Using video in medical education: What it takes to succeed
Published online: 5 September, TAPS 2017, 2(3), 15-21
DOI: https://doi.org/10.29060/TAPS.2017-2-3/OA1034
Eng-Tat Ang1, Siti Nabihah Binte Abu Talib1, Mark Thong2 & Tze Choong Charn2
1Department of Anatomy, Yong Loo Lin School of Medicine, National University Health System, Singapore; 2Department of Otolaryngology, Sengkang Hospital, Singhealth, Singapore
Abstract
Videos when properly embedded within the curriculum might make learning the basic sciences such as human anatomy much more engaging for medical students. It is unclear how the use of video is advantageous. Possible scientific causations for such an observation include visual and auditory stimulation, coupled with ease of access for the learner. Video usage empowers the medical students to learn in an active manner. However, this cannot happen if motivation for self-directed learning is lacking. This research aims to 1) Elucidate qualitative and quantitative comments on how videos help to enhance anatomy learning. 2) Quantify the level of motivation for self-directedness in order for videos to be impactful amongst medical students. A short video was embedded into selected part of the 1st year anatomy curriculums (pharynx and larynx) for selected medical students (n=100). Separately, all students in the cohort (n=300) were assessed for their attitude towards active learning via a survey on motivation levels. This was done using the modified PRO-SDLS. Results showed that 85% of the participants enjoyed learning the anatomy of the pharynx and larynx with embedded videos (P<0.05). Specifically, they liked the Q&A sessions, the virtual chat platform, and the mode of delivery. Participants perceive it to be clearer, and more structured (P<0.05). Concomitantly, all medical students surveyed exhibited unusually high motivation for self-directed learning (³ agreeing with probe questions in the PRO-SDLS) (P<0.05). This allows videos to be impactful. In conclusion, with videos, medical students appreciated the relevance of basic regional anatomy more in a statistically significant manner compared to controls. However, a threshold motivation is required for active learning to be successful.
Keywords: Video; ENT Anatomy; Feedback; Medical Education
Practice Highlights
- Medical students are generally an intrinsically self-driven group so didactic lectures may not be the optimal way to teach them.
- An appropriate short video embedded in the curriculum will trigger active learning amongst medical students.
- A certain threshold for Self-directedness (motivation) must be present for videos to be impactful.
I. INTRODUCTION
The use of video is fast becoming popular within medical education (Baldwin et al., 2016; Dong & Goh, 2015). In the larger scheme of academic medicine, the advent of media such as YouTube and Dailymotion coupled with ease of access to electronic gadgets and the internet is threatening the traditional way of learning (Egle, Smeenge, Kassem, & Mittal, 2015; Hansen et al., 2016; Pusz & Brietzke, 2012). Furthermore, expectations of millennial medical students, and the teaching-learning environments in general, are slowly but surely evolving (Lim & Seet, 2008; Youm & Wiechmann, 2015). More importantly, the learning and resource gathering habits of medical students and residents are also changing, as they depend increasingly on audio-visuals to score better in examinations (Ahmad, Sleiman, Thomas, Kashani, & Ditmyer, 2016). Specifically in the context of anatomy education, millennials often resort to YouTube videos to further enhance their learning (Barry et al., 2016). Taken together, medical education as we once know is under considerable pressure to change. In the face of these developments, teachers need to adopt newer teaching-learning techniques and delivery methods. One such modality is the usage of videos. So what does it take to make this endeavour really successful? The scientific basis for this observation is unclear. It could be the result of an array of factors but was recently explained using the science of learning (Mayer, 2010). All things considered, it is crucial that faculty members reinvent themselves to stay on top of the challenges, and to customise their institution´s curriculum to match and complement student´s needs. This will ensure accurate and proper dissemination of relevant knowledge, as well as scholarly information (Egle et al., 2015; Pusz & Brietzke, 2012; Volsky, Baldassari, Mushti, & Derkay, 2012). Traditionally, at the Yong Loo Lin School of Medicine (YLLSoM), National University of Singapore (NUS), medical students have learnt human anatomy from a well-wrought system of lectures, practical classes and small group tutorials (Ang et al., 2012). In recent times, due to curricular reforms, lecture times are proposed to be shortened, and in place of it, more interactive sessions. One initiative is the use of videos to trigger active learning, leaving more time for interactions, questions and answers (Q&A), and for reflections. A quick literature review shows that the use of multimedia (videos) to achieve such aims has been attempted in other parts of the world, with fairly convincing outcomes (Catling, Williams, & Baker, 2014; Soh, Reed, Poulos, & Brennan, 2013). These include drug prescriptions, detecting radiological lesions, and in general pathology education (Thakore & McMahon, 2006). We hope to emulate this pedagogy to teach medical students basic anatomy of the ear, nose, and throat (ENT) in a clinically-orientated manner at this institution. We believe this endeavour will help medical students in their anatomy education, and to help teachers understand the values of videos, and to further encourage buy-ins from key stake holders (Calaman et al., 2016; Choi-Lundberg, Low, Patman, Turner, & Sinha, 2016). We hypothesize that students will enjoy learning from videos in class, and its success hinges on having a high level of self-directedness (motivation) in learning.
