Start small and aim big in conducting a basic surgical skills workshop for medical students
Submitted: 30 July 2021
Accepted: 17 January 2022
Published online: 5 April, TAPS 2022, 7(2), 46-50
https://doi.org/10.29060/TAPS.2022-7-2/SC2662
Kheng Tian Lim1 & Bao Yun Koh2
1Department of General Surgery, Khoo Teck Puat Hospital, Singapore; 2Education Development Office, Khoo Teck Puat Hospital, Singapore
Abstract
Introduction: Medical students (MS) may lack the knowledge and experience in performing basic surgical skills (BSS) when they first commence their postgraduate surgical training. We conducted a pilot BSS workshop with specific learning outcomes for MS.
Methods: Our BSS workshop program consisted of reading the pre-workshop online modules, watching the instructional videos of skills demonstration, and completing the pre-workshop multiple-choice questions (MCQ). MS attended the onsite workshop a week later, which consisted of a basic surgical theory lecture, live demonstration of the skills by the teaching faculty and, supervised skills training coupled with feedback. Surgical skills taught were knot tying, suturing techniques, laparoscopic peg transfer, precision cutting, application of endoloop ties. A standardised surgical skills rubric was used to assess the competency and safety of BSS. A post-workshop MCQ was administered to assess the knowledge learned. The criteria for successful completion of BSS were a satisfactory grade in the surgical skills assessment and a pass score in the MCQ.
Results: All the participating MS achieved a satisfactory grade in the surgical skills assessment and passed the MCQ. Several pedagogical methods were used to enhance knowledge learning and practical skills competency including a flipped classroom in blended learning, technology-enhanced learning, kinesthetic learning, and providing effective feedback.
Conclusion: MS taught in BSS workshop can achieve competency in knowledge, skills, safe attitude and prepare them for future postgraduate surgical training. In the current COVID-19 pandemic, our challenge is to develop similar BSS in a safe environment using technology-enhanced tools such as online instructional videos and online feedback.
Keywords: Assessment, Basic Surgical Skills, Competency, Feedback, Medical Students, Outcome-based Education
I. INTRODUCTION
Medical students (MS) may lack the knowledge and experience in performing certain basic surgical skills (BSS) when they first commence their postgraduate surgical training in hospitals. Traditionally, BSS are usually not taught formally in the undergraduate medical curriculum until much later in the postgraduate level. The opportunity for teachers to teach BSS and for MS to learn is much dependent on the situation in operating rooms during assigned core surgical postings or student selective postings.
In Singapore, Yong Loo Lin School of Medicine, National University of Singapore (NUS) provides basic and advanced clinical procedural simulation training to undergraduate MS. Skills taught include gowning, scrubbing techniques, suturing, and knot-tying. Lee Kong Chian School of Medicine, Nanyang Technological University (NTU) teaches suturing and knot-tying skills in dry laboratory to undergraduate MS. All these stimulated practical skills and experience acquired by MS are transferrable to real patients’ environments. In addition, SingHealth Academy, an educational arm of SingHealth, provides BSS workshop training at the postgraduate level for interested learners. In the United Kingdom and Ireland, the BSS course is a curriculum-mandated course for postgraduate Core Surgical Training programmes.
Healthcare institution partners such as Khoo Teck Puat Hospital (KTPH), provide clinical training for MS of NUS and NTU. Our Department of General Surgery (GS) identifies the need in the learning outcomes for the graduating MS, to equip them with the competent foundation of BSS for postgraduate surgical training, although not a graduating competency requirement set by Singapore Medical Council. We conducted a small pilot workshop at our institution, aiming at educational quality improvement for our MS in three learning domains, namely surgical knowledge, practical surgical skills, and attitudes in safety that are common to all forms of surgery.
II. METHODS
A. Workshop organization, MS and Teaching Faculty, Teaching Materials
The Department of GS and Education Development Office (EDO), KTPH organised a 1-day BSS workshop for MS with the request from MS and was scheduled on 20th December 2019. Planning over three months was required to prepare the learning objectives and outcomes, workshop programme schedule, venue, teaching materials, surgical scrubs, sustenance, and coordination by the workshop director and EDO. Both the local and overseas MS were invited and recruited for training. Experienced local teaching faculty members were invited and briefed on the teaching methodology, feedback provision, and assessment criteria.
MS who agreed to participate were given instructions to read the pre-workshop fundamentals of the BSS document, watch the instructional video clips of the BSS demonstration and, complete pre-workshop multiple-choice questions (MCQ), all of which were provided online 1 week before the workshop. These pre-workshop activities may help to motivate the MS and provide an opportunity for self-assessment of their understanding of the BSS topics. MS were allowed to post questions to the workshop director for guidance. The course content and MCQ were prepared by the course director to be appropriate to the MS level.
