Using simulation and inter-professional education to teach infection prevention during resuscitation
Submitted: 21 February 2020
Accepted: 13 July 2020
Published online: 5 January, TAPS 2021, 6(1), 93-108
https://doi.org/10.29060/TAPS.2021-6-1/OA2229
Kah Wei Tan1, Hwee Kuan Ong2 & Un Sam Mok3
1Ministry of Health Holdings, Singapore; 2Department of Physiotherapy, Singapore General Hospital, Singapore; 3Division of Anaesthesiology and Peri-operative Medicine, Singapore General Hospital, Singapore
Abstract
Introduction: During resuscitations, healthcare professionals (HCPs) find balancing the need for timely resuscitation and adherence to infection prevention (IP) measures difficult. This study explored the effects of an innovative teaching method, using in-situ simulation and inter-professional education to enhance compliance to IP through better inter-professional collaboration.
Methods: The study was conducted in the Surgical Intensive Care Unit (SICU) in a 1200-beds teaching hospital. HCPs working in the SICU were conveniently allocated to the intervention or control group based on their work roster. The intervention group attended an in-situ simulated scenario on managing cardiac arrest in an infectious patient. The control group completed the standard institution-wide infection control eLearning module. Outcomes measured were: (a) attitudes towards inter-professional teamwork [TeamSTEPPS Teamwork Attitudes Questionnaire (TAQ)], (b) infection prevention knowledge test, (c) self-evaluated confidence in dealing with infectious patients and (d) intensive care unit (ICU) audits on infection prevention compliance during actual resuscitations.
Results: 40 HCPs were recruited. 29 responded (71%) to the pre- and post-workshop questionnaires. There were no significant differences in the TeamSTEPPS TAQ and infection prevention knowledge score between the groups. However, ICU audits demonstrated a 60% improvement in IP compliance for endotracheal tube insertion and 50% improvement in parenteral medication administration. This may be attributed to the debriefing session where IP staff shared useful tips on compliance to IP measures during resuscitation and identified threats that could deter IP compliance in SICU.
Conclusion: Learning infection prevention through simulated inter-professional education (IPE) workshops may lead to increased IP compliance in clinical settings.
Keywords: Inter-Professional Education, Simulation Infection Control, Resuscitation, Inter-Professional Teamwork
Practice Highlights
- Use of a simulated scenario to improve infection prevention during resuscitation.
- Improving attitudes towards inter-professional collaboration amongst healthcare professionals.
- Evaluating the efficacy of a simulated scenario through clinical audit.
I. INTRODUCTION
Adherence to infection prevention is paramount in the intensive care unit (ICU) as hospital acquired infections in the critically ill are associated with increased morbidity, mortality, length of stay and healthcare cost (Gandra & Ellison, 2014). However, during resuscitations, healthcare professionals (HCPs) may experience difficulty in balancing the need for resuscitation and adherence to infection prevention guidelines, resulting in suboptimal compliance to basic infection prevention measures (Steinemann et al., 2016). Moreover, resuscitation is a time-critical endeavour that requires good collaboration in a team comprising of different HCPs fulfilling different roles with different priorities, and lapses in teamwork may arise in a team comprising of HCPs with different roles and priorities (Barr, Koppel, Reeves, Hammick, & Freeth, 2009).
Inter-professional education (IPE) is defined as “occasions when two or more professions learn with, from and about each other to improve collaboration and quality of care” by the Centre for Advancement of Interprofessional Education (CAIPE) (Steinert, 2005). It is known to improve patient safety through improving communication, understanding and knowledge to encourage active participation from different HCPs (Oandasan, 2007; Wong, Lee, Allen, & Foong, 2020). Research has shown that active collaboration amongst HCPs in the workplace resulted in improved patient outcomes and provider satisfaction (Wagner, Parker, Mavis, & Smith, 2011). Previous studies had investigated the outcomes of using IPE workshops to teach infection prevention in non-emergency clinical settings or using standardised patients, and concluded that knowledge and confidence in infection prevention and inter-professional teamwork had improved (Mundell, Kennedy, Szostek, & Cook, 2013).
Currently, infection prevention education in our institute is didactic and web-based. Although this method is effective in disseminating information, there are no opportunities to learn with different HCPs or apply knowledge to real-life scenarios. On the basis that resuscitation is traditionally taught using simulation and has been proven to be highly effective (Perkins, 2007), we developed an IPE simulation workshop on infection prevention during resuscitation.
We hypothesised that the in-situ simulation workshop involving different HCPs will result in improved attitudes towards inter-professional teamwork and improved compliance to infection prevention guidelines, compared to our standard institutional infection control (IC) education.
II. METHODS
A. Study Population
We conducted a non-randomised experimental study amongst HCPs working in the Surgical Intensive Care Unit (SICU) of the Singapore General Hospital (SGH). All HCPs working in the SICU were eligible to participate in the study. There were no exclusion criteria. Informed consent was obtained from all participating HCPs. Information on participants’ profession, the year they obtained their professional qualification, the number of years they had worked in critical care and prior experience in simulation training were collected. HCPs from Anaesthesiology, Nursing, Physiotherapy, Pharmacy, Speech and Language Therapy, Dietetics and Infection Prevention were involved. A working day was picked to run the workshop and HCPs on duty that day were allocated to the intervention group, while those there were not on duty were assigned to the control group.
B. In-Situ Simulation Workshop
Participants in the intervention group (n=25) underwent a two-hour in-situ simulation workshop in the SICU on the scenario of a cardiac arrest in an infectious patient (Annex A). The training faculty comprised of HCPs from various professions such as Anaesthesiology, Nursing, Physiotherapy, Pharmacy, Speech and Language Therapy, Dietetics and Infection Prevention. Each workshop consisted of HCPs from five to seven different professions. The learning outcomes of the workshop were (i) to practice infection prevention precautions for transmission-based infections during resuscitations and (ii) to improve attitudes towards inter-professional teamwork during a crisis situation.
The workshop was designed based on Kolb’s experiential learning theory (Kolb & Fry, 1975), which is a four-stage learning cycle consisting of (i) concrete experience, (ii) reflective observation, (iii) abstract conceptualisation and (iv) active experimentation. Concrete experience was facilitated through in-situ simulation where participants experienced real-life constraints of resuscitating an infectious patient. Following the simulation, a debrief was held by the faculty that facilitated reflective observation and abstract conceptualisation. Learning points discussed include (i) issues faced in adhering to infection prevention guidelines in a resuscitation setting, (ii) inter-professional teamwork and (iii) threats that could deter IC compliance in SICU. The final stage, active experimentation, was facilitated through actual application of learning points surmised from the workshop, and evaluated through real-time ICU audits.
