Safety walk-round education to develop risk prediction skills of novice health professional students
Submitted: 1 October 2020
Accepted: 3 December 2020
Published online: 4 May, TAPS 2021, 6(2), 78-87
https://doi.org/10.29060/TAPS.2021-6-2/OA2406
Yoshitaka Maeda1, Yoshikazu Asada2, Yoshihiko Suzuki1, Akihiro Watanabe3, Satoshi Suzuki3 & Hiroshi Kawahira1
1Medical Simulation Center, Jichi Medical University, Japan; 2Center for Information, Jichi Medical University, Japan; 3Faculty of Health and Medical Sciences, Kanagawa Institute of Technology, Japan
Abstract
Introduction: Students in the early years of medical school should learn clinical site risk assessment skills. However, the effect of this training on clinically inexperienced students is not clear, and it is difficult for students to predict risks from a wide range of perspectives. This study aims to develop and implement three patterns of safety walk rounds (SWR) in a class of students with no clinical experience.
Methods: Three types of SWR were conducted: (A) 37 students observed a familiar classroom and predicted safety risks; (B) 39 students created a profile of a fictitious student in advance and then used Type A parameters; (C) 100 students participated. First, Type A was conducted as a practice. Next, students observed a hospital and predicted risks. All participants in Types A to C had no clinical experience. We classified all risks into perception, comprehension, and action.
Results: For each safety walk-round, there were two types of risk prediction. In Type A, risks such as perception and comprehension were more than 80%. In Types B and C, action risks were 60%. Students had little experience in observing facilities and none at finding safety risks.
Conclusion: Each method had a different risk prediction tendency. Combining the methods could enable students to acquire comprehensive skills in assessing hidden environmental patient safety risks.
Keywords: Patient Safety Education, Undergraduate Education, Risk Assessment Skill, Safety Walk-Rounds
Practice Highlights
- Proposes a patient safety education method incorporating safety walk rounds (SWR).
- Clarifies the risk prediction tendency of clinically inexperienced students in each SWR pattern.
- Students conducting SWR in familiar classrooms tend to predict certain risks.
- Creating fictitious user profiles before SWR enables prediction of action risks.
- Combining different SWR types could enable comprehensive risk assessment skills.
I. INTRODUCTION
In Japan, first-year medical students are recent high school graduates. 60% of universities that train medical professionals provide patient safety education to fourth year medical students at the start of clinical training (Ishikawa et al., 2008). Further, lower grade educational methods do not include specific guidelines for patient safety education, and students in lower grades do not have sufficient medical knowledge to immediately apply their patient safety knowledge in clinical practice. This problem has been pointed out not only in Japan but also in the US and Canada (Alper et al., 2009). Conversely, the Telluride Interdisciplinary Roundtable (Mayer et al., 2009) and Lucian Leape Institute (2010) showed that patient safety education should be included in the curriculum of all grades. This would enable students to learn the necessity and importance of patient safety knowledge and consider patient safety as an implementation science while continuously practising patient safety skills (Nakajima, 2012).
However, many medical schools teach basic patient safety knowledge through lectures on accident analysis tools, legal responsibility knowledge, ethics, and infection (Mayer et al., 2009); however, students lack education on non-technical skills (Mayer et al., 2009; Nakajima, 2012; Walton et al., 2010). Students should be trained in awareness of safety weaknesses, threats (risks) in the workplace or operations, and how to avoid these risks (Doi et al., 2012). Topic 6 of the World Health Organization’s (WHO’s) Patient Safety Curriculum Guide indicates that students need to take appropriate corrective action when they see an unsafe situation or environment (Walton et al., 2010). However, the WHO guidelines do not explain how these risk assessment skills can be taught to students. Literature that examines the effectiveness of risk assessment skills training for early-year medical students is deficient.
