Promoting medical students’ reflection through feedback interaction: The RAISE model
Submitted: 2 April 2024
Accepted: 12 September 2024
Published online: 7 January, TAPS 2025, 10(1), 27-35
https://doi.org/10.29060/TAPS.2025-10-1/OA3247
Estivana Felaza1, Ardi Findyartini1,2, Rita Mustika1, Jenny Bashiruddin1, Joedo Prihartono3, Lucia RM Royanto4 & Subha Ramani5
1Department of Medical Education, Faculty of Medicine Universitas Indonesia, Indonesia; 2Medical Education Centre, Indonesia Medical Education and Research Institute (IMERI), Faculty of Medicine Universitas Indonesia, Indonesia; 3Department of Public Health, Faculty of Medicine Universitas Indonesia, Indonesia; 4Faculty of Psychology Universitas Indonesia, Indonesia; 5Brigham Women and Child Hospital, Harvard Medical School, USA
Abstract
Introduction: Professional identity formation requires students’ ability to reflect, which can be supported by constructive feedback from teachers. Feedback practice faces many challenges, including those related to sociocultural aspects. Feedback can be optimised by implementing a model suitable to the attributes of students, teachers, and the clinical environment. This study aimed to develop a suitable feedback model and test its effectiveness in promoting reflection.
Methods: The model was designed based on the theoretical framework and identified feedback-related attributes in FMUI. Expert reviews and cognitive interviews were conducted before the model was tested. The model’s effectiveness was tested using a quasi-experimental design involving 74 students in the Paediatric Module. Students were asked to reflect on their mini-CEX experience after receiving feedback from teachers, and the depth of reflection was compared between students in the intervention and control group. The depth of reflection was measured using Kember scoring, and bivariate analysis was conducted using SPSS 20.0.
Results: The model consists of 5 steps including: Rapport building, Acknowledge students’ strengths, Identify aspect(s) that need improvement, Share teachers’ experiences, and Establish a plan to improve. Deep reflection was more frequently found in the intervention group. Mann-Whitney test showed that the difference between groups was statistically significant (Z=2.964, p=0.003), indicating that reflection in the intervention group was deeper than the control group.
Conclusion: The feedback model formulated based on feedback-related attributes in FMUI was named the RAISE model. Upon testing, students receiving the model could reflect more deeply compared to those receiving the standard model.
Keywords: Feedback, Clinical, Reflection, Sociocultural
Practice Highlights
- Constructive feedback is needed for medical students to optimally form their professional identity, especially in clinical settings
- The RAISE model which was developed based on feedback-related attributes can be implemented in clinical education
- The RAISE model consists of five steps: Building rapport, Acknowledge students’ strengths, Identify aspect(s) to improve, Share teachers’ experience, and Establish a plan to improve
- The RAISE model promotes students’ ability to reflect on their experiences
I. INTRODUCTION
Medical students’ professional identity is mostly formed during their clinical education (Cruess et al., 2015). Professional identity formation is a long and complex process that occurs through the integration of values and norms of the profession. Socio-constructivist theory can explain how learning occurs in clinical settings through the involvement of students in a medical community of practice. As students immerse themselves in the clinical environment, they engage in numerous interactions with their surroundings. The interactions expose them to professional values, which are gradually internalised as students develop their new identity as medical doctors (Cruess et al., 2015).
Optimal professional identity formation requires students’ ability to reflect on their experiences. Reflection enables students to extract meaning from their hectic day-to-day activities, and create plans to continuously improve themselves (Mann et al., 2009). The ability to reflect is also essential in their future profession as doctors. Reflection was defined as critically analysing one’s own experience to reach new and deeper comprehension and insight. Experience become the object to reflect, and the process of recalling and analysing the experience was conducted with the intention of improving future performance (Mann et al., 2009). Reflection also becomes the media to process feelings and emotions, and create plans to improve performance, which leads to improved clinical decision-making ability (Rozental et al., 2021). The importance of reflective practice made it necessary to provide students with opportunity to become skilful in conducting reflection.
The analysis of reflection should include many perspectives to get comprehensive views and insights. One of the ways to support reflection is through the provision of constructive feedback (Husebo et al., 2015; Sandars, 2009). Feedback has been shown to be beneficial in helping students improve their performance (Choi et al., 2020; Johnson et al., 2020; Trehan et al., 2015). Information given through feedback assists students in identifying the improvement needed and the strategies they can use. Feedback can initiate reflections by pointing out the gap between the intended outcome and the current performance; and it can also strengthen reflection by confirming students’ judgment and promoting insights into their performance (Nicol & MacFarlane-Dick, 2006).
