Online medical interview training in preclinical medical education: Educational outcomes comparable to face-to-face training
Submitted: 24 October 2024
Accepted: 5 July 2025
Published online: 7 October, TAPS 2025, 10(4), 26-34
https://doi.org/10.29060/TAPS.2025-10-4/OA3552
Shoko Horita1,2, Masashi Izumiya2, Satoshi Kondo2,3,4, Junki Mizumoto2,5,6, Hiroko Mori6,7 & Masato Eto2
1Department of Medical Education, School of Medicine, Teikyo University, Itabashi-ku, Tokyo, Japan; 2Department of Medical Education Studies, International Research Centre for Medical Education, Graduate School of Medicine, The University of Tokyo, Bunkyo-ku, Tokyo, Japan; 3Department of Medical Education, Graduate School of Medicine, University of Toyama, Toyama, Japan; 4Center for Medical Education and Career Development, Graduate School of Medicine, University of Toyama, Toyama, Japan; 5Department of Family Practice, Ehime Seikyo Hospital, Matsuyama, Ehime, Japan; 6Center for General Medicine Education, School of Medicine, Keio University, Shinjuku, Tokyo, Japan; 7Professional Development Centre, The University of Tokyo Hospital, Bunkyo-ku, Tokyo, Japan
Abstract
Introduction: Conventionally, face-to-face education has been prevalent in medical education because it can help medical students learn interpersonal skills, including medical interviews and physical examination. However, because of the coronavirus disease 2019 pandemic, face-to-face education was suspended to prevent the spread of the infection. As face-to-face classes in Japan were discontinued when the pandemic began in the spring of 2020, we developed an online education program to develop medical interview skills. We were interested in determining the educational outcomes between face-to-face and online medical interview classes. Therefore, we compared them before and after the pandemic.
Methods: Fourth-year students of the University of Tokyo Medical School took medical interview classes. Under consent, the score of the medical interview area of the preclinical clerkship, Objective Structured Clinical Examination (OSCE), as a high-stakes examination, which falls at the top level of the Kirkpatrick’s model, was compared by year or before and after the pandemic.
Results: The online group showed higher item-wise scores of the medical interview of the preclinical clerkship OSCE than the face-to-face group. In terms of the global score, no significant difference was observed. In the computer-based test (CBT), the online group had higher scores compared with the face-to-face group.
Conclusion: The educational outcomes of online medical interview classes were not inferior to those of conventional face-to-face classes, as revealed by high-stakes examination preclinical clerkship OSCE. Similar to face-to-face education, online education is a viable option for developing interpersonal skills.
Keywords: COVID-19 Pandemic, Medical Interview, OSCE, Educational Outcome, Online Education, Interpersonal Skills, Communication Skills
Practice Highlights
- Due to the COVID-19 pandemic, we shifted medical interview classes from face-to-face to online.
- The online group had interview global OSCE scores non-inferior to those of the face-to-face group.
- The online group had higher interview elementary OSCE scores than the face-to-face group.
I. INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic severely restricted face-to-face teaching and affected almost all levels and fields of education, including undergraduate preclinical medical education (Bastos et al., 2022; Crawford et al., 2020). Moreover, it resulted in drastic changes in medical education. Globally, face-to-face learning was forcibly discontinued as part of infection control. Thus, to continue medical education, online or remote learning was rapidly introduced (Daniel et al., 2021; Gordon et al., 2020). Various instrumental trans communication devices, including video conferencing tools, simulation, virtual reality, and augmented reality, were used to facilitate online learning. However, this rather hasty shift from face-to-face to online learning brought some confusion into the field of medical education. In the UK, Dost et al. (2020) reported that medical students were unsatisfied with online classes compared with face-to-face classes.
Globally, tele-education is increasingly being encouraged around the world (American Medical Association, 2016). In the field of medical interview (Budakoğlu et al., 2021; Hammersley et al., 2019; Zaccariah et al., 2022), telemedicine is gradually becoming common, showing favourable results. However, because of technical problems, tele-education did not spread smoothly (Zaccariah et al., 2022). Additionally, the educational outcomes of both strategies have not been satisfactorily studied (Khamees et al., 2022). Recently, some reports showing that the educational outcome of online classes are equal or more effective than traditional face-to-face education, however, they are restricted mainly in knowledge-based education (Alshaibani et al., 2023; Basuodan, 2024; Saad et al., 2023). Furthermore, few studies have compared high-stakes examination, including the Objective Structured Clinical Examination (OSCE), and no study has compared the educational results between face-to-face classes and tele-education (online) using the top level of Kirkpatrick’s model (Kirkpatrick, 1996).
