Use of simulation-based learning in Japanese undergraduate nursing education: National survey results
Submitted: 26 January 2021
Accepted: 25 June 2021
Published online: 4 January, TAPS 2022, 7(1), 44-54
https://doi.org/10.29060/TAPS.2022-7-1/OA2471
Mitsumi Masuda1, Machiko Saeki Yagi2 & Fumino Sugiyama3
1Nagoya City University, Nagoya, Aichi, Japan; 2Jichi Medical University, Shimotuke, Tochigi, Japan; 3National College of Nursing, Japan, Kiyose, Tokyo, Japan
Abstract
Introduction: Simulation-based learning (SBL) is a practical and efficient learning method that involves the replacement of a portion of clinical education with quality simulation experiences. It has been utilised in various countries, such as the United States, Canada, and South Korea. However, based on current regulations in Japan, clinical education cannot be replaced with simulation experience. For future curriculum integration, it is necessary to clarify the current use of SBL and tackle systematic educational strategies of SBL. Therefore, this national survey aimed to clarify the prevalence and practices of SBL in undergraduate nursing education programs in Japan.
Methods: This article presents the results of our national survey in Japan. It presents the questionnaire based on the International Nursing Association for Clinical Simulation and Learning Standards of Best Practice and demonstrates the use of simulation-based learning in Japanese undergraduate nursing programs.
Results: Overall, the schools using simulation-based education (SBE) comprised 346 schools (82.4%) of the sample. Those equipped with high-fidelity simulators were 146 schools (27.6%); the rest owned medium-fidelity simulators. Almost all undergraduate nursing education systems were equipped with simulators, however, the frequency of use was low. SBL was incorporated into the curriculum at many undergraduate nursing education institutions, and awareness of the INACSL Standard of Best Practice: SimulationSM was extremely low.
Conclusion: This study shows that SBL is not properly utilised in undergraduate nursing programs, even though many schools are equipped with simulators. Thus, further study on barriers to simulator use is needed.
Keywords: Simulation-based Learning, Curriculum, International Nursing Association for Clinical Simulation and Learning Standard of Best Practice: SimulationSM, Japan, Undergraduate Nursing Education
Practice Highlights
- Almost all undergraduate nursing education programs use SBL.
- The frequency of use of SBL was low in almost all undergraduate nursing education systems.
- SBL was incorporated into the curriculum at many undergraduate nursing education institutions.
- Awareness of the INACSL Standard of Best Practice: SimulationSM was extremely low.
I. INTRODUCTION
A. Use of Simulation-based Learning in Undergraduate Nursing Education
Simulation-based learning (SBL) is a practical and efficient learning method developed in various countries, such as the United States (Zarifsanaiey et al., 2016), Canada (Chiniara et al., 2013), and South Korea (Kim et al., 2016; Shin et al., 2015), that allows aspiring practitioners to experience realistic clinical situations in a safe environment. An overview of past studies on SBL shows that it facilitates high satisfaction, confidence, critical thinking, clinical reasoning, and communication skills in nursing students (Adamson, 2015; Boling & Hardin-Pierce, 2016; Carter et al., 2016). Pal et al. (2018) study showed that learning had progressively improved with each session of simulation with corresponding decrease in stress. Further, the landmark National Council of State Boards of Nursing (NCSBN) National Simulation Study provided evidence that up to 50% of traditional clinical experience can be substituted by simulation in prelicensure nursing programs (Hayden et al., 2014). The results of this study provide substantial evidence that similar outcomes in nursing knowledge, clinical competency and National Council Licensure Examination-Registered Nurse (NCLEX-RN®) pass rates are observable in comparison to 10%, 25% and 50% substitution by simulation (Hayden et al., 2014). As a result, many educators in the United States are examining and revising regulations to allow replacement of a proportion of clinical education with quality simulation experiences (Breymier et al., 2015). The NCSBN study states that substituting simulation for clinical hours requires the use of high-quality simulations (Hayden et al., 2014). Therefore, the NCSBN developed the International Nursing Association for Clinical Simulation and Learning (INACSL) Standards of Best Practice: SimulationSM (Alexander et al., 2015). The INACSL Standard of Best Practice: SimulationSM (the INACSL Standards), provides guidelines for simulation design, outcomes and objectives, and professional integrity (INACSL Standards Committee, 2016), among other aspects, providing a strong foundation for simulation-based education when developing, implementing, and evaluating SBL.