Many problems are still found in the practice of feedback in clinical settings, such as the message not being specific enough and the limited time available for interaction. In addition, the Indonesian culture adds certain unique challenges to feedback practice, as identified in our previous study (Felaza et al., 2023). These challenges can be associated with the cultural dimensions of high-power distance and collectivism in Indonesian society. Teachers, experienced and have expertise, are believed by students to know what is best. In a busy clinical environment, the hierarchical gap creates a preference of both teachers and students to engage in directive feedback. In receiving feedback, students tend to appear receptive even when not fully agreeing with the feedback. Being a collectivistic society, group approaches in seeking, providing, and processing feedback practices were commonly found. Students share their feedback experiences with their peers, resulting in collective perception of teacher that they had interacted with (Felaza et al., 2023). Similar challenges have been reported in other studies conducted in Indonesia and Thailand (Areemit et al., 2020; Suhoyo et al., 2018).
Considering the importance of feedback in facilitating students’ professional identity formation, and the way feedback practice is affected by sociocultural aspects, there is a need to develop a feedback model suitable to the attributes of students, teachers, and the clinical environment in Indonesia. This study aims to develop a feedback model relevant to our setting and assess its effectiveness in supporting students’ reflective ability. This study proposes two research aims:
- To develop a feedback model suitable for the Indonesian clinical education setting.
- To evaluate the effectiveness of the feedback model in supporting students’ reflective ability.
II. METHODS
This quantitative research was conducted using a design-based research (DBR) approach, comprising the following steps of identifying the problem, designing a solution, evaluating its effectiveness in a real-life setting, and reflecting on the outcomes (Scott et al., 2020). The first step of our DBR was the identification of feedback-related attributes in FMUI, in a study conducted in September 2023. The next steps, described in detail below, included development of a feedback model within our institution based on data from the previous study, followed by evaluation of its effectiveness in promoting reflection.
A. Feedback model development
The development of the model was guided by a theoretical framework from literature and findings of students’, teachers’, and environmental attributes in our setting. Socio-constructivism, as the theoretical framework, perceives learning as a process of making meanings from experiences through social interactions. Discourses between teacher and students exposes students to thought process and professional norms and values which later can be internalised within themselves. The attributes identified were environmental attributes (limited time, collectivistic, hierarchical, and the need for a safe environment), teachers’ attributes (busy, expert, and having the skill to provide feedback), and students’ attributes (dependent on feedback, less able to read between the lines, perceived to be less resilient, appear to be receptive of feedback, critical, and values teacher’s experience). These findings have been published on September 2023 (Felaza et al., 2023). Along with the socio-constructivist approach as the theoretical framework, these attributes would become the foundation in the development of the model.
Review by experts and cognitive interviews were conducted to ensure the model’s readiness for implementation. Review panel included experts on medical education and communication, program coordinator, and module coordinators. The model was sent via e-mail, and experts were asked to provide feedback on each step and the overall applicability of the model. Cognitive interviews involved clinical teachers from surgery-related and non-surgery-related specialties as future users of the model. After receiving explanation of the model, the teachers practiced the model on their clinical teaching activities. Interviews were held with each teacher to gain input on the experience. Inputs from expert review and cognitive interviews were used to refine the model. The final version of the model was taught to clinical teachers in Paediatric Module as a preparation to test the model. The model was tested during Mini-Clinical Evaluation Exercise (Mini-CEX) by comparing its effectiveness with the Feedback Sandwich method as the standard model being used in FMUI. Mini-CEX is a workplace-based assessment which evaluate students’ performance of clinical skills in real setting. The assessment was originally intended for formative purposes as the clinical teacher observes the performance and provide feedback for students (Hejri et al., 2019). The sandwich model was found to be the common method used for feedback provision in FMUI, and it starts with informing students of the positive aspects of their performance, followed by the negative ones, and closed with another positive aspect (Jug et al., 2019).
B. Testing the effectiveness of the model
The design used was quasi-experimental, involving 5th-year FMUI medical students during their clinical rotation in Paediatric Module. There were 37 students in each group and the data collection took place in May 2022–March 2023. Students in the intervention group received feedback using the new model, while their peers in the control group received feedback using the Sandwich model (Jug et al., 2019). Upon completing data collection in the control group, authors conducted training for teachers on how to utilise the new model, followed by data collection in the intervention group.
