Impact of Scholarly Project on students’ perception of research skills: A quasi-experimental study
Submitted: 22 January 2022
Accepted: 4 May 2022
Published online: 4 October, TAPS 2022, 7(4), 50-58
https://doi.org/10.29060/TAPS.2022-7-4/OA2748
Nguyen Tran Minh Duc, Khuu Hoang Viet & Vuong Thi Ngoc Lan
University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
Abstract
Introduction: The Scholarly Project provides medical students with an opportunity to conduct research on a health and health care topic of interest with faculty mentors. Despite the proven benefits of the Scholarly Project there has only been a gradual change to undergraduate medical education in Vietnam. In the academic year of 2020-2021, the University of Medicine and Pharmacy (UMP) at Ho Chi Minh City launched the Scholarly Project as part of an innovative educational program. This study investigated the impact of the Scholarly Project on the research skills perception of participating undergraduate medical students.
Methods: A questionnaire evaluating the perception of fourteen research skills was given to participants in the first week, at midterm, and after finishing the Scholarly Project; students assessed their level on each skill using a 5-point Likert scale from 1 (lowest score) to 5 (highest score).
Results: There were statistically significant increases in scores for 11 skills after participation in the Scholarly Project. Of the remaining three skills, ‘Understanding the importance of “controls”’ and ‘Interpreting data’ skills showed a trend towards improvement while the ‘Statistically analyse data’ skill showed a downward trend.
Conclusion: The Scholarly Project had a positive impact on each student’s perception of most research skills and should be integrated into the revamped undergraduate medical education program at UMP, with detailed instruction on targeted skills for choosing the optimal study design and follow-up assessment.
Keywords: Study Skills, Scholarly Project, Undergraduate, Medical Education, Self-Assessment
Practice Highlights
- The Scholarly Project is an essential component of the undergraduate medical education curriculum.
- Targeted researching skills is a valuable method to optimise competency-based criteria.
- The initial choice of study design is important to the overall research skill self-perceptive improvement.
I. INTRODUCTION
Scholarly Project has emerged as an essential component of the modern undergraduate medical curriculum. This entails mentored study in a single topic area and may include classical hypothesis-driven research, literature reviews, or the creation of a medically-related product (Boninger et al., 2010). By researching a topic, designing and implementing experiments and analysing the results, students not only gain knowledge and experience but also essential skills including critical thinking, time management, collaboration, information technology and confidence, all of which benefit their academic endeavours and result in higher undergraduate graduation rates (Bickford et al., 2020; Carson, 2007). Furthermore, the Scholarly Project program, which allows students to learn about research, was rated positively by most undergraduates. In addition, it provides faculty members with assistance in their research projects and the chance to influence future generations (Dagher et al., 2016). It has also been noted that the process of exposing undergraduate students to research benefits the researchers who take part as instructors by refining and shaping their scientific minds (Zydney et al., 2002).
The number of research studies with Vietnamese authorship published in ISI-indexed journals increased considerably between 2001 and 2015, with an annual growth rate of 17%. However, the majority of this growth (77%) was accounted for by international collaboration research rather than domestic-only projects, especially in the clinical medicine area. Thus, scientific research in Vietnam had not changed considerably or achieved independence in this field (Nguyen et al., 2016).
In the academic year of 2020-2021, the University of Medicine and Pharmacy at Ho Chi Minh City (UMP), Vietnam, pioneered the launch of a one-year Scholarly Project for all fifth-year medical students. This medical student population is the first generation to learn under the refreshed Undergraduate Medical Curriculum of the UMP and the first class to experience the Scholarly Project. Undergraduate research experiences are characterised by four features: mentorship, originality, acceptability, and dissemination (Kardash, 2000). Assessment of undergraduate research experience, which determines whether students gained any research skills (such as identifying the research question, collecting data, thinking independently and creatively) is best performed after completing the research program (Blockus et al., 1997; Manduca, 1997). The quasi-experimental work presented here provides one of the first investigations into how the Scholarly Project at the UMP, Vietnam, impacted on the participating students’ perception of how their medical research skills improved in the academic year of 2020-2021.
