Traits of effective clinical educators: Perspectives of physiotherapy students and educators
Submitted: 17 January 2024
Accepted: 14 May 2024
Published online: 1 October, TAPS 2024, 9(4), 57-60
https://doi.org/10.29060/TAPS.2024-9-4/SC3234
Nicole Huiyi Ong1, Boon Chong Kwok2,3, Siti Munirah Aman4, Steven Michael Dans Macabasco5 & Wai Pong Wong2
1Department of Physiotherapy, Singapore General Hospital, Singapore; 2Health and Social Sciences, Singapore Institute of Technology, Singapore; 3Rehabilitation, Clinical Pilates Family Physiotherapy, Singapore; 4Department of Rehabilitation, Outram Community Hospital, Singapore; 5Rehabilitation, NTUC Eldercare, Singapore
Abstract
Introduction: Clinical practice education is an important curriculum in developing physiotherapy students to professionals. This curriculum is largely dependent on clinical educators. Although traits of effective clinical educators had been studied in Western population, it was unclear if the Asian population would yield similar traits. Hence, we studied perspectives of students and academic educators to identify top five core traits of an effective clinical educator. The findings will then help guide policy development for clinical educator training and development.
Methods: A survey was circulated to physiotherapy students and academic educators through convenience sampling. We studied 16 traits – enthusiasm, availability, clarity, clinical competence / knowledge, feedback skills, organisational skills, professionalism, well prepared, scholarly activity, non-judgemental, respect students’ autonomy / independence, sincerity, listening skills, evidence-based practice, role model, and awareness of students’ learning needs.
Results: The top five traits identified by students and academic educators were similar in four traits – clinical competency / knowledge, clarity, feedback skills, and enthusiasm, and differed in the choice of “non-judgemental” by students and “awareness of students’ learning needs” by academic educators. Interestingly, when the top six traits were considered instead of five, students and academic educators identified the same traits but in different ranked orders.
Conclusion: The study found six common core traits of an effective clinical educator from the perspectives of students and academic educators. Continuing education development for clinical educators should focus on these six traits prior to other 10 sub-traits.
Keywords: Training, Development, Education, Allied Health, Entrustable Professional Activities, Mentoring
I. INTRODUCTION
Clinical Practice Education (CPE) is a core component in undergraduate allied health studies, partnering clinicians with additional role as a Clinical Educator (CE) (Gibson et al., 2019). A study evaluating effective residency teaching for doctors identified 15 traits that a CE should possess, which are enthusiasm, competence-knowledge, clarity, availability, non-judgemental, independence, feedback skills, role model, professionalism, sincere, organised, well-prepared, evidence-based practice, scholarly activity and listening skills (Buchel & Edwards, 2005). A recent study found that being aware of the learning needs of students could be the 16th trait a CE should possess (Francis et al., 2016). Considering recent shift towards the use of the Entrustable Professional Activity framework for work place competency review at student and professional levels (Kwok et al., 2023), it is important to consider which top five traits are considered core competence of a CE as defined by the pinnacle of entrustment at Level 5.
Perspectives of critical traits of an effective CE might differ between students, CEs and academic educators (AEs). Students in early years of undergraduate study and CEs identified similar top five traits of an ideal CE (Cross, 1995). In the study by Cross (1995), CEs should be approachable, possess good communication skills, be knowledgeable and demonstrate enthusiasm in teaching, including clinical competency (Cross, 1995). Competency of CEs was similarly desired among academic educators, alongside “being approachable” and “good communicator”, whereas two differences were noted as compared to CEs and students, which were “interested in learning process of the students” and “concerned about patient care” (Cross, 1995). It is possible that among the Asian population, competency of the CEs would be similarly desired. Recent studies might have considered different trait terms as compared to the classic study, for instance, “learning process” was likely subsumed under “learning needs” (Francis et al., 2016). It is unclear whether the Asian population will present with different trait ranking as compared to Western population.
Therefore, this study was undertaken to identify the top five essential traits of an effective CE. In view of notable differences between perspectives of students and AEs in past literature, this study explored similarities and differences of perspectives between students and AEs. In addition, we explored what gaps might exist in developing CEs. In this study, the AEs, all of whom used to be CEs, could provide useful and important inputs on the traits required of a CE. The findings would then provide directions for future policy development pertaining to clinical education and professional supervision.
II. METHODS
A. Study Design
A survey was conducted through convenience sampling. The study was conducted between March to December 2022. The study was approved by the Institutional Review Board of the Singapore Institute of Technology (SIT-IRB-2022031).
B. Participants
Students in the third year of undergraduate physiotherapy programme and AEs of the physiotherapy faculty (as of April 2022) were involved in the survey. Large variations in response rate exists in convenience sampling, so we projected at least 50% response rate for the students and also the AEs. Students who had withdrawn from the programme were excluded. Associate faculty educators were excluded because they were only involved in ad hoc teaching sessions. Informed consent was sought at the beginning of the survey and digitally recorded.
C. Procedures
The survey described the 16 traits that contribute to an effective CE, which provided participants with knowledge about each trait, which was externally validated by five physiotherapists from the public and private sectors with experience ranging from eight to 25 years. The demographic data included student identification numbers to ensure that each response was unique. Thereafter, the data was de-identified to ensure anonymity during data analysis. As the sample size for the AEs was small, no personal data was collected to ensure anonymity. A survey invitation including a standardised survey link was distributed via email to all eligible participants. Participants were then asked to rank the 16 traits from 1 to 16, with 1 being the most important trait and 16 being the least important. Survey items were not randomised. The online survey was hosted on the secured Qualtrics Survey System (Qualtrics XM, 333 W. River Park Drive, Provo, UT 84604 USA). Student participants were first notified via email, followed by four reminder notifications, two months apart, via the cohort group chat on WhatsApp. AEs were first notified via email, followed by two reminder notifications via WhatsApp three months apart.
D. Statistical Analysis
Data analyses were performed using IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, N.Y., USA). Continuous variables are presented with means (standard deviations) and categorical variables with counts (percentages). Friedman test was used to analyse the mean rank of each trait. Then Kendall’s coefficient of concordance (Kendall’s W) was used to test the level of agreement among students for the mean ranks of the traits, as well as among AEs. The level of agreement was interpreted based on common recommendation and should yield statistical significance at p < 0.05.
III. RESULTS
A total of 81 students completed the survey (response rate of 46.6%) and a total of five AEs completed the survey (response rate of 41.7%). The average age, mean (standard deviation), of the students is 24.5 (4.1) years, and 52 of them are female (64.2%). The traits were ranked and presented in Table 1. Among the top five traits, there were four similar traits found between students and AEs, which were clinical competency / knowledge, clarity, feedback skills, and enthusiasm. The students ranked “non-judgemental” within the top five traits, whereas the AEs identified “awareness of students’ learning needs”. If the top six traits were considered, both students and AEs yielded similar traits. In the traits ranking, the students showed fair level of agreement, approximating closely to moderate agreement, Kendall’s W = 0.38, p < 0.001, while AEs showed moderate level of agreement, Kendall’s W = 0.51, p = 0.001.
|
Rank |
Students (n = 81) |
Academic Educators (n = 5) |
||
|
Traits |
Mean rank |
Traits |
Mean rank |
|
|
1 |
Clinical competency / knowledge |
4.51 |
Awareness of students’ learning needs |
3.20 |
|
2 |
Non-judgemental |
4.78 |
Feedback skills |
4.00 |
|
3 |
Clarity |
4.94 |
Clinical competency / knowledge |
4.20 |
|
4 |
Feedback skills |
5.01 |
Enthusiasm |
5.60 |
|
5 |
Enthusiasm |
7.06 |
Clarity |
6.80 |
|
6 |
Awareness of students’ learning needs |
7.27 |
Non-judgemental |
7.00 |
|
7 |
Availability |
7.93 |
Role model |
7.60 |
|
8 |
Sincerity |
8.56 |
Professionalism |
8.00 |
|
9 |
Respect students’ autonomy / independence |
8.68 |
Listening skills |
8.60 |
|
10 |
Listening skills |
9.35 |
Respect students’ autonomy / independence |
9.80 |
|
11 |
Professionalism |
9.51 |
Well prepared |
10.20 |
|
12 |
Organisational skills |
9.56 |
Organisational skills |
10.40 |
|
13 |
Role model |
10.23 |
Availability |
10.80 |
|
14 |
Well prepared |
11.69 |
Sincerity |
11.20 |
|
15 |
Evidence-based practice |
11.75 |
Evidence-based practice |
13.00 |
|
16 |
Scholarly activity |
15.19 |
Scholarly activity |
15.60 |
|
Table 1. Ranking of clinical educator traits by students and academic educators |
||||
IV. DISCUSSION
The study was initiated to identify the top five traits an effective CE should possess through the perspectives of students and AEs. The students and AEs differed only in the selection of one trait. Interestingly, when the top six traits were considered, students and AEs were aligned in traits selection and only differed in the ranking of traits. These six traits were 1) clinical competence / knowledge, 2) non-judgemental, 3) clarity, 4) feedback skills, 5) enthusiasm in teaching, and 6) awareness of students’ learning needs. The level of agreement found among students was fair and among the AEs was moderate for the rankings of traits in this study.
A few differences were observed in the top five traits as compared to western culture. Four traits were similar to those identified in the past – clinical competence / knowledge, clarity, feedback skills and enthusiasm in teaching (Cross, 1995). Whilst “clinical competence / knowledge” was ranked first by the students, we caution that these traits must be complemented by appropriate “feedback skills” and “clear communication”. A key difference between students and AEs was the identification of “non-judgemental” and “awareness of students’ learning needs” in the top five traits. The differences between students and AEs were essentially non-existent if we recognise top six traits as core competencies of an effective CE as compared to five traits. In view that the AEs were also past CEs, the rankings by the AEs provide valuable insights and could be used to align the students’ expectations.
The study found two common traits that were ranked lower among students and AEs – evidence-based practice and scholarly activity. It is possible that the students and AEs have assumed that “evidence-based practice” was a part of “clinical competency”, given the fact that “evidence-based practice” is essential in clinical practice. Moving forward, it would be of interest to study the perspectives of the students and AEs with regards to “evidence-based practice” in clinical education. Future research could explore the traits as “must have”, “should have” and good-to-have” categories, which could help identify the critical traits (“must have”).
The study has a few limitations. Although self-reported survey could lead to response bias, we did not detect similar responses in consecutive order during data inspection. Next, we set out to collect 50% response rate, unfortunately, we were slightly away from the target as some respondents did not complete or withdrew their participation. As such, the sample size of the AEs was small and so perspectives from the AEs might require careful considerations. The study also did not allow for qualitative inputs from the respondents to explore other traits that were not listed. Lastly, we were unable to engage participation from CEs as the survey was not compulsory as part of their role.
V. CONCLUSION
This study identified six core traits an effective CE should possess. These traits are clinical competence / knowledge, non-judgemental, clarity, feedback skills, enthusiasm in teaching, and awareness of students’ learning needs. We identified that evidence-based practice and scholarly activity traits were potential gaps in career development of CEs as they were ranked lower among students and AEs.
Notes on Contributors
NHO was involved in study conceptualisation, data collection, data analysis, data interpretation and drafting manuscript.
BCK was involved in study conceptualisation, data analysis, data interpretation, drafting manuscript and final revision of manuscript.
SMA was involved in study conceptualisation, data collection and revising the manuscript.
SMDM was involved in study conceptualisation, data collection and revising the manuscript.
WPW initiated the study conceptualisation, project administration, data interpretation and review of the drafted manuscript.
Ethical Approval
The study was approved by the Institutional Review Board of the Singapore Institute of Technology (SIT-IRB-2022031).
Data Availability
Based on the ethics approval, data will not be shared on a repository. The anonymised dataset can be obtained from the corresponding author with reasonable request.
Acknowledgement
The authors thank the physiotherapy students and educators from the Singapore Institute of Technology for their study participation.
Funding
This study is unfunded.
Declaration of Interest
None of the authors has any conflict or financial interest to declare.
References
Buchel, T. L., & Edwards, F. D. (2005). Characteristics of effective clinical teachers. Family Medicine, 37(1), 30-35. https://www.ncbi.nlm.nih.gov/pubmed/15619153
Cross, V. (1995). Perceptions of the ideal clinical educator in physiotherapy education. Physiotherapy, 81(9), 506-513. https://doi.org/10.1016/S0031-9406(05)66680-1
Francis, A., Hills, C., MacDonald-Wicks, L., Johnston, C., James, D., Surjan, Y., & Warren-Forward, H. (2016). Characteristics of an ideal practice educator: Perspectives from practice educators in diagnostic radiography, nuclear medicine, nutrition and dietetics, occupational therapy and physiotherapy and radiation therapy. Radiography, 22(4), 287-294. https://doi.org/10.1016/j.radi.2016.04.001
Gibson, S. J., Porter, J., Anderson, A., Bryce, A., Dart, J., Kellow, N., Meiklejohn, S., Volders, E., Young, A., & Palermo, C. (2019). Clinical educators’ skills and qualities in allied health: A systematic review. Medical Education, 53(5), 432-442. https://doi.org/10.1111/medu.13782
Kwok, B. C., Zulimran, M., & Sue, P. (2023). Re-designing performance management for healthcare – The performance empowerment, advancement and career excellence (PEACE) system. International Journal of Productivity and Performance Management, 72(7), 2183-2193. https://doi.org/10.1108/IJPPM-12-2022-0610
*Boon Chong Kwok
10 Dover Drive,
Singapore Institute of Technology,
Singapore 138683
96916703
Email: boonchong.kwok@singaporetech.edu.sg /
kwokboonchong@gmail.com
Submitted: 19 December 2023
Accepted: 26 April 2024
Published online: 1 October, TAPS 2024, 9(4), 50-56
https://doi.org/10.29060/TAPS.2024-9-4/SC3194
Craig S. Webster1, Jack Forsythe2, Antonia Verstappen1, Phillippa Poole3, Tim Wilkinson4 & Marcus A. Henning1
1Centre for Medical and Health Sciences Education, School of Medicine, University of Auckland, Auckland, New Zealand; 2Auckland District Health Board, Te Whatu Ora, Auckland, New Zealand; 3School of Medicine, University of Auckland, Auckland, New Zealand; 4Education Unit, University of Otago, Christchurch, New Zealand
Abstract
Introduction: A valid, longitudinal approach is critical for service planning in healthcare and to understand career choice in medical graduates.
Methods: We quantitatively analysed self-reported influences underlying career choice in a national cohort of medical graduates over the first five years of their careers. Participants rated career influences on importance across 26 items using a 5-point Likert scale (1=not at all, 5=a great deal).
Results: We included 659 New Zealand medical graduates (mean 25.4 years old, 376 F, 283 M) from the University of Auckland and the University of Otago, graduating in 2012 and 2013 (85% response rate). Responses were linked longitudinally over their post-graduate years 1, 3 and 5, and underwent principal component analyses. At graduation the factor rated as the most important in career choice had a mean (SD) item score of 3.9 (0.7) and comprised: Medical School Experiences; Specialty Experience; Mentors; and Self-Appraisal – consistent with graduates securing initial employment. Factors which explained the most variance in career choice over the five years after graduation indicated that the costs of medical school and further training were consistently rated as the least important in career choices, while flexibility in working hours were consistently rated as the most important. Factors remained relatively stable over time, showing variation in scores of only a median of 0.5 Likert points, indicating further opportunities for career choice research.
Conclusion: Our results regarding costs of medical training are reassuring, and suggest that greater flexibility in working hours may attract graduates to underserved specialties.
Keywords: Medical Education, Career Choice, Career Influences, Cost, Debt, Measurement, Medical Graduates, National Longitudinal Study, Working Hours, Work Culture
I. INTRODUCTION
A common strategic aim of medical schools throughout the world is to supply the range of graduates who will best meet the healthcare needs of their communities (Gorman, 2018). However, fulfilling this aim is far from straight-forward, with perhaps the most critical difficulty involving understanding the influences that underlie career choice in medical graduates and how these vary over time.
The financial burden of completing medical school and further training has been one of the most widely studied influences underlying career choice, with suggestions that rising costs may encourage graduates to pursue specialties perceived to be more highly paid, often in cities, thus undersupplying primary healthcare and rural locations. However, in New Zealand medical graduates are otherwise free to choose their preferred career path and choices may be influenced by many things other than training costs and debt, including personal interest, employment conditions, specialty availability and lifestyle preferences (Webster et al., 2020; Webster et al., 2017).
Therefore, in the following, we analyse the self-reported influences underlying career choice in a national cohort of medical school graduates during the first five years of their careers using quantitative data drawn from the existing longitudinal Medical Schools Outcomes Database (MSOD).
II. METHODS
The MSOD project is a bi-national longitudinal questionnaire study that aims to improve healthcare delivery in Australia and New Zealand (Poole et al., 2019). At graduation and in postgraduate years (PGY), graduates are asked to specify their preferred area(s) of medicine, and complete a schedule of influencing items, indicating the degree to which each was important in their choice, using a 5-point Likert scale with anchors of 1 (not at all) to 5 (a great deal) – see Supplementary Table 1 for full question set.
A. Data Analysis
We conducted a series of principal component analyses (SPSS v27, IBM Corporation, New York) of the responses to the 26 influencing item questions at each time point to identify factors within responses, and describe them over time.
III. RESULTS
Data from a national cohort of 659 New Zealand medical school graduates who had graduated from the University of Auckland and the University of Otago in 2012 and 2013 were included. The response rate for completed questionnaires in the Exit cohort was 85% – representing a sampling margin of error of only 1% at the 95% level of confidence. The mean (SD) age of participants in the cohort was 25.4 (2.7) years, with a higher proportion of female graduates (376 F vs 283 M). Over the next five years, this Exit cohort self-reported on the same set of influences underlying career choice at PGY1, PGY3 and PGY5 – maintaining a response rate between 53% and 56%, and a sampling margin of error of 3%.
We used conventional settings during analysis, comprising varimax rotation and suppression of loadings below 0.3. The Kaiser-Meyer-Olkin measure of sampling adequacy across time points demonstrated a median (range) of 0.77 (0.75 to 0.82), indicating distinct and reliable factors at each time point. In addition, Bartlett’s test of sphericity was highly significant at each time point, (2338<c2<3498, p<0.0001), demonstrating correlation with little redundancy in items (Kaiser, 1974).
|
Influencing items* |
Factor numbers and item loadings |
||||
|
|
A: Exit (yrs 2012 and 2013) |
||||
|
|
1 |
2 |
3 |
4 |
5 |
|
Costs Voc. Training |
0.855 |
||||
|
Costs Med. School |
0.832 |
||||
|
Insurance Risk |
0.675 |
||||
|
Parents/Relatives |
0.536 |
||||
|
Prestige |
0.528 |
||||
|
Training Yrs |
0.508 |
||||
|
Financial Prospects |
0.463 |
||||
|
Research/Teaching |
0.442 |
||||
|
Location |
0.440 |
||||
|
Flexible Hrs |
0.862 |
||||
|
Working Hrs |
0.838 |
||||
|
Domestic Circum. |
0.633 |
||||
|
Work Culture |
0.416 |
||||
|
Career Prospects |
0.725 |
||||
|
Procedural Work |
0.698 |
||||
|
Job Security |
0.555 |
||||
|
Voc. Training Avail. |
0.409 |
||||
|
Med. School Exp. |
0.836 |
||||
|
Specialty Exp. |
0.787 |
||||
|
Mentors |
0.752 |
||||
|
Self-Appraisal |
0.388 |
||||
|
Typical Patients |
0.643 |
||||
|
Helping People |
0.642 |
||||
|
Intel. Content |
0.532 |
||||
|
Variance explained, % |
15.8 |
11.1 |
9.5 |
9.3 |
7.3 |
|
Factor score, mean (SD)** |
2.3 (0.7) |
3.6 (0.8) |
3.3 (0.9) |
3.9 (0.7) |
3.8 (0.7) |
|
|
B: PGY1 (yrs 2013 and 2014) |
||||
|
|
2 |
1 |
4 |
3 |
5 |
|
Working Hrs |
0.847 |
||||
|
Flexible Hrs |
0.831 |
||||
|
Domestic Circum. |
0.673 |
||||
|
Training Yrs |
0.538 |
||||
|
Voc. Training Avail. |
0.494 |
||||
|
Location |
0.411 |
||||
|
Job Security |
0.391 |
||||
|
Costs Voc. Training |
0.836 |
||||
|
Costs Med. School |
0.765 |
||||
|
Insurance Risk |
0.673 |
||||
|
Research/Teaching |
0.547 |
||||
|
Specialty Exp. |
0.791 |
||||
|
Med. School Exp. |
0.777 |
||||
|
Training Exp./Doc. |
0.590 |
||||
|
Helping People |
0.393 |
||||
|
Post-Grad. Work |
0.302 |
||||
|
Prestige |
0.730 |
||||
|
Financial Prospects |
0.712 |
||||
|
Procedural Work |
0.576 |
||||
|
Intel. Content |
0.604 |
||||
|
Career Prospects |
0.566 |
||||
|
Work Culture |
0.451 |
||||
|
Typical Patients |
0.395 |
||||
|
Self-Appraisal |
0.368 |
||||
|
Variance explained, % |
12.4 |
11.4 |
9.2 |
8.8 |
8.3 |
|
Factor score, mean (SD)** |
3.1 (0.8) |
1.8 (0.7) |
3.6 (0.7) |
2.7 (0.9) |
3.6 (0.6) |
|
|
C: PGY3 (yrs 2015 and 2016) |
||||
|
|
1 |
2 |
5 |
4 |
3 |
|
Costs Voc. Training |
0.806 |
||||
|
Costs Med. School |
0.803 |
||||
|
Financial Prospects |
0.635 |
||||
|
Prestige |
0.621 |
||||
|
Insurance Risk |
0.596 |
||||
|
Career Prospects |
0.544 |
||||
|
Job Security |
0.511 |
||||
|
Research/Teaching |
0.367 |
||||
|
Flexible Hrs |
0.849 |
||||
|
Working Hrs |
0.827 |
||||
|
Domestic Circum. |
0.732 |
||||
|
Voc. Training Avail. |
0.399 |
||||
|
Intel. Content |
0.669 |
||||
|
Training Exp./Doc. |
0.581 |
||||
|
Work Culture |
0.576 |
||||
|
Post-Grad. Work |
0.558 |
||||
|
Typical Patients |
0.540 |
||||
|
Self-Appraisal |
0.451 |
||||
|
Procedural Work |
0.374 |
||||
|
Specialty Exp. |
0.911 |
||||
|
Med. School Exp. |
0.892 |
||||
|
Training Yrs |
0.521 |
||||
|
Location |
0.476 |
||||
|
Helping People |
0.464 |
||||
|
Variance explained, % |
13.7 |
13.1 |
11.5 |
7.5 |
5.4 |
|
Factor score, mean (SD)** |
2.3 (0.7) |
3.4 (0.9) |
3.8 (0.6) |
3.1 (1.2) |
3.1 (0.7) |
|
|
D: PGY5 (yrs 2017 and 2018) |
||||
|
|
2 |
3 |
1 |
5 |
4 |
|
Flexible Hrs |
0.822 |
||||
|
Working Hrs |
0.791 |
||||
|
Domestic Circum. |
0.687 |
||||
|
Location |
0.454 |
||||
|
Career Prospects |
0.790 |
||||
|
Prestige |
0.633 |
||||
|
Job Security |
0.613 |
||||
|
Financial Prospects |
0.604 |
||||
|
Procedural Work |
0.521 |
||||
|
Research/Teaching |
0.508 |
||||
|
Voc. Training Avail. |
0.355 |
||||
|
Costs Voc. Training |
0.859 |
||||
|
Costs Med. School |
0.831 |
||||
|
Insurance Risk |
0.604 |
||||
|
Training Yrs |
|
0.563 |
|||
|
Parents/Relatives |
0.350 |
||||
|
Typical Patients |
0.600 |
||||
|
Helping People |
0.585 |
||||
|
Intel. Content |
0.562 |
||||
|
Self-Appraisal |
0.507 |
||||
|
Work Culture |
0.464 |
||||
|
Training Exp./Doc. |
0.432 |
||||
|
Post-Grad. Work |
0.429 |
||||
|
Specialty Exp. |
0.896 |
||||
|
Med. School Exp. |
0.881 |
||||
|
Variance explained, % |
12.1 |
11.3 |
11.1 |
8.3 |
7.8 |
|
Factor score, mean (SD)** |
3.4 (0.9) |
2.8 (0.7) |
1.8 (0.7) |
3.9 (0.6) |
2.9 (1.2) |
|
*See Supplementary Table 1 for full item descriptors **Mean (SD) of 5-point Likert scores making up factor |
|||||
Table 1. Principal component analyses of influences underlying career choice in medical graduates to five years after graduation
Table 1 shows the results of the principal component analyses, demonstrating well-formed factors at each time point. Factors are reported in the descending order of their variance explained (VE), and with a factor score, being the mean (SD) of the Likert question scores making up the factor. The VE is a measure of the amount of variability in the participants’ responses that can be explained by the factor, hence higher levels of VE indicate agreement by a larger number of graduates. The factor score indicates the degree to which graduates consider the factor to be important or unimportant in their choices.
For example, at Exit from medical school (Table 1A), Factor 1 accounts for the largest VE (15.8%), comprising the 9 question items that are, on average, the least influential in determining career choice for graduates, with a factor score of 2.3 (out of 5). These least influential items are: Costs of Vocational Training; Costs of Medical School; Insurance Risk; Parents/Relatives; Prestige; Training Years; Financial Prospects; Research/Teaching; and Location. By contrast, Factor 4 at Exit, with the highest factor score of 3.9 and explaining 9.3% of the variance, contains the 4 items rated as the most influential by graduates in determining career choice. These most influential items are: Medical School Experiences; Specialty Experience; Mentors; and Self-Appraisal. These results are consistent with new graduates making the most of their abilities and opportunities to secure their first healthcare role. Other factors at Exit fall within these two extremes.
It is worth noting that the item Parent/Relatives fails to load over the 0.3 threshold on any factor at PGY1 or PGY3 (hence does not appear). Some change in factor structures over time do occur, reflecting changing priorities for graduates. For example, Factor 2 at Exit has a relatively high factor score of 3.6 (VE=11.1%) indicating that the items Flexible Hours, Working Hours, Domestic Circumstances, and Work Culture are important for new graduates. However, by PGY1 (Table 1B) this factor then picks up the items of Training Years, Vocational Training Availability, Location and Job Security, and becomes important to a greater number of graduates by becoming the factor with the largest variance explained (VE=12.4%). This result suggests that graduates are adjusting to their new working lives and are planning for their futures in terms of further training.
Factor 1 and Factor 2 consistently demonstrate high levels of variance explained and contain a common core of three influencing items. Factor 1, with a median (range) score of 2.1 (1.8 to 2.3) across all time points, continues to describe influences on career choice rated as the least important for medical graduates, and consistently contains the items Costs of Vocational Training, Costs of Medical School, and Insurance Risk. By contrast, Factor 2 is consistently rated as relatively important, with a median (range) score of 3.4 (3.1 to 3.6) across time points, and consistently contains the items Flexible Hours, Working Hours, and Domestic Circumstances.
Our results demonstrate the existence of well-formed factors in the MSOD data at each time point. Despite some change in factor structure over time, the scores for each factor remain relatively stable, with a median (range) variation in scores of only 0.5 (0.3 to 1.0) Likert points. Table 1 contains results which allow substantial scope for hypothesis formation and future research, including targeted work to better understand the decision points in the critical first five years of a graduate’s career.
IV. DISCUSSION
Better understanding the influences underlying career choice in medical graduates is a strategically important and practical concern when aiming to match graduate production with professional and community needs. This study is the among the first to conduct a quantitative analysis of the self-reported influences underlying medical graduate career choice in a prospective, national cohort of the same graduates over the critical first five years of their careers.
The financial burden of completing medical school and vocational training is one of the most widely studied influences in career choice for medical graduates. It is therefore reassuring that our findings demonstrate that these costs are among the least influential considerations at all time points in the five years after graduation for our cohort.
Factor 2 in the present study consistently contains the items Flexible Hours, Working Hours and Domestic Circumstances, and is rated as important over the first five years of graduates’ careers. Flexibility around working hours and a desire to practice part-time has traditionally been thought of as largely important for female medical graduates (Heiliger & Hingstman, 2000). However, this is no longer the case, with many male graduates in recent decades also desiring more lifestyle-friendly working arrangements allowing the flexibility to spend more time with family (Heiliger & Hingstman, 2000). Taken together with the evidence that the costs of medical school and further training are the least influential in career choice, our results therefore strongly suggest that the ability to offer greater flexibility in working hours is likely to be useful in recruiting medical graduates to underserved specialties.
It is a practical and pressing necessity that healthcare workforce planning is guided by the best available evidence. A strength of the current study is the ability to link the same participants longitudinally, thus eliminating an important source of bias. Women in the current study made up 57% of medical graduate respondents, reflecting the fact that in recent years in New Zealand and Australia female graduates have outnumbered male graduates. A further strength is the high response rates, yielding a sampling margin of error of only 3% or less at all time points, which compares favourably with many questionnaire studies of medical graduates.
V. CONCLUSION
Despite widespread concern over rising debt levels and the cost of medical school, our results are reassuring in that the costs of medical school and vocational training were consistently rated as the least important influences in career choice. Our results also suggest that offering greater flexibility around working hours may assist in attracting medical graduates to underserved specialties. Our description of well-formed factors in the influences underlying career choice in the national MSOD questionnaire data provides a useful basis for further research to better understand key decision points in the critical first five years of graduates’ careers.
Notes on Contributors
Craig Webster was involved in the conceptualisation of this paper, data analysis, writing and revision.
Jack Forsythe was involved in the conceptualisation of this paper, data analysis, writing and revision.
Antonia Verstappen was involved in accessing data for this paper, writing and revision.
Phillippa Poole was involved in the writing and revision of this paper.
Tim Wilkinson was involved in the writing and revision of this paper.
Marcus Henning was involved in the writing and revision of this paper.
Ethical Approval
This study was carried out in accordance with all regulations of the host organisations and with the approvals of the Human Participants Ethics Committees of the University of Auckland (approval numbers 022388 and 018456) and the University of Otago (approval number 07-155), New Zealand. All participants gave written informed consent to participate in the study, including for anonymised aggregated data to be published.
Data Availability
The ethics approval for the longitudinal MSOD project currently does not permit the sharing of non-aggregated data. However, this restriction is under review and so non-aggregated data may be available from the corresponding author in the near future.
Acknowledgement
We thank the Health Career Pathways Project, Faculty of Medical and Health Sciences, University of Auckland, and the Medical Schools Outcomes Database Longitudinal Tracking Project at the University of Auckland and the University of Otago for assistance and data access.
Funding
JF received a summer studentship stipend from the Faculty of Medical and Health Sciences, University of Auckland, New Zealand in support of this research. The Medical Schools Outcomes Database Longitudinal Tracking Project is supported by a grant from Health Workforce New Zealand.
Declaration of Interest
All authors have no potential conflicts of interest.
References
Gorman, D. (2018). Matching the production of doctors with national needs. Medical Education, 52(1), 103-113. https://doi.org/10.1111/medu.13369
Heiliger, P. J., & Hingstman, L. (2000). Career preferences and the work-family balance in medicine: Gender differences among medical specialists. Social Science and Medicine, 50(9), 1235-1246. https://doi.org/10.1016/s0277-9536(99)00363-9
Kaiser, H. F. (1974). An index of factorial simplicity. Psychometrika, 39, 31–36. https://doi.org/10.1007/BF02291575
Poole, P., Wilkinson, T. J., Bagg, W., Freegard, J., Hyland, F., Jo, C. E., Kool, B., Roberts, E., Rudland, J., Smith, B., & Verstappen, A. (2019). Developing New Zealand’s medical workforce: Realising the potential of longitudinal career tracking. New Zealand Medical Journal, 132(1495), 65-73.
