Can digital media affect the learning approach of medical students?
Published online: 2 January, TAPS 2019, 4(1), 13-23
DOI: https://doi.org/10.29060/TAPS.2019-4-1/OA1058
Sonali Prashant Chonkar1,2, Hester Lau Chang Qi2, Tam Cam Ha3, Melissa Lim2, Mor Jack Ng2 & Kok Hian Tan1,2,4,5,6
1Duke-NUS Medical School, Singapore; 2Division of Obstetrics & Gynaecology (O&G), Kandang Kerbau Women’s and Children’s Hospital (KKH), Singapore; 3The University of Wollongong, Australia, 4SingHealth Duke-NUS Joint Office of Academic Medicine, Singapore; 5Yong Loo Lin School of Medicine, NUS, Singapore; 6Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
Abstract
Background: Students’ learning approaches have revealed that deep learning approach has a positive impact on academic performance. There are suggestions of a waning interest in deep learning to surface learning.
Aim: To assess if digital media can reduce the incidence of surface learning approach among medical students
Method: A digital video introducing three predominant learning approaches (deep, strategic, surface) was shown to medical students between March 2015 and January 2017. The Approaches and Study Skills Inventory for Students (ASSIST), was administered at the beginning and end of their clinical attachment, to determine if there were any changes to the predominant learning approaches. A survey was conducted using a 5-point Likert scale to assess if video resulted in change.
Results: Of 351 students, 191 (54.4%) adopted deep, 118 (33.6%) adopted strategic and 42 (12.0%) adopted surface as their predominant learning approach at the beginning of their clinical attachment. At the end of their clinical attachment, 171 (49.6%) adopted deep, 143 (41.4%) adopted strategic and 31 (9.0%) adopted surface learning as their predominant learning approach. The incidence of students predominantly using surface approach decreased from 42 (12.0%) to 31 (9.0%), although not statistically significant. Qualitative feedback from students stated that they were more likely to adopt non-surface learning approaches after viewing the video.
Conclusion: This evaluation highlighted the potential of digital media as an educational tool to help medical students reflect on their individual learning approaches and reduce the incidence of surface learning approach.
Keywords: Learning Approaches, ASSIST, Digital Media, Video, Deep Learning, Surface Learning
Practice Highlights
- Digital media can help educate the students about three learning approaches: deep learning, strategic learning and surface learning approach.
- Digital media can encourage students to reflect on their own predominant learning approach.
- Digital media has potential to reduce the medical students’ reliance on surface learning approach.
- Approaches to learning may be influenced by curriculum structure.
I. INTRODUCTION
Medical students are exposed to staggering amounts of information during their career and have to assimilate information, apply clinical reasoning and undertake high stakes assessments. Most schools however, do not concentrate so much on the way students comprehend this knowledge. The way a student learns is affected by how the student was taught, the policies of the department and school, and the student’s own learning style (Newble & Entwistle, 1986). It is an acquired trait dependent on the learning context (Entwistle, 1997). There is little effort employed by teachers to enhance the possibility that individual students will achieve their full potential. Studying students’ approach to learning thus becomes an important factor that can determine both the quality and quantity of students’ learning (Amini, Tajamul, Lotfi, & Karimian, 2012).