C. Evaluation of Outcomes
Evaluation of the effectiveness and impact of the workshop was done in accordance with Kirkpatrick’s evaluation framework (Kirkpatrick, 1994), which emphasised the need to go beyond the immediate reactions of participants by assessing them on four different levels, which are (i) Reaction, (ii) Learning, (iii) Behaviour and (iv) Results. “Reaction” was evaluated through the post-workshop questionnaire and participants’ responses in the post-workshop debrief with regards to the effectiveness of simulated workshops in improving inter-professional teamwork and encouraging compliance to infection prevention guidelines. The second level, “Learning”, was evaluated by discussing learning points of the workshop in the debrief, and getting participants to note down their most important takeaways regarding infection prevention and IPE in the post-workshop questionnaire. “Behavioural changes” were assessed through a real-time observational study that assessed participants’ ability to observe proper infection prevention practices during actual resuscitations in the SICU. Results, the fourth level, were difficult to evaluate due to the small sample size that we recruited.
D. Outcomes of Study
There are two primary outcomes of this study: (i) attitudes towards inter-professional teamwork and (ii) infection prevention knowledge and practices.
Changes in attitudes towards inter-professional teamwork were assessed using the TeamSTEPPS Teamwork Attitudes Questionnaire (TAQ 1.0), based on scores in the following subcategories; Team Structure, Leadership, Situation Monitoring, Mutual Support and Communication (Appendix 1). Qualitative comments on key learning points with regards to teamwork were also collected during the debriefing sessions.
Changes in infection prevention knowledge and practice were assessed in five ways:
- An infection prevention self-evaluation questionnaire on a 5-point Likert Scale (Appendix 2).
- A multiple-choice quiz developed by the Institutional Infection Prevention Nurse Educators (Appendix 3A and 3B).
- Questionnaire on effectiveness of the simulation (for participants in the intervention group only) (Appendix 4).
- Qualitative feedback on the learning points concerning infection prevention. (Appendix 5).
- Clinical audit data that evaluated compliance to infection prevention guidelines during resuscitations in the SICU. Two months after the simulation workshop, the data was collected by a trained hospital-based infection prevention team based on real-time observations. The audit checklist assessed proper use of personal protective equipment (PPE), hand hygiene, administration of parenteral medications and insertion of endotracheal tube (ETT).
Statistical analysis was performed using SPSS for Mac, Version 20.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were analysed using the t-test, and categorical variables were analysed using the Fisher and Chi square test. A p-value of less than 0.05 was taken to be statistically significant.
III. RESULTS
The study recruited a total of 40 HCPs. Of the 40 clinical staff working in the SICU asked to rank their responses, 29 (71%) responded to the pre- and post-workshop TAQ, self-evaluation of infection prevention knowledge and infection prevention knowledge quiz. Healthcare professions represented included doctors (31%), nurses (34%), pharmacists (10%), physiotherapists (10%), speech and language therapists (10%) and dieticians (3%).
The intervention and control groups were not significantly different in terms of the number of years post-graduation, years of working experience in critical care and the number of simulated training sessions they have attended, excluding basic cardiac life support (BCLS) and advanced cardiac life support (ACLS). Similarly, there were no significant differences in self-evaluation of infection prevention knowledge and infection prevention scores at baseline. However, we noted significantly higher scores in the control group in Team Structure (mean difference=2.76), Leadership (mean difference =3.8), and Communication (mean difference=2.54; Table 1).
|
|
Intervention [Range] (n=16) |
Control [Range] (n=13) |
P-value |
|
|
Mean no. of years since graduation |
8.65 [4-23] |
8.67 [5-20] |
0.996 |
|
|
Mean no. of years in critical care |
3.78 [0-10] |
5.13 [0-15] |
0.413 |
|
|
Mean no. of prior simulation training sessions (excluding BCLS/ACLS) |
1.52 [0-15] |
2.33 [0-12] |
0.474 |
|
|
Self-evaluation of infection prevention knowledge |
13.3 [10-20] |
14.6 [8-19] |
0.179 |
|
|
Infection prevention baseline MCQ scores |
5.47 [5-6] |
5.78 [5-6] |
0.103 |
|
|
TeamSTEPPS Teamwork Attitudes Questionnaire 2.0 |
||||
|
|
Team Structure |
23.04 [19-30] |
25.80 [20-30] |
0.046* |
|
Leadership |
24.13 [18-29] |
27.93 [21-30] |
0.009* |
|
|
Situation Monitoring |
23.43 [20-30] |
25.73 [21-30] |
0.100 |
|
|
Mutual Support |
18.91 [15-26] |
19.33 [15-27] |
0.678 |
|
|
Communication |
22.39 [19-29] |
24.93 [20-30] |
0.042* |
|
Table 1. Baseline characteristics of the Intervention and Control groups
A. Inter-Professional Teamwork
Within the intervention group, there were no significant changes between pre- and post-workshop TeamSTEPPS TAQ scores in most subcategories, with the exception of an improvement in post-workshop Mutual Support scores (mean difference=3.21), which translated to a 17.0% increase from baseline (Table 2). The lack of a significant change in most subcategories could possibly be due to the already high baseline scores prior to the workshop.
|
|
Pre-workshop mean (SD) [Range] (n=16) |
Post-workshop mean (SD) [Range] (n=16) |
Mean difference |
P-value |
Percentage increase/% |
|
Self-evaluation of infection prevention knowledge |
13.57 (3.32) [10-20] |
14.71 (1.90) [9-19] |
1.14 |
0.230 |
8.4 |
|
Infection prevention quiz scores |
5.85 (0.38) [5-6] |
4.85 (0.69) [4-6] |
-1.00 |
0.000 |
-17.1 |
|
Team Structure |
24.14 (2.69) [19-30] |
25.36 (2.50) [21-30] |
1.22 |
0.058 |
5.1 |
|
Leadership |
25.64 (2.76) [18-30] |
25.9 (2.55) [24-30] |
0.26 |
0.780 |
1.0 |
|
Situation Monitoring |
24.71 (3.29) [18-30] |
25.36 (3.10) [24-30] |
0.65 |
0.272 |
2.6 |
|
Mutual Support |
18.93 (2.43) [18-30] |
22.14 (2.03) [18-28] |
3.21 |
0.002 |
17.0 |
|
Communication |
23.43 (2.56) [20-30] |
23.86 (2.45) [22-30] |
0.43 |
0.551 |
1.8
|
Table 2. Comparison of pre- and post-workshop scores within the intervention group
The intervention group also had greater percentage increases in the TAQ 2.0 Team Structure, Leadership and Communication sub-categories compared to the control group (Table 3).
|
|
Intervention (n=16) |
Control (n=13) |
P-value |
||
|
|
Mean change (SD) |
Percentage change/% |
Mean change (SD) |
Percentage change/% |
|
|
Change in scores for self-evaluation of infection prevention knowledge |
1.14 (3.39) |
8.4 |
0.78 (0.97) |
5.2 |
0.758 |
|
Change in infection prevention scores |
-1.00 (0.71) |
-17.1 |
-1.63 (1.19) |
-29.0 |
0.145 |
|
Change in scores for Team Structure |
0.42 (1.86) |
5.1 |
0.67 (1.45) |
1.3 |
0.661 |
|
Change in scores for Leadership |
-0.42 (2.35)
|
1.0 |
-0.09 (1.38) |
-3.1 |
0.693 |
|
Change in scores for Situation Monitoring |
1.00 (2.00) |
2.6 |
0.27 (1.35) |
2.6 |
0.323 |
|
Change in scores for Mutual Support |
4.33 (2.19) |
17.0 |
3.18 (3.82) |
25.3 |
0.380 |
|
Change in scores for Communication |
0.33 (3.17) |
1.8 |
0.45 (2.34) |
1.4 |
0.919 |
Table 3. Comparison of changes in pre- and post-workshop scores between the Intervention and Control groups
The most common learning point for IPE was the importance of learning the different roles and capabilities that different HCPs can play and the need to involve other HCPs to ensure an effective resuscitation effort. The learning points listed support change in perceptions related to interprofessional roles that the quantitative scale did not capture.