Webster, C. S., Ling, C., Barrow, M., Poole, P., & Henning, M. (2017). A cross-disciplinary assessment of student loans debt, financial support for study and career preferences upon graduation. New Zealand Medical Journal, 130(1459), 43-53.
Webster, C. S., McKillop, A., Bennett, W., & Bagg, W. A. (2020). A qualitative and semiquantitative exploration of the experience of a rural and regional clinical placement programme. Medical Science Educator, 30(2), 783-789. https://doi.org/10.1007/s40670-020-00949-6
*Craig Webster
Centre for Medical and Health Sciences Education,
School of Medicine, University of Auckland,
Private Bag 92-019
Auckland 1142, New Zealand
+649 923 6525
Email: c.webster@auckland.ac.nz
Submitted: 12 December 2023
Accepted: 25 March 2024
Published online: 1 October, TAPS 2024, 9(4), 40-49
https://doi.org/10.29060/TAPS.2024-9-4/SC3254
Vivien Lee1, Jeffrey Jiang1, Anna Szücs1, V Vien Lee1, Low Si Hui2, Faith Teo1, Jose M Valderas1 & Victor Loh1
1Division of Family Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2National University Polyclinics, Singapore
Abstract
Introduction: Globally, persons with disabilities (PWD) face structural and social barriers to inclusive healthcare. Medical schools, as crucibles of medical professional identity formation, have the responsibility to foster person-centredness toward all patients, including PWD, among her graduates. We co-designed with PWD a “Communications with Persons with Disabilities” workshop and evaluated its impact.
Methods: The workshop enlisted PWD as patient educators, occurred within the third-year undergraduate Family Medicine posting, and was designed to positively impact communications skills and attitudes toward PWD. Students (n=135) were surveyed pre- and post- workshop following a mixed-methods approach (demographic data, Attitude Towards Disabled Persons (ATDP)-O scale, feedback questions, and post-workshop free reflections). Descriptive analysis was used for demographic and feedback questions, and thematic analysis for reflections. Paired t-test was used to evaluate change in ATDP-O scores.
Results: There were 69 survey respondents (51.11%). Most students agreed that communications training with PWD could be strengthened in medical school, and that the workshop was relevant to their future medical career (n=68, 98.55%). Attitudes towards PWD significantly improved after the workshop (ATDP-O change: +9.29 points (12.7%), p <0.001). Student reflections included attitudes, such as the importance of seeing the person beyond the disability, and a call for action towards inclusivity and accessibility of care for PWD.
Conclusion: Students’ attitudes were positively affected by involving PWD in the curriculum. Further research is needed for assessing the impact of how a longitudinal PWD curriculum could affect medical trainees and improve social inclusiveness in healthcare practice.
Keywords: Medical Education, Communication, Persons with Disabilities, Disability, Social Inclusiveness, Student Attitudes, Person Centred Care, Active Learning
I. INTRODUCTION
Globally, persons with disabilities (PWD) face structural and social barriers to inclusive healthcare. In Singapore, few are comfortable with direct personal interaction with PWD (National Council of Social Service Singapore, 2019).
With respect to medical education, different disability curriculum from didactic lectures to longitudinal patient experiences have been described (Ali et al., 2023). Overall evidence suggests that more frequent and positive contact with PWD increased positive attitudes (Ali et al., 2023; National Council of Social Service Singapore, 2019).
Medical schools, as crucibles of medical professional identity formation, have the responsibility to foster person-centredness toward all patients, including PWD, among her graduates. In July 2022, the National University of Singapore’s Division of Family Medicine developed with PWD, piloted and assessed a four-hour experiential workshop for third-year medical students called “Communication with PWD” in July 2022.
The four-hour workshop was prefaced by pre-event reading materials. A plenary started on site learning, followed by fishbowl discussions where student volunteers took turns to perform a clinical consultation with PWD who enacted scripted role-plays. There was a ratio of one tutor and PWD to a group of ten to fifteen students. Each student would encounter three broad categories of disability (vision, hearing, mobility) during the fishbowl sessions. Students interacted with PWD after each role play. Reflections and debrief by tutors would close the workshop.
This study aimed to evaluate the workshop’s impact on students’ attitudes towards PWD for: (Q1) differences in pre-workshop attitudes towards PWD between male and female medical students; (Q2) within-person changes in students’ overall attitudes towards PWD pre-post workshop; (Q3) associations between pre-workshop attitudes towards PWD and personal experience with PWD; and (Q4) exploration of how the workshop has affected students’ attitudes towards caring for PWDs.
II. METHODS
A. Study Design
This study had a mixed methods design including a pre- and post-intervention survey (quantitative), and reflections (qualitative). Students attending the 3rd and 4th Family Medicine Rotation (January to March 2023) of Academic Year 2022/23 were invited to participate in the study. The questionnaire was administered in person. Students completed the questionnaires independently. A waiver of consent was applied for reflections.
B. Survey
The pre-workshop questionnaire comprised demographic information and the 20-item Attitude Towards Disabled Persons (ATDP)-O scale (Yuker et al., 1960). The questions were scored on six-point Likert scale from “I disagree very much” (-3) to “I agree very much” (+3). The post-workshop questionnaire comprised the ATDP-O scale and feedback questions.
We used the original ATDP-O form as it had been used in other studies on medical students (Arabi et al., 2021) and was deemed reliable (reliability coefficient .80) and valid by prior psychometric analyses (Yuker et al., 1960). Performance in local context was assessed through cognitive testing with five randomly selected medical students who were classmates of study participants and excluded from the study sample.
C. Reflections
Student reflection sheets included a single open-ended statement: “Please pen a question or a reflection you’d like to share from the session today”. Reflections were transcribed verbatim and de-identified before analysis. All reflections were used to limit selection bias.
D. Data Analysis
Numeric data was analysed by R software (version 4.31). Internal consistency of the scale in our study sample was measured with Cronbach’s alpha. We used two samples independent unpaired t-test to evaluate Q1 (differences in baseline ATDP-O scores between males and females), two samples paired t-test to evaluate Q2 (change in pre-post workshop ATDP-O scores), and two samples independent unpaired t-tests, Welch’s t-tests and Spearman’s correlation tests to evaluate Q3 (difference in baseline ATDP-O scores across different types/levels of contact with PWD). In the evaluation of Q3, two samples independent unpaired t-test was used when two groups have similar sample sizes or similar variances while Welch’s t-test was used when there’s unequal variances or disparate sample sizes between two groups. Spearman’s correlation was used to analyse associations with ordinal variables.
Student reflections were analysed thematically. Four researchers (VLE, VVL, AS, FT) reviewed the data and generated initial codes independently. Multiple discussions were conducted to explore different perspectives and increasingly develop codes. Based on codes generated, potential themes and subthemes were developed over several iterations. Final themes and subthemes were reviewed in relation to the entire dataset.
III. RESULTS
Of 135 students invited, 69 students consented to the study and completed both the pre- and post-workshop questionnaire. The results are summarised (Table 1a and 1b).
Cognitive testing confirmed that students had no difficulties understanding questions nor suggested any edits for clarification. The internal consistency of the scale was α = 0.72 (pre-workshop) and α = 0.78 (post-workshop).
(Q1) Female gender had a significantly higher baseline ATDP-O scores (p = 0.028).
(Q2) There was a significant improvement of 9.29 points (12.7%) in the ATDP-O score post workshop (p <0.001).
(Q3) Previous experience of training to care for PWD (p<0.001) and previous experience caring for PWD (p = 0.033) had significantly lower baseline ATDP-O scores.
|
Results |
Number (%) |
ATDP-O baseline score Mean (SD) |
Statistics |
||
|
Overall |
N=69 |
72.71 (10.46) |
|
||
|
By age (Mean = 21.59, SD = 0.96) |
Pearson’s r(67) = – 0.02, p = .857 |
||||
|
By gender |
|||||
|
Female |
37 (53.62%) |
75.32 (8.61) |
t(67) = 2.30, p = .025*
|
||
|
Male |
32 (46.38%) |
69.69 (11.69) |
|||
|
By ethnicity |
|||||
|
Chinese |
56 (81.16%) |
73.18 (10.20) |
F(2, 66) = 1.64, p = .201 |
||
|
Indian |
12 (17.39%) |
69.33 (11.18) |
|||
|
Others |
1 (1.45%) |
87.00 (.) |
|||
|
Self-reported disability |
|||||
|
No |
66 (95.65%) |
72.74 (10.59) |
t(2) = 0.14, p = .900 |
||
|
Yes |
3 (4.35%) |
72.00 (8.89) |
|||
|
Self-reported training to care for PWD |
|||||
|
No |
67 (97.10%) |
73.06 (10.42) |
t(7) = 7.45, p < .001* |
||
|
Yes |
3 (4.35%) |
61.00 (1.41) |
|||
|
Self-reported frequency of care for PWD (ranked variable ranging from never = 1 to often = 4) |
|||||
|
Never |
34 (49.28%) |
75.7 (9.5) |
Spearman’s rho(67) = – 0.26, p = .033* |
||
|
Rarely |
22 (31.88%) |
69.8 (11.8) |
|||
|
Sometimes |
12 (17.39%) |
69.5 (9) |
|||
|
Often |
1 (1.45%) |
75 (.) |
|||
|
Self-reported knowledge of PWD who is important to them |
|||||
|
No |
53 (76.81%) |
73.57 (10.95) |
t(67) = 1.24, p = .219
|
||
|
Yes |
16 (23.19%) |
69.88 (8.34) |
|||
|
Self-rated likelihood of pursuing career in Family Medicine (ranked variable ranging from very unlikely = 1 to very likely = 5) |
|||||
|
Very likely |
9 (13.04%) |
72.1 (10) |
Spearman’s rho(67) = 0.03 , p = .803 |
||
|
Likely |
18 (26.09%) |
73.2 (11.5) |
|||
|
Undecided |
37 (53.62%) |
73.5 (10.3) |
|||
|
Unlikely |
4 (5.80%) |
63.5 (8.9) |
|||
|
Very unlikely |
1 (1.45%) |
78 (.) |
|||
|
Do you feel your education about persons with disabilities in medical school has been adequate so far? |
|||||
|
Agree |
1 (1.45%) |
– |
– |
||
|
Neither disagree nor agree |
19 (27.54%) |
– |
– |
||
|
Disagree |
42 (60.87%) |
– |
– |
||
|
Strongly disagree |
7 (10.14%) |
– |
– |
||
|
Would you find it important to include education and training on persons with disabilities? |
|||||
|
Strongly agree |
23 (33.33%) |
– |
– |
||
|
Agree |
39 (56.52%) |
– |
– |
||
|
Neither disagree nor agree |
5 (7.25%) |
– |
– |
||
|
Disagree |
1 (1.45%) |
– |
– |
||
|
Strongly disagree |
1 (1.45%) |
– |
– |
||
|
Do you feel that the education provided during the Communications with Persons with Disabilities workshop was relevant to your future career as doctors? |
|||||
|
Strongly agree |
45 (65.22%) |
– |
– |
||
|
Agree |
23 (33.33%) |
– |
– |
||
Table 1a. Baseline ATDP-O scores and curriculum feedback
|
Results |
ATDP-O score Mean (SD) |
Pre-Post workshop comparison statistics |
|
Descriptive statistics |
||
|
Pre-workshop ATDP-O score |
72.71 (10.46) |
t(68) = 8.69, p < .001*
|
|
Post-workshop ATDP-O score |
82.00 (11.46) |
|
|
Difference in ATDP-O scores |
||
|
Overall sample |
9.29 (8.88) |
t(68) = 8.69, p < .001 |
|
By age (Mean = 21.59, SD = 0.96) |
Pearson’s r(67) = – 0.06, p = .643 |
|
|
By gender |
||
|
Female |
8.62 (9.33) |
t(67) = – 0.67, p = .505 |
|
Male |
10.06 (8.41) |
|
|
By ethnicity |
||
|
Chinese |
9.02 (9.45) |
F(2, 66) = 0.15, p = .859 |
|
Indian |
10.33 (6.21) |
|
|
Others |
12.00 (.) |
|
|
Self-reported disability |
||
|
No |
9.50 (8.06) |
t(2) = 0.36, p = .752 |
|
Yes |
4.67 (23.12) |
|
|
Self-reported training to care for PWD |
||
|
No |
9.09 (8.92) |
t(1) = – 2.17, p = .230 |
|
Yes |
16.00 (4.24) |
|
|
Self-reported frequency of care for PWD (ranked variable ranging from never = 1 to often = 4) |
||
|
Never |
8.8 (6.1) |
Spearman’s rho(67) = 0.05, p = .678 |
|
Rarely |
11.5 (9.1) |
|
|
Sometimes |
9.4 (10.8) |
|
|
Often |
-22 (.) |
|
|
Self-reported knowledge of PWD who is important to them |
||
|
No |
10.72 (7.61) |
t(67) = 2.52, p = .014*
|
|
Yes |
4.56 (11.20) |
|
|
Self-rated likelihood of pursuing career in Family Medicine (ranked variable ranging from very unlikely = 1 to very likely = 5) |
||
|
Very likely |
10.4 (9.2) |
Spearman’s rho(67) = 0.07, p = .547 |
|
Likely |
10.9 (7.8) |
|
|
Undecided |
7.9 (9.5) |
|
|
Unlikely |
11.5 (9.3) |
|
|
Very unlikely |
11 (.) |
|
Table 1b. Difference in ATDP-O scores post workshop
Most students found the workshop a positive experience and reported feelings of thankfulness and inspiration towards patient educators. Four themes emerged from the students’ post-workshop reflections, of which we highlight those related to attitudes – Humanizing mindsets towards PWD (Theme 1) and Call for action towards inclusivity and accessibility (Theme 2). The other themes were Knowledge and Skills, as students included knowledge and communication skills they acquired during the workshop (Appendix 1 and 2).
A. Theme 1 – Humanising Mindset towards Persons with Disabilities
Students expressed attitudes of empathy, sensitivity, and humanising care through viewing PWD as individuals beyond their disabilities. A student reflected
“Being able to speak to members of these respective communities helped me to understand how empowered PWD can be… It is essential that [PWD] are treated as exactly that, [and] not characterised by their disabilities.”
On providing care for PWD, students noted the distinction between empathy and sympathy, and highlighted the importance of empathy instead of pity. As summed up by a student,
“Not to sympathise but to empathise. Not to see them and pity them”
B. Theme 2 – Call for Action towards Inclusivity and Accessibility
Concurrent with attitudes expressed in the reflections, students discussed the need to improve inclusivity and accessibility from an individual and societal perspective. One student wrote,
“As doctors, we need to try our best to alleviate their disease burden, and at the same time, make their journey to accessing healthcare more seamless with less barriers.”
Beyond self-improvement, students were aware of the need to shift their own perspectives of disability from a medical to a social model. Students also reflected the need for greater national efforts towards societal inclusivity for PWD. A student reflected,
“I think policymakers and organisations should periodically involve PWD to [better] take their needs into consideration as they have the right to integrate into our society just as much as everyone else.”
IV. DISCUSSION
Our study showed positive change in attitudes towards PWD among medical students after a workshop with improvement of 9.29 points in the ATDP-O score (Table 1b), reinforced by their post-workshop reflections. To our knowledge, this is the first study in Asia evaluating an educational intervention focusing on communications skills training with PWD. Based on student reflections, the communications workshop was effective in developing knowledge and communication skills, prompting the key attitudes of humanizing care, and a call for action towards societal inclusivity and accessibility towards PWD.
We intentionally had PWD co-designing the workshop and playing key roles as patient educators. Student reflections support these curriculum design decisions. Our work coheres with literature that a contact-based approach with PWD would be impactful: reducing anxiety and improving empathy levels, rather than more theoretical approaches to promote attitudes towards PWD (Arabi et al., 2021).
Our study corroborates the widely reported result that female gender positively influenced baseline attitudes towards PWD in medical students (Satchidanand et al., 2012). A possible explanation is females having a propensity to exhibit more empathetic feelings toward others. There is a greater change in attitudes in males than females after the workshop, but this change is not significant.
In contrast to prior research that consistently associated increased contact with PWD with more positive attitudes (Satchidanand et al., 2012), we found that having previous experience with PWD influenced baseline ATDP-O scores negatively (Table 1a). Moreover, there was a significantly smaller change in ATDP-O scores if they knew a PWD who is important to them (Table 1b). A possible explanation is “caregiver fatigue” due to unavailability of support to allow adequate care for PWD (Arabi et al., 2021). The type of previous experience may thus be key factors in shaping current attitudes towards PWDs.
This study has several limitations. We cannot determine if positive change in attitudes post-workshop would translate into changes in clinical practice in the future. The survey was not compulsory for students, potentially leading to selection bias. We tried to overcome the selection bias by including all student reflections.
V. CONCLUSION
There was significant improvement in students’ attitudes towards PWD post-workshop, as shown through the ADTP-O score and reflection analysis. Medical students benefit particularly from the fishbowl discussions which allows students to interact with persons with disability, growing our future generations of healthcare professionals who humanise care.
Notes on Contributors
Author VLE conceptualised the study, developed the methodology, conducted the investigation, did the formal analysis and visualization of data, wrote the original draft, reviewed and edited the manuscript. Author JJ conceptualized the study, developed the methodology and original draft, reviewed and edited the manuscript. Author AS developed the methodology, did the formal analysis of data, reviewed and edited the manuscript. Author VVL did the formal analysis of data, wrote the original draft, reviewed and edited the manuscript. Author LSH did the formal analysis and visualization of data. Author FT did the formal analysis, reviewed and edited the manuscript. Author JMV supervised the conceptualization and methodology of the study, reviewed and edited the manuscript. VLO supervised the conceptualization of the study, developed the methodology, reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Ethical Approval
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of the National University of Singapore on 11 November 2022 (NUS-IRB-2022-608).
Data Availability
Quantitative data repository can be freely accessed at: https://doi.org/10.6084/m9.figshare.24013134
Qualitative data repository can be freely accessed at: https://doi.org/10.6084/m9.figshare.24051195
Funding
There was no funding for this research study.
Declaration of Interest
Authors VLE, JJ and VLO are tutors in the “Communications with Persons with Disabilities” workshop. There are otherwise no other conflicts of interest.
References
Ali, A., Nguyen, J., Dennett, L., Goez, H., & Rashid, M. (2023). A scoping review for designing a disability curriculum and its impact for medical students. Canadian Medical Education Journal, 14(3), 75–86. https://doi.org/10.36834/cmej.74411
Arabi, H., Adarmouch, L., & Ahmed Eladip, G. (2021). The assessment of student doctors’ attitude towards disabled people after teaching them a module. Acta Bio-Medica: Atenei Parmensis, 92(2), e2021059. https://doi.org/10.23750/abm.v92i2.9547
National Council of Social Service Singapore. (2019). Public Attitudes Towards Persons with Disabilities 2019. https://www.ncss.gov.sg/docs/default-source/ncss-publications-doc/pdfdocument/public-attitudes-towards-persons-with-disabilities-2019-infographics.pdf
Satchidanand, N., Gunukula, S. K., Lam, W. Y., McGuigan, D., New, I., Symons, A. B., Withiam-Leitch, M., & Akl, E. A. (2012). Attitudes of healthcare students and professionals toward patients with physical disability: A systematic review. American Journal of Physical Medicine & Rehabilitation, 91(6), 533–545. https://doi.org/10.1097/PHM.0b013e3182555ea4
Yuker, H. E., Block, J. R., & Campbell, W. J. (1960). A scale to measure attitudes toward disabled persons. In Human Resources Study Number 5. Human Resources Foundation.
*Vivien Lee
1E Kent Ridge Rd,
Singapore 119228
Email: vivienl@nus.edu.sg
Submitted: 3 April 2024
Accepted: 22 July 2024
Published online: 1 October, TAPS 2024, 9(4), 33-39
https://doi.org/10.29060/TAPS.2024-9-4/OA3282
Meltem Saygılı1, Aysun Kandemir Türe1 & Şirin Özkan2
1Department of Health Management, Kırıkkale University, Kırıkkale, Türkiye; 2Department of Medical Services and Techniques, Vocational School of Health Services, Uludag University, Türkiye
Abstract
Introduction: Many societal changes threaten the sustainability of health systems. Entrepreneurs play a significant role in creating sustainable innovations necessary for development and structural change. This study aimed to evaluate how university students studying health sciences perceive individual entrepreneurship during the COVID-19 pandemic and to explore the impact of COVID-19-related hopelessness on their perception of entrepreneurship.
Methods: Six hundred eighty-one undergraduate students from the faculty of health sciences in Türkiye, participated in the study. The Individual Entrepreneurship Perception Scale and Beck Hopelessness Scale were used to collect data.
Results: The results revealed that the students’ perception of individual entrepreneurship was high, while their hopelessness levels were moderate. In addition, a moderate negative relationship was found between the students’ hopelessness levels and their perception of individual entrepreneurship. The regression analysis showed that the students’ hopelessness levels and sub-dimensions (hope, loss of motivation, and future expectation) accounted for 26.3% of the total variance in individual entrepreneurship perception. Increased hopelessness regarding the sub-dimensions of hope, loss of motivation, and expectations for the future decreased their individual entrepreneurship perceptions.
Conclusions: These findings suggest that individual entrepreneurship perception among health sciences students could be negatively impacted during extraordinary periods related to health crises like pandemics. Developing hope, motivation, and expectations for the future is crucial to enhancing individual entrepreneurship perception among health sciences students.
Keywords: Individual Entrepreneurship Perception, Hopelessness, Health Sciences, University Students, COVID-19 Pandemic
Practice Highlights
- University education plays a critical role in developing students’ perceptions of entrepreneurship.
- Students’ perceptions of entrepreneurship are affected by changing environmental conditions.
- The COVID-19 pandemic has led to a significant increase in awareness of Healthcare Entrepreneurship.
- The COVID-19 pandemic has negatively affected students’ expectations and hopes for the future.
- Health sciences students experienced the psychological effects of the pandemic more intensely.
I. INTRODUCTION
Entrepreneurs are described as individuals who “implement bold new ideas from the outset, taking on the risks of the business or venture that enables innovation to happen” (Suryavanshi et al., 2020). Entrepreneurship education seeks to provide students with in-depth knowledge, motivation, and skills to increase entrepreneurial intentions’ success in various settings (Sampene et al., 2023). In developing economies such as Türkiye, government efforts to improve unemployment conditions are directed towards developing students’ positive attitudes towards entrepreneurship and increasing their interest in self-employment.
Universities are crucial in developing students’ entrepreneurial intentions (Bagheri, 2018). It is critical to examine and develop the entrepreneurial potential of university students trained to fulfill important roles in the field of health services in the future. This is because students and newly graduated healthcare professionals with entrepreneurial skills are now needed to develop innovative healthcare delivery models that can improve the quality of healthcare services, improve treatment outcomes, and reduce the cost of care (Fashami et al., 2021; Mohamed et al., 2023). It is stated that healthcare is one of the main industrial areas where user entrepreneurship takes place worldwide (Schiavone et al., 2020) and the pandemic environment brings unique opportunities for entrepreneurs, especially in healthcare. However, research shows that fear and worry due to the COVID-19 pandemic are making the future workforce anxious and hopeless about their professional futures (Duplaga & Grysztar, 2021; Tao et al., 2023). In such an environment, it is predicted that university students, especially those who are trained to work in health service delivery, may act in different ways in their decisions about their professional future.
Because an individual’s perception of current conditions can significantly, positively, or negatively affect the formation of entrepreneurial intentions and the likelihood of starting an enterprise (Krichen & Chaabouni, 2022). Considering the increasing entrepreneurship opportunities in healthcare and the negative effects of the COVID-19 pandemic on healthcare services, it has become important to address the entrepreneurship perceptions of students who will serve in this field in the future and to evaluate the hopelessness experienced. When the literature was examined, no other research addressing entrepreneurship in the context of hopelessness was found. Therefore, we believe that our research findings will make a valuable contribution to filling this gap in the literature.
A. Universities, Health Sciences Education and Entrepreneurship
Recent years have focused on the role of universities in industrial competitiveness and their impact on social change (Hart & Rodgers, 2023), and universities in teaching and initiating entrepreneurship have emerged as leading actors. Recent research examining students’ attitudes toward entrepreneurship reveals that universities have a critical role in developing entrepreneurial spirit and perceptions of entrepreneurship in students (Krichen & Chaabouni, 2022; Liao et al., 2022; Sampene et al., 2023). Moreover, university students now value real experience more and prefer universities that offer entrepreneurship opportunities and experiences (Taneja et al., 2024).
Universities providing education in healthcare have traditionally emphasised vocational training and unfortunately, there are very few university programs with curricula that focus on innovation and entrepreneurship in healthcare (Suryavanshi et al., 2020). Consequently, most newly graduated physicians and other healthcare professionals start their careers without the knowledge, experience, and courage to integrate their medical knowledge with the healthcare business world, and thus are unable to commercialise new healthcare delivery methods (Boore & Porter, 2011).
B. Hopelessness Experienced by Students Due to the COVID-19 Pandemic and Perception of Individual Entrepreneurship
Students are one of the groups that experience the psychological effects of the pandemic most intensely (Marahwa et al., 2022). Studies conducted with students during the pandemic period showed that students experienced higher levels of anxiety and depressive symptoms due to uncertainties about the future and the negative effects of the pandemic on their educational lives (Alnıaçık et al., 2021; Hajinasab et al., 2022; Kaplan Serin & Doğan, 2023; Zhang et al., 2021). Moreover, it was also determined that students’ hopelessness levels were higher in the first wave of the pandemic and during the quarantine period and decreased with normalisation (Tao et al., 2023). In addition, it has been found that students who are educated in the field of health and have clinical experience are more anxious and hopeless than undergraduate students who are educated outside the field of health (Pretorius, 2021). Although entrepreneurship is a future-oriented orientation and is perceived as the ability to turn negative situations into opportunities, it is estimated that the psychological effects of COVID-19 may negatively affect entrepreneurial intention in students. Therefore, this study aims to examine the effect of hopelessness experienced by health sciences faculty students during the COVID-19 pandemic on their perception of individual entrepreneurship.
II. METHODS
A. Sampling and Participants and Data Collection
The study was conducted with university students studying at the Faculty of Health Sciences in Türkiye. The faculty consists of six departments, namely Physiotherapy and Rehabilitation, Health Management, Social Work, Nutrition and Dietetics, Child Development and Nursing, and has 2335 students. The sample size required for the study was calculated using the formula (n=[z²xp(1-p)/d²]/1+[z²xp(1-p)/d²N]) and it was determined that a minimum of 337 participants would be sufficient with a 5% error level and 95% confidence level. Participants were selected using a simple random sampling technique and volunteerism was taken as a basis in obtaining the data. The study was conducted between April and May 2022 and 681 valid questionnaires were returned from the participating students.
Data were collected using the socio-demographic information form, Individual Entrepreneurship Perception Scale, and Beck Hopelessness Scale. The Individual Entrepreneurship Perception Scale is a 5-point Likert scale consisting of 31 items and six sub-dimensions: planning, locus of control, self-confidence, communication, motivation, and self-discipline. This scale was developed by Incik and Uzun in 2017 to assess university students’ perceptions of entrepreneurship. The reliability coefficients (Cronbach’s Alpha) of the sub-dimensions of the Individual Entrepreneurship Perception Scale and the total scale were found to be 0.80, 0.84, 0.75, 0.75, 0.75, 0.72, 0.75, 0.60 and 0.92, respectively (Incik & Uzun, 2017). For this study, it was determined that the Cronbach Alpha values of the Individual Entrepreneurship Perception Scale ranged between 0.69 and 0.93 (Table 2).
The Hopelessness Scale was initially developed by Beck et al. in 1974 and subsequently adapted into Turkish by Durak and Palabıyıkoğlu in 1994. This scale comprises 20 items divided into three sub-dimensions: expectations for the future, loss of motivation, and hope. Each question in the scale requires a ‘yes’ or ‘no’ response, and the maximum achievable score is 20. An increase in the overall score denotes a higher level of hopelessness. The reliability coefficients for the sub-dimensions of the scale were calculated to be 0.78, 0.72, and 0.72, respectively (Durak & Palabıyıkoğlu, 1994). Table 2 presents the Cronbach’s alpha coefficients for the sub-dimensions and the scale, which were found to be 0.75, 0.77, 0.74, and 0.88, respectively.
B. Statistical Analysis
The statistical analyses used were performed in SPSS v23.0. Descriptive analyses such as percentage, mean, standard deviation, reliability analysis (Cronbach’s Alpha), and normality tests were performed to obtain the results. To test the normal distribution, kurtosis, and skewness values were calculated for each scale’s sub-dimensions and total scores. It was determined that the values obtained were in the range of -1.5 to +1.5 and the data showed a normal distribution (Tabachnick & Fidell, 2013). The results of the analysis are presented in Table 2. In addition, multiple linear regression analysis was used to investigate the relationship between hopelessness and students’ perception of individual entrepreneurship.
