Tips and Best Practices in Medical Education: Integrating Foundational and Clinical Sciences across the Medical Curriculum
https://doi.org/10.29060/TAPS.2025-10-2/TT002
Neil Osheroff
Department of Biochemistry, Vanderbilt University School of Medicine, United States of America; Department of Medicine (Hematology/Oncology), Vanderbilt University School of Medicine, United States of America
Since the time of the Flexner report, it has been accepted that science is the foundation of clinical practice (Finnerty et al., 2010; Flexner, 1910; Grande, 2009; Haramati et al., 2024; Lindsley et al., 2024; Slivkoff et al., 2019; Weston, 2018; Woods et al., 2006). However, the methods traditionally used to teach sciences to medical students have been questioned in the post-Flexner era (AAMC-HHMI Committee, 2009; Cooke et al., 2010; Fulton et al., 2012; Slivkoff et al., 2019). For nearly 100 years, the foundational sciences were taught in a discipline-oriented fashion, primarily through passive learning approaches (lectures), and largely separated from clinical practice (AAMC-HHMI Committee, 2009; Flexner, 1910). Consequently, in the pre-clerkship phase, scientific details were often overtaught and disconnected from clinical applications. This approach frequently required students to “re-learn” their foundational sciences in the setting of patient care. The disconnect between science and medicine was further exacerbated in the later phases of medical training by physicians who taught in a manner that emphasized pattern recognition over scientific underpinnings. We have come to understand that these pedagogical approaches to medical education were neither efficient nor optimal.
Adult learning theory has provided strong evidence that medical trainees are better at learning, applying information to new circumstances, and making informed clinical decisions when the foundational and clinical sciences are taught side-by-side in an integrated fashion (Bandiera et al., 2018; Bucklin et al., 2021; Kulasegaram et al., 2015; Kulasegaram et al., 2013; Lisk et al., 2016; Mylopoulos & Woods, 2014). Learning is also heighted when active rather than passive approaches are employed. In the pre-clerkship phase, small group active learning sessions (problem-based learning, team-based learning, case-based learning, etc.) provide outstanding platforms for integrating foundational and clinical sciences (Bucklin et al., 2021). Similarly, in the clinical workplace, practitioners can integrate science and medicine by probing or explaining the underlying basis of disease and treatment or employing other forms of active learning (Dahlman et al., 2018; Daniel et al., 2021; Hashmi et al., 2024; Spencer et al., 2008).
Some have questioned the need for pre-clerkship science education in medical schools, professing that the heart of medical education is the clinical experience (Emanuel, 2020). However, in the post-genomic era, this perspective would seem to be the antithesis of modern medical practice (AAMC-HHMI Committee, 2009; Haramati et al., 2024). Now more than ever, to ensure the best quality of care for their patients, physicians need to understand the scientific underpinnings of their actions.
If we truly believe that science is the foundation of clinical practice, we should not teach either in isolation. As a first step, we need to stop thinking about foundational and clinical sciences as being separate. I would argue that they are both on the spectrum of “biomedical sciences,” represent two sides of the same coin, and should be taught in an integrated fashion across the entirety of the medical school curriculum. Although this integration has been (or is being) addressed in the pre-clerkship phases at most medical schools, it has proven more challenging in the clinical phases (Brauer & Ferguson, 2015; Pettepher et al., 2016; White & Ghobadi, 2022). While science and medicine are inherently intertwined, interactions between the two in the latter phases of training are often more casual than causal. It is time for the foundational and clinical sciences to be integrated across the continuum of medical training to ensure that future physicians have the skills necessary to provide the highest caliber of care for their patients.
Acknowledgements
Work in the author’s laboratory is funded in part by NIH grants R01 GM126363 and R01 AI170546. The author is grateful to Dr. Emily Bird for critical reading of the manuscript and insightful comments.
Declaration of Interest
The author declares no conflict of interest.
References
Bandiera, G., Kuper, A., Mylopoulos, M., Whitehead, C., Ruetalo, M., Kulasegaram, K., & Woods, N. N. (2018). Back from basics: integration of science and practice in medical education. Medical Education, 52(1), 78-85. https://doi.org/10.1111/medu.13386
Brauer, D. G., & Ferguson, K. J. (2015). The integrated curriculum in medical education: AMEE Guide No. 96. Medical Teacher, 37(4), 312-322. https://doi.org/10.3109/0142159X.20 14.970998
Bucklin, B. A., Asdigian, N. L., Hawkins, J. L., & Klein, U. (2021). Making it stick: Use of active learning strategies in continuing medical education. BMC Medical Education, 21(1), Article 44. https://doi.org/10.1186/s12909-020-02447-0
AAMC-HHMI Committee (2009). Scientific foundations for future physicians.
Cooke, M., Irby, D. M., & B’Brien, B. C. (2010). Educating physicians: A call for reform of medical school and residency. Jossey-Bass.
Dahlman, K. B., Weinger, M. B., Lomis, K. D., Nanney, L., Osheroff, N., Moore, D. E., Jr., Estrada, L., & Cutrer, W. B. (2018). Integrating foundational sciences in a clinical context in the post-clerkship curriculum. Medical Science Educator, 28(1), 145-154.
Daniel, M., Morrison, G., Hauer, K. E., Pock, A., Seibert, C., Amiel, J., Poag, M., Ismail, N., Dalrymple, J. L., Esposito, K., Pettepher, C., & Santen, S. A. (2021). Strategies from 11 U.S. medical schools for integrating basic science into core clerkships. Academic Medicine, 96(8), 1125-1130. https://doi.org/10.1097/ACM.0000000000003908
Emanuel, E. J. (2020). The inevitable reimagining of medical education. JAMA, 323(12), 1127-1128. https://doi.org/10.1001/ jama.2020.1227
Finnerty, E. P., Chauvin, S., Bonaminio, G., Andrews, M., Carroll, R. G., & Pangaro, L. N. (2010). Flexner revisited: The role and value of the basic sciences in medical education. Academic Medicine, 85(2), 349-355. https://doi.org/10.1097/ACM.0b013e3181c88b09
Flexner, A. (1910). Medical education in the United States and Canada: A report to the Carnegie Foundation for the Advancement of Teaching. The Carnegie Foundation for the Advancement of Teaching.
Fulton, T. B., Ronner, P., & Lindsley, J. E. (2012). Medical biochemistry in the era of competencies: Is it time for the Krebs cycle to go? Medical Science Educator, 22(1), 29-32. https://doi.org/10.1007/BF03341749
Grande, J. P. (2009). Training of physicians for the twenty-first century: Role of the basic sciences. Medical Teacher, 31(9), 802-806. https://doi.org/10.1080/01421590903137049
Haramati, A., Bonaminio, G., & Osheroff, N. (2024). Professional identity formation of medical science educators: An imperative for academic medicine. Medical Science Educator, 34(1), 209-214. https://doi.org/10.1007/s40670-023-01922-9
Hashmi, S., Riaz, Q., Qaiser, H., & Bukhari, S. (2024). Integrating basic sciences into clerkship rotation utilising Kern’s six-step model of instructional design: Lessons learned. BMC Medical Education, 24(1), Article 68. https://doi.org/10.1186/ s12909-024-05030-z
Kulasegaram, K., Manzone, J. C., Ku, C., Skye, A., Wadey, V., & Woods, N. N. (2015). Cause and effect: Testing a mechanism and method for the cognitive integration of basic science. Academic Medicine, 90(11 Suppl), S63-S69. https://doi.org/10.1097/ACM.0000000000000896
Kulasegaram, K. M., Martimianakis, M. A., Mylopoulos, M., Whitehead, C. R., & Woods, N. N. (2013). Cognition before curriculum: Rethinking the integration of basic science and clinical learning. Academic Medicine, 88(10), 1578-1585. https://doi.org/10.1097/ACM.0b013e3182a45def
Lindsley, J. E., Abali, E. E., Asare, E. A., Chow, C. J., Cluff, C., Hernandez, M., Jamieson, S., Kaushal, A., & Woods, N. N. (2024). Contribution of basic science eeducation to the professional identity development of medical learners: A critical scoping review. Academic Medicine, 99(11), 1191-1198. https://doi.org/10.1097/ACM.0000000000005833
Lisk, K., Agur, A. M. R., & Woods, N. N. (2016). Exploring cognitive integration of basic science and its effect on diagnostic reasoning in novices. Perspectives on Medical Education, 5(3), 147-153. https://doi.org/10.1007/s40037-016-0268-2
Mylopoulos, M., & Woods, N. (2014). Preparing medical students for future learning using basic science instruction. Medical Education, 48(7), 667-673. https://doi.org/10.1111/medu.12426
Pettepher, C. C., Lomis, K. D., & Osheroff, N. (2016). From theory to practice: Utilising competency-based milestones to assess professional growth and development in the foundational science blocks of a pre-clerkship medical school curriculum. Medical Science Educator, 26(3), 491-497. https://doi.org/10.1007/s40670-016-0262-7
Slivkoff, M. D., Bahner, I., Bonaminio, G., Brenneman, A., Brooks, W. S., Chinn, C., El-Sawi, N., Haight, M., Hurtubise, L., McAuley, R. J., Michaelsen, V., Rowe, B., Vari, R. C., & Yoon, M. (2019). The role of basic science in 21st century medical education. Medical Science Educator, 29(3), 881-883.
Spencer, A. L., Brosenitsch, T., Levine, A. S., & Kanter, S. L. (2008). Back to the basic sciences: An innovative approach to teaching senior medical students how best to integrate basic science and clinical medicine. Academic Medicine, 83(7), 662-669. https://doi.org/10.1097/ACM.0b013e318178356b
Weston, W. W. (2018). Do we pay enough attention to science in medical education? Canadian Medical Education Journal, 9(3), e109-e114.
White, B., & Ghobadi, A. (2022). Models of clinical integration into basic science education for first-year medical students. Medical Teacher, 45(3), 333-335. https://doi.org/10.1080/ 0142159X.2022.2134002
Woods, N. N., Neville, A. J., Levinson, A. J., Howey, E. H., Oczkowski, W. J., & Norman, G. R. (2006). The value of basic science in clinical diagnosis. Academic Medicine, 81(10 Suppl), S124-S127. https://doi.org/10.1097/00001888-200610001-00031
Submitted: 25 January 2024
Accepted: 20 December 2025
Published online: 1 April, TAPS 2025, 10(2), 46-56
https://doi.org/10.29060/TAPS.2025-10-2/OA3228
Chhaya Divecha1, Miriam Simon2 & Ciraj Mohammed3
1Department of Paediatrics, College of Medicine and Health Sciences, National University of Science and Technology, Oman; 2Department of Psychiatry and Behavioural Science, College of Medicine and Health Sciences, National University of Science and Technology, Oman; 3Department of Medical Education, College of Medicine and Health Sciences, National University of Science and Technology, Oman
Abstract
Introduction: Paediatric milestones provide a structured method for observing and monitoring a child’s progress and should be part of core paediatric curriculum. However, a literature review reveals that primary care physicians and pediatricians feel inadequate about their knowledge and practice of developmental paediatrics, thus exposing the lacunae in training.
Methods: An intervention was planned amongst final-year medical undergraduate students in Oman during their paediatric rotation. A 90-minute multimodal active learning module incorporating diverse learning orientations was planned and administered as a skill-lab session. Its effectiveness in learner motivation, engagement, and faculty participation was evaluated using a questionnaire based on the ICAP (Interactive, Constructive, Active, and Passive) framework, administered to students at the end of the session.
Results: Responses of the 62 participants indicated a significant association between their overall experience and tasks related to the active, constructive, and interactive elements of the module (p=0.001). The faculty’s role in facilitating the session significantly contributed to students’ overall experience (p=0.000). On linear regression, active, constructive, and interactive components of the module were moderate to high predictors of the participants’ overall learning experience.
Conclusion: It was beneficial to base the teaching module on established learning theories. Active learning strategies proactively fostered student engagement and self-directed learning during the session. Faculty played an important role in planning and customising the content, flow, and delivery to maximise meaningful learning. Such interactive collaboration, especially for theoretical concepts in medicine, enables better student engagement, providing enhanced opportunities for learning, practice, and feedback.
Keywords: Active Learning, Child Development, Undergraduate Medical Education, Student Engagement, ICAP Framework
Practice Highlights
- Active learning strategies can foster student engagement in teaching paediatrics.
- The use of interactive collaboration for theoretical concepts in medicine is effective.
- The role of faculty is crucial to maximise meaningful student learning.
- Utilisation of learning theories to design modules is beneficial for successful content delivery.
I. INTRODUCTION
Clinical curriculum while preparing students for patient care frequently focuses on abnormal pathologies with normal development or physiology often being neglected or underemphasised (Densen, 2011). Developmental and behavioral paediatrics are integral components of pediatric clinical practice. Paediatric milestones provide a structured method to monitor a child’s progress with a comprehensive understanding of development across all domains (gross motor, fine motor, language, and social) and thus must be adequately addressed in the core paediatrics curriculum. However, review of literature reveals that primary care physicians and paediatricians feel inadequate about their knowledge and practice of developmental paediatrics, thus exposing the gaps in education and training (Bauer et al., 2009; Beggs et al., 2005; Bright et al., 2019; Chödrön et al., 2021; Comley et al., 2008; Honigfeld et al., 2012).
Large group didactic classrooms often involve passive reception, leading to lack of engagement among learners (Huggett & Jeffries, 2021). Undergraduate medical curriculum is transitioning from a passive, teacher-centered approach to a learner-centered, active learning strategy, which has demonstrated enhanced students’ understanding, retention of complex concepts, improved student motivation, and overall course satisfaction (McCoy et al., 2018; O’Sullivan et al., 2022). Innovative active learning approaches on developmental milestones largely employ live visits to community resource sites along with instructional videos, reflective reports, observing live parent-child pairs, and use of short video clips (Clark et al., 2012; Comley et al., 2008). In addition, interactive DVDs containing animated cartoons and questions, live interviews, case vignettes, case write-ups, stimulus videos, observation experiences, discussion groups, field trips, and personal experiences have been documented as teaching-learning strategies (Fox et al., 2007; Leiner et al., 2011). Digital resources such as “Beyond Milestones”, developed as free online material for medical professionals using real-life developmental assessments, have shown improved scores on knowledge, observational expertise, confidence, and learner satisfaction (Connolly et al., 2014).
Though observing children in real-life scenarios (including wards, outpatient departments, well-baby clinics, schools, community centers, etc.) creates opportunities for interactive and authentic learning, restrictions in availability of exposure, time, and faculty, especially during the COVID pandemic have compounded the woes of clinical training. The aforementioned reasons prompted us to develop an active learning module using the ICAP framework to introduce developmental milestones in the paediatric curriculum. This framework identifies four modes of cognitive engagement in active learning: Interactive (I), Constructive (C), Active (A), and Passive (P). Passive modes of cognitive engagement involve receipt of information, compared to active modes which require learners to physically manipulate information provided (Chi & Wylie, 2014). Engagement further increases in the constructive mode as students generate diagrams, questions, etc., and is maximum in the interactive mode where peers collaborate and co-construct knowledge through the process of questioning and responding during a conversation. Research reveals that learning achievement is lowest at P and increases in the order of A, C, and I (Chi & Wylie, 2014). Given that the ICAP framework involves both interactive and active learning, we hypothesised that its application to the education of developmental milestones would further promote and expand learning and performance of undergraduate medical students. Additionally, it would help identify and address gaps in their knowledge and understanding of developmental milestones.
In this study, we developed an innovative learning module for developmental milestones using the ICAP model. The module was active, interactive, experiential, and grounded in the major theories of learning (behaviorism, cognitivism, constructivism, humanism, and social learning theories) to maximise opportunities for learning. This pilot study aimed at testing the effectiveness of the module in terms of learner motivation, engagement, and faculty participation.
II. METHODS
The current study was conducted at a private medical college in Oman. It was a cohort study with a quantitative survey and qualitative component. Final-year undergraduate medical students doing their 6-week clinical rotation in Paediatrics were introduced to the teaching module during their skill-lab session (in groups of 6 to 8 students). Verbal consent was obtained for learner feedback.
The learning session was planned and conducted by faculty researchers with expertise in paediatrics, developmental psychology, and medical education. The learning outcomes of this module on developmental milestones were:
- To identify age-appropriate milestones in children from birth to 5 years of age.
- To apply knowledge of milestones for various domains (gross motor, fine motor, language, and social/cognitive) to assess development in various age groups (birth to 5 years).
- To differentiate between normal and delayed development in children.
The specific learning outcomes were addressed through various strategies as summarised in Figure 1.

Figure 1. Flow chart depicting the sequence of activities mapped with specific learning objectives
The module was planned for 90 minutes and included learning activities based on principles of active and adult learning. Pre-reading material for the multimodal active learning session on developmental milestones was provided (https://aqmedia.org/filestore/2/0/3/6_83bcb34c55b2770/6302_012d2ba650720b8.pdf). Various constructs that underpin major learning theories were adopted while designing the learning approaches which are detailed here:
A. Lid Opener and Think Pair Share
Having a child with a disability can profoundly affect family dynamics, resulting in psychosocial challenges like parental stress, social isolation, mobility limitations, child behavioral issues, and difficulties in coping and adjustment (Woolfson, 2004). Students were shown a short video of a child with developmental delay and its psychosocial impact on the child and family. They were then divided into pairs/groups and asked to reflect on the video in terms of how watching the video made them feel, what they believed the child and family might be going through, and why an awareness of typical developmental milestones is important. Following group discussion, one representative from each group shared the pertinent points that emerged with the larger group.
B. Discourse
The session covered fundamentals related to detection of milestones in children from birth to 5 years of age through a lecturette by faculty from the Paediatrics Department.
C. Exploration via Self-directed Learning Activity
During this section, students were briefed about the interactive activity and divided into two sub-groups (3 to 4 members per group). An instruction sheet explaining the activity was provided. A group leader for each sub-group was identified to monitor group dynamics and ensure active participation. The ‘Paediatric Developmental Milestones Interactive Table’ from Aquifer Pediatrics website’s free student resources was shown on a smart board. The table involved a grid of milestones (gross motor, fine motor, communication/social, cognitive/adaptive) against ages (2 months, 4 months, 6 months, 9 months, 12 months, 15 months, 18 months, 24 months, 2 years, 3 years, 4 years, 5 years). Students explored their knowledge of the milestones by clicking on each square and further reinforced it by double clicking (which would show appropriate video clips of 2 to 8 seconds). During this activity, learners engaged in self-directed learning through the use of the interactive table to compare milestones in various domains across age groups.
D. Case-Based Learning (CBL)-Trigger and Buzz Groups
Following the SDL activity, students were led into Case-Based learning, where they were shown a video of a child undergoing developmental assessment by a doctor. They were asked to identify milestones and estimate the developmental age of the child. To prompt further discussion, a buzz group format in small groups was employed to discuss their findings. The facilitator moved around to help and encourage participation in group discussions. After that, the sub-groups presented their findings to the entire group, which sparked additional discussion and feedback.
E. Game-Based Learning
The acquired knowledge of milestones was further intensified through gamification. A game of BINGO was played, where each student received a bingo ticket with pictures of milestones (sample in Figure 2). The facilitator drew cards from the bingo pile (with age and domain) and students were asked to identify the appropriate milestone picture for that age/domain on their ticket. The first one to get a line of 5 pictures (horizontal/vertical/ diagonal) was declared the winner.

Figure 2. Sample of bingo ticket with milestones
F. Scaffolding
The faculty would wrap up the case and summarise major learning points thus consolidating the knowledge about milestones. Throughout the learning session, the facilitator provided cognitive scaffolding by leading the students through different questions, prompts, tasks, and structured interactions enabling them to learn more about developmental milestones. Students had opportunities to work with their existing knowledge and build further on it through the various learning activities, group discussions and faculty-led facilitation.
G. Reflection on Action
Students were divided into groups (2 or 3 students per group) to reflect on their entire learning experience using Borton’s model of reflection (Rolfe, 2014). Their reflections elucidated the “what”- their experience of the activities, “so what”- how the module improved on their prior knowledge and understanding about the topics and “now what”- providing suggestions for improvement and preference for similar active learning strategies in future sessions. Individual sharing within groups was followed by sharing between groups via their representatives.
H. Data Collection and Analysis
Students were asked to complete a feedback form about their learning experience during the activity via an anonymised electronic feedback form administered at the end of the session. The form had 15 items evaluating their learning experience – 11 quantitative (Likert scale-based) and 4 qualitative questions. The quantitative feedback responses were analysed based on the four domains of the ICAP model- questions were framed for Interactive, Constructive, Active, and Passive engagement of students during the active learning strategies. There were 4 items (Max score=20) about the interactive components of the module, 3 items (Max score=15) based on constructive elements, and two items each (Max score=10) on the active and passive engagement of students during the module. In addition, 4 quantitative items assessed feedback on faculty involvement and students’ overall experience.
Data was analysed using IBM’s Statistical Package for Social Studies (SPSS 22; IBM Corp., Armonk, NY, USA). Descriptive statistical methods such as percentages, mean and standard deviation were employed. Cronbach’s alpha method was used to assess internal consistency/test reliability. The Shapiro-Wilk method was used to test normality. Inferential statistical methods such as the Spearman’s correlation analysis and Chi-square test were used to explore significant associations between variables. Linear regression was also used to explore various predictors of the participants’ learning experience. Thematic analysis was performed for qualitative feedback.
III. RESULTS
A. Overview of Study Participants
A total of 62 students from the final clinical year of the MD program participated in this study; 91% were females and 9% were males. The average age of participants was 24.4 years (SD=0.707).
Results indicate high internal consistency for the survey items developed. Full scale (15 items) Cronbach’s alpha value of 0.808 was obtained. Results of the Shapiro-Wilk test of normality for all survey items (p=0.000) indicate that participant’s responses were not normally distributed. Non-parametric tests were thus employed for data analyses.
B. Analysis of Learner Feedback
In general, participants agreed that the session on developmental milestones was enjoyable.
The preference for game-based interactive/collaborative learning was high. The learner responses categorised item wise are provided in Table 1.
|
Item |
Strongly Agree |
Agree |
Can’t say |
Disagree |
Strongly Disagree |
Mean |
SD |
|
The pre-reading material on developmental milestones was easily understandable
|
59.7% |
35.5% |
4.8% |
0 |
0 |
4.548 |
0.591 |
|
The session established clear learning outcomes and objectives.
|
91.9% |
8.1% |
0 |
0 |
0 |
4.919 |
0.274 |
|
The case-based activity on developmental milestones provided relevant opportunity to witness theory in practice.
|
83.9% |
16.1% |
0 |
0 |
0 |
4.839 |
0.370 |
|
Presentation of real-world contexts followed by discussion in groups helped me learn better.
|
88.7% |
9.7% |
1.6% |
0 |
0 |
4.871 |
0.383 |
|
The game-based activity enabled me to build an emotional connection to learning and the subject matter.
|
82.3% |
16.1% |
0 |
1.6% |
|
4.790 |
0.516 |
|
This session provided me opportunities for feedback and practice
|
83.9% |
16.1% |
0 |
0 |
0 |
4.839 |
0.370 |
|
I enjoyed the session on developmental milestones as it actively engaged me with the course material through case study and discussion.
|
87.1% |
12.9% |
0 |
0 |
0 |
4.871 |
0.338 |
|
The session assisted us in organising our thoughts, reflecting on our understanding, and finding gaps in our reasoning.
|
74.2% |
21% |
4.8% |
0 |
0 |
4.694 |
0.560 |
|
I prefer similar sessions to learn theoretical concepts in paediatrics and medicine.
|
88.7% |
9.7% |
1.6% |
0 |
0 |
4.871 |
0.383 |
|
Today’s session was well-planned and helped me work on my own to accomplish learning goals independently.
|
82.3% |
17.7% |
0 |
0 |
0 |
4.823 |
0.385 |
|
The faculty supported students in the learning process during the session.
|
98.4% |
1.6% |
0 |
0 |
0 |
4.984 |
0.127 |
|
The faculty regulated the level of information and maintained my ability to be responsible for my learning.
|
87.1% |
11.3% |
1.6% |
0 |
0 |
4.855 |
0.398 |
|
The session made me identify psychosocial issues associated with developmental delays
|
69.4% |
21% |
8.1% |
1.6% |
0 |
4.581 |
0.714 |
|
I found myself motivated, engaged and self-directed during the entire session.
|
82.3% |
14.5% |
3.2% |
0 |
0 |
4.790 |
0.483 |
|
Using the interactive online module to explore developmental milestones helped improve my learning in this area. |
66.1% |
25.8% |
6.5% |
1.6% |
0 |
4.565 |
0.692 |
Table 1. Analysis of survey responses based on dimensions of the ICAP Model
C. Analysis of Feedback on Faculty Involvement and Overall Experience
The mean score on the participants’ feedback on the involvement of faculty members during the session was 9.839 (SD=0.450) and their overall experience was 9.710 (SD=0.686).
D. Association among Various Survey Dimensions
Results indicated significant associations between learner’s overall experience and tasks related to the active component of the session (p=0.000), constructive engagement (p=.000), and interactive collaboration with peers (p=0.001). Results also indicated significant associations between the interactive and constructive components of the session (p=0.000), faculty’s role in facilitating the session and students’ overall experience (p=0.000), and faculty involvement with the passive component (designing the initial reading material) (p=0.000).