II. METHODS
A. Description of the Scholarly Project
The Scholarly Project is a compulsory academic module that aims to enable fifth-year medical students to conduct medical research early in their careers. It provides these students with an active experience in conducting a research project with faculty members starting at the beginning of the fifth academic year. The data reported here were collected from medical students and mentors who participated during the 2020-2021 academic year.
For most medical students, the Scholarly Project provides the first exposure to the field of research. There are 48 groups of nine medical students, including one team leader, one secretary, and team members, with one faculty mentor. Medical students are expected to contribute actively to the best of their ability in committed teamwork and an ethical manner.
Members of the faculties of Medicine and Public Medicine who have active ongoing research projects are eligible to participate in the Scholarly Project. Faculty members act as mentors to the students and facilitate the students’ learning process by providing supervision, guidance, and support. In addition, members should allocate suitable tasks for each student based on their skills, expertise, interests, and background.
B. Scholarly Project Steps
1) Student orientation: Student orientation occurred in the first week, informing students of the program’s procedure, and their roles and responsibilities (Figure 1). Also, in the first week, the medical student curriculum included a medical research course, describing the formation of research ideas, study design and statistics, literature searching and referencing, and research ethics. Students were also provided with important dates and deadlines for the Scholarly Project stage.
2) Matching: Matching is the process of pairing students with project mentors. From the first weeks of the Scholarly Project, each student team is required to create a team profile on the university website, including the scientific interest, skill, and research fields of interest for each team member. Each medical student team then chose a mentor from a provided list, taking into account medical research fields and their research curriculum vitae. Each team picked up to 2 mentors, in order of preference. After the deadline, mentors chose which team they would like to work with based on the students’ choice; this process continued until all teams were paired.
3) Work initiation: Students were expected to initiate contact with the faculty member after being notified via the university website that they have been matched to a project. During the second week of the Scholarly Project, faculty members and students discussed the research project, and the roles and responsibilities. Upon finalising the agreement between the two parties, students completed a meeting report form, which was signed by both the mentor(s) and the team leader. During online learning periods due to COVID-19, online meetings were encouraged, along with completion of the meeting report form. This meeting report form included information about topics discussed during the meeting, future work, each student’s role in the research project, and confirmed the next appointment date. Student teams and faculty members scheduled meetings based on the design of their study. In follow-up meetings, faculty mentors continued to discuss and evaluate the medical students’ work, and further plans were discussed. There was no upper limit for the number of meetings. However, there was a second required meeting at the third week of the Scholarly Project, which was nearly the end of the modules, for the research team to update the collected data, trouble-shooting solutions, or feedback.
4) Presentation: In the final week of the fifth-year curriculum, a Scholarly Project Symposium provided the opportunity for research teams to present their project findings. This allowed the scientific committee to evaluate both the performance of each student and the research project in general. Another aim of the symposium was for medical students to learn and share their findings with other teams, and the presentation also provides a valuable reference for the subsequent classes.
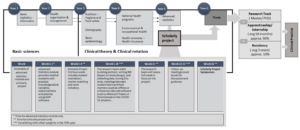
Figure 1. Integration of the Scholarly Project into the new reformed undergraduate and postgraduate medical curriculum in Vietnam.