The OSCE (Harden et al., 1975) has been widely accepted as a form to assess clinical performance in medical education. Currently, OSCEs are used worldwide to appraise medical students’ communication and clinical skills. Various educational methods have been evaluated using OSCE as one of the indicators of educational outcomes (Guetterman et al., 2019). In Japan, passing the preclinical clerkship (pre-CC) OSCE has become legally obligatory as one of the elements for promotion to the CC course since the spring of 2023. In 2023, the pre-CC OSCE in Japan is conducted in at least eight areas, which are medical interview, “Basic Clinical Procedure”, “Basic Life Support”, and physical examinations of “head and neck”, “chest”, “vital signs”, “abdomen”, and “neurological examinations”.
In the present study, we aimed to determine the educational outcomes between face-to-face and online medical interview classes. We provided medical interview classes to fourth-year medical students before taking the pre-CC OSCE, face-to-face classes before 2019, and tele-education (online) after 2020. We decided to conduct research in medical interview, other than the other areas of the pre-CC OSCE, because of the importance of the medical interview as the basis of medical practice. Moreover, it was inevitable that the medical interview classes had to be implemented as online classes to protect the simulated patients form the risk of infection, which was another main reason for selecting medical interview for this research. In another point of view, medical interview classes were able to implement via online. As mentioned above, no prior studies have compared face-to-face and online medical interview training using both high-stakes OSCE score and Kirkpatrick’s top-level outcomes, our study would have significant importance.
II. METHOD
A. Participants
This study was approved in 2021 by the ethics committee of the University of Tokyo (UTokyo) Faculty of Medicine (Approval No. 2021005NI). All methods were performed in accordance with the relevant guidelines and regulations. Moreover, the data of students who provided consent for the secondary use of their data (Approval No. 11763) in another research approved in 2017 were included.
B. Sample Population
Students in the UTokyo Faculty of Medicine were asked if they were willing to participate in “A Study of the Educational Effectiveness of Online “Medical interviewing Practice” in the post-class reflection questionnaire of the “Online medical interview classes or the waiting period after the pre-CC OSCE. Out of 229 students (2021 and 2022), 87 students participated in this study. A summary of the annual participants is shown in Appendix 1. In early 2020 almost all the classes in UTokyo were stopped due to the COVID-19 pandemic, which made it difficult to contact students face-to-face and to obtain participants in the previous research (Approval No. 11763); and as this research started in 2021, it was practically difficult to obtain consent to participate in this study in 2020. In 2020 the online medical interview classes have just been launched, which significantly improved in 2021. Hence, we thought that it would be better to exclude the small participants of 2020 from the analysis to keep the validity of this study.
C. Details of Medical Interview Classes
Before 2019, the medical interview classes were performed as follows: Early in their fourth year, students joined classes introducing the outline of medical interview. A few days before the class, students watched an instructional video of a medical interview performed by the Common Achievement Tests Organization (CATO) (2005) in Japan. Afterward, students in a group of eight to nine faced the simulated patient in a classroom in the UTokyo and performed a medical interview roleplay. Thereafter, feedback about the technical factor of the medical interview as well as rapport status and nonverbal communications such as faces and gesture was provided by the students themselves, other students, simulated patients, and teachers. Since 2020, most face-to-face classrooms, including those in the present study, were closed because of the COVID-19 pandemic and were replaced with online classes. The present face-to-face class was also held online with the simulated patients and teachers using Zoom(R). Using the “Close-Up” function of Zoom(R), the simulated patient and student were faced with each other, whereas other participants (e.g., other students, other simulated patients, and the teacher) were not on the television (Appendix 2). After the roleplay was over, all students and the teacher came back on the television and provided feedback to the student, similar to face-to-face classes. Moreover, the class was recorded using the function of Zoom(R) and provided to students exclusively for review. After the class students reflected on the reflection sheet (until 2019) or the Learning Management System (from 2020) which was reviewed and commented on by teachers. The contents of the reflections were used for this study to investigate the impressions of the students.
