills are required. Academic Medicine, 86, 1348.
Solomon, P., & Crowe, J. (2001). Perceptions of student peer tutors in a problem-based learning programme. Medical Teacher, 23, 181–186.
Spitz, H., & Sadock, B. (1973). Psychiatric training of graduate nursing students: Use of small interactional groups. New York State Journal of Medicine, 73, 1334–1338.
Sutcliffe, K. M., Lewton, E., & Rosenthal, M. M. (2004). Communication failures: An insidious contributor to medical mishaps. Academic Medicine, 79, 186–194.
Tuckman, B. W. (1965). Developmental sequence in small groups. Psychological Bulletin, 63, 384–399.
Tuckman, B. W., & Jensen, M. A. (1977). Stages of small-group development revisited. Group & Organization Studies, 2, 419–427.
Vasan, N. S., DeFouw, D. O., & Holland, B. K. (2008). Modified use of team-based learning for effective delivery of medical gross anatomy and embryology. Anatomical Sciences Education, 1, 3–9.
Weber, W. (2013). Conversational Capacity: The Secret to Building Successful Teams that Perform when the Pressure is on. Columbus, OH: McGraw-Hill.
Wiseman, L., Bradwejn, J., & Westbroek, E. M. (2014). A new leadership curriculum: The multiplication of intelligence. Academic Medicine, 89, 376–379.
*Wojciech Pawlina, M.D.
Department of Anatomy
Mayo Clinic College of Medicine and Science
Mayo Clinic
Rochester, MN. USA
Email: pawlina.wojciech@mayo.edu
Published online: 2 May, TAPS 2018, 3(2), 38-46
DOI: https://doi.org/10.29060/TAPS.2018-3-2/OA1041
Michiko Goto1, Junji Haruta2, Ai Oishi3, Kazue Yoshida4, Kenji Yoshimi5, Yousuke Takemura1,6 & Hisashi Yoshimoto7
1Department of Education and Research in Family and Community Medicine, Mie University Graduate School of Medicine, Tsu, Japan; 2Department of General Medicine and Primary Care, University of Tsukuba Hospital, Tsukuba, Japan; 3Primary Palliative Care Research Group, Usher Institute of Population Health Sciences and Informatics, University of Edinburgh Medical School, Edinburgh, UK; 4Department of Adult Health and Psychiatric Nursing, Faculty of Mie University, Tsu, Japan; 5Department of Contemporary Sociology, School of Sociology, Bukkyo University, Kyoto, Japan; 6Department of Family Medicine, Mie University School of Medicine, Mie, Japan, 7General Medicine and Primary Care, University of Tsukuba, Faculty of Medicine, Tsukuba, Japan
Abstract
Background: With the rapid aging of the population, collaboration among the various medical professions throughout the country is becoming increasingly indispensable in Japan. To promote collaboration in medical care, it is necessary to introduce the concept of collaboration to students at an early stage of their professional education. Despite this need, there are no core medical, healthcare and welfare education curricula in Japan that include interprofessional education (IPE). Therefore, the status of IPE in Japanese schools of medicine and other healthcare-related services is unclear.
Methods: We sent 3,430 questionnaires to 13 schools of medicine and related healthcare providers: doctors, nurses, physical therapists, registered dieticians, dentists, dental hygienists, social workers, pharmacists, occupational therapists, clinical psychologists, medical administrators, certified care workers, and speech therapists. The items addressed implementation rate of IPE, teaching methods and grading methods.
Results: Of the 3,430 surveys distributed, 572 completed surveys were returned (response rate 17%). Of the completed surveys, 493 qualified as valid, resulting in a final response rate of 14%. Only 19% (n = 93) of the analysed medical educational institutions included IPE instruction in their curricula.
Conclusion: While many educational institutions were conducting IPE, there were important inter-institutional differences with respect to attitudes towards IPE, teaching methods, and evaluation methods. This study was unprecedented in scale, and provides important basic information for the future development of IPE in Japan.
Keywords: Interprofessional Education, Healthcare Professions, Teaching Methods, Grading Methods, Collaboration
Practice Highlights
- IPE is being implemented in about 19% of the educational institutions contacted, and is represented in 13 medical, healthcare and social
- Of the 13 represented professions, all implemented IPE in at least some of their participating schools.
- The greatest proportion (68%) of IPE was delivered through group learning.
- Essays were the most frequent (65%) evaluation method used in IPE.
I. INTRODUCTION
The Japanese population is aging at an unparalleled rate, whereas birth rates are declining (Cabinet Office, 2011). The population aged 65 years and older is now over 30 million. The Ministry of Health, Labour and Welfare estimates that the population aged 65years and older in Japan will peak at approximately 39 million people in 2042, and the percentage of the population that is 75 years or older will continue to increase after that point. Therefore, by 2025, the ministry aims to establish an Integrated Community Care System (ICCS) comprising medical care, nursing care, disease prevention, housing, and support in daily living (Ministry of Health, Labour and Welfare, 2016). This system would enable older people to live out their lives in their local communities according to their own values.
Because the ICCS is interprofessional by nature, there is a need for professionals who can promote collaboration among medical, healthcare, and welfare services (Hughes et al., 1992; Janssonc, Isacsson & Lindholm, 1992; Lemieux-Charles & McGuire, 2006). Training of professionals with such abilities is urgently required. Under the motto “learning together,” the World Health Organization stresses the importance of training health workers who can respond to the health needs of the people they serve while working in an interprofessional team to optimise available resources (Gilbert, Yan, & Hoffman, 2010; World Health Organization [WHO], 1988). To achieve this, education within individual specialties is insufficient. Rather, it is essential that the idea of collaborating with various specialties is introduced into the early stage of students’ professional education (Subcommittee on Elderly Health, Committee on Health/Human Life Science, Science Council of Japan, 2011). The need for such human resource development is not a unique issue to Japan; it is a global issue considering that the population aging is a worldwide problem.
The UK and Australia have well-known examples of advanced interprofessional education (IPE) (Barr, Marion, D’Avray, & Thistlethwaite, 2013; The Interprofessional Curriculum Renewal Consortium, Australia, 2013). In Asia, Singapore’s population is aging almost as rapidly (estimated at 22.3% by 2025) as Japan’s (Oizumi, 2007), and authorities at the National University of Singapore are reportedly developing IPE (Jacobs et al., 2013). In Japan, similarly, Saitama Prefectural University launched IPE modules in 2006, and Gunma University and 10 health and welfare higher education institutions initiated IPE in 2008 (Japan Interprofessional Working and Education Network [JIPWEN], 2016). Because of the activities of these leading institutions, the number of health and welfare schools that have implemented IPE is growing. However, IPE is not yet regarded as compulsory in Japanese health-related professional education.
Langton (2009) has identified five models of IPE among British institutions of higher education. However, it is not clear how IPE is carried out in these models and little is known about what kind of curriculum is being implemented. Two relatively large-scale surveys have already been published in Japan (Oshima, 2009; Ogawa, Takahashi & Miyazaki, 2015). One addressed recognition of and potential for IPE development, while the other collected information on the current status of and problems with IPE. The former dealt with five professions (doctor, nurse, physical therapist, occupational therapist, social worker), the latter with eight (doctor, nurse, physical therapist, occupational therapist, social worker, pharmacist, dentist, dietitian). Both of the survey reports were limited to universities; there are no nationwide surveys that include technical colleges (5-year graduate educational institutions including high school level), junior colleges, and vocational schools, all of which are still an essential part of professional education. Vocational schools in Japan provide practical vocational and technical education in 1- to 3-year courses. More than 40% of graduates from vocational schools work in the health and welfare field with national licenses (Ministry of Education, Culture, Sports, Science and Technology, 2013). However, it is not clear how much IPE is carried out, nor what the teaching methods and evaluation criteria are at such schools.
The present national survey conducted in Japan aims to clarify the current status of IPE, implementation percentages of IPE by profession and school type, and teaching methods and evaluation criteria employed.
II. METHODS
A. Questionnaire Development
We reviewed large-scale surveys conducted in the UK, Canada, Australia, and the US. Our analysis showed that, across these countries, there was no unified survey at the national level, and that the contents of the surveys differed depending on the context of the country and institution (Barr et al., 2013; Formicola et al., 2012; International Network Health Policy and Reform, 2011; Rafter et al., 2006; The Interprofessional Curriculum Renewal Consortium, Australia, 2013).
