Has novel coronavirus infection affected the professional identity recognised by medical students? – A historical cohort study
Submitted: 19 May 2022
Accepted: 21 September 2022
Published online: 3 January, TAPS 2023, 8(1), 3-12
https://doi.org/10.29060/TAPS.2023-8-1/OA2817
Junji Haruta1,2, Ayumi Takayashiki2, Ryohei Goto2, Takami Maeno2, Sachiko Ozone2 & Tetsuhiro Maeno2
1Medical Education Center, School of Medicine, Keio University, Japan; 2Department of Primary Care and Medical Education, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan
Abstract
Introduction: The pandemic caused by the novel coronavirus (COVID-19) has produced dramatic changes in the learning environment for clinical practice in medical education, and the impact on medical students has been significant. However, few program evaluation studies involving professional identity, now emphasised in medical education, have compared current with pre-COVID-19 programs. Here, we compared the professional identity recognised by medical students in the years before and during COVID-19.
Methods: Medical students who participated in clinical practice were evaluated using the Japanese version of the Professional Self-Identity Questionnaire (PSIQ), a 9-item inventory rated using 7-point Likert scales. They answered on the first day of a 4-week clinical practice module within a community-based medical education (CBME) program and at graduation in 2018-2019 (pre-COVID-19 pandemic) and in 2019-2020 (during-COVID-19 pandemic). We compared the mean difference in total PSIQ score of the 2019-2020 students to those of the 2018-2019 students as a historical cohort using an unpaired t-test.
Results: Participants were 104 medical students in the 2018-2019 academic year and 92 in the 2019-2020 academic year. PSIQ was increased at graduation. Mean difference in total PSIQ score was statistically higher for the 2019-2020 students (13.5 ± 9.4) than for the 2018-2019 students (10.3 ± 8.1) (t =2.6, df =195, p = 0.01).
Conclusion: Although clinical practice was restricted by COVID-19, this had some positive impact on the strengthening of professional identity recognised by medical students. This finding may have been influenced by the imprinting of professional norms and changes in society.
Keywords: Novel Coronavirus Infection, Professional Identity, Clinical Practice, Questionnaire Survey, Program Evaluation
Practice Highlights
- Professional identity recognised by medical students in Japan was assessed by questionnaire.
- Changes during clinical practice were compared between two grades using a historical cohort.
- Medical students’ recognised professional identity scores improved after one year in both cohorts.
- Medical students experienced the COVID-19 pandemic showed some positive impact on professional identity.
- Medical students internalised their role as healthcare professionals owing to COVID-19 pandemic.
I. INTRODUCTION
The pandemic caused by the novel coronavirus (COVID-19) has caused unprecedented disruption to medical education systems around the world (Kaul et al., 2021; Khasawneh et al., 2020; Lucey & Johnston, 2020; Papapanou et al., 2021). In particular, the pandemic has made it difficult to continue medical educational programs, including regular lectures, and face-to-face lectures, experiments, and clinical practice involving patients (Al Samaraee, 2020; Emanuel, 2020; Shankar & Wilson, 2020). The Association of American Medical Colleges took the unprecedented decision to suspend clinical practice and issued guidance instructing medical students to avoid clinical practice involving direct patient contact (Association of American Medical Colleges, 2020). The many university hospitals in the U.S. have made it a priority to utilise students in controlling the spread of COVID-19 infection. Other countries followed this precedent. Medical students accordingly lost the opportunity to learn through patients in clinical practice. In Japan also, clinical practice was suspended at many universities.
Commonly implemented alternative teaching methods were online interactive discussions and video lectures (Chiodini, 2020; Mian & Khan, 2020). To prevent the spread of COVID-19 from medical students in clinical practice (Alsoghair et al., 2021), students were required to socially distance not only from patients but also from healthcare providers and faculty members. However, implementing the requisite changes to curricula, such as interrupting or drastically postponing clinical practice, was difficult, forcing faculties to develop curricula that provided students with opportunities to supplement their ongoing clinical practice as early as possible, while making use of online devices (Ross, 2020). These changes in the learning environment affected medical students’ learning. For example, a survey of 2nd-6th grade students at the University of Geneva found that 2/3 of the medical students experienced decreased motivation and concentration in distracting learning environments such as home, whereas some medical students who were exposed to clinical practice during the COVID-19 pandemic showed an increased sense of belonging to the profession (Wurth et al., 2022). A change in perception with remote learning in response to the COVID-19 pandemic among Canadian undergraduate students also revealed a significant decrease in students’ achievement goals, engagement, and perceptions of success, and an increase in perceptions of cheating (Daniels et al., 2021). Perceptions of learning due to changes in the curriculum due to COVID-19 have been investigated and controversially reported, but few reports have investigated professional identity as a foundation for becoming a physician.
