Perceptions of Do Not Attempt Resuscitation (DNAR) amongst nurses in an Asian modern ageing society
Published online: 4 September, TAPS 2018, 3(3), 35-38
DOI: https://doi.org/10.29060/TAPS.2018-3-3/SC1062
Li-Phing Clarice Wee
Ng Teng Fong General Hospital, Singapore
Abstract
Objectives: Do Not Attempt Resuscitation (DNAR) orders have been used in hospitals worldwide for the past 30 years, but are still considered to be a challenging and difficult area of practice. Nurses being the frontline healthcare professionals should be involved during the decision-making process and are required to have good understanding of the DNAR order, in order to provide effective and efficient care. Our aim was to investigate: nurses’ involvement during decision-making process, level of understanding of issues surrounding DNAR orders; and how they perceive care for patients with DNAR orders.
Methods: A descriptive crossed sectional study design using electronic questionnaires was adopted for the study. The study was conducted among 400 nurses at a tertiary hospital in Singapore.
Results: This study showed that 44.5% of nurses reported physicians did not involve them in decisions for DNAR orders; only 8% felt that they should be involved in the decision-making process. Even if they did not agree with the order, 63.2% would still comply whilst 21% of them were willing to discuss this further with the treatment teams. Most agreed that antibiotics, intravenous fluids, oxygen therapy and artificial feeding were appropriate for patients with DNAR orders. Majority (57.1%) expressed uneasiness in discussing end of life issues with patients even in specialty areas.
Conclusion: Nurses should be encouraged to advocate for their patient and take part in the decision-making process. Communication between the medical team and nurses can be improved and there is an obvious need for further improvement in education and collaboration in this area.
Keywords: Do Not Attempt resuscitation, End-of-Life, Withdrawal, Palliative Care
I. INTRODUCTION
Do-Not-Attempt Resuscitation (DNAR) orders have been used in hospitals worldwide for over the past 30 years with the intention of preventing non-beneficial treatments for hospitalized patients. These orders provide direction for the medical team and often take place after discussion with the patient, their family members and the multidisciplinary team as this decision is often complex with possible legal, ethical and moral implications. Although these decisions are typically initiated by physicians, nurses play a key role in DNAR discussions as well (Gendt et al., 2006).
Nurses are often the first point of contact for a patient and have the responsibility to act as patient advocates (Fitz, Fuld, Haydock & Palmer, 2010). They are in the best position to fulfil a liaison role between physicians and patients; conveying patient preferences to the physicians and influencing acceptance by the patient or surrogate decision-maker of the medical recommendations of DNAR (Gendt et. al, 2006). Many studies have shown that healthcare workers tend to provide less medical care to DNAR patients and inconsistencies around what continuing care should be given to patients exist. Similarly, DNAR orders can also influence the delivery of nursing care. Fitz et. al (2010)’s study showed that a significant number of nurses believed a DNAR order altered nursing observation frequency, pain relief and fluids administered.
Though end-of-life care and patients with DNAR orders can co-exist, there might be a fine line in terms of treatment goals and outcomes. A study done by Stewart and Baldry (2010) found that a DNAR decision is perceived by some as equivalent to withdrawal of active treatment. The aim of the study was to identify nurses’ involvement during the decision-making process, level of understanding of issues surrounding DNAR orders; and how they perceive care for patients with DNAR orders.
II. METHODS
A. Design and Setting
A descriptive crossed sectional study design using electronic questionnaires was adopted for the study. It was conducted at 700-bedded hospital in Singapore where approximately 2500 nurses work full-time.
B. Sample
Convenience sampling method was adopted for the recruitment of nurses in the study and 400 nurses participated in the study.
C. Instruments Used
The questionnaire was adapted from a previous study with the author’s permission (O’Hanlon, O’Connor, S., Peters & O’Connor, M., 2013) and piloted on 50 nurses working in the ICU and High Dependency Unit (HDU). Thereafter, the questionnaire was further modified and consisted of 24 questions to improve the clarity of some questions and to better address the aims of the study.
D. Data Collection and Analysis
Ethical approval was obtained from the Institutional Review Board prior to data collection. Data was collected over a period of 5 months (June – October 2016). Consent was assumed if the survey was completed. Responses were collected anonymously through an electronic platform with a secured login. Responses were confidential and descriptive statistics analysis was used to analyse the data.
