From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality
Submitted: 6 June 2024
Accepted: 3 September 2024
Published online: 7 January, TAPS 2025, 10(1), 10-16
https://doi.org/10.29060/TAPS.2025-10-1/RA3430
Han Ting Jillian Yeo, Dujeepa D. Samarasekera & Shuh Shing Lee
Centre for Medical Education (CenMED), Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Despite significant efforts to address gender equality in medical education, the issue persists. The narrative review aimed to address the research question: What are the strategies implemented to address issues of gender inequality in medical education and what were their outcomes?
Methods: Seven major electronic databases of CINAHL, Embase, ERIC, PsyInfo, PubMed, SCOPUS and Web of Science were reviewed. Search phrases used were (Medical education) AND (Gender equality) OR (Gender bias) OR (Gender diversity) OR (Gender discrimination). Original research articles were included, together with systematic reviews with outcomes reporting on strategies to address gender equality.
Results: Articles unrelated to medical education (e.g. allied health and nursing education) and non-English articles were excluded from the study. A total of 1248 articles were identified, and 23 articles met the inclusion criteria. Training programs (n=14; 60.8%) for medical students and faculty have successfully increased awareness on the issues of gender equality and boost confidence in handling cases on gender inequality, yet implicit bias remains with leadership continuing to be associated more strongly with males.
Conclusion: Leadership bodies in Institutions of Higher Education and policymakers would be in an ideal position to address these issues through shaping policies and provision of training for hiring bodies and faculty.
Keywords: Medical Education, Gender Equality, Strategies
Practice Highlights
- Training programs for medical students and faculty can increase awareness of gender equality.
- Structural and cultural barriers preventing women from attaining leadership roles remain entrenched.
- Targeted training for hiring committees and faculty can help mitigate implicit biases.
I. INTRODUCTION
There has been significant progress in the landscape of medical education since 2000 as women’s representation in health professions has increased steadily across the globe. In 2019, nearly half of all doctors in countries in the Organisation for Economic Co-operation and Development were women (Organisation for Economic Co-operation and Development, 2022). However, beneath the surface of this endeavor lies a persistent and pervasive issue concerning gender equality. The World Health Organisation (WHO) (2007) defines gender equality as the absence of discrimination in the allocation of benefits or resources, access to services, or the provision of opportunities based on a person’s sex, thereby enabling individuals to achieve their full potential. Efforts have been made towards achieving gender equality and inclusivity. Changes in the recruitment processes of residency programs in the United States and Canada have shown an increasing ratio of females among residents and faculty (Jain et al., 2022; Ying et al., 2023). Studies evaluating the assessments of medical students and residents have suggested reduced biases in scorings of examinees based on gender (Hannon et al., 2021; Jacques et al., 2016).
Yet, gender inequality remains prevalent in other aspects of medical education. Sexual harassment in the form of sexist behavior or comments were commonly reported among females in the workplace during residency trainings (DeWane et al., 2020; Ellis et al., 2019; Jackson & Drolet, 2021). Learning opportunities were unequal as female residents performed disproportionately lesser number of procedures (Olson et al., 2023; Sobel et al., 2023) and were given less operative autonomy as compared to their male counterparts hence affecting their preparedness for practice (Joh et al., 2020; Meyerson et al., 2019). The impact of gender inequality is far-reaching. Negative emotions, such as helplessness, and lowered self-esteem, were often described by students or residents who had experienced or observed gender inequality (Kristoffersson et al., 2016; Madeeh Hashmi et al., 2013). Additionally, lowered job satisfaction, feelings of burnout and an increased risk of attrition were reported among those who have experienced or observed gender inequality (Bruce et al., 2015; Ellis et al., 2019; Jackson & Drolet, 2021).
Achieving gender equality in medical education is critical, however, literature highlighted that it continues to persist despite various interventions. Numerous studies have documented progress in gender equality following the implementation of specific interventions, but there is a scarcity of comprehensive reviews consolidating these efforts. Hence, this narrative review aimed to address the research question: What are the strategies implemented to address issues of gender inequality in medical education and what were their outcomes?
II. METHODS
A narrative review was conducted based on the framework proposed by Ferrari (2015). Two researchers (SSL and JYHT) searched seven major electronic databases of CINAHL, Embase, ERIC, PsyInfo, PubMed, SCOPUS and Web of Science for the English-language articles or articles which were translated to English and published between 2013 to 2023. The search terms were broadened using the Boolean operator (“OR/AND”) to search the ‘medical’ subject heading (MeSH) to recognise the significance of the study. As a result, the search phrases were (Medical education) AND (Gender equality) OR (Gender bias) OR (Gender diversity) OR (Gender discrimination).
