The COVID-19 pandemic: Impact on interns in a paediatric rotation
Submitted: 21 August 2020
Accepted: 12 November 2020
Published online: 4 May, TAPS 2021, 6(2), 57-65
https://doi.org/10.29060/TAPS.2021-6-2/OA2378
Nicholas Beng Hui Ng1,2, Mae Yue Tan1,2, Shuh Shing Lee3, Nasyitah binti Abdul Aziz3, Marion M Aw1,2 & Jeremy Bingyuan Lin1,2
1Khoo Teck Puat-National University Children’s Medical Institute, National University Health System Singapore; 2Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Centre for Medical Education (CenMED), Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: The coronavirus disease 2019 (COVID-19) pandemic has brought about additional challenges beyond the usual transitional stresses faced by a newly qualified doctor. We aimed to evaluate the impact of COVID-19 on interns’ stress, burnout, emotions, and implications on their training, while exploring their coping mechanisms and resilience levels.
Methods: Newly graduated doctors interning in a Paediatric department in Singapore, who experienced escalation of the pandemic from January to April 2020, were invited to participate. Participants completed the Perceived Stress Scale (PSS), Maslach’s Burnout Inventory (MBI), and Connor Davidson Resilience Scale 25-item (CD-RISC 25) pre-pandemic and 4 months into COVID-19. Group interviews were conducted to supplement the quantitative responses to achieve study aims.
Results: Response rate was 100% (n=10) for post-exposure questionnaires and group interviews. Despite working through the pandemic, interns’ stress levels were not increased, burnout remained low, while resilience remained high. Four themes emerged from the group interviews – the impacts of the pandemic on their psychology, duties, training, as well as protective mechanisms. Their responses, particularly the institutional mechanisms and individual coping strategies, enabled us to understand their unexpected low burnout and high resilience despite the pandemic.
Conclusion: This study demonstrated that it is possible to mitigate stress, burnout and preserve resilience of vulnerable healthcare workers such as interns amidst a pandemic. The study also validated a multifaceted approach that targets institutional, faculty as well as individual levels, can ensure the continued wellbeing of healthcare workers even in challenging times.
Keywords: COVID-19, Stress, Burnout, Resilience, Junior Doctor, Intern
Practice Highlights
- Intern doctors face additional and unique challenges in a pandemic, besides the usual stresses of their school-to-work transition.
- Our study shows that a multi-faceted approach that target institution, faculty and individual can lead to reduced burnout and preserved resilience in these doctors.
I. INTRODUCTION
With the coronavirus disease 2019 (COVID-19) pandemic, there are new stressors contributing to burnout in healthcare workers. We were particularly interested in evaluating the impact of COVID-19 on newly qualified doctors doing their internship, also known as House Officers or post-graduate year 1 doctors in Singapore. This is a particularly vulnerable group of healthcare workers as the school-to-work transitional year is traditionally a challenging period with high reports of burnout (Low et al., 2019; Sturman et al., 2017).
In Singapore, our first case of COVID-19 was on 23 January 2020. By February 2020, Singapore had one of the highest numbers of cases out of China (Chia & Moynihan, 2020). A global pandemic was declared on 12 March 2020. In early April 2020, the government tightened local measures with a ‘Circuit Breaker’, akin to the lockdowns in many countries (Ministry of Health Singapore, 2020).
Newly graduated doctors in Singapore complete a 12-month training period (4-month rotations in 3 different disciplines) prior to full medical registration. The period of January to April 2020 was during their third block and coincided with the full evolution of the pandemic, which came with multiple unexpected changes in work within the hospital. These included new protocols for personal protection, team segregation and mechanisms to cope with the increase in COVID-19 cases. In our department, interns and residents were divided into active and passive teams rotating fortnightly, where the active team had to shoulder the responsibility of caring for at risk or COVID-19 paediatric patients, with an intense overnight call duty schedule, different from the weekly frequency in the non-pandemic setting. In addition to work changes, there were also cancellation of overseas leave as well as cessation of scheduled teaching sessions.
With these changes, we aimed to evaluate the impact of the COVID-19 pandemic on interns in our department, focusing on their psychological well-being in terms of stress and burnout, and impact on clinical training. Our secondary aim was to explore the interns’ resilience, coping mechanisms and identify systemic measures they perceived as helpful during this pandemic.
II. METHODS
A. Study Design and Sample
This was a mixed-methods quantitative and qualitative study involving interns who worked from January to April 2020, in a paediatric department at a tertiary academic hospital that actively admitted COVID-19 patients. Informed consent was obtained from all participants for both the quantitative and qualitative components of the study.
B. Quantitative Data Methodology
Pre-pandemic data on perceived stress, burnout and resilience levels were collected a priori in early January 2020, when the interns first joined the department. This was part of a baseline evaluation of a separate study. We employed validated scales: the Perceived Stress Scale (PSS) (Cohen et al., 1983), the Maslach Burnout Inventory (MBI) for Health Services Survey (Maslach & Leiter, 2016), and the Connor-Davidson Resilience Scale 25-item (CD-RSIC 25) (Connor & Davidson, 2003) to measure stress, burnout and resilience respectively. The PSS measures the perception of stress, and is designed to tap how unpredictable, uncontrollable, and overloaded respondents find their lives. Scores ranging from 0-13, 14-26, and 27-40 are mild, moderate, and high perceived stress, respectively. The MBI is a 22-item inventory with scores in 3 domains of burnout: emotional exhaustion (EE), depersonalization (DP), and low personal accomplishment (PA) based on multiple questions for each of these subscales. We used a strict definition of burnout as having fulfilled criteria in all 3 domains of the MBI (i.e. high EE ≧ 27, high DP ≧ 10, and low PA ≦ 33). A liberal definition (i.e. high EE ≧ 27 and high DP ≧ 10 with or without a low PA) was also measured as both definitions are widely adopted in literature (Rotenstein et al., 2018). The CD-RISC 25-item (English version) is a validated scale to measure resilience. It gives a score ranging from 0 to 100, with higher scores reflecting greater resilience. On completion of the posting in end April 2020, the interns repeated the same set of questionnaires.
C. Qualitative Data Methodology: Group Discussions
We conducted group interviews to further evaluate the responses obtained from the questionnaires and to better understand the impact on the interns. Invitation emails were sent to all interns; participation was voluntary. The questions were developed to explore the challenges, emotions, psychological states and reflections of their coping mechanisms and supportive measures of the interns while working in the pandemic. The questions were developed and refined by the authors after discussion and consensus (Appendix 1). Two group interviews were conducted on separate days by the same interviewer, to maintain team segregation and physical distancing. Each group had 5 participants. The sessions were recorded and subsequently transcribed by an independent party.
D. Data Analysis
Quantitative data on the validated scales were scored according to the corresponding manuals. Descriptive and comparative analysis was done with SPSS, Version 23. For the interviews, thematic analysis was conducted. Two of the authors (SS & NAA) read the transcripts to understand fully the data, generated the initial codes independently. Next, codes with consistently similar content were grouped into sub-categories, and similar sub-categories were then combined into categories to form themes. In the event there were differing views on the coding or theme, they re-examined the primary data and further discussed to achieve consensus.
III. RESULTS
A. Quantitative Results
We had a 90% response rate (n=9) for the pre-exposure and 100% (n=10) for the post-exposure questionnaires. There was no change in PSS scores among the interns despite the pandemic, with both median scores in the moderate stress category at 17.5 post-exposure and 17 pre-exposure. There was no high perceived stress in all interns post-exposure. Using the strictest definition of burnout, burnout remained low at 20% post-exposure, compared to 11.1% pre-exposure (Table 1). When a more liberal definition of burnout is used as discussed in the methodology section, only 20% of participants were burnout post-exposure, compared to 66.7% of participants pre-exposure. High resilience levels were maintained, with median score of 74 pre-exposure and 72.5 post-exposure.
|
Measures |
Pre-exposure, (n=9) |
Post-exposure, (n=10) |
p value |
|
Perceived Stress Scale (PSS) |
|||
|
Median (SD) |
17 (6.75) |
17.50 (5.70)
|
N.A |
|
Low stress, n (%) |
4 (44.4%) |
3 (30%)
|
0.65 |
|
Moderate stress, n (%) |
4 (44.4%) |
7 (70%)
|
0.37 |
|
High stress, n (%) |
1 (11.1%) |
0 (0%)
|
0.474 |
|
Maslach Burnout Inventory (MBI) |
|||
|
No burnout, n (%) |
3 (33.3%) |
4 (40.0%) |
0.999 |
|
Strict definition of burnout, n (%) |
1 (11.1%) |
2 (20.0%)
|
0.999 |
|
Liberal definition of burnout, n (%) |
6 (66.7%) |
2 (20%) |
0.09 |
Table 1: Quantitative results showing scores on the Perceived Stress Scale and Maslach Burnout Inventory of the interns pre-pandemic, compared with scores post-exposure. (SD= Standard Deviation).
B. Qualitative Results
We had 100% participation in the group interviews (n=10). Four themes emerged from the qualitative analysis – psychological impact (feelings), impact on duties, impact on teaching and learning as well as preventive measures and support system. These are summarised in Table 2.
|
Key Theme 1: Psychological Impact (Feelings) |
|
|
Sub-themes |
Sample of quotations |
|
a) Loss of control coping with many changes
b) Emotional exhaustion (fear, burnout, uncertainty, loneliness)
c) Positive feelings |
“…throughout the pandemic, there were a lot of unexpected changes and uncertainty among the junior doctors especially the PGY1s (referring to interns)…”
“…COVID gives people much stress due to the uncertainty in a lot of things…” “the thought of COVID patients is scary” “…if I really contract this (COVID-19) I wouldn’t have too much concern (but) I was more scared I would pass it on to my family “…stress stemming from fear” “… cannot help but experienced feelings of isolation and loneliness… I avoided my mother, who is immunocompromised as I worry about passing the infection to her even when I am off active COVID-care duty…” “feeling of being protected alleviated stress and concerns related to contracting the virus” “…months during pandemic (in the posting) were enriching and enjoyable…” “working during pandemic is deemed as “a badge of honour” “felt the months during pandemic situation was a ‘good learning experience’”
|
|
Key Theme 2: Impact on Duties |
|
|
Sub-themes |
Sample of quotations |
|
a) Changes in clinical duties
b) Dealing with rapidly changing protocols
|
“felt that manpower shortage coupled with more frequent on-call duties within two weeks causes early burnout”
“…I think on the ground level the protocol is always bleak, for example who to swab and when…” “delayed updating of protocol online led to a bit of confusion” “not getting updated instantaneously and lack of accessible to the information” |
|
Key Theme 3: Impact on Teaching and Learning |
|
|
Sub-themes |
Sample of quotations |
|
a) Clinical exposure
b) Changes in teaching approaches |
“…in terms of the variety of cases in posting, it is significantly affected due to pandemic that changed demographic of attendees”
“…there wasn’t much teaching on-going until recently when we got the online platforms which I do feel is more helpful…” “due to having lesser patients, feels consultants have more time to teach” “while there is no group teaching, there is more teaching of cases on wards” |
|
Theme 4: Protective Measures and Support System |
|
|
Sub-themes |
Sample of quotations |
|
a) Rotation system which ensured sufficient manpower and rest
b) Institutional measures for personal protection against COVID-19 infection
c) Seniors, Peers and Staff support
d) Self-adaptability and resilience
|
“…we have enough manpower to actually toggle between the rotations for COVID-care and non-COVID services…”
“…PGY1s (Interns) are protected as we don’t swab the patients and we don’t have to expose ourselves to the possible aerolisation of the secretions, so I think that really protected us and relieved our stress…”
“… regular meetings (with) seniors that sat down to uncover our worries… seniors were open to taking feedback about rostering and manpower…” “…I really think it’s the support that has been given by the department and the institution, and the seniors especially have been very supportive…”
“…think of the hardships faced by other health professionals, one’s situation will not compare to theirs” “…stay strong, persevere, and that everyone will get through it together by supporting each other” “…remember that it was a choice and that it is also a privilege to be in medicine…” |
Table 2: Summary of key themes and sub-themes as well as verbatim quotations from our interns, from the group interviews.
1) Theme 1 – Psychological Impact (Feelings): Most interns perceived that the pandemic had caused drastic changes in their personal and work lives, with various psychological impacts. They expressed increased emotional exhaustion such as stress and burnout, that is mainly related to changes in their clinical duties (Theme 2). The interns also shared about risks of COVID-19 infection to self and especially to family and loved ones, increasing their worries and stress. Interns followed physical distancing measures and team segregation at work, but several interns avoided their loved ones at home, especially the elderly and immunocompromised. For these interns, they further shared feelings of isolation and loneliness. Positive emotions such as feeling secure, valued and protected existed simultaneously and were mainly associated with the protective measures and support systems (Theme 4) in the workplace. Some also reported that the posting was still enjoyable and felt proud to be working in the pandemic.
2) Theme 2 – Impact on Duties: The interns highlighted there were many changes in institutional work processes and their duties due to the pandemic. Due to manpower changes, there were pervasive reports of physical fatigue. There were however those who felt the workload was still manageable. Interns also raised the issue of non-timely information and unclear protocols which often led to confusion and uncertainty in their work.
3) Theme 3 – Impact on Teaching and Learning: There were mixed comments on this. As a result of strict physical distancing and team segregation, initial planned teaching sessions on general paediatrics were cancelled and the interns felt they “missed out” on their clinical training. Sessions were subsequently conducted using web-based platforms, which many found helpful. All interns felt that learning was restricted in the pandemic. Although it was beneficial to learn about pandemic response and management of suspected or affected COVID-19 patients, they felt their exposure to general paediatrics was reduced due to the limited variety of ward cases. However, there were some who felt there was better quality of teaching on the ward rounds as consultants had more time to teach with fewer elective and non-urgent cases in the rotations of non-COVID care.
4) Theme 4 – Preventive Measures and Support Systems: Despite the impacts on the interns’ psychology, duties and learning, they also shared on the various protective measures and support systems they perceived helped them cope. This was also the main reason for reported positive feelings of protection and support. Departmental and institutional work processes were implemented to take care of the interns’ physical and psychological welfare such as a rotational system of team segregation, which they reported provided a strict work-rest cycle as well as respite from COVID-care. In addition, seniors and faculty also ensured interns were competent and comfortable dealing with COVID-19 patients prior to taking on high risk duties such as swabbing patients. Support from multiple levels (seniors, department, institution) helped them through. In particular, the seniors and faculty provided support to the interns through regular “check-in” meetings where they could share concerns and provide feedback. The interns also shared that as a result of the strong support received, they were able to develop adaptability, perseverance and resilience, and they were even grateful to be in healthcare at this time.
IV. DISCUSSION
According to the demand-control-support model (Thomas, 2004), occupational stress causes burnout when job demands are high, individual autonomy is low and when job stress interferes with home life (Campbell et al., 2001; Linzer et al., 2001). On that note, we hypothesised that with the COVID-19 pandemic, interns would have increased stress and burnout, in addition to their routine difficulties in the transition from student to doctor. The pandemic-related concerns our interns had were similar to many healthcare workers globally – including the fear of contracting COVID-19 and more so transmitting it to vulnerable loved ones (Chen et al., 2020). Physical fatigue was also seen in our interns given the more intensive work schedule (Sasangohar et al., 2020). Although the total amount of admissions during the period was reduced to 40% of the usual load, the need for team segregation had led to a smaller pool of interns covering each clinical area. In addition, each intern had to do more in-house night calls while on active service. Segregation also meant that there would be less cross-coverage of duties where interns would receive less support from peers who would otherwise have been able to help with the workload on the ground. Another important aspect that had led to reported stress among many was the frequent changes in clinical workflows coupled with the lack of timely and reliable information (Wu et al., 2020). Many interns also highlighted concerns with regards to compromise and interference with their paediatric internship training (Liang et al., 2020). Despite all these, objectively the interns’ perceived stress was maintained without increase in burnout.
Burnout is known to be inversely related to resilience – this pattern is also reflected in our results. Resilience is the process of adapting well in the face of adversity, trauma, tragedy, threats or even significant sources of stress (Southwick et al., 2014). Our interns had high resilience scores, above what has previously been published among physicians (McKinley et al., 2020). One reason for this may be the development of resilience through a time of crisis, a phenomenon well encapsulated by the Crisis Theory: during a crisis or disequilibrium such as the current pandemic, people make attempts to adapt and seek solutions to restore stability. (Brooks et al., 2017; Caplan, 1964). The development of resilience is increasingly emphasised as an integral strategy to combat burnout. Potentially, the mitigating factors, coping mechanisms and support shared by our interns in the interviews, could explain their low burnout and high resilience.
Our interns perceived many systemic measures helped them cope with the pandemic – giving testament to the importance of institutional leadership in implementing safeguards for psychological health (Dewey et al., 2020; Wu et al., 2020). Protocols relating to staff protection, availability of personal protective equipment (Rasmussen et al., 2020) were some of the measures common to institutions worldwide. Furthermore, interns being the most junior member of the team, were spared from doing aerosolising procedures such as intubation, nebulisation administration and airway suctioning that were deferred to clinicians with prior experience and training. This allowed interns time to learn and improve in their competency and confidence prior to assuming these responsibilities. The interns were also thankful for the protected work-rest cycles (Wu et al., 2020), and that they were allowed to take paid leave – which is essential, more so in the pandemic to reduce fatigue and allowed time for rejuvenation.
Other than institutional support, direct support from seniors and faculty were significant in our interns’ responses in helping them, supporting the importance of mentorship (Ramanan et al., 2006). Despite feeling that they might not have reliable and timely access to important updates, they felt supported under the direct guidance of seniors who took the lead on the ground. Regular fortnightly ‘check-in’ sessions were conducted to elicit concerns, obtain feedback, and ensure continual wellbeing. This channel of communication was well received by interns: they appreciated the faculty’s concerns, had the autonomy of being able to input and contribute to the care of patients, the opportunity to air grievances confidentially and importantly, had closure on concerns they have raised regarding their rotations and training (Fischer et al., 2019). The enhanced collegiality between interns, support from seniors and improved cooperation among healthcare workers during this time of crisis naturally also contributed to reduced burnout levels, a finding well established in literature.(Li et al., 2013)
In terms of the impact of training, teaching sessions were initially discontinued to maintain physical distancing. Moreover, the interns had a higher proportion of time spent in the provision of COVID-19 care, which meant traditional general paediatric exposure was compromised. However, within 4 weeks of the pandemic, departmental teaching activities were restored via web-based sessions which interns found useful. The role of faculty in persisting with academic continuity, is again important in mitigating the impact of the pandemic on learning – some interns felt they had more teaching on the wards as consultants had more time to teach for each patient.
We believe that the perceived continual institutional and senior support for our interns allowed them to maintain high personal resilience, that could have mitigated their stress and burnout. In this pandemic, interns demonstrated adaptability and perseverance to the many changes, ability to persevere as well as finding gratitude amidst the challenges and focusing on their goal to help patients and fight the pandemic, which are all known features of resilience (Bird & Pincavage, 2016; Zwack & Schweitzer, 2013).
To our knowledge, this is the first research study in the pandemic that objectively evaluated the impact of the COVID-19 on interns’ psychological state, resilience and training. However, we recognise our study limitations. The small population would mean that it would be difficult to derive statistical comparisons in the pre- and post-exposure results. However, we believe the temporal exposure of the pandemic for this group of interns during their posting, made the pre- and post-pandemic results valid. The results were further supported by qualitative findings from a good group interview participation (100%) and in-depth discussion, that provided substantial explanations to the trend of results. We recognise that 2-4 months might be a short duration for negative psychological effects such as stress, and burnout to set in. Nonetheless, the amount of unprecedented changes and intensity of work for the interns involved within this period, were undoubtedly high. Another study limitation is the inclusion of Paediatric interns only and the possible lower exposure to COVID-19 as compared to their adult counterparts due to decreased disease morbidity and mortality in children. Although this factor could potentially result in less impact on the psychological factors studied, we believe other interns are likely to face similar concerns and challenges in the pandemic, due to their similar backgrounds and job scopes across most departments and disciplines.
This study elucidated the impact of the pandemic on interns in terms of their stress, burnout, as well as clinical duties and training. Despite increasing concerns on the psychological well-being of healthcare workers in the pandemic, our study has demonstrated that it is possible to mitigate their stress, burnout and preserve resilience, even in vulnerable new medical graduates. Our findings objectively validated the importance and effectiveness of the multi-faceted approach that target institution, faculty as well as the individual level, to build resilience and combat burnout in healthcare providers in this pandemic and beyond.
Notes on Contributors
Nicholas BH Ng contributed to conception and design of study, interpretation of data, drafting and critical revising of the article. Mae Yue Tan contributed to analysis and interpretation of data, drafting and critical revising of the article. Shuh Shing Lee contributed to analysis and interpretation of data, drafting and critical revising of the article. Nasyitah bte Abdul Aziz contributed to analysis and interpretation of data, drafting of the article. Marion M Aw contributed to interpretation of data, drafting and critical revising of the article. Jeremy BY Lin contributed to conception and design, interpretation of data, drafting and critical revising of the article. All authors gave final approval of the version to be published.
Data Availability
The data for this study can be found at https://doi.org/10.6084/m9.figshare.12924029.v1. The access to these datasets are available for use subject to approval of the authors of this article.
Ethical Approval
Ethics approval was obtained from the NHG Domain Specific Review Board (DSRB), with NHG DSRB reference number of 2020/00392.
Acknowledgement
The authors would like to thank the interns who participated in this study.
Funding
Funding for this study was obtained from NUHS Fund Limited – Medical Affairs (Education) Fund.
Declaration of Interest
All authors have no conflicts of interest to declare.
References
Bird, A., & Pincavage, A. (2016). A curriculum to foster resident resilience. MedEdPORTAL, 12, 10439. https://doi.org/10.15766/mep_2374-8265.10439
Brooks, S. K., Dunn, R., Amlôt, R., Rubin, G. J., & Greenberg, N. (2017). Social and occupational factors associated with psychological wellbeing among occupational groups affected by disaster: A systematic review. Journal of Mental Health, 26(4), 373-384. https://doi.org/10.1080/09638237.2017.1294732
Campbell, D. A., Jr., Sonnad, S. S., Eckhauser, F. E., Campbell, K. K., & Greenfield, L. J. (2001). Burnout among American surgeons. Surgery, 130(4), 696-702; discussion 702-695. https://doi.org/10.1067/msy.2001.116676
Caplan, G. (1964). Principles of preventive psychiatry. Basic Books.
Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D., Wang, L., He, L., Sheng, C., Cai, Y., Li, X., Wang, J., & Zhang, Z. (2020). Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry, 7(4), e15-e16. https://doi.org/10.1016/s2215-0366(20)30078-x
Chia, R., & Moynihan, Q. (2020, February 20). This alarming map shows where the coronavirus has spread in Singapore, one of the worst-hit areas outside of China Business Insider Singapore. Business Insider. https://www.businessinsider.com/coronavirus-singapore-map-shows-spread-worst-hit-outside-china-2020-2?IR=T.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behaviour, 24(4), 385-396.
Connor, K. M., & Davidson, J. R. (2003). Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression and Anxiety, 18(2), 76-82. https://doi.org/10.1002/da.10113
Dewey, C., Hingle, S., Goelz, E., & Linzer, M. (2020). Supporting clinicians during the COVID-19 pandemic. Annals of Internal Medicine, 172(11), 752-753. https://doi.org/10.7326/M20-1033
Fischer, J., Alpert, A., & Rao, P. (2019). Promoting intern resilience: Individual chief wellness check-ins. MedEdPORTAL, 15, 10848. https://doi.org/10.15766/mep_2374-8265.10848
Li, B., Bruyneel, L., Sermeus, W., Van den Heede, K., Matawie, K., Aiken, L., & Lesaffre, E. (2013). Group-level impact of work environment dimensions on burnout experiences among nurses: A multivariate multilevel probit model. International Journal of Nursing Studies, 50(2), 281–291. https://doi.org/10.1016/j.ijnurstu.2012.07.001
Liang, Z. C., Ooi, S. B. S., & Wang, W. (2020). Pandemics and their impact on medical training: Lessons From Singapore. Academic Medicine. https://doi.org/10.1097/acm.0000000000003441
Linzer, M., Visser, M. R., Oort, F. J., Smets, E. M., McMurray, J. E., & de Haes, H. C. (2001). Predicting and preventing physician burnout: results from the United States and the Netherlands. The American Journal of Medicine, 111(2), 170-175. https://doi.org/10.1016/s0002-9343(01)00814-2
Low, Z. X., Yeo, K. A., Sharma, V. K., Leung, G. K., McIntyre, R. S., Guerrero, A., Lu, B., Lam, C. C. S. F., Tran, B. X., Nguyen, L. H., Ho, C. S., Tam, W. W., & Ho, R. C. (2019). Prevalence of burnout in medical and surgical residents: A meta-analysis. International Journal of Environmental Research and Public Health, 16(9). https://doi.org/10.3390/ijerph16091479
Maslach, C. J. S., & Leiter, M. P. (2016). Maslach burnout inventory manual. Mind Garden Inc.
McKinley, N., McCain, R. S., Convie, L., Clarke, M., Dempster, M., Campbell, W. J., & Kirk, S. J. (2020). Resilience, burnout and coping mechanisms in UK doctors: A cross-sectional study. British Medical Journal Open, 10(1), e031765. https://doi.org/10.1136/bmjopen-2019-031765
Ministry of Health (MOH), Singapore. (2020). Circuit breaker to minimise further spread of COVID-19. https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19. (Retrieved April 3, 2020)
Ng, N. B. H (2020). The COVID-19 Pandemic: Impact on Paediatric Postgraduate Year One Doctors [Data set]. Figshare. https://figshare.com/s/74c81ca193638a553ea2
Ramanan, R. A., Taylor, W. C., Davis, R. B., & Phillips, R. S. (2006). Mentoring matters. Mentoring and career preparation in internal medicine residency training. Journal of General Internal Medicine, 21(4), 340-345. https://doi.org/10.1111/j.1525-1497.2006.00346.x
Rasmussen, S., Sperling, P., Poulsen, M. S., Emmersen, J., & Andersen, S. (2020). Medical students for health-care staff shortages during the COVID-19 pandemic. The Lancet, 395(10234), e79-e80. https://doi.org/10.1016/s0140-6736(20)30923-5
Rotenstein, L. S., Torre, M., Ramos, M. A., Rosales, R. C., Guille, C., Sen, S., & Mata, D. A. (2018). Prevalence of burnout among physicians: A systematic review. The Journal of the American Medical Association, 320(11), 1131-1150. https://doi.org/10.1001/jama.2018.12777
Sasangohar, F., Jones, S. L., Masud, F. N., Vahidy, F. S., & Kash, B. A. (2020). Provider burnout and fatigue during the COVID-19 pandemic: Lessons learned from a high-volume intensive care unit. Anesthesia and Analgesia, 131(1), 106–111. https://doi.org/10.1213/ane.0000000000004866
Southwick, S. M., Bonanno, G. A., Masten, A. S., Panter-Brick, C., & Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5,(1), 25338. https://doi.org/10.3402/ejpt.v5.25338
Sturman, N., Tan, Z., & Turner, J. (2017). “A steep learning curve”: Junior doctor perspectives on the transition from medical student to the health-care workplace. BMC Medical Education, 17(1), 92. https://doi.org/10.1186/s12909-017-0931-2
Thomas, N. K. (2004). Resident burnout. The Journal of the American Medical Association, 292(23), 2880-2889. https://doi.org/10.1001/jama.292.23.2880
Wu, P. E., Styra, R., & Gold, W. L. (2020). Mitigating the psychological effects of COVID-19 on health care workers. Canadian Medical Association Journal, 192(17), E459-e460. https://doi.org/10.1503/cmaj.200519
Zwack, J., & Schweitzer, J. (2013). If every fifth physician is affected by burnout, what about the other four? Resilience strategies of experienced physicians. Academic Medicine, 88(3), 382-389. https://doi.org/10.1097/ACM.0b013e318281696b
*Jeremy Bingyuan Lin
1E Kent Ridge Road,
NUHS Tower Block Level 12,
Singapore 119228
Tel: (65) 6772 4847
Email: jeremy_lin@nuhs.edu.sg
Submitted: 28 July 2020
Accepted: 18 November 2020
Published online: 4 May, TAPS 2021, 6(2), 48-56
https://doi.org/10.29060/TAPS.2021-6-2/OA2367
Oscar Gilang Purnajati1, Rachmadya Nur Hidayah2 & Gandes Retno Rahayu2
1Faculty of Medicine, Universitas Kristen Duta Wacana, Yogyakarta, Indonesia; 2Department of Medical Education, Faculty of Medicine, Universitas Gadjah Mada, Yogyakarta, Indonesia
Abstract
Introduction: Objective Structured Clinical Examination (OSCE) examiners come from various backgrounds. This background variability may affect the way they score examinees. This study aimed to understand the effect of background variability influencing the examiners’ score agreement in OSCE’s procedural skill.
Methods: A mixed-methods study was conducted with explanatory sequential design. OSCE examiners (n=64) in the Faculty of Medicine Universitas Kristen Duta Wacana (FoM-UKDW) took part to assess two videos of Cardio-Pulmonary Resuscitation (CPR) competence to get their level of agreement by using Fleiss Kappa. One video portrayed CPR according to performance guideline, and the other portrayed CPR not according to performance guidelines. Primary survey, CPR procedure, and professional behaviour were assessed. To confirm the assessment results qualitatively, in-depth interviews were also conducted.
Results: Fifty-one examiners (79.7%) completed the assessment forms. From 18 background categories, there was a good agreement (>60%) in: Primary survey (4 groups), CPR procedure (15 groups), and professional behaviour (7 groups). In-depth interviews revealed several personal factors involved in scoring decisions: 1) Examiners use different references in assessing the skills; 2) Examiners use different ways in weighting competence; 3) The first impression might affect the examiners’ decision; and 4) Clinical practice experience drives examiners to establish a personal standard.
Conclusion: This study identifies several factors of examiner background that allow better agreement of procedural section (CPR procedure) with specific assessment guidelines. We should address personal factors affecting scoring decisions found in this study in preparing faculty members as OSCE examiners.
Keywords: OSCE Score, Background Variability, Agreement, Personal Factor
Practice Highlights
- The examiners’ background variability influences the OSCE scoring agreement results.
- The reason for assessment inaccuracy remains unclear regarding the score agreement.
- The absence of assessment instruments that could provide a loophole for examiners to improvise.
- Personal factors affecting scoring decisions found in this study should be addressed in preparing OSCE examiners.
I. INTRODUCTION
To assess medical students’ competencies in a variety of skills, most medical schools in Indonesia implement the Objective Structured Clinical Examination (OSCE) both as a clinical skills examination at the undergraduate stage and as a national exit exam (Rahayu et al., 2016; Suhoyo et al., 2016). Most OSCE stations test both communication domains and specific clinical skills that will be assessed based on rubrics and scoring checklists which relies on examiners’ observations (Setyonugroho et al., 2015). The OSCE has a challenge in its complexity to standardise the scores, which are very depend on OSCE examiners’ perceptions (Pell et al., 2010). In a well-designed OSCE the examinees performance should only influence the examinees’ score, with minimal effects from other sources of variance (Khan et al., 2013). Research showed that there are influences of examiner’s background variability on OSCE results although they have been asked to standardise their behaviour (Pell et al., 2010) The decision and behaviour of OSCE examiners will affect the quality of assessment, including making a pass or fail decision, considering the complexity of knowledge, skill, and attitude in medical education (Colbert-Getz et al., 2017; Fuller et al., 2017).
Examiners’ observations also rely on their clinical practice experience, OSCE examining experience, and gender conformity (Mortsiefer et al., 2017). Even in OSCE that is held in the most standard conditions, the examiner factor has the biggest role in scoring inaccurately (Mortsiefer et al., 2017). However, the reason for this inaccuracy remains unclear since there are concerns regarding the scoring agreement of examiners in OSCE and how the result might be affected by this issue. There is a need to consider the influence of examiners’ background variability (gender, educational level, clinical practice experiences, length of clinical practice experiences, OSCE experience, and OSCE training experience) when preparing teachers as OSCE examiners. This study aimed to understand background variability as a factor influencing examiners’ scoring agreement in assessing students’ performance in procedural skill, as the first step of faculty development program to ensure the standard quality for examiners.
II. METHODS
A. Study Design
This mixed-method study used a sequential explanatory design. This mixed-method approach is expected to provide more comprehensive results and better understanding than using a separated method (Creswell & Clark, 2018).
This study comprised of 2 sequential phases of data collection and analysis (QUANTITATIVE: qualitative) using sequential design. First, quantitative data were collected as a cross-sectional study of the examiners’ strength of agreement using Fleiss Kappa while assessing the clinical skill performance recorded in the 2 videos: one video portrayed CPR according to performance guideline and the other portrayed CPR not according to performance guideline. We used these 2 videos in order to portray more comprehensively how the consistency of OSCE examiner agreement both on good and poor clinical skill performance.
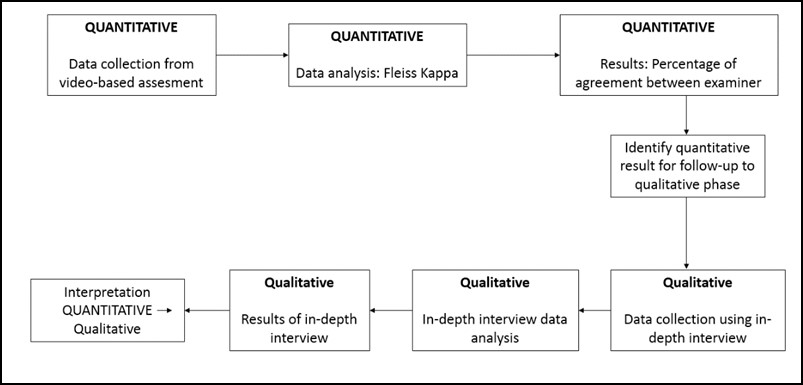
Figure 1 Mixed method explanatory design
In the second phase, in-depth interviews were used to complement the quantitative results to gain more information and a detailed confirmation about how the scores were decided (Stalmeijer et al., 2014). In this stage of study, researchers explored and explained the examiners’ OSCE experiences and behaviour when they give a score on a clinical skill examination and the influences on their scoring regarding their backgrounds.
B. Materials and/or Subjects
The strength of agreement of the videos’ score came from 64 OSCE examiners FoM UKDW. Mortsiefer et al., (2017), explained that more subjects are better when investigate examiner characteristics associated with inter-examiner reliability (Mortsiefer et al., 2017). In the second phase, in-depth interviews were conducted with 6 examiners of FoM UKDW, selected by purposive sampling regarding their scores and how they represented their own unique background (Table 1).
Researcher (OGP) provided all the participants with written information about this research and addressed ethical issues in an informed consent form. Researcher ensured participants understand the research protocol and clarified any questions regarding this study. Participants who agreed to take part, sign the informed consent form prior to the data collection.
We held interviews in FoM UKDW with maximum 30 minutes of duration each interview. The inclusion criteria for examiners who were selected for this study were involved as full-time faculty members, had over 4 times OSCE examination experience, and had done OSCE examiner training, expecting that they had enough interaction with other faculty members and had influences from medical doctor education (Park et al., 2015). The exclusion criteria were participant did not answer the research invitation and did not fill the assessment form completely. Main researcher (OGP) conducted the interview. Main researcher was a male, student of Master of Health Profession Education Universitas Gadjah Mada, and the staff of FoM UKDW.
C. Statistics
1)Quantitative data analysis: We grouped examiners into 18 groups based on their background which were gender, educational level, clinical practice experiences, length of clinical practice experiences, OSCE experience, and OSCE training experience as shown in Table 1. We analysed all gathered data using IBM SPSS Statistics 25 and Microsoft Office Excel 365 (IBM Corp., Chicago). We presented quantitative data as a strength of agreement in percentage. The strength of agreement was calculated using Fleiss Kappa to determine the agreement between each group of each examiner background on whether CPR performances (primary survey, CPR Procedure, and professional behaviour), that portrayed in those 2 videos, were exhibiting score either “0”, “1”, “2”, or “3” based on the assessment guideline and rubric’s criteria (Purnajati, 2020). Based on recent research, agreement above 60% was considered as a substantial and adequate agreement (Stoyan et al., 2017; Vanbelle, 2019).
2) Qualitative data analysis: In-depth interviews were analysed using thematic analysis. We prepared a structured list of questions. It consisted of one key question: What was your experience in scoring the OSCE? The other additional questions evaluated the experiences of examiners in OSCE scoring including: the use of other references, differences in assessment weighting, use of own decision, clinical practice experience affecting the decision, and gender related decision making. Next, the collected data resulting from in-depth interviews were recorded using audio file recorder, read, and categorised into themes whenever they were related. The transcripts and identified themes were then given to an external coder in this study. This step was followed by our agreement for each theme. There was no repeated interview.