C. Study Setting and Participants
This one-group pretest-posttest study had a quasi-experimental design. Research skills assessed were chosen based on fourteen individual research skills (Kardash, 2000). The questionnaire has been used previously, with a Cronbach’s alpha calculated at 0.9 and item-total correlation varied between 0.49 to 0.76 (Kardash, 2000). The questionnaire was translated into Vietnamese, then the local language version was pre-tested and the final text was amended as necessary. The translation process was undertaken in accordance with Guidelines for the Cross-Cultural Adaptation Process (Beaton et al., 2000). Translations were evaluated and compared with the original questionnaire by the Education and Research Council of the UMP to ensure accuracy of the Vietnamese version prior to study initiation. Medical student surveys were administered during the first week of the Scholarly Project and students were asked to indicate their current level of performance for each skill and the extent to which they hoped that the project would develop each skill on a 5-point Likert scale from 1–5 (where higher scores indicate greater skill level). Surveys were repeated at midterm and during the last week of the Scholarly Project module; at these times the students used the same scale to rate the extent to which they felt capable of performing each skill and how they believed the internship had developed their skills in general. Medical students had to provide informed consent on the first page of the electronic form before accessing the rest of the questionnaire.
D. Statistical Analysis
Raw data were extracted from the online survey link for each participating medical student and saved in Excel sheets. R (R Core Team, Vienna, Austria) was applied to analyse data. First, scores for each skill at baseline were compared with those obtained after project completion using a paired t-test (Student’s t-test). The same method was used to compare expected skill level evaluated at baseline and the actual skill level rating at the end of the Scholarly Project. A p-value of <0.05 was considered to be statistically significant.
III. RESULTS
A. Response Rate and Participant Data
Of 384 students participating in the Scholarly Project, 194 (50.5%) completed the survey. The majority of participants were male (60%) and had the role of project team member (75.3%) (See Table 1). The most common Scholarly Project design was a cross-sectional study (47.9%), followed by study protocol development (21.1%), case/case series report (11.9%), and literature review (10.3%) (Table 1). Twenty-one different departments with a wide range of specialties provided scientific mentors for the Scholarly Projects undertaken by 48 research groups (See Table 1).
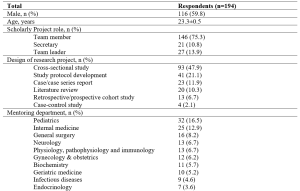
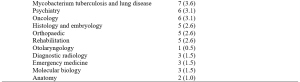
Table 1. Demographic and project characteristics for survey respondents.
Values are mean ± standard deviation, or number of respondents (%).
B. Research Skills at Baseline, Midterm and Project Completion
At baseline, self-rated competency was highest for ‘Understand the importance of “controls”’, ‘Understand contemporary concepts’, ‘Identify a specific question’, and ‘Observe and collect data’ (Figure 2). All skills had self-evaluating levels above “moderate” (score of >3), except for ‘Write research for publication’ (mean score 2.696). Students expected that all skills would increase after participating in the Scholarly Project (p<0.001).
In the midterm survey, five skill groups showed significant improvement from baseline (Figure 2). These were ‘Make use of scientific literature’, ‘Identify a specific question’, ‘Observe and collect data’, ‘Relate results to the “bigger picture”’, and ‘Orally communicate research project skills’. Conversely, there was a significant decrease in self-rated skill for ‘Statistically analyse data’ and ‘Interpret data skills’, while other skill ratings were stable (Figure 2).
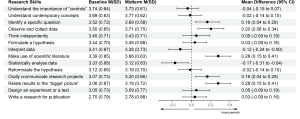
Figure 2. Change in self-rated medical research skills of 194 participants from baseline to the midterm of the Scholarly Project
M: mean; SD: standard deviation; CI: confidence interval
At the completion of the Scholarly Project, the five skills that showed improvement at the midterm assessment showed continued improvement, and another six skills had also improved significantly compared with baseline (Figure 3). However, scores for ‘Understand the importance of “controls”’, ‘Interpret data’ and ‘Statistically analyse data” did not change significantly from baseline, and the mean score for the latter parameter was actually slightly below baseline (Figure 3).
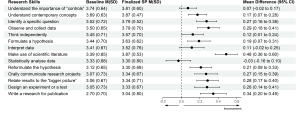
Figure 3. Change in self-rated medical research skills of 194 participants from baseline to completion of the Scholarly Project (SP)
M: mean; SD: standard deviation; CI: confidence interval.
