Supporting paediatric residents as teaching advocates: Changing students’ perceptions
Submitted: 16 October 2019
Accepted: 11 February 2020
Published online: 1 September, TAPS 2020, 5(3), 62-70
https://doi.org/10.29060/TAPS.2020-5-3/OA2204
Benny Kai Guo Loo1, Koh Cheng Thoon2, Jessica Hui Yin Tan1, Karen Donceras Nadua2 & Cristelle Chu-Tian Chow1
1General Paediatric Service, KK Women’s and Children’s Hospital, Singapore; 2Infectious Diseases Service, KK Women’s and Children’s Hospital, Singapore
Abstract
Introduction: Residents-as-teachers (RAT) programmes benefit both medical students and residents. However, common barriers encountered include busy clinical duties, congested lesson schedules and duty-hour regulations.
Methods: The study aimed to determine if providing a structured teaching platform and logistic support, through the Paediatric Residents As Teaching Advocates (PRATA) programme, would enhance residents’ teaching competencies and reduce learning barriers faced by medical students. The programme was held over 23 months and participated by 502 medical students. Residents were assigned as intervention group tutors and conducted bedside teachings. The evaluation was performed by medical students using paper surveys with 5-point Likert scales at the start and end of the programme.
Results: We found that students in the intervention groups perceived residents to be more competent teachers. The teaching competencies with the most significant difference were residents’ enthusiasm (intervention vs control: 4.34 vs 3.92), giving constructive feedback (4.23 vs 3.83) and overall teaching effectiveness (4.27 vs 3.89). Higher scores indicated better teaching competency. Similarly, the intervention groups perceived fewer barriers. More improvement was noted in the intervention groups with regards to busy ward work as a teaching barrier as the scores improved by 0.49, compared to 0.3 in the control groups.
Conclusion: This study demonstrated that providing a structured teaching platform could enhance residents’ teaching competencies and logistic support could help overcome common barriers in RAT programmes. This combination could enhance future RAT programmes’ effectiveness.
Keywords: Paediatric, Resident-As-Teacher, Teaching Competency, Barrier, Clinical Duty, Lesson Schedule, Duty-Hour Regulation
Practice Highlights
- RAT programme with structured, dedicated teaching platforms can improve residents’ teaching competencies.
- Assigning tutor responsibilities to residents can increase their level of enthusiasm and perception of self-importance as a tutor.
- Busy work commitment, congested lesson schedules and duty-hour regulations are barriers in RAT programmes.
- Logistic support is effective in overcoming common barriers in RAT programmes.
I. INTRODUCTION
Residents play a vital role in the education of medical students. They spend up to 25% of their time teaching and research has shown that they can improve medical students’ knowledge and examination scores (McKean, & Palmer, 2015). With the shift of postgraduate medical training in Singapore to the residency system under Accreditation Council on Graduate Medical Education-International (ACGME-I) in 2011, teaching is recognised as an important competency for residents (Accreditation Council for Graduate Medical Education, 2017).
Studies have demonstrated the benefits of residents-as-teachers (RAT) programmes for both residents and medical students (Hill, Yu, Barrow, & Hattie, 2009). A controlled trial of RAT programme involving 24 obstetrics and gynaecology residents showed that their teaching skills have improved via objective structured teaching examination (Gaba, Blatt, Macri, & Greenberg, 2007). Subjectively, residents feel that teaching improves their clinical knowledge (Post, Quattlebaum, & Benich III, 2009). A successful RAT programme also enhances the students’ perception of the resident as a physician (Wamsley, Julian, & Wipf, 2004), as well as higher overall satisfaction with the clinical posting (Huynh, Savitski, Kirven, Godwin, & Gil, 2011). Furthermore, effective resident teachers can influence the students’ future career choices (Musunuru, Lewis, Rikkers, & Chen, 2007).
