Faculty development of medical educators: Training evaluation and key challenges
Submitted: 10 January 2022
Accepted: 22 April 2022
Published online: 5 July, TAPS 2022, 7(3), 23-32
https://doi.org/10.29060/TAPS.2022-7-3/OA2742
Tun Tun Naing1, Yuriko Minamoto2, Ye Phyo Aung1 & Marlar Than1
1Department of Medical Education, Defence Services Medical Academy, Myanmar, 2Meiji University, Tokyo
Abstract
Introduction: With the evolution of healthcare needs for the community and the changing trends in medical education in the 21st century, medical educators need to be prepared for their tasks in the coming decades. Medical educator training is crucial but other factors can also affect the development of their competency. This study aims to measure the impact of the medical educators’ training course and find out the key challenges encountered by the medical educators in Myanmar.
Methods: A retrospective quantitative design was conducted on 45 respondents by four levels of Kirkpatrick’s model assessment consisting of 39 statements and 9 items of key challenges, using five-point Likert scale. The item scores were analysed as mean and standard deviation, ‘t’ test and ANOVA were used for relationship between impact of training and demographic background.
Results: There was significant association between the impact of training and the educational background (p=0.03), job position (p=0.02), and academic year attended (p=0.03). The respondents distinctly agreed that the training increased their knowledge and attitudes and that they could apply the learnt lessons practically in their workplace (minimum 3.75±0.60 and maximum 4.28±0.50). Regarding the key challenges, respondents viewed that their institution needed to support more scholarship opportunities and academic recognition; encourage networking and strengthen ICT-based medical education system (minimum 2.55±0.84 – maximum 4.17±0.71).
Conclusion: This study indicates that enhancing the competency of medical educators with medical educator training programs is effective and useful; but inadequacy of institutional support for faculty development and internet facilities posed challenges in the overall faculty development.
Keywords: Medical Education, Faculty Development, Impact of Medical Educator’s Training, Kirkpatrick’s Model, Key Challenges
Practice Highlights
- Medical educator training program is crucial for enhancing competency in medical educators.
- Medical educator training program inspires medical educators to apply their knowledge and skills in their daily departmental activities.
- Beyond training, medical schools must address a balance of capacity for teaching, research and service functions for their faculty.
- Encouraging institutional support such as reward, recognition, and appreciation for their performance should be encouraged as an admirable institutional culture.
- Inadequacy of institutional support for faculty development and internet facilities posed challenges in the overall faculty development.
I. INTRODUCTION
Nowadays, with the evolution of healthcare needs for the community and changes in medical education trends, faculty development in medical education is challenging. Sheets and Schwenk (1990) explained that any activity that enhances the knowledge and skills of individual faculty members are very fundamental to their performance in a department or residency program such as teaching skills, clinical skills, research and administrative skill (Sheets & Schwenk, 1990). Developing the skills of faculty members is not effortless. The ability to teach is not inborn, although the graduate from medical school is supposed to be capable of teaching (McLean et al., 2008). Besides content, teaching involves ‘process,’ and to develop the ‘art’ of teaching, academics required to support (Benor, 2000).
The present-day teacher must be aware of and become part of the far- reaching changes taking place in medical education. Accordingly, in the 21st century, many changes can be found, such as teachers’ conventional roles being shifted to different roles, such as facilitators, curriculum planners, resource developers, educational administrators, and researchers (Crosby, 2000). Significant trends in underpinned theories of medical education are now focusing on patient-centred and culturally competent medical doctors and the ultimate aim of medical education is to improve the patient and community outcomes by promoting competent and caring practitioners (competent medical doctors) (McLean et al., 2008).
According to Harden and Laidlaw (2017), the competencies and attributes expected of an effective teacher includes not only mastery of the content area but also the technical competencies necessary to serve as an information provider, a role model, a facilitator of learning, a curriculum planner, an assessor, a manager and a scholar” (p. 9). Most medical schools worldwide have been implementing specific training for medical educators to develop the necessary skills as medical educators. The study conducted by Steinert (2014), pointed out that nowadays, most medical schools and educational organisations offer various programs and activities in response to educational trends in teaching and assessment for helping faculty members improve their skills as teachers and educators. Additionally, the World Federation of Medical Education (WFME) entails that for a basic standard of staff development: “the medical school must have a staff policy that addresses a balance of capacity for teaching, research and service functions. It also encourages ensuring recognition of meritorious academic activities, with appropriate emphasis on both research attainment and teaching qualifications” (World Federation for Medical Education, 2015).