E. Spearman’s Correlation
Spearman’s correlation across the various survey dimensions based on the ICAP model indicated high positive inter-dimension correlation. A significant correlation was also seen between the survey dimensions and the full-scale scores.
F. Linear Regression
Linear regression analysis was carried out to explore various predictors of the participants’ learning experience. The active (R2=0.438), constructive (R2=0.718), and interactive components (R2=0.644) are moderate to high predictors of the participants’ overall learning experience.
G. Thematic Analysis of Qualitative Items
The following themes and elaborations emerged on analysis of student feedback relating to their experience during the active learning module on developmental milestones which are summarised in Table 2.
|
Themes |
Elaboration of theme |
Samples of students’ feedback |
|
(i) Elevated learning experience
|
Participants expressed positive feedback regarding all components of the active learning session. They enjoyed the game-based activities, technology-integrated tasks, while at the same time enhancing their knowledge on developmental disorders from a clinical perspective.
|
“The bingo game brought a surprisingly fun twist to a boring topic and the competitiveness of the group as well as the doctors fun proctoring made it an overall pleasant and enjoyable experience. In short, this was a session I’m glad I got out of bed for.” “The smart board table was an active way of remembering.” “Encourage us to learn more and attend to skill lab. It was wonderful.” “A lot better than what I thought I would feel compared to a normal session. Confident to answer any questions related to developmental milestones.” |
|
(ii) Efficacious collaborative interactions
|
Students reported increased interest in learning as the session involved working together with their peers. Participants felt that continual interaction throughout the session strengthened learning.
|
“The group interactions really helped me retain the information. It was a fun experience and something new and out of the ordinary.” “Interactions made the information much easier to understand.” “It was interactive which made it interesting.” “I interacted throughout the session, learned quite a lot of information, very helpful.” |
|
(iii) Reflective outlook to patient care
|
Participants appreciated the inclusion of humanism in the learning experience. The incorporation of reflective practice in patient and caregiver experiences is a vital component that may impact future outcomes related to patient care. |
“Playing the video which wasn’t pure scientific as usual, it is emotional also, so it touches both the doctor and the human inside me.” “Watching the video of cerebral palsy and then reflecting over why development is very important.” |
|
(iv) Supportive learning environment
|
Student feedback highlighted the presence of a positive, non-judgmental environment that ensured improvement of learning in a relaxed/ stress-free setting. |
“We were able to make mistakes and learn from them without the fear of being criticised” “It was very fun and interactive. No pressure was there and not scary.” “It was interactive and very useful and most important comfortable and didn’t feel like we were being pressured and that surely helped us learn way better.” “Very happy and I enjoyed it a lot. My favourite session since the beginning of the year… no pressure was put on us, so we were able to actually learn instead of being terrified.” |
Table 2. Thematic analysis of qualitative feedback
IV. DISCUSSION
Monitoring a child’s development over time via milestones is a core part of paediatric curriculum and practice, as it enables early identification of delay or atypical progress, allowing timely referral. As an alternative to traditional learning through lectures as practiced routinely, we utilised active learning strategies that addressed multiple learning orientations for enhanced student engagement and learning.
A. Designing the Module and Active Learning Strategies based on Learning Theories
The developmental milestone module designed to involve multimodal active learning strategies has been described in the methods section. The session began with a novel “lid-opener” showing a real-life video of a child with developmental delay and the psychosocial impact of the disability on the child and family, followed by an active learning strategy; think pair and share (TPS). We explored the utility of “cognitive” orientations to learning by positioning learners to seek and understand the structure of knowledge for meaningful learning. TPS has been known to enhance the process of clinical learning by allowing students to experience different viewpoints on a particular problem and express as well as to listen to others as compared to a traditional classroom lecture (Ganatra et al., 2021; Linsenmeyer, 2021).
A significant proportion (91%) of students agreed that using the interactive module to explore milestones helped improve their learning on the topic which is also reflected in the qualitative feedback (Table 2). The interactive smart board allowed students to explore milestones in a self-directed activity and enabled higher-order cognition through active engagement with the course content. Technology in learning is stimulating for millennial learners and allows them to use online novel educational tools to maneuver their learning process (George & Dreibelbis, 2021). The wide availability of mobile devices, laptops, smart boards, etc. provides the teacher opportunities to use these new technologies effectively to transform learning into a more collaborative, personalised, and empowering experience that is rooted in connectivism- the learning theory of the digital era. We employed a multimodal approach integrating diverse activities such as videos, interactive smart boards, and gamification (via the BINGO game). Integrating many information sources nurtures the learner’s ability to reflect on connections between fields, ideas, and concepts, a core skill linked to the theory of connectivism. (Goldie, 2016).
Case-based learning (CBL) effectively links theory and practice and prepares students for actual clinical application of knowledge through inquiry (Thistlethwaite et al., 2012). The hypothetico-deductive reasoning inherent to a “constructivist” framework was applied while designing this approach (Kalinowski & Pelakh, 2024). It increases the learner’s engagement and motivation for learning through creativity, challenge, interest, and enjoyment afforded through the case-study method. An important part of CBL involves problem-solving through free discussions and with often no correct or incorrect answers, thus broadening the students’ reasoning process (Thistlethwaite et al., 2012). We used a CBL trigger in the form of a video demonstrating an assessment of a child’s development, allowed students analyse the video individually followed by buzz group discussions to share their understanding. All our students unanimously agreed that the case-based activity gave them ample opportunity to witness theory in practice. Buzz groups also provide an opportunity to apply contextual thinking to actual practice and develop collaborative skills. Studies have shown that buzz groups improve clinical reasoning and learning, promote teamwork, increase motivation to learn, improve academic performance through a conducive learning environment, and provide a chance for all members to participate and share their opinions within their sub-group (Abbasi et al., 2017; Balslev et al., 2015; Shrivastava, & Shrivastava, 2018). The elements of exploration and experimentation ensured that the theory of constructivism rooted in the connection of new knowledge to pre-existing knowledge was effectively utilised in the CBL process. Co-creation of this knowledge with peer interactions can be attributed to social learning theories of cognitivism and constructivism.
Selective and purposeful gamification has been known to increase learner motivation and engagement and, ultimately, learning (Rutledge et al., 2018). This was evident in our study where a vast majority (98%) of students agreed that the game-based activity helped them build an emotional connection with the process of learning and concepts being learned, which is also reflected in the qualitative feedback (Table 2). Game-based learning (GBL) builds emotional connections by immersing learners in engaging and interactive environments. These environments evoke emotions such as curiosity, excitement, and empathy, which enhance motivation and deepen the learning experience (Loderer et al., 2020). Based on constructivist theory, the game-based activity integrated their knowledge of age-appropriate milestones with a fun-based BINGO theme. The instant feedback that served as formative assessment in this segment had a behaviorist orientation that is specific and quantifiable.
B. Student Engagement using Multimodal Active Learning Strategies
Studies have noted a preference for multi-modal learning strategies by medical students which have been shown to improve academic performance, and promote deeper learning and enquiry (Alkhasawneh et al., 2008; James et al., 2011; Lujan & DiCarlo, 2006; Nicholson et al., 2016). Different learners have different learning styles and use of a variety of strategies can engage learners synergistically. We used various active learning strategies to facilitate student engagement as shown in Figure 3 which incorporated the ICAP framework of Interactive, Constructive, Active, and Passive activities. In addition, the use of learning theories to rationalise the framing of learning objectives, selection of specific teaching-learning methods/strategies, and design of appropriate evaluation strategies ensured student engagement and meaningful learning.
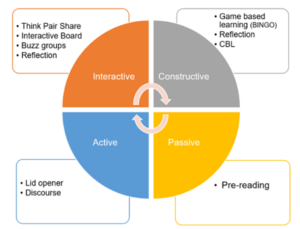
Figure 3. Summary of active learning strategies used in the module based on ICAP framework
The module had more activities involving interactive and constructive domains as compared to the active and passive modes. It is known that student learning and engagement improve as they move from passive to active to constructive to interactive modes (Chi & Wylie, 2014). Significant association between overall experience and interactive collaboration with peers (p=0.001) as well as constructive engagement (p=0.000) was observed. The feedback was also structured to measure student engagement in all four behaviors. We observed high mean scores in interactive and constructive domains. Learners agreed on enough opportunities for feedback, and practice and appreciated the engagement through case studies and discussions. Effective use of multiple active learning strategies thus enabled self-directed learning and students felt that they could accomplish the learning goals independently. The results underpin the utility of behaviorism and humanism as orientations for the learning process in such activities.
C. Individual and Collaborative Learning
The combination of active learning strategies facilitated engagement at both individual and collaborative levels. Students were involved in individual learning through pre-reading, lid-opener, discourse on development, case-based learning, and game (BINGO). These activities provided opportunities to self-regulate and moderate their learning. It also allowed them to organise their thoughts and reflect on their understanding. Active learning has a positive impact on memory and knowledge transfer and hence, individual self-studying before discussion improves the effectiveness of collaboration (Beggs et al., 2005). Activities initiated with an individual thinking process were balanced by subsequent group discussions. Collaborative activities in the form of Think pair share (TPS) after lid-opener, Buzz groups after CBL learning, and interactive table enabled constructive interaction among students and exchange of information and concepts. The collaborative activities helped students work together towards problem-solving, observe both their own and another’s learning process, discover different ways of approaching a situation, and find gaps in their reasoning. It also helped to build on their team skills, leadership, clinical competence, and interpersonal communication which are core attributes of professionalism in our curriculum (Branch, 2015).
D. Faculty Involvement
Though activities in the module were planned to encourage self-directedness, faculty role in the preparation and implementation of these strategies cannot be undermined. We adopted an amalgamation of humanistic and social cognitive orientation to strengthen the relationship between quality of instructional design and outcomes, thereby influencing learning directly. Perhaps for the same reasons we found a significant association between faculty facilitation with overall learning experience (p=.000). Students felt that the faculty supported them through the learning process throughout the session (100%) and regulated information besides allowing students to be responsible for their learning (98%). There was also a significant association between faculty involvement and the passive component (pre-reading material, discourse) (p=0.00); students agreed that pre-reading material was easily understandable (95%) and clear objectives and outcomes laid down before the session facilitated their understanding (100%). It must be noted that faculty can personalise the module based on the strengths, interests, cultural competencies, and time restraints of the student. Thus, rather than delivering a “one size fits all” module, the faculty can customise the content based on the student’s needs and limitations.
Involving various sensory processes enables better processing and retention of information; thus, enhancing the learning process (Friedlander et al., 2011). As more methods are employed, they are likely to engage more senses thus improving learning. Neuroscientific rationale for constructivist cognition may be seen as a possible explanation (Dennick, 2016).
While the use of active learning techniques in undergraduate medical education is not entirely novel, our approach is distinctive in that we’ve designed an entirely active learning module addressing various orientations to student learning, which ensures individual and collaborative student engagement. The study’s primary advantage is the creation and application of a targeted educational resource to teach developmental paediatrics to undergraduate students. This not only addresses the gap in effectively integrating developmental paediatrics into the core paediatrics curriculum but also demonstrates the feasibility of using a fully active learning approach in other clinical topics. Our detailed methodology aims to assist other educators in transforming their content into interactive teaching modules. The module not only meets the institutional requirement for increasing active learning sessions in the clinical years but also addresses a broader need by offering a framework and learning strategies that can be effectively applied to different topics and courses.
We could only assess student engagement based on their perception, i.e. level 1 of the New World Kirkpatrick Model (reaction), and have not quantified their ability to learn, understand, and apply their learning which constitutes higher levels of the model (Liao & Hsu, 2019). Additional limitations include the fact that this is a pilot study, tailored to a specific context and curriculum, which may restrict its generalisability. It also does not directly compare with other learning methods and lacks long-term tracking of students.
V. CONCLUSION
Paediatric topics such as developmental paediatrics are delivered mainly through didactic orientations and fail to capture student engagement leading to poor comprehension. Our study demonstrates that medical students enjoy sessions involving multimodal active learning strategies, particularly while discussing theoretical concepts that provide opportunities for practice and feedback. Heterogeneous learning strategies which underpin various learning theories and constructs have been shown to increase student motivation and engagement, thus contributing towards retention and deep learning. The faculty have an important role in planning such modules to customise the content and delivery for successful student engagement and effective learning thereafter. The framework and active learning strategies presented in the module can be applied more broadly to other subjects adapting to the needs of other undergraduate faculty in their teaching, thus making active teaching strategies easily transferable. We recommend future research be planned to include pre- and post-session assessments or a crossover study with a control group for comprehensive evaluation. Furthermore, the implementation of active learning strategies to create entirely active modules in other courses within the undergraduate medical program can be explored to assess its potential for broader applicability.
Notes on Contributors
Dr. Chhaya Divecha, Associate Professor of Paediatrics was involved in the conceptualisation and design of the study, literature search, data collection and drafting the manuscript.
Dr. Miriam Simon, Associate Professor of Behavioral Science was involved in the design of the study, analysis, interpretation of results and drafting the manuscript.
Dr. Ciraj Mohammed, Professor of Medical Education was involved in the design of the study and revised the manuscript for scientific content.
All authors have read and approved the final manuscript.
Ethical Approval
Approval to conduct this study was obtained from the institution’s Ethics and Biosafety Committee (NU/COMHS/EBC0036/2022).
Data Availability
Data will be made available by the authors on acceptance of the manuscript.
Acknowledgement
The authors wish to thank the participants for their cooperation in the study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interests.
References
Abbasi, F., Mofrad, M. N., Borhani, F., & Nasiri, M. (2017). Evaluation of the effect of training by buzz group method on nursing diagnostic skills of nursing students. Research Journal of Pharmacy and Technology, 10(1), 213-218. https://doi.org/10.5958/0974-360x.2017.00045.2
Alkhasawneh, I. M., Mrayyan, M. T., Docherty, C., Alashram, S., & Yousef, H. Y. (2008). Problem-based learning (PBL): Assessing students’ learning preferences using VARK. Nurse Education Today, 28(5), 572–579. https://doi.org/10.1016/j.nedt.2007.09.012
Balslev, T., Rasmussen, A. B., Skajaa, T., Nielsen, J. P., Muijtjens, A., De Grave, W., & Van Merriënboer, J. (2015). Combining bimodal presentation schemes and buzz groups improves clinical reasoning and learning at morning report. Medical Teacher, 37(8), 759–766. https://doi.org/10.3109/0142159X.2014.986445
Bauer, S. C., Smith, P. J., Chien, A. T., Berry, A. D., & Msall, M. (2009). Educating pediatric residents about developmental and social–emotional health. Infants & Young Children, 22(4), 309-320. https://doi.org/10.1097/IYC.0b013e3181bc4da0
Beggs, S., Sewell, J., Efron, D., & Orkin, C. (2005). Developmental assessment of children: A survey of Australian and New Zealand paediatricians. Journal of Paediatrics and Child Health, 41(8), 444–448. https://doi.org/10.1111/j.1440-1754.2005.00664.x
Branch, W. T. (2015). Teaching professional and humanistic values: Suggestion for a practical and theoretical model. Patient Education and Counseling, 98(2), 162–167. https://doi.org/10.1016/j.pec.2014.10.022
Bright, M. A., Zubler, J., Boothby, C., & Whitaker, T. M. (2019). Improving developmental screening, discussion, and referral in pediatric practice. Clinical Pediatrics, 58(9), 941–948. https://doi.org/10.1177/0009922819841017
Chi, M. T. H., & Wylie, R. (2014). The ICAP framework: Linking cognitive engagement to active learning outcomes. Educational Psychologist, 49(4), 219–243. https://doi.org/10.1080/00461520 .2014.965823
Chödrön, G., Barger, B., Pizur-Barnekow, K., Viehweg, S., & Puk-Ament, A. (2021). “Watch Me!” Training increases knowledge and impacts attitudes related to developmental monitoring and referral among childcare providers. Maternal and Child Health Journal, 25(6), 980–990. https://doi.org/10.1007/s10995-020-03097-w
Clark, B., Andrews, D., Taghaddos, S., & Dinu, I. (2012). Teaching child development to medical students. The Clinical Teacher, 9(6), 368–372. https://doi.org/10.1111/j.1743-498X.2012.00581.x
Comley, L., Janus, M., Marshall, D., & Niccols, A. (2008). The early years: Child development in undergraduate medical school training. Canadian Family Physician, 54(6), 876.e1-4.
Connolly, A. M., Cunningham, C., Sinclair, A. J., Rao, A., Lonergan, A., & Bye, A. M. (2014). ‘Beyond Milestones’: A randomised controlled trial evaluating an innovative digital resource teaching quality observation of normal child development. Journal of Paediatrics and Child Health, 50(5), 393–398. https://doi.org/10.1111/jpc.12485
Dennick, R. (2016). Constructivism: Reflections on twenty-five years teaching the constructivist approach in medical education. International Journal of Medical Education, 7, 200–205. https://doi.org/10.5116/ijme.5763.de11
Densen, P. (2011). Challenges and opportunities facing medical education. Transactions of the American Clinical and Climatological Association, 122, 48–58.
Fox, G., Katz, D. A., Eddins-Folensbee, F. F., & Folensbee, R. W. (2007). Teaching development in undergraduate and graduate medical education. Child and Adolescent Psychiatric Clinics of North America, 16(1), 67-94. https://doi.org/10.1016/j.chc.2006.07.006
Friedlander, M. J., Andrews, L., Armstrong, E. G., Aschenbrenner, C., Kass, J. S., Ogden, P., Schwartzstein, R., & Viggiano, T. R. (2011). What can medical education learn from the neurobiology of learning? Academic Medicine, 86(4), 415–420. https://doi.org/10.1097/ACM.0b013e31820dc197
Ganatra, S., Doblanko, T., Rasmussen, K., Green, J., Kebbe, M., Amin, M., & Perez, A. (2021). Perceived effectiveness and applicability of Think-Pair-Share including storytelling (TPS-S) to enhance clinical learning. Teaching and Learning in Medicine, 33(2), 184–195. https://doi.org/10.1080/10401334.2020.1811094
George, D. R., & Dreibelbis, T. D. (2021). Active learning in ‘The cloud’: Using “social” technologies to expand the medical classroom. In A. Fornari & A. Poznanski (Eds.), How-to guide for active learning (pp. 85-99). Springer.
Goldie, J. G. (2016). Connectivism: A knowledge learning theory for the digital age? Medical Teacher, 38(10), 1064–1069. https://doi.org/10.3109/0142159X.2016.1173661
Honigfeld, L., Chandhok, L., & Spiegelman, K. (2012). Engaging pediatricians in developmental screening: The effectiveness of academic detailing. Journal of Autism and Developmental Disorders, 42(6), 1175–1182. https://doi.org/10.1007/s10803-011-1344-4
Huggett, K. N., & Jeffries, W. B. (2021). Overview of active learning research and rationale for active learning. In A. Fornari & A. Poznanski (Eds.), How-to guide for active learning (pp. 1-7). Springer.
James, S., D’Amore, A., & Thomas, T. (2011). Learning preferences of first year nursing and midwifery students: Utilising VARK. Nurse Education Today, 31(4), 417–423. https://doi.org/10.1016/j.nedt.2010.08.008
Kalinowski, S. T., & Pelakh, A. (2024). A hypothetico-deductive theory of science and learning. Journal of Research in Science Teaching, 61(6), 1362–1388. https://doi.org/10.1002/tea.21892
Leiner, M., Krishnamurthy, G. P., Blanc, O., Castillo, B., & Medina, I. (2011). Comparison of methods for teaching developmental milestones to pediatric residents. World Journal of Paediatrics, 7(2), 161–166. https://doi.org/10.1007/s12519-011-0269-5
Liao, S. C., & Hsu, S. Y. (2019). Evaluating a continuing medical education program: New world Kirkpatrick model approach. International Journal of Management, Economics and Social Sciences, 8(4), 266-279.
Linsenmeyer, M. (2021). Brief activities: Questioning, brainstorming, think-pair-share, jigsaw, and clinical case discussions. In A. Fornari & A. Poznanski (Eds.), How-to guide for active learning (pp. 39-66). Springer.
Loderer, K., Pekrun, R., & Plass, J. L. (2020). Emotional foundations of game-based learning. In J. L. Plass, R. E. Mayer, & B. D. Homer (Eds.), Handbook of game-based learning (pp. 111–151). MIT Press.
Lujan, H. L., & DiCarlo, S. E. (2006). First-year medical students prefer multiple learning styles. Advances in Physiology Education, 30(1), 13–16. https://doi.org/10.1152/advan.00045.2005
McCoy, L., Pettit, R. K., Kellar, C., & Morgan, C. (2018). Tracking active learning in the medical school curriculum: A learning-centered approach. Journal of Medical Education and Curricular Development, 5, 2382120518765135. https://doi.org/10.1177/2382120518765135
Nicholson, L. L., Reed, D., & Chan, C. (2016). An interactive, multi-modal anatomy workshop improves academic performance in the health sciences: A cohort study. BMC Medical Education, 16, Article 7. https://doi.org/10.1186/s12909-016-0541-4
O’Sullivan, S., Campos, L. A., & Baltatu, O. C. (2022). “Involve Me and I Learn”: Active learning in a hybrid medical biochemistry first year course on an American-style MD program in the UAE. Medical Science Educator, 32(3), 703–709. https://doi.org/10.1007/s40670-022-01545-6
Rolfe, G. (2014). Reach touch and teach: Terry Borton. Nurse Education Today, 34(4), 488–489. https://doi.org/10.1016/j.nedt.2013.11.003
Rutledge, C., Walsh, C. M., Swinger, N., Auerbach, M., Castro, D., Dewan, M., Khattab, M., Rake, A., Harwayne-Gidansky, I., Raymond, T. T., Maa, T., & Chang, T. P. (2018). Gamification in action: Theoretical and practical considerations for medical educators. Academic Medicine, 93(7), 1014–1020. https://doi.org/10.1097/ACM.0000000000002183
Shrivastava, S. R., & Shrivastava, P. S. (2018). Exploring the scope of introducing buzz group in teaching community medicine to undergraduate medical students. MAMC Journal of Medical Sciences, 4(2), 109.
Thistlethwaite, J. E., Davies, D., Ekeocha, S., Kidd, J. M., MacDougall, C., Matthews, P., Purkis, J., & Clay, D. (2012). The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Medical Teacher, 34(6), e421–e444. https://doi.org/10.3109/0142159X.2012.680939
Woolfson, L. (2004). Family well-being and disabled children: A psychosocial model of disability-related child behaviour problems. British Journal of Health Psychology, 9(1), 1–13. https://doi.org/10.1348/135910704322778687
*Dr. Miriam Simon
Department of Psychiatry and Behavioral Science
College of Medicine and Health Sciences
National University of Science and Technology
PO Box 391; PC 321
Sohar, Sultanate of Oman
+96826852039
Email: miriamsimon@nu.edu.om
Published online: 7 January, TAPS 2025, 10(1), 1-3
https://doi.org/10.29060/TAPS.2025-10-1/EV10N1
The present healthcare environment requires practitioners who are not only technically proficient but also compassionate, empathetic, and fully committed to a patient-centred approach. These professionals can be best described as “holistic practitioners,” given their emphasis on supporting the complete well-being of patients, as well as addressing patients’ physical, emotional, social, and spiritual needs. Our editorial explores strategies for nurturing such practitioners who focus on the person as a whole, rather than merely treating individual diseases.
Building Competence Through Integrated Knowledge and Skills
Competence in healthcare now requires more than a strong grounding in biomedical and clinical sciences. It requires blending knowledge and skills across various disciplines with a focus on a patient-centred approach. This holistic approach involves embracing interprofessional education, which allows students to learn alongside other healthcare roles, while fostering the teamwork essential for comprehensive care (Samarasekera et al., 2024).
Cultivating Empathy and Compassion
Empathy and compassion are key qualities that distinguish a healthcare provider as a genuine healer. Developing empathy involves understanding the patient’s perspective and their unique experiences. Techniques like role-playing, patient storytelling, and reflective exercises can help practitioners view health issues from the patient’s viewpoint. This approach nurtures true empathy that goes beyond simply recognising a patient’s emotions to fostering authentic concern. A medical education culture that values compassion as much as the technical skill underlying clinical practice creates and cultivates practitioners who truly care about the person behind the diagnosis (Samarasekera et al., 2022).
Promoting Efficient, Patient-Centred Care
While efficiency in healthcare is crucial, it must not overshadow patient attentiveness. Holistic practice prioritises streamlining processes to enhance outcomes without compromising empathy or care quality. Training in time management, communication, and systems-based approaches can help practitioners balance effectiveness with patient-centredness. This approach is aptly described by Groopman (2007), who highlights the need for practitioners to deeply listen to the patient narrative. The requirement for attentive listening can be augmented using digital tools, such as electronic health records and telemedicine, which can improve efficiency while supporting personalised care. Furthermore, emerging technologies like AI and wearable health devices offer proactive insights for practitioners, enhancing preventive care and lightening practitioner workload. In telemedicine, training in empathetic communication ensures patients feel genuinely heard, even during virtual appointments.