Of the surveys we reviewed, a UK survey of 127 institutions representing 16 professions seemed to be the most appropriate reference for us, given our aim of evaluating the actual situation and curriculum framework of the institutions for healthcare professions. We developed our questionnaire on IPE health and welfare schools in 2013 as follows.
First, a native Japanese speaker translated the questionnaire from the UK survey into Japanese. All the authors reviewed this translation to ensure that it matched the current situation in Japan; a draft version of the questionnaire was then formulated. Next, three college faculty members who were engaged in IPE were asked to complete the draft questionnaire and to provide feedback. The comments and suggestions of the faculty members were used to develop the final version of the questionnaire.
The survey items covered the following topics: target specialty or profession; type of school (technical college, vocational school, junior college, university, graduate school of a university); presence or absence of IPE and IPE training; curriculum profile (course title, target profession, instructors, hours, units, teaching method, grading system); course details (outcomes assessment, course review process, research involvement/practice-oriented, joint program with extramural institutions, collaborators, challenges in implementing IPE); and, open-ended comments. Medicine, dentistry, and pharmacy are 6-year programs, were categorized as undergraduate level.
Figure 1. The process for developing the questionnaire on IPE
B. Participants and Recruitment
The questionnaire was sent to the chief administrative officers at 3,430 health and welfare schools, covering 13 healthcare and social care professions, where medical professionals who are a key part of the ICCS are trained in Japan: doctors, nurses, physical therapists, registered dietitians, dentists, dental hygienists, social workers, pharmacists, occupational therapists, clinical psychologists, medical administrators, certified care workers, and speech therapists. Except for medical schools, the schools chosen to receive questionnaires were those listed on the websites of the academic societies of the aforementioned professions (Yodosha Meibo Henshushitsu, 2013). To choose medical schools, we used a directory of medical schools.
The questionnaire was mailed on December 18, 2013, along with an informed consent form, cover letter, and a return envelope, to the chief administrative officers in charge of curriculum management at each school. The closing date of the questionnaire was set as January 28, 2014.
C. Data Analysis
The data were screened by two researchers (MG and AO) and analysed using Excel 2013 software (Microsoft Japan, Tokyo, Japan). We did not analyse statistically. Summary data are presented as frequencies and percentages.
The research protocol of this study was approved by the Research Ethics Committee of the Mie University School of Medicine.
III. RESULTS
In total, 572 completed questionnaires were returned (response rate 17%), of which the number of valid responses was 493 (14%). 3% were excluded because the department was not identifiable.
A. Implementation Rate of IPE Curriculum
The percentage of the responding schools that provided IPE was 19% (93 of 493), with a total of 236 curricula, a median of 22.5 hours, and a quadrant range of 10 to 40 hours.
The following professions are listed in order of IPE implementation rate: speech therapy 60%; dentistry 55.6%; medicine 37.5%; occupational therapy 31.3%; pharmacy 29%; clinical psychology 29%; dental hygiene 23.4%; social work 20%; physical therapy 16%; nursing 13.6%; medical secretarial 13.3%; certified care work 12.1%; and nutrition 11.1%. There were no occupations in which IPE was completely absent (See Table 1).
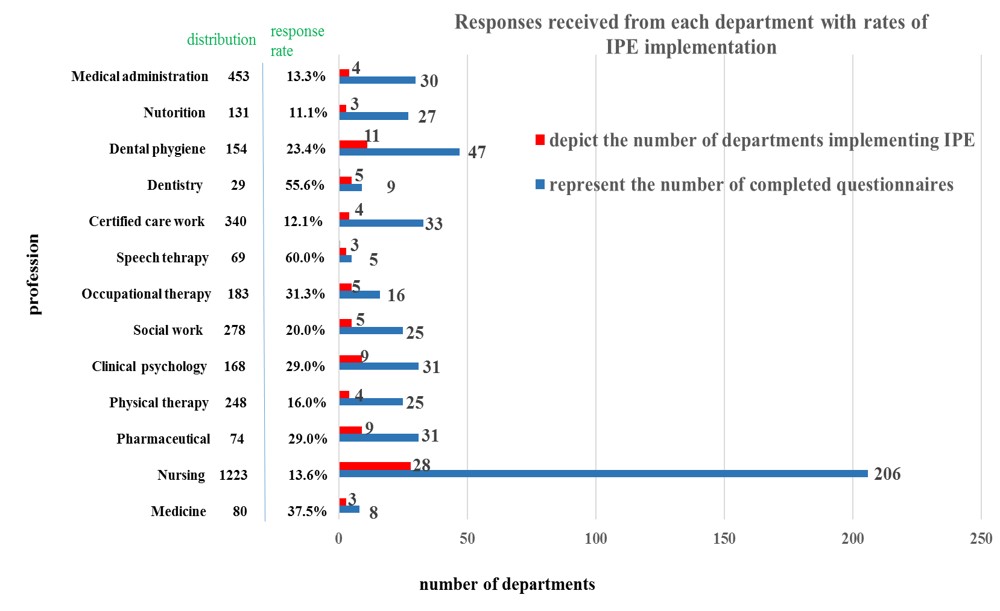
Note: Distribution represents the number of questionnaires distributed to departments
Table 1. Responses received from each department with percentages of IPE implementation
B. Implementation by School Type
The number of valid responses and the institutions providing IPE courses or modules are shown in Table 2. Universities providing undergraduate degrees had the highest percentage (33%) of IPE within their curricula, followed by those with graduate degrees (28%), 3-year vocational schools (14%), junior colleges (9%), technical colleges (7%), and 2-year vocational schools (5%).
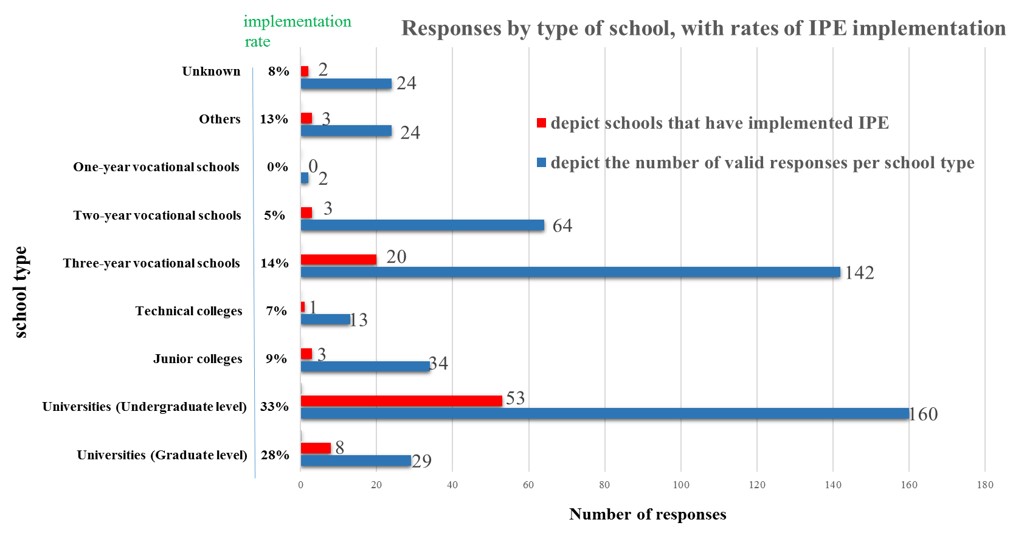
Table 2. Responses by type of school, with percentages of IPE implementation
C. Teaching Methods
Teaching methods in 244 courses that included IPE at 93 institutions were analysed. The results are shown in Table 3. The greatest proportion of IPE was delivered through group learning (e.g., case-based learning, problem learning, practice learning, experiential learning, or role-play exercises; 68%), followed by lectures (48%). Lectures alone represented 21% of the answers; only three courses or modules included e-learning (1%).