III. RESULTS
A. Quantitative Data Result
We deposited both quantitative and qualitative data in an online repository (Purnajati, 2020). The study participants in this quantitative phase were 64 OSCE examiners who are full-time faculty members. Twelve participants were excluded because did not fulfil the inclusion criteria. Fifty-one (79.7%) examiners who returned the completed assessment form are described below in Table 1.
|
Quantitative Phase Participant |
|||
|
Background |
Groups |
Number of Participant (N=51) |
|
|
Gender |
Male |
22 (43%) |
|
|
Female |
29 (57%) |
||
|
Education |
Bachelor undergraduate |
19 (37%) |
|
|
Master’s degree |
16 (31%) |
||
|
Doctoral degree |
3 (6%) |
||
|
Specialist doctor |
13 (25%) |
||
|
Clinical Practice Experience |
General practitioner |
28 (55%) |
|
|
Specialist |
14 (27%) |
||
|
No clinical practice |
9 (18%) |
||
|
Duration of clinical practice experience |
< 2 years |
9 (18%) |
|
|
2-5 years |
17 (33%) |
||
|
>5 years |
25 (49%) |
||
|
OSCE experience |
< 2 years |
9 (18%) |
|
|
2-5 years |
24 (47%) |
||
|
>5 years |
18 (35%) |
||
|
OSCE examiner training |
< 3 times |
21 (41%) |
|
|
3-5 times |
17 (33%) |
||
|
>5 times |
13 (25%) |
||
|
Qualitative Phase Participants. |
|||
|
a Video portrayed CPR according to performance guideline. b Video portrayed CPR not according to performance guidelines |
|||
Table 1. Descriptive characteristics of participants
The assessment rubric was divided into three main competencies: (1) primary survey, (2) CPR procedure, and (3) professional behaviour. The results showed overall agreement on each main competency based on each examiners’ background variability by using Fleiss Kappa. The percentage of agreement is shown in Figure 2, 3, and 4.
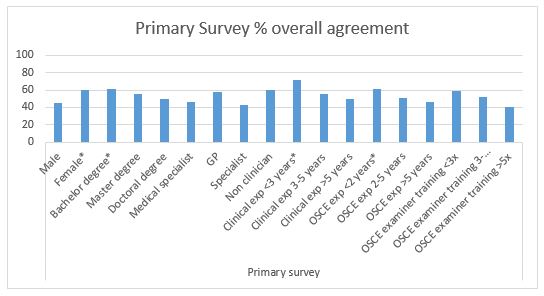
Figure 2. Primary Survey percentage of overall agreement (n = 51). Agreement above 60% (*) is considered as a substantial and adequate agreement
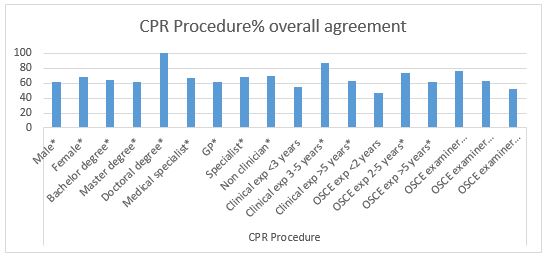
Figure 3. CPR Procedure percentage of overall agreement (n=51). Agreement above 60% (*) is considered as a substantial and adequate agreement
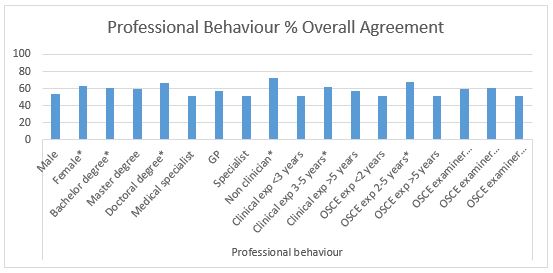
Figure 4. Professional Behaviour percentage of overall agreement (n=51). Agreement above 60% (*) is considered as a substantial
After completing the CPR competency assessment, all examiners’ background characteristics met a cutoff of approval above 60% in assessing CPR procedure except for examiners with clinical practice experience <3 years, OSCE testing experience <2 years, and OSCE examiner training> 5 years (Figure 3). This finding showed a good strength of agreement in assessing CPR procedure regardless of examiners’ background. However, there were many instances where the cut-off point of 60% was not achieved in the aspects of primary surveys and professional behaviour (Figure 2 and 4), which showed fair strength of agreement between examiners when they examined these competencies.
B. Qualitative Data Results
Two theme categories were determined: (1) OSCE experience and (2) specific behaviour in OSCE. The first theme contains of 3 sub-themes: (1) student performance, (2) examiner background effect, and (3) using assessment instrument. The second theme consists of 5 sub-themes: (1) use of assessment references, (2) score weighting, (3) personal inferences, (4) clinical experience, and (5) gender conformity.
Theme 1: Examiners argued that they understand the difference in student performance in performing clinical skills and can distinguish from the coherent skills performed by students according to checklist.
“Very easy in giving an assessment, because everything is in accordance with the assessment rubric”
(ID 35)
“The plot is clear, well organised”
(ID 26)
“You can compare the inadequacies; it is enough to be compared”
(ID 11)
“The 2 different students are quite striking, so in my opinion it is not too difficult”
(ID 28)
Nevertheless, some examiners had difficulty to distinguish student performance when only used a checklist. Examiner background did not affect their way in scoring clinical skills performance, but some background may have the potential to affect their scoring, such as clinical practice experience.
“I am trying to avoid personal interpretations, as much as possible, but of course that cannot be 100 percent. In my opinion, the assessment rubric still gives room for subjectivity”
(ID 28)
In this research, it seemed easy for examiners to understand the assessment instrument when giving score to those 2 videos and their understanding were good.
Theme 2: Interviews revealed that: 1) Examiners use other references such as their clinical experience in assessing the skills;
“If the assessment guideline is unclear, the students are also unclear, yes I will improvise. Or when the assessment guideline is clear and the students are unclear which criteria are included, yes I will improvise”
(ID 35)
“Maybe yes, because once again the template at the beginning is not very clear”
(ID 23)
2) Examiners use different ways in giving weight of competence, for example, procedural steps are considered more important than primary survey;
“For those that I feel have a small weight because the instructions are also short, so I don’t have to look carefully”
(ID 24)
“When I feel that competence is not important, it does not get my emphasis, the more emergency that will get more attention.”
(ID 28)
3) The first impression of examinees might affect their decision in scoring their performance;
“That first impression will affect me in giving value. I will be more critical. I see more, pay more attention to the small things they do”
(ID 24)
4) Clinical practice experience drives examiners to establish a personal standard on how a doctor should be;
“Clinical experience when practice is one of the judgments”
(ID 24)
“The reference is just my instinct because it has been running as a doctor after all these years. Yes, I use my previous knowledge”
(ID 26)
And 5) Gender of examinees does not affect their decision, while their professionalism (e.g. showing respect to patients) will surely affect their decision.
“I pay more attention especially to politeness and professional behaviour”
(ID 24)
“Students of any gender still have the same standard of evaluation, a score of professionalism which is more influential”
(ID 23)
IV. DISCUSSION
Examiners’ agreement in this study was high in assessing the CPR procedure, which has a fixed and specific procedure in almost all groups of examiners. These results are consistent and can be explained by results from previous studies, which show that assessment with specific cases will provide high inter-examiner agreement (Erdogan et al., 2016). The differences in the examiner’s background will not have much influence on their agreement in giving an assessment in a specific case. This was supported by the opinions of examiners in the in-depth interviews who stated that in the CPR assessment procedure, assessment instruments are clear, easy to understand, with clear procedure flow, and performance that is easily distinguished, which made it easier for examiners to be able to distinguish student performance. A specific assessment instrument that could not provide a loophole for examiners to improvise assessment, made the opportunity for examiners to portray their subjectivity was minimised. This simplicity could lead to high agreement among examiners in specific competencies as shown in this study and based on clear evidence can increase the reliability of the assessment (Daniels et al., 2014) .
In this study, it was found in the primary survey assessment and professional behaviour which has an assessment guide that is not as specific as the CPR procedure, the percentage of agreement between examiner groups was lower, with only a few of them reaching 60% of agreement. This difference happened for reasons confirmed in the in-depth interviews which raised the issue that although the examiners tried to minimise their subjectivity in assessing, but it was said that there were still gaps in the assessment guide that still gives room for subjectivity. There are also examiners who were dissatisfied with the checklist, so they used their personal decisions in evaluating students.
According to a recent study, this could be due to the lack of specific instructions in the general assessment guidelines which will result in lower inter-examiner reliability compared to the use of more specific assessment guidelines (Mortsiefer et al., 2017). In the primary survey section and professional behaviour, there were also aspects of communication that were judged to be more susceptible to bias than physical examination skills because physical examination is more well-documented, clear instructions, and more widely accepted by examiners (Chong et al., 2018) The validity and reliability of a clinical skills assessment depend on factors including how the student’s performance on the exam, the character of the population, the environment, and even the assessment instrument itself can affect how examiners carry out the assessment (Brink & Louw, 2012). These phenomena were seen in the in-depth interviews which revealed that there were certain moments namely when the student being tested does not match the expectations written in the assessment guide and when the assessment guide is not clear so that it still gives room for subjectivity examiner. In addition, in the in-depth interviews the results also revealed that the examiners differentiated their attention on certain competencies with certain criteria such as the length of information in the assessment rubric, so that competencies that were considered not important did not get as much attention.
This finding may be in line with previous research which stated that constructs and conceptual definitions in this category that still provide a gap in the subjectivity of examiners cause shifting attention focus and weighting of their judgments to be different so that there are differences in important aspects between examiners (Schierenbeck & Murphy, 2018; Yeates et al., 2013). The difference in these important aspects can bring examiners to reorganise competency weights so that simpler and easier competencies (in this case those that have clearer and more detailed assessment guidelines) will be done first, and more complex ones (in this case, guides that have lower rigidity ratings) will be assessed later with the possibility of using more narratives (Chahine et al., 2015). This reorganisation can reflect how the examiners’ decision, allowing them to direct their attention to the more important aspects as the testers revealed in in-depth interviews with this research.
The personal factor, such as assessment references is a potential variability of the assessment conducted by the examiner. Examiners are trained and understand the use of assessment instruments, but produce varying assessments because they do not apply assessment criteria appropriately, but use personal best practice, use other test participants better as benchmarks, use patient outcomes (e.g. correct diagnosis, do patients understand, etc.), and use themselves as a comparison (Gingerich et al., 2014; Kogan et al., 2011; Yeates et al., 2013).
Another personal factors, including first impressions, can occur spontaneously unconsciously and can be a source of difference in judgment between examiners (Gingerich et al., 2011). First impressions based on observers’ observations have the same decisions and influences as social interactions, so it makes sense that first impressions are able to influence judgments, can be accurate and have a relationship with the final assessment results, but do not occur in examiners in general (Wood, 2014; Wood et al., 2017).
In providing assessments, there are gaps for examiners to give different competency weights to other examiners. Providing assessments based on targets that differ from competency standards and comparisons with the performance of other examinees will make the examiners recalibrate their own weighting and this is an explanation why there are variations in assessment and differences in the important points of the examinees’ performance among examiners (Gingerich et al., 2018; Yeates et al., 2015; Yeates et al., 2013).
The variability of personal factors between examiners can be conceptualise more as a different emphasis on building doctor-patient relationships and / or certain medical expertise rather than variations in the examiner’s background itself. The examiners’ own understanding can be conceptualized as a combination of whether what the examinees do is good enough and whether what they do is enough to build a doctor-patient relationship.
This research had some limitations such as it only used specific cases (i.e., CPR) to minimise the bias of the assessment instrument so that it would reveal more bias in the examiners themselves. In more complicated cases such as communication skills and clinical reasoning it is also necessary to provide a more complete picture of how the examiners’ scores agree in other cases. Generalization also became a limitation in this study because it only involved examiners from one medical education institution, however the study participants sufficiently described the variability of the examiner’s background.
V. CONCLUSION
This study identifies several factors of examiner background variability that influence examiners’ judgment in terms of inter-examiner agreement. Female examiners, bachelor education, less OSCE experience, and non-clinician examiners allow better agreement of procedural section (CPR procedure) with specific assessment guidelines. Cases that have unspecified assessment guidelines in this research, primary survey and professional behaviour, have lower agreement among examiners and must be examined deeper. We should note that personal factors of OSCE examiners can influence assessment discrepancies. However, the reasons for using these personal factors in scoring OSCE performance might be affected by unknown biases that require further research. Therefore, to improve clinical skills assessment such as OSCE for undergraduate medical programme, we must address personal factors affecting scoring decisions found in this study in preparing faculty members as OSCE examiners.
Notes on Contributors
Oscar Gilang Purnajati, MD was student of Master of Health Professions Education Study Program, Faculty of Medicine, Universitas Gadjah Mada, Indonesia. He concepted the research, reviewed the literature, designed the study, acquisited funding, conducted interviews, analysed quantitative data and transcripts, and wrote the manuscript.
Rachmadya Nur Hidayah, MD., M.Sc., Ph.D is lecturer of Department of Medical Education, Faculty of Medicine, Universitas Gadjah Mada, Yogyakarta, Indonesia. She supervised author Oscar Gilang Purnajati, developed the concepted framework for the study, critically analysed the data, cured the data, and reviewed the final manuscript.
Prof. Gandes Retno Rahayu, MD., M.Med.Ed, Ph.D is professor at the Department of Medical Education, Faculty of Medicine, Universitas Gadjah Mada, Yogyakarta, Indonesia. She supervised author Oscar Gilang Purnajati, advised the design of the study, critically analysed the data, gave critical feedback to the conducted interviews, reviewed the final manuscript.
All the authors have read and approved the final manuscript.
Ethical Approval
This study was approved by Health Research Ethics Committee Faculty of Medicine Universitas Kristen Duta Wacana (Reference No.1068/C.16/FK/2019).
Data Availability
All data were deposited in an online repository. The data is available at Open Science Framework with DOI: https://doi.org/10.17605/OSF.IO/RDP65
Acknowledgements
The author would like to thank Hikmawati Nurrokhmanti, MD, M.Sc for helping with the process of coding the in-depth interview transcripts. The author also would like to thank the staffs of Faculty of Medicine, Universitas Kristen Duta Wacana for supporting the research.
Funding Statement
This work was supported by the Universitas Kristen Duta Wacana (No. 075/B.03/UKDW/2018) as a part of study scholarship.
Declaration of Interest
No potential conflict of interest relevant to this article was reported.
Abbreviations and specific symbols
OSCE: Objective Structured Clinical Examination.
References
Brink, Y., & Louw, Q. A. (2012). Clinical instruments: Reliability and validity critical appraisal. Journal of Evaluation in Clinical Practice,18(6), 1126-1132. https://doi.org/10.1111/j.1365-2753.2011.01707.x
Chahine, S., Holmes, B., & Kowalewski, Z. (2015). In the minds of OSCE examiners: Uncovering hidden assumptions. Advances in Health Sciences Education : Theory and Practice, 21(3), 609–625. https://doi.org/10.1007/s10459-015-9655-4
Chong, L., Taylor, S., Haywood, M., Adelstein, B.-A., & Shulruf, B. (2018). Examiner seniority and experience are associated with bias when scoring communication, but not examination, skills in objective structured clinical examinations in Australia. Journal of Educational Evaluation for Health Professions, 15(17). https://doi.org/10.3352/jeehp.2018.15.17
Colbert-Getz, J. M., Ryan, M., Hennessey, E., Lindeman, B., Pitts, B., Rutherford, K. A., Schwengel, D., Sozio, S. M., George, J., & Jung, J. (2017). Measuring assessment quality with an assessment utility rubric for medical education. MedEdPORTAL : The Journal of Teaching and Learning Resources, 13, 1-5. https://doi.org/10.15766/mep_2374-8265.10588
Creswell, J. W., & Clark, V. L. P. (2018). Designing and conducting mixed method research. SAGE Publications, Inc.
Daniels, V. J., Bordage, G., Gierl, M. J., & Yudkowsky, R. (2014). Effect of clinically discriminating, evidence-based checklist items on the reliability of scores from an internal medicine residency OSCE. Advances in Health Sciences Education : Theory and Practice, 19(4), 497-506. https://doi.org/10.1007/s10459-013-9482-4
Erdogan, A., Dong, Y., Chen, X., Schmickl, C., Berrios, R. A. S., Arguello, L. Y. G., Kashyap, R., Kilickaya, O., Pickering, B., Gajic, O., & O’Horo, J. C. (2016). Development and validation of clinical performance assessment in simulated medical emergencies: An observational study. BMC Emergency Medicine, 16, 4. https://doi.org/10.1186/s12873-015-0066-x
Fuller, R., Homer, M., Pell, G., & Hallam, J. (2017). Managing extremes of assessor judgment within the OSCE. Medical Teacher, 39(1), 58-66. https://doi.org/ 10.1080/0142159X.2016.1230189
Gingerich, A., Kogan, J., Yeates, P., Govaerts, M., & Holmboe, E. (2014). Seeing the ‘black box’ differently: Assessor cognition from three research perspectives. Medical Education, 48(11), 1055–1068. https://doi.org /10.1111/medu.12546
Gingerich, A., Regehr, G., & Eva, K. W. (2011). Rater-based assessments as social judgments: Rethinking the etiology of rater errors. Academic Medicine : Journal of the Association of American Medical Colleges, 86(10), S1-S7. https://doi.org/10.1097/ACM.0b013e31822a6cf8
Gingerich, A., Schokking, E., & Yeates, P. (2018). Comparatively salient: Examining the influence of preceding performances on assessors’ focus and interpretations in written assessment comments. Advances in Health Sciences Education: Theory and Practice, 23(5), 937-959. https://doi.org /10.1007/s10459-018-9841-2
Khan, K. Z., Ramachandran, S., Gaunt, K., & Pushkar, P. (2013). The Objective Structured Clinical Examination (OSCE): AMEE Guide No. 81. Part I: An historical and theoretical perspective. Medical Teacher, 35(9), 1437-1446. https://doi.org/ 10.3109/0142159X.2013.818634
Kogan, J. R., Conforti, L., Bernabeo, E., Iobst, W., & Holmboe, E. (2011). Opening the black box of clinical skills assessment via observation: A conceptual model. Medical Education, 45(10), 1048-1060. https://doi.org/10.1111/j.1365-2923.2011.04025.x
Mortsiefer, A., Karger, A., Rotthoff, T., Raski, B., & Pentzek, M. (2017). Examiner characteristics and interrater reliability in a communication OSCE. Patient Education and Counseling, 100(6), 1230-1234. https://doi.org/ 10.1016/j.pec.2017.01.013
Park, S. E., Kim, A., Kristiansen, J., & Karimbux, N. Y. (2015). The Influence of Examiner Type on Dental Students’ OSCE Scores. Journal of Dental Education, 79(1), 89-94.
Pell, G., Fuller, R., Homer, M., & Roberts, T. (2010). How to measure the quality of the OSCE: A review of metrics – AMEE guide no. 49. Medical Teacher, 32(10), 802-811. https://doi.org/ 10.3109/0142159X.2010.507716
Purnajati, O. G. (2020). Does objective structured clinical examination examiners’ backgrounds influence the score agreement? [Data set]. Open Science Framework. https://doi.org/ 10.17605/OSF.IO/RDP65
Rahayu, G. R., Suhoyo, Y., Nurhidayah, R., Hasdianda, M. A., Dewi, S. P., Chaniago, Y., Wikaningrum, R., Hariyanto, T., Wonodirekso, S., & Achmad, T. (2016). Large-scale multi-site OSCEs for national competency examination of medical doctors in Indonesia. Medical Teacher, 38(8), 801-807. https://doi.org /10.3109/0142159X.2015.1078890
Schierenbeck, M. W., & Murphy, J. A. (2018). Interrater reliability and usability of a nurse anesthesia clinical evaluation instrument. Journal of Nursing Education, 57(7), 446-449. https://doi.org/10.3928/01484834-20180618-12
Setyonugroho, W., Kennedy, K. M., & Kropmans, T. J. B. (2015). Reliability and validity of OSCE checklists used to assess the communication skills of undergraduate medical students: A systematic review. Patient Education and Counseling, 98(12), 1482-1491. https://doi.org/ 10.1016/j.pec.2015.06.004
Stalmeijer, R. E., McNaughton, N., & Van Mook, W. N. (2014). Using focus groups in medical education research: AMEE Guide No. 91. Medical Teacher, 36(11), 923-939. https://doi.org/ 10.3109/0142159X.2014.917165
Stoyan, D., Pommerening, A., Hummel, M., & Kopp-Schneider, A. (2017). Multiple-rater kappas for binary data: Models and interpretation. Biometrical Journal, 60(5), 381-394. https://doi.org/ 10.1002/bimj.201600267
Suhoyo, Y., Rahayu, G. R., & Cahyani, N. (2016). A national collaboration to improve OSCE delivery. Medical Education, 50(11), 1150–1151. https://doi.org/ 10.1111/medu.13189
Vanbelle, S. (2019). Asymptotic variability of (multilevel) multirater kappa coefficients. Statistical Methods in Medical Research, 28(10-11), 3012-3026. https://doi.org /10.1177/0962280218794733
Wood, T. J. (2014). Exploring the role of first impressions in rater-based assessments. Advances in Health Sciences Education : Theory and Practice, 19(3), 409-427. https://doi.org/ 10.1007/s10459-013-9453-9
Wood, T. J., Chan, J., Humphrey-Murto, S., Pugh, D., & Touchie, C. (2017). The influence of first impressions on subsequent ratings within an OSCE station. Advances in Health Sciences Education : Theory and Practice, 22(4), 969-983. https://doi.org/10.1007/s10459-016-9736-z
Yeates, P., Moreau, M., & Eva, K. (2015). Are examiners’ judgments in osce-style assessments influenced by contrast effects? Academic Medicine : Journal of the Association of American Medical Colleges, 90(7), 975-980. https://doi.org /10.1097/ACM.0000000000000650
Yeates, P., O’Neill, P., Mann, K., & Eva, K. (2013). Seeing the same thing differently: Mechanisms that contribute to assessor differences in directly-observed performance assessments. Advances in Health Sciences Education : Theory and Practice, 18(3), 325-341. https://doi.org/10.1007/s10459-012-9372-1
*Oscar Gilang Purnajati
Faculty of Medicine,
Universitas Kristen Duta Wacana,
Jl. Dr. Wahidin Sudirohusodo No. 5-25.
Yogyakarta City,
Special Region of Yogyakarta
55224, Indonesia.55224, Indonesia.
Tel: +62-274-563929
Email: oscargilang@staff.ukdw.ac.id
Submitted: 8 July 2020
Accepted: 23 October 2020
Published online: 4 May, TAPS 2021, 6(2), 38-47
https://doi.org/10.29060/TAPS.2021-6-2/OA2338
Enjy Abouzeid1, Rebecca O’Rourke2, Yasser El-Wazir1, Nahla Hassan1, Rabab Abdel Ra’oof1 & Trudie Roberts2
1Faculty of Medicine, Ismailia, Egypt; 2LIME, University of Leeds, United Kingdom
Abstract
Introduction: Although, several factors have been identified as significant determinants in online learning, the human interactions with those factors and their effect on academic achievement are not fully elucidated. This study aims to determine the effect of self-regulated learning (SRL) on achievement in online learning through exploring the relations and interaction of the conception of learning, online discussion, and the e-learning experience.
Methods: A non-probability convenience sample of 128 learners in the Health Professions Education program through online learning filled-out three self-reported questionnaires to assess SRL strategies, the conception of learning, the quality of e-Learning experience and online discussion. A scoring rubric was used to assess the online discussion contributions. A path analysis model was developed to examine the effect of self-regulated learning on achievement in online learning through exploring the relations and interaction among the other factors.
Results: Path analysis showed that SRL has a statistically significant relationship with the quality of e-learning experience, and the conception of learning. On the other hand, there was no correlation with academic achievement and online discussion. However, academic achievement did show a correlation with online discussion.
Conclusion: The study showed a dynamic interaction between the students’ beliefs and the surrounding environment that can significantly and directly affect their behaviour in online learning. Moreover, online discussion is an essential activity in online learning.
Keywords: Online Learning, Conception of Learning, E-learning Experience, Human-Computer Interface, Self-regulated Learning, Path Analysis
Practice Highlights
- The learner who views learning as a constructive process will show better use of self-regulated learning strategies.
- Learners’ beliefs and perceptions can shape the learning experience.
- Online discussion can directly and significantly affect academic achievement in online learning.
- Self-regulated learning is responsible for a small portion of the change in academic achievement.
- Online discussion may affect self-regulated learning negatively.
I. INTRODUCTION
In just a few years, online e-learning has become part of the mainstream in medical education for postgraduates in both developed and developing countries. The use of online e-learning may provide solutions for many educational problems, especially for health professions graduates. It can help them achieving their developmental and educational goals despite the lack of time and overburdened schedules. This raised the need for better understanding of learning in online learning context.
The training that most schools offer to students and instructors on online leaning is mainly limited to using technologies that allow learners to interact with instructors and other learners effectively and flexibly. However, learners in online learning are facing several and complex challenges due to the nature of this context. Online learning is a form of distance learning that represent not only the access to learning experience via the use of technology and internet but also it relies on connectivity, flexibility and ability to promote varied interactions (Hiltz & Turoff, 2005). It characterised by autonomy and relative isolation due to the lack of face-to-face support. One of these important challenges is the need for self-regulated skills. It has been reported that these skills are more important in online learning as compared to traditional one (Azevedo et al., 2008).
Self-regulation is defined as the degree to which students are metacognitively, motivationally, and behaviourally active participants in their learning process (Zimmerman, 1986). This definition focused on students’ proactive use of specific behaviours to improve their academic achievement. In short, the ability to regulate one’s learning process is a critical skill to achieve personal learning objectives in online courses due to the absence of the support and guidance that is typically available in face-to-face learning environments (e.g., an instructor setting deadlines and structuring the learning process). Therefore, online learners need to determine when and how to engage with course content without any other support than the course content and structure, which can pose a challenge for many learners (Lajoie & Azevedo, 2006).
Hence, it seems reasonable to assume that SRL may be a reliable predictor of academic performance. It has been shown that self-regulated learners are more effective learners (Toering et al., 2012), who attain higher grades in medical education (Lucieer et al., 2016). However, the effect of SRL on academic achievement in online learning is still unclear.
Several factors may interact and affect learning in online learning. However, some had received only limited discussion in the medical education literature while others had relatively little empirical testing. Although several research studies have investigated the effect of conception of learning on learners’ approaches, efforts, and motivation, however the effect of conception of learning on self-regulation is still insufficiently explored. Moreover, it can be assumed that students in online learning context may show different conceptions of learning as studies have shown that conception of learning is a context-depended construct that may differ according to the domain of the study or the surrounding context (Chiu et al., 2016; Tsai & Tsai, 2014). Additionally, SRL processes depend on both the learner and the surrounding environment (Bembenutty, 2006). As a result, we assumed that the learners’ perception of the quality of the surrounding learning environment might directly affect their behaviour and outcomes. In other words, the quality and interactivity of the learning environment may shape the learners’ attitude towards the learning experiences and influence the behavioural control of the learner (Zhao, 2016).
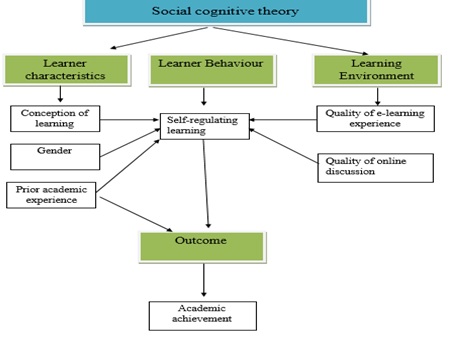
Figure 1: The study conceptual framework
Therefore, a model was hypothesized to explore the interaction between self-regulated learning, the conception of learning, online discussion, and the e-learning experience in an online environment, and how this interaction may affect academic achievement. This cross-sectional study provides an exciting opportunity to advance our knowledge about the learning process in online learning by raising the following questions:
- What is the relationship between SRL and academic achievement in online learning?
- What are the interactions between personal characteristics, beliefs, behaviours, and environment in online learning?
- Does these interactions affect academic achievement in online learning?
II. METHODS
A. Type of the Study and Setting
An observation cross-sectional study was performed at the Faculty of Medicine, Suez Canal University, Egypt. The Medical Education Department offers postgraduate online learning programs in Medical Education to the graduates of Health Professions Education specialties. The program is one of the first online programs in health professions education in the Arab region. It is a two-year program in which students submitted weekly assignments through WordPress / Eleum and receive online feedback on the same Learning Management system (LMS). Also, participate in an online discussion forum through the web-based application Listserv on Google group.
B. Participants and Sampling
‘Out of 231 learners in the online program, a non-probability convenience sample of 128 learners was recruited in the current study; of which, 88 participants had an input in the online discussion’. The subjects were selected from all the program fellows based on their approval to be included in the study sample. The participants were asked to participate in the study through a mass email composed of a detailed description of the nature of the study, the purpose of the study and its relevance to the field of medical education. In all cases, fellows were informed that any information they included in the questionnaires would be treated with confidentiality.
C. Data Collection Tools
Instruments were selected in the current study because it was constructed and used in relevant contexts and the design of the final version of the questionnaires were validated using factor; reliability and test- retest analysis.
1) Measuring learners’ self-regulated learning: The Online Self-Regulated Learning Questionnaire (OSLQ) was used to measure the self-regulated learning behaviours of the fellows (Barnard et al., 2008). The OSLQ consists of six subscale constructs including: environment structuring; goal setting; time management; help seeking; task strategies; and self-evaluation.
2) Measuring learners’ conception of learning: The mental model section of the Inventory of Learning Style (ILS) was used to explore the learners’ conception of learning. The questionnaire was kindly provided by J.D. Vermunt, who originally developed this inventory (Vermunt, 1998). The conception of learning section is composed of 25 items categorised under five scales: construction of knowledge, intake of knowledge, use of knowledge, stimulating education & cooperation of learning.
3) Measuring of the quality of e-learning experience: The e-Learning Experience Questionnaire was used to explore the role of the learning environment (Ginns & Ellis, 2007). The questionnaire consisted of subscales which would reflect students’ perceptions of Good Teaching, Good Resources Clear Goals and Standards, Appropriate Assessment, Generic skills, Appropriate Workload and student interaction.
4)Online discussion: The assessment of the fellows’ input in the online discussion was done by using a scoring rubric that was included in a framework proposed by Nandi et al. (2009). This framework defines several themes on which qualitative online interaction can be designed and assessed. The scoring rubric composed of three broad categories: content, interaction quality and participation.
5) Academic achievement: The fellows’ final grade is the sum of the educational units’ mean which, in turn, is the sum of the unit assignments’ mean was used as an indicator of academic achievement. The academic achievement was categorized into four categories according to the final mean of the units: excellent: means 9-10, very good: means 8, good: means 7 and pass: means 6 and fail means > 6.
III. RESULTS
Data analysis was conducted using Statistical Package for the Social Sciences (SPSS®) version 20 software and International Business Machines SPSS Amos™ version 20. Out of the 231 learners in the Health Professions Education program through distance learning, 128 postgraduate learners were included in the study. The sample composed of 40 males and 88 female learners. Furthermore, they were divided according to their previous academic rank into 2 groups (Dr: 69 & Prof: 59 students). Student t-test revealed that there is no significant difference between male and female in SRL, t (126) = 1.43, conception of learning, t (126) = 0.13, quality of E-learning experience, t (126) = 0.78, online discussion, t (126) = -1.46 and academic achievement, t (126) = -0.79, p<0.05.
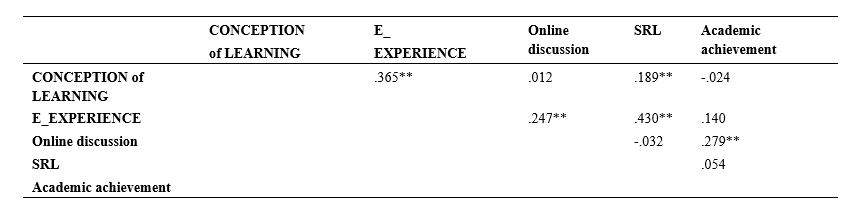
Table 1: Correlation between SRL, quality of e-Learning experience, conception of learning, online discussion and academic achievement using Pearson’s product moment correlation.
Table 1 shows that SRL have a statistically significant relation with Quality of e-Learning experience, conception of learning while there was no correlation with academic achievement and online discussion. However, academic achievement showed correlation with online discussion.
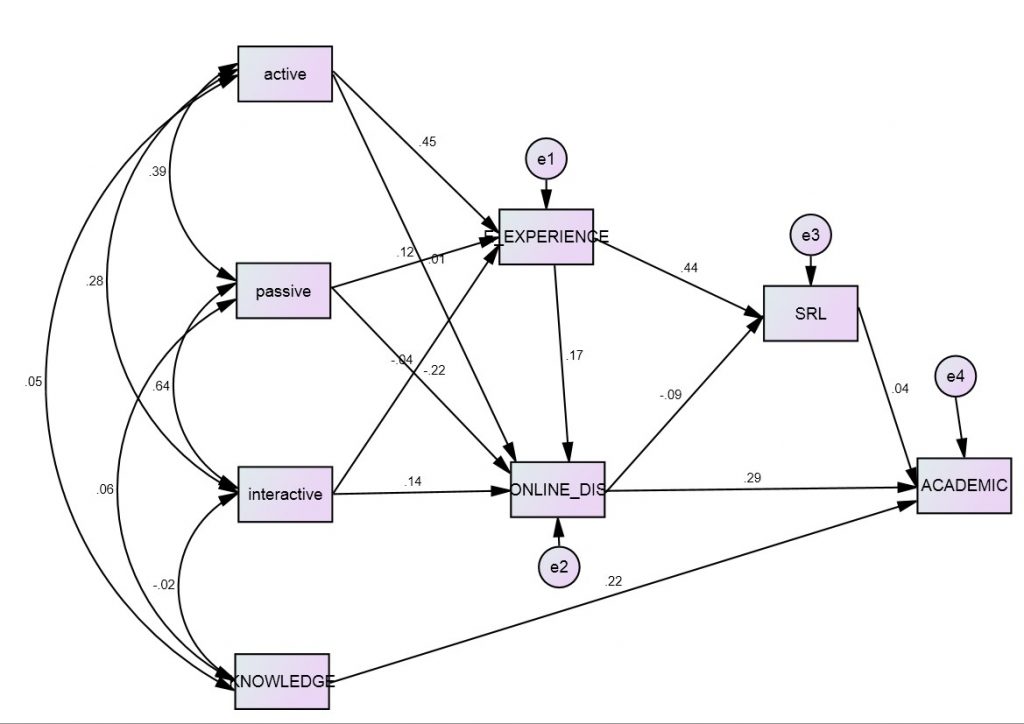
Figure 2: Path analysis for the relationships between SRL, quality of e-Learning experience, conception of learning, online discussion, and academic achievement1.
_______________________
1Active: active conception of learning group (Use of knowledge & Construction of knowledge), Passive: passive conception of learning group ( Intake of knowledge), Interactive: interactive conception of learning group ( Stimulating of learning & Cooperation), Knowledge: Prior academic experience, E-experience: Quality of e-Learning experience, Online_dis: Quality of online discussion, SRL: Self-regulating learning, Academic: Academic achievement and *** : statistical significance difference at the p= 0.05 level
Figure 1 illustrates a summary of the conceptual path model created between the different study variables. The model showed a good fit between a good fit between the tested model and the data (χ2= 5.84, df =10, χ2/df =0.584, The Goodness of Fit Index (CFI =1.00), The Normed Fit Index (NFI =0.96), The Root Mean Square Error of Approximation (RMSEA =0.00). Some path coefficients were statistically significant (p < 0.05) and some paths also demonstrated practical significance (β > 0.3).
Quality of e-experience is directly affected by the active conception of learning (β = 0.45). SRL is affected directly by quality of e-experience (β = 0.44) and indirectly affected by active conception of learning. Finally, the online discussion is negatively affected SRL (β = -0.09). Academic achievement is directly influenced by online discussion (β = 0.29) and prior experience/academic rank (knowledge) (β = 0.22). However, SRL has a small effect on academic achievement (0.04).
IV. DISCUSSION
At this time of transformative change in the use of technology in medical education, it is recommended to study how online learning can be improved in terms of the inter-relationship of conception of learning, self-regulated capacity and learner’s achievement. This study is of high relevance to all medical schools that adopt or plan to incorporate online learning in their curricula. It is noteworthy that many medical schools in the Asia Pacific region are increasingly adopting online learning in their programs as it may solve some medical education challenges in the region (Karunathilake & Samaraskera, 2019).
The results of the path analysis have revealed that conception of learning, quality of e-learning experience and online discussions are significant factors for learning in online context. Despite previous studies having explored the effect of satisfaction and SRL (Liaw & Huang, 2013) however, the link between conceptions of learning, perception of e-learning experience and SRL was discussed in only a very few studies so far (Kassab, et al., 2015; Zhao & Chen ,2016).
The developed model has gained advantage through confirming that as student perceptions of the quality of e-learning experience becomes more positive their self-reported degree of self-regulation in online learning also increases. It can be explained as the students’ positive perception of satisfaction and usefulness from different dimensions of the e-learning experience may help them in applying positive behaviours because they are motivated and enjoying the learning experiences. This supports researchers who have concluded that user satisfaction and self-regulation are highly correlated in e-learning environments (Liaw & Huang, 2013).
Additionally, the findings of this study added that the active conception of learning only are positively and significantly related to quality of learning experience and SRL. This relation should be tracked to the role of conceptions of learning in the students’ learning approach. Students with active conception of learning will adopt deeper approaches that in turn will foster the learner -content interaction. This interaction will affect student motivation and satisfaction (Barger et al., 2016; Tsai P. S., et al., 2011).
These current findings indicate that as students’ active conception of learning become more positive, their self-regulation indirectly improves. This point was tested by the current COVID-19 pandemic that revealed that students can take learning into their own hands. Enforced online learning is showing everyone that students can play a much more proactive role in content discovery and assume more responsibility for their own growth as learners. In other words, when the students’ perception of learning had changed, they own the reins of their learning (Ciotti, 2020). It was also supported by extant research literature. Loyens et al. (2008) found structural positive relations between students’ constructive conceptions of learning on the one hand and their use of deep processing and self-regulation strategies on the other. Moreover, the learning conceptions ‘construction of knowledge’ was negatively related to external regulation and lack of regulation.