III. RESULTS
The study involved students with an average age of 21.3 years, ranging from 18 to 44 years old. 86% of the participants were female students, and the majority (52.3%) reported a grade point average of 3 or above (with a scale of 0 to 4). 68.3% of the students lived in the city center with their families. Among the students’ mothers, 37.7% had a primary school graduate degree, and 81.4% were not working. On the other hand, 32.2% of the students’ fathers had a high school graduate degree, and 78.4% were actively working. Most of the students (68.3%) stayed in dormitories. Regarding career plans after graduation, most students expressed their interest in working in a health institution (public or private). At the same time, only 15.6% said they wanted to start their own business. 15% of the students were still undecided about their work plans (Table 1).
|
Variables |
n |
% |
Variables |
n |
% |
|
Department |
Place of Residence Outside Education |
||||
|
Health Management (HM) |
122 |
17.9 |
City Centre |
465 |
68.3 |
|
Nursing (HEM) |
124 |
18.3 |
District |
171 |
25.1 |
|
Child Development (CDE) |
114 |
16.7 |
Village |
45 |
6.6 |
|
Nutrition and Dietetics (ND) |
116 |
17.0 |
Education Level of Mother |
||
|
Physiotherapy and Rehabilitation (FTR) |
140 |
20.6 |
Illiterate |
23 |
3.4 |
|
Social Work (SW) |
65 |
9.5 |
Primary School |
257 |
37.7 |
|
Classroom |
Middle School |
171 |
25.1 |
||
|
Grade 1 |
159 |
23.4 |
High School |
178 |
26.2 |
|
Grade 2 |
188 |
27.6 |
University |
52 |
7.6 |
|
Grade 3 |
165 |
24.2 |
Education Level of Father |
||
|
Grade 4 |
169 |
24.8 |
Primary School |
173 |
25.4 |
|
Gender |
Middle School |
141 |
20.7 |
||
|
Woman |
585 |
85.9 |
High School |
219 |
32.2 |
|
Male |
96 |
14.1 |
University |
148 |
21.7 |
|
Age |
Employment Status of Mother |
||||
|
18-20 years old |
277 |
40.7 |
Working |
127 |
18.6 |
|
21-22 years old |
272 |
39.9 |
Not working |
554 |
81.4 |
|
23 years and older |
132 |
19.4 |
Employment Status of Father |
||
|
Academic Average |
Working |
534 |
78.4 |
||
|
2.99 and below |
260 |
38.2 |
Not working |
147 |
21.6 |
|
3 and above |
356 |
52.3 |
Income Status |
||
|
Total |
616 |
90.5 |
Scholarship |
190 |
27.9 |
|
Not specified |
65 |
9.5 |
Tuition loan |
211 |
31.0 |
|
Career Future Plan After Graduation |
Working |
51 |
7.5 |
||
|
I will definitely be working in an organization (public-private) |
225 |
33.0 |
Only my family supports me |
229 |
33.6 |
|
Where Do You Live During Your Education? |
|||||
|
I tend to be an employee in an organization (public-private) |
240 |
35.2 |
Dormitory |
465 |
68.3 |
|
Undecided |
102 |
15.1 |
Apart |
171 |
25.1 |
|
I tend to start my own business. I have my own business |
114 |
16.7 |
Home+ Staying with my family |
45 |
6.6 |
|
Total |
681 |
100 |
Total |
681 |
100 |
Table 1. Sociodemographic characteristics of the students
|
Variables |
Cronbach’s Alpha |
Mean |
SD |
Skewness |
Kurtosis |
|
Planning |
0.770 |
21.72 |
3.82 |
-0.271 |
0.233 |
|
Focus of Control |
0.810 |
30.96 |
4.73 |
1.141 |
1.157 |
|
Self Confidence |
0.792 |
23.42 |
3.86 |
-0.231 |
0.772 |
|
Communication |
0.694 |
15.54 |
2.57 |
0.880 |
0.424 |
|
Motivation |
0.709 |
15.18 |
2.78 |
-0.559 |
0.596 |
|
Self-Discipline |
0.726 |
11.14 |
2.31 |
-0.306 |
-0.031 |
|
Individual Entrepreneurship Perception Scale Total Score |
0.937 |
117.95 |
16.85 |
-0.406 |
0.899 |
|
Hope |
0.739 |
3.01 |
2.09 |
0.292 |
-0.991 |
|
Loss of Motivation |
0.766 |
3.76 |
2.33 |
0.295 |
-0.971 |
|
Future Expectations |
0.750 |
2.28 |
1.71 |
0.157 |
-1.273 |
|
Beck Hopelessness Scale Total Score |
0.885 |
9.06 |
5.36 |
0.232 |
-0.981 |
Table 2. Average scores of the participants from the Individual Entrepreneurship Perception Scale and Beck Hopelessness Scale
The data above show the mean scores of the participants obtained from the Individual Perception of Entrepreneurship Scale and Beck Hopelessness Scale used for the research. Despite the difficulties brought on by the pandemic and other negative experiences, students within the health sciences field scored high in individual entrepreneurship perception (Mean: 117.95±16.84 Min:44-Max:155). The study also found that the student’s level of hopelessness was moderate (Mean: 9.06±5.36 Min:0-Max:20) (Table 2).
|
Variables |
B |
SE |
β |
t |
p |
VIF |
|
(Constant) |
131.996 |
1.113 |
|
118.644 |
<.001 |
|
|
1. Hope |
-19.278 |
2.611 |
-.342 |
-7.383 |
<.001 |
1.974 |
|
2. Loss of Motivation |
-6.568 |
2.659 |
-.114 |
-2.470 |
.014 |
1.949 |
|
3. Future Expectations |
-5.830 |
2.589 |
-.119 |
-2.252 |
.025 |
2.547 |
|
R =0.513 R² =0.263 F =80.449 p<0.001 Durbin Watson=1.895 |
|
|||||
Table 3. Multiple Linear Regression Analysis results on hopelessness levels and its effect on individual entrepreneurship perception
*Criterion: Perception of Individual Entrepreneurship
In Table 3, the regression model proved significant and reliable (F=80.449; p<0.001), with the hopelessness levels and sub-dimensions of the participants accounting for 26.3% of the total variance in individual entrepreneurship perception. The study found that the participants’ hopelessness perceptions about the sub-dimensions of hope (t=-7.383; p<0.001), loss of motivation (t=-2.470; p=0.014), and expectations for the future (t=-2.252; p=0.025) had a statistically significant impact on their individual entrepreneurship perceptions. As participants’ levels of hopelessness increased, their individual entrepreneurship perceptions decreased. Based on the standardised regression coefficient (β), the predictor variables’ relative order of importance on individual entrepreneurship perception is hope (β=-0.342), expectations about the future (β=-0.119), and loss of motivation (β=-0.114) shown in Table 3.
IV. DISCUSSION
The results obtained from this study; health sciences students have a positive outlook on individual entrepreneurship despite the challenges created by the adverse conditions due to the pandemic. Studies conducted among health sciences students in Türkiye before the pandemic revealed that students’ perceptions of individual entrepreneurship were at a moderate level (Baltacı & Baydin, 2023; Göktekin et al., 2022). According to these results, it can be said that the pandemic process increased the awareness of individual entrepreneurship in students studying in the field of health sciences. This is a phenomenon that should be considered in discussions about current market trends and potential business opportunities.
In addition, this research revealed that students had moderate levels of hopelessness during the pandemic period. Although this result is slightly higher than the findings of a previous study conducted with associate degree students in Türkiye during the pandemic (Okur & Şentürk, 2022); similar results were obtained in studies conducted with undergraduate students of the faculty of health sciences in the international literature (Pretorius, 2021).
Finally, regression analysis findings showed that participants’ hopelessness levels and their sub-dimensions collectively explained 26.3% of the total variance in their individual entrepreneurship perceptions. This result suggests that hopelessness significantly affects students’ perceptions of entrepreneurship. Similarly, a study conducted with Chinese university students supports these findings by showing that the COVID-19 pandemic had a significant and negative impact on students’ entrepreneurial intentions and behaviors (Wang et al., 2023). However, this regression analysis result also implies that hopelessness caused by negative emotions during the pandemic cannot alone determine students’ perceptions of individual entrepreneurship. Other factors that may affect the individual entrepreneurship perceptions of students studying in the field of health sciences in similar health crises such as the COVID-19 pandemic should also be investigated.
Although it is stated that the pandemic period is full of opportunities for health entrepreneurship, it should be taken into consideration that entrepreneurial intention/perception is affected by many environmental factors. The related literature points out that ‘hope’ is a critical source of motivation for individuals who want to become entrepreneurs (Gódány et al., 2021). However, studies conducted during the pandemic period revealed that students perceived a high level of individual entrepreneurship risk (Krichen & Chaabouni, 2022). On the other hand, studies show that fear and anxiety caused by the COVID-19 pandemic negatively affect students’ perceptions of entrepreneurship (Loan et al., 2021). In particular, health sciences students are reported to experience higher levels of anxiety compared to other students studying in non-health fields, which leads to hopelessness and changes in career plans (Alnıaçık et al., 2021). Therefore, the results of this study are supported by the findings of previous studies.
V. CONCLUSION
Our research has shown that students who are trained to provide health services during periods of extraordinary health crises such as pandemics may experience hopelessness about their professional future and that students’ perceptions of individual entrepreneurship are negatively affected by this situation. The content and purpose of the university education received play a critical role in the development of students’ individual entrepreneurship perceptions.
Therefore, entrepreneurship courses should be carefully integrated into the curricula of all students studying in the field of health sciences, students should be motivated to take the course and encouraged to become entrepreneurs. In addition, interviews, company visits, and project studies with successful health entrepreneurs during similar crisis periods can increase students’ interest in health entrepreneurship and reduce their level of hopelessness. For a more comprehensive understanding of the relationships examined in the study, the inclusion of qualitative research methods in future studies may increase the depth of the analysis.
Notes on Contributors
MS, reviewed the literature, designed the research, analyzed data, co-wrote the manuscript, critically reviewed and edited the manuscript, and then read it through before final approval.
AKT, co-wrote the manuscript, and critically reviewed and edited the manuscript.
ŞÖ, prepared the manuscript for publication, critically reviewed, and edited the manuscript.
Ethical Approval
This study was conducted according to the ethical standards of the 1964 Declaration of Helsinki. Approval was obtained from Kırıkkale University Faculty of Health Sciences (Date: 30.03.2022; Number: E.88159) and Kırıkkale University Non-Interventional Research Ethics Committee (Date: 07.04.2022, Decision No: 2022.04.13).
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgment
All authors would like to thank all participants.
Funding
No financial support was received from any institution or organisation in the conduct and publication of this research.
Declaration of Interest
There is no conflict of interest between the authors.
References
Alnıaçık, E., Of, M., Balkaş, J., Tülemez, S., Mirzayev, M., & Alfarra, H. (2021). The effects of university students’ psychological resilience and hopelessness on their perception of career future during the pandemic process. Business & Management Studies: An International Journal, 9(1), 248-266. https://doi.org/10.15295/bmij.v9i1.1757
Bagheri, A. (2018). University students’ entrepreneurial intentions: Does education make a difference? In N. Faghih, & M. Zali (Eds.), Entrepreneurship education and research in the Middle East and North Africa (MENA) perspectives on trends, policy and educational environment: Contributions to management science (pp. 131-154). Springer. https://doi.org/10.1007/978-3-319-90394-1_8
Baltacı, N., & Baydin, N. Ü. (2023). Analysis of individual innovativeness, entrepreneurship, curiosity, and exploration characteristics of nursing students. Journal of Inönü University Vocational School of Health Services, 11(2), 1440-1454. https://doi.org/10.33715/inonusaglik.1164998
Beck, A. T., Weissman, A., Lester, D., & Trexler, L. (1974). The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology, 42(6), 861-865. https://doi.org/10.1037/h0037562
Boore, J., & Porter, S. (2011). Education for entrepreneurship in nursing. Nurse Education Today, 31(2), 184-191. https://doi.org/10.1016/j.nedt.2010.05.016
Duplaga, M., & Grysztar, M. (2021). The association between future anxiety, health literacy and the perception of the COVID-19 pandemic: A cross-sectional study. Healthcare, 9(1), 1–18. https://doi.org/10.3390/healthcare9010043
Durak, A., & Palabıyıkoğlu, R. (1994). Beck hopelessness scale validity study. Crisis Journal, 2(2), 311-319. https://doi.org/10.1501/Kriz_0000000071
Fashami, F. M., Nili, M., Farahani, A. V., Shaikh, N., Dwibedi, N., & Madhavan, S. S. (2021). Determining the entrepreneurial and intrapreneurial intentions of student pharmacists in Iran. American Journal of Pharmaceutical Education, 85(2), 113-122. https://doi.org/10.5688/ajpe8080
Gódány, Z., Machová, R., Mura, L., & Zsigmond, T. (2021). Entrepreneurship motivation in the 21st century in terms of pull and push factors. TEM Journal-Technology Education Management Informatics, 10(1), 334-342.https://doi.org/10.18421/TEM101-42
Göktekin, Z., Aslan, R., & Yildiz, E. (2022). Determination of the entrepreneurship levels of the students of the faculty of health sciences and the factors affecting these levels. Ahi Evran University Journal of Institute of Social Sciences, 8(2), 379-392. https://doi.org/10.31592/aeusbed.907637
Hajinasab, N., Amiri, M., Sharifi, M., Sanati, T., Dolatabadi, Z., & Amiri-Farahani, L. (2022). The relationship between social support and hopelessness among Iranian students during Coronavirus disease 2019 (COVID-19) pandemic. The Open Public Health Journal, 15(1), 1-9. https://doi.org/10.2174/18749445-v15-e2209290
Hart, P. F., & Rodgers, W. (2023). Competition, competitiveness, and competitive advantage in higher education institutions: A systematic literature review. Studies in Higher Education, 1–25. https://doi.org/10.1080/03075079.2023.2293926
Incik, E. Y., & Uzun, N. B. (2017). Validity and reliability study of individual entrepreneurship perception scale. Mustafa Kemal University Journal of Institute of Social Sciences, 14(39), 471-485. https://dergipark.org.tr/tr/pub/mkusbed/issue/31632/331276
Kaplan Serin, E., & Doğan, R. (2023). The relationship between anxiety and hopelessness levels among nursing students during the COVID-19 pandemic and related factors. OMEGA-J Death Dying, 87(3), 793-813. https://doi.org/10.1177/00302228211029144
Krichen, K., & Chaabouni, H. (2022). Entrepreneurial intention of academic students in the time of COVID-19 pandemic. Journal of Small Business and Enterprise Development, 29(1), 106-126. https://doi.org/10.1108/JSBED-03-2021-0110
Liao, Y. K., Nguyen, V. H. A., Chi, H. K., & Nguyen, H. H. (2022). Unraveling the direct and indirect effects of entrepreneurial education and mindset on entrepreneurial intention: The moderating role of entrepreneurial passion. Global Business and Organizational Excellence, 41(3), 23-40. https://doi.org/10.1002/joe.22151
Loan, L. T., Doanh, D. C., Thang, H. N., Nga, N. T. V., Van, P. T., & Hoa, P. T. (2021). Entrepreneurial behaviour: The effects of the fear and anxiety of COVID-19 and business opportunity recognition. Entrepreneurial Business and Economics Review, 9(3), 7-23. https://doi.org/10.15678/EBER.2021.090301
Marahwa, P., Makota, P., Chikomo, D. T., Chakanyuka, T., Ruvai, T., Osafo, K. S., Huang, T., & Chen, L. (2022). The psychological impact of COVID-19 on university students in China and Africa. PLoS ONE, 17(8), Article e0270824. https://doi.org/10.1371/journal.pone.0270824
Mohamed, M. E., Elshaer, I. A., Azazz, A. M., & Younis, N. S. (2023). Born not made: The impact of six entrepreneurial personality dimensions on entrepreneurial intention: Evidence from healthcare higher education students. Sustainability, 15(3), 2266-2278. https://doi.org/10.3390/su15032266
Okur, E., & Şentürk, A. Y. (2022). Coronavirus anxiety in vocational school students studying in the field of health in the coronavirus pandemic period. Journal of Adnan Menderes University Faculty of Health Sciences, 9(3), 499-512. https://doi.org/10.46237/amusbfd.978275
Pretorius, T. L. (2021). Depression among health care students in the time of COVID-19: The mediating role of resilience in the hopelessness–depression relationship. South African Journal of Psychology, 51(2), 269-278. https://doi.org/10.1177/0081246321994452
Sampene, A. K., Li, C., Khan, A., Agyeman, F. O., & Opoku, R. K. (2023). Yes! I want to be an entrepreneur: A study on university students’ entrepreneurship intentions through the theory of planned behavior. Current Psychology, 42(25), 21578-21596. https://doi.org/10.1007/s12144-022-03161-4
Saygılı, M., Kandemir Türe, A., & Özkan, Ş. (2022). The effect of hopelessness on individual entrepreneurship perception in health science students. Research Square. https://doi.org/10.21203/rs.3.rs-2381250/v1
Schiavone, F., Tutore, I., & Cucari, N. (2020). How digital user innovators become entrepreneurs: A sociomaterial analysis. Technology Analysis & Strategic Management, 32(6), 683-696. https://doi.org/10.1080/09537325.2019.1696955
Suryavanshi, T., Lambert, S., Lal, S., Chin, A., & Chan, T. M. (2020). Entrepreneurship and innovation in health sciences education: A scoping review. Medical Science Educator, 30, 1797-1809. https://doi.org/10.1007/s40670-020-01050-8
Tabachnick, B. G., & Fidell, L. S. (2013). Using multivariate statistics (6th ed.). Pearson Education.
Taneja, M., Kiran, R., & Bose, S. C. (2024). Assessing entrepreneurial intentions through experiential learning, entrepreneurial self-efficacy, and entrepreneurial attitude. Studies in Higher Education, 49(1), 98-118. https://doi.org/10.1080/03075079.2023.2223219
Tao, Y., Niu, H., Hou, W., Zhang, L., & Ying, R. (2023). Hopelessness during and after the COVID‐19 pandemic lockdown among Chinese college students: A longitudinal network analysis. Journal of Clinical Psychology, 79(3), 748-761. https://doi.org/10.1002/jclp.23439
Wang, J., Xu, M., Li, X., & Ni, Y. (2023). A latent class analysis of hopelessness in relation to depression and trauma during the COVID-19 pandemic in China. Journal of Affective Disorders, 329, 81-87. https://doi.org/10.1016/j.jad.2023.02.077
Zhang, Y., Bao, X., Yan, J., Miao, H., & Guo, C. (2021). Anxiety and depression in Chinese students during the COVID-19 pandemic: A meta-analysis. Frontiers in Public Health, 9, Article 697642. https://doi.org/10.3389/fpubh.2021.697642
*Meltem Saygılı
Department of Health Management,
Prof. Dr. Fuat Sezgin Health Campus
Faculty of Health Sciences
Kırıkkale University
71450 Merkez/Kırıkkale, Türkiye
+90 318 3423738/7732
Email: meltemsaygili@kku.edu.tr
Submitted: 21 February 2024
Accepted: 16 July 2024
Published online: 1 October, TAPS 2024, 9(4), 26-32
https://doi.org/10.29060/TAPS.2024-9-4/OA3255
Aletheia Chia1, Menghao Duan1 & Sashikumar Ganapathy2,3
1Paediatric Medicine, KK Women’s and Children’s Hospital, Singapore; 2Department of Emergency Medicine, KK Women’s and Children’s Hospital, Singapore; 3Paediatric Academic Clinical Programme, Duke-NUS Medical School, Singapore
Abstract
Introduction: Mentoring is an essential component of post-graduate medical training programs worldwide, with potential benefits for both mentors and mentees. While factors associated with mentorship success have been described, studies have focused on intrapersonal characteristics and are largely based in Western academic programs. Mentorship occurs in a broader environmental milieu, and in an Asian context, cultural factors such as respect for authority, hierarchy and collectivism are likely to affect mentoring relationships. We aim to explore the lived experience of mentors within an Asian postgraduate medical training program, and thus identify challenges and develop best practices for effective mentoring.
Methods: 14 faculty mentors from a post-graduate paediatric residency program were interviewed between October 2021 to September 2022. Data was collected through semi-structured one-on-one interviews, with participants chosen via purposeful sampling. Qualitative analysis was done via a systematic process for phenomenological inquiry, with interviews thematically coded separately by 2 independent reviewers and checked for consistency.
Results: 4 main thematic concepts were identified: “professional, but also personal”, “respect and hierarchy”, “harmony and avoidance of open conflict” and the “importance of trust and establishing a familial relationship”. Mentors also highlighted the value of structure in Asian mentoring relationships.
Conclusion: Cultural factors, which are deeply rooted in social norms and values, play an important role in shaping mentoring relationships in an Asian context. Mentoring programs should be tailored to leverage on the unique cultural norms and values of the region in order to promote career growth and personal development of trainees and mentors.
Keywords: Medical Education, Graduate Medical Education, Professional Development
Practice Highlights
- Cultural factors are key in shaping Asian mentoring relationships.
- This includes being ‘professional, but also personal’, ‘respect and hierarchy’, ‘harmony and avoidance of open conflict’ and the “importance of trust and establishing a familial relationship’.
- Mentoring programs should be tailored to leverage on the unique local cultural norms and values.
I. INTRODUCTION
Mentoring is an essential component of post-graduate medical training programs worldwide. Mentorship is a reciprocal, interdependent relationship between a mentor (often a faculty member who is senior and experienced) and a mentee (beginner or protégé in the field) (Sambunjak et al., 2006). Benefits for mentees include aiding career preparation, development of clinical and communication skills, independence, and preventing burnout (Flint et al., 2009; Ramanan et al., 2006; Spickard et al., 2002). Mentors derive satisfaction from aiding the next generation, motivation for ongoing learning and institutional recognition (Burgess et al., 2018).
Variables associated with mentoring success have been described. Key components identified by mentors and mentees are communication and accessibility, caring personal relationship, mutual respect and trust, exchange of knowledge, independence and collaboration, and role modelling (Eller et al., 2014). Personality differences, lack of commitment, conflict of interests and mentor’s lack of experience can contribute to unsuccessful mentoring relationships (Straus et al., 2013).
However, mentorship occurs in a broader environmental milieu. Sambunjak (2015) described an ecological model of mentoring in academic medicine, with a first societal level of cultural, economic and political factors; a second institutional level of system- and organisation-related factors, and a third level of intrapersonal and interpersonal characteristics. Studies on mentorship have mainly focused on the latter and are situated in Western academic programs. In an Asian context, cultural factors such as respect for authority, hierarchy and collectivism may affect mentoring relationships (Chin & Kameoka, 2019). Trainees may show more deference to their mentors, and mentors may be more directive than collaborative. An Asian study surveying Doha’s postgraduate paediatric program found 75% mentees unsatisfied in their mentoring relationship (Khair et al., 2015).
We aim to explore the lived experience of mentors within an Asian postgraduate medical training program, and thus identify the challenges faced by trainees and mentors and develop best practices for effective mentoring.
II. METHODS
A. Study Design
This qualitative study is based on an interpretive phenomenological approach of participants’ lived experiences in their mentoring relationships. Through close examination of individual experiences, phenomenological analysis seeks to capture the meaning and common features, or essences, of an experience (Starks & Trinidad, 2007).
Semi-structured interviews were conducted. The interview guide was designed to follow a pre-determined structure whilst allowing for flexibility in probing. It was based on insights from literature on key socio-cultural determinants of successful mentoring relationships. Data was collected until saturation, with no new themes emerging.
B. Setting
We studied a paediatric residency program of a tertiary academic centre in Singapore, with 47 residents and 180 faculty members.
A formal mentorship program (Figure 1) has been in place since 2010. Residents indicate preferred faculty mentors at the start of residency, and are advised to consider specialty of interest, characteristics, and gender. Matches are subject to availability, review by the residency program, and mentor acceptance. Residents have one formal mentor throughout the 6 years unless the mentorship is terminated by mutual agreement between mentor and mentee.
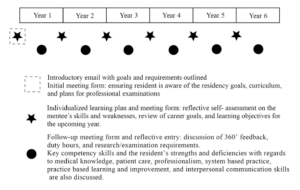
Figure 1. Mentorship program structure, with suggested meeting timings and requisite forms. Meetings are required minimally 6-monthly and are scheduled on an ad-hoc basis by the mentor and mentee.
C. Participants
Purposive sampling to identify mentors in the residency program who would provide comprehensive and relevant insights. Considerations included age, gender, race, and years of mentorship and faculty experience. Study members and their mentors were excluded.
Study information sheets were provided to participants with assurance of confidentiality, and written informed consent obtained from each participant. The study was approved by the SingHealth Institution Review Board.
D. Analysis
Qualitative analysis was done via a systematic process for phenomenological inquiry (Creswell & Creswell, 2022), whereby statements were analysed and categorised into clusters of meaning that represent phenomenon of interest. Transcripts were interpreted independently by 2 reviewers (AC, MD) and reviewed by a 3rd study member (SG). Iterative data analysis and collection was performed, with coding done after each interview to identify new themes and inform further interviews.
III. RESULTS
We interviewed 14 mentors from October 2021 to September 2022. 8 were male and 6 were female. 12 were Chinese, 1 Indian, and 1 of other ethnicity. This was representative of faculty demographics. Mentors had two to eleven years of mentorship experience within the program, and one to five existing and prior mentees.
Mentors described their lived experiences in their mentoring journey, providing insights into key values and their relationships’ evolution. 4 main thematic concepts were identified: “professional, but also personal”, “respect and hierarchy”, “avoidance of open conflict” and the “importance of trust”. Mentors also highlighted the value of structure in Asian mentoring relationships.
A. Professional, but also Personal
All mentors agreed that the relationship was predominantly professional, with their key role being that of professional and career guidance. They described their roles as:
“Guidance through difficult decisions or challenges” (#1), “leaning the real world of medicine” (#2), “driving professional development” (#12) and providing “timely and wise advice to support the journey” (#13)
Relationships “predominantly focused on professional or educational aspects… as that’s what it was meant to be” (#10), and were “mainly limited to career-related matters (#11)”.
However, many also identified personal connection as key. While the focus was primarily professional, awareness of personal or emotional aspects aided in understanding their mentors to further professional development and psycho-emotional growth. This included sharing of family lives, and emotional difficulties faced at work.
As the journey progresses it becomes a lot more about the psycho-emotional aspect, and about their mental health and personal well-being. (#1)
A lot of time is spent discussing family issues. If we knew more about the personal life of our mentee it’s so much easier to tailor the advice based on the individual’s unique circumstances. (#3)
A minority of mentors kept their relationship strictly professional and preferred not to talk about aspects outside of work, as it was ‘easier’ (#10) and shared concerns of ‘overstepping certain norms’ (#11).
B. Respect and Hierarchy
Respect was a key factor brought up when exploring the socio-cultural aspects of mentoring in our Asian community. Mentors varied in their opinion as to the extent that this resulted in a hierarchical relationship, and if this had a negative or positive impact on the relationship.
All agreed that respect is a key value in mentoring relationships:
Culturally there’s a large part to play as we’re taught to respect our elders. (#1)
Respecting elders – definitely it’s more prominent in our Asian culture. (#2)
Many mentors highlighted that this resulted in a hierarchical relationship. This manifested in the way senior doctors were addressed strictly by title, polite communication, and consideration of what would be ‘proper’ to discuss or ask a mentor to do.
The hierarchical kind of mindset is still very strong, and is something that is not necessarily healthy. (#4)
You would always see your mentor as someone higher than you. It’s similar to the way in our Asian context we see our parents. a certain sense of distance (#11).
The way medicine is a 师傅徒弟 kind of thing (‘master and disciple’) (#13)
Many shared that this could be a barrier to open communication with juniors wanting to “respect and agree” with their mentors (#14), slowing the growth of some relationships.
No matter how much honesty and trust there is. If they want to say something that their mentor is not happy to hear, or strikes them as being a bit rude or disrespectful – they won’t say it. (#1)
Our culture does say to respect your senior, don’t argue and don’t disagree with your senior. Sometimes they’re not very vocal, ‘ok sir ok sir’. And then later you find out they have certain issues. (#9)
One mentor felt that hierarchy did not play a large part in his mentoring relationships. This was possibly personality related, describing himself as naturally “quite informal”.
Mentors also highlighted factors that mitigated the hierarchical nature of their relationship. This included time, and setting clear boundaries and goals of the relationship.
When we give… a clear boundary and aim with no go zones, then culture may not necessarily be that important anymore (#10)
A minority of mentors felt that hierarchy and respect was not a limiting factor in their relationships:
If the primary aim is having someone to offer you guidance and a different point of view, even if the mentee sees you as someone who is not equal, you can still have that effectiveness. (#11)
C. Harmony, Avoiding Open Conflict and Confrontation
Another socio-cultural concept highlighted was the avoidance of confrontation. While some of this was linked to avoiding disagreements given the hierarchical nature of the relationship, avoiding open conflict and striving for harmony was also a key factor.
Rather than openly bringing up something, to avoid being confrontational we have evolved other means of trying to work our way through that conflict. There is a conscious and deliberate effort to avoid open and confrontational conflict. (#3)
When I was in the UK, they really questioned their mentors quite a lot – almost like a quarrel. That kind of questioning style may not be that well received in our own culture. (#2)
When mentees had differing opinions from their mentors “they would rather not talk about the topic again, or just ask someone else” in order to preserve the relationship (#1).
Within our program, this resulted in difficulties in exiting the relationship to avoid “offending” the mentor:
When the mentor-mentee relationship is breaking down, culturally it can be more difficult for mentees to request to swap. That’s very detrimental to both the mentor and the mentee in the long run. (#1)
This also manifested in avoiding overly ‘emotional’ discussions, with discussion often being more “superficial”, “reserved” (#7) and “factual” (#5) in nature.
Conversely, one mentee shared that younger mentees being of a “younger generation” were more open to speaking their mind, and that this would continue to evolve.
D. Importance of Trust and Establishing a Familial Relationship
In exploring key values for successful mentoring relationships, many highlighted the importance of trust and building up an established relationship.
Chemistry and compatibility when starting out was key. Mentors often felt more comfortable if there was a pre-existing relationship they had their mentors and had “shared commonalities and chemistry”. Honesty and trust were key in enabling the relationship to progress. This included respecting each other’s confidentiality. Relationships without trust was difficult as mentors “had to keep guessing what they want”, and “whatever you plan may not be the real goals of what they actually want” (#2). Over time, establishing the relationship made it easier to confide in each other, overcoming boundaries brought on by hierarchy.
It’s about forming relationships before you can start reflecting with the person. Over time we get to know each other, and seeing that what is shared is truly kept private and confidential. Once we have trust among each other it (reservations) doesn’t become a barrier. (#7)
There must be a certain comfort and trust level before one readily does share vulnerabilities. (#2)
This can be enabled by being approachable, and creating safe environments where mentors can share their difficulties without consequence. However, this could be compromised if mentors have to take up a supervisory role or be involved in remediation processes.
Mentors who developed close and trusting relationships with their mentees described it as familial in nature. This could be as a big brother or sister who would give advice to their younger siblings in non-threatening and neutral ways. It was also described by one mentor as parental in nature.
One interviewer highlighted that whilst Asian cultural factors may limit mentoring, there were also potential benefits:
We must find the best of both worlds. The independence that the Western systems have is good, but Asians tend to be better at teamwork and team spirit. (#13)
E. Value of Structure in an Asian Mentorship Relationship
Many mentors highlighted the value of having a framework for their mentoring relationship. Formalisation of the relationship and having a structure provided a foundation for discussions and enabled them to set boundaries. This prevented it from becoming awkward or “random and situation-based” (#15), and also helped faculty who were “still learning the whole journey of mentoring” (#7).
When we don’t know what to talk about it becomes quite awkward and uncomfortable. But if in the Asian context the mentor brings to it some structure, and they respect that structure, that structure is helpful. (#10)
A minority of mentors felt having a framework was too rigid or unnecessary.
The structure must be there to guide the mentors, but the mentors chosen must also be of a certain maturity so they can find their own way. We must not be too prescriptive or rigid. (#13)
IV. DISCUSSION
In this study, we explored the lived experiences of mentors within an Asian paediatric postgraduate training program. Existing studies have explored characteristics of effective and ineffective mentor relationships, but less is known about the impact of sociocultural factors. Key thematic concepts identified such as “respect and hierarchy” and “avoidance of open conflict” highlighted the importance of cultural factors in shaping mentoring relationships in an Asian context. These are deeply rooted in social norms and values of the region.
Hierarchy is a fundamental aspect of many Asian cultures, where individuals are expected to show respect and deference to their ‘elders’ or those in positions of authority. This was also observed in other Asian communities. A study in postgraduate medicine in Japan found that mentees had an inner desire to “respect the mentor’s ideas”, with both mentees and mentors embracing “paternalistic mentoring” (Obara et al., 2021). In our interviews, this was most apparent in the way mentees addressed their mentors: by title and respectfully. On a deeper level, this was a barrier to open communication. Open sharing was identified as crucial for a constructive mentoring relationship (Burgess et al., 2018), with the lack of it a cause of failed mentoring relationships (Straus et al., 2013). The willingness to share personal experiences by both mentors and mentees is key for effective mentoring and career growth. Additionally, this is not conducive to fostering creativity and innovation, which are increasingly important in the medical profession.
Communication was also affected by avoidance of open conflict and confrontation. Asian cultures have been described as collectivist, where the needs of the group take precedence over that of the individual, and intragroup harmony is paramount (Chin & Kameoka, 2019). In mentoring relationships, this translates to prioritising a successful and harmonious relationship over personal goals. Indirect communication styles are also more common in many Asian cultures. This has been described as high-context communication, whereby “most of the information is either in the physical context or internalised in the person, while very little is in the coded, explicit, transmitted part of the message” (Hall, 1976). Relying on indirect language nonverbal cues rather than explicitly stating one’s thoughts and feelings can hinder open communication.
