The effectiveness of smartphone ophthalmoscope compared to direct ophthalmoscope as a teaching tool
Submitted: 6 January 2022
Accepted: 4 May 2022
Published online: 4 October, TAPS 2022, 7(4), 22-34
https://doi.org/10.29060/TAPS.2022-7-4/OA2735
Amelah Abdul Qader1,2, Hui Meng Er3 & Chew Fei Sow3
1School of Postgraduate Studies, International Medical University, Kuala Lumpur, Malaysia; 2University of Cyberjaya, Faculty of Medicine, Cyberjaya, Malaysia; 3IMU Centre for Education, International Medical University, Kuala Lumpur, Malaysia
Abstract
Introduction: The direct ophthalmoscope is a standard tool for fundus examination but is underutilised in practice due to technical difficulties. Although the smartphone ophthalmoscope has been demonstrated to improve fundus abnormality detection, there are limited studies assessing its utility as a teaching tool for fundus examination in Southeast Asian medical schools. This study explored the perception of medical students’ toward using a smartphone ophthalmoscope for fundus examination and compared their abilities to diagnose common fundal abnormalities using smartphone ophthalmoscope against direct ophthalmoscope.
Methods: Sixty-nine Year-4 undergraduate medical students participated in the study. Their competencies in using direct ophthalmoscope and smartphone ophthalmoscope for fundus examination on manikins with ocular abnormalities were formatively assessed. The scores were analysed using the SPSS statistical software. Their perceptions on the use of smartphone ophthalmoscopes for fundus examination were obtained using a questionnaire.
Results: The students’ competency assessment scores using the smartphone ophthalmoscope were significantly higher than those using the direct ophthalmoscope. A significantly higher percentage of them correctly diagnosed fundus abnormalities using the smartphone ophthalmoscope. They were confident in detecting fundus abnormalities using the smartphone ophthalmoscope and appreciated the comfortable working distance, ease of use and collaborative learning. More than 90% of them were of the view that smartphone ophthalmoscopes should be included in the undergraduate medical curriculum.
Conclusion: Undergraduate medical students performed better in fundus examination on manikins with ocular abnormalities using smartphone ophthalmoscope compared to direct ophthalmoscope. Their positive perceptions toward smartphone ophthalmoscope support its use as a supplementary teaching tool in undergraduate medical curriculum.
Keywords: Medical Students, Smartphone, Ophthalmoscope, Teaching Tool
Practice Highlights
- The smartphone ophthalmoscope is a useful supplementary teaching tool for fundus examination in undergraduate medical education.
- Fundus examination is performed at a safe working distance from the patient using a smartphone ophthalmoscope.
- Students are able to detect fundus abnormalities with greater ease and accuracy using a smartphone ophthalmoscope compared to a direct ophthalmoscope.
- Students appreciate the collaborative learning through peer discussion of the fundus findings using the smartphone ophthalmoscope.
I. INTRODUCTION
Fundus examination is one of the essential procedures which provides information about ocular conditions that may compromise the quality of vision and lead to blindness (Leonardo, 2018). The direct ophthalmoscope (DO) is one of the robust ocular clinical examination tools to be grasped during clinical skill training in medical schools as well as clinical practice. However, students have difficulty mastering the technique of using it (Kim & Chao, 2019), particularly when they have to coordinate their hand movements at a very near distance to the patient and close one eye when examining the patient’s fundus through the pupil (MacKay et al., 2015). They also have to adjust the power of the direct ophthalmoscope lenses to get a clearer picture if there is a refractive error with the patient’s eye or their own eyes. Instead of concentrating on detecting fundus findings, the students are preoccupied with adjusting the direct ophthalmoscope.
Technical constraints may be the main reason for the underuse of direct ophthalmoscopes. Experienced physicians who use the direct ophthalmoscope may lack confidence and frequently miss significant abnormalities (Purbrick & Chong, 2015), causing delayed diagnosis of preventable eye disorders and permanent vision impairment (Myung et al., 2014). This has led to the exploration of alternative tools to overcome some of these challenges (Giardini et al., 2014; Kim & Chao, 2019). Smartphone ophthalmoscope, for example, is a breakthrough digital portable retinal imaging system that allows medical practitioners to view the fundus with high-definition images or video of a routine ophthalmoscope examination.