However, the findings did not show significant relation between SRL and academic achievement. The current study confirmed that some variation in learners’ performance could be explained by the students’ self-regulated learning skills. Nevertheless, this finding can be explained by the importance of introducing SRL skills explicitly in the learning objectives and syllabus with enough space for the learners to develop and apply SRL skills during the program activities. Self-regulated learning skills need to be taught (Zimmerman, 1989) and learners should be provided with appropriate instructions to guide them to develop and apply SRL skills. It may be expected that senior or postgraduate leaners can develop these skills alone because there is correlation between maturity and SRL skills (Premkumar, et al., 2013; Reio & Davis, 2005). However, studies showed that the use of learning strategies is domain-specific and a learner who is highly self-regulated in one situation may be very much less self-regulated in a new and unfamiliar context (Fisher et al., 2001). Therefore, it seems important that learners need be trained to extend their metacognitive knowledge base and make it more coherent in both under and post graduate learning.
It is interesting to note that there was a statistically significant relation between online discussion and academic achievement. The study program provides an interactive learning environment through the listserv activity. It is an interactive multiple-edged activity that can foster different types of interactions; learner-learner, learner-instructor, and learner- content. These interactions are assumed to affect the learners’ behaviours and achievement positively. Therefore, the social interaction may be crucial element in the formation of online learning communities. As demonstrated by previous studies these interactions will enhances the individual’s regulation of cognition, metacognition, behaviour, and motivation which in turn affects the achievement (Alzahrani, 2017; Delaney et al., 2019).
Given this, it is somewhat surprising that online discussion negatively affects online self-regulation. Students needs to be deeply involved in online discussion so they can plan, monitor, and reflect upon their interactions with other students (Delen & Liew, 2016). But the negative relation between online discussion and SRL shows that students may not be engaged in deep-level interaction with other students for knowledge creation. Instead, many online students participate minimally in discussions only to meet participation requirements (Hew et al., 2010). In the current study, 42% of the participants were evaluated as satisfactory while 1% as excellent. Moreover, 32% of the participants had no input in the discussion.
Additionally, the design of the online forum, especially the proportion of online interactions required for assessment purposes and how the online discussion is evaluated, may also be a factor in the results. The small portion that the evaluation of the online discussion contributes to the final grade in the current study may cause the students not to take online interaction with other students seriously. This point was also reported by Cho & Cho, (2017), who found online discussion is often evaluated by the h number of posts and accounts for 10% of the total grades.
A. Study Limitation
Although the research design of the current study does not lack rigor, these data must be interpreted with caution. With such a relatively small sample size and the sampling techniques, the findings might not to be validated in a larger population. The sample also may affect the interactions in path analysis. Moreover, the tool used to measure the students’ self-regulated learning skills. Some students may have overestimated or down estimated their self-regulated learning skills, which may have influenced the findings.
V. SIGNIFCANCE AND CONCLUSION
This study offers some insight into learning process in online environment; this information can potentially be used as a guide for the future developer of online learning programs to identify the significant factors that may shape their students learning experience and impact the quality of online programs in the region. The study provided evidence which suggests that structure and interaction are critical factors in online learning and that student beliefs and interactivity can play an important role in their achievement and perception of the e-learning experience. Moreover, it confirms the importance of the quality of online discussion in online learning due to the direct and significant relationship with academic achievement.
Notes on Contributors
Enjy Abouzeid reviewed the literature, designed the study, developed the methodological framework of the study, collected the data, analysed the data, and written the manuscript. Rebecca O’Rourke advised on the design of the study and gave critical feedback on manuscript drafts. Yasser El-Wazir advised on the design of the study and gave critical feedback on manuscript drafts. Nahla Hassan gave critical feedback on manuscript drafts. Rabab Abdel Ra’oof advised on the design of the study and gave critical feedback on manuscript drafts. Trudie Roberts advised on the design of the study and gave critical feedback on manuscript drafts. All authors have read and approved the final manuscript.
Ethical Approval
All the students were voluntarily involved in the study and the purpose of the study was clearly communicated to them. An informed consent was administrated to them including the purpose, terms, and conditions. Approval from research Ethics Committee, Faculty of Medicine Suez Canal University No 2455 was taken before starting data collection.
Funding
No funding was raised for this research.
Declaration of Interest
The authors report no conflicts of interest in this work.
References
Alzahrani, M. (2017). The effect of using online discussion forums on students’ learning. Turkish Online Journal of Educational Technology, 16(1), 164-176.
Azevedo, R., Moos, D. C., Greene, J. A., Winters, F. I., & Cromley, J. C. (2008). Why is externally-regulated learning more effective than self-regulated learning with hypermedia? Educational Technology Research and Development, 56(1), 45-72.
Barger, M. M., Wormington, S. V., Huettel, L. G., & Linnenbrink-Garcia, L. (2016). Developmental changes in college engineering students’ personal epistemology profiles. Learning and Individual Differences, 48, 1-8.
Barnard, L., Paton, V. O., & Lan, W. Y. (2008). Online self-regulatory learning behaviours as a mediator in the relationship between online course perceptions with achievement. International Review of Research in Open and Distance Learning, 9(2), 1-11.
Bembenutty, H. (2006). Self-regulation of learning. Academic Exchange Quarterly, 10(4), 221-248.
Chiu, Y. L., Lin, T. J., & Tsai, C. C. (2016). The conceptions of learning science by laboratory among university science-major students: Qualitative and quantitative analyses. Research in Science & Technological Education, 34(3), 359-377.
Cho, M.-H., & Cho, Y.-J. (2017). Self-regulation in three types of online interaction: A scale development. Distance Education, 38(1), 70-83. https://doi.org/10.1080/01587919.2017.1299563
Ciotti. (2020). Covid-19 is transforming how we think about online learning. Retrieved March 30, 2020, from https://enterprise.press/blackboards/covid-19-transforming-think-online-learning/2020
Delaney, D., Kummer, T.‐F., & Singh, K. (2019). Evaluating the impact of online discussion boards on student engagement with group work. British Journal of Educational Technology, 50(2), 902-920. https://doi.org/10.1111/bjet.12614
Delen, E., & Liew, J. (2016). The use of interactive environments to promote self-regulation in online learning: A literature review. European Journal of Contemporary Education, 15(1), 24-33.
Fisher, M., King, J., & Tague, G. (2001). Development of a self-directed learning readiness scale for nursing education. Nurse Education Today, 21(7), 516-525. https://doi.org/10.1054/nedt.2001.0589
Ginns, P., & Ellis, R. (2007). Quality in blended learning: Exploring the relations between on-line and face-to-face teaching and learning. The Internet and Higher Education, 10(1), 53-64.
Hew, K. F., Cheung, W. S., & Ng, C. S. L. (2010). Student contribution in asynchronous online discussion: A review of the research and empirical exploration. Instructional Science. 38(6), 571-606.
Hiltz, S. R., & Turoff, M. (2005). Education goes digital: The evolution of online learning and the revolution in higher education. Communications of the Association for Computing Machinery. 48(10), 59-64.
Karunathilake, I., & Samaraskera, D. (2019). Technology enhanced medical education in the Asia Pacific region-Diversity as advantages. Research Gate. https://www.researchgate.net/publication/337185891_Technology_Enhanced_Medical_Education_in_the_Asia_Pacific_Region-Diversity_as_Advantages
Kassab, S. E., Al-Shafei, A. I., Salem, A. H., & Otoom, S. (2015). Relationships between the quality of blended learning experience, self-regulated learning, and academic achievement of medical students: A path analysis. Advances in Medical Education and Practice, 6, 27-34. https://doi.org/10.2147/AMEP.S75830
Lajoie, S. P., & Azevedo, R. (2006). Teaching and learning in technology-rich environments. In P. A. Alexander & P. H. Winne (Eds.), Handbook of Educational Psychology (pp. 803-821). Routledge.
Liaw, S. S., & Huang, H. M. (2013). Perceived satisfaction, perceived usefulness and interactive learning environments as predictors to self-regulation in e-Learning environments. Computer & Education, 60, 14-24.
Loyens, S. M. M., Rikers, R. M. J. P., & Schmidt, H. G. (2008). Relationships between students’ conceptions of constructivist learning and their regulation and processing strategies. Instructional Science, 36(5), 445-462.
Lucieer, S. M., Jonker, L., Visscher, C. H., Rikers, R. M. J. P., & Themmen, A. P. N. (2016). Self-regulated learning and academic performance in medical education. Medical Teacher, 38(6), 585-593.
Nandi, D., Chang, S. & Balbo, S. (2009). A conceptual framework for assessing interaction quality in online discussion forums. In Same places, different spaces. Proceedings of the 26th ASCILITE conference. Australian Society for Computers in Learning in Tertiary Education.
Premkumar, K., Pahwa, P., Banerjee, A., Baptiste, K., Bhatt, H., & Lim, H. J. (2013). Does medical training promote or deter self-directed learning? A longitudinal mixed-methods study. Academic Medicine, 88(11), 1754-1764.
Reio, T., & Davis, W. (2005). Age and gender differences in self-directed learning readiness: A developmental perspective. International Journal Self-directed Learning, 2, 40-49.
Toering, T., Elferink-Gemser, M. T., Jonker, L., Heuvelen, M. J. G., & Visscher, C. (2012). Measuring self-regulation in a learning context: Reliability and validity of the self-Regulation of learning self-report scale (SRL-SRS). International Journal of Sport and Exercise Psychology, 10(1), 24-38.
Tsai, P. S., Tsai, C.-C., & Hwang, G. H. (2011). College Students’ conceptions of context-aware ubiquitous learning: A phenomenographic analysis. The Internet and Higher Education, 14, 137-141.
Tsai, P.-S., & Tsai, C.-C. (2014). College students’ skills of online argumentation: The role of scaffolding and their conceptions. Internet and Higher Education. 21, 1–8.
Vermunt, J. D. (1998). The regulation of constructive learning processes. British Journal of Educational Psychology, 68, 149-171.
Zhao, H. (2016). Factors influencing self-regulation in E-learning 2.0: Confirmatory factor model. Canadian Journal of Learning and Technology, 42(2).
Zhao, H., & Chen, L. (2016). How can self-regulated learning be supported in e-learning 2.0 environment: A comparative study. Journal of Educational Technology Development and Exchange, 9(2), 1-28.
Zimmerman, B. J. (1986). Development of self-regulated learning: Which are the key subprocesses? Contemporary Educational Psychology, 16, 307-313.
Zimmerman, B. J. (1989). Models of self-regulated learning and academic achievement. In B. J. Zimmerman & D. H. Schunk (Eds.), Self-regulated learning and academic achievement: Theory, research, and practice (pp. 1-25). Springer.
*Enjy Abouzeid
6A Hassan El Bassry Street,
Ismailia, Egypt
Email: Enjyabouzeid@yahoo.com
Submitted: 24 June 2020
Accepted: 8 September 2020
Published online: 4 May, TAPS 2021, 6(2), 31-37
https://doi.org/10.29060/TAPS.2021-6-2/OA2328
Julie Yun Chen1,2, Weng-Yee Chin1, Agnes Tiwari3, Janet Wong3, Ian C K Wong4, Alan Worsley4, Yibin Feng5, Mai Har Sham6, Joyce Pui Yan Tsang1,2 & Chak Sing Lau7
1Department of Family Medicine and Primary Care, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; 2Bau Institute of Medical and Health Sciences Education, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; 3School of Nursing, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; 4Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; 5School of Chinese Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; 6School of Biomedical Sciences, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; 7Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong, Hong Kong
Abstract
Introduction: The demanding nature of medical and health sciences studies can cause stress among students in these disciplines affecting their wellbeing and academic performance. The Perceived Stress Scale (PSS-10) is a widely used measure of perceived stress among medical students and healthcare professionals that has not yet been validated among medical and health sciences students in Hong Kong. The aim of this study is to establish the construct validity and reliability of the PSS-10 in this context.
Methods: 267 final year medical and health sciences students were surveyed using the PSS-10. The data were analysed using exploratory factor analysis for construct validity and Cronbach’s alpha coefficient and corrected item-total correlations for reliability.
Results: Exploratory factor analysis revealed a two-factor structure for PSS-10, with Cronbach’s alpha of 0.865 and 0.796, indicating good internal consistency. Corrected item-total correlations showed satisfactory correlation ranged from 0.539 to 0.748 for all items and their respective subscale. Both tests supported PSS-10 as a two-factor scale.
Conclusion: The PSS-10 is a valid measure for assessing perceived stress in Hong Kong medical and health sciences students.
Keywords: Undergraduate Students, Medicine, Nursing, Pharmacy, Health Sciences, Validation, Perceived Stress
Practice Highlights
- It is important to have a valid instrument for early detection of stress in health science students.
- Perceived Stress Scale (PSS-10) has a two-factor structure, a finding that is consistent with most other studies.
- PSS-10 has satisfactory internal consistency and reliability.
- PSS-10 can be used to assess the level of stress in medical and health sciences students.
I. INTRODUCTION
Undertaking studies in healthcare disciplines can be stressful as the programmes are demanding and students are often competing with higher achieving peers from admission to graduation. Significant stress can lead to psychological distress that has negative implications on current and future performance. Medical students have a higher prevalence of distress and poorer mental quality of life than their non-medical peers (Dyrbye et al., 2006; Shin et al., 2016), and also experience sleep deprivation, anxiety, and feelings of social isolation as revealed in focus group interviews conducted by Henning et al. (2010). There may also be a negative impact in quality of patient care (Firth-Cozens, 2001) and higher rate of medical errors (West et al., 2009). High perceived stress level correlated to impaired clinical performances in nursing students, including application of knowledge, clinical skills and communication (Ye et al., 2018). High level of stress and impaired quality of life were also found in third year pharmacy students in the United States (Marshall et al., 2008). In a study on pre-medical and health sciences students, higher perceived stress was a predictor of poor academic achievement (Henning et al., 2018).
As in many Asian cultures, Hong Kong students in general are under pressure to perform well in school as education is viewed as a crucial stepping-stone to success (S. Chan, 1999; Tan & Yates, 2011). This pressure may be particularly pronounced in medical students who manifest a greater degree of psychological distress, including perceived stress, depressive symptoms and anxiety, than other university students (Wong et al., 2005). A survey on medical students from the University of Hong Kong also revealed that majority of medical students were screened positive for minor psychiatric disorders and up to 95% of them were burned out (Chau et al., 2019). Many students may be “pushed” into a career path by extrinsic factors such as parental expectation (Sreeramareddy et al., 2007) or as a part of family tradition. Asian medical students may also tend to focus on academic achievement and seek to outperform their peers (Henning et al., 2011). Given the risk for developing high level of stress for these students, and the particularly intense environment in Hong Kong, it is important to have a valid instrument for early detection of stress so that appropriate strategies may be instituted at an early stage.
The Perceived Stress Scale (PSS-10) (Cohen, 1988) is widely used to measure perceived stress among healthcare students and doctors in different countries (Jones et al., 2015; Wongpakaran & Wongpakaran, 2010), and healthcare workers in Hong Kong (Chua et al., 2004). Healthcare students and healthcare workers may respond differently to a stressful event, as shown in the studies by Chua et al. (2004) and Wong et al. (2004), where the psychological effects of the SARS outbreak were different for healthcare students and workers. PSS-10 has been translated and validated in various languages, including Spanish, Turkish, Portuguese, Chinese, Thai and Japanese, among different populations such as patients, students, pregnant women, and adults in the general population (Lee, 2012). These validation studies are fundamentally robust, yet validating the PSS-10 is important in the specific undergraduate medical and health professions educational context in Hong Kong. Our study population is subject to different cultural, societal and educational influences that affect the perception of stress and the understanding of the items in the instrument so validation studies done elsewhere may not be applicable to our local context. The aim of this study is therefore, to establish the construct validity and reliability of the PSS-10 for use in this population.
II. METHODS
A. Participants and Data Collection
All final year students undertaking studies in Li Ka Shing Faculty of Medicine in the University of Hong Kong (HKUMed) in the academic year of 2014-2015 were the target population of this study. A research assistant, who was not involved in teaching and assessment of the students, invited the students to participate in the study during a designated compulsory face-to-face teaching session for each programme. Those who provided written consent completed a written questionnaire in January – February 2015 or June 2015. The specific time for each cohort was chosen to avoid known stressful periods such as exams. The questionnaire included the PSS-10 and demographic information.
B. Measure
The Perceived Stress Scale (PSS-10) (Cohen, 1988) was chosen as the instrument for measuring perceived stress. We considered other often-used instruments including the Depression Anxiety Stress Scale (DASS) (Lovibond & Lovibond, 1995) that measures depression and anxiety, in addition to stress and the General Health Questionnaire (GHQ) (Goldberg & Hillier, 1979) that measures medical complaints as a reflection of emotional stress, but these looked at broader conceptualisations of psychological distress beyond the scope of our study. PSS-10 was the most fit-for-purpose in measuring stress in terms of respondents’ views about their lives. In addition, we wished to be able to compare the stress in medical and health professions students to other key local comparator populations (e.g. university students, doctors, general population etc) and using the same instrument would facilitate this comparison.
PSS-10 is a 10-item instrument that assesses the extent of stress of respondents. PSS-10 is the abbreviated version of the original instrument with 14 items (PSS-14). A brief version with four items (PSS-4) is also available. Among the three versions of PSS, PSS-10 was found to be superior in psychometric properties, in terms of validity and reliability, than the other two versions (Lee, 2012). In the PSS-10, respondents rate statements about how unpredictable, uncontrollable, and overloaded they find their lives on a 5-point Likert scale from “never” to “very often”. Each response is converted to a score of 0 to 4 with the overall PSS score computed as the total score of the 10 items, with four reverse-coded items. The higher the score, the worse the perceived stress, with a maximum score of 40. There is no specific cut-off score that corresponds to high or low stress. We used the original English version of PSS-10 because as an English-medium university, students at HKUMed are taught in English (except during bedside teaching and clinical practicums) and students are proficient in English.
C. Data Analysis
To establish the construct validity of the PSS-10, exploratory factor analysis (EFA) was performed on the responses to PSS-10 items by final year medical students, using principal component extraction with varimax rotation and the criterion of eigenvalue greater than 1.00. The Kaiser-Meyer-Olkin (KMO) measure equal to or greater than 0.5 was used to indicate sampling adequacy, while the Barlett’s Test of Sphericity with p<0.001 was used to ensure the appropriateness of the data set for EFA. Cumulative variance explained in the factor structure identified by EFA model was reported.
Cronbach’s alpha coefficient and corrected item-total correlations were used to examine reliability. Cronbach’s alpha coefficient was calculated to assess the internal consistency of each scale, which was considered acceptable if greater than 0.7 (Nunnally, 1994). Corrected item-total correlations were evaluated by Pearson’s correlation coefficient. A correlation of more than 0.4 was considered satisfactory (Wolfinbarger & Gilly, 2003).
III. RESULTS
A total of 267 students completed the survey, with an overall response rate of 86.5%. 104 (39%) of the respondents were male (Table 1). Female students had significantly higher perceived stress than male students (20.84 vs 18.59; p<0.001). Table 2 shows the descriptive statistics for PSS-10 items and total score by programme of study.
|
|
All (n=267) |
Average PSS-10 |
|
Age (mean) |
22.71 |
19.95 |
|
Gender |
||
|
Male |
104 |
18.59 |
|
Female |
160 |
20.84 |
|
Programme of study |
||
|
MBBS |
120 |
18.17 |
|
BNurs |
94 |
21.20 |
|
BChinMed |
13 |
21.77 |
|
BPharm |
28 |
22.39 |
|
BBMS |
10 |
20.20 |
|
MBBS: Bachelor of Medicine and Bachelor of Surgery; BNurs: Bachelor of Nursing; BChinMed: Bachelor of Chinese Medicine; BPharm: Bachelor of Pharmacy; BBMS: Bachelor of Biomedical Sciences *Numbers may not add up to the total number of respondents due to missing data |
||
Table 1. Demographic of respondents and average PSS-10 score
|
|
|
All (n=265) |
MBBS (n=120) |
BNurs (n=94) |
BChinMed (n=13) |
BPharm (n=28) |
BBMS (n=10) |
|
In the last month, how often have you… |
|||||||
|
1. |
been upset because of something that happened unexpectedly |
2.10 |
1.83 |
2.27 |
2.62 |
2.39 |
2.30 |
|
2. |
felt that you were unable to control the important things in your life |
2.05 |
1.79 |
2.19 |
2.31 |
2.46 |
2.40 |
|
3. |
felt nervous and “stressed” |
2.19 |
1.87 |
2.39 |
2.31 |
2.64 |
2.60 |
|
4. |
felt confident about your ability to handle your personal problems |
2.19 |
2.25 |
2.21 |
2.00 |
1.93 |
2.20 |
|
5. |
felt that things were going your way |
2.11 |
2.21 |
2.07 |
2.00 |
1.93 |
1.90 |
|
6. |
found that you could not cope with all the things that you had to do |
1.97 |
1.77 |
2.07 |
2.23 |
2.39 |
2.00 |
|
7. |
been able to control irritations in your life |
2.19 |
2.25 |
2.12 |
2.15 |
2.14 |
2.40 |
|
8. |
felt that you were on top of things |
1.79 |
2.00 |
1.66 |
1.46 |
1.46 |
1.90 |
|
9. |
been angered because of things that were outside of your control |
1.94 |
1.81 |
2.19 |
1.85 |
1.82 |
1.60 |
|
10. |
felt difficulties were piling up so high that you could not overcome them |
1.96 |
1.77 |
2.15 |
2.08 |
2.14 |
1.70 |
|
|
Total* |
19.93 |
18.17 |
21.20 |
21.77 |
22.39 |
20.20 |
|
MBBS: Bachelor of Medicine and Bachelor of Surgery; BNurs: Bachelor of Nursing; BChinMed: Bachelor of Chinese Medicine; BPharm: Bachelor of Pharmacy; BBMS: Bachelor of Biomedical Sciences *Total score is calculated by the sum of the 10 PSS items, with item 4, 5, 7 and 8 reverse coded. |
|||||||
Table 2. Mean score for PSS-10 items by programme of study
A. Exploratory Factor Analysis on PSS-10
Using the final year medical and health sciences student data for EFA (Table 3), the KMO measure for PSS-10 was 0.823, indicating sampling adequacy. The scale had a p-value of <0.001 for the Bartlett’s Test of Sphericity, confirming variability in the data was sufficient. The factor loadings of varimax rotated solution and the eigenvalue of the two factors identified (Perceived Helplessness and Perceived Control) are shown in Table 3. The cumulative variances explained were 61.386%.
B. Reliability
Cronbach’s alpha for the two factors were 0.865 and 0.796 respectively, which indicates good internal consistency reliability (Table 4). To determine the robustness of the analysis, each item was deleted in turn from the calculation and the resulting Cronbach’s alpha remained high (0.724-0.859). Corrected item-total correlations showed satisfactory correlation for all items and their respective subscale (range from 0.539 to 0.748) (Table 4). Items with the highest corrected item-total correlation were item 2 (“felt that you were unable to control the important things in your life”), item 3 (“felt nervous and ‘stressed’”), and item 10 (felt difficulties were piling up so high that you could not overcome them). Both tests supported the PSS-10 as a two-factor scale.
|
|
Factor loading |
|
||||
|
Perceived helplessness |
Perceived control |
|
||||
|
In the last month, how often have you… |
|
|||||
|
2. |
felt that you were unable to control the important things in your life |
0.826 |
-0.168 |
|
||
|
1. |
been upset because of something that happened unexpectedly |
0.793 |
0.021 |
|
||
|
3. |
felt nervous and “stressed” |
0.793 |
-0.167 |
|
||
|
10. |
felt difficulties were piling up so high that you could not overcome them |
0.782 |
-0.154 |
|
||
|
9. |
been angered because of things that were outside of your control |
0.712 |
0.099 |
|
||
|
6. |
found that you could not cope with all the things that you had to do |
0.698 |
-0.132 |
|
||
|
4. |
felt confident about your ability to handle your personal problems |
-0.017 |
0.815 |
|
||
|
5. |
felt that things were going your way |
-0.102 |
0.811 |
|
||
|
7. |
been able to control irritations in your life |
-0.100 |
0.774 |
|
||
|
8. |
felt that you were on top of things |
-0.086 |
0.732 |
|
||
|
Eigenvalue |
3.879 |
2.260 |
|
|||
|
% of variance |
38.791 |
22.595 |
|
|||
|
|
Cumulative % of variance |
61.386 |
|
|||
Table 3. Factor loadings by exploratory factor analysis for PSS-10
|
|
|
Corrected Item-Total Correlation |
Cronbach’s Alpha if Item Deleted |
|
|
In the last month, how often have you… |
|
|||
|
Perceived helplessness (Cronbach’s Alpha = 0.865 ) |
|
|||
|
1. |
been upset because of something that happened unexpectedly |
0.674 |
0.840 |
|
|
2. |
felt that you were unable to control the important things in your life |
0.748 |
0.826 |
|
|
3. |
felt nervous and “stressed” |
0.705 |
0.835 |
|
|
6. |
found that you could not cope with all the things that you had to do |
0.591 |
0.854 |
|
|
9. |
been angered because of things that were outside of your control |
0.562 |
0.859 |
|
|
10. |
felt difficulties were piling up so high that you could not overcome them |
0.688 |
0.838 |
|
|
Perceived control (Cronbach’s Alpha = 0.796) |
|
|||
|
4. |
felt confident about your ability to handle your personal problems |
0.635 |
0.732 |
|
|
5. |
felt that things were going your way |
0.652 |
0.724 |
|
|
7. |
been able to control irritations in your life |
0.609 |
0.745 |
|
|
8. |
felt that you were on top of things |
0.539 |
0.781 |
|
|
Cut-offs for item-total correlation: <0.4 indicates poor correlation between item and total score. |
|
|||
Table 4. Corrected Item-Total Correlation
IV. DISCUSSION
A. Exploratory Factor Analysis
Exploratory factor analysis for PSS-10 revealed a two-factor structure, which was consistent with the findings in the original study (Cohen, 1988) and other validation studies (Andreou et al., 2011; Chaaya et al., 2010; Lesage et al., 2012; Leung et al., 2010; Örücü & Demir, 2009; Siqueira et al., 2010; Wongpakaran & Wongpakaran, 2010). The two factors identified in our study were related to the concept of control and ability to cope, as reflected in the positively-worded items, and the concept of helplessness, as reflected in negative items, respectively. The three items that loaded most heavily on the helplessness factor related to a lack of control (item 2), anxiety (item 3) and feeling overwhelmed (item 10).
B. Locus of Control
It was evident that feeling unable to control important things in life (Item 2) greatly contributed to perceived stress of students. (Table 4) External locus of control, where people believe external factors control success or failure, is associated with higher stress (Linn & Zeppa, 1984) and understandable for healthcare students. For example, the teaching timetable is often changed at the last minute as the teachers might have urgent clinical duties or they may be expected to do more self-directed learning in which the breadth or depth of the learning may not be made clear. The expectations for clinical skills in clinical settings are often different from what was taught in school (Gibbons et al., 2008). The uncertainty of the curriculum, progress and assessment also contribute to stress in healthcare students (Elzubeir et al., 2010). Moreover, as the most junior member of the healthcare team, students have no decision-making capacity and may feel helpless when confronted with situations beyond their expertise or observe actions contrary to their personal views (Jennings, 2009).
C. Anxiety
Feeling nervous (item 3) was another contributing factor for perceived stress (Table 4). Medical and health sciences students are required to sit high-stakes examinations in order to be promoted to the next year of study or to graduate, where test anxiety is understandably prevalent (Encandela et al., 2014). Clinical competency exams such as OSCEs are particularly anxiety-provoking (Muldoon et al., 2014). This is especially relevant to the final year students in this study, as the final summative exams in all programmes are intense. In particular, the written final Bachelor of Medicine and Bachelor of Surgery (MBBS) exam covers material from the whole year and all disciplines including medicine, surgery, psychiatry, obstetrics and gynaecology, paediatrics, orthopaedics, and family medicine, and also includes a clinical competency test in each discipline. This final exam constitutes the licensing exam to become a doctor in Hong Kong.
In addition, the vast majority of students admitted to undergraduate healthcare professions studies in Hong Kong are secondary school graduates. The age-related level of maturity may affect their ability to cope with a strenuous, content-rich curriculum as well as the pressures of clinical practicums and clerkships. Students have raised concerns about exam-induced anxiety and the heavy academic workload and in fact, the most common reason for students to seek counselling support at our institution is because of academic-related stress or psychological distress.
Working in the clinical environment also produces anxiety, especially when starting a new rotation in a new discipline when students often lack clinical experience, are unfamiliar with the ward, encounter difficult patients, and have a fear of making mistakes (Sharif & Masoumi, 2005). The hierarchical medical culture is more pronounced in healthcare settings and can be intimidating for undergraduate healthcare professions students who are seen as the lowest rung on the ladder. Other situations where the students are singled-out, such as during simulations, being observed, evaluated or video-recorded, also increases anxiety (Nielsen & Harder, 2013) especially as these teaching sessions are done in small groups. The style of learning for our students in these clinical years also require a more proactive, interactive and self-reliant style of learning. In addition to scheduled bedside teaching with a clinician, students have to seek out patients to clerk in order to hone their clinical skills and gain clinical experience. This may be an adjustment to students used to a more traditional classroom style and textbook learning.
D. Overwhelmed
The third most important item contributing to high perceived stress was the feeling of being overwhelmed with the workload and difficulties (item 10) (Table 4). Healthcare studies are well-known for being content heavy. Students have a heavy workload including long hours of lectures, tutorials, laboratories and clinical attachments, and are also expected to spend substantial time on independent study. Because most healthcare professions students in Hong Kong are admitted to such programmes directly upon completion of secondary education, higher diploma or associate degree, the curricula are even more packed with basic foundational as well as profession-specific advanced content.
Students in their final year of study have to contend with clinical experiential learning but must also further develop their knowledge base. This entails acquiring a huge volume of factual content as well as applying concepts to clinical scenarios. Students must work more independently in clinical attachments and may have some responsibility for patient care or administrative work. For example, nursing students’ progress from having practicums in small groups to shadowing a practising nurse, and working as a member of the nursing team in the ward in their senior years.
In addition, clinical teaching settings in Hong Kong, can be challenging learning environments especially the tertiary care teaching hospitals where much of the training takes place. The business of routine patient care already involving a multitude of staff makes it a daunting place for healthcare professions students who have to compete with each other for the opportunity to clerk patients.
In the clinical environment, students also come face-to-face with difficult situations and experience feelings that they may have difficulty resolving. This may include having problems communicating communication with patients or their families, struggling with ethical dilemmas such as witnessing a medical error, or experiencing the illness experience of patients and the helplessness of not being able alleviate their suffering. Medical students can be overwhelmed by the burden of suppressing their own natural emotions when facing the pain and suffering of their patients (Jennings, 2009). Likewise, nursing students also expressed that workload from clinical work and their own studies exceeded their physical and emotional capacity (C. K. Chan et al., 2009).
E. Limitations
At the time of data collection, no data were collected for other scales of similar or opposite construct. Hence no convergent or divergent validity could be calculated. Also, test-retest reliability could not be done as this was a one-off cross-sectional survey. Despite these limitations our data supported a two-factor structure of the PSS-10, consistent with the original and other previous studies.
V. CONCLUSION
Demonstrating good construct validity and internal consistency, PSS-10 is a valid measure for assessing self-reported stress in medical students as well as in health sciences students. Longitudinal studies on student stress using this measure will help to assess the extent and patterns of stress in a high-risk population in order to develop timely interventions.
Notes on Contributors
JY Chen and JPY Tsang reviewed the literature, designed the study, performed data collection and data analysis, and developed the manuscript. WY Chin, A Tiwari, J Wong, ICK Wong, A Worsley, Y Feng, MH Sham and CS Lau advised on the study design, facilitated data collection and gave critical feedback on the manuscript. All authors have read and approved the final manuscript.
Ethical Approval
Ethical approval of this study was granted by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (Reference No.: UW 14-472). All participants have given written consent for their data to be used in the research and for publication.
Acknowledgements
We would like to thank the students of HKUMed for participating in the study, and the administrative staff of Li Ka Shing Faculty of Medicine, School of Nursing, School of Chinese Medicine, Department of Pharmacology and Pharmacy, and School of Biomedical Sciences for helping with the logistical arrangement of the questionnaire administrations.
Funding
This work was supported by a Teaching Development Grant funded by the University of Hong Kong.
Declaration of Interest
The authors declare that there is no conflict of interest.
References
Andreou, E., Alexopoulos, E. C., Lionis, C., Varvogli, L., Gnardellis, C., Chrousos, G. P., & Darviri, C. (2011). Perceived stress scale: Reliability and validity study in Greece. International Journal of Environmental Research and Public Health, 8(8), 3287-3298.
Chaaya, M., Osman, H., Naassan, G., & Mahfoud, Z. (2010). Validation of the Arabic version of the Cohen Perceived Stress Scale (PSS-10) among pregnant and postpartum women. BMC Psychiatry, 10(1), 111.
Chan, C. K., So, W. K., & Fong, D. Y. (2009). Hong Kong baccalaureate nursing students’ stress and their coping strategies in clinical practice. Journal of Professional Nursing, 25(5), 307-313.
Chan, S. (1999). The Chinese learner–A question of style. Education & Training, 41(6/7), 294-305.
Chau, S. W., Lewis, T., Ng, R., Chen, J. Y., Farrell, S. M., Molodynski, A., & Bhugra, D. (2019). Wellbeing and mental health amongst medical students from Hong Kong. International Review of Psychiatry, 31(7-8), 626-629.
Chua, S. E., Cheung, V., Cheung, C., McAlonan, G. M., Wong, J. W., Cheung, E. P., Chan, M. T., Wong, M. M., Tang, S. W., Choy, K. M., Wong, M. K., Chu, C. M., & Tsang, K. W. (2004). Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. The Canadian Journal of Psychiatry, 49(6), 391-393. https://doi.org/10.1177/070674370404900609
Cohen, S. (1988). Perceived stress in a probability sample of the United States. In S. Spacapan & S. Oskamp (Eds.), The social psychology of health. The Claremont Symposium on applied social psychology (pp. 31-67). Sage.
Dyrbye, L. N., Thomas, M. R., Huntington, J. L., Lawson, K. L., Novotny, P. J., Sloan, J. A., & Shanafelt, T. D. (2006). Personal life events and medical student burnout: A multicenter study. Academic Medicine, 81(4), 374-384. https://doi.org/10.1097/00001888-200604000-00010
Elzubeir, M., Elzubeir, K., & Magzoub, M. (2010). Stress and coping strategies among Arab medical students: Towards a research agenda. Education for Health, 23(1), 355.
Encandela, J., Gibson, C., Angoff, N., Leydon, G., & Green, M. (2014). Characteristics of test anxiety among medical students and congruence of strategies to address it. Medical Education Online, 19(1), 25211.
Firth-Cozens, J. (2001). Interventions to improve physicians’ well-being and patient care. Social Science & Medicine, 52(2), 215-222.
Gibbons, C., Dempster, M., & Moutray, M. (2008). Stress and eustress in nursing students. Journal of Advanced Nursing, 61(3), 282-290.
Goldberg, D. P., & Hillier, V. F. (1979). A scaled version of the General Health Questionnaire. Psychological Medicine, 9(1), 139-145.
Henning, M. A., Hawken, S. J., Krageloh, C., Zhao, Y. P., & Doherty, I. (2011). Asian medical students: Quality of life and motivation to learn. Asia Pacific Education Review, 12(3), 437-445.
Henning, M. A., Krageloh, C., Hawken, S., Zhao, Y., & Doherty, I. (2010). Quality of life and motivation to learn: A study of medical students. Issues in Educational Research, 20(3), 244-256.
Henning, M. A., Krägeloh, C. U., Booth, R., Hill, E. M., Chen, J., & Webster, C. (2018). An exploratory study of the relationships among physical health, competitiveness, stress, motivation, and grade attainment: Pre-medical and health science students. The Asia Pacific Scholar, 3(3), 5-16.
Jennings, M. (2009). Medical student burnout: Interdisciplinary exploration and analysis. Journal of Medical Humanities, 30(4), 253.
Jones, G., Hocine, M., Salomon, J., Dab, W., & Temime, L. (2015). Demographic and occupational predictors of stress and fatigue in French intensive-care registered nurses and nurses’ aides: A cross-sectional study. International Journal of Nursing Studies, 52(1), 250-259.
Lee, E.-H. (2012). Review of the psychometric evidence of the perceived stress scale. Asian Nursing Research, 6(4), 121-127.
Lesage, F.-X., Berjot, S., & Deschamps, F. (2012). Psychometric properties of the French versions of the Perceived Stress Scale. International Journal of Occupational Medicine and Environmental Health, 25(2), 178-184.
Leung, D. Y., Lam, T.-h., & Chan, S. S. (2010). Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health, 10(1), 513.
Linn, B. S., & Zeppa, R. (1984). Stress in junior medical students: Relationship to personality and performance. Journal of Medical Education. 59(1), 7-12.
Lovibond, S. H., & Lovibond, P. F. (1995). Manual for the Depression Anxiety Stress Scales. (2nd. Ed.) Psychology Foundation.
Marshall, L. L., Allison, A., Nykamp, D., & Lanke, S. (2008). Perceived stress and quality of life among doctor of pharmacy students. American Journal of Pharmaceutical Education, 72(6), 137. https://doi.org/10.5688/aj7206137
Muldoon, K., Biesty, L., & Smith, V. (2014). ‘I found the OSCE very stressful’: Student midwives’ attitudes towards an objective structured clinical examination (OSCE). Nurse Education Today, 34(3), 468-473.
Nielsen, B., & Harder, N. (2013). Causes of student anxiety during simulation: What the literature says. Clinical Simulation in Nursing, 9(11), e507-e512.