“The workshop improves knowledge of the roles that other healthcare professionals are able to perform, for example, a physiotherapist being qualified to help in CPR during resuscitation.”
(Nursing participant, ID 16)
B. Infection Prevention Knowledge and Practices
Although there were no statistically significant differences between the groups, better infection prevention scores were noted in the intervention group. The intervention group had a percentage increase of 3.2% (8.4% vs 5.2%) in self-evaluated infection prevention knowledge. The questions on infection prevention knowledge were supposed to be of similar difficulty, and we avoided repeating the same set of questions, as we did not want participants to discuss or look up the answers. For both groups, there was a decrease in infection prevention knowledge scores post-workshop; however, there was a smaller decrease in the intervention group (-17.1%) compared to the control group (-29.0%) (Table 3). We speculate that this may be due to the post-workshop questions being more difficult compared to the pre-workshop questions. Another reason that may have contributed to the decrease in scores is the limited number of questions (n=6), which may have confounded our results.
The participants shared a rich diversity of infection prevention learning points during the debrief session. Examples included correct steps in the donning of personal protective equipment, strategies to clean the intravenous (IV) injection hub quickly and effectively, and identification of threats that deterred proper infection prevention compliance during the simulation such as the lack of a disposable dish on the resuscitation trolley to keep intravenous drugs and intubation equipment clean. The most common learning point for infection prevention was the importance of adhering to infection prevention practices during resuscitation such as the accurate administration of parenteral medications. The learning points listed support change in perceptions related to interprofessional roles that the quantitative scale did not capture.
“The importance of practicing infection prevention measures such as the need for changing soiled gloves in between administering parenteral medications, but yet not compromising on resuscitation.”
(Physiotherapist, ID 8)
The clinical audit conducted after the simulation workshop showed that compliance rates in accurate parenteral medication administration improved by 50%, while compliance rates in ETT insertion improved by 60% post-workshop, compared to pre-workshop performance (Table 4).
|
|
Pre-workshop |
Post-workshop |
Percentage change in compliance rates/% |
||
|
|
Number of instances of compliance |
Number of instances of non-compliance |
Number of instances of compliance |
Number of instances of non-compliance |
|
|
PPE |
24 (100%) |
0 (0%) |
24 (96%) |
1 (4%) |
-4 |
|
Hand hygiene |
10 (100%) |
0 (0%) |
2 (100%) |
0 (0%) |
0 |
|
Parenteral medication administration |
6 (50%) |
6 (50%) |
9 (100%) |
0 (0%) |
50 |
|
ETT insertion |
2 (40%) |
3 (60%) |
10 (100%) |
0 (0%) |
60 |
Table 4. Comparison of compliance rates to infection prevention during real-time resuscitations pre- and post-workshop
IV. DISCUSSION
The study was designed, conducted and written before the COVID-19 pandemic. Since the pandemic, there had been some changes in infection prevention guidelines in aerosol general procedures such as tracheal intubation (Perkins, et al., 2020), which was not reflected in our study. Our study had highlighted the importance of using simulation and inter-professional collaboration to enhance infection prevention education, and these were also emphasised in many publications regarding infection prevention during the pandemic (Wong, et al., 2020). For example, there had been recommendations of using a buddy system for PPE donning and doffing, and using high fidelity simulation to prepare for the COVID-19 crisis (Bricknell, Hodgetts, Beaton, & McCourt, 2016). However, many of these publications were reviews and opinions rather than research studies (Foong, et al., 2020; Lim, Wong, Teo, & Ho, 2020).
To our knowledge, there are no publications on the use of in-situ simulation to teach infection prevention during resuscitations in an IPE setting. Current literature evaluating the impact of simulated IPE workshops in teaching infection prevention had mixed results with regards to the effectiveness of such workshops in improving attitudes towards inter-professional teamwork and enhancing compliance rates to infection prevention practices. In the study by Luctkar-Flude et al. (2016), there was significant improvement in infection prevention knowledge, but little change in inter-professional teamwork. Although knowledge related to aseptic technique improved significantly immediately post-workshop, long-term retention was poorer (Wagner, et al., 2011).
A. The Utility of Simulation in Improving Infection Prevention
Our results from the clinical audit conducted during actual resuscitations in the SICU demonstrated a large improvement after the workshop in accurate parenteral medication administration and ETT insertion. This finding supports the hypothesis that an inter-professional simulated workshop is more effective than traditional didactic web-based methods in improving adherence to infection prevention practices, which could be due to three added elements present in simulated workshops.
Firstly, simulation provides interaction amongst different HCPs and enables collaborative learning in small groups (Dolmans, Michaelsen, van Merriënboer, & van der Vleuten, 2015). Secondly, the debriefing process promotes reflective learning and provides real-time feedback (Ziv, Wolpe, Small, & Glick, 2003). Thirdly, the learning is contextualized as participants learn infection prevention principles that are embedded in authentic clinical scenarios, and simulated cardiac arrest in an infectious patient is a common scenario that reflects the reality of practice (Morison & Jenkins, 2007).
Simulation also enables participants to discover innovative solutions, thereby enabling optimal adherence to infection prevention protocols while ensuring a timely resuscitation response with limited manpower. An example of one of the interesting solutions discussed include the designation of specific roles during resuscitation, such as assigning one HCP to be in charge of the airway and another to be in charge of administering intravenous drugs so as to avoid contamination.
B. Encouraging Inter-Professional Teamwork Through Simulation
Simulated scenarios with a focus on IPE also encourage active engagement and collaboration amongst participants, which had been demonstrated to result in improved attitudes towards teamwork (Huitt, Killins, & Brooks, 2015). During the debriefing process, study investigators facilitated the discussion to allow HCPs from different specialties to give feedback and volunteer information on how they could better contribute to the resuscitation effort and work more cohesively as a team, thereby enabling HCPs to discover more about the capabilities of their fellow colleagues. This discussion helps to create a sense of shared purpose within teams (Freytag, Stroben, Hautz, Eisenmann, & Kammer, 2017), which is a defining characteristic of an effective team (Drinka & Clark, 2000), and also reinforces the idea that a team can often achieve what an individual cannot.