Original research articles were included into the study, together with systematic reviews with outcomes reporting on strategies to address gender equality. Articles unrelated to medical education (e.g. allied health and nursing education) and non-English articles were excluded from the study. Figure 1 showed a flow chart of the process of literature selection for the narrative review.
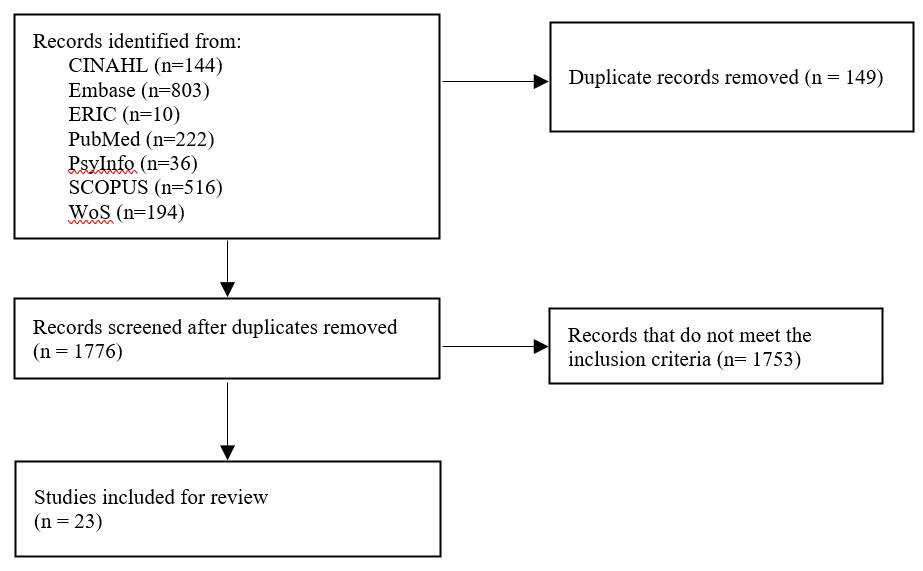
Figure 1. Flow diagram showing the selection of articles
Based on the inclusion and exclusion criteria outlined, both researchers (SSL and JYHT) independently reviewed the title and abstracts of all articles and reviewed the full article when necessary. Articles were categorised based on the types of strategies that were implemented, target audient, method of evaluation and evaluation findings.
III. RESULTS
After removing duplicate articles, a total of 1248 articles were identified through the literature search strategy. Following a thorough examination of the titles and abstracts as well as a review of the articles’ references lists, 23 articles met the review criteria (Table 1). Articles were published between 2015 to 2022. Majority of studies were conducted in the United States (n=16), Canada (n=1), United States and Canada (n=1), Germany (n=1), Sweden (n=1), Switzerland (n=1), Taiwan (n=1), and United Kingdom (n=1).
The findings from this narrative review were divided into two sections: (1) an overview of the interventions implemented to address gender equality and (2) an evaluation of the interventions implemented.
A. Interventions Implemented to Address Gender Equality
Interventions implemented could be divided into micro, meso and macro levels interventions to address gender equality. Micro levels interventions focused on supporting individuals in understanding concepts on gender bias and diversity, its impact on the workplace and strategies to overcome gender bias. These aims could be achieved through training programs for faculty and medical students (n=14; 60.8%). Other micro level interventions described in the articles included giving doctors labelled badges and empowering residents to nominate their chief resident (Olson et al., 2022).
Meso level interventions focused on improving the institutions’ systems, structures, and procedures. Two articles described the formation of task forces in medical societies and higher education institutions (HEIs) to monitor trends and address gender issues (Kandi et al., 2022; Lieberman et al., 2018). Holding a public symposium as a platform to discuss issues on gender equality and enforcing guidelines on writing letter recommendations for medical residency applications were other meso level interventions (Sakowski et al., 2020; Zhang et al., 2021).
Macro level interventions involved shaping policies on a broader, national, or international scale. One study by Chang et al. (2020) shared on three national career developments program aimed at increasing women faculty professional effectiveness. Another macro level intervention involved awarding institutions with Bronze, Silver, and Gold for efforts in addressing gender equity (Caffrey et al., 2016).