B. Use of Simulation-based Learning in Japan
In Japan, although there have been many studies on individual educators’ simulation-based education practices, the research has been largely exploratory (Inagaki et al., 2018; Inukai & Nagosi, 2018; Yagi, 2018). In addition, there are very few examples of instructions based on set standards like the INACSL standards. The spread of SBL and the increase in nursing schools have caused the following problems: lack of educators with SBL experience, difficulty ensuring an appropriate learning environment, and procuring quality educators, among others. For future curriculum integration, learning program reviews and the current use of SBL must be identified. Therefore, this national survey aimed to clarify the prevalence and practices of SBL in undergraduate nursing education in Japan.
II. METHODS
A. Research Period
Data were collected from November 1, 2019, to January 31, 2020.
B. Subjects
This study constituted a survey that was conducted on the nursing specialties of all nursing schools in Japan. The research subject institutes were a total of 730 nursing schools in Japan, including 263 universities or colleges awarding a baccalaureate degree, 18 junior colleges awarding an associate degree, and 449 vocational schools awarding a diploma. The research subjects were 5,110 individuals consisting of a sample of coordinators in seven nursing specialties per school, namely foundations of nursing, adult nursing, geriatric nursing, pediatric nursing, maternal nursing, psychiatric nursing, and home nursing. The inclusion criteria of our study were the respondents nominated by the head of the education / research institution, nursing department, or nursing vocational school corresponding to the seven specialties. The criteria for nomination were those most involved in SBL in that particular specialty, and those responsible for exercises, if unknown. Thus, the individual and nursing specialty means the same. Out of the total number of 5110 individuals, the calculation of sample size was done with an acceptable error of 5%, a confidence level of 95%, and a response rate of 50%. It indicated that at least 358 respondents were required to fulfil the objectives of this study. The total number of respondents in our study was 420.
C. Data Collection
An independently created, anonymous, self-administered online questionnaire survey (survey) was conducted via Survey Monkey. The head of the education/research institution, nursing department, or nursing vocational school at each of the 730 nursing schools in Japan was sent a request for research participation, the access code necessary for the survey, and contact information of the researchers. Responses were then requested from seven individuals nominated by the head of the education/research institution, nursing department, or nursing vocational school corresponding to the seven specialties. The research subjects accessed Survey Monkey using the access code provided.
D. Survey Content
In the questionnaire, school characteristics and the status of SBL used were created independently based on previous research. The main items in the questionnaire were developed following the INACSL Standards. (Beroz, 2017; Gore et al., 2012; Hayden, 2010; Utsumi et al., 2017). Each item was discussed by the research members and the validity of the content was confirmed. In addition, a pilot test was conducted on several faculty members at the authors’ institution. The target faculty members for this pilot test were selected and requested to be non-responders to this survey. As a result of the pilot test, the wording of the items was corrected and explanations were added to simulation-specific terms such as S.M.A.R.T (specific, measurable, assignable, realistic, and time related) (Doran, 1981), cue, and professional integrity.
1) School characteristics: This section comprised three items including the facility type of the subject’s affiliated school, the respondent’s primary specialisation, and the number of faculty members.
2) The status of SBL use: This section comprised 11 items including the status of simulation-based education use, whether the school was equipped with a simulator, frequency of simulator use, and adoption in the curriculum.
3) The status of the INACSL Standards application: Each item of the INACSL Standards was incorporated as a question resulting in a total of 41 questions. Permission to use a Japanese version of the INACSL Standards was granted by the developer.
E. Data Analysis
Descriptive statistics were used to analyse school characteristics and survey forms. Excel 2019 and SPSS Statistics (Version 24.0) was used to manage data collection and conduct analysis.
F. Ethical Considerations
When providing an explanation and acquiring consent from survey respondents, it was made clear that subjects could decide whether to participate according to their own free will, that there would be no disadvantages for nonparticipation, and that withdrawal from participation after submission would not be feasible as it would be impossible to match individuals to any one anonymous online survey, as no personal identifiable data were collected. Respondents were sent the survey via Survey Monkey and communication was protected. The consent form was added to Survey Monkey and respondents had to consent prior to accessing it. Concerning the security of Survey Monkey, the service used for this study, communications were protected through SSL/TLS encryption, and access was restricted for all ports aside from 80 and 443 (https) using a firewall.
