Comparison of in-class learning engagement of PGY-1 interns during online and in-person teachings using a modified classroom observational tool
Submitted: 13 January 2022
Accepted: 9 May 2022
Published online: 4 October, TAPS 2022, 7(4), 35-49
https://doi.org/10.29060/TAPS.2022-7-4/OA2699
Yuan Kit Christopher Chua1*, Kay Wei Ping Ng1*, Eng Soo Yap2,3, Pei Shi Priscillia Lye4, Joy Vijayan1, & Yee Cheun Chan1
1Department of Medicine, Division of Neurology, National University Hospital Singapore, Singapore; 2Department of Haematology-oncology, National University Cancer Institute Singapore, Singapore; 3Department of Laboratory Medicine, National University Hospital Singapore, Singapore; 4Department of Medicine, Division of Infectious Diseases, National University Hospital Singapore, Singapore
*Co-first authors
Abstract
Introduction: In-class engagement enhances learning and can be measured using observational tools. As the COVID-19 pandemic shifted teaching online, we modified a tool to measure the engagement of instructors and students, comparing in-person with online teaching and different class types.
Methods: Video recordings of in-person and online teachings of six identical topics each were evaluated using our ‘In-class Engagement Measure’ (IEM). There were three topics each of case-based learning (CBL) and lecture-based instruction (LLC). Student IEM scores were: (1) no response, (2) answers when directly questioned, (3) answers spontaneously, (4) questions spontaneously, (5) initiates group discussions. Instructor IEM scores were: (1) addressing passive listeners, (2) asking ≥1 students, (3) initiates discussions, (4) monitors small group discussion, (5) monitoring whole class discussions.
Results: Twelve video recorded sessions were analysed. For instructors, there were no significant differences in percentage time of no engagement or IEM scores when comparing in-person with online teaching. For students, there was a significantly higher percentage time of no engagement for the online teaching of two topics. For class type, there was overall less percentage time of no engagement and higher IEM scores for CBL than LLC.
Conclusion: Our modified IEM tool demonstrated that instructors’ engagement remained similar, but students’ engagement reduced with online teaching. Additionally, more in-class engagement was observed in CBL. “Presenteeism”, where learners were online but disengaged was common. More effort is needed to engage students during online teaching.
Keywords: Engagement, Observational Tool, Online Learning, E-learning, COVID-19, Medical Education, Research
Practice Highlights
- Lectures to large class (LLC) and case-based learning (CBL) are associated with lower levels of student engagement when conducted on a virtual platform.
- Instructors’ engagement during online teachings remained similar to that of in-person teachings.
- LLC is associated with reduced student engagement than CBL.
I. INTRODUCTION
Educational theories suggest that learning should be an active process. According to social constructivist theory, learning can be better achieved by social interactions in the learning environment (Kaufman, 2003). Active learning strategies fostering the students to interact with each other and the instructor such as discussions, talks, questions, may yield desirable learning outcomes in terms of knowledge, skills, or attitudes (Rao & DiCarlo, 2001). Therefore, using in-class learner engagement as an important keystone of active learning strategies is known to stimulate and enhance the learner’s assimilation of content and concepts (Armstrong & Fukami, 2009; Watson et al., 1991).
There is good evidence for the importance of engagement in online learning and use of an engagement metric has been advocated to better understand student online interactions to improve the online learning environment (Berman & Artino, 2018). While medical literature suggests that virtual education games foster engagement (McCoy et al., 2016), the level of engagement and learning fostered by online methods for group discussion and teaching is unknown. Teleconferencing is among some of the methods suggested for maintaining education during the COVID-19 pandemic (Chick et al., 2020).
Possible methods of quantifying student engagement include direct observation and student self-report. O’Malley et al. (2003) has published a validated observation instrument called STROBE to assess in-class learner engagement in health professions without interfering with learner activities. This observation instrument is used to document observed dichotomized types of instructor and student behaviors in 5-minute cycles and quantify the number of questions asked by the instructor and students in different class subtypes. This instrument as well as revised forms of this instrument has since been used as “in-class engagement measures” to compare instructor and student behaviors in different class types (Alimoglu et al., 2014; Kelly et al., 2005).