To address these issues, we focused on Safety walk rounds (SWR), in which a safety manager goes to a workplace, listens to staff opinions on safety, and observes the workplace to identify safety issues before an accident (Hafey, 2017; Womack, 2013). Singer and Tucker (2014) pointed out that SWR enhances safety culture. The effects of SWR in the radiology department have reduced the number of unsafe events by half (Donnelly et al., 2008). Additionally, other studies reported that safety managers grow more sensitive to safety issues using SWR and that motivation regarding safety is increased (Frankel et al., 2003; Singer & Tucker, 2014). However, its educational effect and applicability to educating clinically inexperienced students are not clear since SWR has not been used for education.
This study aims to develop and implement three patterns of SWR in a class of students with no clinical experience. We clarify the risk prediction tendency of students in each SWR pattern and discuss the effects.
II. METHODS
A. Development Process of Three Types of SWR
We developed three patterns of SWRs to help clinically inexperienced students predict risk and considered what motivates students to learn. We used the ARCS model proposed by J. M. Keller in 1983, which is a framework using four elements: Attention (stimulating the learner’s interest, intellectual curiosity, and inquisitiveness); Relevance (making the content familiar and meaningful); Confidence (encouraging learners to learn); and Satisfaction (giving the learner a sense of satisfaction and motivation to learn more) (Keller, 1987). ARCS is an acronym for these elements.
· SWR in daily situations (SWR-D): Experts are better at predicting risks than novices as the latter has limited knowledge of important aspects of each situation (Murata et al., 2009). Hence, clinically inexperienced students might find it difficult to predict risks in clinical situations. Using the ARCS model, students need to be given Attention, Confidence and Satisfaction. Therefore, we developed SWR in daily situations (SWR-D). Students observe daily situations in classrooms and school buildings for instances of safety risk and take pictures. We use daily situations as classrooms and school buildings are familiar environments for students, and there are many safety risks for educating students.
· SWR in daily situations using the Persona method (SWR-DP): It may be difficult for students who have never performed SWR to observe safety risks in daily situations, and students’ Confidence should be high. Therefore, we combined the persona method with SWR to create a virtual profile of a virtual user, including name, gender, age, and information about the system (e.g., technological literacy). The Persona method has been used to examine the safety of driving support systems (Lindgren et al., 2007). We hypothesize that the Persona method would help students to predict risk from the perspective of a specific user. The student considers the problems the virtual user will face and their behaviour (Cooper, 2004; Mulder & Yaar, 2006). Students created fictitious student profiles (personas) and conducted SWR assuming that the persona students would spend one day in school buildings and classrooms.
· SWR in clinical situations (SWR-C): It may be difficult for students to associate SWR with patient safety in clinical practice, as SWR in daily situations were not related to clinical practice conducted. Further, students might not be motivated to learn—using the ARCS model, students need to see Relevance and Satisfaction. Therefore, we developed the SWR in clinical situations (SWR-C). First, to practice SWR, students performed SWR-D. After SWR-D, they observed clinical situations in hospitals to predict risks (SWR-C).
B. Description of Participants and SWR Implementation Process
This study involved first-year medical students and third-year students in the medical engineer training courses who had no clinical experience. After participating in each SWR pattern, students were asked for their opinions.
1) SWR-D: The participants included 37 students in the third-year medical engineer training course and 100 students who had been in medical school for one month. SWR-D was administered to the third-year (2018) medical engineer training students in one session. SWR-D was implemented as one of the required general education courses for first-year medical students in 2019. An exercise using SWR-D was given to all participants who worked in groups of four to five. Students photographed incidences of safety risk (30 minutes) and collaborated to identify the risks in each photo (20 minutes).
2) SWR-DP: The participants included 39 students (different from SWR-D) in the third-year medical engineer training course. SWR-DP was administered to the third-year (2019) medical engineering students in one session and conducted in groups of four to five. Each group considered one persona (virtual student profile) for the first 20 minutes, and SWR-D was conducted as before.