Although residents acknowledge that teaching is part of their duty and have the desire to teach, there are also many barriers encountered. A common problem is the heavy burden of clinical duties and lack of uninterrupted time (Wamsley et al., 2004). The limitation of time was further worsened by the introduction of duty-hour regulations (Brasher, Chowdhry, Hauge, & Prinz, 2005). The residents understandably prioritise clinical work and are exhausted after completion of clinical duties, leaving little time or energy to focus on education. Other challenges include a lack of confidence and insufficient training as an educator (Yedidia, Schwartz, Hirschkorn, & Lipkin, 1995). A survey of paediatric residents indicated that prior training in teaching can benefit the residents in teaching students (Busari, Scherpbier, Van Der Vleuten, & Essed, 2000).
A. Conceptual Framework
As learning involves knowledge organisation through the continuous addition and modification of concepts and relations over time, it is understandable that experts would have a more complex knowledge structure compared to novices (Meller, M. Chen, R. Chen, & Haeseler, 2013). The difference in knowledge structure between the experts and novices would be significant. Intermediate learners, such as paediatric residents, in this case paediatric residents, with a knowledge structure more similar to novices, would, therefore, be able to better appreciate and address the cognitive problems encountered by the medical students. Paediatric residents would be in an optimal position to minimise the distance between what the novice already knows and what needs to be learned, also referred to as the “zone of proximal development” (Ten Cate, Snell, Mann, & Vermunt, 2004).
Engaging residents as teachers utilise the principles of near-peer teaching. Social and cognitive congruence, demonstrated by Schmidt and Moust (1995), as well as Lockspeiser, O’Sullivan, Teherani, and Muller (2008), supports the near-peer teaching relationship. Social congruence enables residents to communicate with students in an informal, empathic way which in turn encourages student engagement and drives learning (Schmidt & Moust, 1995). Cognitive congruence, whereby residents have a better appreciation of students’ deficits in knowledge, enables residents to clarify problems at a level appropriate and relevant to students (Lockspeiser et al., 2008).
Utilising these principles, we have developed the RAT programme, Paediatric Residents As Teaching Advocates (PRATA), for our residents to engage in formal, structured teaching duties. The authors believe that residents can teach more effectively with a structured teaching platform, and medical students will experience fewer barriers with logistic support from RAT programme.
II. METHODS
A controlled, prospective, pre-post study was carried out at KK Women’s and Children’s Hospital (KKH), Department of Paediatric Medicine, from June 2014 to April 2016. As this study was categorised as an education quality improvement, Singhealth Centralised Institutional Review Board (CIRB) indicated that formal IRB review was not required. Implied informed consent was obtained from participants during a briefing prior to the data collection.
A. Study Setting and Participants
KKH is the largest academic paediatric medical centre in Singapore, with a capacity of more than 800 inpatient beds. The paediatric residency programme also trains more than half of the paediatric residents nationwide.
Third-year medical students from the NUS Yong Loo Lin School of Medicine are attached to KKH for 1-month clinical posting as part of their paediatric training. Every batch of students consists of 6 tutorial groups and each group has 5 to 6 students. Each tutorial group is assigned to a ward team for the entire posting. The students are also required to evaluate and provide feedback on their tutors at the end of the posting.
Four to five paediatric consultants are assigned to each tutorial group as their dedicated tutors. These consultants are paediatric specialists who have completed a recognised training programme and are accredited by the Specialist Accreditation board. Every consultant has more than 3 years’ experience of teaching medical students.
All paediatric residents in their first 3 years of training (n=49) had attended workshops on “Effective Bedside Teaching using the Five-Minute Preceptor” (half-day programme with lectures and practice sessions on microteaching skills for effective clinical teaching) and “Giving Effective Feedback” (half-day programme with lectures and role-play sessions on a 4-step model for constructive feedback). These residents were invited to take part in the PRATA programme through email and participation was voluntary. Thirty-three paediatric residents (67%) participated in the PRATA programme.
B. Study Implementation
The study coordinators randomly assigned 3 medical student tutorial groups to be intervention groups and the remaining 3 groups as controls at the beginning of each posting. A total of 51 intervention and 51 control groups were assigned over 17 batches of students. The intervention included assigning 1 resident to the tutor group with a structured teaching schedule to assist with logistics coordination (Figure 1). The resident was to conduct 2 bedside teaching sessions, focusing on history taking and physical examination techniques. Two administrators from the education office were involved in the scheduling of the teaching roster according to the residents’ ward roster and work commitments, and in line with ACGME-I duty-hour restrictions. This ensured that the arrangements were specifically catered for the respective residents as they were often in different areas of work and thus have varying work commitments.