The D-EYE smartphone ophthalmoscope was developed by Doctor Andrea Russo in 2015 (Russo et al., 2015). It is a small, portable, and inexpensive retinal imaging system that can capture retinal images using an attachment to a smartphone that uses a cross-polarisation technique to reduce corneal reflections. It is integrated with the smartphone’s autofocus feature to accommodate the patient’s refractive error.
A. Problem and Rationale
Fundus examination requires extensive practice to develop adequate interpretation skills (Leonardo, 2018). Medical students are taught to use the direct ophthalmoscope in order to recognise retinal signs of life-threatening disorders (Benbassat et al., 2012). The International Council of Ophthalmology recognises direct ophthalmoscope examination as one of the seven core ocular medical education competencies. All graduating medical students are expected to recognise common abnormalities of the ocular fundus using a direct ophthalmoscope (Dunn et al., 2021). However, there is a lack of competencies among the medical graduates using this tool (MacKay et al., 2015). This needs to be addressed as at least 2.2 billion people globally have visual impairment or blindness, of which at least 1 billion have deterioration in vision that could have been prevented if they were screened or detected earlier, World Health Organization (2019). Tan et al. (2020) reported several favourable studies carried out in Italy, UK, and India on the advantages of smartphone ophthalmoscopes for fundus examination and visualisation of the retinal image. In a randomised cross-over study done by Curtis et al. (2021) on the ease of use of D-EYE smartphone ophthalmoscope versus direct ophthalmoscope, 44 Year-one medical students in Canada examined the patients’ fundus for optic disc assessment and compared their findings with the respective photographs provided. The ease of use and confidence was more significant with the D-EYE smartphone ophthalmoscope.
Although the smartphone ophthalmoscope is available in Southeast Asian countries such as Malaysia, it is not commonly used in public hospitals and general practitioner clinics. This is probably due to resource constraint issues in developing countries. Moreover, there are limited studies assessing its use, in particular, there is no literature report on such studies among undergraduate medical students in Southeast Asia. However, based on the positive findings from the literature, it has been proposed that smartphone ophthalmoscope be included in clinical skill training for fundus examination among undergraduate medical students at the university where this study was conducted. Therefore, this study was carried out to explore the students’ perceptions of using smartphone ophthalmoscopes for fundus examination and determine whether their competencies in fundus examination improved using this tool compared to using the direct ophthalmoscope. In this study, the D-EYE smartphone ophthalmoscope was chosen over the other types of smartphone ophthalmoscope due to reasons including the ease of data management using the available app facility, cost feasibility and convenience. The two research questions of the study were:
1) What were the perceptions of medical students on the use of smartphone ophthalmoscope for fundus examination?
2) Was there a difference between students’ competencies in fundus examination when using the smartphone ophthalmoscope compared to the direct ophthalmoscope?
The cognitive theory of multimedia learning can be applied in the context of fundus examination using a smartphone ophthalmoscope. Using a smartphone ophthalmoscope, the student can visualise the fundus on the smartphone screen. According to the cognitive theory of multimedia learning (Figure 1), the students engage in active cognitive processing in order to create a cohesive mental representation of their experiences based on their recall knowledge of fundus structures and ocular abnormalities. This will allow them to integrate the findings with other relevant information. They can then describe their findings and organise the selected images into a “mental model” of the items they are learning. Finally, their prior knowledge of ocular disorders is incorporated and reconciled with these verbal explanations and graphical representations.
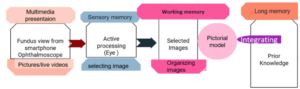
Figure 1. Cognitive theory of multimedia learning
According to the social constructivism theory, learning is social, active and constructed through social interaction (Lötter & Jacobs, 2020). Technologies have been shown to enhance students’ problem solving by breaking down complex concepts into sub-problems (Kim & Hannafin, 2011). A smartphone ophthalmoscope is an appropriate tool for encouraging active interaction between the students and lecturer to work on real-world problems in the teaching and learning environment. When the students perform fundus examination using the smartphone ophthalmoscope, they can see the findings on the screen together with their peers and the lecturer. This will allow them to gain more knowledge and understanding as they can discuss and link the new ideas in the context of their prior knowledge.
