Combination of Teddy Bear Hospital and Virtual Reality Training increases empathy of medical students
Submitted: 5 January 2022
Accepted: 24 February 2022
Published online: 5 July, TAPS 2022, 7(3), 33-41
https://doi.org/10.29060/TAPS.2022-7-3/OA2739
Javier Zheng Huan Thng1, Fion Yun Yee Tan1, Marion Margaret Hui Yong Aw1,2 & Shijia Hu3
1Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Paediatrics, Khoo Teck Puat-National University Children’s Medical Institute, National University Health System, Singapore; 3Faculty of Dentistry, National University of Singapore, Singapore
Abstract
Introduction: In paediatric practice, healthcare professionals are required to connect with the child and interact at his/her level. However, it can be very difficult for medical students to put themselves in the shoes of the young child, to empathize and understand how a child actually feels while being treated. The Teddy Bear Hospital (TBH) can serve as a platform for medical students to learn how to communicate and empathise with children. Additionally, virtual reality (VR) can be used to portray a child’s viewpoint. This study aims to assess how TBH and VR can improve learning outcomes for medical students.
Methods: A cohort study was conducted on 20 first-year medical students taking part in TBH sessions. The medical students did a Pre-, Post- and 1-year Post-intervention Jefferson Scale of Empathy to assess their empathy levels. They also completed a 1-year Post-intervention quantitative and qualitative survey on their experience.
Results: There was a significant increase in Jefferson score compared to Pre-intervention (116.95 ± 8.19) for both Post-intervention (121.65 ± 11.03) and 1-year Post-intervention (123.31 ± 8.86). More than 80% believed that participating in TBH improved their confidence and ability to interact with children, while 50% felt that VR scenarios helped prepare them for the TBH. Thematic analysis of qualitative responses described (1) Personal development, (2) Insights into interacting with children, and (3) Structure and curriculum.
Conclusion: TBH improved empathy and communication with children among pre-clinical medical students and the use of VR can be used to augment sessions.
Keywords: Education, Medical Student, Simulation Training, Teddy Bear Hospital, Virtual Reality
- The Teddy Bear Hospital sessions, consisting of physical simulation of medical scenarios with children, increased empathy of medical students.
- The use of virtual reality scenarios to portray the viewpoint of a child can augment the teaching of the Teddy Bear Hospital.
- The Teddy Bear Hospital and virtual reality sessions improved the comfort, increased confidence, and self-perceived ability of interacting with children in medical students.
I. INTRODUCTION
In paediatric practice, healthcare professionals are required to connect with the child and interact at his/her level. This is especially important, when the child is encountering new and unfamiliar situations or when they are unwell and face potentially challenging and painful procedures (Mead & Bower, 2002). However, it can be very difficult for new practitioners to put themselves in the shoes of the young child, to empathise and understand how a child actually feels while being treated (Dwamena et al., 2012). This is particularly true for medical students, who not only have to grapple with the unfamiliar medical aspects of pediatric disease, but may also need to manage a frightened and uncooperative child at the same time (MacDonald-Wicks & Levett-Jones, 2012). Furthermore, having limited interaction with children means that most medical students have a difficult time empathising with them.
Empathy is an important element in a physician-patient relationship, as it has shown to improve communication and therapeutic goals (Mercer & Reynolds, 2002). However, several studies have shown significant decrease in empathy over the course of medical school (Neumann et al., 2011). Although there have been numerous methods and approaches developed to enhance empathy in medical students (Batt-Rawden et al., 2013), including interventions based around the patient narrative (e.g. creative writing, blogging, drama, poetry, fiction, and film), problem-based learning, interpersonal skills training, patient interviews, and experiential learning (simulation of patient experience). Among these interventions, experiential (immersive) learning experiences have shown promising results (Halton & Cartwright, 2018). These scenarios can be conducted either physically or virtually. It can involve the learner completing a simulated task or experience a scenario from the point of view of someone else so as to put themselves in someone else’s shoes.