In Myanmar, there are five civilian medical schools and one military medical school (Defence Services Medical Academy); however, no private medical school exists yet. Defence Services Medical Academy (DSMA), was established on 19th November 1992 in Mingalodon, Yangon and is listed in the World Directory of Medical Schools. The Ministry of Health and Sports, Myanmar, established a medical educator’s training program in 2003 for the medical educators from the civilian medical schools; likewise, the Directorate of Medical Services under the Ministry of Defence also started the medical educator training program for the military medical school in 2011. Both these medical educators’ training programs emphasize on developing the competent skills of medical educators.
Although medical educator training is crucial to improve medical educators’ quality in medical school, other influencing factors can affect the competency of medical educators. The impact of training depends not only on the program design of the training program but also on other factors such as learner characteristics and educational environment (Iqbal & AlSheikh, 2018). In a study conducted by Peeraer and Van Petegem (2012), the faculty members were able to apply teaching strategies and methods in their teaching activities after the faculty development training. Nevertheless, they faced some challenges, such as time constraints and scarce resources that impede their behavioural changes from becoming sustainable.
The medical educator training program in DSMA is a distance learning, diploma course with four face-to-face hands-on workshops. Individual written assignments are given on 10 fundamental modules that provide medical educators with the knowledge and skills about educational psychology, curriculum design and planning, objectives and contents, teaching-learning strategy, teaching-learning media, assessment and evaluation, educational leadership, communication skills, as well as conducting an educational workshop and educational research: throughout the one-year course. Since 2011, nine successive medical educator training courses have been conducted, and approximately 200 medical teachers from DSMA have successfully completed these courses and graduated.
Currently, there is no published evidence-based research investigating the crucial issues to develop competent medical educators in Myanmar. This study intends to focus on the training perspectives and the commitment of institutional support for the development of the medical skills. Therefore, the main objective of this study is to find out the impact of the medical educator’s training course conducted in the military medical school and to explore the key challenges encountered by the trainees.
II. METHODS
A. Research Design
A retrospective design was used to investigate the impact of the medical educator training course and the medical educators’ perception regarding their key challenges. By applying the program theory, a logic model for training program was applied, illustrated in Figure 1.

Figure 1. Logic model for training evaluation Adapted from (Rossi, et al., 2004)
B. Kirkpatrick’s Model
To investigate the impact of the training, the Kirkpatrick evaluation measurement tool was utilized (Appendix 1). The four-levels in the Kirkpatrick’s model are: 1) Reaction evaluation, Learning evaluation Behaviour evaluation and Result evaluation (Kirkpatrick & Kirkpatrick, 2006).
C. Research Framework

Figure 2. Research framework
D. Data Collection
Survey questionnaires were formulated in three sections. The first session aimed to get demographic information, the second one intended for Kirkpatrick’s evaluation by 39 evaluation questions, and the last was constructed by nine items to explore the critical challenges for medical educators. Questionnaires were developed based on the contents and expected outcomes of the medical educator training course that has been to delivered throughout the courses. These are related to the knowledge, attitude and skills that gained after the course regarding educational psychology, curriculum design and planning, objectives and contents, teaching-learning strategy & media, assessment and evaluation, educational leadership, communication skills, conducting an educational workshop and educational research. Moreover, questionnaires attributed to possible challenges that have been encountered by medical educators were adapted from the research outcomes of Huwendiek et al. (2010). All evaluation questions were self-administered and had the five-point Likert scale items ranging from 5 (strongly agree) to 1 (strongly disagree). Informed verbal consent was obtained from the respondents in respective of respondents’ autonomy before data collection. Ethics approval was obtained from the Ethical Review Committee of the Defence Services Medical Academy, Yangon, Myanmar.
E. Sampling Procedure
Every medical educator is eligible if they had already completed the training and currently engaging in the undergraduate and postgraduate medical education programs at the military medical school, in Myanmar. Among the 120 persons who meet eligibility, approximately 30% of the population (45 participants) responded to the evaluation survey and convenience sampling was practiced.