To be effective clinicians, it is important that medical students acquire not only knowledge and skills but also professional identity formation (Cruess et al., 2014; Hafferty & Franks, 1994). Professional identity is defined as “attitudes, values, knowledge, beliefs, and skills shared with others in a professional group” (Crossley & Vivekananda-Schmidt, 2009). Professional identity formation is noted as an ongoing process influenced by several factors, including practice experience and professional socialisation (Adams et al., 2006). In this study, we adopted a theoretical framework which is based on a concept that illustrates the interplay of professional identity formation and socialisation through a complex conscious and unconscious process centered on role models, mentors, and the accumulation of individual experiences (Cruess et al., 2015). Because clinical practice is a period in which medical students meet role models and mentors and gain their first experiences as a healthcare provider, clinical practice is major contributor to the development of professional identity in medical students (Haruta et al., 2020).
Although studies have reported that medical education programs altered by the COVID-19 pandemic have affected medical students’ perceptions of the role of the physician and their learning strategies (Findyartini et al., 2020; Wurth et al., 2022), little is known about the influence of curricula changes on medical students with regard to their professional identity formation as physicians affected by role models, mentors, and individual experience (Stetson et al., 2020).
Here, we aimed to compare professional identity as a physician as perceived by medical students in clinical practice before and during COVID-19 using the Professional Self Identity Questionnaire (PSIQ).
II. METHODS
A. Setting
Japan first faced the challenge of the COVID-19 pandemic in January 2020, and a state of emergency was declared for all regions of Japan on April 16, 2020 (Prime Minister’s Office of Japan, 2020). During that time, some medical universities suspended clinical training and implemented online education instead. The COVID-19 Outline of Measures for COVID-19 formulated by the Japanese Ministry of Education, Culture, Sports, Science and Technology was sent to all higher education institutions, including medical schools, on June 5, 2020 (Hayashi et al., 2022), with the main advice that universities should operate in a resilient manner for experiential educational practices such as clinical practice. Under these circumstances, leaders of Japanese medical schools were asked to consult various stakeholders and make decisions on whether or not to continue clinical practice, often leaving detailed instructions to local operations managers in each field (Hayashi et al., 2022). In contrast, primary care physicians were forced to adapt to local conditions (Haruta et al., 2021).
Students enter medical school in Japan after graduating from high school, and the curriculum is six years long. Clinical training usually takes place in the fourth to sixth years. This schedule is also implemented at the University of Tsukuba in Japan: clinical training is divided into a first half from October of the fourth year to September of the fifth year and a second half from October of the fifth year to June of the sixth year, for a total of 78 weeks. After clinical training, medical students spend time studying for graduation and national exams, in addition to attending lectures.
The first phase of this clinical practice consists of a four-week rotation in basic departments such as internal medicine, surgery, obstetrics and gynecology, pediatrics, and emergency medicine, mainly at affiliated hospitals. The second phase incorporates some elective subjects and includes 4 weeks’ mandatory clinical practice in a CBME curriculum and a further 4 weeks’ clinical practice in a department of interest. Typically, 15 to 17 students rotate every 4 weeks through clinical practice in the CBME curriculum. This clinical training was conducted before the pandemic, but was discontinued in response to it at the end of March 2020. In March, medical students continued clinical training while all elementary and junior high schools were closed. All clinical training was then cancelled in April 2020 and replaced with report assignments only. These were replaced in May and June with online training and on-demand assignments. Sixth-year students in the class of 2020, and subsequently also in 2021 and 2022, were required to adhere to health observation recording and infection prevention behaviors in accordance with the University of Tsukuba Hospital staff behavior guidelines, which had not been previously followed. Similarly, they were also restricted from participating in training hospital tours and extracurricular activities, which were usually a part of their training.
