Impact of COVID-19 on health profession education in Singapore: Adoption of innovative strategies and contingencies across the educational continuum
Submitted: 20 July 2020
Accepted: 6 November 2020
Published online: 13 July, TAPS 2021, 6(3), 14-23
https://doi.org/10.29060/TAPS.2021-6-3/RA2346
Claude Jeffrey Renaud1, Zhi Xiong Chen2,6, Heng-Wai Yuen3, Lay Ling Tan4, Terry Ling Te Pan5 & Dujeepa D. Samarasekera6
1Department of Medicine, Khoo Teck Puat Hospital, Singapore; 2Department of Physiology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Department of Otorhinolaryngology-Head & Neck Surgery, Changi General Hospital, Singapore; 4Department of Psychological Medicine, Changi General Hospital, Singapore; 5Department of Anaesthesiology, National University Health System, Singapore; 6Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: The Coronavirus-19 pandemic has had profound effects on health professions education (HPE) posing serious challenges to the continued provision and implementation of undergraduate, postgraduate and continuing medical education (CME). Across these HPE domains, the major disruptions included the exclusion of undergraduate learners from clinical learning environments, restricted intra-, inter-institutional and overseas movement of medical professionals, termination of face-to-face learner-educator interactions, deployment of postgraduate learners into non-scope service settings, and CME postponement.
Methods: In this review we report on how in Singapore various adaptive measures were instituted across the 3 HPE domains at institutional and national level to maintain adequate resources at the frontline to meet service exigencies, promote healthcare professionals’ wellbeing and safety as well as mitigate the spread of the pandemic.
Results: We identified several strategies and contingencies developed to address these challenges. These involved the use of online learning platforms, distributed and asynchronous learning, an undergraduate Pathway Programme, and use of innovative hands-on technology like simulation. Robust, well pre-planned pandemic preparedness, effective communication, as well as provision of psychological support resources ensured maintenance of service and academic continuity, trust and resilience within HPE. However, several challenges remain, namely the timing and manner of conducting formative and summative assessments, cybersecurity, and the indispensable hands-on, in-person experiential learning for surgical training.
Conclusion: Strong leadership with vision and planning, good communication, prioritising learners’ and educators’ wellbeing and safety, and harnessing existing and emerging online learning technologies are crucial elements for effective contingencies for HPE disruption during pandemics.
Keywords: Pandemic Preparedness, COVID-19, Curriculum Development, Online Learning and Assessment, Learner Wellbeing and Safety, Health Profession Education
Practice Highlights
- COVID-19 pandemic has caused profound disruption to medical education and Singapore is no exception.
- Health professions education community (undergraduate, residency and continuous professional development) had to rethink traditional learning approaches.
- There is a need for contingencies that integrate service and academic continuity and safety.
- Implementing contingencies requires coordinated national and institutional pandemic pre-preparedness.
- There remain uncertainties as to the long-term effectiveness of these contingencies on learning.
I. INTRODUCTION
Singapore had its first case of Coronavirus 19 (COVID-19) on 23rd January 2020 and scaled up its response from DORSCON (Disease Outbreak Response System Condition) Yellow to Orange 2 weeks later as the crisis evolved to pandemic proportion (Ashokka et al., 2020; J.E.L. Wong et al., 2020). This involved setting up a suite of strategies aimed at containing community transmission (Lee et al., 2020).
At the healthcare service and health profession education (HPE) level, these strategies centred on mobilising adequate resources at the frontline, mandating use of personal protective equipment (PPE) in high-risk areas and restricting healthcare workers’ movement (Ashokka et al., 2020; Lee et al., 2020; Liang et al., 2020; C. Wong et al., 2020; J.E.L. Wong et al., 2020). In addition, undergraduate medical education put a stop to clinical clerkships and large and small on-campus learning and restructured formative and summative assessments.
As the very stakeholders and resources required for HPE were diverted to fighting the pandemic, HPE faced extraordinary disruption. Educators and learners had to delicately balance service continuity, patients’ and learners’ wellbeing and safety versus maintaining a business-as-usual approach to learning. Moreso, the entire HPE community had to critically relook at the applicability of competency-based learning which is traditionally predicated on the principles of authentic supervised patient experience, programmatic assessment, learners as part of a community of practice and continuous professional development (CPD) (Harris et al., 2010; Iobst et al., 2010).
Previous public health emergencies like Severe Acute Respiratory Syndrome (SARS) have taught that such disruptions can provide unique opportunities for contingency planning in HPE especially when there is little time for wholesale programme redesign (Lim et al., 2009; Patil & Yan, 2003). This report thus describes the experience of 3 HPE domains in Singapore in mitigating the dissonance between optimal pandemic preparedness, unconstrained academic continuity and learners’ and educators’ well-being.
II. METHODS
A comprehensive review of the adaptive contingency strategies adopted at 1 undergraduate (Yong Loo Lin School of Medicine), Singapore residency programmes and across the CPD was made by looking at institutional and governmental programmes during the early phase of the pandemic and prevalent COVID-19 related literature on HPE. As this research is a description of events that have already happened and did not involve HPE stakeholders’ directly and interventionally, participants’ informed consent and internal review board approval were not required for its conduct.