Recognising cultural diversity is essential in delivering patient-centred care. Cultural competency training helps practitioners respect and understand diverse healthcare beliefs and practices (Vella et al., 2022). Providing the groundwork for holistic patient interaction will likely require medical education to embrace role-play and simulations with diverse patient scenarios, which leads to preparing practitioners to meet the unique needs of various communities and facilitate more inclusive care.
The Role of Self-Care and Well-being in Clinical Practice
The phrase “Physician, heal thyself” highlights the importance of self-care for healthcare practitioners, emphasising the importance of professionals themselves initiating, promoting and cultivating personal health and wellbeing (Mills et al., 2018). Maintaining strong physical, mental, and emotional health enables practitioners to provide the highest quality of care. Self-care directly impacts patient care by building resilience, empathy, and sound decision-making, especially under pressure. Accentuating self-care among clinicians fosters a sustainable healthcare environment, preparing practitioners to meet the challenges of their roles more effectively and to minimise the occurrence of burnout, moral distress, and compassion fatigue (Sanchez-Reilly et al., 2013).
Resilience, often described as “grit”, is vital in healthcare, where professionals face high-stakes and emotionally taxing situations (Samarasekera & Gwee, 2020). This trait supports practitioners in maintaining focus and motivation, even under prolonged stress. When practitioners engage in holistic practices, such as prioritising their own well-being through regular exercise, mindfulness, and ensuring quality sleep, they can bolster resilience and adapt better to challenges, avoiding burnout (Rich et al., 2020). Practitioners with strong self-care habits not only enhance their own lives but also improve their ability to connect with patients meaningfully.
It is likely that holistic practitioners are better able to communicate, display empathy, and build trust with patients (Mills et al., 2018). They also maintain better focus and emotional balance, which are critical for accurate diagnoses and effective clinical decisions. Practitioners experiencing stress or burnout risk adversely impacting care quality, potentially leading to increased errors and reduced patient satisfaction (Sanchez-Reilly et al., 2013).
By modelling healthy behaviours, clinicians set an example for patients, subtly encouraging positive lifestyle choices. When practitioners view their own wellness as integral to patient care, they embody a holistic approach that values both practitioner and patient well-being. Promoting self-care within the curriculum is also essential. Institutions can support this by embedding wellness programmes, resilience training, and mindfulness practices, helping students value their own well-being. Mentorship programmes with experienced clinicians provide support, fostering a model of work-life balance, resilience, and self-care.
Addressing Holistic Skills Gaps
One major challenge in holistic training is the intensive academic and clinical workload, which often overshadows the human aspects of care (Mills et al., 2018). Medical education tends to focus heavily on medical knowledge, diagnostic and procedural skills, at times de-emphasising empathy, communication, and emotional intelligence. This can inadvertently lead practitioners to prioritise efficiency over patient connection. Furthermore, the rigorous demands of medical training may lead to a culture where self-care is undervalued, affecting practitioners’ overall well-being.
Another obstacle is the limited opportunity for interprofessional learning. Holistic care relies on collaboration across healthcare roles, yet many training programmes work in isolation, reducing exposure to real-world teamwork. This will likely limit understanding the interconnected nature of healthcare roles, making it difficult to deliver fully integrated care.
Healthcare practitioners practising holistic care may face ethical challenges, such as maintaining boundaries while showing empathy. Dedicated ethics training, with case studies on boundary management and unbiased care, can prepare practitioners to meet these challenges. Ethical frameworks, like the “Four Principles” of medical ethics namely autonomy, beneficence, non-maleficence, and justice—serve as valuable guidelines for balanced, patient-centred decision-making. Interprofessional education should be prioritised, allowing students to work alongside those from other healthcare disciplines and develop respect for each role’s contributions. Such collaboration enhances communication skills and prepares practitioners to deliver comprehensive, patient-centred care.
Conclusion
Creating a healthcare workforce that is competent, compassionate, and efficient begins with focusing on the practitioners themselves. By embracing self-care, healthcare providers build the resilience and empathy needed to face the demands of clinical practice while improving patient outcomes. Holistic practitioners not only treat patients but embody wellness, showing compassion, commitment, and integrity. Emphasising practitioner well-being as essential to holistic care strengthens the healthcare system, fostering a culture of respect, trust, and shared commitment to patient-centred health.
Dujeepa D. Samarasekera
Centre for Medical Education (CenMED), NUS Yong Loo Lin School of Medicine,
National University Health System, Singapore
Marcus A. Henning
Centre for Medical and Health Sciences Education, Faculty of Medical and Health Sciences,
University of Auckland, New Zealand
Shuh Shing Lee & Han Ting Jillian Yeo
Centre for Medical Education (CenMED), NUS Yong Loo Lin School of Medicine,
National University Health System, Singapore
Groopman, J. (2007). How doctors think. Houghton Mifflin. https://doi.org/10.1172/jci33149
Mills, J., Wand, T., & Fraser, J. A. (2018). Exploring the meaning and practice of self-care among palliative care nurses and doctors: A qualitative study. BMC Palliative Care, 17, Article 63. https://doi.org/10.1186/s12904-018-0318-0
Rich, A., Aly, A., Cecchinato, M. E., Lascau, L., Baker, M., Viney, R., & Cox, A. L. (2020). Evaluation of a novel intervention to reduce burnout in doctors-in-training using self-care and digital wellbeing strategies: A mixed-methods pilot. BMC Medical Education, 20, Article 294. https://doi.org/10.1186/s12909-020-02160-y
Samarasekera, D. D., Chong, Y. S., Ban, K., Lau, L. S. T., Gallagher, P. J., Chen, Z. X., Müller, A. M., Ngiam, N. S., Wong, M. L., Lau, T. C., Dunn, M. C., & Lee, S. S. (2024). Transforming healthcare with integrated inter-professional education in a research-driven medical school. Medical Teacher, 1-8. https://doi.org/10.1080/0142159x.2024.2409293
Samarasekera, D. D., & Gwee, M. C. (2020). Grit in healthcare education and practice. The Asia Pacific Scholar, 5(1), 1. https://doi.org/10.29060/TAPS.2020-5-1/EV5N1
Samarasekera, D. D., Lee, S. S., Yeo, J. H. T., Yeo, S. P., & Ponnamperuma, G. (2022). Empathy in health professions education: What works, gaps and areas for improvement. Medical Education, 57(1), 86-101. https://doi.org/10.1111/medu.14865
Sanchez-Reilly, S., Morrison, L., Carey, E., Bernacki, R., O’Neill, L., Kapo, J., Periyakoil, V., & Thomas, J. (2013). Caring for oneself to care for others: Physicians and their self-care. The Journal of Supportive Oncology, 11(2), 75-81. https://doi.org/10.12788/j.suponc.0003
Vella, E., White, V. M., & Livingston, P. (2022). Does cultural competence training for health professionals impact culturally and linguistically diverse patient outcomes? A systematic review of the literature. Nurse Education Today, 118, Article 105500. https://doi.org/10.1016/j.nedt.2022.105500
Submitted: 6 June 2024
Accepted: 3 September 2024
Published online: 7 January, TAPS 2025, 10(1), 10-16
https://doi.org/10.29060/TAPS.2025-10-1/RA3430
Han Ting Jillian Yeo, Dujeepa D. Samarasekera & Shuh Shing Lee
Centre for Medical Education (CenMED), Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Despite significant efforts to address gender equality in medical education, the issue persists. The narrative review aimed to address the research question: What are the strategies implemented to address issues of gender inequality in medical education and what were their outcomes?
Methods: Seven major electronic databases of CINAHL, Embase, ERIC, PsyInfo, PubMed, SCOPUS and Web of Science were reviewed. Search phrases used were (Medical education) AND (Gender equality) OR (Gender bias) OR (Gender diversity) OR (Gender discrimination). Original research articles were included, together with systematic reviews with outcomes reporting on strategies to address gender equality.
Results: Articles unrelated to medical education (e.g. allied health and nursing education) and non-English articles were excluded from the study. A total of 1248 articles were identified, and 23 articles met the inclusion criteria. Training programs (n=14; 60.8%) for medical students and faculty have successfully increased awareness on the issues of gender equality and boost confidence in handling cases on gender inequality, yet implicit bias remains with leadership continuing to be associated more strongly with males.
Conclusion: Leadership bodies in Institutions of Higher Education and policymakers would be in an ideal position to address these issues through shaping policies and provision of training for hiring bodies and faculty.
Keywords: Medical Education, Gender Equality, Strategies
Practice Highlights
- Training programs for medical students and faculty can increase awareness of gender equality.
- Structural and cultural barriers preventing women from attaining leadership roles remain entrenched.
- Targeted training for hiring committees and faculty can help mitigate implicit biases.
I. INTRODUCTION
There has been significant progress in the landscape of medical education since 2000 as women’s representation in health professions has increased steadily across the globe. In 2019, nearly half of all doctors in countries in the Organisation for Economic Co-operation and Development were women (Organisation for Economic Co-operation and Development, 2022). However, beneath the surface of this endeavor lies a persistent and pervasive issue concerning gender equality. The World Health Organisation (WHO) (2007) defines gender equality as the absence of discrimination in the allocation of benefits or resources, access to services, or the provision of opportunities based on a person’s sex, thereby enabling individuals to achieve their full potential. Efforts have been made towards achieving gender equality and inclusivity. Changes in the recruitment processes of residency programs in the United States and Canada have shown an increasing ratio of females among residents and faculty (Jain et al., 2022; Ying et al., 2023). Studies evaluating the assessments of medical students and residents have suggested reduced biases in scorings of examinees based on gender (Hannon et al., 2021; Jacques et al., 2016).
Yet, gender inequality remains prevalent in other aspects of medical education. Sexual harassment in the form of sexist behavior or comments were commonly reported among females in the workplace during residency trainings (DeWane et al., 2020; Ellis et al., 2019; Jackson & Drolet, 2021). Learning opportunities were unequal as female residents performed disproportionately lesser number of procedures (Olson et al., 2023; Sobel et al., 2023) and were given less operative autonomy as compared to their male counterparts hence affecting their preparedness for practice (Joh et al., 2020; Meyerson et al., 2019). The impact of gender inequality is far-reaching. Negative emotions, such as helplessness, and lowered self-esteem, were often described by students or residents who had experienced or observed gender inequality (Kristoffersson et al., 2016; Madeeh Hashmi et al., 2013). Additionally, lowered job satisfaction, feelings of burnout and an increased risk of attrition were reported among those who have experienced or observed gender inequality (Bruce et al., 2015; Ellis et al., 2019; Jackson & Drolet, 2021).
Achieving gender equality in medical education is critical, however, literature highlighted that it continues to persist despite various interventions. Numerous studies have documented progress in gender equality following the implementation of specific interventions, but there is a scarcity of comprehensive reviews consolidating these efforts. Hence, this narrative review aimed to address the research question: What are the strategies implemented to address issues of gender inequality in medical education and what were their outcomes?
II. METHODS
A narrative review was conducted based on the framework proposed by Ferrari (2015). Two researchers (SSL and JYHT) searched seven major electronic databases of CINAHL, Embase, ERIC, PsyInfo, PubMed, SCOPUS and Web of Science for the English-language articles or articles which were translated to English and published between 2013 to 2023. The search terms were broadened using the Boolean operator (“OR/AND”) to search the ‘medical’ subject heading (MeSH) to recognise the significance of the study. As a result, the search phrases were (Medical education) AND (Gender equality) OR (Gender bias) OR (Gender diversity) OR (Gender discrimination).
Original research articles were included into the study, together with systematic reviews with outcomes reporting on strategies to address gender equality. Articles unrelated to medical education (e.g. allied health and nursing education) and non-English articles were excluded from the study. Figure 1 showed a flow chart of the process of literature selection for the narrative review.
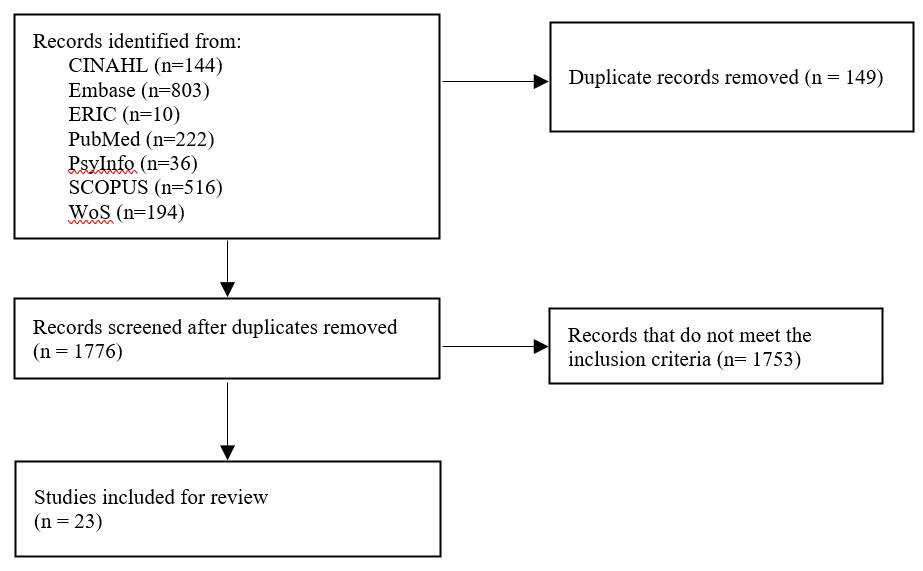
Figure 1. Flow diagram showing the selection of articles
Based on the inclusion and exclusion criteria outlined, both researchers (SSL and JYHT) independently reviewed the title and abstracts of all articles and reviewed the full article when necessary. Articles were categorised based on the types of strategies that were implemented, target audient, method of evaluation and evaluation findings.
III. RESULTS
After removing duplicate articles, a total of 1248 articles were identified through the literature search strategy. Following a thorough examination of the titles and abstracts as well as a review of the articles’ references lists, 23 articles met the review criteria (Table 1). Articles were published between 2015 to 2022. Majority of studies were conducted in the United States (n=16), Canada (n=1), United States and Canada (n=1), Germany (n=1), Sweden (n=1), Switzerland (n=1), Taiwan (n=1), and United Kingdom (n=1).
The findings from this narrative review were divided into two sections: (1) an overview of the interventions implemented to address gender equality and (2) an evaluation of the interventions implemented.
A. Interventions Implemented to Address Gender Equality
Interventions implemented could be divided into micro, meso and macro levels interventions to address gender equality. Micro levels interventions focused on supporting individuals in understanding concepts on gender bias and diversity, its impact on the workplace and strategies to overcome gender bias. These aims could be achieved through training programs for faculty and medical students (n=14; 60.8%). Other micro level interventions described in the articles included giving doctors labelled badges and empowering residents to nominate their chief resident (Olson et al., 2022).
Meso level interventions focused on improving the institutions’ systems, structures, and procedures. Two articles described the formation of task forces in medical societies and higher education institutions (HEIs) to monitor trends and address gender issues (Kandi et al., 2022; Lieberman et al., 2018). Holding a public symposium as a platform to discuss issues on gender equality and enforcing guidelines on writing letter recommendations for medical residency applications were other meso level interventions (Sakowski et al., 2020; Zhang et al., 2021).
Macro level interventions involved shaping policies on a broader, national, or international scale. One study by Chang et al. (2020) shared on three national career developments program aimed at increasing women faculty professional effectiveness. Another macro level intervention involved awarding institutions with Bronze, Silver, and Gold for efforts in addressing gender equity (Caffrey et al., 2016).
The target audience for most interventions were medical students (n=7), these included interventions tailored for women medical students. Other main target audiences included faculty (n=4), residents (n=3) and HEIs (n=2).
B. Addressing Gender Inequality through Training Programs
The duration of the 15 training programmes specified spanned from 15 minutes to 15 weeks long. Seven training programs targeted medical students, 4 training programs targeted faculty, 2 training programs targeted internal medical residents.
Training programs primarily focused on creating an awareness of gender inequality in the workplace through defining terminologies surrounding gender inequality, showing data on gender inequality and its impact on the workplace (Carnes et al., 2015; Driscoll et al., 2019; Farkas et al., 2022; Girod et al., 2016; Jacobs et al., 2022; Kisiel et al., 2020; Lattanza et al., 2016; Sabin et al., 2022). Five programs shared strategies and frameworks to handle situations insinuating gender inequality in the workplace and provided opportunities for practice (Bromberg et al., 2022; Carnes et al., 2015; Farkas et al., 2022; Jacobs et al., 2022; Sabin et al., 2022). Five training programs incorporated elements to guide participants on their career progression through networking opportunities, mentorship programs and leadership training (Chang et al., 2020; Deng et al., 2021; Gaida et al., 2020; Harbold et al., 2021; Lattanza et al., 2016). Training programs developed as part of the Perry’s Initiative for women medical students provided hands-on opportunities to engage in operative procedures to encourage more females to enter the field of orthopaedic surgery (Harbold et al., 2021; Lattanza et al., 2016). Two training programs adopted the approach of engaging in reflexivity with a gendered perspective into one’s own practice and literature materials (Geiser et al., 2022; Liao & Wang, 2020).
C. Evaluation and Findings on the Strategies Implemented
The Kirkpatrick model was adopted to categorise how evaluation of interventions was conducted and the findings.
1) Kirkpatrick Level 1 – Reaction: Participants’ reactions were evaluated for the following strategies: workshops, public symposium, recognition of efforts and empowerment to nominate chief residents (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). Participant satisfaction surveys were the main tool adopted to determine if participants found the strategies useful and identify areas for improvement (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). One qualitative study by Caffrey et al. (2016) used semi-structured interviews. In general, the interventions were perceived positively in all articles (Bromberg et al., 2022; Jacobs et al., 2022; Klein et al., 2020; Sakowski et al., 2020). However, one study by Caffrey et al. (2016) focusing on recognising institutions which promote gender equity had reported a higher and disproportionate workload on women who were involved in the application process.
2) Kirkpatrick Level 2 – Learning: Participants in 6 studies reported an increased awareness of gender bias after workshops were conducted (Caffrey et al., 2016; Carnes et al., 2015; Deng et al., 2021; Girod et al., 2016; Liao & Wang, 2020; Sabin et al., 2022). Awareness of gender bias can be described in different facets: (1) having an understanding that society has yet to provide equal opportunities for all regardless of their backgrounds; and (2) gaining awareness on the presence of socially constructed gender norms. Two workshops had reported an increase in internal medicine residents’ confidence in responding to incidences related to gender inequality (Bromberg et al., 2022; Farkas et al., 2022).
While strategies had largely positive outcomes with regards to learning, Carnes et al. (2015) and Girod et al. (2016) revealed that workshops on gender bias led to no significant differences in gender/ leadership Implicit Association Test scores suggesting that there remains a persistent association of leadership with males more than females. Gaida, Kujumdshiev and Stengler (2020) shared that low numbers of medical students were able to identify gender sensitive topics despite a week-long elective course on issues of gender equality supported by a mentorship program.
3) Kirkpatrick Level 3 – Behaviour: Reviewed literature revealed conflicting findings on the impact of the interventions on participants’ behaviour. Interventions made to medical assessments (unconscious bias training of examiners, structured interview formats for interviewers and guidelines for writing letter of recommendations) observed no changes in scores and biased language used (Driscoll et al., 2019; Langhan et al., 2022; Zhang et al., 2021).While Olson et al. (2022) had shown a reduction in reported events on gender bias, Kisiel et al. (2020) reported an increase in sexual harassment and gender discrimination events attributing it to an increased awareness in such behaviours.
4) Kirkpatrick Level 4 – Results: Studies which evaluated the overall impact of the interventions on organizational structure showed optimistic results. Articles introducing the Perry’s Initiative to increase women medical students’ exposure to orthopaedic surgery and engineering reported an increased match rates of alumni students to orthopaedics (Harbold et al., 2021; Lattanza et al., 2016). Training of faculty search committee member yielded an increase in number of female candidates throughout the entire hiring process and eventually positions offered to them (Jacobs et al., 2022). Chang et al. (2020) also reported higher rates of promotion for women faculty who had participated in national career development programs.
IV. DISCUSSION
The review highlighted that training programs for students and faculty were not only positively received by students and faculty but were able to create awareness on gender inequality and boost confidence in handling cases on gender inequality. Yet faculty training programs failed to address the implicit bias among faculty who tend to associate leadership with male more than female. This was concurred by more recently published literature reporting that females hold fewer leadership positions in academia or residency programs and hence having potential implications on their career advancement opportunities (Dhingra et al., 2021; Sethi et al., 2022). Achieving gender equality in leadership body is important. The presence of female in any leadership position was correlated with an increase in the number of female faculty or female fellows (Sethi et al., 2022; Sulibhavi et al., 2021). One study also suggested that an increase in the number of female surgical faculty was correlated a decrease in attrition among residents (Saberi et al., 2021).
Macro and meso level interventions via implementation of career development programs and training of recruitment committee showed far reaching impacts on increasing diversity of hires and promotional rates of female faculty. This could serve as a guidance to the leadership bodies in HEIs that the engagement of targeted interventions on training hiring bodies and the provision of faculty development to women faculty can they level the playing field for both genders. Till date few studies reviewed the impact of macro level intervention, and perhaps by sharing the policies in place for training faculty and hiring bodies can the society see an exponential impact on addressing the issues of gender equality.
Lastly, it was evident from the review of selected literature that most research in the areas of gender quality was conducted in the Global North. Given that issues on gender equality tend to be contextual and cultural in nature, there would be a need for medical educators in the Global South to engage in scholarly work in this domain to identify the issues on the ground and identify targeted ways to address the issues on hand.
V. CONCLUSION
While training programs for medical students and faculty have successfully increased awareness of gender equality issues, implicit bias persists, particularly concerning female representation in leadership positions. Despite heightened awareness, the structural and cultural barriers preventing women from attaining leadership roles remain firmly entrenched. Leadership bodies within HEIs and policymakers are uniquely positioned to address these persistent issues. By shaping and implementing equitable policies, they can foster an environment that actively promotes gender diversity. Additionally, targeted training for hiring committees and faculty can help mitigate implicit biases, ensuring a more inclusive and representative leadership. Addressing these challenges requires a multifaceted approach, combining policy reform, education, and continuous evaluation to create lasting change in gender equality within medical education.
Notes on Contributors
Ms. Jillian Yeo was involved in writing the manuscript, conducting the literature search, reviewing the literature retrieved and synthesising the data. Dr Lee Shuh Shing was involved in conducting the literature search, reviewing the literature retrieved and synthesising the data. Dr Dujeepa was involved in the conceptual development of the study and reviewing the manuscript.
Ethical Approval
As this study was a narrative review, ethical approval and IRB application was not required.
Data Availability
The list of articles included in the narrative review can be accessed here:
https://doi.org/10.6084/m9.figshare.25980352.v1 (Yeo, 2024)
Funding
No funding sources are associated with this paper.
Declaration of Interest
There are no conflicts of interests related to the content presented in the paper.