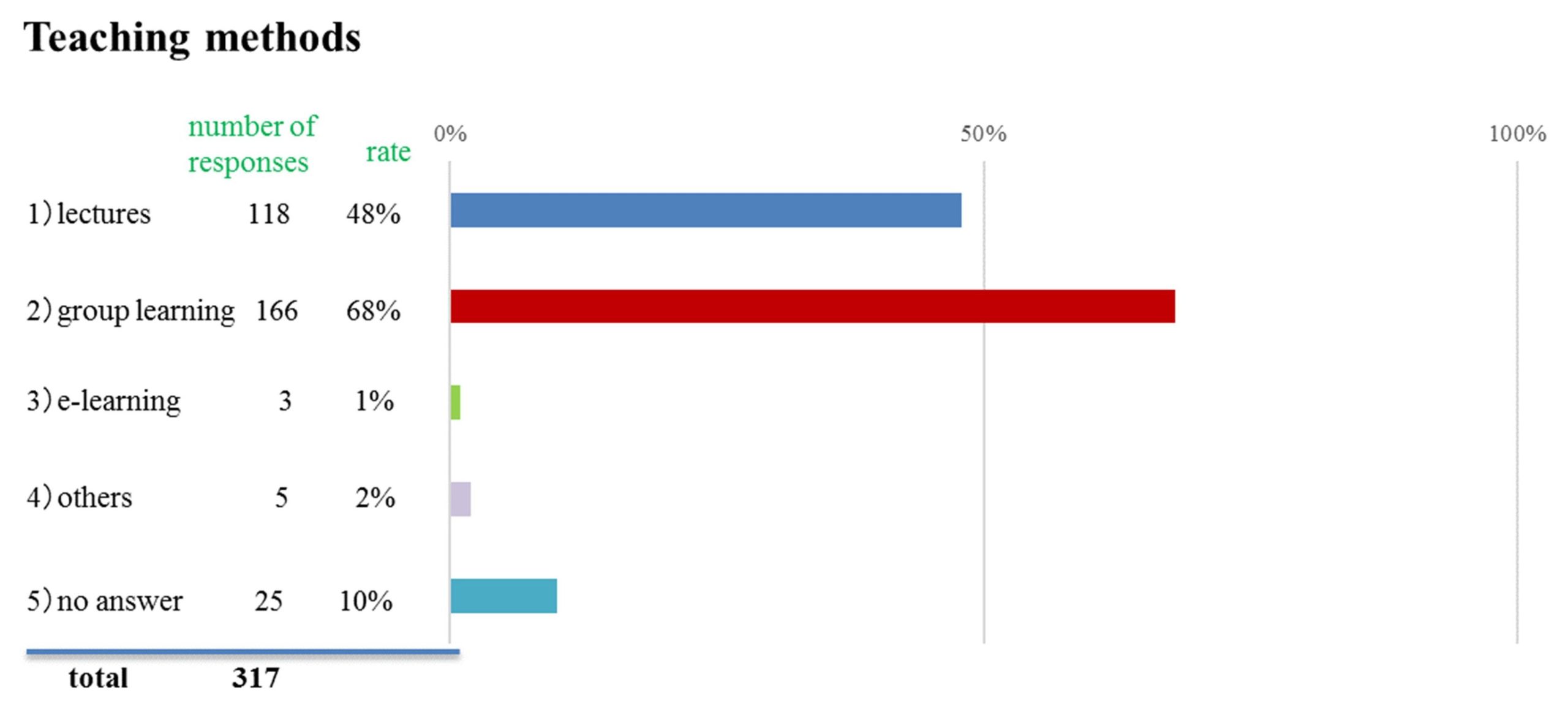
Table 3. Teaching methods used for the delivery of IPE
D. Grading Methods
Of 244 grading systems reported (multiple answers allowed), essays were the most frequent evaluation method (65%), followed by paper exams (25%), portfolios (9%), and Objective Structure Clinical Examinations (OSCE) (6%). Other methods included attendance, peer review, poster presentations, oral presentations, self-evaluation, and interviews.
E. Interest in IPE Survey Results
The majority of respondents (n = 306, 62%) indicated interest in knowing the outcome of this survey.
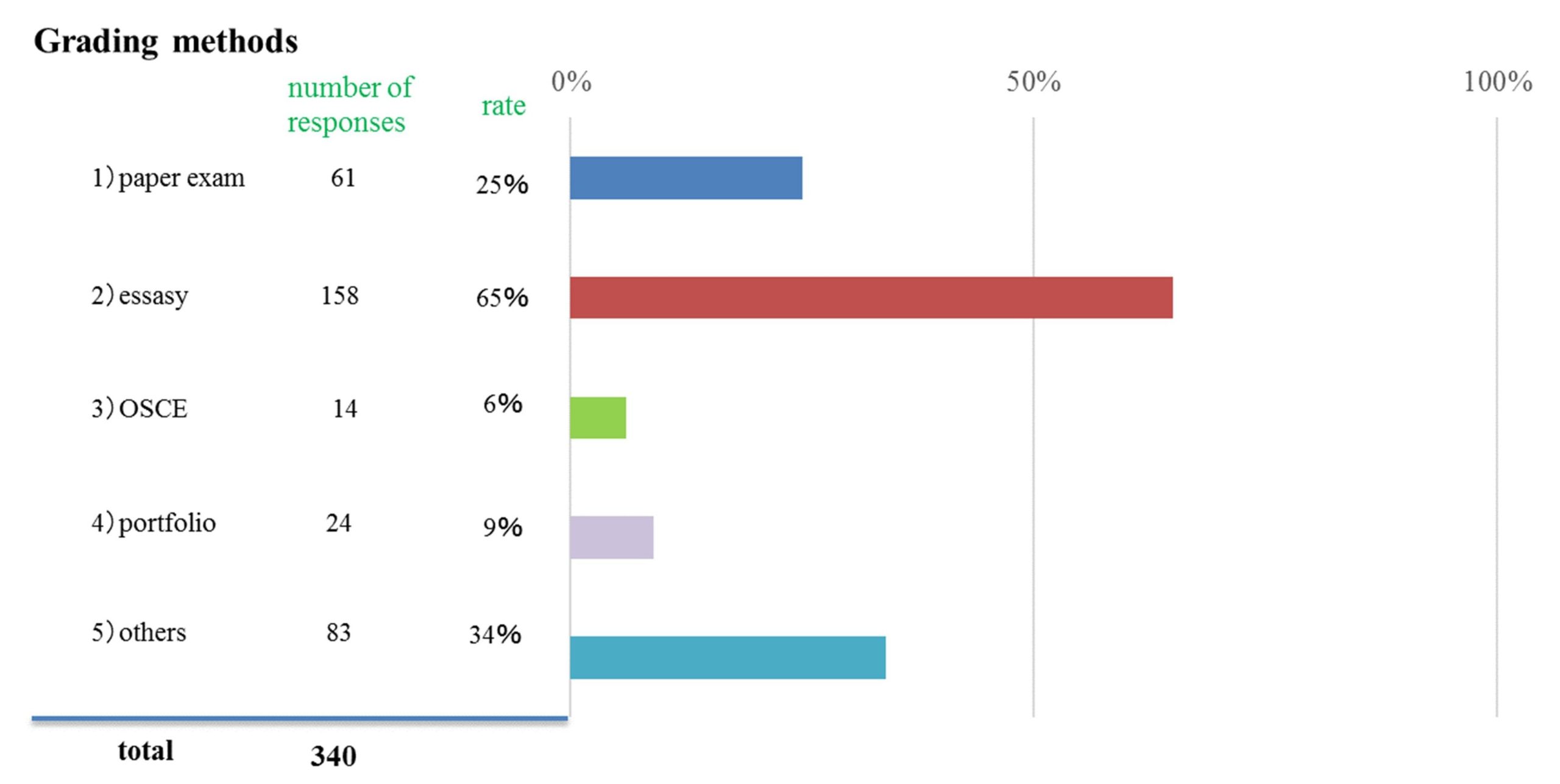
Table 4. Grading methods used for IPE
IV. DISCUSSION
Our results showed that 19% of the health and welfare schools surveyed provided IPE courses or modules. However, the rate of IPE implementation is not keeping pace with the need for service, because the percentage of the population, 65 years or older, is increasing unprecedently in Japan. (the aging rate in 2010 was 23%) (Cabinet Office, 2014). Unfortunately, because no implementation frequency surveys have been conducted in the UK or Australia, it is not possible to compare our results with those of other countries (Barr, et al., 2013; The Interprofessional Curriculum Renewal Consortium, Australia, 2013). To disseminate IPE, which requires considerable resources for coordination with other departments or extramural institutions, it may be necessary to boost organizational support at the institutional level or at the policy-making level for all health and welfare institutions.