In our institution, a hybrid curriculum of case-based learning as well as lecture-style courses is used to teach the post graduate year one (PGY-1) interns. We had video recordings of these courses performed in-person prior to the COVID-19 pandemic. With the advent of the pandemic, these courses were shifted onto Zoom teleconferencing platform, but delivered by the same instructors, in the same class format.
We therefore aimed to determine and compare in-class learning engagement levels via observing instructor and student behaviours in different platforms of learning (either observed online or in-person retrospectively via video recording) delivered by the same instructor before and during the COVID-19 pandemic. We also aimed to compare instructor and student behaviours in different class types (either case-based learning or lecture style instruction). To do this, we planned to modify a known in-person observational tool for student engagement – “STROBE” (O’Malley et al., 2003) for use in analysing and recording the behaviours of students in both online and in-person teaching.
II. METHODS
A. Observed Class Types
In this study, we observed two different class types, case-based learning (CBL), as well as lecture-based instruction to teach basic medical/surgical topics to a large classroom (LLC) of PGY-1 interns. Video recordings of these in-person teachings were made in 2017. Both these class types were replicated in the same format on an online Zoom teleconferencing platform and were delivered by nearly all of the same tutors using the same content and Powerpoint slides during the COVID-19 pandemic in 2020. We aimed to view the 2017 video-recordings of the in-person teachings and compare them with the 2020 online teaching of PGY-1 interns. Written consent was obtained from the tutors and implied consent from the students. Students were informed beforehand via email that the sessions were going to be observed and they were again reminded at the start of each session where they had the chance to opt out. Subsequently, all student feedback and observation scores were amalgamated and de-identified. This study was approved by the institution’s ethics board.
Three topics each of case-based learning as well as lecture-style instruction were selected in chronological order as scheduled for students. Each topic of instruction was allotted up to a maximum of 90 minutes of time, but the instructor could choose to end the class earlier if the session was completed. Description of both class types are below.
1) Description of case-based learning in large classroom
The content of the learning was designed by the instructor, and consisted of clinical cases involving patient scenarios, where the main pedagogy was problem-solving and answering case-based questions relating to the patient scenario (e.g., diagnosis, reading clinical images or electrocardiograms, creating an investigation or treatment plan). Each case would typically take about 15 to 20 minutes to complete, and there would typically be five to six cases. Students were expected to answer the questions, and the instructor gave feedback on the answers and provided additional information, sometimes via additional Powerpoint slides. Class discussions were encouraged where students were encouraged to debate and discuss with each other over their classmates’ answers. The titles of the case-based learning were “ECG – tachydysrhythmias”, “Approach to a confused patient” and “Approach to chest pain”.
2) Description of lecture in large classroom
This is a typical lecture-style instruction performed with participation of around 86 PGY1-interns and one instructor. The instructor delivers information via a Powerpoint slide presentation and rarely adds clinical case-based questions into the slides to invite student discussion. The titles of the lectures were “Cardiovascular health – hypertensive urgencies”, “Trauma – chest, abdomen and pelvis” and “Stroke”.
B. Instructor and Student Characteristics
The instructors all had at least ten years of teaching experience in medical education, and all had been teaching the same topics to the PGY-1 interns for at least the last five years. Student feedback scores on their teaching activities have been satisfactorily high (mean 4.63 for 2019, the year prior to the shift to online learning for the pandemic). All the tutors (except for one instructor who taught “Stroke”) had taught the same topics using the same content and Powerpoint slides in 2017 via in-person teaching which was caught on camera.
The students were all PGY-1 interns, who have been asked by the institution to attend at least 70% of a mandatory one-year long teaching program where they are given weekly instruction on various medical or surgical topics. The teaching program commences from May of each year. There were 86 PGY-1 interns commencing their rotations in our institution and attending the teaching program from May 2020. There were 75 PGY-1 interns attending the teaching program in the video recordings caught in 2017.