II. METHODS
The entire first year medical students cohort (M1) from the YLLSoM (n=300) was recruited for the research, and surveyed using the Personal Responsibility Orientation to Self-Direction in Learning Scale (PRO-SDLS) (Stockdale & Brockett, 2011). This is to ascertain, and assess the level of baseline self-directedness/ motivation in their daily learning. They were polled on how much they agree with a list of statements provided in the modified scale (See Appendix). The responses are categorised by a Likert scale involving 5 options – “Strongly agree”, “Agree”, “Sometimes”, “Disagree” and “Strongly disagree” (Komorita, 1963). This is to quantify the 4 domains, namely: 1) Initiatives; 2) Control; 3) Self-efficacy; 4) Motivation.
A. Participants
In the research, selected medical students from the M1 cohort (n = 100; equal number of males and females; 19-21 years old) were asked to provide qualitative and quantitative feedback with regards to videos in ENT anatomy education. As a pre-requisite, it is assumed that these students would have also already attended all lectures and practical classes pertaining to the anatomy of the pharynx and larynx.
1) Without video: All students in the cohort were educated through a system of lectures, practical classes, and tutorials based on a prescribed list of objectives outlined at the beginning of the class. The lecture was covered in a didactic manner, and the tutorials manned by different tutors (n=16) using varying techniques in engaging these students. However, there was no active learning using any prescribed videos.
2) With video: The following links were provided for these students:
(1)http://vidcast.nus.edu.sg/camtasiarelay/Pharynx_Larynx_-_20150211_183654_26.html
A video was embedded into the tutorial teaching the head and neck anatomy (Dr. Ang’s group), and students were instructed to view them before coming to class. Controls for the intervention were the rest of the cohorts. The video (~15 minutes duration), features an introduction, learning objectives, demonstrations, self-tests using plastic anatomical models, clinical anatomy via endoscopy and fluoroscopy images. After tackling the questions individually, the group received feedback, and was given the opportunity to raise questions via an electronic bulletin board. During the class, participants were further directed to other learning resources in the Internet. To consolidate the learning, students were allowed to review the videos ad libitum, interact with classmates, and post questions to their tutor via the bulletin board. Both qualitative and quantitative feedback were obtained and tabulated from the surveys and observations based on best practice (Kelley, Clark, Brown, & Sitzia, 2003; Tai & Ajjawi, 2016), and this was carried out before and at the end of the intervention. At the end of session, all participants need to fill up the post-PRO-SDLS survey.
B. Data Analysis
The PRO-SDLS data from the entire cohort was collected via SurveyMonkey® (online). Further analysis, descriptive statistics and graphs were generated using the SPSS 24 with ad hoc consultation with the faculty Biostatistician. Whenever possible, the non-parametric Mann Whitney test was carried out to test any significant difference between participants’ perception towards the use of the video versus the control. In instances when there were 2 or more categories, the ANOVA test was used. Next, the binary logistic regression model (see Fig.1) was used to estimate and further predict the amount of self-directedness (motivation) required for videos to be impactful in medical education, all in the context of ENT anatomy education. Approval for the study was granted by the NUS institutional review board (NUS IRB B-15-186).