Our survey showed that IPE was most prevalent in universities (undergraduate level), which had higher implementation percentages than did specialized training schools. This is arguably related to the freedom that universities have in organizing the curriculum of their 4-year undergraduate education, through which they can reflect their ideas regarding both their specialized and liberal arts fields (Hayashi, 2003; Ministry of Education, Culture, Sports, Science and Technology, 2001). Conversely, the implementation of IPE in vocational schools may be affected by these schools’ focus on obtaining professional qualifications within a shorter timeframe, which may make it more difficult to cover a broader range of subjects (Tsukahara, 2005).
This survey revealed the difficulty of practicing IPE at vocational schools. However, some specialized vocational schools are now improving or expanding their curricula to 4 years and making it easier to obtain qualifications (e.g., nurses can get a health nurse or midwifery license), which improves the outlook for the introduction of IPE in the future. In 4-year curricula, the proportion of total class hours dedicated to practical training and exercises exceeds 40% in the medical field; there is great potential for introducing IPE in the future if the practical training in multi-professional curricula can be capably coordinated (Ministry of Education, Culture, Sports, Science and Technology, 2013). We speculate that the key to introducing IPE in vocational schools will be the way in which the practical training or exercise is used.
Our results for teaching methods showed that 68% of the curricula incorporated some form of group learning approach, 48% included lectures, and 21% were based on lectures alone. Abu-Rish reported that in the 83 programs studied, 57.8% were small group discussions, 48.2% were case-based or question-based learning; and 36.1% were large-group lecture (Abu-Rish et al., 2012). In the UK study, all the learning methods reported were interactive (Barr et al., 2013). The UK-based Centre for the Advancement of IPE maintains that IPE occurs when two or more professions “learn with, from, and about each other” (Centre for The Advancement of Interprofessional Education, 2017). In light of this definition, it is a heartening result that the interactive strategy is dominant: 68% of respondents reported use of group learning.
We do not know whether 21% lectures alone should be interpreted as high figure. While it is necessary to confirm the details of the lecture format, lectures, which simply transfer knowledge from the instructor to the students, may not be sufficiently conducive to collaboration. Lectures are useful as a form of teaching that conveys information to a large number of people at once. Japanese educators may tend to rely on lecturing because they do not have enough knowledge about and experience with active learning, a method in which learners are taking part more deliberately, rather than merely listening to and memorizing the lecture passively. Japan may also have fewer educational environments designed for active learning. However, the Australian survey reported that 21 of the 70 curricula also included lectures; therefore, we do not think that lectures are unnecessary (The interprofessional Curriculum Renewal Consortium, Australia, 2013); however, we suggest that lectures will be more useful if they are designed to complement the interactive program.
The Japanese Media Developmental Education Centre has reported that 46.1% of higher education institutions use IT-based methods such as e-learning (Media Education Development Centre, 2006): Universities use it for 56.7% of courses, colleges for 24.4%, and special training colleges for 72.1% (Mima & Yamaguchi, 2005). In our survey, by contrast, only three courses (1%) included e-learning for IPE, which is much lower than the 58% reported in the UK (Barr et al., 2013). Importantly, online learning could enable geographically distant schools to hold joint sessions. It could also assist in launching an online IPE course or module at institutions that cannot start their own because of a lack of suitable disciplinary combinations (Luke et al., 2009).
The most common method for evaluating IPE learning was the term essay (65%), followed by the paper exam (25%). Thistlethwaite and Moran (2010) has suggested that IPE outcome evaluations should focus more on changes in the learners’ attitudes or actions than on their knowledge, in which case, self-evaluation is often carried out. Therefore, the essay may be inadequate. For self-reflection and self-evaluation, a portfolio method would be better. Thistlethwaite, Kumar, Moran, Saunders and Carr (2015) reported that in a recent review of pre-qualification IPE evaluations, of the 90 studies included, only 5 reported on assessment of student knowledge via a written test. Abu-Rish et al (2012) reported that 39.8% of the assessment methods were knowledge-based. But in the Australian survey (The interprofessional Curriculum Renewal Consortium, Australia, 2013), teamwork and team function were also evaluated. Our questionnaire did not ask for details about assessment processes. Future studies should, therefore, investigate how IPE competencies are evaluated with paper exams, as well as determine the extent to which rubrics and other evaluation tools have been introduced.
The programs may use attendance as an assessment tool because appropriate validated assessment tools have not been developed yet. Attendance was used for some portion of evaluation in the Australian survey (The Interprofessional Curriculum Renewal Consortium, Australia, 2013). Summative assessment of IPE as attendance may be unavoidable, because prequalification professional education focuses on the individual, rather than the collaboration unit. Given the current situation in Japan, where IPE practice has preceded development of appropriate assessment methods, essays and paper exams have been the major methods of evaluating IPE. As a next step, we must develop valid and reliable tools for such evaluations; this is a challenge for those engaged in IPE not only in Japan, but around the world.
In April 2016, we developed the “Interprofessional competency framework in Japan” (Haruta et al., 2016) to define the skills necessary for collaboration among multiple professional academic associations. Thus, our future tasks include the development of reports and OSCE evaluation methods based on competency for collaboration.
Additionally, we are also conducting a survey with faculties to investigate their awareness, learning environments, outcomes, and evaluations of IPE. We also intend to conduct qualitative and individual research with universities or vocational schools that offer advanced approaches, by visiting the institutions directly and interviewing people in charge of IPE. In this way, we can clarify and disseminate effective learning methods and tips for overcoming the barriers to IPE introduction. Finally, we will compare IPE tips in Western countries with those in Japan.
Given that Japan will implement IPE from now on, our analyses may also be useful for Asian countries with similar cultural backgrounds. Also, developing countries that do not have detailed data or any organizations promoting IPE such as in the UK, Australia and Canada, may find our data collection methods useful. We believe this will result in the spread of IPE not only in Japan but also in many other Asian countries and developing countries.
The implementation rate of IPE in Japan was as low as 19%; however, our low survey response rate may have affected the results. This low rate may also reflect the inclusion of vocational schools, junior colleges and special training schools. We suspect that the low response rate may have had to do with a failure to reach the appropriate persons in the institutions. Although we sent the survey to the chief administrative officer in charge of curriculum management at each institution, with the expectation that it would be passed to the curriculum director of IPE where such a position existed, this may not have occurred in every instance. Because some courses involved different divisions or departments, and occasional extracurricular sessions, the recipients may have experienced difficulty finding the appropriate instructors. We initially anonymized the survey to facilitate the completion process. We expected that the responses would come from each individual professional but some responses came from administrative offices; in such cases, we were unable to identify the department, and those responses were therefore excluded. In retrospect, we believe it would have been preferable to identify the person in charge of IPE at each institution before sending the questionnaires.
It should be pointed out that the response rates in previous Japanese studies have been similarly low at 24.6% (Oshima, 2009) and 32.8% (Ogawa et al., 2010). The UK survey (Barr et al., 2013) mentioned earlier made reference to difficulties in identifying interprofessional curricula, suggesting that a questionnaire-based investigation of IPE has inherent limitations. Our future work will improve this survey, and evolve toward locating responsible institutional contacts to provide regular updates regarding IPE curricula.
V. CONCLUSION
IPE is being implemented in about 19% of the educational institutions contacted, and is represented in 13 occupations. We clarified the current level of IPE in graduate, undergraduate, technical college, junior college, and vocational schools for these 13 major healthcare and social care professions in Japan. This study can provide important fundamental information for the development of IPE curriculum and serve as a springboard from which to develop deeper empirical insights.
Notes on Contributors
Michiko Goto is an Assistant Professor in Department of Education and Research in Family and Community Medicine, Mie University Graduate School of Medicine.
Junji Haruta is an Assistant Professor in Department of General Medicine and Primary Care, University of Tsukuba Hospital, Japan.
Ai Oishi is a PhD candidate at the Usher Institute of Population Health Sciences and Informatics, University of Edinburgh, UK.
Kazue Yoshida is an Associate professor in Graduate School of Medicine, Course of Nursing, Faculty of Medicine Mie University, Mie, Japan.
Kenji Yoshimi is a Lecturer in Department of Contemporary Sociology, School of Sociology, Bukkyou University, Kyoto, Japan.