In the recent years, there is a greater shift in focus to explore students’ approach to learning, particularly on these three distinct learning approaches – deep, strategic and surface approaches (Subasinghe & Wanniachchi, 2009; Wickramasinghe & Samarasekera, 2011; Samarakoon, Fernando, & Rodrigo, 2013; Shankar, Balasubramanium, & Dwivedi, 2014; Reid, Evans, & Duvall, 2012; Shah et al., 2016; Shankar, Dubey, Binu, Subish, & Deshpande, 2005; Aaron & Skakun, 1999; Cebeci, Dane, Kaya, & Yigitoglu, 2013; Amini et al., 2012). Deep learners focus developing interest in ideas, on reflecting and making connections between related concepts, thereby gaining a more thorough understanding, as well as better retention of content. Strategic learners adopt a systematic manner of studying with overt emphasis on learning certain concepts to excel in assessments. However, there may not be adequate integration across the topics as compared to deep approach and learners sometimes lack conceptual understanding (Leite, Svinicki, & Shi, 2010). Surface learners memorise all the information with little or no conceptual understanding and as a result, often find little interest in the concepts learned and tend not to read beyond what is stated in the syllabus. They may also be poorly motivated and result in being ineffective learners with a low level of understanding. Trigwell and Prosser (1991) suggested a negative correlation between surface learning approach and quality of learning, and the opposite for deep learners. Subasinghe et al. (2011) concluded that the adoption of deep and strategic learning approach will be beneficial to medical students, since their learning involves critical analysis and application of concepts for complex clinical situations. They also found that students with deep approach tend to achieve higher performance and vice versa.
While it is comforting that majority of the medical students preferred deep and strategic learning approaches (Subasinghe & Wanniachchi, 2009; Shankar et al., 2014; Reid et al., 2012; Shankar et al., 2005), Amini et al., (2012) and Aaron and Skakun (1999) found their medical students were more inclined towards the surface learning approach. Cecebi et al. (2013) found that their third year medical students preferred surface learning compared to the first and second year, suggesting the possibility of a waning interest in the deep learning approach as students progress through medical school. Being aware of our medical students’ predominant learning approaches in order to shift them to move towards more effective learning approaches was an important endeavour.
In this age of advanced information technology, teaching methods have evolved to meet the opportunities and challenges in undergraduate medical education (S.O. Ekenze, Okafor, O. S. Ekenze, Nwosu, & Ezepue, 2017; Shelton, Corral, & Kyle 2017). Multimedia e-learning enhances both teaching and learning (Ruiz, Mintzer, & Leipzig, 2006). Videos are being utilised in higher education to deliver useful content that can engage students (Mitra, Lewin-Jones, Barrett, & Williamson, 2010). We used digital video as an intervention to engage our students to reflect on the three predominant learning approaches, so that they become aware of their own predominant learning approach and reassess their approach. The advantages of using a video is that it can be easily used in multiple locations, updates added as required, short time frame to deliver information and can be re-watched at any time convenient to the audience.
This study aimed (i) to evaluate the learning approaches of medical students in Singapore, (ii) to assess if a video digital media intervention is effective in introducing the idea of ‘surface’, ‘strategic’ and ‘deep’ learning approaches and whether any change in that approach resulted.
II. METHODS
A. Participants
The study population comprised 351 Singaporean medical students from SingHealth who attended the Obstetrics and Gynaecology (O&G) clinical rotation a SingHealth from March 2015 to January 2017.
B. Study Design
We used the Approaches and Study Skills Inventory for Students (ASSIST) questionnaire (see Appendix) to assess the students’ learning approaches at the beginning and the end of the students’ O&G posting in SingHealth (Figure 1).
The ASSIST questionnaire is a revised version of the Approaches to Studying Inventory (ASI), developed by Tait, Entwistle and McCune (1998). The questionnaire has been validated in various cultures globally, including amongst eastern cultural population such as Chinese university students and also across the western student population in Britain and Scotland (Gadelrab, 2011; Albedin, Jaarfar, Husain, & Abdullah, 2013). The ASSIST questionnaire comprises of 52 questions divided into 13 subscales of 4 questions. Each questions is scored on a five-point Likert scale (1 for “low” through 3 for “average” to 5 for “high”), with 16 questions pertaining to surface and deep learning each and 20 questions relating to strategic learning. An example of a question assessing deep approach is “I try to relate ideas I come across to those in other topics or other courses whenever possible.”; strategic approach is “I think I’m quite systematic and organised when it comes to revising for exams.”; and surface approach is “I find I have to concentrate on just memorising a good deal of what I have to learn.” The scores for sets of 4 were combined into 13 subscales and further grouped to give each respondent a score for deep, strategic and surface approach. The predominant learning approach is defined as the approach which has the highest mean score amongst the three approaches. The predominant learning approach is calculated based on the mean of the respective questions for each of the three learning approaches.