Looking more closely at analytical skills relating to six types of study design showed that self-rated skill for the ability to interpret data for a literature review decreased significantly, as did self-rated skill scores for statistically analyse data in relation to study protocol development and literature review (Table 2). In contrast, there was a significant improvement in self-rated skill for data interpretation for cross-sectional studies and for statistical analysis of data in cohort studies (Table 2).
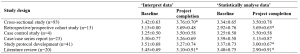
Table 2. Self-evaluated skill level scores for ‘Interpret data’ and ‘Statistically analyse data’ from baseline to completion of the Scholarly Project
Values are mean ± standard deviation. *p<0.05 vs baseline.
IV. DISCUSSION
A. Impact of Scholarly Project on Students’ Perception of Research Skills
Our results show that ratings for most skills increased during and after the Scholarly Project. Increases in ratings for ‘Identifying a specific question’, ‘Orally communicate research projects’, and ‘Relate results to the “bigger picture”’ in our study were consistent with data from Schor et al. (2005), who reported that the Scholarly Project could be beneficial by fostering analytical thinking skills, improving oral communication skills, and enhancing skills for evaluating and applying new knowledge to their profession (Schor et al., 2005). A significant increase in ‘Make use of scientific literature’ in our study reflects the idea-forming process at the study design stage of the Scholarly Project, during which students could practice the ability to read and critically evaluate medical literature. These are essential components of undergraduate medical education, irrespective of whether students intend to pursue a career in academic medicine or in public or private clinical practice (Holloway et al., 2004).
B. Data-related Skills and the Concept of a Control Group
The two skills of ‘Statistically analyse data’ and ‘Interpret data’ are introduced mainly in the Advanced Statistics Module with a training period of 2 weeks before starting the Scholarly Project, and briefly presented in the ‘Basic statistics informatics’ module during the first year of training and in the ‘Basic epidemiology’ module during the third year of the undergraduate curriculum. Therefore, baseline assessments in our study took place after the Advanced Statistics Module, which could have influenced ratings on the above skills. Given that our midterm assessment was performed at a time when most students had not had the opportunity to practice these skills, there may have been a negative impact on self-evaluation. The change in scores for ‘Statistically analyse data’ and ‘Interpret data’ at the midterm assessment was therefore influenced by an external factor (the Advanced Statistics Module) and an internal factor (the Scholarly Project). Therefore, future assessments of the impact of the Scholarly Project on learning should not have the quasi-experimental design used here, but instead, use an interrupted time-series design. This will mean that several surveys would be conducted before starting the Advanced Statistics Module, with the aim of eliminating confounding factors.
The final assessment showed significant improvements in scores for ‘Statistically analyse data’ and ‘Interpret data skills’ compared with the midterm survey. When applied in students’ projects, the improvement of these two skills indirectly supported the aforementioned context. This highlights the value of active learning compared with passive learning. It has conclusively been shown that cramming statistical knowledge means that students do not understand basic concepts to apply appropriately (Leppink, 2017). As noted by Leppink, statistics should be integrated into medical subjects; familiarity with these subjects and the repeated use of these skills provides opportunities to develop statistical skills. The Scholar Project is a typical example of this trend. However, only the ‘Statistically analyse data skill’ showed a downward pattern, while the ‘Interpret data skill’ increased slightly, suggesting that the Scholarly Project should focus more on these skills. Additional studies that take these variables into account are needed.