II. METHODS
The study was approved by the International Medical University Joint-Committee on Research and Ethics (IMU-JC). Informed consent was obtained from all respondents. The nature and purpose of the study were explained to them. The respondents were assured of anonymity and confidentiality of the collected information.
A. Study Setting
The data were collected from Year-4 undergraduate medical students who undertook ophthalmology rotation for the academic year 2020/2021, at the University of Cyberjaya, Malaysia.
In the fourth year of the medical curriculum, the students undertake four major postings (Orthopedic, Family Medicine, Psychiatry and a speciality posting) over two semesters (Semesters 7 and 8). These are conducted in four rotations per year (rotations 1 & 2 in Semester 7, rotations 3 & 4 in Semester 8). The speciality posting includes Ophthalmology, Anaesthesia, ENT and Radiology. The duration of each of these speciality posting is two weeks. In the ophthalmology posting the students are taught the principles of history taking and ocular examination in the Clinical Skill Training Department and in the hospital, where they clerk patients with eye conditions. Additionally, they learn about basic common eye conditions during interactive sessions and case-based discussion sessions in small groups. However, during the COVID-19 pandemic, the posting was affected by lockdown measures. Therefore, the case-based discussion sessions were conducted online, and ocular examination was demonstrated through online interactive video sessions. Nevertheless, there was a window of opportunity where the students could return to the campus physically for a one-week revision. During this period, the students practice ophthalmoscopy examination on manikins in the Clinical Skill Training Department.
B. Study Design
The direct ophthalmoscope examination technique was introduced to the students virtually through video demonstrations and during online interactive discussion sessions. During the revision week, the students were trained for two hours to perform fundus examination using the direct ophthalmoscope. For the smartphone ophthalmoscope, they were briefed and trained on its use for 20-30 minutes. The training was conducted by a member of the teaching staff (who is the researcher in this study, AMAQ). Following that, the students were required to examine various slides of fundus images provided in the manikins (M1 and M2).
The selected slides on the manikins represented the common pathological fundus findings, i.e. optic disc swelling, branch retinal vein occlusion, optic atrophy/glaucoma and diabetic retinopathy/ maculopathy. Each student performed the fundus examination on M1 and M2 using the direct and smartphone ophthalmoscopes separately (approximately 2-3 minutes on each manikin) on the same day. The students were required to fill in their findings based on their observation (without discussing with their peers) on the formative assessment forms (shown in Appendix 1) and indicate the tools they utilised (direct or smartphone ophthalmoscopes). The formative assessment form was adapted from Mamtora et al. (2018) and had been validated by two ophthalmologists in the department.
To avoid bias, all the completed formative assessment forms were collected and submitted to another researcher (SCF) who was not involved in marking (to remove information on the tool used by the student on each form). These were then returned to the researcher in this study, (AMAQ) for marking.
After completing the formative assessment, the students were requested to fill in an online questionnaire regarding their perception on the use of smartphone ophthalmoscope for fundus examination. This questionnaire (Appendix 2) was adapted from Nagra & Huntjens (2020). In addition, the students were requested to provide the reasons for their suggestions to include smartphone ophthalmoscopes or replace direct ophthalmoscopes with smartphone ophthalmoscopes in the medical curriculum.
C. Data Analysis
All data were statistically analysed using SPSS version 23. The paired t-test was used to compare the performance of the students in the formative assessments using direct ophthalmoscopes and smartphone ophthalmoscopes. The number of students getting the correct diagnosis using both tools was statistically analysed using the McNemar (Chi Square) test (Liao & Lin, 2008). The statistical significance was determined based on the p-values (the difference is significant if p ≤ 0.05). The responses of the students in the perceptions questionnaire related to the ease of use, confidence, and preference were analysed.
III. RESULTS
Sixty-nine Year-4 medical students participated in this study. The demographic data are shown in Table 1.