D. Pre-CC OSCE and Computer-Based Test (CBT)
In Japan, medical students usually take the pre-CC OSCE in the fourth year, prior to the two-year CC course. Before 2022, the minimum assessment factors were medical interview, physical examinations (including head and neck, chest, abdomen, neurological examinations), basic clinical procedure, and basic life support. The examinations were administered by CATO. The evaluation criteria are not publicly available because of CATO policy. Two scores are used in the evaluation: global score (GS) which means the evaluation as a total performance and item-wise score (IS) which means scores by checklist. Before 2023, the borderline was set by each institute. At least one certified evaluator per area was responsible, and each evaluator was a faculty member. Moreover, CATO sent at least one external evaluator per area and an external supervisor. After each performance, each examinee was evaluated by two or three evaluators per room. The pre-CC OSCE is one of the examinations that students must pass to proceed to the CC course.
Aside from the pre-CC OSCE, students must also pass the CBT. The CBT corresponds to the assessment of medical knowledge prior to the CC (Horita et al., 2021). In 2023, the pre-CC OSCE and CBT have been made official, and students must pass both examinations before they can take the national board examination in Japan.
E. Data Analysis
The pre-CC OSCE scores were analysed using R, Rstudio, JMP version17.0 (SAS Institute, N.C., USA) and Microsoft Excel (Microsoft Corporation, W.A., USA). Non-paired T test, Mann-Whitney U test, and Steel-Dwass test were used respectively, for parametric or non-parametric comparisons.
III. RESULTS
A. Year-to-Year Comparison of the Pre-CC OSCE Results in the Medical Interview area and CBT Results
First, we compared the year-to-year results of the pre-CC OSCE in the medical interview area. Table 1 and Figure 1 shows a statistical summary of the pre-CC OSCE scores in 2022, 2021, 2019, and 2018. The results of non-parametric tests revealed that the p-values in the IS between 2022 and 2019, 2022 and 2018, and 2021 and 2018 were below 0.05, whereas no significant difference was observed in the GS.
|
Year |
IS/GS |
Average |
SD |
SE |
Bottom 95 |
Upper 95 |
|
2022 |
IS |
85.67 |
9.19 |
1.18 |
83.32 |
88.02 |
|
GS |
4.41 |
0.68 |
0.09 |
4.24 |
4.58 |
|
|
2021 |
IS |
82.69 |
9.71 |
1.90 |
78.77 |
86.61 |
|
GS |
4.62 |
0.75 |
0.15 |
4.31 |
4.92 |
|
|
2019 |
IS |
79.04 |
10.19 |
1.07 |
76.92 |
81.16 |
|
GS |
4.33 |
0.89 |
0.09 |
4.14 |
4.51 |
|
|
2018 |
IS |
73.63 |
9.94 |
1.10 |
71.43 |
75.83 |
|
GS |
4.26 |
0.79 |
0.09 |
4.09 |
4.44 |
Table 1. Averages of IS and GS of the medical interview area per the pre-CC OSCE implementation year. IS, item-wise score; GS, global score; SD, standard deviation; SE, standard error
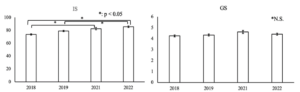
Figure 1. Average of IS and GS. The error bar shows standard error
|
Year |
Average |
SD |
SE |
Bottom 95 |
Upper 95 |
|
2022 |
566.62 |
121.03 |
15.50 |
535.63 |
597.62 |
|
2021 |
576.07 |
106.64 |
20.52 |
533.89 |
618.26 |
|
2019 |
565.02 |
119.91 |
12.71 |
539.76 |
590.28 |
|
2018 |
529.72 |
116.34 |
12.93 |
503.99 |
555.44 |
Table 2. Year-by-year score distribution of CBT (IRT score)
B. Comparison Before and After the Pandemic
The medical interview classes were held face-to-face before the pandemic (2018 and 2019) and online after the pandemic (2021 and 2022). We compared the results of pre-CC OSCE medical interview and CBT before and after the pandemic. A summary of the results is shown in Table 3 and Figure 2. The results of statistical analyses revealed a significant difference in the medical interview IS and CBT between the face-to-face group and the online group (p < 0.001 and 0.032 respectively). However, no significant difference in GS was observed.