III. RESULTS
Herein, is a detailed outline of the contingencies implemented across the 3 HPE domains which are also summarised in Table 1.
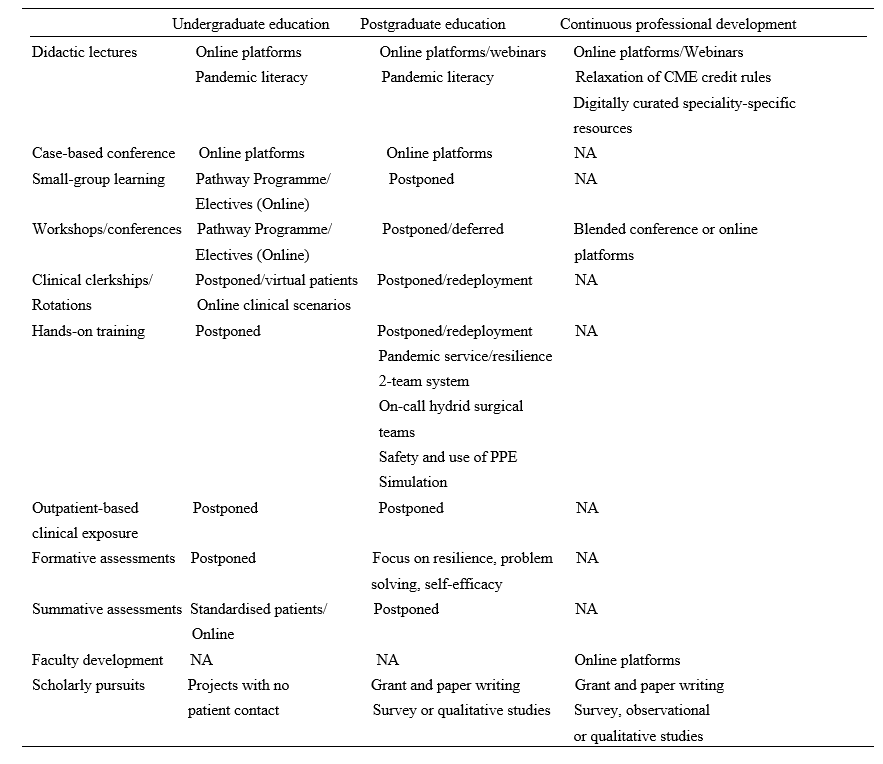
Table 1. Summary of disruptions and contingences across the health profession education spectrum during COVID-19 pandemic in Singapore.
Note: NA=not applicable; PPE= personal protective equipment
A. Contingencies in Undergraduate Medical Education: Experience of Yong Loo Lin School of Medicine
At the Yong Loo Lin School of Medicine which is the largest of the three medical schools in Singapore, the Education Team led by the Vice Dean (Education) started preparing in February 2020 for the possibility of loss of clinical teaching. Those most affected would be Phase 3 and 4 (Year 3 and 4) medical students. Phase 5 (Year 5) students were preparing for their Final Professional Examinations even though assessment was significantly disrupted across all Phases. Phase 1 and 2 (Year 1 and 2) students have relatively less clinical learning exposure and assessments, and were finishing their curricula and preparing for exams. Focusing on the Phase 3 and 4 students, first, their vacation and elective periods were brought forward respectively. Next, to give students meaningful learning opportunities that do not require patient contact, the Pathway Programme which had been launched before the pandemic was paced up (National University Singapore, Yong Yoo Lin School of Medicine, 2020).
The Pathway Programme consists of six Pathways. They are Health and Humanity, Health Informatics, Inquiry and Thinking, Medical Education and Medical Innovation and Entrepreneurship all led by a team of trained educationists. In addition, a non-Pathway initiative called Education Innovation completed the suite of new education offerings for the students. The sixth Pathway Behavioural and Implementation Science was partially offered under Inquiry and Thinking through a series of lectures on Health Economics. Below we describe what each Pathway is about.
1) Behavioral and implementation science: This pathway exposes medical students to principles of behavioural and implementation science, and applies this knowledge to effectively design and deliver healthcare in real-world settings, and lays the foundation for them to become active agents of change in clinical practice.
2) Health and humanity: This pathway aims to nurture emotionally resilient, socially conscious and globally minded health leaders through rekindling one’s love for medicine and humanity. Through experiential activities, inspirational workshops and hands-on project work in the community, students develop critical thinking skills in global health, teamwork and leadership skills to inspire health for all.
3) Health informatics: This pathway aims to enable students to gather and critically evaluate research and health informatics data, equipping them with the skills necessary to apply the principles of health informatics, summarise and visualise datasets to perform basic analyses, so they become data-science competent clinicians who can identify and analyse medical data to address clinical issues.
4) Inquiry and thinking: This pathway aims to inspire and motivate our medical students to develop a sense of curiosity so as to foster a habit of inquiry that is able to dynamically utilise a range of thinking methods, processes and skillsets to tackle questions and problems. The end goal of this pathway is to groom a pipeline of thinking doctors who can advance healthcare in any aspect they desire.
