A tiered mentorship framework in an Orthopaedic Surgery Residency Programme
Published online: 7 January, TAPS 2020, 5(1), 54-60
DOI: https://doi.org/10.29060/TAPS.2020-5-1/OA2095
Min Jia Chua1, Gen Lin Foo2 & Ernest Beng Kee Kwek2
1National Healthcare Group, Ministry of Health Holdings, Singapore; 2Department of Orthopaedic Surgery, Woodlands Health Campus, Singapore
Abstract
Introduction: Mentoring is a vital component of a well-rounded medical teaching environment, as evidenced by its implementation in many residency programmes. This study aims to evaluate the perceived value of mentoring by faculty and near-peer mentoring to the orthopaedic surgery resident.
Methods: An online survey comprising multiple choice questions and scaled-response questions with a few open-ended questions was created and distributed to all residents, from residency years 2 to 5, within an orthopaedic residency programme in Singapore to gather their views on a tiered mentorship programme.
Results: 100% of surveyed residents responded. 68.4% of junior residents had a senior resident mentor while 84.8% of all residents had a faculty mentor. Junior residents generally viewed senior resident mentors as being crucial and beneficial for training, with scores comparable to those for faculty mentors. Residents who had mentors, in particular those who had chosen their own mentors, tended to be more satisfied than their counterparts. The most desired characteristics of mentors among the residents included approachability, willingness to share, being able to give feedback and experience. 66.7% of residents felt that near-peer mentorship should be required in the residency programme but only 30.3% of them felt that it should be formalised. 78.8% of residents surveyed felt that mentorship by faculty was required.
Conclusion: Residents viewed mentoring by faculty and near-peer mentoring as being beneficial and crucial to their orthopaedic residency training. We propose that an ideal mentoring programme should be tiered, allow choice of mentors and include near-peer mentoring as a requirement but not necessarily monitored.
Keywords: Orthopaedic Surgery, Resident Education, Mentoring, Medical Teaching, Tiered Mentorship
Practice Highlights
- Study to evaluate value of mentoring by faculty and near-peer mentoring to orthopaedic surgery resident.
- Residents viewed mentoring by faculty and near-peer mentoring programmes as being beneficial and crucial.
- Ideal mentoring programme should be tiered and allow choice of mentors.
- Near-peer mentoring should be a requirement but not necessarily monitored.
I. INTRODUCTION
Mentoring has long been a crucial element of effective resident medical education (Sambunjak, Straus, & Marusic, 2006), with many programmes adopting mentoring by faculty as an integral component of their residency programme. Various models of mentoring and types of mentoring activities have been described including didactic sessions, regular mentor-mentee meetings and group projects (Kashiwagi, Varkey, & Cook, 2013). The benefits of mentoring have also been shown in various studies, by aiding personal and professional development during residency, helping with
career preparation (Ramanan, Taylor, Davis, & Phillips, 2006), improving professional and social skills (increased self-confidence, improved communication skills; Buddeberg-Fischer, & Herta, 2006).
There is however, little data looking at how Orthopaedic residents view mentorship programmes (Flint, Jahangir, Browner, & Mehta, 2009). Furthermore, most studies look at mentoring by faculty with little emphasis on near-peer mentoring. In fact, a literature review has shown that no studies have looked at and compared the two entities in orthopaedic residency programmes.
In our residency programme, a tiered mentorship framework, where both mentoring by faculty and near-peer mentoring are practised, has been in place since 2014. In the former, a mentor of associate consultant grade and above who is in post-fellowship training will mentor a resident while in the latter, a senior resident mentor will mentor a junior resident two residency years below him or her.
The objective of having a near-peer mentorship framework in our programme was to bridge some of the gaps in traditional mentorship. In mentorship by faculty models, there will inevitably be hierarchical distance between mentors and mentees and residents may not feel as at ease approaching their mentors for certain issues. Furthermore, there may be a shortage of faculty members who are also strapped for time and may not be able to devote enough time for holistic mentorship of residents. These mentors are also further away from their residency training years and may not be able to understand some of the issues their mentees face in the current residency climate. It was envisaged that senior residents who are near-peers on the ground will be able to address some of the abovementioned shortcomings in the traditional mentorship model.
Currently, mentorship by faculty is formally monitored by the programme and mandates at least bi-annual meetings with a mentoring form to be filled in while near-peer mentorship is a self-directed initiative by the residents which is more informal with no stipulated frequency of meetings and no compulsory documentation under the residency programme requirements.