Yousuke Takemura is Professor and Chair in Department of Family Medicine, Mie University School of Medicine & Graduate School of Medicine, Mie, Japan.
Hisashi Yoshimoto is an Assistant Professor in Department of Primary Care and Medical Education, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan.
Ethical Approval
This study was approved by the Research Ethics Committee of the Faculty of Medicine at Mie University (No. 1396).
Acknowledgements
The authors would like to thank all of the participants who cooperated in this questionnaire, and to convey special thanks to Takashima, our office secretary.
Declaration of Interest
The authors declare that they have no competing interests.
References
Abu-Rish, E., Kim, S., Choe, L., Varpio L., Malik E., White, A. A., & Zierler, B. (2012). Current trends in interprofessional education of health Sciences students: A literature review. Journal of Interprofessional Care, 26, 444–451.
Barr, H., Marion, D’Avray, M.H.L., & Thistlethwaite, J. (2013). A Survey of pre-registration interprofessional education in the United Kingdom 2010-2012.
Retrieved from http://caipe.org.uk/silo/files/ipergsurvey30april2013finalforewordq.pdf.
Cabinet Office (2011). The situation of aging. Heisei era 2011 aged society white paper. Tokyo: Government of Japan.
Retrieved from http://www8.cao.go.jp/kourei/whitepaper/w-011/zenbun/html/s1-1-1-02.html.
Cabinet Office (2014). International trend of aging. Annual Report on the Aging Society: 2014 (Summery). Tokyo: Government of Japan. Retrieved from http://www8.cao.go.jp/kourei/english/annualreport/2014/pdf/c1-1.pdf.
Centre for The Advancement of interprofessional Education (2017). Interprofessional Education Guidelines. Retrieved from https://www.caipe.org/resources/publications/caipe-publications/caipe-2017-interprofessional-education-guidelines-barr-h-ford-j-gray-r-helme-m-hutchings-m-low-h-machin-reeves-s.
Formicola, A. J., Andries, S. C., Buchnan, J. A., Childs, G. S., Gibbs, M., Inglehart, M. R., Evans, L. (2012). Interprofessional education in US and Canadian dental schools: An ADEA Team Study Group report. Journal of Dental Education, 76(9), 1250–1268.
Gilbert, J. H. V., Yan, J., & Hoffman, S. J. (2010). A WHO Report: Framework for action on interprofessional education and collaborative practice. Journal of Allied Health Association of Schools of Allied Health Professions, 39, 196–197.
Haruta, J., Sakai I., Otsuka M., Yoshimoto, H., Yoshida K., Goto, M., & Shimoi, T. (2016). Development of an interprofessional competency framework in Japan. Journal of Interprofessional Care, 30 (5), 675-677. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27351518.
Hayashi, M. (2003). Problem of general education brought about by the relaxation of standards for the establishment of universities. Memoirs of the Osaka Institute of Technology (Series B), 48(2), 13-26. Retrieved from https://www.oit.ac.jp/japanese/toshokan/tosho/kiyou/jinshahen/48-2/jin-sya_2/hayashi_masahito.html.
Hughes, S. L., Cummings, J., Weaver, F., Manheim, L., Braun, B., & Conrad, K. (1992). A randomized trial of the cost effectiveness of VA hospital-based home care for the terminally ill. BMC Health Services – Research, 26(6), 801–817.
International Network Health Policy and Reform (2011). Interprofessional Education: A progress report.
Retrieved from http://www.hpm.org/en/Surveys/CPRN_-_Canada/12/Interprofessional_Education___A_progress_report.html.
Jacobus, J. L., Samarasekera, D. D., Chui, W. K., Chan, S. Y., Wong, L., Liaw, S. Y., Chan, Y. C. S. (2013). Building a successful platform for interprofessional education for health professions in an Asian university. Medical Teacher, 35(5), 343–347.
Jansson, A., Isacsson, A., & Lindholm, L. H. (1992). Organization of health care teams and the population’s contacts with primary care. Scandinavian Journal of Primary Health Care, 10(4), 257–265.
Japan Interprofessional Working and Education Network [JIPWEN] (2016). News. Website. Retrieved from http://jipwen.dept.showa.gunma-u.ac.jp/jp/?cat=6.
Langton, H. (2009). Interprofessional education in higher education institutions: models, pedagogies and realities. In: Blutesau, P. & Jackson, A, (Eds.), Interprofessional Education. Making It Happen (pp. 37–58). Basingstoke: Palgrave Macmillan.
Lemieux-Charles, L., & McGuire, W. L. (2006). What do we know about health care team effectiveness? A review of the literature. Medical Care Research and Review, 63(3), 263–300.
Luke, R., Solomon, P., Baptiste, S., Hall, P., Orchard, C., Rukholm, E., & Carter, L. (.2009). Online interprofessional health sciences education: From theory to practice. Journal of Continuing Education in the Health Professions, 29(3), 161–167.
Media Education Development Centre. (2006). A survey about education with IT such as e-learning. Tokyo: Media Education Development Centre, 29–30.
Mima, N., & Yamauchi, Y. (2005). Designing “future learning.” Space, activities and community. Tokyo: University of Tokyo Press.
Ministry of Education, Culture, Sports, Science and Technology (2001). Notification: Enforcement of ministerial ordinance to revise part of university establishment standard.
Retrieved from http://www.mext.go.jp/b_menu/hakusho/nc/t19910624001/t19910624001.html.
Ministry of Education, Culture, Sports, Science and Technology. (2013). The creation of “Specialized occupation practice”~ pioneering trials which use the framework specialized occupation practice ~July 12th, 2013. Research Cooperation Conference for Assurance and Improvement of Quality of Vocational Schools. Retrieved from http://www.mext.go.jp/component/b_menu/shingi/toushin/__icsFiles/afieldfile/2011/01/31/1301878_5_1.pdf.
Ministry of Health, Labour and Welfare (2016). Integrated Community Care System: To implementation Integrated Community Care System.
Retrieved from http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/kaigo_koureisha/chiiki-houkatsu/.
Ogawa, S., Takahashi, Y., & Miyazaki, M. (2015). The Current Status and Problems with the Implementation of Interprofessional Education in Japan: An Exploratory Study. Journal of Research in Interprofessional Practice and Education, 5(1), 1-15. Retrieved from http://www.jripe.org/index.php/journal/article/viewArticle/181.
Oizumi. K. (2007). Aging Asia. The time when the conditions of prosperity change. Tokyo: Chuou kouron shinsha.
Oshima, N. (2009). A survey on the recognition and the potential for development of interprofessional education (IPE) at universities in the areas of health care and social service in Japan. Hoken Iryou Fukushi Rennkei, 1(1), 27–33.
Rafter, M. E., Pesun, I. J., Herren, M., Linfante, J. C., Mina, M., Wu, C. D., & Casada, J. P. (2006). A preliminary survey of interprofessional education. Journal of Dental Education, 70(4), 417–427.
Subcommittee on Elderly Health, Committee on Health/Human Life Science, Science Council of Japan. (2011). Towards interprofessional education for supporting the community-dwelling elderly.
Retrieved from http://www.scj.go.jp/ja/info/kohyo/pdf/kohyo-21-t133-2.pdf.
Tsukahara, S. (2005). New development and role of the technical school. Nippon roudoukennkyuuzasshi (in Japanese), 542, 70-80. Retrieved from http://web.jil.go.jp/institute/zassi/backnumber/2005/09/pdf/070-080.pdf.
The Interprofessional Curriculum Renewal Consortium, Australia (2013). Interprofessional health education: A national audit. Retrieved from http://umanitoba.ca/programs/interprofessional /media/IPE_National_Audit_Report_Australia_2013(1).pdf.
Thistlethwaite, J., & Moran, M. (2010). Learning outcomes for interprofessional education (IPE): Literature review and synthesis. Journal of Interprofessional Care, 4(5), 503–513.
Thistlethwaite, J., Kumar, K., Moran, M., Saunders, R., Carr, S. (2015). An exploratory review of pre-qualification interprofessional education evaluations. Journal of Interprofessional Care, 29(4), 292–297.
World Health Organization [WHO] (1988). Learning together to work together for health. Report of a WHO study group on multiprofessional education of health personnel: The team approach. (World Health Organisation Techical Report Series 769:1-72). Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/3140499.
