Challenges and experiences to develop a Japanese language course for international medical students in Japan: Maximising acquisition of Japanese language by applying adult learning theories
Submitted: 14 June 2021
Accepted: 22 July 2021
Published online: 4 January, TAPS 2022, 7(1), 3-8
https://doi.org/10.29060/TAPS.2022-7-1/GP2655
Nagisa Shinagawa1, Tomoaki Inada2, Harumi Gomi3, Haruko Akatsu3, Motofumi Yoshida3 & Yutaka Kawakami3
1Graduate School of Medicine, International University of Health and Welfare, Japan; 2International Center, Jumonji University, Japan; 3School of Medicine, International University of Health and Welfare, Japan
Abstract
Introduction: The International University of Health and Welfare (IUHW) School of Medicine was founded in 2017 with the intention of providing medical content in English a historical first in Japan. Twenty international medical students have been accepted annually, with the majority possessing less than beginner level Japanese language proficiency at the time of enrolment. However, proficiency in Japanese, especially in the context of medicine is required for academic success and program completion. To address this, the IUHW School of Medicine has developed a course in medical Japanese with the objective of facilitating international students’ acquisition of medical Japanese and reinforcing such acquisition through various listening, speaking, reading, and writing activities. This study aims to describe the Japanese language education program for international students at the IUHW School of Medicine, with particular focus on the development of the curriculum and course content.
Methods: The course is designed based on the following educational strategies and their applications: (a) Synchronisation of both medical and Japanese contents; (b) Collaborative learning; (c) Japanese output of medical content learned in English; (d) Practical output through making/giving a presentation and discussion with medical experts; (e) Detailed language feedback from language experts; (f) Reinforcing the vocabulary knowledge by writing; and (g) Building up vocabulary and expressions with relevant contents.
Results: Our observations suggest that our international students have been able to continue their medical education in Japanese smoothly.
Conclusion: The content-based instructional design that includes second language acquisition strategies may also be applicable to other Asian languages such as Korean and Chinese.
Practice Highlights
- We have developed a medical Japanese language course to facilitate international students’ acquisition of Japanese medical language and to reinforce such acquisition through various listening, speaking, reading, and writing activities.
- According to the course design, Japanese language teachers introduce medical vocabulary and expressions into their lessons, and medical teachers determine their application by checking for errors in their Japanese-language presentation of medically-related content.
- This is the first effort in Japan to systematically teach medical Japanese to international students at the elementary level at a medical school.
- This approach has had a positive effect on international students’ acquisition of medical Japanese.
I. INTRODUCTION
International medical students’ need for linguistic educational support has been well reported by researchers in various countries. Many international students in Europe and the United States who have passed the language proficiency tests of their host institutions and are judged to have high language proficiency reportedly continue to have language-related problems in their academic and clinical work at medical schools (Michalski et al., 2017). To address this issue, educational courses for international students studying medicine in a second or third language are being implemented (Huhn et al., 2018). Although reports of such efforts in Chinese medical schools have surfaced in recent years (Zhang et al., 2019), no reports on systematic Japanese language education for international medical students have been published, in part due to the small number of international students in Japanese medical schools.
At the International University of Health and Welfare (IUHW) School of Medicine in Japan, 20 international medical students have been accepted annually since its foundation in 2017. However, the majority of admitted international students have possessed less than beginner level Japanese language proficiency at the time of enrolment. Notably, although international students have been accepted at university medical schools in Japan in the past, most of them have had high levels of Japanese language proficiency at the time of admission.
IUHW School of Medicine’s admission policy is as follows:
“Students must have achieved outstanding grades, outstanding English capability, a future-oriented and global outlook, and be strongly resolved to contribute to the development of the fields of health, medicine, and welfare in both their home country and the global community, in response to medical needs in Japan and overseas.”
This policy of accepting international students with limited Japanese proficiency is to facilitate the acceptance of outstanding students from Asia regardless of their Japanese ability and thus train them to become international medical doctors.
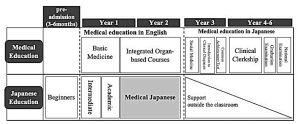
Figure 1. Medical Education Curriculum (top row) and Japanese Education Curriculum (bottom row) at International University of Health and Welfare School of Medicine, Japan
Figure 1 presents a simplified version of the curriculum of IUHW School of Medicine as well as the Japanese language education curriculum. At IUHW, medical education is carried out in English during the first two years of the six-year curriculum. International students come to Japan three to six months prior to entering medical school and attend several intensive pre-admission Japanese language courses. It is a condition of admission that students must acquire a beginner’s level of general Japanese before entering medical school. After enrolment, international students learn medicine together with Japanese students in English, while simultaneously continuing to learn Japanese. From the third year onwards, they learn medicine in Japanese and take the Common Achievement Tests (CAT) in Japanese; these comprise computer-based testing (CBT) for medical knowledge and an objective structured clinical examination (OSCE) on clinical skills. Both components are national tests that determine progression to the following year of study. All medical students in Japan must pass the CAT to proceed to a clinical clerkship. Essentially, passing the CAT is the prerequisite for passing the National Medical Licensure Examination, required to practice medicine as a physician in Japan.
