Compounding training in pharmacy education in Singapore: Perceptions of final year undergraduate pharmacy students and compounding pharmacists
Published online: 2 January, TAPS 2018, 3(1), 15-26
DOI: https://doi.org/10.29060/TAPS.2018-3-1/OA1048
Yuen Teng Choo1, Mui-Ling Tan1, Cheong Hian Goh2 & Wai-Ping Yau1
1Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore, 2Health Products Regulation Group, Health Sciences Authority, Singapore
Abstract
Aim: To assess the importance of compounding training in today’s pharmacy education in Singapore, this study examined the perception of final year National University of Singapore (NUS) pharmacy undergraduates on compounding training in pharmacy education and their awareness of compounding services in Singapore in relation to compounding pharmacists’ perception, practice and role of pharmacy compounding in Singapore.
Methods: A cross-sectional survey was carried out between November 2013 and January 2014. It comprised of a questionnaire survey conducted on 134 final year pharmacy undergraduates, and face-to-face interviews conducted on 7 retail compounding pharmacists. Questionnaire responses were analysed using descriptive statistics, while the interviews were transcribed verbatim and analysed by thematic coding.
Results: Less than 40% of final year pharmacy undergraduates were aware of compounding activities and compounding pharmacies in Singapore. Nonetheless, majority agreed that compounding should be included in the pharmacy curriculum (83.6%) as it is an important part of pharmacy education (78.3%) and pharmacy profession (61.2%). All the interviewed compounding pharmacists felt that compounding in pharmacy education has provided them with the basics to build on knowledge and skills at work. Compounded medications were also viewed as necessary by 71.4% of the pharmacists in fulfilling the needs of certain patient populations.
Conclusion: Compounding training is necessary in pharmacy education. Pharmacy compounding has evolved from its traditional role into a professional speciality of customizing medications to meet different patient needs today. Hence, knowledge and skills in pharmacy compounding remain a relevant foundation for practising pharmacists to enhance pharmaceutical care at work.
Keywords: Pharmacy compounding; Pharmacy education; Pharmacy students; Compounding pharmacists; Perceptions; Survey
Practice Highlights
- Majority of the pharmacy undergraduates and retail compounding pharmacists surveyed considered compounding as an important part of pharmacy education and also an integral aspect of the pharmacy profession.
- Most of the retail compounding pharmacists felt that there was a place for compounding as a specialised service in Singapore to meet the needs of special populations and for individualised patient care.
- Students were more confident at preparing oral liquid preparations than topical preparations, but the latter were reported by retail compounding pharmacists as being more frequently compounded in practice.
- There is a need to build students’ confidence in compounding and to better prepare them to meet the needs of the compounding industry.
- Compounding training is necessary in pharmacy education.
I. INTRODUCTION
Pharmacy compounding is defined as the preparation of a patient-specific medication by a pharmacist in response to an individual prescription from a medical practitioner (Cauthon, Bowman, & Gurney, 2013). Traditionally, compounded medications are prepared for various reasons, from individual ingredients or by reformulating a medicinal product (Giam, McLachlan, & Krass, 2011). This includes instances where a product is made in response to a patient’s needs, e.g. allergy, or a more appropriate dosage form of the medicine formulated for improved patient compliance and administration. Over the years, the rise of mass drug manufacturing by the pharmaceutical industry has resulted in a drop in compounding of medications (Cauthon et al., 2013; Giam, McLachlan, & Krass, 2012). However, though demand was low, pharmacy compounding persisted especially when not all patients’ needs were met by manufactured medications, such as the non-suitability of manufactured products for certain patient groups and the unavailability of certain products in the market (Cauthon et al., 2013; Eley & Birnie, 2006; Mullarkey, 2009; Pegues, 2006).
Today, there appears to be resurgence in pharmacy compounding as a specialised service offered in more pharmacies, especially in Australia and the United States (U.S.) where pharmacy compounding accounts for about 1% of the prescription needs (Cauthon et al., 2013; Giam et al., 2012; Wilson, Blythe, & Sharfstein, 2012). It has been suggested that an increasing trend in the provision of compounding services by pharmacies was linked to the greater role that pharmacists can now play in the therapy of patients with the use of compounded medications (Giam et al., 2012; Maine, 2008). This resulted in improved communication and collaboration between pharmacists, and both doctors and patients, leading to greater professional satisfaction of pharmacists who provide this specialised service (Giam et al., 2012; Maine, 2008).
Compounding is incorporated in the curriculum of pharmacy schools in many countries (Aspden et al., 2011). In Singapore, formal training on compounding also remains by and large an integral aspect of the pharmacy curriculum. However, little is known about the compounding scene, such as the demand for compounded products in Singapore, or the relevance for pharmacists to be equipped with such skills in pharmacist professional training. Nonetheless, pharmacists are the only healthcare professionals with formal training in the knowledge and skills of compounding, and pharmacy compounding still remains an inherent part of the profession (Eley & Birnie, 2006; Mullarkey, 2009; Shrewsbury et al., 2012).
In order to assess the importance of compounding training in today’s pharmacy education in Singapore, the perspectives of both undergraduates in the pharmacy course as well as pharmacists working in compounding pharmacies need to be considered. This study thus examined the perception of final year National University of Singapore (NUS) pharmacy undergraduates on compounding training in pharmacy education and their awareness of compounding services in Singapore in relation to compounding pharmacists’ perception, practice and role of pharmacy compounding in Singapore. By gathering the views of graduating pharmacy students and practising pharmacists, the course content in pharmacy education can be tailored to meet the needs of the compounding industry in Singapore.
II. METHODS
A. Study Design
A cross-sectional study, comprising of a self-administered questionnaire survey and a face-to-face interview, was conducted from November 2013 to January 2014.