In our debriefing, the participants noted the importance of learning the different roles and capabilities that different HCPs can play and the need to involve other HCPs to ensure an effective resuscitation effort, which can subsequently translate to a positive change in patient care and collaborative practice (Hammick, Freeth, Koppel, Reeves, & Barr, 2007). For example, the nursing and medical participants did not realise that physiotherapists, pharmacists and speech and language therapists are BCLS trained and can perform effective chest compression, and the medical participants did not realise nurses can perform cardiac defibrillation during a cardiac arrest. Better collaboration and understanding of other HCPs’ roles can improve task delegation to fully maximise available manpower, and aids in crisis resource management.
C. Debriefing–An Essential Component of a Simulated Workshop
According to the experiential learning style theory (Kolb & Fry, 1975), reflective practice is an integral component that allows learners to fully integrate the learning experience. It allows HCPs to transit from merely experiencing the simulation to deriving critical learning points (Savoldelli, et al., 2006), as constructive discussion and feedback allow participants to better understand potential areas of improvement and reinforces proper infection prevention practice (Gerolemou, et al., 2014). The importance of feedback and discussion is aptly demonstrated in our study, with participants noting that accurate parenteral medication administration was one of their main takeaways from the debriefing process, and there being a subsequent 50% improvement in parenteral medication administration in our observational study.
An effective debriefing process was facilitated through the creation of a non-threatening environment by using open-ended questions, positive reinforcement, constructive feedback and active engagement of all HCPs present (Fanning & Gaba, 2007). While there are many debriefing tools present such as the Organ Specific Autoimmune Disease (OSAD) debriefing tool (Ahmed, et al., 2012), and Advocacy Inquiry (Gururaja, Yang, Paige, & Chauvin, 2008), we believe that the cornerstone of a successful debrief is through the creation of an environment that allows participants to freely voice their queries and concerns, and subsequent discussion to tease out relevant learning points that serve as important takeaway messages.
D. Other Observations
Interestingly, we noted significant differences in Team Structure and Leadership between the Intervention and Control groups in the pre-test questionnaire. This could be due to difference in number of years that the intervention and control groups have worked in SICU, with the intervention group having worked a mean number of 3.78 years compared to the control group’s 5.13 years, although this difference was not statistically significant. Studies have shown that HCPs who have worked together for longer periods of time and on a daily basis are more likely to develop trust and confidence in their teams (Bosch & Mansell, 2015). Less-experienced healthcare staff may feel more uncomfortable with inter-professional teamwork compared to more experienced staff, further highlighting the importance of increasing exposure to IPE for younger HCPs.
E. Challenges Encountered in the Implementation of a Simulated Infection Prevention IPE Workshop
The conception and organisation of an infection control workshop that incorporates both simulation and IPE improved our understanding of existing challenges to the development of a coherent curriculum and implementation of simulated workshops (Buckley, et al., 2012). There were numerous challenges encountered in the implementation of such workshops.
Examples include:
- Simulated workshops are resource intensive. Monthly faculty meetings were held for five months before the workshop, and each workshop required the presence of a HCP from at least five different specialties. In addition, beds in the SICU had to be specially set aside for the workshop to take place.
- Learning outcomes had to be crafted carefully to ensure that all HCPs could benefit from an effective IPE session.
- Faculty development was crucial and the faculty was trained to ensure that the post-simulation debriefing could take place effectively and learning outcomes were met.
- Scheduling conflicts were encountered as implementation of the workshop required HCPs with different work schedules to be present at the same time.
The effectiveness of the workshop could be better evaluated with multiple SICU audits of resuscitations pre- and post-workshop, as this would truly demonstrate translation of learning to real-life practice. However, it is difficult to coordinate logistically. Whenever a real-time resuscitation in the SICU occurred, our hospital-based infection prevention team had to be mobilised within a few minutes without advanced notice to the SICU to conduct the audit on infection prevention compliance during resuscitation, which proved to be challenging.
Nevertheless, these challenges can be resolved if HCPs are strongly committed to better healthcare and our study showed that it is possible to overcome the above-mentioned challenges (Byakika-Kibwika, et al., 2015). We hope that our experience would help shed light on future barriers to implementation of similar in-situ simulated IPE workshops.
F. Plans for the Future
Our study showed that simulation IPE workshops encouraged mutual support amongst different HCPs and improved infection prevention practices during resuscitation. However, implementation of the workshop was costlier and more labour intensive compared to current online video infection prevention education. Currently, we now run in-situ simulations in SICU every month on crisis resource management, and infection prevention is one of the important learning outcomes.
This workshop was conducted before the COVID-19 pandemic and there was no limitation on the maximum number of participants. In the future, with the SICU roster having changed to shift work, the workshop will only be conducted amongst HCPs within a particular shift to avoid cross-contamination with other shifts. A larger debrief room may be needed to allow for social distancing as well.
G. Limitations of our study
Limitations of our study include the small sample size, making it difficult to draw generalisations, as the study cannot show any statistically significant difference when comparing the control and intervention groups even though positive trends were observed. Furthermore, longer follow-up is required to evaluate long-term changes in behaviour, attitudes and retention of knowledge.
V. CONCLUSION
Our study showed that learning infection prevention through simulated IPE workshops is an innovative way to teach infection prevention and may lead to increased infection prevention compliance in clinical settings, as demonstrated by the clinical audit conducted. In light of the ongoing COVID-19 pandemic, use of a simulated scenario may help enhance infection prevention practices to limit the spread of transmission-based infections. Simulation may also help improve attitudes towards inter-professional teamwork and collaboration, which are crucial in resuscitations.
Notes on Contributors
Kah Wei Tan is a Medical Officer working with Ministry of Health Holdings (MOHH). Kah Wei Tan performed data collection and data analysis, reviewed the literature and wrote the manuscript.
Hwee Kuan Ong is a Senior Principal Physiotherapist in the Department of Physiotherapy, Singapore General Hospital. Hwee Kuan Ong performed data collection and data analysis and wrote the manuscript.
May Un Sam Mok is a Senior Consultant in the Division of Anaesthesiology and Peri-operative Medicine, Singapore General Hospital. May Un Sam Mok developed the methodological framework for the study, designed the study, reviewed the literature and wrote the manuscript.
Ethical Approval
The study is approved by SingHealth Centralised Institutional Review Board (CIRB reference: 2016/3001).
Acknowledgement
We would like to acknowledge the SICU staff for providing assistance in conducting the survey.
Funding
Funding was obtained from the Academic Medicine Education Institute (AMEI) grant.
Declaration of Interest
There is no conflict of interest to declare.
References
Ahmed, M., Sevdalis, N., Paige, J., Paragi-Gururaja, R., Nestel, D., & Arora, S. (2012). Identifying best practice guidelines for debriefing in surgery: A tri-continental study. American Journal of Surgery, 203(4), 523-529.
Barr, H., Koppel, I., Reeves, S., Hammick, M., & Freeth, D. (2009). Effective Interprofessional Education: Arguments, Assumption & Evidence. Oxford: Blackwell.