|
|
Group |
Number |
Average |
SE |
Bottom 95 |
Upper 95 |
|
OSCE (medical interview) IS |
F-to-F |
164 |
76.18 |
0.79 |
74.62 |
77.74 |
|
online |
85 |
84.71 |
1.10 |
82.54 |
86.87 |
|
|
OSCE (medical interview) GS |
F-to-F |
164 |
4.28 |
0.06 |
4.15 |
4.40 |
|
online |
85 |
4.47 |
0.09 |
4.30 |
4.64 |
|
|
CBT (IRT score) |
F-to-F |
162 |
546.5 |
9.39 |
528.1 |
565.0 |
|
online |
86 |
569.7 |
12.9 |
544.3 |
595.1 |
Table 3. Comparison of pre-CC OSCE (IS and GS respectively) and CBT results between the face-to-face (F-to-F) group and the online group

Figure 2. Comparison of pre-CC OSCE (IS and GS respectively) and CBT results between the face-to-face (F-to-F) group and the online group. The error bar shows standard error.
IV. DISCUSSION
We found no significant negative effects in some of the important educational outcomes in medical students’ scores of the medical interview due to online education caused by the COVID-19 pandemic. The quality of the medical interview after the emergence of the pandemic was no less than that before the pandemic. The same could be said for other indicators, including the CBT and other areas of the OSCE (data not shown).
One of the reasons why the scores of the online classes were not inferior to those of face-to-face classes might be because of the availability of each student to review the video recordings. We provided each student with a recording of their own performance in the class for self-review, which was not always provided in face-to-face classes. We also provided students with feedback from the teacher and other students during online classes. This is consistent with the findings of a previous study, which found that video reviewing of the OSCE performance is effective (Mookherjee et al., 2019). Moreover, the students accepted online classes well, and their motivation for learning was not affected despite the lack of face-to-face communication with simulated patients. During the reflection, some students noted that “I learned a lot in this class, though the class was held online” and that “I thought that online classes are not so bad” (data not shown). There were almost no complaints regarding online classes. We guess that in the environment that the face-to-face classes were restricted and the students experienced suspended classes the students felt satisfied for joining the classes even online. Further investigation will be needed regarding this point.
Recently, Khamees et al. (2022) pointed out the lack of control groups and poor transferability in numerous publications due to singularity of institution, department, and program. In the present study, the marks of students on high-stakes examinations before the pandemic were used as a comparison between face-to-face and online classes. Some studies have revealed that there are no significant differences in educational outcomes between face-to-face and online classes in basic medicine (Omole et al., 2023), and pharmacological education (Aoe et al., 2023). However, when it comes to high-stakes examinations, it remains unclear whether online education is not inferior to face-to-face education. Saad et al (2023) have showed that in some areas (clinical reasoning and history taking) of pre-clinical OSCE, students showed no less than comparable results, arguing that these skills are amenable to online learning in a medical school in Australia. Their results in some areas like medical interview in Japanese OSCE support our results. However, in their study, it is not clear about the details of the OSCE assessment, whether the assessment is by item-wise or global. In recent years, the pre-CC OSCE results have been recognized as an important educational outcome also for educational institutions (Hirsh et al., 2012). Our result, the educational outcome in the high-stakes examination, can be considered to fall in the top tier, the result, in the Kirkpatrick’s four-level model (Kirkpatrick, 1996). Moreover, our research is unique and important as few studies have directly compared the educational outcomes between face-to-face classes and online classes in high-stakes examination.
In Japan, the Medical Practitioners Act was revised in 2023, allowing medical students to perform some medical procedures under the supervision of a teaching physician after passing the pre-CC OSCE and CBT. This change also made the pre-CC OSCE a requirement for the national board examination. Hence, the pre-CC OSCE in Japan has become even more important, as much the responsibility for the education even greater. Our results show that online classes can contribute to the practice of “Medical interviews”.
It must be noted that online classes are not a complete alternative to face-to-face classes. Many studies have indicated that online education has some negative aspects (e.g., the need for infrastructure and devices, high cost, lack of personal interaction, etc.) (Arja et al., 2022; Mortazavi et al., 2021; Shaiba et al., 2023). One of the most significant elements that are difficult to teach in online classes is nonverbal communication. However, as Ishikawa et al. (2010) reported, although students are capable of understanding nonverbal communication despite struggling to change their performance through educational intervention, it is well recognized that nonverbal communication is difficult to teach even in face-to-face classes. Additionally, when it comes to procedural skills such as venipuncture, the educational outcomes in the online learning group were inferior to that of face-to-face learning group and students also felt that they were not taught satisfactorily (Dost et al., 2020; Saad et al., 2023). We should keep in mind that online education does not fully replace face-to-face education.