B. Study Design
Training in clinical practice at the University of Tsukuba consists of a first phase for 4th and 5th year students and a second phase for 5th and 6th year students. CBME is included in the latter phase. Data from 5th-year medical students who participated in clinical practice in a 4-week community-based medical education (CBME) program from October 2019 to March 2020 and who graduated in March 2021 were compared to those of the previous year’s students (2018-2019) as a historical cohort. This cohort included 6th-year medical students who graduated in March 2020 and who had participated in a similar clinical practice program the previous year, from October 2018 to May 2019. As in the 2018-2019 academic year, a questionnaire was administered using the PSIQ in the 2019-2020 academic year. The PSIQ, conducted as part of program evaluation of the CBME program, was administered on the first day of the 4-week clinical practice of the program and at graduation. Study participants included 118 fifth- and sixth-year medical students who participated in clinical practice in the CBME program from October 2018 to May 2019 (pre-COVID-19 pandemic) and 100 fifth- and sixth-year medical students who participated from October 2019 to March 2020 (during-COVID-19 pandemic). The 35 participants from April-May 2020, when the 4-week clinical practice in the CBME program was switched to online practice due to COVID-19, were excluded because they could not be pre-evaluated.
C. Instrument: Japanese Version of the Professional Self Identity Questionnaire (PSIQ)
The Professional Self-Identity Questionnaire (PSIQ) is a 9-item inventory which is rated using 7-point Likert scales (Crossley & Vivekananda-Schmidt, 2009). This instrument measures the sense of students in identifying their current position on a continuum between ‘first-day student’ and ‘qualified doctor’ when engaged in each of nine domains of professional activity. These nine domains include “Teamwork,” “Communication,” “Conducting assessment,” “Cultural awareness,” “Ethical awareness,” “Using records,” “Dealing with emergencies,” “Reflection,” and “Teaching”. Each item is rated on a 7-point Likert scale. For this research, we set 1 point as “equivalent to the first day of clinical practice” and 7 points as “equivalent to the first day of initial residency”. The PSIQ is an assessment sheet form originally designed in English. The original study was validated in a sample of 496 medical students across multiple phases of education, and the overall internal reliability (Cronbach’s alpha) was reported to be 0.93 (Crossley & Vivekananda-Schmidt, 2009). Previously, we developed a Japanese version of the PSIQ and operationally defined PSIQ scores as professional identity as a physician as perceived by medical students. Cronbach’s alpha of the Japanese PSIQ was reported to be 0.93 (Haruta et al., 2021), which allows students to measure changes in their own professional identity by tracking each of the nine professional activities over time. We set the total score on this scale as the main outcome of this study. The study showed that this was a reliable and valid tool for program evaluation during clinical practice (Haruta et al., 2021).
D. Participants and Data Collection
In 2018-2019 (pre-COVID-19 pandemic) and 2019-2020 (during-COVID-19 pandemic), we assessed the professional identity of medical students from October of their fifth year to May of the sixth year using PSIQ. The survey was administered on the first day of clinical practice in the CBME program as PSIQ 1 (September 2018 to May 2019 and September 2019 to March 2020) and at graduation as PSIQ 2 (2020 January, and January 2021) (Figure 1).
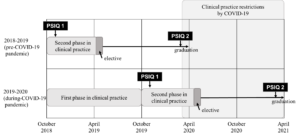
Figure 1. Timing in clinical practice and the PSIQ in 2018-2019 and 2019-2020
On the first day of clinical practice in the CBME program, the authors (JH, TaM, AT) explained the purpose of the study to the students. The authors informed the students that the study would be undertaken as a program evaluation and research, and that their grades would not be influenced in case they did not agree to participate. Those students who agreed to participate signed a consent form giving permission to use their data. Subsequently, the authors asked medical students to fill out the PSIQ as a paper-based, self-administered questionnaire, and to include their student ID number. At graduation, all medical students completed the PSIQ on the internet or on paper as a self-administered questionnaire, again with their student ID number. The study was approved by the Ethics Committee of the University of Tsukuba (No. 1329).
E. Data Analysis
To evaluate the differences in total PSIQ and scores for each item between the first day of clinical practice in the CBME program and the time of graduation, effect sizes (Cohen’s d) were determined for the total PSIQ and scores for each item. In addition, the Shapiro-Wilk test was performed to determine data distribution. For comparison of means for the difference in total PSIQ between 2018-2019 and 2019-2020, an unpaired t-test was applied. The Shapiro-Wilk test confirmed that data distribution for both PSIQ 1 and 2 were not normal. However, since the distribution of PSIQ 2-1 was consistent with normality, a t-test was employed. Missing values were excluded. Data analysis was conducted using SPSS ver. 26 with significance set at the p<0.05 level for total scores as the primary outcome of the PSIQ. Additionally, to deal with the possibility of multiplicity in the simultaneous assessment of each item score, significance levels were Bonferroni corrected, with p< 0.005 (Lee & Lee, 2018).