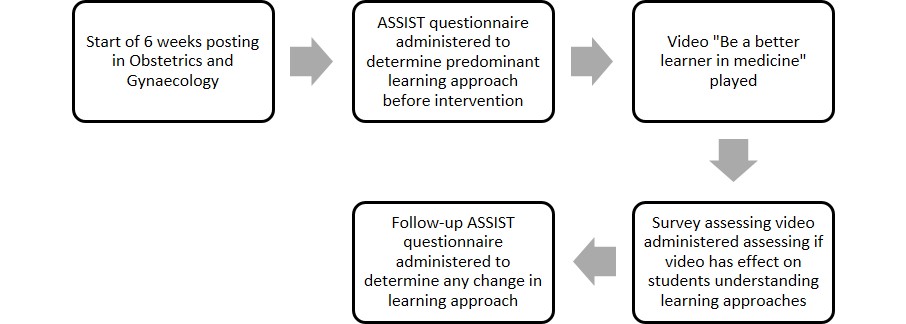
Figure 1. An illustration of the study design – Beginning with the administration of ASSIST questionnaire, to the video intervention and the follow-up ASSIST questionnaire again to determine any change in learning approach
After completing the first questionnaire the same group of students were shown a video (Chonkar et al., 2018) entitled, “Be a better learner in medicine”, featuring three students. The video provided an introduction to three learning approaches and a description of these approaches. It then illustrated how learners adopting the three learning approaches would react and respond in three different scenarios in the context of learning the management of an high risk obstetrics condition: a normal tutorial, when studying in their own time and when being assessed during a test. As outlined by Rondon-Berrios and Johnston (2016), there are multiple techniques of successful teaching in a clinical environment including, role modelling and pattern recognition. The video capitalises on these two techniques to show how students who adopted these three different learning approaches would usually behave and illustrated the outcomes at the end of the video.
In the first scenario of the video, the student who adopted the surface learning approach decided to memorise information about the high-risk obstetric conditions from sources such as handbooks and lecture notes. There was no attempt to understand the basic pathophysiology of the condition or the underlying principle of management. The second student who adopted the strategic approach, used resources like important literature highlighted by the tutor and past year questions for targeted preparation to perform well in the final exam. There were attempts in clinical reasoning while managing the obstetric high risk condition. The student did not spend enough time to thoroughly understand underlying principles of management of medical disorder in pregnancy but rather selectively spent time studying selected topics which were deemed to be important. The deep learner went in depth to understand the basic pathophysiology and systematically approached the management with clinical reasoning with respect to stages of pregnancy that the patient could be in for that obstetric condition. The student further understood the critical aspect of the underlying principle of management of obstetric high risk conditions i.e. trying to balance the risks of prematurity due to early delivery versus the risks of continuing pregnancy endangering the mother and foetus, which can be applied to almost all other obstetric conditions. The student in the third scenario equipped herself by applying this underlying principle to other obstetric high-risk conditions when studying.
The final scene depicted the three students attempting their final posting examination. The surface learner experienced ‘brain freeze’ with clinical reasoning and was unable to remember the facts. The student adopting the strategic approach was able to apply some clinical reasoning to the question which she had previously identified to be important from examination point of view but did not do so well when another condition that was tested was not in her ‘radar screen’ of topics. The student who adopted the deep learning approach was able to apply correct clinical reasoning and underlying obstetrics principles to both obstetric conditions tested, even though one of the conditions was not familiar to her yet she was able to answer well. The video ended with a summary of the three learning approaches and the importance of adopting a non-surface learning approach to enhance learning and retention of knowledge.