The target audience for most interventions were medical students (n=7), these included interventions tailored for women medical students. Other main target audiences included faculty (n=4), residents (n=3) and HEIs (n=2).
B. Addressing Gender Inequality through Training Programs
The duration of the 15 training programmes specified spanned from 15 minutes to 15 weeks long. Seven training programs targeted medical students, 4 training programs targeted faculty, 2 training programs targeted internal medical residents.
Training programs primarily focused on creating an awareness of gender inequality in the workplace through defining terminologies surrounding gender inequality, showing data on gender inequality and its impact on the workplace (Carnes et al., 2015; Driscoll et al., 2019; Farkas et al., 2022; Girod et al., 2016; Jacobs et al., 2022; Kisiel et al., 2020; Lattanza et al., 2016; Sabin et al., 2022). Five programs shared strategies and frameworks to handle situations insinuating gender inequality in the workplace and provided opportunities for practice (Bromberg et al., 2022; Carnes et al., 2015; Farkas et al., 2022; Jacobs et al., 2022; Sabin et al., 2022). Five training programs incorporated elements to guide participants on their career progression through networking opportunities, mentorship programs and leadership training (Chang et al., 2020; Deng et al., 2021; Gaida et al., 2020; Harbold et al., 2021; Lattanza et al., 2016). Training programs developed as part of the Perry’s Initiative for women medical students provided hands-on opportunities to engage in operative procedures to encourage more females to enter the field of orthopaedic surgery (Harbold et al., 2021; Lattanza et al., 2016). Two training programs adopted the approach of engaging in reflexivity with a gendered perspective into one’s own practice and literature materials (Geiser et al., 2022; Liao & Wang, 2020).
C. Evaluation and Findings on the Strategies Implemented
The Kirkpatrick model was adopted to categorise how evaluation of interventions was conducted and the findings.
1) Kirkpatrick Level 1 – Reaction: Participants’ reactions were evaluated for the following strategies: workshops, public symposium, recognition of efforts and empowerment to nominate chief residents (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). Participant satisfaction surveys were the main tool adopted to determine if participants found the strategies useful and identify areas for improvement (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). One qualitative study by Caffrey et al. (2016) used semi-structured interviews. In general, the interventions were perceived positively in all articles (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). However, one study by Caffrey et al. (2016) focusing on recognising institutions which promote gender equity had reported a higher and disproportionate workload on women who were involved in the application process.
2) Kirkpatrick Level 2 – Learning: Participants in 6 studies reported an increased awareness of gender bias after workshops were conducted (Caffrey et al., 2016; Carnes et al., 2015; Deng et al., 2021; Girod et al., 2016; Liao & Wang, 2020; Sabin et al., 2022). Awareness of gender bias can be described in different facets: (1) having an understanding that society has yet to provide equal opportunities for all regardless of their backgrounds; and (2) gaining awareness on the presence of socially constructed gender norms. Two workshops had reported an increase in internal medicine residents’ confidence in responding to incidences related to gender inequality (Bromberg et al., 2022; Farkas et al., 2022).
While strategies had largely positive outcomes with regards to learning, Carnes et al. (2015) and Girod et al. (2016) revealed that workshops on gender bias led to no significant differences in gender/ leadership Implicit Association Test scores suggesting that there remains a persistent association of leadership with males more than females. Gaida, Kujumdshiev and Stengler (2020) shared that low numbers of medical students were able to identify gender sensitive topics despite a week-long elective course on issues of gender equality supported by a mentorship program.
3) Kirkpatrick Level 3 – Behaviour: Reviewed literature revealed conflicting findings on the impact of the interventions on participants’ behaviour. Interventions made to medical assessments (unconscious bias training of examiners, structured interview formats for interviewers and guidelines for writing letter of recommendations) observed no changes in scores and biased language used (Driscoll et al., 2019; Langhan et al., 2022; Zhang et al., 2021).While Olson et al. (2022) had shown a reduction in reported events on gender bias, Kisiel et al. (2020) reported an increase in sexual harassment and gender discrimination events attributing it to an increased awareness in such behaviours.