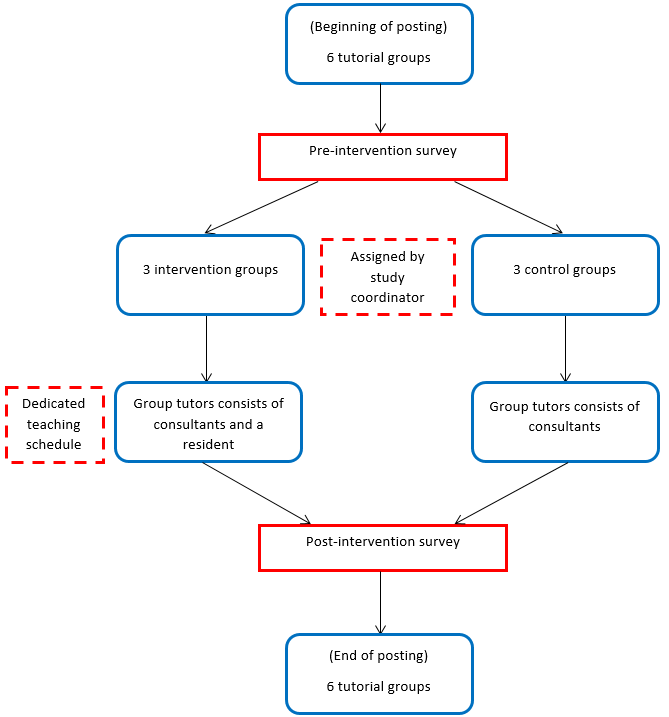
Note: A total of 17 batches of students with 51 intervention and 51 control groups participated in the programme.
Figure 1. PRATA programme protocol diagram (per batch)
For comparison, the existing teaching interactions between residents and medical students in the wards were evaluated in the control groups. As the students were attached to the same ward team for the posting, the residents in the ward team could teach the medical students. Often, these teaching sessions were unplanned, brief and limited by the burden of clinical work.
Apart from the additional resident tutor in the intervention groups, both groups of students received the same standard of medical education, comprising of the same series of planned lectures, the number of bedside tutorials by the consultants, and the duration of ward and clinic attachments.
C. Survey Forms
Paper surveys were given to all students at the beginning (9-question survey) and the end of the posting (18-question survey). These surveys were anonymised and collected by the study coordinators. The survey design was based on 2 studies by Copeland and Hewson (2000), and Hill et al. (2012). These rating instruments were chosen as they were widely used in assessing RAT programmes, applicable in a variety of clinical setting and frequently cited to date. To suit the local context, relevant questions were extracted by the study coordinators based on residents’ feedback and modified accordingly. A 5-point Likert scale was used for the questions, ranging from strongly disagree to strongly agree. A free-text box was included for any comments on both surveys.