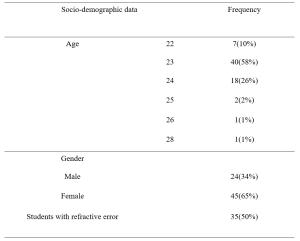
Table 1: Demographic data
A. Comparison of Formative Assessment Scores Using Smartphone Ophthalmoscope and Direct Ophthalmoscope
The mean scores of the students were higher using the smartphone ophthalmoscope (59%) than the direct ophthalmoscope (39%). The same trend was observed for the students with and without refractive error. The results are shown in Table 2. A higher number of students were able to make the correct diagnosis for all fundus abnormalities using the smartphone ophthalmoscope compared to the direct ophthalmoscope. The difference is statistically significant (p-value < 0.05). The results are presented in Table 3. The data that support the findings are openly available in Figshare at https://figshare.com/s/d45da87ea42c596e714b
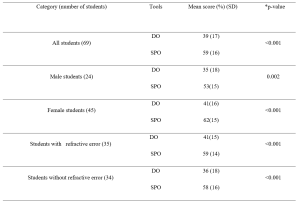
Table 2: Comparison of formative assessment scores using direct ophthalmoscope (DO) and smartphone ophthalmoscope (SPO).
*p-value (paired t-test)
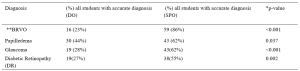
Table 3: Comparison of correct diagnosis using direct ophthalmoscope and smartphone ophthalmoscope.
*McNemar (Chi square) test (Liao & Lin, 2008),
**(Branch retinal vein occlusion)
A. Students’ Perceptions on the Use of Smartphone Ophthalmoscope for Fundus Examination
A total of 69 students participated in the online questionnaire. All the students appreciated that their peers could share the findings with them on the smartphone screen. Most of the students (87%) preferred using smartphone ophthalmoscopes over direct ophthalmoscopes, and 86% felt confident when using the smartphone ophthalmoscope. In addition, the comfortable working distance was appreciated by 87% of the students. The responses of the participants are shown in Table 4.
|
Online student evaluation Form
|
Likert scale 1= Strongly disagree 2= disagree, 3 = Neutral, 4 =agree, 5= Strongly agree |
||||
|
Section 1 Perception on smartphone ophthalmoscope use |
1 |
2 |
3 |
4 |
5 |
|
I feel confident while using it |
1.4% |
2.9% |
8.7% |
56.5% |
30.4% |
|
I feel easy to view the fundus |
0.0% |
5.8% |
11.6% |
44.9% |
37.7% |
|
I feel comfortable when my peer can observe with me the findings |
0.0% |
0.0% |
0.0% |
30.4% |
69.6% |
|
My hand is steady while I am performing examination |
0.0% |
4.3% |
20.3% |
40.6% |
34.8% |
|
I can pick the finding faster |
0.0% |
4.3% |
21.7% |
42.0% |
31.9% |
|
Smartphone ophthalmoscope user-friendly |
0.0% |
1.4% |
7.2% |
39.1% |
52.2% |
|
I prefer to use it
|
0.0% |
4.3% |
8.7% |
40.6% |
46.4% |
|
Online student evaluation Form |
Likert scale 1= Strongly disagree 2= disagree, 3 = Neutral, 4 =agree, 5= Strongly agree
|
||||
|
Section 2 Efficiency of smartphone ophthalmoscope |
1 |
2 |
3 |
4 |
5 |
|
It takes shorter duration to detect finding |
0.0% |
4.3% |
27.5% |
33.3% |
34.8% |
|
It has comfortable working distance |
0.0% |
0.0% |
13.0% |
40.6% |
46.4% |
|
I found difficulty in handling it |
10.1% |
44.9% |
21.7% |
20.3% |
2.9% |
|
I think Smartphone ophthalmoscope must be added to the medical curriculum |
0.0% |
0.0% |
4.3% |
47.8% |
47.8% |
|
I think direct ophthalmoscope should be replaced by smartphone ophthalmoscope |
1.4% |
10.1% |
26.1% |
33.3% |
29.0% |
Table 4: Responses of participants in the questionnaire to evaluate their perception and efficiency on the use of smartphone ophthalmoscope for fundus examination
B. Students’ Preference for Types of Ophthalmoscopes
Most of the students (94%) suggested that the smartphone ophthalmoscope be included in the medical curriculum, and 62% suggested to replace the direct ophthalmoscope with the smartphone ophthalmoscope. Their preference was mainly attributed to the efficiency, ease of use (for those with refractive error and amblyopia (lazy eye)), autofocus function using the smartphone, and the possibility of using both eyes to see the images on the smartphone screen. In addition, the comfortable working distance, ease of cleaning after use and peer discussion were cited. Meanwhile, 11% of the students suggested keeping direct ophthalmoscope alongside the smartphone ophthalmoscope in the curriculum. They opined that smartphone ophthalmoscope should be included as an additional teaching and learning tool for fundus examination but disagreed that it should replace direct ophthalmoscope totally as the smartphone ophthalmoscope might not be readily available in all healthcare settings. One of the participants commented that “eye examination using direct ophthalmoscope was thought to be a basic procedural skill that doctors must-have. Smartphone ophthalmoscope was a newer technology that might not be available in hospitals, unlike direct ophthalmoscope, which was more common“.