4) Kirkpatrick Level 4 – Results: Studies which evaluated the overall impact of the interventions on organizational structure showed optimistic results. Articles introducing the Perry’s Initiative to increase women medical students’ exposure to orthopaedic surgery and engineering reported an increased match rates of alumni students to orthopaedics (Harbold et al., 2021; Lattanza et al., 2016). Training of faculty search committee member yielded an increase in number of female candidates throughout the entire hiring process and eventually positions offered to them (Jacobs et al., 2022). Chang et al. (2020) also reported higher rates of promotion for women faculty who had participated in national career development programs.
IV. DISCUSSION
The review highlighted that training programs for students and faculty were not only positively received by students and faculty but were able to create awareness on gender inequality and boost confidence in handling cases on gender inequality. Yet faculty training programs failed to address the implicit bias among faculty who tend to associate leadership with male more than female. This was concurred by more recently published literature reporting that females hold fewer leadership positions in academia or residency programs and hence having potential implications on their career advancement opportunities (Dhingra et al., 2021; Sethi et al., 2022). Achieving gender equality in leadership body is important. The presence of female in any leadership position was correlated with an increase in the number of female faculty or female fellows (Sethi et al., 2022; Sulibhavi et al., 2021). One study also suggested that an increase in the number of female surgical faculty was correlated a decrease in attrition among residents (Saberi et al., 2021).
Macro and meso level interventions via implementation of career development programs and training of recruitment committee showed far reaching impacts on increasing diversity of hires and promotional rates of female faculty. This could serve as a guidance to the leadership bodies in HEIs that the engagement of targeted interventions on training hiring bodies and the provision of faculty development to women faculty can they level the playing field for both genders. Till date few studies reviewed the impact of macro level intervention, and perhaps by sharing the policies in place for training faculty and hiring bodies can the society see an exponential impact on addressing the issues of gender equality.
Lastly, it was evident from the review of selected literature that most research in the areas of gender quality was conducted in the Global North. Given that issues on gender equality tend to be contextual and cultural in nature, there would be a need for medical educators in the Global South to engage in scholarly work in this domain to identify the issues on the ground and identify targeted ways to address the issues on hand.
V. CONCLUSION
While training programs for medical students and faculty have successfully increased awareness of gender equality issues, implicit bias persists, particularly concerning female representation in leadership positions. Despite heightened awareness, the structural and cultural barriers preventing women from attaining leadership roles remain firmly entrenched. Leadership bodies within HEIs and policymakers are uniquely positioned to address these persistent issues. By shaping and implementing equitable policies, they can foster an environment that actively promotes gender diversity. Additionally, targeted training for hiring committees and faculty can help mitigate implicit biases, ensuring a more inclusive and representative leadership. Addressing these challenges requires a multifaceted approach, combining policy reform, education, and continuous evaluation to create lasting change in gender equality within medical education.
Notes on Contributors
Ms. Jillian Yeo was involved in writing the manuscript, conducting the literature search, reviewing the literature retrieved and synthesising the data. Dr Lee Shuh Shing was involved in conducting the literature search, reviewing the literature retrieved and synthesising the data. Dr Dujeepa was involved in the conceptual development of the study and reviewing the manuscript.
Ethical Approval
As this study was a narrative review, ethical approval and IRB application was not required.
Data Availability
The list of articles included in the narrative review can be accessed here:
https://doi.org/10.6084/m9.figshare.25980352.v1 (Yeo, 2024)
Funding
No funding sources are associated with this paper.
Declaration of Interest
There are no conflicts of interests related to the content presented in the paper.