References
Bromberg, G. K., Gay, E. A., Hills-Dunlap, K., & Burnett-Bowie, S. M. (2022). Using a virtual platform to teach residents how to respond to bias. Journal of General Intern Medicine, 37(11), 2871-2872. https://doi.org/10.1007/s11606-021-07156-y
Bruce, A. N., Battista, A., Plankey, M. W., Johnson, L. B., & Marshall, M. B. (2015). Perceptions of gender-based discrimination during surgical training and practice. Med Education Online, 20, 25923. https://doi.org/10.3402/meo.v20.259 23
Caffrey, L., Wyatt, D., Fudge, N., Mattingley, H., Williamson, C., & McKevitt, C. (2016). Gender equity programmes in academic medicine: A realist evaluation approach to Athena SWAN processes. BMJ Open, 6(9), e012090. https://doi.org/10.1136/bmjopen-2016-012090
Carnes, M., Devine, P. G., Baier Manwell, L., Byars-Winston, A., Fine, E., Ford, C. E., Forscher, P., Isaac, C., Kaatz, A., Magua, W., Palta, M., & Sheridan, J. (2015). The effect of an intervention to break the gender bias habit for faculty at one institution: A cluster randomised, controlled trial. Academic Medicine, 90(2), 221-230. https://doi.org/10.1097/acm.0000000000000552
Chang, S., Guindani, M., Morahan, P., Magrane, D., Newbill, S., & Helitzer, D. (2020). Increasing promotion of women faculty in academic medicine: Impact of National Career Development Programs. Journal of Women’s Health (Larchmt), 29(6), 837-846. https://doi.org/10.1089/jwh.2019.8044
Deng, M., Nham, E., Malvea, A., Ramsay, T., Seabrook, C., & Watterson, J. (2021). Exploring the impact of the surgical exploration and discovery (SEAD) program on medical students’ perceptions of gender biases in surgery: A mixed-method evaluation. Journal of Surgical Education, 78(4), 1236-1249. https://doi.org/10.1016/j.jsurg.2020.11.016
DeWane, M. E., Mattessich, S., Wu, R., & Whitaker-Worth, D. (2020). A survey study of resident experiences of sexual harassment during dermatology training. Journal of the American Academy of Dermatology, 83(2), 594-596. https://doi.org/10.1016/j.jaad.2019.07.023
Dhingra, S., Killaspy, H., & Dowling, S. (2021). Gender equality in academic psychiatry in the UK in 2019. BJPsych Bulletin, 45(3), 153-158. https://doi.org/10.1192/bjb.2020.116
Driscoll, S. W., Robinson, L. R., Raddatz, M. M., & Kinney, C. L. (2019). Is there evidence of gender bias in the oral examination for initial certification by the American Board of Physical Medicine & Rehabilitation? American Journal of Physical Medicine & Rehabilitation, 98(6), 512-515. https://doi.org/10.1097/phm.0000000000001126
Ellis, R. J., Hewitt, D. B., Hu, Y. Y., Johnson, J. K., Merkow, R. P., Yang, A. D., Potts, J. R., 3rd, Hoyt, D. B., Buyske, J., & Bilimoria, K. Y. (2019). An empirical national assessment of the learning environment and factors associated with program culture. Annals of Surgery, 270(4), 585-592. https://doi.org/10.1097/sla.0000000000003545
Farkas, A. H., Scholcoff, C., Lamberg, M., Shah, H., Fletcher, K., & Yecies, E. (2022). Preparing residents to respond to incidences of gender discrimination and sexual harassment: An interactive workshop. Southern Medical Journal, 115(10), 740-744. https://doi.org/10.14423/smj.0000000000001459
Ferrari, R. (2015). Writing narrative style literature reviews. Medical Writing, 24(4), 230-235. https://doi.org/10.1179/20474 80615Z.000000000329
Gaida, P., Kujumdshiev, S., & Stengler, K. (2020). Gender sensitivity in career mentoring – A project report from the medical faculty of Leipzig University. GMS Journal for Medical Education, 37(2), Doc24. https://doi.org/10.3205/zma001317
Geiser, E., Schilter, L. V., Carrier, J.-M., Clair, C., & Schwarz, J. (2022). Reflexivity as a tool for medical students to identify and address gender bias in clinical practice: A qualitative study. Patient Education Counselling, 105(12), 3521-3528. https://doi.org/10.10 16/j.pec.2022.08.017
Girod, S., Fassiotto, M., Grewal, D., Ku, M. C., Sriram, N., Nosek, B. A., & Valantine, H. (2016). Reducing implicit gender leadership bias in academic medicine with an educational intervention. Academic Medicine, 91(8), 1143-1150. https://doi.org/10.1097/acm.0000000000001099
Hannon, M., Duffey, K., Bharel, S., Redfield, R., Greidinger, A., Stewart, E., & Diemer, G. (2021). Investigating gender disparities in internal medicine residency awards. The American Journal of Medicine, 134(3), 405-409. https://doi.org/10.1016/j.amjmed.2020.11.003
Harbold, D., Dearolf, L., Buckley, J., & Lattanza, L. (2021). The Perry Initiative’s impact on gender diversity within orthopedic education. Current Reviews in Musculoskeletal Medicine, 14(6), 429-433. https://doi.org/10.1007/s12178-021-09717-4
Jackson, K. R., & Drolet, B. C. (2021). #MedicineToo – Gender bias in medical training: A national survey of residents. Journal of General Internal Medicine, 36(12), 3894-3896. https://doi.org/10.1007/s11606-021-06613-y
Jacobs, N. N., Esquierdo-Leal, J., Smith, G. S., Piasecki, M., & Houmanfar, R. A. (2022). Diversifying academic medicine: One search committee at a time. Front Public Health, 10, 854450. https://doi.org/10.3389/fpubh.2022.854450
Jacques, L., Kaljo, K., Treat, R., Davis, J., Farez, R., & Lund, M. (2016). Intersecting gender, evaluations, and examinations: Averting gender bias in an obstetrics and gynecology clerkship in the United States. Education for Health (Abingdon, England), 29(1), 25-29. https://doi.org/10.4103/1357-6283.178926
Jain, A., Nichols, G., Tarabishy, S., Scomacao, I., & Herrera, F. A. (2022). A comparison of applicant and resident physician demographics among surgical subspecialties from 2009 to 2019: Trends in gender and underrepresented minorities in medicine. Annals of Plastic Surgery, 88(4), 451-459. https://doi.org/10.1097/sap.0000000000003041
Joh, D. B., van der Werf, B., Watson, B. J., French, R., Bann, S., Dennet, E., & Loveday, B. P. T. (2020). Assessment of autonomy in operative procedures among female and male New Zealand general surgery trainees. Journal of the American Medical Association Surgery, 155(11), 1019-1026. https://doi.org/10.1001/jamasurg.2020.3021
Kandi, L. A., Jarvis, T. L., Movtchan, N. V., Hammond, J. B., Teven, C. M., & Rebecca, A. M. (2022). Characterization of national medical societies’ accessible resources to support underrepresented minority and female trainees. Journal of the American Medical Association Network Open, 5(9), Article e2230243. https://doi.org/10.1001/jamanetworkopen.2022.30243
Kisiel, M. A., Kühner, S., Stolare, K., Lampa, E., Wohlin, M., Johnston, N., & Rask-Andersen, A. (2020). Medical students’ self-reported gender discrimination and sexual harassment over time. BioMed Central Medical Education, 20(1), Article 503. https://doi.org/10.1186/s12909-020-02422-9
Klein, R., Law, K., & Koch, J. (2020). Gender representation matters: Intervention to solicit medical resident input to enable equity in leadership in graduate medical education. Academic Medicine, 95(12S), S93-S97. https://doi.org/10.1097/acm.0000000000003698
Kristoffersson, E., Andersson, J., Bengs, C., & Hamberg, K. (2016). Experiences of the gender climate in clinical training – a focus group study among Swedish medical students. BioMed Central Medical Education, 16(1), Article 283. https://doi.org/10.1186/s12909-016-0803-1
Langhan, M. L., Goldman, M. P., & Tiyyagura, G. (2022). Can behavior-based interviews reduce bias in fellowship applicant assessment? Academic Pediatrics, 22(3), 478-485. https://doi.org/10.1016/j.acap.2021.12.017
Lattanza, L. L., Meszaros-Dearolf, L., O’Connor, M. I., Ladd, A., Bucha, A., Trauth-Nare, A., & Buckley, J. M. (2016). The Perry Initiative’s medical student outreach program recruits women into orthopaedic residency. Clinical Orthopaedics and Related Research, 474(9), 1962-1966. https://doi.org/10.1007/s11999-016-4908-y
Liao, H. C., & Wang, Y. H. (2020). Integrating the gender perspective into literature studies to enhance medical university students’ gender awareness and critical thinking. International Journal of Environmental Research and Public Health, 17(24). https://doi.org/10.3390/ijerph17249245
Lieberman, J. A., Ehrhardt, A. A., Simpson, H. B., Arbuckle, M. R., Fyer, A. J., & Essock, S. M. (2018). Eliminating the glass ceiling in academic psychiatry. Academic Psychiatry, 42(4), 523-528. https://doi.org/10.1007/s40596-017-0810-5
Madeeh Hashmi, A., Rehman, A., Butt, Z., Awais Aftab, M., Shahid, A., & Abbas Khan, S. (2013). Gender discrimination among medical students in Pakistan: A cross sectional survey. Pakistan Journal of Medical Sciences, 29(2), 449-453. https://doi.org/10.12669/pjms.292.3256
Meyerson, S. L., Odell, D. D., Zwischenberger, J. B., Schuller, M., Williams, R. G., Bohnen, J. D., Dunnington, G. L., Torbeck, L., Mullen, J. T., Mandell, S. P., Choti, M. A., Foley, E., Are, C., Auyang, E., Chipman, J., Choi, J., Meier, A. H., Smink, D. S., Terhune, K. P., . . . George, B. C. (2019). The effect of gender on operative autonomy in general surgery residents. Surgery, 166(5), 738-743. https://doi.org/10.1016/j.surg.2019.06.006
Organisation for Economic Co-operation and Development. (2022). The proportion of female doctors has increased in all OECD countries over the past two decades. https://www.oecd.org/gender/data/the-proportion-of-female-doctors-hasincreased-in-all-oecd-countries-over-the-past-two-decades.htm
Olson, E. M., Dines, V. A., Ryan, S. M., Halvorsen, A. J., Long, T. R., Price, D. L., Thompson, R. H., Tollefson, M. M., Van Gompel, J. J., & Oxentenko, A. S. (2022). Physician identification badges: A multispecialty quality improvement study to address Professional misidentification and bias. Mayo Clinic Proceedings, 97(4), 658-667. https://doi.org/10.1016/j.mayocp.2022.01.007
Olson, E. M., Sanborn, D. M., Dyster, T. G., Kelm, D. J., Murray, S. G., Santhosh, L., & DesJardin, J. T. (2023). Gender disparities in critical care procedure training of internal medicine residents. American Thoracic Society Scholar, 4(2), 164-176. https://doi.org/10.34197/ats-scholar.2022-0025OC
Saberi, R. A., Herrera Gomez, L. C., Brady, A. C., Sola, J. E., Velazquez, O. C., & Neville, H. L. (2021). AAMC data shows effect of surgery faculty diversity on general surgery resident attrition rate at programs sponsored by LCME-accredited medical schools. Journal of Surgical Education, 78(4), 1123-1126. https://doi.org/10.1016/j.jsurg.2020.11.015
Sabin, J., Guenther, G., Ornelas, I. J., Patterson, D. G., Andrilla, C. H. A., Morales, L., Gurjal, K., & Frogner, B. K. (2022). Brief online implicit bias education increases bias awareness among clinical teaching faculty. Medical Education Online, 27(1), Article 2025307. https://doi.org/10.1080/10872981.2021.2025307
Sakowski, S. A., Feldman, E. L., Jagsi, R., & Singer, K. (2020). Energizing the conversation: How to identify and overcome gender inequalities in academic medicine. Journal of Continuing Education in the Health Professions, 40(4), 274-278. https://doi.org/10.1097/ceh.0000000000000296
Sethi, S., Edwards, J., Webb, A., Mendoza, S., Kumar, A., & Chae, S. (2022). Addressing gender disparity: Increase in female leadership increases gender equality in program director and fellow ranks. Digestive Diseases and Sciences, 67(2), 357-363. https://doi.org/10.1007/s10620-020-06686-5
Sobel, A. D., Lavorgna, T. R., Ames, S. E., Templeton, K. J., & Mulcahey, M. K. (2023). Interpersonal interactions and biases in orthopaedic surgery residency: Do experiences differ based on gender? Clinical Orthopaedics and Related Research, 481(2), 369-378. https://doi.org/10.1097/corr.0000000000002457
Sulibhavi, A., Kaufmann, M. R., Shetty, K. R., Wulu, J. A., Tracy, L. F., & Levi, J. R. (2021). Factors associated with distribution of female otolaryngology residents in United States. Laryngoscope, 131(2), E367-E372. https://doi.org/10.1002/lary.28746
Yeo, J. (2024). Gender equality Data and flow chart.docx (Version 1). Figshare. https://doi.org/10.6084/m9.figshare.25980352.v1
Ying, Y., Dupre, J., & Bhanji, F. (2023). Female surgical trainee recruitment and attrition – A 10-year national retrospective review. The American Journal of Surgery, 225(2), 282-286. https://doi.org/10.1016/j.amjsurg.2022.07.020
Zhang, N., Blissett, S., Anderson, D., O’Sullivan, P., & Qasim, A. (2021). Race and gender bias in internal medicine program director letters of recommendation. Journal of Graduate Medical Education, 13(3), 335-344. https://doi.org/10.4300/jgme-d-20-00929.1
*Han Ting Jillian Yeo
10 Medical Drive,
Singapore 117597
Email: jillyeo@nus.edu.sg
Submitted: 24 December 2023
Accepted: 31 July 2024
Published online: 7 January, TAPS 2025, 10(1), 4-9
https://doi.org/10.29060/TAPS.2025-10-1/GP3201
Muhamad Saiful Bahri Yusoff1,2
1Department of Medical Education, School of Medical Sciences, Universiti Sains Malaysia, Malaysia; 2Centre for the Development of Academic Excellence, Universiti Sains Malaysia, Malaysia
Abstract
Introduction: This article explores the dynamic relationship between the Scholarship of Teaching and Learning (SoTL) and the well-being of students and educators within the context of medical education.
Methods: The author critically reviewed the salient views and knowledge at the intersection of SoTL, well-being, and resilience. By critically examining literature, insights from various studies were synthesised, offering a detailed overview of the current state of knowledge in this field. This review guided the identification of key practices and recommendations.
Results: SoTL emerges as a transformative force, enhancing well-being for both students and educator through evidence-based practices and innovative teaching methods. The article explores the crucial role of SoTL in fostering resilience, not only among students but also among educators. Despite promising evidence, challenges in implementing SoTL for well-being persist, requiring strategic approaches to overcome traditional paradigms. The discussion extends to the global implications of SoTL, emphasising the need for collaborative efforts to foster better educational practices and establish inclusive learning environments.
Conclusion: As we assess the evidence for transformative change, a call-to-action echoes, urging global collaboration, research endeavors, and institutional support to realise the full potential of SoTL, ultimately creating environments where both learners and educators thrive.
Practice Highlights
- Employ evidence-based teaching methods derived from SoTL practices.
- Prioritise individuals’ mental, emotional, and social growth through SoTL practices.
- Cultivate adaptive learning approaches to enhance student resilience through SoTL practices.
- Acknowledge and bolster the well-being of educators through SoTL practices.
- Embrace cross-cultural collaboration within the realm of SOTL practices.
I. INTRODUCTION
The Scholarship of Teaching and Learning (SoTL) involves a systematic examination of teaching practices and their impact on student outcomes, aiming to achieve optimal educational results and contribute to societal enhancement (Luan et al., 2019). Rooted in research, evidence, and critical reflection, SoTL enhances practices within specific disciplines and professions (Coleman et al., 2023). Typically led by discipline-specific teachers, SoTL-based projects focus on improving both teaching methods and students’ learning experiences (Coleman et al., 2023). In the evolving educational landscape, including advancements in technology and shifts in learning methods, SoTL is essential for improving instructional techniques and evaluating their impact on both academic success and the well-being of students and educators. Wellbeing signifies the state of positive emotions, effective functioning, the realisation of one’s potential, a sense of control, purpose, and positive relationships (Ruggeri et al., 2020). Within traditional teaching methods, a pivotal research question arises: Do we have enough evidence to advocate for a significant change acknowledging the diverse experiences of educators and learners? This prompts a close examination of the current educational landscape, evolving roles of educators and learners, and the urgent need for a comprehensive understanding of well-being and resilience in the context of SoTL.
II. METHODS
The author critically reviewed the salient views and knowledge at the intersection of SoTL, well-being, and resilience. By critically examining selected literature from diverse studies, insights were synthesised to present a detailed overview of the current state of knowledge in this field. The approach allowed for an in-depth exploration of how SoTL principles are implemented and their impact on the well-being of students and educator. The synthesis of study findings resulted in a comprehensive understanding and practical recommendations for transformative educational practices.
III. RESULTS
A. Current Landscape of Teaching and Learning
The current way we teach relies heavily on traditional methods, often involving direct instruction and focusing on course content. While these methods have traditionally aimed at spreading knowledge, we are now questioning their impact on the well-being of students and educator (Coleman et al., 2023; Khairul Anhar Holder et al., 2023). Conventional teaching, with its emphasis on standardised assessments and delivering content, might unintentionally lead to increased stress and reduced resilience among learners. It’s clear that education is changing, and there is a growing call for a more comprehensive approach to teaching and learning. This means exploring methods that not only promote academic success but also prioritising the well-being and resilience of everyone involved in education.
B. Current Concept of Scholar of Teaching and Learning (SoTL)
SoTL is a dynamic approach to education, dedicated to improving teaching methods and enhancing student learning experiences (Coleman et al., 2023; Luan et al., 2019). It employs transformative teaching methods that connect academic content with real-world contexts, fostering critical thinking skills. SoTL involves reflective practice, where educators systematically assess and improve teaching using evidence-based research and educational theory. SoTL promotes knowledge sharing among educators, encouraging collaboration and professional development. Through educational inquiry, SoTL engages educators in thorough investigations, contributing to knowledge creation that enhances teaching practices. Ultimately, SoTL serves as a catalyst for transforming education by advocating for experiential learning, innovative teaching methods, and inclusive strategies, preparing students for success in a changing global landscape. SoTL encompasses transformative pedagogy, reflective practice, teacher dissemination, educational inquiry, and educational transformation (see Figure 1).
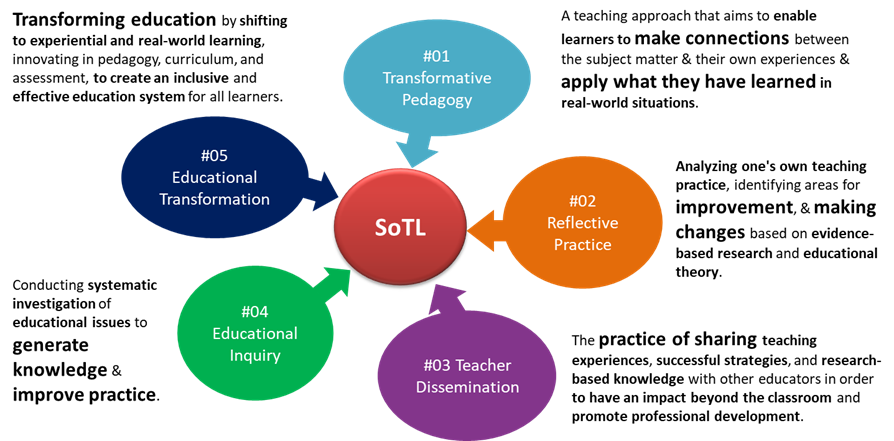
Figure 1. The key characteristics of SoTL
C. Defining Well-being and Resilience in Medical Education
In medical education, well-being goes beyond simply being stress-free (Roslan et al., 2022; Ruggeri et al., 2020). Alongside well-being, resilience becomes essential for overcoming challenges since it is the ability to recover from setbacks, adapt to changing circumstances, and thrive in adversity (Khairul Anhar Holder et al., 2023; Roslan et al., 2022). Figure 2 illustrates the interconnected components and outcomes of well-being in medical education. The left side highlights factors contributing to well-being such as resilience, while the right side shows the outcomes of enhanced well-being, such as better patient care, and reduced burnout.
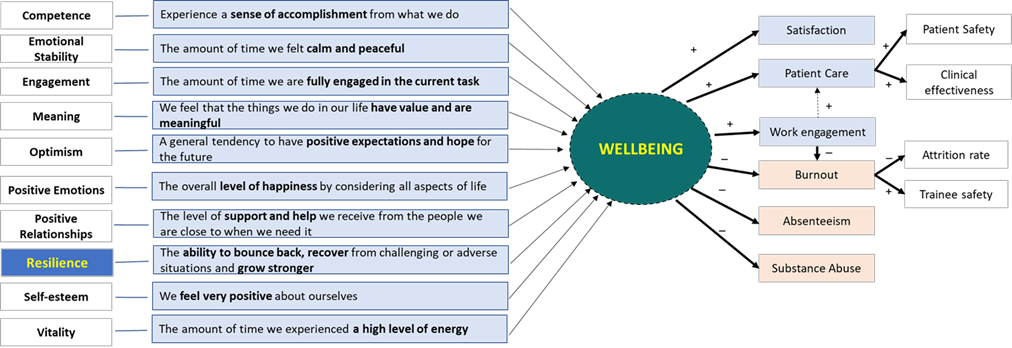
Figure 2. The interconnectedness of wellbeing and resilience in medical education
D. Roles of SoTL in Enhancing Well-being and Resilience
SoTL proves to influence student well-being enhancement within educational environments (Coleman et al., 2023; Luan et al., 2019). As educators embrace evidence-based practices, the imperative of prioritising well-being in pedagogical discourse becomes evident. SoTL, employing rigorous research and reflective teaching, seeks strategies that not only elevate academic success but also positively contributes to the student experience. Research findings highlight the substantial impact of teaching practices guided by SoTL principles on student engagement, motivation, and satisfaction (Coleman et al., 2023; Khairul Anhar Holder et al., 2023). This intertwining of SoTL with well-being underscores its pivotal role in shaping a more comprehensive and enriching educational experience (Coleman et al., 2023).
E. Educator Well-being
Teaching, with its inherent demands and complexities, can significantly influence educators’ well-being. SoTL recognises the critical role of supporting educator well-being as essential for sustainable and effective teaching practices. Educator well-being extends beyond workload management to encompass the emotional and intellectual dimensions of teaching. Institutions embracing SoTL principles prioritise initiatives such as professional development, mentorship programs, and fostering a conducive work environment (Coleman et al., 2023; Luan et al., 2019). These endeavors not only elevate teaching quality but also contribute to the personal and professional growth of educators, leading to their well-being.
F. Student Well-being
The core of SoTL lies in its significant impact on students’ well-being, surpassing traditional measures of academic success by recognising the intricate connection between a student’s educational success and their overall well-being (Khairul Anhar Holder et al., 2023). The implementation of evidence-based teaching practices, guided by SoTL principles, establishes an environment conducive to positive mental, emotional, and social development among students. Research indicates that students exposed to such approaches report higher levels of satisfaction, motivation, and a sense of belonging within the academic setting (Coleman et al., 2023). Through innovative teaching methods, SoTL fosters holistic student development, addressing diverse needs and serve as a catalyst for student well-being, cultivating a rewarding and supportive educational experience (Coleman et al., 2023; Luan et al., 2019).
G. Challenges in Implementing SoTL for Well-being
Despite the potential of SoTL to improve student and educator well-being, its implementation faces challenges, notably overcoming traditional teaching paradigms. Resistance to change within academic institutions, often rooted in institutional cultures and ingrained beliefs, can hinder the integration of SoTL-informed practices. Cultural and institutional barriers may also manifest in the allocation of resources and recognition. SoTL demands time, collaboration, and institutional support for meaningful implementation, posing challenges for institutions in prioritising these aspects over more traditional academic pursuits (Luan et al., 2019). The complex challenges associated with integrating SoTL for well-being underscore the necessity for strategic approaches to overcome these obstacles and pave the way for transformative changes in educational practices (Coleman et al., 2023).
H. The Need for Resilience in Learning Environments
In the ever-evolving field of education, resilience stands out as a crucial quality for navigating the complexities of learning environments (Khairul Anhar Holder et al., 2023; Roslan et al., 2022; Ruggeri et al., 2020). Students who develop resilience not only excel academically but also build a mindset that prepares them for uncertainties in the future. SoTL plays a vital role in fostering resilience by promoting pedagogical strategies that encourage adaptive learning. Through experiential approaches, collaborative projects, and real-world applications of knowledge, SoTL contributes to the development of resilient learners (Coleman et al., 2023). SoTL emphasises the transformative potential of educational practices that not only convey knowledge but also equip learners with the resilience needed to thrive in an ever-changing world (Coleman et al., 2023; Luan et al., 2019).
I. Evaluating the Evidence for Transformational Change
Do we have enough evidence to support a transformative change in educational practices? Recent studies indicate a strong connection between SoTL-informed teaching practices and positive outcomes, both academically and well-being (Coleman et al., 2023). However, challenges exist due to variability in methodologies, research scope, and the need for longitudinal studies to assess sustained effects. The evidence is promising, showing improved student engagement, increased educator satisfaction, and positive learning environments (Coleman et al., 2023). Further research is needed to establish causal relationships and identify specific SoTL elements contributing significantly to well-being. A global perspective is crucial, requiring collaborative, cross-cultural research efforts to enrich the evidence base and ensure global applicability of transformative changes.
J. Implications for Global Medical Education
Exploring SoTL’s impact on student and educator well-being has profound implications for global medical education. Applied globally, SoTL principles can transcend cultural and institutional boundaries, fostering a more inclusive and responsive educational landscape (Roslan et al., 2022; Ruggeri et al., 2020). Successful SoTL implementations globally offer insights for transformative changes in education (Coleman et al., 2023; Luan et al., 2019). However, addressing cultural nuances, regional differences, and institutional variations requires a careful global approach to applying SoTL principles. Global medical education benefits from collective efforts, fostering cross-cultural exchanges of SoTL best practices (Coleman et al., 2023). The wide-reaching implications of SoTL, underscored by a system-learner-oriented framework for well-being (Figure 3), highlight the need for collaborative endeavors to shape a more equitable global educational experience. SoTL should be reimagined as an emerging practice for researchers to impact teaching, learning, and assessment, promoting well-being (Coleman et al., 2023).
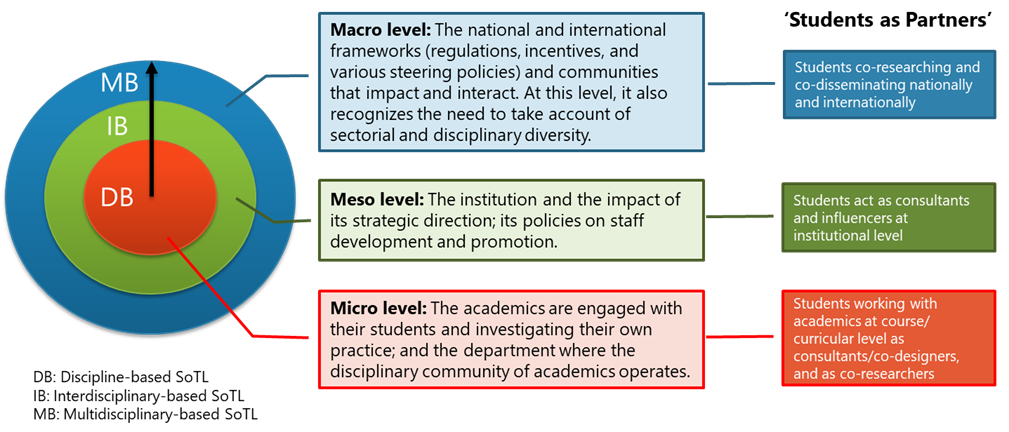
Figure 3. A System-Learner-Oriented SoTL for Wellbeing Framework
IV. DISCUSSION
The current education landscape is undergoing a significant shift away from traditional teaching practices due to their potential unwanted impact on student and educator well-being (Coleman et al., 2023; Khairul Anhar Holder et al., 2023). This recognition has led to a growing urgency for transformative changes aligned with global academic needs. SoTL, encompassing transformative pedagogy, reflective practice, teacher dissemination, educational inquiry, and transformation, emerges as a guiding light in this educational shift, committing to enhancing teaching methodologies and student learning experiences despite facing challenges (Coleman et al., 2023; Luan et al., 2019).