Yodosha Meibo Henshushitsu (Yodosha Directory Editing Group) (Ed.). (2013). Iiku Kikan Meibo 2013-’14. (Directory of Medical Institutions 2013–’14). Tokyo: Yodosha.
*Michiko Goto, M.A., Ph.D
Assistant Professor
Department of Education and Research in
Family and Community Medicine
Mie University Graduate School of Medicine
2-174 Edobashi, Tsu 514-8507 Mie JAPAN
Phone: +81-59-231-9087
Fax: +81-59-231-5289
Email:tamgoto@clin.medic.mie-u.ac.jp
Published online: 2 May, TAPS 2018, 3(2), 47-53
DOI: https://doi.org/10.29060/TAPS.2018-3-2/OA1037
Kun Hwang, Ae Yang Kim & Hun Kim
Department of Plastic Surgery, Inha University School of Medicine, Incheon, Korea
Abstract
Background: We analyzed book reports written by medical students on 1) Bulgakov’s A Young Doctor’s Notebook and 2) Zweig’s The Right to Heresy: Castellio against Calvin.
Methods: About 50 medical students were asked to read the above books. In the book reports, the following questions were included: 1) Do patients have confidence in medical doctors? What is needed to gain a patient’s trust? Can a doctor’s good will and efforts make patients trust their doctor? Would it be helpful for a doctor to write a narrative of his or her own experiences to obtain patients’ trust? 2) Should the medical doctor engage in wide variety of activities or focus on the medical profession? Would you risk your life for your convictions? Why is tolerance by medical doctors currently needed?
Results: Of the students, 50% thought that patients do not have confidence in their medical doctors, while 34% answered that patients trust doctors; 46% answered that competence is needed for a doctor to be trusted by patients, 84% stated that good will and efforts will make patients trust their doctor, and 60% replied that it would be useful for a doctor to write a narrative of own experiences to obtain patients’ trust. Eighty-four percent thought that it is desirable for medical doctors to participate in a wide variety of activities, and 60% answered that they would risk their life for their convictions.
Discussion: Our findings regarding students’ perceptions indicate that these readings are good teaching materials for medical humanities.
Keywords: Books; Medicine in Literature; Writing; Students, Medical; Physicians; Humans
Practice Highlights
- Half of the students thought patients do not have confidence in their medical doctors, while one-third answered that patients trust doctors.
- About half of the students (46%) answered that competence is needed for a doctor to be trusted by patients.
- The majority of students (84%) answered that a doctor’s good will and efforts make patients trust their doctor.
- Most students (84%) thought that the participation of medical doctors in a wide variety of activities is desirable and reported that they would risk their lives for their for their convictions.
I. INTRODUCTION
In Korea, several attempts have been made to use literature in medical education. Through telling, hearing, reading, and writing illness narratives, Hwang insisted that medical doctors and medical students can learn empathy and clinical wisdom (Hwang, 2013). Lee said that ‘medicine in the literature’ can give deep understanding and insight into patients. She insisted that doctors can also develop self-awareness through literature (Lee & Rhee, 2003).
Several special study modules in literature and medicine have been conducted previously (Calman, Downie, Duthie, & Sweeney, 1988; Lancaster, Hart, & Gardner, 2002; Jacobson et al., 2004). In a 4-week course for medical students in Newcastle, UK, the themes included empathy, death and dying, disability, madness and creativity, addiction, domestic violence, ethical dilemmas, doctor/patient communication, doctors’ emotions, and end-of-life decisions (Lancaster, Hart, & Gardner, 2002).
In this study, we analyzed the perceptions of medical students applying contextual relevance to literature, after having read Bulgakov’s A Young Doctor’s Notebook and Zweig’s The Right to Heresy: Castellio against Calvin. Synopsis of these 2 books could be found in Part IV. Discussion section.
II. METHODS
A. Bulgakov’s A Young Doctor’s Notebook
Participants: The participants included 50 medical students in their sophomore class (second year of a 4-year course). The mean overall age was 28.8±3.2 years. A month before the classroom lecture, they were asked to read Bulgakov’s A Young Doctor’s Notebook (written in the 1920s, first English translation in 1975) and to have a discussion in groups of 7. The Korean translation (by Lee BH, 2011) was provided to students (Lee, 2015).
Semi-structured theme lists: In their book reports on Bulgakov’s A Young Doctor’s Notebook, the students were asked to address the following questions:
- Do patients in Korea have confidence in their medical doctors?
- What is needed to gain a patient’s trust?
- Can a doctor’s good will and efforts make patients trust their doctor?
- Would it be helpful for a doctor to write a narrative of his or her own experiences to obtain patients’ trust?
B. Zweig’s The Right to Heresy: Castellio against Calvin
Participants: The participants in this study included 50 medical students in their third year of a 4-year program. The mean overall age was 27.4±2.3 years.
Book: A Korean translation of Zweig’s The Right to Heresy: Castellio against Calvin, 1936 (Original title: Castellio gegen Calvin oder Ein Gewissen gegen die Gewalt) was provided to each student one month before the forum (Zweig, 1936).
Questionnaires: In their analysis of Zweig’s The Right to Heresy, the students were asked to address the following questions:
- Should medical doctors engage in in a wide variety of activities or focus solely on the medical profession?
- Would you risk your life for your convictions?
- Why is tolerance necessary for medical doctors?
These books brought up questions that we considered in our previous studies (K. Hwang, Lee, S. Y. Kim, S. W. Hwang, & A. Y. Kim, 2014; Hwang, Hong, & Heo, 2014; K. Hwang, H. Kim, A. Y. Kim, S. W. Hwang, & S. H. Hwang, 2016; S. W. Hwang, H. Kim, A. Y. Kim, & K. Hwang, 2016).
Students were divided into 7 focus groups and 7-8 students were allocated to each group. Each group participated in a focus group discussion, and during their discussion, they chose between the options of yes, no, and undecided, and articulated the reasons for their choice.
These discussions were summarized in PowerPoint slides, and a member of each group presented in an open forum discussion in front of all the students and 2 moderating professors.
After the forum, they were asked to write a book report. The answers to the questions were provided as free text. However, based on the focus group discussion and open forum, their replies could be analyzed in terms of yes, no, and undecided answers.
Factors potentially affecting their decisions were also analyzed (age, sex, marital status, number of family members, volunteer work hours, and severity of experienced illness).
SPSS version 19.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. To compare the answers of each group, the chi-square test was used. For the odds ratio and 95% confidence intervals, logistic regression analysis was used. When the p-value was less than 0.05, the data were interpreted as statistically significant.
III. RESULTS
The results of the questionnaires were as follows:
A. Bulgakov’s A Young Doctor’s Notebook
1) Do patients in Korea have confidence in their medical doctors?
Of the 50 respondents, 25 students (50%) answered that patients do not have confidence in their medical doctors, while 17 (34%) replied that patients trust doctors. The remaining 8 (16%) answered that patients are ambivalent. Two students (4%) noted that trust is evolving into distrust recently due to recent events in the news (a bill passed that allows victims of medical malpractice to begin legal proceedings without the consent of hospitals and doctors, and an event occurred in which syringes were reused for injections, infecting hundreds of patients with hepatitis C) (Korea Herald, 2016a, 2016b).
Students over 28 years of age were more likely to answer that patients have confidence in their medical doctors than those under 28 years (OR=5.143; 95% CI, 1.384-19.108, p=0.014 [logistic analysis]).
No significant differences were found according to gender, number of family members, volunteer work hours, or severity of experienced illness (p>0.05).
2) What is needed to gain a patient’s trust?
The virtues that doctors must have in order to be trusted by their patients were competence (54%), followed by professionalism (14%), a sense of ethics (10%), and a suitable demeanor (6%).
Among the 50 respondents, 27 students (54%) answered that competence is needed for doctors to be trusted by their patients. About half of them (14 students) answered that the following are also needed, along with competence: communication and conversation skills (8), a suitable demeanor and sense of ethics (7), professionalism (2), effort (2), empathy (1), self-confidence (1), and sense of responsibility (1) (Table 1).