5) Medical education: This pathway exposes medical students to concepts and principles in HPE, to equip them with foundational skills in HPE, with a focus on educational innovation and scholarship of teaching and learning, so as to groom future clinical educators.
6) Medical innovation and entrepreneurship: This pathway aims to nurture medical students with the 6Cs attributes: Curiosity, Creativity, Compassion, Collegiality, Collaboration, and Commercial Intelligence. The programme gradually exposes medical students to concepts and principles in innovation, and the selective elements equip students with foundational skills in innovation and entrepreneurship.
With the elective period brought forward, Phase 4 students were exposed to the Pathway Programme from early-March to early-May 2020 through two weeks of front-loading online lectures, followed by four to eight weeks of projects. Most Pathways followed the general structure with slight variations between them. For Phase 3 students, they enjoyed an early vacation before encountering a shortened Pathway Programme from early-April to early-May 2020, comprising of 2 weeks of front-loading online lectures and 2 weeks of projects, which students had the option of continuing into Phase 4.
Using Inquiry and Thinking Pathway as an example, topics of front-loading online lectures included ‘Complexity and Systems Thinking’, ‘Habits of Inquiry and Critical Thinking’ and ‘Evidence-based Medicine and Search Methods’. More than 80 projects were offered by prospective supervisors with more than 70 students getting involved in projects. Each student was guided in the project by the supervisor as well as engaged in a one to two-hour weekly reflection sessions with a separate mentor or the supervisor who doubled up as a mentor. Students were required to submit a weekly reflection write-up of 50 words or more. At the end of the Pathway Programme, students submitted a single slide of their projects for evaluation. Top two projects from each Pathway were selected to present and compete in a Grand Finale on 8 May 2020 before the School’s leadership, a panel of judges, their peers and overseas observers. The Grand Finale attracted over 200 participants. Single slides of all projects were compiled into an e-book to be shared with students and faculty members.
B. Postgraduate Training: Experience of Residency Programmes across Singapore Three Sponsoring Institutions (SIs)
Since SARS, Singapore has steadily been bolstering critical resource reserves and expertise in pandemic preparedness, culminating in the setup of the 330-bed purpose-built National Centre for Infectious Diseases (NCID) at the National Healthcare Group (NHG) Novena campus (Lee et al., 2020; Seah, 2020). Concurrently, postgraduate medical education underwent significant transformation with the adoption of Accreditation Council for Graduate Medical Education (ACGME) styled competency-based learning, culminating in the setup of three residency SIs of which NHG is one (Huggan et al., 2012; Khoo et al., 2014). Thus during the build-up to COVID-19 pandemic, NCID, residents and faculty at NHG 27 residency programmes formed the initial frontliners in managing the pandemic before being later joined by the other two SIs (C. Wong et al., 2020).
Care delivery and learning had to be restructured so that adequate manpower could be redeployed at screening centres, emergency departments, outbreak wards and critical care units. Frontline residents had to endure long and exhausting shifts wearing PPEs and prolonged time away from family, not to mention postponed leaves. Residents and faculty also had to be segregated into independent two-team system with phased two-weekly rotations to avoid manpower attrition and service disruption as a result of staff infection, quarantine or burnout. Elective surgeries, continuity clinics, grand rounds, face-to-face case conferences, cross-institutional elective rotations, in-person programme selection interviews as well as summative assessment had to be deferred. Postgraduate specialty conferences, courses and workshops, whether local or international, also had to be postponed or cancelled due to travel restrictions, further limiting opportunities for learning.
As a result of these changes several resourceful strategies were implemented to balance the palpable tensions between service, wellbeing and learning.
The first was maintaining open and transparent communication between institutional and academic leaders, faculty and residents so that the rationale for a pandemic-mode centralised command-control leadership model could be accepted. This allowed residents to grasp the real sense of urgency brought in by COVID-19, thus facilitating speedier buy-in and compliance to ever changing human resource and education policies. In addition, this strategy helped build up trust in the institutional support structure and contain the spread of parallel distracting infodemics, allowing residents to focus on service delivery, learning and well-being.
The second strategy was the promotion of residents’ physical and psychological safety and wellbeing. This entailed ensuring all residents had adequate orientation to the proper use of PPEs and could easily access them. Well-being and resilience support resources like in-person or anonymous virtual outreach psychological crisis intervention counselling and peer support through online debriefing and feedback were put in place across all hospitals under the three SIs. The ancillary effect was that residents felt their safety, their families’ and patients’ was valued and that there was fair and equitable work and rest allocation. Further, ACGME cancelled all accreditation and Clinical Learning Environment Review site visits and took steps to reframe and relax some accreditation criteria (Nasca, 2020). This went a long way in allaying residents’ anxieties regarding clinical progression.
The third strategy was leveraging existing online tools to maintain some element of learning continuity without the need to invest in significantly expensive technologies, curricular redesign or faculty re-development. Programmes transferred their core didactic lectures, journal clubs and case-based discussions onto distributed learning platforms such as Zoom, Go to meeting, Google meet or WebEx for synchronous learning. Access to Webinars had the added advantage of providing opportunities for asynchronous learning. Zoom teleconferencing in particular, remains the most popular due to its affordable subscription, large participant capacity and easier accessible collaborative interface and a breakout feature that enables mounting learning models like team-based learning.