References
Bromberg, G. K., Gay, E. A., Hills-Dunlap, K., & Burnett-Bowie, S. M. (2022). Using a virtual platform to teach residents how to respond to bias. Journal of General Intern Medicine, 37(11), 2871-2872. https://doi.org/10.1007/s11606-021-07156-y
Bruce, A. N., Battista, A., Plankey, M. W., Johnson, L. B., & Marshall, M. B. (2015). Perceptions of gender-based discrimination during surgical training and practice. Med Education Online, 20, 25923. https://doi.org/10.3402/meo.v20.259 23
Caffrey, L., Wyatt, D., Fudge, N., Mattingley, H., Williamson, C., & McKevitt, C. (2016). Gender equity programmes in academic medicine: A realist evaluation approach to Athena SWAN processes. BMJ Open, 6(9), e012090. https://doi.org/10.1136/bmjopen-2016-012090
Carnes, M., Devine, P. G., Baier Manwell, L., Byars-Winston, A., Fine, E., Ford, C. E., Forscher, P., Isaac, C., Kaatz, A., Magua, W., Palta, M., & Sheridan, J. (2015). The effect of an intervention to break the gender bias habit for faculty at one institution: A cluster randomised, controlled trial. Academic Medicine, 90(2), 221-230. https://doi.org/10.1097/acm.0000000000000552
Chang, S., Guindani, M., Morahan, P., Magrane, D., Newbill, S., & Helitzer, D. (2020). Increasing promotion of women faculty in academic medicine: Impact of National Career Development Programs. Journal of Women’s Health (Larchmt), 29(6), 837-846. https://doi.org/10.1089/jwh.2019.8044
Deng, M., Nham, E., Malvea, A., Ramsay, T., Seabrook, C., & Watterson, J. (2021). Exploring the impact of the surgical exploration and discovery (SEAD) program on medical students’ perceptions of gender biases in surgery: A mixed-method evaluation. Journal of Surgical Education, 78(4), 1236-1249. https://doi.org/10.1016/j.jsurg.2020.11.016
DeWane, M. E., Mattessich, S., Wu, R., & Whitaker-Worth, D. (2020). A survey study of resident experiences of sexual harassment during dermatology training. Journal of the American Academy of Dermatology, 83(2), 594-596. https://doi.org/10.1016/j.jaad.2019.07.023
Dhingra, S., Killaspy, H., & Dowling, S. (2021). Gender equality in academic psychiatry in the UK in 2019. BJPsych Bulletin, 45(3), 153-158. https://doi.org/10.1192/bjb.2020.116
Driscoll, S. W., Robinson, L. R., Raddatz, M. M., & Kinney, C. L. (2019). Is there evidence of gender bias in the oral examination for initial certification by the American Board of Physical Medicine & Rehabilitation? American Journal of Physical Medicine & Rehabilitation, 98(6), 512-515. https://doi.org/10.1097/phm.0000000000001126
Ellis, R. J., Hewitt, D. B., Hu, Y. Y., Johnson, J. K., Merkow, R. P., Yang, A. D., Potts, J. R., 3rd, Hoyt, D. B., Buyske, J., & Bilimoria, K. Y. (2019). An empirical national assessment of the learning environment and factors associated with program culture. Annals of Surgery, 270(4), 585-592. https://doi.org/10.1097/sla.0000000000003545
Farkas, A. H., Scholcoff, C., Lamberg, M., Shah, H., Fletcher, K., & Yecies, E. (2022). Preparing residents to respond to incidences of gender discrimination and sexual harassment: An interactive workshop. Southern Medical Journal, 115(10), 740-744. https://doi.org/10.14423/smj.0000000000001459
Ferrari, R. (2015). Writing narrative style literature reviews. Medical Writing, 24(4), 230-235. https://doi.org/10.1179/20474 80615Z.000000000329
Gaida, P., Kujumdshiev, S., & Stengler, K. (2020). Gender sensitivity in career mentoring – A project report from the medical faculty of Leipzig University. GMS Journal for Medical Education, 37(2), Doc24. https://doi.org/10.3205/zma001317
Geiser, E., Schilter, L. V., Carrier, J.-M., Clair, C., & Schwarz, J. (2022). Reflexivity as a tool for medical students to identify and address gender bias in clinical practice: A qualitative study. Patient Education Counselling, 105(12), 3521-3528. https://doi.org/10.10 16/j.pec.2022.08.017
Girod, S., Fassiotto, M., Grewal, D., Ku, M. C., Sriram, N., Nosek, B. A., & Valantine, H. (2016). Reducing implicit gender leadership bias in academic medicine with an educational intervention. Academic Medicine, 91(8), 1143-1150. https://doi.org/10.1097/acm.0000000000001099