There were no significant differences according to age, gender, number of family members, volunteer work hours, or severity of experienced illness for this question (p>0.05).
| Answer | n | ||
| Answers | Students | ||
| Competence only | 14 | 14 | |
| + Communication and conversation skill | 8 | 13 | |
| + Attitude and sense of ethics | 7 | ||
| + Professionalism | 2 | ||
| Competence | + Effort | 2 | |
| + Empathy | 1 | ||
| + Self-confidence | 1 | ||
| + Sense of responsibility | 1 | ||
| Subtotal | 36 | 27 | |
| Professionalism only | 3 | 3 | |
| + Sense of ethics | 4 | 4 | |
| Professionalism | + Empathy | 2 | |
| + Self-confidence | 1 | ||
| Subtotal | 10 | 7 | |
| Sense of ethics | Sense of ethics only | 3 | 3 |
| + Revision of education | 1 | 2 | |
| + Love | 1 | ||
| Subtotal | 5 | 5 | |
| Demeanor only | 2 | 2 | |
| Demeanor | + Conversation skill | 1 | 1 |
| Subtotal | 3 | 3 | |
| Other | Policy improvement | 3 | 3 |
| Communication | 1 | 1 | |
| Courage | 1 | 1 | |
| Effort | 1 | 1 | |
| Self-confidence | 1 | 1 | |
| Sense of responsibility | 1 | 1 | |
| Total | 62 | 50 | |
Table 1. What is needed to gain a patient’s trust?
3) Can a doctor’s good will and efforts make patients trust their doctor?
Of the 50 respondents, 42 students (84%) answered affirmatively to this question. Seven (14%) replied that good will and effort are not sufficient to gain trust. The remaining respondent (2%) was unsure.
There were no significant differences in age, gender, number of family members, volunteer work hours, or severity of experienced illness regarding this question (p>0.05).
4) Would it be helpful for a doctor to write a narrative of his or her own experiences to obtain patients’ trust?
Of the 50 respondents, 30 students (60%) answered ‘yes’ to this question, while 13 (26%) replied negatively. The remaining 5 (10%) answered that this possibility has both pros and cons.
There were no significant differences in age, gender, number of family members, volunteer work hours, or severity of experienced illness regarding this question (p>0.05).
B. Zweig’s The Right to Heresy: Castellio against Calvin
1) Should medical doctors engage in a wide variety of activities or focus solely on the medical profession?
Among the 50 students, 48 included the answer in their book report and 2 did not. Among them, 42 (84%) thought the participation of medical doctors in a wide variety of activities is desirable. A few students (3, 6%) responded that medical doctors should focus on the medical profession alone. Three students (6%) had ambivalent thoughts.
The major reasons for the preference for participation of medical doctors in a wide variety of activities are as follows: to broaden the medical doctor’s horizons (15, 36%), and to contribute to society with responsibility and leadership (10, 24%).
Other reasons were, in order, not to be intolerant or narrow-minded (6, 14%), the demand of the era (5, 12%), for integration of academic disciplines (4, 10%), and in preference of diversity (2, 4%).
There was no significant difference in age group, gender, number of family members, or voluntary work hours associated with the motivation of the medical doctor.
2) Would you risk your life for your convictions?
Among the 50 students, 30 (60%) responded that they would risk their lives for their convictions, while 16 (32%) would not. Four students (8%) answered that they could not make up their mind.
The major reasons for taking risk for one’s convictions are as follows: “One’s convictions are worth risking one’s life” (14, 47%) and “One’s convictions are an important value which changes the world, as seen in the case of Servetus” (8, 27%). Other opinions were “Though I cannot risk my life for my convictions, I respect people who do” (3, 10%), “We exist because of the people who risked their lives for their convictions” (3, 10%), and “I would adapt myself to circumstances with various convictions” (2, 6%).
The reasons for not taking risk for one’s convictions are as follows: “One’s convictions are important but not worth enough to risk one’s life” (4, 25%), “I have important work to do in this life” (4, 25%), “Deviant convictions are rather harmful to society” (4, 25%), “I do not have the courage to risk my life” (3, 19%), and “Life itself is more important than convictions” (1, 6%).
There was no significant difference in these responses by age group, gender, number of family members, or volunteer work hours.
3) Why is tolerance required of medical doctors?
Among the 50 respondents, 11 students (22%) reported that tolerance is required for communication with individuals and another 11 (22%) for better treatment results.
Ten students responded that tolerance is needed to understand patients’ pain (20%). Seven students (14%) thought that tolerance is required because medical science is in progress and another 7 (14%) to adapt to diversifying society. Two students (4%) reported needing tolerance for their character training, and another 2 (4%) reported that doctors need tolerance for leadership (Table 2).
| Reason | N | (%) |
| For communication with individuals | 11 | 22 |
| For better treatment results | 11 | 22 |
| To understand patients’ pain | 10 | 20 |
| Medical science is in progress | 7 | 14 |
| To adapt to diversifying society | 7 | 14 |
| For their character training | 2 | 4 |
| For leadership | 2 | 4 |
| Total | 50 | 100 |
Table 2. Why is it necessary for a medical doctor to be tolerant
IV. DISCUSSION
A. Bulgakov’s A Young Doctor’s Notebook
The plot of A Young Doctor’s Notebook can be summarized as follows. This book is the collection of a medical doctor’s narrated experiences. A freshly graduated doctor, the protagonist of A Young Doctor’s Notebook arrives in a remote village with no electricity, a long day by coach from the nearest town. He has a well-equipped medical center, a good library, and competent assistants, but he carries immense responsibility as the only doctor. Many of the stories involve the protagonist facing a medical challenge of some kind. With no practical experience, he faces up to this and (usually) succeeds without exposing his fears or uncertainties. Recurring themes include the severity of the cold and the blizzards, the isolation, and the backwardness of peasant attitudes to health and medical care. Sometimes patients have confidence in their young medical doctor, but in some situations distrust him (Lee, 2015).
Trust in physicians reflects the patient’s optimistic acceptance of vulnerability and the expectation that the physician will do what is best for his or her welfare (Gopichandran & Chetlapalli, 2015). Trust in physicians influences the health and well-being of older adults, as well as pediatric patients (Simon, Zhang, & Dong, 2014; Singh, 2016). However, there have been few studies investigating how physicians can instill confidence in patients (Maruani et al., 2013; Fiscella et al., 2004).
Through an analysis of this book, we hoped to explore medical students’ thoughts about whether patients have confidence in their medical doctors, what is needed to gain a patient’s trust, and whether a doctor’s good will and efforts make patients trusting their doctor.
B. Zweig’s The Right to Heresy: Castellio against Calvin
Three important characters appear in Zweig’s The Right to Heresy: John Calvin, Michael Servetus, and Sebastian Castellio. The first character is John Calvin. He was born in France and was a second-generation religious reformer after Martin Luther. He fought against the corruption of the Catholic Church at the time. He wrote the Institutes of the Christian Religion (Institutio Religionis Christiane) in 1535 in Geneva, Switzerland, which presented a doctrine that puritans (Protestants) should observe. During his theocracy in Geneva, Calvin expelled and even killed many people who crossed his will. He cut the figure of a dreadful dictator.
The second is Sebastian Castellio. He was a humanist scholar who studied and translated the Bible. He used decent words against the dictatorial reign of Calvin. He knew that he was merely a “mosquito in front of the elephant.” However, he held his convictions as an intellectual against injustice.
The third is Miguel Servetus. He was a medical doctor who first described the function of pulmonary circulation. He was also a theologian who wrote a book to some concepts associated with the Trinity, and wished to meet Calvin and discuss their opinions. Servetus published Reconstruction of the Christian under the name of Michel de Villeneuve to avoid risk. Because Servetus wrote some different opinions against Calvin’s Institutes of the Christian Religion, Calvin was angry about the writings of Servetus and demonized him. Using trickery, Calvin found evidence that Servetus was the author of that book. Servetus was eventually accused of heresy by both the Catholic and Protestant, and was eventually burned by the council of Geneva, which was under control of Calvin. Until the last moment, with his body chained in the engulfing flames, Servetus did not withdraw his beliefs in his doctrine and kept his convictions.
When Castellio watched this injustice, he decided to face Calvin. In his book called About Heretics, he argued that Calvin definitely did wrong to the theologian from Spain. Castellio defended the freedom of thinking and wrote that the recklessness of burning Servetus was an “obvious murder.” In other words, “To kill the people who keep their beliefs is a religious murder.” Castellio believed that only toleration could save humanity from such violence. The writings of Castellio, however, could not be distributed to the readers under Calvin’s reign. After their deaths, the writings came to light.