C. Observation Tool
A revised form of STROBE (O’Malley et al., 2003) was used to analyze and record the behaviors of the instructor and students in classes, to provide a more objective third-person measure of student engagement. The original STROBE tool was an instrument that was developed to objectively measure student engagement across a variety medical education classroom settings. The STROBE instrument consists of 5-minute observational cycles repeated continuously throughout the learning session with relevant observations recorded on a data collection form. Within each cycle, observers record selected aspects of behavior from a list of specified categories that occur in each interval recorded. Observations include macrolevel elements such as structure of class, major activity during time, and a global judgment of the proportion of class members who appear on task, as well as microlevel elements such as instructor’s behavior and the behaviors of four randomly selected students. Observers also record who the behaviours of instructors and students were directed at. After which, observers tally the number of questions asked by the students and instructor in the remainder of the 5 minutes. The revision of this tool was made by the 3 Clinician-educators from the research team (CYC, YES, KN), having discussed what kind of instructor and student behaviors were considered as “active student engagement”, keeping the main statements and principles of the original STROBE tool. The scale was modified to make it suitable for use in an online learning setting, where the observers may not be able to observe the student’s body language cues when the student does not turn on his/her video function. We called this modified scale our ‘In-class engagement measure’. The modified scales were as follows:
A 5-item list of instructor and student behaviors was therefore created and rated from 1 to 5 each, with different scales for instructor and student. For the student behavior scale, each item was to show progressively increasing levels of interaction, and perceived engagement, both with the instructor and with each other. For the instructor behavior list, each item was also about progressively interactive behaviors by the instructor to get the students to engage. We called these scales our “In-class Engagement Measure (IEM)”. The scales were as follows:
Student:
- No response even when asked
- Answers only when directly questioned
- Answers questions spontaneously
- Speaks to instructor spontaneouslyg.,Poses questions, discusses concepts
- Speaks to instructor and 1 or more other student during a discussion
Instructor:
- Talking to entire class while all the students are passive receivers
- Telling/asking to one or a group of students, or teaching/showing an application on a student
- Starting or conducting a discussion open to whole class, or assigning some students for some learning tasks
- Listening/monitoring actively discussing one or a group of students
- Listening/monitoring actively discussing entire class
For the student behaviour list, we also sub-categorized the student behaviour item “1”, where “1*” was defined as no response when a question was posed to a specific student and not just the whole class, where the student-in-question would have his/her name called by the tutor.
D. Observation Process
Drawing from the described process for the STROBE observation tool (O’Malley et al., 2003), as well as other described modifications of the STROBE tool (Alimoglu et al., 2014), we used the same observation units and cycles. Modifications to the original described process for the STROBE observation tool was made to make it suitable for not being in-person when observing a large group of students and their instructor. Three observers from the research team (CYC, YES, KN) observed and recorded the instructor and student behaviors for the three case-based learning and three lecture-style learning conducted live online in 2020, and as a video recording of in-person teaching in 2017. A total of 12 lectures were therefore analyzed. One observation unit was a 5-minute cycle. The 5-minute cycle would proceed as such: The observer would write the starting time of the cycle and information about the class (number of students, title of session). The observer would select a student from the class and observe that student for 20 seconds and mark the type of engagement observed according to the IEM scale created. As the observers were not in-person for the teaching at either the 2017 video recording, and for the 2020 online learning, students who responded to the instructor or posed questions were marked at the same time by all the three observers. The 5-minute cycle would consist of four 20-second observations of individual learners, so marking of student engagement would be performed four times within that cycle with different students in succession. The observer would also observe the instructor for that 5-minute cycle and similarly mark the instructor’s behavior once for that 5-minute cycle. For the remainder of the modified STROBE cycle, the observer would tally the number of questions asked by all the students and the instructor.
Observers independently and separately observed and marked the students’ and instructors’ behaviors. Due to the lack of in-person observation, students who responded or posed questions during the session were uniformly chosen for marking by the three observers. If a student had already been marked once during that cycle, the same student was not used for remaining three observations within the same cycle. At the end of the marking, two observers (KN and YES) compared their scores for both students and instructor. The marks given by the third observer (CYC) was used to validate the final score awarded and used as the tiebreaker when there was a discrepancy in the marks given by the first two observers.