IV. DISCUSSION
The students scored significantly higher in the formative assessment for fundus abnormalities using the smartphone ophthalmoscope compared to the direct ophthalmoscope. The findings from this study were consistent with those of Kim and Chao (2019) and Dunn et al. (2021). In addition, the study also showed that the difference was statistically significant regardless of the presence of refractive error.
The students with refractive error and amblyopia have commented that they found the smartphone ophthalmoscope more convenient and efficient than the direct ophthalmoscope. They stated that they had difficulty using their amblyopic eye when performing the examination using the direct ophthalmoscope as they had to follow the ‘Three R rule’ in which students should use their right eye and their right hand when examining the right eye of the patient at the side of the patient at about 45 degrees to avoid kissing position with the patient. The students with refractive errors highlighted another issue that they needed to adjust the direct ophthalmoscope very frequently to get a proper and clear view. However, when they used the smartphone ophthalmoscope, they were able to perform the examination using both eyes, as they could view the fundus on the smartphone screen without having to close one eye. Fifty percent of the students in this study reported they had refractive errors. In the study by Al-Rashidi et al. (2018), it was found that 89 out of 162 medical students (54 %) had refractive errors. In this study, a significantly higher number of students obtained the correct diagnosis of branch retinal vein occlusion (86%) and glaucoma (62%) using the smartphone ophthalmoscope compared to the direct ophthalmoscope (p-value < 0. 001).
In a study conducted by Mrad et al. (2021) on the accurate method for glaucoma screening, they found that the D-EYE smartphone ophthalmoscope was more accurate for capturing fundus images and assessing the optic disc in detecting glaucoma compared to the direct ophthalmoscope. In addition, Mamtora et al. (2018) reported that it was more convenient and easier to detect optic disc and blood vessels using the D-EYE smartphone ophthalmoscope. Providing alternative tools in medical education could help students learn and perform more efficiently during their teaching and learning activities.
In our study, 86% of the students felt confident using the smartphone ophthalmoscope, and 83% of them found it easy to view the fundus. The majority of the students (91%) found the smartphone ophthalmoscope user friendly, and 73% indicated that they were able to identify the findings quickly while using the smartphone ophthalmoscope. It has been reported previously that medical students preferred smartphone ophthalmoscopes to direct ophthalmoscopes and were more likely to make correct and faster diagnoses (Nagra & Huntjens, 2020). Though mastering the technique of using the direct ophthalmoscope is important, it is equally paramount to be able to identify the fundus findings accurately. The cognitive load theory states that the human working memory can only hold a certain number of interrelated objects (Chu, 2014). Motivational components can enhance student learning by boosting generative processing as long as the learner is not constantly overburdened with needless processing or diverted from critical processing (Mayer, 2014). The technical challenges faced while using the direct ophthalmoscope could hamper the students’ ability to recognise the features associated with fundus abnormalities. The smartphone ophthalmoscope offers an advantage in this context.
In this study, 87 % of the students found that the working distance of a smartphone ophthalmoscope was more comfortable compared to the typical 1–3 cm working distance of a direct ophthalmoscope. This finding was similar to the study conducted by Huntjens & Nagra (2020), where they found that 92% of the students preferred the longer working distance of 20–60 cm of the D-EYE smartphone ophthalmoscope.