Residents were either assigned mentors or chose mentors at the start of the second year of their residency but due to various factors including efflux of faculty mentors or other administrative reasons, some residents do not have either senior resident or faculty mentors or both.
The objectives of this study were to 1) evaluate the orthopaedic surgery residents’ perception of mentoring by faculty and near-peer mentoring and 2) establish factors perceived as being important in mentors and a successful mentoring environment.
II. METHODS
An anonymised online survey with voluntary participation was administered to all orthopaedic surgery residents, from residency years 2 to 5 (R2 to R5), in our orthopaedic surgery residency programme. No identifiers were collected to ensure protection of the privacy of survey respondents. The choice of survey as the tool was to maximise response rates without compromising on data collection through comprehensive survey questions. There were two sets of questions evaluating the residents’ perception of mentoring by faculty and near-peer mentoring. The near-peer mentoring questions differed depending on whether the resident was a senior or junior resident and whether the resident possessed a mentee or mentor respectively. The mentoring by faculty questions varied depending on the presence of a mentor. The survey questions presented to the respondent were modified real-time based on their initial answers to the previous questions, hence eliminating questions which were not relevant.
These survey questions were adapted from a census survey conducted by the American Academy of Orthopaedic Surgeons (Flint et al., 2009) on residents with regard to their experience in, and opinion of mentorship programmes and the prevalence of such programmes.
The questions administered were largely multiple-choice questions and scaled-response questions with a few open-ended questions. The multiple-choice and scaled-response questions covered the characteristics and perception of the mentoring environment (including how beneficial and crucial they found the mentoring programme, their satisfaction with the programme, their ideal mentorship framework, etc.), the perception of the value of mentoring (for instance to what extent they felt it supported their educational experience, aided with networking and making career decisions) and the characteristics of an ideal mentor. For the scaled response questions, respondents were asked to rate the importance of and their satisfaction with the different facets of their mentoring experience or environment on a scale ranging from 1 to 5.
The open-ended section of the survey allowed residents to air what they had achieved or hoped to achieve through the mentorship programme as well as general comments about the programme and suggestions for improvement.
Standard institutional review board procedures were followed and ethics board approval was obtained. Data analysis was performed using SPSS.
III. RESULTS
The survey was administered to a total of 33 residents across the residency batches from R2 to R5 in the residency year, with a response rate of 100%. Of the respondents, 19 were junior residents (8 R2 and 11 R3) and 14 were senior residents (6 R4 and 8 R5).
Of the junior residents, 68.4% (13/19) of them had senior residents while 78.6% (11/14) of the surveyed senior residents had junior resident mentees, with two of the senior residents having two junior resident mentees. 84.8% (28/33) of surveyed residents had faculty mentors (further details in Table 1).
| Residency year | Number with faculty mentors | Number without faculty mentors | Number with SR mentors (R2 and R3) or mentees (R4 and R5) | Number without SR mentors (R2 and R3) or mentees (R4 and R5) |
| R2 | 6/8 (75%) | 2/8 (25%) | 7/8 (87.5%) | 1/8 (12.5%) |
| R3 | 11/11 (100%) | 0/11 (0%) | 6/11 (54.5%) | 5/11 (45.5%) |
| R4 | 3/6 (50%) | 3/6 (50%) | 4/6 (66.7%) | 2/6 (33.3%) |
| R5 | 8/8 (100%) | 0/8 (0%) | 7/8 (87.5%) | 1/8 (12.5%) |
Table 1. Breakdown of residents with faculty and senior resident (SR) mentors/mentees
Of the junior residents with a senior resident mentor, 53.8% (7/13) of them chose their own mentors while the rest had their mentors assigned. Of the residents with a faculty mentor, 60.7% (17/28) of them chose their own mentors. 69.2% (9/13) of junior residents met up with their senior resident mentors at least twice a year while 82.1% (23/28) of residents met up with their faculty mentors at least half-yearly or more frequently.
It was found that junior residents viewed senior resident mentors as being moderately beneficial and crucial to their training, with average scores of 3.92 on a scale of 1 to 5 (Figure 1). Of note, it was found that residents with senior resident mentors viewed near-peer mentorship as being more crucial and beneficial compared to their counterparts without senior resident mentors. Similar results were also echoed by the residents regarding their faculty mentors, with average scores of 3.89 and 4.14 for how crucial and beneficial faculty mentors were to residents with mentors and average scores of 3.6 and 4.0 for residents without mentors.