E. Collation of Post Teaching Survey Feedback
Apart from the data derived from our modified observational tool, we also reviewed data from surveys conducted by the educational committee after each of these teaching sessions (see Table 1). These were general surveys used to solicit student feedback on the teaching sessions. They were distributed in-person in 2017, with the same forms distributed to the students online in 2020. Responses from the students were in response to five statements, with scoring 0 to 5 (1 for Strongly disagree, 2 for disagree, 3 for neither agree nor disagree, 4 for agree, and 5 for Strongly agree). These feedback forms had an overall feedback score marked by the student, as well as a score marked by the student in response to a question assessing for self-reported engagement – “The session was interactive and engaging”. The other questions were “The session has encouraged self-directed learning and critical thinking”, “The session was relevant to my stage of training”, “The session helped me advance my clinical decision-making skills”, and “The session has increased my confidence in day-to-day patient management”. Means of the feedback scores were taken as a qualitative guide, and we analyzed the overall feedback scores (“Overall feedback score” in Table 1), and the scores in response to the question assessing for self-reported engagement (“Self-reported engagement feedback score” in Table 1).
F. Statistical Analyses
Descriptive statistics were used to determine frequencies and median number of questions asked, as well as mean student feedback scores and absolute duration of each teaching session. Fisher exact test was also performed to analyze the differences in scores between different lectures and case-based learning, and the scores in the 2017 in-person learning versus that of the 2020 online learning. For analysis of the scores, we dichotomized our scores using the cut-off of “1”, or our first item on the behavior list for both students and instructors, as we felt that the first item reflected an extreme non-participation for both student and instructor, which if left to continue, can result in negative learning and teaching behaviors.
III. RESULTS
A. Class Types, Characteristics, Feedback Scores
A total of 12 sessions were observed, consisting of in-person and online teaching sessions of six topics (Table 1). There were 3 topics of CBL and LLC each. Duration of the class sessions range from 30-55 minutes for the in-person sessions and 40-90 minutes for the online sessions. Total number of PGY-1 students eligible to attend the in-person teaching sessions in 2017 was 82, and 86 for the online teaching sessions in 2020. Student attendance for the in-person sessions ranged from 11 (13.4%) to 31 (37.8%) and that for the online session ranged from 28 (32.6%) to 77 (89.5%). Median (range) of feedback scores for in-person sessions were 4.57 (4.25 to 4.72) vs 4.32 (4.04 to 4.61) for online sessions. Median (range) of self-reported engagement scores for in-person sessions were 4.55 (4.25 to 4.79) vs 4.34 (4.00 to 4.67) for online sessions (Table 1).
Table 1. Class types and characteristics (*Different tutors, but using same content)
B. Instructors’Engagement Behaviour
1) Comparing in-person vs online teaching: Percentage time during which there is no engagement/interaction (or scoring “1” on the IEM score). This ranges from 0-80% for in-person teaching vs 0-100% for online teaching (Table 2A). For each topic, there is no significant difference between percentage time of no engagement.
Most frequent IEM scores. Most frequent IEM scores for each 5-minute segment were 3 for in-person teaching (48.9%) and online teaching (52.9%) (Table 2B).
2) Comparing CBL vs LLC: Percentage time during which there is no engagement/interaction. This ranges from 0-23.1% for CBL vs 50-100% for LLC (Table 2A).
Most frequent IEM scores. Most frequent IEM score was 3 for CBL (77.3%) and 1 for LLC (71.4%). (Table 2B).
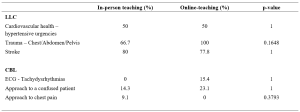
Table 2A. Comparison of instructors’ behaviour showing percentage time with no engagement (scoring “1” on the IEM score)
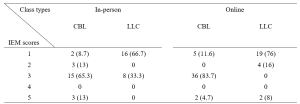
Table 2B. Numbers (percentages) of a particular IEM score received for a 5-minutes segment of teaching – for instructors
C. Students’ Engagement Behaviour
1) Comparing in-person vs online teaching: Percentage time during which there is no engagement/interaction. This ranges from 0-95% for in-person teaching vs 78.8-100% for online teaching (Table 3A). There is significant difference in percentage time of no engagement in two topics (ECG, chest pain), where there is higher percentage of no engagement time with online teaching.
Most frequent IEM scores. Most frequent IEM scores were 1 for both in-person teaching (63.8%) and online teaching (85.1%) (Table 3B).
2) Comparing CBL vs LLC: Percentage time during which there is no engagement/interaction. This ranges from 0-81.9% for CBL vs 84.4-100% for LLC (Table 3A).
Most frequent IEM scores.