A survey containing five relevant questions was conducted with answers on a 5-point Likert scale to assess if video was effective in helping students understand the three learning approaches and reflect on their own approach. The survey explored if students were willing to change their learning approach to a more favourable one. Positive response was then defined as those responses that were rated a 4 or 5 (Agree/Strongly Agree), Neutral response was those rated as 3 and Negative response was those rated as 1 or 2 (Disagree/Strongly Disagree).
C. Statistical Analyses
The data were analysed using Microsoft Excel program and Statistical Package for Social Sciences (SPSS) version 22. Scores were aggregated pre- and post-intervention. The differences between the mean scores from ASSIST questionnaire administered pre- and post-intervention were analysed using Mann-Whitney test for standard deviation and p-value significance. Significant p-value was taken as p<0.05 in this study.
III. RESULTS
A total of 351 students completed the pre-video ASSIST questionnaire. Six students were unavailable to complete the ASSIST questionnaire at the end of the posting. The demographic characteristics of the 345 medical students are listed in Table 1.
A. Type of Predominant Learning Approach Pre and post-video intervention
As seen in Table 2, more students adopted the deep learning approach prior to the beginning of the rotation (Deep 54.4% vs Surface 12.0% vs Strategic 33.6%). After 6-weeks of rotation in O&G, the strategic learners increased from 33.6% to 41.4%. The surface learners decreased from 12.0-9.0% and the deep learners decreased from 54.4% to 49.6%.
Further analysis of the pre- and post-intervention scores of the ASSIST questionnaire actually showed that only the increased in strategic learners was statistically significant. The decrease in the numbers of deep and surface learners was both statistically insignificant (Table 3).
| Characteristics of medical students | Numbers (%) |
| Total number of students | 345 |
| Average age , years (range) | 23 (21-35) |
| Sex | |
| – Male, n (%) | 152 (44.1) |
| – Female, n (%) | 193 (55.9) |
| Race | |
| – Chinese, n (%) | 314 (91.0) |
| – Non-Chinese, n (%) | 31 (9.0) |
| Nationality | |
| – Singaporean, n (%) | 316 (91.6) |
| – Non-Singaporean, n (%) | 29 (8.4) |
| Medical School | |
| – Yong Loo Lin School of Medicine, n (%) | 275 (79.7) |
| – Duke-NUS, n (%) | 70 (20.3) |
Table 1. Demographic characteristics of medical students
| Predominant Learning Approach | No. of students at the beginning of rotation (%) | No. of students after 6-weeks rotation (%) |
| Surface | 42 (12.0) | 31 (9.0) |
| Strategic | 118 (33.6) | 143 (41.4) |
| Deep | 191 (54.4) | 171 (49.6) |
| Total no. of students | 351 | 345 |
Table 2. Predominant learning approach adopted by students at the beginning and the end of 6-weeks rotation
| Predominant learning approach | Mean score at the beginning of posting | Mean score at the end of posting | Standard deviation | p-value |
| Surface | 62.6 | 61.4 | 11.1-11.7 | 0.060 |
| Strategic | 72.7 | 74.6 | 9.94-11.0 | 0.014 |
| Deep | 74.8 | 75.9 | 8.9-10.8 | 0.120 |
Table 3. The change in of the mean aggregate scores of ASSIST questionnaire for the various predominant learning approaches at the beginning and the end of 6-weeks rotation, after the video intervention
| Video Survey Questions | Negative response
(%) |
Neutral
response (%) |
Positive response
(%) |
| The learning approaches explained in the video were clear | 1(0.3) | 19(7.0) | 249(92.0) |
| The video was engaging | 18(6.6) | 58(21.5) | 193(71.0) |
| The duration of the video was just right | 24(8.9) | 44(16.3) | 201(74.7) |
| I was able to reflect on my predominant learning approach after watching the video | 7(2.6) | 28(10.4) | 234(86.9) |
| I am more likely to adopt the non-surface learning approach after viewing the video | 16(5.9) | 52(19.3) | 201(74.7) |
Table 4. Participants’ response to survey on video “Be a Better Learner in Medicine”
B. Participants’ Response to Survey on Video “Be a Better Learner in Medicine”
The video survey was completed by a total of 269 students. As seen in Table 4, 249 (92.0%) students thought the learning approaches explained in the video were clear, 234 (86.9%) students agreed the video helped them reflect on their predominant learning approach and 201 (74.7%) admitted that they are more likely to adopt non-surface learning approach after viewing the video. The video was found to be engaging by 193 (71.0%) students and 201 (74.7%) students thought that the duration of the video was just right.
