Challenges and innovations in undergraduate medical education during the COVID-19 pandemic – A systematic review
Submitted: 13 December 2021
Accepted: 22 April 2022
Published online: 5 July, TAPS 2022, 7(3), 1-9
https://doi.org/10.29060/TAPS.2022-7-3/OA2722
Claire Jing-Wen Tan1, Cathryn Cai2, Farida Ithnin2 & Eileen Lew2
1Department of Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Women’s Anaesthesia, KK Women’s and Children’s Hospital, Singapore
Abstract
Introduction: The COVID-19 pandemic has caused significant disruption to undergraduate medical education globally, with worldwide implementation of social distancing and lock-down measures. This systematic review aims to identify challenges in undergraduate medical education during the pandemic and report creative approaches that have been employed to ensure continuity of education.
Methods: A MEDLINE (PubMed) search was performed for articles published between 1 February 2020 and 1 September 2020, corresponding to the pandemic’s global upsurge. Studies, commentaries, perspectives, and correspondence reporting challenges, adaptations and innovations in undergraduate medical education were screened. Data was grouped in accordance with the research questions it sought to address and analysed qualitatively.
Results: 43 studies were included. The COVID-19 pandemic has resulted in lost opportunities for clinical exposure, reduced motivation, and heightened anxiety among medical students. Traditional teaching and assessment methods have transitioned to virtual platforms, harnessing video conferencing, social media, and virtual or augmented reality technologies. The long-term effectiveness of these solutions is uncertain, but immediate benefits conferred include increased access, improved time management, and cultivation of self-directed learning. The lack of authentic clinical experiences and patient interaction remains a major concern. Technical challenges and digital fatigue were also highlighted as pertinent challenges.
Conclusions: The COVID-19 pandemic has provided unexpected, yet invaluable opportunities to explore new pedagogies that may be instrumental in shaping medical education in the new norm. As future members of the healthcare workforce, medical students should be integrated into current healthcare systems to equip them with knowledge and skills to manage future pandemics.
Keywords: COVID-19, Education, Medical, Undergraduate, Medical Student, Telemedicine
Practice Highlights
- The COVID-19 pandemic has caused significant disruption to undergraduate medical education globally.
- Undergraduate medical students faced diminished clinical exposure, poor motivation, and isolation.
- The pandemic has provided unexpected yet invaluable opportunities to explore new teaching pedagogies.
- Institutions should continually adapt these strategies as methods of teaching in the new norm.
I. INTRODUCTION
The appearance of the novel coronavirus (SARS-CoV-2) was first reported in December 2019 (Huang et al., 2020). Since then, the COVID-19 outbreak has become a full-blown global health emergency, with more than 5.3 million deaths reported to date, disruptions in economies and education systems, and increased mental health issues amidst a climate of uncertainty (Torales et al., 2020).
Major disruptions to medical education and training have been experienced worldwide. At the height of the pandemic, universities and medical schools suspended in-campus learning and clinical training to curb the spread of infections (Murphy, 2020; Theoret & Ming, 2020). Non-essential health services were ceased to focus resources on managing the pandemic. With medical faculty deployed to the frontlines, little time and capacity was available for training and teaching. There were reservations deploying medical students in clinical areas, due to safety concerns and consumption of personal protective equipment (PPE) in the face of shortages (Hilburg et al., 2020).
Mitigating measures have challenged academic institutes to explore new pedagogies to sustain and bolster education efforts beyond the crisis. Creative approaches to ensure continuity of medical student education include the transition to e-learning and virtual clerkships, enabled through online video-conferencing platforms, social media, and virtual reality technology. Assessment formats have also been adapted to accommodate virtual evaluation of clinical competencies. While the effectiveness of these approaches remains to be proven, they are instrumental in allowing medical education to continue during the pandemic and into the new norm.
This qualitative systematic review aims to define the challenges associated with medical student education at the height of the COVID-19 pandemic, highlight creative approaches and innovations that were employed to sustain medical education in these unprecedented times, and review their limitations and effectiveness.
II. METHODS
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Page et al., 2021). Literature search was performed on MEDLINE (PubMed) using a combination of the following search terms: (COVID-19 OR pandemic) AND (undergraduate medical education OR undergraduate medical training). The search was tailored for the period of 1 February 2020 to 1 September 2020, to focus on the height of the pandemic.
Articles were included if they met the following criteria: published in English; reported challenges, strategies, and adaptations in conducting undergraduate medical education during the COVID-19 pandemic. To ensure comprehensive coverage, case reports, case and cohort studies, commentaries, perspectives, and correspondence were included. Articles pertaining to postgraduate medical education and non-medical education, non-English articles and systematic reviews were excluded.
Two reviewers (CJT and CC) independently screened the titles and/or abstracts of all articles and selected only articles that met inclusion criteria. Any disagreement was resolved by discussion with senior authors (FI and EL). Data extracted included: challenges encountered in the implementation of undergraduate teaching; innovations, strategies and adaptations employed to facilitate teaching and assessment; perceived limitations and effectiveness of described strategies; original authors’ conclusions. The data was collated on a spreadsheet, grouped by categories, and analysed qualitatively.