The use of smartphone ophthalmoscope as a teaching tool increases student engagement and enhances their learning experience. All students appreciated that their peers could observe the findings together with them on the smartphone screen. They were able to discuss among themselves, as well as with the lecturer. Learning must be an engaging and meaningful experience for the learners to be productive (Mellis et al., 2013). Learners will utilise strategies developed earlier in their training to optimise their knowledge and skills through reflection. When the students record the fundus images, they can discuss their interpretation of findings with the lecturers and peers. Feedback from this process will improve their learning efforts (Kaufman, 2019). The feedback and reflection facilitate the construction of new knowledge, as well as strategies for improving the performance as all of them could see the same findings on the smartphone screen and discuss accordingly.
In our study, 93% of the students’ suggested that smartphone ophthalmoscopes should be included in the medical curriculum. It was easier for them to see the findings without spending a longer time trying to focus by squinting and shutting one eye to look for the findings, as the image is automatically adjusted in a smartphone ophthalmoscope. This has been highlighted as one of the advantages of using the smartphone ophthalmoscope in medical training and screening in primary care centres (Nagra & Huntjens, 2020). Smartphone-based fundus image could even replace the direct ophthalmoscope in clinical medicine (Wintergerst et al., 2020). In our study, out of the 69 students, only eight students (11%) opined that the direct ophthalmoscope should not be totally replaced with a smartphone ophthalmoscope. From their point of view, the direct ophthalmoscope is a must-know clinical skill that contributes to their professional identity. In particular, the smartphone ophthalmoscope may not be easily available in developing countries due to resource constraints. The direct ophthalmoscope is one of the fundamental skills that all clinicians should be able to perform. It is included in the assessment of the final year undergraduate curriculum as well as the postgraduate membership assessment. (Purbrick & Chong, 2015).
With a specific instructional scaffolding strategy, smartphone ophthalmoscopes can be used as a prologue to the direct ophthalmoscope. Students will be able to share the fundus pictures with their peers through the screen simultaneously for the same patient during clinical practice sessions in packed clinics, without having to struggle with the technical challenges of the direct ophthalmoscope. As a result, patients will be less burdened in terms of examination time, and students will be able to evaluate more patients with fundus abnormalities in a shorter amount of time. The concept of just-in-time learning can be a useful pedagogical tool for medical academicians to improve their teaching and learning approach in the age of technology. The just-in-time learning idea uses technology to deliver teaching and learning activities, allowing learning communities to understand better and practise (Naseem et al, 2019). According to Riel (2000), academics continue to play an essential role in encouraging learners to apply their knowledge effectively. As new technologies emerge, educators must prepare students to be lifelong learners who are digitally literate and resourceful in their application of technology.
A. Limitations of the Study
As the study was conducted during the COVID-19 pandemic, the duration for recruitment and training of the students was limited. As a result, the students had a shorter period of face-to-face clinical training. This limited the student’s exposure to performing fundus examinations on real patients in the hospital and using the various ophthalmoscopic tools. In addition, the lack of practice could have affected the students’ performance in the formative assessment on fundus examination using the smartphone and direct ophthalmoscopes. Therefore, we recommend repeating this study when the COVID-19 situation is resolved.
Another limitation of the study was that the students performed the fundus examination on the same manikins using the direct ophthalmoscope followed by the smartphone ophthalmoscope (or vice versa) on the same day. This could result in bias in their judgement in identifying the fundus abnormalities. Nevertheless, the students were reminded to be objective and record their findings accurately based on their observations using either tool.
V. CONCLUSION
Smartphone ophthalmoscope is an effective teaching tool for improving the skills in detecting common clinical ocular diseases. It provides a comfortable working distance and promotes collaborative learning by enabling peer discussion. It is also convenient for students with refractive errors. Therefore, the smartphone ophthalmoscope is a valuable supplementary teaching tool for fundus examination and is highly recommended to be included in the undergraduate medical curriculum.
Notes on Contributors
AMAQ designed and conducted the study, reviewed the literature, analysed the data and wrote the manuscript EHM designed the study, analysed the data, gave critical feedback and edited the manuscript before submission. SCF designed the study, gave critical feedback and edited the manuscript before submission.
Ethical Approval
The study was approved by the International Medical University Joint-Committee on Research and Ethics (IMU-JC), Project ID No.: MHPE I/2021(01). Informed consent was obtained from all respondents, and the nature and purpose of the study were explained to them. The respondents were assured of anonymity and confidentiality of the collected information.