3) SWR-C: The participants included 100 students (same as SWR-D) who had been in medical school for one month. Each student was assigned one clinical department in advance. Two weeks after the SWR-D, early exposure training was conducted. During training, students found safety risks in clinical situations and outlined the identified risks in reports as photography was not allowed for confidentiality.
C. Statistical Analysis
The risks predicted by students in each SWR pattern were counted and classified into the following: perception—difficulty perceiving something that exists in the outside world (e.g., signs that are difficult to read); comprehension—difficulty understanding the meaning of something that exists in the outside world and in planning what action to take (e.g., signs that are difficult to understand); and action—difficulty performing the intended action (e.g., places where it is difficult to walk).
These classifications are based on Norman’s seven stages of action (Norman & Draper, 1986) where human actions are classified into seven stages: forming the goal, forming the intention, specifying an action, executing the action, perceiving the state of the world, interpreting the perception, and evaluating the outcome (Norman, 1988). This is a representative model widely used for the design evaluation of man-machine systems such as computers (Fleming & Koman, 1998) to understand human cognitive behaviour that leads to human error in medical treatment (Zhang et al., 2002; Zhang et al., 2004).
D. Ethical Considerations in This Research
The ethical requirements in this study are in accord with the Declaration of Helsinki. We emphasized and explained to students that participation was voluntary and that declining to cooperate would have no influence on their grades. We also explained that consent to participate could be withdrawn at any time, that the results of this study may be published after processing, and that the students’ personal information would not be revealed. The students entered their consent in the e-learning system Moodle. This study was considered exempt by the Jichi Medical University Review Board (Number 18-014).
III. RESULTS
The total number of perception, comprehension, and action risks in each SWR is shown in Figure 1. Table 1 shows typical predicted risks and some of the images taken by students. The data that support the findings of this study are openly available in Figshare at <http://doi.org/10.6084/m9.figshare.13012664 (Maeda et al., 2021)>.
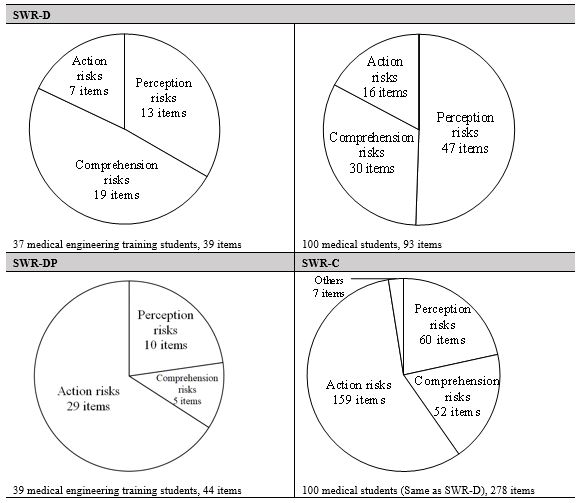
Figure 1. Classification results of risks predicted by students in each SWR pattern
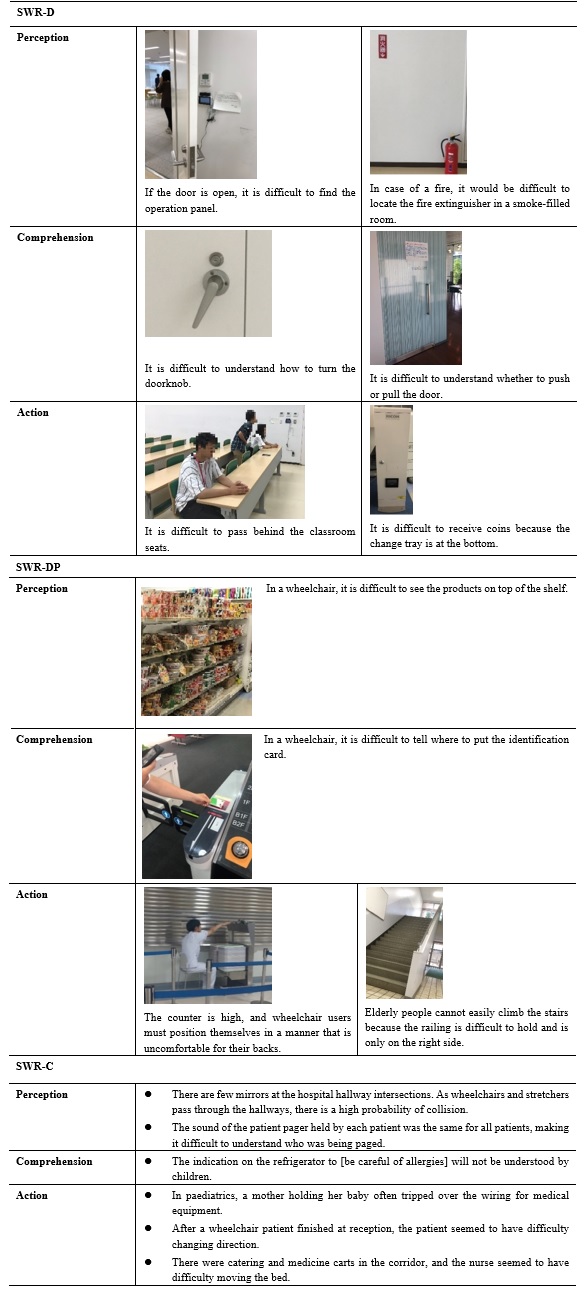
Table 1. Typical risks and captured images for each SWR pattern