B. Questionnaire Survey
1) Study population: The target group was final year pharmacy undergraduates in NUS, which is the only university providing professional pharmacy education in Singapore. These students had completed all compounding modules in the curriculum, and with prior pharmacy practice experience (i.e. completed 6-week preceptorship programme in retail and hospital settings, respectively). Based on a 95% confidence level, proportion of 0.5 and a ±5% precision level, the minimum sample size targeted was 109 students out of the class size of 150.
2) Survey instrument: A self-designed questionnaire with 16 closed- and open-ended questions was used to gather information on students’ experience in compounding outside of the curriculum, as well as their awareness of compounding services and opinions on compounding in pharmacy education in Singapore. The questionnaire was first pilot-tested on three registered/pre-registration pharmacists who completed the questionnaires and provided feedback to improve the ease of understanding the questions. Results from the pilot test were not included in the final analysis.
3) Questionnaire administration: The voluntary, anonymous survey questionnaire was self-administered by final year NUS pharmacy undergraduates at the end of a pharmacy lecture. Questionnaires were completed and collected back on the spot.
C. Interview Survey
1) Study population: The target group was compounding pharmacists who worked in retail pharmacies whose mainstay of the business was compounding. These pharmacists were included as their job scope was primarily on pharmacy compounding. Pharmacists who carried out some compounding activities in hospitals and pharmaceutical companies were excluded.
Potential pharmacies that largely provided compounding services were identified from an online search on the open access Infosearch portal of the Health Sciences Authority of Singapore (http://eservice.hsa.gov.sg/prism/common/enquirepublic/SearchPharmacy.do?action=load). Retail compounding pharmacies were included after confirmation of their provision of compounding service through phone calls. All 11 pharmacists working at these included pharmacies were then approached in person and invited to participate in this study.
2) Survey instrument: Interviews with the pharmacists were conducted using a 16-question semi-structured interview guide that centred on pharmacy compounding. It was adapted with slight modification from a previous study (Giam et al., 2012) to obtain information on retail compounding pharmacists’ education, career, challenges, motivations and opinions, and their pharmacy operations. The interview guide was first pilot-tested on three registered/pre-registration pharmacists who were interviewed and provided feedback to improve the ease of understanding the questions. Results from the pilot test were not included in the final analysis.
3) Conduct of interview: For consistency, all the interviews were conducted by one trained investigator (YTC). Face-to-face interviews with the pharmacists were conducted at their retail compounding pharmacies during non-peak hours. Field notes were taken during the interviews and the interviews were also audio-recorded for pharmacists who consented to recording. Written informed consent was obtained from the interviewed pharmacists for participation in the interview and audio-recording, respectively.
D. Data Analysis
Data was analysed using IBM SPSS Statistics software (version 21). Descriptive statistics and chi-square tests were conducted. Statistical significance was set at p<0.05. Data from the interviews were transcribed verbatim and analysed by thematic coding.
III. RESULTS
A. Questionnaire Survey
1) Demographics of respondents surveyed: 139 final year pharmacy undergraduates were issued the questionnaire, out of which 134 completed questionnaires were received (response rate: 96.4%). The respondents have all participated in some form of pharmacy-related activities through either the pharmacy preceptorship programme or via their own work or internship experiences (Table 1).
2) Awareness of compounding activities and compounding pharmacies: Overall, most students (73.1%) were unaware of the existence of compounding pharmacies in Singapore. Only 38.1% (n=51) came across compounding activities in pharmacies, which were mainly during their hospital preceptorship programme (41/51, 80.4%). It is also interesting to note that most (84.3%) were unaware of contemporary issues in compounding, specifically the fungal meningitis outbreak associated with the use of contaminated compounded medication in the U.S. (Wilson et al., 2012).
3) Opinions on compounding in pharmacy education and practice: 83.6% of the students felt that compounding should be included in the pharmacy curriculum, with the top 2 reasons mentioned being that compounding is a traditional and exclusive specialised skill of pharmacists and that compounding skills will be useful when practising as a pharmacist (Table 2). Most also agreed that compounding is an important part of pharmacy education (78.3%) and pharmacy profession (61.2%) (Figure 1A).
Most students indicated that the time devoted to teaching compounding (67.9%), the breadth (76.9%) and depth (63.4%) of content taught in compounding, as well as the compounding knowledge (70.1%) and skills (68.7%) acquired, were just right in the NUS pharmacy curriculum (Table 3). Majority indicated that they understood the benefits (82.9%) and risks (80.6%) associated with compounded medications (Figure 1A). In addition, more than half of the respondents agreed that they have the knowledge (53.7%) and skills (60.4%) needed to compound medications (Figure 1A). Nonetheless only a minority felt that they were able to compound medications of good quality (32.1%) and ensure their compounded medications are free from contamination (17.9%) (Figure 1A).
Of the compounded formulations learnt in the NUS pharmacy curriculum, most respondents felt that suspensions (91.8%), solutions (87.3%) and extemporaneous preparations using commercially available products (79.9%) were relevant in pharmacy practice (Figure 1B). While most felt confident in compounding solutions (84.3%) and suspensions (79.1%), comparatively fewer students were confident in compounding extemporaneous preparations using commercially available products (64.1%) (Figure 1C). It is also interesting to note that although 70.9% of pharmacy undergraduates did feel that skin preparations, such as creams, gels and lotions, were relevant in pharmacy practice (Figure 1B), only around 60% have the confidence to compound them (Figure 1C). In addition, while more than half of the respondents (53.8%) felt that sterile preparations were relevant in pharmacy practice (Figure 1B), only 24.6% indicated that they were confident in compounding sterile preparations (Figure 1C).
When asked if the respondents would be interested in taking an advanced elective course in compounding if available, only slightly less than half (47.0%) were interested (Table 2). Those who felt that the time spent teaching compounding and that the breadth and depth of compounding taught were too little tend to express interest in taking this advanced elective course in compounding (p<0.05) (Table 3). Among those who were not interested in an advanced elective compounding course, the top 3 reasons mentioned were that it may not be relevant to future practice, they had other interests, and compounding taught in current pharmacy curriculum is sufficient (Table 2).