III. RESULTS
As shown in Table 1, participants analysed in the 2018-2019 academic year (pre-COVID-19 pandemic) included 104 medical students (response rate: 88.1%) who responded at both time points (first day of clinical practice in the CBME program and at graduation), 33 of whom were female. In the 2019-2020 academic year (during-COVID-19 pandemic), 92 medical students (response rate: 92.0%) who responded at both time points were included, 33 of whom were female. One student who did not give consent to have their data used in this study was excluded.
|
2018-2019 (pre-COVID-19 pandemic) |
2019-2020 (during-COVID-19 pandemic) (n=92) |
|
|
Age, mean ± standard deviation |
20.6±1.5 |
21.2±3.4 |
|
Gender, number of persons (%) |
||
|
Male |
66 (63.5) |
51 (55.4) |
|
Female |
33 (31.7) |
33 (35.9) |
|
Unknown |
5 (4.8) |
8 (8.7) |
Table 1. Characteristics of medical students included in the analysis
Table 2 shows that the means of total PSIQ scores and each PSIQ item for 2018-2019 and 2019-2020 were increased at graduation. A comparison of the mean for the difference using the unpaired t-test in total PSIQ score for 2018-2019 and 2019-2020 revealed that it was statistically higher for the 2019-2020 students (13.5 ± 9.4) than for the 2018-2019 students (10.3 ± 8.1) (t =2.6, df =195, p = 0.01). However, there were no statistically significant differences using the unpaired t-test with Bonferronni correction at a 0.005 level of significance in mean scores for 9 items of the PSIQ, namely “Teamwork” (t=0.96 df=195, p=0.341), “Communication” (t=1.84, df=195, p=0.068), “Conducting assessment” (t=2.31, df=195, p=0.24) “Cultural awareness” (t=1.41, df=195, p=0.022), “Ethical awareness” (t=2.25, df=195, p=0.161), “Using records” (t=2.67, df=195, p=0.026), “Dealing with emergencies” (t=2.33, df=195, p=0.008), “Reflection” (t=2.32, df=195, p=0.021) and “Teaching” (t=2.19, df=195, p=0.030). The effect size (Cohen’s d) for total PSIQ scores from the first day of clinical practice in the CBME program to graduation was Δ1.3 in 2018-2019 and Δ1.4 in 2019-2020. The effect size (Cohen’s d) for each item of the PSIQ was Δ1.4 in 2018-2019. Range for items was Δ0.8-1.1 in 2018-2019 and Δ0.9-1.2 in 2019-2020.
|
|
Fiscal year (usually April 1 to March 31) |
First day of the CBME program (1) |
At graduation (2) |
Mean difference in PSIQ (2)-(1) |
t score |
Df |
p-value |
Cohen’s d |
|
Total score (Main outcome) |
2018-2019 (pre-COVID-19 pandemic) |
28.5±7.6 |
38.8±8.5 |
10.3±8.1 |
2.60 |
195 |
0.01 |
1.3 |
|
2019-2020 (during-COVID-19 pandemic) |
28.0±6.6 |
41.6±9.2 |
13.5±9.4 |
1.4 |
||||
|
Sub-analysis |
|
|
||||||
|
Teamwork |
2018-2019 |
3.0±1.2 |
4.4±1.0 |
1.4±1.2 |
0.96 |
195 |
0.341 |
1.1 |
|
2019-2020 |
3.0±1.1 |
4.6±1.1 |
1.6±1.3 |
1.2 |
||||
|
Communication |
2018-2019 |
3.7±1.1 |
4.7±1.1 |
1.0±1.2 |
1.84 |
195 |
0.068 |
0.8 |
|
2019-2020 |
3.5±1.1 |
4.9±1.1 |
1.4±1.3 |
1 |
||||
|
Conducting assessment |
2018-2019 |
3.2±1.0 |
4.4±1.1 |
1.2±1.2 |
2.27 |
195 |
0.024 |
1 |
|
2019-2020 |
3.1±1.0 |
4.7±1.1 |
1.6±1.3 |
1.2 |
||||
|
Cultural awareness |
2018-2019 |
2.9±1.1 |
4.2±1.3 |
1.3±1.3 |
2.31 |
195 |
0.022 |
1 |
|
2019-2020 |
2.8±1.1 |
4.5±1.3 |
1.8±1.5 |
1.2 |
||||
|
Ethics awareness |
2018-2019 |
3.4±1.2 |
4.5±1.1 |
1.1±1.3 |
1.41 |
195 |
0.161 |
0.9 |
|
2019-2020 |
3.5±1.2 |
4.9±1.1 |
1.4±1.4 |
1 |
||||
|
Using record entries |
2018-2019 |
3.4±1.0 |
4.5±1.1 |
1.0±1.1 |
2.25 |
195 |
0.026 |
0.9 |
|
2019-2020 |
3.4±0.9 |
4.8±1.1 |
1.4±1.3 |
1.1 |
||||
|
Dealing with emergencies |
2018-2019 |
2.5±1.1 |
3.8±1.3 |
1.3±1.2 |
2.67 |
195 |
0.008 |
1.1 |
|
2019-2020 |
2.3±1.2 |
4.1±1.4 |
1.9±1.7 |
1.1 |
||||
|
Reflection |
2018-2019 |
3.3±1.1 |
4.3±1.1 |
1.0±1.3 |
2.32 |
195 |
0.021 |
0.8 |
|
2019-2020 |
3.2±0.9 |
4.6±1.3 |
1.4±1.5 |
1 |
||||
|
Teaching |
2018-2019 |
3.1±0.9 |
4.1±1.1 |
0.9±1.1 |
2.19 |
195 |
0. 030 |
0.8 |
|
2019-2020 |
