Tackling study-work chasm: Perceptions of the role of mentorship in the healthcare workplace
Submitted: 30 May 2021
Accepted: 8 April 2022
Published online: 5 July, TAPS 2022, 7(3), 10-22
https://doi.org/10.29060/TAPS.2022-7-3/OA2539
Hanyi Li1, Elaine Li Yen Tan1,3, Mun Loke Wong2 & Marianne Meng Ann Ong1,3
1National Dental Centre Singapore, Singapore; 2Faculty of Dentistry, National University of Singapore, Singapore; 3Oral Health Academic Clinical Programme, Duke-NUS Medical School, Singapore
Abstract
Introduction: As young healthcare professionals (HCPs) enter the workforce, they find challenges adapting as academic training and workplace settings often do not mirror each other. Mentorship is a possible solution to help bridge this transition. The aim of this study was to gather information from HCPs with regards to their views towards mentorship as a strategy to help in the transition of newly qualified HCPs from study to work.
Methods: Two 3-hour interactive workshops entitled “Bridging the Study-Work Chasm” were organised, and participants were invited to complete a survey voluntarily after the workshop. The survey comprised questions regarding the benefits of mentorship, qualification of mentors, time commitment for mentoring, elements of an effective mentorship programme, and barriers to its effectiveness. The anonymised responses were analysed descriptively.
Results: Fifty-two out of 62 participants from various healthcare backgrounds completed the survey. 96.2% of respondents felt a study-work chasm exists in the healthcare workplace with 90.4% indicating that a mentorship programme would help to bridge the chasm. More than 70% of participants agreed or strongly agreed that mentoring would boost confidence, reduce anxiety, and aid in study-work transition. It was identified that to produce a more effective mentorship programme, time commitment, training, and proper organisation of the programme would be necessary.
Conclusion: It was perceived that a mentorship programme can help to bridge the study-work chasm in the healthcare landscape in Singapore, and will best serve mentors and mentees by committing the proper time and training to ensure its effectiveness.
Keywords: Training-Work Transition, Graduate, Healthcare Professionals, Mentorship
Practice Highlights
- Despite receiving extensive training during their education, healthcare professionals still experience many challenges as they enter the workforce.
- Globally it has been reported that differences in training and workplace demands, coupled with the need to take direct responsibility for patients, propagate anxiety and perceived incompetence in fresh graduates. This could result in compromised work performance and patient outcomes.
- A study-work chasm exists in the healthcare work space, and should be addressed.
- Mentorship was shown to be accepted as a popular solution amongst healthcare workers in Singapore, and the benefits were discussed.
- Elements of a good mentorship programme as well as challenges in setting one up were identified, laying the groundwork for future implementation of such programmes in local public healthcare institutions.
I. INTRODUCTION
Healthcare professionals (HCPs) are known to receive extensive training during their pre-qualification education. However, there still exists many challenges as they enter the workforce. These include increasing workload, encountering patients with more complex conditions, generational diversity in the workforce, performance anxiety, and bullying when transitioning to the workforce (Hofler & Thomas, 2016). While facing these challenges in a new working environment marks the beginning of a fresh process of learning, there are indications that this may be more than what newly qualified professionals can cope with (Teunissen & Westerman, 2011).
There are several contextual differences between pre-employment learning in the university and post-employment learning in the workplace. Fundamentally, the focus of education and real-world practice are different. The commonplace practice of test-taking in school focuses on knowledge retention, with minimal consideration for practical value in the workplace (Lave & Wenger, 1991). A good example of this is the learning of ethical guidelines, which can be easy to regurgitate in school assignments and tests, but are far more difficult to apply on the job (Le Maistre & Paré, 2004). In school, tasks and assignments follow a certain syllabus and scope, which are more structured and predictable than what is expected at the workplace. Similarly, these tasks and assignments in school are indicators of performance and avenues for feedback, while at the workplace such similar opportunities are limited (Wendlandt & Rochlen, 2008).
Healthcare training has had elements of practical application, but the adequacy of these exposures is questionable. Clinical shadowing and observation are known to be helpful, but cannot take the place of actual hands-on clinical experience (Brennan et al., 2010). With increased patient safety concerns, there has also been a shift towards simulation, which reduces meaningful contact with patients and poses challenges when students are expected to ultimately transfer their learning to real-life practice (Bleakley & Bligh, 2008).
