Training nurses to perform water swallow test with use of standardised patients
Submitted: 31 August 2020
Accepted: 17 February 2021
Published online: 13 July, TAPS 2021, 6(3), 91-94
https://doi.org/10.29060/TAPS.2021-6-3/SC2353
Melissa Su Yi Yong, Xing Tong Yong, Olga Hillary Li Chew & Kuan Chen Zenne T’ng
Speech Therapy Department, Tan Tock Seng Hospital, Singapore
Abstract
Introduction: During the COVID-19 epidemic in Singapore, there was an urgent demand to train more nurses within a short timeframe to perform the Water Swallow Test (WST). The previous training model involved training with actual patients and was time-consuming. Hence, the model was revamped and standardised patients (SPs) were engaged for nurses’ training. This study further investigated nurses’ feedback about the new training model and compared the efficiency and learner-reported outcomes of the previous and new models.
Methods: Nurses who completed WST training from January 2018 to July 2020 were enrolled. Training records were accessed to determine the number of nurses trained under the previous and new models. Nurses were invited to complete post-training evaluation forms and their responses were analysed. Descriptive statistics and the Mann-Whitney U test were used for data analysis.
Results: Under the previous model, 52 nurses were trained over 2 years, whereas under the new model, 112 nurses were trained over two months. From the evaluation form responses, the majority of nurses trained under the new model agreed that they achieved the learning objectives and were confident in performing the WST. There was also no significant difference (p>0.05) found between learner-reported outcomes for both training models.
Conclusion: Our findings demonstrated that the new model that engaged SPs was more efficient in training more nurses. Nurses were also satisfied with the new training model, which achieved similar learner-reported outcomes as the previous model.
Keywords: Water Swallow Test, Standardised Patients, Train-the-Trainer, Dysphagia Screening
I. INTRODUCTION
The Water Swallow Test (WST) is a screening tool used to determine if a patient i) is at risk of aspiration, ii) requires swallowing assessment by a Speech Therapist (ST), and iii) can commence oral feeding (Suiter & Leder, 2008). In hospitals, doctors and nurses perform the WST on patients. Given the importance and potential medical sequelae of the WST, nurses require training before performing the test with patients.
At our institution, WST training is conducted using principles of train-the-trainer (Pearce et al., 2012) and flipped classroom model (Betihavas et al., 2016) to certify nurses as providers and trainers. A provider can conduct the WST on patients, and a trainer can train new providers and conduct the WST.
Previously, training was targeted at nurses in Stroke and Intensive Care Unit (ICU) wards. Trainers and providers had to complete an online module and quiz. Practical training was then conducted on actual patients either by a ST or certified trainer. Each practical was three hours and conducted with suitable patients.
When COVID-19 cases surged in Singapore, there was a pressing requirement to train more providers in ICU wards and at the National Centre for Infectious Diseases (NCID). However, there were challenges in continuing with the existing training model. Training with actual patients was too lengthy to meet the demand for more providers and could not be conducted during the outbreak to minimise patient contact. Therefore, the WST training model was revamped and standardised patients (SPs) were engaged (Kowitlawakul et al., 2015) to overcome the above challenges.
Under the new model, training was targeted at nurses in ICU, outbreak and general wards. Nurses had to complete an online module and quiz before attending training sessions in performing the WST with SPs. Eight providers were scheduled per session, which lasted three hours. The SPs were either a ST, nurse, or therapy assistant due to restrictions in the hospital’s visiting policy to engage professional SPs during the outbreak. The SP followed a standardised script demonstrating different signs of dysphagia. Figure 1 shows details on the previous and new training models.
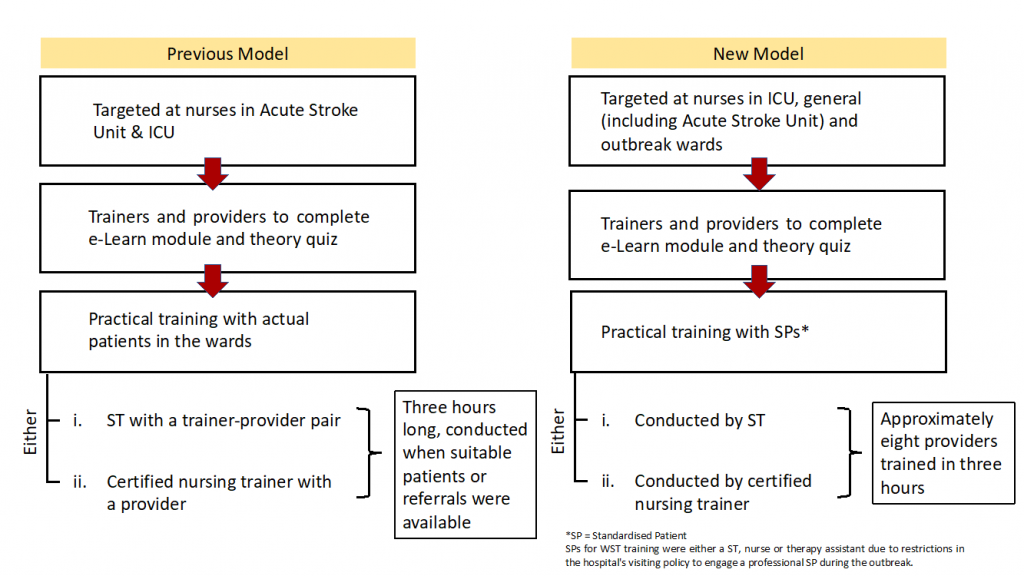
Figure 1: Previous and New Training Models
With the new training model implemented, the following research questions were posed:
1) Is the new training model more efficient in training providers to perform the WST compared to the previous model?