3.2±1.0 |
4.5±1.2 |
1.3±1.4 |
1 |
Table 2. Unpaired t-test analysis and effect sizes for the Professional Identity Self-Assessment Form
IV. DISCUSSION
We found that the means of total and each PSIQ score of medical students who graduated during the COVID-19 pandemic were statistically increased compared to those of students graduating before the pre-COVID-19 pandemic. These findings indicate that, compared with students in the preceding year, the COVID-19 pandemic had a certain positive impact on professional identity formation in medical students with regard to clinical practice.
Considering the framework we used, in which the interaction and reflection of role models, mentors, and individual experiences are key, we believe that all participants were influenced by COVID-19. In addition, professional identity formation is reported to be strongly influenced by environment, context, and other personal variables. (Jarvis-Selinger et al., 2012) The increase in total PSIQ score from the previous year’s medical students may have been due not only to changes in clinical practice, but also to changes in what is expected of medical students by the university hospital and society. In light of these factors, medical students had fewer opportunities to acquire the knowledge and skills required of physicians in the clinical setting directly from role models and mentors, but may nevertheless have been affected by compliance with COVID-19 control measures conducted by the university hospital, and thereby followed the norms of medical professionals communicated through intentional and unintentional messaging. In addition, with the all-engrossing impact of the COVID-19 pandemic throughout society, we speculate that at least some of the students in the COVID-19 group were consulted by family and social contacts as experts and authorities on a daily or more frequent basis, and that such constant reinforcement might also have encouraged PIF. That is, medical students under the COVID-19 pandemic may have internalised the values and norms of the medical professional (Kinnear et al., 2021). Since professional identity formation involves social and relational factors, it is possible that the students’ life and social changes due to COVID-19 reinforced their recognised professional identity (Goldie, 2012).
The more uncertain and ambiguous the period, the more important reflection becomes in PIF. To cope with such uncertainties as the transition from the classroom curriculum to online platforms, rapid changes in the clinical practice environment, and the isolation caused by social distancing, medical students need a well-formed professional identity and socialisation practices (Costello, 2005). Poor PIF is reported to manifest in burnout (Abedini et al., 2018), and depression and anxiety disorders have increased in COVID-19 (Daniels et al., 2021). Since a core component of PIF is the acceptance of uncertainty and ambiguity, medical educators may have provided reflection opportunities for medical students to consciously consider the social factors manifested in COVID-19, such as individual and professional duties, resource priorities, and health disparities, all of which have a positive impact on PIF and socialisation (Stetson et al., 2020). Alternatively, emotion-focused coping strategies (e.g., arts engagement) and problem-solving strategies (e.g., volunteering) to reduce medical students’ anxiety, fear, and stress may be effective (Moula et al., 2022). Students require time and space to reflect on their emergent identity as professionals in these crisis situations (Moula et al., 2022). The extended time for independent learning may have allowed the students to subconsciously reflect on their professional identity, taking seriously the changes in society caused by COVID-19. PIF scores may have accordingly increased in this study.