The security of observing from a distance and the safe environment for experimentation and reflection that students experience in school have to be left behind as they enter the workplace, apply textbook knowledge in real-life situations, and deal with workplace systems and politics (Le Maistre & Paré, 2004). Efforts to prepare for this transition are misplaced (Kilminster et al., 2011), and the training and educational opportunities aimed to help with this transition, such as those in the transitional year, have been lacklustre and ineffective (Lambert et al., 2013). Therefore, a study-work chasm exists in many places, and is a pertinent and critical issue that requires addressing.
Among efforts to help in the transition of students to new HCPs at the workplace, mentorship has been seen as a possible solution (Andrews & Wallis, 1999; Dalgaty et al., 2017). Mentorship, as previously defined by The Standing Committee on Postgraduate Medical and Dental Education in the United Kingdom, is the guidance in “the development and re-examination of their own ideas, learning, and personal and professional development” by “listening and talking in confidence to the mentee” (Oxley & Standing Committee on Postgraduate Medical and Dental Education, 1998). It has also been built into medical practice guidelines, such as that in the UK (General Medical Council, 2012), as a key element in training and professional development.
Mentorship has been seen as a viable approach not only to address any gaps in professional skills, but also aid junior healthcare workers in personalised professional development in the workplace, to enhance job satisfaction, motivation, and self-esteem (Souza & Viney, 2014). The role of a mentor in medical education is to help mentees identify areas of strength and weaknesses in a comfortable and safe learning environment, offer guidance and advice, and motivate and support them to work towards their personal long-term goals (Burgess et al., 2018). Mentors have roles overlapping that of coaches and advisors in medical education. However, coaches tend to focus more on skills or knowledge-based content, and may have a relationship that is of shorter duration and of less depth than between mentors and mentees (Lin & Reddy, 2019). Advisors often oversee a group of individuals in an organisation. Therefore, they develop a more structured relationship compared to that between mentors and mentees, and tend to work towards an outcome based on the needs of the organisation (Hastings & Kane, 2018). Thus, mentoring has been a widely recognised method of helping young people learn, demonstrate their abilities and potential, as well as develop their identity (Fuller & Unwin, 1998). This is extensively explored and studied in many healthcare institutions and systems today.
The aim of this study was to gather information from HCPs about their views towards mentorship as a strategy to help in the transition of newly qualified HCPs from study to work.
II. METHODS
This was a descriptive study on the perceptions of the study-work chasm by HCPs. The protocols were sent to SingHealth Centralised Institutional Review Board (References: 2017/2687 and 2021/2044) and they were deemed exempt from review.
Two three-hour interactive workshops, entitled “Bridging the Study-Work Chasm”, were held in September 2017 and 2018. The workshops invited participation from HCPs in SingHealth, one of the three public healthcare clusters in Singapore.
Each 3-hour workshop comprised two short talks on ‘Is there a Chasm?’ and ‘Bridging the Chasm’, followed by small-group discussions, then sharing and discussions with the large workshop group. A round-up and summary was done by the respective facilitator after each large-group discussion.
The first talk on ‘Is there a Chasm?’ gave a definition of a study-work chasm and the small groups were then asked to describe how such a chasm manifested in the workplace with two questions: “How do we know if a study-work chasm exists?” and “What contributes to this study-work chasm?” After the sharing by the small groups with the large group and some discussion, the facilitator then summarised differences between learning in an academic setting versus learning in the workplace that could contribute to the study-work chasm.
The second talk on ‘Bridging the Chasm’ invited participants to think about and discuss in their small groups how they could bridge the study-work chasm and what were some of the anticipated barriers in doing this. These were then shared with the large group followed by a summary by the facilitator on how coaching and mentoring could be used to bridge the chasm. Facilitators finally concluded the workshop session with a summary of points, addressing questions and answers, and getting participants to complete the survey and workshop evaluation forms.
The survey was carried out by having the participants fill up either an online survey form via scanning a QR code, or a hardcopy version. Implied consent was obtained with the submission of the survey. The survey consisted of 26 items and two open-ended questions (Appendix 1). The first part utilised dichotomous questions to survey participants about their past and current experiences with mentoring, and their views towards whether a study-work chasm existed and whether mentoring could be a solution to bridge this gap. The second part comprised two open-ended questions, asking participants about the elements of an effective mentorship programme, and barriers to having one. The third part allowed participants to rate their level of agreement with 15 statements, related to the benefits of mentoring, the qualification of mentors, and time commitment for mentoring, on a Likert-like scale of 1-5 (1: Strongly Disagree; 5: Strongly Agree). Questions were adapted from a questionnaire that was developed and pilot-tested in a previous study (Lopez et al., 2010).