We saw a lack of significant differences in GS, both in year-by-year comparison and comparison between face-to-face and online groups. Although the tasks allocated to each university by CATO differ every year, the checkpoints are essentially common in quite a few areas; so, a comparison was made for both year by year and before and after the pandemic. GS usually reflects holistic assessment, which is difficult to produce results via technical education, whereas it might be easier for learners and teachers to deal with item-wise assessment (Govaerts et al., 2011; Jonsson & Svingby, 2007; Sadler, 2009). Moreover, in online classes, we used a checklist of the students’ performance (not shown to the students, but comments were given according to the checklist), which might have contributed to the improvement of IS. As to CBT, it is standardized by the accumulated examinations and the Item Response Theory and is assessed basically by knowledge base. The educational strategies that mainly should impact on the assessment of CBT, based on the lecture, have not changed before and after the pandemic, in the face-to-face classes or online classes. During the pandemic, the extra-curricular activities of the students were restricted, and several articles argue that self-studying time of the students increased (Barton et al., 2021; Guluma & Brandl, 2023). These might have contributed to the smaller elevation of CBT-IRT than the IS of pre-CC OSCE.
We need to take into consideration the confounding of several factors such as the curriculum changes, instructor training, student characteristics and students’ self-study time. While online classes have been a change in the curriculum, the rest remains unchanged. The instructors and students needed to become familiar with online classes, but there was no change in the educational goals of the class itself. Additionally, in the first year of the pandemic in 2020, we were unable to get enough data and the online class itself was implemented as “being built”. By 2021 and 2022, the class was almost stable. However, getting used to online classes of the instructors and students could be a confounding factor. The class tool (Zoom®) was continuously improved, which might be a minor confounding factor. Additionally, the students might have had excellent ITC skills, which might also be a confounding factor.
Some frameworks describing the evidence of online medical education outcome might contribute to generalizing our results (Martinengo et al., 2024; McGee et al., 2024; Wilcha, 2020). Needless to say, there are confrontations regarding the limitations of these generalizations, pointing out the context-depending factors, high heterogeneity among studies and “The Covid-19 Effects” (Abdull Mutalib et al., 2022; Liu et al., 2016; Martinengo et al., 2024; McGee et al., 2024). However, these frameworks will be applicable in generalizing our results; although there are some potential confounding factors such as the students, the instructors, the educational resources and the “pandemic era” itself, the online medical interview education could be an effective educational curriculum for educating medical interview skills as well as some interpersonal skills.
A. Limitations
One of the limitations of this study is that it was performed in a single institution. Hence, the generalizability of this study may be lower than that of multi-institutional studies. However, not much variation exists in the nature of students and in the educational curriculum they experience. Of course, to make the evidence more robust and further validate, multi-centred or multi-institutional studies are still needed. At the same time, these factors should not be too disparate as it is very difficult to find a suitable population for these factors. In this regard, our participants and classes can be considered as a reasonable population.
Another limitation of this study is the number of participants. In 2020, we could not obtain enough participants because of the pandemic. After the pandemic, our students and staff shifted to online classes, and the number of face-to-face classes decreased. In 2021 and 2022, we decided to obtain consent for participation in this study in the waiting time after face-to-face OSCE examination as it was difficult to obtain consent only during online classes. In this context, the participants may have a positive view of various aspects of student life including studies, which may be a potential bias of sample population. Additionally, the waiting time after the OSCE examination was short for some students, which might have made it difficult to think about understanding the concept of this research and whether consent should be given.
In this study, qualitative analyses investigating if the students were positive about the classes are limited to some extent. During the pandemic, the psychological situation and the learning behaviour of the students might have differed from that of before the pandemic. To investigate this aspect, qualitative studies will be needed.
Moreover, the evaluation criteria of the pre-CC OSCE are not open to the public due to CATO policy. This probably leads to a lack of transparency of the evaluation, causing another limitation of this study. However, Japanese OSCE evaluation criteria is similar to CANMED’s OSCE checklist (Kassam et al., 2016), which will support the validity of the results of Japanese OSCE and our results.
Finally, this study retrospectively compared the educational effect between students before and after the pandemic, which may limit the causal inferences of educational outcome effects of face-to-face versus online in medical interview OSCE. A randomized controlled trial will be needed to verify the results obtained in this study.