4) Place for compounding as a specialised service: 44.8% of the respondents felt that there is a place for compounding as a specialised service in Singapore, mainly because they saw the benefits of having compounded medications for special populations or for individualised patient care (Table 2). In contrast, among the 55.2% who felt that there was no place for compounding as a specialised service in Singapore, their main reason was that most products are commercially available or can be manufactured or prepared using machines in advance (Table 2).
| Demographics | n | (%) |
| Final year pharmacy undergraduates (n=134): | ||
| Gender | ||
| Male | 58 | (43.3) |
| Female | 76 | (56.7) |
| Participation in pharmacy-related activitiesa | ||
| Preceptorship I (Retail pharmacy)
Preceptorship I (Polyclinic pharmacy) Preceptorship II (Hospital pharmacy) Overseas work experience in a pharmacy Internship in industry |
115
20 123 13 12 4 |
(85.8)
(14.9) (91.8) (9.7) b (9.0) c (3.0) |
| Retail compounding pharmacists (n=7): | ||
| Gender | ||
| Male | 2 | (28.6) |
| Female | 5 | (71.4) |
| Age | ||
| ≤ 40 years | 5 | (71.4) |
| > 40 years | 2 | (28.6) |
| Pharmacy training | ||
| Locally trained | 6 | (85.7) |
| Foreign trained | 1 | (14.3) |
| Length of pharmacy course underwent | ||
| 3 years | 2 | (28.6) |
| 4 years | 5 | (71.4) |
| Years of working experience, median (range) | 11 | (4 – 47) |
| Previous work experience | ||
| Retail only | 2 | (28.6) |
| Retail and polyclinic | 1 | (14.3) |
| Retail and hospital | 1 | (14.3) |
| Retail and industry | 1 | (14.3) |
| Retail, hospital and industry | 2 | (28.6) |
a Each respondent could indicate more than one category from this list.
b Hospital pharmacy: 11 (8.2%); Retail pharmacy: 1 (0.7%); Charity organisation: 1 (0.7%)
c Taiwan: 7 (5.2%); United States: 3 (2.2%); Canada: 1 (0.7%); Not specified: 1 (0.7%)
Table 1. Demographics of final year pharmacy undergraduates surveyed (n=134) and retail compounding pharmacists interviewed (n=7)
B. Interview Survey
1) Demographics of respondents interviewed: Of the 11 retail compounding pharmacists approached, 7 accepted the interview (response rate: 63.6%). The other four pharmacists declined to participate as they were too busy (n=3) or not comfortable with sharing proprietary information of the pharmacy in an interview (n=1). Of the pharmacists interviewed, their years of working experience varied widely from 4 to 47 years (median=11 years) (Table 1). All pharmacists had previous work experience in retail pharmacies.
2) Compounding training in pharmacy education: All 7 pharmacists believed that pharmacy education provided them with the basics in compounding (Table 4): ‘…it sets a foundation… if I were not in pharmacy school, you wouldn’t know the properties of chemicals, what they do and how, so basically you can’t compound things or make things in terms of any way I want to.’ (Pharmacist 3). 71.4% also felt that compounding was a specialised skill that pharmacists were trained in.
While it is generally agreed that compounding is an integral aspect of pharmacy education, there were differences in opinions among the responses on how well pharmacy education has prepared them for compounding in pharmacy practice (Table 4). The depth of content taught in compounding or the time devoted to teaching compounding was insufficient to some pharmacists (28.6%) but just right to other pharmacists (28.6%). 42.9% of the respondents also felt that the clinical aspect of pharmacy was viewed as more important presently and more focused on compared with compounding training in pharmacy education (Table 4).
| n | (%) | |
| Do you think compounding should be included in the pharmacy curriculum? Why? | ||
| Yes (n=112; 83.6%) | ||
| · A traditional, exclusive specialised skill of pharmacists. | 33 | (29.5) |
| · Compounding skills may/ will be useful someday when practising as a pharmacist. | 32 | (28.6) |
| · Compounding knowledge and/ or skills are essential/ important/ good to know as part of pharmacy education. | 27 | (24.1) |
| · There are benefits of having compounded medications (e.g. for special populations, for individualised patient care). | 18 | (16.1) |
| · Interesting/ fun. | 16 | (14.3) |
| No (n=22; 16.4%) | ||
| · Most products are/ can be manufactured or prepared using machines in advance. | 7 | (31.8) |
| · Compounding appears to be uncommon in Singapore. | 5 | (22.7) |
| · Time-consuming/ inefficient. | 5 | (22.7) |
| · Can be trained at work. | 1 | (4.5) |
| · Compounding in the pharmacy curriculum is not necessary. | 1 | (4.5) |
| · Manufacturing, rather than compounding, can ensure products of good quality. | 1 | (4.5) |