Nunnally, J. C. (Ed.) (1994). Psychometric Theory (3rd ed.). McGraw Hill.
Örücü, M. Ç., & Demir, A. (2009). Psychometric evaluation of perceived stress scale for Turkish university students. Stress and Health, 25(1), 103-109.
Sharif, F., & Masoumi, S. (2005). A qualitative study of nursing student experiences of clinical practice. BMC Nursing, 4(1), 6.
Shin, H. K., Kang, S. H., Lim, S.-H., Yang, J. H., & Chae, S. (2016). Development of a Modified Korean East Asian Student Stress Inventory by Comparing Stress Levels in Medical Students with Those in Non-Medical Students. Korean Journal of Family Medicine, 37(1), 14-17.
Siqueira, R. R., Ferreira Hino Adriano, A., & Romélio Rodriguez Añez, C. (2010). Perceived stress scale: Reliability and validity study in Brazil. Journal of Health Psychology, 15(1), 107-114.
Sreeramareddy, C. T., Shankar, P. R., Binu, V., Mukhopadhyay, C., Ray, B., & Menezes, R. G. (2007). Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Medical Education, 7(1), 26.
Tan, J. B., & Yates, S. (2011). Academic expectations as sources of stress in Asian students. Social Psychology of Education, 14(3), 389-407.
West, C. P., Tan, A. D., Habermann, T. M., Sloan, J. A., & Shanafelt, T. D. (2009). Association of resident fatigue and distress with perceived medical errors. The Journal of the American Medical Association, 302(12), 1294-1300.
Wolfinbarger, M., & Gilly, M. C. (2003). eTailQ: Dimensionalizing, measuring and predicting etail quality. Journal of Retailing, 79(3), 183-198.
Wong, J. G. W. S., Cheung, E. P., Cheung, V., Cheung, C., Chan, M. T., Chua, S. E., McAlonan, G. M., Tsang, K. W. T., & Ip, M. S. (2004). Psychological responses to the SARS outbreak in healthcare students in Hong Kong. Medical Teacher, 26(7), 657-659.
Wong, J. G. W. S., Patil, N. G., Beh, S. L., Cheung, E. P., Wong, V., Chan, L. C., & Lieh Mak, F. (2005). Cultivating psychological well-being in Hong Kong’s future doctors. Medical Teacher, 27(8), 715-719.
Wongpakaran, N., & Wongpakaran, T. (2010). The Thai version of the PSS-10: An Investigation of its psychometric properties. BioPsychoSocial Medicine, 4(1), 6.
Ye, Y., Hu, R., Ni, Z., Jiang, N., & Jiang, X. (2018). Effects of perceived stress and professional values on clinical performance in practice nursing students: A structural equation modeling approach. Nurse Education Today, 71, 157-162.
*Julie Chen
Department of Family Medicine &
Bau Institute of Medical and Health Sciences Education,
Li Ka Shing Faculty of Medicine,
University of Hong Kong
21 Sassoon Rd, Pok Fu Lam
Hong Kong
Email: juliechen@hku.hk
Submitted: 19 June 2020
Accepted: 21 October 2020
Published online: 4 May, TAPS 2021, 6(2), 25-30
https://doi.org/10.29060/TAPS.2021-6-2/OA2327
Nicola Ngiam1,2 & Chuen-Yee Hor1
1Centre for Healthcare Simulation, National University of Singapore, Singapore; 2Khoo Teck Puat-National University Children’s Medical Institute, National University Hospital, Singapore
Abstract
Introduction: Standardised patients (SPs) have been involved in medical education for the past 50 years. Their role has evolved from assisting in history-taking and communication skills to portraying abnormal physical signs and hybrid simulations. This increases exposure of their physical and psychological domains to the learner. Asian SPs who come from more conservative cultures may be inhibited in some respect. This study aims to explore the attitudes and perspectives of Asian SPs with respect to their role and case portrayal.
Methods: This was a cohort questionnaire study of SPs involved in a high-stakes assessment activity at a university medical school in Singapore.
Results: 66 out of 71 SPs responded. Racial distribution was similar to population norms in Singapore (67% Chinese, 21% Malay, 8% Indian). SPs were very keen to provide feedback to students. A significant number were uncomfortable with portraying mental disorders (26%) or terminal illness (16%) and discussing Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (HIV/AIDS, 14%) or Sexually Transmitted Diseases (STDs, 14%). SPs were uncomfortable with intimate examinations involving the front of the chest (46%, excluding breast), and even abdominal examination (35%). SPs perceive that they improve quality of teaching and are cost effective.
Conclusion: The Asian SPs in our institution see themselves as a valuable tool in medical education. Sensitivity to the cultural background of SPs in case writing and the training process is necessary to ensure that SPs are comfortable with their role. Additional training and graded exposure may be necessary for challenging scenarios and physical examination.
Keywords: Standardised Patients, Perspective, Asian, Medical Education, Survey
Practice Highlights
- The Asian SPs in our institution see themselves as a valuable tool in medical education.
- Sensitivity to the cultural background of SPs in case writing and the training process is necessary to ensure that SPs are comfortable with the roles that they portray.
- Additional training and graded exposure for SPs may be necessary for challenging scenarios and physical examination in the Asian context.
I. INTRODUCTION
Standardised patients (SPs) have been involved in medical education since the 1960s (Barrows & Abrahamson, 1964). SP methodology has been widely used in North America and Europe. By the 1990s, majority of American medical schools were using the SP methodology in teaching clinical skills, assessments and for providing feedback to learners (Anderson et al., 1994). The prevalence of employing SP methodology in medical education in Asia is presumed to be less ubiquitous. It is therefore imperative to understand the views of Asian SPs so that the SP methodology can be fostered.
SPs started out simulating medical symptoms and patient concerns as well as evaluating medical interviewing skills in 1976 (Barrows & Abrahamson, 1964; Stillman et al., 1976). Their role has evolved to demonstrating abnormal physical signs, providing feedback on medical interviewing skills and being involved in hybrid simulations. This increases their exposure to the medical environment and to different medical experiences that they may not have experienced before. Certain experiences may potentially cause psychological distress. The SP could be in a vulnerable position and personal attitudes and beliefs towards illness should be taken into consideration when engaging SPs to portray these roles.
This is particularly true in Asian SPs. For example, patients may not be willing to discuss mental health issues for fear of social stigma and shame (Kramer et al., 2002). Asian SPs are also likely to be more conservative and modest with regards to physical examination. This can be extrapolated from findings that cultural attitudes toward breast cancer screening tests and modesty are some reasons why Asian women are reluctant to seek out breast cancer screening (Parsa et al., 2006).
In the past, SPs were routinely employed in objective structured clinical examinations at our medical school. They were not required to provide any form of feedback to the learners. We endeavoured to develop a more structured SP training program at our institution. In the initial phase, this study was conducted to survey the attitudes of the SPs who work at our institution towards case portrayal and the value of SP methodology.
II. METHODS
This was an anonymous cohort questionnaire study. An online questionnaire was administered to standardized patients who were recruited to work at a high-stakes objective structured clinical examination at a university medical school. Participants were sent a link to an electronic survey by email after the event. Participation was voluntary. Questions about race, age, gender and years of experience as an SP were asked. The importance of the contribution of an SP to medical education and their comfort with discussing medical conditions, portraying abnormal signs and undergoing different physical examinations were evaluated. A Likert scale of 1-5 was used where appropriate. This questionnaire study is covered by the institutional review board approval (Study Reference Number: 09-288) of the standardised patient program in our institution. Being an anonymous, voluntary survey, the consent was implied when the participants filled and returned the completed survey.
Descriptive statistics and the electronic survey were generated using Vovici software version 6 (Vovici Corp, Dulles, Virginia, United States).
III. RESULTS
66 out of 71 SPs (93%) responded. 40% of the SPs were aged 31-40 years (Figure 1) and 72% were female. Racial distribution was similar to population norms in Singapore (67% Chinese, 21% Malay, 8% Indian, 4% others).
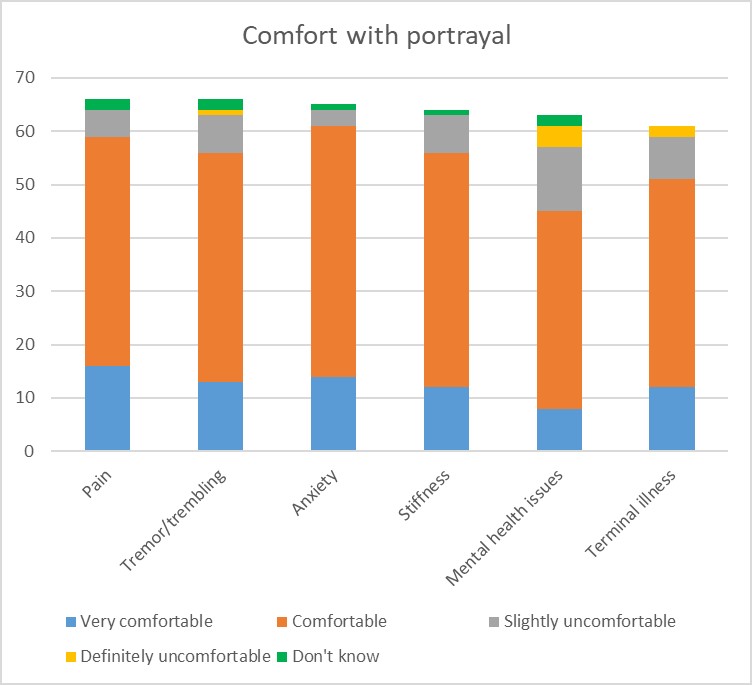
Figure 1: SP comfort with portrayal
With regards to their role, 95% of SPs felt it was important for them to be involved in teaching students and providing feedback. A significant number were uncomfortable with portraying mental disorders (26%) or terminal illness (16%) (Figure 1) and discussing HIV/AIDS (14%) or sexually transmitted diseases (14%) (Figure 2). With regards to death and dying, 6% of SPs were uncomfortable discussing this while another 6% were unsure about it. As expected, SPs were uncomfortable with examinations involving the front of the chest (46%, excluding breast examination) and even abdominal examination (35%). The 60% of the female SPs surveyed were uncomfortable with breast examination (Figure 3). SPs perceive themselves to improve the quality of teaching (98%) and to be cost effective (98%). The majority of this group of SPs (83%) felt that this was a viable option for sustainable employment.
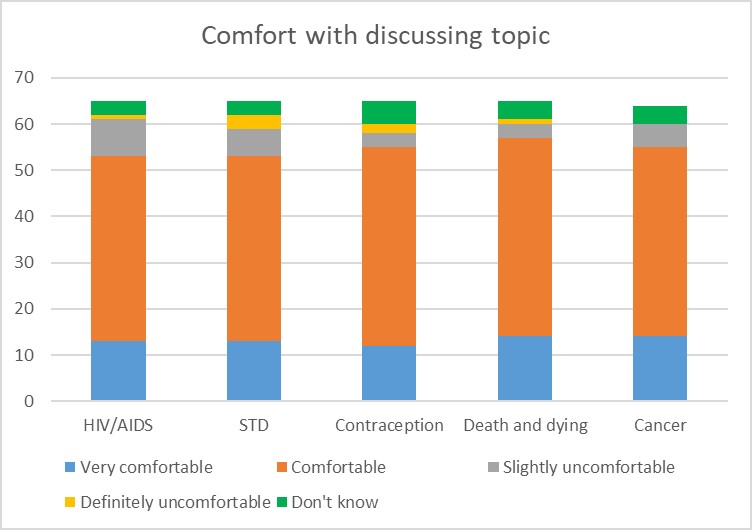
Figure 2: SP comfort with discussing topic
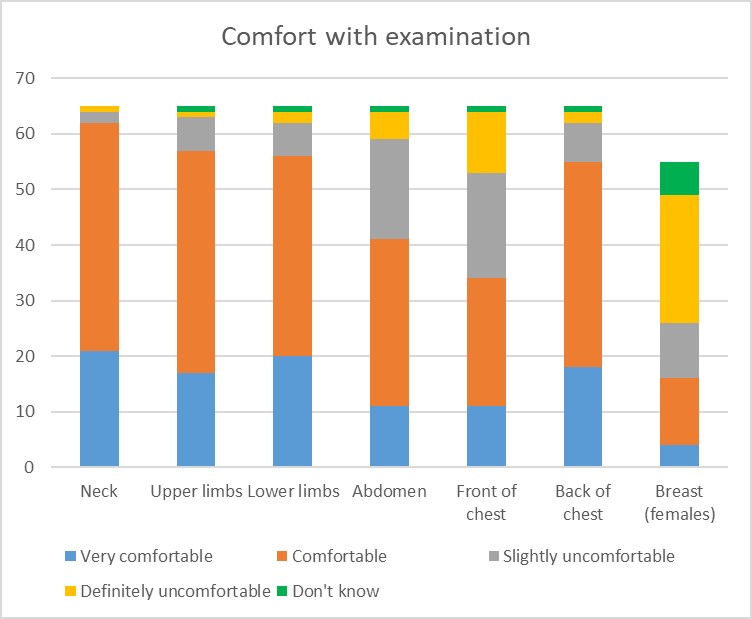
Figure 3: SP comfort with physical examination
IV. DISCUSSION
The benefits of SP methodology in providing a safe environment for practice and experiential learning are well established. In an effort to expand the use of SP methodology at our institution, information regarding the acceptability and feasibility were required. In the past, SPs were mainly employed in summative assessment activities and did not provide learners with feedback. Before pushing the boundaries of the SP job description, it was important to understand the perspectives of our SPs and which areas of SP work they would feel comfortable or uncomfortable with.
The areas of interest were comfort with portraying roles that involved taboo topics such as mental health issues, sexually transmitted disease, death and dying. In many Asian cultures, mental illness is stigmatizing; it reflects poorly on family lineage and can influence others’ beliefs about the suitability of an individual for marriage. (Kramer et al., 2002). Many people of Asian descent view people with mental illnesses as dangerous and aggressive (Lauber & Rössler, 2007) and believe that mental illness is a punishment from God (Fogel & Ford, 2005). In China, mental health problems are believed to be a result of weak character, having evil spirits, or punishment for not respecting ancestors (Lam et al., 2006). Asian American women avoid seeking treatment for depression and suicide ideation because of Asian family and community stigma associated with mental health issues (Augsberger et al., 2015). With regards to sexual practices and sexually transmitted disease, literature shows that Chinese men regard homosexual-related stigma and discrimination as major barriers to HIV testing. Most men were reluctant to obtain an HIV test in fear that their homosexual identity would be exposed, and they sometimes encountered discrimination even from medical personnel (Wei et al., 2014). Living with HIV in an Asian society is fraught with difficulty in the context of fear and disapproval (Ho & Goh, 2017). Death and dying are generally considered taboo in Asian cultures. Open discussions about death are regarded as a bad omen (Hall & Hall, 1976). Even for those who are dying, discussion about death is avoided because it is believed that such talk may hasten the dying process or even cause death prematurely (Xu, 2007). The avoidance if discussion about death and dying in traditional Chinese culture has been found to impede the ability to discuss advanced care planning (Cheng, 2018). These cultural beliefs were reflected in the discomfort expressed by some study participants with portrayal of roles involving mental health issues, HIV or sexually transmitted diseases, terminal illness and death and dying. This is evidence that some of our SPs do have traditional Asian perspectives regarding these sensitive issues but it is encouraging that a larger proportion are comfortable with these issues. This informs us that SPs should be given advanced notice regarding the content of the case that they are expected to portray so that they can make an informed choice when accepting roles. This is especially important when taboo or sensitive content is involved. SPs should also be given an option to withdraw from the assignment if they feel uncomfortable with the content of the case after they have been trained for the case.
In view of the more conservative nature of Asians, the hypothesis was that there could be areas of the body that SPs would not be willing to have examined by students. Asian women seem to be more conservative as only 53% of respondents in a study did breast self-examinations (Sim et al., 2009; Tan et al., 2005) reported that, between 2000 and 2003, 21.5% of women in Singapore presented with stage III or IV breast cancer which may potentially be due to cultural attitudes toward breast cancer screening tests and modesty, which inhibit Asian women from participating in breast cancer screening (Parsa et al., 2006). Spiritual and religious beliefs were found to act as a barrier to breast cancer screening in Singaporean Malay women (Shaw et al., 2018). As expected, more than half of our female SPs were uncomfortable with breast examination. When both genders were considered, examination of the front of chest (excluding breast) and abdominal examination were also flagged as concerns. This made us aware of the hesitance of some SPs in this area and the need to explore this further while trying to expand the role of the SP. In developing our SP program, consent for physical examination needs to be explained in detail and comfort of the individual SP with any physical examination must be taken into consideration.
The SPs in our study perceived themselves to be of value in medical education. Standardized patients in a study in Switzerland felt motivated, engaged, and willing to invest effort in their task and did not mind the increasing demands of their work as long as the social environment in SP programs was supportive (Schlegel et al., 2016). This is encouraging for a developing SP program to know as we feel confident to expand the job scope of our SPs as long as adequate explanation and training is provided to support the SPs. With more structured coaching and exposure, we expect that SPs will become more comfortable with more challenging roles and would be willing to push the boundaries of their comfort zone.
One limitation of this study is the large majority of female participants. This was a convenience sample to optimize response rate. Further studies should aim to include a more balanced gender representation. Another limitation would be that only quantitative data was collected. In exploring perspectives, focused interviews with qualitative analysis would have provided a more in-depth understanding of the beliefs and values of the SPs.
V. CONCLUSION
This study provides initial insights into the perspectives of Asian SPs at a university medical school in an Asian country. They see themselves as a valuable tool in medical education and are willing to expand their role in the curriculum. Faculty and trainers need to be sensitive to the cultural background of our SPs in case writing and the training process to ensure that SPs are comfortable with the roles that they portray. This is of particular relevance to SP programs that employ predominantly Asian SPs. There is evidence from this study of discomfort with portraying patients with mental health issues, terminal illness and sexually transmitted diseases. The areas of exposure required in physical examination also need to be carefully considered. Additional training and graded exposure may be necessary for SPs willing to be involved in these scenarios and certain types of physical examination. Concerns about the scenario from the SPs may not be immediately apparent. The results presented here will make SP trainers more aware of the possibility of SP discomfort. Future research will be required on what type of training and what other factors will promote comfort with these scenarios as well as the impact of taking on such roles on the SPs.
Notes on Contributors
Nicola Ngiam conceptualized and designed the study, analyzed the data and interpreted the results, wrote the manuscript draft, revised it, read it and gave final approval of the manuscript.
Hor Chuen-Yee developed the methodological framework for the study, performed data collection and data analysis, revised the manuscript, read it and gave final approval of the manuscript.
Ethical Approval
This study is covered by the institutional review board approval (Study Reference Number: 09-288).
Acknowledgement
We thank Dr Dimple Rajgor for her assistance in editing, formatting, reviewing, and in submitting the manuscript for publication.
Funding
No funding source required.
Declaration of Interest
The authors have no conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Anderson, M. B., Stillman, P. L., & Wang, Y. (1994). Growing use of standardized patients in teaching and evaluation in medical education. Teaching and Learning in Medicine: An International Journal, 6(1), 15-22.
Augsberger, A., Yeung, A., Dougher, M., & Hahm, H. C. (2015). Factors influencing the underutilization of mental health services among Asian American women with a history of depression and suicide. BMC Health Services Research, 15, 542-542. https://doi.org/10.1186/s12913-015-1191-7.
Barrows, H. S., & Abrahamson, S. (1964). The programmed patient: A technique for appraising student performance in clinical neurology. Academic Medicine, 39(8), 802-805.
Cheng, H. W. B. (2018). Advance care planning in Chinese seniors: Cultural perspectives. Journal of Palliative Care, 33(4), 242-246.
Fogel, J., & Ford, D. (2005). Stigma beliefs of Asian Americans with depression in an internet sample. Canadian Journal of Psychiatry, 50(8), 470-478.
Hall, E. T., & Hall, E. (1976). How cultures collide. Psychology Today, 10(2), 66-74.
Ho, L. P., & Goh, E. C. L. (2017). How HIV patients construct liveable identities in a shame based culture: The case of Singapore. International Journal of Qualitative Studies on Health and Well-Being, 12(1), 1333899. https://doi.org/10.1080/17482631.2017.1333899
Kramer, E., Kwong, K., Lee, E., & Chung, H. (2002). Cultural factors influencing the mental health of Asian Americans. The Western Journal of Medicine, 176(4), 227-231.
Lam, C. S., Tsang, H., Chan, F., & Corrigan, P. W. (2006). Chinese and American perspectives on stigma. Rehabilitation Education, 20(4), 269-279. https://doi.org/10.1891/088970106805065368
Lauber, C., & Rössler, W. (2007). Stigma towards people with mental illness in developing countries in Asia. International Review of Psychiatry, 19(2), 157-178.
Parsa, P., Kandiah, M., Abdul, H. R., & Zulkefli, N. (2006). Barriers for breast cancer screening among Asian women: A mini literature review. Asian Pacific Journal of Cancer Prevention, 7(4), 509-514.
Schlegel, C., Bonvin, R., Rethans, J., & der Vleuten Van, C. (2016). Standardized patients’ perspectives on workplace satisfaction and work-related relationships: A multicenter study. Simulation in Healthcare: Journal of the Society for Simulation in Healthcare, 11(4), 278-285.
Shaw, T., Ishak, D., Lie, D., Menon, S., Courtney, E., Li, S. T., & Ngeow, J. (2018). The influence of Malay cultural beliefs on breast cancer screening and genetic testing: A focus group study. Psycho‐Oncology, 27(12), 2855-2861.
Sim, H., Seah, M., & Tan, S. (2009). Breast cancer knowledge and screening practices: A survey of 1,000 Asian women. Singapore Medical Journal, 50(2), 132-138.
Stillman, P. L., Sabers, D. L., & Redfield, D. L. (1976). The use of paraprofessionals to teach interviewing skills. Pediatrics, 57(5), 769-774.
Tan, E., Wong, H., Ang, B., & Chan, M. (2005). Locally advanced and metastatic breast cancer in a tertiary hospital. Annals of the Academy of Medicine, Singapore, 34(10), 595-601.
Wei, C., Yan, H., Yang, C., Raymond, H., Li, J., Yang, H., Zhao, J., Huan, X., & Stall, R. (2014). Accessing HIV testing and treatment among men who have sex with men in China: A qualitative study. AIDS Care, 26(3), 372-378.
Xu, Y. (2007). Death and dying in the Chinese culture: Implications for health care practice. Home Health Care Management & Practice, 19(5), 412-414.
*Nicola Ngiam
Department of Medicine
National University Health System
1E Kent Ridge Rd,
Singapore 119228
Email address: nicola_ngiam@nuhs.edu.sg
Submitted: 28 March 2020
Accepted: 23 September 2020
Published online: 4 May, TAPS 2021, 6(2), 9-24
https://doi.org/10.29060/TAPS.2021-6-2/OA2242
De Zhang Lee1, Jia Yi Choo1, Li Shia Ng2, Chandrika Muthukrishnan1 & Eng Tat Ang1
1Department of Anatomy, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Otolaryngology, National University Hospital, Singapore
Abstract
Introduction: Gamification has been shown to improve academic gains, but the mechanism remains elusive. We aim to understand how psychological constructs interact, and influence medical education using mathematical modelling.
Methods: Studying a group of medical students (n=100; average age: 20) over a period of 4 years with the Personal Responsibility Orientation to Self-Direction in Learning Scale (PRO-SDLS) survey. Statistical tests (Paired t-test) and models (logistic regression) were used to decipher the changes within these psychometric constructs (Motivation, Control, Self-efficacy & Initiative), with gamification as a tool. Students were encouraged to partake in a maze (10 stations) that challenged them to answer anatomical questions using potted human specimens.
Results: We found that the combinatorial effects of the maze and Script Concordance Test (SCT) resulted in a significant improvement for “Self-Efficacy” and “Initiative” (p<0.05). However, the “Motivation” construct was not improved significantly with the maze alone (p<0.05). Interestingly, the “Control” construct was eroded in students not exposed to gamification (p<0.05). All these findings were supported by key qualitative comments such as “helpful”, “fun” and “knowledge gap” by the participants (self-awareness of their thought processes). Students found gamification reinvigorating and useful in their learning of clinical anatomy.
Conclusion: Gamification could influence some psychometric constructs for medical education, and by extension, the metacognition of the students. This was supported by the improvements shown in the SCT results. It is therefore proposed that gamification be further promoted in medical education. In fact, its usage should be more universal in education.
Keywords: Psychometric Constructs, Medical Education, Motivation, Initiative, Self-efficacy
Practice Highlights
- Student’s enjoyment (interest) of the curriculum will determine the eventual academic outcome.
- Metacognition (defined as the “learning of learning”, “knowing of knowing” and/ or the awareness of one’s thought processes) was improved with SCT and gamification.
- Gamification is useful as a form of augmentation for didactic teaching but should never replace it.
- Different type of psychometric scale (e.g. LASSI versus PRO-SDLS) used in your research will produce varying results.
- Gamification is resource intensive and needs extra time to prepare compared to didactic approaches.
I. INTRODUCTION
Psychology is integral to healthcare and education but has often been overshadowed, compared to the other basic disciplines (Choudhry et al., 2019; Pickren, 2007). This is ironical because human psyche needs to be properly understood in order to manage them effectively (Wisniewski & Tishelman, 2019). Presently, the study of psychology does not feature prominently in the medical curriculum (Gallagher et al., 2015) with the exception of psychiatry (Douw et al., 2019). This gap needs to be addressed (Paros & Tilburt, 2018). In this research, we seek to understand the constructs for good medical learning via gamification which has wide ranging effects (Mullikin et al., 2019). The psychometric constructs to be analysed were as follows: 1) “Motivation”; define as the desire to learn out of interest or enjoyment (Yue et al., 2019). 2) “Initiative”; refers to how proactive a student is to learning (Boyatzis et al., 2000). 3) “Control”; is how much influence one has over the circumstances (Sheikhnezhad Fard & Trappenberg, 2019). 4) “Self-Efficacy”; relates to how confident one is, to do what needs to be done (Michael et al., 2019). We believe that these constructs contribute to the student’s awareness of their own thought processes (metacognition) towards their medical education.
Gamification” is defined as a process of adding game-like elements to something so as to encourage more participation (Rutledge et al., 2018; Van Nuland et al., 2015). The idea of using games to “lighten up” medical education in the clinical setting was first proposed in 2002 (Howarth-Hockey & Stride, 2002). The authors observed increased engagement and participation during lunchtime medical quizzes in the hospital. They therefore concluded that medical education could be fun, and since then, gamification has been taken seriously by the community (Evans et al., 2015; Nevin et al., 2014). In essence, gamification could be something as simple as having board games (Ang et al., 2018) but importantly, its impact on students’ learning must be evaluated and validated. Most studies in the literature did not fulfil this requirement (Graafland et al., 2012). The impact of games on the behavioral and/or psychological outcomes should be studied (Graafland et al., 2017; Graafland et al., 2014).
A PubMed search would reveal that there are numerous self-reporting tools such as LASSI (Learning and Strategies Study Inventory (Muis et al., 2007), MSLQ (Motivated Strategies for Learning Questionnaire (Villavicencio & Bernardo, 2013), and the SRLPS (Self-regulated Learning Perception Scale) (Turan et al., 2009) etc. Given the choices, how does one decide which one to adopt for their studies? In our research, we chose to use the PRO-SDLS survey questions with some modifications. The choice was both serendipitous and practical, as we have previously validated it via the Cronbach alpha (>0.7). In our earlier work, feedback scores and results yielded inconclusive evidence to support enhanced motivation among our students. Furthermore, was this due to gamification? With the current endeavour, we aim to prove via mathematical modelling that there are indeed alterations to the psychometric constructs. Hence, we re-analyse the old data set together with additional new information, using statistical analysis tools such as the logistic regression model, Wilcoxon tests, and the Paired t-test.
Medical teaching and learning is a complex endeavour based on an apprenticeship model (Cortez et al., 2019), which may or may not be an ideal arrangement (Sheehan et al., 2010). Furthermore, the decision making is often delegated to the seniors (Chessare, 1998). Conversely, gamification could empower the students to take charge of one’s learning, including decision making (Shah et al., 2013). Furthermore, one needs to understand what works from what is empirical (Cote et al., 2017). While our initial research addressed the impact of the games on academic performance, we now sought to further understand its effects on the psychometric dimensions. This will help to understand the psychology of self-directed (or regulated) learning. We hypothesize that the amount of gamification will impact these constructs. In summary, we hope to achieve the following:
Aims:
- Understanding the role of psychometric constructs and gamification in medical education via suitable mathematical modelling.
- To decipher the interaction of different psychometric constructs (Motivation, Self-efficacy, Control and Initiatives) in producing desired learners’ behaviours (metacognition) via the anatomy maze.
II. METHODS
First-year medical students (M1) took part in this retrospective analytical research. Two randomised groups of medical students (n=75, median age: 20 years) consented to the study (Group 1 & 2). A randomised group of students (n=25) exposed to no gamifications (Group 0) served as the control. Every student was required to complete a pre- and post- PRO-SDLS for the research. There were no penalties for withdrawing from the IRB-approved project (See IRB: B-16-205).
Gamification was carried out according to the scheme in Figure 1. Each group was divided into 3 to 4 subgroups that would enter the maze with a clue card (see example in Figure 1) linked to a specific pot specimen. They were required to explore the museum for the next clue and had to answer the hidden questions (see examples in Appendix) which would provide further directions. At the conclusion, students were given a competitive pop quiz that had no impact on their summative academic grades.
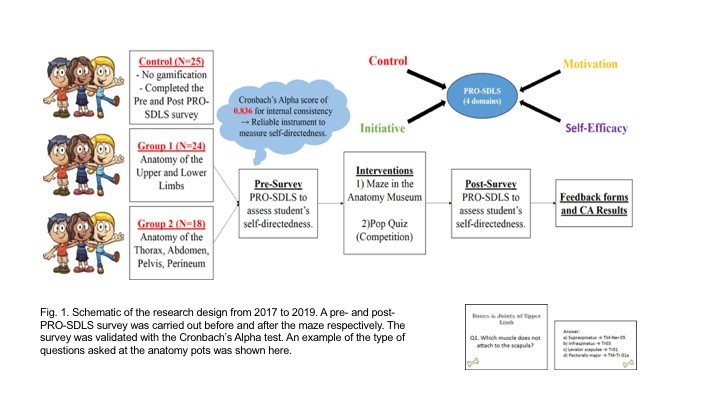
The main purpose was to assess formative knowledge acquisition. The validated PRO-SDLS include the following psychometric constructs: “Motivation” (7 questions), “Initiative” (6 questions), “Control” (6 questions) and “Self-Efficacy” (6 questions). (See Sup. Materials). The responses are then collapsed into an average accordingly. A higher score indicated more agreeability towards that construct for self-directed learning (Ang et al., 2017). The survey was designed with backward scoring to ensure accuracy. For quantification purposes, we subtracted the pre-feedback from the post-feedback scores for each question. An increased score for a particular construct suggests improvement (Cazan & Schiopca, 2014). Furthermore, students in Group 2 were given Script Concordance Test (SCT) quizzes (See Sup. Materials) as part of gamification (Lubarsky et al., 2013; Lubarsky et al., 2018; Wan et al., 2018). SCT were meant to enhance clinical reasoning. All data were analysed from two perspectives:
- The magnitude of score increase (or decrease) of the post- PRO-SDLS survey responses, with respect to the pre- responses.
- The odds of a student reporting an increased score in the post- PRO-SDLS survey responses.
In (a), the paired differences for each student’s response were studied using a parametric approach (paired t-test). In (b), we studied the odds of increased score for each construct, and investigate if grouping affected these odds. More formally, for each construct k (where k is one of the four constructs), we define variable as the probability of a student from group showing an increase in score for construct (and hence, as the probability that the student’s score decreased or remained unchanged). The value of can be estimated by dividing the number of students from group with an increased score for construct by the total number of students from group . If the interventions are unsuccessful, we would expect to be around since a student’s score would likely either increase or decrease at random, with an equal probability. This can be tested using the t-test.
An alternative approach would be to study the odds of success, which can be written as . A common mathematical model used to study these odds is the logistic regression model. For each construct, the logistic regression model studies the odds of a student from a given group showing an increased or decreased score. The overall significance of the model can be tested using the p-value obtained from the likelihood ratio test, while the significance of the individual odds can be tested using the t-test. For more details on the logistic regression model, we refer the reader to (Agresti, 2003).
We utilised the open source software R (Team, 2019) to perform our statistical analysis.
III. RESULTS
Participation rate in the gamification endeavour was consistently 90±5%, and there was zero withdrawal from it, accompanied by reported favourable qualitative comments.
A. Studying the Absolute Scores
The average change in scores across all the groups for each construct is given in Table 1. From these scores, we believe that our gamification exercises may have had a positive impact on “Self-Efficacy” and “Initiative”. To visualize the spread of responses, we have prepared box plots of the post – pre scores (available in Supplementary Materials).
|
Groups |
Constructs |
|||
|
Self-Efficacy |
Initiative |
Motivation |
Control |
|
|
0 |
0.07 |
-0.05 |
0.11 |
0.03 |
|
1 |
0.13 |
0.26 |
0.05 |
0.01 |
|
2 |
0.13 |
0.20 |
0.12 |
0.07 |
Table 1: Average post-pre scores
To determine if the construct scores pre and post intervention were different, we used the paired t-test, under the null hypothesis that there is no change. The p-values obtained are summarized in Table 2.
|
Groups |
Constructs |
|||
|
Self-Efficacy |
Initiative |
Motivation |
Control |
|
|
0 |
0.46 |
0.57 |
0.43 |
0.79 |
|
1 |
0.07 |
0.00 |
0.54 |
0.86 |
|
2 |
0.01 |
0.00 |
0.09 |
0.14 |
Table 2: p-values of t-test (to 2 decimal places)
We observe that the null hypothesis of no difference between pre and post intervention levels for all constructs are not rejected (under p=0.05) for the control group. Both tests also failed to show any significant change for the “Control” construct.
There is strong evidence that the classroom interventions employed by Groups 1 and 2 had an impact on “Initiative” levels of students, reflected by the small p-values obtained using both tests. The average increase in “Initiative” scores for students in Groups 1 and 2 are 0.71 and 0.67, respectively, which are similar. Recall that the students in Group 2 participated in the SCT, in addition to the maze which is common across both groups. This suggests that the SCT has a negligible impact on “Initiative”.
There is also strong evidence (p=0.05) to show that the games enhanced the “Self-Efficacy” levels among the students. The t-test also gives strong evidence (p=0.05) that there is a significant change in Group 2, and milder evidence for Group 1 (p=0.10). The average increase in “Self-Efficacy” levels for Groups 1 and 2 are 0.63 and 0.56, respectively. Again, the differences are negligible, and this suggests that the SCT has a negligible impact. Finally, there is mild evidence (p=0.10) of a significant change in “Motivation” for Group 2, but no such evidence for Group 1. The average increase in “Motivation” score for Group 2 is 0.55. This time, the SCT might have helped to improve students’ motivation.
B. Studying the Odds of Score Improvement
We will now turn our attention to modelling the odds of a student reporting an increase in construct score. Earlier, we defined as the probability of a student from group showing an increase in score for construct , and explained why we would expect to be around if the games have no impact on the odds of “success”. The t-test was used to test this, under the null hypothesis that for all groups and constructs. The p-values obtained are summarised in Table 3.
|
Groups |
Constructs |
|||
|
Self-Efficacy |
Initiative |
Motivation |
Control |
|
|
0 |
0.56 |
0.56 |
0.85 |
0.07 |
|
1 |
0.08 |
0.00 |
0.78 |
0.25 |
|
2 |
0.57 |
0.08 |
0.57 |
0.85 |
Table 3: p-values of t-test (to 2 decimal places)
We first notice that the p-values reported using both tests are almost identical. Interestingly, there is mild evidence (p=0.10) that the value of “Control” construct for Group 0 deviates significantly from 0.5, and it is estimated to be 0.32. This means that the students in the control group reported a drop in “Control” levels.
There is also mild evidence (p=0.10) that the probability of a student reporting an increase in “Self-Efficacy” for Group 1 deviates significantly from 0.5. This probability is estimated to be 0.63, which indicates that the odds of a student from Group 1 reporting an increase in “Self-Efficacy” levels is higher compared to the others.
Finally, there is evidence that the probability of reporting an increase in “Initiative” levels for students from Groups 1 and 2 deviates significantly from 0.5. The probabilities for Group 1 and Group 2 are 0.71 and 0.67, respectively.
Next, we will model our data using the logistic regression model. We will fit four models, one for each construct. For each model, we calculate the odds of a student from a given group showing an increased or decreased score. An odds of greater than 1 means that the student is more likely to show an increased score, while an odds of less than 1 means the opposite. An odds of exactly 1 means that the student is neither more nor less likely to show a changed score. The statistical significance of the individual odds and the overall model fit for each construct was computed using the t-test, and likelihood ratio test, respectively. The results are summarised in Table 4, with the statistically significant (p=0.10) odds highlighted in blue, together with their respective p-values.
|
Odds |
Constructs |
|||
|
Self-Efficacy |
Initiative |
Motivation |
Control |
|
|
Group 0 |
0.92 |
0.79 |
1.27 |
0.47 (0.08) |
|
Group 1 |
1.08 |
2.41 (0.02) |
1.67 |
0.72 |
|
Group 2 |
1.25 |
1.99 (0.10) |
1.26 |
0.93 |
|
|
Constructs |
|||
|
Self-Efficacy |
Initiative |
Motivation |
Control |
|
|
p-value |
0.93 |
0.01 |
0.22 |
0.29 |
Table 4: (top) Coefficients for each construct (significant odds in blue, p-values in brackets) (bottom) p-values to assess logistic regression model fit using likelihood ratio test
Under the logistic regression model, not rejecting the null hypothesis for a given odds means that we assume it takes on the value 1. It should be noted that the individual coefficients should be examined when the model is determined to be significant under the likelihood ratio test, as the coefficients obtained under a poor model fit may not be meaningful.