The control group concept is taught in Basic Epidemiology during the third year of Basic Science and the first sessions of the Scholarly Project. The control group has a pivotal role in study design should have elements that match the experimental group’s characteristics, except for the intervention/variable applied to the latter (Kinser & Robins, 2013). This scientific control group enables the experimental study of one variable at a time, and it is an essential part of the scientific method. Two identical experiments are carried out in a controlled experiment: in one of them, the treatment or tested factor is applied (experimental group), whereas in the other group (control), the tested factor is not applied (Pithon, 2013). However, due to the limitation that only four respondents had a project with a case-control study design, the ‘Understand the importance of “controls”’ skill only showed a modest improvement, despite having been taught previously, which is similar to a previous undergraduate research study (Kardash, 2000). Compared with cross-sectional study design, which was the most popular design for studies in this Scholarly Project, case-control studies often required a greater amount of human and facility resources. We suggest that a case-control study with a small sample size of 10–20 could be a suitable study design for medical students to understand how best to conduct research with a control group.
Of the 194 respondents in our study, 56.7% of the cohort should have been able to fully experience all fourteen of the skills assessed. In contrast, those who participated in study protocol development, literature review, and case/case series report projects had limited opportunities to practice analytical skills. Similar to our findings, a previous study demonstrated that only 13% of 475 projects conducted by medical students contained four main research skill areas, including research methods, information gathering, critical analysis and review, and data processing (Murdoch-Eaton et al., 2010). Furthermore, the COVID-19 outbreak during the academic year 2020-2021 significantly impacted the originally planned Scholarly Project data collection process. As a result, some research teams switched to more feasible design studies such as study development or literature review, which potentially influenced the two skills of statistical analysis and data interpretation skills. Therefore, it could be hypothesised that these conditions are less likely to occur if participants recognise the skills required for research before designing the study protocol. Thus, there is room for further progress in determining the optimal project descriptions provided to medical students participating in the Scholarly Project to allow them to benefit from the research opportunities and fully develop essential skills.
C. The Role of Scholarly Project in Medical Education in Vietnam
This Scholarly Project is an essential step in curriculum reform for Vietnam’s medical education system. In the last two decades, medical educators in Vietnam have collaborated to promote the social trend for undergraduate medical education, and identify the goals and outcomes of learning from medical graduates in expected knowledge, attitudes, and skills (Hoat et al., 2009). Furthermore, Vietnamese policymakers created an environment that enabled academic innovation by implementing the necessary changes to national university autonomy policies (Duong et al., 2021). These policies enable public universities to be financially independent, manage their operation and human resources, prioritise technology, and develop new curricula. The Scholarly Project helps to train physicians who are better prepared to meet patient requirements and health needs (Fan et al., 2012). Based on competency in medical education, the Scholarly Project focuses on outcomes, emphasises the application of knowledge and practice, and promotes greater learner-centeredness (Carraccio et al., 2002; Frank et al., 2010; Iobst et al., 2010). In addition, the Scholarly Project helps to reduce the time spent in passive lectures, which can negative affect medical students (Deslauriers et al., 2019; Schwartzstein et al., 2020; Schwartzstein & Roberts, 2017). Instead, students are encouraged to explore research topics based on their interests, human and institutional resources, and university mentors’ guidance and follow-up. Compared with the large class sizes from Vietnam’s traditional teaching method, the Scholarly Project (with an average of eight students and one mentor) provides low faculty-to-students ratios, creating desired small group learning. Starting for the first time in the 2020-2021 school year, Scholarly Project had to adapt to the impact of the COVID-19 pandemic, with two periods of online learning required in September 2020 and May 2021 due to local COVID-19 outbreaks. To help manage this, the university applied for technical assistance from Microsoft Office 365 with a full-access subscription to maintain the scheduled small group meetings between students and their mentors while optimising social distancing (Duong et al., 2021).
We recommend introducing the 14-skill questionnaire as a tool for medical students to self-monitor their improvement during participation in the Scholarly Project. From the mentors’ perspective, the questionnaire provides a reliable and convenient reference for providing feedback to students and suggestions about areas that need further improvement. These approaches could also be utilised in other institutions, either locally or internationally, who include a Scholarly Project for a number of reasons: (1) the Scholarly Project is a lengthy module that could be impacted by unexpected events (e.g. COVID-19); (2) the need for routine self-check and mentor feedback to facilitate the required research skills improvement; and (3) because the questionnaire is a validated, convenient and accessible method for both medical students and mentors.