V. CONCLUSION
Because of the COVID-19 pandemic, we were forced to change our medical interview classes from face-to-face to be online. However, in high-stakes examinations such as the pre-CC OSCE and CBT, the results of the online group were not inferior to those of the face-to-face group. We consider this result extremely important because we directly compared the educational outcomes of high-stakes examinations between online and face-to-face groups who took the same medical interview classes, and because this evaluation falls in the top level of Kirkpatrick’s model. Our results suggest that online education provides a viable option in teaching interpersonal skills and support the integration of online medical interview training into preclinical curricula, particularly in resource-constrained settings. Randomized controlled trials and multi-institutional studies are needed to further validate our results.
Notes on Contributors
SH and ME conducted the whole research.
SH, MI, SK, JM, HM, and ME performed the classes and collected the data.
SH performed data analyses.
SH, MI, SK, JM, HM, and ME contributed to writing the manuscript.
Ethical Approval
This study was approved by the ethics committee of the UTokyo Faculty of Medicine (Approval No. 2021005NI). All methods were performed in accordance with the relevant guidelines and regulations. Moreover, the data of students who provided consent to the secondary use of their data in another research, given by the ethics committee of the UTokyo Faculty of Medicine (Approval No. 11763), were included.
Data Availability
The data in this study are not publicly available because of confidentiality agreements with the participants, conditions obligating CATO, and confidential nature of the data.
Acknowledgement
We thank the students of the UTokyo Medical School who participated in this study. We also thank the UTokyo Staff for their cooperation.
Funding
This study was funded by JSPS KAKENHI Grant Number 24K06092 and ACRO incubation grants of Teikyo University.
Declaration of Interest
The authors have no potential conflicts to disclose.
References
Abdull Mutalib, A. A., Md. Akim, A., & Jaafar, M. H. (2022). A systematic review of health sciences students’ online learning during the COVID-19 pandemic. BMC Medical Education, 22(1), 524. https://doi.org/10.1186/s12909-022-03579-1
Alshaibani, T., Almarabheh, A., Jaradat, A., & Deifalla, A. (2023). Comparing online and face-to-face performance in scientific courses: A retrospective comparative gender study of Year-1 students. Advances in Medical Education and Practice, 14, 1119–1127. https://doi.org/10.2147/amep.s408791
American Medical Association. (2016, June 15). AMA encourages telemedicine training for medical students, residents. AMA Press Releases.
Aoe, M., Esaki, S., Ikejiri, M., Ito, T., Nagai, K., Hatsuda, Y., Hirokawa, Y., Yasuhara, T., Kenzaka, T., & Nishinaka, T. (2023). Impact of different attitudes toward face-to-face and online classes on learning outcomes in Japan. Pharmacy, 11(1), 16. https://doi.org/10.3390/pharmacy11010016
Arja, S. B., Fatteh, S., Nandennagari, S., Pemma, S. S. K., Ponnusamy, K., & Arja, S. B. (2022). Is emergency remote (online) teaching in the first two years of medical school during the COVID-19 pandemic serving the purpose? Advances in Medical Education and Practice, 13, 199–211. https://doi.org/10.2147/amep.s352599
Barton, J., Rallis, K. S., Corrigan, A. E., Hubbard, E., Round, A., Portone, G., Kuri, A., Tran, T., Phuah, Y. Z., Knight, K., & Round, J. (2021). Medical students’ pattern of self-directed learning prior to and during the coronavirus disease 2019 pandemic period and its implications for Free Open Access Meducation within the United Kingdom. Journal of Educational Evaluation for Health Professions, 18, 5. https://doi.org/10.3352/jeehp.2021.18.5
Bastos, R. A., Carvalho, D. R. D. S., Brandão, C. F. S., Bergamasco, E. C., Sandars, J., & Cecilio-Fernandes, D. (2021). Solutions, enablers and barriers to online learning in clinical medical education during the first year of the COVID-19 pandemic: A rapid review. Medical Teacher, 44(2), 187–195. https://doi.org/10.1080/0142159x.2021.1973979