III. RESULTS
A total of 123 studies were identified using the search strategy, of which 43 studies eventually met inclusion criteria. The PRISMA study flow-diagram (Figure 1) demonstrates our research algorithm. The data that support the findings of this study are openly available in Figshare at http://doi.org/10.6084/m9.figshare.172968 56 (Tan et al., 2021).
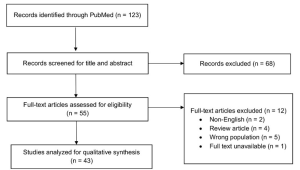
Figure 1: PRISMA flow-diagram of study selection
A. Challenges Arising from the COVID-19 Pandemic
1) Reduced clinical exposure:
Due to the enforcement of safe distancing measures, nearly all medical schools have suspended in-person classes and transitioned to online teaching. Scheduled summer and term breaks have been brought forward to provide a state of academic quarantine (Ashokka et al., 2020). Loss of patient interaction has been consistently cited as one of the biggest challenges in delivering clinical education during the pandemic. Across institutions, medical students have been withdrawn from clinical postings to protect them from infectious transmission and mitigate PPE shortages (Hilburg et al., 2020). With deployment of healthcare workers to the frontlines, clinicians focused attention and resources on patient care, with education taking a backseat (Hilburg et al., 2020; Tolsgaard et al., 2020).
Pre-clerkship medical students were less affected by the online transition, as preclinical contents can be easily adapted for digital learning (Newman & Lattouf, 2020). In contrast, students on clerkship rotations for procedural-based disciplines who rely heavily on patient interactions were severely impacted (Calhoun et al., 2020; Darras et al., 2021; Khalil et al., 2020). Without direct patient interaction, students cannot fully master physical examination skills, although history-taking and other communication skills can arguably be taught through virtual interactions with real or simulated patients. The development of professionalism and communication skills, including discussion of care plans in a multidisciplinary setting and presentation of academic work at professional platforms (Hammond et al., 2020; Rafi et al., 2020), have also been compromised.
2) Unpreparedness for the future:
With a truncated curriculum and migration to digital learning, some students have been disheartened by missed learning opportunities (Rallis & Allen-Tejerina, 2020). They felt incompetent (Hilburg et al., 2020) and unprepared for clinical examinations and patient encounters (Shahrvini et al., 2020). A survey study conducted across 33 medical schools in the United Kingdom reported that 49.5% of final-year students started work in hospitals ahead of anticipated schedule to meet increased manpower demands during the pandemic (Choi et al., 2020). Affected students admitted to feeling ill-equipped, due to the curtailing of final-year examinations and student assistantship programmes (Choi et al., 2020). There is concern that loss of training opportunities could disrupt the supply chain of specialists (Tolsgaard et al., 2020) and future workforce planning (Halbert et al., 2020).
The sense of inadequacy among students is compounded by widespread cancellation of summer elective placements and research programs, originally intended to provide avenues for further enrichment (Rallis & Allen-Tejerina, 2020). Consequently, students have missed out on opportunities to explore interests and immerse in rigorous clinical and research environments to guide them in making informed residency choices (Go & Rajasekaran, 2020).
3) Loss of motivation:
With the move to online learning and cancellation of examinations in some universities, students reported diminished motivation to study (Khalil et al., 2020), exacerbated by inexperience in distant-based learning, poor technical skills and frequent technical difficulties (Muflih et al., 2020). Students have also expressed frustration at the lack of clear communication with faculty members regarding curriculum and assessment plans, fueling negative learning attitudes (Shehata et al., 2020).
4) Socio-emotional isolation:
With loss of social interaction, medical students felt increasingly disconnected from their peers. Interruptions in normal routines and pressure from stay-home orders further fuelled feelings of isolation, apprehension and uncertainty about the future (Shahrvini et al., 2020). An increase in mental health issues was reported among medical students during the pandemic (Shahrvini et al., 2020). To address this, institutions have strengthened peer support systems (Ashokka et al., 2020) and initiated coaching programmes to impart coping skills and help students pursue personalised goal setting (Maini et al., 2020).
B. Innovations, Adaptations, and Strategies Employed in Undergraduate Medical Education
1) Online learning platforms:
Traditional face-to-face teaching has been largely replaced by online learning. ‘Live’ synchronous learning conducted over video-conferencing platforms, including Zoom, Microsoft Team, Google Hangouts, Skype, and WebEx, incorporate functions like screen-sharing, virtual whiteboards, mind-mapping tools, and polling for an interactive experience (Shahrvini et al., 2020). ‘Break-out’ room functions allow students to be further divided into smaller groups for interactive discussions (Darras et al., 2021; Ferrel & Ryan, 2020). Students can also ask and answer questions using the chat function or microphones (Singh et al., 2020). Synchronous tutorial sessions can also be recorded for future reference (Atreya & Acharya, 2020). Some institutions have adopted a flipped classroom approach, with learning material provided to students in advance of online discussions (Naidoo et al., 2020; Singh et al., 2020). Asynchronous lectures, on the other hand, are pre-recorded and have the distinct advantage of cultivating self-directed learning (Farooq et al., 2020).