D. Study Limitations
Although the survey was sent to all medical students participating in the Scholarly Project, only just over half of students responded. Therefore, the impact of the Scholarly Project on non-responding medical students may not reflect the trends reported here, limiting the generalizability of our findings. Nonresponse bias is another potential limitation, although this is not necessarily associated with a lower response rate (Davern, 2013; Halbesleben and Whitman, 2012). Participants might perceive that self-evaluation about how much their research skills had improved could indirectly reflect their level of participation in Scholarly Project, the contribution of their mentor, and the level of their academic performance, leading to social desirability bias in their responses. We attempted to reduce nonresponse and social desirability bias, and any perception that responses could impact on academic assessments, by making survey responses anonymous and keeping the study survey completely separate from any academic assessments (e.g. grade-point average). Another limitation is the lack of a control group of medical students, but this is difficult because participation in the Scholarly Project is mandatory for all students. Using a control group would have strengthened the study from a methodological perspective and allowed investigation of the impact of specific aspects of the Scholarly Project.
Respond shift bias is inevitable while conducting this research. To reduce this, instead of completing self-evaluation for all fourteen skills initially and then after the completion of the whole project, students should assess their skill level immediately after the completion of each Module. However, response shift bias happened because respondents perceived the purpose of the survey as assessing the program’s effectiveness. In the context of our research, even if assessments were completed after each Module, students would realise the aim of the survey meaning that respond-shift bias would not decrease considerably.
V. CONCLUSION
Scholarly Project is an excellent learning opportunity for medical students in the refreshed undergraduate medical curriculum. Participating in a Scholarly Project provides students with research experience, including the knowledge, structure, and support needed to engage in scholarly work. By providing the foundations for scholarly work, medical students can enter the health care workforce with solid clinical expertise and the basic skills required to conduct high-quality projects that improve the safety and quality of care delivered to patients. We suggest integrating the Scholarly Project curriculum throughout the undergraduate medical education curriculum in Vietnam. This is important in terms of early experience of medical research and fostering a good understanding of medical scientific research for all future doctors, regardless of their ultimate career destination.
Notes on Contributors
N.T.M.D. and K.H.V. drafted and revised the manuscript. V.T.N.L. helped in reviewing the manuscript. All authors (N.T.M.D., K.H.V., V.T.N.L.) have made substantial contributions to the conception and design of the work and the acquisition, analysis, and interpretation of data. All authors read and approved the final manuscript.
Ethical Approval
The authors declare that this study did not require human ethics approval and did not include experiments on animal or human subjects. This study was submitted to the Institutional Review Board (IRB) at University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam. This project was determined to be exempt from IRB review. All methods were carried out in accordance with relevant guidelines and regulations. Respondents were informed that their participation in the survey was completely voluntary and there were no risks associated with their participation.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available for reasons of data protection but are available from the corresponding author on reasonable request.
Acknowledgement
The authors would very much like to acknowledge Ms. Le Minh Chau, Mr. Ung Nguyen Vu Hoang, Ms. Duong Kim Ngan, Mr. Nguyen Hai Dang, Ms. Tran Thi Hong Ngoc, Mr. Giang Luu Thanh Hoang, and Mr. Nguyen Hoang Nhan (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam) for their support of this study.
Funding
No funding has been received for the study.
Declaration of Interest
The authors declare that they have no competing interests.
References
Beaton, D. E., Bombardier, C., Guillemin, F., & Ferraz, M. B. (2000). Guidelines for the process of cross-cultural adaptation of self-report measures. Spine, 25(24), 3186-3191. https://doi.org/10.1097/00007632-200012150-00014
Bickford, N., Peterson, E., Jensen, P., & Thomas, D. (2020). Undergraduates interested in STEM research are better students than their peers. Education Sciences, 10(6), 150. https://doi.org/10.3390/educsci10060150
Blockus, L., Kardash, C. M., Blair, M., & Wallace, M. (1997). Undergraduate internship program evaluation: A comprehensive approach at a research university. Council on Undergraduate Research, 18, 60–63.