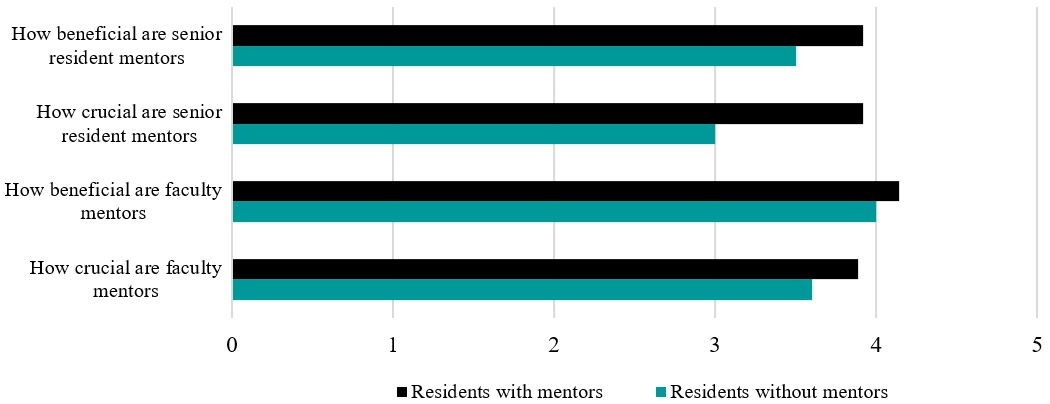
Figure 1. Chart showing how crucial and beneficial residents viewed senior resident and faculty mentors
In terms of satisfaction levels with the mentoring programme, residents with mentors (senior resident and faculty mentors) were also more satisfied with the mentoring programme than their peers without mentors, with average scores of 4.31 and 4.33 for residents with senior and faculty mentors respectively compared to average scores of 3.75 and 4.00 for residents without senior and faculty mentors.
A further subgroup analysis yielded that respondents with a self-selected mentor from both the senior resident and faculty mentor groups had higher scores for satisfaction levels (4.28 and 4.41 respectively) compared to those who had assigned mentors (4.16 and 4.20). Those with self-selected mentors in the faculty mentor group also felt that their mentor aided them more in supporting their educational experience and in making career decisions.
84.6% (11/13) of junior residents who had a senior resident mentor felt that their senior resident mentor was able to provide them with advice about career, employment, or difficult cases in the future while 89.3% (25/28) of residents with faculty mentors felt the same about their faculty mentors.
In terms of desired characteristics in a senior resident mentor, approachability, willingness to share and experience were the top three most desired characteristics (Figure 2A). Similar results were echoed in the results for faculty mentors, with ability to give feedback also highly valued (Figure 2B).
66.7% (22/33) of all residents felt that near-peer senior resident mentoring should be required in the resident programme but only 30.3% (10/33) thought that it should be formalised. Some of those who felt that near-peer mentoring should not be required expressed that they would like it to be up to the individual resident and that residents who are in need would approach senior residents directly of their own accord. 78.7% (26/33) of residents surveyed were of the opinion that faculty mentorship by faculty was required. Those who felt that faculty mentorship should not be required offered reasons including the hectic schedule of consultants and the unpredictable flow of faculty members into the private practice which would make it difficult for residents to maintain the same mentor throughout residency training.