Basuodan, R. (2024). Comparisons of the academic performance of Medical and Health-Sciences students related to three learning methods: A cross-sectional study. Advances in Medical Education and Practice, 15, 1339–1347. https://doi.org/10.2147/amep.s493782
Budakoğlu, I. İ., Sayılır, M. Ü., Kıyak, Y. S., Coşkun, Ö., & Kula, S. (2021). Telemedicine curriculum in undergraduate medical education: a systematic search and review. Health and Technology, 11(4), 773–781. https://doi.org/10.1007/s12553-021-00559-1
Common Achievement Tests Organization (CATO). (2005). Common Achievement Tests Organization. https://www.cato.or.jp/index.html
Crawford, J., Butler-Henderson, K., Rudolph, J., Malkawi, B., Glowatz, M., Burton, R., Magni, P. A., & Lam, S. (2020). COVID-19: 20 countries’ higher education intra-period digital pedagogy responses. Journal of Applied Learning & Teaching, 3(1). https://doi.org/10.37074/jalt.2020.3.1.7
Daniel, M., Gordon, M., Patricio, M., Hider, A., Pawlik, C., Bhagdev, R., Ahmad, S., Alston, S., Park, S., Pawlikowska, T., Rees, E., Doyle, A. J., Pammi, M., Thammasitboon, S., Haas, M., Peterson, W., Lew, M., Khamees, D., Spadafore, M., … Stojan, J. (2021). An update on developments in medical education in response to the COVID-19 pandemic: A BEME scoping review: BEME Guide No. 64. Medical Teacher, 43(3), 253–271. https://doi.org/10.1080/0142159x.2020.1864310
Dost, S., Hossain, A., Shehab, M., Abdelwahed, A., & Al-Nusair, L. (2020). Perceptions of medical students towards online teaching during the COVID-19 pandemic: A national cross-sectional survey of 2721 UK medical students. BMJ Open, 10(11), e042378. https://doi.org/10.1136/bmjopen-2020-042378
Gordon, M., Patricio, M., Horne, L., Muston, A., Alston, S. R., Pammi, M., Thammasitboon, S., Park, S., Pawlikowska, T., Rees, E. L., Doyle, A. J., & Daniel, M. (2020). Developments in medical education in response to the COVID-19 pandemic: A rapid BEME systematic review: BEME Guide No. 63. Medical Teacher, 42(11), 1202–1215. https://doi.org/10.1080/0142159x.2020.1807484
Govaerts, M. J. B., Schuwirth, L. W. T., Van Der Vleuten, C. P. M., & Muijtjens, A. M. M. (2010). Workplace-based assessment: Effects of rater expertise. Advances in Health Sciences Education, 16(2), 151–165. https://doi.org/10.1007/s10459-010-9250-7
Guetterman, T. C., Sakakibara, R., Baireddy, S., Kron, F. W., Scerbo, M. W., Cleary, J. F., & Fetters, M. D. (2019). Medical students’ experiences and outcomes using a virtual human simulation to improve communication skills: Mixed methods study. Journal of Medical Internet Research, 21(11), e15459. https://doi.org/10.2196/15459
Guluma, K. Z., & Brandl, K. (2022). Virtual learning allows for adaptation of study strategies in a cohort of U.S. medical students. Medical Teacher, 45(1), 89–96. https://doi.org/10.1080/0142159x.2022.2105690
Hammersley, V., Donaghy, E., Parker, R., McNeilly, H., Atherton, H., Bikker, A., Campbell, J., & McKinstry, B. (2019). Comparing the content and quality of video, telephone, and face-to-face consultations: A non-randomised, quasi-experimental, exploratory study in UK primary care. British Journal of General Practice, 69(686), e595–e604. https://doi.org/10.3399/bjgp19x704573
Harden, R. M., Stevenson, M., Downie, W. W., & Wilson, G. M. (1975). Assessment of clinical competence using objective structured examination. BMJ, 1(5955), 447–451. https://doi.org/10.1136/bmj.1.5955.447
Hirsh, D., Gaufberg, E., Ogur, B., Cohen, P., Krupat, E., Cox, M., Pelletier, S., & Bor, D. (2012). Educational outcomes of the Harvard Medical School–Cambridge integrated clerkship. Academic Medicine, 87(5), 643–650. https://doi.org/10.1097/acm.0b013e31824d9821
Horita, S., Park, Y., Son, D., & Eto, M. (2021). Computer-based test (CBT) and OSCE scores predict residency matching and National Board assessment results in Japan. BMC Medical Education, 21(1). https://doi.org/10.1186/s12909-021-02520-2