C. Qualitative Feedback on the Video “Be a Better Learner in Medicine”
There were many qualitative comments from the students who completed the survey. There were 95 comments expressing positive views, 21 comments expressing negative views and 4 neutral comments with respect to the video depicting the learning approaches.
Some of the positive comments were “It is a more useful tool and approach to learning”, “I feel inspired by the video”, “Video illustration is helpful to elaborate different types of learner”, “The video made me reflect a little on how I learn”, “Likes the way the video brings the idea of deep learning” and “Good video to stimulate thinking on learning method”.
Addition examples of positive comments were “I feel that my own approach has been ineffective and I want my learning to improve”, “Recognise how important it is to adopt deep learning”, “It shows that my current learning method is inadequate and it shows how I should work on it”, “It is clear that deep learning allows students to learn from principle”, “I think it is important and useful to understand what we’re learning and apply it in new scenarios or situations”, “Deep is better approach with longer retention & understanding eventually beneficial to future patients.”
Some of the negative comments were “Ideally, deep approach is desirable but due to a lack of time, sometimes surface approach can be more time effective as temporary stop-gap measure”, “The amount needed to study and time needed to be a deep learner is a deterrent”, “May not have the luxury of time. (Deep learning requires a lot of time)”, “Time constraint”, “Sometimes deep learning takes time, and the short time we are given to study may push students more towards strategic thinking.”
IV. DISCUSSION
Medical students have to retain large amounts of information and at the same time have to keep themselves abreast with the latest research. The students also need to cope with heavy workloads and tight course schedules in medical school while struggling to understand and retain information with good time management skills being essential. Our study found that the majority of our students adopted the deep approach as their predominant learning approach (54.4%) followed by the strategic approach (33.6%) prior to the intervention. It is heartening to note that surface learning approach was the least preferred approach adopted by our medical students. While encouraging, there was still a substantial proportion (12%) of medical students who adopted surface learning approach as their predominant learning approach. With the rapidly advancing medical sciences, students may not have enough time to see, read and assimilate all necessary information before their assessments. This may force some of the slow learners to adopt the surface learning approach. Some students commented that surface learning approach could be adopted easily as a temporary measure due to time constraints. This might explain why 12% of medical students adopted predominantly surface learning approach in our study, and those students who were more inclined towards surface learning approach in previous studies (Aaron & Skakun, 1999; Cebeci et al., 2013; Amini et al., 2012).
After the video intervention, we noted a decrease in the surface learning approach and an increase in the strategic learning approach. As reflected in Table 3, the mean score of surface learning decreased from 62.6 to 61.4 (p=0.06.) and that of strategic and deep learning approaches increased (strategic – 72.7 to 74.6, p=0.014; deep 74.8-75.9, p = 0.120). Though this decrease in surface learning approach and increase in deep learning approaches were not statistically significant, these results reflected the potential for digital media (in the form of a video) to effect a change in the students’ learning approaches. As depicted in the qualitative comments in the video survey, some students stated that time constraint was an important factor that prevented students from adopting deep approach. The increase in strategic learning approach may be due to the need for students to pass certain assessments at the end of posting examination, as required by their schools and clerkship. A number of students had commented that adoption of strategic learning approach helped them achieve good outcomes during assessments. The students might have felt that adopting the strategic approach would be more expedient by selecting and studying the important topics amongst the intensive curricular topics and that might help them do well in a short period of attachment. The packed shortened curriculum may influence approaches to learning as evidenced from the comments in this study.