III. RESULTS
A. School Characteristics
Requests were sent to 5,110 individuals (one for each of the seven specialties at 730 schools) and 639 responses were received (response rate 12.5%). Of these, 420 respondents completed the entire survey (8.2%). The respondents’ affiliated schools included 132 universities and colleges (31.4%), 7 junior colleges (1.7%), and 281 vocational schools (66.9%). Thus, over half of the respondents were affiliated with vocational schools as shown in Table 1 (Masuda, 2021).
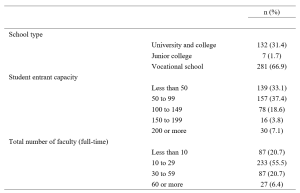
Table 1. School type, entrant capacity, and number of faculty
B. SBL Use
1) SBL use and equipping a high-fidelity and a medium-fidelity simulator and task trainer use: Concerning the status of SBL use, 346 schools (82.4%) responded that they are using SBL, while 74 schools (17.6%) responded that they are not. Among all schools surveyed, 346 (82.4%) were equipped with a simulator for medical/nursing education, while 74 (17.6%) were not. Concerning simulator types, the most common high-fidelity simulator capable of modelling biological reactions and pathology and performing drug administration and other procedures was the SimMan®, which was owned by 27 schools (6.4%) followed by a delivery simulator owned by 25 schools (6.0%). SCENARIO was also common (21 schools, 5.0%). SCENARIO is a high-fidelity simulator similar to SimMan® which hit the market in Japan in 2017 but is cheaper than SimMan®. Meanwhile, roughly 70% of schools (304 schools, 72.4%) were not equipped with a high-fidelity simulator. There were 361 schools (86.0%) equipped with at least one type of medium-fidelity simulator, allowing control of the creation of biological responses such as breath sounds, consciousness, and blood pressure. Regarding virtual reality (VR), 409 schools (97.4%) did not have VR facilities. VR refers to a computer-generated simulation in which a person can interact within an artificial three-dimensional environment using electronic devices, such as special goggles with a screen or gloves fitted with sensors. In this simulated artificial environment, the user is able to have a realistic-feeling experience. Concerning standardised patient (SP) simulation, 164 schools (39.0%) reported that they used SP while 254 schools (60.5%) did not, as shown in Table 2 (Masuda, 2021).
|
n (%) |
n (%) |
||||||||
|
Foundation |
Adult |
Pediatric |
Maternal |
Geriatric |
Psychiatric |
Home |
|||
|
Using simulation-based education (schools) |
|||||||||
|
Yes |
346 (82.4) |
||||||||
|
No |
74 (17.6) |
||||||||
|
Using simulation-based education (specialties) |
|||||||||
|
Yes |
223 (53.1) |
58 (16.8) |
55 (15.9) |
44 (12.7) |
48 (13.9) |
57 (16.5) |
45 (13.0) |
39 (11.3) |
|
|
No |
197 (46.9) |
22 (11.2) |
27 (13.7) |
20 (10.2) |
19 (9.6) |
40 (20.3) |
43 (21.8) |
26 (13.2) |
|
|
Equipped with a simulator for medical/nursing education (schools) |
|||||||||
|
Yes |
346 (82.4) |
||||||||
|
No |
74 (17.6) |
||||||||
|
Equipped with a high-fidelity simulator*1 (may select multiple answers) |
|||||||||
|
SimMan® |
27 (6.4) |
6 (22.2) |
4 (14.8) |
4 (14.8) |
2 (7.4) |
7 (25.9) |
3 (11.1) |
1 (3.7) |
|
|
iStan® |