F. Data Analysis
Data obtained from the survey was entered in Microsoft Excel files and analysed by SPSS software. The item scores of each evaluation were analysed as descriptive analysis such as mean and standard deviation to compare the response rate. The t-test and ANOVA analysis were used to determine the relationship between respondents’ demographic characteristics and Kirkpatrick’s four-level evaluation results. Descriptive analysis was used to explore the key challenges of medical educators.
III. RESULTS
Forty-five medical educator attendees who satisfactorily completed one of the medical education courses held at DSMA between 2011 and 2019, individually expressed their views on the impact of the medical educator training courses and disclosed the key challenges regarding faculty development in medical education. The data that support the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.figshare.17074637 (Naing et al., 2021).
There were 39 evaluation questions, and each evaluation level has specific items, respectively. The internal consistency of each of the scales was examined by using Cronbach’s alpha. The alpha score was satisfactory: 0.65 for reaction evaluation (11 items), 0.86 for learning evaluation (10 items), 0.81 for behavioral evaluation (11items), and 0.84 for result evaluation (7 items).
A. Demographic Characteristics
Of the demographic characteristics, three factors (age, gender, and expertise), had no significant association with the impact of the training, but the respondents’ educational background (p=0.03), job’s position (p=0.02), academic year they attended (p=0.03) showed statistically significant association with the impact of training (Table 1). However, the proportionally unequal number of respondents in each group may affect the results.
|
Demographic Characteristics |
Reaction Evaluation |
Learning Evaluation |
Behavioral evaluation |
Result Evaluation |
|
Mean ± SD |
Mean ± SD |
Mean ± SD |
Mean ± SD |
|
|
Age(N=45) |
||||
|
<=40 (N=26) |
4.05±0.20 |
4.08±0.27 |
3.93±0.26 |
4.00±0.35 |
|
41-50 (N=11) |
4.10±0.27 |
4.30±0.44 |
3.99±0.22 |
4.22±0.39 |
|
>= 50 (N=8) |
4.06±0.28 |
4.12±0.38 |
4.01±0.44 |
4.10±0.40 |
|
‘F’ value |
0.17 |
1.55 |
0.28 |
1.30 |
|
‘p’ value |
0.83 |
0.22 |
0.75 |
0.28 |
|
Gender(N=45) |
||||
|
Male(N=33) |
4.06±0.23 |
4.10±0.31 |
3.93±0.26 |
4.07±0.39 |
|
Female(N=12) |
4.09±0.24 |
4.26±0.41 |
4.04±0.36 |
4.08±0.33 |
|
‘t’ value |
-0.474 |
-1.44 |
-1.16 |
-0.07 |
|
‘p’ value |
0.63 |
0.15 |
0.24 |
0.94 |
|
Education(N=45) |
||||
|
Master(N=31) |
4.05±0.27 |
4.09±0.31 |
3.90±0.27 |
3.99±0.37 |
|
Doctoral(N=14) |
4.09±0.20 |
4.25±0.39 |
4.09±0.28 |
4.25±0.32 |
|
‘t’ value |
-0.50 |
-1.49 |
-2.18 |
-2-23 |
|
‘p’ value |
0.61 |
0.14 |
0.03* |
0.03* |
|
Expertise in medical Sciences(N=45) |
|
|||
|
Basic Sciences(N=14) |
4.04±0.26 |
4.10±0.33 |
3.86±0.30 |
4.06±0.33 |
|
Paraclinical(N=16) |
4.09±0.19 |
4.25±0.33 |
4.09±0.24 |
4.20±0.36 |
|
Clinical(N=9) |
4.02±0.28 |