Furthermore, learning management systems, like Google Classroom, Blackboard, Impartus, and Slack provide centralised platforms for tutors to share teaching materials and multimedia resources, with plug-ins to track students’ progress (Singh et al., 2020). Medical schools have also collaborated to share online resources, through OnlineMedEd, Geeky Medics, Oxford Medical Simulation, and Aquifer (Schaffir et al., 2020).
2) Social media:
Taking advantage of its popularity, tutors have turned to social media platforms for the dissemination of class schedules and learning materials during the pandemic (Iqbal et al., 2020). In one medical college, Telegram was used to create class groups and upload educational resources (Iqbal et al., 2020). At another institution, ophthalmology faculty members created Whatsapp student groups to upload quizzes, reference materials, and teaching videos (Sud et al., 2020).
The use of social media successfully enhanced student participation and collaborative learning (Naidoo et al., 2020). The ability to stay anonymous gave students the confidence to discuss topics without fear of being judged by their peers (Iqbal et al., 2020). As the complex technical interfaces, information overload and digital fatigue could cause distractions (Iqbal et al., 2020), its use should be moderated.
3) Virtual laboratory sessions:
Traditional anatomy classes, using ‘live’ cadaveric dissections, have been discontinued and substituted by novel online formats at some institutions (Darras et al., 2021). Students have been taught to appreciate anatomy via three-dimensional (3D) computer models (Remtulla, 2020) and virtual dissections on digital applications (Longhurst et al., 2020). Comprehensive learning materials have also been uploaded on Virtual Learning Environments (Ashokka et al., 2020; Longhurst et al., 2020; Naidoo et al., 2020). Institutions also conducted real-time tutorials and ‘live’ dissection sessions online (Longhurst et al., 2020). The University of Hong Kong implemented a web-based programme to provide basic surgical skills training to final-year undergraduate students. Tutors demonstrated surgical skills on ‘live’ camera, while students practised suturing at home using kits that were distributed in advance (Co & Chu, 2020).
4) Virtual clinical experience:
Technological advancements have enabled the use of simulations and virtual reality to address gaps associated with distance learning (Remtulla, 2020). Students have been able to learn history taking, clinical reasoning and communication skills via remote role-play with simulated patients (Mukhtar et al., 2020). Videos demonstrating communication, physical examination and procedural skills have also been utilised as teaching aids (Sam et al., 2020). Some universities have even implemented virtual placements with live-streamed ward rounds, empowering students to participate remotely in discussions and case presentations (Sam et al., 2020). At one university, students on virtual surgical electives could observe surgeries remotely, as attending surgeons wore head-mounted cameras to capture the surgical field (Chao et al., 2021).
With the ramp-up of telemedicine services during the pandemic, students have had opportunities to facilitate patient care through telephone or video consultations, enabling them to develop to cultivate interpersonal skills. Students have been roped in to provide virtual updates to patients’ families (Hilburg et al., 2020) and assist in scribing during virtual consultations (Rallis & Allen-Tejerina, 2020). Time pressures (Oki et al., 2021) and breaches in patient confidentiality (Rallis & Allen-Tejerina, 2020) were highlighted as potential concerns. With telemedicine being increasingly integrated into mainstream health services in the new norm, it is imperative to incorporate telemedicine training into the medical curricula to produce a telehealth-ready workforce (Iancu et al., 2020).
Although virtual clinical clerkships cannot fully substitute for hands-on clinical experiences (Nic Dhonncha & Murphy, 2021; Rafi et al., 2020; Roskvist et al., 2020; Sud et al., 2020), they have a role in promoting student engagement with tutors and patients, and helping students develop indispensable clinical skills (Chao et al., 2021).
5) Assessments:
Due to logistical, manpower and technical constraints, some universities have cancelled semester assessments (Tokuç & Varol, 2020). Others have adopted alternative methods to evaluate competencies. A study conducted at 14 medical universities in the United Kingdom and Republic of Ireland revealed that 7% of universities cancelled written examinations, 14% eliminated summative practical assessments and a further 36% cancelled assessments altogether (Longhurst et al., 2020). Only 21% of schools implemented online digital spotter or open-book examinations (Longhurst et al., 2020). Institutions that eliminated examinations altogether laid claim to facing difficulties adapting traditional examination formats to online assessments, and cited the lack of experience and training as underlying factors (Farooq et al., 2020).
Open-book examinations were implemented at some universities and were associated with reduced pressure among students (Hilburg et al., 2020; Nic Dhonncha & Murphy, 2021). Due to its initial success, there are now calls for widespread adoption of open-book examination formats (Hammond et al., 2020). Other institutions have opted for continuous formative assessment in place of scheduled summative assessments (Choi et al., 2020; Shehata et al., 2020).