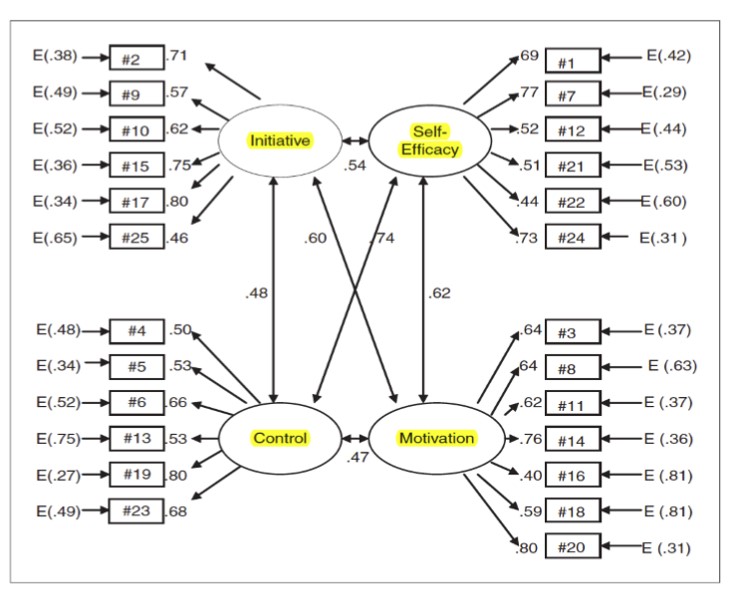 Note: Bidirectional arrows denote interrelation. E = Error. Figure 1. The PRO-SDLS allows the investigators to gauge the levels of initiative, self-efficacy, control and motivation in the participants. These domains have been proven to be important in the learning process for adults (Stockdale & Brockett, 2011).
Note: Bidirectional arrows denote interrelation. E = Error. Figure 1. The PRO-SDLS allows the investigators to gauge the levels of initiative, self-efficacy, control and motivation in the participants. These domains have been proven to be important in the learning process for adults (Stockdale & Brockett, 2011).
III. RESULTS
A. Modified PRO-SDLS survey
The online response rate for the pre-PRO-SDLS survey was a dismay 5-15% of the cohort. However, in the corresponding author’s groups, the responses were 100% for both pre- and post-PRO-SDLS respectively. The results demonstrated some statistical differences in trends across the 25 questions, and the 4 considered domains with video as an intervention. Specifically designed to measure self-directedness, the pre-modified PRO-SDLS revealed that medical students exhibited “Initiative” (≥85% responding agreed or strongly agreed), “Control” (≥80% responding agreed or strongly agreed), “Self-efficacy” (≥80% agreed or strongly agreed) and “Motivation” (≥75% agreed or strongly agreed). With regression modelling, it was further estimated that when “Initiative”, “Control” and “Self-efficacy” were increased, motivation was likely to be increased further, and hence more active learning.
1) Qualitative comments: Based on the feedback, participants like embedded videos during tutorial because it empowered them to learn at their own pace. In addition, the audio-visuals facilitated their learning. This was evidently expressed by some students when they articulated: “…We could pause and replay certain segments whenever in doubt…” and “….The images and audio aided our understanding of the subject matter…..”. Furthermore, the pre-video and post-video tests were very much appreciated by the students as it generated opportunities for discussion with peers and real opportunities to see if one has really understood the subject. This was opined by some students as follows: “ ……..The Q&A helps to make it interactive and helps to clear doubts……….” and “……….I found that the pedagogy (pre-test + video + interactive session) helped me learn the content better” and “……I was given an opportunity to participate actively in discussion with my classmates…….” Generally, students did not perceive the usage of technology as disruptive to their learning process. This was apparent when some students expressed the following: “…….the usage of “Pigeonhole” helped me to interact more effectively with the teacher……..” and “……using the “keypad” helped me learn more efficiently…….”. It appears that the embedded video in the tutorial was beneficial to the student’s learning process, and the use of technology was not getting into the way of learning as some have suggested otherwise.