Implementing SoTL for well-being faces many challenges, including resistance to change, institutional cultures, and fixed beliefs (Coleman et al., 2023; Luan et al., 2019). The need for resources, time, collaboration, and institutional support becomes apparent for meaningful implementation. This highlight potential lack of awareness amongst educator regarding SoTL practices, emphasising the importance of strategic approaches. Additionally, resilience in learning environments is vital for maintaining well-being and achieving academic success (Roslan et al., 2022; Ruggeri et al., 2020). In medical education, building resilience among students and educator is essential for coping with challenges (Khairul Anhar Holder et al., 2023) and recovering from setbacks effectively (Roslan et al., 2022).
Evaluating the current evidence on SoTL and its impact on well-being reveals promising connections but shows up the need for further research (Coleman et al., 2023). Recognising the variability in methodologies, research scope, and the necessity for longitudinal studies is crucial. Comprehensive evaluations and robust evidence are needed to validate the effectiveness of SoTL practices and their long-term impact on both student and educator well-being. This includes an in-depth examination of SoTL’s potential benefits and challenges to ensure that its implementation leads to meaningful and sustainable improvements in educational practices.
Advocating for a global perspective highlight diverse educational contexts worldwide. Collaborative, cross-cultural research efforts are vital to enrich the evidence base and ensure the global applicability of transformative changes. The extension of educational experiences and innovations through sharing practices and policies will be crucial. By integrating SoTL principles, fostering a culture of continuous improvement, and prioritising well-being, global medical education can create supportive, resilient, and effective learning environments that cater to the holistic development of students and educator.
V. CONCLUSION
Integrating SoTL with student and educator well-being signifies a transformative shift in global education. The evidence reveals that adoption of SoTL principles as a pathway to comprehensive educational experiences, emphasising the connection between teaching methods and well-being. A resounding call to action emphasises the essential need for global collaboration, dedicated research, and institutional support to unlock SoTL’s full potential. Only through these collective efforts can educational environments foster the flourishing of student and educator, marking a paradigm shift worldwide.
Notes on Contributors
MSBY contributes to the conception of the work, the acquisition of data for the work, drafts the work or revising it critically for important intellectual content, approves the final version to be published, and agrees to be accountable for all aspects of the work.
Acknowledgement
The content of this article is mainly based on a presentation titled “SOTL in Student and Faculty Well-being and Resilience – Do We Have Enough Evidence for a Transformational Change?” given by the author at the 20th Asia Pacific Medical Education Conference in Singapore. This article has undergone language editing by ChatGPT 3.5 to enhance its syntax and improve overall clarity.
Funding
This paper has not received any fundings.
Declaration of Interest
The author declared no conflict of interests.
References
Coleman, K., Uzhegova, D., Blaher, B., & Arkoudis, S. (2023). The educational turn: Rethinking the scholarship of teaching and learning in higher education. Springer Nature, Singapore. https://doi.org/10.1007/978-981-19-8951-3
Luan, W. S., Khambari, M. N. M., Razali, A. B. M., Rashid, S. A. & Ching, F. T. H. (2019). Scholarship of teaching and learning @UPM. Centre for Academic Development (CADe), Universiti Putra Malaysia, Malaysia. https://cade.upm.edu.my/upload/doku men/20220624103811eBook_-_SoTL@UPM_(Complete).pdf
Ruggeri, K., Garcia-Garzon, E., Maguire, Á., Matz, S., & Huppert, F. A. (2020). Well-being is more than happiness and life satisfaction: A multidimensional analysis of 21 countries. Health and Quality of Life Outcomes, 18(1), 1-16. https://doi.org/10.1186/ s12955-020-01423-y
Roslan, N. S., Yusoff, M. S. B., Morgan, K., Razak, A. A., & Shauki, N. I. A. (2022). Evolution of resilience construct, its distinction with hardiness, mental toughness, work engagement and grit, and implications to future healthcare research. Education in Medicine Journal, 14(1), 99-114. https://doi.org/10.21315/eimj 2022.14.1.9
Khairul Anhar Holder, N. A., Pallath, V., Vadivelu, J., & Foong C. C. (2023). Using document phenomenology to investigate academic failure among year 1 undergraduate Malaysian medical students. BMC Medical Education, 23(310), 1-19. https://doi.org/10.1186/s12909-023-04285-2
*Assoc. Prof. Dr Muhamad Saiful Bahri Bin Yusoff
Department of Medical Education,
School of Medical Sciences,
Universiti Sains Malaysia,
Kelantan, Malaysia
+60169629640
Email: msaiful_bahri@usm.my
Submitted: 2 April 2024
Accepted: 12 September 2024
Published online: 7 January, TAPS 2025, 10(1), 27-35
https://doi.org/10.29060/TAPS.2025-10-1/OA3247
Estivana Felaza1, Ardi Findyartini1,2, Rita Mustika1, Jenny Bashiruddin1, Joedo Prihartono3, Lucia RM Royanto4 & Subha Ramani5
1Department of Medical Education, Faculty of Medicine Universitas Indonesia, Indonesia; 2Medical Education Centre, Indonesia Medical Education and Research Institute (IMERI), Faculty of Medicine Universitas Indonesia, Indonesia; 3Department of Public Health, Faculty of Medicine Universitas Indonesia, Indonesia; 4Faculty of Psychology Universitas Indonesia, Indonesia; 5Brigham Women and Child Hospital, Harvard Medical School, USA
Abstract
Introduction: Professional identity formation requires students’ ability to reflect, which can be supported by constructive feedback from teachers. Feedback practice faces many challenges, including those related to sociocultural aspects. Feedback can be optimised by implementing a model suitable to the attributes of students, teachers, and the clinical environment. This study aimed to develop a suitable feedback model and test its effectiveness in promoting reflection.
Methods: The model was designed based on the theoretical framework and identified feedback-related attributes in FMUI. Expert reviews and cognitive interviews were conducted before the model was tested. The model’s effectiveness was tested using a quasi-experimental design involving 74 students in the Paediatric Module. Students were asked to reflect on their mini-CEX experience after receiving feedback from teachers, and the depth of reflection was compared between students in the intervention and control group. The depth of reflection was measured using Kember scoring, and bivariate analysis was conducted using SPSS 20.0.
Results: The model consists of 5 steps including: Rapport building, Acknowledge students’ strengths, Identify aspect(s) that need improvement, Share teachers’ experiences, and Establish a plan to improve. Deep reflection was more frequently found in the intervention group. Mann-Whitney test showed that the difference between groups was statistically significant (Z=2.964, p=0.003), indicating that reflection in the intervention group was deeper than the control group.
Conclusion: The feedback model formulated based on feedback-related attributes in FMUI was named the RAISE model. Upon testing, students receiving the model could reflect more deeply compared to those receiving the standard model.
Keywords: Feedback, Clinical, Reflection, Sociocultural
Practice Highlights
- Constructive feedback is needed for medical students to optimally form their professional identity, especially in clinical settings
- The RAISE model which was developed based on feedback-related attributes can be implemented in clinical education
- The RAISE model consists of five steps: Building rapport, Acknowledge students’ strengths, Identify aspect(s) to improve, Share teachers’ experience, and Establish a plan to improve
- The RAISE model promotes students’ ability to reflect on their experiences
I. INTRODUCTION
Medical students’ professional identity is mostly formed during their clinical education (Cruess et al., 2015). Professional identity formation is a long and complex process that occurs through the integration of values and norms of the profession. Socio-constructivist theory can explain how learning occurs in clinical settings through the involvement of students in a medical community of practice. As students immerse themselves in the clinical environment, they engage in numerous interactions with their surroundings. The interactions expose them to professional values, which are gradually internalised as students develop their new identity as medical doctors (Cruess et al., 2015).
Optimal professional identity formation requires students’ ability to reflect on their experiences. Reflection enables students to extract meaning from their hectic day-to-day activities, and create plans to continuously improve themselves (Mann et al., 2009). The ability to reflect is also essential in their future profession as doctors. Reflection was defined as critically analysing one’s own experience to reach new and deeper comprehension and insight. Experience become the object to reflect, and the process of recalling and analysing the experience was conducted with the intention of improving future performance (Mann et al., 2009). Reflection also becomes the media to process feelings and emotions, and create plans to improve performance, which leads to improved clinical decision-making ability (Rozental et al., 2021). The importance of reflective practice made it necessary to provide students with opportunity to become skilful in conducting reflection.
The analysis of reflection should include many perspectives to get comprehensive views and insights. One of the ways to support reflection is through the provision of constructive feedback (Husebo et al., 2015; Sandars, 2009). Feedback has been shown to be beneficial in helping students improve their performance (Choi et al., 2020; Johnson et al., 2020; Trehan et al., 2015). Information given through feedback assists students in identifying the improvement needed and the strategies they can use. Feedback can initiate reflections by pointing out the gap between the intended outcome and the current performance; and it can also strengthen reflection by confirming students’ judgment and promoting insights into their performance (Nicol & MacFarlane-Dick, 2006).
Many problems are still found in the practice of feedback in clinical settings, such as the message not being specific enough and the limited time available for interaction. In addition, the Indonesian culture adds certain unique challenges to feedback practice, as identified in our previous study (Felaza et al., 2023). These challenges can be associated with the cultural dimensions of high-power distance and collectivism in Indonesian society. Teachers, experienced and have expertise, are believed by students to know what is best. In a busy clinical environment, the hierarchical gap creates a preference of both teachers and students to engage in directive feedback. In receiving feedback, students tend to appear receptive even when not fully agreeing with the feedback. Being a collectivistic society, group approaches in seeking, providing, and processing feedback practices were commonly found. Students share their feedback experiences with their peers, resulting in collective perception of teacher that they had interacted with (Felaza et al., 2023). Similar challenges have been reported in other studies conducted in Indonesia and Thailand (Areemit et al., 2020; Suhoyo et al., 2018).
Considering the importance of feedback in facilitating students’ professional identity formation, and the way feedback practice is affected by sociocultural aspects, there is a need to develop a feedback model suitable to the attributes of students, teachers, and the clinical environment in Indonesia. This study aims to develop a feedback model relevant to our setting and assess its effectiveness in supporting students’ reflective ability. This study proposes two research aims:
- To develop a feedback model suitable for the Indonesian clinical education setting.
- To evaluate the effectiveness of the feedback model in supporting students’ reflective ability.
II. METHODS
This quantitative research was conducted using a design-based research (DBR) approach, comprising the following steps of identifying the problem, designing a solution, evaluating its effectiveness in a real-life setting, and reflecting on the outcomes (Scott et al., 2020). The first step of our DBR was the identification of feedback-related attributes in FMUI, in a study conducted in September 2023. The next steps, described in detail below, included development of a feedback model within our institution based on data from the previous study, followed by evaluation of its effectiveness in promoting reflection.
A. Feedback model development
The development of the model was guided by a theoretical framework from literature and findings of students’, teachers’, and environmental attributes in our setting. Socio-constructivism, as the theoretical framework, perceives learning as a process of making meanings from experiences through social interactions. Discourses between teacher and students exposes students to thought process and professional norms and values which later can be internalised within themselves. The attributes identified were environmental attributes (limited time, collectivistic, hierarchical, and the need for a safe environment), teachers’ attributes (busy, expert, and having the skill to provide feedback), and students’ attributes (dependent on feedback, less able to read between the lines, perceived to be less resilient, appear to be receptive of feedback, critical, and values teacher’s experience). These findings have been published on September 2023 (Felaza et al., 2023). Along with the socio-constructivist approach as the theoretical framework, these attributes would become the foundation in the development of the model.
Review by experts and cognitive interviews were conducted to ensure the model’s readiness for implementation. Review panel included experts on medical education and communication, program coordinator, and module coordinators. The model was sent via e-mail, and experts were asked to provide feedback on each step and the overall applicability of the model. Cognitive interviews involved clinical teachers from surgery-related and non-surgery-related specialties as future users of the model. After receiving explanation of the model, the teachers practiced the model on their clinical teaching activities. Interviews were held with each teacher to gain input on the experience. Inputs from expert review and cognitive interviews were used to refine the model. The final version of the model was taught to clinical teachers in Paediatric Module as a preparation to test the model. The model was tested during Mini-Clinical Evaluation Exercise (Mini-CEX) by comparing its effectiveness with the Feedback Sandwich method as the standard model being used in FMUI. Mini-CEX is a workplace-based assessment which evaluate students’ performance of clinical skills in real setting. The assessment was originally intended for formative purposes as the clinical teacher observes the performance and provide feedback for students (Hejri et al., 2019). The sandwich model was found to be the common method used for feedback provision in FMUI, and it starts with informing students of the positive aspects of their performance, followed by the negative ones, and closed with another positive aspect (Jug et al., 2019).
B. Testing the effectiveness of the model
The design used was quasi-experimental, involving 5th-year FMUI medical students during their clinical rotation in Paediatric Module. There were 37 students in each group and the data collection took place in May 2022–March 2023. Students in the intervention group received feedback using the new model, while their peers in the control group received feedback using the Sandwich model (Jug et al., 2019). Upon completing data collection in the control group, authors conducted training for teachers on how to utilise the new model, followed by data collection in the intervention group.
Data was collected by asking students to record their voices as they reflect by thinking out loud. FMUI students have been introduced to reflection since the beginning of their academic years, and have experienced completing reflective writing assignments in several modules. For this study, they were instructed to reflect on their experience during mini-CEX. The depth of the reflection was then scored using Kember’s scoring. The scoring was developed by Kember based on Mezirow’s four levels of reflection, and it has been adapted to Bahasa Indonesia (Soemantri et al., 2022). Mezirow divided reflection to 4 levels based on its depth, starting from habitual action which showed no reflection, thoughtful action/understanding, reflection, and critical reflection (Kember et al., 2000). The scoring process was conducted separately by the first author (EF) and two co-authors (AF & RM) and later compared in team discussions to reach an agreed score. Bivariate analysis to test to compare the depth of the reflection between the intervention and the control group was conducted using SPSS 20.0.
III. RESULTS
The criteria for the feedback model were developed based on attributes found from the previous stage (as shown in Table 1 and Table 2).
|
|
Attributes |
Criteria of the Feedback Model |
|
Feedback environment |
|
Can be conducted in a limited time Utilise the high-power distance and collectivism to strengthen the importance of feedback Conducted in a safe environment
|
|
Teachers |
|
Practical Utilise the high-power distance to strengthen Using the faculty development program to strengthen feedback
|
|
Students |
|
Conducted consistently Delivered clearly Avoiding belittlement and sarcasm Conducted in a safe environment Accommodate discussions Enable teachers to share experiences
|
Table 1. Attributes of Factors Affecting Feedback and The Criteria of the Feedback Model
|
Step Proposed |
Criteria of the Feedback Model |
|
Rapport Building |
Develop safe environment
|
|
Acknowledge student’s strengths |
Avoid belittlement and sarcasm Accommodate discussions
|
|
Invite student to reflect |
Avoid belittlement and sarcasm Accommodate discussions
|
|
Share teacher’s experience and tips |
Enable teachers to share experiences Utilise the high power distance to strengthen the importance of feedback
|
|
Establish a plan to improve |
Accommodate discussions
|
Table 2. Steps Proposed and How it Accommodates the Criteria of the Feedback Model
The model was named RAISE as an abbreviation of the first letter in each step. The RAISE model was reviewed by an expert panel, consisting of 3 experts in medical education, 2 experts in communication, and 4 clinical program coordinators. Overall, the RAISE model was perceived as suitable to be implemented in the clinical settings by the expert panel (Figure 1). The crucial aspects that needed to be ensured were teachers’ comprehension of the reasoning behind each step, and the adjustability of the model to be applied in limited time and variability of contexts. Rapport building was considered an essential initial step to start feedback interaction. For the second step, it was advised that teachers ask the student to state positive aspects of performance first before confirmation based on their judgment. The focus of the third step was the areas for improvement, a term that experts emphasised. The step which was initially named ‘invite student to reflect’ was changed into ‘identify aspect that needs improvement’. This revision was made to prevent the misconception that reflection was exclusively covered in the 3rd step. In the fourth step, teachers share their experiences from which students can learn and develop ideas to improve their performance. The information shared should be relevant and can be delivered in a manner that is non-threatening and relevant for the students. The final step in the RAISE model focuses on the action plan for improvement. The agreed plan should be feasible and ready to be implemented.
Figure 1. RAISE Model After Expert Review
The model was then utilised by four clinical teachers in various teaching sessions, and cognitive interviews were conducted to gain insight into the experiences. They reported that the model was relatively easy to implement and able to accommodate the limited time available. The model helped develop rapport between teacher and students and enable the two of them to interact more effectively. Continuation between each step was seamless and the conversation did not have to be interrupted due to the movement from one step to another.
The final version was then taught to 22 clinical teachers in August 2022. The training was organised by the first author and two of the co-authors, who had expertise in medical education and experience in conducting faculty development. Various activities were held in the training (video appraisal, discussions, role play, and reflection) to ensure teachers’ ability to perform feedback provision using the RAISE model.
The final version was compared with the Sandwich model, the standard model being used in FMUI, to evaluate its effectiveness. The comparison between the steps of the two models can be seen in Table 3. As shown in the comparison, the strength of the RAISE model lies in its effort to establish rapport from the start of the feedback conversation, its way of facilitating reflection, and the opportunity it provides for teachers to share their experiences.
|
RAISE Model |
Standard Model |
|
Build rapport |
|
|
Discussing positive aspects of performance |
Delivering positive aspects of performance |
|
Discussing negative aspects of performance |
Delivering negative aspects of performance |
|
|
Delivering positive aspects of performance |
|
Sharing teacher’s experience |
|
|
Establishing improvement plan |
|
Table 3. Comparison Between the RAISE Model and the Standard Model
The effectiveness of the model was then tested during mini-CEX in Paediatric Module by comparing the depth of reflection in the experimental and control group. There were 37 students in each group with majority of students in experimental and control groups (30 and 28 students respectively) were female and belonged in the year 2018 batch.
Students reflected on the feedback they received, and the depth of the reflection was rated using the Kember score with the score ranging from 1-4 (1: no reflection; to 4: deep reflection). The distribution of the depth of students’ reflection is shown in Table 4.
|
Kember Score |
Intervention Group (%) |
Control Group (%) |
|
1 (no reflection) |
|
|
|
2 (comprehension) |
2 (5.4%) |
16 (43.2%) |
|
3 (reflection) |
26 (70.2%) |
17 (45.9%) |
|
4 (deep reflection) |
9 (24.4%) |
4 (11.9%) |
Table 4. Distribution of the Depth of Students’ Reflection
The distribution showed most of the students’ reflections in the intervention group were scored 3 based on the Kember score (26 students or 70.2%); while the score in the control group was almost evenly divided between 2 (16 students or 43.2%) and 3 (17 students or 45.9%). Deep reflection was more frequently found in the intervention group (9 students or 24.4%) compared to the control group (4 students or 11.9%).
Mann-Whitney test was used to compare the depth of students’ reflection between the intervention and the control group. The test showed that the mean rank in the intervention group was 30.61 and in the control group was 44.39. The difference between the two groups was statistically significant (Z = 2.964, p = 0.003), indicating that students’ reflections in the intervention group were deeper than their peers in the control group.
IV. DISCUSSION
This study aimed to develop a culturally relevant feedback model that nurtured reflective ability of medical students and to evaluate its effectiveness. The results indicated that students receiving feedback using the RAISE model could reflect more deeply compared to their peers receiving feedback using the standard model. The RAISE model was designed to enable feedback practice in an interactive manner, while feedback using Sandwich model was more directive. The RAISE model starts by building rapport between teacher and student in order to create a safe environment which helps student to optimally conduct reflection. The 2nd and 3rd steps of the model guide students’ reflection systematically, covering both the positive and negative aspects of the performance. On the 4th step, teachers’ sharing of their experiences helps to enrich students’ reflection, enabling them to learn from the experience, as well as strengthening and further maintaining the rapport between them. The final step concludes the interaction with a plan that students can implement to improve. Each of these steps portrays how reflection is guided and supported by the teacher through the feedback interaction.
The RAISE model was developed based on the socio-constructivist theory that describes learning as a way of constructing meaning from experiences. In clinical settings, students are exposed to a variety of experiences to build comprehension, acquire skill proficiency, and integrate professional norms and values. Effective feedback interactions between teachers and students facilitate students’ reflective process and support them in identifying effective ways to improve their performance (Wenger, 2020). Through these interactions, students are exposed to the teacher’s thought process, as well as their professional norms and values. The process that starts as inter-mental between teacher and student gradually becomes internalised into intra-mental within the student (Amineh & Asl, 2015; Tappan, 2010). This process enables teachers to guide students to reach their zone of proximal development (ZPD). Students are supported at each stage of their performance through the concept of scaffolding, and the level of support given would be decreased gradually as students gain the ability for independent clinical practice (Fani & Ghaemi, 2011).
Our previous study highlighted the need for rapport development and the act of sharing teachers’ own experiences in developing the feedback model (Felaza et al., 2023). Rapport was considered essential to create a safe environment for students. Interactions that empowered students in an authentic and safe environment, and teachers as role models in practicing reflection, were needed for creating reflective habits among students (Gathu, 2022; Mann et al., 2009). A sense of safety in feedback interaction was built upon a good relationship between teacher and students, mutual goals, and students’ perception of the teacher’s credibility (Sargeant et al., 2017). In the RAISE model, the safe environment has been developed since the beginning by building rapport between teacher and students. When students reflect, they would need to be open in analysing their experience. Destructive feedback would create reluctance for students to share their reflections (Chan & Lee, 2021; Khoiriyati & Sari, 2021). The model started by asking students’ perceptions of their performance, and their previous experience with similar situations; encouraging them to be open and reflective. The questions were relatively easy to answer and able to lighten the situation. Safety was continuously built through constructive dialogue between teachers and students which created an environment that was safe for reflection (MacNeil et al., 2020; Telio et al., 2015). Mutual goals also can implicitly be seen in students’ perception of the teacher’s intention. When the students believe that feedback was given to help them improve, they would be more willing to openly reflect (Blakey et al., 2019; Eva et al., 2012).
The reflection process is initiated when the condition cannot be handled simply by the automatic action the individual usually conducts or habitual act (Mann et al., 2009). The initiation of reflection might also be triggered by feedback. The feedback information made the individuals realise the quality of their performance, highlighting the strength and weaknesses that requires improvement (Husebo et al., 2015; Mann et al., 2009). When students receive feedback that is aligned with their perception regarding the quality of their performance, reflection usually occurs faster. However, for feedback information that is not aligned, students need to first manage the negative emotion it might evoke, analyse the message, and contemplate what action plan should be taken (Sargeant et al., 2009).
Teachers, perceived as knowledgeable figures, have numerous valuable experiences they can share. By incorporating the act of sharing experience, every feedback interaction would provide lessons from which students can extract meaningful understanding. This particular approach has not been seen explicitly in other feedback models. Other than enriching students’ comprehension, the sharing also provides a sense of relatedness with the teacher, and a role model on how to become reflective (Burgess et al., 2020). A role model in practicing reflection was an important aspect of strengthening students’ motivation. Teachers who practice self-reflection confirm to students that such practice can be done in their profession as doctors. Teachers’ reflective behaviour also showed the students that admitting weaknesses was not an embarrassing act, and on the contrary, it was an important skill to master to improve (Gishen & Chakrabarti, 2022). In the RAISE model, the opportunity for teachers to demonstrate reflection was mostly done in the 4th step. In this step, teachers can share their experiences that was relevant to the situation the students faced. Upon sharing the experience, the teacher can explain the lesson learned from that experience. Students receiving feedback using the RAISE model claimed that this step exposed them to teachers’ openness and minimised the power distance between them. Students also felt more motivated by listening to the experiences. Sense of relatedness was one of the factors that increased intrinsic motivation. The teachers’ willingness to share their experiences creates a connection between them and students, and strengthens students’ internal motivation (Kusurkar et al., 2011).
Other than being influenced on a systemic level by cultural aspects, such as power distance and collectivism; reflection is also affected in individual level by students’ and teachers’ reflective ability, teachers’ ability in facilitating reflection, and the relationship between teacher and students (Chan & Lee, 2021). The RAISE model supports teachers in facilitating students’ reflection through the use of reflective questions and the opportunity to show students how reflection was practiced by themselves as they shared their experiences. The rapport built during the interactions also strengthens the teacher-student relationship which further enables students to be more open and trusting in conducting their reflection.