Bosch, B., & Mansell, H. (2015). Interprofessional collaboration in health care: Lessons to be learned from competitive sports. Canadian Pharmacists Journal, 148(4), 176-179.
Bricknell, M., Hodgetts, T., Beaton, K., & McCourt, A. (2016). Operation GRITROCK: The defence medical services’ story and emerging lessons from supporting the UK response to the Ebola crisis. Journal of the Royal Army Medical Corps, 162(3), 169-175.
Buckley, S., Hensman, M., Thomas, S., Dudley, R., Nevin, G., & Coleman, J. (2012). Developing interprofessional simulation in the undergraduate setting: Experience with five different professional groups. Journal of Interprofessional Care, 26(5), 362-369.
Byakika-Kibwika, P., Kutesa, A., Baingana, R., Muhumuza, C., Kitutu, F. E., Mwesigwa, C., … Sewankambo, N. K. (2015). A situation analysis of inter‑professional education and practice for ethics and professionalism training at Makerere University College of Health Sciences. BMC Research Notes, 8, 598.
Dolmans, D., Michaelsen, L., van Merriënboer, J., & van der Vleuten, C. (2015). Should we choose between problem-based learning and team-based learning? No, combine the best of both worlds! Medical Teacher, 37(4), 354-359.
Drinka, T. J. K., & Clark, P. G. (2000). Health Care Teamwork: Interdisciplinary Practice and Teaching. Westport, CT: Auburn House.
Fanning, R. M., & Gaba, D. M. (2007). The role of debriefing in simulation-based learning. Simulation in Healthcare: Journal of the Society for Simulation in Healthcare, 2(2), 115-125.
Foong, T. W., Ng, E. S. H., Khoo, C. Y. W., Ashokka, B., Khoo, D., & Agrawal, R. (2020). Rapid training of healthcare staff for protected cardiopulmonary resuscitation in the COVID-19 Pandemic. British Journal of Anaesthesia, 125(2), e257–e259.
Freytag, F., Stroben, F., Hautz, W. E., Eisenmann, D., & Kammer, J. E. (2017). Improving patient safety through better teamwork: How effective are different methods of simulation debriefing? Protocol for a pragmatic, prospective and randomised dtudy. (2017). BMJ Open, 7(6), e015977.
Gandra, S., & Ellison, R. T. (2014). Modern trends in infection control practices in intensive care units. Journal of Intensive Care Medicine, 29(6), 311-326.
Gerolemou, L., Fidellaga, A., Rose, K., Cooper, S., Venturanza, M., Aqeel, A., … Khouli, S. (2014). Simulation-based training for nurses in sterile techniques during central vein catheterization. American Journal of Critical Care, 23(1), 40-48.
Gururaja, R. P., Yang, T., Paige, J. T., & Chauvin, S. W. (2008). Examining the Effectiveness of Debriefing at the Point of Care in Simulation-Based Operating Room Team Training. Rockville, MD: Agency for Healthcare Research and Quality (US).
Hammick, M., Freeth, D., Koppel, I., Reeves, S., & Barr, H. (2007). A best evidence systematic review of interprofessional education: BEME Guide no. 9. Medical Teacher, 29(8), 735-751.
Huitt, T. W., Killins, A., & Brooks, W. S. (2015). Team-based learning in the gross anatomy laboratory improves academic performance and students’ attitudes toward teamwork. Anatomical Sciences Education, 8(2), 95-103.
Kirkpatrick, D. L. (1994). Evaluation Training Programs: The Four Levels. San Francisco: Berrett-Koehler.
Kolb, D. A., & Fry, R. E. (1975). Toward an Applied Theory of Experiential Learning. New York: John Wiley & Sons.
Lim, W. Y., Wong, P., Teo, L., & Ho, V. K. (2020). Resuscitation during the COVID-19 pandemic: Lessons learnt from high-fidelity simulation. Resuscitation, 152, 89-90.
Luctkar-Flude, M., Hopkins-Rosseel, D., Jones-Hiscock, C., Pulling, C., Gauthier, J., Knapp, A., … Brown, C. (2016). Interprofessional infection control education using standardized patients for nursing, medical and physiotherapy students. Journal of Interprofessional Education and Practice, 2, 25-31.
Morison, S., & Jenkins, J. (2007). Sustained effects of interprofessional shared learning on student attitudes to communication and team working depend on shared learning opportunities on clinical placement as well as in the classroom. Medical Teacher, 29(5), 464-470.
Mundell, W. C., Kennedy, C. C., Szostek, J. H., & Cook, D. A. (2013). Simulation technology for resuscitation training: A systematic review and meta-analysis. Resuscitation, 84(9), 1174-1183.
Oandasan, I. (2007). Teamwork and healthy workplaces: Strengthening the links for deliberation and action through research and policy. HealthcarePapers, 7, 98-103.
Perkins, G. D. (2007). Simulation in resuscitation training. Resuscitation, 73(2), 202-211
Perkins, G. D., Morley, P. T., Nolan, J. P., Soar, J., Berg, K., Olasveengen, T., … Neumar, R. (2020). International Liaison Committee on Resuscitation: COVID-19 consensus on science, treatment recommendations and task force insights. Resuscitation, 151, 145-147.
Savoldelli, G. L., Nalik, V. N., Park, J., Joo, H. S., Chow, R., & Hamstra, S. J. (2006). Value of debriefing during simulated crisis management: oral versus video-assisted oral feedback. Anesthesiology, 105(2), 279-285.
Steinemann, S., Kurosawa, G., Wei, A., Ho, N., Lim, E., Suares, G., … Berg, B. (2016). Role confusion and self-assessment in interprofessional trauma teams. The American Journal of Surgery, 211(2), 482-488.
Steinert, Y. (2005). Learning together to teach together: Interprofessional education and faculty development. Journal of Interprofessional Care, 19(Suppl 1), 60-75.
Wagner, P. D., Parker, C. J., Mavis, B. E., & Smith, M. K. (2011). An interdisciplinary infection control education intervention: Necessary but not sufficient. The Journal of Graduate Medical Education, 3(2), 203-210.
Wong, J., Goh, Q. Y., Tan, Z., Lie, S. A., Tay, Y. C., Ng, S. Y., … Soh, C. R. (2020). Preparing for a COVID-19 pandemic: A review of operating room outbreak response measures in a large tertiary hospital in Singapore. Canadian Journal of Anesthesia, 67, 732-745.
Wong, M. L., Lee, T. W. O., Allen, P. F., & Foong, K. W. C. (2020). Dental education in Singapore: A journey of 90 years and beyond. The Asia Pacific Scholar, 5(1), 3-7.
Ziv, A., Wolpe, P. R., Small, S. D., & Glick, S. (2003). Simulation-based medical education: an ethical imperative. Simulation in Healthcare Journal of the Society for Simulation in Healthcare, 78(8), 783-788.