Data was collected by asking students to record their voices as they reflect by thinking out loud. FMUI students have been introduced to reflection since the beginning of their academic years, and have experienced completing reflective writing assignments in several modules. For this study, they were instructed to reflect on their experience during mini-CEX. The depth of the reflection was then scored using Kember’s scoring. The scoring was developed by Kember based on Mezirow’s four levels of reflection, and it has been adapted to Bahasa Indonesia (Soemantri et al., 2022). Mezirow divided reflection to 4 levels based on its depth, starting from habitual action which showed no reflection, thoughtful action/understanding, reflection, and critical reflection (Kember et al., 2000). The scoring process was conducted separately by the first author (EF) and two co-authors (AF & RM) and later compared in team discussions to reach an agreed score. Bivariate analysis to test to compare the depth of the reflection between the intervention and the control group was conducted using SPSS 20.0.
III. RESULTS
The criteria for the feedback model were developed based on attributes found from the previous stage (as shown in Table 1 and Table 2).
|
|
Attributes |
Criteria of the Feedback Model |
|
Feedback environment |
|
Can be conducted in a limited time Utilise the high-power distance and collectivism to strengthen the importance of feedback Conducted in a safe environment
|
|
Teachers |
|
Practical Utilise the high-power distance to strengthen Using the faculty development program to strengthen feedback
|
|
Students |
|
Conducted consistently Delivered clearly Avoiding belittlement and sarcasm Conducted in a safe environment Accommodate discussions Enable teachers to share experiences
|
Table 1. Attributes of Factors Affecting Feedback and The Criteria of the Feedback Model
|
Step Proposed |
Criteria of the Feedback Model |
|
Rapport Building |
Develop safe environment
|
|
Acknowledge student’s strengths |
Avoid belittlement and sarcasm Accommodate discussions
|
|
Invite student to reflect |
Avoid belittlement and sarcasm Accommodate discussions
|
|
Share teacher’s experience and tips |
Enable teachers to share experiences Utilise the high power distance to strengthen the importance of feedback
|
|
Establish a plan to improve |
Accommodate discussions
|
Table 2. Steps Proposed and How it Accommodates the Criteria of the Feedback Model
The model was named RAISE as an abbreviation of the first letter in each step. The RAISE model was reviewed by an expert panel, consisting of 3 experts in medical education, 2 experts in communication, and 4 clinical program coordinators. Overall, the RAISE model was perceived as suitable to be implemented in the clinical settings by the expert panel (Figure 1). The crucial aspects that needed to be ensured were teachers’ comprehension of the reasoning behind each step, and the adjustability of the model to be applied in limited time and variability of contexts. Rapport building was considered an essential initial step to start feedback interaction. For the second step, it was advised that teachers ask the student to state positive aspects of performance first before confirmation based on their judgment. The focus of the third step was the areas for improvement, a term that experts emphasised. The step which was initially named ‘invite student to reflect’ was changed into ‘identify aspect that needs improvement’. This revision was made to prevent the misconception that reflection was exclusively covered in the 3rd step. In the fourth step, teachers share their experiences from which students can learn and develop ideas to improve their performance. The information shared should be relevant and can be delivered in a manner that is non-threatening and relevant for the students. The final step in the RAISE model focuses on the action plan for improvement. The agreed plan should be feasible and ready to be implemented.
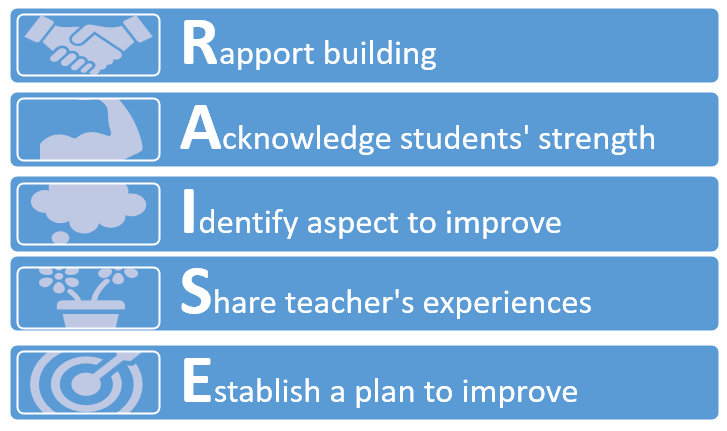
Figure 1. RAISE Model After Expert Review
The model was then utilised by four clinical teachers in various teaching sessions, and cognitive interviews were conducted to gain insight into the experiences. They reported that the model was relatively easy to implement and able to accommodate the limited time available. The model helped develop rapport between teacher and students and enable the two of them to interact more effectively. Continuation between each step was seamless and the conversation did not have to be interrupted due to the movement from one step to another.