To date, medical Japanese has rarely been research on the efficiency and methods of teaching medical Japanese to foreign students is rare due to the relatively small number of international medical students and foreign doctors in Japan. However, in recent years, research has revealed that medical Japanese is a distinct language that includes grammar and expressions that differ from general Japanese, with 80% of the vocabulary not covered in general Japanese language education curricula (Yamamoto et al., 2018).
Considering the precedents of other countries mentioned above, the Japanese language is not an exception for international medical students in Japan. However, if only general Japanese language classes are conducted, students will not only fail to acquire the knowledge and operational skills of medical Japanese but will be furthermore unable to acquire and retain the vast quantities of medical terminology they will encounter. As such, the IUHW School of Medicine has developed its own course in medical Japanese.
This study aims to describe the Japanese language education program for international students at the IUHW School of Medicine, with particular focus on the development of the “medical Japanese” course and its content. It is hoped that this paper will contribute to the development of educational curriculums for international medical students especially those from Asian countries who plan to study medicine in a second or third language.
II. SCOPE AND BACKGROUND INFORMATION
IUHW School of Medicine’s international students are currently, from Vietnam, Myanmar, Cambodia, Indonesia, Laos, Malaysia, Mongolia, Korea, China, and the United States (As of 2020). Most are from Southeast Asian countries, and, as noted, they arrive in Japan three to six months before beginning formal medical study with little or no Japanese language skills. At the IUHW School of Medicine, they begin learning Japanese from the “Hiragana”, a sort of Japanese language alphabet similar to the ABCs of English. After completing the beginner level course, they begin the formal study of medicine, and they will continue studying Japanese along with medicine in all years of study. The first and second semesters of the first year are dedicated to intermediate level study and the third term of the first year to the third term of the second year, they learn medical Japanese.
The objectives of the medical Japanese course are facilitating students’ acquisition of medical language through various listening, speaking, reading, and writing activities, reinforcing such acquisition, and developing their ability to deliver presentations in Japanese based on medical knowledge acquired in English. It was designed to provide content-based instruction (Grabe & Stoller, 1997) and was developed using various approaches to second language acquisition, such as collaborative learning and output-based activities.
Adult learning theory is the theoretical background for the development of this course. “A need to know” is an important element of adult learning theory. As students aim to become physicians in Japan, they often feel a strong need to acquire Japanese language skills and academic proficiency in Japanese. Particularly, since they know they will be studying medicine in Japanese from their third year on, they feel they must acquire medical Japanese before that time. As such, using medical content for Japanese language learning can satisfy this need and assist them in maintaining their internal motivation to learn. This leads us to “motivation to learn,” another important element of adult learning theory.
Adult learning theory focuses on self-directed learning involving the teaching of adults to be in control of their learning. Since students study medicine in English daily during their first two years of medical education, synchronising medical content with Japanese medical language learning facilitates their learning of medical terms, expressions, and phrases in Japanese using their existing knowledge. As they transit to studying medicine in Japanese from the third year onwards, international students become more autonomous inside and outside the classroom. Moreover, they work together with their Japanese classmates to utilise their content knowledge from the first two years to promote efficient acquisition of Japanese medical terms. From their third year of medical education onwards, since no additional formal Japanese language instruction is offered, international students are expected to primarily act as autonomous learners.
At the IUHW School of Medicine, from the third term in the first year to the end of the second year, the following 13 Integrated Organ-based Courses are provided: the Cardiovascular System, the Respiratory System, the Digestive System, the Endocrine System, the Renal System including Urology, the Gynecological System including the Mammary Gland, the Motor and Dermatological System including Connective Tissue, the Neurological System including Psychiatry, the Sensory Organ System, the Hematological System, Development and Abnormalities from Foetus to Child, Infectious Diseases, and Oncology including Radiotherapy and Palliative Care.
In the medical Japanese course, the units are aligned with the abovementioned specialties (see Figure 2). Group presentations are delivered on specific themes within those specialties. The composition of one unit is presented in Table 1. The teacher (hereafter “medical teacher”) of each organ-system subject selects four themes for each unit. For each theme, the key points to be learned in the second year are stipulated. For example, the Cardiovascular System medical teacher presents the key points, including pathology, epidemiology, diagnosis, treatment, and prognoses for various diseases (themes) such as hypertension, acute myocardial infarction, atrial fibrillation, and aortic stenosis.