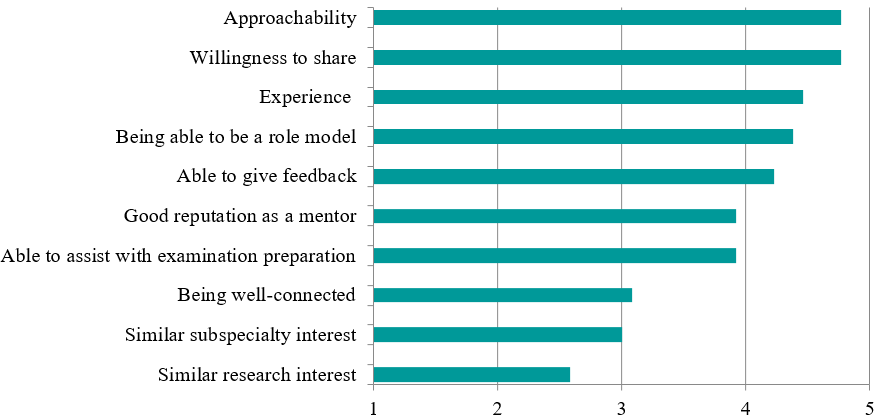
Figure 2A. Chart depicting the desired characteristics scores in senior resident faculty mentors, ranked from most to least desired
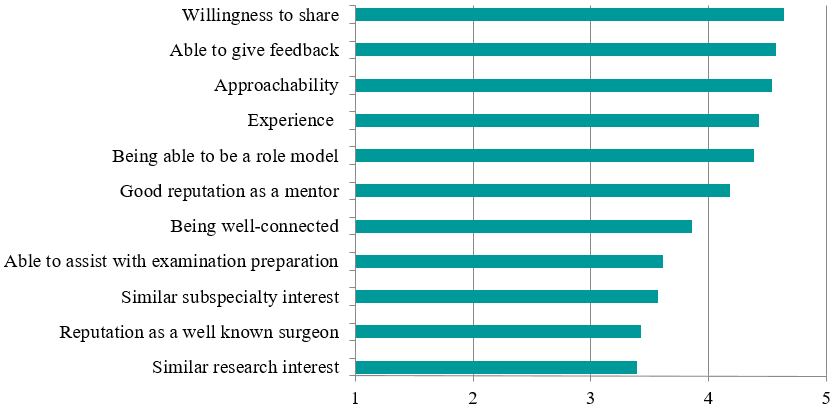
Figure 2B. Chart depicting the desired characteristics scores in faculty mentors, ranked from most to least desired
IV. DISCUSSION
Traditionally, the art of medicine and especially surgery has been passed down through an apprenticeship model (Gofton & Regehr, 2006). Multiple studies have shown that various aspects such as career paths, research output as well as personal development can be influenced greatly by mentorship (Calligaro, Dougherty, Sidawy, & Cronenwett, 2004; Gedde, Budenz, Haft, Lee, & Quigley, 2007). In fact, close to 80% of paediatric residents polled in a survey gave feedback that having a mentor was either very useful or crucial to survival during their residency years (Curtis, Adam, & Shelov, 1995). Over 20 years later, it appears that little has changed, with similar results being echoed in our study, with high scores reported for how crucial and beneficial faculty and senior resident mentorship was viewed as being by residents.
There are myriad challenges which one will face when mentoring orthopaedic residents. In comparison to teaching medical students, teaching an orthopaedic resident is often longer, more intense and calls for greater responsibility for teaching while compared to fellowship training (post-residency for subspecialty training); the mentor is teaching a much less knowledgeable and skilled protégé (Levine, Braman, Gelberman, & Black, 2013). There is hence an enhanced requirement for timely provision of feedback and assessment, and for nurturing the resident through his or her years of training. As Hill and Boone (2002) mentioned in their paper, mentoring aims “to provide a young aspiring professional with a tangible and immediate role model”. (p. 73)
For successful mentoring to occur, it requires reciprocity and has to be a “collaborative learning relationship” (Bland, Taylor, Shollen, Weber-Main, & Mulcahy, 2009). Levine et al. (2013) proposed certain obligations for a mentee to fulfil to maintain the mentor-mentee relationship and enhance the likelihood of success, including demanding and accepting feedback, seeking opportunities for self-improvement, following through, being prepared, requiring accountability, and more.
For the mentors, some traits which have been viewed as being important by surgical trainees include enthusiasm for the practice of surgery, commitment to excellence, good surgical technique, good leadership qualities, integrity and professionalism (Healy, Glynn, Malone, Cantillon, & Kerin, 2012). Certain more desirable traits of mentors which we have noted in our study include approachability, willingness to share and impart knowledge, experience as well as ability to give feedback. A mentor who has these traits will be better equipped to pass on his knowledge and skills to his mentee and hence provide a more well-rounded learning environment for the resident.
Nevertheless, we understand that mentoring is no mean feat and hence, it is recommended that both faculty members and senior residents take it upon themselves to train specific skill sets and develop desirable traits for mentoring which will enable them to successfully take on this mantle of responsibility. Mentoring workshops have been shown to improve mentoring competency and thereby improve outcomes for optimally mentored mentees (Lau et al., 2016; Gandhi & Johnson, 2016).