In general, medical teachers should have made efforts to promote medical students’ professional identity formation even during the COVID-19 pandemic (Goldhamer et al., 2020). Professional identity formation is not a process that should be left to chance; it should be explicitly supported through systematic support and curriculum initiatives (Cruess et al., 2015; Schumacher et al., 2012). In reality, it is necessary to require rapid changes in clinical practice to prevent infection caused by COVID-19, and it has been difficult to promote systematic support for professional identity formation for medical students. However, COVID-19 might not have negatively affected the professional identity recognised by medical students who were in clinical practice immediately after the pandemic. The efforts of Japanese medical educators to implement online and other types of learning to replace clinical practice, and the well-considered efforts of faculty to make clinical practice as feasible as possible may have served as role models or mentors, and influenced medical students’ professional identity formation.
This study has three limitations. First, because there was a difference of 8-17 months between the first day of clinical practice in the CBME program and graduation, given that more clinical practice experience may strengthen the professional identity recognised by medical students, it is possible that differences in clinical practice experience may have affected PSIQ scores. Second, extrapolation from this study should be done with care, since it is a comparison of a one-year questionnaire survey at a single university. Third, a degree of response bias may be present due to the self-reporting design, with inclusion of student ID number. Fourth, evaluation at three or more points may allow a more precise comparison of changes, given that professional identity formation is a dynamic process. Even allowing for these limitations, our findings provide meaningful feedback to medical students and faculty, particularly given the paucity of studies evaluating and comparing changes in professional identity formation – which consists of multiple factors – before and during the COVID-19 pandemic. For the future of medical education, it is imperative to track the professional identity recognised by physicians whose student experience in clinical practice was restricted under the COVID-19 pandemic, and was accordingly significantly changed compared with other years.
V. CONCLUSION
Comparison of the professional identity recognised by medical students whose experience of clinical practice was affected by the COVID-19 pandemic to that of students in the previous year showed some positive impact on professional identity. This lack of negative difference in recognised professional identity even under restricted clinical practice may have been influenced by the imprinting of professional norms and changes in society.
Notes on Contributors
JH, AT, SO, TaM and TeM were involved in the conception and design of this study. JH, AT, and TaM collected the data. JH and RG conducted data analysis. JH mainly wrote the paper. AT, SO, TaM and TeM gave critical feedback on the manuscript. All authors have read and approved the final manuscript.
Ethical Approval
This study was approved by the Ethics Committee of the University of Tsukuba’s Faculty of Medicine and Medical Sciences (No. 1329). All participants have given written consent for their data to be used in the research and for publication.
Data Availability
It is not possible to share data since we did not obtain consent from participants to share all data collected.
Acknowledgement
We thank the faculty staff members Shoji Yokoya, Hisashi Yoshimoto, Shogen Suzuki, Naoto Sakamoto, Yu Yamamoto, Yoshihiro Kataoka, Shoichi Masumoto, Haruka Kuno, Takashi Inaba, Shuhei Hamada, Shogo Kawada, and Sayaka Nin of the Department of Primary Care and Medical Education, Faculty of Medicine, University of Tsukuba. Additionally, we thank the healthcare staff who taught the medical students at the CBME program sites in clinical practice.
Funding
This study was funded by the education/research fund of Department of Primary Care and Medical Education, Faculty of Medicine, University of Tsukuba.
Declaration of Interest
There are no companies or other entities with which the authors have conflict of interest relationships that should be disclosed in relation to the content of the paper.