*Kah Wei Tan
1 Maritime Square,
#11-25 HarbourFront Centre,
Singapore 099253
Email address: kahwei.tan@mohh.com.sg
Submitted: 2 April 2020
Accepted: 3 June 2020
Published online: 5 January, TAPS 2021, 6(1), 109-113
https://doi.org/10.29060/TAPS.2021-6-1/SC2243
Wen Hao Chen1, Shairah Radzi1, Li Qi Chiu2, Wai Yee Yeong3, Sreenivasulu Reddy Mogali1
1Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore; 2Department of Emergency Medicine, Tan Tock Seng Hospital, Singapore; 3Singapore Centre for 3D Printing, School of Mechanical and Aerospace Engineering, Nanyang Technological University, Singapore
Abstract
Introduction: Simulation-based training has become a popular tool for chest tube training, but existing training modalities face inherent limitations. Cadaveric and animal models are limited by access and cost, while commercial models are often too costly for widespread use. Hence, medical educators seek a new modality for simulation-based instruction. 3D printing has seen growing applications in medicine, owing to its advantages in recreating anatomical detail using readily available medical images.
Methods: Anonymised computer tomography data of a patient’s thorax was processed using modelling software to create a printable model. Compared to a previous study, 3D printing was applied extensively to this task trainer. A mixture of fused deposition modelling and material jetting technology allowed us to introduce superior haptics while keeping costs low. Given material limitations, the chest wall thickness was reduced to preserve the ease of incision and dissection.
Results: The complete thoracostomy task trainer costs approximately SGD$130 (or USD$97), which is significantly cheaper compared to the average commercial task trainer. It requires approximately 118 hours of print time. The complete task trainer simulates the consistencies of ribs, intercostal muscles and skin.
Conclusion: By utilising multiple 3D printing technologies, this paper aims to outline an improved methodology to produce a 3D printed chest tube simulator. An accurate evaluation can only be carried out after we improve on the anatomical fidelity of this prototype. A 3D printed task trainer has great potential to provide sustainable simulation-based education in the future.
Keywords: Medical Education, Chest Tube, Thoracostomy, Simulation, 3D Printing
I. INTRODUCTION
Training opportunities in procedures such as chest tube insertions are increasingly limited amidst a growing population of trainees. Yet, the deliberate practice remains essential to improving proficiency and preventing possible complications such as lung parenchymal damage (Hernandez, El Khatib, Prokop, Zielinski, & Aho, 2018). Hence, many institutions have adopted simulation-based training to provide realistic training opportunities while mitigating harm to patients.
Cadaveric and animal models are limited by access and cost, and raise religious and ethical concerns (Kovacs, Levitan, & Sandeski, 2018). In addition, commercial models tend to be very costly (e.g. Trauma-Man® at USD~$25,000). As such, new modalities are desired.
Three-dimensional (3D) printing can accurately recreate anatomical details from imaging data through precision modelling and a wide range of compatible printing materials (Mogali et al., 2018). Together with its decreasing cost, it has become an attractive technology for creating inexpensive and anatomically accurate simulation modalities.
A previous study from the Federal University of Parana, Brazil (Bettega et al., 2019) outlined the development and evaluation of a low-cost chest tube simulator. The bony structures were 3D printed, while the remainder of the model was manually assembled using silicone sheets, foam pads, and balloons.
They compared 2 groups of participants using a porcine rib model, and their 3D printed simulator respectively. They found subjective improvements in confidence and safety amongst both groups and showed no difference between the objective grades. Hence, they concluded that their 3D printed simulator was equivalent to the animal model concerning the simulation of a chest tube placement.
However, there exist many other 3D printing technologies and materials, which can potentially be applied to create superior haptics and anatomical detail. Hence, this paper aims to outline a methodology of integrating multiple 3D printing modalities to create a cost-efficient 3D printed chest tube simulator.
II. METHODS
An anonymised computerized tomography (CT) file of a healthy human thorax (2.5 mm slices thickness) in Digital Communication in Medicine (DICOM) format was downloaded from the databank provided by 3D Slicer (https://www.slicer.org/, Version 4.10.2). The CT data was available freely for research and educational use at the time of this study.
3D Slicer was employed to segment the thoracic bony structures using a radiodensity based threshold algorithm, which traces the bone based on the Hounsfield units. Due to a lack of contrast possibly from the poor resolution of the CT images, we were not able to segment the respective soft tissue layers using thresholding. Hence, the intercostal muscles were manually drawn with the paintbrush function. Intrathoracic organs were all removed to create a central cavity. From initial experimentation, we found that incision and dissection were too difficult to perform if the task trainer was printed at the true thoracic thickness. Hence, a decision was made to thin out the chest wall. At the 4th and 5th intercostal space midaxillary line, the mean chest wall thickness is 39mm (Laan et al., 2016), but our model measured at 18mm at this corresponding anatomical landmark.
Further processing was done to smoothen the contours of the model (see Appendix, A). Subsequently, the anatomical structures were saved as stereolithography (STL) file and exported into Materialise Magics (Version 20 by Materialise, Belgium).
On Magics, cut and Boolean techniques were used to create the replaceable component. This space was demarcated by the 5th to 6th intercostal space, between anterior axillary to the mid axillary line. To create a secure fit for the replaceable piece, a groove was created and reinforced using the cut and punch function which generates teething to maximise friction. The main frame measured 23cm (length) x 19.5cm (width) x 23.5cm (height), while the replaceable part measured 9cm (length x 8.1cm (width) x 0.8cm (height). The Fix Wizard and Shrink Wrap Part functions were used to repair the surface mesh and eliminate holes and loose shells. The models were then exported using IdeaMaker® (Raise3D, USA) and uploaded to the printer.
The model was printed in two parts: the main frame was printed using fusion deposition modelling (FDM). This technology extrudes a continuous filament of melted thermoplastic, repeated by layer based on the design coordinates. Bones were printed with polylactic acid (PLA) which is a rigid material while the intercostal muscles were printed with thermoplastic urethane (TPU) which is a flexible material. Support was printed using PLA. We utilised a dual nozzle extrusion printer (Raise3D Pro 2, Raise3D, USA) to allow us to print the bony and soft tissue simultaneously, thereby increasing convenience. The following settings were used: printing speeds were reduced to 25mm/s, retraction of the TPU extrusion head was disabled, nozzle temperatures were set at 200°C, and build plate temperature was at 65°C. Post-print processing was done to remove the support, with subsequent filing and sanding.
The replaceable part was printed using Objet500 Connex 3 (Stratasys Ltd, Eden Prairie, MN), a multi-material printer utilising material jetting technology. This technology drops liquid photopolymers onto the build tray and simultaneously cures the material using UV light. As such, we can mix plastic and rubber to create hybrid consistencies (Mogali et al., 2018) of varying shore hardness. Two materials were selected to achieve the desired haptics: VeroWhite (FullCure, RGD835) was the stiff plastic photopolymer used for bones, while Tango Plus (FullCure, 930) was the rubber photopolymer used for simulating soft tissue. Support resin (FullCure, 706) was also used for printing. Post-printing processing was required to remove the support resin.