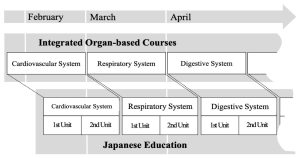
Figure 2. Linkage with Specialties
|
Time period |
Contents |
Details of Activities |
|
1 |
Vocabulary and contents learning |
Learning the vocabulary and contents of the theme using textbook. |
|
2 |
Presentation preparation |
Making the slides and the script |
|
3 |
Presentation rehearsal |
Check the slides and the script |
|
4 |
Presentation 1 |
・Presentation of the two groups ・Q&A session ・Plenary formative feedback session |
|
5 |
Presentation 2 |
・Presentation of the two groups ・Q&A session ・Plenary formative feedback session |
|
6 |
Presentation feedback |
・Individual feedback ・Overall general feedback ・Mini-reports |
|
7 |
Reading comprehension |
Reading the computer-based testing (CBT) workbook |
Table 1. Composition of One Unit
III. EDUCATIONAL STRATEGIES AND THEIR APPLICATIONS
We constructed the course based on educational strategies such as, synchronised medical contents and Japanese terms, small group discussion, and extensive reading, as detailed below.
A. Synchronisation of Both Medical and Japanese Contents
We intentionally synchronise the medical content and Japanese medical vocabulary to promote contextual learning for our students. The first hour of the session is preparatory time where the vocabulary and contents related to the particular theme. During this time, the vocabulary and expressions that are essential to the presentation are self-learned, after which class activities are carried out to reinforce understanding and apply content knowledge. As for the class activities, we conduct a variety of quizzes using interactive applications, such as Kahoot™ and Quizlet™. The Japanese language has three different sets of characters used in writing, and thus some medical terms are not easy for students to read. We use these interactive quiz applications to check for ability to read and comprehend each medical term.
B. Collaborative Learning
To promote deeper learning, group work for collaborative learning has been implemented.
In the second hour, students are divided into four groups, and presentation preparation is conducted. When the group leader initiates a review of the first session, the content of the theme is reconfirmed, along with the flow of the presentation and how the presentation frames should be distributed among the teammates.
Subsequently, students prepare the slides and presentation scripts individually, and then check with each other.
C. Japanese Output of Medical Content Learned in English
In the third hour, a rehearsal of the presentation is conducted, and two Japanese teachers listen to two group presentations (each 30 minutes per group). They write down any noteworthy points on a whiteboard and provide their feedback. They also check the slides for mistaken “Kanji” (Chinese characters in Japanese written format), for missing source references and pronunciation errors.
D. Practical Output through Making/Giving a Presentation, and Discussion with Medical Experts
In the fourth and fifth hours, presentations are made. In each hour, two groups deliver 15-minute presentations, each of which is followed by a 10-minute question and answer (Q&A) session and a 5-minute plenary formative feedback session. The medical teachers who teach the covered content in English listen to the presentations, answer questions, provide supplementary explanations, and correct students’ presentation as needed. The medical teachers use various categories to assess the presentations, such as the overall structure and appropriate application of medical knowledge. Simultaneously, the Japanese teachers assess the presentations for grammar and pronunciation.
E. Detailed Language Feedback by Language Experts
In the sixth hour, students will be given two types of feedback for the presentation: “individual feedback” and “feedback to everybody“. For the “individual feedback”, the students individually review their video-recorded presentations, based on a “presentation feedback sheet” created by the Japanese teachers. More specifically, this sheet includes comments about any pronunciation/expression errors made by the students. During “feedback to everybody”, the Japanese teacher explain and describe the Japanese expressions used by the students in the presentations and used by the medical teachers in the plenary formative feedback session, and the students further reflect on their Japanese.
F. Reinforcing the Vocabulary Knowledge by Writing
After receiving this feedback, the students write a mini-report. They are asked to summarise the contents of their presentations in a report, which is then reviewed by a Japanese teacher who corrects it and gives individual feedback later. It is generally desirable to learn specialised terms in the context of specialised subjects. It is also important to be exposed to the same words multiple times to acquire and retain vocabulary. By writing the summary related to the presentation contents, the students are given the opportunity to come into contact with medical terms multiple times.