The tool used to assess students’ learning approach – ASSIST questionnaire also posed some limitations for this study. Despite the ASSIST questionnaire being validated in many cultures and, it may not fully be reflective of the true approach to learning of students, especially if they answered the questions in a way that they thought would have been the approved answers (Reid et al., 2012). In addition, ASSIST questionnaire is a self-rated tool, so the results are subjective. There may be greater awareness and a change in the students’ perception towards their learning approaches after watching the video illustrating how adopters of the various learning approaches would behave. This would have affected the results of the ASSIST questionnaire.
The video helped raise awareness of various learning approaches and engage students to reflect and reassess their predominant learning approach. The number of students adopting non-surface learning approach increased after watching the video. There is a potential to discourage them from adopting surface learning approach as reflected in the qualitative feedback which showed that many became aware of the disadvantages of surface learning. A number of students were also convinced after the video that the surface learning approach was not favourable for them to retain a lot of information that they will need to use in clinical setting. While this was a good outcome, the difference was not statistically significant. Moreover, the video was just a short intervention of 12 minutes and not followed by further education or reinforcement of the appropriate learning approach throughout the posting. It is also difficult to change entrenched learning approach behaviour. In addition, most of the medical students are in their final few years of medical school, and have most likely been using their current learning approach successfully over the previous few years in medical school, and see no point in changing their learning approach. Other possible limitations include the small sample size of medical students who were involved in this study that have affected the results.
Multiple previous studies have found that many factors are involved in encouraging deep learning approach among medical students such as appropriate workload, clear goals with informative feedback and targeted assessments (Reid, Duvall, & Evans, 2005; Rushton, 2005). To facilitate deep learning, the curriculum can be adjusted to address these factors. Instead of factual overload, faculty can allocate more teaching time towards case-based scenarios and tutorials that focus on applying the understanding of pathophysiology, concepts and care management principles learned. This will aid students in tackling complex patient problems, a reality they will face when they become active practitioners. Smaller tutorial groups to focus on individualised targeted feedback after formative assessment may help in encouraging the usage of deep learning approach. The format of assessment can also be more encompassing, to reward understanding instead of pure memorising (Rushton, 2005).
The predominant deep and strategic learning approach is a reflection of self-motivation among medical students, which is inherent (Amini et al., 2012). But many students may not be aware of their own predominant learning approach and may not realize that they may adopt different approaches according to different circumstances. With the increase in the number of medical students and limited number of core faculty and time, finding a solution to encourage independent deep learning and discourage surface learning approach amongst our students would be beneficial in the long run, ensuring that students develop the most favourable learning approach from the start and keep honing this learning approach skill as they progress in their medical career.
Medical schools will also need to look into their curriculum and time-lines of individual clinical attachments periodically to ensure that they are able to deliver core knowledge without compromising on understanding of concepts. Perhaps, targeting students in their pre-clinical years and introducing the concept of various learning approaches would set a good foundation and aid in deeper learning during clinical years. Discouraging medical students from adopting surface learning approach would be beneficial in achieving expected long term goals and this would ultimate translate into higher quality education and patient care.
V. CONCLUSION
This study highlights the potential of digital media as an educational tool to enable medical students to become better learners (Gadelrab, 2011). With the use of a video, students were able to reflect on their predominant learning approaches, which is relevant with the evolving teaching andragogy that emphasises self-directed learning. The students were exposed to the potential pitfalls of adopting surface learning in the video and this likely encouraged some of the surface learners not to use surface learning approach, in order to better help them cope with the increasing need to apply strategic thinking, deep thinking and critical analysis during complex situations. This project can help spearhead efforts to optimize students’ learning, to move the medical education landscape forward.