The anonymised survey data was collated and analysed descriptively. Common repetitive words that appeared in the responses to the open-ended questions were noted and these were grouped into key themes. The percentage of responses representing each theme was tabulated.
III. RESULTS
A. Respondents
Sixty-two participants comprising HCPs from various backgrounds – doctors, dentists, nurses, ancillary workers, and allied health professionals – attended both workshops. There were no repeat participants who attended the two workshops. The data that support the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.figshare.14740332 (Li et al., 2021). Among the 62 participants, 52 completed the survey, achieving a response rate of 83.9%. A majority (78.8%) of the respondents were females. Dentists were the largest healthcare group represented, comprising 42.6% of respondents, followed by doctors, comprising 21.2%. The age group of 30 to 39 years old had the strongest representation of 44.2%. Most respondents had more than five years of working experience, with 44.2% of respondents having six to 10 years of experience, and 51.9% of respondents having more than 10 years of experience (Figure 1). Among the respondents, 96.2% (50 out of 52) felt that a study-work chasm existed in the healthcare workspace, with 90.4% (47 out of 52) indicating that a mentorship programme would help to bridge the chasm, and a majority (90.4%) of respondents agreed that mentoring would be a viable strategy (the remaining 5 respondents were neutral). A good majority of respondents (67.3%) noted they did not have a mentor when they first started work.
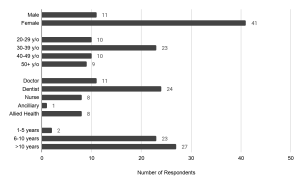
Figure 1. Demographics of survey respondents: gender, age, healthcare group, and number of years of working experience.
B. Key Features of An Effective Mentorship Programme
There was a total of 63 responses describing features of an effective mentorship programme, and the key themes were identified in Figure 2(a). Respondents raised attributes pertaining to the attitude and dynamics of the mentor and mentee, and the organisation of such a programme. Some respondents submitted multiple attributes.
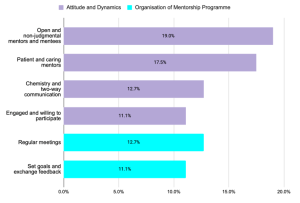
Figure 2(a). Key themes describing key features of an effective mentorship programme
Pertaining to attitude and dynamics, both the mentor and mentee must firstly be engaged and willing to participate in the programme (11.1% of responses). The mentor and mentee should have attributes of open-mindedness and humility (19.0% of responses), and the mentor also ought to be patient, caring, and non-judgmental (17.5% of responses). Finally, the mentor-mentee pair must have good two-way communication, and some degree of interpersonal “chemistry” to bond (12.7% of responses).
Pertaining to the organisation of a mentor-mentee programme, many (12.7% of responses) raised that there should be planned regular meetings, and participants should set goals and expectations and discuss timely feedback (11.1% of responses). However, there was no indication of an ideal frequency of meeting. Some other organisational features were also mentioned. Regarding mentor-mentee pairing, it was noted that the mentor-mentee ratio was an important factor, though there was no indication of a preferred ratio in the responses; others raised that both mentor and mentee should be from relevant fields, for instance from the same department. Some also mentioned that the mentorship programme could be built into the career progression pathway of the mentee to ensure continuation, and even to build it into licensing requirements, such as in the housemanship year for junior doctors.
C. Barriers to Effective Mentorship Programme
There was a total of 53 responses describing barriers to an effective mentorship programme, and the key themes were identified in Figure 2(b). Respondents acknowledged that several aspects of effective mentorship previously mentioned were difficult to achieve, many of which revolved around commitment and mentor-mentee dynamics. A lack of time was identified as the top barrier to implementing a mentoring programme (49.1% of responses). As mentorship can be time consuming, there might be difficulty getting sufficient mentors to willingly commit the time; similarly, it might be challenging to match the availability of mentors and mentees around hectic work hours. Furthermore, there was significant mention (41.5% of responses) about whether the seniority of mentors may result in difficulty breaking the ice with the mentees, or if cultural differences may hinder the understanding of differing perspectives. Some respondents also raised that not all mentors may have the personality, skills or willingness to render effective mentorship, as evidenced in 17.0% of the responses. Finally, some respondents questioned if and how the role of mentors and work supervisors should be differentiated in the workplace.