Hierarchy and a lack of open communication may result in mentors taking on the role of advisors or coaches rather than true mentors. While there is no universal definition of mentorship, key features are that of a long-term dyadic relationship that encompasses educational, training and professional aspects that is personal and reciprocal (Sambunjak & Marusic, 2009). This is in contrast to tutors or coaches that primarily exhibit educational functions, or counsellors that exhibit personal functions. If the mentor-mentee relationship if influenced by hierarchical norms, mentors may be seen as figures of authority rather than partners in development. Cultural respect for authority figures and an emphasis on conformity may also discourage mentees from questioning or having open conversations with their mentors, limiting mutual learning.
Challenges with hierarchy and communication can be overcome with the aid of a structured program, and eventually establishment of trust and ‘familial’ relationships. A structured program can guide mentors and mentees in having open communication. In an Asian context, mentors may initially play a more authoritative role in guiding and directing their mentees with the aid of a structured guide, from which more two-way communication may open up as the relationship becomes more established. Whilst desirable mentors have characteristically been described as not “bossy” or authoritative (Sambunjak & Marusic, 2009), a study of Japanese physician-scientist mentor-mentees viewed more paternalistic mentoring as favourable (Obara et al., 2021). However, this will need to be individualised, as a highly directive mentoring style may not be well-suited to those who prefer a more collaborative and participatory mentoring relationship. Communication and learning styles may also continue to evolve with as incoming trainee physicians belong increasingly to Generation Z (1997-2012) instead of Generation Y/Millennials (1981-1996). A study of the mentorship experiences of Gen Z women medical students by Li et al (2024) described how current society had afforded them more opportunities for empowerment and expression, and emphasised the importance of tailored mentorship that considered the mentee’s identify and intersectionality.
Having mutual respect and trust were also key. The mentee and mentor having a pre-existing relationship and familiarity helped, and was more common in our context given that mentees could indicate their mentor of interest. Mutual respect and having a personal connection were also identified as key components in effective mentoring relationships by Eller (2014) and Straus (2013).
Whilst we had initially hypothesised that Asian sociocultural concepts would limit mentorship relationships to be largely professional, mentors shared that mutual respect, trust, and time enabled the relationship to also extend to sharing of personal matters and psychosocial wellbeing. Successful relationships were even described as ‘familial’, with a sense of fulfilment from both parties. A family-like relationship and a sense of loyalty to the mentor and organisation was also described in Japanese mentoring relationships (Obara et al., 2021). Such relationships may be more common in more collectivist cultures. These can be furthered by fostering a sense of community amongst mentees and mentors, such as through group activities, peer support, and shared learning experiences.
A. Limitations
This study was conducted in one of the two paediatric training centres in Singapore. Future studies should expand to other postgraduate programs to improve applicability of the results.
The investigators were participants in the program as mentees or mentors, with potential for bias in analysis. To minimise this, transcripts were analysed independently by two investigators followed by review by the third investigator. While our study focused on the lived experience of mentors, examining the perspective of mentees would be able to provide a more balanced and comprehensive understanding of mentoring relationships and highlight gaps where they can be better supported, and should be considered in future studies.
Our study did not delve into gender dynamics. Female medical trainees may face unique challenges, and male mentors may be stereotypically less nurturing and more process-oriented. Existing studies are varied: a survey of American cardiologists found sex concordance to be beneficial (Abudayyeh et al., 2020), whereas Jackson (2003) did not find same-gender matching to be important in an US academic program. In our initial interviews, gender did not come up as a significant factor and was hence not a focus subsequently. The role of gender in our program may have been minimised by a balanced gender ratio, with 59% of faculty female.
B. Future Research and Practical Implications
Given the significant influence of sociocultural factors on mentoring relationships, mentoring programs should be tailored to reflect the unique cultural norms and values of the region. In Asian cultures, this would include methods to reduce hierarchy, ensuring accessibility to mentors, and having a structured program. Training on mentorship for mentors and mentees would be beneficial to promote characteristics of effective mentoring relationships, and should include a focus on culturally sensitive mentoring with a recognition of how culturally-shaped beliefs can affect mentorship. This is particularly important in multicultural societies where cross-cultural mentorship is more common.
V. CONCLUSION
Cultural factors play an important role in shaping mentoring relationships in an Asian context. Whilst such these may be limiting to a degree, these can be also be leveraged on to further effective mentoring programs. Mentoring programs should be tailored to reflect the unique cultural norms and values of the region to promote career growth and personal development of trainees and mentors.
Notes on Contributors
AC, MD and SG contributed to study conception and design. Participant interviews were conducted by AC. Analysis and thematic interpretation were done by AC, MD with review by SG. All authors were involved in drafting the manuscript and reviewing it critically, and all read and approved the final manuscript.
Ethical Approval
The study was approved by the SingHealth Institution Review Board (IRB number 2021/2542).
Data Availability
The data of this qualitative study are not publicly available due to confidentiality agreements with the participants.
Funding
No funding was received for conducting this study.
Declaration of Interest
The authors declare that they have no competing interests.
References
Abudayyeh, I., Tandon, A., Wittekind, S. G., Rzeszut, A. K., Sivaram, C. A., Freeman, A. M., & Madhur, M. S. (2020). Landscape of mentorship and its effects on success in cardiology. JACC: Basic to Translational Science, 5(12), 1181-1186. https://doi.org/10.1016/j.jacbts.2020.09.014
Burgess, A., van Diggele, C., & Mellis, C. (2018). Mentorship in the health professions: A review. The Clinical Teacher, 15(3), 197-202. https://doi.org/10.1111/tct.12756
Chin, D., & Kameoka, V. A. (2019). Mentoring Asian American scholars: Stereotypes and cultural values. American Journal of Orthopsychiatry, 89(3), 337-342. https://doi.org/10.1037/ort0000 411
Creswell, J. W., & Creswell, J. D. (2022). Research design: Qualitative, quantitative, and mixed methods approaches. SAGE Publications.
Eller, L. S., Lev, E. L., & Feurer, A. (2014). Key components of an effective mentoring relationship: A qualitative study. Nurse Education Today, 34(5), 815-820. https://doi.org/10.1016/j.nedt. 2013.07.020
Flint, J. H., Jahangir, A. A., Browner, B. D., & Mehta, S. (2009). The value of mentorship in orthopaedic surgery resident education: The residents’ perspective. The Journal of Bone and Joint Surgery, 91(4), 1017-1022. https://doi.org/10.2106/JBJS.H.00934
Hall, E. T. (1976). Beyond culture. Anchor Press/Double Day.
Jackson, V. A., Palepu, A., Szalacha, L., Caswell, C., Carr, P. L., & Inui, T. (2003). “Having the right chemistry”: A qualitative study of mentoring in academic medicine. Academic Medicine, 78(3), 328-334. https://doi.org/10.1097/00001888-200303000-00020
Khair, A. M., Abdulrahman, H. M., & Hammadi, A. A. (2015). Mentorship in pediatric Arab board postgraduate residency training program: Qatar experience. Innovations in Global Health Professions Education. https://doi.org/10.20421/ighpe2015.6
Li, C., Veinot, P., Mylopoulos, M., Leung, F. H., & Law, M. (2024). The new mentee: Exploring Gen Z women medical students’ mentorship needs and experiences. The Clinical Teacher, 21(3), e13697. https://doi.org/10.1111/tct.13697
Obara, H., Saiki, T., Imafuku, R., Fujisaki, K., & Suzuki, Y. (2021). Influence of national culture on mentoring relationship: A qualitative study of Japanese physician-scientists. BMC Medical Education, 21(1), 300. https://doi.org/10.1186/s12909-021-02744-2
Ramanan, R. A., Taylor, W. C., Davis, R. B., & Phillips, R. S. (2006). Mentoring matters: Mentoring and career preparation in internal medicine residency training. Journal of General Intermal Medicine, 21(4), 340-345. https://doi.org/10.1111/j.1525-1497.20 06.00346.x
Sambunjak, D. (2015). Understanding wider environmental influences on mentoring: Towards an ecological model of mentoring in academic medicine. Acta Medica Academica, 44(1), 47-57. https://doi.org/10.5644/ama2006-124.126
Sambunjak, D., & Marusic, A. (2009). Mentoring: What’s in a name? JAMA, 302(23), 2591-2592. https://doi.org/10.1001/jama. 2009.1858
Sambunjak, D., Straus, S. E., & Marusic, A. (2006). Mentoring in academic medicine: A systematic review. JAMA, 296(9), 1103-1115. https://doi.org/10.1001/jama.296.9.1103
Spickard, A., Gabbe, S. G., & Christensen, J. F. (2002). Mid-career burnout in generalist and specialist physicians. JAMA, 288(12), 1447-1450. https://doi.org/10.1001/jama.288.12.1447
Starks, H., & Trinidad, S. B. (2007). Choose your method: A comparison of phenomenology, discourse analysis, and grounded theory. Qualitative Health Research, 17(10), 1372-1380. https://doi.org/10.1177/1049732307307031
Straus, S. E., Johnson, M. O., Marquez, C., & Feldman, M. D. (2013). Characteristics of successful and failed mentoring relationships: A qualitative study across two academic health centers. Academic Medicine, 88(1), 82-89. https://doi.org/10.1097/ACM.0b013e31827647a0
*Dr Aletheia Chia
Department of Paediat,
KK Women’s and Children’s Hospital
100 Bukit Timah Road
Singapore 229899
Email: aletheia.chia@mohh.com.sg
Submitted: 8 January 2024
Accepted: 2 July 2024
Published online: 1 October, TAPS 2024, 9(4), 14-25
https://doi.org/10.29060/TAPS.2024-9-4/OA3212
Hema Suryavanshi1, Santosh R Patil2, Kaladhar Reddy Aileni3 & Mohmed Isaqali Karobari4
1Department of Oral Pathology and Microbiology, Chhattisgarh Dental College & Research Institute, India; 2Department of Oral Medicine and Radiology, Chhattisgarh Dental College & Research Institute, India; 3Department of Preventive Dentistry, College of Dentistry, Jouf University, Kingdom of Saudi Arabia; 4Dental Research Unit, Centre for Global Health Research, Saveetha Institute of Medical and Technical Sciences, India
Abstract
Introduction: Oral health education is essential for adolescents, yet traditional methods face challenges in engaging this demographic. This study evaluates the effectiveness of a multimedia-based dental education program among high school students. This study was carried out to assess the impact of a comprehensive multimedia-based dental education program on oral health knowledge and practices among high school students.
Methods: A total of 228 students were recruited and randomly assigned to experimental (n=114) and control (n=114) groups. The experimental group received a four-week multimedia program, while the control group followed the standard curriculum. Outcome measures included oral health knowledge scores, brushing frequency, flossing habits, dietary choices, and observational assessments. Statistical analysis employed descriptive statistics, paired t-tests, and analysis of covariance (ANCOVA).
Results: The multimedia-based program led to a significant increase in oral health knowledge scores in the experimental group compared to the control group (Mean Change: 14.6, p < 0.001). Moreover, the experimental group demonstrated higher brushing frequency (p < 0.001), increased flossing habits (p < 0.001), and improved dietary choices (p < 0.05). Observational assessments showed higher adherence to oral hygiene practices in the experimental group (p < 0.001).
Conclusion: The multimedia-based dental education program effectively improved oral health knowledge and practices among high school students. This approach holds promise for scalable and engaging oral health education strategies.
Keywords: Multimedia-based Education, Oral Health, Adolescents, Dental Education, Health Promotion, Preventive Dentistry
Practice Highlights
- Integrated multimedia elements enhanced participant engagement, utilising videos, e-learning modules, and pamphlets.
- Positive shifts in oral health practices observed, with increased brushing and flossing frequencies in the experimental group.
I. INTRODUCTION
Oral health education serves as a cornerstone in empowering adolescents with the knowledge and skills necessary to maintain optimal oral hygiene. By educating young individuals about the importance of regular brushing, flossing, and dental check-ups, as well as the impact of dietary choices on oral health, preventive practices can be instilled early on. This not only helps in preventing common dental problems like cavities and gum disease but also promotes overall health and quality of life (Nakre & Harikiran, 2013).
Furthermore, addressing oral health education during adolescence is strategic as it provides an opportunity to intervene during a critical developmental stage. By targeting adolescents with effective educational interventions, it becomes possible to shape behavior and instill healthy habits that can last a lifetime. This proactive approach not only benefits the individual’s oral health but also reduces the burden on healthcare systems by minimising the need for costly and invasive dental treatments later in life (Tadin et al., 2022).
The increasing prevalence of dental problems presents a significant public health challenge, as untreated oral diseases can lead to pain, discomfort, and even serious complications such as tooth loss, systemic infections, and impaired overall health (Texas Dental Association, 2008). Moreover, dental problems impose a substantial economic burden on healthcare systems, with costs associated with treatment, emergency care, and lost productivity. In light of these challenges, effective educational interventions are crucial for curbing the burden of oral diseases (Ghoneim et al., 2022). Oral health education programs aim to raise awareness about the importance of oral hygiene, preventive measures, and regular dental check-ups. By providing individuals with the knowledge and skills necessary to maintain good oral health practices, these interventions can empower them to take proactive steps to prevent dental problems and minimise their impact (Kassebaum et al., 2017). This study addresses this need by investigating the impact of a multimedia-based dental education program on the oral health knowledge and practices of high school students.
Adolescence represents a critical period for establishing lifelong health behaviors, and oral health is no exception (National Institutes of Health, 2021). Unfortunately, global studies indicate a concerning prevalence of dental issues among adolescents, including dental caries, gingivitis, and poor oral hygiene practices (Agbelusi & Jeboda., 2006, Zhang et al., 2021). Such issues not only impact immediate health but can also lead to long-term consequences, emphasising the urgency of effective oral health education.
Traditional oral health education methods often face challenges in engaging and effectively conveying information to adolescents. Conventional classroom lectures and textbook-based approaches may struggle to capture the attention of this demographic, potentially limiting the efficacy of such interventions. However, there is evidence to suggest that traditional oral health education has been effective in improving oral health knowledge (Angelopoulou et al., 2015), reducing plaque accumulation, and promoting oral health in adolescents (Gousalya et al., 2022). On the other hand, it is important to note that traditional models of oral health education have been criticised for their didactic delivery and failure to acknowledge the individual context and motivations of the recipients (Ford & Farah., 2012).
As technology becomes increasingly integrated into daily life, leveraging multimedia platforms for health education emerges as a promising strategy to enhance engagement and knowledge retention (George et al., 2014).
The primary objective of this study was to assess the effectiveness of a comprehensive multimedia-based dental education program in improving oral health knowledge and promoting positive oral hygiene practices among high school students. By employing a well-structured intervention and rigorous evaluation, this research aims to contribute valuable insights that can inform the design and implementation of future oral health education initiatives.
The significance of this study lies in its potential to inform evidence-based oral health education strategies for adolescents, especially in regions facing resource constraints. If successful, the multimedia-based approach could serve as a scalable and cost-effective model for widespread implementation in school settings. Ultimately, the outcomes may contribute not only to the improvement of oral health outcomes among adolescents in the study setting but also to the development of best practices with broader implications for global oral health promotion.
II. METHODS
A. Intervention
A comprehensive multimedia-based dental education program was developed by a team of experienced dental educators, multimedia designers, and content developers. The program included visually engaging educational videos covering various aspects of oral health, interactive e-learning modules to reinforce key concepts, and informative pamphlets providing supplementary written material.
Throughout the intervention period, the research team closely monitored the attendance and participation of students in both the experimental and control groups. Attendance records, completion rates of e-learning modules, and participation levels in interactive sessions were meticulously documented to assess the program’s adherence.
1) Program feedback and modification: Continuous feedback sessions were held with both students and educators to evaluate the effectiveness of the multimedia-based dental education program. Adjustments and modifications were made in real-time based on feedback received, ensuring the program remained dynamic and responsive to the specific needs and preferences of the participants.
2) Quality assurance: To maintain consistency and quality across program delivery, educators underwent training sessions, and periodic evaluations were conducted to assess their adherence to the prescribed curriculum and teaching methodologies.
B. Study Design
A randomised controlled trial was conducted involving 228 high school students, aged 14 to 18, recruited from four local high schools in Burhanpur, India, after obtaining permission from the school authorities. Institutional Review Board (IRB) approval with approval number GGSCDS&RC/2022/IEC/168 was obtained prior to the start of this study. Students and their parents/guardians were provided with detailed information about the study, and informed consent was obtained from all participants. The study was conducted between January 2022 and December 2023.
A sample size calculation was conducted prior to the initiation of the study to ensure adequate statistical power. Based on previous literature and anticipated effect sizes, the calculation indicated that a sample size of 228 participants would provide sufficient power to detect significant differences in oral health knowledge and practices between the experimental and control groups. Factors such as an alpha level of 0.05, a power of 0.80, and an effect size estimate derived from similar interventions were taken into consideration during the calculation. This approach ensured that the study was adequately powered to detect meaningful differences in the outcomes of interest.
Random assignment of participants to the experimental and control groups was performed using a computer-generated randomisation sequence. The sequence was generated by an independent researcher not directly involved in the implementation of the study. Participants were assigned to the experimental or control group based on their identification numbers, ensuring an equal chance of allocation to either group. This randomisation process helped minimise selection bias and ensure that any differences observed between the groups could be attributed to the intervention rather than systematic differences in participant characteristics.
Given that participants were recruited from multiple local high schools in Burhanpur, India, cluster randomisation was employed to minimise contamination between groups. High schools were considered as clusters, and randomisation was carried out at the school level to prevent potential contamination of intervention effects between students within the same school. This approach helped maintain the integrity of the study design and reduce the risk of cross-group contamination, thereby enhancing the internal validity of the findings.
To address potential biases related to academic performance, we collected demographic information from all participants, including indicators of academic achievement. This information allowed us to assess any confounding variables during data analysis. Additionally, randomisation was employed to ensure that participants with varying academic backgrounds were equally distributed between the experimental and control groups, minimising the impact of academic performance on study outcomes.
1) Experimental group (n=114): Prior to the intervention, informed consent was obtained from both students and their parents/guardians. The multimedia-based dental education program was delivered to the experimental group during regular school hours. The intervention spanned four weeks, with carefully structured sessions designed to cover topics such as oral anatomy, proper brushing and flossing techniques, the impact of diet on oral health, and the importance of regular dental check-ups. Each week, students participated in interactive discussions, watched educational videos, completed e-learning modules, and received informational pamphlets to reinforce the acquired knowledge. To ensure engagement and understanding, the program incorporated quizzes, group activities, and open discussions facilitated by trained dental educators.
2) Control group (n=114): The control group received the standard oral health education provided as part of the existing school curriculum. The standard curriculum included traditional classroom lectures, textbook readings, and basic demonstrations of oral hygiene practices. No additional multimedia resources were introduced to the control group to maintain a clear distinction from the experimental group.
C. Development of Survey Instrument
The survey instrument utilised for baseline assessment underwent a rigorous validation process to ensure its reliability and validity in measuring participants’ oral health knowledge. The validation process included several key steps aimed at enhancing the quality and accuracy of the survey instrument.
The survey items were delved based on an extensive review of existing literature on oral health knowledge among adolescents. Content experts in the fields of dentistry, public health, and education were consulted to ensure that the survey items adequately covered essential concepts related to oral health.
Prior to the commencement of the main study, a pilot test of the survey instrument was conducted with a small group of high school students similar to the study population. Feedback from the pilot test participants was carefully analysed, and adjustments were made to the wording and clarity of the survey items based on their input.
The survey instrument underwent thorough review by a panel of experts comprising professionals from diverse backgrounds, including dentistry, education, and survey design. The expert panel assessed the relevance, comprehensibility, and appropriateness of the survey items for the target population, providing valuable feedback for further refinement.
D. Outcome Measurements and Analysis
In this study, a comprehensive set of outcome measures was employed to assess the impact of the intervention on participants’ oral health knowledge and practices. The study commenced with a baseline assessment, during which demographic data, oral health history, and participants’ knowledge of oral health practices were collected. Throughout the four-week intervention period, participants’ oral health practices were evaluated weekly through self-reports and observations, ensuring continuous monitoring of their adherence and engagement with the program. Following the intervention, a post-intervention assessment was conducted, and participants’ oral health practices were monitored for an additional two weeks to assess the sustainability of behavior changes beyond the intervention period.
1) Pre-intervention assessment: Before the initiation of the intervention, a thorough baseline assessment of participants’ oral health knowledge was conducted using validated surveys (Appendix A). These surveys covered a wide spectrum of oral health concepts, including the anatomy of teeth and gums, the significance of fluoride, and common dental diseases. Individual knowledge scores were calculated, establishing a baseline measure for each participant, with the maximum score for the knowledge assessment set at 100 (Appendix B).
2) Post-intervention assessment: Following the four-week intervention period, participants from both the experimental and control groups underwent a post-intervention survey (Appendix C). This survey mirrored the pre-intervention assessment and allowed for a direct comparison of changes in knowledge. Individual knowledge scores were recalculated, and the difference between pre- and post-intervention scores was used to quantify the impact of the educational program.
3) Brushing frequency: Participants’ brushing habits were assessed through a combination of self-reporting and observation. Each participant maintained a detailed log, recording the frequency and duration of their toothbrushing activities. Trained researchers also conducted periodic observations to validate self-reported data, enhancing the reliability of the findings.
4) Flossing habits: Similar to brushing, participants self-reported their flossing habits, detailing the frequency and thoroughness of their flossing routine. Periodic checks were conducted to corroborate self-reported data, ensuring the accuracy of the information gathered.
5) Dietary choices: The study assessed participants’ dietary habits related to oral health, including the consumption of sugary snacks and beverages. Dietary logs and self-reporting were used, and nutritional assessments were conducted to evaluate participants’ awareness of the relationship between diet and oral health.
Trained researchers conducted periodic observations to assess participants’ oral health practices in a naturalistic setting. This included direct observations of toothbrushing and flossing routines, as well as an assessment of participants’ adherence to recommended oral hygiene practices.
Throughout the study, continuous monitoring and quality checks were implemented to ensure the accuracy and reliability of the outcome measures. Any deviations or unexpected trends in the data were promptly investigated, and corrective actions were taken as needed. This approach ensured the robustness of the study’s outcome assessments.
Descriptive statistics were employed for demographic data. Paired t-tests were used to compare pre- and post-intervention knowledge scores. Analysis of covariance (ANCOVA) was conducted to assess the impact of the intervention on oral health practices, controlling for baseline differences. IBM SPSS Statistics software (version 22.0) was utilised for data analysis, with a predetermined significance level set at p < 0.05.
III. RESULTS
The demographic characteristics table illustrates a well-balanced study population, with both the experimental and control groups having similar age distributions (16.2 ± 1.0 vs. 16.1 ± 0.9) and gender representation (Male/Female: 56/58 vs. 55/59). Baseline knowledge scores align closely, with mean scores of 45.2 (experimental) and 44.8 (control) and standard deviations of 8.3 and 8.1, respectively (Table 1).
|
Group |
Experimental (n=114) |
Control (n=114) |
Total (N=228) |
|
Age (Mean ± SD) |
16.2 ± 1.0 |
16.1 ± 0.9 |
16.15 ± 0.95 |
|
Gender (Male/Female) |
56/58 |
55/59 |
111/117 |
|
Mean Knowledge Score (Pre-Intervention) |
45.2 |
44.8 |
|
|
SD (Pre-Intervention) |
8.3 |
8.1 |
Table 1. Demographic characteristics and baseline knowledge scores
The post-intervention knowledge scores show a substantial improvement in the experimental group (59.8 ± 7.5) compared to the control group (46.2 ± 8.5). The mean change in knowledge scores is notably higher in the experimental group (14.6) compared to the control group (1.4), demonstrating the statistically significant impact of the multimedia-based dental education program (p < 0.001) (Table 2).
|
Group |
Experimental |
Control |
|
Mean Knowledge Score (Post-Intervention) |
59.8 |
46.2 |
|
SD (Post-Intervention) |
7.5 |
8.5 |
|
Mean Change in Knowledge Score |
14.6 |
1.4 |
|
p-value (Paired t-test) |
<0.001 |
0.205 |
Table 2. Primary outcome – Oral health knowledge scores
The secondary outcomes highlight positive changes in oral health practices within the experimental group. Participants in this group demonstrated higher mean brushing frequency (14.3 vs. 12.7 times/week) and flossing frequency (3.2 vs. 1.5 times/week). Furthermore, there was a substantial reduction in sugary snacks (25% vs. 5%) and an increase in healthy dietary choices (20% vs. 7%) within the experimental group, supported by a significant p-value (p < 0.05) (Table 3).
|
Group |
Experimental |
Control |
|
Mean Brushing Frequency (times/week) |
14.3 |
12.7 |
|
SD (Brushing Frequency) |
2.1 |
2.5 |
|
Mean Flossing Frequency (times/week) |
3.2 |
1.5 |
|
SD (Flossing Frequency) |
1.8 |
1.2 |
|
% Reduction in Sugary Snacks |
25% |
5% |
|
% Increase in Healthy Dietary Choices |
20% |
7% |
|
p-value (Chi-square test) |
<0.05 |
— |
Table 3. Secondary outcomes – Oral health practices
Observational assessments reveal a higher percentage of high adherence in the experimental group (75%) compared to the control group (40%). Program adherence monitoring further supports these findings, with the experimental group showing higher average attendance (3.8 vs. 3.5), completion rates of e-learning modules (95% vs. 80%), and participation in interactive sessions (90% vs. 75%) (Table 4).
|
Group |
Experimental |
Control |
|
High Adherence (%) |
75% |
40% |
|
Moderate Adherence (%) |
20% |
50% |
|
Low Adherence (%) |
5% |
10% |
|
p-value (Chi-square test) |
<0.001 |
— |
|
Average Attendance (out of 4 weeks) |
3.8 |
3.5 |
|
Completion Rate of E-learning Modules |
95% |
80% |
|
Participation in Interactive Sessions |
90% |
75% |
Table 4. Observational assessments and program adherence monitoring
Participants in the experimental group expressed higher overall satisfaction (8.9 vs. 6.5) and perceived educational value (9.2 vs. 5.8) compared to the control group. Moreover, 95% of participants in the experimental group expressed willingness to recommend the program, while only 45% in the control group were inclined to do so. These feedback indicators affirm the positive reception of the educational intervention (Table 5).
|
Group |
Experimental |
Control |
|
Overall Satisfaction (Scale 1-10) |
8.9 |
6.5 |
|
Perceived Educational Value (Scale 1-10) |
9.2 |
5.8 |
|
Willingness to Recommend Program |
95% |
45% |
Table 5. Program feedback
IV. DISCUSSION
Oral health education is a crucial component of overall health promotion, particularly among adolescents who are at a critical stage in developing lifelong habits. The present study aimed to evaluate the effectiveness of a multimedia-based dental education program on oral health knowledge and practices among high school students in India.
The primary outcome of the study revealed a substantial improvement in oral health knowledge among participants who underwent the multimedia-based dental education program. The mean change in knowledge scores for the experimental group was 14.6, indicating a significant positive impact (p < 0.001). This aligns with existing literature emphasising the efficacy of multimedia approaches in enhancing health education outcomes (Smith et al., 2020). Interactive and visually engaging materials, such as videos and e-learning modules, have been shown to effectively convey health information, promoting better retention and understanding (George et al., 2014).
The significant increase in post-intervention knowledge scores supports the notion that multimedia interventions can effectively bridge gaps in oral health literacy (Sharma et al., 2022). These findings are consistent with studies that highlight the advantages of incorporating technology-based educational tools in oral health promotion programs (Ardekani et al., 2022; Scheerman et al., 2018).
Beyond knowledge enhancement, the study demonstrated positive changes in oral health practices among participants in the experimental group. The increased mean brushing frequency (14.3 times/week) and flossing frequency (3.2 times/week) in the experimental group compared to the control group (p < 0.001) underscores the program’s impact on promoting healthier oral hygiene habits.
Research has consistently shown that knowledge alone may not necessarily translate into behavioral change (Prochaska & Velicer., 1997). However, the multifaceted approach of the multimedia-based program, incorporating educational videos, interactive modules, and pamphlets, appears to have effectively influenced participants’ behaviors. This is in line with the Health Belief Model, which posits that enhancing knowledge, perceived susceptibility, and perceived benefits can contribute to behavior change (Rosenstock et al., 1998).
The study’s examination of dietary choices adds a valuable dimension to the outcomes, revealing a reduction in sugary snack consumption and an increase in healthy dietary choices among participants in the experimental group (p < 0.05). This is consistent with broader public health efforts that emphasise the role of diet in oral health (Scardina & Messina, 2012, Tungare & Paranjpe, 2023). The observed positive changes in dietary habits align with the socio-ecological model, which underscores the impact of individual, interpersonal, and environmental factors on health behavior (McLeroy et al., 1988).
The multimedia approach likely played a crucial role in conveying the link between diet and oral health. Interactive elements and visual aids may have heightened participants’ awareness, contributing to better-informed dietary choices (Pouriayevali et al., 2023).
Program adherence monitoring revealed high levels of engagement among participants in the experimental group. The average attendance, completion rates of e-learning modules, and participation in interactive sessions were consistently higher compared to the control group. This robust program adherence is indicative of the acceptability and perceived value of the multimedia-based dental education program among the participants.
Participant feedback further substantiates the program’s success. High levels of overall satisfaction (8.9 out of 10) and perceived educational value (9.2 out of 10) reinforce the positive reception of the program. Moreover, the overwhelmingly high willingness to recommend the program (95%) underscores the potential for scalability and sustained impact.
The choice of Burhanpur, a town in central part of India, as the study setting is particularly relevant. India grapples with a significant oral health burden, with a high prevalence of dental diseases among its population (Gambhir et al., 2013). Adolescents in semi-urban and rural areas often face challenges in accessing adequate oral health education, necessitating innovative approaches to bridge this gap. Burhanpur town, as a representative setting, allows for insights that can be extrapolated to similar regions, contributing to the broader discourse on effective oral health interventions.
While the standard curriculum included live demonstrations of oral hygiene practices, it’s important to recognise that traditional pedagogical methods may not always effectively engage students, particularly in high school settings where attention spans can be limited. Live demonstrations, while valuable, may not always fully capture the interest and participation of students, especially when presented in isolation from interactive and immersive learning experiences. Despite the inclusion of demonstrations, the standard curriculum may have relied primarily on didactic lectures, which could have contributed to reduced engagement and enthusiasm among students.
In contrast, the multimedia-based approach employed in the experimental group was designed to provide a more interactive and immersive learning experience. By incorporating interactive discussions, educational videos, e-learning modules, and informational pamphlets, this approach aimed to engage students through multiple sensory modalities and learning styles. While live demonstrations were not explicitly included in the multimedia-based approach, the educational videos and e-learning modules were carefully crafted to simulate real-life scenarios and provide step-by-step guidance on oral hygiene practices. Furthermore, the interactive nature of the discussions and activities encouraged active participation and peer learning, fostering a collaborative learning environment that aligns with Kolb’s experiential learning theory.
The use of multimedia resources in educational settings offers several advantages, including scalability and cost-effectiveness. While there may be initial investments required for content creation, curriculum design, and expertise, multimedia materials have the potential for long-term reuse and adaptation, making them a cost-effective solution in the context of education. Additionally, the widespread availability of digital tools and platforms has significantly reduced the barriers to content creation, allowing educators to develop high-quality multimedia materials at relatively low cost. While traditional methods may appear to have lower upfront costs, they may lack the scalability, flexibility, and engagement potential of multimedia approaches, ultimately limiting their effectiveness in reaching and engaging diverse learner populations.
A. Implications and Limitations
The positive outcomes of this study have significant implications for oral health education interventions targeting high school students. The use of multimedia resources in school settings can offer a scalable and cost-effective approach to reach a large audience. Implementing similar programs in schools may contribute to the establishment of healthier oral hygiene practices early in life, potentially reducing the prevalence of dental issues in adulthood.