The final version was then taught to 22 clinical teachers in August 2022. The training was organised by the first author and two of the co-authors, who had expertise in medical education and experience in conducting faculty development. Various activities were held in the training (video appraisal, discussions, role play, and reflection) to ensure teachers’ ability to perform feedback provision using the RAISE model.
The final version was compared with the Sandwich model, the standard model being used in FMUI, to evaluate its effectiveness. The comparison between the steps of the two models can be seen in Table 3. As shown in the comparison, the strength of the RAISE model lies in its effort to establish rapport from the start of the feedback conversation, its way of facilitating reflection, and the opportunity it provides for teachers to share their experiences.
|
RAISE Model |
Standard Model |
|
Build rapport |
|
|
Discussing positive aspects of performance |
Delivering positive aspects of performance |
|
Discussing negative aspects of performance |
Delivering negative aspects of performance |
|
|
Delivering positive aspects of performance |
|
Sharing teacher’s experience |
|
|
Establishing improvement plan |
|
Table 3. Comparison Between the RAISE Model and the Standard Model
The effectiveness of the model was then tested during mini-CEX in Paediatric Module by comparing the depth of reflection in the experimental and control group. There were 37 students in each group with majority of students in experimental and control groups (30 and 28 students respectively) were female and belonged in the year 2018 batch.
Students reflected on the feedback they received, and the depth of the reflection was rated using the Kember score with the score ranging from 1-4 (1: no reflection; to 4: deep reflection). The distribution of the depth of students’ reflection is shown in Table 4.
|
Kember Score |
Intervention Group (%) |
Control Group (%) |
|
1 (no reflection) |
|
|
|
2 (comprehension) |
2 (5.4%) |
16 (43.2%) |
|
3 (reflection) |
26 (70.2%) |
17 (45.9%) |
|
4 (deep reflection) |
9 (24.4%) |
4 (11.9%) |
Table 4. Distribution of the Depth of Students’ Reflection
The distribution showed most of the students’ reflections in the intervention group were scored 3 based on the Kember score (26 students or 70.2%); while the score in the control group was almost evenly divided between 2 (16 students or 43.2%) and 3 (17 students or 45.9%). Deep reflection was more frequently found in the intervention group (9 students or 24.4%) compared to the control group (4 students or 11.9%).
Mann-Whitney test was used to compare the depth of students’ reflection between the intervention and the control group. The test showed that the mean rank in the intervention group was 30.61 and in the control group was 44.39. The difference between the two groups was statistically significant (Z = 2.964, p = 0.003), indicating that students’ reflections in the intervention group were deeper than their peers in the control group.
IV. DISCUSSION
This study aimed to develop a culturally relevant feedback model that nurtured reflective ability of medical students and to evaluate its effectiveness. The results indicated that students receiving feedback using the RAISE model could reflect more deeply compared to their peers receiving feedback using the standard model. The RAISE model was designed to enable feedback practice in an interactive manner, while feedback using Sandwich model was more directive. The RAISE model starts by building rapport between teacher and student in order to create a safe environment which helps student to optimally conduct reflection. The 2nd and 3rd steps of the model guide students’ reflection systematically, covering both the positive and negative aspects of the performance. On the 4th step, teachers’ sharing of their experiences helps to enrich students’ reflection, enabling them to learn from the experience, as well as strengthening and further maintaining the rapport between them. The final step concludes the interaction with a plan that students can implement to improve. Each of these steps portrays how reflection is guided and supported by the teacher through the feedback interaction.