| · There could be risk of contamination with compounded medications. | 1 | (4.5) |
| If an elective to provide students with a more advanced course in compounding is available, will you be interested in taking the module? Why? | ||
| Yes (n=63; 47.0%) | ||
| · Sounds interesting and/ or fun. | 34 | (54.0) |
| · Aids professional development/ enrichment through improving knowledge and honing skills in compounding. | 18 | (28.6) |
| · Provides compounding skills that may/ will be needed someday when practising as a pharmacist. | 12 | (19.0) |
| · Compounding is an important part of pharmacy education. | 2 | (3.2) |
| No (n=71; 53.0%) | ||
| · Compounding does not seem relevant/ applicable/ important to future practice. | 19 | (26.8) |
| · Not interested in taking advanced course in compounding/ have other interests that do not involve compounding/ pharmacy. | 17 | (23.9) |
| · Compounding taught in current pharmacy curriculum is sufficient. | 13 | (18.3) |
| · The current workload in school is too heavy/ takes up too much time already. | 7 | (9.9) |
| · Not a hands-on person. | 4 | (5.6) |
| · Not interested in pursuing compounding in future career. | 4 | (5.6) |
| · Taking this advanced elective course may affect academic results. | 3 | (4.2) |
| Do you think there is a place for compounding as a specialised service in pharmacy practice in Singapore? Why? | ||
| Yes (n=60; 44.8%) | ||
| · There are benefits of having compounded medications (e.g. for special populations, for individualised patient care). | 22 | (36.7) |
| · It is a specialised skill that pharmacists are trained in. | 10 | (16.7) |
| · It is a niche market with potential. | 9 | (15.0) |
| · Have seen compounding as a specialised service in Singapore. | 5 | (8.3) |
| · Compounding skills may/ will be useful someday when practising as a pharmacist. | 4 | (6.7) |
| No (n=74; 55.2%) | ||
| · Most products are commercially available/ can be manufactured or prepared using machines in advance. | 28 | (37.8) |
| · Demand for compounding service is low. | 13 | (17.6) |
| · Compounding is time-consuming/ inefficient/ technically challenging. | 8 | (10.8) |
| · Compounding appears to be uncommon/ not widely used in Singapore. | 7 | (9.5) |
| · Compounding is outsourced to companies or carried out by pharmacy technicians instead of pharmacists now. | 3 | (4.1) |
| · There are other areas of pharmacy that are more important these days and should be focused on. | 3 | (4.1) |
| · Manufacturing, rather than compounding, can ensure products of good quality and efficacy. | 2 | (2.7) |
| · Pharmacists not interested in compounding. | 1 | (1.4) |
a For each question, some respondents provided more than one reason while some did not indicate specific reasons(s).
Table 2. Identified reasons for opinions provided by final year pharmacy undergraduates (n=134) on compounding in pharmacy education and practicea
| Statements | Interested in taking advanced elective course in compounding if available | ||||||
| Overall | Yes | No | |||||
| (n=134) | (n=63) | (n=71) | |||||
| n | (%) | n | (%) | n | (%) | p value | |
| Time devoted to teaching compounding | < 0.0005* | ||||||
| Too little | 22 | (16.4) | 20 | (31.7) | 2 | (2.8) | |
| Just right | 91 | (67.9) | 41 | (65.1) | 50 | (70.4) | |
| Too much | 21 | (15.7) | 2 | (3.2) | 19 | (26.8) | |
| Breadth of content taught in compounding | 0.007* | ||||||
| Too little | 19 | (14.2) | 14 | (22.2) | 5 | (7.0) | |
| Just right | 103 | (76.9) | 47 | (74.6) | 56 | (78.9) | |
| Too much | 12 | (9.0) | 2 | (3.2) | 10 | (14.1) | |
| Depth of content taught in compounding | 0.005* | ||||||
| Too little | 40 | (29.9) | 27 | (42.9) | 13 | (18.3) | |
| Just right | 85 | (63.4) | 34 | (54.0) | 51 | (71.8) | |
| Too much | 9 | (6.7) | 2 | (3.2) | 7 | (9.9) | |
| Compounding knowledge acquired | 0.149 | ||||||
| Too little | 31 | (23.1) | 18 | (28.6) | 13 | (18.3) | |
| Just right | 94 | (70.1) | 43 | (68.3) | 51 | (71.8) | |
| Too much | 9 | (6.7) | 2 | (3.2) | 7 | (9.9) | |
| Compounding skill set acquired | 0.151 | ||||||
| Too little | 35 | (26.1) | 21 | (33.3) | 14 | (19.7) | |
| Just right | 92 | (68.7) | 40 | (63.5) | 52 | (73.2) | |
| Too much | 7 | (5.2) | 2 | (3.2) | 5 | (7.0) | |
* p < 0.05: results are statistically significant.
Table 3. Opinions of final year pharmacy undergraduates (n=134) on compounding in the NUS pharmacy curriculum in relation to their interest in taking an advanced elective course in compounding if available
(A)
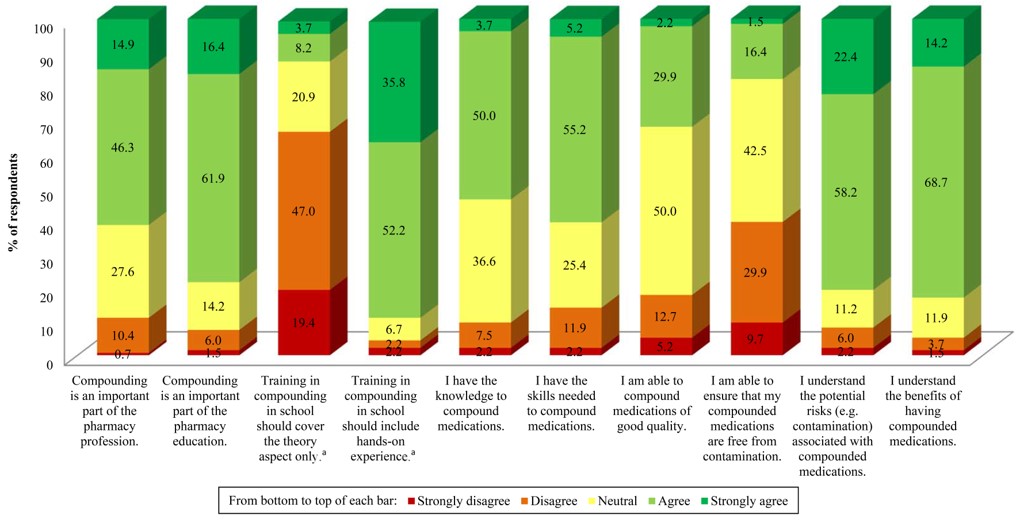
a Numbers do not add up to 100% due to non-response of participants.