Stefan Zweig studied and summarized the story of these three historical characters and wrote a famous book: The Right to Heresy: Castellio against Calvin. This book emphasized the importance ‘toleration’.
We attempted to see if medical students would express willingness to risk their lives for their convictions and explain why tolerance is required of the medical doctor by analyzing the book reports of on Zweig’s The Right to Heresy.
The students pointed out Calvin’s intolerance to Servetus and regarded Calvin as a dictator. They thought it was ironic that Calvin, who fought against Catholics for their intolerance, treated Servetus without tolerance and eventually killed him. They agreed with Zweig, who suffered under Hitler, and tried to draw connections between the similar figures of the tyrants through Calvin’s story.
The students were concerned about the ‘many little Calvins’ around them who do not even listen to others’ opinions, leading to a ‘society of impossible communication.’
Most students (84%) responded that the participation of medical doctors in a wide variety of activities is desirable, and a few students (6%) responded that they preferred to focus on the medical profession only. They gave the examples of several role models of medical doctors who contributed a great deal to society, such as Che Guevara, Lu Hsün (魯迅), and Fr. John Lee Tae-seok, a Korean priest. Another interesting example was Paula Pareto, the first woman to win an individual gold medal for Argentina, in judo at the Rio Olympics, who also studied medicine at the University of Buenos Aires.
Most students (60%) responded that they would risk their life for their convictions, while (32%) would not. This result was expected because the medical profession cannot be performed without having convictions devoted to patients.
We were able to observe that the students took great pains to answer the question of why tolerance is required of the medical doctor. The most common answers were for communication (22%), for better treatment results (22%), and to understand patients’ pain (20%). Here, we could see that the students wanted to be good doctors by developing their proper humanity.
As reported in a paper from Cardiff, a literature and medicine special study module was designed and evaluated for third year undergraduate medical students, by tutors from an academic department of general practice. Developing subjects was challenging for students and tutors (Jacobson et al., 2004). In the present study, 7-8 students were allocated to focus groups and asked to choose between yes, no, and undecided answers, as well as to indicate why they chose their answer. Additionally, they were asked to write a book report. We view our method as a combination of a focus group with a semi-structured theme approach, as reported by some previous authors (Heaney, Tolhurst, & Baines, 2004; Denham & Shaddock, 2004).
It is thought that, to some extent, Korean culture and the system of medical practice in Korea influenced students’ perceptions of the book and their reactions, so this study may present some interesting inter-cultural perspectives.
Since the present study did not have a pre-test and post-test design, we could not see the impact of this teaching mode on students’ beliefs or attitudes in a qualitative manner, which is a limitation of this study. Other minor limitations are the small sample size and the fact that students were asked to reflect on different themes regarding the 2 books.
V. CONCLUSION
A Young Doctor’s Notebook allowed the readers to reflect on the virtues necessary to get a patient’s trust. Through reading The Right to Heresy, the students became aware of the importance of tolerance and determined that they would respect other people’s opinions. These books may be suitable teaching materials for the medical humanities.
Notes on Contributors
Kun Hwang is a Fellowship Professor of Department of Plastic Surgery at Inha University School of Medicine, Incheon, South Korea. He conceived the idea, planned the research, and wrote the manuscript.
Ae Yang Kim is an Adjunct Professor of Inha University School of Medicine, Incheon, South Korea, and director of Eun Hye OB & GY Clinic, Seoul, South Korea. She analysed students’ reports.
Hun Kim is on the PhD course in Department of Plastic Surgery at Inha University School of Medicine, Incheon, South Korea. He contributed statistical analysis and the table.
Ethical Approval
This study received approval from the institutional review board (IRB) of Inha University (approval number 170220-8A).
Acknowledgements
This study was supported by National Research Foundation of Korea (NRF-2017R1A2B4005787).
Declaration of Interest
The authors have no conflict of interest to declare.
References
Calman, K. C., Downie, R. S., Duthie, M., & Sweeney, B. (1988). Literature and medicine: a short course for medical students. Medical Education, 22(4), 265-269.
Denham, L. A., and Shaddock, A. J. (2004). Recruitment and retention of rural allied health professionals in developmental disability services in New South Wales. Australian Journal of Rural Health, 12, 28-29.
Fiscella, K., Meldrum, S., Franks, P., Shields, C. G., Duberstein, P., McDaniel, S. H., & Epstein, R. M. (2004). Patient trust: is it related to patient-centered behavior of primary care physicians? Medical Care, 42(11), 1049-1055.
Gopichandran, V., & Chetlapalli, S. K. (2015). Trust in the physician-patient relationship in developing healthcare settings: a quantitative exploration. Indian Journal of Medical Ethics, 12(3), 141-148.
Heaney, S. E., Tolhurst, H., and Baines, SK (2004). Choosing to practice in rural dietetics: what factors influence that decision? Australian Journal of Rural Health, 12, 192-196.
Hwang, I. K. (2013). Teaching Medical Humanities through an Illness Narrative. Korean Journal of Medical Education, 25(2), 81-88. https://doi.org/10.3946/kjme.2013.25.2.81.
Hwang, K., Lee, S. J., Kim, S. Y., Hwang, S. W., & Kim, A. Y. (2014). Medical doctor as a captain of a ship: An analysis of a book report of Conrad’s “Lord Jim”. Journal of Educational Evaluation for Health Professions, 11, 33.
Hwang, K., Hong, H. S., & Heo, W. Y. (2014). Would medical students enter an exclusion zone in an infected district with a high mortality rate? An analysis of book reports on “28” (secondary publication). Journal of Educational Evaluation for Health Professions, 11, 15.
Hwang, K., Kim, H., Kim, A. Y., Hwang, S. W., & Hwang, S. H. (2016). What is like to be a devoted doctor? An analysis of book reports on The Painted Veil. Korean Journal of Medical Education, 28(1), 103-109.
Hwang, S. W., Kim, H., Kim, A. Y., & Hwang K. (2016). Analysis of medical student’s book reports on Cronin’s The Citadel: Would young doctors give up ideals for prestige and wealth? Korean Journal of Medical Education, 28(2), 231-235.
Jacobson, L., Grant, A., Hood, K., Lewis, W., Robling, M., Prout, H., & Cunningham, A. M. (2004). A literature and medicine special study module run by academics in general practice: two evaluations and the lessons learnt. Medical Humanities, 30(2), 98-100.
Korea Herald (2016a, May 19). Assembly passes undisputed bill in final session. Retrieved from http://www.koreaherald.com/view.php?ud=20160519000882.
Korea Herald (2016b, March 4). Doctor in reused syringe infection case found dead. Retrieved from http://www.koreaherald.com/view.php?ud=20160304000566.
Lancaster, T., Hart, R., & Gardner, S. (2002). Literature and medicine: evaluating a special study module using the nominal group technique. Medical Education, 36(11), 1071-1076.
Lee, Y. M. & Rhee, Y. H. (2003). How Can Literature Contribute to Medical Education? Korean Journal of Medical Education, 15(2), 83-90. Retrieved from http://kjme.kr/journal/view.php?number=697.
Bulgakov, M. (1970). Zapiski Iunogo Vracha [The Notes of a Young Doctor] (Lee, B. H., trans). Russia: Prideaux Press.
Maruani, A., Léger, J., Giraudeau, B., Naouri, M., Le Bidre, E., Samimi, M., & Delage, M. (2013). Effect of physician dress style on patient confidence. Journal of the European Academy Dermatology and Venereology, 27(3), e333-e337.
Simon, M. A., Zhang, M., & Dong, X. (2014). Trust in physicians among U.S. chinese older adults. The Journals of Gerontology. Series A, Biological sciences and medical sciences, 69 Suppl 2, S46-S53.
Singh, M. (2016). Communication as a Bridge to Build a Sound Doctor-Patient/Parent Relationship. The Indian Journal of Pediatrics, 83(1), 33-37.
Zweig, S. (1936). The Right to Heresy, New York: The Viking Press.
*Kun Hwang, M. D., Ph.D.
Department of Plastic Surgery
Inha University School of Medicine
Incheon, Korea
Email: jokerhg@inha.ac.kr
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









