Why do Team-Based Learning educators use TBL?
Published online: 2 January, TAPS 2018, 3(1), 38-41
DOI: https://doi.org/10.29060/TAPS.2018-3-1/SC1040
Sean Wu1, Julia Farquhar1, 2, Scott Compton1
1Duke-NUS Medical School, Singapore; 2School of Medicine, Duke University, USA
Abstract
Aim: Evidence suggests that Team Based Learning (TBL) is an effective teaching method for promoting student learning. Many people have also suggested that TBL supports other complex curriculum objectives, such as teamwork and communication skills. However, there is limited rigorous, substantive data to support these claims. Therefore, the purpose of this study was to assess medical educators’ perceptions of the outcomes affected by TBL, thereby highlighting the specific areas of TBL in need of research.
Methods: We reviewed the published research on TBL in medical education, and identified 21 unique claims from authors regarding the outcomes of TBL. The claims centred on 4 domains: learning, behaviours, skills, and wellbeing. We created a questionnaire that asked medical educators to rate their support for each claim. The survey was distributed to the medical educators with experience teaching via TBL and who were active users of the Team Based Learning Collaborative listserv.
Results: Fifty responses were received. Respondents strongly supported claims that TBL positively impacts behaviours and skills over traditional, lecture based teaching methods, including the promotion of self-directed learning, active learning, peer-to-peer learning, and teaching. In addition, respondents strongly supported claims that TBL promotes teamwork, collaboration, communication and problem solving. Most participants reported that TBL is more effective in promoting interpersonal, accountability, leadership and teaching skills.
Conclusion: Medical educators that use TBL have favourable perceptions of the practice across a variety of domains. Future research should examine the actual effects of TBL on these domains.
Keywords: Team Based Learning; Medical Education; Teaching
I. INTRODUCTION
Team-based learning (TBL), originally developed for use in business schools, is now a growing teaching modality in medical education. The process of TBL is comprised of three components: advance preparation, individual and team readiness assurance tests (RATs), and in-class application of content through team exercises (Parmelee, Michaelsen, Cook, & Hudes, 2012). In a TBL course, students are typically assigned into teams of 5 to 7, and receive preparatory materials before class. At the beginning of the TBL process, each individual completes a readiness assurance test (I-RAT). Students next re-take the same readiness assurance test during class as a team (T-RAT), reaching consensus to select a single best answer, and receive immediate feedback. Students typically then have the option to write evidence-based appeals for their wrong answers, and finally an instructor clarifies lingering questions. Following the readiness assurance phase, the teams then work on solving applied problems, followed by whole class discussions. Evidence suggests that TBL is a popular teaching modality, with approximately one-third of US schools and colleges of pharmacy implementing it into the curriculum (Allen et al., 2013).
A number of studies have shown TBL to be as academically effective or more effective than traditional lecture-based courses by promoting mastery over several core medical subjects (Fatmi, Hartling, Hiller, Campbell, & Oswald, 2013; Koles, Stolfi, Borges, Nelson, & Parmelee, 2010; Nieder, Parmelee, Stolfie, & Hudes, 2005). These studies have focused specifically on the academic outcomes of TBL, yet TBL as a teaching modality is often assumed to support complex curriculum objectives such as teamwork and communication skills. Despite these assumptions, little substantive data exists to support these claims. For the current body of research to progress and to improve our understanding of the true effects of TBL, these assumed outcomes need to be explicitly described and articulated. Following which, individual outcomes can be studied and interventions can be proposed to further develop TBL as a medical teaching modality. Therefore, the purpose of this study was to assess TBL medical educators’ perceptions of the outcomes affected by TBL, thereby providing a framework for future research.
II. METHODOLOGY
A. Development of Questionnaire
We identified 21 claims of the positive effects of TBL in various published papers and textbooks. We categorized these claims into 4 domains: learning, behaviours, skills, and well-being. Examples of references to each claim are available from the corresponding offer. We subsequently compiled those claims and used them as the basis for a questionnaire in order to assess the support for each claim among TBL users.
The final questionnaire consisted of 6 demographic questions, followed by the claims within each domain: learning (4 questions), behaviours (4 questions), skills (8 questions) and wellbeing (5 questions). In addition, we asked 3 questions related to the extent that TBL skills learned in classroom settings translates to clinical settings.
Cognitive interviews were conducted with ten TBL educators to determine if the questions were clear and interpreted as intended. Relevant edits were made and the questionnaire was revised. We then assessed reliability using the test-retest method. Eight TBL educators responded to the questionnaire twice within two weeks. The test-retest reliability of the instrument was 0.927 (df = 8, p<0.001) based on Spearman’s correlation coefficient, thus demonstrating its suitability for research use.