Students’ reflective ability was crucial in their education process and later as they became member of the medical profession. Experiences in the clinical learning environment, which depicts the authentic professional world that students would enter, expose students to norms and values. Through reflection, students create meanings from these experiences which facilitate the formation of their professional identity as medical doctors (Winkel et al., 2017).
This study showed that implementation of the RAISE model, a feedback model developed based on the feedback-related attributes in Indonesian settings, enabled students to reflect more deeply on their performance. Findings from the study suggested that the RAISE model was suitable for supporting students’ reflection in a setting with high power distance and collectivistic background. However, it should be noted as a limitation of this study that reflection was an internal process and the effect might not be visible immediately. The changes in comprehension, perspectives, and even students’ attitude occurs gradually along the reflection process that was taking place. Therefore, further research is needed to observe the effect of reflection which might require longitudinal observation of students’ performance. The study involved a single institution in Jakarta, and therefore research and certain adjustments might be needed before the model can be implemented in different settings.
V. CONCLUSION
The feedback model formulated based on the feedback-related attributes in our clinical setting was named the RAISE model. It consists of 5 steps, which are Rapport building, Acknowledge student’s strengths, Identify aspects that need improvement, Share teacher’s experience and tips, and Establish a plan to improve. Our data indicate that students receiving feedback using the RAISE model were able to reflect more deeply compared to their peers receiving the standard model. We conclude that the model’s ability to create a safe environment, build rapport between teachers and learners, and teachers’ role-modelling of reflective practice can encourage students to be more self-reflective of their clinical performance.
Notes on Contributors
Estivana Felaza, Ardi Findyartini, Rita Mustika, Jenny Bashiruddin, Joedo Prihartono, Lucia RM Royanto, and Subha Ramani contributed to all processes of this research, and have read and approved this manuscript.
Dr. dr. Estivana Felaza, MPdKed is a Lecturer in Faculty of Medicine, Universitas Indonesia. She reviewed the literatures, designed the study, performed data collection and analysis, and wrote the manuscript.
Prof. dr. Ardi Findyartini, PhD is a Professor of Medical Education in the Faculty of Medicine, Universitas Indonesia. She developed the methodological framework for this research, involved in scoring the students’ reflections (data), provided feedback on the data collection, data analysis, and the manuscript writing process.
Dr. dr. Rita Mustika, M.Epid is an expert in Medical Education and a Lecturer in the Faculty of Medicine, Universitas Indonesia. She developed the methodological framework for this research, was involved in scoring the students’ reflections (data), provided feedback on the data collection, data analysis, and manuscript writing process.
Prof. Dr. dr. Jenny Bashiruddin, SpTHT-KL(K) is a Professor in Otolaryngology and an expert in Medical Education. She provided feedback on the theoretical and methodological framework of this research, data collection, data analysis, and the manuscript writing process.
Dr. dr. Joedo Prihartono, MPH is an expert in Statistics and a Senior Lecturer in Community Medicine, Faculty of Medicine, Universitas Indonesia. He provided feedback on the methodological framework of this research, data collection, data analysis, and the manuscript writing process.
Dr. Lucia RM Royanto, M.Si, Sp.Ed is an expert in Educational Psychology and a Senior Lecturer in the Faculty of Psychology, Universitas Indonesia. She provided feedback on the theoretical framework of this research, data collection, data analysis, and the manuscript writing process.
Dr. Subha Ramani, MBBS, MPH, PhD, FAMEE is an expert in Medical Education and an Associate Professor of Medicine in Harvard Medical School. She provided feedback on the theoretical and methodological framework of this research, data collection, data analysis, and the manuscript writing process.
Ethical Approval
The study was approved by the Research Ethics Review Committee of the Faculty of Medicine, Universitas Indonesia (approval number: KET-1114/UN2.F1/ETIK/ PPM.00.02/2021). The subjects of this study were informed verbally and in writing of the purpose, the methods, and the confidentiality of the data being collected. Each subjects’ involvement in this research were voluntary, and consent were signed upon receiving the necessary information.
Data Availability
Datasets generated and/or analysed in this study are available upon request via electronic mail to the corresponding author.
Acknowledgement
The authors would like to acknowledge the contributions of the students and clinical teachers who willingly involved and cooperated in this study.
Funding
No funding was obtained for this study.
Declaration of Interest
All authors have no declaration of interest.
References
Amineh, R. J., & Asl, H. D. (2015). Review of constructivism and social constructivism. Journal of Social Science, Literature & Language, 1(1), 9–16.
Areemit, R. S., Cooper, C. N., Wirasorn, K., Paopongsawan, P., Panthongviriyakul, C., & Ramani, S. (2020). Hierarchy, “Kreng Jai”, and feedback: A grounded theory study exploring perspectives of clinical faculty and medical students in Thailand. Teaching and Learning in Medicine, 33(3), 235–244. https://doi.org/10.1080/10401334.2020.1813584
Blakey, A. G., Smith-Han, K., Anderson, L., Collins, E., Berryman, E., & Wilkinson, T. (2019). “They cared about us students”: Learning from exemplar clinical teaching environments. BMC Medical Education, 19, 119–128. https://doi.org/10.1186/ s12909-019-1551-9
Burgess, A., van Diggele, C., Roberts, C., & Mellis, C. (2020). Feedback in the clinical settings. BMC Medical Education, 20(Suppl 2), 458–463. https://doi.org/10.1186/s12909-020-02280-5
Chan, C. K. Y., & Lee, K. K. W. (2021). Reflection literacy: A multilevel perspective on the challenges of using reflections in higher education through a comprehensive literature review. Educational Research Review, 32(2), Article 100376. https://doi.org/10.1016/j.edurev.2020.100376
Choi, S., Oh, S., Lee, D. H., & Yoon, H. S. (2020). Effects of reflection and immediate feedback to improve clinical reasoning of medical students in the assessment of dermatologic conditions: A randomized controlled trial. BMC Medical Education, 20, 146–154. https://doi.org/10.1186/s12909-020-02063-y
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2015). A schematic representation of the professional identity formation and socialization of medical students and residents: A guide for medical educators. Academic Medicine, 90(6), 718–725. https://doi.org/10.1097/acm.0000000000000700
Eva, K. W., Armson, H., Holmboe, E., Lockyer, J., Loney, E., Mann, K., & Sargeant, J. (2012). Factors influencing responsiveness to feedback: On the interplay between fear, confidence, and reasoning process. Advance in Health Science Education, 17, 15–26. https://doi.org/10.1007/s10459-011-9290-7
Fani, T., & Ghaemi, F. (2011). Implications of Vygotsky’s zone of proximal development in teacher education. Social Behavioral Science, 29, 1549–1554. https://doi.org/10.1016/j.sbspro.2011.11. 396
Felaza, E., Findyartini, A., Mustika, R., Bashiruddin, J., Royanto, L. R. M., Prihartono, J., & Ramani, S. (2023). Deeper look into feedback practice in an Indonesian context: Exploration of factors in undergraduate clinical setting. Korean Journal of Medical Education, 35(3), 263–273. https://doi.org/10.3946/kjme.2023.264
Gathu, C. (2022). Facilitators and barriers of reflective learning in postgraduate medical education: A narrative review. Journal of Medical Education and Curriculum Development, 9, 1–8. https://doi.org/10.1177/23821205221096106
Gishen, F., & Chakrabarti, R. (2022). Medical students’ perceptions of reflective practice in the undergraduate curriculum. MedEd Publish, 12, 53–67. https://doi.org/10.12688/mep.19211.3
Hejri, S. M., Jalili, M., Masoomi, R., Shirazi, M., Nedjat, S., & Norcini, J. (2019). The utility of mini clinical examination exercise in undergraduate and postgraduate medical education: A BEME review: BEME guide no. 59. Medical Teacher, 42(2), 1–18. https://doi.org/10.1080/0142159x.2019.1652732
Husebo, S. E., O’Reagen, S., & Nestel, D. (2015). Reflective practice and its role in simulation. Clinical Simulation in Nursing, 11, 368–375. http://doi.org/10.1016/j.ecns.2015.04.005
Johnson, C. E., Weerasuria, M. P., & Keating, J. L. (2020). Effect of face-to-face verbal feedback compared with no alternative feedback on the objective workplace task performance of health professionals: A meta-analysis and systematic review. BMJ Open, 10(3), Article e030672. https://doi.org/10.1136/bmjopen-2019-030672
Jug, R., Jiang, X., & Bean, S. M. (2019). Giving and receiving effective feedback. Archives of Pathology and Laboratory Medicine, 143, 244–250. https://doi.org/10.5858/arpa.2018-0058-RA
Kember, D., Leung, D. Y. P., Jones, A., Loke, A. Y., MacKay, J., Sinclair, K., Tse, H., Webb, C., Wong, F. K. Y., Wong, M., & Yeung, E. (2000). Development of a questionnaire to measure the level of reflective thinking. Assessment and Evaluation in Higher Education, 25(4), 381–395. http://doi.org/10.1080/713611442
Khoiriyati, A., & Sari, N. K. (2021). Reflective practice on nursing students: A qualitative study. Indonesian Nursing Journal of Education and Clinic, 6(2), 201–209. http://doi.org/10.24990/in jec.v6i2.391
Kusurkar, R., Croiset, G., & Ten Cate, O. (2011). Twelve tips to stimulate intrinsic motivation in students through autonomy-supportive classroom teaching derived from self-determination theory. Medical Teacher, 33, 978–982. https://doi.org/10.3109/01 42159x.2011.599896
MacNeil, K., Cuncic, C., Voyer, S., Butler, D., & Hatala, R. (2020). Necessary but not sufficient: Identifying conditions for effective feedback during internal medicine residents’ clinical education. Advances in Health Science Education, 25, 641–654. https://doi.org/10.1007/s10459-019-09948-8
Mann, K., Gordon, J., & MacLeod, A. (2009). Reflection and reflective practice in health professions education: A systematic review. Advances in Health Science Education, 14, 595–621. https://doi.org/10.1007/s10459-007-9090-2
Nicol, D., & MacFarlane-Dick, D. (2006). Formative assessment and self-regulated learning: A model and seven principles of good feedback practice. Studies in Higher Education, 31(2), 199–218. https://doi.org/10.1080/03075070600572090
Rozental, L., Meitar, D., & Karnielli-Miller, O. (2021). Medical students’ experiences and needs from written reflective journal feedback. Medical Education, 55, 505–517. https://doi.org/10.1111/medu.14406
Sandars, J. (2009). The use of reflection in medical education: AMEE Guide no 44. Medical Teacher, 31, 685–695. https://doi.org/10.1080/01421590903050374
Sargeant, J. M., Mann, K. V., van der Vleuten, C. P., & Metsemakers, J. F. (2009). Reflection: A link between receiving and using assessment feedback. Advances in Health Science Education, 14, 399–410. https://doi.org/10.1007/s10459-008-9124-4
Scott, E. E., Wenderoth, M. P., & Doherty, J. H. (2020). Design-based research: A methodology to extend and enrich biology education research. CBE Life Science Education, 19(3), 1–12. https://doi.org/10.1187/cbe.19-11-0245
Soemantri, D., Mustika, R., & Greviana, N. (2022). Inter-rater reliability of reflective writing assessment in an undergraduate professionalism course in medical education. Education in Medicine Journal, 14(1), 87–97. http://doi.org/10.21315/eimj2022.14.1.8
Suhoyo, Y., Schönrock-Adema, J., Emilia, O., Kuks, J. B. M., & Cohen-Schotanus, J. (2018). Clinical workplace learning: Perceived learning value of individual and group feedback in a collectivistic culture. BMC Medical Education, 18, 79–84. https://doi.org/10.1186/s12909-018-1188-0
Tappan, M. (2010). Sociocultural psychology and caring pedagogy: Exploring Vygotsky’s hidden curriculum. Educational Psychology, 33(1), 23–33. http://doi.org/10.1207/s15326985ep3301_2
Telio, S., Ajjawi, R., & Regehr, G. (2015). The “Educational Alliance” as a framework for reconceptualizing feedback in medical education. Academic Medicine, 90(5), 609–614. https://doi.org/10.1097/acm.0000000000000560
Trehan, A., Barton-Vaness, A., Carty, M. J., McCulloch, P., & Maruthappu, M. (2015). The impact of feedback of intraoperative technical performance in surgery: A systematic review. BMJ Open, 5, Article e006759. http://doi.org/10.1136/bmjopen-2014-006759
Wenger, E. (2020). Communities of practice and social learning systems: The career of a concept. Organization, 7(2), 225–246. http://doi.org/10.1177/135050840072002
Winkel, A. F., Yingling, F., Jones, A. A., & Nicholson, J. (2017). Reflection as a learning tool in graduate medical education: A systematic review. Journal of Graduate Medical Education, 5, 430–439. https://doi.org/10.4300/jgme-d-16-00500.1
*Estivana Felaza
Faculty of Medicine Universitas Indonesia,
Jalan Salemba Raya No 6,
Jakarta 10430, Indonesia
Email: estivanafelaza@gmail.com;
estivana.felaza01@ui.ac.id
Submitted: 13 June 2024
Accepted: 14 October 2024
Published online: 7 January, TAPS 2025, 10(1), 36-47
https://doi.org/10.29060/TAPS.2025-10-1/OA3438
Sivapalan Sanchayan1, Sisira Dharmaratne2, Shalika Pathirana3, Pavithra Godamunne3 & Madawa Chandratilake3
1Department of Medical Education, Faculty of Medicine, University of Jaffna, Sri Lanka; 2Translational Health Research Institute, Western Sydney University, Australia; Department of Medical Education, Faculty of Medicine, University of Kelaniya, Sri Lanka
Abstract
Introduction: Selection for basic medical training is highly contextual. The use of cognitive aptitude tests, which commonly supplement measures of prior academic achievement in the selection process of medical schools internationally, is rarely reported from resource-constrained settings in South Asia. We report on the psychometric properties of an aptitude test designed based on the UCAT format, administered to first-year medical undergraduates to determine its utility.
Methods: The aptitude test was administered online to first-year medical students shortly after their admission to two medical faculties in Sri Lanka (n=328). The reliability of the test was determined using Cronbach’s alpha. Overall and subtest scores were computed, and the scores of different demographic groups were compared using the t-test. Factor analysis of the subtests was performed.
Results: The internal consistency of the test was 0.63. The difficulty and discrimination indices were within the acceptable range. The mean score of the aptitude test (AT) was 70.9/100 (SD 8.88). The mean score for females was higher than for males (p=0.04). No statistically significant differences in AT scores were observed between different ethnicities or religions. The entry academic scores demonstrated a weak correlation with the overall AT score (Pearson’s correlation coefficient r=0.27), verbal reasoning (r=0.24), the human body (r=0.19), quantitative reasoning (r=0.18), and situational judgement (r=0.128). Factor analysis indicated items that need revision.
Conclusion: The results indicate the potential value of aptitude tests in Sri Lanka and in similar jurisdictions where selection criteria have yet to expand beyond prior academic performance. A way forward in introducing such tests has been outlined.
Keywords: Medical Student Selection, Medical Student Admission, Selection Criteria
Practice Highlights
- Aptitude tests assess cognitive and non-cognitive attributes desirable for healthcare professionals.
- The use of aptitude tests is rarely reported from resource constrained settings in South Asia.
- Sri Lanka uses only the national high school examination performance for medical school admission.
- This study indicates the potential value of aptitude tests in Sri Lanka and in similar jurisdictions.
I. INTRODUCTION
Selection for basic medical training is highly contextual and influenced by educational, geographical, socioeconomic, and political factors (Dharmaratne & Ponnamperuma, 2020; Patterson et al., 2018). High academic achievement has long been considered an appropriate criterion for ranking candidates for medical school (McManus et al., 2013; Patterson et al., 2017). However, this approach has been contested due to the low predictive validity of pre-university performance for medical school success (McManus et al., 2013; Prideaux et al., 2011).
Aptitude tests have emerged to assess cognitive and non-cognitive traits desirable for medical and healthcare professions (Gliatto et al., 2016; Greatrix & Dowell, 2020; Powis et al., 2021). Despite evidence on their potential to improve selection processes (Bala et al., 2022; Greatrix et al., 2021), most resource-constrained jurisdictions, including Sri Lanka, rely solely on prior academic achievement (Soemantri et al., 2020; University Grants Commission, 2023). This study represents an initial step in Sri Lanka toward introducing aptitude tests and reports on the psychometric properties of a test developed to measure cognitive attributes.
The Sri Lankan medical school admission system uses national high school examination results (G.C.E. AL) as the only criterion for admission (Dharmaratne & Ponnamperuma, 2020; University Grants Commission, 2023). The results of three AL subjects (Chemistry, Physics, and Biology) are considered, and an average Z score is used to rank individuals (University Grants Commission, 2023). A minimum of two credit passes and one simple pass is required for eligibility. A few candidates with foreign examination results equivalent to the G.C.E. AL Examination and meeting equitable minimum requirements are also admitted (University Grants Commission, 2023).
G.C.E. AL examination results have shown a mild correlation with subsequent undergraduate performance, with a maximum predictive correlation coefficient of 0.37 (de Silva et al., 2004, 2006; Hewage et al., 2011; Mettananda et al., 2006). These low figures may underestimate the true relationship, as range restriction among high-achieving candidates can affect the statistical accuracy of predictive validity measures (Zimmermann et al., 2017). Studies in the UK, addressing range restriction, found that prior academic performance is the best predictor of subsequent performance, accounting for 65% of the variance in undergraduate performance (McManus et al., 2013). However, this leaves 35% of the variance unexplained.
Aptitude tests are used worldwide to support medical student selection. The United Kingdom Clinical Aptitude Test (UKCAT), now named UCAT, has been used for nearly two decades (Greatrix & Dowell, 2020). The UCAT consists of 200 items in five subtests delivered over two hours (Paton et al., 2022). Results of the UKCAT and UCAT have been used to discriminate between high-achieving students during selection and predict undergraduate and postgraduate performance (Bala et al., 2022; MacKenzie et al., 2016; McManus et al., 2013; Paton et al., 2022).
However, there are additional qualities beyond academic readiness (prior academic performance and cognitive traits) that are necessary qualities of medical professionals that include desirable behaviours and attitudes that could indicate successful development as healthcare practitioners in the future (Patterson et al., 2018). The Ottawa consensus statement recommends that best practice selection should involve the use of selection criteria based on multi-source multi-method job analysis studies (Patterson et al., 2018). This necessitates the use of other selection processes such as structured interviews or multiple mini interviews (MMI).
This study aims to evaluate the psychometric properties of an aptitude test based on the UCAT format, administered to first-year medical undergraduates at two medical faculties in Sri Lanka. Specifically, the objectives are to evaluate the psychometric properties of the test, determine the relationship between Z scores at the AL examination and aptitude test scores, and compare the performance of different demographic groups in the aptitude test.
II. METHODS
A cross-sectional observational study was conducted in the faculties of medicine at the universities of Kelaniya and Jaffna, Sri Lanka. Including these two faculties allowed for the recruitment of an adequate number of students from the three main ethnic groups (Sinhala, Tamil, and Sri Lankan Moors) and a wider range of Z scores. All first-year students in 2023 from these faculties were invited to participate. Students admitted through selection criteria other than Sri Lankan advanced level performance were excluded. We obtained a sample size of 328 students who consented to participated in the study (response rate of 80.8%).
The aptitude test comprised 50 items across six subtests: abstract reasoning (8 items), the human body (8 items), quantitative reasoning (8 items), decision-making (8 items), verbal reasoning (8 items), and situational judgment (10 items). Except for the “the human body” subtest, all others were modelled after the UKCAT examination. The “human body” subtest was designed to assess advanced-level knowledge of human biology from the Sri Lankan school curriculum. Test items were selected by a panel of experts in psychology and medical education from the Faculty of Medicine, University of Kelaniya with the help of disability studies experts who use a similar test for selection to their course. These experts, being native Sri Lankans, ensured the items were culturally relevant and conceptually and semantically equivalent (Hambleton & Zenisky, 2010). Similar methods were used to finalise the Sinhala and Tamil versions of the test, translated by competent translators. Appendix 1 shows sample test items from each subtest. The test was piloted on 15 students and identified issues were corrected.
The test was administered via the online learning management system (LMS) of the respective faculties under examination conditions, with invigilators ensuring adherence to university examination protocols. Students had one hour to complete the test, available in English, Sinhala, and Tamil. Participants could choose the language they were most comfortable with to simulate AL examination conditions and to minimise interpretation errors.
Descriptive statistics and internal consistency (Cronbach’s alpha) were calculated for the test and each subtest and item analysis (Paniagua & Swygert, 2016) was performed. Correlations between the aptitude test score, subtest scores, and Z scores were calculated using Pearson’s correlation coefficient, and relationships to other demographic factors were analysed using Student’s t-test. Factor analysis was performed using R statistical package.
Written informed consent was obtained from the students before the test administration. Ethics approval was granted by the ethics review committee of the Faculty of Medicine, University of Kelaniya, and permission for the study was obtained from the deans of the respective medical faculties.
III. RESULTS
328 students participated in the study, yielding an overall response rate of 80.8%. The descriptive statistics of these students are presented in Table 1. The male-to-female ratio of the sample (31.7% to 68.3%) closely mirrors the demographics of the national cohort of medical undergraduates from the previous academic year (34% to 66%), as reported by the University Grants Commission, Sri Lanka (University Grants Commission, 2022).
|
Total group n=328 |
n |
(%) |
|
Gender |
|
|
|
Male |
104 |
(31.7) |
|
Female |
224 |
(68.3) |
|
Ethnicity |
|
|
|
Sinhala |
161 |
(49.1) |
|
Tamil |
123 |
(37.5) |
|
Moor |
43 |
(13.1) |
|
Other |
1 |
(0.3) |
|
Religion |
|
|
|
Buddhism |
143 |
(43.6) |
|
Hinduism |
108 |
(32.9) |
|
Islam |
43 |
(13.1) |
|
Christianity |
34 |
(10.4) |
|
University |
|
|
|
Jaffna (response rate) |
186 |
(90.7) |
|
Kelaniya (response rate) |
142 |
(70.6) |
Table 1. Descriptive statistics of the demographic variables of the sample
The overall mean aptitude test (AT) score was 70.9 (SD 8.88), with a median of 72. Female students had a higher mean AT score than male students (p=0.044, Table 2), while there was no statistically significant difference in the Z scores between genders (p=0.122). No significant differences in mean AT scores were found between ethnicities and religions. The Faculty of Medicine, University of Kelaniya, had a higher mean AT score (73.7, SD 8.7) than the Faculty of Medicine, Jaffna (68.8, SD 8.4, p=0.000). Similarly, the mean Z score at Faculty of Medicine, University of Kelaniya (2.10, SD 0.07) was higher than at Jaffna (1.89, SD 0.13, p=0.000).
|
AT score |
Z score |
|||
|
Female |
Male |
Female |
Male |
|
|
Mean |
71.6 |
69.4 |
1.99 |
1.96 |
|
Median |
72.0 |
72.0 |
2.06 |
1.99 |
|
Standard Deviation |
8.4 |
9.7 |
0.15 |
0.16 |
Table 2. Comparison of means of AT scores and Z scores between males and females
The internal consistency of the test was 0.628 and the subscales ranged between 0.2 to 0.47 (Table 3).
|
|
Mean |
SD |
Cronbach’s alpha |
|
Abstract Reasoning |
13.4 |
2.32 |
0.339 |
|
The Human Body |
14.6 |
1.72 |
0.248 |
|
Quantitative Reasoning |
13.5 |
2.31 |
0.411 |
|
Decision Making |
10.3 |
2.61 |
0.197 |
|
Verbal Reasoning |
10.2 |
3.17 |
0.433 |
|
Situational Judgment |
8.8 |
3.93 |
0.473 |
Table 3. Data regarding the subtests of the aptitude test
Difficulty and discrimination indices for each test item were calculated (Table 4). The difficulty index represents the proportion of students who answered each item correctly (Paniagua & Swygert, 2016). The mean difficulty index was 70.9% (SD 23.5), ranging from 19.2% to 99.4%. The discrimination index was calculated as the difference between the proportion of students who answered an item correctly in the top group (those who obtained the top 27% in the overall score) and bottom group (bottom 27% scorers) and measures an item’s ability to differentiate between students who performed best and those who performed worst on the test (Paniagua & Swygert, 2016). The mean discrimination index was 19% (SD 12) and ranged from 0 to 50%. There was only one item with the lowest discrimination index of 0. It had a difficulty index of 99.4% indicating that most students had scored it correctly. Items that adversely affected the reliability of the subtests were identified (Appendix 2).
|
Difficulty Index |
Proportion of questions (%) |
|
0 – ≤ 30 |
8 |
|
30 – ≤ 70 |
32 |
|
> 70 |
60 |
Table 4. Distribution of the difficulty indices of the aptitude test questions
The correlation analysis revealed several key findings regarding the relationship between Z and AT scores. The correlation coefficient between Z score and AT score was 0.268 (p=0.000), indicating a weak correlation. The coefficient of determination (r²) was calculated to be 0.072, suggesting that only 7.2% of the variability in AT scores could be explained by Z scores. This signifies a limited association between Z scores and overall AT performance. Further analysis was conducted on the correlation between Z scores and subtest scores. There was a weak but statistically significant correlation between Z scores and the subtests of verbal reasoning (r=0.24, p=0.000), human body (r=0.19, p=0.001), quantitative reasoning (r=0.18, p=0.001), and situational judgment (r=0.128, p=0.021). However, the correlations between Z scores and the subtests of abstract reasoning and decision-making were not statistically significant.
