Education of medical students in child and adolescent psychiatry
Submitted: 14 March 2020
Accepted: 20 July 2020
Published online: 5 January, TAPS 2021, 6(1), 30-39
https://doi.org/10.29060/TAPS.2021-6-1/OA2235
Yit Shiang Lui, Abigail HY Loh, Tji Tjian Chee, Jia Ying Teng, John Chee Meng Wong & Celine Hsia Jia Wong
Department of Psychological Medicine, National University Health System, Singapore
Abstract
Introduction: A good understanding of basic child-and-adolescent psychiatry (CAP) is important for general medical practice. The undergraduate psychiatry teaching programme included various adult and CAP topics within a six-week time frame. A team of psychiatry tutors developed two new teaching formats for CAP and obtained feedback from the students about these teaching activities.
Methods: Medical students were introduced to CAP via small group teaching in two different modes. One mode was the “Clinical Vignettes Tutorial” (CVT) and the other mode “Observed Clinical Interview Tutorial” (OCIT). In CVT, tutors would discuss clinical vignettes of real patients with the students, followed by explanations about theoretical concepts and management strategies. OCIT involved simulated-patients (SPs) who assisted by acting as patients presenting with problems related to CAP, or as parents for such patients. At each session, students were given the opportunity to interview “patients” and “parents”. Feedback was given following these interviews. The students then completed surveys about the teaching methods.
Results: Students rated very-positive feedback for the teaching of CAP in small groups. Almost all found these small groups enjoyable and that it helped them apply what they had learnt. Majority agreed that the OCIT sessions increased their level of confidence in speaking with adolescents and parents. Some students agreed that these sessions had stimulated their interest to know more about CAP.
Conclusion: Small group teaching in an interactive manner enhanced teaching effectiveness. Participants reported a greater degree of interest towards CAP, and enhanced confidence in treating youths with mental health issues as well as engaging their parents.
Keywords: Child Adolescent Psychiatry, Medical Education, Small Group, Teaching
Practice Highlights
- Psychiatric disorders are among the most common medical conditions experienced by children and adolescents, and data from the Singapore Mental Health survey conducted in 2010 had shown the prevalence rates of emotional and behavioural problems among Singaporean youth to be at 12.5%.
- Most medical students had limited exposure to Child & Adolescent Psychiatry (CAP) in their medical curriculum due to reduced proportions of teaching time and opportune clinical exposures allocated to CAP programmes.
- This would be further compounded by the limited number of child and adolescent psychiatrists involved in teaching at medical schools and supervising clinical postings.
- This manuscript described synergistic teaching methods employed in educating medical students within the field of Child & Adolescent Psychiatry and examined the effectiveness and acceptability of CAP teaching using small-group teaching classes.
- The CAP small group interactive teaching sessions for medical students received good feedback from majority of the participants and translated to applicability and skillsets transferability.
I. INTRODUCTION
Psychiatric disorders are among the most common medical conditions experienced by children and adolescents during their developmental years. Epidemiological data from developed countries demonstrated transitions from acute and infectious diseases to chronic conditions, that included mental health problems as well (Baranne & Falissard, 2018; Kyu et al., 2016; World Health Organization, 2014). Recent global health surveys had estimated the median prevalence of psychiatric disorders present in children and adolescents to be about 12% (Costello, Egger, & Angold, 2005). Data from the Singapore Mental Health survey conducted in 2010 had shown the prevalence rates of emotional and behavioural problems among Singaporean youth to be at 12.5% which was comparable with global data (Lim, Ong, Chin, & Fung, 2015). Some studies had also demonstrated a growing trend of a burgeoning proportion of disabilities in children and adolescents that would be attributable to mental health disorders. Therefore, increasingly more health resources would be expected to meet these demands (Baranne & Falissard, 2018; Erskine et al., 2015). This would largely come in the form of services focusing on prevention, identification, and management of child and adolescent psychiatric disorders (Baranne & Falissard, 2018; Costello et al., 2005; Erskine et al., 2015). There is hence a demand to fill the gap for escalating mental health needs in this population of children and adolescents. Delays in accessing prompt and adequate assessment may incur socio-economic costs and bring about further psychiatric comorbidities.