4.03±0.33 |
3.90±0.29 |
3.96±0.40 |
|
Others(N=6) |
4.15±0.21 |
4.10±0.41 |
3.90±0.32 |
3.92±0.45 |
|
‘F’ value |
0.45 |
0.95 |
1.94 |
1.19 |
|
‘p’ value |
0.71 |
0.42 |
0.13 |
0.32 |
|
Job Position (N=45) |
|
|||
|
Assistant lecturer(N=27) |
4.04±0.21 |
4.07±0.27 |
3.93±0.26 |
3.99±0.35 |
|
Lecturer(N=11) |
4.04±0.24 |
4.16±0.35 |
3.90±0.18 |
4.12±0.38 |
|
Associate Professor(N=3) |
4.33±0.29 |
4.70±0.30 |
4.33±0.29 |
4.38±0.35 |
|
Professor(N=4) |
4.11±0.30 |
4.15±0.52 |
4.02±0.56 |
4.25±0.45 |
|
‘F’ value |
1.49 |
3.47 |
2.02 |
1.47 |
|
‘p’ value |
0.23 |
0.02* |
0.12 |
0.23 |
|
Teaching experience (N=45) |
|
|||
|
< = 5 Years(N=17) |
4.02±0.24 |
4.11±0.37 |
3.88±0.27 |
4.13±0.45 |
|
(6-10) Years(N=15) |
4.15±0.19 |
4.12±0.24 |
4.03±0.23 |
4.01±0.32 |
|
(11-15) Years(N=7) |
4.00±0.23 |
4.11±0.28 |
3.90±0.44 |
4.08±0.29 |
|
> = 6 Years(N=6) |
4.07±0.28 |
4.31±0.54 |
4.06±0.24 |
4.04±0.39 |
|
‘F’ value |
1.00 |
0.55 |
1.05 |
0.24 |
|
‘p’ value |
0.41 |
0.64 |
0.37 |
0.86 |
|
Year of Services (N=45) |
|
|||
|
< = 10 Years(N=5) |
4.05±0.13 |
4.16±0.15 |
3.96±0.18 |
4.08±0.27 |
|
(11-15) Years(N=16) |
4.08±0.23 |
4.04±0.29 |
3.90±0.29 |
3.96±0.37 |
|
(16-20) Years(N=12) |
4.08±0.28 |
4.25±0.39 |
4.01±0.27 |
4.16±0.39 |
|
> = 21 Years(N=12) |
4.04±0.23 |
4.16±0.40 |
3.98±0.35 |
4.13±0.40 |
|
‘F’ value |
0.08 |
0.83 |
0.35 |
0.77 |
|
‘p’ value |
0.97 |
0.48 |
0.78 |
0.51 |
|
Academic Year (N=45) |
|
|
|
|
|
2011-2013(N=11) |
4.03±0.25 |
4.25±0.35 |
4.00±0.31 |
4.10±0.32 |
|
2014-2016(N=9) |
4.00±0.34 |
3.93±0.35 |
3.78±0.34 |
3.79±0.45 |
|
2017-2019(N=25) |
4.11±0.17 |
4.17±0.32 |
4.00±0.24 |
4.16±0.33 |
|
‘F’ value |
0.94 |
2.47 |
2.09 |
3.64 |
|
‘p’ value |
0.40 |
0.10 |
0.13 |
0.03* |
(*) means 0.05 level of significant
Table 1. Relationship between demographic characteristics and Kirkpatrick’s evaluation
B. Kirkpatrick’s Four Level of Evaluation
When looking at the reaction evaluation, most of the respondents gave favourable agreement on the management of training, teaching skills of the trainers, and training methods, however, there was relatively weakness in the proper preparation of training contents by facilitators (3.86±0.45), providing training materials (3.88±0.53). Looking upon the learning evaluation responses, all of the respondents expressed a high level of satisfaction on their understandings and awareness. Regarding learning behaviour, majority agreed that they can apply their learning to their workplace but comparatively lower response score was found in planning educational research (3.84±0.56), how to apply educational theories in medical education practices (3.84±0.52) and arrange an educational workshop programme (3.75±0.60). Although the medical educator training affects the respondents to get better improvement in most faculty development activities, there is still a need to develop the participation of respondents in research development activities with comparatively lowest evaluation scores of (3.80±0.66).