Factor analysis was performed using the most prominent two factors of each of the six subtests separately as they each measure well defined and different cognitive domains. The factor loading of abstract reasoning subtest is shown in figure 1. “Question 3” shows a strong positive loading on Factor 1, suggesting that this item heavily measures the trait most represented by this factor whilst “Question 5” shows a slight negative loading on Factor 1, indicating it measures a trait that is perhaps inversely related to what is captured by this factor. “Question 1” and “Question 2” are both located positively on Factor 2 but with minimal loading on Factor 1. This suggests that they are measuring traits more aligned with Factor 2. The items “Question 1”, “Question 2″ and “Question 3”, appear to be critical for measuring distinct aspects of abstract reasoning as shown by their stronger loadings. “Question 5” shows a strong negative loading on Factor 2, suggesting that it measures a trait that contrasts with what Factor 2 represents. “Question 4”, ” Question 6″, “Question 7”, and “Question 8” are clustered around the origin. This indicates that these items have weaker loadings on both factors, meaning they may not strongly measure the traits represented by either factor, or they could be measuring a balanced mix of both traits. While these questions contribute to the test, they might need to be reviewed to enhance their discriminative power or clarity in measuring specific abstract reasoning skills.
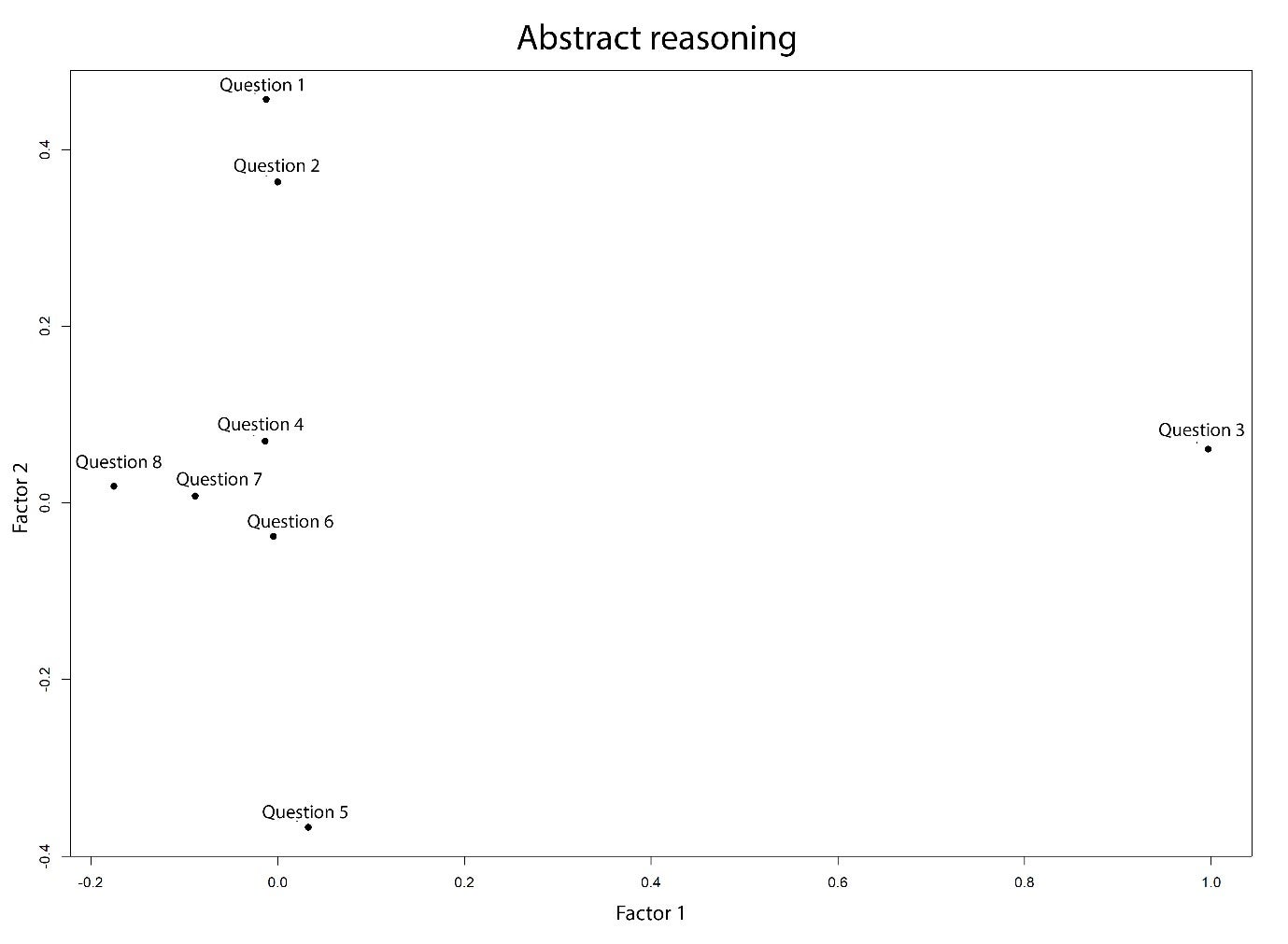
Figure 1. Two factor loading of the abstract reasoning subtest
The factor loadings of the other five subtests are shown in Appendix 3. Regarding the human body subtest, Factor 1 might represent knowledge or understanding of structural aspects of the human body, given the strong loading by “Question 11” and reasonable loading by other items. This factor could reflect knowledge regarding human biology whilst Factor 2 seems to capture a different dimension, suggested by the negative loading of “Question 15”. In quantitative reasoning, most questions are clustered near the centre with a slight spread along Factor 1, indicating moderate influence by this factor across the items. “Question 19” and “Question 22” are slightly farther along Factor 1 suggesting a stronger influence by the trait measured by this factor. Regarding the subtests of decision making, verbal reasoning and situational judgment, Factor 1 and Factor 2 seemed to be capturing different dimension of these subtests thereby suggesting the need for revision of their items.
IV. DISCUSSION
This study aimed to design an aptitude test and investigate its psychometric properties among first-year medical students from two selected faculties of Medicine in Sri Lanka. The results indicate that overall internal reliability of the aptitude test was marginal (Cohen et al., 2018). However, the reliability of the UKCAT has been 0.86 or above overall and between 0.58 – 0.86 for the subtests (MacKenzie et al., 2016). These findings demonstrate the value of evaluating and reviewing aptitude tests locally. Further, reviewing test items that adversely affected the internal consistency of the subtests for clarity and improved alignment with the construct, could improve the overall validity. It is likely that the low number of test items has further contributed to the low-reliability score (Taber, 2018). The UKCAT consists of 200 test items, as opposed to the 50 items in the aptitude test employed by the current study. The item analysis indicated that most of the questions were easy, with 60% having a difficulty index of more than 70%. The discriminating capacity of the items was low (mean discrimination index was 19%). This could be attributed to the aptitude test being administered to students who have performed well in the advanced level examination and already have been selected to medical school.
There was a weak correlation between the aptitude test score and the Z score (0.27), indicating that the test assessed a significantly different aspect of cognitive skills compared to traditional AL examinations. This observation encourages exploring how the aptitude test may be incorporated into the selection process. Different selection authorities use aptitude scores differently (Greatrix & Dowell, 2020). Overall, among the universities which employ UKCAT, the weightage given for school leaver level academic performance in the selection process has increased, while the use of aptitude test scores as an absolute or relative cutoff to be achieved also has increased over the period of 2008-2015 (Greatrix & Dowell, 2020). However, empirical evidence on a best way of using UKCAT or UCAT in the selection process is not available (Greatrix & Dowell, 2020). Therefore, implementing a valid aptitude test as a supplementary test and exploring predictive validities of such a test across a national sample is likely to provide more robust evidence of the utility of aptitude tests in the Sri Lankan context.
This study used an aptitude test developed and deployed systematically and modelled on a widely tested international aptitude test format for medical school selection. The sample was representative of demographics of the national cohort of medical students and included all three major ethnic groups and students with a wide range of Z scores. However, the limited number of test items may have offset these strengths. The authors did not have access to participants’ raw scores at the advanced level examination, which may have provided a more appropriate measure of performance for statistical manipulation. In addition, the aptitude test was administered to students who have already been selected to medical school, whereas ideally, it should have been administered to medical school applicants. Despite the limitations, the aptitude test returned an acceptable internal reliability score, and further analysis demonstrated a way forward.
V. CONCLUSION
This study was the first time in the literature that an aptitude test was evaluated in medical education settings in the Sri Lankan context. Using an aptitude test to select students for medical school in Sri Lanka and similar settings, where admission processes have not diversified, is potentially valuable. However, further studies are necessary to establish evidence to support the adoption of such a test in the Sri Lankan and other similar resource-constrained contexts where prior educational achievement primarily informs selection decisions. In the Sri Lankan context, further evaluating the psychometric properties and the predictive validity of an improved aptitude test using a national cohort is recommended as the way forward.
Notes on Contributors
Dr. Sivapalan Sanchayan contributed to the development of the aptitude test, administering the test, collection of data, analysis and writing of the manuscript.
Dr. Sisira Dharmaratne contributed to the conceptualisation, study design, development of the aptitude test, data analysis and writing of the manuscript.
Ms. Shalika Pathirana took part in developing and administering the test, data collection and reviewing the manuscript.
Dr. Pavithra Godamunne contributed to the conceptualisation, study design, development of the aptitude test, data collection, analysis and revision of the manuscript.
Prof. Madawa Chandratilake took part in the conceptualisation, study design, data analysis and revision of the manuscript
Ethical Approval
Ethical clearance (P/223/12/2018) was obtained from the Faculty of Medicine, University of Kelaniya, Sri Lanka.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available to preserve the confidentiality of the participants in this study but are available from the corresponding author on reasonable request.
Acknowledgement
We acknowledge the contribution of Ms. B. N. Jayasena (former lecturer, Department of Disability Studies, Faculty of Medicine, University of Kelaniya) and Ms. L. K. E. Chathurika (former lecturer, Department of Disability Studies, Faculty of Medicine, University of Kelaniya) in the development of the aptitude test. We also acknowledge the contribution of Dr. Rasiah Thayakaran (Research fellow in Health Informatics, Institute of Applied Health Research, University of Birmingham) in performing factor analysis.
Funding
The research received no specific grant from any funding agency.
Declaration of Interest
The authors have no conflicts of interest to disclose.
References
Bala, L., Pedder, S., Sam, A. H., & Brown, C. (2022). Assessing the predictive validity of the UCAT-A systematic review and narrative synthesis. Medical Teacher, 44(4), 401–409. https://doi.org/10.1080/0142159X.2021.1998401
Cohen, L., Manion, L., & Morrison, K. (2018). Research Methods in Education. Routledge.
de Silva, N. R., Pathmeswaran, A., & de Silva, H. J. (2004). Selection of students for admission to a medical school in Sri Lanka. The Ceylon Medical Journal, 49(3), 81–85. https://doi.org/10.4038/cmj.v49i3.3245
de Silva, N. R., Pathmeswaran, A., de Silva, N., Edirisinghe, J. S., Kumarasiri, P. V., Parameswaran, S. V., Seneviratne, R., Warnasuriya, N., & de Silva, H. J. (2006). Admission to medical schools in Sri Lanka: Predictive validity of selection criteria. The Ceylon Medical Journal, 51(1), 17–21. https://doi.org/10.4038/cmj.v51i1.1371
Dharmaratne, S., & Ponnamperuma, G. (2020). Selection for health professions education. In M. Chandratilake & A. Olupeliyawa (Eds.), 14 topics in health professions education (pp. 120–132). College of Medical Educationists, Sri Lanka.
Gliatto, P., Leitman, I. M., & Muller, D. (2016). Scylla and charybdis: The MCAT, USMLE, and degrees of freedom in undergraduate medical education. Academic Medicine, 91(11), 1498–1500. https://journals.lww.com/academicmedicine/Fulltext/ 2016/11000/Scylla_and_Charybdis__The_MCAT,_USMLE,_and_Degrees.16.aspx
Greatrix, R., & Dowell, J. (2020). UKCAT and medical student selection in the UK – what has changed since 2006? BMC Medical Education, 20(1), 1–12. https://doi.org/10.1186/s12909-020-02214-1
Greatrix, R., Nicholson, S., & Anderson, S. (2021). Does the UKCAT predict performance in medical and dental school? A systematic review. BMJ Open, 11, Article e040128. https://doi.org/10.1136/BMJOPEN-2020-040128
Hambleton, R. K., & Zenisky, A. L. (2010). Translating and adapting tests for cross-cultural assessments. In D. Matsumoto, F. J. R. van de Vijver (Eds.), Cross-cultural research methods in psychology (pp. 46–70). Cambridge University Press.
Hewage, S. N., Salgado, L. S. S., Fernando, G. M. O., Liyanage, P., Pathmeswaran, A., & De Silva, N. R. (2011). Selection of medical students in Sri Lanka: Time to re-think criteria? Ceylon Medical Journal, 56(1), 22–28.
MacKenzie, R. K., Cleland, J. A., Ayansina, D., & Nicholson, S. (2016). Does the UKCAT predict performance on exit from medical school? A national cohort study. BMJ Open, 6, Article e011313. https://doi.org/10.1136/BMJOPEN-2016-011313
McManus, I. C., Dewberry, C., Nicholson, S., & Dowell, J. S. (2013). The UKCAT-12 study: Educational attainment, aptitude test performance, demographic and socio-economic contextual factors as predictors of first year outcome in a cross-sectional collaborative study of 12 UK medical schools. BMC Medicine, 11, Article 244. https://doi.org/10.1186/1741-7015-11-244
McManus, I. C., Dewberry, C., Nicholson, S., Dowell, J. S., Woolf, K., & Potts, H. W. W. (2013). Construct-level predictive validity of educational attainment and intellectual aptitude tests in medical student selection: Meta-regression of six UK longitudinal studies. BMC Medicine, 11, Article 243. https://doi.org/10.1186/1741-701 5-11-243
Mettananda, D. S. G., Wickramasinghe, V. P., Kudolugoda Arachchi, J., Lamabadusuriya, S. P., Ajanthan, R., & Kottahachchi, D. (2006). Suitability of selection criteria as a measure of outcome of medical graduates: University of Colombo. The Ceylon Journal of Medical Science 49, 1–12.
Paniagua, M. A., & Swygert, K. A. (2016). Constructing written test questions for the basic and clinical sciences (4th ed.). National Board of Medical Examiners.
Paton, L. W., McManus, I. C., Cheung, K. Y. F., Smith, D. T., & Tiffin, P. A. (2022). Can achievement at medical admission tests predict future performance in postgraduate clinical assessments? A UK-based national cohort study. BMJ Open, 12, Article e056129. https://doi.org/10.1136/bmjopen-2021-056129
Patterson, F., Cousans, F., Edwards, H., Rosselli, A., Nicholson, S., & Wright, B. (2017). The predictive validity of a text-based situational judgment test in undergraduate medical and dental school admissions. Academic Medicine, 92(9), 1250–1253. https://doi.org/10.1097/ACM.0000000000001630
Patterson, F., Roberts, C., Hanson, M. D., Hampe, W., Eva, K., Ponnamperuma, G., Magzoub, M., Tekian, A., & Cleland, J. (2018). 2018 Ottawa consensus statement: Selection and recruitment to the healthcare professions. Medical Teacher, 40(11), 1091–1101. https://doi.org/10.1080/0142159X.2018.149 8589
Powis, D. A., Munro, D., & Bore, M. R. (2021). Is the UCAT appropriate for selecting undergraduate medical students? Medical Journal of Australia, 214(2), 77–78. https://doi.org/10.5694/mja2.50906
Prideaux, D., Roberts, C., Eva, K., Centeno, A., Mccrorie, P., Mcmanus, C., Patterson, F., Powis, D., Tekian, A., & Wilkinson, D. (2011). Assessment for selection for the health care professions and specialty training: Consensus statement and recommendations from the Ottawa 2010 conference. Medical Teacher, 33(3), 215–223. https://doi.org/10.3109/0142159X.2011.551560
Soemantri, D., Karunathilake, I., Yang, J. H., Chang, S. C., Lin, C. H., Nadarajah, V. D., Nishigori, H., Samarasekera, D. D., Lee, S. S., Tanchoco, L. R., & Ponnamperuma, G. (2020). Admission policies and methods at crossroads: A review of medical school admission policies and methods in seven Asian countries. Korean Journal of Medical Education, 32(3), 243–256. https://doi.org/10.3946/KJME.2020.169
Taber, K. S. (2018). The use of Cronbach’s Alpha when developing and reporting research instruments in science education. Research in Science Education, 48(6), 1273–1296. https://doi.org/10.1007/ s11165-016-9602-2
University Grants Commission. (2022). Sri Lanka university statistics 2022. Ministry of Higher Education. https://www.ugc.ac.lk/downloads/statistics/stat_2022/Chapter%202.pdf
University Grants Commission. (2023). Admission to undergraduate courses of the universities in Sri Lanka – 2022/2023. Ministry of Higher Education. https://www.ugc.ac.lk/downloads/admissions/Handbook_2022_23/student_handbook_english.pdf
Zimmermann, S., Klusmann, D., & Hampe, W. (2017). Correcting the predictive validity of a selection test for the effect of indirect range restriction. BMC Medical Education, 17, Article 246. https://doi.org/10.1186/s12909-017-1070-5
*S. Sanchayan
Faculty of Medicine,
University of Jaffna,
Adiyapatham Road,
Kokuvil West, Kokuvil, Sri Lanka
Email: sanch.s6@gmail.com,
sanchayan@univ.jfn.ac.lk
Submitted: 6 May 2024
Accepted: 12 September 2024
Published online: 7 January, TAPS 2025, 10(1), 48-52
https://doi.org/10.29060/TAPS.2025-10-1/SC3349
Craig S. Webster1,2, Antonia Verstappen1, Jennifer M. Weller1 & Marcus A. Henning1
1Centre for Medical and Health Sciences Education, School of Medicine, University of Auckland, Auckland, New Zealand; 2Department of Anaesthesiology, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand
Abstract
Introduction: We aimed to determine the extent to which non-technical skills and attitudes acquired during undergraduate interprofessional simulation in an Advanced Cardiac Life Support (ACLS) course translated into clinical work.
Methods: Following ACLS simulation training for final-year nursing and medical students, we conducted a 1-year follow-up survey, when graduates were in clinical practice. We used the Readiness for Interprofessional Learning Scale (RIPLS – higher scores indicate better attitudes to interprofessional practice), and nine contextual questions with prompts for free-form comments. RIPLS scores underwent repeated-measures between-groups (nurses vs doctors) analysis at three timepoints (pre-course, post-course and 1-year).
Results: Forty-two surveys (58% response) were received, demonstrating translation of non-technical skills and attitudes to clinical practice, including insights into the skills and roles of others, the importance of communication, and improved perceptions of preparedness for clinical work. However, RIPLS scores for doctors decreased significantly upon beginning clinical work, while scores for nurses continued to increase, demonstrating a significant interaction effect (reduction of 5.7 points to 75.7 versus an increase of 1.3 points to 78.1 respectively – ANOVA, F(2,76)=5.827, p=0.004). Responses to contextual questions suggested that reductions in RIPLS scores for doctors were due to a realisation that dealing with emergency life support was only a small part of their practice. However, the prevailing work cultures of nurses and doctors in the workplace may also play a part.
Conclusion: We demonstrated the translation of non-technical skills and attitudes acquired in undergraduate simulation to the clinical workplace. However, results are tempered for junior doctors beginning practice.
Keywords: Work Culture, Translation, RIPLS, Simulation, Advanced Cardiac Life Support, Undergraduate Education, Skills and Attitudes, Patient Safety
I. INTRODUCTION
Preparing undergraduate healthcare students for their future roles in the clinical workplace is a central concern for modern healthcare educators and is of critical importance for the maintenance of adequate healthcare services throughout the world (Barnes et al., 2021). Modern healthcare is inherently multidisciplinary, yet much of the training received by healthcare practitioners remains siloed within professional groups, and this is particularly the case at the undergraduate level. The use of simulation in healthcare has become increasingly important in recent years as a way to offer safe and immersive training. Conducting simulation with interprofessional healthcare teams allows those who will work together to be trained together, and can have the double benefit of promoting the acquisition of technical and non-technical skills in participants, while also allowing insight into the skills, roles and knowledge of other team members from different professional groups (Jowsey et al., 2020).
We previously reported on the development and evaluation of an interprofessional Advanced Cardiac Life Support (ACLS) course for undergraduate nursing and medical students in their final year at the University of Auckland, aimed at increasing technical resuscitation and non-technical teamwork skills (Webster et al., 2018). The evaluation study, using a mixed-methods design and recruiting 69% of the entire year’s student cohort, demonstrated significant improvements in scores on the Readiness for Interprofessional Learning Scale (RIPLS) over the course of the training day, and important interprofessional and attitudinal insights into the skills and knowledge of other team members related to communication, teamwork, leadership, realism, and professional roles. Medical and nursing students both reported that such insights would not have occurred during uniprofessional simulation and felt that the course had better prepared them for work in the clinical context. At the end of the training day we invited participants to take part in a further follow-up survey timed to occur approximately one year later, at a time when participants would typically be working clinically.
Our aim in the present study was to determine the extent to which the non-technical skills and attitudes acquired during the undergraduate interprofessional ACLS simulation course translated into the clinical work of the former course participants.
II. METHODS
We conducted a 1-year follow-up survey comprising a further RIPLS questionnaire and nine additional contextual questions, with quantitative response scales and prompts for explanatory free-form comments (see Supplementary Table 1). The survey was mailed to participants who had elected to supply their contact information, along with a post-paid return envelope. All participants gave written informed consent to participate. One postal and one email reminder was also sent if a reply was not forthcoming.
The RIPLS is a validated questionnaire comprising 19 questions using 5-point Likert response scales (anchors, 1=strongly disagree to 5=strongly agree), and yielding a possible total score from 19 to 95 points where higher scores indicate a greater willingness to engage in interprofessional practice (Parsell & Bligh, 1999). In the present analysis, RIPLS responses from each participant in the 1-year follow-up survey were paired with their own corresponding RIPLS scores at two previous time points and underwent repeated-measures between-groups (nurses vs doctors) analysis at three timepoints (pre-course, post-course and 1-year). Responses to quantitative ratings on contextual questions used identical 5-point Likert scales and were summarised along with exemplar quotations from the free-form comments (Supplementary Table 1).
III. RESULTS
Between August 2014 and November 2015, 42 survey responses were received, representing a 58% response rate from the 73 participants who elected to give contact information for the follow-up survey. Two nurses were not working clinically at the time of the survey, and their responses were excluded from analysis – resulting in a total of 14 nurses and 26 doctors being included in the present study. All doctors were working in hospitals at the time of the 1-year survey, as were 71% of nurses. The remaining nurses were working in primary healthcare or general practice. RIPLS data did not significantly depart from a normal distribution (Shapiro-Wilk test, p=0.22), therefore parametric analysis was conducted using SPSS v.27 (IBM SPSS Statistics, Armonk, New York).
A one-way repeated measures ANOVA demonstrated a significant interaction effect between time point and professional group (F(2, 76)=5.827, p=0.004), demonstrating that at the 1-year time point mean RIPLS scores for doctors fell significantly by 5.7 points, while mean RIPLS scores for nurses continued to increase by 1.3 points (Figure 1).
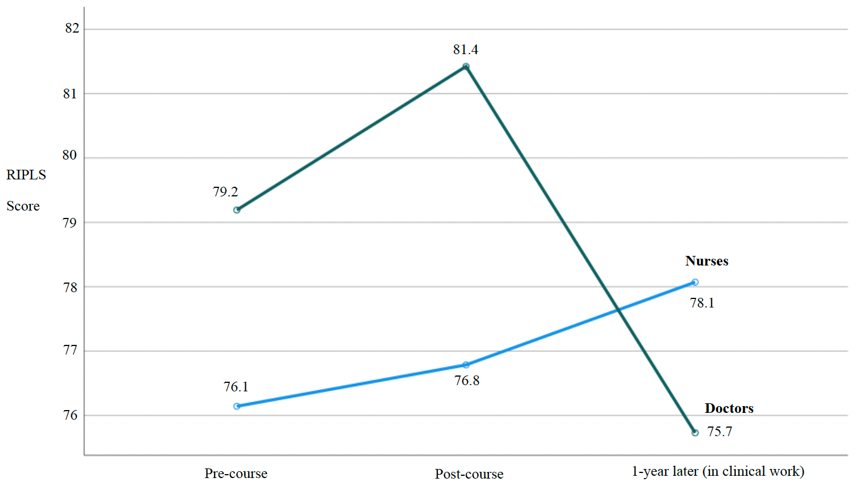
Figure 1. RIPLS scores for nurses and doctors paired over three time points
The results of the contextual questions in the present study (1-year time point) demonstrated strong support by nurses and doctors for the value of the interprofessional ACLS course in general terms and more specifically in terms of feeling part of the team, better understanding the skills and roles of others, and feeling more confident in clinical practice – with all mean responses ranging from high 3’s to >4 (see Supplementary Table 1 for complete summary). Participants strongly agreed that the interprofessional ACLS course should continue to be offered (with an overall mean score of 4.68 out of 5). The single reverse-scored question asking whether ACLS training would have been more effective if conducted uniprofessionally demonstrated strong disagreement with an overall mean score of 1.65. Exemplar quotations from free-form comments provided a context for the quantitative results in terms of demonstrating that the ACLS training better prepared doctors and nurses for emergencies, helped to improve their communication, and was a realistic form of training – for example, stating “Much more ‘real life’ when other professions involved” (doctor) and “Interdisciplinary teamwork is huge in the real world…” (nurse).