Boninger, M., Troen, P., Green, E., Borkan, J., Lance-Jones, C., Humphrey, A., Gruppuso, P., Kant, P., McGee, J., Willochell, M., Schor, N., Kanter, S. L., & Levine, A. S. (2010). Implementation of a longitudinal mentored scholarly project: An approach at two medical schools. Academic Medicine, 85(3), 429–437. https://doi.org/10.1097/acm.0b013e3181ccc96f
Carraccio, C., Wolfsthal, S. D., Englander, R., Ferentz, K., & Martin, C. (2002). Shifting Paradigms. Academic Medicine, 77(5), 361–367. https://doi.org/10.1097/00001888-200205000-00003
Carson, S. (2007). A new paradigm for mentored undergraduate research in molecular microbiology. CBE—Life Sciences Education, 6(4), 343–349. https://doi.org/10.1187/cbe.07-05-0027
Dagher, M. M., Atieh, J. A., Soubra, M. K., Khoury, S. J., Tamim, H., & Kaafarani, B. R. (2016). Medical Research Volunteer Program (MRVP): Innovative program promoting undergraduate research in the medical field. BMC Medical Education, 16(1), Article 160. https://doi.org/10.1186/s12909-016-0670-9
Davern, M. (2013). Nonresponse rates are a problematic indicator of nonresponse bias in survey research. Health Services Research, 48(3), 905–912. https://doi.org/10.1111/1475-6773.12070
Deslauriers, L., McCarty, L. S., Miller, K., Callaghan, K., & Kestin, G. (2019). Measuring actual learning versus feeling of learning in response to being actively engaged in the classroom. Proceedings of the National Academy of Sciences, 116(39), 19251–19257. https://doi.org/10.1073/pnas.1821936116
Duong, D. B., Phan, T., Trung, N. Q., Le, B. N., Do, H. M., Nguyen, H. M., Tang, S. H., Pham, V. A., Le, B. K., Le, L. C., Siddiqui, Z., Cosimi, L. A., & Pollack, T. (2021). Innovations in medical education in Vietnam. BMJ Innovations, 7(Suppl 1), s23–s29. https://doi.org/10.1136/bmjinnov-2021-000708
Fan, A. P., Tran, D. T., Kosik, R. O., Mandell, G. A., Hsu, H. S., & Chen, Y. S. (2012). Medical education in Vietnam. Medical Teacher, 34(2), 103–107. https://doi.org/10.3109/0142159x.2011.613499
Frank, J. R., Snell, L. S., Cate, O. T., Holmboe, E. S., Carraccio, C., Swing, S. R., Harris, P., Glasgow, N. J., Campbell, C., Dath, D., Harden, R. M., Iobst, W., Long, D. M., Mungroo, R., Richardson, D. L., Sherbino, J., Silver, I., Taber, S., Talbot, M., & Harris, K. A. (2010). Competency-based medical education: Theory to practice. Medical Teacher, 32(8), 638–645. https://doi.org/10.3109/0142159x.2010.501190
Halbesleben, J. R. B., & Whitman, M. V. (2012). Evaluating survey quality in health services research: A decision framework for assessing nonresponse bias. Health Services Research, 48(3), 913–930. https://doi.org/10.1111/1475-6773.12002
Hoat, L. N., Lan Viet, N., van der Wilt, G., Broerse, J., Ruitenberg, E., & Wright, E. (2009). Motivation of university and non-university stakeholders to change medical education in Vietnam. BMC Medical Education, 9(1), Article 49. https://doi.org/10.1186/1472-6920-9-49
Holloway, R., Nesbit, K., Bordley, D., & Noyes, K. (2004). Teaching and evaluating first and second year medical students’ practice of evidence-based medicine. Medical Education, 38(8), 868–878. https://doi.org/10.1111/j.1365-2929.2004.01817.x