The advent and advancement of virtual reality (VR) media provide the opportunity for the portrayal of different viewpoints (Lok et al., 2006). A recent study found that empathy in medical students was improved with VR portraying the viewpoint of an older patient with conditions such as macular degeneration and hearing loss (Dyer et al., 2018). However, there has not been any research done on the use of VR to simulate the point of view of a child in a medical setting. The power of immersive media can be harnessed to simulate interactions between a child and healthcare professionals, exhibiting both positive and negative examples. More importantly, it can be used to introduce an inexperienced practitioner to the viewpoint of a child patient. This will help foster empathy and drive home the effectiveness of behaviour management skills (Stewart et al., 2013).
The Teddy Bear Hospital (TBH) is an international initiative, carried out by students from Medical Faculties, aimed at reducing children’s anxiety around medical environments, procedures and professionals (Bloch & Toker, 2008; Santen & Feldman, 1994; Siegel et al., 2018). TBH simulates the different medical environments and clinical situations which children may encounter in a friendly manner using they own toys (such as teddy bears). This simulation takes the form of multi-station role-plays, which could include a check-up by the doctor, watching a doctor applying a cast for a limb fracture or performing a procedure (e.g., taking a blood sample), or receiving an injection (all performed on teddy bears, who are the patients). In addition to reducing anxiety in young children, the TBH has also been used to teach medical students communication with children in a medical setting (Nheu et al., 2018; Ong et al., 2018). Although the qualitative feedback from medical students have been generally positive (Nheu et al., 2018; Ong et al., 2018), there have not been objective measures of the effect of the TBH on the empathy of medical students.
Both VR and TBH are immersive interventions that can potentially increase the empathy of medical student, they can also improve the learning experience by allowing students to experience effective techniques to interact with children and practice those techniques. However, each intervention has inherent disadvantages. VR usually follows a scripted scenario that does not allow students to practice and interact in real-time. While TBH is time and resource intensive, and cannot be conducted is situations such as a pandemic. Therefore, evaluating the effects of a combination of the 2 techniques can inform on the individual effectiveness as well as in combination.
This study aims to determine the effect of virtual and physical simulation on the empathy and learning experience of medical students. This will be done through a combination of VR instruction and practical simulation in a TBH experience, in which medical students are exposed to and educated on the positive interactions with a child patient in various medical scenarios.
II. METHODS
This is a cohort study of first year medical students who took part in TBH sessions in January 2020 and were followed up in January 2021. Subjects were recruited from volunteers who signed up to participate in TBH sessions. Subjects were reassured that their responses are strictly confidential and will have no impact on their grades or teaching received. Medical students who have participated in previous TBH sessions were excluded. Written informed consent was taken prior to participation. This study was approved by the Institutional Review Board (NUS-IRB Reference Number: S-19-151) and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
As this was a pilot study, no sample size calculation was conducted prior to study initiation.
A. Survey Content and Timing
The Jefferson Scale of Empathy (Sidney Kimmel Medical College, Thomas Jefferson University, PA, USA) was used to assess the level of empathy (Hojat et al., 2018). It is a 20-item scale that was developed specifically to measure empathy in health professions education, including medical students. The S-version of the survey, for medical students, was administered in this study. The survey forms were purchased from Thomas Jefferson University, Center for Research in Medical Education and Health Care. The Jefferson scores were calculated out of a maximum of 140. The survey was conducted in its original English version as the language medium for education in Singapore is English and all participants are proficient.
1) Pre-intervention: Prior to the TBH session, the subjects completed the Jefferson Scale of Empathy to assess baseline empathy scores. The subjects then underwent a small group teaching session of one hour including viewing of two VR scenarios, conducted by the same instructors (JT & FT). The small group teaching sessions covered topics pertaining to doctor-patient relationship, and the developmental and psycho-affective challenges of interacting with children. The two VR scenarios depicted a child’s point of view in the setting of getting an injection (mooc vid, Scenario 1, 2019) and visiting the dentist (mooc vid, Scenario 2, 2019). The scenarios are interactive and the point of view can be manipulated by the viewer. After watching the VR scenarios, discussions where subjects can critique the healthcare providers’ actions and share their learning points were carried out. During this session, the subjects were also briefed about the different scenarios in the TBH session, including the content to be covered.