Despite the largely positive findings, exemplar quotations also allowed some insight into why doctors’ RIPLS scores were high at the end of the ACLS course, but then fell significantly upon entry into clinical practice at the 1-year time point. Exemplar quotations suggested that once in the clinical workplace junior doctors better appreciated that the technical skills in the ACLS course made up only a small part of their scope of practice, stating that there “are many things… you are unable to do and it is important to know what level of knowledge and ability other individuals may have” and that ACLS “does not make up a large part of my clinical practice” (Supplementary Table 1).
IV. DISCUSSION
Our results demonstrate the translation of non-technical skills and attitudes acquired during undergraduate interprofessional simulation training to the clinical workplace. Our findings show particular benefits for nurses, and reinforce the value of the interprofessional ACLS course as an important part of the undergraduate curriculum. While the overall evaluation of the ACLS course was positive, the differential response in RIPLS scores between nurses and doctors upon entry into the clinical workplace is an intriguing result which clearly warrants further research.
We know of no previous study that has followed the same cohort of undergraduate participants after an interprofessional simulation course up to the point where they have entered the clinical workplace. The ability to pair responses for the same participants across all three time points in our study is a strength, as this avoids the variability that would be present if there were different participants at each time point, and so gives us more confidence in our findings.
Our results suggest that the significant reduction in RIPLS scores upon entry into the clinical workplace for junior doctors may be due to a realisation that the technical skills learnt in the ACLS course make up only a small part of a doctor’s domain of practice. However, recent research into the experiences of junior doctors during interprofessional collaboration suggests that the interaction effect in RIPLS scores across professional groups may also be a consequence of the different work cultures of nurses and doctors. Evidence suggests, including from our own University, that doctors typically believe that they should take individual responsibility for their clinical work, while nurses have a more collective view of patient care (Horsburgh et al., 2006; van Duin et al., 2022). Thus, the prevailing workplace cultures could reinforce and promote nurses’ willingness to work interprofessionally (hence explaining the increase in their RIPLS scores), while for doctors the prevailing individualistic work culture may reduce their willingness to work interprofessionally (hence contributing to the reduction in their RIPLS scores, Figure 1).
Further work to investigate this intriguing interaction effect, and the dynamics of work cultures and professional identity formation, would likely involve mixed-method research, perhaps using observation, interviews or focus groups and quantitative measures such as RIPLS (Jowsey et al., 2020). In addition, such studies conducted with clinicians at various levels of experience within a hospital could potentially yield insight into the state of the prevailing clinical work cultures and may allow some estimate of whether incoming graduates with interprofessional training could change these cultures, and when a critical mass of such graduates may allow this to happen. In the meantime, our results suggest that prevailing work cultures may represent a challenge for interprofessional teamwork initiatives, at least in medicine.
V. CONCLUSION
Our follow-up study demonstrated the translation of the non-technical skills and attitudes acquired during undergraduate interprofessional simulation training to the clinical workplace in terms of insights into the skills and roles of others, the importance of communication, and perceptions of preparedness to deal with emergencies. However, these results appear to be tempered for junior doctors beginning clinical work likely due to realisations around the applicability of ACLS training to their scope of practice and the influences of their prevailing workplace culture.
Notes on Contributors
Craig S. Webster was involved in the conceptualisation of this study, data analysis, writing and revision.
Antonia Verstappen was involved in data collection and analysis, writing and revision.
Jennifer M. Weller was involved in the conceptualisation of this study, writing and revision.
Marcus A. Henning was involved in the writing and revision of this paper.
Ethical Approval
This study was carried out in accordance with all regulations of the host organisation and with the approval of the Human Participants Ethics Committee of the University of Auckland (reference number 9073). All participants gave written informed consent to participate.
Data Availability
The complete data set for this study is openly available on the Figshare repository, https://doi.org/10.6084/m9.figshare.25750230
Funding
This study was conducted without funding.
Declaration of Interest
All authors have no potential conflicts of interest.
References
Barnes, T., Yu, T. W., & Webster, C. S. (2021). Are we preparing medical students for their transition to clinical leaders? A national survey. Medical Science Educator, 31(1), 91-99. https://doi.org/10.1007/s40670-020-01122-9
Horsburgh, M., Perkins, R., Coyle, B., & Degeling, P. (2006). The professional subcultures of students entering medicine, nursing and pharmacy programmes. Journal of Interprofessional Care, 20(4), 425-431. https://doi.org/10.1080/13561820600805233
Jowsey, T., Petersen, L., Mysko, C., Cooper-Ioelu, P., Herbst, P., Webster, C. S., Wearn, A., Marshall, D., Torrie, J., Lin, M. P., Beaver, P., Egan, J., Bacal, K., O’Callaghan, A., & Weller, J. (2020). Performativity, identity formation and professionalism: Ethnographic research to explore student experiences of clinical simulation training. PLoS One, 15(7), e0236085. https://doi.org/10.1371/journal.pone.0236085
Parsell, G., & Bligh, J. (1999). The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Medical Education, 33(2), 95-100. https://doi.org/10.1046/j.1365-2923.1999.00298.x
van Duin, T. S., de Carvalho Filho, M. A., Pype, P. F., Borgmann, S., Olovsson, M. H., Jaarsma, A. D. C., & Versluis, M. A. C. (2022). Junior doctors’ experiences with interprofessional collaboration: Wandering the landscape. Medical Education, 56(4), 418-431. https://doi.org/10.1111/medu.14711
Webster, C. S., Hallett, C., Torrie, J., Verstappen, A., Barrow, M., Moharib, M. M., & Weller, J. M. (2018). Advanced cardiac life support training in interprofessional teams of undergraduate nursing and medical students using mannequin-based simulation. Medical Science Educator, 28(1), 155-163. https://doi.org/10.1007/s40670-017-0523-0
*Craig Webster
Centre for Medical and Health Sciences Education
School of Medicine, University of Auckland
Private Bag 92-019
Auckland 1142, New Zealand.
Email: c.webster@auckland.ac.nz
Submitted: 31 January 2024
Accepted: 3 September 2024
Published online: 7 January, TAPS 2025, 10(1), 56-58
https://doi.org/10.29060/TAPS.2025-10-1/PV3239
Chan Choong Foong1, Mohamad Nabil Mohd Noor1 & Galvin Sim Siang Lin2
1Medical Education and Research Development Unit, Faculty of Medicine, Universiti Malaya, Malaysia; 2Department of Restorative Dentistry, Kulliyyah of Dentistry, International Islamic University Malaysia, Malaysia
I. INTRODUCTION
Contemporary undergraduate medical education is increasingly emphasising the cultivation of student ownership and autonomy, entrusting learners with the responsibility to take charge of their own studies. Across Asian countries, high school graduates embark on their medical education journey at the age of 19 to 20 years, stepping into the realm of adulthood and assuming accountability for their academic pursuits. As the landscape of medical education undergoes transformative shifts propelled by technological advancements and evolving pedagogical approaches, one enduring tradition faces scrutiny: the imposition of compulsory lecture attendance.
Intriguingly, amid the broader trend toward fostering student autonomy, some Asian medical schools grapple with concerns about low lecture attendance. Rather than embracing the prevailing ethos of adult learning, these institutions respond by adopting autocratic measures to enforce mandatory attendance. This perplexing approach begs the question: Why, in an era of educational evolution and empowerment, do certain medical schools resort to rigid mandates to address the issue of diminished lecture participation?
This article does not engage in a debate about the efficacy of lectures; instead, it delves into the heart of the matter — the compulsory attendance. Considering medical teachers’ dissatisfaction with students’ lecture attendance rates, it becomes imperative to explore the underlying frustrations that lead institutions toward autocratic measures. What lies at the core of this apparent contradiction between the shift toward learner autonomy and the persistence of compulsory lecture attendance?
II. THE FRUSTRATIONS AND OUR ARGUMENTS
1. Some medical teachers may argue that frustration lies in the association between lecture attendance and academic performance.
Our arguments are as follows. First, research data show a mixture of supporting and opposing evidence (Doggrell, 2020b). Second, if this association holds true, it implies that high-achieving students should be afforded the freedom to forego lectures. Alternatively, medical students who acquire lecture content from other media, such as recorded lectures or online resources (e.g. YouTube videos), and offline resources (e.g. reference books) should also have the freedom to skip lectures. Third, it appears more rational to correlate academic performance with students’ active engagement during lectures rather than their mere physical attendance. Students who attend lectures to avoid punishment may be reluctant to become involved. Despite their outward presence, if these students remain preoccupied with internet-connected devices, does their mere attendance satisfy the expectations of medical teachers? The scenario becomes even more poignant when considering the time medical teachers spend managing students who are not engaged in lectures. This time could otherwise have been meaningfully invested in students genuinely seeking to absorb and engage with the lecture content.
2. Some medical teachers contend that the crux of the frustration lies within professionalism, positing that attending lectures is an integral aspect of student professionalism.
Our arguments are as follows. First, a systematic review discussing unprofessional behaviours among medical students does not identify lecture attendance as a dimension of professionalism (mak-Van der Vossen et al., 2017). Second, even if one were to categorise lecture absenteeism as unprofessional, the AMEE Guide No. 61, titled “Integrating professionalism into the curriculum”, does not advocate for compulsory attendance as a prescribed professional solution (O’Sullivan et al., 2012).
Some medical teachers draw parallels by likening student absenteeism to the unacceptable conduct of on-duty medical practitioners. However, this analogy lacks validity. The execution of medical duties by practitioners necessitates a specific venue, such as a clinic, and adherence to fixed working hours. In contrast, medical students can fulfil their learning responsibilities at any time and from any location, exemplified by the ability to engage with recorded lectures. For the analogy to be valid, lectures must be proven irreplaceable in delivering certain medical content.
3. Some medical teachers contend that their frustration lies in low lecture attendance, adversely affecting their morale for teaching (Emahiser et al., 2021).
Our arguments are as follows. First, although low attendance can be upsetting and disappointing, medical teachers should not request compulsory attendance to appease their emotional and moral demands. While commenting on student absenteeism as unprofessional, do these teachers, in turn, project a more professional image by demanding mandatory attendance? Second, the variability in audience size for different lectures or lecturers warrants the teachers’ self-reflections on their teaching methods (Emahiser et al., 2021). Third, there is perhaps no downside to the teaching styles employed by medical teachers; however, some medical students have preferences for different learning methods (Emahiser et al., 2021). Alternatively, the characteristics of Generation Z learners, marked by a limited attention span and a preference for online learning environments, may not align with the assumptions underlying compulsory lectures. Mandating attendance presupposes a one-size-fits-all approach, and debatably, lectures might not be the panacea for optimal academic performance among medical students.
4. Some medical teachers may argue that the frustration stems from the perception that many Asian high school leavers are not mature enough to make decisions.
Our central argument posits that, irrespective of the potential benefits of lectures, they should not be mandated. How can medical students cultivate maturity if they are not afforded the opportunity to exercise decision-making in the first place? It is ironic that, while Asian medical schools try to promote adult learning principles into their curriculum, they endorse paternalism in conditioning student behaviours. Our stance is not a discouragement of lecture attendance; rather, we oppose the imposition of paternalism in moulding the physicians of tomorrow.
III. OUR PROPOSALS
To address the challenge of low lecture attendance, our proposal for medical teachers is to reconsider the delivery method of lectures. Let us acknowledge the need for our teaching methods to evolve in response to technological advancements and the distinctive learning preferences of Generation Z. Following is an actual reason for absence – “I don’t consider the lecturer adds to the material given on the PowerPoints” and a reason for attending – “It allows for interaction with course staff and/or students” (Doggrell, 2020a). Thus, it becomes imperative for medical institutions to train educators with interactive strategies (e.g., inquiry activities) that complement lectures and motivate students to actively participate in the learning process. Consequently, faculty development programs that are in line with evolving learning science and the changing needs of learners are deemed necessary.
Next, we should reconsider the emotional need to see students physically. Theoretical and empirical evidence suggests that recorded lectures work effectively, as students can pause and play the recordings, which enables them to learn at their own pace. Medical teachers must accept that, with the tremendous amount of available teaching and learning materials online, attending lectures is no longer the sole source of knowledge. Considering flexible attendance policies that accommodate students’ individual needs and recognising the importance of adapting to evolving educational practices and preferences are equally essential.
For medical students, our suggestion is to foster ownership and autonomy in their studies, predicated on an understanding of the potential repercussions on their academic performance. Medical students should be empowered to make informed choices, cognisant that each choice carries consequences. This approach aligns with the principles observed in medicine, where patients retain the autonomy to continue or discontinue treatment at their own risk. If adult learning is deemed fundamental to the future medical curriculum, Asian medical teachers ought to relinquish paternalistic tendencies.
This shift does not imply a cessation of support for student learning. Instead, we shift to help students “learning to learn”, for instance, to promote the understanding of (including but not limited to) andragogy and self-regulated learning. It may not be the lecture attendance that some low-achieving medical students have missed; rather, it could be the cultivation of appropriate mindsets about learning, including aspects like time management and motivation.
IV. CONCLUSION
In conclusion, our scrutiny of compulsory lecture attendance reveals that it neither serves as a panacea for academic performance nor aligns seamlessly with the principles of professionalism or the preferred learning styles of Generation Z. Rather than acting as an antidote, the imposition of compulsory attendance manifests as a form of paternalism within Asian medical schools. This paternalistic approach, rather than nurturing, acts as a toxic element for aspiring medical professionals, hindering the cultivation of autonomy and adult learning principles in the trajectory of futuristic medical education. To remedy this issue, delivery method of lectures should consider state-of-the-art learning science, matched with the changing needs of students.
Notes on Contributors
Chan Choong Foong conceptualised and designed the work, and drafted the manuscript. Mohamad Nabil Mohd Noor conceptualised and designed the work, and drafted the manuscript. Galvin Sim Siang Lin interpreted the findings from past studies for the work, and revised the manuscript critically. All authors have read and approved the submitted manuscript.
Funding
The authors did not receive support from any organisation for the submitted work.
Declaration of Interest
The author declares that there is no conflict of interest.
References
Doggrell, S. A. (2020a). No apparent association between lecture attendance or accessing lecture recordings and academic outcomes in a medical laboratory science course. BMC Medical Education, 20, Article 207. https://doi.org/10.1186/s12909-020-02066-9
Doggrell, S. (2020b). A systematic review of the relationship between lecture attendance and academic outcomes for students studying the human biosciences. International Journal of Innovation in Science and Mathematics Education, 28(1), 60-76. https://doi.org/10.30722/IJISME.28.01.005
Emahiser, J., Nguyen, J., Vanier, C., & Sadik, A. (2021). Study of live lecture attendance, student perceptions and expectations. Medical Science Educator, 31, 697-707. https://doi.org/10.1007/s40670-021-01236-8
Mak-van Der Vossen, M., van Mook, W., van Der Burgt, S., Kors, J., Ket, J. C., Croiset, G., & Kusurkar, R. (2017). Descriptors for unprofessional behaviours of medical students: A systematic review and categorisation. BMC Medical Education, 17, Article 164. https://doi.org/10.1186/s12909-017-0997-x
O’Sullivan, H., van Mook, W., Fewtrell, R., & Wass, V. (2012). Integrating professionalism into the curriculum: AMEE Guide No. 61. Medical Teacher, 34(2), e64-e77. https://doi.org/10.3109/0142159X.2012.655610
*Chan Choong Foong
Medical Education and Research Development Unit,
Faculty of Medicine, Universiti Malaya,
50603 Kuala Lumpur, Malaysia
Email: foongchanchoong@um.edu.my
Submitted: 6 May 2024
Accepted: 23 September 2024
Published online: 7 January, TAPS 2025, 10(1), 59-61
https://doi.org/10.29060/TAPS.2025-10-1/CS3339
Kye Mon Min Swe1, Amit Bhardwaj2 & Hnin Pwint Phyu3
1School of Medicine, Newcastle University Medicine Malaysia, Malaysia; 2Department of Orthopaedics, Sengkang General Hospital, Singapore; 3M Kandiah Faculty of Medical and Health Science, University Tunku Abdul Rahman, Malaysia
I. INTRODUCTION
Telemedicine is defined as delivering healthcare services across distances using telecommunication technology (Waseh & Dicker, 2019). It helps ensure continuity of care for vulnerable patients to address the unique demands on our health system, especially in times of crisis, such as the COVID-19 pandemic, via virtual follow-up. It is also helpful in engaging medical students in training and patient care (Aron et al., 2020).
During the pandemic, virtual follow-up (VF) home visits were introduced in the integrated family medicine curriculum for Year 4 students. The family medicine curriculum for Year 4 students highlights the significance of comprehending chronic illnesses within the broader framework of the patient’s family and environment via the Follow-up Study of Patients with Chronic Illnesses programme, traditionally conducted through in-person patient visits. This study investigated the challenges faced while conducting virtual follow-up (VF) patient visits amidst the COVID-19 pandemic.
II. METHODS
A cross-sectional study was conducted via online survey questionnaires upon completing the family medicine posting. The online feedback questionnaires were used to explore the challenges of virtual follow-up (VF) via open-ended questionnaires. All participants were duly informed about the study and obtained their consent. The ethical approval was obtained from the Scientific Ethical Review Committee of the University Tunku Abdul Rahman.
III. RESULTS
In this study, among 49 students from year 4 MBBS, 47 year-four medical students participated in the research, and all the students were aged between 20-24. The students were grouped into 18 groups for VF home visits, each containing 2-3 students. A total of 18 chronic illness patients were virtually followed during the COVID-19 pandemic. The challenges and benefits faced by the students during virtual patient follow-up visits were explored via the open-ended questions and shown in Table 1.
|
Challenges |
|
I. Challenges related to follow-up consultation. “Patient refused to have clerked, and we had to clerk family members instead.” “Difficult to obtain updates on the patient’s condition.” “Not really interactive, more like a Q&A session.” “Difficult to express concern for the patient over video conferencing too.” “Cannot observe patient hard to assess patient current condition, hard to assess patient current condition.” “Unable to assess patient’s full motor function through video call as we could not perform physical examination.” “Difficult to access the physical environment.” “Cannot know the patient’s living condition.” |
|
II. Challenges in making appointments with the patients. “Patient didn’t pick up the phone; Patient was not very responsive.” “We could not contact her sometimes.” “Patient no reply to my text, the patient refuses to have a virtual call, and it is hard to conduct the visit.” “The patient kept postponing the virtual visit, and it was difficult to arrange a time with the patient.” |
|
III. Challenges related to technical problems. “The unclear or low video call quality during the virtual follow-up” “We can listen to the patients clearly, but the image or the video was not that clear.” “Blur voice call” “Patient is unable to use video calls such as WhatsApp calls.” “Difficulty arranging a virtual visit with the elderly patient as he is unfamiliar with the gadgets.” “Difficulty in video calling patient as she doesn’t know how to use WhatsApp video or other social platforms.” “Patient does not have access to a smartphone.” |
|
Benefits |
|
I. The benefit of a virtual follow-up visit “It’s a new experience”. “Convenient” “Time is more flexible.” “No need to travel, less travelling and saving cost” “Virtual home visit has reduced risk of transmission.” |
|
II. The benefit of a follow-up visit to a patient with chronic illness. “Teamwork makes working easier and enjoyable.” “Teamwork helped us plan and conduct virtual home visits before the deadline.” “I learnt the importance of home visits.” “Patient is a better teacher than the textbook”. “Delightful, enjoyed learning other people’s culture.” “Learnt interacting with the patient, sharing information with the patient.” “Learnt about real-life follow-up with patients who are not compliant with medical treatment.” |
Table 1. The Challenges and Benefits When Conducting Virtual Follow-up Home Visits
IV. DISCUSSION
Although the experiences of VF visits are challenging, medical students found the experiences valuable. The students found the importance of VF for chronic illness, which made them aware of the challenges and benefits of telemedicine. The challenges were similar to the studies from literature, such as technological difficulties, lack of familiarity with telehealth platforms, lack of access to internet or devices and sufficient internet connection speed, especially with patients with low socioeconomic status, which hinder effective communication and assessment. Moreover, patients with physical, cognitive, and language disabilities may find it hard to use the technology. Another challenge was the inability to perform an in-person clinical examination, and the students found less confidence in evaluating patient conditions through a screen, which impacted the quality of care delivered (Cheng et al., 2022; Pathipati et al., 2016).
To overcome these challenges, it is essential to provide comprehensive training focused on telehealth skills to familiarise students with virtual platforms and their functionalities. Additionally, implementing a mentorship programme or clinical attachment with telehealth practitioners guiding medical students during VF visits can foster confidence and communication skills. Encouraging regular feedback sessions will allow students to improve their techniques and address specific concerns in real-time.
As medical education shifts toward integrating telehealth, understanding the challenges students encounter is essential in preparing the next generation of healthcare professionals. The study identified a range of challenges, including technological barriers, such as unfamiliarity with telemedicine platforms, as well as issues related to patient engagement and communication. Medical students reported difficulties building rapport with patients, which is essential for effective follow-up, and expressed concerns regarding their ability to conduct comprehensive assessments virtually.
By documenting these challenges, this study contributes to the existing literature by highlighting medical students’ specific hurdles in the VF context. While experiencing the challenges, the VF visits allowed students exposed to various acute and chronic patient cases to learn about a holistic approach to managing chronic illness, work with teamwork, and have the opportunity to communicate with the patient and their family members. (Cheng et al., 2022; Iancu et al., 2020).
The findings inform educators and curriculum developers of the need for enhanced training programmes focusing on telehealth competencies. Physical follow-up visits have resumed following the pandemic, and a hybrid approach has been embraced to nurture telemedicine concepts and overcome challenges. It recommended medical institutions integrate telemedicine into curricula, ensuring today’s students are prepared for the evolving landscape of medical practice.
V. CONCLUSION
In conclusion, challenges exist in conducting virtual follow-up visits for chronic illness patients, targeting educational strategies to mitigate these difficulties. By equipping medical students with the necessary skills and support, healthcare institutions can enhance the effectiveness of virtual follow-ups, ultimately improving patient care and outcomes in a digital healthcare environment.
Notes on Contributors
Dr Kye is the corresponding author for this paper. She designed the study, analysed the data, and prepared the manuscript, working with the co-author.
Dr Amit and Dr Hnin contributed substantially to the final manuscript’s design, editing and preparation.
Ethical Approval
The research study was approved by Universiti Tunku Abdul Rahman Scientific and Ethical Review Committee on 20th April 2021 (Approval number: UTAR/SERC/92/2021).
Acknowledgement
We would like to acknowledge the Year 4 medical students of UTAR (Academic Year 2020/2021) for voluntary participation in this study.
Funding
There was no funding for this research study.
Declaration of Interest
The authors declare no conflicts of interest, including financial, consultant, institutional or other relationships.
References
Aron, J. A., Bulteel, A. J. B., Clayman, K. A., Cornett, J. A., Filtz, K., Heneghan, L., Hubbell, K. T., Huff, R., Richter, A. J., Yu, K., & Weil, H. F. (2020). A role for telemedicine in medical education during the COVID-19 pandemic. Academic Medicine, 95(11), e4-e5. https://doi.org/10.1097/ACM.0000000000003572
Cheng, C., Humphreys, H., & Kane, B. (2022). Transition to telehealth: Engaging medical students in telemedicine healthcare delivery. Irish Journal of Medical Science, 191, 2405-2422. https://doi.org/10.1007/s11845-021-02720-1
Iancu, A. M., Kemp, M. T., & Alam, H. B. (2020). Unmuting medical students’ education: Utilizing telemedicine during the COVID-19 pandemic and beyond. Journal of Medical Internet Research, 22(7), e19667. https://doi.org/10.2196/19667
Pathipati, A. S., Azad, T. D., & Jethwani, K. (2016). Telemedical education: Training digital natives in telemedicine. Journal of Medical Internet Research, 18(7), e193. https://doi.org/10.2196/ jmir.5534
Waseh, S., & Dicker, A. P. (2019). Telemedicine training in undergraduate medical education: Mixed methods review. JMIR Medical Education, 5(1), e12515. https://doi.org/10.2196/12515
*Dr Kye Mon Min Swe
Newcastle University Medicine Malaysia,
No 1, Jalan Sarjana 1,
Kota Ilmu, Educity@Iskandar,
Nusajaya, 79200, Johor, Malaysia
601115133799
Email: drkyemonfms@gmail.com
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.
- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.
- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