Most frequent IEM scores were 1 for both CBL (65.3%) and LLC (91.8%) (Table 3B).
Presence of 1* scores, where “1*” was defined as no response when a question was posed to a specific student called by name. There was no 1* IEM score for in-person teaching for either CBL or LLC, and 8.4% (12/143) of the “1” responses were 1* for online-teaching for CBL and 6.5% (6/92) of the “1” responses were 1* for LLC.
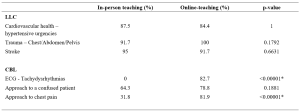
Table 3A. Comparison of students’ behaviour showing percentage time with no engagement (scoring “1” on the IEM score)
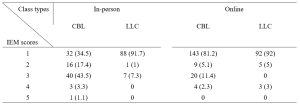
Table 3B. Numbers (percentages) of a particular IEM score received for a 5-minutes segment of teaching – for students
D. Number of Questions Asked Per 5-minute Cycle
Median number of questions asked by instructors ranged from 0-2 for in-person teaching and 1-3 for online teaching (See Appendix 1). These range from 1-3 for CBL vs 0-1 for LLC.
Median number of questions asked by students in all sessions were 0.
The results for this study can be derived from the dataset uploaded onto the online repository accessed via https://doi.org/10.6084/m9.figshare.18133379.v1 (Chua et al., 2022).
IV. DISCUSSION
We modified the known STROBE instrument (O’Malley et al., 2003) to create an observational tool “IEM” which could be used to quantify instructor and student engagement despite the observer not being present in-person. Our IEM scores were derived by taking scores that were in agreement when independently scored by two main observers (YES and KN). The third observer (CYC) was used as the validator of the scores by the two main observers. When there was a discrepancy in the scores awarded by the two observers, the score which was in agreement with the score awarded by CYC was used. To give an indication of the IEM tool’s effectiveness where the observer is not present in-person, we postulated that our modified IEM score should still demonstrate the well-documented difference in engagement between lecture-style learning and case-based learning sessions (Kelly et al., 2005). Our modified IEM score did indeed show more frequent higher scores as expected for case-based learning sessions (Tables 2B and 3B). We also compared our IEM scores with the students’ self-reported engagement scores (Table 1) that had been collected as part of student feedback. The general correlation in the trend of observed IEM scores with that of the students’ self-reported engagement scores also suggest the usefulness of our modified STROBE tool in situations where the observer is not present in-person, although this needs to be further validated in prospective studies.
Our initial study hypothesis was that students may find themselves more engaged in online teaching sessions and open to posing questions to the instructor and their peers, due to the presence of the “chat”, “likes” and “poll” functions available on the Zoom tele-conferencing platform, which may be more familiar to a younger generation accustomed to using social media. We had postulated that live online lectures would encourage further engagement from students who would not otherwise participate in-person, due to the less intimidating online environment where they can ask and answer questions more anonymously (Kay & Pasarica, 2019; Ni, 2013). In an Asian-pacific context, video conferencing had been found to be able to improve access for participation for more reticent participants who prefer written expression, through alternative communication channels like the ‘chat box’, although there was a potential trend to reduced engagement. (Ong et al., 2021).
Our data, shows, that Zoom teleconferencing during the COVID-19 pandemic can be associated with reduced student engagement. The percentage time where there was no engagement was significantly higher with online sessions (Table 3A) and the most frequent IEM score was lower (1 for online vs 3 for in-person), for CBL sessions (Table 3B). This phenomenon in medical education during the COVID-19 pandemic has previously been described. Using student and instructor feedback, students were more likely to have reduced engagement during virtual learning (Longhurst et al., 2020; Dost et al., 2020), and would have increased difficulties maintain focus, concentration and motivation during online learning (Wilcha, 2020).
Our data also suggests that for the instructor to even try to achieve close to the same levels of engagement as before, a longer duration of time was spent by each instructor per topic when executing CBL (Table 1). This may include time where the instructor needs multiple attempts at questioning and discussion before there is a student response. It is also possible that for in-person learning, the instructor relies greatly also on non-verbal cues (e.g., body language, nods of the head, collective feel of the room) to determine if a question has been satisfactorily answered, and therefore can move on quicker than when on a Zoom platform where one cannot see most, or even every student.