Iobst, W. F., Sherbino, J., Cate, O. T., Richardson, D. L., Dath, D., Swing, S. R., Harris, P., Mungroo, R., Holmboe, E. S., & Frank, J. R. (2010). Competency-based medical education in postgraduate medical education. Medical Teacher, 32(8), 651–656. https://doi.org/10.3109/0142159x.2010.500709
Kardash, C. M. (2000). Evaluation of undergraduate research experience: Perceptions of undergraduate interns and their faculty mentors. Journal of Educational Psychology, 92(1), 191–201. https://doi.org/10.1037/0022-0663.92.1.191
Kinser, P. A., & Robins, J. L. (2013). Control group design: enhancing rigor in research of mind-body therapies for depression. Evidence-Based Complementary and Alternative Medicine, 2013. https://doi.org/10.1155/2013/140467
Leppink, J. (2017). Helping medical students in their study of statistics: A flexible approach. Journal of Taibah University Medical Sciences, 12(1), 1–7. https://doi.org/10.1016/j.jtumed.2016.08.007
Manduca, C. (1997). Broadly defined goals for undergraduate research projects: A basis for program evaluation. Council on Undergraduate Research, 18(2), 64–69.
Murdoch-Eaton, D., Drewery, S., Elton, S., Emmerson, C., Marshall, M., Smith, J. A., Stark, P., & Whittle, S. (2010). What do medical students understand by research and research skills? Identifying research opportunities within undergraduate projects. Medical Teacher, 32(3), e152–e160. https://doi.org/10.3109/01421591003657493
Nguyen, T. V., Ho-Le, T. P., & Le, U. V. (2016). International collaboration in scientific research in Vietnam: An analysis of patterns and impact. Scientometrics, 110(2), 1035–1051. https://doi.org/10.1007/s11192-016-2201-1
Pithon, M. M. (2013). Importance of the control group in scientific research. Dental Press Journal of Orthodontics, 18(6), 13–14. https://doi.org/10.1590/s2176-94512013000600003
Schor, N. F., Troen, P., Kanter, S. L., & Levine, A. S. (2005). The scholarly project initiative: Introducing scholarship in medicine through a longitudinal, mentored curricular program. Academic Medicine, 80(9), 824–831. https://doi.org/10.1097/00001888-200509000-00009
Schwartzstein, R. M., Dienstag, J. L., King, R. W., Chang, B. S., Flanagan, J. G., Besche, H. C., Hoenig, M. P., Miloslavsky, E. M., Atkins, K. M., Puig, A., Cockrill, B. A., Wittels, K. A., Dalrymple, J. L., Gooding, H., Hirsh, D. A., Alexander, E. K., Fazio, S. B., & Hundert, E. M. (2020). The Harvard Medical School pathways curriculum: Reimagining developmentally appropriate medical education for contemporary learners. Academic Medicine, 95(11), 1687–1695. https://doi.org/10.1097/acm.0000000000003270
Schwartzstein, R. M., & Roberts, D. H. (2017). Saying goodbye to lectures in medical school — Paradigm shift or passing fad? New England Journal of Medicine, 377(7), 605–607. https://doi.org/10.1056/nejmp1706474
Zydney, A. L., Bennett, J. S., Shahid, A., & Bauer, K. W. (2002). Impact of undergraduate research experience in engineering. Journal of Engineering Education, 91(2), 151–157. https://doi.org/10.1002/j.2168-9830.2002.tb00687.x
*Nguyen Tran Minh Duc
217 Hong Bang Street, Ward 11,
District 5, Ho Chi Minh City, Vietnam
+84 988 127 948
Email: ntmduc160046@ump.edu.vn
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