Increasing the numbers of trained child and adolescent psychiatrists may be necessary to meet the current and projected needs in youth mental health (Baranne & Falissard, 2018; Breton, Plante, & St-Georges, 2005; Thomas & Holzer, 2006). Globally, as well as in Singapore, the number of such specialists fell short of meeting the demands, and increased recruitment was needed to address this workforce shortage (Breton et al., 2005; Lim et al., 2015; Thomas & Holzer, 2006). Hence, there had been moves in recent years to increase exposure to, and interest in, child and adolescent psychiatry (CAP) among medical students (Hunt, Barrett, Grapentine, Liguori, & Trivedi, 2008; Malloy, Hollar, & Lindsey, 2008; Plan, 2002; Thomas & Holzer, 2006). Most medical students had limited exposure to CAP in their medical curriculum due to reduced proportions of teaching time and opportune clinical exposures allocated to CAP programmes. This would be further compounded by the limited number of child and adolescent psychiatrists involved in teaching at medical schools and supervising clinical postings (Dingle, 2010; Lim et al., 2015; Plan, 2002; Sawyer & Giesen, 2007). It remained important however that medical students were taught CAP, given the burden of mental health disorders in our youths today (Dingle, 2010; Hunt et al., 2008; Kaplan & Lake, 2008; Sawyer & Giesen, 2007; Thomas & H, 2006). Other specialist practitioners such as family medicine specialists and paediatricians also frequently managed youths with psychiatric problems. Understanding early childhood development, critical milestones in childhood and adolescents would be essential in any specialty that had to interact and manage children as part of routine practice (Hunt et al., 2008; Plan, 2002). This would form the basis why CAP would be taught in medical schools as part of regular and wider curricula (Dingle, 2010; Hunt et al., 2008; Kaplan & Lake, 2008; Malloy et al., 2008; Plan, 2002; Sawyer & Giesen, 2007). The current medical school pedagogy may have underestimated the salience of teaching CAP in the undergraduate curriculum. This resulted in allocating much less time, attention as well as teaching resources towards CAP. Curriculum designers will also have severely under-appreciated the transferability of skillset due to the inherent challenges in undertaking interviews with children and their parents.
A. The Curriculum and Teaching Methods
In Yong Loo Lin School of Medicine at the National University of Singapore, CAP teaching would be embedded within a six-week General Psychiatry clerkship for Fourth-Year medical students. CAP teaching would consist of a period of 20-hour centralised teaching at the affiliated National University Hospital, together with clinical attachments to the outpatient child psychiatry clinics in other restructured hospitals. The 20-hour teaching would include online lectures made accessible through students’ Intranet, didactic lectures delivered in large group setting by clinical tutors, as well as small group teaching classes. In this paper, the authors examined the effectiveness and acceptability of CAP teaching using these small group teaching classes.
A comprehensive CAP education will ensure the following domains are included such as emotional symptomatology (e.g. depression, anxiety, enuresis), conduct and disruptive behavioural problems (e.g. attention deficit disorder, conduct disorder, bullying), developmental delays (e.g. specific learning, speech or autistic spectrum) and relationship difficulties, personal habits and injuries (e.g. abuse, suicide, digital overuse). Knowledge will include normal child developmental psychology as well as the assessment and management of common CAP conditions. Practice imparts interview skills of CAP and counselling of young parents.
Small group teaching sessions consisted of several components in its general pedagogic approach. The aim of these sessions was to cover the teaching of core knowledge and practices in common CAP cases, as well as training of interview skills required in communicating with children, adolescents, and their parents. Each session would start off with a series of lectures on four major domains of CAP: (1) emotional symptoms, (2) conduct and disruptive behavioural problems, (3) developmental delays, and (4) relationship difficulties, personal habit, and injuries. The lectures would be followed by both “Clinical Vignettes Tutorial” (CVT) and “Observed Clinic Interview Tutorials” (OCIT). The teaching sessions were structured as such in view of time constraints in the undergraduate curriculum that precluded comprehensive clinical exposure—a combination of didactics and simulated practice was designed to maximise the transferability of necessary theoretical knowledge and practical skills set for the students.