Residents from surgical residency programmes who rely on direct-patient encounter and hands-on experience for learning were more significantly impacted. Importantly, because non-emergency visits to hospitals were halted, elective procedures and surgeries were postponed or cancelled and, the number of patients and learning opportunities was thus greatly reduced. This was further aggravated by the shift of many training institutions and teaching hospitals to pandemic service (Liang et al., 2020). In many instances, surgical residents were redeployed to frontline areas, like screening centres, which are beyond their usual scope of practice (C. Wong et al., 2020).
Curriculum development contingencies thus went beyond online didactic content dissemination to embrace enhanced distributed learning approaches like videos, podcasts, virtual reality and simulated learning (C. Wong et al., 2020). Some programmes improvised by forming on-call hybrid surgical teams, which allowed surgical residents some measure of hands-on exposure to generic emergency or semi-elective cases during on calls but not necessarily within the scope of their area of interest.
C. Contingencies for Continuous Professional Development (CPD)
The disruption brought on by closure of higher educational institutions, scaling down of healthcare organisations and travel restrictions, compelled educators and health care professionals to adapt and embrace curricular changes and transition to virtual learning and use of technology for simulated learning.
Continuing medical education (CME) and CPD are integral parts of the development of a healthcare professional in providing optimal clinical care for his/her patient. CME is aimed at maintaining or updating the requisite knowledge, skills, professional performance and relationships and crucially, is a requirement for maintenance of certification in the discipline or specialty of the healthcare profession (Davis et al., 2008). CPD on the other hand caters to a broader range of competencies that reflect the healthcare profession attitudes towards learning and learning needs (Filipe et al., 2018). Every specialty and governing medical body has its stipulated requirements. In Singapore, the Singapore Medical Council (SMC) states that all fully and conditionally registered doctors are required to meet the compulsory CME requirements of 50 core points for the qualifying period before their practising certificate can be renewed (Singapore Medical Council, 2020a). While most CME activities involve attendance at local, regional or international scientific meetings or conferences, self-study, review and authorship of articles are also considered core CME points. Most hospitals hold regular Grand Ward Rounds, journal clubs and peer review learning sessions at departmental and institutional levels, which also contribute towards core CME points.
However, with Singapore moving to DORSCON Orange, many of these learning activities were immediately suspended as staff scrambled to reorganise clinical services amidst the pandemic imperative for team separation and safe distancing. Thus, traditional face-to-face meetings were replaced by online meetings and webinars facilitated by virtual platforms mentioned previously. In tandem the SMC relaxed requirements for CME credits by allowing healthcare professionals to log in attendance to online sessions, including webinars (Singapore Medical Council, 2020b). There was also an increase in allocation of CME credits for self-study (e.g., reading of referenced journals listed in PubMed). COVID-19-related CME activities were also considered core points for all doctors (Singapore Medical Council, 2020b).
While, much of the recent global CME content has primarily focused on increasing understanding of COVID-19 and its infectious nature across various medical disciplines, there has been lesser emphasis on its medical and psychological impact to health. It has nonetheless enabled healthcare professionals to better provide optimal care for patients while adopting best available evidenced practice relating to all aspects of this rapidly contagious disease. Thus, online information dissemination has been at an unprecedented high with multiple local, regional and international webinars and resource websites being made readily accessible. Professional societies have also made available to their members regularly curated digital speciality-specific resources on best practices pertaining to COVID-19 management (Academy of Medicine Singapore, 2020).
In addition to CME, healthcare professionals have traditionally relied on annual live face-to-face local, regional and international scientific conferences, symposiums, and educational workshops to network as a learning community and keep abreast of domain-specific advances. With strict travel restrictions these have been cancelled, postponed or moved online as webinars, interactive content, forums and chats.
Some conference organisers decided to still proceed to issue notices of acceptance of abstract submissions as ‘proof’ of scholarly work or allowed online presentation. Other creative ways of continuing with international conferences have included a “blended conference” approach with a mix of face-to-face and online content to support those attending onsite and online (Nadarajah et al., 2020). With careful attention paid to safe distancing for onsite participants, such “blended conferences” provide the all-important human face-to-face interactions which online webinars and conferences, though functional in most parts, sorely lack. They also provide the best of both worlds and may indeed be the new normal in the foreseeable future as COVID-19 further changes the HPE landscape relating to international travel and social interaction.
Similarly, Singapore’s three medical school curriculum development centres rapidly transited in-person to virtual faculty development sessions. This allowed educators openly dispersed by social distancing and clinical exigencies to continue tapping on the best pedagogic practices, interact and engage in interprofessional learning.
IV. DISCUSSION
The COVID-19 pandemic disruptions have reinforced the need for agency and adaptation in HPE. We have shown that through well-coordinated, multisectoral efforts, solutions can be harnessed to minimise their negative impact on learning. However COVID-19, unlike other recent coronavirus epidemics like SARS and Middle East Respiratory Syndrome (MERS) seems a more formidable crisis (Jones, 2020; Peeri et al., 2020). It may not go away quickly without the advent of effective vaccines and sustained infection control measures. These contingencies are therefore aimed at promoting service and academic continuity, safety and resilience. Whilst they are useful blueprints for pandemic preparedness and responsiveness in the short term, they may not be applicable in all contexts or in a crisis of attrition. Further, they have their own strengths and limitations.