Skin coloured silicone sheets of 5 mm thickness were wrapped around the model using generic superglue. The task trainer was cable tied to stainless steel supports and screwed onto a laminated wood baseplate. Cut sponges were wrapped in duct tape to simulate the lung parenchyma and placed into the central cavity created.
III. RESULTS
The completed task trainer is shown in Figure 1. Both the main frame and replaceable piece provided simulation for the ribs, intercostal muscles, and skin.
The 3D thoracostomy task trainer costs approximately SGD$130 (or USD$97) (excluding manpower and printer cost)–see Appendix, B). The baseplate and mount were repurposed and did not add to costs.
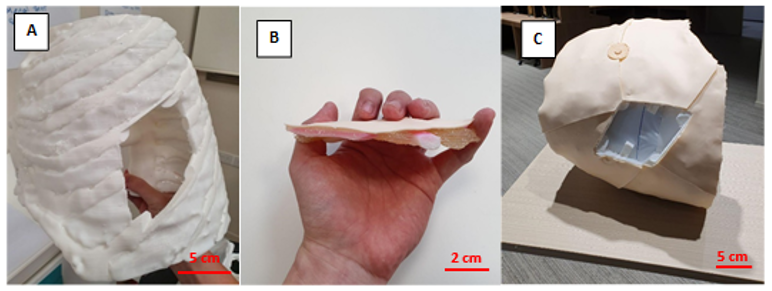
Note. A = completed hemithorax main frame using FDM printing; B= replaceable piece; C = task trainer without the replaceable piece. Figure 1. Photos of the completed task trainer
The main frame required 676g of polylactic acid and 114g of thermoplastic urethane. The replaceable piece required 30g of VeroWhite, 22g of Tango Plus, and 66g of Support706. It took a total of approximately 118 hours to print the entire task trainer.
IV. DISCUSSION
Our methodology addressed several issues with the model as outlined by the Brazilian team (Bettega et al., 2019). The proposed methodology here required less manual assembly of components, thereby saving time and improving fabrication. By utilising dual extrusion printing, construction was simplified while integrating an additional material for varying consistencies. The creation of a replaceable piece also meant long term savings in the cost of utilising this model. These logistical advantages would make it easier to adopt our proposed task trainer.
Secondly, simple materials such as foam pads and silicone sheets were inferior in simulating human tissue. Our utilisation of material jetting technology with the Objet500 Connex 3 (Stratasys Ltd, Eden Prairie, MN) printer allowed us to blend plastic and rubber materials to better recreate the consistency of human tissue. This technology and blend of materials have been extensively validated in other simulation models (Mogali et al., 2018).
Cost remains an important impedance to the widespread use of simulation in procedural education. We performed a surface comparison of our product against an existing commercial model in use by a local hospital in Singapore (LF03770U by Lifeform, NASCO, USA). The task trainer outlined here (~USD$97) is significantly cheaper than the commercial trainer (~USD$1,800). Also, our material blend provides superior haptics and bony structures in the replaceable component, as compared to a plain silicone insert in the Lifeform model. These should provide improvements in the quality and quantity of simulation opportunities for training physicians.
Unfortunately, we were not able to recreate the anatomical thickness of the thorax given our material limitations at the time of writing. This inaccurate depth of dissection creates a confounding variable when evaluating our task trainer against existing cadaveric or commercial simulators. Hence, an evaluation of this task trainer was withheld to address this limitation in our future prototype. Moving forward, we plan to invite physicians to validate the efficacy of our improved task trainer.
V. CONCLUSION
We have outlined the methodology for creating a 3D printed tube thoracostomy task trainer using a combination of printing technologies. The outlined task trainer could potentially provide superior haptics at a lower cost while improving fabrication. However, an equitable validation against an existing modality of simulation can only be done after we achieve a comparable anatomical fidelity.
In our continued search for sustainable simulation models, 3D printing shows great potential in reproducing anatomical detail with superior cost efficiency. The growing availability of 3D printing infrastructure makes the large-scale adoption of such task trainers ever more realistic. It makes it therefore worthwhile to invest in the creation of the perfect 3D printed task trainer.
Notes on Contributors
Mr. Wen Hao Chen is an undergraduate medical student with the Lee Kong Chian School of Medicine, Singapore. He was involved in the development of the task trainer, along with co-authoring the submitted manuscript.
Dr. Shairah Radzi is a research fellow with the Lee Kong Chian School of Medicine, Singapore. She was involved in the development of the task trainer, along with co-authoring the submitted manuscript.
Dr. Li Qi Chiu is a consultant physician in the Department of Emergency Medicine in Tan Tock Seng Hospital, Singapore. She was involved in the development of the task trainer, along with co-authoring the submitted manuscript.
Assoc. Prof Wai Yee Yeong is the Associate Chair (Students) of the School of Mechanical and Aerospace Engineering, Nanyang Technological University, Singapore. She was involved in the development of the task trainer, providing her technical expertise on the 3D printing process, along with co-authoring the submitted manuscript.
Asst. Prof Sreenivasulu Reddy Mogali is the Head of Anatomy and Principal Investigator in Clinical Anatomy and Medical Education at Lee Kong Chian School of Medicine, Singapore. He was involved in the development of the task trainer, along with co-authoring the submitted manuscript. He serves as the principal investigator.
Ethical Approval
Approved by Nanyang Technological University’s Institutional Review Board (2019-07-017). The CT scans used were anonymised and provided free for education and research use by 3D Slicer (https://www.slicer.org/, Version 4.10.2).
Acknowledgement
The authors thank the staff and faculty of the Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore for supporting this research; Singapore Centre for 3D Printing, Nanyang Technological University for their technical support.
Funding
This project was funded by the Ministry of Education Research Start-Up Grant, Lee Kong Chian School of Medicine, Nanyang Technological University Singapore.
Declaration of Interest
All authors declare no conflict of interest. The authors alone are responsible for the content and writing of the article.
