Cross-sectional study on the perceptions, attitudes, and practices of senior residents on overnight calls in a tertiary hospital during the COVID-19 pandemic
Submitted: 14 December 2023
Accepted: 14 May 2024
Published online: 1 October, TAPS 2024, 9(4), 76-80
https://doi.org/10.29060/TAPS.2024-9-4/CS3215
Vanda Wen Teng Ho1 & Kay Choong See2
1Division of Geriatric Medicine, Department of Medicine, National University Hospital, Singapore; 2Division of Respiratory and Critical Care Medicine, Department of Medicine, National University Hospital, Singapore
I. INTRODUCTION
Residents are vital to the medical workforce, especially for overnight call duties. Transitioning from junior roles to handling overnight calls as senior residents (SRs) can be anxiety-inducing, leading to decline in cognitive performance and fatigue (Weiss et al., 2016). These pose concerns for patient safety and quality of supervision, as SRs often serve as the most senior staff on-site overnight. However, calls offer valuable training opportunities, fostering autonomy, decision-making skills, and preparation for future consultant roles. The challenge is to ensure that overnight calls are safe for both patients and physicians while being conducive to learning.
During the COVID-19 pandemic, the health system’s reallocation of manpower substantially increased the workload. While there remains conflicting evidence on the optimal on-call arrangement, the Accreditation Council for Graduate Medical Education stipulates a maximum of 24 consecutive hours of direct patient care to safeguard against negative effects of chronic sleep deprivation (Nasca et al., 2010). In our tertiary hospital, two medical SRs performed stay-in overnight calls ranging from 15 to 21 hours (1700-0800h on weekdays and 1100-0800h on weekends). Before each call, SRs started work at 0700h. One SR was in-charge of the intensive care unit (ICU) and the other was on the general medicine floor. During each call, the ICU SR was responsible for supervising 2 stay-in junior residents, 2-5 new patient admissions and 20 existing ICU patients; the general medicine SR was responsible for supervising a team of four stay-in junior residents, 30-50 new patient admissions, and 100-150 existing inpatients. After each call, SRs would continue with the morning ward rounds before ending work. SRs could seek help by calling the duty consultant, who stayed out of hospital.
With limited data on SRs’ call experiences during the pandemic, understanding their perceptions and attitudes would be essential for system improvement and preparation for future challenges. Therefore, we aimed to explore the perceptions, attitudes, and practices of SRs with regards to overnight stay-in calls during the COVID-19 pandemic, as well as avenues for improvements in the call system.
II. METHODS
An electronic survey was conducted via monthly email invitation to SRs in the internal medicine department of a 1,200-bed tertiary university hospital between November 2021 and January 2022. All SRs approached had at least three calls per month. Each email invitation was sent to 40 SRs who consisted of the hospital’s on-call medicine pool. Consent was exempt as this was an anonymised survey (NHG DSRB reference number: 2021/00413). Participants were asked to provide their opinions on various aspects of these calls using a 5-point Likert scale. Monthly prompts to complete the survey were issued.
III. RESULTS
Out of the 40 medical SRs surveyed, 20 responded (50% rate). Their education backgrounds were split between the United Kingdom (n=7) and Singapore (n=13). All trained and worked as SRs in the same hospital group for 4-9 years (median 5 years). The specialties represented included advanced internal medicine (4 respondents), endocrinology (4 respondents), geriatric medicine (3 respondents), neurology (2 respondents), rheumatology (2 respondents), and one respondent each from respiratory and critical care medicine, haematology, infectious diseases. Two participants declined to state their specialty.
In terms of perception, SRs generally agreed that calls contributed to their development as specialists and were essential to their training. They found the learning experience during calls to be valuable for exposure to diverse cases, different from their specialist training which mostly occurred during daytime clinical work. In terms of attitude, most SRs felt prepared and confident for their calls. However, around one-quarter expressed doubts about handling difficult call situations. Many SRs believed that the patient experience overnight could be greatly improved. Nearly half perceived overnight patient care quality as compromised, with 95% noting a decline post-call. While the majority felt safe on-call, fifteen SRs agreed that they would ask for help on-call. Worryingly, only 55% were comfortable doing so and 60% preferred having more supervision during calls.