2 (0.5) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (50.0) |
0 (0.0) |
0 (0.0) |
1 (50.0) |
|
|
Apollo™ |
1 (0.2) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (100.0) |
|
|
BabySim® |
11 (2.6) |
2 (18.2) |
1 (9.1) |
3 (27.3) |
1 (9.1) |
2 (18.2) |
1 (9.1) |
1 (9.1) |
|
|
Delivery simulator |
25 (6.0) |
3 (12.0) |
3 (12.0) |
1 (4.0) |
7 (28.0) |
4 (16.0) |
3 (12.0) |
4 (16.0) |
|
|
SCENARIO |
21 (5.0) |
7 (33.3) |
5 (23.8) |
2 (9.5) |
2 (9.5) |
2 (9.5) |
3 (14.3) |
0 (0.0) |
|
|
Equipped with other high-performance simulator |
59 (14.0) |
13 (22.0) |
9 (15.3) |
10 (16.9) |
5 (8.5) |
9 (15.3) |
8 (13.6) |
5 (8.5) |
|
|
Not equipped with a high-fidelity simulator |
304 (72.4) |
44 (14.5) |
45 (14.8) |
34 (11.2) |
43 (14.1) |
54 (17.8) |
38 (12.5) |
46 (15.1) |
|
|
Equipped with a medium-fidelity simulator*2 (may select multiple answers) |
|||||||||
|
Physiko |
265 (63.1) |
61 (23.0) |
50 (18.9) |
21 (7.9) |
25 (9.4) |
44 (16.6) |
26 (9.8) |
38 (14.3) |
|
|
Nursing Anne® |
46 (11.0) |
7 (15.2) |
11 (23.9) |
3 (6.5) |
6 (13.0) |
5 (10.9) |
7 (15.2) |
7 (15.2) |
|
|
SimManALS® |
13 (3.1) |
4 (30.8) |
3 (23.1) |
0 (0.0) |
0 (0.0) |
1 (7.7) |
4 (30.8) |
1 (7.7) |
|
|
Other |
37 (8.8) |
10 (27.0) |
5 (13.5) |
9 (24.3) |
9 (24.3) |
2 (5.4) |
1 (2.7) |
1 (2.7) |
|
|
Not equipped with a medium-fidelity simulator |
138 (32.9) |
7 (5.1) |
11 (8.0) |
18 (13.0) |
29 (21.0) |
28 (20.3) |
27 (19.6) |
18 (13.0) |
|
|
Equipped with a task trainer*3 |
|||||||||
|
Yes |
331 (78.8) |
62 (18.7) |
53 (16.0) |
42 (12.7) |
49 (14.8) |
50 (15.1) |
30 (9.1) |
45 (13.6) |
|
|
No |
89 (21.2) |
7 (7.9) |
11 (12.4) |
7 (7.9) |
9 (10.1) |
22 (24.7) |
22 (24.7) |
11 (12.4) |
|
|
Equipped with VR |
|||||||||
|
Yes |
11 (2.6) |
1 (9.1) |
3 (27.3) |
2 (18.2) |
0 (0.0) |
2 (18.2) |
1 (9.1) |
2 (18.2) |
|
|
No |
409 (97.4) |
68 (16.6) |
61 (14.9) |
47 (11.5) |
58 (14.2) |
70 (17.1) |
51 (12.5) |
54 (13.2) |
|
|
Using standardised patients in simulation (specialties) |
|||||||||
|
Yes |
164 (39.0) |
38 (23.2) |
30 (18.3) |
16 (9.8) |
22 (13.4) |
27 (16.5) |
10 (6.1) |
21 (12.8) |
|
|
No |
254 (60.5) |
31 (12.2) |
34 (13.4) |
33 (13.0) |
35 (13.8) |
45 (17.7) |
41 (16.1) |
35 (13.8) |
|
*1 High-fidelity simulator: The broad range of full body manikins that have the ability to mimic, at a very high level, human body functions (Lioce et al., 2020).
*2 Medium-fidelity simulator: The broad range of full body mannequins with installed human qualities such as breath sounds without chest rise (Smiley, 2019).
*3 Task trainer: A device designed to provide training in just the key elements of the procedure or skill being learned, such as lumbar puncture, or part of total system (Lioce et al., 2020).
Table 2. Simulation-based education use, equipping a high-fidelity and medium-fidelity simulator, and task trainer use
2) Frequency of simulator use and adoption in the curriculum: The application of SBL was infrequent with most schools (98 schools, 23.3%) using such programs once every year, followed by 97 schools (23.1%), which used SBL once every six months, and 72 schools (17.1%) using them once every two to three months, as shown in Table 3 (Masuda, 2021).