|
Effectiveness of Resident Teaching |
Strongly Disagree |
Disagree |
Neutral |
Agree |
Strongly Agree |
|
My medical knowledge and/or clinical skills have improved significantly during the clerkship after being taught by residents |
|
|
|
|
|
|
We received adequate teaching from residents during the clerkship |
|
|
|
|
|
|
The resident established a good learning environment |
|
|
|
|
|
|
The resident stimulated me to learn independently |
|
|
|
|
|
|
The resident offered regular and constructive feedback (both positive and negative) in a timely manner and in an appropriate setting |
|
|
|
|
|
|
The resident clearly specified what we were expected to know and do for the tutorial |
|
|
|
|
|
|
The resident was able to adjust the teaching according to my needs (experience, competence, interest) |
|
|
|
|
|
|
The resident asked questions that promoted learning (e.g. clarification, reflective questions) |
|
|
|
|
|
|
The resident gave clear explanations or reasons for his/her opinions, advice and actions etc. |
|
|
|
|
|
|
The resident was able to effectively coach me on my clinical skills |
|
|
|
|
|
|
The resident taught or demonstrated effective patient and/or family communication skills |
|
|
|
|
|
|
The residents are enthusiastic about teaching |
|
|
|
|
|
|
The resident made teaching relevant to patient care |
|
|
|
|
|
|
Overall, the resident was an effective teacher |
|
|
|
|
|
|
Barriers to Resident Teaching |
Strongly Disagree |
Disagree |
Neutral |
Agree |
Strongly Agree |
|
Ward work was too busy and residents had no time for teaching |
|
|
|
|
|
|
There were too many lectures and tutorials outside of the ward to allow for resident teaching |
|
|
|
|
|
|
Personal Impact of Resident Teaching |
Strongly Disagree |
Disagree |
Neutral |
Agree |
Strongly Agree |
|
The resident tutor was a positive role model for me |
|
|
|
|
|
|
After being taught and interacting with my resident teacher, it would make me more likely consider/select Paediatrics as my choice for future residency training |
|
|
|
|
|
|
Any other comments:
|
The pre-programme survey (Appendix) asked the students about their expectations of residents as teachers, as well as the perceived barriers to receiving resident teachings. The post-programme survey (Table 1) focused on the students’ evaluation of residents’ teaching competencies, the impact of resident teachings and the barriers encountered. For the post-programme survey, the intervention groups evaluated the resident from their tutor group, whereas the control groups evaluated the resident from the ward team.
D. Statistical Analysis
Data were expressed as mean scores with standard deviations. For questions about residents’ teaching competencies, post-programme differences were evaluated between groups using the Mann-Whitney U test. For questions on barriers to receiving resident teachings, pre and post-programme differences were evaluated within and between groups using the Wilcoxon signed-rank test and the Mann-Whitney U test respectively. A p-value of less than 0.05 was taken to be significant for all tests. Analyses were conducted using SPSS version 19.
III. RESULTS
A. Participant Demographics
A total of 502 medical students from 17 batches participated in the PRATA programme over 23 months. Overall, there was 100% pre-programme and 81% (410 students) post-programme participation. The post-programme participation was 74% in the control group and 88% in the intervention group. The baseline demographics were comparable between the groups.
B. Resident Teaching Competencies
A higher score indicated better teaching competency. The intervention group students gave significantly better scores across all aspects for the residents’ teaching competencies as compared to the control groups (Table 2). The biggest difference was noted in the question of the enthusiasm shown by the residents. The intervention groups scored 4.34 and the control groups scored 3.92. The next greatest difference was from the question of residents giving regular and constructive feedback. The scores for the intervention and control groups were 4.23 and 3.83 respectively. The overall assessment of residents as effective teachers showed a similar trend as the intervention groups scored 4.27 and the control groups scored lower at 3.89. The differences in these competencies were all statistically significant.
|
Post-programme survey questions on resident teaching competencies |
Control (n = 188) |
Intervention (n = 222) |
P# |
|
Mean* (SD) |
Mean* (SD) |
||
|
My medical knowledge and/or clinical skills have improved significantly during the clerkship after being taught by residents |
3.92 (0.53) |
4.05 (0.65) |
0.01 |
|
We received adequate teaching from residents during the clerkship |
3.62 (0.79) |
3.94 (0.75) |
<0.01 |
|
The resident established a good learning environment |
3.94 (0.59) |
4.27 (0.57) |
<0.01 |
|
The resident stimulated me to learn independently |
3.88 (0.61) |
4.10 (0.62) |
<0.01 |
|
The resident offered regular and constructive feedback (both positive and negative) in a timely manner and in an appropriate setting |
3.83 (0.66) |
4.23 (0.61) |
<0.01 |
|
The resident clearly specified what we were expected to know and do for the tutorial |
3.72 (0.68) |
4.09 (0.68) |
<0.01 |
|
The resident was able to adjust the teaching according to my needs (experience, competence, interest) |
3.91 (0.64) |
4.22 (0.66) |
<0.01 |
|
The resident asked questions that promoted learning (e.g. clarifications, probes, reflective questions) |
3.94 (0.62) |
4.24 (0.61) |
<0.01 |
|
The resident gave clear explanations or reasons for his/her opinions, advice and actions etc. |
3.95 (0.58) |
4.28 (0.58) |
<0.01 |
|
The resident was able to effectively coach me on my clinical skills |
3.84 (0.68) |
4.17 (0.65) |
<0.01 |
|
The resident taught or demonstrated effective patient and/or family communication skills |
3.89 (0.69) |
4.20 (0.62) |
<0.01 |
|
The residents are enthusiastic about teaching |
3.92 (0.65) |
4.34 (0.67) |
<0.01 |
|
The resident made teaching relevant to patient care |
3.90 (0.61) |
4.26 (0.59) |
<0.01 |
|
Overall, the resident was an effective teacher |
3.89 (0.63) |
4.27 (0.67) |
<0.01 |
Note: *Higher mean score indicates better competency.