However, it is essential to acknowledge the study’s limitations. The sample was confined to a specific geographic location (Burhanpur, India), limiting the generalisability of the findings. Additionally, the short-term nature of the intervention and follow-up may not capture the long-term sustainability of behavior changes. Future research could explore the durability of the observed improvements over an extended period.
B. Future Recommendations
The future recommendations stemming from our study on the impact of a multimedia-based dental education program on high school students’ oral health knowledge and practices are aimed at enhancing the sustainability and effectiveness of oral health interventions. Long-term follow-up studies are recommended to assess the durability of observed improvements. Tailoring interventions to specific cultural contexts and integrating them into the standard school curriculum can ensure relevance and broad reach. Engaging families and communities, leveraging technology for interactive learning experiences, addressing socioeconomic disparities, and fostering interdisciplinary collaboration are also emphasised. By prioritising these recommendations, we can advance efforts to promote oral health literacy and practices among adolescents, leading to better overall oral health outcomes.
V. CONCLUSION
In conclusion, the findings of this study highlight the effectiveness of a multimedia-based dental education program in enhancing oral health knowledge and promoting positive oral health practices among high school students. The incorporation of interactive and visually engaging educational tools demonstrated not only an increase in knowledge scores but also positive changes in brushing habits, flossing practices, and dietary choices. These outcomes contribute to the growing body of evidence supporting the efficacy of multimedia interventions in health education.
By addressing the limitations and building upon these positive findings, future research can further refine and optimise multimedia-based dental education programs. The potential for widespread implementation in school settings holds promise for improving oral health outcomes among adolescents, ultimately contributing to the broader goal of preventive oral healthcare.
Notes on Contributors
HM conceptualised the study, conducted data analysis, and significantly contributed to manuscript writing. SRP aided in data acquisition, reviewed the methodology, and participated in manuscript drafting. KRA provided insights into experimental design and data interpretation. MIK actively contributed to data analysis, results interpretation, and manuscript revisions.
Ethical Approval
The submitted manuscript has obtained ethical clearance from the GGSCDS&RC Ethics Committee, with approval number GGSCDS&RC/2022/IEC/168. All standard institutional review board (IRB) procedures were diligently adhered to during the study. The authors emphasise the importance of ethical considerations and confirm compliance with the required ethical standards.
Data Availability
According to institutional policy, research dataset isavailable on reasonable request to the corresponding author.
Funding
This study did not receive any external funding.
Declaration of Interest
Authors declare that they do not have possible conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Agbelusi, G. A., & Jeboda, S. O. (2006). Oral health status of 12-year-old Nigerian children. West African Journal of Medicine, 25(3), 195-198. https://doi.org/10.4314/wajm.v25i3.28277
Angelopoulou, M., Kavvadia, K., Taoufik, K., & Oulis, C. (2015). Comparative clinical study testing the effectiveness of school-based oral health education using experiential learning or traditional lecturing in 10-year-old children. BMC Oral Health, 15(1), Article 51. https://doi.org/10.1186/s12903-015-0036-4
Ford, P., & Farah, C. (2012). Oral health therapists: What is their role in Australian health care? International Journal of Dental Hygiene, 11(1), 22-27. https://doi.org/10.1111/j.1601-5037.2012.00564.x
Gambhir, R. S., Brar, P., Singh, G., Sofat, A., & Kakar, H. (2013). Utilisation of dental care: An Indian outlook. Journal of Natural Science, Biology, and Medicine, 4(2), 292-297. https://doi.org/10.4103/0976-9668.116972
George, P. P., Papachristou, N., Belisario, J. M., Wang, W., Wark, P. A., Cotic, Z., Rasmussen, K., Sluiter, R., Riboli–Sasco, E., Tudor Car, L., Musulanov, E. M., Antonio Molina, J., Heng, B. H., Zhang, Y., Wheeler, E. L., Shorbaji, N. A., Majeed, A., & Car, J. (2014). Online eLearning for undergraduates in health professions: A systematic review of the impact on knowledge, skills, attitudes, and satisfaction. Journal of Global Health, 4(1), Article 010406. https://doi.org/10.7189/jogh.04.010406
Ghoneim, A., Ebnahmady, A., D’Souza, V., Parbhakar, K. K., He, H., Gerbig, M., Singhal, S., & Quiñonez, C. (2022). The impact of dental care programs on healthcare system and societal outcomes: A scoping review. BMC health services research, 22(1), Article 1574. https://doi.org/10.1186/s12913-022-08951-x
Gousalya, V., M. N., Dhamodhar, D., Sindhu, R., Prabu, D., Elakiya, S. (2022). Systematic literature review on the effect of play way – A game based oral health education on oral hygiene of school-going children. Indian Journal of Contemporary Dentistry, 11(1), 9-17. https://doi.org/10.37506/ijocd.v11i1.18808
Kassebaum. N. J., Smith, A. G. C., Bernabé, E., Fleming, T. D., Reynolds, A. E., Vos, T., Murray, C. J. L., & Marcenes, W & GBD 2015 Oral Health Collaborators. (2017). Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: A systematic analysis for the Global burden of diseases, injuries, and risk factors. Journal of Dentistry Research, 96(4), 380-387. https://doi.org/10.1177/0022034517693566
McLeroy, K. R., Bibeau, D., Steckler, A., & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351-377. https://doi.org/10.1177/109019818801500401
Movaseghi Ardekani, F., Ghaderi, F., Kaveh, M. H., Nazari, M., & Khoramaki, Z. (2022). The effect of an educational intervention on oral health literacy, knowledge, and behavior in Iranian adolescents: A theory-based randomized controlled trial. BioMed Research International, 5421799. https://doi.org/10.1155/2022/5421799
Nakre, P. D., & Harikiran, A. G. (2013). Effectiveness of oral health education programs: A systematic review. Journal of International Society of Preventive & Community Dentistry, 3(2), 103–115. https://doi.org/10.4103/2231-0762.127810
National Institutes of Health (2021). Oral Health in America: Advances and Challenges. National Institute of Dental and Craniofacial Research (US).
Pouriayevali, B., Ehteshami, A., Kohan, S., & Saghaeiannejad Isfahani, S. (2023). Mothers’ views on mobile health in self-care for pregnancy: A step towards mobile application development. Journal of Education and Health Promotion, 1, 308. https://doi.org/10.4103/jehp.jehp_534_22
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12(1), 38-48. https://doi.org/10.4278/0890-1171-12.1. 38
Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the Health Belief Model. Health Education Quarterly, 15(2), 175-183. https://doi.org/10.1177/109019818801500203
Scardina, G. A., & Messina, P. (2012). Good oral health and diet. Journal of Biomedicine and Biotechnology, 2012, 720692. https://doi.org/10.1155/2012/720692
Scheerman, J. F. M., van Meijel, B., van Empelen, P., Kramer, G. J. C., Verrips, G. H. W., Pakpour, A. H., Van den Braak, M. C. T., van Loveren, C. (2018). Study protocol of a randomized controlled trial to test the effect of a smartphone application on oral-health behavior and oral hygiene in adolescents with fixed orthodontic appliances. BMC Oral Health, 18(1), 19. https://doi.org/10.1186/s12903-018-0475-9
Sharma, S., Mohanty, V., Balappanavar, A. Y., Chahar, P., & Rijhwani, K. (2022). Role of digital media in promoting oral health: A systematic review. Cureus, 14(9), e28893. https://doi.org/10.7759/cureus.28893
Smith, A. C., Thomas, E., Snoswell, C. L., Haydon, H., Mehrotra, A., Clemensen, J., & Caffery, L. J. (2020). Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). Journal of Telemedicine and Telecare, 26(5), 309-313. https://doi.org/10.1177/1357633X20916567
Tadin, A., Poljak Guberina, R., Domazet, J., & Gavic, L. (2022). Oral hygiene practices and oral health knowledge among students in Split, Croatia. Healthcare, 10(2), 406. https://doi.org/10.3390/healthcare10020406
Texas Dental Association (2008). Building better oral health: A dental home for all Texans. Texas Dental Journal, Suppl, 1–56.
Tungare, S., & Paranjpe, A. G. (2023). Diet and nutrition to prevent dental problems. In: StatPearls [Internet]. StatPearls Publishing.
Zhang, M., Lan, J., Zhang, T., Sun, W., Liu, P., & Wang, Z. (2021). Oral health and caries/gingivitis-associated factors of adolescents aged 12-15 in Shandong province, China: A cross-sectional Oral health survey. BMC Oral Health, 21(1), 288. https://doi.org/10.1186/s12903-021-01640-x
*Santosh R Patil
Department of Oral Medicine and Radiology,
Chhattisgarh Dental College & Research Institute
Rajnandgaon 491441, India
Email: drpsantosh@gmail.com
Submitted: 16 December 2022
Accepted: 25 June 2024
Published online: 1 October, TAPS 2024, 9(4), 6-13
https://doi.org/10.29060/TAPS.2024-9-4/OA2928
Pooja Sachdeva & Derrick Chen-Wee Aw
Department of General Medicine, Sengkang General Hospital, Singapore
Abstract
Introduction: Case write-ups and reflective journals have been used as assessment tools of learning in clinical rotations in Yong Loo Lin school of medicine. It is timely to review the current process of conducting these assessments and effectiveness as an assessment tool. This study aims to understand faculty outlook towards these assessments.
Methods: This is a study that involves a survey-based questionnaire with both closed and open-ended questions, sent out to faculty marking the students’ assignments. This survey was anonymous & voluntary and was disseminated by administrative assistants. The purpose of this survey was to collect the feedback from faculty about current process with intentions of improving the effectiveness of these assessments. The suggestions for improvement were incorporated in the survey and faculty was invited to comment over these suggestions and provide further suggestions if any.
Results: Fifty-two responses from faculty were collected and analysed. Ninety percent of respondents thinks that this is an effective tool to assess and promote self-directed learning. Qualitative feedback was received about need of improvement in a) alignment of the submissions timings with rotation postings b) marking rubric to incorporate factors such as case complexity and weightage to different components of case write-ups, c) timely feedback to students, and d) follow up on action plans.
Conclusion: Case write-ups and reflective journals are still effective learning and assessment tools. They promote self-directed learning and clinical analysis in students. Feedback and action plans are the backbone of these assessments and optimal utilisation of these is recommended.
Keywords: Undergraduate Medical Education, Case Write-ups, Medical Assessments, Reflective Journals
Practice Highlights
- Case write-ups promote critical analysis & clinical judgement and reflection develops metacognition.
- Students should be guided and encouraged to choose cases to promote self-directed learning.
- Marking rubrics need revising and faculty development on how to utilise them.
- Timing of submission needs to be improved to facilitate feedback and follow-up.
- Direct and timely feedback to students and follow up on actions plans improve utility.
I. INTRODUCTION
The medical curriculum has many assessments designed over professional years to assess the knowledge and competence of medical students such as OSCE, Mini CEX, Case write ups, Reflective Journals, multiple choice questions (MCQs), portfolios etc (Miller, 1990). Few assessments such as Mini-CEX and OSCE have gained popularity over last few decades as there is robust evidence in support of these assessments as a tool to promote and assess students’ learning. Patrício et al. (2013) and Mortaz Hejri et al. (2020) have explored the utility of OSCE and Mini CEX respectively in undergraduate & postgraduate education and concluded that reliability, flexibility, and validity of these assessments are the strengths that make them widely acceptable. With growing research in field of medical education assessments, it is important and wisely to seek understanding of current written assessments such as case write-ups and reflective journals in terms of their effectiveness and processes in conducting them. McLeod (1989) surveyed the students and faculty about the effectiveness of case write-ups and written assignments in the undergraduate medical curriculum. There was broader agreement among students and faculty that these assessments were useful educational tools, however, there were concerns about the variability of marking criteria and standard of evaluation (Fortson A, (n.d.); Larsen et al., 2016). Over the years, these assessments have been standardised by using an assessment template that guides the students and marking rubric to assist assessors to mark students to reduce interrater variability (McGlade et al., 2012; McLeod, 1987).
Written assignments on patient cases in which a student had participated in clinical care have been a de rigueur component of posting assessments in the Yong Loo Lin School of Medicine, the National University of Singapore (NUS) for decades. Although the assessment template and marking rubrics have evolved through the years, their objectives have remained unchanged: to encourage deep analysis and reflection on the medical and biopsychosocial aspects of a patient’s clinical problems, investigations, and management; to promote self-directed learning on knowledge gaps, and to enhance confidence in clinical reasoning and practical approaches. Tutors benefit by gaining greater insight into their student’s learning experiences and the effectiveness of their clinical teaching. By providing timely interventions with feedback, tutors promote learning and reflection and contribute to the summative evaluation of the posting. In recent years, tutors are required to provide written feedback to students.
Throughout the years, informal feedback on the value of such written assignments has been sporadically provided by students in their end-of-posting comments, and periodically gathered from teachers at annual get-together discussions. An internal audit was conducted via a formal survey for tutors and students in 2012-13 concerning the learning value and feasibility within a year of launching the latest iteration of these written assignments. Overall sentiments were mixed from both faculty and students regarding its utility and effectiveness as a learning exercise. Therefore, it is time to perform an evaluation to determine if these written assignments should continue as usual or be refined to better reflect the program objectives as well as the requirements of a good clinical assessment.
II. BACKGROUND
Phase three medical students from the Yong Loo Lin School of Medicine in their Medicine rotations in various healthcare institutions are required to submit one outpatient case write-up and two inpatient reflective journals at the sixth to eighth weeks of their 12-week posting. The assessment is standardised as submission needs to follow a format as per assessment template with each component carrying a certain weightage. A marking rubric is also designed to guide the assessor to mark students to make it objective, reliable, and reproducible. The core tutors will mark and provide written feedback on these submissions based on a rubric provided by the school. Face-to-face feedback is encouraged but not mandated. The scores of these written assignments form 30% of the overall posting assessment, and the latter contributes a maximum of 9.4% to the final phase 3 MBBS examination.
Our study was conducted to identify faculty’s viewpoint toward these written assignments as an assessment tool and if it is being conducted in a manner where it promotes learning. Constructive feedback was also collected to seek ways to improve this further. A questionnaire, including mostly closed-end questions with recommended suggestions for improvements with some open-ended questions was prepared and disseminated to faculty through administrative support. The results of this questionnaire are discussed in this paper.
III. METHODS
In this study, we prepared a knowledge, attitudes, and practices (KAP) questionnaire for faculty assessing students’ assignments. The faculty constituted associate consultants and above in public institutions in Singapore who have tutored the students in Yong Loo Lin School of Medicine in their clinical rotations and have marked their written assessments. There were no inclusion criteria, hence all faculty members who have tutored the students and have marked these assessments were invited to answer this survey. The survey was sent out through administrative assistants in respective departments of public institutions for ease of dissemination and to avoid pressurising the participants. The responses from faculty who have not marked these assessments were not counted towards final analysis. The author aimed to collect constructive feedback from faculty about the current process and suggestions for improvement in this assessment tool. The study was conducted over a period of three months from Sep 2020 to Dec 2020 in Singapore for Yong Loo Lin School of Medicine.
The questionnaire was anonymous, and it included eighteen questions, designed to understand the strengths and limitations of these case write-ups and reflective journals based on the Context, Input, Process, and Product (CIPP) method of program evaluation, developed by Stufflebeam (2002) with the aim of providing suggestions for improvement in current delivery or content. The questions included objectives of these assessments, frequency, process, and standardisation training for marking them. It also included the questions regarding familiarity of faculty with these assessments in terms of numbers of these assessments marked per year, marking rubrics and their expectations from the students. Lastly, there were open ended questions regarding feedback for improving the current process and strengthening these assessments for serving the purpose of assessment of students’ learning. An implied consent was obtained from study participants as questionnaire was voluntarily answered. The responses to this survey were collected, collated, and analysed for the understanding of faculty viewpoint and outlook towards these assessments. Feedback was analysed and recommendations were formulated to improve current process of these assessments.
IV. RESULTS
The survey was disseminated to 150 faculty members, and it collected a total of 52 responses (n=52) from two public health clusters over a period of three months with a response rate of 34%. The survey was sent out in September 2020 and monthly reminders were sent till December 2020. The faculty who marked at least one assignment was offered to participate, but there was low response rate, due to lack of inducement or survey fatigue. About 88% (n=46) of respondents had marked 2 to 6 assignments in an academic year while 4% (n=2) had marked more than 10. Ninety percent (90%) (n=47) of faculty think that these written assignments are tools to promote and assess learning. Factors that make them useful were the opportunity for students to choose their cases in outpatient and inpatient settings thus, promoting self-directed learning (29%, n=15) and for assessors to provide feedback and an action plan (30%, n=16). Although when approached by students for a choice of cases, faculty mostly assigned the cases themselves (56%, n=29). The complexity of the selected case (47%, n=24) and common vs uncommon case (30%, n=16) were the principal factors that influenced the marking by assessors. The discussion and reflection sections in these write-ups provided insight into students’ understanding of the case that influenced the overall passing scores (12%, n=6). Marking rubric provided to faculty was used only about half of the time (48%, n=25) faculty used the rubric. Of the 48% (n=25) of assessors who used rubrics for marking, most of them found the rubric to be user-friendly (40%, n=10). Although the same write-up assessment is used to assess learning at distinct phases of the MBBS curriculum (Phase III and Phase IV), 89%, (n=46) of assessors marked it against the expected level of students’ training.
While 60% (n=31) of the assessors provided the overall score, feedback, and action plans directly to the students, either in personal meetings or by email or phone, 40% (n=20) handed over the assessment to an educational administrative assistant. Faculty in the survey responded that face-to-face meetings provided “clearer discussion” and “personal engagement with the student” and were “faster and more effective,” yet the organisation such as “timing of submission mostly at the end of the posting” or “busy schedules of both assessors and students” made it harder to meet students personally. Most of the assessors (69%, n=36) provided action plans which included looking up literature for deeper learning and similar case review for expanding understanding of the patient’s presentation. In a few instances, it also involved rewriting of write-ups (11%, n=5). However, these actions were not followed up very actively. Only a few assessors (10%, n=5) made phone calls or emailed the students to follow up.
Faculty feedback was sought about improvement in the current Input and Process of these assessments. 40% (n=20) of faculty think that weightage to the different components of these write-ups should be flexible and adjusted. 53% (n=28) of assessors suggested that analysis of the case with clinical reasoning and differential diagnosis should bear higher weightage than the clinical presentation, management, or student’s reflection. The number of submissions (16%, n=8) and timing of submissions during a rotation (22%, n=11) should be made uniform and aligned with the training weeks so that timely and face-to-face feedback can be arranged. In our survey, 40 % (n=20) of faculty’s feedback was a written statement to the educational administration. The results of the study are in the data repository and can be accessed by readers if they wish to see detailed responses from faculty in Figshare repository at https://doi.org/10.6084/m9.figshare.24471661.v1 (Sachdeva & Aw, 2023).
V. DISCUSSION
Clinical rotations are the placements planned by universities for medical students to have real-time patient encounters in public hospitals. This is the continuation of the undergraduate medical education curriculum whereby students learn to apply their medical knowledge acquired in initial foundation years and continue to learn bedside manners, verbal and nonverbal communication, eye contact, and body language to prepare them for their future roles as doctors.
Assessments during these rotations must include all the areas of learning such as the patient’s clinical presentation, diagnostic approach for the patient’s symptoms, the analytic ability of students, and communication with the patient and his management. A variety of assessment tools to perform a comprehensive holistic evaluation of a student’s performance are undertaken in clinical rotations such as Mini CEX, Case logbooks, student portfolios, and written assignments such as case write-ups and reflective journals. While Mini CEX has gained its popularity over last few decades due to its rapid results, synchronous feedback and direct observation of encounter, other assessments such as case write-ups, reflective journals do contribute to learning and supplements the medical education assessments and have been the part of curriculum.
Assessments such as Mini-CEX (clinical encounter) are assessor-observed case presentations that assess the student’s ability to ask history questions and perform a clinical examination to formulate a list of differentials and thus develop a diagnostic approach (Kogan et al., 2002). It also assesses skills such as bedside manners, verbal and nonverbal communication, use of jargon, and speed of speech. There is a provision for giving feedback to the students about their learning and agreeing on an action plan to improve upon the student’s learning gaps at the end of the encounter. This assessment does not provide the opportunity for reflection-on-action and in-depth patient management (Schon, 1984).
Case write-ups on the other hand are akin to a case presentation but the focus is on identifying knowledge gaps by students themselves. Students collect data on patients’ clinical presentation and investigations performed that help in formulating a diagnostic plan (McLeod, 1989). They analyse the information to reach a final diagnosis. Students refer to literature for common and uncommon presentations of the patient’s condition and learn management based on the evidence. It also provides the opportunity to learn details about a certain medical disease. However, this literature then needs to be individualised for the patient based on his comorbidities and social factors. In the end, students are asked to submit this write-up along with their reflections on their learning from the patient and assessment.
Reflective journals are like case write-ups however, the emphasis is on learning and evolution alongside the clinical encounter. Boyd & Fales (1983) have explained reflective writing as an internal experience that is triggered by an encounter which results in changed perspective. Students are expected to write about the patient encounter, their interpretation about clinical outcome and management and their learning along the encounter as per stages in cycle of reflection (Gibbs, 1998). Mello & Wattret (2021) highlighted reflection as a skill that prepares students for lifelong learning.
|
Assessment |
Mini CEX |
Case write-ups and reflective Journals |
|
Directly observed |
Yes |
No |
|
Case presentation and differentials |
Yes |
Yes |
|
Access to investigations |
Provided by accessor on request |
Access is granted |
|
Management plan |
Proposed by learner |
Assessed and discussed by learner |
|
Reflection-in-action |
Yes |
No |
|
Reflection-on action |
No |
Yes |
|
Literature review |
No |
Yes |
|
Feedback to learners |
Yes, communicated directly at end of encounter |
Yes, communicated directly or indirectly* |
|
Action Plan |
Yes |
Yes |
|
Resources required |
The patient, learner and accessor must be present at same time (synchronous learning) (Kunin et al., 2014) |
The patient, learner and accessor need not be present at same time (asynchronous learning) (Kunin et al., 2014) |
|
Assessment focus |
Communication skills, bedside manners, professionalism, case presentation and diagnosis and approach to diagnosis (Kogan et al., 2002) |
Clinical reasoning, in depth understanding of disease presentation, Evidence-Based Medicine (EBM) practice and learner’s reflection (McLeod, 1989). Reflective journals focus more on learning evolution based on one’s experience. |
|
Marking |
More objective (valid, reproducible) |
More subjective (assessor guided) ** |
|
Assessment tool |
Formative (Joshi et al., 2017) |
Summative (Bussard, 2015) |
Table 1. Comparison of Mini CEX and case write-ups as assessment tools
*For direct feedback, assessor needs to have follow up communication with the student.
**it can be made objective with descriptors provided in the, marking template for each domain that is being assessed.
Evidence has shown that case write-ups do provide assessors the ability to understand students’ learning and analytical skill (McLeod, 1989) and unlike Mini CEX, it involves reflections by students that deepen learning and memory (Fortson & Sisk, 2007). Similarly, Bjerkvik & Hilli (2019) emphasised that reflective journals promote deeper understanding, critical analysis, metacognition and promotes self-development. Onishi (2008) noted that case presentations during clinical rotations promote the assessor’s understanding of student learning which is consistent with our faculty response as most of our faculty (n=47, 90%) agree that case write-ups are important tools to assess learning. However, since these are not observed assessments at the bedside and require submission, there is no face-to-face contact with the student to give instant feedback and discuss action plans, if any. The discussion of feedback and action plan requires separate communication such as a meeting or phone calls or emails between the assessor and student. If appropriate feedback is not provided or communicated, it is a lost opportunity for improvement in students’ learning.
Results from our survey have highlighted a few areas that needed the attention in optimal utilisation of these assessments. First is, the choice of cases, either by faculty or by students is not uniform. The case selection by students promotes self-directed learning. Presently, students are given a list of cases that may help them select one, but the enlisted cases may not be encountered during their rotation. In such situations, faculty suggesting the choice of cases can provide directions to students. Lee et al. (2010) demonstrated that students who were encouraged to choose their cases based on their knowledge gaps, learning strategies, and study time, were more inclined towards self-directed learning. Self-directed learning has been a cornerstone of adult learning, and it provides learners autonomy and control over their learning and prepares them for lifelong self-management outside educational institutions (Goldman, 2009; Lee et al., 2010). Understandably, students’ choice of cases is influenced by the curriculum, tutorials, and objectives of a particular rotation. Case write-ups and Reflective Journals in our context included both inpatient and outpatient encounters hence providing the choice for both acutely sick vs stable chronic patients. Since the students were encouraged to choose their cases for these assessments on their own, it provided them the opportunity to meet their personal goals and learning deficits. However, if asked for guidance, slightly more than half the faculty (56%, n=29) would assign the cases themselves, and of note, such selection of cases, in various forms of frequency and complexity, did affect the marking by faculty by a considerable amount (about 30 to 45%). Nonetheless, the reflective journals involve writing about one’s learning evolution about a case from preset knowledge to acquired knowledge after encounter. Hence, both these written assignments, case write-ups and reflective journals on any encounter tend to improve learning by making students do literature search and individualise this current evidence-based management search in context of the chosen patient. It still serves the purpose of learning, although personal selection of patients encourages students to work on their own interest, at their own pace and promotes deeper understanding tailored to one’s own pre-existing gaps or deficiencies in knowledge. The authors think that faculty assigning cases will inadvertently compromise the extent of self-directed learning to a significant degree and adjusting the marking based on the frequency and complexity is a qualitative component that warrants further investigation. We recommend the school generate a simple set of guidelines to help students to make an informed and wise selection of suitable cases for their written assignments. Focus group discussions with tutors who regularly mark students on such assignments may provide useful directions in the guidelines’ construction.
Results of this survey also raised the inconsistency in faculty use of marking rubrics. McLeod (1989) raised the major concerns about the variability of criteria and standards of evaluation of these written assessments.
Kogan & Shea (2003) addressed these concerns and assessed the evaluation of write-ups against a pre-set evaluation form that increased the validity and reliability of scoring these write ups. Peggy (2014) also highlighted the use of standardised scoring rubric for case write-ups to reduce the interrater variability and improve the reliability of these assessments. Hence, the scoring rubrics must have descriptors for faculty to mark the students against their performances and it not only makes the assessment fair, but also contributes to individualised and appropriate feedback for students for further improvement in respective domains (Cyr et al., 2014; Kogan & Shea, 2005). Thus, the author recommends that universities or schools must emphasise on faculty training and thereby its use in marking these assignments.
This also brought about the feedback, provided by faculty in this survey about components of this rubric. Reflective journals and case reports assess similar yet different components of learning. While case reports accounts more for critical analysis, clinical judgement, evidence-based management for a particular patient, the reflective journals assess the student’s ability to assimilate an encounter with new acquired knowledge and reflect on their individual learning and growth (Sandars, 2009). Hence, rubric should be tailored to these assessments’ subcomponents accordingly. A small fraction of faculty (12%, n=6) in our survey responded that the discussion and analysis of information by students influenced their marking of the write-up as it provided them invaluable insight into students’ clinical reasoning. In line with this, half of the faculty (53%, n=27) recommended that analytic skills be ranked higher in weightage as compared to data collection on patient history and examination. Hence, marking rubric should emphasise more on clinical judgement and critical analysis in case write-ups than components such as history taking and examination as latter can be assessed in detail with other assessments such as Mini CEX or OSCE examinations. At the same time, complexity of the case and atypical presentation must also account for separate marks to encourage students for choosing challenging and difficult cases. Similarly, for reflective journals rubrics must have weightage on self-reflection cycle, changes in attitudes and perception and how the encounters have changed one’s learning and future practice. The role of rubric in standardisation of these written assessments is paramount as former provides a structure of written submissions for students and reliable and valid scoring tool for faculty.
Results of our survey also highlighted pertinent inadequacy in these assessments that is inability to provide the face-to-face feedback to the students in timely fashion, contributed by timing of submissions of these assessments towards the end of rotation. There is ample literature to support that feedback is a backbone of any formative assessment (Clynes & Raftery, 2008; Nicol & Macfarlane‐Dick, 2006) as it promotes self-regulation of training and highlights the discrepancies in the trainee’s current vs expected learning outcome. Hence like every other assessment, the templates of case write-ups are imbued with spaces for feedback and action plans which the majority of faculty (60%, n=31) have personally communicated to the students. Face-to-face feedback has a higher impact on performance improvement than written indirectly communicated or no feedback as the former provides two-way engagement, however, this impact depends upon the supervisor’s training and content & organisation of feedback (Johnson et al., 2020; Pelgrim et al., 2012). The final stage of providing any feedback as per Pendleton’s rule (Pendleton, 1984). Pendleton’s rule is an agreement between the learner and assessor for a joint action plan for improvement. Presently, there is no timeline for students to submit these written assignments to their core supervisor, hence if these are submitted towards the end of the rotation, the opportunity for face-to-face feedback and discussion on action plans is underutilised. Hence, it would be worthwhile to align the submission with weeks of rotation so that timely and personal feedback can be provided and agreed action plans can be followed within the rotation.
This study highlighted that though an action plan was agreed upon, it was not actively followed up with students 90% (n=47) of the time – as such, the accountability of this assessment is reduced. The most common reason for the inability to follow up on action plans was coordination (having to schedule a meeting between the assessor and student when the student may have moved on to the next rotation). This can be modified if students are instructed to submit their assignments at least one or two weeks before the end of posting to allow ample time for both parties to schedule a meet-up. Alternatively, there could be an end-of-posting mandatory meet-up with the clinical supervisor to provide overall feedback for rotation and to discuss action plans. Additionally, the school could also mandate a follow-up meeting, over an interactive online platform if a face-to-face meeting is not feasible, for a supervisor to review the outcomes of the actions undertaken by the student. The school may even consider recruiting student mentors to follow up instead.
Overall, this survey has provided useful insight into these assessments’ conduct and has highlighted the factors that limit the utility of these written assessments. With the faculty agreeing that these assessments are still worthy educational and learning assessment tools, there is a need to improve marking standardisation of these assessments and like other assessments, formative feedback to students on gaps in knowledge must be provided. These assessments have been part of curriculum for decades and their role in students learning must be utilised to its full potential.
There are limitations in our study such as lower number of respondents and qualitative feedback. As survey is voluntary and anonymous, it is limited in its research capability for recommendations and qualitative feedback as latter is respondent dependent. Hence, further qualitative research such as focussed group discussions is required to understand the ways, these assessments can be utilised to their full potential as learning and assessment tools.
VI. CONCLUSION
In conclusion, written assignments are still worthy and useful tools to assess the learning of students during clinical rotations. It promotes self-directed learning by allowing students to select their case and provides the opportunity for the assessor to assess the knowledge gaps of students about case management. Since the case choice affects the marking by the assessor, authors recommend that students are given free reign, within a set of recommended guidelines.
Marking and scoring should be adjusted to include variables such as case selection and complexity in the marking rubric provided to the assessors, hence authors also recommend updating marking rubrics in consultation with faculty, with subsequent faculty development for compulsory use of this rubric.
For these assessments to be more effective, structured, timely and direct feedback should be given to students with action plans that must be followed. The hurdles in following up on action plans such as change of rotations can be dealt with by adjusting the timing of submission of these assessments during a posting and creating opportunities for follow-up. Hence, authors also recommend face-to-face feedback by ensuring adequate timing of assessments and appropriate follow up for action plans to maximise educational improvement opportunities.