The higher number of attendees for online learning compared to in-person attendance (see Table 1) highlights one of the strengths of online learning, which is where online learning is more easily accessible for students who would save on time getting to a designated lecture room and provides flexibility for students to enter and exit (Dost et al., 2020). Unfortunately, this also likely encourages the phenomenon of “presenteeism”, where students are not focused on the learning session, but instead engage in other tasks simultaneously, e.g., reading or composing emails, or completing work tasks instead of having dedicated protected teaching time. Resident learners have been described to participate in nearly twice as many non-teaching session related activities per hour during an online session than when in-person (Weber & Ahn, 2020). This has likely contributed to the number of 1* scores we had, where the student has logged into the Zoom platform, but is not available to even respond in the negative when called upon to answer a question. This presenteeism, however, is not just a problem for online learning, but even for in-person learning, where pretending to engage has been found to be a significant unrecognized issue (Fuller et al., 2018).
The main implication that our study highlights that to improve student engagement when using online learning, a face-to-face platform cannot simply be transposed into a virtual platform. It had been suggested that engagement during live virtual learning could be enhanced with the use of interactive quizzes with audience polling functions (Morawo et al., 2020) and possibly other methods such as “gamification” (Nieto-Escamez & Roldan-Tapia, 2021). Our instructors for the CBL sessions had used both poll functions and live questioning for their sessions, but without increased success in engagement. Smaller groups are likely required to enhance student engagement, but this would lead to the need for increased time and teaching manpower. Increasing the opportunity for interaction via a virtual platform would also require the need to create additional online resources, which would take up more faculty time where creating new resources can take at least three times as much work compared to a traditional format (Gewin, 2020). Online resources would need to be modified in such a way that increases student autonomy to increase student engagement in medical education (Kay & Pasarica, 2019). Our study also shows that as a first step, in time and resource-limited settings, a case-based approach to teaching would be more ideal to enhance student engagement than lecture style teaching.
A culture of accountability also needs to be fostered within the online teaching sessions, where students need to be educated on how Zoom meetings can be more enriching when cameras are on (Sharp et al., 2021). PGY-1 interns, as recent graduates, also need to be educated on the aspect of professionalism when entering the medical work force, where they can be called upon to answer questions during meetings or conferences. When initial questions are not voluntarily answered, our tutors often practice “cold-calling”, which can help keep learners alert and ready (Lemov, 2015). Unfortunately, these evidence-based teaching methods that work well when the student is in-person, ultimately will fail if online students are not educated on their need to be accountable to the instructor or their peers.
This study has several limitations. Firstly, the level of student engagement may also be affected by external factors, such as a different physical learning environment, class size and avenues of communication. The stresses of the on-going pandemic may also have affected student engagement, as a decrease in quality of life and stress would negatively impact student motivation (Lyndon et al., 2017). Secondly, the topics for lecture to large class and case-based learning were not identical as these topics were picked in chronological order and there were no topics in the curriculum that had material for both the lecture and case-based learning class types. This difference in topics may have potentially contributed to confounding when we try to make direct comparisons between the two class types, although, we have attempted to mitigate this by including a variety of topics in each class type. Thirdly, the improved student engagement and feedback scores for in-person learning may also have had some bias given the smaller student size for in-person learning. It is also possible that only the more motivated, and hence more likely to be engaged students, would turn up for in-person learning. Fourthly, due to the online nature as well as the retrospective viewing of the video recordings, the observers were not present in-person to observe the non-verbal cues of the students or instructors. The tool, however, was modified to take into account only the verbal output that could be observed online or via video recording. Lastly, our IEM tool will benefit from more studies and research to further confirm its validity in observing students when the observer is not present in-person.
V. CONCLUSION
Lectures are associated with reduced student engagement than case-based learning, while both class types are associated with lower levels of student engagement when conducted on a virtual platform. Instructor levels of engagement, however, remain about the same. This highlights that a face-to-face platform cannot simply be transposed into a virtual platform, and it is important to address this gap in engagement as this can lower faculty satisfaction with teaching and ultimately result in burnout. Blended teaching or smaller group teaching as the world turns the corner in the COVID-19 pandemic may be one way to circumvent the situation but is also constrained by faculty time and manpower. Our study also shows that as a first step, in time and resource-limited settings, a case-based approach to teaching would be more ideal to enhance student engagement than lecture style teaching.