G. Building Up Vocabulary and Expression with Relevant Content
In the seventh hour, extensive reading is conducted. Materials include the questions and commentaries for the 8–10 questions related to the presentation themes; these are selected by the medical teachers for each organ-system subject from a commercially available computer-based testing (CBT) workbook (Question Bank CBT, MEDIC MEDIA Co., Ltd.). It is important to note that the objective is not to answer comprehension questions but rather to understand the characteristic medical expressions, reinforce that understanding, and build vocabulary. Furthermore, the purpose is to familiarise the students with the question format in anticipation of the CBT examination they will undertake in their third year.
IV. DISCUSSION
This paper described the development of a medical Japanese course at the IUHW School of Medicine aiming to foster international students’ mastery of medical Japanese through various listening, speaking, reading, and writing activities.
Our observations suggest that IUHW School of Medicine’s international students have been able to continue their medical education in Japanese smoothly. The course assessment is based on the following two points: a vocabulary test for each Integrated Organ-based Course, and a rubric assessment by medical teachers and Japanese teachers at the time of presentation. In addition, we conducted questionnaires and interviews every end-of-semester with students. From the questionnaires, we could see that the students feel that this course will surely be useful for the medical school classes given in Japanese after the third year. The following compilation of comments from the interviews are illustrative: “I was able to reconstruct the fragmented knowledge in my mind by presenting in Japanese in this class what I learned in other medical courses in English.” “Since this class was synchronised with the medical courses, I was not only interested in giving my own presentation, but also in listening to other groups’ presentations.” “There were things that I did not understand in the medical courses that I was able to understand after listening to the presentations in this class.”
These results indicate that the Japanese medical course promotes students simultaneous learning of language forms (vocabulary, grammar, etc.) and medical content.
V. CONCLUSION
The content-based instructional design of our Japanese medical language course applies second language acquisition strategies simultaneously with adult learning theories such as contextual learning and collaborative learning. It is a teaching format for learning medical knowledge through the medium of English, and simultaneously learning another language other than English. In this case, the method was applied to Japanese language acquisition, specifically Japanese medical language acquisition. The method also offers scaffolding for international students to prepare them to continue their medical learning in Japanese on their own after the course. Having observed the Japanese language course over the three years since its implementation, we speculate that this method is applicable not only to the study of Japanese but also to the study in other Asian languages such as Korean and Chinese.
Notes on Contributors
NS reviewed the literature, designed the study and wrote the manuscript. TI advised the design of the study, gave critical feedback to the writing of the manuscript. HG gave scientific insight and advice, critically reviewed and edited the manuscript. HA, MY and YK have read and approved the final manuscript.
Acknowledgement
The authors wish to express sincere appreciation to Ahmed E. Hegab, Yuko Shiima, and Florescu M. Cosmin, International University of Health and Welfare, Medical School, for their constructive discussions and feedback during the preparation of this manuscript.
Funding
There is no funding for this paper.
Declaration of Interest
None of the authors have any competing interests.
References
Grabe, W., & Stoller, F. L. (1997). Content-Based Instruction: Research Foundations. https://carla.umn.edu/cobaltt/modules/principles/grabe_stoller1997/foundation.pdf (Accessed 7 April 2021).
Huhn, D., Al Halabi, K., Alhalabi, O., Armstrong, C., Castell Morley, A., Herzong, W., & Nikendei, C. (2018). Interactive peer-guided examination preparation course for second-year international full-time medical students: Quantitative and qualitative evaluation. GMS Journal for Medical Education, 35(5). https://doi.org/10.3205%2Fzma001203
Michalski, K., Farhan, N., Motschall, E., Vach, W., & Boeker, M. (2017). Dealing with foreign cultural paradigms: A systematic review on intercultural challenges of international medical graduates. PLOS ONE, 12(7), e0181330. https://doi.org/10.1371/journal.pone.0181330
Yamamoto, K., Inada, T., & Shinagawa, N. (2018). Ishikokkashikenno meishigoino taisuuyuudohini motozuku bunsekito kyoozaikaihatuno kanousei [Log-likelihood Analysis of Nouns in the National Examination for Medical Practitioners and the Development of Teaching Materials for International Medical Students]. Nihongo / Nihongo kyouiku. [Japanese/Japanese Education], (9), 245-260.
Zhang, J., Cheng, M., Guo, N., Xing, A., & Xu, L. (2019). ‘Standardized patients’ in teaching the communication skill of history-taking to four-year foreign medical undergraduates in the department of obstetrics and gynaecology. BMC Medical Education, 19(108). https://doi.org/10.1186/s12909-019-1541-y
*Nagisa Shinagawa
International University of Health and Welfare,
4-3 Kouzunomori, Narita,
Chiba 286-8686 Japan
Tel: +81-476-20-7701
Email: sinagawa@iuhw.ac.jp