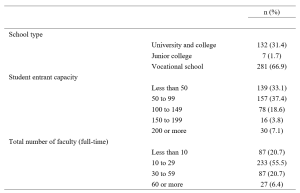
Table 3. Frequency of simulator use and adoption in the curriculum
C. The Status of INACSL Standards Application
Awareness of the INACSL Standards was low with over 90% of respondents stating, “I don’t know of them” (383 respondents, 91.2%) and only 8.8% (37 respondents) stating “I know of them.” Nonetheless, looking at specific items concerning simulation design, over half of the respondents reported using learning objectives, scenario design, methods for ensuring fidelity, learner levels and outcomes, and debriefing. However, rates of application were low for all other items, reaching only 20 to 30%, as shown in Supplementary Table S1 (Masuda, 2021).
IV. DISCUSSION
A. The Status of SBL Use
We surveyed the status of SBL use at nursing schools throughout Japan. The results revealed that 82.4% of those surveyed, use simulation-based education, validating that SBL is widespread in undergraduate nursing education. A nationwide survey in the United States in 2015 found the rate to be 99% (Breymier et al., 2015). Thus, although SBL is gaining popularity in Japan, the country continues to trail the United States in overall usage. Concerning the use of SBL by specialty, simulation is commonly used in foundation of nursing, followed by adult nursing and geriatric nursing. Meanwhile, simulation is used by less than 50% of schools for maternal nursing, pediatric nursing, psychiatric nursing, and home nursing. In countries such as the United States and South Korea, it is primarily used for specialties that require clinical practice in hospitals, such as adult nursing, and clinical nursing, but use for psychiatric and home nursing is limited (Kardong-Edgren et al., 2012; Shin et al., 2015). Thus, our findings were similar to those in these previous studies (Kardong-Edgren et al., 2012; Shin et al., 2015). The less frequent use of psychiatric and home nursing may be due to the inappropriate use of simulators such as SimMan® for medical field or the limited number of simulators in schools.
Concerning schools being equipped with simulators, roughly only 30% of schools had a high-performance simulator, but in comparison mid-level performance simulators were common, being present at approximately 80% of schools. Previous studies (Hayden, 2010; Smiley, 2019) and a meta-analysis (Kim et al., 2016) have shown that roughly 90% of schools implement programs, using either a high- or medium-fidelity simulator. It seems that Japan is catching up to countries with advanced SBL in terms of access to high- and medium-fidelity simulators. In addition, it is that the results were similar to 77.8% equipped with a task trainer of the schools. Nonetheless, the results of the present survey revealed that the frequency of use remains low. In other words, our findings suggest that although Japanese schools are sufficiently equipped with simulators, they are not optimally used.
Simulators are an expensive instructional tool, but it is not enough to simply purchase them. It is essential to further study the obstacles to their application and prepare an environment in which their use is possible. While high- and medium-fidelity simulators from Laerdal Medical were common, use of SCENARIO—a simulator put on the market by Kyoto Kagaku Co., Ltd. in 2017—is rapidly increasing. This rise may be influenced by the fact that SCENARIO is made in Japan. Moreover, not only is SCENARIO lightweight and relatively cheap, it also features native Japanese instructions reflecting the clinical situation, culture, and background of Japan rather than scenarios and an instruction manual written in English. Regarding simulator access by different specialties, it is only natural that the results matched those for the status of simulator-based education use, with foundation of nursing, adult nursing, and geriatric nursing having the most simulators. The rate of 39% of SP utilisation found in this survey was on par with the rate of 36% in bachelor’s programs in the United States (Kardong-Edgren et al., 2012), and a systematic review of 40 published studies from countries such as the United States, South Korea, UK, Australia, found that 25% used SPs (Kim et al., 2016). On the other hand, our results revealed that VR is virtually unused in undergraduate nursing education in Japan. This lags behind the US results of 25% for use in internet-based virtual hospitals and 34% for virtual intravenous injection programs (Kardong-Edgren et al., 2012).