Notes on Contributors
Sonali Chonkar, Melissa Lim and Kok Hian Tan conceived, designed the video script and the study. Melissa Lim acquired the data; Mor Jack Ng analysed and interpreted the data. Kok Hian Tan critically revised the article and gave invaluable inputs at every stage of writing and data acquisition/analysis. Tam Cam Ha and Hester Lau assisted in the revision and editing of the article.
Ethical Approval
The study was approved and given the exempt status by our institution’s Centralised Institutional Review Board of SingHealth (CIRB) committee. All students participated voluntarily and informed consent was obtained before participating in the study. The CIRB reference number for our study is 2013/232/D.
Acknowledgements
The authors would like to thank all medical students of NUS Yong Loo Lin School of Medicine, Duke-NUS Medical School and NTU Lee Kong Chian School of Medicine for participating in this joint study. We would like to thank Ms Mabel Yap from Duke-NUS Secretariat Office for her assistance in the research. We would like to thank Ms Hester Lau, Ms Tang Wan Chu, Ms Goh Jia Ying, Ms Amy Tan, Ms Alicia Lim and the staff of Division of Obstetrics & Gynaecology at KKH for the assistance in the production of the video.
Funding
This study was supported by a Teaching Enhancement Grant (TEG – AY 2014/2015) from NUS Centre for Development of Teaching and Learning.
Declaration of Interest
The authors declare that they have no competing interests.
References
Aaron, S., & Skakun, E. (1999). Correlation of students’ characteristics with their learning styles as they begin medical school. Academic Medicine, 74(3), 260-262.
Albedin, N. F. Z., Jaarfar, Z., Husain, S., & Abdullah, R. (2013) The Validity of ASSIST as a measurement of learning approach among MDAB students. Procedia – Social and Behavioural Sciences, 90, 549-557.
Amini, M., Tajamul, S., Lotfi, F., & Karimian, Z. (2012). A survey of study habits of medical students in Shiraz Medical School. Future of Medical Education Journal, 2(3), 28-34. https://doi.org/10.22038/fmej.2012.354.
Cebeci, S., Dane, S., Kaya, M., & Yigitoglu, R. (2013). Medical students’ approaches to learning and study skills. Procedia – Social and Behavioural Sciences, 93, 732-736. https://doi.org/10.1016/j.sbspro.2013.09.271.
Chonkar, S. P., Lau, H. C. Q., Tang, W. C., Goh, J. Y., Mohammad N. B, A., Lim M., & Tan H. K. (2018, September 18). Be a predominantly deep learner in medicine [Video file]. Retrieved from https://youtu.be/ttnSCoun_sA.
Ekenze, S. O., Okafor, C. I., Ekenze, O. S., Nwosu, J. N., & Ezepue, U. F. (2017). The value of internet tools in undergraduate surgical education: Perspective of medical students in a developing country. World Journal of Surgery, 41(3), 672-680. http://doi.org/10.1007/s00268-016-3781-x.
Entwistle, N. (1997). Contrasting perspectives on learning. In F. Marton, D. Hounsell & N. Entwistle (Eds.), The Experience of Learning: Implications for teaching and studying in higher education (3rd ed) (pp. 3-22). Retrieved from: http://www.docs.hss.ed.ac.uk/iad/Learning_teaching/Academic_teaching/Resources/Experience_of_learning/EoLChapter1.pdf.
Gadelrab, H. F. (2011). Factorial structure and predictive validity of approaches and study skills inventory for students (ASSIST) in Egypt: A confirmatory factor analysis approach. Electronic Journal of Research in Educational Psychology, 9(3), 1197-1218.
Leite, W. L., Svinicki, M., & Shi, Y. (2010). Attempted validation of the scores of the VARK: Learning styles inventory with multitrait–multimethod confirmatory factor analysis models. Educational and Psychological Measurement, 70(2), 323-339. https://doi.org/10.1177/0013164409344507.