#Mann-Whitney U test used for between-group comparisons.
Table 2. Results of survey questions relating to resident teaching competencies
C. Barriers to Resident Teachings
A lower mean score indicated less significant barrier to receiving resident teachings. Generally, the mean scores on barriers reported by the intervention groups decreased more than the control groups after the programme. For the question on busy ward work as a barrier for residents to teach, both groups started with the same mean score of 3.52. At the end of the posting, more improvement was noted in the intervention groups as the mean score decreased to 3.03, as compared to 3.22 in the control groups. Although the difference was statistically significant within the groups, it was not significant when comparing the post-programme difference between the groups (Table 3). For the question about too many lectures and tutorials as a barrier for students to attend resident teachings, the score decreased from 2.90 to 2.59 in the intervention groups. In contrast, the scored increased from 2.90 to 3.07 in the control groups, which meant that the barrier remained significant throughout their posting. The difference in the intervention groups and the post-programme difference between the groups were both statistically significant (Table 3).
|
Survey questions on barriers to resident teaching |
Control group (n = 188) |
Intervention group (n = 222) |
Control vs Intervention |
||||
|
Pre-programme Mean* (SD) |
Post-programme Mean* (SD) |
Pre-Post Difference P# |
Pre-programme Mean* (SD) |
Post-programme Mean* (SD) |
Pre-Post Difference P# |
Post Difference P^ |
|
|
Ward work was too busy and residents had no time for teaching |
3.52 (0.81) |
3.22 (0.89) |
<0.01 |
3.52 (0.79) |
3.03 (1.01) |
<0.01 |
0.42 |
|
There were too many lectures and tutorials outside of the ward to allow for resident teaching |
2.90 (0.76) |
3.07 (0.87) |
0.31 |
2.90 (0.82) |
2.59 (0.95) |
<0.01 |
<0.01 |
Note: *Lower mean score indicates less severe barrier.
#Wilcoxon signed-rank test used for within-group comparisons.
^Mann-Whitney U test used for between-group comparisons.
Table 3. Results of survey questions relating to barriers to receiving resident teachings
IV. DISCUSSION
RAT programmes have demonstrated improvement in residents’ teaching competencies and contribute significantly to the education of medical students (Hill et al., 2009). Although barriers to resident teachings such as excessive workload and duty hour regulations have been identified (Wamsley et al., 2004), there is limited literature on overcoming these obstacles in RAT programmes.
The main aims of the PRATA programme are to provide paediatric residents with a structured teaching platform to improve their teaching competencies and logistic support to overcome common barriers in RAT programmes. The residents in the PRATA programme had the added elements of a dedicated environment for teaching and assuming the role and responsibility as a teaching faculty. The education office also provided these residents with logistic support to reduce scheduling conflicts and duty-hour violations.