In SWR-D, the number of action risks was lower than that of perception and comprehension risks. Risks related to guidance signs for school buildings and classrooms, signs, maps, doors, and operation panels for electric lights were predicted. Also, for example, a group of students who pointed out that it was difficult to find a fire extinguisher did not simply point out the problem of perception, but pointed out that “in the case of a fire, it would have been difficult to find the fire extinguisher in a room filled with smoke”. In other words, they imagined a fire situation that differed from the current conditions of the site they observed.
In SWR-DP, students created the persona shown in Table 2. Many students created fictitious profiles of students who had disabilities or who were elderly. Despite observing the same school building as SWR-D, the number of action risks is almost 70% of the total number (Figure 1). Table 1 shows that many students made extensive predictions from the same perspective as the persona—the risks associated with persons with some kind of disability. For example, from the height of the eyes of a person in a wheelchair, students predicted problems with the visibility of products in a shop, the height of a counter in a cafeteria, and with the routes, the persona would be likely to take within a building. Most identified problems pertained to a lack of easy access to the environment. In one image (Table 1), a student is seen simulating being in a wheelchair at the cafeteria counter.
|
Male, 70 years old, 160 cm, 55 kg, using a cane, hearing loss, narrow vision. He entered college to re-learn after retirement. He goes to school by bus. He is worried about being able to see the whiteboard. He is worried that he will be late for class because he moves more slowly. |
|
Male, 18 years old, 141 cm, 85 kg. He uses a wheelchair because he lost his left leg in a traffic accident. He is apprehensive about moving between classrooms. |
Table 2. Example of a persona (fictitious student profile) created by SWR-DP students
In SWR-C, action risks were the most frequent (Figure 1). Of the total 251 risks, approximately 90% were risks to patients and approximately 10% to healthcare professionals. From Table 1, regarding action, we can see that students observed the behaviour and embarrassment of patients at hospitals and predicted risks based on them (e.g., “The mother holding her baby was almost stumbling”; “Patients in wheelchairs were difficult to move”). In perception and comprehension, students brainstormed risks from the patients’ perspective (e.g., “The indication on the refrigerator to [be careful of allergies] will not be understood by children”). The students identified risks from the child’s perspective.