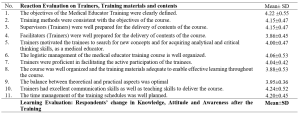



Table 2. Kirkpatrick’s Four Level of Evaluation of Medical Educator Training
C. Key Challenges in Faculty Development
It was found that majority of the evaluation scores for the statement items in the faculty development area were much lower than the scores for the items in the training’s impact. The most noticeable and lowest scores were found in the item of financial investment of medical educators (2.68±0.73), research collaboration in other universities (2.60±0.88) and networking with the international university for career development of medical educators (2.55±0.84). However, they agreed that the currently used undergraduate curriculum of the institution is appropriate for them to practically apply their pedagogic skills gained from the training course(4.17±0.71).
|
No. |
Statement |
Mean±SD |
|
1. |
Depending on the performance in faculty development activities, our institution appreciates rewards for medical educators as an institutional policy. |
2.80±0.75 |
|
2. |
Medical educators in our university have the opportunity to apply the Institutional scholarship program for research and carrier development. |
2.84±0.79 |
|
3. |
The financial investment for medical educators in our institution is acceptable in the current situation. (e.g. teaching-learning materials, research facilities, ICT based technology) |
2.68±0.73 |
|
4. |
There are adequate networks and collaboration with an international university to promote the carrier development of medical educators. (e.g. MOU) |
2.60±0.88 |
|
5. |
ICT based medical education system in our university is well functioned and applicable. |
2.73±0.80 |
|
6. |
The number of medical educators in our university is sufficient to achieve the mission of our university. |
2.71±0.84 |
|
7. |
The institutions’ current undergraduate curriculum is appropriate for us to practically apply the pedagogic skills gained from the training course. |
4.17±0.71 |
|
8. |
Research development activities of our university, including research funding, research skills of medical educators, and research facilities, are well functioning. |
2.80±0.78 |
|
9. |
The research collaboration with other universities or research centers to promote research innovation is acceptable. |
2.55±0.84 |
Table 3. Key Challenges in faculty development in medical education by respondents
IV. DISCUSSION
This study investigates the medical educator training program, which aims to develop the competency skills of medical educators who are involved in the faculty development activities at DSMA, Myanmar. Regarding the overall impact of the training, the respondents expressed their positive perception on the organisation of the program; the training improved their knowledge and attitudes as a medical educator; and it was practically applicable in their daily work. The positive perception of the training was not surprising because most of the trainees voluntarily attended the course and were highly motivated to accomplish self- improvement after attending the course. The findings are consistent with another study where ‘overall satisfaction with faculty development programs was high, and they consistently found the program helpful, enjoyable and relevant to their objectives’ (Steinert et al., 2016, p.779). Similarly, another study done by Yolsal et al. (2003) showed that the participants who enrolled in the similar training of trainers (TOT) course explored positive perception, and they agreed it was required to be acquainted with those kinds of instructional practices (Yolsal et al., 2003). The possible reason for the respondents’ satisfaction with the impact of training in the current study, could also be due to the organized training preparation and training context and, the course itself used mainly a distance learning format with flexible training schedules for them when compared to other full-time courses in other specialties. It was also found that significant improvements in self-efficacy of medical educators in the domain of the teaching relevant subject contents and developing creative ways to cope with system constraints after experiencing 12 months faculty development program in Bhutan (Tenzin et al., 2019).
In this study, for learning evaluation, most respondents believed that they gained in terms of knowledge, attitude, and skills and that it had an impact on the teaching effectiveness. It revealed that most of the medical educators gained benefits after the training, and the increase in confidence facilitated them to become more involved in participating in faculty development activities and curriculum planning activities. Similarly, F.J. Ciller and N. Herman explained that as a goal of an educational development program, changes in attitudes and perception serves as a foundation for further changes in behaviour (Cilliers & Herman, 2010).Even more, the review articles of Steinert et al. (2016) highlighted most of the faculty development interventions focus on teaching effectiveness by improving their teaching skills, assessment skills, designing curriculum, and educational leadership skills (Steinert et al., 2016).
When analysing the relationship between the various demographic background and impact of the training, it was revealed that the job position, educational background, and difference in academic year among the respondents were significantly associated with the impact of training. There might be many possible reasons why this was significant. For example, the course preparation, the changes in placement of trainers in several years might also be a possible issue, and variation in individual performance also considered. However, in this survey, those factors were not explored. Fishbein et al. (2003) explained that interpersonal variation and the organization’s favorable situation could be impact factors for behavioural change at the organization level (Fishbein et al., 2003).