We notice that the significant terms flagged out by the t-test (Table 3) largely agree with the significant terms of the logistic regression model, except for the “Self-Efficacy” odds for Group 1. However, the “Self-Efficacy” model was not determined to be a good fit using the likelihood ratio test.
The only model which was deemed to be a good fit was the one for the “Initiative” construct. The odds for Group 0 is deemed to be insignificant (and hence assumed to be 1), while the odds for Groups 1 and 2 are statistically significant. We can interpret this model as follows,
- Since the odds for Group 0 is statistically insignificant under the t-test, we assume the odds to be 1. In other words, it is equally likely for a student from the control group to show an increase or decrease in score.
- The odds for both Group 1 and 2 are statistically significant. The odds of success of Group 1 is 2.41, which can be translated to a roughly 7 in 10 chance (probability of 0.71) for a student in this group showing an improved score. A similar interpretation can be made for Group 2, which showed an odds of 1.99. This translates to a slightly lower probability of 0.67 for a student from Group 2 displaying an improved score.
With this, we have presented a logistic regression approach of mathematically modelling these odds. A search on Google Scholar and PubMed yielded no previous work which made us of this mathematical modelling approach on the PRO-SDLS survey data. With the derived odds, we can compare the degree of success of the various classroom interventions. The logistic regression modelling approach is therefore, proposed as a complement of the t-test approach, which is restricted to detecting the presence of statistically significant differences.
C. Qualitative Comments (underlined words underpinning for metacognition)
1) Positive feedbacks:
- “The maze games were the most helpful as they helped me to consolidate my learning, and also enables me to ask the tutor any questions that I have from class. They allowed me to learn anatomy in a fun, enjoyable and memorable way”
- “It allowed me to visualize the things that I was learning and helped with clarifying doubts”
- “The extra question posted at each station was helpful”
- “Wanting to be able to identify things in the museum makes me more motivated to prepare beforehand”
- “Allows me to identify the knowledge gap so that I can work on it”
- “I like the quiz as it motivates me to study beforehand and shows me the gaps in my knowledge”
- “The clinically relevant questions made me think a lot”
2) Negative feedbacks:
- “I prefer didactic teaching”
- “We did not interact much with the exhibits”
- “The maze was more of a mini quiz or test to check if we remember anything”
- “Perhaps we could go into more complex concepts”
- “More challenging questions”
- “Students just follow each other around the anatomy museum and it defeats the purpose of the maze”
- “The maze could have a competitive element to make it more exciting. Maybe more MCQ questions per model so we can make use of it more”
IV. DISCUSSION
We undertook this research to decipher how gamification as a concept helps medical students learn a basic subject like human anatomy. We also want to understand how psychometric constructs interact to produce behavioural changes towards self-directed learning. This was done by analysing the data from the PRO-SDLS via statistical tests. Put simply, one needs to understand that medical education is a very complex process that demands balance between apprenticeship (fellowship) (Sheehan et al., 2010), and a dose of self-directed learning (van Houten-Schat et al., 2018). With our initial research into gamification of anatomy education (Ang et al., 2018), there were other studies suggesting similar benefits (Felszeghy et al., 2019; Nicola et al., 2017; Van Nuland et al., 2015). We are therefore convinced that gamification could help to engage students and improve academic gains. However, the notion of gaming can be very broad (Virtual Reality, board games, digital apps etc.), so there is a need to understand the underlying psychology. With that in mind, we re-analyse our previous data with the existing, using proven statistical tools to decipher the learning psychology of these medical students, and their awareness of their own thought processes (metacognition).
We earlier hypothesised that gamification would influence these dependent constructs differently and indeed this was the outcome. In our analysis, we found that the combinatorial effects of the maze and SCT resulted in a significant improvement for “Self-Efficacy” and “Initiative”. While the maze alone did not significantly improve “Motivation”, we saw mild evidence of an improvement in terms of psychometric scores, when the SCT and maze were used in combination. In lay terms, the maze encouraged these students to learn on their own. By extension, one could also argue that gamification will help the students in making decisions since “Motivation” and “Initiatives” are key attributes (Vohs et al., 2008). The ability to make a simple clinical judgement, and the courage to act on them, are the virtues that we should be imbuing in the medical students, and some junior doctors. Interestingly, there is mild evidence that the “Control” construct was undergoing erosion in the students not exposed to gamification, as the course progresses. This adverse result is not seen in both groups exposed to the games. Perhaps the more relaxed classroom setting with gamification helped students to feel more in control of their learning process. Logically, this made a lot of sense across the education landscape.
A follow up question would be, does the feedback confirm the results given in our qualitative analysis? Recall that in our logistic regression model, students from both non-control groups displayed a statistically significant improvement in “Initiative” levels. This is supported by some of the positive feedback received for our endeavours, such as being “motivated to prepare beforehand”, “identify the knowledge gap” and work on them, as well as helping them to “think a lot” about the course content. Furthermore, some of the negative feedback, such as requests for more challenging questions, or more questions in general, suggests that the students are taking the initiative to learn more. This certainly adds credence to the findings of our proposed logistic regression model, as well as highlighting the importance of studying both qualitative and quantitative feedback.
There are caveats that one should be aware when implementing gamification. The formative part of the endeavour could be variable, and dependent on numerous factors such as the tutor involved, and the type of games, interventions, and reporting scales used. In the feedback, 76% of the participants felt that the maze should continue as an adjunct but not to totally replace didactic tutorials. In other words, introducing gaming elements into the curriculum should be done judiciously. With reverse scoring, it was shown that “Self-Efficacy” fell as the level of gamification is increased. In lay terms, students might be feeling that the maze trivialize the learning of the subject. As a counter measure, and to maintain quality assurance, we could introduce video lectures from previous years to allay these fears. In summary, we now confirmed that gamification works, and it influences learning outcomes as demonstrated by others (Burgess et al., 2018; Goyal et al., 2017; Kollei et al., 2017; Kouwenhoven-Pasmooij et al., 2017; Kurtzman et al., 2018; O’Connor et al., 2018; Patel et al., 2017; Savulich et al., 2017). Separately, there were criticisms as to why SCT was introduced into the research. We believed that such augmentation will add “fun” for the pre-clinical students to tackle the various clinical scenarios and clinical anatomy.
V. LIMITATIONS OF THE STUDY
Our research necessitated that the students take part in the maze and the SCT. Although it was not compulsory, no students opted out of it. Some critics would misconstrue this to be a form of forced play. According to Jane McGonigal, gamification should ideally not be mandated (Roepke et al., 2015).
VI. CONCLUSION
Through statistical modelling, we have shown how the “Initiative”, “Motivation”, and “Self-Efficacy” constructs could potentially benefit from gamification. The before-after experimental set up allowed for powerful comparisons to be made. Studying the odds of construct score improvement, alongside the raw scores, allowed us to study the data from different perspectives. Though this approach, we discovered how the potential benefits of our gamification exercises outweigh the potential adverse effects. Gamification had resulted in improved “Initiative” in these medical students. We believe that their decision-making skills will also be boosted if existing culture allows for more self-discovery (to improve “Initiative”, “Control” and “Self-efficacy”) and autonomy. If these recommendations are duly considered and implemented thoughtfully, there is little doubt that our future doctors will be better equipped to serve humanity. This may also help to avoid possible burnout in residents (Hale et al., 2019).
Stronger conclusion and potential for applications are as follows: In a continuum, we started gamifying anatomy education and proven that academic grades could be improved by the process (Ang et al., 2018). We then asked a fundamental question in how exactly it happened. This was done by carrying out a psychometric analysis on the participants. We discovered that psychometric constructs were important, and this was proven in this manuscript. The impact of gamification is now elevated given the COVID-19 pandemic that necessitated more online teaching. Moving forward, we believe that gamification should move towards creating an electronic application that the students may access 24/7. This will ensure that medical teaching will be fortified and be somewhat protected from further disruptions.
Notes on Contributors
Lee De Zhang graduated with a degree in Statistics and Computer Science. He reviewed the literature, analysed the data and wrote part of the manuscript.
Eng Tat Ang, Ph.D., is a senior lecturer in anatomy at the Department of Anatomy at the YLLSoM, NUS. He reviewed the literature, designed the research, collected and analysed the data. He developed the manuscript.
Choo Jiayi, BSc (Hons) graduated with a degree in life sciences. She executed the research, and help collected the data. She contributed to the development of the manuscript.
M Chandrika, MBBS, DO, MSc is an instructor at the Department of Anatomy at the YLLSoM, NUS. She helped to execute the research and collected the data.
Ng Li Shia, MBBS, Master of Medicine (Otorhinolaryngology), MRCS(Glasg) is a consultant at the Department of Otolaryngology, Head & Neck Surgery (ENT), National University Hospital. She developed the SCT questions.
Ethical Approval
This project has received full IRB and Ethical clearance (NUS IRB: B-16-205).
Acknowledgements
A big thank you to all students who took part in the research, and to the CDTL, NUS, for providing a teaching enhancement funds to support this research. Appreciation also due to Dr Patricia Chen (Dept. of Psychology, NUS) for her helpful advice.
Funding
NUS TEG AY2017/2018 was awarded to help the investigators pay Mr De Zhang Lee for the statistical modelling that gamification drove medical education via a MAZE.
Declaration of Interest
All authors have no conflict of interest to declare.
References
Agresti, A. (2003). Categorical data analysis. John Wiley & Sons.
Ang, E. T., Abu Talib, S. N., Samarasekera, D., Thong, M., & Charn, T. C. (2017). Using video in medical education: What it takes to succeed. The Asia Pacific Scholar. 2(3), 15-21.
Ang, E. T., Chan, J. M., Gopal, V., & Li Shia, N. (2018). Gamifying anatomy education. Clinical Anatomy, 31(7), 997-1005. https://doi.org/10.1002/ca.23249
Boyatzis, R. E., Murphy, A. J., & Wheeler, J. V. (2000). Philosophy as a missing link between values and behaviour. Psychological Reports, 86(1), 47-64. https://doi.org/10.2466/pr0.2000.86.1.47
Burgess, J., Watt, K., Kimble, R. M., & Cameron, C. M. (2018). Combining Technology and Research to Prevent Scald Injuries (the Cool Runnings Intervention): Randomized Controlled Trial. Journal of Medical Internet Research, 20(10), e10361. http://doi.org/10.2196/10361
Cazan, A. M., & Schiopca, B. A. (2014). Self-directed learning, personality traits and academic achievement. Procedia-Social and Behavioral Sciences (127), 640-644.
Chessare, J. B. (1998). Teaching clinical decision-making to pediatric residents in an era of managed care. Pediatrics, 101(4 Pt 2), 762-766; discussion 766-767. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/9544180
Choudhry, F. R., Ming, L. C., Munawar, K., Zaidi, S. T. R., Patel, R. P., Khan, T. M., & Elmer, S. (2019). Health literacy studies conducted in australia: A scoping review. International Journal of Environmental Research and Public Health, 16(7). https://doi.org/10.3390/ijerph16071112
Cortez, A. R., Winer, L. K., Kassam, A. F., Hanseman, D. J., Kuethe, J. W., Quillin, R. C., 3rd, & Potts, J. R., 3rd. (2019). See none, do some, teach none: An analysis of the contemporary operative experience as nonprimary surgeon. Journal of Surgical Education, 76(6), e92-e101. https://doi.org/10.1016/j.jsurg.2019.05.007
Cote, L., Rocque, R., & Audetat, M. C. (2017). Content and conceptual frameworks of psychology and social work preceptor feedback related to the educational requests of family medicine residents. Patient Education and Counseling, 100(6), 1194-1202. https://doi.org/10.1016/j.pec.2017.01.012
Douw, L., van Dellen, E., Gouw, A. A., Griffa, A., de Haan, W., van den Heuvel, M., Hillebrand, A., Van Mieghem, P., Nissen, I. A., Otte, W. M., & Reijmer, Y. D. (2019). The road ahead in clinical network neuroscience. Network Neuroscience, 3(4), 969-993. https://doi.org/10.1162/netn_a_00103
Evans, K. H., Daines, W., Tsui, J., Strehlow, M., Maggio, P., & Shieh, L. (2015). Septris: a novel, mobile, online, simulation game that improves sepsis recognition and management. Academic Medicine, 90(2), 180-184. https://doi.org/10.1097/ACM.0000000000000611
Felszeghy, S., Pasonen-Seppänen, S., Koskela, A., Nieminen, P., Härkönen, K., Paldanius, K. M., Gabbouj, S., Ketola, K., Hiltunen, M., Lundin, M., & Haapaniemi, T. (2019). Using online game-based platforms to improve student performance and engagement in histology teaching. BMC Medical Education, 19(1), 273. https://doi.org/10.1186/s12909-019-1701-0
Gallagher, S., Wallace, S., Nathan, Y., & McGrath, D. (2015). ‘Soft and fluffy’: medical students’ attitudes towards psychology in medical education. Journal of Health Psychology, 20(1), 91-101. https://doi.org/10.1177/1359105313499780
Goyal, S., Nunn, C. A., Rotondi, M., Couperthwaite, A. B., Reiser, S., Simone, A., Katzman, D. K., Cafazzo, J. A., & Palmert, M. R. (2017). A mobile app for the self-management of Type 1 Diabetes among adolescents: A randomized controlled trial. Journal of Medical Internet Research mHealth and uHealth, 5(6), e82. https://doi.org/10.2196/mhealth.7336
Graafland, M., Bemelman, W. A., & Schijven, M. P. (2017). Game-based training improves the surgeon’s situational awareness in the operation room: a randomized controlled trial. Surgical Endoscopy, 31(10), 4093-4101. https://doi.org/10.1007/s00464-017-5456-6
Graafland, M., Schraagen, J. M., & Schijven, M. P. (2012). Systematic review of serious games for medical education and surgical skills training. British Journal of Surgery, 99(10), 1322-1330. https://doi.org/10.1002/bjs.8819
Graafland, M., Vollebergh, M. F., Lagarde, S. M., van Haperen, M., Bemelman, W. A., & Schijven, M. P. (2014). A serious game can be a valid method to train clinical decision-making in surgery. World Journal of Surgery, 38(12), 3056-3062. https://doi.org/10.1007/s00268-014-2743-4
Hale, A. J., Ricotta, D. N., Freed, J., Smith, C. C., & Huang, G. C. (2019). Adapting Maslow’s Hierarchy of Needs as a Framework for Resident Wellness. Teaching and Learning in Medicine, 31(1), 109-118. https://doi.org/10.1080/10401334.2018.1456928
Howarth-Hockey, G., & Stride, P. (2002). Can medical education be fun as well as educational? British Medical Journal, 325(7378), 1453-1454. https://doi.org/10.1136/bmj.325.7378.1453
Kollei, I., Lukas, C. A., Loeber, S., & Berking, M. (2017). An app-based blended intervention to reduce body dissatisfaction: A randomized controlled pilot study. Journal of Consulting and Clinical Psychology, 85(11), 1104-1108. https://doi.org/10.1037/ccp0000246
Kouwenhoven-Pasmooij, T. A., Robroek, S. J., Ling, S. W., van Rosmalen, J., van Rossum, E. F., Burdorf, A., & Hunink, M. G. (2017). A blended web-based gaming intervention on changes in physical activity for overweight and obese employees: Influence and usage in an experimental pilot study. Journal of Medical Internet Research Serious Games, 5(2), e6. https://doi.org/10.2196/games.6421
Kurtzman, G. W., Day, S. C., Small, D. S., Lynch, M., Zhu, J., Wang, W., Rareshide, C. A., & Patel, M. S. (2018). Social incentives and gamification to promote weight loss: The lose it randomized, controlled trial. Journal of General Internal Medicine, 33(10), 1669-1675. https://doi.org/10.1007/s11606-018-4552-1
Lubarsky, S., Dory, V., Duggan, P., Gagnon, R., & Charlin, B. (2013). Script concordance testing: from theory to practice: AMEE guide no. 75. Medical Teacher, 35(3), 184-193. https://doi.org/10.3109/0142159X.2013.760036
Lubarsky, S., Dory, V., Meterissian, S., Lambert, C., & Gagnon, R. (2018). Examining the effects of gaming and guessing on script concordance test scores. Perspectives on Medical Education, 7(3), 174-181. https://doi.org/10.1007/s40037-018-0435-8
Michael, K., Dror, M. G., & Karnieli-Miller, O. (2019). Students’ patient-centered-care attitudes: The contribution of self-efficacy, communication, and empathy. Patient Education and Counseling. https://doi.org/10.1016/j.pec.2019.06.004
Muis, K. R., Winne, P. H., & Jamieson-Noel, D. (2007). Using a multitrait-multimethod analysis to examine conceptual similarities of three self-regulated learning inventories. British Journal of Educational Psychology, 77(Pt 1), 177-195. https://doi.org/10.1348/000709905X90876
Mullikin, T. C., Shahi, V., Grbic, D., Pawlina, W., & Hafferty, F. W. (2019). First year medical student peer nominations of professionalism: A methodological detective story about making sense of non-sense. Anatomical Sciences Education, 12(1), 20-31. https://doi.org/10.1002/ase.1782
Nevin, C. R., Westfall, A. O., Rodriguez, J. M., Dempsey, D. M., Cherrington, A., Roy, B., Patel, M., & Willig, J. H. (2014). Gamification as a tool for enhancing graduate medical education. Postgraduate Medical Journal, 90(1070), 685-693. https://doi.org/10.1136/postgradmedj-2013-132486
Nicola, S., Virag, I., & Stoicu-Tivadar, L. (2017). vr medical gamification for training and education. Studies in Health Technology and Informatics, 236, 97-103. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28508784
O’Connor, D., Brennan, L., & Caulfield, B. (2018). The use of neuromuscular electrical stimulation (NMES) for managing the complications of ageing related to reduced exercise participation. Maturitas, 113, 13-20. https://doi.org/10.1016/j.maturitas.2018.04.009
Paros, S., & Tilburt, J. (2018). Navigating conflict and difference in medical education: insights from moral psychology. BMC Medical Education, 18(1), 273. https://doi.org/10.1186/s12909-018-1383-z
Patel, M. S., Benjamin, E. J., Volpp, K. G., Fox, C. S., Small, D. S., Massaro, J. M., Lee, J. J., Hilbert, V., Valentino, M., Taylor, D. H., & Manders, E. S. (2017). effect of a game-based intervention designed to enhance social incentives to increase physical activity among families: The BE FIT randomized clinical trial. Journal of the American Medical Association Internal Medicine, 177(11), 1586-1593. https://doi.org/10.1001/jamainternmed.2017.3458
Pickren, W. (2007). Psychology and medical education: A historical perspective from the United States. Indian Journal of Psychiatry, 49(3), 179-181. https://doi.org/10.4103/0019-5545.37318
Roepke, A. M., Jaffee, S. R., Riffle, O. M., McGonigal, J., Broome, R., & Maxwell, B. (2015). Randomized controlled trial of superbetter, a smartphone-based/internet-based self-help tool to reduce depressive symptoms. Games for Health Journal, 4(3), 235-246. https://doi.org/10.1089/g4h.2014.0046
Rutledge, C., Walsh, C. M., Swinger, N., Auerbach, M., Castro, D., Dewan, M., Khattab, M., Rake, A., Harwayne-Gidansky, I., Raymond, T. T., & Maa, T. (2018). Gamification in action: Theoretical and practical considerations for medical educators. Academic Medicine, 93(7), 1014-1020. https://doi.org/10.1097/ACM.0000000000002183
Savulich, G., Piercy, T., Fox, C., Suckling, J., Rowe, J. B., O’Brien, J. T., & Sahakian, B. J. (2017). Cognitive training using a novel memory game on an ipad in patients with amnestic mild cognitive impairment (aMCI). International Journal of Neuropsychopharmacology, 20(8), 624-633. https://doi.org/10.1093/ijnp/pyx040
Shah, A., Carter, T., Kuwani, T., & Sharpe, R. (2013). Simulation to develop tomorrow’s medical registrar. The Clinical Teacher, 10(1), 42-46. https://doi.org/10.1111/j.1743-498X.2012.00598.x
Sheehan, D., Bagg, W., de Beer, W., Child, S., Hazell, W., Rudland, J., & Wilkinson, T. J. (2010). The good apprentice in medical education. New Zealand Medical Journal, 123(1308), 89-96. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/20201158
Sheikhnezhad Fard, F., & Trappenberg, T. P. (2019). A novel model for arbitration between planning and habitual control systems. Frontiers in Neurorobotics, 13, 52. https://doi.org/10.3389/fnbot.2019.00052
Team, R. C. (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing.
Turan, S., Demirel, O., & Sayek, I. (2009). Metacognitive awareness and self-regulated learning skills of medical students in different medical curricula. Medical Teacher, 31(10), e477-483. https://doi.org/10.3109/01421590903193521
van Houten-Schat, M. A., Berkhout, J. J., van Dijk, N., Endedijk, M. D., Jaarsma, A. D. C., & Diemers, A. D. (2018). Self-regulated learning in the clinical context: A systematic review. Medical Education, 52(10), 1008-1015. https://doi.org/10.1111/medu.13615
Van Nuland, S. E., Roach, V. A., Wilson, T. D., & Belliveau, D. J. (2015). Head to head: The role of academic competition in undergraduate anatomical education. Anatomical Sciences Education, 8(5), 404-412. https://doi.org/10.1002/ase.1498
Villavicencio, F. T., & Bernardo, A. B. (2013). Positive academic emotions moderate the relationship between self-regulation and academic achievement. British Journal of Educational Psychology, 83(Pt 2), 329-340. https://doi.org/10.1111/j.2044-8279.2012.02064.x
Vohs, K. D., Baumeister, R. F., Schmeichel, B. J., Twenge, J. M., Nelson, N. M., & Tice, D. M. (2008). Making choices impairs subsequent self-control: A limited-resource account of decision making, self-regulation, and active initiative. Journal of Personality and Social Psychology, 94(5), 883-898. https://doi.org/10.1037/0022-3514.94.5.883
Wan, M. S., Tor, E., & Hudson, J. N. (2018). Improving the validity of script concordance testing by optimising and balancing items. Medical Education, 52(3), 336-346. https://doi.org/10.1111/medu.13495
Wisniewski, A. B., & Tishelman, A. C. (2019). Psychological perspectives to early surgery in the management of disorders/differences of sex development. Current Opinion in Pediatrics, 31(4), 570-574. https://doi.org/10.1097/MOP.0000000000000784
Yue, P., Zhu, Z., Wang, Y., Xu, Y., Li, J., Lamb, K. V., Xu, Y., & Wu, Y. (2019). Determining the motivations of family members to undertake cardiopulmonary resuscitation training through grounded theory. Journal of Advanced Nursing, 75(4), 834-849. https://doi.org/10.1111/jan.13923
*Ang Eng Tat
Department of Anatomy
Yong Loo Lin School of Medicine
MD10, National University of Singapore
Singapore 117599
Email address: antaet@nus.edu.sg
Submitted: 14 March 2020
Accepted: 20 July 2020
Published online: 5 January, TAPS 2021, 6(1), 30-39
https://doi.org/10.29060/TAPS.2021-6-1/OA2235
Yit Shiang Lui, Abigail HY Loh, Tji Tjian Chee, Jia Ying Teng, John Chee Meng Wong & Celine Hsia Jia Wong
Department of Psychological Medicine, National University Health System, Singapore
Abstract
Introduction: A good understanding of basic child-and-adolescent psychiatry (CAP) is important for general medical practice. The undergraduate psychiatry teaching programme included various adult and CAP topics within a six-week time frame. A team of psychiatry tutors developed two new teaching formats for CAP and obtained feedback from the students about these teaching activities.
Methods: Medical students were introduced to CAP via small group teaching in two different modes. One mode was the “Clinical Vignettes Tutorial” (CVT) and the other mode “Observed Clinical Interview Tutorial” (OCIT). In CVT, tutors would discuss clinical vignettes of real patients with the students, followed by explanations about theoretical concepts and management strategies. OCIT involved simulated-patients (SPs) who assisted by acting as patients presenting with problems related to CAP, or as parents for such patients. At each session, students were given the opportunity to interview “patients” and “parents”. Feedback was given following these interviews. The students then completed surveys about the teaching methods.
Results: Students rated very-positive feedback for the teaching of CAP in small groups. Almost all found these small groups enjoyable and that it helped them apply what they had learnt. Majority agreed that the OCIT sessions increased their level of confidence in speaking with adolescents and parents. Some students agreed that these sessions had stimulated their interest to know more about CAP.
Conclusion: Small group teaching in an interactive manner enhanced teaching effectiveness. Participants reported a greater degree of interest towards CAP, and enhanced confidence in treating youths with mental health issues as well as engaging their parents.
Keywords: Child Adolescent Psychiatry, Medical Education, Small Group, Teaching
Practice Highlights
- Psychiatric disorders are among the most common medical conditions experienced by children and adolescents, and data from the Singapore Mental Health survey conducted in 2010 had shown the prevalence rates of emotional and behavioural problems among Singaporean youth to be at 12.5%.
- Most medical students had limited exposure to Child & Adolescent Psychiatry (CAP) in their medical curriculum due to reduced proportions of teaching time and opportune clinical exposures allocated to CAP programmes.
- This would be further compounded by the limited number of child and adolescent psychiatrists involved in teaching at medical schools and supervising clinical postings.
- This manuscript described synergistic teaching methods employed in educating medical students within the field of Child & Adolescent Psychiatry and examined the effectiveness and acceptability of CAP teaching using small-group teaching classes.
- The CAP small group interactive teaching sessions for medical students received good feedback from majority of the participants and translated to applicability and skillsets transferability.
I. INTRODUCTION
Psychiatric disorders are among the most common medical conditions experienced by children and adolescents during their developmental years. Epidemiological data from developed countries demonstrated transitions from acute and infectious diseases to chronic conditions, that included mental health problems as well (Baranne & Falissard, 2018; Kyu et al., 2016; World Health Organization, 2014). Recent global health surveys had estimated the median prevalence of psychiatric disorders present in children and adolescents to be about 12% (Costello, Egger, & Angold, 2005). Data from the Singapore Mental Health survey conducted in 2010 had shown the prevalence rates of emotional and behavioural problems among Singaporean youth to be at 12.5% which was comparable with global data (Lim, Ong, Chin, & Fung, 2015). Some studies had also demonstrated a growing trend of a burgeoning proportion of disabilities in children and adolescents that would be attributable to mental health disorders. Therefore, increasingly more health resources would be expected to meet these demands (Baranne & Falissard, 2018; Erskine et al., 2015). This would largely come in the form of services focusing on prevention, identification, and management of child and adolescent psychiatric disorders (Baranne & Falissard, 2018; Costello et al., 2005; Erskine et al., 2015). There is hence a demand to fill the gap for escalating mental health needs in this population of children and adolescents. Delays in accessing prompt and adequate assessment may incur socio-economic costs and bring about further psychiatric comorbidities.
Increasing the numbers of trained child and adolescent psychiatrists may be necessary to meet the current and projected needs in youth mental health (Baranne & Falissard, 2018; Breton, Plante, & St-Georges, 2005; Thomas & Holzer, 2006). Globally, as well as in Singapore, the number of such specialists fell short of meeting the demands, and increased recruitment was needed to address this workforce shortage (Breton et al., 2005; Lim et al., 2015; Thomas & Holzer, 2006). Hence, there had been moves in recent years to increase exposure to, and interest in, child and adolescent psychiatry (CAP) among medical students (Hunt, Barrett, Grapentine, Liguori, & Trivedi, 2008; Malloy, Hollar, & Lindsey, 2008; Plan, 2002; Thomas & Holzer, 2006). Most medical students had limited exposure to CAP in their medical curriculum due to reduced proportions of teaching time and opportune clinical exposures allocated to CAP programmes. This would be further compounded by the limited number of child and adolescent psychiatrists involved in teaching at medical schools and supervising clinical postings (Dingle, 2010; Lim et al., 2015; Plan, 2002; Sawyer & Giesen, 2007). It remained important however that medical students were taught CAP, given the burden of mental health disorders in our youths today (Dingle, 2010; Hunt et al., 2008; Kaplan & Lake, 2008; Sawyer & Giesen, 2007; Thomas & H, 2006). Other specialist practitioners such as family medicine specialists and paediatricians also frequently managed youths with psychiatric problems. Understanding early childhood development, critical milestones in childhood and adolescents would be essential in any specialty that had to interact and manage children as part of routine practice (Hunt et al., 2008; Plan, 2002). This would form the basis why CAP would be taught in medical schools as part of regular and wider curricula (Dingle, 2010; Hunt et al., 2008; Kaplan & Lake, 2008; Malloy et al., 2008; Plan, 2002; Sawyer & Giesen, 2007). The current medical school pedagogy may have underestimated the salience of teaching CAP in the undergraduate curriculum. This resulted in allocating much less time, attention as well as teaching resources towards CAP. Curriculum designers will also have severely under-appreciated the transferability of skillset due to the inherent challenges in undertaking interviews with children and their parents.
A. The Curriculum and Teaching Methods
In Yong Loo Lin School of Medicine at the National University of Singapore, CAP teaching would be embedded within a six-week General Psychiatry clerkship for Fourth-Year medical students. CAP teaching would consist of a period of 20-hour centralised teaching at the affiliated National University Hospital, together with clinical attachments to the outpatient child psychiatry clinics in other restructured hospitals. The 20-hour teaching would include online lectures made accessible through students’ Intranet, didactic lectures delivered in large group setting by clinical tutors, as well as small group teaching classes. In this paper, the authors examined the effectiveness and acceptability of CAP teaching using these small group teaching classes.
A comprehensive CAP education will ensure the following domains are included such as emotional symptomatology (e.g. depression, anxiety, enuresis), conduct and disruptive behavioural problems (e.g. attention deficit disorder, conduct disorder, bullying), developmental delays (e.g. specific learning, speech or autistic spectrum) and relationship difficulties, personal habits and injuries (e.g. abuse, suicide, digital overuse). Knowledge will include normal child developmental psychology as well as the assessment and management of common CAP conditions. Practice imparts interview skills of CAP and counselling of young parents.
Small group teaching sessions consisted of several components in its general pedagogic approach. The aim of these sessions was to cover the teaching of core knowledge and practices in common CAP cases, as well as training of interview skills required in communicating with children, adolescents, and their parents. Each session would start off with a series of lectures on four major domains of CAP: (1) emotional symptoms, (2) conduct and disruptive behavioural problems, (3) developmental delays, and (4) relationship difficulties, personal habit, and injuries. The lectures would be followed by both “Clinical Vignettes Tutorial” (CVT) and “Observed Clinic Interview Tutorials” (OCIT). The teaching sessions were structured as such in view of time constraints in the undergraduate curriculum that precluded comprehensive clinical exposure—a combination of didactics and simulated practice was designed to maximise the transferability of necessary theoretical knowledge and practical skills set for the students.
In the CVT, tutors would discuss clinical vignettes derived from real-life patients, and their underpinning theoretical concepts for about 2½ hours. This teaching activity would have covered the principles of psychopharmacology in the youths, as well as three distinct childhood conditions: a) Adolescent Depression with self-harm behaviour, b) Post-traumatic Stress Disorder in an adolescent and c) Adjustment Disorder in an adolescent with chronic medical illnesses. The anonymised vignettes were based on actual patient profiles. During each interactive discussion of these clinical presentations, students were encouraged by tutors to raise critical questions as pertinent portions of the history unfolded to enhance their analytic thinking of the cases and remember these teachable moments.
The second teaching activity of the OCITs would take place after a second series of lectures on other CAP conditions had been conducted. During this three-hour long OCIT, students would be provided opportunities to interview simulated patients (SPs). Each group would comprise of 12 to 18 students led by one clinical tutor.
The four pre-prepared clinical scenarios included one case of an adolescent with Anorexia Nervosa; another of an adolescent with Social Anxiety Disorder; a parent of a child with Attention Deficit Hyperactivity Disorder; and last but not least a parent of a child with features of Autism Spectrum Disorder. Each of these scenarios would include a case template that comprised an interesting title, the learning and assessment objective, the student’s task and the script for the SP complete with an opening statement, standard statements and character presentation (behaviour, affect and mannerism).
Students would take turn to interview the SPs in attempts to collate accurate and adequate clinical information to arrive at provisional diagnoses. The students were then tasked to discuss the possible differential diagnoses, to provide treatment options as well as to formulate prognoses of the conditions with the SPs. The SPs were in turn invited to comment on the interactions they had with the students. The clinical tutors would also conduct follow-up discussions to provide feedback to the students on aspects of their interviewing techniques and knowledge of the clinical conditions. The discussions also focused on the differential diagnoses and management strategies for various conditions.
II. METHODS
Paper and pen self-report surveys for both the CVT and OCIT sessions were done to evaluate the student participants’ learning, experience, and interest in CAP (Appendix A). Student participants were asked to grade responses on a five-point Likert scale (1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree and 5 = Strongly agree), in relation to statements such as “I found the session enjoyable” and “The case scenarios were relevant”. The surveys were completed and submitted anonymously at the end of each teaching session. The surveys also included a free–text segment for any open feedback, in which the question asked the student participants to list down “The best things about the session” and “Some ways which I think can make the sessions better”. The surveys utilised for each teaching session differed slightly owing to varied content validity of the teaching methods, but the questions were largely identical for most of the surveys. Implied informed consent was provided for by the participating students during the surveys.
For the current study, the authors analysed data from the surveys completed by the Fourth-Year undergraduate medical students who were rotated to the six-week Psychiatry clerkship period of five months between July and November in 2017.
Descriptive statistics were used to analyse the findings of the survey.
III. RESULTS
A total of 289 students completed the survey between July 2017 and November 2017. With regards to the CVT, majority of the students agreed or strongly agreed that the sessions were enjoyable (90.7%) and beneficial to their overall learning (90.7%; Table 1). They provided feedback that the session had helped them to apply what they had learnt (95.8%), and that the case scenarios were relevant (98.2%).
|
Survey Statement |
Participants Who Indicated “Agree” Or “Strongly Agree” |
||
|
|
|
N |
% |
|
1 |
“I found the session enjoyable…”
|
262 |
90.7 |
|
2 |
“The session helped me to apply what I have learnt…”
|
277 |
95.8 |
|
3 |
“The case scenarios were relevant…”
|
284 |
98.2 |
|
4 |
“My clinical tutor was effective in facilitating the session…”
|
281 |
97.2 |
|
5 |
“The session stimulated my interest in Child and Adolescent Psychiatry…”
|
247 |
85.5 |
|
6 |
“There was sufficient time for each section…”
|
272 |
94.1 |
|
7 |
“Overall, I found the session beneficial…”
|
262 |
90.7 |
Table 1. Survey results for the Clinical Vignettes Tutorial (CVT)
For the OCIT, most of the survey respondents agreed or strongly agreed that the activity had helped them to learn psychiatric interviewing skills (97.7%), increased their confidence in speaking with adolescents or parents (95.1%) (Table 2). Most of the students who responded to the survey had reported that the simulated patients’ performances were realistic (97.7%). A large proportion of the respondents indicated that the teaching session had met their learning objectives (98.5%).
|
Survey Statement |
Participants Who Indicated “Agree” Or “Strongly Agree” |
||
|
|
|
N |
% |
|
1 |
“The session helped me to learn psychiatric interviewing skills…”
|
260 |
97.7 |
|
2 |
“The session increased my confidence in speaking to adolescents/parents…”
|
253 |
95.1 |
|
3 |
“The session helped me to apply what I have learnt…”
|
248 |
96.9 |
|
4 |
“The session stimulated my interest in Child and Adolescent Psychiatry…”
|
219 |
83.3 |
|
5 |
“My clinical tutor provided useful feedback…”
|
259 |
97.3 |
|
6 |
“The simulated patients’ performances felt realistic…”
|
258 |
97.7 |
|
7 |
“There was sufficient time for each case…”
|
256 |
95.9 |
|
8 |
“Overall, the session met the learning objectives…”
|
257 |
98.5 |
Table 2. Survey results for the Observed Clinical Interview Tutorial (OCIT)
Examining the effectiveness of these teaching activities in stimulating the students’ interest towards CAP, 83.3% of the respondents indicated that the CVT had done so, while a slightly higher proportion (85.5%) of the respondents reported that the OCIT stimulated their interest in CAP.
Majority of the respondents indicated that the clinical tutors were effective in facilitating the CVT (97.2%). Similarly, most of the respondents reported that the clinical tutors provided useful feedback during the OCIT (97.3%).
Entries in the free-text feedback section about what the students liked best about the CVT and OCIT included comments such as “good for application”, session allowed for “practice of interviewing skills” and “helped consolidate knowledge” (Figure 1). Several students liked the “interactive” nature of the interviews and discussions, as well as “feedback” from tutors, which also helped in their learning.
Figure. 1. Open comment feedback to the survey question “The best things about the sessions were…”
In areas that the students indicated for further improvement, they had cited for a “shorter” duration in each teaching session (Figure 2). This was likely due to the nature of a full day programme of CAP teaching which could last eight hours in a day with a one-hour lunch break. Others had shared that they preferred “smaller” groups so students could get more chances to practice interviewing the SPs and also be provided “more time for discussion” to allow more in-depth feedback as well as discussion of each clinical condition. Some students remarked that Objective Structured Clinical Examination (OSCE) styled marking schemes could help enhance their learning experiences as this method might be more structured, compared to an open discussion.