Notes on Contributors
Dr. Pooja Sachdeva has contributed to the conceptual development of this study, survey questionnaire development, dissemination of the survey to faculty, data collection, and analysis. This manuscript has been written, read, and finally approved by her.
Dr. Derrick Aw has contributed to the conceptual development of this study, survey questionnaire development, and student and faculty engagement. This manuscript was read, edited, and finally approved by him.
Ethical Approval
The study was approved by the Singhealth Institutional Review Board (IRB) with reference no 2020/2688.
Data Availability
The data that supports the findings of this study are openly available in Figshare repository at https://doi.org/10.6084/m9.figshare.24471661.v1 (Sachdeva & Aw, 2023).
Acknowledgement
We acknowledge the contributions of Dr Shweta Rajkumar Singh for editing the final manuscript.
Funding
There is no funding received for the study.
Declaration of Interest
There are no conflicts of interest.
References
Bjerkvik, L. K., & Hilli, Y. (2019). Reflective writing in undergraduate clinical nursing education: A literature review. Nurse Education in Practice, 35, 32–41. https://doi.org/10.1016/j.nepr.2018.11.013
Boyd, E. M., & Fales, A. W. (1983). Reflective learning: Key to learning from experience. Journal of Humanistic Psychology, 23(2), 99–117. https://doi.org/10.1177/0022167883232011
Bussard, M. E. (2015). Clinical judgment in reflective journals of prelicensure nursing students. The Journal of Nursing Education, 54(1), 36–40. https://doi.org/10.3928/01484834-20141224-05
Clynes, M., & Raftery, S. (2008). Feedback: An essential element of student learning in clinical practice. Nurse Education in Practice, 8(6), 405–411. https://doi.org/10.1016/j.nepr.2008.02.003
Cyr, P. R., Smith, K. A., Broyles, I. L., & Holt, C. T. (2014). Developing, evaluating and validating a scoring rubric for written case reports. International Journal of Medical Education, 5, 18–23. https://doi.org/10.5116/ijme.52c6.d7ef
Fortson, A. (n.d.). Reflective journaling as assessment and teaching. http://www.reap.ac.uk
Gibbs, G. (1998). Learning by Doing: A guide to teaching and learning methods. Oxford Brookes University.
Goldman, S. (2009). The educational kanban: Promoting effective self-directed adult learning in medical education. Academic Medicine, 84(7), 927–934. https://doi.org/10.1097/ACM.0b013e3181a8177b
Johnson, C. E., Weerasuria, M. P., & Keating, J. L. (2020). Effect of face-to-face verbal feedback compared with no or alternative feedback on the objective workplace task performance of health professionals: A systematic review and meta-analysis. BMJ Open, 10(3), e030672. https://doi.org/10.1136/bmjopen-2019-030672
Joshi, M., Singh, T., & Badyal, D. (2017). Acceptability and feasibility of mini-clinical evaluation exercise as a formative assessment tool for workplace-based assessment for surgical postgraduate students. Journal of Postgraduate Medicine, 63(2), 100–105. https://doi.org/10.4103/0022-3859.201411
Kogan, J. R., Bellini, L. M., & Shea, J. A. (2002). Implementation of the mini-CEX to evaluate medical students’ clinical skills. Academic Medicine, 77(11), 1156–1157. https://doi.org/10.1097/00001888-200211000-00021
Kogan, J. R., & Shea, J. A. (2003). An assessment measure to evaluate case write-ups in a medicine core clerkship. Medical Education, 37(11), 1035–1036. https://doi.org/10.1046/j.1365-2923.2003.01660.x
Kogan, J. R., & Shea, J. A. (2005). Psychometric characteristics of a write-up assessment form in a medicine core clerkship. Teaching and Learning in Medicine, 17(2), 101–106. https://doi.org/10.1207/s15328015tlm1702_2
Kunin, M., Julliard, K. N., & Rodriguez, T. E. (2014). Comparing face-to-face, synchronous, and asynchronous learning: Postgraduate dental resident preferences. Journal of Dental Education, 78(6), 856–866.
Larsen, D. P., London, D. A., & Emke, A. R. (2016). Using reflection to influence practice: Student perceptions of daily reflection in clinical education. Perspectives on Medical Education, 5(5), 285–291. https://doi.org/10.1007/s40037-016-0293-1
Lee, Y.-M., Mann, K. V., & Frank, B. W. (2010). What drives students’ self-directed learning in a hybrid PBL curriculum. Advances in Health Sciences Education: Theory and Practice, 15(3), 425–437. https://doi.org/10.1007/s10459-009-9210-2
McGlade, K., Cargo, C., Fogarty, D., Boohan, M., & McMullin, M. (2012). Handwritten undergraduate case reports. The Clinical Teacher, 9(2), 112–118. https://doi.org/10.1111/j.1743-498X.2011.00494.x
McLeod, P. J. (1987). Faculty assessments of case reports of medical students. Journal of Medical Education, 62(8), 673–677. https://doi.org/10.1097/00001888-198708000-00008
McLeod, P. J. (1989). Assessing the value of student case write-ups and write-up evaluations. Academic Medicine, 64(5), 273–274. https://doi.org/10.1097/00001888-198905000-00016
Mello, L. V., & Wattret, G. (2021). Developing transferable skills through embedding reflection in the science curriculum. Biophysical Reviews, 13(6), 897–903. https://doi.org/10.1007/s12551-021-00852-3
Miller, G. E. (1990). The assessment of clinical skills/competence/performance. Academic Medicine, 65(9), S63.
Mortaz Hejri, S., Jalili, M., Masoomi, R., Shirazi, M., Nedjat, S., & Norcini, J. (2020). The utility of mini-clinical evaluation exercise in undergraduate and postgraduate medical education: A BEME review: BEME Guide No. 59. Medical Teacher, 42(2), 125–142. https://doi.org/10.1080/0142159X.2019.1652732
Nicol, D. J., & Macfarlane-Dick, D. (2006). Formative assessment and self-regulated learning: A model and seven principles of good feedback practice. Studies in Higher Education, 31(2), 199–218. https://doi.org/10.1080/03075070600572090
Onishi, H. (2008). The role of case presentation for teaching and learning activities. The Kaohsiung Journal of Medical Sciences, 24(7), 356–360. https://doi.org/10.1016/s1607-551x(08)70132-3
Patrício, M. F., Julião, M., Fareleira, F., & Carneiro, A. V. (2013). Is the OSCE a feasible tool to assess competencies in undergraduate medical education? Medical Teacher, 35(6), 503–514. https://doi.org/10.3109/0142159X.2013.774330
Pelgrim, E. A. M., Kramer, A. W. M., Mokkink, H. G. A., & van der Vleuten, C. P. M. (2012). The process of feedback in workplace-based assessment: Organisation, delivery, continuity. Medical Education, 46(6), 604–612. https://doi.org/10.1111/j.1365-2923.2012.04266.x
Pendleton, D. (1984). The consultation: An approach to learning and teaching. Oxford University Press.
Sachdeva, P. & Aw D. C. W. (2023). Case write-ups survey responses [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.24471661.v1
Sandars, J. (2009). The use of reflection in medical education: AMEE Guide No. 44. Medical Teacher, 31(8), 685–695. https://doi.org/10.1080/01421590903050374
Schon, D. A. (1984). The reflective practitioner: How professionals think in action. Basic Books.
Stufflebeam, D. (2002). The CIPP model for evaluation. In The International Handbook of Educational Evaluation, 49, 279–317. https://doi.org/10.1007/0-306-47559-6_16
*Pooja Sachdeva
110 Sengkang East Way,
Singapore 544886
96170342
Email address: pooja.sachdeva@singhealth.com.sg
Submitted: 3 July 2023
Accepted: 18 June 2024
Published online: 1 October, TAPS 2024, 9(4), 61-64
https://doi.org/10.29060/TAPS.2024-9-4/SC3071
Victoria Scudamore, Sze Yi Beh, Adam Foster & Michaela Goodson
School of Medicine, Newcastle University Medicine Malaysia, Malaysia
Abstract
Introduction: This study compares online and in-person delivery of a weekly clinical reasoning seminar for fourth-year medical students at a Malaysian medical school. During the easing of COVID-19 pandemic restrictions, the initial eight seminars took place online, followed by eleven in-person seminars. This study looks at student preference for online or in-person delivery and how these reasons differ due to gender.
Methods: An online questionnaire was sent to fourth-year medical students after returning to in-person seminars. The response rate was 60/128 (46.88%) and the data was analysed using SPSS software.
Results: 65% of students preferred in-person seminars and a larger proportion of female students (71.43%) preferred in-person sessions compared to male students (50.00%), although this was not statistically significant (p=0.11). A significantly larger proportion of female students preferred in-person seminars for the following reasons compared to male students: enjoyment (p=0.041), developing history-taking skills (55.56%) and for formulating differential diagnoses (p=0.046). Students were asked whether online or in-person seminars were most appropriate for eighteen reasons, they felt in-person seminars were most appropriate for 16/18 of these reasons.
Conclusions: More students preferred in-person clinical reasoning seminars and a higher proportion of these students were female. A significantly larger proportion of female students felt in-person seminars were better for; enjoyment and for developing history-taking skills and formulating differential diagnoses, compared to male students. The students preferred online seminars for home comforts and ease of travel, but they preferred in-person seminars for the other 16/18 reasons listed including all reasons linked to learning skills and interreacting with others.
Keywords: Online Teaching, In-person Teaching, Gender, Clinical Reasoning, Medical Students
I. INTRODUCTION
Fourth-year medical students at Newcastle Medical School Malaysia attend weekly clinical reasoning seminars as part of their ‘Clinical Decision Making’ (CDM) module. Each week of CDM covers a different medical speciality and students attend a seminar where the group works through a presentation with patient cases and they discuss how to diagnose, investigate and manage the patient. The sessions are attended by eleven students and the groups remain the same throughout the year. In 2021-22 the initial eight seminars took place online using Zoom video conferencing software and as COVID-19 restrictions eased in Malaysia the final eleven sessions took place in-person.
The academic performance of students undertaking online and in-person clinical reasoning seminars has been researched and third-year medical student academic performance was comparable in both settings (Babenko et al., 2022). However, there is currently no research regarding medical student preference for online or in-person delivery of clinical reasoning seminars. Medical student preference for online or in-person delivery of all parts of the curriculum has been analysed and second-year medical students at a US medical school had a preference for online lectures and there was a correlation between these students and those who felt online lectures reduced stress (Altaf et al., 2022).
A cohort study analysed participation in a teaching programme for US graduate physicians and this showed female students asked and answered less questions during in-person sessions compared to online sessions (Cromer et al., 2022). The results of this study are contrasting with my observations whereby female students participated less in online seminars and their participation increased when seminars returned to an in-person setting. This could be due to differences in the research environments or due to the group of observed students being small with less statistical significance.
My first research question was to understand medical student preference and reason for preference of online or in-person delivery of clinical reasoning seminars. My second research question was to establish if student preference differed due to gender and why.
II. METHODS
The data was collected using survey methodology with a self-developed questionnaire made using Microsoft forms. The questionnaire was emailed to all fourth-year medical students after they had experienced both session deliveries. Students were provided with a consent form and informed the research project was optional and were asked to provide voluntary consent before participating. Participants were informed they could withdraw from the project at any time up until the data was anonymised during data collection.
The survey response rate was 60/128 (46.88%), the low participation numbers are likely due to the data collection being optional and undertaken in the students own time. This could lead to a nonresponse bias, as it is likely the more engaged students participated and students with less motivation who did not participate may have responded differently. The data was analysed using SPSS software. Chi-squared tests were used to cross-tabulate the results and to calculate p-values to indicate data with statistical significance.
III. RESULTS
Overall 65% of students preferred in-person seminars and 71.43% (30/42) of female students preferred in-person sessions compared to 50.00% (9/18) of male students (p=0.11). The students were asked if they felt online or in-person seminars were best for eighteen different reasons (see table 1). There were three statistically significant reasons female students preferred in-person sessions more than male students (p<0.05). These were Enjoyment (p=0.041), developing history-taking skills (p=0.011) and formulating differential diagnoses (p=0.046).
The students felt in-person sessions were most appropriate for 16/18 of the reasons listed in (table 1). The reasons with the highest proportion of students feeling in-person were the most appropriate were; interaction with friends (95.00%), interaction with the facilitator (91.67%), and developing clinical reasoning skills (91.67%). There were only two reasons students felt online sessions were most appropriate, these were home comforts (98.33%) and ease of travel (91.67%).
Original data can be accessed in Figshare at https://doi.org/10.6084/m9.figshare.23616627.v1 and https://doi.org/10.6084/m9.figshare.23616630.v1
Results are ranked from reasons with the highest proportion of students thinking in-person was most appropriate for that reason. P-values have been calculated to establish if there is statistical significance between the results for male and female students, significant results are highlighted in bold.
|
|
All students |
Female students |
Male students |
P-value |
|
Interaction with friends |
57/60 (95.00%) |
39/42 (92.86%) |
18/18 (100.00%) |
0.245 (>0.05) |
|
Interaction with the facilitator |
55/60 (91.67%) |
39/42 (92.86%) |
16/18 (88.89%) |
0.610 (>0.05) |
|
Developing clinical reasoning skills |
55/60 (91.67%) |
39/42 (92.86%) |
16/18 (88.89%) |
0.610 (>0.05) |
|
Learning from the facilitator |
51/60 (85.00%) |
35/42 (83.33%) |
16/18 (88.89%) |
0.581 (>0.05) |
|
Flow |
47/60 (78.33%) |
33/42 (78.57%) |
14/18 (77.78%) |
0.945 (>0.05) |
|
Developing history-taking skills |
46/60 (76.67%) |
36/42 (85.71%) |
10/18 (55.56%) |
0.011 (<0.05) |
|
Developing knowledge |
45/60 (75.00%) |
33/42 (78.57%) |
12/18 (66.67%) |
0.329 (>0.05) |
|
Ease of sharing opinions |
45/60 (75.00%) |
33/42 (78.57%) |
12/18 (66.67%) |
0.329 (>0.05) |
|
Enjoyment |
44/60 (73.33%) |
34/42 (80.95%) |
10/18 (55.56%) |
0.041 (<0.05) |
|
Learning from peers |
41/60 (68.33%) |
28/42 (66.67%) |
13/18 (72.22%) |
0.672 (>0.05) |
|
Formulating differential diagnoses |
41/60 (68.33%) |
32/42 (76.19%) |
9/18 (50.00%) |
0.046 (<0.05) |
|
Interpreting clinical data |
40/60 (66.67%) |
29/42 (69.05%) |
11/18 (61.11%) |
0.550 (>0.05) |
|
Formulating management plans |
39/60 (65.00%) |
29/42 (69.05%) |
10/18 (55.56%) |
0.315 (>0.05) |
|
Better for mental health |
36/60 (60.00%) |
26/42 (61.90%) |
10/18 (55.56%) |
0.645 (>0.05) |
|
Developing communication skills |
35/60 (58.33%) |
22/42 (52.38%) |
13/18 (72.22%) |
0.153 (>0.05) |
|
Interpreting investigations |
35/60 (58.33%) |
27/42 (64.29%) |
8/18 (44.44%) |
0.153 (>0.05) |
|
Ease of travel |
5/60 (8.33%) |
5/42 (11.90%) |
0/18 (0.00%) |
0.126 (>0.05) |
|
Home comforts |
1/60 (1.67%) |
1/42 (2.38%) |
0/18 (0.00%) |
0.509 (>0.05) |
|
Table 1. The proportion of medical students who felt in-person sessions were the most appropriate for the listed reasons. |
||||
IV. DISCUSSION
Overall, more students in our cohort preferred in-person clinical reasoning seminars and a larger proportion of these students were female than male, however, the difference in preference based on gender did not show statistical significance. This could be due to a smaller cohort of male respondents (18/60) compared to female respondents (42/60). However, even in a study of 488 medical and dental students there was no significant difference in preference for online or in-person delivery when asked about all sessions in the curriculum (Al-Azzam et al., 2020). A larger sample size of medical students will need to be analysed to establish if gender significantly influences student preference for online or in-person delivery of clinical reasoning seminars.
Students felt in-person seminars were better for 16/18 of the listed reasons. This included all reasons pertaining to interaction with other students and staff and all reasons regarding learning a variety of skills. The only two reasons students felt online sessions were better were ease of travel and home comforts. Therefore, this data suggests the only reasons the medical students preferred online seminars were due to the convenience of the setting, and they felt the learning and interaction were superior in in-person seminars.
Of these eighteen reasons, three reasons showed a significant difference in response based on gender, with more female students preferring in-person seminars for the following reasons: enjoyment, development of history-taking skills and formulating differential diagnoses. History-taking and formulating differential diagnoses are more commonly undertaken by doctors within in-person environments. Therefore, female medical students may have a stronger preference for learning skills in the same setting they will be undertaken in when they are doctors.
This study helps to identify the components of clinical reasoning seminars male or female students prefer to undertake online or in-person. Future research could try to identify the reasons for these preferences and to establish if female students have a stronger preference for learning a skill in the same environment it would be undertaken in when they become a doctor.
This research will have most transferability to educators designing clinical reasoning modules to undergraduate students. It may also have some transferability to any undergraduate seminars and to postgraduate medical education. Also, understanding the environment each gender prefers to learn in and why, could help to designing future educational programmes. Especially if these programmes have previously shown differing participation or attainment based on gender.
V. CONCLUSION
In conclusion, students preferred in-person clinical reasoning seminars compared to online seminars and a higher percentage of female students preferred in-person compared to male students, although this was not statistically significant. Students had the strongest preference for in-person sessions due to interaction with friends and the facilitator and for developing clinical skills. Students had the strongest preference for online sessions due to home comforts and ease of travel. Female students preferred in-person seminars compared to male students for the following statistically significant reasons: enjoyment, developing history-taking skills and formulating differential diagnoses.
Notes on Contributors
Dr Victoria Scudamore was involved in data collection, data analysis and wrote this manuscript in full.
Dr Sze Yi Beh was involved in data collection and data analaysis.
Dr Adam Foster was involved in data collection and data analysis.
Dr Michaela Goodson supervised and advised on data collection and analysis.
Ethical Approval
Research and ethics approval was granted by the research committee at Newcastle University Medicine Malaysia on 08/02/2022 (Approval number: 18547/2022).
Data Availability
The data used in this paper is available in the Figshare repository through the following links with associated DOI’s https://doi.org/10.6084/m9.figshare.23616627.v1 and https://doi.org/10.6084/m9.figshare.23616630.v1. The data is shared on the Figshare repository under the CC0 licence (no rights reserved) as there is no copywritten information included.
Funding
No additional funding was used to undertake this project.
Declaration of Interest
There are no potential conflicts of interest to declare.
References
Al-Azzam, N., Elsalem, L., & Gombedza, F. (2020). A cross-sectional study to determine factors affecting dental and medical students’ preference for virtual learning during the COVID-19 outbreak. Heliyon, 6(12), 4. https://doi.org/10.1016/j.heliyon.2020.e05704
Altaf, R., Kling, M., Hough, A., Baig, J., Ball, A., Goldstein, J., Brunworth, J., Chau, C., Dybas, M., & Jacobs, R. J. (2022). The association between distance learning, stress level, and perceived quality of education in medical students after transitioning to a fully online platform. Cureus, 14(4), 3. https://doi.org/10.7759/cureus.24071
Babenko, O., Ding, M., & Lee, A. S. (2022). In-person or online? The effect of delivery mode on team-based learning of clinical reasoning in a family medicine clerkship. Medical Sciences, 10(3), 41. https://doi.org/10.3390/medsci10030041
Cromer, S. J., D’Silva, K. M., Phadke, N. A., Lord, E., Rigotti, N. A., & Baer, H. J. (2022). Gender differences in the amount and type of student participation during in-person and virtual classes in academic medicine learning environments. JAMA Network Open, 5(1), 1. https://doi.org/10.1001/jamanetworkopen.2021.43139
*Dr Victoria Scudamore
Newcastle University Medicine Malaysia
No. 1 Jalan Sarjana 1,
Kota Limu, EduCity@Iskandar,
Iskandar Puteri, Johor, Malaysia, 79200
Email: victoria.scudamore@nhs.net
Submitted: 5 July 2023
Accepted: 12 December 2023
Published online: 2 July, TAPS 2024, 9(3), 1-14
https://doi.org/10.29060/TAPS.2024-9-3/OA3045
Dujeepa D Samarasekera1, Shuh Shing Lee1, Su Ping Yeo1, Julie Chen2, Ardi Findyartini3,4, Nadia Greviana3,4, Budi Wiweko3,5, Vishna Devi Nadarajah6, Chandramani Thuraisingham7, Jen-Hung Yang8,9, Lawrence Sherman10
1Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Family Medicine and Primary Care/ Bau Institute of Medical and Health Sciences Education, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong; 3Medical Education Center, Indonesia Medical Education & Research Institute (IMERI), Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia; 4Department of Medical Education, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia; 5Department of Obstetrics and Gynaecology, Faculty of Medicine Universitas Indonesia/Cipto Mangunkusumo Hospital, Jakarta, Indonesia; 6IMU Centre of Education and School of Medicine, International Medical University, Kuala Lumpur, Malaysia; 7Department of Family Medicine, School of Medicine, International Medical University, Kuala Lumpur, Malaysia; 8Medical Education and Humanities Research Center and Institute of Medicine, College of Medicine, Chung Shan Medical University, Taichung, Taiwan; 9Department of Dermatology, Chung Shan Medical University Hospital, Taichung, Taiwan; 10Meducate Global, LLC, Florida, USA
Abstract
Introduction: Continuing medical education and continuing professional development activities (CME/CPD) improve the practice of medical practitioners and allowing them to deliver quality clinical care. However, the systems that oversee CME/CPD as well as the processes around design, delivery, and accreditation vary widely across countries. This study explores the state of CME/CPD in the East and South East Asian region from the perspective of medical practitioners, and makes recommendations for improvement.
Methods: A multi-centre study was conducted across five institutions in Hong Kong, Indonesia, Malaysia, Singapore and Taiwan. The study instrument was a 28-item (27 five-point Likert scale and 1 open-ended items) validated questionnaire that focused on perceptions of the current content, processes and gaps in CME/CPD and further contextualised by educational experts from each participating site. Descriptive analysis was undertaken for quantitative data while the data from open-ended item was categorised into similar categories.
Results: A total of 867 medical practitioners participated in the study. For perceptions on current CME/CPD programme, 75.34% to 88.00% of respondents agreed that CME/CPD increased their skills and competence in providing quality clinical care. For the domain on pharmaceutical industry-supported CME/CPD, the issue of commercial influence was apparent with only 30.24%-56.92% of respondents believing that the CME/CPD in their institution was free from commercial bias. Key areas for improvement for future CME/CPD included 1) content and mode of delivery, 2) independence and funding, 3) administration, 4) location and accessibility and 5) policy and collaboration.
Conclusion: Accessible, practice-relevant content using diverse learning modalities offered by unbiased content providers and subject to transparent and rigorous accreditation processes with minimal administrative hassle are the main considerations for CME/CPD participants.
Keywords: Medical Education, Health Profession Education, Continuing Professional Development, Continuing Medical Education, Accreditation
Practice Highlights
- Identifying professional practice gaps of clinicians should be the first step.
- The state of CME/CPD varies among countries and addressing relevant needs is crucial.
- Clinicians agreed that CME/CPD improves their skills and knowledge but lacked time to participate.
- Potential improvements include relevant content free from commercial bias and delivery mode.
- Systematic governance and aligned regulations by physician credentialing agencies is recommended.
I. INTRODUCTION
Lifelong learning is an essential skill for all healthcare professionals. This is particularly true when new models of healthcare delivery are being implemented and there is increased focus on outcomes and values such as shorter hospital stay, greater accountability and transparency and emphasis on patient engagement (Sachdeva, 2016; Vinas et al., 2020). Recent literature highlights that continuing medical education and continuing professional development programs (CME/CPD) are crucial in providing current contextually relevant educational and developmental activities in maintaining knowledge, skills, and performance for clinicians and have proven to be effective (Cervero & Gaines, 2015; Drude et al., 2019; Forsetlund et al., 2009). CME is defined as “educational activities which serve to maintain, develop, or increase the knowledge, skills, and professional performance and relationships that a physician uses to provide services for patients, the public, or the profession” (Accreditation Council for Continuing Medical Education, n.d.), while CPD is usually a broader and more inclusive term referring to the combination of formal CME and other activities type that are designed to assist healthcare professionals to acquire skills and knowledge essential for their professional growth (Sherman & Chappell, 2018). Critical systematic reviews of the literature have shown that CME/CPD improves practice and support professional activities of medical practitioners to deliver best patient care (Cervero & Gaines, 2015; Sachdeva, 2016).
Although CME/CPD has undergone enormous changes and growth over the past 25 years, the advancement in CPD still considerably lag behind as compared to undergraduate and graduate medical education (Sachdeva et al., 2016). Goals and objectives in CME/CPD are often poorly defined and there is a paucity of the curricular structure for medical practitioners (Sachdeva, 2016). Despite consistent evidence sharing that formal CME/CPD activities, such as conferences and workshops, have little or no long-lasting effect on medical practitioners, many CME/CPD providers continue to include these approaches as their major educational offerings while clinicians continue to attend to improve their practice (Mann, 2002). Additionally, there are environments where CME/CPD is not mandatory, and in some instances, non-existent (Sherman & Nishigori, 2020).
Despite CME/CPD’s importance, the state of CME/CPD varies widely across regions and countries. Unlike Europe and the United States, there is no parallel accreditation system for CME/CPD in Asia. CME/CPD does not follow a standard process in all countries and the requirements are also different. A short summary of the CME/CPD system in the countries which are studied in this article is provided in Appendix 1. However, there is still a lack of empirical data in understanding the CME/CPD in Asia. Only one study was conducted in Japan to assess the state of CPD in the country and to identify the gaps in the understanding of the medical practitioners’ needs (Sherman & Nishigori, 2020). Hence, this study aims to explore the state of CME/CPD in the East and South East Asian region from the perspective of medical practitioners, and make recommendations for improvement.
A. Theoretical Framework
Researchers have been proposing few theoretical frameworks which are related to CME/CPD. For this study, we will be using the Process of Change and Learning framework by Fox et al. (1989) to provide an overarching view on the process of change and learning among medical practitioners. This will be further enhanced by using adult learning theory (Knowles, 1989).
No discussion of practice informing theory in CME could exclude the work of Fox et al. (1989), who studied the process of change and learning in the lives of medical practitioners. They interviewed more than 350 medical practitioners to find out the types of learning activities that clinicians undertake and the important factors in the process of learning and change. The framework is illustrated in Figure 1.
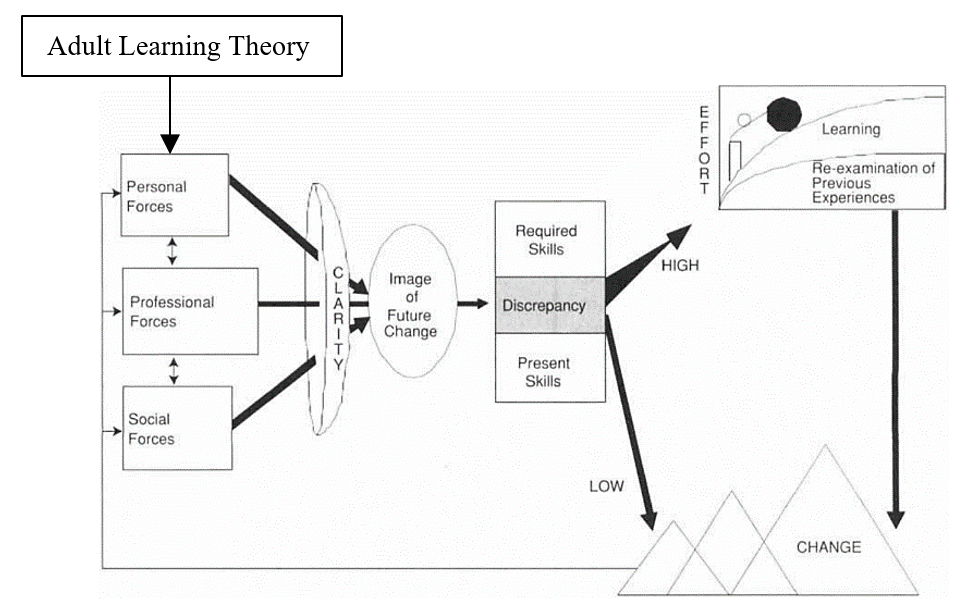
Figure 1. Theoretical Framework related to CME/CPD using the process of change and learning (Fox et al., 1989) and adult learning theory (Knowles, 1989)
This framework clearly illustrated how change and learning occurs through several processes and how these changes were influenced by three forces. The actual process of change involves three iterative steps – preparing for the change, making the change, and sustaining or implementing the change in practice.
Through validated studies, we understand that there are three forces to prepare for the change, mainly personal, professional and social forces. Professional forces were found to be the most frequently motivated change. Personal forces, such as the desire for personal well-being, were infrequent and usually not the sole force for change. More often they were combined with professional forces, e.g. the desire to further one’s career. Social forces were also cited, usually combined with professional forces, e.g. relationships with colleagues.
Once the image of change has been developed, medical practitioners will evaluate the discrepancy between what new knowledge and skills are needed to achieve the change and estimate their current capacities. As shown in Figure 1, the perceived discrepancy is positively correlated with the effort that a medical practitioner will put in in learning. Therefore, the next step may involve attending a formal CME event if the discrepancy is high – to understand what is required and to assess or verify one’s own capabilities.
Although the Process of Change and Learning Framework provides us a big picture on how medical practitioners engaged in change and learning, it is insufficient to understand the humanist approach in understanding learning for human growth. It is widely recognised that autonomy and self-directed learning are the developmental nature for human desire to learn (Personal Forces). This behaviour is usually motivated by a mixture of external and internal motivation. This is important for the development of individuals toward autonomy, the self-directed learning, reflective practice and critical reflection, experiential learning, and transformative learning.
II. METHODS
This is a multi-centred study which employed a survey using a validated questionnaire and the section below will describe the data collection process, sampling of participants and data analysis coupled with a qualitative data gathering focus group with educational experts from each place participating. Five sites were involved in this study: Hong Kong, Indonesia, Malaysia, Singapore and Taiwan. Ethical approval was obtained from the respective Institutional Review Board [Reference Number: DSRB-2019-0449 (Singapore), UW 19-840 (HKU/HA HKW IRB) (Hong Kong), KET-1035/UN2.F1/ETIK/PPMetc.00.02/2019 (Indonesia), (CCH-IRB-200425) (Taiwan), IMU 467/2019 (Malaysia)].
The same questionnaire that was used and validated previously in Japan was modified for use in this region (Nishigori and Sherman, 2018). The questionnaire is a self-administered, 28-item test comprising 27 single or multiple-choice questions and an open-ended question for comments. Respondents were asked to rate on a 5-point Likert scale (Strongly Disagree to Strongly Agree) for some of the questions. Demographic questions were included at the start of the survey (e.g. specialty, years of practice, prior participation in CME/CPD activities) followed by the following domains:
- Perceptions and satisfaction of clinicians with regard to current CME/CPD available for them
- Adequacy of the current CME/CPD available
- Impacts of CME/CPD in content coverage, evaluation, and development of learning
- Gaps in CME/CPD
- Future areas to focus on
The items were finalised following a group of experts’ meeting held in Singapore (March 2019) whereby the representatives (medical educationalists and medical practitioners) from participating sites discussed and went through the questions thoroughly. The meeting was moderated by an expert with over 28 years of experience in CME/CPD, and who designed the original study questionnaire. To add more local context and ensure that respondents were able to answer accurately, the questionnaire was translated into the native language and terms by the representatives in some locations.