Our study also found that residents with self-selected mentors had higher satisfaction with the mentoring programme and felt that these mentors were able to support them more in their educational experience and making career decisions, a finding echoed in other studies (Yamada, Slanetz, & Boiselle, 2014). We postulate that this is because residents who selected their own mentors would be able to choose mentors who had desirable traits and whom they saw as ideal role models or were like-minded in their approach. Mentees have been shown to select role models—partners with whom they enjoy working and often report a mutual attraction or chemistry that sparks the development of the relationship (Kram, 1983).
As previously alluded to, mentoring by faculty is practised in many institutions and residency programmes but near-peer mentoring is often overlooked. The original intent of having a tiered mentorship framework in our programme was to ensure a holistic approach to mentoring of residents. It was envisioned that the senior resident mentor would be able to help ease the junior resident into the training programme and deal with immediate junior-level issues as well as assist in intermediate examination preparation while the senior faculty mentors would be able to provide a more overarching view as well as guidance and career advice. In the literature, it was found that mentees were generally less intimidated by near-peer mentors, felt they could relate better to them, and the near-peers understood them better as they had recently gone through situations they (the mentees) were now facing (Akinla, Hagan, & Atiomo, 2018). It was also shown that near-peer mentoring was a way of promoting professional and personal development, aid transition and maintain well-being of mentees (Akinla et al., 2018).
Residents in our programme were generally of the opinion that tiered mentorship was necessary but that near-peer mentoring should be informal, without any stipulated frequency of meetings, documentation of meetings and forms to fill up unlike mentoring by faculty. This is likely because senior residents are usually just a few years senior to the junior resident and both the mentors and mentees prefer a more informal environment and style of mentoring. This also enables junior residents to be more at ease to freely discuss any issues with the senior resident mentor. Furthermore, both the senior and junior residents have far more opportunities for interaction compared to the faculty mentor and the resident.
In the survey administered, aside from the previously mentioned results, we have also found that near-peer mentoring has positive effects on both the mentor as well as the mentee, with mentees commenting that senior resident mentors could provide pertinent directions as they started junior residency. Similarly, senior resident mentors felt that senior resident mentorship gave them an avenue to provide guidance and encouragement to their juniors, to allow them to benefit from past mistakes and to learn more efficiently. Furthermore, a tiered mentoring system contributes to a positive learning environment, creating a culture of camaraderie amongst seniors and juniors, resulting in a more closely-knit professional community.
Our residency programme encompasses both senior resident and faculty mentoring with the details on its implementation in our programme covered above. Moreover, it is the first to look at tiered mentoring and its impact on residents in orthopaedic surgery, with a 100% response rate among residents in our programme.
However, we acknowledge that this study does have some limitations. The first is that of the small sample size, which contributed to many of the variables being studied not having a statistically significant difference. Though we are limited by the small sample size due to the number of residents in the programme, we were able to achieve a high response rate as well as sub-divide the residents based on other variables including presence of a mentor and method of selection of mentor to allow for comparison between different groups. Other limitations include the fact that this study was only carried out in one institution which practised said model of mentorship. In addition, the mentorship programme had only been in place for two years when the survey was administered and its effects may not have been that far-reaching and apparent given the relatively short period of implementation, though this could form the basis for a longitudinal study in the future at further time points.
Future studies should be undertaken in the future to explore this field further. Studies involving various institutions which practice this model could be considered. Another area of study could be to look at objective measures like the Orthopaedic In-Training Examination and clinical rotation scores, exit examination success percentages and more. This would allow us to find out the tangible measurable effects that mentoring has on residents.
V. CONCLUSION
In conclusion, our study has found that mentoring by faculty and near-peer mentoring programmes are generally viewed as being beneficial and crucial to residency training and we believe that programmes should consider instituting tiered mentorship to reap the benefits.
We propose that an ideal mentoring environment should be 1) one that is tiered (encompassing both mentoring by faculty and near-peer mentoring), 2) a system that allows residents to choose their mentors, and 3) have near-peer mentoring as a required part of residency but on a more informal basis.
Notes on Contributors
Dr Chua Min Jia is a senior resident in orthopaedic surgery at the National Healthcare Group. He was involved in devising of the survey questionnaire, data collection and analysis and was the primary author of this manuscript.
Dr Foo Gen Lin is an associate consultant in the Department of Orthopaedic Surgery at the Woodlands Health Campus in Singapore. He was involved in devising of the survey questionnaire and editing of the manuscript.