Figure 2. Open comment feedback to the survey question “Some ways which I think can make the sessions better are…”
IV. DISCUSSION
This study evaluated the effectiveness and acceptability of small group tutorials for CAP conditions, which are packaged inseparably as part of a medical undergraduate psychiatry teaching programme. CVT and OCIT are synergistically designed to complement each other in the curriculum. The surveys used to compile the medical undergraduates’ responses had focused on their learning experience with the CAP curriculum. The effectiveness of the teaching methods namely CVT and OCIT would be determined from transferability of the requisite knowledge base and the clinical skills, as well as availability of opportunities to experience interviewing for the participants. The survey responses were also used to gauge the performance of the SPs and the clinical tutors’ usefulness. In addition, the degree of how impactful the teaching sessions had in generating interest towards CAP was also evaluated.
The fourth-year medical students gave good feedback for the small group teaching sessions. They reported that the CVT were enjoyable, beneficial and had allowed them to apply what they had learnt. For the OCIT, most of the respondents indicated that the session had helped them to learn psychiatric interviewing skills, increased their level of confidence in speaking with adolescents and parents, and had helped them to apply in clinical scenarios what they had learnt. There is discernible difference between the feedback for CVT and OCIT. The students’ feedback for CVT affirmed applicability of the knowledge content of CAP whereas those for OCIT concurred with transferability of interviewing skills in terms of confidence level.
In the open feedback segment of the survey, respondents reported that they had particularly liked the interactive and hands-on aspect of the session, the frequent opportunities for evaluation and feedback, as well as for practice. However, they highlighted that certain factors such as the size of grouping, the length of the sessions and random allocation of conditions could be improved further to enhance their learning experience. Overall, their feedback still indicated positive experiences in these small group sessions, and this translated to an increased knowledge base, a heightened level of confidence, and burgeoned interest in CAP among the student participants.
This study’s limitations included the challenges inherent with attempting to accurately assess the students’ genuine experiences and feelings towards the sessions; with possible biases (recall and Hawthorne effect) in responding to questionnaires; and the lack of correlation to actual performances in real-world settings. Furthermore, what remained unanswered was how such sessions might truly generate interest leading to possibly pursuit of a career in CAP. In addition, it is uncertain whether changing the teaching methods with the curriculum could inspire more medical students and young doctors to consider specialising in this field and raise the number of residency applications. The data from our study did appear to be consistent with findings from other CAP clinical teaching programmes. In these programmes, more exposure to CAP and increased clinical opportunities did correlate with changes in impressions towards and appreciation of clinical interactions with children, increased positive views of CAP as part of medical practice, and heightened interest in CAP as a field of medical specialty (Dingle, 2010; Kaplan & Lake, 2008; Malloy et al., 2008; Martin, Bennett, & Pitale, 2005).
In the current undergraduate medical curriculum, the amount of time allocated to teaching CAP is relatively small compared to other topics. Child and adolescent psychiatric cases can be particularly complex and their management demand sensitive handling, which may pose challenges to real world practice. Youth patients and their parents may value privacy and sometimes do not allow medical students to be involved in initial assessments and subsequent follow-up consultations. These factors collectively pose unique challenges to teaching and equipping medical students with the skills and knowledge to address child and adolescent mental health disorders. While clinical contact and patient experience would be preferred and desirable for training, it may be impractical given the various constraints mentioned above (Kaplan & Lake, 2008). Hence, other creative methods of “exposure” to CAP patients should be incorporated into teaching rotations to offer medical students the opportunities to expand this knowledge base, apply the knowledge to practice scenarios, and further their clinical and communication skills. Small group sessions such as the CVTs and OCITs are teaching activities that can be used to overcome some of these challenges.
Our study showed that small group interactive teaching is effective in helping medical students to apply what they have learnt about CAP, increase their confidence in speaking to adolescents as patients and learn psychiatric interviewing skills. It also exposes them to a wide range of relevant CAP cases to which they can apply their theoretical knowledge and practice interview and management techniques. Furthermore, we have found that all this can be adequately achieved in a tailored environment that is conducive for learning. The collective constructive feedback had been used to further improve the content and deliverability style so as to enhance implementation in future batches. It has also been conceptualised to compare CVT and OCIT as individual teaching methods for future scholarly research.
V. CONCLUSION
The CAP small group interactive teaching sessions for medical students received good feedback from majority of the participants. This positive validation would spur the authors on to explore further how this pedagogy could help spark interests in Child and Adolescent Psychiatry among medical students given the shortfall of child and adolescent psychiatrists worldwide.
Notes on Contributors
AHYL analysed and interpreted data. CHJW, together with TJY and JCMW planned and conducted the child psychiatry small group teaching and collected feedback data from the medical students. TJY developed the feedback questionnaire. YSL, together with AHYL, CHJW and TTC planned and wrote the manuscript. All authors read and approved the final manuscript.
Ethical Approval
NHG DSRB reference number 2019/00431 for exemption.
Data Availability
Datasets generated and/or analysed during the current study are available from corresponding author on reasonable request.
Acknowledgements
The authors wish to thank the team from Centre for Healthcare Simulation, Yong Loo Lin School of Medicine, National University of Singapore for the invaluable support in recruiting and training the simulated patients for the CAP teaching program. We appreciate the participation of the simulated patients and medical students in the teaching programme.
Funding
There is no funding for this paper.
Declaration of Interest
As far as all the authors are concerned, we do not know of, or foresee any future competing interests. We are not aware of any issues relating to journal policies in submitting this manuscript. All the authors have approved of the manuscript for submission. The authors declare that they have no competing interests.
References
Baranne, M. L., & Falissard, B. (2018). Global burden of mental disorders among children aged 5–14 years. Child and Adolescent Psychiatry and Mental Health, 12(1), 19.
Breton, J. J., Plante, M. A., & St-Georges, M. (2005). Challenges facing child psychiatry in Quebec at the dawn of the 21st Century. The Canadian Journal of Psychiatry, 50(4), 203-212.
Costello, E. J., Egger, H., & Angold, A. (2005). 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. Journal of the American Academy of Child & Adolescent Psychiatry, 44(10), 972-986.
Dingle, A. D. (2010). Child psychiatry: What are we teaching medical students? Academic Psychiatry, 34(3), 175-182.
Erskine, H. E., Moffitt, T. E., Copeland, W. E., Costello, E. J., Ferrari, A. J., Patton, G., … & Scott, J. G. (2015). A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychological Medicine, 45(7), 1551-1563.
Hunt, J., Barrett, R., Grapentine, W. L., Liguori, G., & Trivedi, H. K. (2008). Exposure to child and adolescent psychiatry for medical students: Are there optimal “teaching perspectives”?. Academic Psychiatry, 32(5), 357-361.
Kaplan, J. S., & Lake, M. (2008). Exposing medical students to child and adolescent psychiatry: A case-based seminar. Academic Psychiatry, 32(5), 362-365.
Kyu, H. H., Pinho, C., Wagner, J. A., Brown, J. C., Bertozzi-Villa, A., Charlson, F. J., … & Fitzmaurice, C. (2016). Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: Findings from the global burden of disease 2013 study. JAMA Pediatrics, 170(3), 267-287.
Lim, C. G., Ong, S. H., Chin, C. H., & Fung, D. S. S. (2015). Child and adolescent psychiatry services in Singapore. Child and Adolescent Psychiatry and Mental Health, 9(1), 7.
Malloy, E., Hollar, D., & Lindsey, B. A. (2008). Increasing interest in child and adolescent psychiatry in the third-year clerkship: Results from a post-clerkship survey. Academic Psychiatry, 32(5), 350-356.
Martin, V. L., Bennett, D. S., & Pitale, M. (2005). Medical students’ perceptions of child psychiatry: Pre-and post-psychiatry clerkship. Academic Psychiatry, 29(4), 362-367.
Plan, S. (2002). A Call to Action: Children Need Our Help! American Academy of Child & Adolescent Psychiatry. Retrieved from https://www.aacap.org/app_themes/aacap/docs/resources_for_primary_care/workforce_issues/AACAP_Call_to_Action.pdf
Sawyer, M., & Giesen, F. (2007). Undergraduate teaching of child and adolescent psychiatry in Australia: Survey of current practice. Australian & New Zealand Journal of Psychiatry, 41(8), 675-681.
Thomas, C. R., & Holzer, C. E., 3rd (2006). The continuing shortage of child and adolescent psychiatrists. Journal of the American Academy of Child & Adolescent Psychiatry, 45(9), 1023-1031.
World Health Organization. (2014). Adolescent health epidemiology. Retrieved from http://www.who.int/maternal_child_adolescent/epidemiology/adolescence/en/
*Yit Shiang Lui
1E Kent Ridge Road
Tower Block, Level 9,
Singapore 119228
Tel: 6772 6331
Email address: yit_shiang_lui@nuhs.edu.sg
Submitted: 14 February 2020
Accepted: 1 July 2020
Published online: 5 January, TAPS 2021, 6(1), 40-48
https://doi.org/10.29060/TAPS.2021-6-1/OA2227
Shirley Beng Suat Ooi1,2, Clement Woon Teck Tan3,4 & Janneke M. Frambach5
1Emergency Medicine Department, National University Hospital, National University Health System, Singapore; 2Department of Surgery, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Department of Ophthalmology, National University Hospital, National University Health System, Singapore; 4Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 5School of Health Professions Education, Faculty of Health, Medicine and Life Sciences, Maastricht University, The Netherlands
Abstract
Introduction: Almost all published literature on effective clinical teachers were from western countries and only two compared medical students with residents. Hence, this study aims to explore the perceived characteristics of effective clinical teachers among medical students compared to residents graduating from an Asian medical school, and specifically whether there are differences between cognitive and non-cognitive domain skills, to inform faculty development.
Methods: This qualitative study was conducted at the National University Health System (NUHS), Singapore involving six final year medical students at the National University of Singapore, and six residents from the NUHS Residency programme. Analysis of the semi-structured one-on-one interviews was done using a 3-step approach based on principles of Grounded Theory.
Results: There are differences in the perceptions of effective clinical teachers between medical students and residents. Medical students valued a more didactic spoon-feeding type of teacher in their earlier clinical years. However final year medical students and residents valued feedback and role-modelling at clinical practice. The top two characteristics of approachability and passion for teaching are in the non-cognitive domains. These seem foundational and lead to the acquisition of effective teaching skills such as the ability to simplify complex concepts and creating a conducive learning environment. Being exam-oriented is a new characteristic not identified before in “Western-dominated” publications.
Conclusion: The results of this study will help to inform educators of the differences in a learner’s needs at different stages of their clinical development and to potentially adapt their teaching styles.
Keywords: Clinical Teachers, Medical Students, Residents, Cognitive/Non-Cognitive, Asian Healthcare, Faculty Development
Practice Highlights
- Approachability and teaching passion are foundational non-cognitive skills in effective clinical teachers.
- These foundational skills are more important for undergraduate than postgraduate teaching.
- Procedural residents can accept less ‘warm’ teachers if they can learn advanced clinical skills.
- Medical students value didactic ‘spoon-feeding’ type of teachers in their earlier clinical years.
- Final year medical students and residents value feedback and role-modelling at clinical practice.
I. INTRODUCTION
“The transformation of our students requires the engagement of innovative and outstanding clinician-teachers who not only supervise students in their development of technical skills and applied knowledge but also serve as role models of the values and attributes of the profession and of the life of a professional” (Sutkin, Wagner, Harris, & Schiffer, 2008). This statement nicely encapsulates the very important role played by outstanding clinical teachers in helping students to ultimately become professionals with the attributes our healthcare system desires. Previous research has extensively investigated characteristics of effective clinical teachers to inform faculty development (e.g. Branch, Osterberg, & Weil, 2015; Hatem et al., 2011; Hillard, 1990; Kernan, Lee, Stone, Freudigman, & O’Connor, 2000; Paukert & Richards, 2000; Singh et al., 2013; Sutkin et al., 2008; White & Anderson, 1995). However, despite the large body of existing research on effective clinical teaching, two issues related to the needs of different groups of learners need further investigation to enable more tailored faculty development.
First, effective clinical teaching may look different in undergraduate as compared with postgraduate education. In many healthcare institutions, clinical teachers are expected to teach across the medical education continuum, i.e., undergraduate medical students, graduate doctors in training, as well as part of continuing medical education, and teaching abilities are a necessary prerequisite in an academic environment (Hatem et al., 2011). Based on the conceptual framework of constructivism (Bednar, Cunningham, Duffy, & Perry, 1991)—a theory which equates learning with creating meaning from experience or contextual learning—Jonassen (1991) argues that constructive learning environments are most effective for acquiring knowledge in the advanced stage of knowledge, the stage between introductory and expert. According to Jonassen (1991), the initial or introductory stage of knowledge acquisition occurs when learners have very little directly transferable prior knowledge about a skill or content area. In this stage, knowledge is best acquired through more objectivistic approaches which can be described as ‘spoon-feeding’. Medical students in general would fit into this introductory stage, in varying degrees depending on their seniority and individual progress in learning. Jonassen’s (1991) second stage is advanced knowledge acquisition where the domains are ill-structured and more knowledge-based. This is in contrast to his third or final stage of knowledge acquisition of experts that require very little instructional support but are able to deal with elaborate structures, schematic patterns and seeing the interconnectedness in knowledge through experience. The stage of junior doctors in training would be fit into the second or advanced stage of learning. Constructivist teachers help students construct knowledge to become active learners rather than passive recipients of knowledge from the teachers or textbooks. In view of this constructivist framework, it appears logical to postulate that as medical students mature to become practicing doctors, their perceptions of effective clinical teachers may change from one who ‘spoon-feeds’ them with medical knowledge to one who encourages them to actively construct new meaning as they become clinically more experienced and have to deal with complex and ill-defined problems. Low, Khoo, Kuan, and Ooi (2020) showed that although the top four characteristics of effective medical teachers are consistent across all 5 years of medical school, characteristics that facilitate active learner participation are emphasised in the clinical years consistent with constructivist learning theory. However, as there is a paucity of comparative research on perceptions of effective clinical teachers among undergraduates as compared to postgraduates to plan more focused faculty development to address the attributes the learners look for in their clinical teachers, this warrants further research.
The second issue relates to potential differences in the clinical teaching role between Asian and Western settings. In Western studies, as noted above, effective clinical teachers are encouraged to stimulate students’ intellectual curiosity leading to more self-directed learning (Hillard, 1990; Kernan et al., 2000; White & Anderson, 1995). In contrast, feelings of uncertainty about the independence required in self-directed learning, a focus on tradition that respects ‘old ways’, hierarchy expecting ‘truths’ to come from persons of higher status, and an achievement orientation to pass and excel in examinations have been identified as more prominent in non-Western than in Western cultures (Frambach, Driessen, Chan, & van der Vleuten, 2012). This is despite the recent introductions of more student-centred education methods. In Singapore for example, there is a move in the Yong Loo Lin School of Medicine (YLLSoM) to try to embed students into healthcare teams (Jacobs & Samarasekera, 2012) and implement newer methods of learning such as flipped classroom. However, many teachers still employ traditional methods of lectures and small group tutorials focused on exam preparation. A comprehensive review study of 68 articles on effective clinical teaching (Sutkin et al., 2008), comprised only one article that reported research from a non-Western setting (Elzubeir & Rizk, 2001). In this article, originating from the United Arab Emirates, there is no discussion on whether there is a difference in the perception of a role model between medical students in Asian countries compared to the West (Elzubeir & Rizk, 2001). Another study conducted in Asia showed differences in the perceptions of first-year and fifth-year medical students in Singapore on what makes an effective medical teacher (Kua, Voon, Tan, & Goh, 2006). More first-year students preferred handouts in contrast to fifth-year students who were less reliant on ‘spoon-feeding’. Research on effective clinical teaching is growing in the Asian setting (Ciraj et al., 2013; Haider, Snead, & Bari, 2016; Kikukawa et al., 2013; Mohan & Chia, 2017; Nishiya et al., 2019; Venkataramani et al., 2016) though there is still a paucity of literature in the Asian setting compared with studies conducted in the West and there are none that directly compared medical students with residents.
Another issue that deserves further attention is the role of non-cognitive domain skills in clinical teaching. Sutkin et al.’s (2008) review study described three main categories of characteristics of good clinical teachers: 1) physician characteristics, 2) teacher characteristics, and 3) human characteristics (Table 1). Approximately two-thirds of the characteristics were in non-cognitive domains (such as those involving relationship skills, emotional states, and personality types), and one-third in cognitive domains (such as those involving reasoning, memory, judgment, perception, and procedural skills). The article noted that cognitive abilities can be taught and learned, in contrast to non-cognitive attributes which are more difficult to develop and teach. Faculty development programmes currently often focus on traditional cognitive skills, such as curriculum design, large-group teaching, and assessment of learners (Searle, Hatem, Perkowski, & Wilkerson, 2006). In contrast, if non-cognitive domains are more important in contributing to outstanding teaching, they might need greater emphasis in the curricula of these workshops. The good news is that according to Schiffer, Rao, and Fogel (2003), non-cognitive behaviours are both measurable and alterable. Most of them have underlying neural networks which are entering our sphere of understanding. Hence non-cognitive skills, although much more challenging to develop than cognitive skills, have a potential to be developed. It is not clear whether there are differences in the distribution between cognitive and non-cognitive domains skills between the perceptions of medical students compared to residents of an effective clinical teacher.
The aim of this qualitative study is to explore the perceived characteristics of an effective clinical teacher among medical students compared to residents graduating from an Asian medical school and whether there is a difference regarding cognitive and non-cognitive domain skills.
II. METHODS
A. Participants
The participants consisted of final/fifth year medical students (M5s) from the Yong Loo Lin School of Medicine (YLLSoM), National University of Singapore (NUS) who were posted to the National University Hospital (NUH) to do their student internship posting in 2016. To ensure sufficient working experience, the National University Health System (NUHS) residents who had graduated from the YLLSoM and who had recently completed their intermediate specialty examinations were recruited. These were third to fifth year residents in different programmes. Maximal variation sampling of the M5s and the residents of both gender, different ethnic groups and from different specialties (for residents only) was done.
B. Design
A pragmatic qualitative research design (Savin-Baden & Howell Major, 2013) was used to get the participants to reflect on their own learning journey affecting their perceptions of the qualities that make an effective clinical teacher from the time they were first exposed to clinical medicine in year 3 (M3) of medical school to final year (M5) for the students, and to residency for the residents.
C. Data Collection
Semi-structured one-on-one interviews using open-ended questions were conducted. A list of M5s doing their student internship programme in the various departments in NUH was invited via an e-mail invitation to participate in this study. To ensure maximal variation sampling, M5s of both gender and as far as possible different ethnic groups were recruited. As for the residents, through the Graduate Medicine Education Office in NUH, residents of both gender, from different ethnic groups and different specialties (both procedural and non-procedural) were selected from those who responded voluntarily to the invitation to participate in this study to ensure maximal variation sampling as residents from procedural specialties may have different perceptions of effective clinical teachers from non-procedural specialties.
Written consent after reading the Participant Information Sheet was taken from the interviewees before the interview was conducted in a quiet room. The interview was audiotaped and lasted between 30 and 45 minutes.
D. Data Analysis
The audiotaped interviews were transcribed. As all the 12 interviews were conducted by the principal investigator (PI) (SO) and although the coding and official analysis of the interviews were done after all the 12 interviews were transcribed, the PI had taken note of themes emerging and decided on ending the interviews after no substantial new themes had emerged.
In the first phase, open coding, initial categories of the information on characteristics of effective clinical teachers by segmenting information and assigning open codes were formed. In the second coding phase, broader categories were developed through conceptually related ideas. The third phase involved selective coding where the individual categories were counterchecked with Sutkin et al.’s (2008) categories of teacher, physician and human characteristics and whether they were in the cognitive or non-cognitive domains (Table 1). Further related categories according to Sutkin et al.’s (2008) classification were brought together.
Physician Characteristics
|
P1 |
Demonstrates medical/clinical knowledge |
|
P2 |
Demonstrates clinical and technical skills/competence, clinical reasoning |
|
P3 |
Shows enthusiasm for medicine |
|
P4 |
A close doctor-patient relationship |
|
P5 |
Exhibits professionalism |
|
P6 |
Is scholarly (does research) |
|
P7 |
Values teamwork and has collegial skills |
|
P8 |
Is experienced |
|
P9 |
Demonstrates skills in leadership and /or administration |
|
P10 |
Accepts uncertainty in medicine |
|
P11 |
Others |
Teacher Characteristics
|
T1 |
Maintains positive relationships with students and a supportive learning environment |
|
T2 |
Demonstrates enthusiasm for teaching |
|
T3 |
Is accessible/available to students |
|
T4 |
Provides effective explanations, answers to questions, and demonstrations |
|
T5 |
Provides feedback and formative assessment |
|
T6 |
Is organized and communicates objectives |
|
T7 |
Demonstrates knowledge of teaching skills, methods, principles, and their application |
|
T8 |
Stimulates students’ interest in learning and/or subject |
|
T9 |
Stimulates or inspires trainees’ thinking |
|
T10 |
Encourages trainees’ active involvement in clinical work |
|
T11 |
Provides individual attention to students |
|
T12 |
Demonstrates commitment to improvement of teaching |
|
T13 |
Actively involves students |
|
T14 |
Demonstrates learner assessment/evaluation skills |
|
T15 |
Uses questioning skills |
|
T16 |
Stimulates trainees’ reflective practice and assessment |
|
T17 |
Teaches professionalism |
|
T18 |
Is dynamic, enthusiastic, and engaging |
|
T19 |
Emphasizes observation |
|
T20 |
Others |
Human Characteristics
|
H1 |
Communication skills |
|
H2 |
Acts as role model |
|
H3 |
Is an enthusiastic person |
|
H4 |
Is personable |
|
H5 |
Is compassionate/emphathetic |
|
H6 |
Respect others |
|
H7 |
Displays honesty |
|
H8 |
Has wisdom, intelligence, common sense, and good judgement |
|
H9 |
Appreciates culture and different cultural backgrounds |
|
H10 |
Consider other’s perspectives |
|
H11 |
Is patient |
|
H12 |
Balances professional and personal life |
|
H13 |
Is perceived as a virtuous person and a globally good person |
|
H14 |
Maintains health, appearance, and hygiene |
|
H15 |
Is modest and humble |
|
H16 |
Has a good sense of humour |
|
H17 |
Is responsible and conscientious |
|
H18 |
Is imaginative |
|
H19 |
Has self-insight, self-knowledge, and is reflective |
|
H20 |
Is altruistic |
|
H21 |
Others |
Note: Italics denotes cognitive characteristics; Bold denotes non-cognitive characteristics.
Table 1. Classification of characteristics of outstanding clinical teachers (Sutkin et al., 2008)
E. Trustworthiness
To enhance the credibility of the research, member checking on the accuracy of interview transcription was done. The same transcription was coded by the PI (SO) and a co-researcher (CT) and the themes and differences were discussed and resolved together. The themes were then discussed with another co-researcher (JF) who is an outsider to the research setting. To contribute to the dependability of the data, a reflexivity diary was kept to reflect on the process and the PI’s role and influence on this study. This is because the PI is the person overall in charge of the residency training and has vast experience in teaching both undergraduate and postgraduate learners and has observed undergraduates seemingly valuing the willingness of time spent teaching in contrast to postgraduate learners who value effective teaching on the job. The PI emphasised to participants that whatever they mentioned in this study would not affect them in any way in their assessments, selection into a residency programme, job selection nor career progression. As a point of note, none of the interviewees mentioned any of the authors by name in the interviews when describing an effective clinical teacher.
III. RESULTS
A total of six final year medical students from the YLLSoM consisting of three males and three females with a mean age of 23 years old were interviewed. As for the residents group, they consisted of four males and two females. There were two internal medicine year 3 residents, one paediatric year 5 resident, one emergency medicine year 4 resident, one orthopaedic year 3 resident and one urology year 4 resident with a mean age of 29 years (range 26-33 years). All of them were of Chinese ethnicity.
The characteristics of effective teachers were mapped onto Sutkin et al.’s (2008) review paper (Table 1) and while the majority of the characteristics could be mapped, those characteristics not able to be mapped would be considered as new characteristics. Referring to the summary of results in Table 2, the top characteristic identified equally by the medical students and residents group was approachability, in the non-cognitive domain. This was described as being “relatable, personable, forming good rapport, warm, able to remember students’ names, having a sense of humour, sharing personal experience”. Medical student 2 aptly described its importance: “Approachability in being willing to teach is an inborn trait. It acts as a screening tool. It opens the door for a student to decide whether or not this clinical tutor is someone she is likely to approach to learn from.” Interestingly, while both the medical students and residents group unanimously identified the need for a clinical teacher to have a threshold level of clinical competence, followed by a teacher who is warm and approachable with a passion to teach, this latter requirement was emphasised as particularly important in undergraduate teaching. In contrast, a postgraduate trainee/resident was able to accept a less warm but skillful clinician to learn advanced surgical skills from as they were more able to do self-directed learning being already in a training programme and they could observe and learn.
|
Total |
MS |
R |
Characteristics |
Teacher |
Physician |
Human |
Cognitive |
Non-Cognitive |
|
10 |
5 |
5 |
Approachability |
X (T3) |
|
X (H4) |
|
x |
|
9 |
3 |
6 |
Passion/enthusiasm in teaching/engaging |
X (T2) |
|
|
|
x |
|
8 |
5 |
3 |
Provide effective explanations, answers to questions, and demonstrations (T4) Demonstrate clinical and technical skills/competence, clinical reasoning (P2) |
X (T4) |
X (P2) |
|
x |
|
|
7 |
3 |
4 |
Creates conducive learning environment
|
X (T1) |
|
X (H11, H15) |
|
x |
|
7 |
3 |
4 |
Role modeling
|
x |
x |
X (H1, H6) |
|
x |
|
7 |
2 |
5 |
Teach at appropriate level/know learning objectives |
X (T6) |
|
|
x |
|
|
7 |
3 |
4 |
Sacrifice time |
x |
|
|
x |
|
|
6 |
3 |
3 |
Realistic/concrete learning |
X (T6) |
|
|
x |
|
|
6 |
2 |
4 |
Feedback, supervision, assessment for learning |
X (T5, T19) |
|
|
x |
|
|
5 |
2 |
3 |
Knowledgeable/up to date/evidence-based |
|
X (P1) |
|
x |
|
|
5 |
4 |
1 |
Exam-oriented |
x |
|
|
x |
|
|
4 |
2 |
2 |
Inspirational to learning |
X (T8, T9, T18) |
|
|
|
x |
|
4 |
1 |
3 |
Clinical thinking/Demonstrate to impart/pedagogy |
X (T9) |
X (P2) |
|
x |
|
|
3 |
2 |
1 |
Nurturing/encouraging/compassion for students & team |
X (T11) |
|
X |
|
x |
|
2 |
0 |
2 |
Allows hands-on/encourages trainees active involvement in clinical work |
X (T10) |
|
|
|
x |
|
|
|
|
Others: Strict, elocution, fair/moral compass (H13, H7), innovative (T12), directs learners, worldly-wise; empathy (H5), interpersonal skills, humour (H16) |
|
|
|
|
|
Note: (T), (P) and (H) refer to the specific Sutkin et al.’s (2008) classification as given in Table 1.
Table 2. Characteristics of effective teachers identified by Medical Students (MS) and Residents (R) classified into teacher, physician and human characteristics and cognitive vs non-cognitive domains and mapped onto Sutkin et al.’s (2008) Classification (Table 1)
The second most important characteristic identified was having a passion/enthusiasm in teaching, in the non-cognitive domain. This was described as “engaging, enthusiastic to help residents learn, enthusiasm/infectious attitude rubs off, lively, draws out from learners, takes time to explain to students”. Resident 5 explained: “Passion is actually demonstrated in the knowledge you display. Because when you are interested in something, you can go on to explore the depth. People who display passion are able to depict the subject matter in a very interesting, personal and in a lively way. Passion is also about the desire to learn about things and to contribute to things. So in a sense teaching is not a passive tool for the diffusion of students … it’s also the ability to be able to draw things out from the students …draw contribution or ideas…”. Passion as a characteristic was mentioned by all the residents but not by all of the medical students.
The third most important characteristic identified can be summarised as “providing effective explanations, answers to questions, and demonstrations” (a teacher characteristic) and “demonstrates clinical and technical skills/competence, clinical reasoning” (a physician characteristic) in the cognitive domain. This was described as “being able to break down concepts into digestible chunks; being able to synthesise and teach in understandable way; how to think, synthesise and use information; concise, targeted, clear thinking; headings, subheadings, elaborations; clarity in giving instructions and thought so that everyone is on the same page; demonstrate better way of presenting and more accurate way of physical examination”. This was identified more in the medical student group than in the resident group.
Most of the other characteristics generally coincided with Sutkin et al.’s (2008) paper. Among the two cognitive domains skills were “teaching at appropriate level/knowing learning objectives” as well as being willing to “sacrifice time” demonstrating commitment for student education. The teachers who sacrificed their time gave additional teaching sessions and did not rush through. The medical students and the residents identified this characteristic as something they really valued in undergraduate teaching. Another characteristic in the cognitive domain was “Realistic/concrete learning” was described as “bedside teaching; teaching with practical aspect, case-based teaching; use of clinical pictures, electrocardiogram, clinical quiz and learning aids”. This form of learning was identified as being effective by both the medical students and residents equally. In contrast, “feedback, supervision, assessment for learning” described as “being able to discuss in detail as physically present; balance between supervision and resisting urge to take over in an operation; good feedback with balance of positive and negative points done in a fun and nice way” was identified more by the residents than the medical students group.
Being “exam-oriented” i.e., the teacher being able to prepare the students well for exams, was notably a characteristic identified mainly by the medical students but was one not identified at all in Sutkin et al.’s (2008) paper nor other more recent references. To quote medical student 1, “I guess especially for medical students, it is whether this tutor prepares us well for the exams and in terms of meeting our academic objectives.” Medical student 5: “He teaches us very exam focused and he synthesises all the information very succinctly for exams.”
The medical students were specifically asked whether they identified a difference in the characteristics they valued in their teachers between when they were first introduced to clinical medicine in M3 compared to now in M5. The students almost unanimously expressed that in M3, as they had just been exposed to clinical medicine, they identified the need to build up their medical knowledge through more content-heavy didactic style of teaching that could be described as more of spoon-feeding than self-directed learning. Medical student 5 said, “Year 3 is more introductory kind of year so we don’t know anything. So what a good tutor to me in year 3 was whoever can teach me approaches, impart didactic teachings like knowledge.” They valued connections back to the basic sciences taught in their first two years of medical school and teachers who taught them how to approach patients. They were open to the gradual introduction of self-directed learning but it should not hold up the pace of the lesson if the students were unable to answer. In contrast, at the time of interview they were in M5 and they had two main aims. Their first aim was to look for good role-models for their upcoming internship and choice of residency for some. Hence, they appreciated bedside teaching with close supervision and feedback on medical knowledge applied to actual clinical care. Moreover, bedside examination skills and patient communications cannot be studied at home. At M5, they valued more self-directed learning as they were more equipped to search for information themselves unlike when they were in M3. They also greatly valued preparation for their final exams which would involve clinical examination in the form of Objective Structured Clinical Examination. In this aspect, they valued teachers who could teach them clinical reasoning on how to synthesise information to be applied to management of actual patients. The second aim had become more important as their final exams drew near. This feedback was also expressed by the residents when they recalled on what they looked for in their undergraduate years.
For the residents who were in their third year of their residency and beyond, they identified the need for more active, self-directed learning. They mentioned the need to ask the ‘why questions’ and to learn evidence-based clinical practice. They appreciated experienced tutors who shared pearls and personal experience with them. They preferred to learn from good teachings during ward rounds and clinics and mentioned that didactic teaching was less important unlike in their undergraduate days and also as a first year resident where they still appreciated more spoon-feeding. As a more senior resident, they found discussions, greater analysis, asking questions to identify knowledge gaps, opportunity to present and testing useful because they already had a fund of medical knowledge.
IV. DISCUSSION
The results of this study suggest that there are differences in the perceived characteristics of an effective clinical teacher among medical students compared to residents. The results support Jonassen’s theory of constructivism (1991) as seen by the medical students at the beginning of their clinical year (M3) wanting more didactic teaching to ‘spoon-feed’ them with medical knowledge. As these students move on to become more senior in M5, and then residency, they start appreciating teachers who help them become more self-directed learners. These more senior learners also value feedback to help them deal with more complex ill-defined problems that they encounter during their daily clinical work. This is supported by more residents than medical students identifying feedback and supervision as well as clinical decision making/thinking as important characteristics of an effective clinical teacher (Table 2).
It is also interesting to note that the top two characteristics of approachability and passion/enthusiasm in teaching are both in the non-cognitive domains. In fact, they are probably fundamental attributes that make a good teacher into a great one as they lead to a lot of teaching experience coupled with feedback from the learners that make them become good at simplifying and explaining concepts well, especially in undergraduate teaching. For the students beyond a baseline clinical competence, they value clinical teachers who want to teach rather than those who may be excellent top clinicians who do not possess the soft skills and the approachability for the students to want to have the courage to learn effectively from him/her. In contrast, the residents are willing to accept less ‘warm’ teachers if they are able to learn advanced clinical skills from them, particularly in the procedural specialties.
One of the characteristics that has not been identified in any of the references, including Sutkin et al.’s (2008) review paper is that of being exam-oriented. This was a characteristic identified by four of the medical students but only by one of the residents who mentioned it while recalling his undergraduate days. This is not too surprising because Frambach et al. (2012) have found that Asian students tend to strive for success and to rank among the top achievers in an examination. The fact that the YLLSoM is Asia’s leading medical school (QS Top Universities, 2015; Times Higher Education, 2015) and hence the crème de la crème of Singapore’s students study at YLLSoM as seen by both the 10th and 90th percentiles of Medical students getting all A grades in their Singapore-Cambridge GCE A-level admission scores (National University of Singapore, 2019) can explain the exam-orientedness of the students. Moreover, Singapore practices meritocracy (Prime Minister’s Office, 2015) and in a small country of only 719.1 km² with a population of 5.35 million (World Bank, 2015) with only three public healthcare clusters, doing well in exams is seen as a tried and tested way of securing a good future. Failing in a high-stakes exam such as the final Bachelor of Medicine and Bachelor of Surgery (MBBS) exams will delay one’s progression to the next stage of one’s career such as admission to a residency training programme, and in a small country like Singapore where it is perceived to have few opportunities of starting afresh, it is not surprising that so much emphasis is placed on doing well in exams and a teacher who is able to prepare students well for exams is greatly valued.
There are several limitations to this study. Although we had wanted to recruit interviewees from different ethnicity, all 12 who responded to our invitation were Chinese, though participating in a multi-cultural and multi-ethnic public school. Another limitation is that this study only explores the perceptions of the learners themselves. It will be more balanced if the viewpoints of the teachers are obtained as well.
V. CONCLUSION
This study suggests that there are differences in the perceptions of an effective clinical teacher between medical students compared to residents. Medical students valued a more didactic spoon-feeding type of teacher in their earlier clinical years. However, final year medical students and residents valued feedback and role-modelling at clinical practice. The top two characteristics of approachability and passion for teaching are in the non-cognitive domains. The results of this study will help to inform educators of the differences in a learner’s needs at different stages of their clinical development and to potentially adapt their teaching styles. In addition, it is also possible for certain non-cognitive domain skills to be developed through recognition of clinical teachers who are role models in showing by example the art of the practice of Medicine and being able to create a conducive non-threatening learning environment. There are definitely faculty development programmes which target at how to develop a conducive learning environment.
Notes on Contributors
Shirley Ooi, MBBS(S’pore), FRCSEd(A&E), MHPE(Maastricht) is senior consultant emergency physician at NUH and associate professor at NUS. She was the Designated Institutional Official NUHS Residency programme at the time of the study. Currently she is the Associate Dean at NUH. This study was her MHPE thesis. She reviewed the literature, designed the study, conducted the interviews, analysed the transcripts and wrote the manuscript.
Clement Tan, MBBS(S’pore), FRCSEd (Ophth), MHPE(Maastricht), is associate professor, senior consultant and head of the Department of Ophthalmology, NUS and NUH. He was the first author’s local MHPE thesis supervisor. He co-analysed the transcripts and approved the final versions of the manuscripts.
Janneke M. Frambach PhD is assistant professor at the School of Health Professions Education, Faculty of Health, Medicine and Life Sciences, Maastricht University, the Netherlands. She was the first author’s MHPE thesis supervisor. She supervised the study from the beginning to the final stage of manuscript writing with its revisions.
Ethical Approval
This study was reviewed and approved by the NUS Institutional Review Board (approval no. 3172), which considered the letter of invitation for recruitment of participants, participant information sheet, written informed consent for the audio-recordings of the one-on-one interviews, interview guide and confidentiality of participants.
Acknowledgements
The authors would like to thank the following for their help, advice and support, without which this study would not have been possible:
- Medical student, Gerald Tan, for his help in transcribing many of the interviews.
- The six YLLSoM medical students who had willingly come forward to be interviewed for this study.
- The six NUHS residents who had willingly spared their time to be interviewed for this study.
Funding
No grant nor external funding was received for this study.
Declaration of Interest
The PI as the interviewer emphasised to the participants that whatever they mentioned in this study would not affect them in any way in their assessments, selection into a residency programme, job selection nor career progression. Moreover, their participation was entirely voluntary. The other two authors had no conflict of interest.
References
Bednar, A. K., Cunningham, D., Duffy, T. M., & Perry, J. D. (1991). Theory into practice: How do we link? In G.J. Anglin (Ed.), Instructional Technology: Past, Present, and Future. Englewood, CO: Libraries Unlimited.
Branch, W. T., Osterberg, L., & Weil, R. (2015). The highly influential teacher: Recognising our unsung heroes. Medical Education, 49, 1121-27.