Ishikawa, H., Hashimoto, H., Kinoshita, M., & Yano, E. (2010). Can nonverbal communication skills be taught? Medical Teacher, 32(10), 860–863. https://doi.org/10.3109/01421591003728211
Jonsson, A., & Svingby, G. (2007). The use of scoring rubrics: Reliability, validity, and educational consequences. Educational Research Review, 2(2), 130–144. https://doi.org/10.1016/j.edurev.2007.05.002
Kassam, A., Cowan, M., & Donnon, T. (2016). An objective structured clinical exam to measure intrinsic CanMEDS roles. Medical Education Online, 21(1), 31085. https://doi.org/10.3402/meo.v21.31085
Khamees, D., Peterson, W., Patricio, M., Pawlikowska, T., Commissaris, C., Austin, A., Davis, M., Spadafore, M., Griffith, M., Hider, A., Pawlik, C., Stojan, J., Grafton-Clarke, C., Uraiby, H., Thammasitboon, S., Gordon, M., & Daniel, M. (2022). Remote learning developments in postgraduate medical education in response to the COVID-19 pandemic: A BEME systematic review: BEME Guide No. 71. Medical Teacher, 44(5), 466–485. https://doi.org/10.1080/0142159x.2022.2040732
Kirkpatrick, D. (1996). Great ideas revisited. Techniques for evaluating training programs. Revisiting Kirkpatrick’s Four-Level model. Training & Development, 50(1), 54–59. https://eric.ed.gov/?id=EJ515660
Liu, Q., Peng, W., Zhang, F., Hu, R., Li, Y., & Yan, W. (2016). The effectiveness of blended learning in health professions: Systematic review and meta-analysis. Journal of Medical Internet Research, 18(1), e2. https://doi.org/10.2196/jmir.4807
Martinengo, L., Ng, M. S. P., De Rong Ng, T., Ang, Y., Jabir, A. I., Kyaw, B. M., & Car, L. T. (2024). Spaced digital education for health professionals: A systematic review and meta-analysis (Preprint). Journal of Medical Internet Research, 26, e57760. https://doi.org/10.2196/57760
McGee, R. G., Wark, S., Mwangi, F., Drovandi, A., Alele, F., & Malau-Aduli, B. S. (2024). Digital learning of clinical skills and its impact on medical students’ academic performance: A systematic review. BMC Medical Education, 24(1). https://doi.org/10.1186/s12909-024-06471-2
Mookherjee, S., Strujik, J., Cunningham, M., Kaplan, E., & Çoruh, B. (2018). Independent and mentored video review of OSCEs. The Clinical Teacher, 16(1), 23–29. https://doi.org/10.1111/tct.12755
Mortazavi, F., Salehabadi, R., Sharifzadeh, M., & Ghardashi, F. (2021). Students’ perspectives on the virtual teaching challenges in the COVID-19 pandemic. Journal of Education and Health Promotion, 10(1), 59. https://doi.org/10.4103/jehp.jehp_861_20
Omole, A. E., Villamil, M. E., & Amiralli, H. (2023). Medical education during COVID-19 pandemic: A comparative effectiveness study of face-to-face traditional learning versus online digital education of basic sciences for medical students. Cureus. https://doi.org/10.7759/cureus.35837
Saad, S., Richmond, C., King, D., Jones, C., & Malau-Aduli, B. (2023). The impact of pandemic disruptions on clinical skills learning for pre-clinical medical students: Implications for future educational designs. BMC Medical Education, 23(1). https://doi.org/10.1186/s12909-023-04351-9
Sadler, D. R. (2008). Indeterminacy in the use of preset criteria for assessment and grading. Assessment & Evaluation in Higher Education, 34(2), 159–179. https://doi.org/10.1080/02602930801956059
Shaiba, H., John, M., & Meshoul, S. (2022). Female Saudi College students’ e-learning experience amidst COVID-19 pandemic: An investigation and analysis. Heliyon, 9(1), e12768. https://doi.org/10.1016/j.heliyon.2022.e12768
Wilcha, R. (2020). Effectiveness of virtual medical teaching during the COVID-19 Crisis: Systematic review. JMIR Medical Education, 6(2), e20963. https://doi.org/10.2196/20963
Zaccariah, Z. R., Irvine, A. W., & Lefroy, J. E. (2022). Feasibility study of student telehealth interviews. The Clinical Teacher, 19(4), 308–315. https://doi.org/10.1111/tct.13490
*Shoko Horita
2-11-1, Kaga, Itabashi-ku,
Tokyo 173-8605, Japan
Email: horitas-tky@umin.ac.jp
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