For strict proctoring to maintain academic integrity during online examinations, web cam and screen capture functions have been harnessed (Hilburg et al., 2020; Mukhtar et al., 2020). Grading systems for examinations have also been modified. Instead of assigning specific grades based on performance, fourth-year medical students on elective courses at the University of Washington School of Medicine were assessed on a pass/fail basis, significantly alleviating students’ stress (Calhoun et al., 2020).
Clinical examinations have been more challenging to administer in compliance with enforced risk mitigation measures. Some schools have chosen to focus on theory assessments instead, while others successfully conducted virtual Objective Structured Clinical Examinations (OSCE), focusing on practical skills and communication capabilities (Naidoo et al., 2020).
C. Barriers and Limitations Associated with Innovations and Adaptations
1) Reduced tutor-student interaction:
Some reports suggest that switching to online learning platforms has compromised student engagement and collaboration (Ashokka et al., 2020; Ferrel & Ryan, 2020; Longhurst et al., 2020). Unlike face-to-face tutorials that facilitate vibrant discussion, online tutorials involve tutors speaking to a blank screen (Atreya & Acharya, 2020; Khalil et al., 2020; Roberts et al., 2020; Sud et al., 2020). The absence of visual cues may lead to communication gaps and loss of personal touch (Khalil et al., 2020; Mukhtar et al., 2020). Specifically, tutors have claimed to face difficulty in gauging students’ understanding (Hilburg et al., 2020; Mukhtar et al., 2020).
Furthermore, it was observed that some students have adopted passive learning attitudes (Sandhaus et al., 2020). It has become exceedingly difficult to engage students in virtual rooms and to retain their attention over prolonged periods (Atreya & Acharya, 2020; Farooq et al., 2020; Roberts et al., 2020). A handful of students were observed to switch off their cameras and mute their microphones, while others claimed they did not feel comfortable to speak up (Roberts et al., 2020).
Strategies have been formulated to increase student participation. Tracking of attendance has been proposed as a means to improve attendance rate, although it remains possible that students may log on but engage in their own activities without paying attention (Atreya & Acharya, 2020). Some tutors have incorporated interactive online quizzes during tutorials (Farooq et al., 2020), while others have decreased tutorial group sizes to optimise engagement (Joseph et al., 2020).
2) Reduced quality of instruction:
With short notice for curricular re-design, universities have faced struggles to obtain the resources necessary for a smooth transition, resulting in disruption to students’ learning in the interim (Oki et al., 2021) and reduced quality of instruction (Shahrvini et al., 2020). Medical students at one university experienced teaching disruption for four weeks during the transition to new teaching methods (Roberts et al., 2020). Tutors have also reported knowledge gaps and time constraints in creating new online educational content, amidst competing professional and personal duties during the pandemic (Newman & Lattouf, 2020).
3) Digital fatigue:
Long hours spent in front of devices have led to exhaustion, poor concentration, and loss of engagement (Shahrvini et al., 2020; Singh et al., 2020). Students also provided feedback on the excessive numbers of lectures and inappropriately long lessons (Khalil et al., 2020; Rafi et al., 2020).
4) Technical challenges:
With the growing reliance on technology, technical issues could compromise the quality of learning and affect learners’ and tutors’ experiences (Atreya & Acharya, 2020; Farooq et al., 2020; Khalil et al., 2020; Sud et al., 2020). Online lectures have often been conducted without real-time technical support (Longhurst et al., 2020), as most institutions lack a dedicated information technology (IT) department (Farooq et al., 2020). Given the steep learning curve with IT (Remtulla, 2020), it is not surprising that students have reported a lack of confidence in completing online assignments (Muflih et al., 2020). Institutions should provide basic computer literacy courses to students and tutors (Muflih et al., 2020).
With families staying home during lockdowns, students often had to share devices (Sud et al., 2020) and internet access (Atreya & Acharya, 2020; Roskvist et al., 2020) with household members. Online learning has also been adversely impacted by limited internet connectivity at remote geographical locations (Cruess et al., 2014; Farooq et al., 2020; Remtulla, 2020; Roskvist et al., 2020) and electrical interruptions from bad weather (Atreya & Acharya, 2020). Although the subscription of costly internet data bundles could circumvent these challenges, socioeconomic disparities could result in the less privileged students falling through the cracks. Hence, institutions must ensure the benefits of online education can be shared equitably by all students (Muflih et al., 2020).
D. Effectiveness of Innovations and Adaptations in Delivering Medical Education
1) Effectiveness of digital learning:
Overall, medical students expressed satisfaction with digital learning during the pandemic (Sandhaus et al., 2020), and reported ample opportunities for clarification (Singh et al., 2020) and communication with classmates and tutors (Muflih et al., 2020). Synchronous virtual lessons were reportedly well-attended, with active student participation (Nic Dhonncha & Murphy, 2021). Not only have online classes been viewed as a viable substitute for in-person teaching (Sud et al., 2020), a significant proportion of pre-clinical students have expressed a preference for online learning over traditional teaching (Khalil et al., 2020), leading to calls for online learning to be retained as a teaching modality post-pandemic. It might be worthwhile to consider the introduction of a hybrid model, comprising both online webinars and face-to-face teaching, in the medical curriculum (Hammond et al., 2020).