Notes on Contributors
Dr Ng Wei Ping Kay and Dr Chua Yuan Kit Christopher are co-first authors and contributed to conceptual development, acquisition, analysis, and interpretation of data for the work. They contributed to drafting and revising the work and approved the final version to be published. They agree to be accountable for all aspects of the work.
Dr Lye Pei Shi Priscillia contributed to conceptual development, acquisition, analysis, and interpretation of data for the work. She contributed to drafting and revising the work and approved the final version to be published. She agrees to be accountable for all aspects of the work.
Dr Joy Vijayan contributed to conceptual development, acquisition, analysis, and interpretation of data for the work. He contributed to drafting and revising the work and approved the final version to be published. He agrees to be accountable for all aspects of the work.
Dr Yap Eng Soo contributed to conceptual development, acquisition, analysis, and interpretation of data for the work. He contributed to drafting and revising the work and approved the final version to be published. He agrees to be accountable for all aspects of the work.
Dr Chan Yee Cheun contributed to conceptual development, acquisition, analysis, and interpretation of data for the work. He contributed to drafting and revising the work and approved the final version to be published. He agrees to be accountable for all aspects of the work.
Ethical Approval
I confirm that the study has been approved by Domain Specific Review Board (DSRB), National Healthcare Group, Singapore, an institutional ethics committee. DSRB reference number: 2020/00415.
Data Availability
The data that support the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.fig share.18133379.v1.
Acknowledgement
We would like to acknowledge Ms. Jacqueline Lam for her administrative support in observing the recordings and online-teaching.
Funding
There was no funding for this research study.
Declaration of Interest
The authors report no conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Alimoglu, M. K., Sarac, D. B., Alparslan, D., Karakas, A. A., & Altintas. (2014). An observation tool for instructor and student behaviors to measure in-class learner engagement: A validation study. Medical Education Online, 19(1), 24037. https://doi.org/10.3402/meo.v19.24037
Armstrong, S. J., & Fukami, C. V. (2009). The SAGE Handbook of Management Learning, Education and Development. SAGE Publications Ltd. https://www.doi.org/10.4135/9780857021038
Berman, N. B., & Artino, A. R. J., (2018). Development and initial validation of an online engagement metric using virtual patients. BMC Medical Education, 18(1), 213. https://doi.org/10.1186/s12909-018-1322-z
Chick, R. C., Clifton, G. T., Peace, K. M., Propper, B. W., Hale, D. F., Alseidi, A. A., & Vreeland, T. J. (2020). Using technology to maintain the education of residents during the COVID-19 Pandemic. Journal of Surgical Education, 77(4), 729–732. https://doi.org/10.1016/j.jsurg.2020.03.018
Chua, Y. K. C., Ng, K. W. P., Yap, E. S., Lye, P. S. P., Vijayan, J., & Chan, Y. C. (2022). Evaluating online learning engagement (Version 1) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.18133379.v1
Dost, S., Hossain, A., Shehab, M., Abdelwahed, A., & Al-Nusair, L. (2020). Perceptions of medical students towards online teaching during the COVID-19 pandemic: A national cross-sectional survey of 2721 UK medical students. BMJ Open, 10(11), e42378. https://doi.org/10.1136/bmjopen-2020-042378
Fuller, K. A., Karunaratne, N. S., Naidu, S., Exintaris, B., Short, J. L., Wolcott, M. D., Singleton, S., & White, P. J. (2018). Development of a self-report instrument for measuring in-class student engagement reveals that pretending to engage is a significant unrecognized problem. PLOS ONE, 13(10), e0205828. https://doi.org/10.1371/journal.pone.0205828
Gewin, V. (2020). Five tips for moving teaching online as COVID-19 takes hold. Nature, 580(7802), 295–296. https://doi.org/10.1038/d41586-020-00896-7
Kaufman, D. M. (2003). Applying educational theory in practice. BMJ, 326(7382), 213–216. https://doi.org/10.1136/bmj.326.7382.213
Kay, D., & Pasarica, M. (2019). Using technology to increase student (and faculty satisfaction with) engagement in medical education. Advances in Physiology Education, 43(3), 408–413. https://doi.org/10.1152/advan.00033.2019
Kelly, P. A., Haidet, P., Schneider, V., Searle, N., Seidel, C. L., & Richards, B. F. (2005). A comparison of in-class learner engagement across lecture, problem-based learning, and team learning using the STROBE classroom observation tool. Teaching and Learning in Medicine, 17(2), 112–118. https://doi.org/10.1207/s15328015tlm1702_4
Lemov, D. (2015). Teach like a champion 2.0: 62 techniques that put students on the path to college. (2nd ed.). Jossey-Bass.