2) TBH session: The TBH session consisted of 5 scenarios namely: (1) Orthopedic Specialist: Meet Mr. Bones, (2) Respiratory Therapist: Help Teddy Breathe, (3) Family Medicine: Help Teddy Stay Healthy, (4) Personal Hygiene: Help Teddy Stay Clean, (5) Operating Theatre: Teddy has a Painful Tummy. The injection process and dental procedures were incorporated into scenarios 3 and 4 respectively. The medical students were divided into teams of 2 to 3, each interacting with a group of 5 to 8 children of the same age. Each team rotated through the different scenarios for 10 minutes. At each scenario, the medical students explained the task to the children and conducted hands-on simulation.
3) Post-intervention: After their first TBH session, the subjects completed a second Jefferson Scale of Empathy.
4) 1-year Post-intervention: One year after the TBH session, students completed a third Jefferson Scale of Empathy, along with a self-administered survey regarding the long-term impact of TBH sessions and the effectiveness of the VR scenarios.
To assess the long-term impact of TBH sessions and the effectiveness of the VR scenarios, a 1-year Post-intervention survey was administered in December 2020. The survey was adapted from a previous study (Ong et al., 2018) and piloted for understanding and readability.
The 1-year Post-intervention impact of TBH sessions was assessed using five questions on a 5-point Likert scale (strongly disagree, disagree, neutral, agree, strongly agree) regarding the effect of TBH sessions on improving the medical student’s ability, confidence and comfort level in communicating with children, and ability to empathize with children’s fear in the healthcare environment. Similarly, the effectiveness of the VR scenarios was assessed using three questions on a 5-point Likert scale, regarding the effect of the VR scenarios on preparation for TBH session, as well as improving the comfort level and confidence in engaging children. The remaining two questions obtained qualitative feedback regarding any difficulties faced as well as takeaways obtained during the TBH session.
B. Data Collection
The subjects completed the TBH sessions in small groups of up to eight volunteers, with up to 30 children, aged between 4 to 8 years old, in each session. It was explained to the children that they were participating in an activity to teach them about what happens during visits to a doctor. These sessions were conducted at the participating pre-schools with medical instruments and teddy bears as simulated patients.
Due to the COVID-19 pandemic situation and restrictions, the survey was collected via an online survey, instead of a planned Focused Group Discussion.
C. Data Analysis
Normality of data was checked using the Shapiro-Wilk test, data analysis of the Jefferson Scale of Empathy score was done via Paired samples correlation, Cohen’s d score and Paired Samples T test using Statistical Package for Social Sciences (SPSS) software (IBM SPSS Statistics 26, Armonk, NY, USA). Descriptive statistics were presented for the survey on learner experience.
Qualitative analysis was done on the medical students’ open-ended responses regarding the long-term impact of TBH sessions and the effectiveness of the VR scenarios. Using thematic content analysis and a qualitative descriptive framework (Creswell & Poth, 2019), emerging themes and illustrative quotes for each theme were extracted. The codes and themes were first done independently by two of the authors (JT & FT), any discrepancies were discussed and reconciled. After which, 2 other authors (SH & MA) reviewed and verified the finalised codes and themes, which were mapped for interpretation. Descriptive summaries and illustrative quotes were used to describe each theme.
III. RESULTS
A. Study Demographics
In total, 20 first time participants were recruited and consent was taken. All 20 were first year medical students; 9 males and 11 females. All participants (n=20) completed the Pre-intervention and Post-intervention survey while 16 completed the 1-year Post-intervention survey, with 4 participants declining to participate in the follow-up. The data that support the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.figshare.17973662 (Hu, 2022).
B. Jefferson Scale of Empathy
There was a significant (p=0.026) increase in the Jefferson score between the Pre-intervention (116.95 ± 8.19) and Post-intervention (121.65 ± 11.03). Similarly, there was a significant (p=0.002) increase from the Pre-intervention to 1-year Post-intervention (123.31 ± 8.86). (Figure 1) However, there was no difference between the Post-intervention and 1-year Post-intervention scores.
Cohen’s d score was used to determine the effect size of the intervention on the mean difference between the Pre- and Post-intervention score (0.48), and the Pre- and 1-year Post-intervention score (0.72). This corresponds to a medium effect of the intervention on the mean differences.