Data Availability
All data are available at https://figshare.com/s/d45da87ea42c596e714b and can be accessed on request and approval from the corresponding author.
Acknowledgement
The authors would like to thank the medical students at the University of Cyberjaya who showed their enthusiasm for learning. And special thanks to the statisticians, Dr Norhafizah Ab Manan, University of Cyberjaya and Dr Shamala Ramasamy, International Medical university, for their advice on statistical tests. The authors would also like to thank Professor Ian Wilson for proofreading the manuscript.
Funding
This study was funded by the International Medical University, Malaysia. MHPE I/2021(01)
Declaration of Interest
Authors declare that they do not have possible conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Al-Rashidi, S. H., Albahouth, A. A., Althwini, W. A., Alsohibani, A. A., Alnughaymishi, A. A., Alsaeed, A. A., Al-Rashidi, F. H., & Almatrafi, S. (2018). Prevalence refractive errors among medical students of Qassim University, Saudi Arabia: Cross-sectional descriptive study. Open Access Macedonian Journal of Medical Sciences, 6(5), 940–943. https://doi.org/10.3889/oamjms.2018.197
Benbassat, J., Polak, B. C. P., & Javitt, J. C. (2012). Objectives of teaching direct ophthalmoscopy to medical students. Acta Ophthalmologica, 90(6), 503–507. https://doi.org/10.1111/j.1755-3768.2011.02221.x
Chu, H.-C. (2014). Potential Negative Effects of Mobile Learning on Students’ Learning Achievement and Cognitive Load—A Format Assessment Perspective. Educational Technology & Society, 17 (1), 332–344
Curtis, R., Xu, M., Liu, D., Kwok, J., Hopman, W., Irrcher, I., & Baxter, S. (2021). Smartphone Compatible versus Conventional Ophthalmoscope: A Randomized Crossover Educational Trial. Journal of Academic Ophthalmology, 13(02), e270–e276. https://doi.org/10.1055/s-0041-1736438
Dunn, H. P., Kang, C. J., Marks, S., Witherow, J. L., Dunn, S. M., Healey, P. R., & White, A. J. (2021). Perceived usefulness and ease of use of fundoscopy by medical students: A randomised cross-over trial of six technologies (eFOCUS 1). BMC Medical Education, 21(1), 41. https://doi.org/10.1186/s12909-020-02469-8
Giardini, M. E., Livingstone, I. A. T., Jordan, S., Bolster, N. M., Peto, T., Burton, M., & Bastawrous, A. (2014). A smartphone based ophthalmoscope. [paper presentation]. 36th Annual International Conference of the Engineering in Medicine and Biology Society, EMBC, Chicago, United States. https://doi.org/10.1109/EMBC.2014.6944049
Kaufman, D. M. (2019). Teaching and Learning in Medical Education. How Theory can Inform Practice. Tim Swanwick, Kirsty Forrest, Bridget C. O’Brien (Eds), Understanding medical education evidence, theory, and practice (pp. 37-69). The Association for the Study of Medical Education.
Kim, M. C., & Hannafin, M. J. (2011). Scaffolding problem solving in technology-enhanced learning environments (TELEs): Bridging research and theory with practice. Computers & Education, 56(2), 403-417. Elsevier Ltd. https://www.learntechlib.org/p/67172/.