In the CVT, tutors would discuss clinical vignettes derived from real-life patients, and their underpinning theoretical concepts for about 2½ hours. This teaching activity would have covered the principles of psychopharmacology in the youths, as well as three distinct childhood conditions: a) Adolescent Depression with self-harm behaviour, b) Post-traumatic Stress Disorder in an adolescent and c) Adjustment Disorder in an adolescent with chronic medical illnesses. The anonymised vignettes were based on actual patient profiles. During each interactive discussion of these clinical presentations, students were encouraged by tutors to raise critical questions as pertinent portions of the history unfolded to enhance their analytic thinking of the cases and remember these teachable moments.
The second teaching activity of the OCITs would take place after a second series of lectures on other CAP conditions had been conducted. During this three-hour long OCIT, students would be provided opportunities to interview simulated patients (SPs). Each group would comprise of 12 to 18 students led by one clinical tutor.
The four pre-prepared clinical scenarios included one case of an adolescent with Anorexia Nervosa; another of an adolescent with Social Anxiety Disorder; a parent of a child with Attention Deficit Hyperactivity Disorder; and last but not least a parent of a child with features of Autism Spectrum Disorder. Each of these scenarios would include a case template that comprised an interesting title, the learning and assessment objective, the student’s task and the script for the SP complete with an opening statement, standard statements and character presentation (behaviour, affect and mannerism).
Students would take turn to interview the SPs in attempts to collate accurate and adequate clinical information to arrive at provisional diagnoses. The students were then tasked to discuss the possible differential diagnoses, to provide treatment options as well as to formulate prognoses of the conditions with the SPs. The SPs were in turn invited to comment on the interactions they had with the students. The clinical tutors would also conduct follow-up discussions to provide feedback to the students on aspects of their interviewing techniques and knowledge of the clinical conditions. The discussions also focused on the differential diagnoses and management strategies for various conditions.
II. METHODS
Paper and pen self-report surveys for both the CVT and OCIT sessions were done to evaluate the student participants’ learning, experience, and interest in CAP (Appendix A). Student participants were asked to grade responses on a five-point Likert scale (1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree and 5 = Strongly agree), in relation to statements such as “I found the session enjoyable” and “The case scenarios were relevant”. The surveys were completed and submitted anonymously at the end of each teaching session. The surveys also included a free–text segment for any open feedback, in which the question asked the student participants to list down “The best things about the session” and “Some ways which I think can make the sessions better”. The surveys utilised for each teaching session differed slightly owing to varied content validity of the teaching methods, but the questions were largely identical for most of the surveys. Implied informed consent was provided for by the participating students during the surveys.
For the current study, the authors analysed data from the surveys completed by the Fourth-Year undergraduate medical students who were rotated to the six-week Psychiatry clerkship period of five months between July and November in 2017.
Descriptive statistics were used to analyse the findings of the survey.
III. RESULTS
A total of 289 students completed the survey between July 2017 and November 2017. With regards to the CVT, majority of the students agreed or strongly agreed that the sessions were enjoyable (90.7%) and beneficial to their overall learning (90.7%; Table 1). They provided feedback that the session had helped them to apply what they had learnt (95.8%), and that the case scenarios were relevant (98.2%).
|
Survey Statement |
Participants Who Indicated “Agree” Or “Strongly Agree” |
||
|
|
|
N |
% |
|
1 |
“I found the session enjoyable…”
|
262 |
90.7 |
|
2 |
“The session helped me to apply what I have learnt…”
|
277 |
95.8 |
|
3 |
“The case scenarios were relevant…”
|
284 |
98.2 |
|
4 |
“My clinical tutor was effective in facilitating the session…”
|
281 |
97.2 |
|
5 |
“The session stimulated my interest in Child and Adolescent Psychiatry…”
|
247 |
85.5 |
|
6 |
“There was sufficient time for each section…”
|
272 |
94.1 |
|
7 |
“Overall, I found the session beneficial…”
|
262 |
90.7 |
Table 1. Survey results for the Clinical Vignettes Tutorial (CVT)
For the OCIT, most of the survey respondents agreed or strongly agreed that the activity had helped them to learn psychiatric interviewing skills (97.7%), increased their confidence in speaking with adolescents or parents (95.1%) (Table 2). Most of the students who responded to the survey had reported that the simulated patients’ performances were realistic (97.7%). A large proportion of the respondents indicated that the teaching session had met their learning objectives (98.5%).