2) Are providers trained under the new model confident that they have achieved the learning objectives of the training and in performing the WST?
3) Is the new training model able to achieve similar learner-reported outcomes for providers as compared to the previous model?
It was hypothesised that:
1) The new training model is more efficient in training providers than the previous model.
2) Majority of providers trained under the new model will feel confident that they achieved the training learning objectives and in performing the WST.
3) The new training model will achieve similar learner-reported outcomes for providers when compared to the previous model.
II. METHODS
Nurses who completed WST training as providers from January 2018 – July 2020 were enrolled. Nurses were trained using the previous training model from January 2018 – April 2020. The new training model was implemented from May 2020.
In order to evaluate the efficiency in training providers under both models, nursing training records were accessed retrospectively to obtain the numbers and dates of providers who completed their training from January 2018 – July 2020. Total training hours under the previous model were computed based on the number of providers who completed training (three hours per provider). Under the new model, total training hours were calculated based on the number of training sessions (three hours per session) conducted from May – July 2020.
In order to evaluate the providers’ confidence in achieving the training’s learning objectives and in performing the WST, providers trained under both models were invited to complete an anonymous course evaluation form generated by the authors and select their responses on a 5-point Likert scale (i.e., strongly agree, agree, neutral, disagree, strongly disagree). The evaluation form was updated along with the new training model, however, these three statements remain unchanged in both versions and were used to analyse learner-reported outcomes:
1. I have a clear understanding of the contraindications of performing the WST.
2. I am confident of accurately identifying all the signs of dysphagia during the WST.
3. I am confident of performing the WST independently.
For data analysis, ‘strongly agree’ and ‘agree’ responses were collapsed into a single category and assigned a score of 1, ‘neutral’ response was assigned a score of 2, and ‘disagree’ and ‘strongly disagree’ responses were collapsed into a single category and assigned a score of 3. Statistical analysis was performed using SPSS statistics version 27.0. Descriptive statistics and the Mann-Whitney U test were used to analyse the evaluation form responses.
Implied consent was obtained from providers who voluntarily completed the form. This study was exempted from a formal NHG Domain Specific Review Board review.
III. RESULTS
A. Number of Providers Trained and Duration Required
Under the previous training model, 52 providers were trained over 24 months (January 2018 – December 2019). The total number of training hours was 156 hours (i.e., 52 providers x three hours). Under the new model, 112 providers were trained in 15 training sessions over two months (end May – mid-July 2020). The total training hours were 45 hours (i.e., 15 sessions x three hours).
Hence, one provider was trained every three-hourly training session and an average of 2.17 providers were trained per month under the previous model. Contrastingly, an average of 7.57 providers were trained every three-hourly training session and an average of 56 providers were trained per month under the new model.
B. Evaluation Form Responses
13 evaluation form responses (Nprevious = 13) were received under the previous model, and 111 responses (Nnew = 111) were received under the new model. The mean scores obtained for the three selected statements were:
1. I have a clear understanding of the contraindications of performing the WST (Previous model: M = 1.08, SD = 0.277; New model: M = 1.22, SD = 0.624).
2. I am confident of accurately identifying all the signs of dysphagia during the WST (Previous model: M = 1.08, SD = 0.277; New model: M = 1.23, SD = 0.567).
3. I am confident of performing the WST independently (Previous model: M = 1.15, SD = 0.555; New model: M = 1.22, SD = 0.563).
C. Comparison of Learner-Reported Outcomes
Scores from the new evaluation form (mean ranks = 62.76, 63.03, 62.90) were higher than scores from the previous form (mean ranks = 60.31, 57.96, 59.08) for all three statements. A Mann-Whitney U test indicated that the differences in scores between the previous and new model for all three statements were not statistically different, UStatement1 (Nnew = 111, Nprevious = 13) = 693.00, z = -0.438, p = 0.661; UStatement2 (Nnew = 111, Nprevious =13) = 662.50, z = -0.786, p = 0.432; UStatement3 (Nnew = 111, Nprevious = 13) = 677.00, z = -0.608, p = 0.543.