Ciraj, A., Abraham, R., Pallath, V., Ramnarayan, K., Kamath, A., & Kamath, R. (2013). Exploring attributes of effective teachers-student perspectives from an Indian medical school. South-East Asian Journal of Medical Education, 7(1), 8-13.
Elzubeir, M. A., & Rizk, D. E. E. (2001). Identifying characteristics that students, interns and residents look for in their role models. Medical Education, 35, 272-277.
Frambach, J. M., Driessen, E. W., Chan, L. C., & van der Vleuten, C. P. M. (2012). Rethinking the globalization of problem-based learning: How culture challenges self-directed learning. Medical Education, 46, 738-747.
Haider, S. I., Snead, D. R., & Bari, M. F. (2016). Medical students’ perceptions of clinical teachers as role model. PloS ONE, 11(3): e0150478. https://doi:10.1371/journal.pone.0150478
Hatem, C. J., Searle, N. S., Gunderman, R., Krane, N. K., Perkowski, L., Schutze, G. E., & Steinert, Y. (2011). The educational attributes and responsibilities of effective medical educators. Academic Medicine, 86(4), 474-480.
Hillard, R. I. (1990). The good and effective teacher as perceived by paediatric residents and faculty. American Journal of Diseases of Childhood, 144, 1106 –1110.
Jacobs, J. L., & Samarasekera, D. D. (2012). How we put into practice the principles of embedding medical students into healthcare teams. Medical Teacher, 34, 1008-1011.
Jonassen, D. H. (1991). Evaluating constructivistic learning. Educational Technology, 31(9), 28-33.
Kernan, W. N., Lee, M. Y., Stone, S. L., Freudigman, K. A., & O’Connor, P. G. (2000). Effective teaching for preceptors of ambulatory care: A survey of medical students. American Journal of Medicine, 108(6), 499-502.
Kikukawa, M., Nabeta, H., Ono, M., Emura, S., Oda, Y., Koizumi, S., & Sakemi, T. (2013). The characteristics of a good clinical teacher as perceived by resident physicians in Japan: A qualitative study. BMC Medical Education, 13(1), 100.
Kua, E. H., Voon, F., Tan, C. H., & Goh, L. G. (2006). What makes an effective medical teacher? Perceptions of medical students. Medical Teacher, 28(8), 738-741.
Low, M. J. W., Khoo, K. S. M., Kuan, W. S., & Ooi, S. B. S. (2020). Cross-sectional study of perceptions of qualities of a good medical teacher among medical students from first to final year. Singapore Medical Journal, 61(1), 28-33.
Mohan, N., & Chia, Y. Y. (2017). Our first steps into surgery: The role of inspiring teachers. The Asia-Pacific Scholar, 2(1), 29-30. https://doi.org/10.29060/TAPS.2017-2-1/PV1027
National University of Singapore. (2019). National University of Singapore Undergraduate Programmes Indicative Grade Profile. Retrieved from http://www.nus.edu.sg/oam/gradeprofile/sprogramme-igp.html
Nishiya, K., Sekiguchi, S., Yoshimura, H., Takamura, A., Wada, H., Konishi, E., Saiki, T., Tsunekawa, K., Fujisaki, K., & Suzuki, Y. (2019). Good clinical teachers in Paediatrics: The perspective of paediatricians in Japan. Paediatrics International, 62(5), 549-555.
Prime Minister’s Office. (2010, May 5). “Old and new citizens get equal chance,” says MM Lee. [Press release].
Paukert, J. L., & Richards, B. F. (2000). How medical students and residents describe the roles and characteristics of their influential clinical teachers. Academic Medicine, 75, 843-845.
QS Top Universities. (2015) QS World University Rankings 2015-20116. Retrieved from: https://www.topuniversities.com/university-rankings/world-university-rankings/2015
Savin-Baden, M., & Howell Major, C. (2013). Pragmatic qualitative research. In M. Savin-Baden & C. H. Major (Eds). Qualitative Research. The Essential Guide to Theory and Practice. London: Routledge.
Schiffer, R. B., Rao, S. M., & Fogel, B. S. (2003). Neuropsychiatry: A Comprehensive Textbook (2nd ed.). Philadelphia, PA: Lippincott Williams and Wilkins.
Searle, N. S., Hatem, C. J., Perkowski, L., & Wilkerson, L. (2006). Why invest in an educational fellowship program? Academic Medicine, 81, 936-940.
Singh, S., Pai, D. R., Sinha, N. K., Kaur, A., Soe, H. H. K., & Barua, A. (2013). Qualities of an effective teacher: What do medical teachers think? BMC Medical Education, 13(128), 1-7.
Sutkin, G., Wagner, E., Harris, I., & Schiffer, R. (2008). What makes a good clinical teacher in Medicine? A review of the literature. Academic Medicine, 83(5), 452-466.
Times Higher Education. (2015). The World University Rankings 2015-16. Retrieved from: https://www.timeshighereducation.com/student/news/best-universities-world-revealed-world-university-rankings-2015-2016
Venkataramani, P., Krishnaswamy, N., Sugathan, S., Sadanandan, T., Sidhu, M., & Gnanasekaran, A. (2016). Attributes expected of a medical teacher by Malaysian medical students from a private medical school. South-East Asian Journal of Medical Education, 10(2), 39-45.
White, J. A., & Anderson, P. (1995). Learning by internal medicine residents: Differences and similarities of perceptions by residents and faculty. Journal of General Internal Medicine, 10, 126-132.
World Bank. (2015). Annual Report 2015. Retrieved from: https://www.worldbank.org/en/about/annual-report-2015
*Shirley Ooi
Emergency Medicine Department,
National University Hospital
9 Lower Kent Ridge Road, Level 4,
National University Centre for Oral Health Building,
Singapore 119085
Tel: (65)6772-2458
Fax: (65)6775-8551
Email: shirley_ooi@nuhs.edu.sg
Submitted: 15 April 2020
Accepted: 5 June 2020
Published online: 5 January, TAPS 2021, 6(1), 49-59
https://doi.org/10.29060/TAPS.2021-6-1/OA2248
Amaya Tharindi Ellawala1, Madawa Chandratilake2 & Nilanthi de Silva2
1Department of Medical Education, Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka; 2Faculty of Medicine, University of Kelaniya, Sri Lanka
Abstract
Introduction: Professionalism is a context-specific entity, and should be defined in relation to a country’s socio-cultural backdrop. This study aimed to develop a framework of medical professionalism relevant to the Sri Lankan context.
Methods: An online Delphi study was conducted with local stakeholders of healthcare, to achieve consensus on the essential attributes of professionalism for a doctor in Sri Lanka. These were built into a framework of professionalism using qualitative and quantitative methods.
Results: Forty-six attributes of professionalism were identified as essential, based on Content Validity Index supplemented by Kappa ratings. ‘Possessing adequate knowledge and skills’, ‘displaying a sense of responsibility’ and ‘being compassionate and caring’ emerged as the highest rated items. The proposed framework has three domains: professionalism as an individual, professionalism in interactions with patients and co-workers and professionalism in fulfilling expectations of the profession and society, and displays certain characteristics unique to the local context.
Conclusion: This study enabled the development of a culturally relevant, conceptual framework of professionalism as grounded in the views of multiple stakeholders of healthcare in Sri Lanka, and prioritisation of the most essential attributes.
Keywords: Professionalism, Culture, Consensus
Practice Highlights
- Medical professionalism is recognised as a culturally dependent entity.
- This has led to the emergence of definitions unique to socio-cultural settings.
- List-based definitions provide operationalisable means of portraying its meaning.
- A Delphi study was conducted to achieve consensus on locally relevant professionalism attributes.
- Using quantitative and qualitative methods, a conceptual framework of professionalism was developed.
I. INTRODUCTION
There is no single definition of medical professionalism that encompasses its many subtle nuances (Birden et al., 2014). The realisation that professionalism is a dynamic, multi-dimensional entity (Van de Camp, Vernooij-Dassen, Grol, & Bottema, 2004), significantly dependent on context (Van Mook et al., 2009), and cultural backdrop (Chandratilake, Mcaleer, & Gibson, 2012), has led to the emergence of definitions specific to cultures and socio-economic backgrounds.
Many of the current definitions originate from Western societies. Certain Eastern cultures have embraced such definitions, though they are undeniably in conflict with local traditional views (Pan, Norris, Liang, Li, & Ho, 2013). In parallel however, countries such as Egypt, Saudi Arabia, Japan, China and Taiwan have explored how professionalism is conceptualised within their contexts (Al-Eraky, Chandratilake, Wajid, Donkers, & Van Merrienboer, 2014; Leung, Hsu, & Hui, 2012; Pan et al., 2013). Such studies have portrayed the interplay between cultural, socio-economic and religious factors in shaping perceptions on professionalism, further fuelling the notion that professionalism must be “interpreted in view of local traditions and ethos” (Al-Eraky et al., 2014, p. 14).
Culture is the embodiment of elements such as attitudes, beliefs and values that are shared among individuals of a community and is therefore, an entity that distinguishes one group of people from another (Hofstede, 2011). Various cultural theories provide insight into inter-cultural differences across the globe (Hofstede, n.d.; Schwartz, 1999). The Sri Lankan cultural context, while aligned with those of its closest geographical neighbours in South Asia in some ways, differs from them in other important aspects.
Certain attempts have been made to explore the meaning of professionalism in Sri Lanka. Chandratilake et al. (2012) provided a degree of insight while comparing cultural similarities and dissonances in conceptualising professionalism among doctors of several nations. Monrouxe, Chandratilake, Gosselin, Rees, and Ho (2017) built on this work with their analysis of professionalism as viewed by local medical students. The sole regulatory authority of the medical profession in the country, the Sri Lanka Medical Council (SLMC, 2009) has delineated what it expects in terms of professionalism, by outlining the constituents of ‘good medical practice’, many of which converge with elements of professionalism described in the literature.
While the work mentioned here has shed some light on the topic, to our knowledge, there were no studies that focused solely on the local conceptualisation of professionalism, drawing on the views of diverse stakeholders of healthcare.
There exist two schools of thought on how professionalism can be defined: as a list of desirable attributes (Lesser et al., 2010), or as an over-arching, value-laden entity that transcends such lists (Irby & Hamstra, 2016; Wynia, Papadakis, Sullivan, & Hafferty, 2014). Unlike the latter, a list may not address the “foundational purpose of professionalism” (Wynia et al., 2014, p. 712); however, it will provide a tangible, operationalisable portrayal (Lesser et al., 2010). It is possibly for this reason that many studies have opted for list-based definitions, an approach that is supported in the East (Al-Eraky & Chandratilake, 2012; Al-Eraky et al., 2014; Pan et al., 2013).
The aim of this study was to develop a culturally appropriate conceptual framework of medical professionalism in Sri Lanka using a combination of qualitative and quantitative methods. We envisioned that identifying a list of desirable attributes would be appropriate, providing a definition that could readily be operationalised for teaching/learning, assessment and research purposes (Wilkinson, Wade, & Knock, 2009).
II. METHODS
A. The Approach
We followed a consensus approach, and opted for the Delphi technique as it was imperative to involve a large number of participants not limited by geographical location (Humphrey-Murto et al., 2017). The method offered the further advantage of providing participants with equal opportunity to express their opinions (De Villiers, De Villiers, & Kent, 2005), thereby negating the possible drawbacks of face-to-face interactions and resulting in a ‘process gain’ (Powell, 2003).
B. Participant Panel
The panel comprised nation-wide stakeholders of healthcare (Table 1), from both rural and urban regions who were presumably exposed to diverse forms of medical services and geographical variations in their distribution.
|
Stakeholder group |
Description |
Number |
|
Medical teachers |
Four Medical Faculties (nation-wide) |
69 (44%) |
|
Medical students |
Four Medical Faculties (nation-wide) – fourth and final years |
36 (23%) |
|
Hospital doctors |
Four Teaching Hospitals (nation-wide) |
14 (9%) |
|
Healthcare staff |
Selected secondary and tertiary hospitals |
5 (3%) |
|
General practitioners |
Selected GP practices around the country |
2 (1%) |
|
Medical administrators |
Selected secondary and tertiary hospitals |
5 (3%) |
|
Policy makers in healthcare |
Ministry of Health, professional associations and regulatory bodies |
2 (1%) |
|
General public |
Employees of selected private and state banks Non-academic staff of four Medical Faculties Teachers of selected private and state schools |
25 (16%) |
Table 1. Composition of the Delphi panel
1) Delphi Round I: The question posed in the first round was ‘What are the attributes of professionalism you would expect in a doctor working in the Sri Lankan context?’. No limitation was posed on the number of answers to this open-ended question. This was piloted among a group comprising local medical educationists, medical officers and members of public and edited based on their feedback. Invitations to participate were emailed and informed consent was obtained through an online link. Participants were then automatically granted access to the online questionnaire. An email reminder was sent to the initial mailing list after one week. The questionnaire was accessible for three weeks from the date of launch. Invitations were emailed to 920 individuals, of which 158 (17.2%) responded.
To analyse the data of Round I, we used conventional content analysis, which is employed when literature and theory on a phenomenon is limited, thereby allowing themes to emerge from and be grounded in the data itself (Hsieh & Shannon, 2005). Initially, individual responses – considered as meaning units – were listed out verbatim, removing exact duplicates. Meaning units varied from single word responses to longer phrases, and were therefore divided into short and long meaning units. The latter were shortened into condensed meaning units, while preserving the original meaning. Finally, condensed and short meaning units were coded. Similar phrases were assigned the same code. A final scrutiny of the codes allowed the removal of synonymous items and coupling of items with similar meaning. We followed this process iteratively till the items had been refined to the maximum extent possible.
With two additional experts, we reviewed the appropriateness of items. Four common misconceptions of professionalism (distractors) were added, in order to prevent inattentive responses to the large number of items included in the subsequent round (Meade & Craig, 2012). A search of literature also revealed a number of evidenced-based items that had not emerged in the data. Three of these were agreed to be relevant and important to the local context, and were therefore added to the list, to ensure that a comprehensive coverage of items was achieved.
2) Delphi Round II: The attributes of professionalism were compiled into another online survey and emailed to all individuals initially invited to participate in the study, three weeks after completion of the first round; 118 of the initial sample (dropout rate = 25.3%) participated in Round II. Respondents were asked to rate each item on a five-point Likert scale ranging from ‘not important’ to ‘very important’, according to perceived importance in the local context. An email reminder was sent out after one week. The form was accessible for three weeks.
The aim of this second round was to select the attributes considered most essential. Content Validity Index (CVI) was chosen for this purpose, over less rigorous methods such as prioritisation by mean. The CVI is the proportion of respondents rating an item as essential (Polit & Beck, 2006). Responses ‘4’ and ‘5’of the Likert scale were determined as reflecting ‘essentialness’. The general acceptance is that in a study with a large number of raters (as in this case), a CVI > 0.78 will indicate that an item is essential (Lynn, 1986).
To avoid the possibility of agreement being due to chance, Kappa statistics – a measure of inter-rater agreement and the probability of chance responses – were computed. K-values can range from -1 to +1; -1 indicating perfect disagreement below chance, +1, perfect agreement above chance and 0, agreement equal to chance (Randolph, n.d.). A K-value ≥0.7 indicates acceptable inter-rater agreement.
As the final step, the prioritised list of attributes was emailed to participants requesting further comments; however, none were received. The Delphi study concluded at this stage.
In order to organise the attributes in a more meaningful manner, we attempted to identify the emerging domains of professionalism. Initially this was performed through an Exploratory Factor Analysis, a method which allows identification of underpinning, latent ‘factors’ that are inferred from the variables. Scholars have recommended however, that quantitative analysis of studies with a social science perspective be complemented with qualitative methods (Tavakol & Sandars, 2014). Therefore, a panel of experts individually sorted the attributes into themes using the constant comparison technique; data was sorted, systematically compared and the emergence of a theme was acknowledged when many similar items appeared across the data set (Maykut & Morehouse, 1994). The results were compared with those of the Factor Analysis and by identifying common domains, a final framework of professionalism was formulated. As an additional measure, the internal consistency (Cronbach’s Alpha) within each domain was computed to determine close clustering of items. The framework developed was vetted by a group of reviewers.
III. RESULTS
A. Profile of Participant Panel
The response rates of the different participant groups are depicted in Table 1. As demographic details were not re-obtained in Round II, the profile of this group could not be determined.
B. Results of Round I
A total of 288 items were initially documented, and condensed to 53 attributes following content analysis. The three evidence-based items and four distractors were added to make a final inventory of 60 items (Table 2).
C. Results of Round II
1) Essential Attributes of Professionalism: Forty-six items achieved a CVI > 0.78 and were therefore labelled as ‘essential’. The attributes are arranged in descending order of importance in Table 2. The Kappa value was 0.77, confirming that rating of items was not due to chance.
|
Attribute of professionalism |
CVI |
|
Possessing adequate medical knowledge and skills |
0.99 |
|
Displaying a sense of responsibility |
0.98 |
|
Being compassionate and caring |
0.97 |
|
Managing limited resources for optimal outcome |
0.97 |
|
Ensuring confidentiality and patient privacy |
0.97 |
|
Being punctual |
0.97 |
|
Maintaining standards in professional practice |
0.97 |
|
Displaying effective communication skills |
0.97 |
|
Displaying honesty and integrity |
0.97 |
|
Displaying commitment to work |
0.97 |
|
Being empathetic towards patients |
0.96 |
|
Being able to work as a member of a team |
0.96 |
|
Being reliable |
0.96 |
|
Displaying professional behaviour and conduct |
0.96 |
|
Being accountable for one’s actions and decisions |
0.96 |
|
Being available |
0.95 |
|
Being responsive |
0.95 |
|
Being clear in documentation |
0.95 |
|
Being patient |
0.94 |
|
Displaying effective problem-solving skills |
0.94 |
|
Understanding limitations in professional competence |
0.94 |
|
Being respectful and polite |
0.94 |
|
Ability to effectively manage time |
0.93 |
|
Being a committed teacher/supervisor |
0.92 |
|
Being open to change |
0.92 |
|
Commitment to continuing professional development |
0.91 |
|
Having scientific thinking and approach |
0.91 |
|
Being accurate and meticulous |
0.91 |
|
Maintaining work-life balance |
0.91 |
|
Displaying self confidence |
0.91 |
|
Ability to provide and receive constructive criticism |
0.90 |
|
Non-judgmental attitude and ensuring equality |
0.90 |
|
Engaging in reflective practice |
0.90 |
|
Respecting patient autonomy |
0.90 |
|
Being accessible |
0.88 |
|
Avoiding substance and alcohol misuse* |
0.86 |
|
Working towards a common goal with the health system |
0.85 |
|
Providing leadership |
0.84 |
|
Being humble |
0.84 |
|
Advocating for patients |
0.83 |
|
Maintaining professional relationships |
0.83 |
|
Adhering to a professional dress code |
0.82 |
|
Avoiding conflicts of interest |
0.82 |
|
Displaying sensitivity to socio-cultural and religious issues related to patient care |
0.81 |
|
Being composed |
0.80 |
|
Stands for professional autonomy** |
0.79 |
|
Being amiable |
0.77 |
|
Displaying sensitivity to socio-cultural and religious issues in dealing with colleagues and students* |
0.76 |
|
Being assertive |
0.75 |
|
Being creative in work related matters |
0.74 |
|
Not money minded |
0.73 |
|
Willingness to work in rural areas |
0.72 |
|
Respecting professional hierarchy** |
0.69 |
|
Possessing knowledge in areas outside of medicine |
0.68 |
|
Being altruistic |
0.65 |
|
Adhering to socio-cultural norms* |
0.64 |
|
Fluency in multiple languages |
0.62 |
|
Abiding by religious beliefs |
0.32 |
|
Displaying self-importance** |
0.19 |
|
Using professional status for personal advantage** |
0.07 |
Note: *Evidence-based items sourced from the literature **Distractors
Table 2. Attributes of professionalism arranged in order of perceived importance
The highest rated attributes were, ‘possessing adequate medical knowledge and skills’, followed by ‘displaying a sense of responsibility’ and ‘being compassionate and caring’. Five items were mentioned collectively across the main stakeholder groups:
- Being empathetic towards patients
- Possessing adequate knowledge and skills
- Displaying effective communication skills
- Displaying honesty and integrity
- Being respectful and polite
2) Development of a Professionalism Framework: The main themes of professionalism identified by the expert panel and through exploratory factor analysis are summarised in Table 3.
|
Panelist 1 |
Panelist 2 |
Panelist 3 |
Factor Analysis |
|
Professionalism in interactions with patients (1) |
Interpersonal (1,2) |
Competency – Competency in managing patients and clinical reasoning (3) |
Qualities required to effectively work within the healthcare team (2) |
|
Professionalism in interactions in the workplace (2) |
Intrapersonal (4)
|
Accountability – Taking responsibility for work performed as a doctor in the clinical context and in interactions with co-workers (2) |
Clinical competency, excellence and continuous development (3)
|
|
Professionalism in fulfilling expectations of the profession and society (3) |
Societal/public (3)
|
Attitude – Thought process, internal qualities of the doctor (4) |
Equal and fair treatment of patients (1)
|
|
|
|
Behaviour – External actions of the doctor (1) |
Humane qualities in dealing with patients (1) |
Table 3. Themes of professionalism identified quantitatively and qualitatively*
Based on the convergence of these domains, a framework was developed, which portrayed professionalism as encompassing three main elements: individual traits, inter-personal interactions and responsibilities to the profession and community (Figure 1). Cronbach Alpha values for the three domains were 0.882, 0.918 and 0.755, thereby confirming the relevance of the constituents to each overarching element.
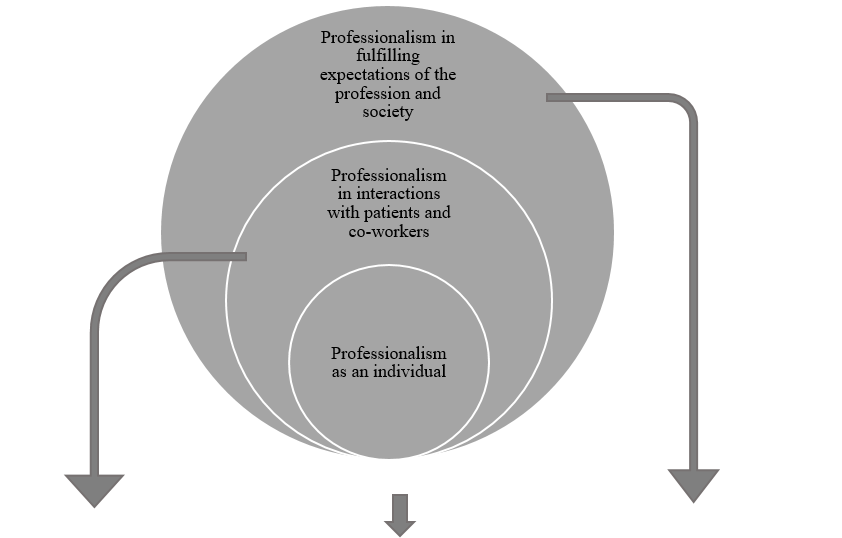
|
Professionalism in interactions with patients and co-workers |
Professionalism as an individual |
Professionalism in fulfilling expectations of the profession and society |
|
Ensuring confidentiality and patient privacy |
Displaying a sense of responsibility |
Managing limited resources for optimal outcome |
|
Displaying effective communication skills |
Being punctual |
Maintaining standards in professional practice |
|
Being empathetic towards patients |
Displaying honesty and integrity |
Displaying professional behaviour and conduct |
|
Being able to work as a member of a team |
Displaying commitment to work |
Working towards a common goal with the health system |
|
Being available |
Being reliable |
Adhering to a professional dress code |
|
Being responsive |
Being accountable for one’s actions and decisions |
Avoiding conflicts of interest |
|
Being respectful and polite |
Being clear in documentation |
Stands for professional autonomy |
|
Being a committed teacher/supervisor |
Displaying effective problem-solving skills |
Possessing adequate medical knowledge and skills |
|
Respecting patient autonomy |
Understanding limitations in professional competence |
Maintaining work-life balance |
|
Being accessible |
Ability to effectively manage time |
Avoiding substance and alcohol misuse |
|
Providing leadership |
Being open to change |
|
|
Advocating for patients |
Commitment to continuing professional development |
|
|
Maintaining professional relationships |
Having scientific thinking and approach |
|
|
Displaying sensitivity to socio-cultural and religious issues related to patient care |
Being accurate and meticulous |
|
|
Being compassionate and caring |
Displaying self confidence |
|
|
Being patient |
Non-judgemental attitude and ensuring equality |
|
|
Ability to provide and receive constructive criticism |
Engaging in reflective practice |
|
|
Being humble |
|
|
|
|
Being composed |
|
Figure 1. A framework of medical professionalism for Sri Lanka
IV. DISCUSSION
A. Framework of Professionalism Attributes
The framework depicts a progressively widening circle, with desirable individual traits at its core, expanding into interactions within the workplace and finally, responsibilities as a professional in wider society. It thus depicts the fundamental areas that must be addressed in aspiring towards professionalism. The three domains are largely congruent with the broad areas of professionalism described by Van de Camp et al. (2004) and Hodges et al. (2011). Though portrayed as distinct entities however, we emphasise that the domains should not be interpreted as evolving in sequential stages; professional development should ideally occur in these areas simultaneously.
Frameworks developed in other Eastern cultures have highlighted significant tenets of local traditions and ethos that have shaped perceptions on professionalism. Confucian values in Taiwan (Ho, Yu, Hirsh, Huang, & Yang, 2011), principles of Bushido in Japan (Nishigori, Harrison, Busari, & Dornan, 2014), and Islamic teachings within Egypt (Al-Eraky et al., 2014), have been shown to be deeply entrenched within such understandings.
Sri Lanka possesses a rich and diverse cultural heritage. British ideologies in particular appear to influence local medical education (Uragoda, 1987), and the conceptualisation of professionalism (Babapulle, 1992; Monrouxe et al., 2017), resulting in a strong emphasis on ethical behaviour. Sri Lanka is widely acknowledged to have a ‘religious’ background. Theravada Buddhism, the religion followed by the majority of Sri Lankans, as well as less widespread religions such as Christianity, Hinduism and Islam, exert a significant influence on local culture (Gildenhuys, 2004). Virtues collectively upheld by these doctrines, such as generosity, impartiality, honesty and peace are thought to be central to the development of professionalism (Keown, 2002). Of these, honesty, impartiality (equality) and peace (composure) were echoed within the theme ‘professionalism as an individual’, as were responsibility, reliability and accountability. These characteristics, built on a foundation of integrity, are fundamental tenets of Sri Lanka’s socio-cultural framework. Thus, we reasoned that ‘professionalism as an individual’ was ideally depicted as central to the local concept of professionalism, highlighting the importance of building a solid foundation of fundamental characteristics.
We also drew on elements of the ‘cultural dimension’ (Hofstede, n.d.) and ‘cultural value’ (Schwartz, 1999) theories in developing the framework. Accordingly, the collectivist nature of local culture provides the basis for qualities that enable harmonious interactions with others, as depicted in the second domain. The hierarchical disposition of local society dictates that the doctor is duty-bound to ensure that responsibilities to the profession and community are met.
B. Essential Attributes of Professionalism
Among the essential items, broad areas encompassing competence, humanism, interpersonal skills and ethics were prioritised. Qualities most consistently mentioned in literature – accountability, integrity and respect – received high ratings (Van de Camp et al., 2004). Reflective practice, understanding limitations in practice, accepting constructive criticism and continuous professional development – ‘cornerstones’ of the medical profession – were also labelled as significant (Chandratilake et al., 2012; Wynia et al., 2014), in contrast to other Eastern settings (Adkoli, Al-Umran, Al-Sheikh, Deepak, & Al-Rubaish, 2011). The striking omission was altruism, which was intriguingly rated as non-essential. Altruism has been named as one of the most consistently valued attributes of professionalism worldwide (Van de Camp et al., 2004), and would assumedly be espoused in the local collectivist culture. Our findings suggest that even qualities accepted as key tenets of professionalism may not be equally valued cross-culturally. However, it has been claimed that altruism is traditionally a Western concept (Nishigori et al., 2014), and the acceptance of altruism as a composite of professionalism has been challenged in recent years, on the premise that selflessness may in fact be causing considerable harm (Harris, 2018; Nishigori, Suzuki, Matsui, Busari, & Dornan, 2019).
Participants rated ‘possessing adequate medical knowledge and skills’ as the most essential professionalism attribute. This coincides with findings from Canada (Brownell & Cote, 2001) and Asia (Leung et al., 2012; Pan et al., 2013), though conflicting with a school of thought that considers competence to be the foundation of professionalism, rather than an integral part of it (Stern, 2006). The primacy afforded to knowledge and skills most likely stems from the significance placed on education, which is upheld in Sri Lanka as the primary means of elevating one’s socio-economic status. The emphasis on responsibility and compassion – the second and third highest rated items – as well as morality and empathy, can be attributed to the deeply religious background of the country. It was unsurprising that respectfulness was prioritised, being a cardinal virtue embraced by Sri Lankans, as in other Eastern settings (Nishigori et al., 2014).
A comparison of professionalism attributes hailed as important in various contexts, with the highest rated qualities locally, revealed a convergence of several items (Table 4). This provides assurance that the local conceptualisation of professionalism reflects the ‘core’ principles of medical professionalism and shows considerable alignment with definitions provided by professional bodies around the world (General Medical Council [GMC], 2013; Medical Professionalism Project, 2002).
|
Sri Lanka |
USA (American Board of Internal Medicine, 2001) |
Western countries (Hilton & Slotnick, 2005) |
Canada (Steinert, Cruess, Cruess, Boudreau, & Fuks, 2007) |
Taiwan (Ho et al., 2011) |
China (Pan et al., 2013) |
|
Knowledge and skills |
|
|
Competence |
Clinical competence |
Clinical competence |
|
Responsibility |
Accountability |
Accountability Social responsibility |
Responsibility |
Accountability |
Accountability |
|
Compassion and caring |
|
|
|
Humanism |
Humanism |
|
Managing limited resources for optimal outcome |
|
|
|
|
Economic consideration |
|
Confidentiality and patient privacy |
|
|
|
|
|
|
Punctuality |
|
|
|
|
|
|
Maintaining standards in professional practice |
Excellence |
|
|
Excellence |
Excellence |
|
Effective communication skills |
|
|
|
Communication |
Communication |
|
Honesty and integrity |
Integrity |
|
Honesty Integrity |
Integrity |
|
|
Commitment to work |
Duty |
|
Commitment |
|
|
|
|
Altruism |
|
Altruism |
Altruism |
Altruism
|
|
|
Respect |
Respect |
|
|
|
|
|
|
Self-awareness Reflection |
Self-regulation |
|
Self-management |
|
|
|
Teamwork |
Teamwork |
|
Teamwork |
|
|
|
Ethical practice |
Ethics |
Ethics |
Ethics |
|
|
|
|
Morality |
|
Morality |
|
|
Honour |
|
|
|
|
|
|
|
|
Autonomy |
|
|
|
|
|
|
|
|
Health promotion |
Table 4. Comparison of main attributes of professionalism identified locally with those of Western and Eastern contexts
Interestingly, certain items globally recognised as insignificant in terms of professionalism (work-life balance, leadership, professional appearance and composure) (Chandratilake et al., 2012), were highlighted as essential locally. The local expectation that professionals maintain an appearance befitting of their social status and the high power-distance between doctor and patient (Hofstede, n.d.), could have contributed to the emphasis on appearance. Similarly, power distance could explain the significance placed on leadership, a crucial skill required to handle subordinates and patients at the ‘lower end’ of the power spectrum. A promising finding was the importance placed on ‘work-life balance’, complementing the lack of emphasis on altruism and coinciding with recommendations of multiple professional bodies that underscore the value of personal well-being (GMC, 2013). The significance assigned to composure can be attributed to Sri Lanka’s conservative nature (Schwartz, 1999), where cultural norms dictate that public displays of intense emotion be suppressed.
It was intriguing to note that of the four distractors—which were expected to be rated as non-essential— ‘stands for professional autonomy’ achieved a CVI just above the baseline. In Sri Lanka, political influence is known to permeate into the workplace; therefore, this attribute can be viewed in light of being able to perform one’s duties in the midst of such pressures. The paternalistic nature of the doctor-patient relationship common to many Eastern cultures, could also underpin the significance afforded to professional autonomy (Ho & Al-Eraky, 2016; Susilo, Marjadi, van Dalen, & Scherpbier, 2019). Incidentally, this item was not corroborated elsewhere in the literature and was therefore, unique to this study. Other items that were exclusive to the Sri Lankan context were clarity in documentation, patience, time management and maintaining professional relationships.
As a whole, it is evident that the local conceptualisation of professionalism—while including areas unique to the Sri Lankan context—greatly coincides with the perceptions representing professionalism shared by the global medical community.
C. Strengths and Limitations
The study has responded to calls for culture-specific discourse on professionalism (Monrouxe et al., 2017) and prioritisation of essential qualities in terms of professionalism (Jha, Bekker, Duffy, & Roberts, 2007). Many studies seeking to define professionalism have drawn on the views of particular stakeholder groups in isolation; few have attempted to collate the views of the many groups (Ho et al., 2011; Leung et al., 2012; Pan et al., 2013). Scholars have challenged the medical profession to determine who should define professionalism, with the belief that this onus should not be placed solely on doctors (Wear & Kuczewski, 2004). The assimilation of views of multiple stakeholder groups therefore, was a significant strength of this study.
Although the initial list of 920 individuals who were invited to participate in the study was representative of all groups of stakeholders, the majority of those who responded were medical teachers and students. Thus, the study results predominantly reflect the views of these two groups. This may have precluded identification of attributes considered essential by the less represented groups, especially the public.
Another limitation of the study was the exclusive use of English, which though widely used in Sri Lanka, is not the first language of the majority of the population. The decision was justified as all potential participant groups were posited to be adequately fluent in English to participate. However, we recognise that providing the option of Sinhalese and Tamil translations may have increased participation in certain groups (healthcare staff and the public).
Finally, we acknowledge that while this framework reflects the current perception regarding medical professionalism, this notion is far from static, and will undeniably evolve with time. We therefore propose that future research involve repeated discussions that may inform the evolution of the current framework with time, being mindful of achieving a fair balance of stakeholder representation to this end.
V. CONCLUSION
This study has enabled us, through a consensus seeking approach, to paint a picture of medical professionalism as grounded in the views of the multiple stakeholders of healthcare in Sri Lanka. The conceptual framework that represents these opinions, reflects how perceptions on professionalism are shaped by cultural, societal, religious, economic and other factors. Moreover, it has enabled identification of individual elements of professionalism that are expected of a doctor in the local context, and prioritisation of those most essential among them.
Notes on Contributors
Amaya Ellawala MBBS, PGDME, MD, is a Lecturer in Medical Education in the Department of Medical Education, Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka. Amaya Ellawala reviewed the literature, developed the methodological framework for the study, performed data collection, analysis and wrote the manuscript.
Madawa Chandratilake MBBS, MMed, PhD, is a Professor of Medical Education at the Department of Medical Education, Faculty of Medicine, University of Kelaniya, Sri Lanka. Madawa Chandratilake contributed to the development of the methodological framework, data analysis and writing of the manuscript.
Nilanthi de Silva MBBS, MSc, MD, is a Senior Professor in the Department of Parasitology, Faculty of Medicine, University of Kelaniya, Sri Lanka. Nilanthi de Silva contributed to the development of the methodological framework, data analysis and writing of the manuscript.
All authors read and approved the final manuscript.
Ethical Approval
Ethics approval was obtained from the Ethics Review Committee, Faculty of Medicine, University of Kelaniya (P/15/01/2016).
Funding
This study was not funded.
Declaration of Interest
The authors declare that they have no competing interests.
References
Adkoli, B. V., Al-Umran, K. U., Al-Sheikh, M., Deepak, K. K., & Al-Rubaish, A. M. (2011). Medical students’ perception of professionalism: A qualitative study from Saudi Arabia. Medical Teacher, 33(10), 840–845.
Al-Eraky, M. M., & Chandratilake, M. (2012). How medical professionalism is conceptualised in Arabian context: A validation study. Medical Teacher, 34(S1), S90–S95.
Al-Eraky, M. M., Chandratilake, M., Wajid, G., Donkers, J., & Van Merrienboer, J. G. (2014). A Delphi study of medical professionalism in Arabian Countries: The Four-Gates Model. Medical Teacher, 36, S8–S16.
American Board of Internal Medicine. (2001). Project Professionalism. Philadelphia, USA: American Board of Internal Medicine.
Babapulle, C. J. (1992). Teaching of medical ethics in Sri Lanka. Medical Education, 26(3), 185–189.
Birden, H., Glass, N., Wilson, I., Harrison, M., Usherwood, T., & Nass, D. (2014). Defining professionalism in medical education: A systematic review. Medical Teacher, 36(1), 47–61.
Brownell, A. K. W., & Cote, L. (2001). Senior residents’ views on the meaning of professionalism and how they learn about it. Academic Medicine, 76(7), 734–737.
Chandratilake, M., Mcaleer, S., & Gibson, J. (2012). Cultural similarities and differences in medical professionalism: A multi-region study. Medical Education, 46(3), 257–266.
De Villiers, M. R., De Villiers, P. J. T., & Kent, A. P. (2005). The Delphi technique in health sciences education research. Medical Teacher, 27(7), 639–643.
General Medical Council. (2013). Good Medical Practice. London, UK: GMC.
Gildenhuys, J. S. H. (2004). Ethics and Professionalism. Stellenbosch. South Africa: Sun Press.
Harris, J. (2018). Altruism: Should it be included as an attribute of medical professionalism? Health Professions Education, 4, 3–8.
Hilton, S. R., & Slotnick, H. B. (2005). Proto-professionalism: How professionalisation occurs across the continuum of medical education. Medical Education, 39, 58–65.