2) Access to learning:
With intermittent lock-down and return of international students to their native countries, online teaching platforms facilitated worldwide access to learning resources (Mukhtar et al., 2020). Medical students have also reported benefits arising from flexibility of learning in the comfort of their homes at their own pace (Cruess et al., 2014; Farooq et al., 2020), and feeling empowered to adopt an individualised approach to learning (Loh & Nalliah, 2010).
3) Time efficiency:
Online learning reduces commute time (Mukhtar et al., 2020; Shahrvini et al., 2020; Sud et al., 2020) and campus-based distractions (Sud et al., 2020). With better utility of time, students have had capacity to engage in concurrent activities like volunteering in COVID-19 relief efforts, thereby contributing to their holistic development (Shahrvini et al., 2020). There is also potential for improved academic performance due to efficient time management, better sleep patterns and reduced anxiety associated with learning within comfort zones (Khalil et al., 2020). Some students have also reported satisfaction of having more family bonding time (Sud et al., 2020).
4) Increased self-directed learning and student-led initiatives:
Sudden cessation of traditional, classroom-based teaching has presented a serendipitous opportunity for students to cultivate active learning behaviours and initiate student-led teaching to their peers (Newman & Lattouf, 2020; Roberts et al., 2020). At the Bristol Medical School, a student-led society delivered peer-led teaching sessions via video conferencing platforms (Roberts et al., 2020). These sessions not only helped mentees master content and clarify misconceptions, but also helped mentors reinforce foundational concepts. Students also leveraged on the prevailing volatility, uncertainty, complexity and ambiguity (VUCA) to learn coping skills and develop resilience and versatility, in preparation for their future careers (Ferrel & Ryan, 2020).
5) Opportunities for faculty development:
The COVID-19 pandemic has provided opportunities for universities to strengthen their current curricula by developing new relevant resources, exploring novel blended learning techniques, and developing alternative assessment methods (Longhurst et al., 2020). In a Strengths, Weaknesses, Opportunities and Threats (SWOT) analysis, 71% of British universities identified opportunities to develop new online resources, while 50% cited avenues for academic collaboration between universities (Joseph et al., 2020). Faculty members have also reported opportunities to upskill in new technologies, incorporate innovative software into current curricula and boost their confidence in navigating virtual learning platforms.
IV. DISCUSSION
The COVID-19 pandemic has caused major disruptions to medical education globally and left students feeling incompetent, unmotivated, and anxious. It has also challenged medical schools to explore novel ways of teaching and training that mitigate the risks associated with the pandemic. Insights gathered in this review could inform a strategy for the development of medical curricula in the post-pandemic era, integrating digital technology and novel pedagogy. As there is a paucity of good-quality studies, the effectiveness of virtual learning remains to be proven. However, online teaching cannot substitute for authentic clinical experiences. Modules using simulations and virtual or augmented reality may bridge the gap in procedural skills training, but the loss of inter-professional interactions could affect students’ ability to internalise the core values of medical professionalism – a fundamental component in medical education. Professionalism is traditionally taught through observation of inter-professional interactions, experiential learning, and role-modelling (Cruess et al., 2014; Loh & Nalliah, 2010). Hence, it is important that clerkship rotations are maintained with risk mitigation measures in place so that students can continue to learn and internalise the attributes of medical professionalism, mentored by their tutors.
The present review also revealed the mind shift of medical educators saddled with a protracted pandemic. Early inclination to exclude medical students from all forms of clinical work at the start of the pandemic has progressed to a collective resolve to equip them with the skills and knowledge to manage a pandemic as the future healthcare workforce (Halbert et al., 2020; Tolsgaard et al., 2020). The cautious re-introduction of clinical training has been facilitated by the availability of vaccination and regular testing. To further mitigate risks, students could be embedded in smaller care teams with close supervision. Clinical rotations could also be shortened to the minimum required to achieve competence, with provision for extension of training if students fail to attain proficiency. The opportunity to participate in the pandemic and show courage and altruism by fighting alongside other healthcare workers could go a long way to bolster their confidence and cultivate a shared sense of purpose among students (Chandratre, 2020).
Mental health issues have taken a toll on medical students, stemming from social isolation, lack of work-life balance, experience of illness and death among colleagues and families, and perceptions of inadequacy. However, there is a paucity of published studies on effective measures to address mental health issues during the COVID-19 pandemic. As a group, medical students have a higher prevalence of mental health issues (Molodynski et al., 2021; Schwenk et al., 2010), and are less likely to seek help (Molodynski et al., 2021). Thus, it is imperative to increase surveillance for this at-risk group and strengthen peer support and engagement channels. Further research should seek to delineate the range of mental health conditions faced by medical students in this pandemic, the influence of socio-cultural factors and effective strategies for surveillance and support.