|
Survey Statement |
Participants Who Indicated “Agree” Or “Strongly Agree” |
||
|
|
|
N |
% |
|
1 |
“The session helped me to learn psychiatric interviewing skills…”
|
260 |
97.7 |
|
2 |
“The session increased my confidence in speaking to adolescents/parents…”
|
253 |
95.1 |
|
3 |
“The session helped me to apply what I have learnt…”
|
248 |
96.9 |
|
4 |
“The session stimulated my interest in Child and Adolescent Psychiatry…”
|
219 |
83.3 |
|
5 |
“My clinical tutor provided useful feedback…”
|
259 |
97.3 |
|
6 |
“The simulated patients’ performances felt realistic…”
|
258 |
97.7 |
|
7 |
“There was sufficient time for each case…”
|
256 |
95.9 |
|
8 |
“Overall, the session met the learning objectives…”
|
257 |
98.5 |
Table 2. Survey results for the Observed Clinical Interview Tutorial (OCIT)
Examining the effectiveness of these teaching activities in stimulating the students’ interest towards CAP, 83.3% of the respondents indicated that the CVT had done so, while a slightly higher proportion (85.5%) of the respondents reported that the OCIT stimulated their interest in CAP.
Majority of the respondents indicated that the clinical tutors were effective in facilitating the CVT (97.2%). Similarly, most of the respondents reported that the clinical tutors provided useful feedback during the OCIT (97.3%).
Entries in the free-text feedback section about what the students liked best about the CVT and OCIT included comments such as “good for application”, session allowed for “practice of interviewing skills” and “helped consolidate knowledge” (Figure 1). Several students liked the “interactive” nature of the interviews and discussions, as well as “feedback” from tutors, which also helped in their learning.
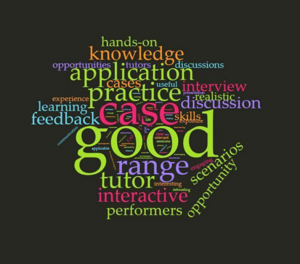
Figure. 1. Open comment feedback to the survey question “The best things about the sessions were…”
In areas that the students indicated for further improvement, they had cited for a “shorter” duration in each teaching session (Figure 2). This was likely due to the nature of a full day programme of CAP teaching which could last eight hours in a day with a one-hour lunch break. Others had shared that they preferred “smaller” groups so students could get more chances to practice interviewing the SPs and also be provided “more time for discussion” to allow more in-depth feedback as well as discussion of each clinical condition. Some students remarked that Objective Structured Clinical Examination (OSCE) styled marking schemes could help enhance their learning experiences as this method might be more structured, compared to an open discussion.

Figure 2. Open comment feedback to the survey question “Some ways which I think can make the sessions better are…”
IV. DISCUSSION
This study evaluated the effectiveness and acceptability of small group tutorials for CAP conditions, which are packaged inseparably as part of a medical undergraduate psychiatry teaching programme. CVT and OCIT are synergistically designed to complement each other in the curriculum. The surveys used to compile the medical undergraduates’ responses had focused on their learning experience with the CAP curriculum. The effectiveness of the teaching methods namely CVT and OCIT would be determined from transferability of the requisite knowledge base and the clinical skills, as well as availability of opportunities to experience interviewing for the participants. The survey responses were also used to gauge the performance of the SPs and the clinical tutors’ usefulness. In addition, the degree of how impactful the teaching sessions had in generating interest towards CAP was also evaluated.