Dr Ernest Kwek Beng Kee is a senior consultant and Chief of the Department of Orthopaedic Surgery at the Woodlands Health Campus in Singapore. He was involved in devising of the survey questionnaire, editing and approval of the final manuscript as well as overall supervision of the project.
Ethical Approval
This study was exempted by the National Healthcare Group Domain Specific Review Boards (DSRB).
Acknowledgement
The authors wish to thank all the orthopaedic surgery residents in our programme who participated in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Interest
There is no conflict of interest to declare.
References
Akinla, O., Hagan, P., & Atiomo, W. (2018). A systematic review of the literature describing the outcomes of near-peer mentoring programs for first year medical students. BMC Medical Education, 18(1), 98.
Bland, C. J., Taylor, A. L., Shollen, S. L., Weber-Main, A. M., & Mulcahy, P. A. (2009). Faculty success through mentoring: A guide for mentors, mentees, and leaders. New York, NY: Rowman & Littlefield Education.
Buddeberg-Fischer, B., & Herta, K. D. (2006). Formal mentoring programmes for medical students and doctors – A review of the Medline literature. Medical Teacher, 28(3), 248-257.
Calligaro, K. D., Dougherty, M. J., Sidawy, A. N., & Cronenwett, J. L. (2004). Choice of vascular surgery as a specialty: Survey of vascular surgery residents, general surgery chief residents, and medical students at hospitals with vascular surgery training programs. Journal of Vascular Surgery, 40(5), 978-984.
Curtis, J. A., Adam, H., & Shelov, S. P. (1995). A formal mentoring program in a pediatric residency. Academic Medicine, 70(5), 453-454.
Flint, J. H., Jahangir, A. A., Browner, B. D., & Mehta, S. (2009). The value of mentorship in orthopaedic surgery resident education: The residents’ perspective. Journal of Bone and Joint Surgery America, 91(4), 1017-1022.
Gandhi, M., & Johnson, M. (2016). Creating more effective mentors: Mentoring the mentor. AIDS and Behavior, 20(Suppl 2), 294-303.
Gedde, S. J., Budenz, D. L., Haft, P., Lee, Y., & Quigley, H. A. (2007). Factors affecting the decision to pursue glaucoma fellowship training. Journal of Glaucoma, 16(1), 81-87.
Gofton, W., & Regehr, G. (2006). Factors in optimizing the learning environment for surgical training. Clinical Orthopaedics and Related Research, 449, 100-107.
Healy, N. A., Glynn, R. W., Malone, C., Cantillon, P., & Kerin, M. J. (2012). Surgical mentors and role models: Prevalence, importance and associated traits. Journal of Surgical Education, 69(5), 633-637.
Hill, J. A., & Boone, S. (2002). Personal perception on mentoring. Clinical Orthopaedics and Related Research, 396, 73-75.
Kashiwagi, D. T., Varkey, P., & Cook, D. A. (2013). Mentoring programs for physicians in academic medicine: A systematic review. Academic Medicine, 88(7), 1029-1037.
Kram, K. E. (1983). Phases of the mentor relationship. Academy of Management Journal, 26(4), 608-625.
Lau, C., Ford, J., Van Lieshout, R. J., Saperson, K., McConnell, M., & McCabe, R. (2016). Developing mentoring competency: Does a one session training workshop have impact? Academic Psychiatry, 40(3), 429-433.
Levine, W. N., Braman, J. P., Gelberman, R. H., & Black, K. P. (2013). Mentorship in orthopaedic surgery-road map to success for the mentor and the mentee: AOA critical issues. Journal of Bone and Joint Surgery America, 95(9), e59.
Ramanan, R. A., Taylor, W. C., Davis, R. B., & Phillips, R. S. (2006). Mentoring matters. Mentoring and career preparation in internal medicine residency training. Journal of General Internal Medicine, 21(4), 340-345.
Sambunjak, D., Straus, S. E., & Marusic, A. (2006). Mentoring in academic medicine: A systematic review. Journal of the American Medical Association, 296(9), 1103-1115.
Yamada, K., Slanetz, P. J., & Boiselle, P. M. (2014). Perceived benefits of a radiology resident mentoring program: Comparison of residents with self-selected vs assigned mentors. Canadian Association of Radiologists Journal, 65(2), 186-191.
*Chua Min Jia
Ministry of Health Holdings,
1 Maritime Square, Singapore 099253
Tel: +65 6357 7713
E-mail: minjia.chua@mohh.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