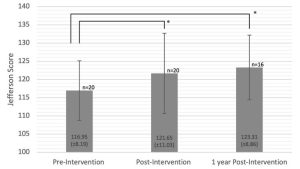
Figure 1. Jefferson Scale of Empathy Score before, immediately after and 1 year after TBH. Error bars represent the standard deviation. Asterisk (*) indicate significant differences between the groups, p<0.05.
C. Quantitative Survey
Quantitative responses from the survey on learner experience were categorised into positive responses (agree, strongly agree) and negative/neutral responses (neutral, disagree, strongly disagree). The total number of responses collected was 16 at 1-year Post-intervention (Table 1).
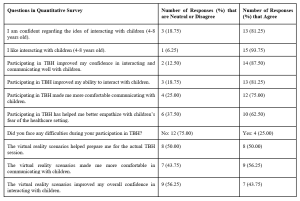
Table 1. Subject’s perception towards their TBH experience
The subjects were generally confident (75%) and enjoyed interacting with young children (94%). More than 80% believed that participating in TBH improved their confidence and ability to interact with children, and 75% felt that participating in TBH made them more comfortable communicating with children. 63% felt that TBH helped improve their ability to empathize with children’s fears of the healthcare setting. Overall, 75% of subjects did not face difficulties during the TBH sessions. In terms of the VR scenarios, around 50% felt that it was effective in preparing for the actual TBH session, with 56% feeling more comfortable and 44% feeling more confident interacting with children.
D. Qualitative Survey
Three major themes were generated from the analysis of the open-ended responses from 16 of the 20 subjects: (1) Personal development, (2) Insights into interacting with children and (3) Structure and curriculum of TBH. These themes were further categorised into sub-themes as shown in Table 2.
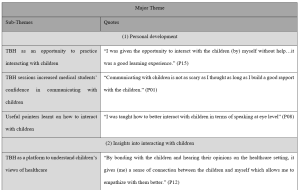
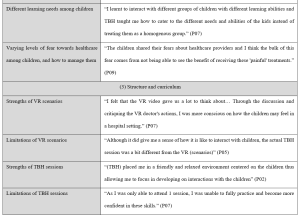
Table 2. Major themes, sub-themes and transcript highlights of qualitative survey
1) Personal development
TBH provided an opportunity for medical students in this study to interact with children in a safe and stress-free environment. These students would otherwise have limited experience communicating with children in that age-group, until actual clinical interactions with sick children.
“I was given the opportunity to interact with the children (by) myself without help…it was a good learning experience.” (P15)
The experience gave these medical students more confidence and reduced their anxiety about interacting with children, as they realized that it was not as difficult as they thought to communicate with children.
“Communicating with children is not as scary as I thought as long as I build a good rapport with the children.” (P01)
Medical students also learnt useful pointers on how to interact and communicate with children, which alleviated their worries and improved their confidence. These pointers include using simpler words, hand actions, speaking at eye level and being more expressive.
“(TBH) allowed me to practice how I interact with children (by) using easier words (and) hand actions” (P01)
“I was taught how to better interact with children in terms of speaking at eye level” (P08)
2) Insights into interacting with children
TBH was a unique platform to understand children’s learning needs and empathize with their views towards healthcare. This was achieved via interactions with the children.
“By bonding with the children and hearing their opinions on the healthcare setting, it gives (me) a sense of connection between the children and myself which allows me to empathize with them better.” (P12)
These interactions allowed medical students to learn how to adapt their teaching styles to suit the different needs of each individual child.
“I learnt to interact with different groups of children with different learning abilities and TBH taught me how to cater to the different needs and abilities of the kids instead of treating them as a homogenous group.” (P07)
These interactions also taught medical students that the children have different levels of fear towards healthcare. While some children were apprehensive, others were unafraid of the TBH sessions.
“The children shared their fears about healthcare providers and I think the bulk of this fear comes from not being able to see the benefit of receiving these ‘painful’ treatments.” (P09)
“The children seemed to be really excited during the TBH sessions, I don’t recall that the children expressed any fear about their experiences” (P16)
In addition to understanding the children’s fears towards healthcare, medical students learnt how to manage these fears by acknowledging them and putting themselves in the children’s shoes.