A major strength is institutional and academic leaders’ sense of long-term planning and commitment to educators’ and learners’ safety through effective communication, being visible and providing programme and system support. In a rapidly evolving disruptive environment, this is crucial, as stakeholders remain engaged and trusting without having to anguish over under-resourcing or abandonment. Recent publications have alluded to the social capital returns of such an “integrative resilience approach” that amplifies individual and system wellbeing and minimises burn-out and contagion (Neufeld & Malin, 2020; Samarasekera et al., 2020; Schwartz et al., 2020; Wald, 2020).
Another strength is the adoption of adaptive online technologies which not only ensures academic continuity but also allows a smooth and rapid quarantine and pandemic curriculum development. Large virtual communities of learners can thus be rapidly mobilised without fundamentally affecting content, quality and institutional bottom lines. Indeed, this may have had the unintended consequences of unprecedentedly boosting attendance rates in medical schools, residency programmes and CPD sessions. Online migration also facilitates quick and mass standardised training and deployment of untrained or returning retired healthcare professionals in general and critical care medicine, allowing healthcare institutions to boost capacity in those critical areas during pandemics (Brunner et al., 2020; Li et al., 2020). More so, these emergent technologies hold a lot of promise for post-pandemic medical education and replication of authentic patient experiences. It is envisioned that they can be interfaced onto learning management systems (LMS) and into areas like virtual patient consults, telemedicine, adaptive learning and extended reality or avatar-like high fidelity simulation (Goh & Sandars, 2020). They are also important as a source of asynchronous learning whereby learners who are too busy with clinical duties or for surgical residents when there is a lack of critical hands- on training (Tolu et al., 2020).
A third strength, is that such crisis can open unintended opportunities for learners to develop competencies outside the core curricular knowledge and procedural skills sphere. For instance, the mere exposure of undergraduate learners not directly involved in patient care to pandemic-related content, volunteering in contact tracing or public awareness centres or restructuring of learning experiences like the Pathway Programme can nurture professional identity, pandemic literacy and doctor-ready qualities like service prioritisation, altruism and resilience (Bauchner & Sharfstein, 2020; Rose, 2020; Stetson et al., 2020). Indeed, the Pathway Programme succeeded in meaningfully engaging medical students at a time when clinical teaching and clinical elective opportunities were frozen. It gave time for the medical school to work out a safe and calibrated approach to resume clinical training in consultation with the relevant government bodies. The fact that it was conceptualised pre-pandemic demonstrates an extraordinary sense of prescience by the academic leadership. The advent of COVID-19 served to accelerate its implementation. It thus not only helped undergraduate medical education to cope with the pandemic but enrich the medical curriculum by catering to the diverse strengths and interests of each learner in order to nurture future-ready doctors for a post-COVID world.
As to residents’ learning, negotiating challenging pandemic duty rosters, making personal choices and sacrifices, navigating processes like resource allocation and public health measures and being deployed into non-core areas, can be just-in-time learning platforms for more nuanced ACGME competencies like professionalism, interpersonal and communication skills, system-based practice and practice-based learning (Hall et al., 2020; Nasca, 2020; Schwartz et al., 2020; Tolu et al., 2020; C. Wong et al., 2020). For surgical residents, there is also an added learning and safety benefit when hitherto straightforward surgical procedures like tracheostomy suddenly come with a myriad of precautions, criteria, and protocols (Givi et al., 2020). Clinic and elective surgery postponement can provide ample opportunities for self-directed learning, exit exams preparation and scholarly pursuits like grant, research ventures and quality improvement projects writing (Schwartz et al., 2020; Tolu et al., 2020). Additionally, prioritisation of public health emergency response training across the HPE spectrum can render healthcare institutions better prepared at handling future pandemics and burn-out (Yang et al., 2020).
Nevertheless, these contingencies have a number of limitations. Namely, moving medical education from the bedside to the ‘web-side’ cannot replace the real patient-centred clinical experience and case-mix learners derive from ward rounds, grand rounds and continuity clinics. Even the Pathway Programme was not without its challenges. With Singapore entering into Circuit Breaker phase of DORSCON Orange on 3rd April 2020, some projects were disrupted as access and movement became more limited (Ministry of Health Singapore, 2020).
Secondly, the utility of online learning is very much predicated on the vagaries of internet penetration and connectivity which makes this approach not always transferable to all socio-economic contexts (Cecilio-Fernandes et al., 2020). More so, for surgical residents, online learning or high-fidelity simulation cannot substitute for in-person learning. The technical skills, haptic feedback, the realism of live surgery, the experiential and contextual learning of ‘being there’ in a surgical team, and the non-cognitive domain skills like collaboration and resilience can be hard to simulate. Reduced contact time between residents and faculty also impacts adversely on opportunities for mentoring, role modelling and supervision. There is also always a danger of breaching learning principles such as cognitive overload when online content design is outside the hands of curriculum developers and programme directors (Kachra & Ma, 2020). As to health professionals, most of these online CME resources represent rather an amalgam of available information that may not have been well curated and pre-approved by accreditation organisations for relevancy.