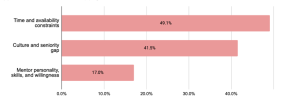
Figure 2(b). Key themes describing barriers to an effective mentorship programme.
Percentages represent the proportion of responses mentioning words related to the theme.
D. Mentorship Benefits and Commitment
On mentorship benefits and commitment, there was strong agreement (more than 70% of participants agreed or strongly agreed) that having a mentor would boost confidence, reduce anxiety, and aid in the transition from study to work (Figure 3). It was also strongly expressed that the participants would have liked a mentor in their first year in the workplace (82.6% agreed), and that the mentorship should extend beyond their first year of work as well – more than half (55.8%) disagreed that the mentorship should only be in the first year, and 90.4% agreed that mentorship would help even in the later years of work. In spite of this, and while a strong majority of 71.2% expressed that they would have liked a long-term mentor-mentee relationship, a large proportion of respondents (44.2%) was neutral towards expecting regular mentor-mentee contact while 38.5% expected mentors to meet regularly with mentees (Figure 4).
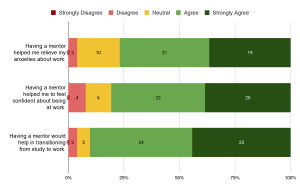
Figure 3. Responses on benefits of mentorship. Numbers in the chart indicate the number of respondents.
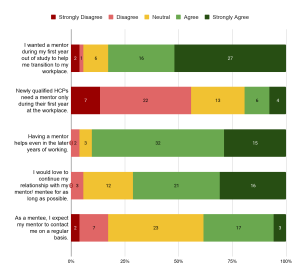
Figure 4. Responses on time commitment of mentorship. Numbers in the chart indicate the number of respondents.
E. Mentor Qualifications and Background
On mentor qualifications, more than half of the respondents agreed that they had adequate knowledge (59.6%) and skills (53.8%) to function as effective mentors. Most of those who agreed (74.2% for knowledge, 67.9% for skills) were HCPs with more than 10 years of experience. A significant proportion responded neutrally as well, with 28.8% and 34.6% for knowledge and skills, respectively. Majority of them (71.4% for knowledge, 52.9% for skills) had 6 to 10 years of work experience in healthcare. Nevertheless, many more (78.8%) agreed that receiving prior training or orientation in mentoring could increase their effectiveness as mentors. When asked about whether young professionals two to three years into their professions make the best mentors, there was strong neutrality in the response (46.1%, the largest proportion). It was noted that all the neutral responses were from HCPs with more than 5 years of experience, with a significant proportion of them (52.2%) having 6 to 10 years of work experience. All except two of the respondents who gave neutral responses had experience as a mentor. Majority (59.6%) preferred mentors to be paired with mentees with similar backgrounds; similarly, there was significant uncertainty around whether mentors from dissimilar professions could be effective, with the same proportion (38.5%) of respondents agreeing and holding a neutral stance towards this view (Figure 5).

Figure 5. Responses on qualification of mentors. Numbers in the chart indicate the number of respondents.
IV. DISCUSSION
The results from this study showed that there was a perceived study-work chasm among this cohort of HCPs. Given the wide range of backgrounds and years of work experience of the respondents, it is also evident that the chasm was perceived across different HCPs and batches of new HCPs entering the workforce.
Indeed, it was reported in the literature that newly qualified HCPs face challenges in the new workplace, indicating a study-work chasm. One such challenge is the lack of hands-on clinical skills. Junior doctors beginning practice and taking direct responsibility for patients found themselves undertaking clinical tasks for which they felt inadequately trained for (Lambert et al., 2013). As such, they expressed anxiety over their competence, especially in areas like prescribing (Brennan et al., 2010; Matheson & Matheson, 2009). It was also reported that new doctors lacked knowledge in pathology and therapeutics (Lempp et al., 2004). These gaps can bring dire consequences to clinical care, influencing assessment, treatment, and outcome of patients (Smith & Poplett, 2002).