References
Abedini, N. C., Stack, S. W., Goodman, J. L., & Steinberg, K. P. (2018). “It’s not just time off”: A framework for understanding factors promoting recovery from burnout among internal medicine residents. Journal of Graduate Medical Education, 10(1), 26–32. https://doi.org/10.4300/JGME-D-17-00440.1
Adams, K., Hean, S., Sturgis, P., & Clark, J. M. (2006). Investigating the factors influencing professional identity of first-year health and social care students. Learning in Health and Social Care, 5(2), 55–68. https://doi.org/10.1111/j.1473-6861.2006.00119.x
Al Samaraee, A. (2020). The impact of the COVID-19 pandemic on medical education. British Journal of Hospital Medicine, 81(7), 1-4. https://doi.org/10.12968/HMED.2020.0191
Alsoghair, M., Almazyad, M., Alburaykan, T., Alsultan, A., Alnughaymishi, A., Almazyad, S., Alharbi, M., Alkassas, W., Almadud, A., & Alsuhaibani, M. (2021). Medical Students and COVID-19: Knowledge, preventive behaviors, and risk perception. International Journal of Environmental Research and Public Health, 18(2), 842. https://doi.org/10.3390/ijerph18020842
Association of American Medical Colleges. (2020). Guidance on medical students’ participation in direct in-person patient contact activities. https://www.aamc.org/system/files/2020-08/meded-August-14-Guidance-on-Medical-Students-on-Clinical-Rotations.pdf
Chiodini, J. (2020). Online learning in the time of COVID-19. Travel Medicine and Infectious Disease, 34, Article 101669. https://doi.org/10.1016/j.tmaid.2020.101669
Costello, C. Y. (2005). Professional identity crisis: Race, class, gender, and success at professional schools. Vanderbilt University Press.
Crossley, J., & Vivekananda-Schmidt, P. (2009). The development and evaluation of a professional self identity questionnaire to measure evolving professional self-identity in health and social care students. Medical Teacher, 3(12), e603–e607. https://doi.org/10.3109/01421590903193547
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2014). Reframing medical education to support professional identity formation. Academic Medicine, 89(11), 1446–1451. https://doi.org/10.1097/ACM.0000000000000427
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2015). A schematic representation of the professional identity formation and socialization of medical students and residents: A guide for medical educators. Academic Medicine, 90(6), 718–725. https://doi.org/10.1097/ACM.0000000000000700
Emanuel, E. J. (2020). The inevitable reimagining of medical education. JAMA, 323(12), 1127–1128. https://doi.org/10.1001/jama.2020.1227
Findyartini, A., Anggraeni, D., Mikhael Husin, J., & Greviana, N. (2020). Exploring medical students’ professional identity formation through written reflections during the COVID-19 pandemic. Journal of Public Health Research, 9(s1), 1918. https://doi.org/10.4081/jphr.2020.1918
Goldhamer, M. E. J., Pusic, M. V., Co, J. P. T., & Weinstein, D. F. (2020). Can covid catalyze an educational transformation? Competency-based advancement in a crisis. New England Journal of Medicine, 383(11), 1003–1005. https://doi.org/10.1056/NEJMP2018570
Goldie, J. (2012). The formation of professional identity in medical students: Considerations for educators. Medical Teacher, 34(9), e641–e648. https://doi.org/10.3109/0142159X.2012.687476
Hafferty, F. W., & Franks, R. (1994). The hidden curriculum, ethics teaching, and the structure of medical education. Academic Medicine, 69(11), 861–871. https://doi.org/10.1097/00001888-199411000-00001
Haruta, J., Maeno, T., Takayashiki, A., Goto, R., Ozone, S., & Maeno, T. (2021). Validation of the professional self-identity questionnaire for medical students during clinical practice in Japan. International Journal of Medical Education, 12, 160–165. https://doi.org/10.5116/ijme.610d.104b
Haruta, J., Ozone, S., & Hamano, J. (2020). Doctors’ professional identity and socialisation from medical students to staff doctors in Japan: Narrative analysis in qualitative research from a family physician perspective. BMJ Open, 10(7), e035300. https://doi.org/10.1136/bmjopen-2019-035300
Hayashi, M., Saiki, T., Kanter, S. L., & Ho, M. J. (2022). Leaders’ perspectives and actions to manage challenges in medical education presented by the COVID-19 pandemic: A nationwide survey of Japanese medical colleges. BMC Medical Education, 22(1), 144. https://doi.org/10.1186/s12909-022-03193-1