Hannon, M., Duffey, K., Bharel, S., Redfield, R., Greidinger, A., Stewart, E., & Diemer, G. (2021). Investigating gender disparities in internal medicine residency awards. The American Journal of Medicine, 134(3), 405-409. https://doi.org/10.1016/j.amjmed.2020.11.003
Harbold, D., Dearolf, L., Buckley, J., & Lattanza, L. (2021). The Perry Initiative’s impact on gender diversity within orthopedic education. Current Reviews in Musculoskeletal Medicine, 14(6), 429-433. https://doi.org/10.1007/s12178-021-09717-4
Jackson, K. R., & Drolet, B. C. (2021). #MedicineToo – Gender bias in medical training: A national survey of residents. Journal of General Internal Medicine, 36(12), 3894-3896. https://doi.org/10.1007/s11606-021-06613-y
Jacobs, N. N., Esquierdo-Leal, J., Smith, G. S., Piasecki, M., & Houmanfar, R. A. (2022). Diversifying academic medicine: One search committee at a time. Front Public Health, 10, 854450. https://doi.org/10.3389/fpubh.2022.854450
Jacques, L., Kaljo, K., Treat, R., Davis, J., Farez, R., & Lund, M. (2016). Intersecting gender, evaluations, and examinations: Averting gender bias in an obstetrics and gynecology clerkship in the United States. Education for Health (Abingdon, England), 29(1), 25-29. https://doi.org/10.4103/1357-6283.178926
Jain, A., Nichols, G., Tarabishy, S., Scomacao, I., & Herrera, F. A. (2022). A comparison of applicant and resident physician demographics among surgical subspecialties from 2009 to 2019: Trends in gender and underrepresented minorities in medicine. Annals of Plastic Surgery, 88(4), 451-459. https://doi.org/10.1097/sap.0000000000003041
Joh, D. B., van der Werf, B., Watson, B. J., French, R., Bann, S., Dennet, E., & Loveday, B. P. T. (2020). Assessment of autonomy in operative procedures among female and male New Zealand general surgery trainees. Journal of the American Medical Association Surgery, 155(11), 1019-1026. https://doi.org/10.1001/jamasurg.2020.3021
Kandi, L. A., Jarvis, T. L., Movtchan, N. V., Hammond, J. B., Teven, C. M., & Rebecca, A. M. (2022). Characterization of national medical societies’ accessible resources to support underrepresented minority and female trainees. Journal of the American Medical Association Network Open, 5(9), Article e2230243. https://doi.org/10.1001/jamanetworkopen.2022.30243
Kisiel, M. A., Kühner, S., Stolare, K., Lampa, E., Wohlin, M., Johnston, N., & Rask-Andersen, A. (2020). Medical students’ self-reported gender discrimination and sexual harassment over time. BioMed Central Medical Education, 20(1), Article 503. https://doi.org/10.1186/s12909-020-02422-9
Klein, R., Law, K., & Koch, J. (2020). Gender representation matters: Intervention to solicit medical resident input to enable equity in leadership in graduate medical education. Academic Medicine, 95(12S), S93-S97. https://doi.org/10.1097/acm.0000000000003698
Kristoffersson, E., Andersson, J., Bengs, C., & Hamberg, K. (2016). Experiences of the gender climate in clinical training – a focus group study among Swedish medical students. BioMed Central Medical Education, 16(1), Article 283. https://doi.org/10.1186/s12909-016-0803-1
Langhan, M. L., Goldman, M. P., & Tiyyagura, G. (2022). Can behavior-based interviews reduce bias in fellowship applicant assessment? Academic Pediatrics, 22(3), 478-485. https://doi.org/10.1016/j.acap.2021.12.017
Lattanza, L. L., Meszaros-Dearolf, L., O’Connor, M. I., Ladd, A., Bucha, A., Trauth-Nare, A., & Buckley, J. M. (2016). The Perry Initiative’s medical student outreach program recruits women into orthopaedic residency. Clinical Orthopaedics and Related Research, 474(9), 1962-1966. https://doi.org/10.1007/s11999-016-4908-y
Liao, H. C., & Wang, Y. H. (2020). Integrating the gender perspective into literature studies to enhance medical university students’ gender awareness and critical thinking. International Journal of Environmental Research and Public Health, 17(24). https://doi.org/10.3390/ijerph17249245
Lieberman, J. A., Ehrhardt, A. A., Simpson, H. B., Arbuckle, M. R., Fyer, A. J., & Essock, S. M. (2018). Eliminating the glass ceiling in academic psychiatry. Academic Psychiatry, 42(4), 523-528. https://doi.org/10.1007/s40596-017-0810-5