“We should never downscale a child’s fear towards healthcare. There is a need to try to understand where they are coming from, (and) to comfort and encourage them to the best of our ability.” (P13)
3) Structure and curriculum
To understand the impact of the newly added VR scenarios, feedback regarding its strengths and limitations were collated. One strength is that the students experienced various case studies through the VR scenarios. This allowed them to be better prepared for the TBH sessions and become more aware of the children’s emotions during their interaction.
“I felt that the VR video gave us a lot to think about… Through the discussion and critiquing the VR doctor’s actions, I was more conscious on how the children may feel in a hospital setting.” (P07)
Another strength is that during the training, medical students were also asked how they would respond to the hypothetical scenarios. By putting them in the hot seat, they were able to exchange ideas and learn from one another.
“The volunteer trainers asked us questions during the volunteer training, when I answered correctly it gave me more confidence and when I listen to other people’s answers, I feel more equipped to handle different situations too” (P15)
The VR scenarios were limited in terms of application to the actual TBH sessions. The scenarios only showed how to engage an individual child, which was different from actual TBH sessions, in which medical students had to teach a group of children.
“Although it did give me a sense of how it is like to interact with children, the actual TBH session was a bit different from the VR (scenarios)” (P05)
Feedback was also collated regarding the strengths and limitations of the TBH sessions.
One strength was the established curriculum so participants did not have to worry about the content but can instead focus on honing their communication skills. The fact that this was a student-run program, and that medical students had their peers as fellow participants, put them at ease and made it a more conducive environment.
“(TBH) placed me in a friendly and relaxed environment centred on the children thus allowing me to focus in developing on interactions with the children” (P02)
A limitation of the TBH sessions was that it was challenging for participants to balance teaching the children and empathising with them.
“I think it’s … difficult to see from the children’s perspective during the session… We are usually more focused on imparting rather than listening because of the inability to elicit responses from all of them.” (P13)
Another limitation of the TBH sessions was that participants are usually able to attend only one session. This may have held them back from being fully adept in their interactions with children.
“As I was only able to attend 1 session, I was unable to fully practice and become more confident in these skills.” (P07)
Finally, there were disagreements about whether the ratio of medical students to children was suitable. While some felt that it was appropriate, others had trouble managing the children.
“The ratio (of) facilitators to children were just nice (and) not overwhelming for either parties” (P15)
“It was just too chaotic and hard to manage so many of them especially since they’re so bubbly and curious” (P16)
IV. DISCUSSION
This was the first study to examine objectively and subjectively, the effect of TBH and VR training on the empathy levels of medical students. There was a statistically significant improvement in the medical student’s level of empathy immediately after the TBH session, which persisted 1 year after the TBH session. The outcomes of this study revealed that the medical students who participated in TBH augmented by VR training assisted them to better empathize with the children they worked with.
Compared with the previous work by Ong et al in the same institution, involving only traditional lecture preparation for TBH (Ong et al., 2018), it appears that the addition of VR training showed an increase in medical students’ perceived improvement in both interacting and teaching children. In that study conducted without the use of VR scenarios, 53% reported improvement in interacting with children and 39% reported improvement in teaching children, compared to the present study of 88% and 75% respectively. Moreover, VR training alone achieved improvements of 44% and 50% which is similar to TBH session alone. A recent study found that VR simulation alone improved the empathy of dental students when managing children (Hu & Lai, 2022), this is encouraging since the VR intervention was not as time and resource intensive as the TBH. Although the cohorts of medical students were different, each cohort is from the same year of training (i.e., first year medical students) and the TBH teaching was done with a standardised protocol and thus relatively similar across the cohorts. It appears that a combination of the 2 methods of training provided a greater magnitude to the student’s perceived improvement in interacting and teaching children. This suggests that although the VR training cannot replace the real TBH interaction with children, it can be used to augment the learning experience of students in communicating with children. Moreover, it can be deployed on a much larger scale to the entire cohort, instead of smaller groups like the labour intensive TBH teaching.