Table 3 shows the students’ opinions of each SWR. In all SWRs, students had little experience in observing the facilities they usually used, and finding safety risks was new to them. In SWR-DP, students said that although they were able-bodied, they could notice accessibility problems by observing the environments from the persona’s perspectives. For SWR-C, students noticed that there were many problems in the design and environment of the hospital facilities and that various safety measures had already been implemented.
|
SWR-D
SWR-DP
SWR-C
|
Table 3. Student opinion on SWR
IV. DISCUSSION
A. Student Risk Predicting Tendency in Each SWR Pattern
The importance of institutional design in patient safety has been pointed out in many publications. For example, environmental design is being considered to avoid various risks, such as falls and patient suicides, mixing up patients, and improper handling of tubes and connectors (Joseph & Rashid, 2007; Michalska & Szewieczek, 2007; Reiling, 2006; Reiling et al., 2003; Reiling et al., 2008). In particular, it has been pointed out that the indoor environment (e.g., noise and lighting) and interior design (e.g., furniture and materials) are important (Joseph & Rashid, 2007). When considering the design, it is necessary to predict both the direct impact risks and the indirect impact risks of accidents as points of view when predicting onsite risks. Direct impact risks are the aspects of hospital design that can directly impact safety outcomes, such as patient falls and medical errors (Joseph & Rashid, 2007). This is considered to correspond to “action” in this study. For example, a tall counter design is directly linked to the undesirable consequence of a wheelchair user being unable to receive a meal. Indirect impact risks are the aspects of hospital design that can cause users to make incorrect decisions that lead to accidents and errors (Joseph & Rashid, 2007). This is considered to correspond to “perception” and “comprehension” in this study. For example, a paediatric refrigerator’s “be careful of allergies” poster does not directly lead to an unsafe outcome; however, if a child is unable to understand, then an incorrect decision to eat food to which the child is allergic may lead to an unsafe outcome.
In SWR-D, many indirect impact risks (perception and comprehension) were predicted. Conversely, few action risks (direct impact risks) were predicted. SWR-DP and SWR-C results were the opposite to SWR-D; many direct impact risks and few indirect impact risks were identified.
In SWR, it is necessary to identify risks through brainstorming and simulation using the operators’ experience and reasoning (Okubo et al., 2014). However, different techniques identify different risk types. Indirect impact risks such as perception and comprehension are related to human internal thinking, such as incorrect decisions. To identify these risks, students need to observe from the perspective of the person concerned and brainstorm the risks. Conversely, the action is observable—a risk that students can predict by observing the actions of the concerned person or simulating behaviour as the concerned person. Subsequently, what caused each SWR to favour predicting one type of risk over another?
In SWR-D, most students observed a familiar daily situation from their (able-bodied) perspective. In SWR-DP, students observed a familiar daily situation from a persona’s point of view that differed from that of an able-bodied person. In SWR-C, they observed unfamiliar clinical situations from the patients’ perspective (it is unknown whether this perspective was different from their own). This suggests that when students observe a familiar environment from their own perspective, they concentrate on brainstorming about risks but do not conduct much action simulation (acting on a simulated basis and identifying risks). Consequently, the risks related to action were few.
Conversely, if students observe risk from others’ perspective, they may not be able to brainstorm well, and they may tend to predict risks by performing action simulations. In SWR-DP, many images of simulations, such as trying to use a cafeteria as a persona (for example, a wheelchair user), were recorded. Notably, novice nurses tend to observe bedsides without being able to imagine the patient’s condition or behaviour (Daikoku & Saito, 2017); it seems difficult to predict risks associated with unfamiliar subjects (people/environment) only by brainstorming.
However, during SWR-C, we asked students to predict risks only by observation to avoid interference with patient care, and students were unable to perform action simulations. Nevertheless, the risks associated with actions were the most predicted. According to the risks predicted by the students (Table 1), students likely found patients who were confused and observed their behaviour. In the clinical situation, there were several observable patients that students could predict many risks based on observable actions.