Regarding the adoption of SBL into the curriculum, over half of the schools surveyed featured SBL in their present curriculum, and this inclusion can be expected to increase further as schools plan to transition to new curriculums shortly. Integration of simulation-based education into the curriculum is already in progress in the United States with studies finding that up to 50% of the time spent on clinical practice could be replaced with simulation-based learning with no change in learning outcomes (Hayden et al., 2014). Studies exploring how much of the curriculum has been replaced are also underway (Breymier et al., 2015; Gore et al., 2012; Hayden, 2010; Smiley, 2019). Based on current regulations of Ministry of Education, Culture, Sports, Science and Technology of Japan, the clinical experience cannot be replaced by simulation but is expected to become possible in the future as curriculum integration progresses. As such, integration of simulation into a curriculum requires a meticulous review of the program of study to identify gaps where simulation best fits to increase learning (Hodge et al., 2008). Additionally, past research on barriers to curriculum integration of simulation-based experience found that lack of time for faculty development was the primary barrier (Adamson, 2015; Sole et al., 2013). Therefore, it will be necessary to account for all obstacles to curriculum integration.
B. The Status of the INACSL Standards Application
Among the theoretical frameworks of SBLs, it was inferred that the Japanese version was the INACSL Standards to be developed and relatively known. Therefore, in this study, we investigated the awareness of the INACSL Standards. As a result, unfortunately, we found that awareness was extremely low and that these standards are not widespread in Japanese undergraduate nursing education. However, the results also suggested that over half of respondents implemented learning objectives, scenario design, methods for ensuring fidelity, learner levels and outcomes, and debriefing on simulation design. A survey of the status of simulation used by the INACSL found the use of conceptual frameworks and theories to be approximately 50% and described this result as extremely low (Beroz, 2017). The results of the present survey found an even lower rate with roughly 90% of respondents stating that they did not know of the INACSL Standards. However, even without having prior knowledge regarding the INACSL Standards, over half of the respondents were following the best practice standards in terms of simulation design. Therefore, it is imperative to correctly understand and apply theories and conceptual frameworks to teaching strategies rather than to know their official names. Nearly half of the educators surveyed were designing their simulation programs according to the INACSL Standards, which is considered a positive result. Despite these positive results for simulation design, other items were found to have low utilisation. It is thought that further popularisation of other items will lead to a comprehensive understanding of simulation program design.
C. Study Limitations
Online surveys are not yet widespread in undergraduate nursing education in Japan. It is also presumed that in Japanese undergraduate nursing educations, the coordinators of the nursing specialties are often held by professors or associate professors, and that the age groups of the subjects were relatively high. Therefore, it is considered that the participants may not be familiar with the online surveys. The inclusion criterion for subjects should have included someone familiar with on-line manipulations such as SurveyMonkey. In addition, it may be a deficiency in due to the lengthiness of the questionnaire, improper selection of respondents, response items or the data collection period has not been sufficiently taken. This aspect was the bias of this survey and may explain the low response rate.
In addition, the development of the questionnaire used in this study is limited to content validation, and no examination of construct validity has been conducted. Therefore, there is a limitation that the validity of the questionnaire is insufficient.
Regarding the classification of simulators, in our study, SimMan ALS® was included in a medium-fidelity simulator, and SimMan® was included in a high-fidelity simulator. However, SimManALS® can also be captured as a high-fidelity simulator. This may have influenced the scoring of “others”. In this study, a completed survey was conducted, and randomisation of confounders was not possible.
Therefore, based on the results obtained in this study, we will plan a more focused survey in the future. We suggest that the results of this study can be used to promote SBL in a more specific method.
Lastly, in 2020-21, opportunities for nursing students to complete practical training in medical facilities are limited as a result of the global pandemic of COVID-19. Hence, it can be said that SBL will play a major role in maintaining learning opportunities and clinical competence in students while ensuring the safety of patients, students, and medical staff. We plan to continue and expand upon our survey research to enable more educational institutions to begin practicing SBL.
V. CONCLUSION
In conclusion, this study provided an initial view of the current status of SBL in Japan. Our results suggested that while many schools are equipped with simulators, they are not properly utilised in the foundation of nursing programs in Japan. Thus, further study of barriers to simulator use is needed. Also, although awareness of INACSL Standards was extremely low, over half of the respondents were designing simulations following the standards, implying that they were making use of some theories or conceptual frameworks in their designs. Our results act as a foundational resource for studying strategies intended to systemise SBL in Japanese undergraduate nursing education. In the future, it will be necessary to specifically survey awareness and use of theories and conceptual frameworks to recommend methods for increasing their application and use in SBL.