Thirdly, the contingencies fail to address the enormous challenges in conducting clinical workplace-based assessments, without compromising their validity, reliability, defensibility and educational impact. Although high-stakes OSCE can be successfully conducted in a pandemic environment, its implementation comes with tremendous logistical and political manoeuvring to ensure students’, examiners’ and patients’ safety and assessment integrity are preserved (Boursicot et al., 2020). Cancelling both formative and summative assessments can delay learners’ progression or completion unless adjustments are made to previously established competency criteria. Undergraduates may fail to graduate on time to join the vital pool of medical workforce and residents may not be able to practise as independent practitioners. This can create anxiety and concern to both learners and educators about how to catch up post-pandemic with piling assessment and case and portfolio backlogs.
Lastly, reliance on third party software entities for online content dissemination contrary to institution-designed LMS or whole-sale programme information technology infrastructure redesign carries cybersecurity, privacy and data ownership risks (Fawns et al., 2020; Sandars et al., 2020). Not all faculty are tech savvy to handle the technical intricacies and the many options in the market. Predatory providers may thus seek to peddle behaviourist tactics onto users for their own corporate gains.
V. CONCLUSION
In summary, the COVID-19 pandemic has been a major threat to HPE in Singapore but it has also created opportunities for adaptive and flexible contingencies so that learning goes on safely with minimum constraints. While there is a need to celebrate these early successes, it is also imperative that we assess and learn from their limitations so that we can further refine and more successfully, collaboratively and iteratively apply them in a prolonged crisis. Furthermore, these experiences can serve as templates for adaptive and value-added learning at both regional and international HPE settings beset by larger service and academic disruption. But most importantly they foreshadow the resilience, reimagining and resourcefulness that are expected of HPE as it transits from the new normal of pandemic crisis management to the post-pandemic next normal of innovative technology-based learning.
Notes on Contributors
Adj Associate Professor Claude J Renaud is a senior consultant nephrologist at Khoo Teck Puat hospital Singapre and Associate Programme Director at the National Healthcare Group Renal Residency Programme. He conceptualised, drafted and revised article and wrote introduction, postgraduate medical education (PGME), discussion and conclusion sections.
Dr Zhi Xiong Chen is a Senior Lecturer in Physiology and Assistant Dean for Education at Yong Loo Lin School of Medicine, National University of Singapore. He conceptualised article and wrote the undergraduate medical education section.
Adj Associate Professor Heng Wai Yuen is senior consultant in the Department of Otorhinolaryngology-Head & Neck Surgery, Changi General Hospital, Singapore and Campus Director, SingHealth Duke-NUS Institute for Medical Simulation (SIMS). He wrote abstract and post graduate medical education sections and revised article.
Adj Associate Professor Tan Lay Ling is senior consultant in the Department of Psychological Medicine, Psychogeriatric Service, at Changi General Hospital (CGH). She wrote the section on continuous professional development and revised article overall.
Dr Terry Ling Te Pan is a Senior Consultant, Department of Anaesthesia, National University Hospital and Advisor, Education Technology Unit, Yong Loo Lin School of Medicine, National University of Singapore. He co-wrote the section on continuous professional development and revised article overall.
Dr Dujeepa D. Samarasekera, director at Centre for Medical Education (CenMED) Yong Loo Lin School of Medicine, National University of Singapore. conceptualised and revised article.
Ethical Approval
This study is a description of events and practices and therefore did not require approval from institutional review boards.
Funding
There is no external funding involved in this study.
Declaration of Interest
Other than Dr Dujeepa D Samarasekera who is Editor of TAPS, all authors have no conflict of interest, including financial, consultant, institutional and other relationships that might lead to bias.