In summary, for clinically inexperienced students to predict many indirect impact risks (perception, comprehension), it is better for them to make observations from their own perspectives in a daily situation where brainstorming can be easily conducted. It is better to ask students to observe an unfamiliar person and environment to identify more direct impact risks (actions). It would be better to create a fictitious user profile (persona) and conduct SWR (SWR-DP) or conduct SWR in a clinical situation unfamiliar to students (SWR-C). In any case, if each SWR is implemented independently, the predicted risks are biased. Therefore, by combining each SWR, it may be possible to develop skills that enable students to find direct impact and indirect impact risks in a well-balanced manner.
B. Limitations
This study evaluates the educational benefits of three SWR patterns and discusses their effectiveness. We could not compare the three patterns of SWR for the following aspects. First, we could not examine the relationship between participants’ background and SWR. This study targeted first-year medical students (SWR-C) and third-year students in the medical engineer training course (SWR-D, SWR-DP). Each student’s age and expertise were different. Therefore, the background of each participant could have affected the participant’s risk prediction tendency. However, all students shared the common background of having no clinical experience and had basic education on patient safety and conducted SWR with a basic knowledge of human factors, such as medical accident analysis methods. Second, we could not conduct a comparative study of each SWR by statistical analysis as there were differences in the way each SWR was conducted. SWR-D and SWR-DP were administered as a group, while SWR-C was administered individually because of restrictions in clinical practice. We could not calculate the average number of hazard predictions per student.
Further, each SWR was conducted in a compulsory class; therefore, there were a large number of students per faculty member. Consequently, we could not observe all students. Therefore, we have little record of how students predicted risks, especially in SWR-C. This is because the simulation actions in clinical situations and photography were restricted.
Additionally, when examining the safety of facility design, it is important to predict risks to healthcare professionals as well as patients (Reiling et al., 2003). However, in SWR-C, 90% of the risks were related to patients. Future studies should examine training methods that enable clinically inexperienced students to predict risks to healthcare professionals.
V. CONCLUSION
In this study, we proposed a patient safety education method incorporating SWR. We conducted SWR-D, SWR-DP, and SWR-C sessions and clarified the risk assessment tendency of students in each SWR pattern. For students to predict many indirect impact risks (perception comprehension), it is better to have students observe a daily situation in which it is easy to identify risks from their own points of view (SWR-D). To find many direct impact risks (action), it is better for students to create a persona and observe a daily situation (SWR-DP) or clinical situation (SWR-C). This suggests that a combination of these SWRs would provide students with the skills to comprehensively predict the patient safety risks in facilities and the environment. By continuously conducting all SWR session types starting at lower grade levels, it is expected that skills related to risk assessment will be effectively acquired. It is expected that SWR education from pre-graduates will increase the number of medical professionals who can conduct an appropriate risk assessment in the field, resulting in improved quality and safety of healthcare.
Notes on Contributors
Yoshitaka Maeda, PhD, a Research Associate at the Medical Simulation Center at Jichi Medical University, Japan, contributed to the conceptualization, methodology, validation, formal analysis, investigation, resources, data curation, writing (original draft, review, and editing), and visualization.
Yoshikazu Asada, PhD, an Assistant Professor at the Center for Information at Jichi Medical University, Japan, contributed to the methodology, validation, formal analysis, and visualization.
Yoshihiko Suzuki, MD, an Assistant Professor at the Medical Simulation Center at Jichi Medical University, Japan, contributed to the conceptualization and methodology.
Akihiro Watanabe, MS, a Research Associate at the Faculty of Health and Medical Sciences at Kanagawa Institute of Technology, Japan, contributed to the validation and investigation.
Satoshi Suzuki, PhD, a Professor at the Faculty of Health and Medical Sciences at Kanagawa Institute of Technology, Japan, contributed to the data curation, writing (review and editing), and visualization.