Kim, Y., & Chao, D. L. (2019). Comparison of smartphone ophthalmoscopy vs conventional direct ophthalmoscopy as a teaching tool for medical students: The COSMOS study. Clinical Ophthalmology, 13, 391–401. https://doi.org/10.2147/OPTH.S190922
Leonardo, D. (2018). Development of a virtual reality ophthalmoscope prototype: Mechatronic Engineering Program Faculty of Engineering, Universidad Militar Nueva Granada, Bogotá D.C., Colombia. http://hdl.handle.net/10654/17843
Liao, Y. Y., & Lin, Y. M. (2008). McNemar test is preferred for comparison of diagnostic techniques. American Journal of Roentgenology, 191(4), 2008. https://doi.org/10.2214/AJR.08.1090
Lötter, M. J., & Jacobs, L. (2020). Using smartphones as a social constructivist pedagogical tool for inquiry-supported problem-solving: An exploratory study. Journal of Teaching in Travel & Tourism, 20(4), 347–363. https://doi.org/10.1080/15313220.2020.1715323
MacKay, D. D., Garza, P. S., Bruce, B. B., Newman, N. J., & Biousse, V. (2015). The demise of direct ophthalmoscopy: A modern clinical challenge. Neurology: Clinical PraFalctice, 5(2), 150–157. https://doi.org/10.1212/CPJ.0000000000000115
Mamtora, S., Sandinha, M. T., Ajith, A., Song, A., & Steel, D. H. W. (2018). Smart phone ophthalmoscopy: A potential replacement for the direct ophthalmoscope. Eye (Basingstoke), 32(11), 1766–1771. https://doi.org/10.1038/s41433-018-0177-1
Mayer, R. E. (2014). Cognitive theory of multimedia learning. The Cambridge Handbook of Multimedia Learning, Second Edition, 43–71. https://doi.org/10.1017/CBO9781139547369.005
Mellis, S., Carvalho, L., & Thompson, K. (2013, December 1-5). Applying 21st century constructivist learning theory to stage 4 design projects. [Conference presentation]. Joint Australian Association for Research in Education Annual Conference, Adelaide. https://files.eric.ed.gov/fulltext/ED603249.pdf
Mrad, Y., Elloumi, Y., Akil, M., & Bedoui, M. H. (2021). A Fast and Accurate Method for Glaucoma Screening from Smartphone-Captured Fundus Images. Irbm, 1, 1–11. https://doi.org/10.1016/j.irbm.2021.06.004
Myung, D., Jais, A., He, L., Blumenkranz, M. S., & Chang, R. T. (2014). 3D Printed Smartphone Indirect Lens Adapter for Rapid, High Quality Retinal Imaging. Journal of Mobile Technology in Medicine, 3(1), 9–15. https://doi.org/10.7309/jmtm.3.1.3
Nagra, M., & Huntjens, B. (2020). Smartphone ophthalmoscopy: Patient and student practitioner perceptions. Journal of Medical Systems, 44(1), Article 10. https://doi.org/10.1007/s10916-019-1477-0
Naseem, A., Ghias, K., Bawani, S., Shahab, M. A., Nizamuddin, S., Kashif, W., Khan, K. S., Ahmad, T., & Khan, M. (2019). Designing EthAKUL: A mobile just-in-time learning environment for bioethics in Pakistan. Scholarship of Teaching and Learning in the South, 3(1), 36–56. https://doi.org/10.36615/sotls.v3i1.70
Purbrick, R. M. J., & Chong, N. V. (2015). Direct ophthalmoscopy should be taught to undergraduate medical students—No. Eye, 29(8), 990-991. https://doi.org/10.1038/eye.2015.91
Riel, M. (2000). Education in the 21st century: Just-in-Time learning or learning communities, Technology and Learning, 137-160.
Russo, A., Morescalchi, F., Costagliola, C., Delcassi, L., & Semeraro, F. (2015). Comparison of smartphone ophthalmoscopy with slit-lamp biomicroscopy for grading diabetic retinopathy. American Journal of Ophthalmology, 159(2), 360-364. https://doi.org/10.1016/j.ajo.2014.11.008
Tan, C. H., Kyaw, B. M., Smith, H., Tan, C. S., & Car, L. T. (2020). Use of smartphones to detect diabetic retinopathy: Scoping review and meta-analysis of diagnostic test accuracy studies. Journal of Medical Internet Research, 22(5), e16658.
Wintergerst, M. W. M., Jansen, L. G., Holz, F. G., & Finger, R. P. (2020). Smartphone-Based Fundus Imaging-Where Are We Now? Asia-Pacific Journal of Ophthalmology, 9(4), 308–314. https://doi.org/10.1097/APO.0000000000000303
World Health Organization. (2019). Report of the 4th global scientific meeting on trachoma: Geneva, 27–29 November 2018. World Health Organization.
*Amelah Mohammed Abdul Qader
University of Cyberjaya Campus
Persiaran Bestari, Cyber 11, 63000 Cyberjaya,
Selangor Darul Ehsan, Malaysia
Email: amelah@cyberjaya.edu.my/ dramelahariqi@gmail.com
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