Longhurst, G. J., Stone, D. M., Dulohery, K., Scully, D., Campbell, T., & Smith, C. F. (2020). Strength, weakness, opportunity, threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the Covid-19 pandemic. Anatomical Sciences Education, 13(3), 301–311. https://doi.org/10.1002/ase.1967
Lyndon, M. P., Henning, M. A., Alyami, H., Krishna, S., Zeng, I., Yu, T.-C., & Hill, A. G. (2017). Burnout, quality of life, motivation, and academic achievement among medical students: A person-oriented approach. Perspectives on Medical Education, 6(2), 108–114. https://doi.org/10.1007/s40037-017-0340-6
McCoy, L., Pettit, R. K., Lewis, J. H., Allgood, J. A., Bay, C., & Schwartz, F. N. (2016). Evaluating medical student engagement during virtual patient simulations: A sequential, mixed methods study. BMC Medical Education, 16, 20. https://doi.org/10.1186/s12909-016-0530-7
Morawo, A., Sun, C., & Lowden, M. (2020). Enhancing engagement during live virtual learning using interactive quizzes. Medical Education, 54(12), 1188. https://doi.org/10.1111/medu.14253
Ni, A. Y. (2013). Comparing the effectiveness of classroom and online learning: Teaching research methods. Journal of Public Affairs Education, 19(2), 199-215. https://doi.org/10.1080/15236803.2013.12001730
Nieto-Escamez, F. A., & Roldan-Tapia, M. D. (2021). Gamifica- tion as online teaching strategy during COVID-19: A mini-review. Frontiers in Psychology, 12, 648522. https://doi.org/10.3389/fpsyg.2021.648552
O’Malley, K. J., Moran, B. J., Haidet, P., Seidel, C. L., Schneider, V., Morgan, R. O., Kelly, P. A., & Richards, B. (2003). Validation of an observation instrument for measuring student engagement in health professions settings. Evaluation & the Health Professions, 26(1), 86–103. https://doi.org/10.1177/0163278702250093
Ong, C. C. P., Choo, C. S. C., Tan, N. C. K., & Ong, L. Y. (2021). Unanticipated learning effects in videoconference continuous professional development. The Asia Pacific Scholar, 6(4), 135-141. https://doi.org/10.29060/TAPS.2021-6-4/SC2484
Rao, S. P., & DiCarlo, S. E. (2001). Active learning of respiratory physiology improves performance on respiratory physiology examinations. Advances in Physiology Education, 25(2), 55–61. https://doi.org/10.1152/advances.2001.25.2.55
Sharp, E. A., Norman, M. K., Spagnoletti, C. L., & Miller, B. G. (2021). Optimizing synchronous online teaching sessions: A guide to the “new normal” in medical education. Academic Pediatrics, 21(1), 11–15. https://doi.org/10.1016/j.acap.2020.11.009
Watson, W. E., Michaelsen, L. K., & Sharp, W. (1991). Member competence, group interaction, and group decision making: A longitudinal study. Journal of Applied Psychology, 76(6), 803–809. https://doi.org/10.1037/0021-9010.76.6.803
Weber, W., & Ahn, J. (2020). COVID-19 conferences: Resident perceptions of online synchronous learning environments. Western Journal of Emergency Medicine, 22(1), 115–118. https://doi.org/10.5811/westjem.2020.11.49125
Wilcha, R. J. (2020). Effectiveness of virtual medical teaching during the COVID-19 crisis: Systematic review. JMIR Medical Education, 6(2), e20963. https://doi.org/10.2196/20963
*Chua Yuan Kit Christopher
5 Lower Kent Ridge Road,
National University Hospital,
Singapore 119074
+65 7795555
Email: christopher_chua@nuhs.edu.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