(B)
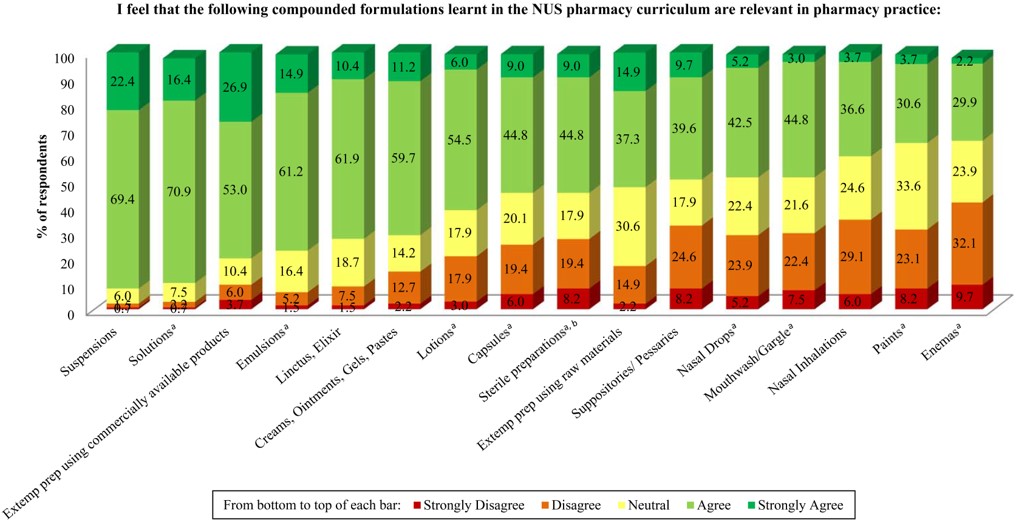
a Numbers do not add up to 100% due to non-response of participants.
b Examples provided in questionnaire: Aseptic solution preparation in ampoules, ophthalmic solutions
(C)
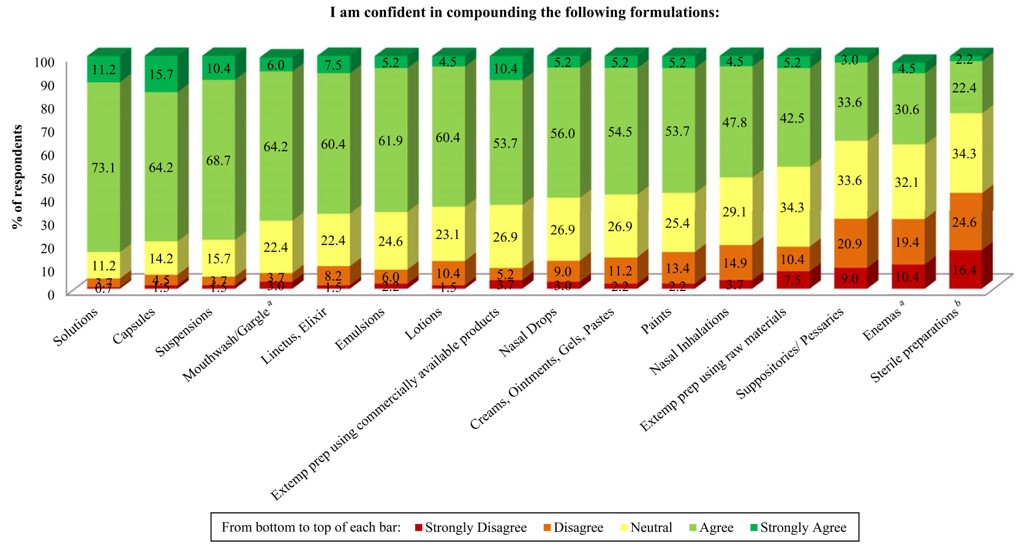
a Numbers do not add up to 100% due to non-response of participants.
b Examples provided in questionnaire: Aseptic solution preparation in ampoules, ophthalmic solutions
Figure 1. Opinions of final year pharmacy undergraduates (n=134) on: (A) statements related to compounding in pharmacy education, (B) the relevance of compounded formulations learnt in the NUS pharmacy curriculum to pharmacy practice, and (C) their confidence in compounding different formulations learnt in the NUS pharmacy curriculum.