B. Dissemination
The final survey was uploaded onto surveymonkey.com and submitted to the Team-Based Learning Collaborative (TBLC) listserv with a request for medical educators to respond. The TBLC listserve is comprised of people interested in TBL, and is open to all educators. The introductory email made explicit that medical educators were the target of the survey.
III. RESULTS
A total of 50 medical educators replied. The participants were a seasoned group of medical educators, having an average of 14 years’ experience in the field. Most respondents were senior faculty members (25% professor, 36% associate professors), while 19% were assistant professors and 20% had other academic appointments. Overall the respondents had substantial experience in using TBL: 96% had created TBL materials, 98% had facilitated TBL discussions, and 78% had designed course curriculum with TBL as the primary educational modality.
As shown in Figure 1, respondents tended to strongly support the various claims that suggest TBL positively impacts learning, behaviour, and skills. In fact, most participants reported that TBL promotes “Deep Learning” and “Application of knowledge” much more, 83% and 98% respectively, than conventional lecture based modalities. Nearly all (96%) reported that TBL is more effective in promoting retention of knowledge than lecture and most (64.5%) replied that TBL is more effective in promoting breadth of knowledge. A minority (25%) of respondents indicated that there is no difference between the two teaching modalities in student learning.
In terms of student behaviour, respondents reported that TBL promotes self-directed learning, active learning, peer-to-peer learning and teaching much more than lecture based teaching modalities. Most (98%) answered that TBL is more effective in teaching self-directed learning, peer-to-peer learning, and peer-to-peer teaching than lecture. All answered that TBL promotes active learning more than traditional lecture based teaching. Only one replied that TBL and lecture-based teaching are equally effective in promoting the aforementioned student behaviours.
Most respondents replied that TBL is more effective than lecture-based teaching in promoting a multitude of student skills. All answered that TBL is better at promoting teamwork, collaboration, communication and problem solving. Most of participants reported that TBL is more effective in promoting interpersonal, accountability, leadership and teaching skills.
Figure 1 also demonstrates that there is less support for the claims surrounding TBL promotion of wellbeing. Nearly half (44%) of the respondents answered that TBL resulted in more competition than lecture-based teaching whereas a quarter replied the opposite. Half reported that TBL leads to more anxiety whereas a quarter replied otherwise. More than half reported that TBL promoted empathy more so than lecture, whereas 35% of respondents were unsure or thought the two teaching modalities equal. Most respondents answered that lecture-based teaching was easier than TBL, yet also answered that TBL was more enjoyable. Interestingly, respondents also reported that TBL-learned skills translated well to the clinical setting. Most, 89.5%, 83.3%, and 66.7% respectively, answered that teamwork, communication, and leadership skills learned in a TBL classroom were applicable to the clinical rotations.
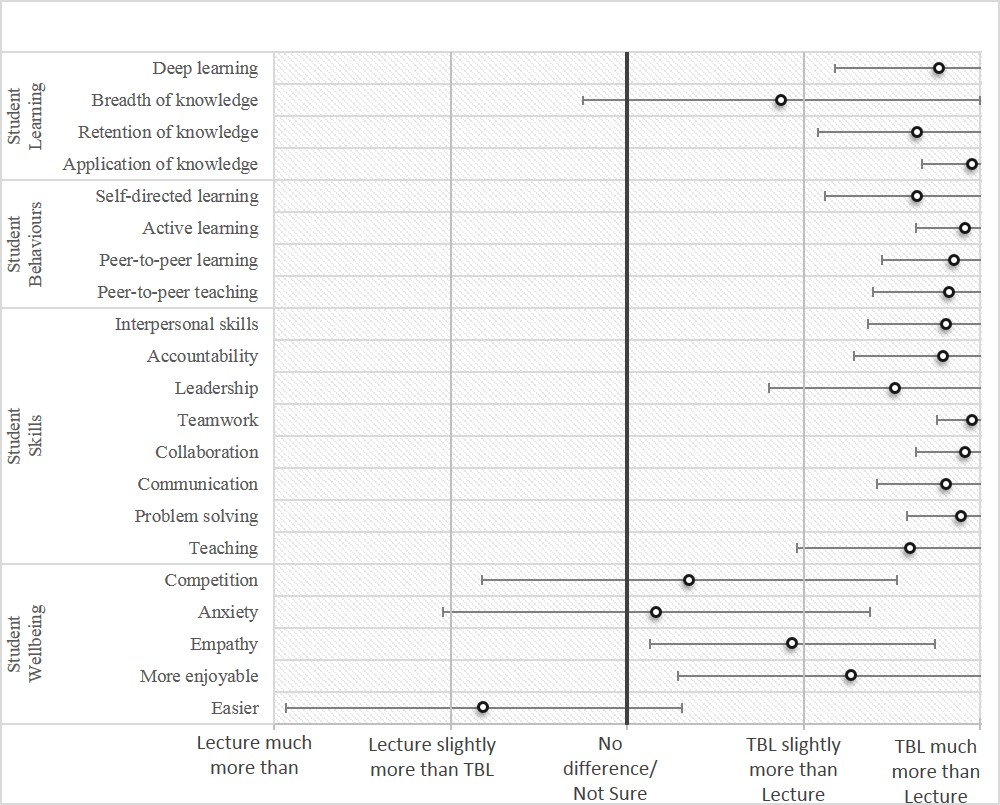
Figure 1. Medical educators’ ratings: lecture-based teaching versus team based learning in promoting different skills
IV. DISCUSSION