2) Quantitative comments: As shown in Fig.2, when polled (A) “The video adequately helped me learn the anatomy”, participants mostly agreed (53%) or strongly agreed (31%) that it did so but some indicated disagreement (13%); (B) “Learning with video promoted more interaction”, the responses were largely positive, strongly agreed (26%) and agreed (44%) while the rest disagreed; (C) “The bulletin helped me to answer my queries”, the responses were strongly agreed (46%) and agreed (37%) while some disagreed (17%). It appears that the participants appreciated learning ENT anatomy better in this manner (all p < 0.05, ANOVA). Moreover, they mostly agreed that the mode of delivery using anatomical models was clinically relevant for their learning but this did not reach statistical significance (p > 0.05). It was also discovered that traits like “Self-efficacy” and “Control” were negatively correlated with the affinity for video learning. However, “Motivation” and “Initiative” were determined to be positively correlated with wanting to learn from videos (p < 0.05) (see Fig.3).
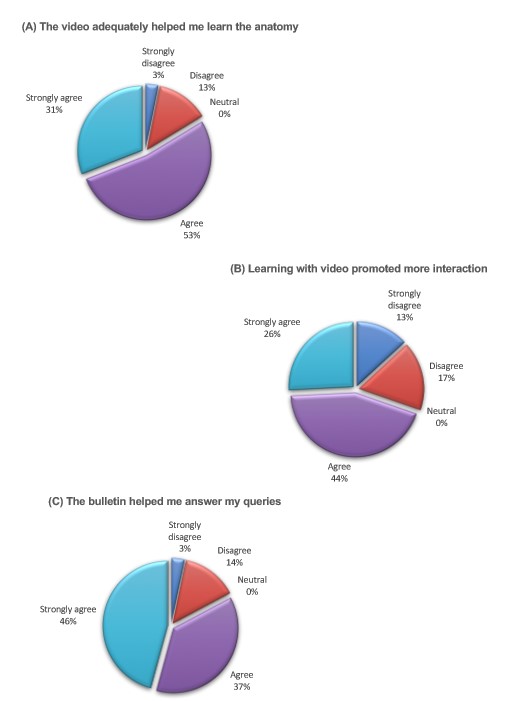
Figure 2. Quantitative results of student’s attitude towards video usage.
Pie charts illustrating the degree of agreement to: (A) The video adequately helped me learn the anatomy. (B) Learning with video promoted more interaction. (C) The bulletin helped me answer my queries.
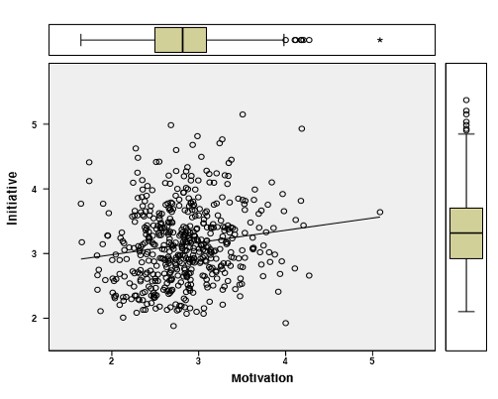
Figure 3. Regression modelling: Using other independent variables in PRO-SDLS to predict and estimate the level of dependent variable “Motivation” required to achieve active learning of ENT anatomy in medical students. “Initiative” and “Motivation” was positively correlated with wanting to learn from videos.
IV. DISCUSSION
Previous studies have described benefits associated with the blended approach of studying to a variety of subject matters, including human anatomy (Catling et al., 2014; Durham, Brettell, Summerside, & McHanwell, 2009; Pereira et al., 2007). In fact, participants in one of the research project definitively outperformed those in the traditional curriculum (Pereira et al., 2007). Specifically, videos have been shown to be just as effective, if not better than conventional histology classes (Rosenberg et al., 2006). This clearly demonstrated the ability of videos to engage students, and to inculcate active learning of the subject matter. All things considered, because of the many independent variables involved (different teachers, presentation formats, and depth of coverage), it remains a challenge to categorically say with absolute certainty, that the use of videos actually enhance the learning process. Indeed, very often, such benefits were simply students’ opinions about the use of such a modality (participants might like it but their academic performance was not improved). We gathered from this research that participants generally appreciated the video presentations for ENT anatomy education, especially the endoscopic segment (Yanagisawa, 1994), as it helped them to understand and apply the knowledge (Mayfield, Ohara, & O’Sullivan, 2013) in a clinically relevant context. Importantly, it allows participants to appreciate anatomy from an “inside” perspective. This would have been impossible in a traditional class using dissected specimens. The participants also enjoyed the opportunity to interact with their peers during, and after the session compared to a conventional class whereby interaction was lacking. Interestingly, some would like the video to be even longer, and with more details included (Egle et al., 2015). They also reported that the pre-tests and post-tests stimulated them to apply, and retain their knowledge more effectively.