Notes on Contributors
Dr. Mitsumi Masuda, PhD, RN, is an associate professor at the Graduate School of Nursing, Nagoya City University. She reviewed the literature, designed the study, performed data collection, data analysis and wrote the manuscript.
Dr. Machiko Saeki Yagi, MS, RN, is a lecturer at the School of Nursing, Jichi Medical University. She developed the methodological framework for the study, performed data collection, data analysis and gave critical feedback to the writing of the manuscript.
Dr. Fumino Sugiyama, PhD, RN, is an associate professor at the School of Nursing, National College of Nursing. She performed data collection and data analysis. All the authors have read and approved the final manuscript.
Ethical Approval
This research was approved by the research ethics review committee of the Nagoya City University, Graduate School of Nursing (Approval no.: 19019-2).
Data Availability
Datasets generated and/or analysed during the current study are available from the following DOI. https://doi.org/10.6084/m9.figshare.14010755.v1.
Acknowledgement
This study was completed with the support of The Murata Science Foundation (2019 No. 28). In addition, we would like to thank Editage (www.editage.com) for assisting with English language editing. We would like to offer our heartfelt thanks to the nursing schools across the country who participated in this study.
Funding
This study was completed with the support of The Murata Science Foundation (2019 No. 28).
Declaration of Interest
The authors declare that they have no competing interests.
References
Adamson, K. (2015). A systematic review of the literature related to the NLN/Jeffries simulation framework. Nursing Education Perspectives, 36(5), 281–291. https://doi.org/10.5480/15-1655
Alexander, M., Durham, C. F., Hooper, J. I., Jeffries, P. R., Goldman, N., Kardong-Edgren, S. S., Kesten, K. S., Spector, N., Tagliareni, E., Radtke, B., & Tillman, C. (2015). NCSBN simulation guidelines for prelicensure nursing programs. Journal of Nursing Regulation, 6(3), 39–42. https://doi.org/10.1016/S2155-8256(15)30783-3
Beroz, S. (2017). A statewide survey of simulation practices using NCSBN simulation guidelines. Clinical Simulation in Nursing, 13(6), 270–277. https://doi.org/10.1016/j.ecns.2017.03.005
Boling, B., & Hardin-Pierce, M. (2016). The effect of high-fidelity simulation on knowledge and confidence in critical care training: An integrative review. Nurse Education in Practice, 16(1), 287–293. https://doi.org/10.1016/j.nepr.2015.10.004
Breymier, T. L., Rutherford-Hemming, T., Horsley, T. L., Atz, T., Smith, L. G., Badowski, D., & Connor, K. (2015). Substitution of clinical experience with simulation in prelicensure nursing programs: A national survey in the United States. Clinical Simulation in Nursing, 11(11), 472–478. https://doi.org/10.1016/j.ecns.2015.09.004
Carter, A. G., Creedy, D. K., & Sidebotham, M. (2016). Efficacy of teaching methods used to develop critical thinking in nursing and midwifery undergraduate students: A systematic review of the literature. Nurse Education Today, 40, 209–218. https://doi.org/10.1016/j.nedt.2016.03.010
Chiniara, G., Cole, G., Brisbin, K., Huffman, D., Cragg, B., Lamacchia, M., Norman, D., Canadian Network For Simulation In Healthcare, & Guidelines Working Group. (2013). Simulation in healthcare: A taxonomy and a conceptual framework for instructional design and media selection. Medical Teacher, 35(8), e1380–e1395. https://doi.org/10.3109/0142159X.2012.733451
Doran, G. T. (1981). There’s a S.M.A.R.T. way to write management’s goals and objectives. Management Review, 70(11), 35-36.