The results of the study indicate that TBL medical educators believe TBL to be better than traditional lecture-based teaching in achieving a vast variety of outcomes. According to the survey results, educators believe that TBL promotes students’ mastery of subject content by encouraging deep and active learning as well as the retention and application of knowledge. They also believe that TBL develops behaviours such as peer-to-peer learning and teaching. An important point is that most TBL educators believe TBL fosters development of key skillsets such as accountability, teamwork, collaboration, and communication that play vital roles in the successful transition of students from classroom learning to clinical clerkships. Yet respondents to this survey may be wary that TBL may negatively affect student wellbeing by increasing competition and difficulty. Interestingly, many of the TBL educators appeared confident that TBL aids in the development of medical students that are independent learners, teamwork-oriented and effective leaders. However, to date, there is little substantive data to suggest that any of these claims are true. Likewise, there was strong support for the notion that skills learnt in classroom TBL sessions translate to the clinical setting. Again, little evidence currently exists to support this claim.
This study is limited by the small convenience sample drawn from the TBL collaborative listserv. The participants may not be representative of TBL educators as a whole. However, the participant profiles reveal that these respondents have extensive experience in medical education and using TBL in the classroom.
V. CONCLUSION
This study should serve as a call to action to educational researchers to investigate the claims of the effects of TBL, particularly those associated with non-academic factors, such as teamwork, leadership, and communication. In fact, the results of this study could serve as the foundation for future research. Ensuing studies can provide evidence towards determining the validity of these assumptions, thereby providing direction for the development of TBL as a teaching modality in medical education.
Notes on Contributors
Sean Wu, MD, is a graduate of the Duke-NUS Medical School and currently an Internal Medicine resident at NUHS. Julia Farquhar is a medical student at the Duke School of Medicine, Durham, NC, USA.
Scott Compton, PhD, is the Associate Dean and Associate Professor of Medical Education, Research, and Evaluation at Duke-NUS Medical School.
Ethical Approval
The approval for this study was obtained from the Institutional Review Board, National University of Singapore.
Declaration of Interest
The authors declare that they have no competing interests.
References
Allen, R. E., Copeland. J., Franks, A. S., Karimi, R., McCollum, M., & Riese, D. J. (2013). Team-based learning in US colleges and schools of pharmacy. The American Journal of Pharmaceutical Education, 77(6). DOI: 10.5688/ajpe776115
Fatmi, M., Hartling, L., Hillier, T., Campbell, S., & Oswald, A.E. (2013). The effectiveness of team-based learning on learning outcomes in health professions education: BEME Guide No. 30. Medical Teacher, 35(12), 1608-24. DOI: 10.31.09/0142159X.2013.849802
Koles, P. G., Stolfi, A., Borges, N. J., Nelson, S., & Parmelee, D.X. (2010). The impact of team-based learning on medical students’ academic performance. Academic Medicine, 85(11), 1739-1745. DOI: 10.1097/ACM.0b013e3181f52bed
Nieder, G. L., Parmelee, D. X., Stolfi, A., & Hudes, P. D. (2005). Team‐based learning in a medical gross anatomy and embryology course. Clinical Anatomy, 18(1), 56-63. DOI: 10.1002/ca.20040
Parmelee, D., Michaelsen, L.K., Cook, S., & Hudes, P.D. (2012). Team-based learning: A practical guide: AMEE Guide No. 65. Medical Teacher, 34(5), e275-e287. DOI: 10.3109/0142159X.2012.651179
* Scott Compton, PhD
Medical Education, Research and Evaluation Department
Duke-NUS Medical School
8 College Road, Singapore 169857.
Tel: +65 6601 1565.
Email: scott.compton@duke-nus.edu.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