| Themes | Responses | n | (%) |
| Compounding training in pharmacy education | · Compounding taught in school set the basics/ formed a foundation. | 7 | (100.0) |
| · It is a specialised skill that pharmacists are trained in. | 5 | (71.4) | |
| · Clinical aspect of pharmacy was deemed more important these days and more focused on than compounding. | 3 | (42.9) | |
| · Compounding in school prepared me well. | 3 | (42.9) | |
| · Compounding in school prepared me minimally. | 2 | (28.6) | |
| Knowledge of compounding in pharmacy practice | · Acquired compounding knowledge and skills outside school from: | ||
| o Experiences/ on-the-job | 7 | (100.0) | |
| o References/ resources | 5 | (71.4) | |
| o Other pharmacists at work | 4 | (57.1) | |
| o External training | 2 | (28.6) | |
| o Customers’ feedback | 1 | (14.3) | |
| o Suppliers of ingredients | 1 | (14.3) | |
| · Knowledge gained in school is lost after years without/ having no avenues for application. | 5 | (71.4) | |
| Motivations in choosing compounding as an area of specialty | · Interesting. | 4 | (57.1) |
| · Ability to customise medications for patients’ needs. | 3 | (42.9) | |
| · Compounding is a traditional and exclusive role of pharmacists. | 3 | (42.9) | |
| · A hands-on type of person. | 1 | (14.3) | |
| · Niche market. | 1 | (14.3) | |
| Challenges faced | · Meeting expectations of patients and doctors. | 5 | (71.4) |
| · A lot of time required to make the preparations. | 4 | (57.1) | |
| · Building up vast amount of knowledge in compounding. | 4 | (57.1) | |
| · Obtaining raw materials. | 2 | (28.6) | |
| · Creating awareness/ interest in compounding services. | 2 | (28.6) | |
| Compounding operations and practices | · Checking and counterchecking by pharmacists during compounding. | 7 | (100.0) |
| · Average shelf-life of compounded products is 6 months. | 7 | (100.0) | |
| · Compounding is a very manual process. | 6 | (85.7) | |
| · Low volume of sales of commercially available medications. | 6 | (85.7) | |
| · Standard practices in place to maintain adequate hygiene levels. | 6 | (85.7) | |
| · Specialisation of products compounded: | |||
| o Skin care | 4 | (57.1) | |
| o Bio-identical hormones | 2 | (28.6) | |
| Common dosage forms compounded | · Skin preparations (e.g. creams, gels, lotions). | 7 | (100.0) |
| · Capsules. | 3 | (42.9) | |
| · Oral liquid preparations (e.g. solutions). | 1 | (14.3) | |
| · Inhalations. | 1 | (14.3) | |
| · Troche. | 1 | (14.3) | |
| Place for compounding as a specialised service in Singapore | · Compounding as a specialised service in Singapore: | ||
| o There is a place for compounding as a specialised service. | 5 | (71.4) | |
| o There is no place for compounding as a specialised service. | 2 | (28.6) | |
| · Demand and awareness for compounding service is low among doctors and patients. | 6 | (85.7) | |
| · There are benefits of having compounded medications (e.g. for special populations, for individualised patient care). | 5 | (71.4) | |
| · Doctors must want compounded medications for patients/ doctors make the final decision. | 4 | (57.1) | |
| · Compounding appears to be uncommon in Singapore. | 4 | (57.1) | |
| · Potential for compounding in skin care to take off. | 3 |
(42.9) |
Table 4. Responses of retail compounding pharmacists interviewed (n=7)
3) Compounding in pharmacy practice: After graduation, the main method of acquiring compounding knowledge and skills for these pharmacists was through on-the-job training to gain more experience (Table 4). On the initial challenges faced when first working in pharmacy compounding, 71.4% of the pharmacists (n=5, all were less than 40 years old) expressed that the compounding knowledge gained in school was mostly forgotten, as they had not applied the knowledge for years since graduation: ‘…after like a few years later and ask you to do a cream and I suddenly forget like how do I start doing it.’ (Pharmacist 4). On the other hand, the pharmacists who were more than 40 years old (n=2) and had the opportunities to compound right after graduation mentioned that the knowledge and skills of compounding did not pose a challenge to them initially. The more senior pharmacists further commented that compounding was part and parcel of their competence as a pharmacist.
Within the operations of the pharmacies, checking and counterchecking during the process of compounding was an integral aspect of the practice of all compounding pharmacists interviewed (Table 4). Compounding was generally described as a very manual process in many of the pharmacies (85.7%).
The most common dosage forms compounded by all the pharmacists interviewed were mainly creams and topical preparations (Table 4): ‘I used to have some mixtures but not anymore. Now is mostly external.’ (Pharmacist 5). Oral liquid dosage forms such as solutions were only mentioned by one (14.3%) pharmacist. No sterile compounding was said to be carried out at all of their facilities: ‘We do not have sterile facilities so we do not make ophthalmic preparations. No injections too.’ (Pharmacist 7). On a side note, 85.7% of the pharmacists mentioned that their pharmacies handled low volume of sales of commercially available medications.
4) Place for compounding as a specialised service: 71.4% of the pharmacists felt that there was a place for compounding as a specialised service in Singapore as compounded medications can provide for the individual and specific needs of patients (Table 4). While 85.7% felt that the demand and awareness of compounding service was low, its relevance was nonetheless highlighted: ‘I think it is here to stay although it would not be so big like compounding pharmacies everywhere. It is still viable; there are still people who have the needs for it.’ (Pharmacist 6).
IV. DISCUSSION
In Singapore, only licensed retail pharmacies can compound medications in accordance to a doctor’s prescription. Pharmacy compounding is traditionally a manual process, and it is important to understand the training of pharmacists in these operations. In this study, pharmacy students and compounding pharmacists provided useful feedback on their academic training and knowledge in pharmacy compounding. It is interesting to note that final year NUS pharmacy undergraduates and retail compounding pharmacists share common views regarding compounding training in pharmacy education and pharmacy practice, as well as whether there is a place for compounding as a specialised service in Singapore.
A. Compounding in Pharmacy Education and Practice
In this study, most final year pharmacy undergraduates and retail compounding pharmacists considered compounding as an important part of pharmacy education and also an integral aspect of the pharmacy profession as it is a specialised skill that pharmacists were trained in. This is in agreement with the results in an Arizona study where 95% of 412 pharmacists surveyed agreed that compounding is an important part of the pharmacy profession and 99% indicated that some aspects of compounding should be taught in pharmacy school (Cauthon et al., 2013).
Over the years, with a switch in the approach in pharmacy education and practice from product-focused to patient-centred care, clinical knowledge appeared to have a more important position in education (Maine, 2008; Ryan et al., 2008), as commented by some surveyed pharmacists and undergraduates. Despite this, compounding itself was reported to lead to greater patient-centred care as opposed to using commercial products for reasons such as the ability to provide individualised medications and develop stronger professional relationship with patients (Cauthon et al., 2013; McPherson & Fontane, 2010). Indeed, compounding skills are still considered important to be imparted to pharmacy students in many pharmacy schools globally (Aspden et al., 2011). From an American Association of Colleges of Pharmacy (AACP) survey study that evaluated compounding education within the curriculum of its member institutions, all 137 respondents unanimously supported the inclusion of compounding education as part of the curriculum in pharmacy school (Shrewsbury et al., 2012), showing the importance of imparting compounding knowledge and skills to pharmacy students.