The RAISE model was developed based on the socio-constructivist theory that describes learning as a way of constructing meaning from experiences. In clinical settings, students are exposed to a variety of experiences to build comprehension, acquire skill proficiency, and integrate professional norms and values. Effective feedback interactions between teachers and students facilitate students’ reflective process and support them in identifying effective ways to improve their performance (Wenger, 2020). Through these interactions, students are exposed to the teacher’s thought process, as well as their professional norms and values. The process that starts as inter-mental between teacher and student gradually becomes internalised into intra-mental within the student (Amineh & Asl, 2015; Tappan, 2010). This process enables teachers to guide students to reach their zone of proximal development (ZPD). Students are supported at each stage of their performance through the concept of scaffolding, and the level of support given would be decreased gradually as students gain the ability for independent clinical practice (Fani & Ghaemi, 2011).
Our previous study highlighted the need for rapport development and the act of sharing teachers’ own experiences in developing the feedback model (Felaza et al., 2023). Rapport was considered essential to create a safe environment for students. Interactions that empowered students in an authentic and safe environment, and teachers as role models in practicing reflection, were needed for creating reflective habits among students (Gathu, 2022; Mann et al., 2009). A sense of safety in feedback interaction was built upon a good relationship between teacher and students, mutual goals, and students’ perception of the teacher’s credibility (Sargeant et al., 2017). In the RAISE model, the safe environment has been developed since the beginning by building rapport between teacher and students. When students reflect, they would need to be open in analysing their experience. Destructive feedback would create reluctance for students to share their reflections (Chan & Lee, 2021; Khoiriyati & Sari, 2021). The model started by asking students’ perceptions of their performance, and their previous experience with similar situations; encouraging them to be open and reflective. The questions were relatively easy to answer and able to lighten the situation. Safety was continuously built through constructive dialogue between teachers and students which created an environment that was safe for reflection (MacNeil et al., 2020; Telio et al., 2015). Mutual goals also can implicitly be seen in students’ perception of the teacher’s intention. When the students believe that feedback was given to help them improve, they would be more willing to openly reflect (Blakey et al., 2019; Eva et al., 2012).
The reflection process is initiated when the condition cannot be handled simply by the automatic action the individual usually conducts or habitual act (Mann et al., 2009). The initiation of reflection might also be triggered by feedback. The feedback information made the individuals realise the quality of their performance, highlighting the strength and weaknesses that requires improvement (Husebo et al., 2015; Mann et al., 2009). When students receive feedback that is aligned with their perception regarding the quality of their performance, reflection usually occurs faster. However, for feedback information that is not aligned, students need to first manage the negative emotion it might evoke, analyse the message, and contemplate what action plan should be taken (Sargeant et al., 2009).
Teachers, perceived as knowledgeable figures, have numerous valuable experiences they can share. By incorporating the act of sharing experience, every feedback interaction would provide lessons from which students can extract meaningful understanding. This particular approach has not been seen explicitly in other feedback models. Other than enriching students’ comprehension, the sharing also provides a sense of relatedness with the teacher, and a role model on how to become reflective (Burgess et al., 2020). A role model in practicing reflection was an important aspect of strengthening students’ motivation. Teachers who practice self-reflection confirm to students that such practice can be done in their profession as doctors. Teachers’ reflective behaviour also showed the students that admitting weaknesses was not an embarrassing act, and on the contrary, it was an important skill to master to improve (Gishen & Chakrabarti, 2022). In the RAISE model, the opportunity for teachers to demonstrate reflection was mostly done in the 4th step. In this step, teachers can share their experiences that was relevant to the situation the students faced. Upon sharing the experience, the teacher can explain the lesson learned from that experience. Students receiving feedback using the RAISE model claimed that this step exposed them to teachers’ openness and minimised the power distance between them. Students also felt more motivated by listening to the experiences. Sense of relatedness was one of the factors that increased intrinsic motivation. The teachers’ willingness to share their experiences creates a connection between them and students, and strengthens students’ internal motivation (Kusurkar et al., 2011).
Other than being influenced on a systemic level by cultural aspects, such as power distance and collectivism; reflection is also affected in individual level by students’ and teachers’ reflective ability, teachers’ ability in facilitating reflection, and the relationship between teacher and students (Chan & Lee, 2021). The RAISE model supports teachers in facilitating students’ reflection through the use of reflective questions and the opportunity to show students how reflection was practiced by themselves as they shared their experiences. The rapport built during the interactions also strengthens the teacher-student relationship which further enables students to be more open and trusting in conducting their reflection.
Students’ reflective ability was crucial in their education process and later as they became member of the medical profession. Experiences in the clinical learning environment, which depicts the authentic professional world that students would enter, expose students to norms and values. Through reflection, students create meanings from these experiences which facilitate the formation of their professional identity as medical doctors (Winkel et al., 2017).