To further understand how the use of videos triggered active learning, we decided to use the modified PRO-SDLS to measure the 4 critical domains in behavioural sciences. These were namely: 1) Initiatives 2) Control 3) Self-efficacy 4) Motivation. On careful analysis, there were differences between the 4 domains after the video intervention (p< 0.05). We believed that the visuals and audios inherent of the video, possibly could have enhanced self-directed drive, in a manner that is time and teacher independent (Mayer, 2010). However, it should be noted that there are still inherent controversies regarding the use of such a scale (PRO-SDLS versus other scales) to validate the many variables (Hoban, Lawson, Mazmanian, Best, & Seibel, 2005; McBride, 1987), so any strict interpretation should be avoided, bearing in mind possible caveats (Hoban et al., 2005) (e.g. subjectivity amongst interpreters). Nonetheless, we were energised by this form of blended teaching (video). In the next phase of our research, we would like to collect and analysed the academic results of participants exposed to video and compare this to the rest of the cohort.
In all honesty, there were some who resisted the use of videos in class (<5% of participants). Here, we need to understand and interpret these outliers carefully. Individual tutors conduct their classes differently, and therefore the degree of interactions varies considerably. We are aware that didactic classes have their benefits, but we opined that videos would encourage more interactions and active learning. Students enjoyed the privilege to review the contents at their own pace, with the possibility to revise pertinent sections. They also felt that the interactions with their tutor, and fellow classmates would further enhance their learning of the subject matter. In essence, it was unanimously agreed that an effective education should not be a didactic monologue, but instead a dialogue between teachers and students.
Both faculty and students are aware that technology certainly could impact their education, but it has to be done in a non-disruptive manner. For instance, all students could view the content together on the projector as a group so that there would be better synergy and dynamics. The Q&A was particularly welcomed by the participants, and helped to reinforce the key issues. Collectively, most of these comments were in line with an earlier study (Mayfield et al., 2013), presenting clinical scenarios appeared to aid students in their contextual learning so that there was less rote memorisation involved. Students appeared very receptive and excited about the application of anatomy to ENT settings.
From the tutor’s perspective, the use of technology to enhance teaching continues to be a love-hate relationship as there would be a reduction in didactic teaching time with the students. However, this could be compensated by more thought provoking interactions during the Q&A session. There was informal consensus amongst tutors (personal communication) that using new technological platform to deliver contents, involves a huge investment of time, energy, and resources. This is indeed very real for the presenter in the video, as he struggled with initial conceptualisation, work flow, and how to engage the students via this approach. While it is true that all teaching involves much deliberate planning, teaching also involves spontaneity and “thinking on the spot”. In this regard, technology and pre-recorded videos may very well inhibit this.
A) Limitations and recommendations
A significant limitation of this project is the lack of direct correlation between exposure to videos and examination outcome, hence there is no way to determine its superiority. Furthermore, one needs to be mindful that the competence of the teachers versus the rest of the colleagues teaching the cohort, should be taken into consideration. We also assume that participants in the study responded in a faithful and thoughtful manner. There were reports suggesting that students do not take surveys seriously (Slade & McConville, 2006). It will be good if future version of such videos could include the following: 1) More interactive quizzes with feedback scores and answers, 2) Case scenarios to strengthen anatomical knowledge, 3) Practice board examination questions.