This study revealed that the PRATA programme improved the students’ perceptions of the residents’ teaching competencies. This is consistent that RAT programmes enhance resident teaching skills (Zackoff, Jerardi, Unaka, Sucharew, & Klein, 2015). The residents in the intervention groups achieved higher scores in all teaching competency domains, and this included innate characteristics (displaying enthusiasm), techniques (giving constructive feedback) and bedside skills (demonstrating effective communication). A higher score indicated better proficiency in that domain. Although both groups of residents were equipped with the same set of teaching skills, those in the PRATA programme were provided with a structured teaching platform as compared to the unpredictable and potentially chaotic ward setting in the control groups. Furthermore, assigning the residents responsibility as the group tutors possibly increased their level of enthusiasm and perception of self-importance as a tutor. Our study demonstrated that residents in RAT programmes that provide structure to apply their teaching skills can be perceived as better educators.
The results also showed that students from both student groups were very worried about the barriers to receiving resident teachings before the programme. They were more concerned about the residents’ busy work commitments as compared to their congested lesson schedules. Our programme was able to reduce the impact of these barriers as both scores improved significantly in the intervention groups. In contrast, the control groups continued to perceive after the posting that their lesson schedules did not permit residents to teach. Overall, the students from the intervention groups seemed to have a more positive learning experience as there were 20% more students who considered working in Paediatric Medicine in the future. The PRATA programme highlighted that logistic support was an important factor to decrease the students’ concerns of these barriers, which could impede them seeking learning opportunities from the residents.
We have identified some limitations of our study. Firstly, the residents participated in the programme voluntarily, therefore we could have recruited residents who were more passionate or more experienced in teaching. Therefore, we aim to recruit all residents and stratify them by their level of training for the subsequent studies. Secondly, there was no standardisation of the teaching topics. The residents in the intervention groups could have taught in the areas they were more confident in, whereas the residents in the control group could only teach about the patients in the ward. For future studies, we can assign the same teaching topics when evaluating the residents’ teaching competencies. Lastly, the improvement of scores in the intervention groups, although statistically significant, can be complex to interpret in the practical setting. A qualitative study on these aspects can give more insight, such as the specific traits or techniques that residents in the programme displayed, or the practical burden of the barrier on the students’ learning.
V. CONCLUSION
This study demonstrated that providing a structured teaching platform could enhance residents’ teaching competencies. This was an important factor as existing resident teachings commonly occur while performing clinical work and in the chaotic ward setting. The study also showed that logistic support could help overcome common barriers in RAT programmes, such as busy work commitments. We believe this combination is important to include in future RAT programmes.
Notes on Contributors
Dr Benny Kai Guo Loo is an Associate Consultant in General Paediatric Service at KK Women’s and Children’s hospital. He has a keen interest in medical education and is currently a Co-ordinator for Yong Loo Lin School of Medicine, NUS and Physician Faculty for Singhealth Paediatric Residency Programme.
A/Prof Koh Cheng Thoon is the Head and Senior Consultant of Infectious Diseases Service at KK Women’s and Children’s hospital. He is also the Academic Vice-Chair for Education in Singhealth Duke-NUS Paediatric Academic Clinical Programme and he was awarded the Wong Hock Boon Society-SMA Charity Fund Outstanding Mentor Award in 2016.
Dr Jessica Hui Yin Tan is a Senior Resident in General Paediatrics Service at KK Women’s and Children’s hospital. She is also a clinical lecturer at the Yong Loo Lin School of Medicine, NUS.
Dr Karen Donceras Nadua is an Associate Consultant in Infectious Diseases Service at KK Women’s and Children’s hospital. She is also a clinical teacher at the Lee Kong Chian School of Medicine.
Dr Cristelle Chu-Tian Chow is a Consultant in General Paediatrics Service at KK Women’s and Children’s hospital. She obtained her Master of Health Professions Education from Maastricht University and is currently the Associate Programme Director for Singhealth Paediatric Residency Programme.
Ethical Approval
The study was categorised as an education quality improvement hence formal Singhealth Centralised Institutional Board review is not required.
Acknowledgements
The authors would like to thank Paediatric Graduate Medical Education and Academic Clinical Programme secretariat, faculty and residents who have helped to make PRATA programme a success. We would also like to thank Prof Sandy Cook, Senior Associate Dean in Duke-NUS, for her guidance in the writing of this manuscript.
Funding
The authors report no funding source for this study.
Declaration of Interest
The authors declare no conflict of interest.