For potential improvements (Fig 1), SRs were asked to rank various choices on a 5-point Likert scale. These choices were specific to overnight calls. Most SRs agreed that the educational value of calls could be enhanced, and they would prefer to have fewer calls during their training. Around two-thirds disagreed with the idea that certain specialties should have more calls or that consultants should perform stay-in calls. Detailed results can be found in the Appendix.
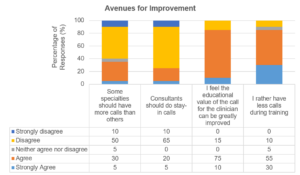
Figure 1. Avenues for improvement for senior residents’ call experience
IV. DISCUSSION
Our survey indicates that SRs felt prepared and recognised the educational value of overnight calls, but there is a clear need for enhanced learning experiences and supervision. Research on junior residents had shown that having in-house overnight hospitalists led to fewer barriers in contacting supervising physicians (Catalanotti et al., 2021) and improved the educational quality of calls (Trowbridge et al., 2010). However, SRs have varying preferences for such supervision, suggesting a need to explore the most suitable form of oversight.
Concerns about compromised patient care during and post-call periods suggest the negative impact of sleep deprivation on performance. Sleep deprivation can impact performance, and the debate around optimal work hours and call types continues, as shorter calls have not demonstrated improved outcomes (Schuh et al., 2011). Alternatives like increasing SRs on call each night should be considered while balancing frequency and stress levels. A larger survey on more hospitalists and SRs from other specialties is needed to confirm these findings and develop appropriate improvements to the on-call system.
V. CONCLUSION
Although the survey was relatively small and limited to one internal medicine department, the findings provide valuable insights for efforts to enhance SRs’ call experiences. Overall, SRs feel confident and safe during overnight calls, but further research is needed to explore and improve three areas: (1) call supervision; (2) learning value of calls; and (3) quality of patient care during and post-call. Graduate medical education programs must prioritise training excellence, resident well-being, and patient care. Our survey revealed challenges associated with overnight calls during a period of high workload marked by the COVID-19 pandemic, which we hope can stimulate the development and study of appropriate interventions.
Notes on Contributors
VWTH and KCS jointly conceptualised this study. VWTH conducted the study, wrote the manuscript, and analysed the data. KCS provided oversight during the study conduct and reviewed the manuscript.
Ethical Approval
This study has been approved by the National Health Group Domain Specific Review Board (reference number: 2021/00413).
Acknowledgement
The authors would like to thank the participating SRs for their responses.
Funding
This study has no funding sources.
Declaration of Interest
There are no interests to declare.
References
Catalanotti, J. S., O’Connor, A. B., Kisielewski, M., Chick, D. A., & Fletcher, K. E. (2021). Barriers to accessing nighttime supervisors: A national survey of internal medicine residents. Journal of General Internal Medicine, 36(7), 1974-1979. https://doi.org/10.1007/s11606-020-06516-4
Nasca, T. J., Day, S. H., & Amis, E. S., Jr. (2010). The new recommendations on duty hours from the ACGME task force. The New England Journal of Medicine, 363(2), e3. https://doi.org/10.1056/NEJMsb1005800
Schuh, L. A., Khan, M. A., Harle, H., Southerland, A. M., Hicks, W. J., Falchook, A., Schultz, L., & Finney, G. R. (2011). Pilot trial of IOM duty hour recommendations in neurology residency programs: Unintended consequences. Neurology, 77(9), 883-887. https://doi.org/10.1212/WNL.0b013e31822c61c3
Trowbridge, R. L., Almeder, L., Jacquet, M., & Fairfield, K. M. (2010). The effect of overnight in-house attending coverage on perceptions of care and education on a general medical service. Journal of Graduate Medical Education, 2(1), 53-56. https://doi.org/10.4300/jgme-d-09-00056.1
Weiss, P., Kryger, M., & Knauert, M. (2016). Impact of extended duty hours on medical trainees. Sleep Health, 2(4), 309-315. https://doi.org/10.1016/j.sleh.2016.08.003
*Dr Vanda Ho
Division of Geriatric Medicine,
Department of Medicine,
National University Health System ,
Tower Block Level 10, 1E Kent Ridge Rd
Singapore 119228
Email: vanda_wt_ho@nuhs.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