This study showed that implementation of the RAISE model, a feedback model developed based on the feedback-related attributes in Indonesian settings, enabled students to reflect more deeply on their performance. Findings from the study suggested that the RAISE model was suitable for supporting students’ reflection in a setting with high power distance and collectivistic background. However, it should be noted as a limitation of this study that reflection was an internal process and the effect might not be visible immediately. The changes in comprehension, perspectives, and even students’ attitude occurs gradually along the reflection process that was taking place. Therefore, further research is needed to observe the effect of reflection which might require longitudinal observation of students’ performance. The study involved a single institution in Jakarta, and therefore research and certain adjustments might be needed before the model can be implemented in different settings.
V. CONCLUSION
The feedback model formulated based on the feedback-related attributes in our clinical setting was named the RAISE model. It consists of 5 steps, which are Rapport building, Acknowledge student’s strengths, Identify aspects that need improvement, Share teacher’s experience and tips, and Establish a plan to improve. Our data indicate that students receiving feedback using the RAISE model were able to reflect more deeply compared to their peers receiving the standard model. We conclude that the model’s ability to create a safe environment, build rapport between teachers and learners, and teachers’ role-modelling of reflective practice can encourage students to be more self-reflective of their clinical performance.
Notes on Contributors
Estivana Felaza, Ardi Findyartini, Rita Mustika, Jenny Bashiruddin, Joedo Prihartono, Lucia RM Royanto, and Subha Ramani contributed to all processes of this research, and have read and approved this manuscript.
Dr. dr. Estivana Felaza, MPdKed is a Lecturer in Faculty of Medicine, Universitas Indonesia. She reviewed the literatures, designed the study, performed data collection and analysis, and wrote the manuscript.
Prof. dr. Ardi Findyartini, PhD is a Professor of Medical Education in the Faculty of Medicine, Universitas Indonesia. She developed the methodological framework for this research, involved in scoring the students’ reflections (data), provided feedback on the data collection, data analysis, and the manuscript writing process.
Dr. dr. Rita Mustika, M.Epid is an expert in Medical Education and a Lecturer in the Faculty of Medicine, Universitas Indonesia. She developed the methodological framework for this research, was involved in scoring the students’ reflections (data), provided feedback on the data collection, data analysis, and manuscript writing process.
Prof. Dr. dr. Jenny Bashiruddin, SpTHT-KL(K) is a Professor in Otolaryngology and an expert in Medical Education. She provided feedback on the theoretical and methodological framework of this research, data collection, data analysis, and the manuscript writing process.
Dr. dr. Joedo Prihartono, MPH is an expert in Statistics and a Senior Lecturer in Community Medicine, Faculty of Medicine, Universitas Indonesia. He provided feedback on the methodological framework of this research, data collection, data analysis, and the manuscript writing process.
Dr. Lucia RM Royanto, M.Si, Sp.Ed is an expert in Educational Psychology and a Senior Lecturer in the Faculty of Psychology, Universitas Indonesia. She provided feedback on the theoretical framework of this research, data collection, data analysis, and the manuscript writing process.
Dr. Subha Ramani, MBBS, MPH, PhD, FAMEE is an expert in Medical Education and an Associate Professor of Medicine in Harvard Medical School. She provided feedback on the theoretical and methodological framework of this research, data collection, data analysis, and the manuscript writing process.
Ethical Approval
The study was approved by the Research Ethics Review Committee of the Faculty of Medicine, Universitas Indonesia (approval number: KET-1114/UN2.F1/ETIK/ PPM.00.02/2021). The subjects of this study were informed verbally and in writing of the purpose, the methods, and the confidentiality of the data being collected. Each subjects’ involvement in this research were voluntary, and consent were signed upon receiving the necessary information.
Data Availability
Datasets generated and/or analysed in this study are available upon request via electronic mail to the corresponding author.
Acknowledgement
The authors would like to acknowledge the contributions of the students and clinical teachers who willingly involved and cooperated in this study.
Funding
No funding was obtained for this study.
Declaration of Interest
All authors have no declaration of interest.
References
Amineh, R. J., & Asl, H. D. (2015). Review of constructivism and social constructivism. Journal of Social Science, Literature & Language, 1(1), 9–16.