In this study, although the self-reported changes showed self-actualization in individual performance to some extent, respondents are not contented with their learning environment in terms of institutional support. Institutional support plays a vital role in faculty development in medical education and every institution can meet its institutional mission and goals by enabling its faculty member to fulfil their particular purposes as teachers, scholars, and leaders according to the research outcome (Boucher et al., 2006). Moreover, Steinert pointed out that many factors are impeding the faculty development, such as unsupportive leadership, resistance to change, lack of faculty motivation, and the unwillingness of faculty to acquire the teaching skills and knowledge (Steinert, 2000).
On exploring the critical challenges of the medical educators, all the respondents believed that their institution should support more scholarship opportunity, academic recognition, networking with other universities in terms of research and professional development, and ICT-based medical education system. According to the survey of (Huwendiek et al., 2010) 806 medical educators from Association for Medical Education Europe (AMEE) revealed that the critical challenges of medical education were lack of academic recognition (40%), funding (36%), faculty development (24%), time for medical education issues (22%), and institutional support (21%) (Huwendiek et al., 2010).
Therefore, to accelerate the faculty development as a holistic approach, it is needed to consider not only training for faculty members but also other factors reward and recognition, ICT system, and networking. This requisite is not only in a military medical school, but internationally most medical schools are trying to support their faculty in accordance with the staff policy requirements as stated in the WFME Global standards for Quality improvement. However, the current research could gather only some self-reported changes in behaviour and whether the changes actually occurred in the workplace has not been proven by observation. Nevertheless, as the opinions were obtained from closed ended questionnaire statements, a further exploratory qualitative study is needed to obtain accurate information on the magnitude of the problem and the specific areas that needed further support from the institution.
V. CONCLUSION
This study revealed the medical educator training could improve their required knowledge, attitude, and skills to practice in the teaching environment, the fundamental need for educational leadership, educational research, and communication skills in the health-care setting. The medical educators who need to be competent could not be motivated only from the training without institutional support. The respondents believed that their institution should encourage institutional support in terms of reward, recognition, scholar allowance, and collaboration with other academic institutions to promote research culture and professional development, ICT-based medical education.
To conclude, the findings of this study exclusively show that military medical schools in Myanmar still need to emphasize the professional identities of medical educators by encouraging institutional support, not just by only focusing on the faculty development training as a mandatory by institutional policy.
Notes on Contributors
Tun Tun Naing reviewed the literatures and developed the conceptual framework and conducted the data analysis and wrote the discussion and conclusion. Finally, he developed the manuscript to submit to TAPS.
Yuriko Minamoto was involved in the formulation of research question and research framework to conduct the research systematically, application of evaluation tools and technique and, proofreading of original thesis and the manuscript.
Ye Phyo Aung participated in the research in the writing of research methodology session, conducted the data collection, and supported choosing research design, proper sampling methods and data collection tools and technique and proofreading of manuscript.
Marlar Than supported the construction of survey questionnaires which is the back bone of the evaluation research and contribute to proofreading of current manuscript.
Ethical Approval
Ethics approval was granted by the Ethical Review Committee of the Defence Services Medical Academy, Yangon, Myanmar. (7 / Ethics 2019).
Data Availability
The data that support the findings of this study are openly available in Figshare repository, http://doi.org/10.6084/m9.figshare.17074637
Acknowledgement
I would also like to express my gratitude to Japanese Government through the Japan International Cooperation Center (JICE) for their support to conduct this research project for completion of master thesis program at Meiji University.
I would like to express my special thanks to my colleagues, and without their support, the survey of my research would not have been achieved. I am indebted to all medical educators from Military Medical Service, Myanmar, who help me respond to my survey sharing with their valuable opinions and experience.
Funding
Conducting the research was operated during the study period supported by JDS Program under the JICA. For this publication , it is conducted for personal and professional development and no funding is involved.
Declaration of Interest
There is no conflict of interest in the current research.