Nonetheless, this systematic review has its limitations. The search was conducted using PubMed for its comprehensive coverage of indexed journal articles, including “in process” citations and links to related citations. However, this could have led to the exclusion of journals not cited by PubMed and the presentation of a more restricted view. References in non-English languages were not analysed. As we have confined our literature search to 1 February 2020 to 1 September 2020 to capture the challenges and innovations in undergraduate medical education at the height of the pandemic, we were unable to report the adaptations to medical education emerging after 1 Sep 2020.
V. CONCLUSION
The COVID-19 pandemic has provided unexpected, yet invaluable opportunities to explore new pedagogies that may be instrumental in shaping medical education in the new norm. Institutions should continue to evaluate and refine these new teaching techniques and content to ensure that the medical curriculum stays relevant and robust. As future members of the healthcare work force in the post-pandemic era, medical students should be integrated into current health systems to equip them with the knowledge, skills, and experience to manage future pandemics. This would also help forge a collective sense of purpose in these uncertain times.
Notes on Contributors
CJT performed the literature search and synthesis, wrote part of the manuscript, and prepared the figure. CC helped with the literature search and wrote part of the manuscript. FI helped in the resolution of disagreements in the literature search and constitution of the manuscript. EL helped in the planning the study, resolution of disagreements in the literature search and constitution of the manuscript.
Ethical Approval
As this study is a systematic review, ethical approval and IRB application was not required.
Data Availability
The data that support the findings of this study are openly available in Figshare repository http://doi.org/10.6084/m 9.figshare.17296856.
Funding
All authors have no funding sources to declare.
Declaration of Interest
All authors declare that they have no competing interests.
References
Ashokka, B., Ong, S. Y., Tay, K. H., Loh, N. H. W., Gee, C. F., & Samarasekera, D. D. (2020). Coordinated responses of academic medical centres to pandemics: Sustaining medical education during COVID-19. Medical Teacher, 42(7), 762-771. https://doi.org/10.1080/0142159x.2020.1757634
Atreya, A., & Acharya, J. (2020). Distant virtual medical education during COVID-19: Half a loaf of bread. The Clinical Teacher, 17(4), 418-419. https://doi.org/10.1111/tct.13185
Calhoun, K. E., Yale, L. A., Whipple, M. E., Allen, S. M., Wood, D. E., & Tatum, R. P. (2020). The impact of COVID-19 on medical student surgical education: Implementing extreme pandemic response measures in a widely distributed surgical clerkship experience. The American Journal of Surgery, 220(1), 44-47. https://doi.org/10.1016/j.amjsurg.2020.04.024
Chandratre, S. (2020). Medical students and COVID-19: Challenges and supportive strategies. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520935059
Chao, T. N., Frost, A. S., Brody, R. M., Byrnes, Y. M., Cannady, S. B., Luu, N. N., Rajasekaran, K., Shanti, R. M., Silberthau, K. R., Triantafillou, V., & Newman, J. G. (2021). Creation of an interactive virtual surgical rotation for undergraduate medical education during the COVID-19 pandemic. Journal of Surgical Education, 78(1), 346-350. https://doi.org/10.1016/j.jsurg.2020.06.039
Choi, B., Jegatheeswaran, L., Minocha, A., Alhilani, M., Nakhoul, M., & Mutengesa, E. (2020). The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: A national survey. BMC Medical Education, 20(1), 206. https://doi.org/10.1186/s12909-020-02117-1
Co, M., & Chu, K. M. (2020). Distant surgical teaching during COVID-19 – A pilot study on final year medical students. Surgical Practice, 24(3), 105– 109. https://doi.org/10.1111/1744-1633.12436
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2014). Reframing medical education to support professional identity formation. Academic Medicine, 89(11), 1446-1451. https://doi.org/10.1097/acm.0000000000000427
Darras, K. E., Spouge, R. J., de Bruin, A. B. H., Sedlic, A., Hague, C., & Forster, B. B. (2021). Undergraduate radiology education during the COVID-19 pandemic: A review of teaching and learning strategies. Canadian Association of Radiologists Journal, 72(2), 194-200. https://doi.org/10.1177/0846537120944821
Farooq, F., Rathore, F. A., & Mansoor, S. N. (2020). Challenges of online medical education in Pakistan during COVID-19 pandemic. Journal of the College of Physicians and Surgeons Pakistan, 30(6), 67–69. https://doi.org/10.29271/jcpsp.2020.Supp1.S67