On a separate note, the outreach of the internet is unquestionable but there were recent alarming reports suggesting that the information found in it may be inaccurate to varying degrees (Egle et al., 2015; Pusz & Brietzke, 2012; Volsky et al., 2012). Students and residents should therefore be more discerning when consulting the internet, during their learning of basic and clinical subjects, and patient management subsequently (Pusz & Brietzke, 2012).
B) Conclusions
We have shown there are value-adding benefits associated with embedded videos in medical teachings, and especially so in anatomy education. Medical students have expressed interest in the use of videos but one has to explore avenues to incorporate it to maximise its benefits (Chan & Robbins, 2006). In addition, we have alluded that a threshold of self-directedness, curiosity and intrinsic motivation must be present in the students in order for videos to be impactful, as pointed out by others (Oudeyer, Gottlieb, & Lopes, 2016). Faculty members should be ready to embrace modalities such as video to enhance their teaching. They should be cognisant that students’ learning behaviours have changed since their own experience some decades ago.
Notes on Contributors
Eng-Tat Ang designed the study, collected and analysed the data, and wrote the first draft of this manuscript. Siti Nabihah Binte Abu Talib contributed ideas, collected and analyzed the data. Tze Choong Charn and Mark Thong acted as clinical consultants to this project. Dr Charn provided critical multimedia files that were embedded into the videos. He also revised the manuscript and provided helpful comments. All authors approved the version submitted for review.
Acknowledgements
The authors are grateful to Mr Yeo Su Ping (CenMed, NUS), Ms Caroline (EduTech, YLLSoM) and Ms Wong Hung Chew (Biostatistician) for their input and technical assistance.
Declaration of Interest
The authors declare no conflict of interest.
References
Ahmad, M., Sleiman, N. H., Thomas, M., Kashani, N., & Ditmyer, M. M. (2016). Use of High-Definition Audiovisual Technology in a Gross Anatomy Laboratory: Effect on Dental Students’ Learning Outcomes and Satisfaction. Journal of Dental Education, 80(2), 128-132.
Ang, E. T., Sugand, K., Hartman, M., Seow, C. S., Bay, B. H., & Abrahams, P. (2012). Singapore’s anatomical future: quo vadis? Anatomical Sciences Education, 5(4), 234-240.
Baldwin, A. C., Mallidi, H. R., Baldwin, J. C., Sandoval, E., Cohn, W. E., Frazier, O. H., & Singh, S. K. (2016). Through the Looking Glass: Real-Time Video Using ‘Smart’ Technology Provides Enhanced Intraoperative Logistics. World Journal of Surgery, 40(1), 242-244.
Barry, D. S., Marzouk, F., Chulak-Oglu, K., Bennett, D., Tierney, P., & O’Keeffe, G. W. (2016). Anatomy education for the YouTube generation. Anatomical Sciences Education, 9(1), 90-96.
Calaman, S., Hepps, J. H., Bismilla, Z., Carraccio, C., Englander, R., Feraco, A., . . . Committee, I. P. S. E. E. (2016). The Creation of Standard-Setting Videos to Support Faculty Observations of Learner Performance and Entrustment Decisions. Academic Medicine, 91(2), 204-209.
Catling, F., Williams, J., & Baker, R. (2014). A prescribing e-tutorial for medical students. Clinical Teacher, 11(1), 33-37.
Chan, C. H., & Robbins, L. I. (2006). E-Learning systems: promises and pitfalls. Academic Psychiatry, 30(6), 491-497.
Choi-Lundberg, D. L., Low, T. F., Patman, P., Turner, P., & Sinha, S. N. (2016). Medical student preferences for self-directed study resources in gross anatomy. Anatomical Sciences Education, 9(2), 150-160.
Dong, C., & Goh, P. S. (2015). Twelve tips for the effective use of videos in medical education. Medical Teacher, 37(2), 140-145.
Durham, J. A., Brettell, S., Summerside, C., & McHanwell, S. (2009). Evaluation of a virtual anatomy course for clinical undergraduates. European Journal of Dental Education, 13(2), 100-109.
Egle, J. P., Smeenge, D. M., Kassem, K. M., & Mittal, V. K. (2015). The Internet School of Medicine: Use of Electronic Resources by Medical Trainees and the Reliability of those Resources. Journal of Surgical Education, 72(2), 316-320.