In addition, many professionals fresh from school experienced difficulties in communicating with patients. The immediate switch to a professional relationship with patients proved stressful for them, especially in the first few weeks of work (Lempp et al., 2004). The findings of the present study mirror this sentiment with a large proportion of the respondents citing their wish for a mentor in their first year or work. The difficulty was especially evident in such school-work transitions revolved around breaking bad news, dealing with difficult and violent patients, and communicating with people with mental illnesses. Despite active practice and drilling with simulated scenarios in school, fresh graduates still expressed that they were inadequately prepared for these in real life (Matheson & Matheson, 2009).
Mentorship was seen very favourably as a possible solution to bridging the chasm. Among these, more than half of the respondents (67.3%) had not experienced mentoring during their initial years of work, indicating that mentorship had not been widely implemented, and can be a new strategy for exploration in the local healthcare system. It is worthy to note that many of the respondents who had experienced mentorship had also viewed mentorship positively. Similarly, residents of a medical residency programme in Singapore viewed mentorship as being crucial and beneficial to their training, as mentors were able to provide guidance and encouragement, and create a more well-rounded learning environment (Chua et al., 2020). This implies that mentorship could potentially exert a positive impact on HCPs.
The benefits of mentorship have been well-reported worldwide. In particular, there have been reports emphasising its benefits on the emotional and psychological health of healthcare workers. For instance, in the United Kingdom, senior doctors as mentors and teachers helped train fresh graduates on the job, and reduced their stress (Brennan et al., 2010), increased motivation, and boosted self-esteem (Souza & Viney, 2014). In Saudi Arabia, use of coaching appeared to reduce depression and anxiety among HCPs in the short-term (Aboalshamat et al., 2015). A study in Denmark reported improved professional identity among their fresh doctors who had undergone group mentorship sessions, and participants developed new ways to deal with their new professional roles with increased awareness of their thinking, feelings, and reactions, making the stressful transition into their workplace more bearable (de Lasson et al., 2016). All these resonate well with the responses from this study, that mentorship can reduce anxiety and boost confidence in new HCPs.
Studies have shown attributes of an effective mentorship programme. Many of these attributes relate to the attitudes of mentors and mentees – trust and respect, responsibility, and taking initiative. The importance of having good communication, connection, and common values between mentors and mentees were also emphasised. These were consistent across countries, as seen in studies in North America (Straus et al., 2013) and the United Kingdom (Ssemata et al., 2017). Notably, these attributes were mentioned significantly in the responses collected in this study as well, specifically those relating to mentor-mentee dynamics.
Barriers to effective mentorship have also been brought up in several studies, and draw similarities to the responses obtained from this study. It was summarised that challenges can arise when there is a mismatch of goals, expectations, and time commitment between mentors and mentees. There can also be hindrances to communication due to generational and personality differences (Zerzan et al., 2009). Qualitative studies targeting students, junior faculty mentees and senior faculty members at healthcare institutions uncovered similar issues (Ssemata et al., 2017; Straus et al., 2013).
In this study, questions and uncertainties were raised pertaining to whether mentors should be supervisors as well, and how regular meetings should be held. It is noteworthy that in the United Kingdom, Ssemata et al. (2017) reported findings that there presented conflicts of interest when mentors were also supervisors. Such an arrangement posed problems with performance judgement, competition, and the amount of honesty in the mentor-mentee relationship. In the same study, it was noted that the mentor-mentee pairing could likely be better maximised if the pairing was selected mutually by the mentor and mentee, instead of being pre-assigned, as this would ensure better chemistry and as a result better commitment and motivation towards the relationship. Regular time commitment was generally agreed upon in literature; however, discussions on frequency were inconclusive, similar to the responses of this present study. It was reported in North America that the preferred frequency of meet-ups according to participating mentors and mentees ranged widely from monthly to half-yearly (Straus et al., 2013).
The literature has identified some other barriers to setting up of an effective mentorship programme not surfaced in our study that are worthy of note. In particular, factors relating to the organisation or system play a big part in the effectiveness of the mentorship programme. Geographical location, for instance, is one barrier identified in systems where mentors and mentees may be situated at different sites, such as different hospital campuses, and have difficulty meeting (Soklaridis et al., 2015). This can be the case when HCPs are posted to different clinical sites, or when HCPs across sites are linked up to increase diversity in mentorship. The strong focus by organisations on delivering clinical service may also have spared little resources and manpower for mentorship programmes (Ploeg et al., 2008), rendering such programmes inadequate support. For instance, the use of manpower and facilities for mentorship activities in job-specific areas such as a clinical simulation can be limited when these are dedicated to patient care (Morgan et al., 2018). Finally, a strong culture of hierarchy seen in healthcare settings, such as among nurses, can be a hindrance to the open-mindedness and non-judgemental nature of mentoring that the programme aspires to achieve (Morgan et al., 2018).