Ferrel, M. N., & Ryan, J. J. (2020). The impact of COVID-19 on medical education. Cureus, 12(3), e7492. https://doi.org/10.7759/cureus.7492
Go, B., & Rajasekaran, K. (2020). Effect of COVID-19 in selecting otolaryngology as a specialty. Head & Neck, 42(7), 1409-1410. https://doi.org/10.1002/hed.26251
Halbert, J. A., Jones, A., & Ramsey, L. P. (2020). Clinical placements for medical students in the time of COVID-19. Medical Journal of Australia, 213(2), 69-69. e61. https://doi.org/10.5694/mja2.50686
Hammond, D., Louca, C., Leeves, L., & Rampes, S. (2020). Undergraduate medical education and Covid-19: Engaged but abstract. Medical Education Online, 25(1), 1781379. https://doi.org/10.1080/10872981.2020.1781379
Hilburg, R., Patel, N., Ambruso, S., Biewald, M. A., & Farouk, S. S. (2020). Medical Education During the Coronavirus Disease-2019 Pandemic: Learning From a Distance. Advances in Chronic Kidney Disease, 27(5), 412-417. https://doi.org/10.1053/j.ackd.2020.05.017
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., Zhang, L., Fan, G., Xu, J., Gu, X., Cheng, Z., Yu, T., Xia, J., Wei, Y., Wu, W., Xie, X., Yin, W., Li, H., Liu, M., . . . Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet, 395(10223), 497-506. https://doi.org/10.1016/S0140-6736(20)30183-5
Iancu, A. M., Kemp, M. T., & Alam, H. B. (2020). Unmuting medical students’ education: Utilizing telemedicine during the COVID-19 pandemic and beyond. Journal of Medical Internet Research, 22(7), e19667. https://doi.org/10.2196/19667
Iqbal, M. Z., Alradhi, H. I., Alhumaidi, A. A., Alshaikh, K. H., AlObaid, A. M., Alhashim, M. T., & AlSheikh, M. H. (2020). Telegram as a tool to supplement online medical education during COVID-19 crisis. Acta Informatica Medica, 28(2), 94-97. https://doi.org/10.5455/aim.2020.28.94-97
Joseph, J. P., Joseph, A. O., Conn, G., Ahsan, E., Jackson, R., & Kinnear, J. (2020). COVID-19 pandemic-medical education adaptations: The power of students, staff and technology. Medical Science Educator, 30(4), 1355-1356. https://doi.org/10.1007/s40670-020-01038-4
Khalil, R., Mansour, A. E., Fadda, W. A., Almisnid, K., Aldamegh, M., Al-Nafeesah, A., Alkhalifah, A., & Al-Wutayd, O. (2020). The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: A qualitative study exploring medical students’ perspectives. BMC Medical Education, 20(1), 285. https://doi.org/10.1186/s12909-020-02208-z
Loh, K. Y., & Nalliah, S. (2010). Learning professionalism by role-modelling. Medical Education, 44(11), 1123. https://doi.org/10.1111/j.1365-2923.2010.03827.x
Longhurst, G. J., Stone, D. M., Dulohery, K., Scully, D., Campbell, T., & Smith, C. F. (2020). Strength, Weakness, Opportunity, Threat (SWOT) Analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the Covid-19 pandemic. Anatomical Sciences Education, 13(3), 301-311. https://doi.org/10.1002/ase.1967
Maini, A., Saravanan, Y., Singh, T. A., & Fyfe, M. (2020). Coaching skills for medical education in a VUCA world. Medical Teacher, 42(11), 1308-1309. https://doi.org/10.1080/0142159x.2020.1788713
Molodynski, A., Lewis, T., Kadhum, M., Farrell, S. M., Lemtiri Chelieh, M., Falcão De Almeida, T., Masri, R., Kar, A., Volpe, U., Moir, F., Torales, J., Castaldelli-Maia, J. M., Chau, S. W. H., Wilkes, C., & Bhugra, D. (2021). Cultural variations in wellbeing, burnout and substance use amongst medical students in twelve countries. International Review of Psychiatry, 33(1-2), 37-42. https://doi.org/10.1080/09540261.2020.1738064
Muflih, S., Abuhammad, S., Karasneh, R., Al-Azzam, S., Alzoubi, K. H., & Muflih, M. (2020). Online education for undergraduate health professional education during the COVID-19 pandemic: Attitudes, barriers, and ethical issues. Research Square. https://doi.org/10.21203/rs.3.rs-42336/v1
Mukhtar, K., Javed, K., Arooj, M., & Sethi, A. (2020). Advantages, limitations and recommendations for online learning during COVID-19 pandemic era. Pakistan Journal of Medical Sciences, 36(Covid19-s4), S27-S31. https://doi.org/10.12669/pjms.36.COVID19-S4.2785
Murphy, B. (2020). COVID-19: How the virus is impacting medical schools. Retrieved 18 Dec, 2020, from https://www.ama-assn.org/delivering-care/public-health/covid-19-how-virus-impacting-medical-schools
Naidoo, N., Akhras, A., & Banerjee, Y. (2020). Confronting the challenges of anatomy education in a competency-based medical curriculum during normal and unprecedented times (COVID-19 Pandemic): Pedagogical framework development and implementation. JMIR Medical Education, 6(2), e21701. https://doi.org/10.2196/21701
Newman, N. A., & Lattouf, O. M. (2020). Coalition for medical education—A call to action: A proposition to adapt clinical medical education to meet the needs of students and other healthcare learners during COVID-19. Journal of Cardiac Surgery, 35(6), 1174-1175. https://doi.org/10.1111/jocs.14590