According to the qualitative analysis, the TBH is a good platform for medical students to practice and develop their communication skills with children. Through TBH, they pick up techniques on how to better communicate with children both from the trainers and their peers. Similar to previous studies, TBH has also been described to be a useful avenue to gain insights into children’s perspectives of the healthcare setting and therefore trains them to be better attuned to the needs and feelings of children (Nheu et al., 2018; Ong et al., 2018). Nonetheless, the medical students suggested some areas of improvements. For example, it was pointed out that the VR scenarios did not depict the actual TBH session, as such, it did not help in teaching children during TBH. However, the goal of the TBH session is to increase medical student’s empathy through teaching rather than training them to be educators. Therefore, the VR scenarios can still bring the desired benefits in terms of the medical student’s ability to empathize and communicate with children. Additionally, some felt that they are unable to fulfil both a teaching and learning role simultaneously and were overwhelmed. This may hinder them from achieving the desired outcome of increasing their empathy. A potential solution would be to expand the existing course material to further help those who struggle with engaging the children or having fewer children paired to each medical student teacher.
There were some limitations to this study. As there was no control group to compare against, it was difficult to determine if the improvements seen from Pre-intervention to Post-intervention were due to the VR training and participation in the TBH session alone. Future studies could consider including a control group in addition to the intervention group. The observed maintenance of the level of empathy from Post-intervention to 1-year Post-intervention could have been confounded by factors such as varying levels of clinical exposure. Additionally, the quantitative survey on learner experience was done 1 year after the TBH session and may be at risk for recall bias, future studies should consider collecting data at multiple time points to evaluate any difference between immediate and long-term effects of the interventions. However, all respondents provided feedback that were very detailed and informative, suggesting that they were able to recall the experience well. Moreover, due to the COVID-19 pandemic situation and restrictions, the survey was collected via an online survey, instead of the planned Focused Group Discussion, resulting in the inability to ask follow-up or clarifying questions. Lastly, the study was conducted on a small group of volunteers who may have biases due to interest in the discipline. However, a significant improvement was still noted in this small pilot study. Expansion of the program into the general curriculum to include a more diverse group of students will be needed to ascertain the effect of TBH on medical students in general.
V. CONCLUSION
In conclusion, the TBH experience for medical students was effective in increasing their levels of empathy and confidence in interacting and teaching children as it provides an opportunity for medical students to interact with children and understand their views of healthcare. The use of VR can augment the TBH experience or be used in situations where the student is unable to attend TBH sessions in person.
Notes on Contributors
JT and FT are considered co-first authors. JT participated in data collection, conducted the data analysis and interpretation, led the writing, and revised the manuscript for important intellectual content. FT participated in data collection, conducted the data analysis and interpretation, led the writing, and revised the manuscript for important intellectual content. MA conceived the idea and revised the manuscript for important intellectual content. SH conceived the idea, conducted the data analysis and interpretation, led the writing, and revised the manuscript for important intellectual content.
Ethical Approval
This study was approved by the Institutional Review Board (NUS-IRB Reference Number: S-19-151) and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Data Availability
The data that support the findings of this study are openly available in Figshare repository, https://doi.org/10.6084/m9.figshare.17973662.
Acknowledgement
The authors would like to thank Dr Lee Shuh Shing and Ms Lim Yih Lin for their help with the statistical analysis and Manzalab for the help in creating the virtual reality scenarios.
Funding
This work was supported by the USPC-NUS Joint Innovative Projects in Higher Education grant (USPC-NUS 2018 SoM).
Declaration of Interest
The authors declare that they have no competing interests.
References
Batt-Rawden, S. A., Chisolm, M. S., Anton, B., & Flickinger, T. E. (2013). Teaching empathy to medical students: An updated, systematic review. Academic Medicine, 88(8), 1171-1177. https://doi.org/10.1097/ACM.0b013e318299f3e3
Bloch, Y. H., & Toker, A. (2008). Doctor, is my teddy bear okay? The “Teddy Bear Hospital” as a method to reduce children’s fear of hospitalization. Israel Medical Association Journal, 10(8-9), 597-599.
Creswell, J. W., & Poth, C. N. (2019). Qualitative inquiry & research design: Choosing among five approaches. SAGE.
Dwamena, F., Holmes‐Rovner, M., Gaulden, C. M., Jorgenson, S., Sadigh, G., Sikorskii, A., Lewin, S., Smith, R. C., Coffey, J., & Olomu, A. (2012). Interventions for providers to promote a patient‐centred approach in clinical consultations. Cochrane Database of Systematic Reviews, (12).