The AACP study reported that compounding education was included at an average of 2.2 semesters (range: 0-6 semesters) in the pharmacy curriculum of the respondents’ institutions, with the time spent on a single compounding laboratory exercise ranging from ≤2.5 hours to ≥6 hours (Shrewsbury et al., 2012). In the NUS undergraduate pharmacy curriculum at the point of this study, compounding education was included in 6 semesters in total in the 4-year pharmacy curriculum in NUS (i.e. 6 out of 8 semesters), with a 3-hour laboratory session per week for around 6 weeks spent on compounding exercises for most modules. Hands-on compounding laboratory sessions were incorporated in Pharmacy Practice I and III, Pharmacy Law, and Dosage Form Design I, II and III modules. In this regard, most undergraduates surveyed generally agreed that the amount of time devoted to compounding and the content of compounding taught in the NUS curriculum is just right. The component of compounding training has continued to be included in the revamped NUS undergraduate pharmacy curriculum starting August 2014.
While school provided the basics in compounding, all the interviewed pharmacists gained the knowledge and skills they needed through experience at work and learning on the job. Nonetheless, the knowledge and skills from pharmacy education was still important to the pharmacists interviewed. It served as a starting point to allow them to take up compounding at work: ‘Of course pharmacy education prepared me before I can do all this.’ (Pharmacist 3). The knowledge gained on the job mainly served to supplement what was taught to pharmacy undergraduates to improve their knowledge and skills in compounding: ‘The basic skills like I said, was from my time in school, but NUS course is very basic. For more advanced skills, it’s mainly on the job…’ (Pharmacist 6). Indeed, 71.4% of the pharmacists also stated that compounding knowledge gained in school is lost when not used for many years after graduation. This was also shown in some studies whereby pharmacy students do not retain all the compounding knowledge and skills they learnt over the course (Eley & Birnie, 2006), and often after graduation, additional training is required during actual practice at work (Kairuz, Noble, & Shaw, 2010). However with sufficient time, the knowledge and skills can be easily recalled once again: ‘…not very familiar with this skill because we have not touched them for a very long time but after a while it’s still quite okay.’ (Pharmacist 4), clearly highlighting the importance of building a foundation in compounding in school.
In our study, both undergraduate students and practising pharmacists perceived compounding to be interesting and can provide for patients’ needs, and in line with the traditional role of pharmacists in compounding. These motivations to compound were largely similar with studies in Australia and the U.S., which also encompassed aspects of developing a stronger professional relationship with the patients and the professional satisfaction derivable by the pharmacists providing the service (Giam et al., 2011, 2012; McPherson & Fontane, 2010).
Our undergraduate students were most confident in compounding oral liquid dosage forms, such as suspensions and solutions, which they felt were most relevant in practice. These were also the most commonly compounded preparations in pharmacy schools in the U.S. (Shrewsbury et al., 2012). In practice, however, the pharmacists interviewed in our study indicated that skin preparations, especially creams, were more commonly compounded instead. Similarly, community pharmacists providing compounding services in the U.S. reported that the most common preparations compounded were first and foremost also dermatological preparations for localised effects (ointments, creams and gels) (90.7%), followed by oral solutions (73.2%) and suspensions (70.4%) (Martin et al., 2009).
In terms of sterile compounding in the curriculum, at least half of the pharmacy undergraduates felt that sterile preparations were relevant to pharmacy practice, even though not all were equally confident in compounding these preparations. This may be due to the range of sterile preparations compounded within the NUS pharmacy curriculum which was not as comprehensive as that in the curriculum of U.S. pharmacy schools. The latter included compounding of a wide range of sterile preparations including intravenous solutions (both small and large volume parenterals), ophthalmic and otic solutions, and chemotherapy in biological safety hood as part of their required course (Shrewsbury et al., 2012). While sterile compounding may not apply in the retail setting as mentioned by the pharmacists interviewed, such skills remain relevant to the compounding industry, especially in hospitals and specialized institutions. Indeed, the AACP study has stressed on the importance of sufficiently training students in sterile compounding within the pharmacy curriculum (Shrewsbury et al., 2012).
B. Place for Compounding
Based on the students’ and practising pharmacists’ perspectives, compounding does not appear to be common in Singapore. According to the pharmacists interviewed, it seems that the demand and awareness for compounding services is low among the doctors and patients. Nonetheless, majority of the pharmacists felt that there was a place for compounding as a specialised service in Singapore to meet the requirements of specific patients. This underscores the need to create greater awareness among doctors and patients, and even pharmacy undergraduates, that there are compounding pharmacists who are capable of compounding alternative options for patients’ therapy apart from commercially available products.
C. Significance of Findings
Our study revealed two findings that are significant to the educational institution. Nearly 30% of students reported to feeling only minimally prepared to compounding and they were more confident at preparing oral liquid preparations (e.g. solutions) than topical preparations (e.g. creams), but the latter were reported by retail compounding pharmacists as being preparations that are more likely to be compounded in practice. These findings serve as feedback to assist with curriculum design. There is a need to build students’ confidence in compounding and to better prepare them to meet the needs of the compounding industry.
D. Strengths and Limitations
As our study focused on retail compounding pharmacists, the results may not be generalizable to the entire compounding industry in Singapore, which extends to the hospitals as well. In addition, the interview was limited by the small sample size due to the inherent small number of pharmacists practising in retail compounding pharmacies. Nonetheless, the study does capture a representative view of the pharmacists from retail compounding pharmacies, with a total response rate of 63.6%. In addition, having the opinions of the undergraduates help supplement that of the pharmacists to provide a more comprehensive evaluation of the importance and relevance of compounding training in pharmacist professional education.
V. CONCLUSION
Compounding in pharmacy education provides pharmacists with the basic skills needed for future careers in compounding. Such training is still emphasized in many pharmacy schools around the world, albeit dedicating different content and depth in the curriculum time.