Nic Dhonncha, E., & Murphy, M. (2021). Learning new ways of teaching and assessment: the impact of COVID-19 on undergraduate dermatology education. Clinical and Experimental Dermatology, 46(1), 170-171. https://doi.org/10.1111/ced.14364
Oki, O., Shah, S., Scrivens, L., & Guckian, J. (2021). COVID-19: Challenges and solutions for the future of UK dermatology undergraduate curriculum delivery. Clinical and Experimental Dermatology, 46(1), 171-173. https://doi.org/10.1111/ced.14386
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., . . . Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
Rafi, A. M., Varghese, P. R., & Kuttichira, P. (2020). The pedagogical shift during COVID 19 pandemic: Online medical education, barriers and perceptions in Central Kerala. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520951795
Rallis, K. S., & Allen-Tejerina, A. M. (2020). Tele-oncology in the COVID-19 era: Are medical students left behind? Trends Cancer, 6(10), 811-812. https://doi.org/10.1016/j.trecan.2020.08.001
Remtulla, R. (2020). The present and future applications of technology in adapting medical education amidst the COVID-19 pandemic. JMIR Medical Education, 6(2), e20190. https://doi.org/10.2196/20190
Roberts, V., Malone, K., Moore, P., Russell-Webster, T., & Caulfield, R. (2020). Peer teaching medical students during a pandemic. Medical Education Online, 25(1), 1772014. https://doi.org/10.1080/10872981.2020.1772014
Roskvist, R., Eggleton, K., & Goodyear-Smith, F. (2020). Provision of e-learning programmes to replace undergraduate medical students’ clinical general practice attachments during COVID-19 stand-down. Education for Primary Care, 31(4), 247-254. https://doi.org/10.1080/14739879.2020.1772123
Sam, A. H., Millar, K. R., & Lupton, M. G. F. (2020). Digital clinical placement for medical students in response to COVID-19. Academic Medicine, 95(8), 1126. https://doi.org/10.1097/acm.0000000000003431
Sandhaus, Y., Kushnir, T., & Ashkenazi, S. (2020). Electronic distance learning of pre-clinical studies during the COVID-19 pandemic: A preliminary study of medical student responses and potential future impact. The Israel Medical Association Journal, 22(8), 489-493.
Schaffir, J., Strafford, K., Worly, B., & Traugott, A. (2020). Challenges to medical education on surgical services during the COVID-19 pandemic. Medical Science Educator, 30(4), 1667–1671. https://doi.org/10.1007/s40670-020-01072-2
Schwenk, T. L., Davis, L., & Wimsatt, L. A. (2010). Depression, stigma, and suicidal ideation in medical students. JAMA, 304(11), 1181-1190. https://doi.org/10.1001/jama.2010.1300
Shahrvini, B., Baxter, S. L., Coffey, C. S., MacDonald, B. V., & Lander, L. (2020). Pre-clinical remote undergraduate medical education during the COVID-19 pandemic: A survey study. Research Square. https://doi.org/10.21203/rs.3.rs-33870/v1
Shehata, M. H., Abouzeid, E., Wasfy, N. F., Abdelaziz, A., Wells, R. L., & Ahmed, S. A. (2020). Medical education adaptations post COVID-19: An Egyptian reflection. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520951819
Singh, K., Srivastav, S., Bhardwaj, A., Dixit, A., & Misra, S. (2020). Medical education during the COVID-19 pandemic: A single institution experience. Indian Pediatrics, 57(7), 678-679. https://doi.org/10.1007/s13312-020-1899-2
Sud, R., Sharma, P., Budhwar, V., & Khanduja, S. (2020). Undergraduate ophthalmology teaching in COVID-19 times: Students’ perspective and feedback. Indian Journal of Ophthalmologyy, 68(7), 1490-1491. https://doi.org/10.4103/ijo.IJO_1689_20
Tan, J. W. C., Cai, C., Ithnin, F., & Lew, E. (2021). Challenges and innovations in undergraduate medical education during the COVID-19 pandemic – A systematic review [Data set]. Figshare. http://doi.org/10.6084/m9.figshare.17296856
Theoret, C., & Ming, X. (2020). Our education, our concerns: The impact on medical student education of COVID-19. Medical Education, 54(7), 591-592. https://doi.org/10.1111/medu.14181
Tokuç, B., & Varol, G. (2020). Medical education in Turkey in time of COVID-19. Balkan Medical Journal, 37(4), 180-181. https://doi.org/10.4274/balkanmedj.galenos.2020.2020.4.003
Tolsgaard, M. G., Cleland, J., Wilkinson, T., & Ellaway, R. H. (2020). How we make choices and sacrifices in medical education during the COVID-19 pandemic. Medical Teacher, 42(7), 741-743. https://doi.org/10.1080/0142159x.2020.1767769
Torales, J., O’Higgins, M., Castaldelli-Maia, J. M., & Ventriglio, A. (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry, 66(4), 317-320. https://doi.org/10.1177/0020764020915212
*Eileen Lew
KK Women’s and Children’s Hospital,
100 Bukit Timah Road
Singapore 229899
Telephone: +65 6394 2422
Email: eileen.lew@singhealth.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