Areemit, R. S., Cooper, C. N., Wirasorn, K., Paopongsawan, P., Panthongviriyakul, C., & Ramani, S. (2020). Hierarchy, “Kreng Jai”, and feedback: A grounded theory study exploring perspectives of clinical faculty and medical students in Thailand. Teaching and Learning in Medicine, 33(3), 235–244. https://doi.org/10.1080/10401334.2020.1813584
Blakey, A. G., Smith-Han, K., Anderson, L., Collins, E., Berryman, E., & Wilkinson, T. (2019). “They cared about us students”: Learning from exemplar clinical teaching environments. BMC Medical Education, 19, 119–128. https://doi.org/10.1186/ s12909-019-1551-9
Burgess, A., van Diggele, C., Roberts, C., & Mellis, C. (2020). Feedback in the clinical settings. BMC Medical Education, 20(Suppl 2), 458–463. https://doi.org/10.1186/s12909-020-02280-5
Chan, C. K. Y., & Lee, K. K. W. (2021). Reflection literacy: A multilevel perspective on the challenges of using reflections in higher education through a comprehensive literature review. Educational Research Review, 32(2), Article 100376. https://doi.org/10.1016/j.edurev.2020.100376
Choi, S., Oh, S., Lee, D. H., & Yoon, H. S. (2020). Effects of reflection and immediate feedback to improve clinical reasoning of medical students in the assessment of dermatologic conditions: A randomized controlled trial. BMC Medical Education, 20, 146–154. https://doi.org/10.1186/s12909-020-02063-y
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2015). A schematic representation of the professional identity formation and socialization of medical students and residents: A guide for medical educators. Academic Medicine, 90(6), 718–725. https://doi.org/10.1097/acm.0000000000000700
Eva, K. W., Armson, H., Holmboe, E., Lockyer, J., Loney, E., Mann, K., & Sargeant, J. (2012). Factors influencing responsiveness to feedback: On the interplay between fear, confidence, and reasoning process. Advance in Health Science Education, 17, 15–26. https://doi.org/10.1007/s10459-011-9290-7
Fani, T., & Ghaemi, F. (2011). Implications of Vygotsky’s zone of proximal development in teacher education. Social Behavioral Science, 29, 1549–1554. https://doi.org/10.1016/j.sbspro.2011.11. 396
Felaza, E., Findyartini, A., Mustika, R., Bashiruddin, J., Royanto, L. R. M., Prihartono, J., & Ramani, S. (2023). Deeper look into feedback practice in an Indonesian context: Exploration of factors in undergraduate clinical setting. Korean Journal of Medical Education, 35(3), 263–273. https://doi.org/10.3946/kjme.2023.264
Gathu, C. (2022). Facilitators and barriers of reflective learning in postgraduate medical education: A narrative review. Journal of Medical Education and Curriculum Development, 9, 1–8. https://doi.org/10.1177/23821205221096106
Gishen, F., & Chakrabarti, R. (2022). Medical students’ perceptions of reflective practice in the undergraduate curriculum. MedEd Publish, 12, 53–67. https://doi.org/10.12688/mep.19211.3
Hejri, S. M., Jalili, M., Masoomi, R., Shirazi, M., Nedjat, S., & Norcini, J. (2019). The utility of mini clinical examination exercise in undergraduate and postgraduate medical education: A BEME review: BEME guide no. 59. Medical Teacher, 42(2), 1–18. https://doi.org/10.1080/0142159x.2019.1652732
Husebo, S. E., O’Reagen, S., & Nestel, D. (2015). Reflective practice and its role in simulation. Clinical Simulation in Nursing, 11, 368–375. http://doi.org/10.1016/j.ecns.2015.04.005
Johnson, C. E., Weerasuria, M. P., & Keating, J. L. (2020). Effect of face-to-face verbal feedback compared with no alternative feedback on the objective workplace task performance of health professionals: A meta-analysis and systematic review. BMJ Open, 10(3), Article e030672. https://doi.org/10.1136/bmjopen-2019-030672
Jug, R., Jiang, X., & Bean, S. M. (2019). Giving and receiving effective feedback. Archives of Pathology and Laboratory Medicine, 143, 244–250. https://doi.org/10.5858/arpa.2018-0058-RA