References
Benor, D. (2000). Faculty development, teacher training and teacher accreditation in medical education: Twenty years from now. Medical Teacher, 22(5), 503-512. https://doi.org/10.1080/01421590050110795
Boucher, B., Chyka, P., Fitzgerald, W., Hak, L., Miller, D., Parker, R., Phelps, S., Wood, G., & Gourley, D. (2006). A comprehensive approach to faculty development. American Journal of Pharma- ceutical Education, 70(2), 27. https://doi.org/10.5688/aj700227
Cilliers, F., & Herman, N. (2010). Impact of an educational development programme on teaching practice of academics at a research‐intensive university. International Journal for Academic Development, 15(3), 253-267. https://doi.org/10.1080/1360144x.2010.497698
Crosby, R. (2000). AMEE Guide No 20: The good teacher is more than a lecturer – the twelve roles of the teacher. Medical Teacher, 22(4), 334-347. https://doi.org/10.1080/014215900409429
Fishbein, M., Hennessy, M., Yzer, M., & Douglas, J. (2003). Can we explain why some people do and some people do not act on their intentions? Psychology, Health &Amp; Medicine, 8(1), 3-18. https://doi.org/10.1080/1354850021000059223
Harden, R. M., & Laidlaw, J. M. (2017). Essential Skills for a Medical Teacher (2nd ed., pp. 9). Elsevier.
Huwendiek, S., Mennin, S., Dern, P., Ben-David, M., Van Der Vleuten, C., Tönshoff, B., & Nikendei, C. (2010). Expertise, needs and challenges of medical educators: Results of an international web survey. Medical Teacher, 32(11), 912-918. https://doi.org/10.3109/0142159x.2010.497822
Iqbal, M., & AlSheikh, M. (2018). Factors affecting the transfer of training to the workplace after a faculty development programme: What do trainers think? Journal of Taibah University Medical Sciences, 13(6), 552-556. https://doi.org/10.1016/j.jtumed.2018.11.001
Kirkpatrick, D., & Kirkpatrick, J. (2006). Evaluating Training Programs: The Four Levels (3rd ed.). Berrett-Koehler Publisher.
McLean, M., Cilliers, F., & Van Wyk, J. (2008). Faculty development: Yesterday, today and tomorrow. Medical Teacher, 30(6), 555-584. https://doi.org/10.1080/01421590802109834
Naing, T. T., Minamoto, Y., Aung, Y. P., & Than, M. (2021). Faculty development of medical educators: Training evaluation and Key Challenges. [Dataset].
Figshare. http://doi.org/10.6084/m9.figshare.17074637
Peeraer, J., & Van Petegem, P. (2012). The limits of programmed professional development on integration of information and communication technology in education. Australasian Journal of Educational Technology, 28(6), 1039-1056. https://doi.org/10.14742/ajet.809
Rossi, P., Lipsey, M., & Freeman, H. (2004). Evaluation: A Systematic Approach (7th ed.). Sage.
Sheets, K., & Schwenk, T. (1990). Faculty development for family medicine educators: An agenda for future activities. Teaching and Learning in Medicine, 2(3), 141-148. https://doi.org/10.1080/10401339009539447
Steinert, Y. (2000). Faculty development in the new millennium: key challenges and future directions. Medical Teacher, 22(1), 44-50. https://doi.org/10.1080/01421590078814
Steinert, Y. (2014). Faculty Development in Health Profession: A Focus on Research and Practice (1st ed.). Springer.
Steinert, Y., Mann, K., Anderson, B., Barnett, B., Centeno, A., Naismith, L., Prideaux, D., Spencer, J., Tullo, E., Viggiano, T., Ward, H., & Dolmans, D. (2016). A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Medical Teacher, 38(8), 769-786. https://doi.org/10.1080/0142159x.2016.1181851
Tenzin, K., Dorji, T., Choeda, T., & Pongpirul, K. (2019). Impact of faculty development programme on self-efficacy, competency and attitude towards medical education in Bhutan: A mixed-methods study. BMC Medical Education, 19(1), 468. https://doi.org/10.1186/s12909-019-1904-4
World Federation for Medical Education. (2015, January 1). Basic medical education WFME global standards for quality improvement. https://wfme.org/download/wfme-global-standards-for-quality-improvement-bme/.
Yolsal, N., Bulut, A., Karabey, S., Ortayli, N., Bahadir, G., & Aydin, Z. (2003). Development of training of trainer’s programmes and evaluation of their effectiveness in Istanbul, Turkey. Medical Teacher, 25(3), 319-324. https://doi.org/10.1080/0142159031000092779
*Tun Tun Naing
No. 94, D-1, Pyay Road,
Mingaladon Township
Yangon, Myanmar
Postal code – 11021
+95 95053402
Email: tuntunnaing@dsma.edu.mm, drhtun1984@gmail.com
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