The workshop was divided into morning and afternoon sessions to cater to a larger group of interested MS coming from overseas. The onsite workshop consisted of a short basic theory lecture, a live demonstration of the practical BSS, MS performing the practical BSS with direct supervision and corrective feedback. BSS taught were knot tying using one-hand, two-hand, and instrumental techniques. Suturing techniques taught included simple, mattress, interrupted, continuous suture. More advanced laparoscopic skills such as laparoscopic peg transfer, precision cutting, and application of endoloop ties were taught. A post-workshop MCQ was administered.
B. Assessment in Knowledge, Skills, and Attitudes
The surgical knowledge was assessed using the pre-and post-workshop MCQ, based on the course content prepared for MS.
The surgical skills assessment was carried out by direct observation of procedural skills (DOPS) using a standardised surgical skills rubric. Open surgery skills assessment included instrument selection and handling, knotting techniques, tissue handling, and suturing techniques. Laparoscopic surgery skills assessment included instrument selection and handling, peg transfer, precision cutting, and ligating loop. The overall summative assessment of global grading in the surgical skills domain by the teaching faculty was either satisfactory or unsatisfactory.
MS were assigned to work in pairs with the ratio of MS: teaching faculty as 2:1. Assessment in the attitude and behavior domain was based on direct observation in the safe handling of sharps and needles, general assisting, and laparoscopic camera assisting skills.
C. Feedback and Competency
The teaching faculty used DOPS to provide feedback on the practical BSS performed by the MS which allowed the MS to improve and progress from a novice to a competent learner level in the skills and attitude domains. The specific, timely, and purposeful feedback served as a channel for MS to improve and reflect on their learning outcomes in these domains.
The competency criteria for successful completion of the BSS workshop were set as a pass mark of 60% in the summative MCQ test and a satisfactory grade in the summative skills assessment by the teaching faculty. A Certificate of Attendance would be awarded to MS who have acquired the competency criteria.
III. RESULTS
Assessment and evaluation data gathered for this workshop and pre-workshop MCQ questions were uploaded to an online repository for archiving and validation purposes. It may be assessed through the following Digital Object Identifier (DOI): https://doi.org/10.6084/m9.figshare.16884877.v2 (Lim & Koh, 2021).
A total of 38 MS signed up for the BSS workshop with 1 dropout. Thirty-seven MS attended the workshop of which 25 were from overseas medical schools. Thirty-six MS attempted the pre-workshop MCQ (10 questions). Thirty-seven MS passed the post-workshop MCQ (15 questions). All MS achieved satisfactory grades in practical skills. There was no needle stick injury reported.
The BSS workshop program evaluation form was administered and completed anonymously for the quality improvement process after verbal consent was taken from the participants. (Table 1).
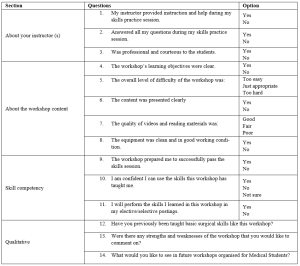
Table 1. BSS Workshop for MS Program Evaluation
IV. DISCUSSION
Bloom’s Taxonomy comprises three learning domains known as cognitive (knowledge), affective (attitude), and psychomotor (skills). Each domain has a hierarchy that corresponds to distinct levels of learning which is important for students to develop holistically. The learning objectives of the BSS workshop for MS are thus designed to fulfil these three domains, specifically to: 1) acquire the fundamental knowledge of BSS (knowledge), 2) demonstrate a variety of surgical knots and suturing skills effectively (skills) and, 3) handle and use of surgical instruments and tissue safely (attitude).
Harden et al. (1999) described an outcome-based education framework that comprises six levels of training to achieve the outcomes. These six levels of training are: 1) awareness of the procedure, 2) full theoretical understanding of the procedure, 3) observation of the procedure, 4) carrying out part of the procedure, 5) undertaking the procedure under the supervision and, 6) undertaking the procedure unsupervised. Similarly, the programme activities of the BSS workshop for MS were developed to cover these six levels of training. The learning outcomes of this workshop are to equip the MS with the competency of BSS for postgraduate surgical training. The teaching faculty members share their knowledge, demonstrate their expertise, advise MS, and provide feedback to improve technical skills and promote learning.
Effective feedback is necessary to enhance learning. Pendleton et al. (2003) described a four-step process for carrying out a feedback session. Ramani and Krackov (2012) described twelve tips for clinical teachers to provide effective feedback to undergraduate and graduate medical trainees. Our teaching faculty members were able to provide effective feedback to MS using these frameworks to establish a respectful learning environment, feedback on direct observation, make feedback timely, reinforce and correct observed behaviors, use specific language to focus on performance, confirm the learner’s understanding and conclude with an action plan.