Gore, T., Van Gele, P., Ravert, P., & Mabire, C. (2012). A 2010 survey of the INACSL membership about simulation use. Clinical Simulation in Nursing, 8(4), e125-e133. https://doi.org/10.1016/j.ecns.2012.01.002
Hayden, J. (2010). Use of simulation in nursing education: National survey results. Journal of Nursing Regulation, 1(3), 52–57. https://doi.org/10.1016/S2155-8256(15)30335-5
Hayden, J. K., Smiley, R. A., Alexander, M., Kardong-Edgren, S., & Jeffries, P. R. (2014). The NCSBN national simulation study: A longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. Journal of Nursing Regulation, 5(2), S3–S40. https://doi.org/10.1016/S2155-8256(15)30062-4
Hodge, M., Martin, C. T., Tavernier, D., Perea-Ryan, M., & Alcala-Van Houten, L. (2008). Integrating simulation across the curriculum. Nurse Educator, 33(5), 210–214. https://doi.org/10.1097/01.NNE.0000312221.59837.38
INACSL Standards Committee. (2016). INACSL standards of best practice: SimulationSM Simulation design. Clinical Simulation in Nursing, 12(S), S5–S12. https://doi.org/10.1016/j.ecns.2016.09.005
Inagaki, N., Inagaki, M., & Kobe, M. (2018). The perceptions of students concerning the changes in their thinking and exercise utilization caused by simulation exercises for critical care nursing practicums. Journal of Nursing Setanan University, 6(1), 3–11.
Inukai, T., & Nagosi, M. (2018). Students’ learning through a simulated seminar using SBAR.https://doi.org/10.15009/00002249
Kardong-Edgren, S., Willhaus, J., Bennett, D., & Hayden, J. (2012). Results of the national council of state boards of nursing national simulation survey: Part Ⅱ. Clinical Simulation in Nursing, 8(4), e117–e123. https://doi.org/10.1016/j.ecns.2012.01.003
Kim, J., Park, J.-H., & Shin, S. (2016). Effectiveness of simulation-based nursing education depending on fidelity: A meta-analysis. BMC Medical Education, 16, 152. https://doi.org/10.1186/s12909-016-0672-7
Lioce, L., Lopreiato, J., Downing, D., Chang, T. P., Robertson, J. M., Anderson, M., Diaz, D. A., Spain, A. E., & the Terminology and Concepts Working Group. (2020). Healthcare Simulation Dictionary -Second Edition. Retrieved from: https://doi.org/10.23970/simulationv2
Masuda, M. (2021). Materials (TAPS) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14010755.v1
Pal, B., Kumar, M. V., Kyaw Soe, H. H., & Pal, S. (2018). A study on the usefulness of high fidelity patient simulation in undergraduate medical education. The Asia Pacific Scholar, 3(1), 42-49.https://doi.org/10.29060/TAPS.2018-3-1/SC1059
Shin, S., Park, J.-H., & Kim, J.-H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Education Today, 35(1), 176–182. https://doi.org/10.1016/j.nedt.2014.09.009
Smiley, R. A. (2019). Survey of simulation use in prelicensure nursing programs: Changes and advancements, 2010-2017. Journal of Nursing Regulation, 9(4), 48–61. https://doi.org/10.1016/S2155-8256(19)30016-X
Sole, M. L., Betsy Guimond, M. E., & Amidei, C. (2013). An analysis of simulation resources, needs, and plans in Florida. Clinical Simulation in Nursing, 9(7), E265–E271. https://doi.org/10.1016/j.ecns.2012.03.003
Utsumi, M., Tokunaga, J., Hirano, S., Fujii, Y., Takamura, N., & Yamamoto, H. (2017). Status of clinical skills education in faculties of pharmaceutical sciences in Japan: A follow-up report. Journal of Japan Association for Simulation-based Education in Healthcare Professionals, 5, 9–16.
Yagi, S. M. (2018). Simulation training for nurses in specified medical acts. The Journal of Japan Society for Clinical Anesthesia, 38(1), 83–87. https://doi.org/10.2199/jjsca.38.83
Zarifsanaiey, N., Amini, M., & Saadat, F. (2016). A comparison of educational strategies for the acquisition of nursing student’s performance and critical thinking: Simulation-based training vs. integrated training (simulation and critical thinking strategies). BMC Medical Education, 16(1), 294. https://doi.org/10.1186/s12909-016-0812-0
*Mitsumi Masuda
1, Kawasumi, Mizuho-cho,
Mizuho-ku, Nagoya,
467-8601, Japan.
Tel: +81-52-853-8063
Email: m.masuda@med.nagoya-cu.ac.jp
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