References
Academy of Medicine Singapore (AMS) (2020, June 2). Resource site on COVID-19. https://www.ams.edu.sg/policy-advocacy/covid-19-resource-page
Ashokka, B., Ong, S. Y., Tay, K. H., Loh, N. H. W., Gee, C. F., & Samarasekera, D. D. (2020). Coordinated responses of academic medical centres to pandemics: Sustaining medical education during COVID-19. Medical Teacher, 42(7), 717-720. https://doi.org/10.1080/0142159X.2020.1757634
Bauchner, H., & Sharfstein, J. (2020). A bold response to the COVID-19 pandemic: Medical students, national service, and public health. The Journal of the American Medical Association, 323(18), 1790-1791, https://doi.org/10.1001/jama.2020.6166
Boursicot, K., Kemp, S., Ong, T. H., Wijaya, L., Goh, S. H., Freeman, K., & Curran, I. (2020). Conducting a high-stakes OSCE in a COVID-19 environment. MedEdPublish, 9(1), 54. https://doi.org/10.15694/mep.2020.000054.1
Brunner, M., Vogelman, B., & Smith, J. (2020). Rapid development of an outpatient‐to‐inpatient crash curriculum for COVID providers. Medical Education. Advanced online publication. https://doi.org/10.1111/medu.14244
Cecilio-Fernandes, D., Parisi, M. C. R., Santos, T. M., & Sandars, J. (2020). The COVID-19 pandemic and the challenge of using technology for medical education in low and middle income countries. MedEdPublish, 9(1), 74. https://doi.org/10.15694/mep.2020.000074.1
Davis, N., Davis, D., & Bloch, R. (2008). Continuing medical education: AMEE education guide No 35. Medical Teacher, 30(7), 652–666. https://doi.org/10.1080/01421590802108323
Fawns, T., Jones, D., & Aitken, G. (2020). Challenging assumptions about “moving online” in response to COVID-19, and some practical advice. MedEdPublish, 9(1), 83. https://doi.org/10.15694/mep.2020.000083.1
Filipe, H. P., Golnik, K. C., & Mack, H. G. (2018). CPD? What happened to CME? CME and beyond. Medical Teacher, 40(9), 914–916. https://doi.org/10.1080/0142159X.2018.1471200
Givi, B., Schiff, B. A., Chinn, S. B., Clayburgh, D., Iyer, N. G., Jalisi, S., Moore, M. G., Nathan, C. A., Orloff, L. A., O’Neill, J. P., Parker, N., Zender, C., Morris, L., & Davies, L. (2020). Safety Recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. The Journal of the American Medical Association Otolaryngology-Head & Neck Surgery, 146(6),579-584. https://doi:10.1001/jamaoto.2020.0780
Goh, P. S., & Sandars, J. (2020). A vision of the use of technology in medical education after the COVID-19 pandemic. MedEdPublish, 9(1), 49. https://doi.org/10.15694/mep.2020.000049.1
Hall, A. K., Nousiainen, M. T., Campisi, P., Dagnone, J. D., Frank, J. R., Kroeker, K. I., Brzezina, S., Purdy, E., & Oswald, A. (2020). Training disrupted: Practical tips for supporting competency-based medical education during the COVID-19 pandemic. Medical Teacher, 42(7), 756-761. https://doi.org/10.1080/0142159X.2020.1766669
Harris, P., Snell, L., Talbot, M., & Harden, R. M. (2010). Competency-based medical education: Implications for undergraduate programs. Medical Teacher, 32(8), 646–650. https://doi.org/10.3109/0142159X.2010.500703
Huggan, P. J., Samarasekara, D. D., Archuleta, S., Khoo, S. M., Sim, J. H. J., Sin, C. S. P., & Ooi, S. B. S. (2012). The successful, rapid transition to a new model of graduate medical education in Singapore: Academic Medicine, 87(9), 1268–1273. https://doi.org/10.1097/ACM.0b013e3182621aec
Iobst, W. F., Sherbino, J., Cate, O. T., Richardson, D. L., Dath, D., Swing, S. R., Harris, P., Mungroo, R., Holmboe, E. S., & Frank, J. R. (2010). Competency-based medical education in postgraduate medical education. Medical Teacher, 32(8), 651–656. https://doi.org/10.3109/0142159X.2010.500709
Jones, D. S. (2020). History in a crisis—Lessons for Covid-19. New England Journal of Medicine, 382(18), 1681–1683. https://doi.org/10.1056/NEJMp2004361
Kachra, R., & Ma, I. W. Y. (2020). Practical tips for faculty development workforce training under pressure in the time of COVID-19 pandemic. MedEdPublish, 9(1), 81. https://doi.org/10.15694/mep.2020.000081.1
Khoo, S. M., Lahiri, M., Huggan, P. J., Archuleta, S., Olszyna, D. P., Goh, W. P., Chua, S. W., & Ho, K. Y. (2014). When traditional model meets competencies in Singapore: Beyond conflict resolution. Annals of the Academy of Medicine Singapore, 43, 544–549.
Lee, V. J., Chiew, C. J., & Khong, W. X. (2020). Interrupting transmission of COVID-19: Lessons from containment efforts in Singapore. Journal of Travel Medicine, 27(3), 1-5. https://doi.org/10.1093/jtm/taaa039
Li, L., Xv, Q., & Yan, J. (2020). COVID-19: The need for continuous medical education and training. The Lancet Respiratory Medicine, 8(4), e23. https://doi.org/10.1016/S2213-2600(20)30125-9
Liang, Z. C., Ooi, S. B. S., & Wang, W. (2020). Pandemics and their impact on medical training: Lessons from Singapore. Academic Medicine, 95(9), 1359-1361. https://doi.org/10.1097/ACM.0000000000003441
Lim, E. C., Oh, V. M., Koh, D. R., & Seet, R. C. (2009). The challenges of “continuing medical education” in a pandemic era. Annals of the Academy of Medicine, Singapore, 38(8), 724–726.