III. RESULTS
Majority of respondents were 21-30 years old females, with an average work experience of less than 5 years. Most of the participants were Chinese and an equal number of participants had a degree or Masters as their highest qualification. Majority of the participants were staff nurses who work in a medical ward, whilst other responses were collected from nurses working in the ICU, emergency department (ED) and surgical wards.
A. Involvement in the Decision-Making Process
Nurses thought that the patient (75.5%), family members (83.5%) and physicians (79%) should be involved in DNAR decision-making process as shown in Figure 1. However, only 8% thought that nurses should be involved in this process. A proportion of nurses (13.8%) reported that they had previously disagreed with a DNAR decision, but 63.2% said that they would still comply with the orders even if they did not agree. Majority (57.1%) of the nurses reported that they were not comfortable discussing end-of-life issues with patients and their family members and a sub-group analysis revealed that this was also true for nurses working in specialty areas like the Intensive Care Unit, High Dependency Unit and Emergency Department.
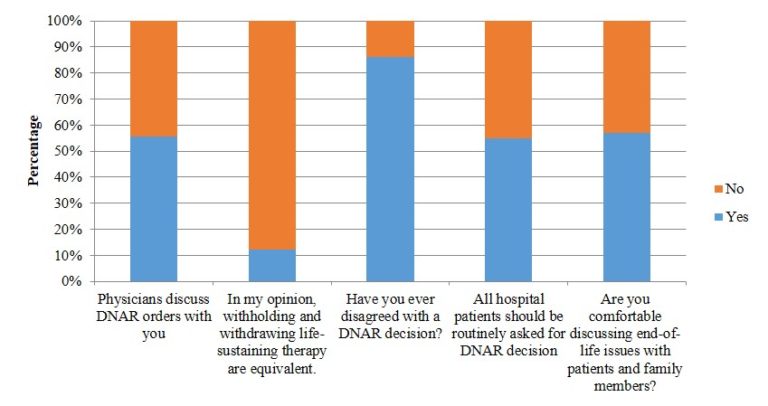
Figure 1. Involvement in the decision-making process (N=400)
B. Perceptions and Understanding
The results in Figure 1 showed that majority (63%) felt that withholding and withdrawing life-sustaining therapy were equivalent. There was no consensus with regards to the survival rate for out-of-hospital cardiac arrest and in-hospital cardiac arrest rates and these were generally overestimated. If a patient had a DNAR order in place, therapies like antibiotics, intravenous fluids, oxygen therapy and nasogastric feeds were deemed to be appropriate. Other therapies like intubation, cardiac compression, defibrillation, surgery, transfer to HD or ICU, dialysis and antiarrhythmic for life threatening cardiac rhythm were thought to be less appropriate. There were no differences observed between junior and senior nurses.
IV. DISCUSSION
To our knowledge, this study is the first to investigate nurses’ involvement during the decision-making process; and how they perceive care for patients with DNAR orders in a Singapore.
The study provided insight to gaps in communication that exist amongst the medical and nursing team; and the central importance of communication between these two teams. From the study, an alarming number of nurses revealed that they were not comfortable discussing end-of-life issues with patients or family members, even if they worked in critical areas.
Unlike Western countries, Singapore does not have a national policy on DNAR or an established framework to guide end-of-life care. Various studies have reported that the distinction between withholding and withdrawing treatment is not always recognised, and an assumption is often made that DNAR equates to withdrawal of active treatment (Stewart & Baldry, 2010). This is also observed in this study as majority of the respondents felt that withholding and withdrawing life-sustaining measures were equivalent. There is often an overlap between the two areas but more importantly, these decisions should be individualised to patients.
Results of the study showed that respondents of this study generally overestimated the survival rate of out-of-hospital cardiac arrest rates, in-hospital survival rates, recovery with good neurological function and survival to discharge. This study also revealed that nurses regarded therapies like IV fluids, antibiotics, oxygen therapy and nasogastric tube feeding as appropriate for patients with a DNAR order. The findings differed from O’Hanlon et. al (2013)’s study that surfaced some confusion over palliation and DNAR orders and only 36% of nurses felt that nasogastric tube feeding was appropriate for patients with DNAR orders. A recent study exploring physician attitudes towards withholding and withdrawal of life-sustaining treatments in end-of-life care saw that most were more ready to withhold and withdraw haemodialysis than enteral feeds (Phua et. al, 2015). This difference could perhaps reflect cultural differences as the Asian culture consider food and nutrition as basic rather than medical care, representing love and hope for health and an expression of filial piety (Phua et. al, 2015).