The fourth-year medical students gave good feedback for the small group teaching sessions. They reported that the CVT were enjoyable, beneficial and had allowed them to apply what they had learnt. For the OCIT, most of the respondents indicated that the session had helped them to learn psychiatric interviewing skills, increased their level of confidence in speaking with adolescents and parents, and had helped them to apply in clinical scenarios what they had learnt. There is discernible difference between the feedback for CVT and OCIT. The students’ feedback for CVT affirmed applicability of the knowledge content of CAP whereas those for OCIT concurred with transferability of interviewing skills in terms of confidence level.
In the open feedback segment of the survey, respondents reported that they had particularly liked the interactive and hands-on aspect of the session, the frequent opportunities for evaluation and feedback, as well as for practice. However, they highlighted that certain factors such as the size of grouping, the length of the sessions and random allocation of conditions could be improved further to enhance their learning experience. Overall, their feedback still indicated positive experiences in these small group sessions, and this translated to an increased knowledge base, a heightened level of confidence, and burgeoned interest in CAP among the student participants.
This study’s limitations included the challenges inherent with attempting to accurately assess the students’ genuine experiences and feelings towards the sessions; with possible biases (recall and Hawthorne effect) in responding to questionnaires; and the lack of correlation to actual performances in real-world settings. Furthermore, what remained unanswered was how such sessions might truly generate interest leading to possibly pursuit of a career in CAP. In addition, it is uncertain whether changing the teaching methods with the curriculum could inspire more medical students and young doctors to consider specialising in this field and raise the number of residency applications. The data from our study did appear to be consistent with findings from other CAP clinical teaching programmes. In these programmes, more exposure to CAP and increased clinical opportunities did correlate with changes in impressions towards and appreciation of clinical interactions with children, increased positive views of CAP as part of medical practice, and heightened interest in CAP as a field of medical specialty (Dingle, 2010; Kaplan & Lake, 2008; Malloy et al., 2008; Martin, Bennett, & Pitale, 2005).
In the current undergraduate medical curriculum, the amount of time allocated to teaching CAP is relatively small compared to other topics. Child and adolescent psychiatric cases can be particularly complex and their management demand sensitive handling, which may pose challenges to real world practice. Youth patients and their parents may value privacy and sometimes do not allow medical students to be involved in initial assessments and subsequent follow-up consultations. These factors collectively pose unique challenges to teaching and equipping medical students with the skills and knowledge to address child and adolescent mental health disorders. While clinical contact and patient experience would be preferred and desirable for training, it may be impractical given the various constraints mentioned above (Kaplan & Lake, 2008). Hence, other creative methods of “exposure” to CAP patients should be incorporated into teaching rotations to offer medical students the opportunities to expand this knowledge base, apply the knowledge to practice scenarios, and further their clinical and communication skills. Small group sessions such as the CVTs and OCITs are teaching activities that can be used to overcome some of these challenges.
Our study showed that small group interactive teaching is effective in helping medical students to apply what they have learnt about CAP, increase their confidence in speaking to adolescents as patients and learn psychiatric interviewing skills. It also exposes them to a wide range of relevant CAP cases to which they can apply their theoretical knowledge and practice interview and management techniques. Furthermore, we have found that all this can be adequately achieved in a tailored environment that is conducive for learning. The collective constructive feedback had been used to further improve the content and deliverability style so as to enhance implementation in future batches. It has also been conceptualised to compare CVT and OCIT as individual teaching methods for future scholarly research.
V. CONCLUSION
The CAP small group interactive teaching sessions for medical students received good feedback from majority of the participants. This positive validation would spur the authors on to explore further how this pedagogy could help spark interests in Child and Adolescent Psychiatry among medical students given the shortfall of child and adolescent psychiatrists worldwide.
Notes on Contributors
AHYL analysed and interpreted data. CHJW, together with TJY and JCMW planned and conducted the child psychiatry small group teaching and collected feedback data from the medical students. TJY developed the feedback questionnaire. YSL, together with AHYL, CHJW and TTC planned and wrote the manuscript. All authors read and approved the final manuscript.
Ethical Approval
NHG DSRB reference number 2019/00431 for exemption.