Ministry of Health Singapore. (2020, June 1). Circuit breaker to minimise further spread of COVID-19. https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19
Nadarajah, V. D., Er, H. M., & Lilley, P. (2020). Turning around a medical education conference: Ottawa 2020 in the time of COVID‐19. Medical Education, 54(8), 760-67. https://doi.org/10.1111/medu.14197
Nasca, T. J. (2020). ACGME’s early adaptation to the COVID-19 pandemic: Principles and lessons learned. Journal of Graduate Medical Education, 12(3), 375-378. https://doi.org/10.4300/JGME-D-20-00302.1
National University of Singapore, Yong Yoo Lin School of Medicine. (2020, June 30). Curriculum structure and requirements. https://www.nus.edu.sg/nusbulletin/yong-loo-lin-school-of-medicine/undergraduate-education/degree-requirements/bachelor-of-medicine-and-bachelor-of-surgery-m-b-b-s/curriculum-structure-and-requirements
Neufeld, A., & Malin, G. (2020). Twelve tips to combat ill-being during the COVID-19 pandemic: A guide for health professionals & educators. MedEdPublish, 9(1), 70. https://doi.org/10.15694/mep.2020.000070.1
Patil, N. G., & Yan, Y. C. H. (2003). SARS and its effect on medical education in Hong Kong. Medical Education, 37(12), 1127–1128. https://doi.org/10.1046/j.1365-2923.2003.01723.x
Peeri, N. C., Shrestha, N., Rahman, M. S., Zaki, R., Tan, Z., Bibi, S., Baghbanzadeh, M., Aghamohammadi, N., Zhang, W., & Haque, U. (2020). The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? International Journal of Epidemiolology, 49(3), 717-720. https://doi.org/10.1093/ije/dyaa033
Rose, S. (2020). Medical student education in the time of COVID-19. The Journal of the American Medical Association, 323(21), 2131-2132. https://doi.org/10.1001/jama.2020.5227
Samarasekera, D. D., Goh, D., & Lau, T. C. (2020). Medical school approach to manage the current COVID-19 crisis. Academic Medicine: Journal of the Association of American Medical Colleges, 95(8), 1126–1127. https://doi.org/10.1097/ACM.0000000000003425
Sandars, J., Correia, R., Dankbaar, M., de Jong, P., Goh, P. S., Hege, I., Masters, K., Oh, S.-Y., Patel, R., Premkumar, K., Webb, A., & Pusic, M. (2020). Twelve tips for rapidly migrating to online learning during the COVID-19 pandemic. MedEdPublish, 9(1), 82. https://doi.org/10.15694/mep.2020.000082.1
Schwartz, A. M., Wilson, J. M., Boden, S. D., Moore, T. J., Bradbury, T. L., & Fletcher, N. D. (2020). Managing resident workforce and education during the COVID-19 pandemic: Evolving strategies and lessons learned. Journal of Bone & Joint Surgery Open Access, 5(2), 1-5. https://doi.org/10.2106/JBJS.OA.20.00045
Seah, I. (2020). Striving as a nation to become an academic leader in the COVID-19 crisis. Singapore Medical Journal, 61(7), 370-372. https://doi.org/10.11622/smedj.2020059
Singapore Medical Council (2020a, May 29). Continuing medical education (CME) for doctors. https://www.healthprofessionals.gov.sg/smc/continuing-medical-education-(cme)-for-doctors
Singapore Medical Council (SMC) (2020b, May 29). Fulfilling continuing medical education (CME) requirements via online platforms. https://www.healthprofessionals.gov.sg/docs/librariesprovider2/continuing-medical-education-(cme)-for-doctors/circular—fulfilling-cme-requirements-via-online-platforms.pdf
Stetson, G. V., Kryzhanovskaya, I. V., Lomen‐Hoerth, C., & Hauer, K. E. (2020). Professional identity formation in disorienting times. Medical Education, 54(8), 765-766. https://doi.org/10.1111/medu.14202
Tolu, L. B., Feyissa, G. T., Ezeh, A., & Gudu, W. (2020). Managing Resident Workforce and residency training during COVID-19 pandemic: Scoping review of adaptive approaches. Advances in Medical Education and Practice, 11, 527–535. https://doi.org/10.3171/2020.4.JNS201012
Wald, H. S. (2020). Optimizing resilience and wellbeing for healthcare professions trainees and healthcare professionals during public health crises—Practical tips for an ‘integrative resilience’ approach. Medical Teacher, 42(7), 744-755. https://doi.org/10.1080/0142159X.2020.1768230
Wong, C., Tay, W., Hap, X., & Chia, F. (2020). Love in the time of coronavirus: Training and service during COVID-19. Singapore Medical Journal, 61(7), 384-386. https://doi.org/10.11622/smedj.2020053
Wong, J. E. L., Leo, Y. S., & Tan, C. C. (2020). COVID-19 in Singapore—current experience: Critical global issues that require attention and action. The Journal of the American Medical Association, 323(13), 1243. https://doi.org/10.1001/jama.2020.2467
Yang, D.-Y., Cheng, S.-Y., Wang, S.-Z., Wang, J.-S., Kuang, M., Wang, T.-H., & Xiao, H.-P. (2020). Preparedness of medical education in China: Lessons from the COVID-19 outbreak. Medical Teacher, 42(7), 787-790. https://doi.org/10.1080/0142159X.2020.1770713
*Claude J Renaud
Department of Medicine,
Division of Renal Medicine,
Khoo Teck Puat Hospital,
90 Yishun Central, Singapore 768828
Email: jeffrey.renaud@ktph.com.sg