Medical practitioners were invited to participate in the study. The study was conducted from July 2019 until May 2020. Voluntary, convenience, and snowball sampling was used and the representatives either disseminate the questionnaire link to their mailing list or through the various national organisation/institutions (Table 1) who then informed their members/faculty, in accordance with the ethics protocol guidelines. Reminders were sent until the response rate no longer increased. Implied consent was obtained from the participants when they proceeded to complete the survey after reading the information about the study on the first page.
|
Hong Kong |
Invitations sent by the local study investigators to members of the specialty colleges of the Hong Kong Academy of Medicine, academic colleagues and doctors who teach medical students [Note: There was no institutional dissemination] |
|
Malaysia |
|
|
Indonesia |
|
|
Singapore |
|
|
Taiwan |
|
Table 1. Organisations/Institutions in each site which disseminated the questionnaire
A. Data Analysis
The investigators from Singapore collated the anonymised raw data file from the five locations and did the first round of analysis. For quantitative data, descriptive analysis was done using Microsoft Excel to compare the data across the 5 locations. For qualitative data (1 open-ended question related to future improvements), a content analysis was used to analyse the data by grouping comments with similar concepts and assigning an appropriate category. These processes were discussed and verified by 3 coders.
III. RESULTS
A. Demographics
The number of responses received is shown in Appendix 2, together with the data from key demographic questions. The data that support the findings of this study are openly available in the Figshare repository – https://doi.org/10.6084/m9.figshare.22345111 (Samarasekera et al., 2023).
In Malaysia and Singapore, Family Physicians made up the majority of their responses, with 43.86% and 44.29% respectively. Internal Medicine clinicians were the main participants in Hong Kong (60.00%) while 42.44% of the respondents in Indonesia were General Physicians.
As for primary practice setting, the majority of respondents from 4 of the sites were from university hospital/academic health centre – Singapore (34.29%), Hong Kong (40.0%), Indonesia (29.76%) and Taiwan (94.66%). For Malaysia, government/municipal hospital (26.96%) and government health clinic (based on the responses from “Others” field) were the most common work settings.
Moving to years in medical practice, many respondents from Indonesia and Malaysia (31.22% and 48.89% respectively) were relatively younger with only 6 – 10 years of practice. Conversely, Hong Kong had the most experienced pool of respondents with 44.00% having more than 25 years of practice.
The majority of the participants had prior medical education training – Singapore (75.71%), Indonesia (85.37%) and Malaysia (78.87%). However, the reverse was observed in Hong Kong (21.74%) and Taiwan (6.85%), which may be related to not catching meaning of the item.
B. Perceptions of the Current CME/CPD System
Regarding the CME/CPD status of the respondents and the system in their place, most were aware of the system, with over 90.00% for Singapore (95.38%), Hong Kong (92.00%) and Malaysia (99.52%). Indonesia (62.44%) and Taiwan (75.34%) had lower awareness.
Regarding the understanding the need for Inter-professional Continuing Education (IPCE) [involving more than one healthcare professions) CPD in their place, more than half of the respondents (Singapore – 75.38%, Hong Kong – 56.00%, Indonesia – 87.80%, Malaysia -72.01%, Taiwan- 69.86%) were aware.
Respondents from Singapore attended more CME/CPD events compared with the others in the year leading to the survey (35.38% attended 41-50 hours; 24.62% attended more than 50 hours). However, Indonesia had 24.10% of the clinicians who did not participate in any activity at all in the last 12 months while 54.97% participated between 11-30 hours. A similar pattern was noted in Taiwan with 13.70% of the participants having not attended and 52.06% participating between 11-30 hours.
Respondents strongly agreed and agreed that participating in some form of CME/CPD would increase their skills and competence (Singapore – 83.08%, Hong Kong – 88.00%, Indonesia -81.46%, Malaysia – 89.71%, Taiwan – 75.34%) and thereby ensuring that they have current knowledge that helps to provide the best care for their patients (Singapore – 84.62%, Hong Kong – 88.00%, Indonesia – 86.34%, Malaysia – 91.38%, Taiwan – 71.23%).
When considering whether participation in CME/CPD should be mandatory for all clinicians, there were 2 distinct groups– those whereby most respondents strongly agreed and agreed (Singapore – 80.00%, Hong Kong – 88.00%, Malaysia – 83.02%) compared to Indonesia (55.61%) and Taiwan (53.42%).
C. Perceptions of Industry-supported CME/CPD
Only 30.24% in Indonesia believed that the CME/CPD in their place is free from commercial bias. However, the number is slightly higher in Hong Kong (48.00%), Malaysia (42.11%) and Taiwan (45.21%) while those from Singapore (56.92%) were more confident that CME/CPD is free from bias.
The majority of the respondents knew that pharmaceutical companies commercially supported some of these programmes that were developed by an independent education provider (Singapore – 81.54%, Hong Kong – 80.00%, Indonesia – 82.44%, Malaysia – 79.67%, Taiwan – 72.60%). Despite these, a large number had participated in these programmes (Singapore – 87.69%, Hong Kong – 68.00%, Indonesia – 64.39%, Malaysia – 84.93%) except Taiwan (57.53%).
When asked about what they think about CME/CPD that is developed by an independent CME/CPD provider with financial support from the pharmaceutical industry, these were the top 3 responses, and the first two are actually misperceptions reported regarding independent CME/CPD:
- The pharmaceutical company can suggest speakers
- The pharmaceutical company works with the educational provider to develop content
- The content is developed independently by the education company to address the needs of the learners
The proportion of respondents who selected these 3 were quite comparable across all sites It is worth noting that none from Indonesia selected “the pharmaceutical company has no influence on the content and speaker selection”. Appendix 3 shows the full data for this question along with other key questions regarding perceptions of respondents to CME/CPD funded by industry.
While approximately 75% of the respondents in Singapore, Hong Kong, Indonesia and Malaysia strongly agreed and agreed that CME/CPD developed by independent CME/CPD providers and supported by the pharmaceutical industry would be beneficial to provide current and clinically important information, the number is smaller in Taiwan (61.64%). As to whether such programmes could be counted towards CME requirement, at least two-third of the respondents in Singapore (80.00%), Hong Kong (68.00%), Indonesia (75.61%), Malaysia (69.61%) agreed and strongly agreed, while only close to half from Taiwan (49.32%) felt that it should be counted. Taiwan’s practicing clinicians suggest CME/CPD is more appropriate to be developed by independent CME/CPD providers rather than supported by the pharmaceutical industry.
D. Future CME/CPD Programme
The survey also had a question comprising 7 options to find out more about clinicians’ preferences. In all 5 locations, the more common reason is that physician will choose an activity based on the relevance of the education to their practice (Singapore – 30.00%, Hong Kong – 26.44%, Indonesia – 31.16%, Malaysia – 31.22%, Taiwan – 23.76%) or their clinical specialty (Singapore – 23.50%, Hong Kong – 26.44%, Indonesia – 21.38%, Malaysia – 29.46%, Taiwan – 27.23%). The next common reason is curiosity for the topic (but not necessarily related to practice) – Singapore (18.50%), Hong Kong (17.24%), Indonesia (15.89%), Malaysia (16.59%), Taiwan (18.81%).
To have a better understanding on the needs of the clinicians regarding CME/CPD activities, respondents were asked on the items that is missing from the CME/CPD currently available to them. The lack of a variety of educational formats such as live, online/web-based, experiential program, preceptorships (Singapore – 17.58%, Hong Kong – 14.29%, Indonesia – 12.35%, Malaysia -13.33%, Taiwan – 20.37%) and shortage of innovative learning environments and new creative formats (Singapore – 18.18%, Hong Kong – 18.57%, Indonesia – 14.74%, Malaysia – 14.35%, Taiwan – 17.28%) were the top 2 choices selected by the respondents in each place. Appendix 4 shows the full data for this question. Among the comments given for “Others”, many respondents from Indonesia felt that current courses are pricy and free courses are scarce thus would like to see more of these. It should be noted that data collection was prior to COVID-19 and thus online learning was uncommon at that time.
Key barriers to participation included courses not offered at convenient times (Singapore – 36.00%, Hong Kong – 29.41%, Indonesia – 21.46%, Malaysia – 31.34%, Taiwan – 27.03%), followed by courses not covered in their budget and topics not relevant/clinically important. For those who selected “Others”, most of them re-emphasised one of the choices (not offered at convenient time) that they did not have time.
Finally, Singapore and Malaysia respondents preferred (1) authoring medical papers and books, (2) serving as a supervisory physician in undergraduate and post-graduate clinical training programs and (3) reading journal-based or other printed materials as their top 3 weighted average mode of CME/CPD. On the other hand, those from Indonesia, Malaysia and Taiwan preferred (1) hands-on learning, (2) live regional educational activities, including lectures, seminars, workshops, and conferences and (3) attending national and international conferences/symposia (in different order among the 3 locations).
Although only one open-ended question was gathered from the participants, it had revealed rich data on the issues and challenges of CME/CPD in their own respective area. The positive comments received were quite generic. Mostly mentioned that the CME/CPD has been running well (Indonesia), acceptable and adequate, relevant and well-structured (Malaysia), still meeting the needs, adequate and organised (Taiwan) and comprehensive, structured CME for every month and good and adequate system in place with little bias in public institution (Singapore). The content analysis revealed 6 categories of areas of improvement as follows:
- Area for improvement 1: Content and mode of delivery
- Area for improvement 2: Independency and funding (includes cost)
- Area for improvement 3: Administration
- Area for improvement 4: Location and accessibility
- Area for improvement 5: Policy and collaboration
- Area for improvement 6: Others (motivation and evaluation)
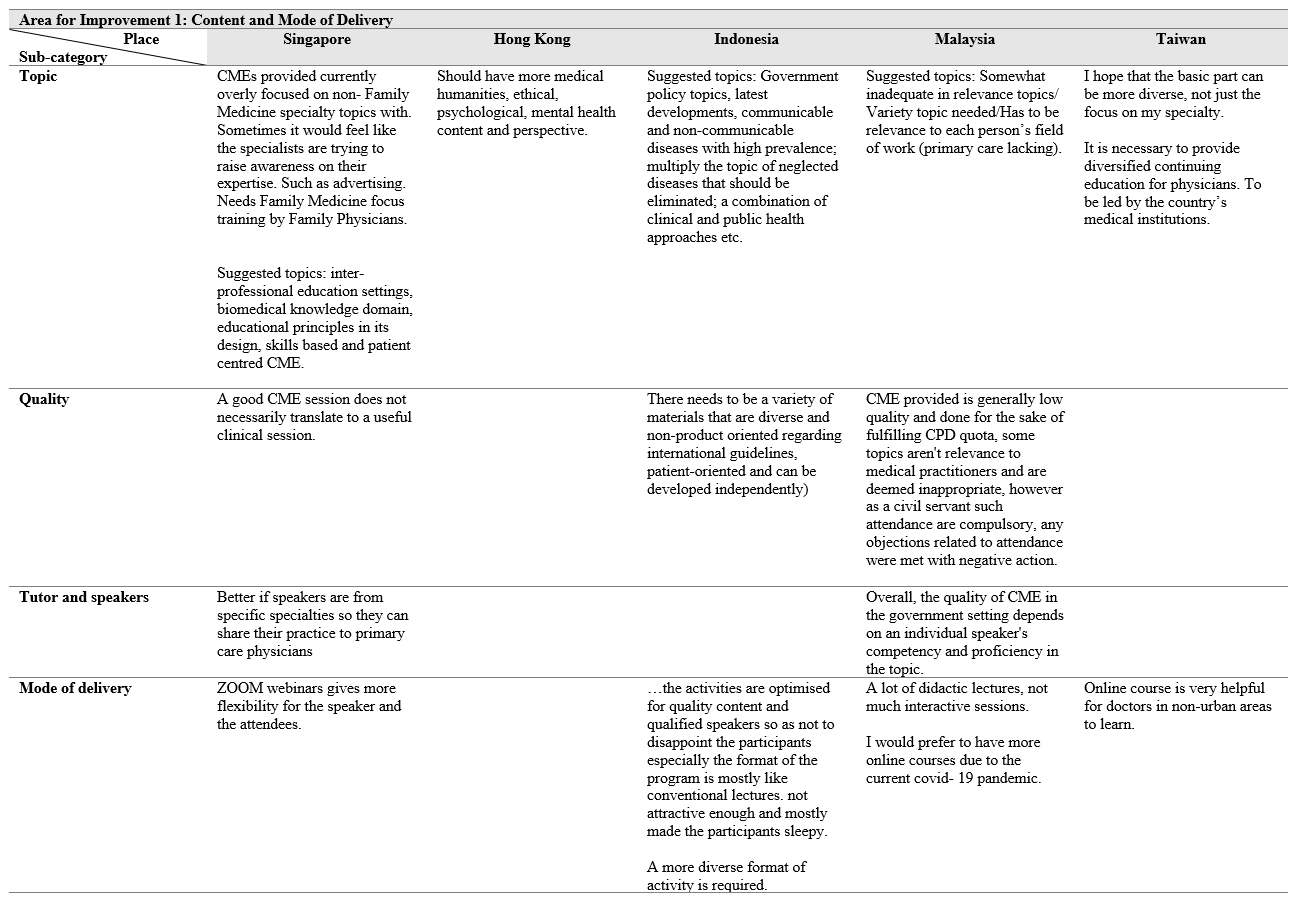
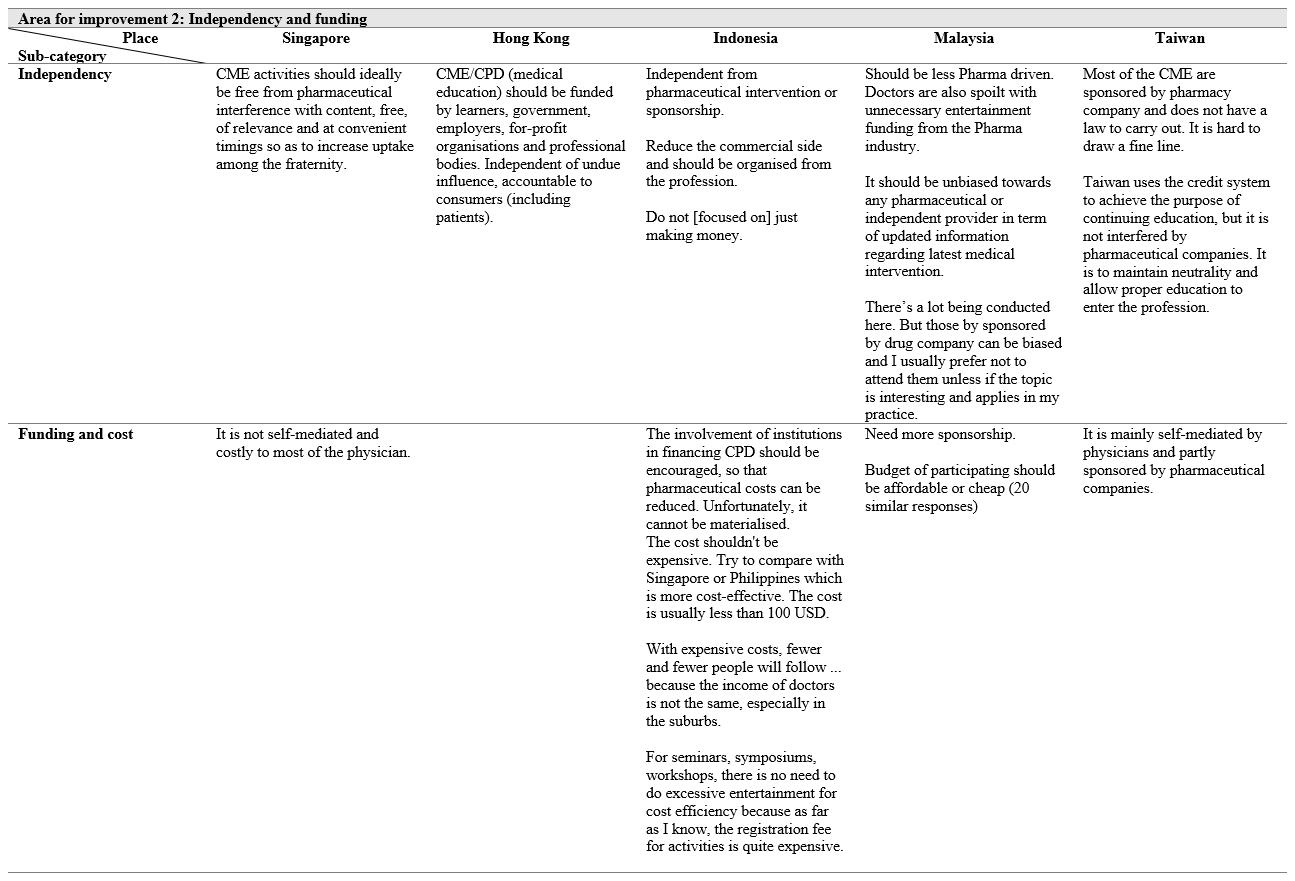
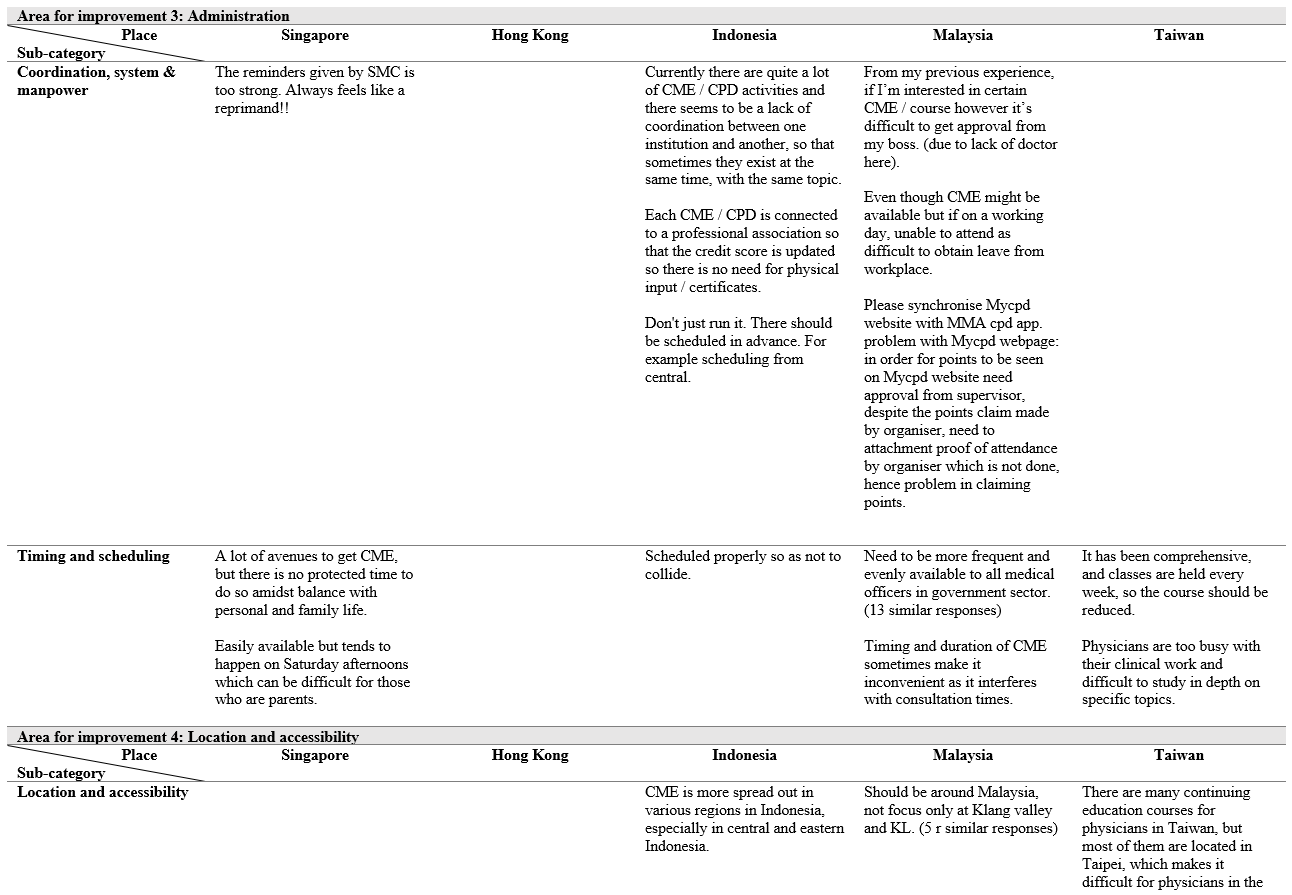
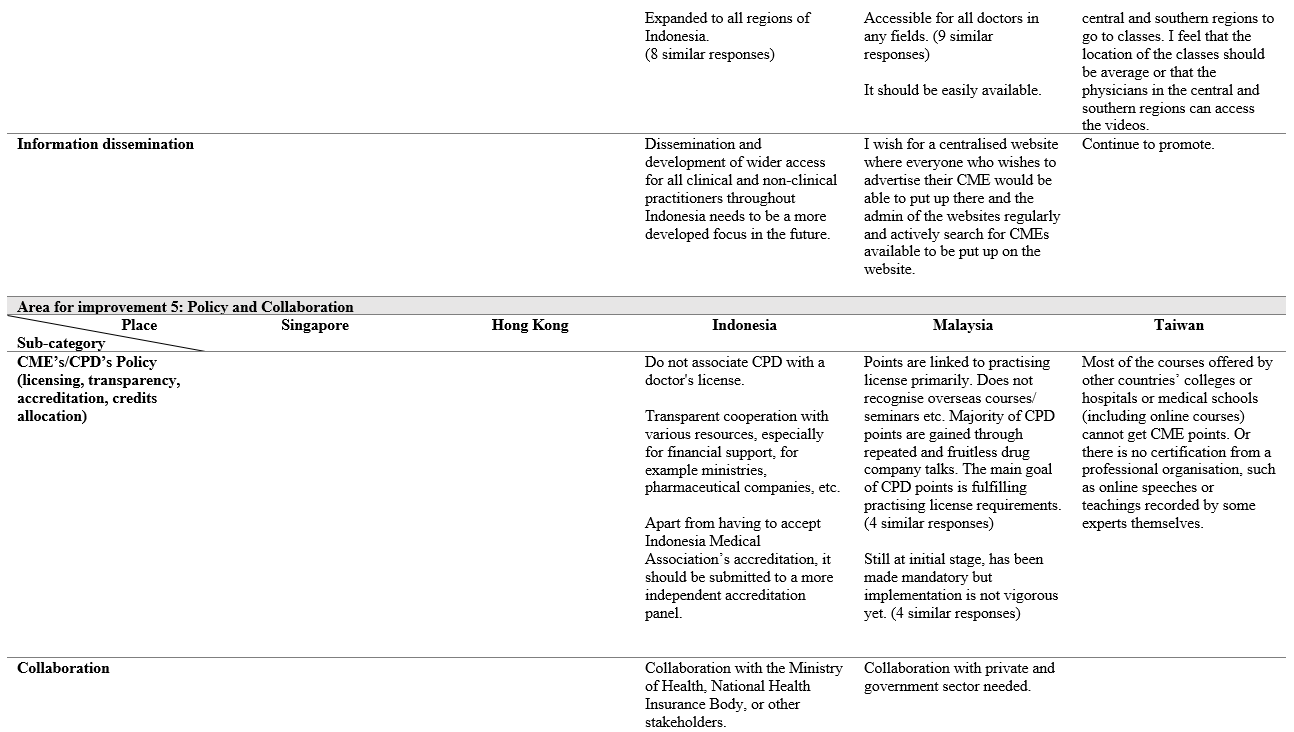
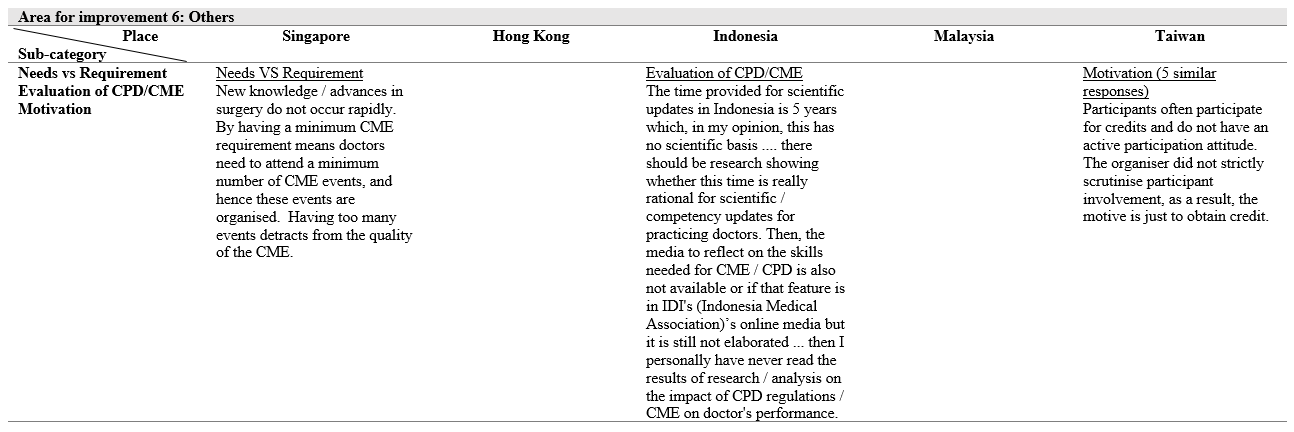
IV. DISCUSSION
The aim of this study was to survey the state of the CME/CPD systems in this region including clinicians’ perceptions on the involvement of the pharmaceutical industry and to see whether their perceptions are aligned with that of the accreditation organisations. These would allow the organisations to come up with relevant policies to improve the CME/CPD systems.
The survey seeks to explore several domains and first looked at their perceptions of the current CME/CPD programme. It is unsurprising that a large proportion of the respondents from all five areas were aware of the CME/CPD programme in their place and most strongly agreed and agreed that participating in some form of CME/CPD would increase their skills and competence (between 75.34% and 88.00%) and thereby ensuring that they have current knowledge that helps to provide the best care for their patients. This is higher than that of Japan whereby only 41% felt that their skills and competence has increased (Sherman and Nishigori, 2018).
However, while respondents from Singapore participated the most in these programmes, those from Indonesia and Taiwan did not participate as much and the two countries are also among the lowest when it comes to agreeing to make CME/CPD mandatory. This could be due to various reasons as highlighted by the question on barriers to the programmes, time constraint or accessibility (from qualitative question) or biasness against industry supported programme. Indeed, a study by Cook et al. on USA medical practitioners found that factors such as time and cost generally influence whether clinicians participate in CME/CPD activities, while topic was the key factor when choosing specific CME/CPD activities (reading an article, local activities, online courses, or attending a far-away course) (Cook et al., 2017).
Moving on to the perceptions of the industry supported CME/CPD programme, a low percentage of the respondents believed that the CME/CPD in their place is free from commercial bias. These observations are supported by qualitative comments such as “most of the CME are sponsored by pharmaceutical company and does not have a law to carry out. It is hard to draw a fine line.” (from Taiwan respondent) and “Do not [focused on] just making money (from new drug advertisement).” (from Indonesian respondent) which suggest that industry involvement is heavy in these locations. Miller and colleagues (2015) had previously looked at the credit systems in locations such as Indonesia. They found that the pharmaceutical industry provides substantial support through grants to the individual medical associations to cover the administrative and operational costs for conducting CME/CPD programmes, although membership fees also contributed to the funds (Miller et al., 2015). Good teaching requires sufficient financial resources. Internationally, most of the countries here have implemented ways to fund the training. In contrast, Indonesia is still facing funding issue and despite pharmaceutical support, medical practitioners still find that some courses are expensive. Therefore, transparency is required when working with pharmaceutical companies and there should be an independent accreditation panel for CME/CPD to ensure this transparency. Some European countries, such as Netherlands, Norway and France have even prohibited the sponsorship from pharmaceutical company for CME/CPD (Löffler et al., 2022).
Content and mode of delivery has been a common area for improvement which was raised by all 5 locations. They wanted to have more diversity and relevance to their fields for work. This is supported by the quantitative findings whereby the respondents in all five locations listed the top two factors they would use to decide whether to attend a programme – relevance of the education to their practice or their clinical specialty. Primary care/ family medicine related topic is lacking across the participating sites. Quality of the delivery is often dependent on the speakers and ZOOM is a more preferred method than didactic lectures. From the close-ended questions, respondents from all five locations would like to see a variety of educational formats (such as live, online/web-based, experiential program, preceptorships) and new creative formats. Online learning is also favourable to those who have limited access to CPD/CME. Comparing to other countries whereby peer exchange has been increasingly used as one of the teaching formats which will be awarded CME/CPD points, we are still lagging behind on how CME/CPD points should be awarded (Löffler et al., 2022). While it is required to register the CME/CPD activities before the event if medical practitioners of those events are to receive the points in countries such as Taiwan and Singapore via the CME Online Platform of Taiwan Medical Association (TMA) and Singapore Medical Council (SMC) respectively, the types of teaching formats which CME/CPD points can be awarded are restricted to activities which are conducted in the traditional formats. Due to the credit points system implemented, Taiwan’s participants expressed that motivation in attending CME/CPD has become chasing after the credit points rather than self-improvement. Malaysia, on the other hand, revealed that the CME/CPD system has just been made mandatory. The implementation of CME/CPD system in the countries examined still need to be more vigorous and flexible for the further development.
CME/CPD is also administratively challenging in Indonesia and Malaysia especially coordination in such huge countries. Hence, the CME/CPD often only takes place in the central part of the place which hinders some doctors from other regions from accessing the CME/CPD courses. Information dissemination is also affected as it is mostly populated in the central regions rather than the more rural regions. As a result, there is imbalanced training among the doctors in rural and urban regions. Having a system that automatically update the credit points instead of doing it manually and synchronisation of different systems to have an overview of the record are some challenges faced in Indonesia and Malaysia. This does not seem to be happening in other European countries as the organisation is carried out by numerous bodies or institutions in a structured manner and are accredited (Löffler et al., 2022). Therefore, operationalisation of CME/CPD will have to be streamlined so that more medical practitioners can benefit from it.
While personal forces and professional forces may motivate medical practitioners to improve their knowledge and skills by taking up courses in CME/CPD, a lack of support from the leaders and change in the system may deter the involvement. Participants have shared that difficulty in taking leave since it will interfere with consultation time, and a lack of doctors in the workplace have led to disapproval from the leader to join CME/CPD. Without proper protected time and resources, the lack of training for medical practitioners will continue to perpetuate.
A. Limitations
There are several limitations to this study. First, this study was conducted prior to the onset of COVID-19. Hence, some of the findings, especially those on the format of CME/CPD, may not be so relevant since most of these programmes are now online. Next, the response rate was not very high in some sites, and for some, many respondents were from the same work setting or speciality. Thus, the findings may not be fully generalisable in these aspects.
V. CONCLUSION
The medical associations in each place is tasked with coming up with educational programmes that meet the needs of a diverse physician workforce. A better understanding of the perspectives of its medical practitioners and implementation of relevant changes could improve clinical care. The recommendations shared in this paper may assist other medical associations with similar issues and for future development of CME/CPD for the countries.
Notes on Contributors
Dujeepa Samarasekera and Shuh Shing Lee designed and led the study in Singapore, contributed in the data collection and analysis, as well as in manuscript development.
Su Ping Yeo contributed to the data collection in Singapore, analysis and manuscript development.