Data Availability
Datasets generated and/or analysed during the current study are available from corresponding author on reasonable request.
Acknowledgements
The authors wish to thank the team from Centre for Healthcare Simulation, Yong Loo Lin School of Medicine, National University of Singapore for the invaluable support in recruiting and training the simulated patients for the CAP teaching program. We appreciate the participation of the simulated patients and medical students in the teaching programme.
Funding
There is no funding for this paper.
Declaration of Interest
As far as all the authors are concerned, we do not know of, or foresee any future competing interests. We are not aware of any issues relating to journal policies in submitting this manuscript. All the authors have approved of the manuscript for submission. The authors declare that they have no competing interests.
References
Baranne, M. L., & Falissard, B. (2018). Global burden of mental disorders among children aged 5–14 years. Child and Adolescent Psychiatry and Mental Health, 12(1), 19.
Breton, J. J., Plante, M. A., & St-Georges, M. (2005). Challenges facing child psychiatry in Quebec at the dawn of the 21st Century. The Canadian Journal of Psychiatry, 50(4), 203-212.
Costello, E. J., Egger, H., & Angold, A. (2005). 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. Journal of the American Academy of Child & Adolescent Psychiatry, 44(10), 972-986.
Dingle, A. D. (2010). Child psychiatry: What are we teaching medical students? Academic Psychiatry, 34(3), 175-182.
Erskine, H. E., Moffitt, T. E., Copeland, W. E., Costello, E. J., Ferrari, A. J., Patton, G., … & Scott, J. G. (2015). A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychological Medicine, 45(7), 1551-1563.
Hunt, J., Barrett, R., Grapentine, W. L., Liguori, G., & Trivedi, H. K. (2008). Exposure to child and adolescent psychiatry for medical students: Are there optimal “teaching perspectives”?. Academic Psychiatry, 32(5), 357-361.
Kaplan, J. S., & Lake, M. (2008). Exposing medical students to child and adolescent psychiatry: A case-based seminar. Academic Psychiatry, 32(5), 362-365.
Kyu, H. H., Pinho, C., Wagner, J. A., Brown, J. C., Bertozzi-Villa, A., Charlson, F. J., … & Fitzmaurice, C. (2016). Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: Findings from the global burden of disease 2013 study. JAMA Pediatrics, 170(3), 267-287.
Lim, C. G., Ong, S. H., Chin, C. H., & Fung, D. S. S. (2015). Child and adolescent psychiatry services in Singapore. Child and Adolescent Psychiatry and Mental Health, 9(1), 7.
Malloy, E., Hollar, D., & Lindsey, B. A. (2008). Increasing interest in child and adolescent psychiatry in the third-year clerkship: Results from a post-clerkship survey. Academic Psychiatry, 32(5), 350-356.
Martin, V. L., Bennett, D. S., & Pitale, M. (2005). Medical students’ perceptions of child psychiatry: Pre-and post-psychiatry clerkship. Academic Psychiatry, 29(4), 362-367.
Plan, S. (2002). A Call to Action: Children Need Our Help! American Academy of Child & Adolescent Psychiatry. Retrieved from https://www.aacap.org/app_themes/aacap/docs/resources_for_primary_care/workforce_issues/AACAP_Call_to_Action.pdf
Sawyer, M., & Giesen, F. (2007). Undergraduate teaching of child and adolescent psychiatry in Australia: Survey of current practice. Australian & New Zealand Journal of Psychiatry, 41(8), 675-681.
Thomas, C. R., & Holzer, C. E., 3rd (2006). The continuing shortage of child and adolescent psychiatrists. Journal of the American Academy of Child & Adolescent Psychiatry, 45(9), 1023-1031.
World Health Organization. (2014). Adolescent health epidemiology. Retrieved from http://www.who.int/maternal_child_adolescent/epidemiology/adolescence/en/
*Yit Shiang Lui
1E Kent Ridge Road
Tower Block, Level 9,
Singapore 119228
Tel: 6772 6331
Email address: yit_shiang_lui@nuhs.edu.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