Madeeh Hashmi, A., Rehman, A., Butt, Z., Awais Aftab, M., Shahid, A., & Abbas Khan, S. (2013). Gender discrimination among medical students in Pakistan: A cross sectional survey. Pakistan Journal of Medical Sciences, 29(2), 449-453. https://doi.org/10.12669/pjms.292.3256
Meyerson, S. L., Odell, D. D., Zwischenberger, J. B., Schuller, M., Williams, R. G., Bohnen, J. D., Dunnington, G. L., Torbeck, L., Mullen, J. T., Mandell, S. P., Choti, M. A., Foley, E., Are, C., Auyang, E., Chipman, J., Choi, J., Meier, A. H., Smink, D. S., Terhune, K. P., . . . George, B. C. (2019). The effect of gender on operative autonomy in general surgery residents. Surgery, 166(5), 738-743. https://doi.org/10.1016/j.surg.2019.06.006
Organisation for Economic Co-operation and Development. (2022). The proportion of female doctors has increased in all OECD countries over the past two decades. https://www.oecd.org/gender/data/the-proportion-of-female-doctors-hasincreased-in-all-oecd-countries-over-the-past-two-decades.htm
Olson, E. M., Dines, V. A., Ryan, S. M., Halvorsen, A. J., Long, T. R., Price, D. L., Thompson, R. H., Tollefson, M. M., Van Gompel, J. J., & Oxentenko, A. S. (2022). Physician identification badges: A multispecialty quality improvement study to address Professional misidentification and bias. Mayo Clinic Proceedings, 97(4), 658-667. https://doi.org/10.1016/j.mayocp.2022.01.007
Olson, E. M., Sanborn, D. M., Dyster, T. G., Kelm, D. J., Murray, S. G., Santhosh, L., & DesJardin, J. T. (2023). Gender disparities in critical care procedure training of internal medicine residents. American Thoracic Society Scholar, 4(2), 164-176. https://doi.org/10.34197/ats-scholar.2022-0025OC
Saberi, R. A., Herrera Gomez, L. C., Brady, A. C., Sola, J. E., Velazquez, O. C., & Neville, H. L. (2021). AAMC data shows effect of surgery faculty diversity on general surgery resident attrition rate at programs sponsored by LCME-accredited medical schools. Journal of Surgical Education, 78(4), 1123-1126. https://doi.org/10.1016/j.jsurg.2020.11.015
Sabin, J., Guenther, G., Ornelas, I. J., Patterson, D. G., Andrilla, C. H. A., Morales, L., Gurjal, K., & Frogner, B. K. (2022). Brief online implicit bias education increases bias awareness among clinical teaching faculty. Medical Education Online, 27(1), Article 2025307. https://doi.org/10.1080/10872981.2021.2025307
Sakowski, S. A., Feldman, E. L., Jagsi, R., & Singer, K. (2020). Energizing the conversation: How to identify and overcome gender inequalities in academic medicine. Journal of Continuing Education in the Health Professions, 40(4), 274-278. https://doi.org/10.1097/ceh.0000000000000296
Sethi, S., Edwards, J., Webb, A., Mendoza, S., Kumar, A., & Chae, S. (2022). Addressing gender disparity: Increase in female leadership increases gender equality in program director and fellow ranks. Digestive Diseases and Sciences, 67(2), 357-363. https://doi.org/10.1007/s10620-020-06686-5
Sobel, A. D., Lavorgna, T. R., Ames, S. E., Templeton, K. J., & Mulcahey, M. K. (2023). Interpersonal interactions and biases in orthopaedic surgery residency: Do experiences differ based on gender? Clinical Orthopaedics and Related Research, 481(2), 369-378. https://doi.org/10.1097/corr.0000000000002457
Sulibhavi, A., Kaufmann, M. R., Shetty, K. R., Wulu, J. A., Tracy, L. F., & Levi, J. R. (2021). Factors associated with distribution of female otolaryngology residents in United States. Laryngoscope, 131(2), E367-E372. https://doi.org/10.1002/lary.28746
Yeo, J. (2024). Gender equality Data and flow chart.docx (Version 1). Figshare. https://doi.org/10.6084/m9.figshare.25980352.v1
Ying, Y., Dupre, J., & Bhanji, F. (2023). Female surgical trainee recruitment and attrition – A 10-year national retrospective review. The American Journal of Surgery, 225(2), 282-286. https://doi.org/10.1016/j.amjsurg.2022.07.020
Zhang, N., Blissett, S., Anderson, D., O’Sullivan, P., & Qasim, A. (2021). Race and gender bias in internal medicine program director letters of recommendation. Journal of Graduate Medical Education, 13(3), 335-344. https://doi.org/10.4300/jgme-d-20-00929.1
*Han Ting Jillian Yeo
10 Medical Drive,
Singapore 117597
Email: jillyeo@nus.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