The above data set and analysis is available online (Yong et al., 2020).
IV. DISCUSSION
A. Efficiency of New Training Model
The new training model was more efficient than the previous model. Comparing the average number of providers trained per month, the new model was 25 times more efficient. Engagement of SPs allowed more staff to be trained in a single session by seven-fold, versus training with actual patients. Several factors made the new model more efficient: i) greater control over scheduling, ii) saving time from identifying suitable patients for training, and iii) reduced motion waste from accessing actual patients. Hence, more nurses could be trained to meet the needs of outbreak wards.
B. Feedback on Training
The mean rating scores for the three statements in the new evaluation form indicated that providers were satisfied with their training, as they mostly agreed or strongly agreed to achieving the training learning objectives and were confident in performing the WST.
C. Comparison of Learner-reported Outcomes under Both Models
No significant differences were found between responses in the previous and new evaluation forms. Thus, regardless of whether providers trained with actual patients or SPs, most perceived they fulfilled their learning objectives and felt confident to perform the WST independently. These findings indicated that providers did not perceive their training quality to be compromised with the use of SPs and shorter training duration.
D. Limitations
A limitation was that only 25% of providers completed the optional evaluation form under the previous model. The staff who responded likely had a positive training experience and this could lead to potential selection bias. We also acknowledge that the three statements from the evaluation form require further validity and reliability testing to analyse providers’ confidence levels and can be explored in future studies.
V. CONCLUSION
Our study demonstrated that having standardised patients as part of the training method translated to a significant increase in the efficiency of WST training. Potential scale-up of this WST training method can ensure that there is a steady pool of providers and trainers in the workforce to cope during peacetime and crises. Adopting the WST as part of routine dysphagia screening ultimately ensures safer feeding management and early access to Speech Therapy intervention. Further directions include investigating the effectiveness and validity of the new WST training model in various healthcare settings, such as acute and community hospitals and nursing homes, to improve training standards for dysphagia screening in the region, especially in light of the ongoing COVID-19 pandemic.
Notes on Contributors
Yong Su Yi Melissa and Yong Xing Tong evaluated the training model, conducted the training and wrote the manuscript. Olga Hillary Chew Li conducted the training and performed data collection. Zenne T’ng Kuan Chen initiated the design of the training model and gave critical feedback to the writing of the manuscript. All authors read and approved the final manuscript.
Ethical Approval
This study has been reviewed by NHG Domain Specific Review Board (DSRB) for determination of ethics requirement and does not require formal review (NHG DSRB Ref: 2020/00953).
Acknowledgements
We would like to acknowledge:
Senior Nurse Educator Kylie Tang and Nurse Educator Zhao Yue for their feedback in the design of the training model, accessing training records for data collection and collaboration in facilitating WST training for the Nursing Services department.
Senior Speech Therapist Ei Leen Fong for vetting the final manuscript
Principal Speech Therapist Kwong Seh Ling for her guidance in the data analysis and feedback on the manuscript.
Funding
There is no funding involved for this study.
Data Availability
All available data can be accessed publicly via https://doi.org/10.6084/m9.figshare.13110617.
Declaration of Interest
The authors declare there are no conflicts of interest.
References
Betihavas, V., Bridgman, H., Kornhaber, R., & Cross, M. (2016). The evidence for ‘flipping out’: A systematic review of the flipped classroom in nursing education. Nurse Education Today, 38, 15-21. https://doi.org/10.1016/j.nedt.2015.12.010
Kowitlawakul, Y., Chow, Y. L., Salam, Z. H., & Ignacio, J. (2015). Exploring the use of standardized patients for simulation-based learning in preparing advanced practice nurses. Nurse Education Today, 35(7), 894–899. https://doi.org/10.1016/j.nedt.2015.03.004
Pearce, J., Mann, M. K., Jones, C., van Buschbach, S., Olff, M., & Bisson, J. I. (2012). The most effective way of delivering a train-the-trainers program: A systematic review. The Journal of Continuing Education in the Health Professions, 32(3), 215–226. https://doi.org/10.1002/chp.21148
Suiter, D. M., & Leder, S. B. (2008). Clinical utility of the 3-ounce water swallow test. Dysphagia, 23(3), 244–250. https://doi.org/10.1007/s00455-007-9127-y
Yong, M., Yong, X. T., Chew, O., & Tng, Z. K. C. (2020). Training nurses to perform water swallow test with use of standardised patients (raw data & analysis) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.13435310.v2
*Yong Su Yi Melissa
Tan Tock Seng Hospital,
11 Jalan Tan Tock Seng,
Singapore 308433
Tel: +65 8522 8013
Email: melissa_sy_yong@ttsh.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