Mitra, B., Lewin‐Jones, J., Barrett, H., & Williamson, S. (2010). The use of video to enable deep learning. Research in Post-Compulsory Education, 15(4), 405-414. https://doi.org/10.1080/13596748.2010.526802.
Newble, D. I., & Entwistle, N. J. (1986). Learning styles and approaches: Implications for medical education. Medical Education, 20(3), 162-175. https://doi.org/10.1111/j.1365-2923.1986.tb01163.x.
Reid, W. A., Evans, P., & Duvall, E. (2012). Medical students’ approaches to learning over a full degree programme. Medical Education Online, 17(1), 17205-17211. http://dx.doi.org/10.3402/meo.v17i0.17205.
Reid, W. A., Duvall, E., & Evans, P. (2005). Can we influence medical students’ approaches to learning? Medical Teacher, 27(5), 401-407. https://doi.org/10.1080/01421590500136410.
Rondon-Berrios, H., & Johnston, J. R. (2016). Applying effective teaching and learning techniques to nephrology education. Clinical Kidney Journal, 9(5), 755-762. http://doi.org/10.1093/ckj/sfw083.
Ruiz, J. G., Mintzer, M. J., & Leipzig, R. M. (2006). The impact of e-learning in medical education. Academic Medicine, 81(3), 207-212.
Rushton, A. (2005). Formative assessment: A key to deep learning? Medical Teacher, 27(6), 509-513. https://doi.org/10.1080/01421590500129159.
Samarakoon, L., Fernando, T., & Rodrigo, C. (2013). Learning styles and approaches to learning among medical undergraduates and postgraduates. BioMed Central Medical Education, 13(1), 42-47. https://doi.org/10.1186/1472-6920-13-42.
Shah, D. K., Yadav, R. L., Sharma, D., Yadav, P. K., Sapkota, N. K., … Islam, M. N. (2016). Learning approach among health sciences students in a medical college in Nepal: A cross-sectional study. Advances in Medical Education and Practice. 7, 137-143. https://doi.org/10.2147/AMEP.S100968.
Shankar, P. R., Balasubramanium, R., & Dwivedi, N. R. (2014). Approach to learning of medical students in a Caribbean medical school. Education in Medicine Journal, 6(2), e33-40. https://doi.org/10.5959/eimj.v6i2.235.
Shankar, P. R., Dubey, A. K., Binu, V. S., Subish, P., & Deshpande, V. Y. (2005). Learning styles of preclinical students in a medical college in western Nepal. Kathmandu University Medical Journal, 4(3), 390-395.
Shelton, P. G., Corral, I., & Kyle, B. (2017). Advancements in undergraduate medical education: Meeting the challenges of an evolving world of education, healthcare, and technology. Psychiatric Quarterly, 88(2), 225-234. https://doi.org/10.1007/s11126-016-9471-x.
Subasinghe, S. D. L. P., & Wanniachchi, D. N. (2009). Approach to learning and the academic performance of a group of medical students – Any correlation. Student Medical Journal, 3(1), 5-10.
Tait, H., Entwistle, N. J., & McCune, V. (1998). ASSIST: A reconceptualisation of the approaches to studying inventory. In C. Rust (Ed.), Improving student learning: Improving students as learners. Oxford: Oxford Brookes University, The Oxford Centre for Staff and Learning Development.
Trigwell, K., & Prosser, M. (1991). Improving the quality of student learning: The influence of learning context and student approaches to learning on learning outcomes. Higher Education, 22(3), 251-266. https://doi.org/10.1007/BF00132290.
Wickramasinghe, D. P., & Samarasekera, D. N. (2011). Factors influencing the approaches to studying of preclinical and clinical students and postgraduate trainees. BioMed Central Medical Education, 11(1), 22-28. https://doi.org/10.1186/1472-6920-11-22.
*Sonali Prashant Chonkar
Address: KK Women’s and Children’s Hospital,
100 Bukit Timah Road
Singapore 229899
E-mail: sonali.chonkar@kkh.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