Dyer, E., Swartzlander, B. J., & Gugliucci, M. R. (2018). Using virtual reality in medical education to teach empathy. Journal of the Medical Library Association, 106(4), 498-500. https://doi.org/10.5195/jmla.2018.518
Halton, C., & Cartwright, T. (2018). Walking in a patient’s shoes: An evaluation study of immersive learning using a digital training intervention. Frontiers in Psychology, 9, 2124. https://doi.org/10.3389/fpsyg.2018.02124
Hojat, M., DeSantis, J., Shannon, S. C., Mortensen, L. H., Speicher, M. R., Bragan, L., LaNoue, M., & Calabrese, L. H. (2018). The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Advances in Health Sciences Education, 23(5), 899-920.
Hu, S. (2022). Raw Jefferson Scores. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.17973662
Hu, S., & Lai, B. W. P. (2022). Increasing empathy for children in dental students using virtual reality. International Journal of Paediatric Dentistry. https://doi.org/10.1111/ipd.12957
Lok, B., Ferdig, R. E., Raij, A., Johnsen, K., Dickerson, R., Coutts, J., Stevens, A., & Lind, D. S. (2006). Applying virtual reality in medical communication education: Current findings and potential teaching and learning benefits of immersive virtual patients. Virtual Reality, 10(3-4), 185-195.
MacDonald-Wicks, L., & Levett-Jones, T. (2012). Effective teaching of communication to health professional undergraduate and postgraduate students: A systematic review. JBI Evidence Synthesis, 10(28), 1-12. https://doi.org/10.11124/jbisrir-2012-327
Mead, N., & Bower, P. (2002). Patient-centred consultations and outcomes in primary care: A review of the literature. Patient education and counseling, 48(1), 51-61.
Mercer, S. W., & Reynolds, W. J. (2002). Empathy and quality of care. British Journal of General Practice, 52(Suppl), S9-S12.
mooc vid. (2019, September 13). Scenario 1 [Video]. YouTube. https://www.youtube.com/watch?v=4f6bZ_Kc2xw
mooc vid. (2019, September 13). Scenario 2 [Video]. YouTube. https://www.youtube.com/watch?v=oz4dm45Imkw
Neumann, M., Edelhäuser, F., Tauschel, D., Fischer, M. R., Wirtz, M., Woopen, C., Haramati, A., & Scheffer, C. (2011). Empathy decline and its reasons: A systematic review of studies with medical students and residents. Academic Medicine, 86(8), 996-1009. https://doi.org/10.1097/ACM.0b013e318221e615
Nheu, L., Uahwatanasakul, W., & Gray, A. (2018). Medical students’ experience of a Teddy Bear Hospital as part of a paediatric curriculum. Focus on Health Professional Education: A Multi-disciplinary Journal, 19(3), 40.
Ong, L., Chua, K. H., Soh, J. Y., & Aw, M. M. H. Y. (2018). Healthcare encounters in young children: Impact of Teddy bear Hospital, Singapore. The Asia Pacific Scholar, 3(3), 24-30. https://doi.org/10.29060/TAPS.2018-3-3/OA1055
Santen, L., & Feldman, T. (1994). Teddy bear clinics: a huge community project. MCN: The American Journal of Maternal/Child Nursing, 19(2), 102-106.
Siegel, B., Lewis, H., Bryan, L., & Batisky, D. (2018). The Teddy Bear Hospital as an outreach tool for reducing medical anxiety: A randomized trial. (2018). Pediatrics, 142(1_MeetingAbstract), 783. https://doi.org/10.1542/peds.142.1MA8.783
Stewart, M., Brown, J. B., Weston, W., McWhinney, I. R., McWilliam, C. L., & Freeman, T. (2013). Patient-centered medicine: Transforming the clinical method. CRC press.
*Shijia Hu
Faculty of Dentistry,
National University of Singapore
9 Lower Kent Ridge Road #10-01
National University Centre for Oral Health,
Singapore 119085
Email: denhus@nus.edu.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