References
Accreditation Council for Graduate Medical Education (2017). Common program requirements. Retrieved from https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_2017-07-01.pdf.
Brasher, A. E., Chowdhry, S., Hauge, L. S., & Prinz, R. A. (2005). Medical students’ perceptions of resident teaching: Have duty hours regulations had an impact? Annals of Surgery, 242(4), 548.
Busari, J. O., Scherpbier, A. J. J. A., Van Der Vleuten, C. P. M., & Essed, G. E. (2000). Residents’ perception of their role in teaching undergraduate students in the clinical setting. Medical Teacher, 22(4), 348-353.
Copeland, H. L., & Hewson, M. G. (2000). Developing and testing an instrument to measure the effectiveness of clinical teaching in an academic medical center. Academic Medicine, 75(2), 161-166.
Gaba, N. D., Blatt, B., Macri, C. J., & Greenberg, L. (2007). Improving teaching skills in obstetrics and gynecology residents: Evaluation of a residents-as-teachers program. American Journal of Obstetrics and Gynecology, 196(1), 87-e1.
Hill, A. G., Srinivasa, S., Hawken, S. J., Barrow, M., Farrell, S. E., Hattie, J., & Yu, T. C. (2012). Impact of a resident-as-teacher workshop on teaching behavior of interns and learning outcomes of medical students. Journal of Graduate Medical Education, 4(1), 34-41.
Hill, A. G., Yu, T. C., Barrow, M., & Hattie, J. (2009). A systematic review of resident‐as‐teacher programmes. Medical Education, 43(12), 1129-1140.
Huynh, A., Savitski, J., Kirven, M., Godwin, J., & Gil, K. M. (2011). Effect of medical students’ experiences with residents as teachers on clerkship assessment. Journal of Graduate Medical Education, 3(3), 345-349.
Lockspeiser, T. M., O’Sullivan, P., Teherani, A., & Muller, J. (2008). Understanding the experience of being taught by peers: The value of social and cognitive congruence. Advances in Health Sciences Education, 13(3), 361-372.
McKean, A. J. S., & Palmer, B. A. (2015). Psychiatry resident-led tutorials increase medical student knowledge and improve national board of medical examiners shelf exam scores. Academic Psychiatry, 39(3), 309-311.
Meller, S. M., Chen, M., Chen, R., & Haeseler, F. D. (2013). Near-peer teaching in a required third-year clerkship. The Yale Journal of Biology and Medicine, 86(4), 583.
Musunuru, S., Lewis, B., Rikkers, L. F., & Chen, H. (2007). Effective surgical residents strongly influence medical students to pursue surgical careers. Journal of the American College of Surgeons, 204(1), 164-167.
Post, R. E., Quattlebaum, R. G., & Benich III, J. J. (2009). Residents-as-teachers curricula: A critical review. Academic Medicine, 84(3), 374-380.
Schmidt, H. G., & Moust, J. H. (1995). What Makes a Tutor Effective? A Structural Equations Modelling Approach to Learning in Problem-Based Curricula. Academic Medicine, 70(8), 708-714
Ten Cate, O., Snell, L., Mann, K., & Vermunt, J. (2004). Orienting teaching toward the learning process. Academic Medicine, 79(3), 219-228.
Wamsley, M. A., Julian, K. A., & Wipf, J. E. (2004). A literature review of “resident-as-teacher” curricula. Journal of General Internal Medicine, 19(5), 574-581.
Yedidia, M. J., Schwartz, M. D., Hirschkorn, C., & Lipkin, M. (1995). Learners as teachers. Journal of General Internal Medicine, 10(11), 615-623.
Zackoff, M., Jerardi, K., Unaka, N., Sucharew, H., & Klein, M. (2015). An observed structured teaching evaluation demonstrates the impact of a resident-as-teacher curriculum on teaching competency. Hospital Paediatrics, 5(6), 342-347.
*Benny K. G. Loo
Division of Paediatric Medicine
KK Women’s and Children’s Hospital
100 Bukit Timah Road, Singapore 229899
Tel: +65 62255554
Email: benny.loo.k.g@singhealth.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