Nevertheless, it is clear from existing literature that a formalised mentorship programme would ensure the best outcomes, as time and resources can be dedicated to the programme to ensure better recruitment, matching and co-ordination between mentors and mentees, proper structure and guidelines so as to ensure mentorship outcomes are reviewed at adequate intervals and achieved within a desired timeframe, and adequate training for mentors to render support and guidance to their mentees. A proper programme can likely reduce the challenges to effective mentorship as raised by the respondents of this study, as well as in other studies. Lack of experience of mentors, for instance, was a main failure in mentoring relationships (Straus et al., 2013). Similarly, in this study, a significant finding was that there was a larger proportion of respondents with relatively fewer years of work experience who gave neutral responses towards statements on whether they had sufficient knowledge and skills to function effectively as mentors, compared to statements on benefits of mentorship and their preferences towards having a mentorship programme. This indicated a lower perceived confidence of these respondents in their effectiveness as mentors. In line with this, there was strong agreement that receiving training and orientation in mentoring would have been preferred prior to them assuming such mentoring roles, presumably regardless of their prior work experiences. This reinforces the need for proper training and resources for mentors in order for the mentorship programme to see positive effects.
This study presents with some limitations. Firstly, while there was a diverse range of backgrounds among the workshop participants, the proportions may not be representative of the healthcare landscape in Singapore. As such, this may introduce a potential source of bias towards views of predominant groups of participants such as the dentists. Nevertheless, the findings provide a useful baseline understanding of how other healthcare professionals view mentoring. This could, in turn, set the stage for more extensive work in this area among other healthcare professionals. Secondly, the respondents participated in the workshop prior to responding to this survey. The workshop raised awareness towards a study-work chasm and presented mentorship as one of the possible solutions. Therefore, it might have resulted in a stronger perception of this chasm among respondents, and induced more favourable views towards mentorship. Nevertheless, the participants’ positive views towards mentorship could be viewed as indications of the strong agreement they had towards mentorship as a solution highlighted in the workshop. In future workshops, qualitative focused-group discussions can be carried out, and questionnaires can be administered before and after the workshop, so as to establish a more accurate perception of study-work chasm among participants.
V. CONCLUSION
This study has shown that with a perceived presence of a study-work chasm in the healthcare landscape in Singapore, there were strong preferences for a mentorship programme in bridging this chasm. The benefits of a mentorship programme, and the attributes and challenges of setting up such an effective programme were identified, and echo the findings from existing studies from other regions and healthcare systems in the world. In particular, there were emphases on positive attitudes of mentors and mentees, and alignment of expectations between them. There was also strong indication that mentors require proper training. A formalised mentorship programme will best serve mentors and mentees by committing the proper time and resources to ensure its effectiveness.
This study lays the groundwork for future efforts to help fresh graduates better transition into the healthcare workplace using mentorship programmes. In particular, the study targeted healthcare professionals working in the healthcare system in Singapore and revealed their sentiments and opinions towards mentorship, paving the way for local efforts to improve healthcare education and mentorship. Moving forward, further studies can be carried out in an in-depth manner to investigate specific areas of concern pertaining to setting up an effective mentorship programme, such as mentor training, time commitment, and mentor-mentee pairing. Studies can be expanded to larger pools of participants, and targeted at specific sectors and participant groups, for example medical doctors in their housemanship year, to better cater to specific professional needs. Focused-group discussions can be carried out to collect more detailed, qualitative responses and feedback from potential mentors and mentees. Furthermore, this information can be used to engage stakeholders in public healthcare institutions in Singapore and the region, and execute pilot tests of formalised mentorship programmes tailor-made to the institution’s structure and the newly qualified HCPs’ needs.
Notes on Contributors
ELY Tan, ML Wong, and MMA Ong planned, developed, and conducted the workshops and data collection. H Li and ELY Tan, together with ML Wong and MMA Ong planned and wrote the manuscript. All authors read and approved the final manuscript.