Hiroshi Kawahira, MD, PhD, FACS, a Professor at the Medical Simulation Center at Jichi Medical University, Japan, contributed to the writing (review and editing), supervision, and project administration.
All the authors have read and approved the final manuscript.
Ethical Approval
This study was approved by the Jichi Medical University Institutional Review Board (protocol number 18-014).
Data Availability
The data that support the findings of this study are openly available in Figshare repository, http://doi.org/10.6084/m9.figshare.13012664
Funding
There is no funder for this study.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
Alper, E., Rosenberg, E. I., O’Brien, K. E., Fischer, M., & Durning, S. J. (2009). Patient safety education at US and Canadian medical schools: Results from the 2006 clerkship directors in internal medicine survey. Academic Medicine, 84(12), 1672-1676. https://doi.org/10.1097/acm.0b013e3181bf98a4
Cooper, A. (2004). The inmates are running the asylum: Why high-tech products drive us crazy and how to restore the sanity (Vol. 2). Sams Publishing.
Daikoku, R., & Saito, Y. (2017). Characteristics of gaze in expert nurses during observation at the bedside. Japanese Journal of Nursing Art and Science, 15(3), 218-226. https://doi.org/10.18892/jsnas.15.3_218
Doi, T., Kawamoto, K., & Yamaguchi, K. (2012). Difference by level of awareness and the years of experience to patient treatment safety. Japanese Journal of Radiological Technology, 68(5), 608-616. https://doi.org/10.6009/jjrt.2012_JSRT_68.5.608
Donnelly, L. F., Dickerson, J. M., Lehkamp, T. W., Gessner, K. E., Moskovitz, J., & Hutchinson, S. (2008). IRQN award paper: Operational rounds: A practical administrative process to improve safety and clinical services in radiology. Journal of the American College of Radiology, 5(11), 1142-1149. https://doi.org/10.1016/j.jacr.2008.05.017
Fleming, J., & Koman, R. (1998). Web navigation: Designing the user experience. O’Reilly Media.
Frankel, A., Gandhi, T. K., & Bates, D. W. (2003). Improving patient safety across a large integrated health care delivery system. International Journal for Quality in Health Care, 15(suppl_1), i31-i40. https://doi.org/10.1093/intqhc/mzg075
Hafey, R. B. (2017). Lean safety gemba walks: A methodology for workforce engagement and culture change. Productivity Press.
Ishikawa, M., Hirao, T., & Maezawa, M. (2008). Study of patient safety education for undergraduates. Medical Education, 39(2), 115-119. https://doi.org/10.11307/mededjapan1970.39.115
Joseph, A., & Rashid, M. (2007). The architecture of safety: Hospital design. Current Opinion in Critical Care, 13(6), 714-719. https://doi.org/10.1097/mcc.0b013e3282f1be6e
Keller, J. M. (1987). Development and use of the ARCS model of instructional design. Journal of Instructional Development, 10(3), 2-10. https://doi.org/10.1007/BF02905780
Lindgren, A., Chen, F., Amdahl, P., & Chaikiat, P. (2007). Using personas and scenarios as an interface design tool for advanced driver assistance systems. In: Stephanidis C. (eds) Universal Access in Human-Computer Interaction. Ambient Interaction. UAHCI 2007. Lecture Notes in Computer Science, vol 4555. Springer. https://doi.org/10.1007/978-3-540-73281-5_49
Lucian Leape Institute. (Eds.). (2010). Unmet needs: Teaching physicians to provide safe patient care. National Patient Safety Foundation.