Ho, M., & Al-Eraky, M. (2016). Professionalism in context: Insights from the United Arab Emirates and beyond. Journal of Graduate Medical Education, 8(2), 268–270.
Ho, M., Yu, K., Hirsh, D., Huang, T., & Yang, P. (2011). Does one size fit all? Building a framework for medical professionalism. Academic Medicine, 86(11), 1407–1414.
Hodges, B. D., Ginsburg, S., Cruess, R., Cruess, S., Delport, R., Hafferty, F., … Wade, W. (2011). Assessment of professionalism: Recommendations from the Ottawa 2010 conference. Medical Teacher, 33(5), 354–363.
Hofstede, G. (n.d.). Cultural Dimensions. Retrieved from http://geerthofstede.com/culture-geert-hofstede-gert-jan-hofstede/6d-model-of-national-culture/
Hofstede, G. (2011). Dimensionalizing cultures: The Hofstede model in context. Online Reading in Psychology and Culture, 2(1), 1–26.
Hsieh, H., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288.
Humphrey-Murto, S., Varpio, L., Wood, T. J., Gonsalves, C., Ufholz, L., Mascioli, K., … Foth, T. (2017). The use of the Delphi and other consensus group methods in medical education research. Academic Medicine, 92(10), 1491–1498.
Irby, D. M., & Hamstra, S. J. (2016). Parting the clouds: Three professionalism frameworks in medical education. Academic Medicine, 91(12), 1606–1611.
Jha, V., Bekker, H. L., Duffy, S. R. G., & Roberts, T. E. (2007). A systematic review of studies assessing and facilitating attitudes towards professionalism in medicine. Medical Education, 41, 822–829.
Keown, D. (2002). Buddhism and medical ethics. Principles of Practice, 7, 39–70.
Lesser, C. S., Lucey, C. R., Egener, B., Braddock, C. H., Linas, S. L., & Levinson, W. (2010). A behavioral and systems view of professionalism. Journal of the American Medical Association, 304(24), 2732–2737.
Leung, D. C., Hsu, E. K., & Hui, E. C. (2012). Perceptions of professional attributes in medicine: A qualitative study in Hong Kong. Hong Kong Medical Journal, 18(4), 318–324.
Lynn, M. R. (1986). Determination and quantification of content validity. Nursing Research, 35, 382–385.
Maykut, P., & Morehouse, R. (1994). Beginning Qualitative Research: A Philosophic and Practical Guide. London, UK: Falmer Press.
Meade, A. W., & Craig, S. B. (2012). Identifying careless responses in survey data. Psychological Methods, 17(3), 437-455.
Medical Professionalism Project. (2002). Medical professionalism in the new millennium: A physicians’ charter. The Lancet, 359, 520-522.
Monrouxe, L. V., Chandratilake, M., Gosselin, K., Rees, C. E., & Ho, M. J. (2017). Taiwanese and Sri Lankan students’ dimensions and discourses of professionalism. Medical Education, 51(7), 1-14.
Nishigori, H., Harrison, R., Busari, J., & Dornan, T. (2014). Bushido and medical professionalism in Japan. Academic Medicine, 89(4), 560–563.
Nishigori, H., Suzuki, T., Matsui, T., Busari, J., & Dornan, T. (2019). A two-edged sword: Narrative inquiry into Japanese doctors’ intrinsic motivation. The Asia Pacific Scholar, 4(3), 24-32.
Pan, H., Norris, J. L., Liang, Y., Li, J., & Ho, M. (2013). Building a professionalism framework for healthcare providers in China: A Nominal Group technique study. Medical Teacher, 35, e1531–e1536.
Polit, D., & Beck, C. (2006). The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Research in Nursing and Health, 29, 489–497.
Powell, C. (2003). The Delphi Technique: Myths and realities – Methodological issues in nursing research. Journal of Advances in Nursing, 41(4), 376–382.
Randolph, J. (n.d.). Online Kappa Calculator. Retrieved from http://justusrandolph.net/kappa/
Schwartz, S. H. (1999). A theory of cultural values and some implications for work. Applied Psychology: An International Review, 48(1), 23–47.
Sri Lanka Medical Council. (2009). Guidelines on Ethical Conduct for Medical and Dental Practitioners Registered with the Sri Lanka Medical Council. Colombo, Sri Lanka: SLMC.
Steinert, Y., Cruess, R. L., Cruess, S. R., Boudreau, J. D., & Fuks, A. (2007). Faculty development as an instrument of change: A case study on teaching professionalism. Academic Medicine, 82(11), 1057-1064.
Stern, A. (2006). Measuring Professionalism. New York, USA: Oxford University Press.
Susilo, A. P., Marjadi, B., van Dalen, J., & Scherpbier, A. (2019). Patients’ decision-making in the informed consent process in a hierarchical and communal culture. The Asia Pacific Scholar, 4(3), 57-66.
Tavakol, M., & Sandars, J. (2014). Quantitative and qualitative methods in medical education research: AMEE Guide No 90: Part II. Medical Teacher, 36(10), 838–848.
Uragoda, C. (1987). A History of Medicine in Sri Lanka – From the Earliest Times to 1948. Colombo, Sri Lanka: Sri Lanka Medical Association.
Van de Camp, K., Vernooij-Dassen, M. J. F. J., Grol, R. P. T. M., & Bottema, B. J. A. M. (2004). How to conceptualize professionalism: A qualitative study. Medical Teacher, 26(8), 696–702.
Van Mook, W. N. K. A., Van Luijk, S. J., O’Sullivan, H., Wass, V., Schuwirth, L. W., & Van Der Vleuten, C. P. M. (2009). General considerations regarding assessment of professional behaviour. European Journal of Internal Medicine, 20(4), e90–e95.
Wear, D., & Kuczewski, M. G. (2004). The professionalism movement: Can we pause? American Journal of Bioethics, 4(2), 1–10.
Wilkinson, T. J., Wade, W. B., & Knock, L. D. (2009). A blueprint to assess professionalism: Results of a systematic review. Academic Medicine, 84(5), 551–558.
Wynia, M. K., Papadakis, M. A., Sullivan, W. M., & Hafferty, F. W. (2014). More than a list of values and desired behaviors: A foundational understanding of medical professionalism. Academic Medicine, 89(5), 712–714.
*Amaya Ellawala
Department of Medical Education,
Faculty of Medical Sciences,
University of Sri Jayewardenepura,
Sri Lanka
Email address: amaya@sjp.ac.lk
Submitted: 17 March 2020
Accepted: 3 June 2020
Published online: 5 January, TAPS 2021, 6(1), 60-69
https://doi.org/10.29060/TAPS.2021-6-1/OA2239
Frank Bate1, Sue Fyfe2, Dylan Griffiths1, Kylie Russell1, Chris Skinner1, Elina Tor1
1University of Notre Dame Australia, Australia; 2Curtin University, Australia
Abstract
Introduction: In 2017, the School of Medicine of the University of Notre Dame Australia implemented a data-informed mentoring program as part of a more substantial shift towards programmatic assessment. Data-informed mentoring, in an educational context, can be challenging with boundaries between mentor, coach and assessor roles sometimes blurred. Mentors may be required to concurrently develop trust relationships, guide learning and development, and assess student performance. The place of data-informed mentoring within an overall assessment design can also be ambiguous. This paper is a preliminary evaluation study of the implementation of data informed mentoring at a medical school, focusing specifically on how students and staff reacted and responded to the initiative.
Methods: Action research framed and guided the conduct of the research. Mixed methods, involving qualitative and quantitative tools, were used with data collected from students through questionnaires and mentors through focus groups.
Results: Both students and mentors appreciated data-informed mentoring and indications are that it is an effective augmentation to the School’s educational program, serving as a useful step towards the implementation of programmatic assessment.
Conclusion: Although data-informed mentoring is valued by students and mentors, more work is required to: better integrate it with assessment policies and practices; stimulate students’ intrinsic motivation; improve task design and feedback processes; develop consistent learner-centred approaches to mentoring; and support data-informed mentoring with appropriate information and communications technologies. The initiative is described using an ecological model that may be useful to organisations considering data-informed mentoring.
Keywords: Data-Informed Mentoring, Mentoring, Programmatic Assessment, E-Portfolio
Practice Highlights
- Students and mentors appreciated the introduction of data-informed mentoring.
- Assessment policies and practices should be integrated with data-informed mentoring.
- Data-informed mentoring presents curriculum challenges in task design and framing feedback.
- The student context informs the data-informed mentoring approach (learner-centred to mentor-directed).
- Data-informed mentoring requires supportive information and communications technologies.
I. INTRODUCTION
An often-cited definition of mentoring, highlights the role of experienced and empathetic others guiding students to re-examine their ideas, learning and personal and professional development (Standing Committee on Postgraduate Medical and Dental Education, 1998).
Heeneman and de Grave (2017) identify some subtle differences between traditional conceptions of mentoring and the type of mentoring that is required under programmatic assessment, which in this paper we refer to as Data-Informed Mentoring (D-IM). For example, D-IM is embedded in a curriculum in which rich data on student progress arises from student interaction with assessment tasks, informing and enhancing their progress (see Appendix). Further, in programmatic assessment, the learning portfolio is typically the setting in which the mentor-mentee relationship develops. This setting brings together institutional imperatives (e.g. assessable tasks), and personal imperatives such as evidence of competence and personal reflection. Situating mentoring in a curriculum and assessment framework impacts upon the mentoring relationship.
Meeuwissen, Stalmeijer, and Govaerts (2019) propose that a different type of mentoring is required under programmatic assessment. Mentors interpret data and feedback provided by content experts across domains of learning thus providing an evidence-base to facilitate student reflection. They might also take on a variety of roles (e.g. critical friend, coach, assessor) that could influence the mentoring relationship including the level of trust that is established with the student. These challenges suggest that conventional definitions of mentoring might not capture the essence of D-IM. Whilst the availability of rich information potentially enhances the mentoring experience and personalises learning, mentors and students are challenged to make sense and act upon this information; students might focus on issues that fall outside of the scope of the data provided (e.g. their wellbeing); mentors may also struggle to delineate boundaries between multiple roles or draw a line on where their scope of practice, as a mentor, begins and ends.
Mentoring is a social construct and as such is best considered through a holistic lens taking account of societal, institutional and personal factors (Sambunjak, 2015). The current study adopted Sambunjak’s “ecological model” (2015, p. 48) as a framework to help understand the impact of D-IM (Figure 1). Societal, institutional and personal forces are inter-related. For example, a student’s approach to D-IM might be influenced by financial circumstances resulting in the need to work part-time (societal); a medical school’s assessment policy (institutional); or a student’s learning style (personal). The model is presented as a set of cogs where the optimal educational experience is achieved if all elements work in harmony. The study uses the ecological model to help answer the central research question that guided the study: how did students and staff react and respond to D-IM?
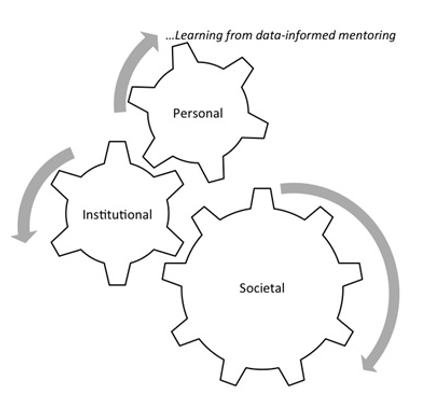
Figure 1. An ecological framework for conceptualizing D-IM (modified from Sambunjak, 2015)
This paper shares findings from the study derived from the first two years of data collection. Its focus is on the implementation of D-IM and how students and staff reacted to this implementation (Kirkpatrick & Kirkpatrick, 2006).
II. METHODS
The School of Medicine Fremantle (the School) of the University of Notre Dame Australia introduced D-IM as part of its incremental approach to programmatic assessment. The School offers a four-year doctor of medicine (MD) with around 100 students enrolling each year. The first two years are pre-clinical consisting of problem-based learning supported by lectures and small group learning. The final two years involve clinical rotations mostly located at hospital sites. Each year of the MD constitutes a course that students need to pass in order to progress to the next year. The School’s assessment mix includes knowledge-based examinations (multiple choice/case-based), Objective Structured Clinical Examinations, work-based assessments and rubric-based assessments (e.g. reflections). Examinations are administered mid-year and end-of-year for pre-clinical students and end-of-year for students in the clinical years.
All performance data informs D-IM. Regular feedback from assessors is provided and collated in an e-portfolio (supported by Blackboard) so that students have opportunities to reflect on their progress and plan future learning. Students are allocated a mentor each year who has access to their students’ e-portfolio.
Mentoring was provided by 26 pre-clinical de-briefing (CD) tutors whose role was to facilitate student reflection on their learning and support and guide their interpretation of the feedback they had received. D-IM was introduced to first year students in 2017 and first and second year students in 2018. Three mentoring meetings were conducted per student per year. CD tutors also have a role in assessing student performance and providing feedback. Each CD tutor has a CD group which is also their mentoring group (8-10 students). However, tasks are assessed and feedback is provided by a different tutor. This means that mentor and assessor functions are separated.
In preparation for the implementation of D-IM, targeted professional development was provided to tutors which unpacked the mentoring role and provided examples of how performance data can be used to underpin mentoring sessions.
The University of Notre Dame Australia Human Research Ethics Committee (HREC) provided ethical approval for the research, and a research team was formed in 2017. Action research guided the conduct of the research, as it aims to understand and influence the change process. Action research is the “systematic collection and analysis of data for the purpose of taking action and making change” (Gillis & Jackson, 2002, p. 264). It involves cycles of planning, implementing, observing and reflecting on the processes and consequences of the action. The subjects of the research have input into cycles and influence changes that are made as a result of feedback and reflection (Kemmis & McTaggart, 2000). Each cycle of the research runs for one year so that planning, action, observation and reflection can inform the next iteration.
Mixed methods research involving qualitative and quantitative methods, was used. Data were collected each year from student questionnaires and focus groups which included mentors. Participation in the research was underpinned by a Statement of Informed Consent. For the questionnaire consent constituted ticking a box on an online form. For the focus group, a physical form was signed before taking part in a focus group. The student questionnaire comprised qualitative and quantitative components and posed 9 statements on mentoring. The questionnaire was critically appraised by a panel of 8 academic staff in May 2017 and it was agreed that the questionnaire had attained face validity before it was administered in September 2017.
Students were asked to rate each statement of the questionnaire according to a Likert-type scale from Strongly Disagree, Disagree, Neutral, Agree to Strongly Agree. For interpretation, a numerical value was assigned to each response from 1=Strongly Disagree through to 5=Strongly Agree. Quantitative data were downloaded from SurveyMonkey as Excel files for extraction of descriptive statistics and then imported into SPSS Version 25. Statistical analysis was undertaken using SPSS version 25. Two statistical tests were conducted. The first test, a non-parametric median test on students’ perception of each aspect of DI-M, is consistent with the purpose of action research to inform future practice. Responses to individual survey items using a Likert-type response scale are ordinal in nature, and the distributions are not identical for the two cohorts, therefore a median test was used. This statistic compares the responses from two independent groups to individual survey items, with reference to the overall pooled median rating for the two cohorts combined. More specifically, the median test examines whether there are the same proportion of responses above and below the overall pooled median rating, in each of the two cohorts, for each individual item. A second test, an aggregate mean score (an integer), was calculated from the students’ responses to the nine statements in each cohort. The mean score for each cohort provided an overall indication on the extent to which respondents were satisfied with the mentoring program. A parametric test, (independent t-test) was used to examine if there were statistically significant differences in mean scores between the two independent cohorts.
Qualitative data were coded from students’ comments to two open-ended questions in the student questionnaire: (1) Please comment on any aspect of the learning portfolio that you feel were particularly beneficial for your learning journey; and (2) Please comment on any aspect of the learning portfolio that could be improved in the future. Qualitative data from mentors through three focus groups in both 2017 and 2018 were recorded, transcribed and imported into Nvivo12 to help identify patterns across and within data sources. Data saturation was achieved after two focus group iterations. Two researchers independently coded students’ comments and staff transcripts and then met to discuss and resolve differences in interpretation. These codes were then presented to the broader team in which ideas were further unpacked and themes developed using Braun and Clarke’s (2006) thematic approach to analysis.
III. RESULTS
In 2017, 29% of the year 1 student cohort responded to the questionnaire (n=33) and in 2018, the response fraction across both Year 1 and Year 2 was 47% (n=98). The 2017 student cohort is described as Cohort 1 and the 2018 Student Cohort is Cohort 2. The response fraction for Cohort 1 increased from 29% in 2017 to 46% in 2018. In 2017, 21 staff participated in focus groups (7 of whom were mentors). In 2018, 17 staff took part (9 mentors). Tables 1-2 compare student responses to the 9 items on mentoring on the following basis:
- Over time in 2017 and 2018 within Cohort 1 (Table 1);
- For first year students–Cohort 1 2017 and Cohort 2 2018 (Table 2).
For each table, median ratings are shown for each item along with the results of the median test to discern statistically significant differences between or within cohorts. Table 1 compares Cohort 1 responses to D-IM over time.
|
Item |
Overall Pooled Median* |
Cohort 1 2017 (n=32) |
Cohort 1 2018 (n=51) |
|
||
|
|
|
n> pooled median |
n<= pooled median |
n> pooled median |
n<= pooled median |
Median Test |
|
The mentoring process was well organised
|
4 |
6 |
26 |
6 |
45 |
χ2 =0.776; df=1; p=0.378 |
|
My mentor was personally very well organised
|
5 |
0 |
32 |
0 |
50 |
n/a**
|
|
There were an appropriate number of mentoring meetings throughout the year
|
4 |
2 |
30 |
4 |
47 |
χ2 =0.074; df=1; p=0.785 |
|
My mentor was respectful
|
5 |
0 |
32 |
0 |
51 |
n/a**
|
|
My mentor listened to me
|
5 |
0 |
32 |
0 |
50 |
n/a**
|
|
My mentor asked thought-provoking questions which helped me to reflect
|
4 |
10 |
22 |
12 |
39 |
χ2 =0.602; df=1; p=0.438 |
|
My mentor added value to my learning
|
4 |
10 |
22 |
11 |
40 |
χ2 =0.975; df=1; p=0.323 |
|
My mentor helped me to set future goals that were achievable
|
4 |
9 |
23 |
11 |
40 |
χ2 =0.462; df=1; p=0.497 |
|
The summaries provided of my performance in the Blackboard Community Site were useful in helping me to reflect on my progress |
3 |
17 |
16 |
14 |
37 |
χ2 =4.983; df=1; p=0.026*** |
Note. *In the median test, a comparison is made between the median rating in each group to the ‘overall pooled median’ from both groups. **Values are less than or equal to the overall pooled median therefore Median Test could not be performed. ***Significant at p < 0.05 level.
Table 1. Student Perceptions of D-IM within Cohort 1 in 2017 and 2018–Median Tests for Individual Items
The only statistically significant difference noted for Cohort 1 was for the summaries of performance provided in Blackboard that were designed to underpin D-IM. The data provided in these summaries was less valued by students who engaged with D-IM in their second year.
The aggregate mean score in response to the statements on D-IM in the survey was positive in 2017 (M=4.02; SD=0.62; n=32). Mentoring continued to be well perceived by Cohort 1 as they progressed to second year in 2018 (M=3.80; SD=0.67; n=51). The slight difference in aggregate mean scores between 2017 and 2018 is not statistically significant (t=1.571; df=82, p=0.120). Table 2 compares first year students’ perceptions of D-IM.
|
Item |
Overall Pooled Median* |
Cohort 1 n=32 |
Cohort 2 n=47 |
|
||
|
|
|
n> pooled median |
<= pooled median |
> pooled median |
<= pooled median |
Median Test |
|
The mentoring process was well organised
|
4 |
6 |
26 |
9 |
37 |
χ2 =0.008; df=1; p=0.928 |
|
My mentor was personally very well organised
|
5 |
0 |
32 |
0 |
47 |
n/a** |
|
There were an appropriate number of mentoring meetings throughout the year
|
4 |
2 |
30 |
8 |
39 |
χ2 =0.998; df=1; p=0.158 |
|
My mentor was respectful |
5
|
0 |
32 |
0 |
47 |
n/a**
|
|
My mentor listened to me |
5 |
0 |
32 |
0 |
47 |
n/a**
|
|
My mentor asked thought-provoking questions which helped me to reflect
|
4 |
10 |
22 |
18 |
29 |
χ2 =0.413; df=1; p=0.520 |
|
My mentor added value to my learning
|
4 |
10 |
22 |
17 |
30 |
χ2 =0.205; df=1; p=0.651 |
|
My mentor helped me to set future goals that were achievable
|
4 |
9 |
23 |
17 |
30 |
χ2 =0.558; df=1; p=0.455 |
|
The summaries provided of my performance in the Blackboard Community Site were useful in helping me to reflect on my progress |
3 |
17 |
16 |
17 |
30 |
χ2 =1.868; df=1; p=0.172 |
Note. *In the median test, a comparison is made between the median rating in each group to the ‘overall pooled median’ from both groups. **Values less than or equal to the overall pooled median therefore Median Test could not be performed.
Table 2. First Year Student Perceptions of D-IM –Median Tests between Cohort 1 and Cohort 2 for Individual Items
No statistically significant differences were noted between cohorts 1 and 2.
The aggregate mean score in response to the statements on D-IM in the survey was positive for Cohort 1 in 2017 (M=4.02; SD=0.62; n=32). Equally positive responses were noted in Cohort 2 in 2018 (M=3.91; SD=0.79; n=47). The difference between aggregate mean scores for first year students’ perceptions is not statistically significant (t=0.686; df=78, p=0.495).
Data from tables 1 and 2 reveals that students are highly satisfied with three aspects of mentoring: the personal organisation of the mentor along with their respectful and listening attributes. Students were also satisfied with the mentoring process, the number of mentoring meetings, the ability of the mentoring to assist in reflection and to add value to their learning, and also the propensity of the mentor to assist in action-planning. However, the summaries provided in the Blackboard environment were a source of dissatisfaction for students.
As discussed, qualitative data were collected from students through the questionnaire and staff through focus groups. The research team collated the qualitative data and confirmed that the qualitative data corroborated quantitative results with students and mentors appreciating the introduction of D-IM. For example, “Mentor sessions are important in providing support to students and…are a welcome introduction” (Yr1 Student, 2017); “Mentoring was useful to develop self-directed learning and to check where you were” (Yr2 Student, 2018); “You get to know the students, things were revealed which would not have been otherwise” (Mentor, 2017); and “Mentoring enabled me to facilitate more, listen more. Definitely a difference when you’re one-on-one with somebody” (Mentor, 2018).
In tune with the action research method adopted by the study which seeks to identify and respond to opportunities for improvement, the Research Team identified three concerns from the qualitative data: differing views of the purpose of D-IM and the role of the mentor; the provision of student feedback and information and communications technologies (ICT); and workload.
A. Differing Views of the Purpose of D-IM and the Role of Mentor
Mentors had differing conceptions of the purpose of D-IM and the role of a mentor. Some mentors perceived their primary function to be one of facilitating reflection and being encouraging whilst others were more directive, providing advice or sharing their own experiences. “I was…a sounding board to prompt their thoughts about how their progress was going. Rather than offering ways of solving problems it was more pointing where problems might lie and encouraging them to think of solutions” (Mentor, 2017); “The basic rule is to guide them… guide them properly, maybe to get them to change their study strategies and other things” (Mentor, 2017).
B. Provision of Student Feedback and ICT
Students reported that feedback was inconsistent in timeliness and quality. Often feedback lacked guidance for improvement or was too late for it to help the student improve their learning: “More in-depth feedback on work, and returned in a timeframe that allows it to be relevant to our learning” (Yr1 Student, 2018); “Marking seemed thoughtless and halfhearted” (Yr2 Student, 2018).The use of a Blackboard Wiki to collate and present data points was also less than ideal with students finding the site difficult to navigate and use although they generally reported that it was safe and secure.
C. Workload
Students understood the role of reflection and appreciated having a mentor although there was some misunderstanding of the role of the portfolio with some students seeing it as extra work: “The amount of work required…was disproportionate” (Yr2 Student, 2018). Some students felt that the added stress and anxiety detracted from their study of medicine: “The portfolio actually detracts from spending time learning content that is essential to clinical years” (Yr2 Student, 2018). These concerns needed to be addressed by the School and are discussed in the context of changes that have and will be made to D-IM for preclinical students in the School.
IV. DISCUSSION
On the whole there was a positive response to D-IM implementation by students and staff. This response is consistent with Frei, Stamm, and Buddeberg-Fischer (2010, p. 1) who found that the “personal student-faculty relationship is important in that it helps students to feel that they are benefiting from individual advice.”
The findings of the research, however, reveal some tensions between the various elements of Sambunjak’s (2015) ecological model that link to the three areas of concern identified in the research. These tensions are shown in Figure 2.

Figure 2. The ecological framework to explore tensions in D-IM
A. Purpose and Role of Mentors and D-IM
The role of the mentor at the School is to support and guide students, and this role was not confused with other functions such as content expert or assessor. In this respect, the role conflict described by Meeuwissen et al. (2019) and Heeneman and deGrave (2017) was not evident at the School. However, mentoring approaches were situated on a continuum between learner-centred and mentor-directed. It is probable that the mentor’s style–empowering, checking or directing (Meeuwissen et al., 2019, p.605)–and their potentially different view of their role impacted on how D-IM sessions played out. Three ways of understanding the role of mentor in medical education have been identified: someone who can answer questions and give advice, someone who shares what it means to be a doctor and someone who listens and stimulates reflection (Stenfors-Hayes, Hult, & Owe Dahlgren, 2011). In a study of mentoring styles of beginning teachers, Richter et al. (2013) found that the mentor’s beliefs about learning have the greatest impact on the quality of the mentoring experience. Although professional development was provided to mentors on their role as facilitators of reflection and these issues were outlined and discussed, there were differences in interpretation of the role in the D-IM context.
Heeneman and de Grave (2017) argue that students need to be self-directed in order to be effective medical professionals. It is posited that a number of factors can influence the extent to which the mentor directs proceedings including the mentor’s experience, role clarity, rate of student progress, depth of student reflections and the perceived importance of the data required for assessment purposes.
In this study most students engaged positively with D-IM, though, albeit with variations in the extent and quality of reflection and action planning. A slight decrease in students’ enthusiasm towards D-IM was noted as they progressed from first to second year. This could be related to the novelty of D-IM diminishing over time that has been evident in other educational technology innovations (Kuykendall, Janvier, Kempton, & Brown, 2012). However, students also have a different mentor in each year. According to Sambunjak (2015), mentoring requires commitment sustained over a long period of time. At Maastricht University, for example, Heeneman and de Grave (2017) report that students are allocated the same mentor for a four-year medical course. It is, therefore, likely that in the current study the short timeframe for mentors to establish student relationships, and the introduction of a different mentor each year contributed to a reduction in student satisfaction.
B. Feedback and ICT Support
D-IM is dependent on quality data. That is, the perceived value of tasks that students engage with, and the feedback that they receive on, these tasks. Findings suggest that students found some tasks repetitive and feedback belated and superficial. Better task design and feedback practices are required. This finding is consistent with those of Bate, Macnish and Skinner (2016) in a study of task design within a learning portfolio. Findings also indicated dissatisfaction with Blackboard ICT environment. The portal was not intuitive and the structure and requirements for use of the template did not stimulate the desired level of reflection.
C. Workload
Students at the School are “time poor” and many work part-time whilst studying. They are graduate entrants used to achieving academic success. Most are millennials comfortable with distilling and manipulating data and using online technologies. These characteristics are consistent with what Waljee, Copra, and Saint (2018) see as the new breed of medical students, being accustomed to distilling information and desirous of rapid career advancement. In these circumstances, it is unsurprising that students valued D-IM as it promoted focused data-driven discussion on their progress. However, it is also unsurprising that students were critical of anything that, in their opinion, did not support the “study of medicine”. Although students were sometimes critical of tasks that fed into D-IM (Bate et al., 2020), the reflective and action planning components of DI-M were not onerous and were at any rate optional.
For most students, grades rather than learning were paramount and this created a competitive environment which fuelled strategic learning in engaging with tasks underpinning D-IM. The School’s Assessment Policy has implications here. Progression is determined by passing discrete assessments and causes students to focus on grades rather than learning. These dispositions play out in D-IM sessions where, for example, goals are sometimes framed around passing examinations rather than addressing deficits in understanding. The School also distinguishes between formative and summative assessment with the result being that formative assessments are less valued by students. Opportunities to test understanding through formative testing are sometimes not taken up and result in less information for students and their mentor to gauge learning progress.
Bhat, Burm, Mohan, Chahine, and Goldszmidt (2018, p. 620) identified a set of “threshold concepts” in medicine that are crucial for students transitioning into clinical practice. Among these are self-directed, metacognitive and collaborative dispositions to learning. However, for a student in the preclinical years, these threshold concepts are not perceived to be the important factors that determine their progress through the course and their aim to become a doctor. Thus the tensions between students valuing mentoring but feeling that reflecting on their performance through D-IM is time-consuming and unrelated to their course progression is a source of tension within the model.
D. Actions as a Result of the Study
The action research approach of this study meant that in all results the Research Team was looking for ways to improve the system. Some issues could be improved quickly. A refinement of the Blackboard environment and a change to a software solution called SONIA was implemented in 2019 to improve the ICT interface and reduce workload. Continuing professional development (PD) for staff is undertaken and takes the research results into account. Within the mentor PD program, the Research Team saw that mentoring requires mentors to be able to diagnose the readiness and willingness of students to consider their learning educational journey. This means that, whilst the D-IM program needs a consistent view of D-IM where mentors see their role as facilitating reflection, different mentoring skills and behaviours are needed by mentors for different students. PD is also needed for students so that they understand the relationship between their achievement of learning and the role of D-IM in their journey.
Some issues are longer-term or resource dependent. A focus on the role of feedback in the system, especially for student reflection and its timeliness for mentoring sessions and action planning is critical to making D-IM valued by students. However, it is not always possible for staff to provide feedback in an optimum timeframe although the quality of the feedback can be improved by clear guidelines, expectations and an intuitive online interface.
Of great complexity and more difficult to resolve is the tension between developing the “threshold concepts” (Bhat et al., 2018); the generic skills which are built on self-reflection and are supported by D-IM and the ways in which a student progresses through the course. These are School-based rules of progression and produce a framework within which D-IM needs to operate.
V. LIMITATIONS OF THE STUDY
The study was conducted at one University and although it will ultimately cover a six-year timeframe, findings should be gauged within the context of this setting. Relatively low response rates were noted, and selection bias is a possibility with students most engaged with D-IM completing the questionnaire. Although professional development was provided to underpin the mentoring role, there was variation in the way tutors interpreted this role. The study was conducted at a time where other changes were occurring at the School (e.g. development of more continuous forms of assessment) and these changes might have impacted on D-IM. The questionnaire used in the study contained nine questions on mentoring. To gain a more nuanced understanding of D-IM at the School, it may be useful to use a comprehensive and validated questionnaire (e.g. Heeneman & de Grave, 2019) capturing the perceptions of mentees and mentors.
VI. CONCLUSION
The School aims to create quality, patient-centred and compassionate doctors who are lifelong learners (Candy, 2006). D-IM is an effective augmentation to the School’s educational program and the paper has demonstrated that it was well received by students and staff. Future directions include consideration of D-IM in clinical mentoring, development of more consistent learner-centred approaches to mentoring; improved task design and feedback; support for D-IM with appropriate ICT; and better integration of D-IM with assessment policies and practices.
Notes on Contributors
Associate Professor Frank Bate completed his PhD at Murdoch University. He is the Director of Medical and Health Professional Education at the School of Medicine Fremantle, University of Notre Dame Australia. He conceptualised and led the research, and was the primary author responsible for developing, reviewing and improving the manuscript.
Professor Sue Fyfe attained her PhD at the University of Western Australia and is an adjunct professor at Curtin University. She assisted in conceptualising the research design, conducted the qualitative data analysis and made a significant contribution to reviewing and improving the manuscript.
Dr Dylan Griffiths has a PhD from the University of Essex and is the Quality Assurance Manager at the School of Medicine Fremantle, University of Notre Dame Australia. He conducted data collection and assisted with preliminary analysis.
Associate Professor Kylie Russell obtained her PhD from the University of Notre Dame Australia. She is currently a Project Officer at the School of Medicine Fremantle, University of Notre Dame Australia. She assisted in the development of the research methodology and made a contribution to reviewing and improving the manuscript.
Associate Professor Chris Skinner completed his PhD at the University of Western Australia. He is Domain Chair of Personal and Professional development at the School of Medicine Fremantle, University of Notre Dame Australia. He assisted in conceptualising the research design and made a contribution to reviewing and improving the manuscript.
Associate Professor Elina Tor completed her PhD at Murdoch University and is the Associate Professor of Psychometrics at the School of Medicine Fremantle, University of Notre Dame Australia. She helped conceptualise the research design, led the quantitative data analysis, and made a significant contribution to reviewing and improving the manuscript.
Ethical Approval
The University of Notre Dame Australia Human Research Ethics Committee (HREC) has provided ethical approval for the research (Approval Number 017066F).
Acknowledgement
The authors acknowledge the thoughtful and insightful feedback provided by staff and students.
Funding
No internal or external funding was sought to conduct this research.
Declaration of Interest
There is no conflict of interest to declare.
References
Bate, F., Fyfe, S., Griffiths, D., Russell, K., Skinner, C., & Tor, E. (2020). Does an incremental approach to implementing programmatic assessment work: Reflections on the change process. MedEdPublish, 9(1), 55. https://doi.org/10.15694/mep.2020.000055.1
Bate, F., Macnish, J., & Skinner, C. (2016). The cart before the horse? Exploring the potential of ePortfolios in a Western Australian medical school. International Journal of ePortfolio, 6 (2), 85-94.
Bhat, C., Burm, S., Mohan, T., Chahine, S., & Goldszmidt, M. (2018). What trainees grapple with: A study of threshold concepts on the medicine ward. Medical Education, 52(6), 620–631. https://doi.org/10.1111/medu.13526
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77-101. https://doi.org/10.1191/1478088706qp063oa
Candy, P. (2006). Promoting lifelong learning: Academic developers and the university as a learning organization. International Journal for Academic Development, 1(1), 7-18. https://doi.org/10.1080/1360144960010102
Frei, E., Stamm, M., & Buddeberg-Fischer, B. (2010). Mentoring programs for medical students: A review of PubMed literature 2000-2008, BMC Medical Education, 10(32), 1-14. https://doi.org/10.1186/1472-6920-10-32
Gillis, A., & Jackson, W. (2002). Research for Nurses: Methods and Interpretation. Philadelphia, PA: F.A. Davis Co.
Heeneman, S., & de Grave, W. (2017). Tensions in mentoring medical students toward self-directed and reflective learning in a longitudinal portfolio-based mentoring system – An activity theory analysis. Medical Teacher, 39(4), 368-376. https://doi.org/10.1080/0142159X.2017.1286308
Heeneman, S., & de Grave, W. (2019). Development and initial validation of a dual-purpose questionnaire capturing mentors’ and mentees’ perceptions and expectations of the mentoring process. BMC Medical Education, 19(133), 1-13. https://doi.org/10.1186/s12909-019-1574-2
Kemmis, S., & McTaggart, R. (2000). Participatory action research. In N. K. Denzin & Y. S. Lincoln (Eds.) Handbook of Qualitative Research (2nd Ed.; pp 567-606). New York: Sage Publications.
Kirkpatrick, D., & Kirkpatrick, J. (2006). Evaluating Training Programs: The Four Levels (3rd ed.). Oakland, CA: Berrett-Koehler Publishers, Inc.
Kuykendall, B., Janvier, M., Kempton, I., & Brown, D. (2012). Interactive whiteboard technology: Promise and reality. In T. Bastiaens & G. Marks (Eds.), Proceedings of E-Learn 2012 – World Conference on E-Learning in Corporate, Government, Healthcare, and Higher Education 1 (pp. 685-690). Retrieved from Association for the Advancement of Computing in Education (AACE), https://www.learntechlib.org/p/41669
Meeuwissen, N., Stalmeijer, R., & Govaerts, M. (2019). Multiple-role mentoring: Mentors conceptualisations, enactments and role conflicts. Medical Education, 53, 605-615. https://doi.org/10.1111/medu.13811
Richter, D., Kunter, M., Lüdtke, O., Klusmann, U., Anders, Y., & Baumert, J. (2013). How different mentoring approaches affect beginning teachers’ development in the first years of practice. Teaching and Teacher Education, 36, 166-177. https://doi.org/10.1016/j.tate.2013.07.012
Sambunjak, D. (2015). Understanding the wider environmental influences on mentoring: Towards an ecological model of mentoring in academic medicine. Acta Medica Academia, 44(1), 47-57. https://doi.org/10.5644/ama2006-124.126
Standing Committee on Postgraduate Medical and Dental Education. (1998). Supporting Doctors and Dentists at Work: An Enquiry into Mentoring. London: SCOPME.
Stenfors-Hayes, T., Hult, H., & Owe Dahlgren, L. (2011). What does it mean to be a mentor in medical education? Medical Teacher, 33(8), 423-428. https://doi.org/10.3109/0142159X.2011.586746
Waljee, J. F., Copra, V., & Saint, S. (2018). Mentoring Millennials. JAMA, 319(15), 1547-1548. https://doi.org/10.1001/jama.2018.3804
*Frank Bate
Medical and Health Professional Education,
School of Medicine Fremantle,
University of Notre Dame Australia,
PO Box 1225, Fremantle,
Western Australia 6959
Telephone: +66 9433 0944
Email address: frank.bate@nd.edu.au
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