Ethical Approval
The study protocols were sent to SingHealth Centralised Institutional Review Board (References: 2017/2687 and 2021/2044) and they were deemed exempt from review.
Data Availability
The data that support the findings of this study are openly available in Figshare with DOI: https://doi.org/10.6084/m9.figshare.14740332
Acknowledgement
The authors would like to thank the administrative team from SingHealth Duke-NUS Oral Health Academic Clinical Programme (Education) for their help and support in the smooth running of the workshops and collection of data.
Funding
No funding was sought for this study.
Declaration of Interest
The authors declare that they have no conflicts of interest, and do not foresee any future competing interests.
References
Aboalshamat, K., Hou, X.-Y., & Strodl, E. (2015). The impact of a self-development coaching programme on medical and dental students’ psychological health and academic performance: A randomised controlled trial. BMC Medical Education, 15(1), 134. https://doi.org/10.1186/s12909-015-0412-4
Andrews, M., & Wallis, M. (1999). Mentorship in nursing: A literature review. Journal of Advanced Nursing, 29(1), 201–207. https://doi.org/10.1046/j.1365-2648.1999.00884.x
Bleakley, A., & Bligh, J. (2008). Students learning from patients: Let’s get real in medical education. Advances in Health Sciences Education, 13(1), 89–107. https://doi.org/10.1007/s10459-006-9028-0
Brennan, N., Corrigan, O., Allard, J., Archer, J., Barnes, R., Bleakley, A., Collett, T., & De Bere, S. R. (2010). The transition from medical student to junior doctor: Today’s experiences of tomorrow’s doctors. Medical Education, 44(5), 449–458. https://doi.org/10.1111/j.1365-2923.2009.03604.x
Burgess, A., van Diggele, C., & Mellis, C. (2018). Mentorship in the health professions: A review. The Clinical Teacher, 15(3), 197–202. https://doi.org/10.1111/tct.12756
Chua, M. J., Foo, G. L., & Kwek, E. B. K. (2020). A tiered mentorship framework in an Orthopaedic Surgery Residency Programme. The Asia Pacific Scholar, 5(1), 54–60. https://doi.org/10.29060/TAPS.2020-5-1/OA2095
Dalgaty, F., Guthrie, G., Walker, H., & Stirling, K. (2017). The value of mentorship in medical education. The Clinical Teacher, 14(2), 124–128. https://doi.org/10.1111/tct.12510
de Lasson, L., Just, E., Stegeager, N., & Malling, B. (2016). Professional identity formation in the transition from medical school to working life: A qualitative study of group-coaching courses for junior doctors. BMC Medical Education, 16(1), 165. https://doi.org/10.1186/s12909-016-0684-3
Fuller, A., & Unwin, L. (1998). Reconceptualising apprenticeship: Exploring the relationship between work and learning. Journal of Vocational Education & Training, 50(2), 153–173. https://doi.org/10.1080/13636829800200043
General Medical Council. (2012, March 12). Leadership and management for all doctors. https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/leadership-and-management-for-all-doctors
Hastings, L. J., & Kane, C. (2018). Distinguishing mentoring, coaching, and advising for leadership development. New Directions for Student Leadership, 2018(158), 9–22. https://doi.org/10.1002/yd.20284
Hofler, L., & Thomas, K. (2016). Transition of new graduate nurses to the workforce. North Carolina Medical Journal, 77(2), 133-136. https://doi.org/10.18043/ncm.77.2.133
Kilminster, S., Zukas, M., Quinton, N., & Roberts, T. (2011). Preparedness is not enough: Understanding transitions as critically intensive learning periods. Medical Education, 45(10), 1006–1015. https://doi.org/10.1111/j.1365-2923.2011.04048.x
Lambert, T. W., Surman, G., & Goldacre, M. J. (2013). Views of UK-trained medical graduates of 1999–2009 about their first postgraduate year of training: National surveys. BMJ Open, 3(4), e002723. https://doi.org/10.1136/bmjopen-2013-002723
Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation (p. 138). Cambridge University Press. https://doi.org/10.1017/CBO9780511815355
Le Maistre, C., & Paré, A. (2004). Learning in two communities: The challenge for universities and workplaces. Journal of Workplace Learning, 16(1/2), 44–52. https://doi.org/10.1108/13665620410521503