Like other aspects of pharmacist professional training, the knowledge and skills in compounding may be honed on-the-job as pharmacists gain experiences in compounding in their career. However, without the basics to start them off on, they would not know where to begin. Even if they thought they had forgotten most of what they learnt in school when they started working in the compounding pharmacies, they were still able to recall with time and pick up the knowledge and skills again. The findings in this study strongly reiterate the need for the continued role of compounding training in the curriculum of pharmacist professional education.
The basics imparted have allowed the pharmacists to move on to advance their knowledge and skills to enhance pharmaceutical care at work. Compounding does not belong to the past. While the true potential of compounding in Singapore seems unclear, doctors continue to work with pharmacists to seek alternatives to commercialised products for their patients. Compounded medications continue to fulfil different patient needs today and pharmacists must be adequately trained and competent to provide this specialised service. Indeed, there is a place for compounding training in pharmacy education in Singapore.
Notes on Contributors
Ms. Yuen Teng Choo, BSc (Pharm) (Hons), is currently a pharmacist at Ng Teng Fong General Hospital. She conducted this research study while she was an Honours year undergraduate student with the Department of Pharmacy at the National University of Singapore.
Ms. Mui-Ling Tan, MSc (Healthcare Management), is a Senior Lecturer at the Department of Pharmacy, National University of Singapore, and a registered pharmacist in Singapore. She teaches pharmacy professional skills and pharmacy law. As coordinator for professional placement, she also manages the pre-employment clinical training (PECT) programme for pharmacy undergraduates.
Dr. Cheong Hian Goh, PhD, is a registered pharmacist in Singapore and is currently Deputy Director of the GDP Unit at the Audit and Licensing Division of the Health Products Regulation Group of Health Sciences Authority (HSA), Singapore. He is also a preceptor to pharmacy undergraduates undergoing PECT at HSA.
Dr. Wai-Ping Yau, PhD, is a Lecturer at the Department of Pharmacy, National University of Singapore, and a registered pharmacist in Singapore. She teaches pharmacokinetics, pharmacostatistics and research methodology. She is also a member of the committee overseeing the pharmacy experiential program in service-oriented undergraduate learning (SOUL) for pharmacy students.
Ethical Approval
The study protocol was approved by the NUS Institutional Review Board.
Acknowledgements
This work was supported by the National University of Singapore Department of Pharmacy (Project Grant C-148-000-003-001).
Declaration of Interest
Authors have no conflicts of interest, including no financial, consultant, institutional and other relationships that might lead to bias.
References
Aspden, T. J., Anderson, C., Rew, A., Tan, J., Woodrow, R., & Zheng, Y. (2011). An investigation into the teaching of extemporaneous compounding skills to pharmacy students in schools of pharmacy in Australia, Canada, New Zealand, South Africa and the United Kingdom. Paper presented at the 9th International Conference: Life Long Learning in Pharmacy, Rotorua, New Zealand.
Cauthon, K. A., Bowman, B. J., & Gurney, M. K. (2013). Compounding practices and beliefs of Arizona pharmacists. International Journal of Pharmaceutical Compounding, 17(2), 154-161.
Eley, J. G., & Birnie, C. (2006). Retention of compounding skills among pharmacy students. American Journal of Pharmaceutical Education, 70(6), 132.
Giam, J. A., McLachlan, A. J., & Krass, I. (2011). Community pharmacy compounding–impact on professional status. International Journal of Clinical Pharmacy, 33(2), 177-182.
Giam, J. A., McLachlan, A. J., & Krass, I. (2012). Characterizing specialized compounding in community pharmacies. Research in Social & Administrative Pharmacy, 8(3), 240-252.
Kairuz, T., Noble, C., & Shaw, J. (2010). Preceptors, interns, and newly registered pharmacists’ perceptions of New Zealand pharmacy graduates’ preparedness to practice. American Journal of Pharmaceutical Education, 74(6), 108.
Maine, L. L. (2008). A Contemporary Perspective on Compounding Education. International Journal of Pharmaceutical Compounding, 12(3), 279.
Martin, K. S., McPherson, T. B., Fontane, P. E., Berry, T., Chereson, R., & Bilger, R. (2009). Independent community pharmacists’ perspectives on compounding in contemporary pharmacy education. American Journal of Pharmaceutical Education, 73(3), 54.
McPherson, T., & Fontane, P. (2010). Patient-centered care in the community-based compounding practice setting. Journal of the American Pharmacists Association, 50(1), 37-44.
Mullarkey, T. (2009). Pharmacy compounding of high-risk level products and patient safety. American Journal of Health-System Pharmacy, 66(17 Suppl 5), S4-S13.
Pegues, D. A. (2006). Improving and enforcing compounding pharmacy practices to protect patients. Clinical Infectious Diseases, 43(7), 838-840.
Ryan, M., Shao, H., Yang, L., Nie, X. Y., Zhai, S. D., Shi, L. W., & Lubawy, W. C. (2008). Clinical pharmacy education in China. American Journal of Pharmaceutical Education, 72(6), 129.
Shrewsbury, R., Augustine, S., Birnie, C., Nagel, K., Ray, D., Ruble, J., Scolaro, K., & Athay Adams, J. (2012). Assessment and recommendations of compounding education in AACP member institutions. American Journal of Pharmaceutical Education, 76(7), S9.
Wilson, L. E., Blythe, D., & Sharfstein, J. M. (2012). Fungal meningitis from injection of contaminated steroids: A compounding problem. JAMA, 308(23), 2461-2462.
* Wai-Ping Yau
Department of Pharmacy
Faculty of Science
National University of Singapore
18 Science Drive 4
Singapore 117543, Singapore
Tel: 6516 8913
Fax: 6779 1554
Email: phaywp@nus.edu.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