Jarvis-Selinger, S., Pratt, D. D., & Regehr, G. (2012). Competency is not enough: Integrating identity formation into the medical education discourse. Academic Medicine, 87(9), 1185–1190. https://doi.org/10.1097/ACM.0b013e3182604968
Kaul, V., Gallo de Moraes, A., Khateeb, D., Greenstein, Y., Winter, G., Chae, J. M., Stewart, N. H., Qadir, N., & Dangayach, N. S. (2021). Medical education during the COVID-19 pandemic. CHEST, 159(5), 1949–1960. https://doi.org/10.1016/j.chest.2020.12.026
Khasawneh, A. I., Humeidan, A. A., Alsulaiman, J. W., Bloukh, S., Ramadan, M., Al-Shatanawi, T. N., Awad, H. H., Hijazi, W. Y., Al-Kammash, K. R., Obeidat, N., Saleh, T., & Kheirallah, K. A. (2020). Medical students and COVID-19: Knowledge, attitudes, and precautionary measures. A descriptive study from Jordan. Frontiers in Public Health, 8, 253. https://doi.org/10.3389/fpubh.2020.00253
Kinnear, B., Zhou, C., Kinnear, B., Carraccio, C., & Schumacher, D. J. (2021). Professional identity formation during the COVID-19 pandemic. Journal of Hospital Medicine, 16(1), 44–46. https://doi.org/10.12788/jhm.3540
Lee, S., & Lee, D. K. (2018). What is the proper way to apply the multiple comparison test? Korean Journal of Anesthesiology, 71(5), 353-360. https://doi.org/10.4097/KJA.D.18.00242
Lucey, C. R., & Johnston, S. C. (2020). The transformational effects of COVID-19 on medical education. JAMA, 324(11), 1033–1034. https://doi.org/10.1001/jama.2020.14136
Mian, A., & Khan, S. (2020). Medical education during pandemics: A UK perspective. BMC Medicine, 18(1), 100. https://doi.org/10.1186/s12916-020-01577-y
Moula, Z., Horsburgh, J., Scott, K., Rozier-Hope, T., & Kumar, S. (2022). The impact of COVID-19 on professional identity formation: An international qualitative study of medical students’ reflective entries in a global creative competition. BMC Medical Education, 22(1), 545. https://doi.org/10.1186/s12909-022-03595-1
Papapanou, M., Routsi, E., Tsamakis, K., Fotis, L., Marinos, G., Lidoriki, I., Karamanou, M., Papaioannou, T. G., Tsiptsios, D., Smyrnis, N., Rizos, E., & Schizas, D. (2021). Medical education challenges and innovations during COVID-19 pandemic. Postgraduate Medical Journal, 98, 321-327. https://doi.org/10.1136/postgradmedj-2021-140032
Prime Minister’s Office of Japan. (2020). [COVID-19] Declaration of a state of emergency in response to the Novel Coronavirus Disease. https://japan.kantei.go.jp/ongoingtopics/_00020.html
Ross, D. A., & the members of National Neuroscience Curriculum Initiative “Quarantine Curriculum” Committee (2020). Creating a “Quarantine Curriculum” to enhance teaching and learning during the COVID-19 pandemic. Academic Medicine, 95(8), 1125–1126. https://doi.org/10.1097/ACM.0000000000003424
Schumacher, D. J., Slovin, S. R., Riebschleger, M. P., Englander, R., Hicks, P. J., & Carraccio, C. (2012). Perspective: Beyond counting hours: The importance of supervision, professionalism, transitions of care, and workload in residency training. Academic Medicine, 87(7), 883–888. https://doi.org/10.1097/ACM.0b013e318257d57d
Shankar, P. R., & Wilson, I. G. (2020). The COVID-19 pandemic and undergraduate medical student teaching-learning and assessment. Canadian Medical Education Journal, 12(1), e190–e191. https://doi.org/10.36834/cmej.70800
Stetson, G. V., Kryzhanovskaya, I. V., Lomen-Hoerth, C., & Hauer, K. E. (2020). Professional identity formation in disorienting times. Medical Education, 54(8), 765–766. http://doi.org/10.1111/medu.14202
Wurth, S., Sader, J., Cerutti, B., Broers, B., Nadia Bajwa, M., Carballo, S., Escher, M., Galetto-Lacour, A., Grosgurin, O., Lavallard, V., Savoldelli, G., Serratrice, J., Nendaz, M., & Audétat-Voiro, M. C. (2022). Correction to: Medical students’ perceptions and coping strategies during the first wave of the COVID-19 pandemic: Studies, clinical implication, and professional identity. BMC Medical Education, 22(1), Article 232. https://doi.org/10.1186/s12909-022-03307-9
*Junji Haruta
35 Shinanomachi Shinjukuku Tokyo
160-8582, Japan
Email: junharujp@keio.jp
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