Maeda, Y., Asada, Y., Suzuki, Y., Watanabe, A., Suzuki, S., & Kawahira, H. (2021). Proposal for safety walk-round education to develop risk prediction skills of novice health professional students [Data set]. Figshare. http://doi.org/10.6084/m9.figshare.13012664
Mayer, D., Klamen, D. L., Gunderson, A., & Barach, P. (2009). Designing a patient safety undergraduate medical curriculum: The Telluride interdisciplinary roundtable experience. Teaching and Learning in Medicine, 21(1), 52-58. https://doi.org/10.1080/10401330802574090
Michalska, J., & Szewieczek, D. (2007). The 5S methodology as a tool for improving the organization. Journal of Achievements in Materials and Manufacturing Engineering, 24(2), 211-214.
Mulder, S., & Yaar, Z. (2006). The user is always right: A practical guide to creating and using personas for the web. New Riders.
Murata, A., Hayami, T., & Moriwaka, M. (2009). Visual information processing characteristics of drivers in prediction of dangerous situation-Comparison among novice, expert and non-licensed person. In IEEE SMC Hiroshima Chapter (Eds.), Proceedings of Fifth International Workshop on Computational Intelligence & Applications, (pp. 254-257). IEEE SMC Hiroshima Chapter.
Nakajima, K. (2012). Patient safety and quality of medical care. Topics: III. Management of patient safety and quality of medical care: Theory and practice; 4. Patient safety and quality improvement education for undergraduate medical students. Nihon Naika Gakkai zasshi. The Journal of the Japanese Society of Internal Medicine, 101(12), 3477. https://doi.org/10.2169/naika.101.3477
Norman, D. A. (1988). The psychology of everyday things. Basic Books.
Norman, D. A., & Draper, S. W. (1986). User centered system design: New perspectives on human-computer interaction. L. Erlbaum Associates.
Okubo, Y., Kuroda, R., & Yamamoto, K. (2014). Health and safety patrol in universities. Journal of Environment and Safety, 5(3), 169-175. https://doi.org/10.11162/daikankyo.14C0702
Reiling, J. (2006). Safe design of healthcare facilities. BMJ Quality & Safety, 15(suppl 1), i34-i40. https://dx.doi.org/10.1136%2Fqshc.2006.019422
Reiling, J., Breckbill, C., Murphy, M., McCullough, S., & Chernos, S. (2003). Facility designing around patient safety and its effect on nursing. Nursing Economics, 21(3), 143.
Reiling, J., Hughes, R. G., & Murphy, M. R. (2008). The impact of facility design on patient safety. In Hughes, R. G (Ed.), Patient safety and quality: An evidence-based handbook for nurses. Agency for Healthcare Research and Quality.
Singer, S. J., & Tucker, A. L. (2014). The evolving literature on Safety walkrounds: Emerging themes and practical messages. BMJ Quality & Safety, 23(10), 789–800. http://dx.doi.org/10.1136/bmjqs-2014-003416
Walton, M., Woodward, H., Van Staalduinen, S., Lemer, C., Greaves, F., Noble, D., Ellis, B., Donaldson, L., & Barraclough, B. (2010). The WHO patient safety curriculum guide for medical schools. BMJ Quality & Safety, 19(6), 542-546. http://dx.doi.org/10.1136/qshc.2009.036970
Womack, J. (2013). Gemba walks: Expanded 2nd edition. Lean Enterprise Institute.
Zhang, J., Patel, V. L., & Johnson, T. R. (2002). Medical error: Is the solution medical or cognitive? Journal of American Medical Informatics Association, 9(6 Suppl 1), s75-77. https://dx.doi.org/10.1197%2Fjamia.M1232
Zhang, J., Patel, V. L., Johnson, T. R., & Shortliffe, E. H. (2004). A cognitive taxonomy of medical errors. Journal of Biomedical Informatics, 37(3), 193-204. https://doi.org/10.1016/j.jbi.2004.04.004
*Yoshitaka Maeda, PhD
3311-1, Yakushiji, Shimotsuke-shi,
(Kinen-tou 7th floor),
Tochigi,Japan, 329-0498
Tel: +81-285-58-7455
Email: y-maeda@jichi.ac.jp
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