Hansen, C., Interrante, J. D., Ailes, E. C., Frey, M. T., Broussard, C. S., Godoshian, V. J., . . . Gilboa, S. M. (2016). Assessment of YouTube videos as a source of information on medication use in pregnancy. Pharmacoepidemiology Drug Safety, 25(1), 35-44.
Hoban, J. D., Lawson, S. R., Mazmanian, P. E., Best, A. M., & Seibel, H. R. (2005). The Self-Directed Learning Readiness Scale: a factor analysis study. Medical Education, 39(4), 370-379.
Kelley, K., Clark, B., Brown, V., & Sitzia, J. (2003). Good practice in the conduct and reporting of survey research. International Journal for Quality in Health Care, 15(3), 261-266.
Komorita, S. S. (1963). Attitude Content, Intensity, and the Neutral Point on a Likert Scale. Journal of Social Psychology, 61, 327-334.
Lim, E. C., & Seet, R. C. (2008). In-house medical education: redefining tele-education. Teaching and Learning in Medicine, 20(2), 193-195.
Mayer, R. E. (2010). Applying the science of learning to medical education. Medical Education, 44(6), 543-549.
Mayfield, C. H., Ohara, P. T., & O’Sullivan, P. S. (2013). Perceptions of a mobile technology on learning strategies in the anatomy laboratory. Anatomical Sciences Education, 6(2), 81-89.
McBride, S. (1987). Validation of an instrument to measure exercise of self-care agency. Research in Nursing & Health, 10(5), 311-316.
Oudeyer, P. Y., Gottlieb, J., & Lopes, M. (2016). Intrinsic motivation, curiosity, and learning: Theory and applications in educational technologies. Progress in Brain Research, 229, 257-284.
Pereira, J. A., Pleguezuelos, E., Meri, A., Molina-Ros, A., Molina-Tomas, M. C., & Masdeu, C. (2007). Effectiveness of using blended learning strategies for teaching and learning human anatomy. Medical Education, 41(2), 189-195.
Pusz, M. D., & Brietzke, S. E. (2012). How good is Google? The quality of otolaryngology information on the internet. Otolaryngology-Head and Neck Surgery, 147(3), 462-465.
Rosenberg, H., Kermalli, J., Freeman, E., Tenenbaum, H., Locker, D., & Cohen, H. (2006). Effectiveness of an electronic histology tutorial for first-year dental students and improvement in “normalized” test scores. Journal of Dental Education, 70(12), 1339-1345.
Slade & McConville (2006) Student Evaluation of Teaching. International Journal for Educational Integrity 2(2), 43-59
Soh, B. P., Reed, W. M., Poulos, A., & Brennan, P. C. (2013). E-tutorial improves students’ ability to detect lesions. Radiologic Technology, 85(1), 17-26.
Stockdale, S. L., & Brockett, R. G. (2011). Development of the PRO-SDLS: A Measure of Self-Direction in Learning Based on the Personal Responsibility Orientation Model. Adult Education Quarterly, 61(2), 161-180.
Tai, J., & Ajjawi, R. (2016). Undertaking and reporting qualitative research. Clinical Teacher, 13(3), 175-182.
Thakore, H., & McMahon, T. (2006). An interactive e-tutorial in pathology. Medical Education, 40(11), 1135.
Volsky, P. G., Baldassari, C. M., Mushti, S., & Derkay, C. S. (2012). Quality of Internet information in pediatric otolaryngology: a comparison of three most referenced websites. International Journal Pediatric Otorhinolaryngology, 76(9), 1312-1316.
Yanagisawa, E. (1994). The use of video in ENT endoscopy: its value in teaching. Ear Nose Throat Journal, 73(10), 754-763.
Youm, J., & Wiechmann, W. (2015). The Med AppJam: a model for an interprofessional student-centered mHealth app competition. Journal of Medical Systems, 39(3), 34.
*Dr. Eng-Tat Ang
Department of Anatomy
Yong Loo Lin School of Medicine
MD10, National University of Singapore
Singapore 117599
Tel: 65168110
Fax: 67787643
Email: antaet@nus.edu.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