Kember, D., Leung, D. Y. P., Jones, A., Loke, A. Y., MacKay, J., Sinclair, K., Tse, H., Webb, C., Wong, F. K. Y., Wong, M., & Yeung, E. (2000). Development of a questionnaire to measure the level of reflective thinking. Assessment and Evaluation in Higher Education, 25(4), 381–395. http://doi.org/10.1080/713611442
Khoiriyati, A., & Sari, N. K. (2021). Reflective practice on nursing students: A qualitative study. Indonesian Nursing Journal of Education and Clinic, 6(2), 201–209. http://doi.org/10.24990/in jec.v6i2.391
Kusurkar, R., Croiset, G., & Ten Cate, O. (2011). Twelve tips to stimulate intrinsic motivation in students through autonomy-supportive classroom teaching derived from self-determination theory. Medical Teacher, 33, 978–982. https://doi.org/10.3109/01 42159x.2011.599896
MacNeil, K., Cuncic, C., Voyer, S., Butler, D., & Hatala, R. (2020). Necessary but not sufficient: Identifying conditions for effective feedback during internal medicine residents’ clinical education. Advances in Health Science Education, 25, 641–654. https://doi.org/10.1007/s10459-019-09948-8
Mann, K., Gordon, J., & MacLeod, A. (2009). Reflection and reflective practice in health professions education: A systematic review. Advances in Health Science Education, 14, 595–621. https://doi.org/10.1007/s10459-007-9090-2
Nicol, D., & MacFarlane-Dick, D. (2006). Formative assessment and self-regulated learning: A model and seven principles of good feedback practice. Studies in Higher Education, 31(2), 199–218. https://doi.org/10.1080/03075070600572090
Rozental, L., Meitar, D., & Karnielli-Miller, O. (2021). Medical students’ experiences and needs from written reflective journal feedback. Medical Education, 55, 505–517. https://doi.org/10.1111/medu.14406
Sandars, J. (2009). The use of reflection in medical education: AMEE Guide no 44. Medical Teacher, 31, 685–695. https://doi.org/10.1080/01421590903050374
Sargeant, J. M., Mann, K. V., van der Vleuten, C. P., & Metsemakers, J. F. (2009). Reflection: A link between receiving and using assessment feedback. Advances in Health Science Education, 14, 399–410. https://doi.org/10.1007/s10459-008-9124-4
Scott, E. E., Wenderoth, M. P., & Doherty, J. H. (2020). Design-based research: A methodology to extend and enrich biology education research. CBE Life Science Education, 19(3), 1–12. https://doi.org/10.1187/cbe.19-11-0245
Soemantri, D., Mustika, R., & Greviana, N. (2022). Inter-rater reliability of reflective writing assessment in an undergraduate professionalism course in medical education. Education in Medicine Journal, 14(1), 87–97. http://doi.org/10.21315/eimj2022.14.1.8
Suhoyo, Y., Schönrock-Adema, J., Emilia, O., Kuks, J. B. M., & Cohen-Schotanus, J. (2018). Clinical workplace learning: Perceived learning value of individual and group feedback in a collectivistic culture. BMC Medical Education, 18, 79–84. https://doi.org/10.1186/s12909-018-1188-0
Tappan, M. (2010). Sociocultural psychology and caring pedagogy: Exploring Vygotsky’s hidden curriculum. Educational Psychology, 33(1), 23–33. http://doi.org/10.1207/s15326985ep3301_2
Telio, S., Ajjawi, R., & Regehr, G. (2015). The “Educational Alliance” as a framework for reconceptualizing feedback in medical education. Academic Medicine, 90(5), 609–614. https://doi.org/10.1097/acm.0000000000000560
Trehan, A., Barton-Vaness, A., Carty, M. J., McCulloch, P., & Maruthappu, M. (2015). The impact of feedback of intraoperative technical performance in surgery: A systematic review. BMJ Open, 5, Article e006759. http://doi.org/10.1136/bmjopen-2014-006759
Wenger, E. (2020). Communities of practice and social learning systems: The career of a concept. Organization, 7(2), 225–246. http://doi.org/10.1177/135050840072002
Winkel, A. F., Yingling, F., Jones, A. A., & Nicholson, J. (2017). Reflection as a learning tool in graduate medical education: A systematic review. Journal of Graduate Medical Education, 5, 430–439. https://doi.org/10.4300/jgme-d-16-00500.1
*Estivana Felaza
Faculty of Medicine Universitas Indonesia,
Jalan Salemba Raya No 6,
Jakarta 10430, Indonesia
Email: estivanafelaza@gmail.com;
estivana.felaza01@ui.ac.id
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