Being a single-centred questionnaire-based study, there are limitations to be considered. Half of the respondents only had 5 years or less of working experience. Religious beliefs of the participants were also not included in this study and this could potentially contribute to the nurses’ views on end-of-life care. As such, findings should not be generalised to the nursing population in Singapore or Asia and a larger study is recommended to replicate the study findings.
A. Implications for Clinical Practice and Further Research
This study has multiple important implications. Firstly, there is clearly a need for more training and increased confidence to improve nurses’ involvement in the DNAR process. Nursing education has traditionally been focused on nursing diagnoses and the practical aspects of care. However, good communication skills surrounding end-of-life conversations are also required in order to advocate and better care for their patients. Perhaps nursing schools and hospitals should consider developing a structured programme to help improve communication skills surrounding difficult topics like end-of-life care and DNAR orders. Nurses should also be encouraged to be more involved in the DNAR process, encouraging open communication especially when expectations are not aligned with patients or family members and the treatment team.
Further research is recommended with a bigger population of nurses from various hospitals throughout Singapore and even Asia to provide more insight into this topic. Future research should also focus on testing the validity of the tool used in this study since it has not been tested after modification of the questionnaire.
As DNAR policies and issues surrounding withdrawal and withholding of care for these patients can vary from hospital to hospital, a national policy guiding physicians and nurses the matter could be developed to better equip healthcare workers with the necessary information needed to care for patients.
V. CONCLUSION
This study gives first insight into the perceptions and understanding of nurses surrounding DNAR orders and the care rendered for these patients. Being at the forefront, nurses should be encouraged to communicate openly with the medical team and advocate for their patients. In order to do so, structured programs and national policies should be considered so as to guide and support nurses through this process.
Notes on Contributors
Wee Li-Phing Clarice is an Advanced Practice Nurse at Ng Teng Fong General Hospital, Singapore.
Institutional Review Board (IRB)
Standard institutional review board (IRB) procedures were followed and approval was obtained by the author. IRB number 2016/00413.
Acknowledgements
The author would like to thank Dr. Ross Freebarin and Dr. Faheem Khan for their valuable suggestions towards the study design and questions; and Dr. Yanika Kowitlawakul for her help in reviewing the article. In addition, the author would also like to thank Ms Syairah Binte Mohd Reduan and Mr. Johnny Wong for their assistance during the pilot study that contributed towards the final questionnaire used in this study.
Declaration of Interest
The author does not have any declaration of conflict of interest, including financial, consultant, institutional and other relationships that might lead to bias.
References
Fitz, Z., Fuld, J., Haydock, S. & Palmer, C. (2010). Interpretation and intent: A study of the (mis)understanding of DNAR orders in a teaching hospital. Resuscitation, 81(9), 1138-1141. https://doi.org/10.1016/j.resuscitation.2010.05.014.
Gendt, C. D., Bilsen, J., Stichele, R. V., Noortgate, N. V. D., Lambert, M. & Deliens, L. (2007). Nurses’ involvement in ‘do not resuscitate’ decisions on acute elder care wards. Journal of Advanced Nursing, 57(4), 404-409.
O’Hanlon, S., O’Connor, S., Peters, C. & O’Connor, M. (2013). Nurses’ attitudes towards Do Not Attempt Resuscitation orders. Clinical Nursing Studies, 1(1), 43-50.
Phua, J., Joynt, G. M., Nishimura, M., Deng, Y., Myatra, S. N., Chan, Y. H. … Koh, Y. (2015). Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Internal Medicine, 175(3), 363-371. https://doi.org/10.1001/jamainternmed.2014.7386.
Stewart, M. & Baldry, C. (2010). The over-interpretation of DNAR. Clinical Governance: An International Journal, 16(2), 119-128. https://doi.org/10.1108/14777271111124473.
*Wee Li-Phing Clarice
Email: clarice_wee@nuhs.edu.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