Lempp, H., Cochrane, M., Seabrook, M., & Rees, J. (2004). Impact of educational preparation on medical students in transition from final year to PRHO year: A qualitative evaluation of final-year training following the introduction of a new Year 5 curriculum in a London medical school. Medical Teacher, 26(3), 276–278. https://doi.org/10.1080/248-0142159042000192046
Li, H., Tan, E. L. Y., Wong, M. L., & Ong, M. M. A. (2021). Tackling study-work chasm: Perceptions of the role of mentorship in the healthcare workplace [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14740332
Lin, J., & Reddy, R. M. (2019). Teaching, mentorship, and coaching in surgical education. Thoracic Surgery Clinics, 29(3), 311–320. https://doi.org/10.1016/j.thorsurg.2019.03.008
Lopez, N., Johnson, S., & Black, N. (2010). Does peer mentoring work? Dental students assess its benefits as an adaptive coping strategy. Journal of Dental Education, 74(11), 1197–1205. https://doi.org/10.1002/j.0022-0337.2010.74.11.tb04993.x
Matheson, C., & Matheson, D. (2009). How well prepared are medical students for their first year as doctors? The views of consultants and specialist registrars in two teaching hospitals. Postgraduate Medical Journal, 85(1009), 582. https://doi.org/10.1136/pgmj.2008.071639
Morgan, M. C., Dyer, J., Abril, A., Christmas, A., Mahapatra, T., Das, A., & Walker, D. M. (2018). Barriers and facilitators to the provision of optimal obstetric and neonatal emergency care and to the implementation of simulation-enhanced mentorship in primary care facilities in Bihar, India: A qualitative study. BMC Pregnancy and Childbirth, 18(1), 420. https://doi.org/10.1186/s12884-018-2059-8
Oxley, J., & Standing Committee on Postgraduate Medical and Dental Education. (1998). Supporting doctors and dentists at work: An enquiry into mentoring. SCOPME.
Ploeg, J., de Witt, L., Hutchison, B., Hayward, L., & Grayson, K. (2008). Evaluation of a research mentorship program in community care. Evaluation and Program Planning, 31(1), 22–33. https://doi.org/10.1016/j.evalprogplan.2007.10.002
Smith, G. B., & Poplett, N. (2002). Knowledge of aspects of acute care in trainee doctors. Postgraduate Medical Journal, 78(920), 335. https://doi.org/10.1136/pmj.78.920.335
Soklaridis, S., López, J., Charach, N., Broad, K., Teshima, J., & Fefergrad, M. (2015). Developing a mentorship program for psychiatry residents. Academic Psychiatry, 39(1), 10–15. https://doi.org/10.1007/s40596-014-0163-2
Souza, B. D., & Viney, R. (2014). Coaching and mentoring skills: Necessities for today’s doctors. BMJ, 348, g4244. https://doi.org/10.1136/bmj.g4244
Ssemata, A. S., Gladding, S., John, C. C., & Kiguli, S. (2017). Developing mentorship in a resource-limited context: A qualitative research study of the experiences and perceptions of the makerere university student and faculty mentorship programme. BMC Medical Education, 17(1), 123. https://doi.org/10.1186/s12909-017-0962-8
Straus, S. E., Johnson, M. O., Marquez, C., & Feldman, M. D. (2013). Characteristics of successful and failed mentoring relationships: A qualitative study across two academic health centers. Academic Medicine, 88(1), 82–89. https://doi.org/10.1097/ACM.0b013e31827647a0
Teunissen, P. W., & Westerman, M. (2011). Opportunity or threat: The ambiguity of the consequences of transitions in medical education. Medical Education, 45(1), 51–59. https://doi.org/10.1111/j.1365-2923.2010.03755.x
Wendlandt, N. M., & Rochlen, A. B. (2008). Addressing the college-to-work transition: Implications for university career counselors. Journal of Career Development, 35(2), 151–165. https://doi.org/10.1177/0894845308325646
Zerzan, J. T., Hess, R., Schur, E., Phillips, R. S., & Rigotti, N. (2009). Making the most of mentors: A guide for mentees. Academic Medicine, 84(1), 140–144. https://doi.org/10.1097/ACM.0b013e3181906e8f
*Eileen Lew
National Dental Centre Singapore
5 Second Hospital Avenue,
Singapore 168938
Email: elaine.tan.l.y@singhealth.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