Julie Chen designed and led the study in Hong Kong, contributed in the data collection and analysis, as well as in manuscript development.
Ardi Findyartini designed and led the study in Indonesia, contributed in the data collection and analysis, as well as in manuscript development.
Nadia Greviana led the data collection in Indonesia, contributed in the data analysis and manuscript development.
Budi Wiweko assisted in the study design in Indonesia, contributed in the data analysis and manuscript development.
Vishna Devi Nadarajah designed and lead the study in Malaysia, contributed to data collection, analysis and manuscript development.
Chandramani Thuraisingham contributed to data collection in Malaysia, analysis and manuscript development.
Jen-Hung Yang designed and lead the study in Taiwan, contributed to data collection, analysis and manuscript development.
Lawrence Sherman designed and led the study, contributed in the data collection and analysis, as well as in manuscript development.
Ethical Approval
This study was given an approval by the following:
Hong Kong: UW 19-840 (HKU/HA HKW IRB)
Indonesia: KET-1035/UN2.F1/ETIK/PPMetc.00.02/2019
Malaysia: IMU 467/2019
Singapore: NHG Domain Specific Review Board (2019/00449)
Taiwan: CCH-IRB-200425
Data Availability
The data that support the findings of this study are openly available in Figshare repository – https://doi.org/10.6084/m9.figshare.22345111
Acknowledgement
The Hong Kong research team would like to thank Professor CS Lau (Dean) and Professor Gilberto Leung (Associate Dean (Teaching and Learning) of the LKS Faculty of Medicine, The University of Hong Kong for their support and for facilitating survey administration and Ms Joyce Lai for research assistance.
The Indonesian research team would like to thank representatives from the Indonesian Medical Association, colleges and directors of specialty education programs who support this study by facilitating the survey administration.
The Malaysian research team would like to thank the Academy of Family Physicians of Malaysia and the Academy of Medicine of Malaysia who supported this study by facilitating the survey administration.
Funding
This study was supported with funding from Pfizer.
Declaration of Interest
The authors declare no conflict of interest. The funding provided by Pfizer is purely to survey the state of CME/CPD in the region, with no commercial interest.
References
Accreditation Council for Continuing Medical Education (n.d.). CME content: Definition and examples. ACCME. Retrieved June 23, 2021 from https://www.accme.org/accreditation-rules/policies/cme-content-definition-and-examples
Cervero, R. M., & Gaines, J. K. (2015). The impact of CME on physician performance and patient health outcomes: An updated synthesis of systematic reviews. The Journal of Continuing Education in the Health Professions, 35(2), 131–138. https://doi.org/10.1002/chp.21290
Cook, D. A., Blachman, M. J., Price, D. W., West, C. P., Berger, R. A., & Wittich, C. M. (2017). Professional development perceptions and practices among U.S. physicians: A cross-specialty national survey. Academic Medicine, 92(9), 1335–1345. https://doi.org/10.1097/ACM.0000000000001624
Drude, K. P., Maheu, M., & Hilty, D. M. (2019). Continuing professional development: Reflections on a lifelong learning process. The Psychiatric Clinics of North America, 42(3), 447–461. https://doi.org/10.1016/j.psc.2019.05.002
Forsetlund, L., Bjørndal, A., Rashidian, A., Jamtvedt, G., O’Brien, M. A., Wolf, F., Davis, D., Odgaard-Jensen, J., & Oxman, A. D. (2009). Continuing education meetings and workshops: Effects on professional practice and health care outcomes. The Cochrane Database of Systematic Reviews, 2009(2), Article CD003030. https://doi.org/10.1002/14651858.CD003030.pub2
Fox, R. D., Mazmanian, P., & Putnam, R. W. (1989). Changing and learning in the lives of physicians. Praeger.
Knowles, M. (1989). The making of an adult educator. Jossey-Bass.
Löffler, C., Altiner, A., Blumenthal, S., Bruno, P., De Sutter, A., De Vos, B. J., Dinant, G., Duerden, M., Dunais, B., Egidi, G., Gibis, B., Melbye, H., Rouquier, F., Rosemann, T., Touboul-Lundgren, P., & Feldmeier, G. (2022). Challenges and opportunities for general practice specific CME in Europe – A narrative review of seven countries. BMC Medical Education, 22(1), Article 761. https://doi.org/10.1186/s12909-022-03832-7
Mann, K. V. (2002). Thinking about learning: Implications for principle-based professional education. The Journal of Continuing Education in the Health Professions, 22(2), 69–76. https://doi.org/10.1002/chp.1340220202
Miller, L. A., Chen, X., Srivastava, V., Sullivan, L., Yang, W., & Yii, C. (2015). CME credit systems in three developing countries: China, India and Indonesia. Journal of European CME, 4(1), Article 27411. https://doi.org/10.3402/jecme.v4.27411
Sachdeva, A. K. (2016). Continuing professional development in the twenty-first century. The Journal of Continuing Education in the Health Professions, 36(Suppl 1), S8–S13. https://doi.org/10.1097/CEH.0000000000000107
Sachdeva, A. K., Blair, P. G., & Lupi, L. K. (2016). Education and training to address specific needs during the career progression of surgeons. The Surgical clinics of North America, 96(1), 115–128. https://doi.org/10.1016/j.suc.2015.09.008
Samarasekera, D. D., Lee, S. S., Yeo, S. P., Chen, J., Findyartini, A., Greviana, N., Wiweko, B., Nadarajah, V. D., Thuraisingham, C., Yang, J. H., & Sherman, L. (2023). Data from Each Participating Country [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.22345111
Sherman, L. T., & Chappell, K. B. (2018). Global perspective on continuing professional development. TheAsia Pacific Scholar, 3(2), 1-5. https://doi.org/10.29060/TAPS.2018-3-2/GP1074
Sherman, L., & Nishigori, H. (2020). Current state and future opportunities for continuing medical education in Japan. Journal of European CME, 9(1), Article 1729304. https://doi.org/10.1080/21614083.2020.1729304
Vinas, E. K., Schroedl, C. J., & Rayburn, W. F. (2020). Advancing academic continuing medical education/Continuing professional development: Adapting a classical framework to address contemporary challenges. The Journal of Continuing Education in the Health Professions, 40(2), 120–124. https://doi.org/10.1097/CEH.0000000000000286
*Dujeepa D. Samarasekera
10 Medical Drive,
Singapore 117597
Email address: dujeepa@nus.edu.sg
Submitted: 2 September 2023
Accepted: 9 January 2024
Published online: 2 July, TAPS 2024, 9(3), 15-21
https://doi.org/10.29060/TAPS.2024-9-3/OA3129
Uzma Khan
Department of Clinical Sciences, College of Medicine, Al Rayan Colleges, Saudi Arabia
Abstract
Objectives: To compare the cut scores and pass/fail rates achieved by arbitrary 60% method and Hofstee method in an undergraduate year 4 end semester objective structured clinical examination (OSCE) and check the possibility of using Hofstee method of standard setting in future exams.
Method: 102 medical students of year 4 underwent a 10 station OSCE exam conducted in a state of art simulation lab in 3 cycles. The cut scores were calculated using arbitrary method aiming at 60% of task achievement and by Hofstee method. The student’s obtained scores were compared for cut scores and pass rates for individual stations and the entire exam.
Results: The arbitrary and Hofstee methods of standard setting leads to different cut scores. For the individual stations it was 60% vs 65-70% and for the overall score it was 60% vs 70%. The percentage of students failing the exam is 13.7% based on arbitrary scores and is 29.4% when Hofstee cut score is applied.
Conclusions: The two methods lead to different cut scores and students’ failure rates. Overall, Hofstee method is more appropriate for assessing competencies in an OSCE exam in medical schools as it leads to calculation of cut scores based on the difficulty level of the station/exam and the examiners expected level of performance by the students.
Keywords: Objective Structured Clinical Examination, Standard Setting, Hofstee Method, Arbitrary Method
Practice Highlights
- Standard settings of OSCE identifies objective, reliable and valid cutoff scores.
- Arbitrary method scrutinises the test content and nominates the percentage of items to be answered correctly.
- Hofstee method is calculative and avoids illogical very high and low scores.
- A retrospective descriptive study design assessing applicability of Hofstee method in low stake exam in a private medical school in Saudi Arabia.
- Students’ failure rate increased with applying Hofstee standard settings in OSCE.
I. INTRODUCTION
Objective structured clinical examination OSCE is invented in 1975 by Harden (Harden & Gleeson, 1979) for the assessment of learners’ clinical competences and behaviors by using actors and choreographed storylines (Hodges, 2003). He succeeded in controlling the classic variables, the patient and the examiner, that enabled him to establish a comprehensive and objective assessment (Khan et al., 2013) of competence by defining clearly what skills, attitudes, problem solving capabilities and factual knowledge are to be measured (Harden et al., 1975).
As quoted by Harden “Competency is the compound of cognitive, psychomotor and affective skills as appropriate, while competence is an attribute of a person” (Khan et al., 2013).
During an OSCE, candidates are supposed to execute different clinical tasks in a simulated setting (Khan et al., 2013). As a rule, the students rotate through several time limited stations in which they are expected to interact with a standardised patient (SP), mannequins or simulation models and perform a specified task meanwhile they are being assessed by examiners using standardised rating instruments (Pugh & Smee, 2013). OSCE gets rid of many detrimental concepts in examining students, faced previously with other exam methods, by compelling them all to go through the same scope and criteria for assessment (Zayyan, 2011). This has made it a valuable evaluative tool in medical practice, so it has been adopted in countries all over the world, in all the high stakes examinations in USA (Dwivedi et al., 2020), Canada (Pugh & Smee, 2013), and the UK (Gormley, 2011).
Reliability and validity of the OSCE exam is directly related to how it is implemented (Harden & Gleeson, 1979) and can be maximised by several ways, the first and the foremost is the designing of structured reconcilable mark schemes for several stations observed by different trained assessors which will eliminate the individual assessor bias (Gormley, 2011). Competence assessment will be more reliable by arranging a variety of patient presentations for different cases and skills and standardising patients’ performance (Dent et al., 2021; Khan et al., 2013).
As a prerequisite of a good test, a process called standard setting must be set that if followed will lead to a fair decision (Boulet et al., 2003). The inferences derived from a test result matter a lot to the examiners, examinees and the institutes (Norcini et al., 2011). Cusimano in his review paper defines standard setting as a process that determines “what is good enough” for assessing competence, which itself is continuously changing, and leads to separation of a competent student from an incompetent (Cusimano, 1996). According to Harden the standard is the score that decides pass fail status of the students, also known as pass fail point. It provides an answer to the question” how much or what is good enough to know?” (Dent et al., 2021). He has defined the standard setting as the process of translating a description of characteristics denoting the desired level of performance into a number that applies to a particular test” (Dent et al., 2021).
At the time of setting the standards, the purpose of the exam must be considered (Kamal et al., 2020) along with the consequences of letting an incompetent examinee get through the exams and acquire medical licensure that could be devastating (Gormley, 2011).
Standard setting methods are designated into norm-referenced, criterion-referenced methods and a third category of combination or compromise methods (Dwivedi et al., 2020; Kamal et al., 2020). In absolute or criterion referenced standards a benchmark is set based on certain predefined criteria and the candidate performance is tested according to that standard competency or mastery. Whereas Norm-referenced, also called relative methods, are based on identification of the cut-off score relative to performance of the group or top scoring students taking the examination, which results in loss of motivation for progressing and improving in top scoring students (Dwivedi et al., 2020).
For assessing the quality of OSCE exam, the determinants are dictated by the method of standard setting. The AMEE Guide 85 describes a number of standard setting methods of which Cohen, Angoff, Borderline Regression, Borderline Group, Hofstee Method, and the fixed arbitrary 60% method are some of the commonly used (McKinley & Norcini, 2014).
Cohen method is the best form of the norm-referenced standard setting methods extensively used in low stakes exams. The best performing students’ mark is used as a reference point to define the difficulty of the exam. The remaining students’ scores are arranged from the lowest to the highest scores; the mean value of the top 5% of the scores is calculated, and finally, 60% of the total mean score is considered as the standard/passing score (Kamal et al., 2020).
Angoff method is entirely based on test/examination items (Pell et al., 2010). In this method the pass mark is statistically calculated on item or station characteristics, and it varies according to the difficulty level of the station defined by the items on checklist, but the students’ performance is not taken into consideration. (Dwivedi et al., 2020; Impara & Plake, 1997).
The borderline methods are reasonable and defensible as they are based on candidates’ performance (Kaufman et al., 2000; Pell et al., 2010). So borderline regression and modified borderline Group methods are also known as “Examinee centered” methods (Dwivedi et al., 2020). Borderline group methods necessitate the examiner be able to identify what is considered as minimally acceptable performance. The mean or median score of minimally acceptable performances is declared as cutoff score (Cusimano, 1996; Humphrey-Murto & MacFadyen, 2002). Apart from checklist scores, a global grade is also awarded which provides insights into quality of assessment (Pell et al., 2010; Smee et al., 2022).
Hofstee method aims to achieve a balance between the norm and criterion reference judgements and is a combination/compromise method (Dwivedi et al., 2020). In this method the examiners specify 4 values before the exam: the maximum and the minimum percentage correct, and the maximum and minimum acceptable percentage of failures (Smee et al., 2022). This method is more calculative, but it avoids illogical very high and very low scores (Cusimano, 1996; Kamal et al., 2020).
The arbitrary 60% method uses faculty wide standard of passing score of 60% in OSCE exam and is the easiest to implement (Humphrey-Murto & MacFadyen, 2002; Kamal et al., 2020; Kaufman et al., 2000).
Until August 2022, the clinical science department at Al Rayyan college of medicine was applying an arbitrary cut off score of 60% as a passing score for OSCE. This decision had always been based on tradition, without taking test content or students’ performance into consideration. The need for a process to differentiate well between a student with adequate competencies from those having inadequate competencies had always been observed (Khan et al., 2013). The examinee centered Hofstee method can help us to adjust cut scores for a station according to its difficulty level and accepted number of students unable to pass such a station. (Downing et al., 2006; Dudas & Barone 2014; Hofstee, 1983).
The purpose of this study is to compare the pass /fail rates of students achieved by applying arbitrary and the Hofstee methods and to assess if Hofstee method can provide us satisfactory results.
II. METHODS
The current study is a descriptive study design conducted at Al Rayyan college of medicine department of clinical science. Al Rayan college of medicine, Al Rayan national colleges is a newly established private institute based in Al-Medina Al-Munawara, under Ministry of education at Kingdom of Saudi Arabia. Having been established in 2017, the first batch of graduates have completed MBBS and have joined the local and international health sector. Currently there are 700 students enrolled and studying in 6 academic years.
This study includes a total number of 102 year 4 students undertaking the final OSCEs in the general practice 1 course with foundation to general practice, Cardiovascular system (CVS) and endocrine and breast modules during semester 1 of academic year 2022-23. The project was approved by the Research Ethical Committee (REC) of Al Rayyan colleges. All the students consented to the use of their data for research and quality control purposes with the agreement that any reports would only use aggregate data with all personal identifiers removed.
The OSCE consisted of 10 stations that sampled common and important patient presentations. Examinees were required to complete each station within 07 min. Performance was scored using 10 predefined competencies related to general practice competencies aligned to course learning outcomes CLOs, designed under the umbrella of the competence specifications for Saudi medical graduates (Saudi Meds). Skill competency assessed were (1) history taking, (2) physical examination, (3) analysis and interpretation of findings, (4) communication, (5) suggestion of appropriate investigations, (6) listing relevant differential diagnoses, (7) management care plan development. For values assessment, there were three competencies: (1) ethical rules and confidentiality, (2) taking and maintaining consent, and (3) time management. Three to four of these competencies were assessed in each station except for clinical approach; management stations where only one competency is evaluated.
3 panels were laid down, each having 10 stations and 2 circuits of students. Students rotated through the stations completing a single circuit in an anticlockwise manner. Every student was examined by a single examiner at each station except for the station of data interpretation chest Xray which was just monitored by a silent invigilator and students were recording their answers on answer sheet.
Examiners were all trained faculty staff from department of clinical sciences, 12 examiners belonged to the college faculty, 17 joined from Taibah college of medicine, Taiba university. They received formal training sessions 2 hours ahead of the exam that began with information about the OSCE (fundamentals, competencies being assessed, rating guidelines and cases and question items were explained), followed by instructions on scoring through a google link. Four Hofstee questions were presented, discussed and answered by each examiner for each station and the mean percentage for each of the four questions across all examiners was computed. Meanwhile examiners were asked to answer the same four questions for the overall scores for the exam.
During the OSCE, examiners scored examinee performances within their assigned stations using the 20-26 items scale for each station except for interpretation; chest x ray station which was the only station having 5 item scale. Global ratings (overall assessment from 0 to 5) were also included.
The examiners decided that the cut score for minimally acceptable performance for the whole exam should be no lower than 57.5% and no higher than 76%. Similarly, they indicated that the failure rate should be at least 9% but no higher than 32%.
For cut score calculation, the student’s obtained score is plotted with scores along X coordinate and the number of candidates along the Y coordinate. A line graph is drawn showing the score and the number of students obtaining that score. The finally calculated Hofstee limits of cut scores and failure rates are drawn on the graph, which resulted in generation of a rectangle, the cross diagonal from top left of the rectangle to bottom right is drawn. The place where it intercepts the plot of cumulative number of candidates is the cut score for the stations. The graph is shown in figure 1. The same graphs were drawn for the individual stations and their cut scores were calculated. The detail of each station is not mentioned to avoid complexity.
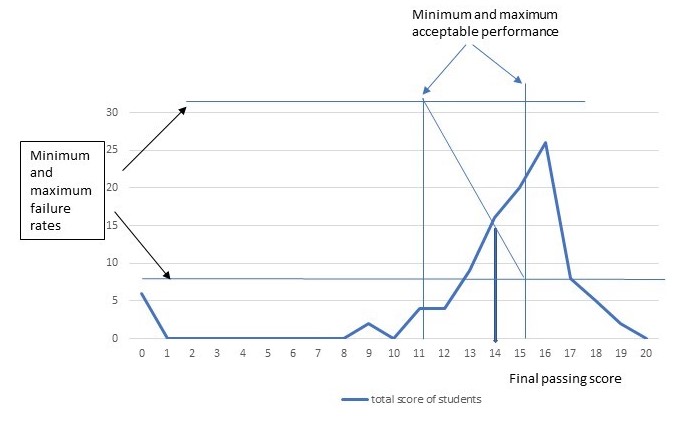
Figure 1. Calculation of final cut score based on examiners provided four Hofstee values
Arbitrary cut score of 60% is applied to students achieved scores and the pass/fail percentage is calculated and recorded in table 2.
III. RESULTS
The OSCE went on without any significant issues. The data provided by the Exam and evaluation Unit (EEU) according to their software showed that the mean score was 75% with a standard deviation of 3.99% and an alpha coefficient of 1.03. Station wise descriptive results show a range in mean scores from 61 to 84%, illustrating a range in station difficulty. The detailed analysis of each station is shown in table 1.
|
Station |
Average % |
SD |
Variance |
Cronbach alpha if item deleted |
Coefficient of determination R2 |
Inter-grade discrimination |
|
Station 1 |
0.69 |
0.47 |
0.22 |
0.94 |
0.73 |
0.03 |
|
Station 2 |
0.84 |
0.23 |
0.05 |
0.74 |
0.62 |
0.03 |
|
Station 3 |
0.77 |
0.21 |
0.04 |
0.76 |
0.46 |
0.02 |
|
Station 4 |
0.73 |
0.33 |
0.11 |
0.72 |
0.60 |
0.03 |
|
Station 5 |
0.73 |
0.22 |
0.05 |
0.67 |
0.28 |
0.02 |
|
Station 6 |
0.61 |
0.56 |
0.31 |
0.68 |
0.62 |
0.03 |
|
Station 7 |
0.83 |
0.99 |
0.08 |
0.82 |
0.74 |
0.02 |
|
Station 8 |
0.78 |
0.32 |
0.10 |
0.83 |
0.46 |
0.02 |
|
Station 9 |
0.81 |
0.21 |
0.04 |
0.64 |
0.45 |
0.02 |
|
Station 10 |
0.71 |
0.38 |
0.14 |
0.81 |
0.67 |
0.03 |
Table 1. Stations Analysis
The descriptive results for the individual stations with their titles, maximum, minimum and average scores obtained are illustrated in Table 2. The cut scores calculated by arbitrary and hofstee methods are applied to the stations and accordingly pass percentages achieved are shown in Table 2.
|
Station |
Mean % |
Minimum marks obtained |
Maximum Marks obtained |
Cut score Hofstee method (%) |
Pass rate according to Hofstee cut score (%) |
Cut score arbitrary method (%) |
Pass rate according to arbitrary cut score |
|
1. History taking DKA patient |
69.1% |
16% |
95.9% |
65 |
63 |
60 |
64.7 |
|
2. Clinical examination of a breathless patient |
83.31% |
37% |
97.3 |
70 |
85 |
60 |
92 |
|
3. Clinical examination breast |
76.99% |
45% |
100 |
70 |
72 |
60 |
89 |
|
4. Clinical approach management of hypertension |
73.31% |
31% |
100% |
70 |
53 |
60 |
73 |
|
5. History taking of a febrile patient |
73.36% |
50% |
92% |
70 |
63 |
60 |
86 |
|
6. Data interpretation chest Xray |
61.17% |
11.1% |
100% |
65 |
54 |
60 |
54 |
|
7. Clinical examination abdomen |
82.68% |
41% |
97.5% |
65 |
84 |
60 |
86 |
|
8. Clinical approach obesity management |
78.48% |
34.3% |
96.8% |
65 |
75 |
60 |
81 |
|
9. History taking breathlessness |
80.80% |
45.7% |
97.1% |
70 |
80 |
60 |
90 |
|
10. Examination neck swelling |
70.47% |
0% |
100% |
70 |
52 |
60 |
70 |
Table 2. Station wise descriptive statistics, the two cut scores and students pass rates according to cut scores
The mean score for the station reflects its level of difficulty ranging from 61.17% to 83.3%. The cut score of the individual stations for the Hofstee method was higher than the cut score for the arbitrary method. So is the difference in pass rates, pass rates achieved with arbitrary cut scores are higher than with Hofstee method, as shown in Table 3.
|
Method |
Cut scores (%) |
Number of students declared Pass |
Pass percentage (%) |
|
Arbitrary method |
60 |
88 |
86 |
|
Hofstee method |
70 |
72 |
70.5 |
Table 3. Comparison of overall cut scores and pass rates
Using Hofstee method and cut of score of 14 out of 20 passing rates achieved is 72 out of 102 which in percentage makes 70.5%. When compared with arbitrary method and cut score of 12 out of 20, students pass rate increased to 88 out of 102 leading to 86% overall. This study points out a higher pass rate for the students by arbitrary method, which creates a doubt on the competency of passing students.
IV. DISCUSSION
In this research, the results of end semester OSCE exam are compared by two methods, arbitrary fixed 60% standard setting method used at our college for the last 4 years and a compromise Hofstee method, which is applied for the very first time.
According to our study, the failure rate has increased from 13.7% to 29.4%, and has almost doubled. In fact, this increase is higher than what had been usually observed previously. This gives the impression that the students who have not yet achieved the required competency would have been allowed to pass. The same observation was made by Dudas et all who did apply Hofstee standard setting to a historic cohort of 116 Johns Hopkins University School of Medicine students from the academic year 2012–2013 to assess the potential impact on grade distributions (Dudas & Barone 2014).
According to the results of a study conducted by Doaa Kamal in Suez Canal University, Egypt in 2020 where four standard methods, the modified Cohen’s, borderline regression, Hofstee methods, and the fixed 60% arbitrary method were compared in determining the passing score in ophthalmology OSCE exam, it was concluded that 60% fixed arbitrary method resulted in a marked difference in failure and pass rates among students and Hofstee method yielded low pass rates which is consistent with my research (Kamal et al., 2020).
Since our exam was dealing with the assessment of multiple competencies, so Hofstee method is more likely to produce a standard appropriate with the purpose of assessment. Secondly the cut scores were calculated by the academic staff who were very much familiar with the OSCE as an assessment tool, the curriculum and the students as well. They were all content experts, fair and open-minded. Some of them were teaching in Taibah university the same content so they were well aware of the acceptable students’ performance. The examiners were meeting the criteria set by Downing et al., so their decision regarding the cut scores and estimation of number of failing students was accepted (Downing et al., 2006).
Schindler et al in his research paper has applied Hofstee cut off scores and found that it can even be used for a multi assessment surgical clerkship and for assigning grades as well and concluded that this method has all the characteristics of an appropriate standard setting method (Schindler et al., 2007).
V. CONCLUSION
Since different competencies reflect the different level of difficulties, the cut scores need to be set for each station dealing with that competency. The arbitrary 60 % method is not appropriate to the purpose of an OSCE exam, but a cut off score calculated by using data from experts’ judgments provides a reasonable result with acceptable failing rates. Thorough and thoughtful preparation on the judges’ part is deemed important. The data gathered from this exam can be reviewed and acted in accordance with to create a standard each academic year.
Notes on Contributors
The author herself contributed to the design of the research, carried out the data acquisition and analysis, interpreted the data and prepared the manuscript.
Ethical Approval
Approval was obtained from the Institutional Research Ethics Committee (IREC) for the collection and publication of student data with approval No. HA-03-M-122-046. Informed consent is taken from the students and special permission from the dean of the college is obtained for the use of students result for this research purpose.
Data Availability
The data generated and analysed in this study are included in this published article. The raw data set analysed can be provided by the author if special interest in it is shown.
Acknowledgement
I would like to thank Dr. Yasir Naseem Khan from the department of basic medical sciences, Al-Rayan college of medicine for useful suggestions and guidance at the final stage of the project.
I would also like to thank the Dean and the Exam and evaluation Unit (EEU) of the Al-Rayan college of medicine for their support.
Funding
The study does not require any funding.
Declaration of Interest
The author declares that she has no competing interests.
References
Boulet, J. R., De Champlain, A. F., & McKinley, D. (2003). Setting defensible performance standards on OSCEs and standardised patient examinations. Medical Teacher, 25(3), 245-249. https://doi.org/10.1080/0142159031000100274
Cusimano, M. D. (1996). Standard setting in medical education. Academic Medicine, 71(10), S112-20. https://doi.org/10.1097/00001888-199610000-00062
Dent, J., Harden, R. M., & Hunt, D. (2021). A practical guide for Medical Teachers (6th ed.). Elsevier.
Downing, S. M., Tekian, A., & Yudkowsky, R. (2006). Procedures for establishing defensible absolute passing scores on performance examinations in health professions education. Teaching and Learning in Medicine, 18(1), 50-57. https://doi.org/10.1207/s15328015tlm1801_11
Dudas, R. A., & Barone, M. (2014). Setting standards to determine core clerkship grades in pediatrics. Academic Pediatrics, 14(3), 294-300. https://doi.org/10.1016/j.acap.2014.01.008
Dwivedi, N., Vijayashankar, N. P., Hansda, M., Ak, D., Nwachukwu, F., Curran, V., & Jillwin, J. (2020). Comparing standard setting methods for objective structured clinical examinations in a Caribbean medical school. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520981992
Gormley, G. (2011). Summative OSCEs in undergraduate medical education. The Ulster Medical Journal, 80(3), 127.
Harden, R. M., & Gleeson, F. (1979). Assessment of clinical competence using an objective structured clinical examination (OSCE). Medical Education, 13(1), 39-54. https://doi.org/10.1111/j.1365-2923.1979.tb00918.x
Harden, R. M., Stevenson, M., Downie, W., & Wilson, G. M. (1975). Assessment of clinical competence using objective structured examination. The British Medical Journal, 1(5955), 447–451. https://doi.org/10.1136/bmj.1.5955.447
Hodges, B. (2003). OSCE! Variations on a theme by Harden. Medical Education, 37(12), 1134-1140. https://doi.org/10.1111/j.1365-2923.2003.01717.x
Hofstee, W. K. (1983). The case for compromise in educational selection and grading. On Educational Testing, 109-127.
Humphrey‐Murto, S., & MacFadyen, J. C. (2002). Standard setting. Academic Medicine, 77(7), 729-732. https://doi.org/10.1097/00001888-200207000-00019
Impara, J. C., & Plake, B. S. (1997). Standard setting: An alternative approach. Journal of Educational Measurement, 34(4), 353-366. https://doi.org/10.1111/j.1745-3984.1997.tb00523.x
Kamal, D., Sallam, M. A., Gouda, E., & Fouad, S. (2020). Is there a “best” method for standard setting in OSCE exams? Comparison between four methods (a cross-sectional descriptive study). Journal of Medical Education, 19(1), Article e106600. https://doi.org/10.5812/jme.106600
Kaufman, D., Mann, K., Muijtjens, A., & Van Der Vleuten, C. P. (2000). A comparison of standard-setting procedures for an OSCE in undergraduate medical education. Academic Medicine, 75(3), 267-271. https://doi.org/10.1097/00001888-200003000-00018
Khan, K., Ramachandran, S., Gaunt, K., & Pushkar, P. (2013). The objective structured clinical examination (OSCE): AMEE Guide No. 81. Part I: An historical and theoretical perspective. Medical Teacher, 35(9), e1437-e1446. https://doi.org/10.3109/0142159x.2 013.818634
Khan, K., Gaunt, K., Ramachandran, S., & Pushkar, P. (2013). The objective structured clinical examination (OSCE): AMEE Guide No. 81. Part II: Organisation & administration. Medical Teacher, 35(9), e1447-e1463. https://doi.org/10.3109/0142159x. 2013.818635
McKinley, D., & Norcini, J. J. (2014). How to set standards on performance-based examinations: AMEE Guide No. 85. Medical Teacher, 36(2), 97-110. https://doi.org/10.3109/0142159x.2013.8 53119
Norcini, J. J., Anderson, M. B., Bollela, V. R., Burch, V., Costa, M. J., Duvivier, R., Galbraith, R. M., Hays, R., Kent, A., Perrott, V., & Roberts, T. (2011). Criteria for good assessment: Consensus statement and recommendations from the Ottawa 2010 Conference. Medical Teacher, 33(3), 206-214. https://doi.org/10.3109/0142159x.2011.551559
Pell, G., Fuller, R., Homer, M., & Roberts, T. (2010). How to measure the quality of the OSCE: A review of metrics – AMEE Guide No. 49. Medical Teacher, 32(10), 802-811. https://doi.org/10.3109/0142159x.2010.507716
Pugh, D., & Smee, S. (2013). Guidelines for the development of objective structured clinical examination (OSCE) cases. Ottawa: Medical Council of Canada. https://doi.org/10.13140/RG.2.1.462 2.0003
Schindler, N., Corcoran, J., & DaRosa, D. A. (2007). Description and impact of using a standard-setting method for determining pass/fail scores in a surgery clerkship. The American Journal of Surgery, 193(2), 252-257. https://doi.org/10.1016/j.amjsurg. 2006. 07.017
Smee, S., Coetzee, K., Bartman, I., Roy, M., & Monteiro, S. (2022). OSCE standard setting: Three borderline group methods. Medical Science Educator, 32(6), 1439-1445. https://doi.org/10.1007/s40670-022-01667-x
Zayyan, M. (2011). Objective structured clinical examination: The assessment of choice. Oman Medical Journal, 219-222. https://doi.org/10.5001/omj.2011.55
*Dr. Uzma Khan
Department of Clinical Sciences,
Al Rayan College of Medicine,
Al Rayan National Colleges
Madina Munawara, Saudi Arabia
Contact: +966542754680
Email: uziik2019@gmail.com, uk.yasser@amc.edu.sa
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