The assessment for learning in the BSS workshop for MS was designed to align with the three learning domains using: 1) pre-and post-workshop MCQ to test surgical knowledge, 2) DOPS by the teaching faculty to test surgical skills and, 3) DOPS in the safe handling of sharps and needles, general assisting and laparoscopic camera assisting skills to test the attitude and behavior. A standardised surgical skills rubric was used for DOPS.
Technology-enhanced learning (TEL) intervention and enhancement can be characterised by 1) replicating existing teaching practices, 2) supplementing existing teaching or, 3) transforming teaching, learning processes, and outcomes (Kirkwood & Price, 2014). Several pedagogical methods were used in this BSS workshop to enhance knowledge learning and skills acquisition such as flipped classroom in blended learning, a mixture of the three characteristics of TEL, kinesthetic learning, and providing effective feedback. In the current COVID-19 pandemic, there are challenges to conducting such a practical workshop. TEL tools that combine online educational materials, instructional videos, feedback, and face-to-face online interaction such as Zoom, and Microsoft Teams are the new norm.
The limitation of this workshop includes the lack of MCQ standardisation process and the quality of the video clips which we intend to improve in the next workshop.
V. CONCLUSION
Conducting a BSS workshop for MS with specific learning outcomes is feasible where the MS can achieve competency in knowledge, skills, safe attitude and prepare them for postgraduate surgical training. In the current COVID-19 pandemic, our challenge is to develop similar BSS in a safe environment using TEL tools.
Notes on Contributors
Dr. Lim Kheng Tian designed the work, reviewed the literature, drafted the work, revised the content critically, and wrote the manuscript. Ms. Koh Bao Yun contributed to the design and administration of the work, gave critical feedback to the content, and revised the manuscript. All authors have read and approved the final manuscript.
Ethical Approval
This 1-day workshop program was conducted for educational quality improvement (QI) with approval from the Department of GS and EDO, KTPH. This article was submitted with Institutional Review Board/Ethical approval for exemption from full review. We have attached the local IRB waiver document NHG DSRB Ref: 2021/00888.
Data Availability
Inline to make research available to the scientific community for data replication and scientific progress, the dataset of this workshop may be found for free through the Figshare website: https://doi.org/10.6084/m9. figshare.16884877.v2
Acknowledgement
The authors want to thank all the MS and teaching faculty who participated in the workshop. We would like to acknowledge Dr. Lee Yao Zong, Associate Consultant of the Department of GS, KTPH for providing help in the laparoscopic educational content. We would like to acknowledge the technical help of Mr. Mohamad Sean Abdullah, former Experimental Surgical Services Development Executive of the Department of GS, KTPH. We would like to acknowledge equipment support from KARL STORZ Endoscopy Singapore Sales Pte Ltd for providing the reusable laparoscopic trainer and laparoscopic instruments. We also like to acknowledge NHG Education for linking up EDO, KTPH with the Singapore Medical Society of Australia and New Zealand (SMSANZ).
Funding
There is no funding for this paper. The suturing materials used in the workshop were funded by the Pre-Employment Clinical Training (PECT) Funds received by KTPH for local MS whilst overseas MS were self-funded. The funder was not involved in the design, delivery of the workshop, or submission of the paper.
Declaration of Interest
All authors declare no conflicts of interest, including financial, consultant, institutional, and other relationships that might lead to bias or a conflict of interest.
References
Harden, R. M., Crosby, J. R., Davis, M. H., & Friedman, M. (1999). AMEE Guide No. 14: Outcome-based education: Part 5-From competency to meta-competency: A model for the specification of learning outcomes. Medical Teacher, 21(6), 546–552. https://doi.org/10.1080/01421599978951
Kirkwood, A., & Price, L. (2014). Technology-enhanced learning and teaching in higher education: What is ‘enhanced’ and how do we know? A critical literature review. Learning, Media and Technology, 39(1), 6–36. https://doi.org/10.1080/17439884.2013.770404
Lim, K. T., & Koh, B. Y. (2021). Start small and aim big in conducting a basic surgical skills workshop for medical students—Repository data (p. 11710 Bytes) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.16884877.v2
Pendleton, D., Schofield, T., Tate, P., & Havelock, P. (2003). The New Consultation. Oxford University Press.
Ramani, S., & Krackov, S. K. (2012). Twelve tips for giving feedback effectively in the clinical environment. Medical Teacher, 34(10), 787–791. https://doi.org/10.3109/0142159X.2012.684916
*Lim Kheng Tian
Department of General Surgery,
Khoo Teck Puat Hospital,
90 Yishun Central,
Singapore 768828.
Tel: +65 65558000
Email: lim.kheng.tian@ktph.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