References
Bettega, A. L., Brunello, L. F. S., Nazar, G. A., De-Luca, G. Y. E., Sarquis, L. M., Wiederkehr, H. de A., … Pimentel, S. K. (2019). Chest tube simulator: Development of low-cost model for training of physicians and medical students. Revista Do Colégio Brasileiro de Cirurgiões, 46(1). https://doi.org/10.1590/0100-6991e-20192011
Hernandez, M. C., El Khatib, M., Prokop, L., Zielinski, M. D., & Aho, J. M. (2018). Complications in Tube Thoracostomy: Systematic review and Meta-analysis. The Journal of Trauma and Acute Care Surgery, 85(2), 410–416. https://doi.org/10.1097/TA.0000000000001840
Kovacs, G., Levitan, R., & Sandeski, R. (2018). Clinical Cadavers as a Simulation Resource for Procedural Learning. AEM Education and Training, 2(3), 239–247. https://doi.org/10.1002/aet2.10103
Laan, D. V., Vu, T. D. N., Thiels, C. A., Pandian, T. K., Schiller, H. J., Murad, M. H., & Aho, J. M. (2016). Chest Wall Thickness and Decompression Failure: A Systematic Review and Meta-analysis Comparing Anatomic Locations in Needle Thoracostomy. Injury, 47(4), 797–804. https://doi.org/10.1016/j.injury.2015.11.045
Mogali, S. R., Yeong, W. Y., Tan, H. K. J., Tan, G. J. S., Abrahams, P. H., Zary, N., … Ferenczi, M. A. (2018). Evaluation by medical students of the educational value of multi-material and multi-colored three-dimensional printed models of the upper limb for anatomical education. Anatomical Sciences Education, 11(1), 54–64. https://doi.org/10.1002/ase.1703
*Sreenivasulu Reddy Mogali
11 Mandalay Road, Singapore 308232
Lee Kong Chian School of Medicine,
Nanyang Technological University
Email: sreenivasulu.reddy@ntu.edu.sg
Submitted: 17 April 2020
Accepted: 05 August 2020
Published online: 5 January, TAPS 2021, 6(1), 114-118
https://doi.org/10.29060/TAPS.2021-6-1/SC2358
Warren Fong1,3,4, Yu Heng Kwan2, Sungwon Yoon2, Jie Kie Phang1, Julian Thumboo1,2,4 & Swee Cheng Ng1
1Department of Rheumatology and Immunology, Singapore General Hospital, Singapore; 2Programme in Health Services and Systems Research, Duke-NUS Medical School, Singapore; 3Duke-NUS Medical School, Singapore; 4Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: This study aimed to examine the perception of faculty on the relevance, feasibility and comprehensiveness of the Professionalism Mini Evaluation Exercise (P-MEX) in the assessment of medical professionalism in residency programmes in an Asian postgraduate training centre.
Methods: Cross-sectional survey data was collected from faculty in 33 residency programmes. Items were deemed to be relevant to assessment of medical professionalism when at least 80% of the faculty gave a rating of ≥8 on a 0-10 numerical rating scale (0 representing not relevant, 10 representing very relevant). Feedback regarding the feasibility and comprehensiveness of the P-MEX assessment was also collected from the faculty through open-ended questions.
Results: In total, 555 faculty from 33 residency programmes participated in the survey. Of the 21 items in the P-MEX, 17 items were deemed to be relevant. For the remaining four items ‘maintained appropriate appearance’, ‘extended his/herself to meet patient needs’, ‘solicited feedback’, and ‘advocated on behalf of a patient’, the percentage of faculty who gave a rating of ≥8 was 78%, 75%, 74%, and 69% respectively. Of the 333 respondents to the open-ended question on feasibility, 34% (n=113) felt that there were too many questions in the P-MEX. Faculty also reported that assessments about ‘collegiality’ and ‘communication with empathy’ were missing in the current P-MEX.
Conclusion: The P-MEX is relevant and feasible for assessment of medical professionalism. There may be a need for greater emphasis on the assessment of collegiality and empathetic communication in the P-MEX.
Keywords: Professionalism, Singapore, Survey, Assessment
I. INTRODUCTION
Medical professionalism is one of the core Accreditation Council for Graduate Medical Education competencies and forms the basis of medicine’s contract with society. Unprofessional behaviour during training of junior doctors has been shown to result in future unprofessional behaviour. Assessment of professionalism not only allows for timely feedback to residents to help them improve, but also allows for development of better curriculum to prevent lapses in medical professionalism. The Professionalism Mini-Evaluation Exercise (P-MEX) had previously been identified as a potential observer-based assessment tool (Kwan et al., 2018), but it has not been validated in a multi-ethnic and multi-cultural Asian context such as Singapore. According to International Ottawa Conference Working Group on the Assessment of Professionalism, professionalism varies across cultural contexts, and therefore cross-cultural validation of the assessment tool for medical professionalism is imperative (Hodges et al., 2011). The current assessment tools adopted in local institutions may not cover the entire continuum of medical professionalism. For example, in the Ministry of Health Holdings (MOHH) C1 form which is currently being used for the assessment of residents on a 6-monthly basis, the assessment of professionalism is summative and consists of only three items (1) Accepts responsibility and follows through on tasks, (2) Responds to patient’s unique characteristics and needs equitably, (3) Demonstrates integrity and ethical behaviour.
We aimed to (1) examine faculty perception of the relevance of the P-MEX for assessment of medical professionalism in the local context, and (2) determine the feasibility and comprehensiveness of the P-MEX as an assessment tool for medical professionalism in Singapore.
II. METHODS
A. Design and Participants
We invited faculty in the SingHealth residency programmes to participate in the study by completing an online anonymous questionnaire in July 2018 to August 2018. Participants were given one week to complete the survey, with three reminder emails sent at one-week, two-weeks and one-month after the deadline for submission. SingHealth Centralised Institutional Review Board approved the conduct of this study (Reference Number: 2016/3009). Implied informed consent was provided by participants before completing the online anonymous questionnaire.
B. Survey Questionnaire
The P-MEX consists of four domains (Doctor-patient relationship skills, Reflective skills, Time management and Inter-professional relationship skills) and 21 sub-domains. Faculty were asked to rate the relevance of each item in P-MEX using a 0-10 numerical rating scale (0 representing not relevant, 10 representing very relevant). The faculty were also asked the following open-ended questions to determine the feasibility and comprehensiveness of the P-MEX- (1) “In your opinion, is a P-MEX form with 21 items too long, making it not feasible for routine use? If so, which items should be removed?” and (2) “In your opinion, are there any missing items (observable actions of a medical professional) that should be included in this form? If so, what new items should be added?” The questionnaire also included additional questions related to demographic characteristics (age, gender, specialty and number of years since becoming a specialist).
C. Analysis
Items were deemed to be relevant to the assessment of medical professionalism when at least 80% of the faculty gave a rating of ≥8. This was determined by expert judgement and prior literature (Avouac et al., 2011). For the open-ended questions on feasibility and comprehensiveness, responses were categorised and the number of the respondents who deemed the 21-item P-MEX to be not feasible (too long) or not comprehensive (there were missing items that should be included) are presented.
III. RESULTS
In total, 555 faculty from 33 residency programmes participated in the survey (response rate 44%). The respondents were 59% male, median age 43 years old, age ranged from 30 to 78 years old. Specialists from medical and surgical disciplines made up 39% and 27% of the respondents respectively, with the remaining respondents coming from diagnostic radiology/nuclear medicine, anaesthesiology, paediatrics and emergency medicine (12%, 11%, 6% and 5% of the respondents respectively).
A. Relevance
Of the 21 items in P-MEX, 17 items were deemed to be relevant (at least 80% of the faculty gave a rating of ≥8). For the remaining four items ‘maintained appropriate appearance’, ‘extended his/herself to meet patient needs’, ‘solicited feedback’, and ‘advocated on behalf of a patient’, the percentage of faculty who gave a rating of ≥8 was 78%, 75%, 74%, and 69% respectively (Figure 1).
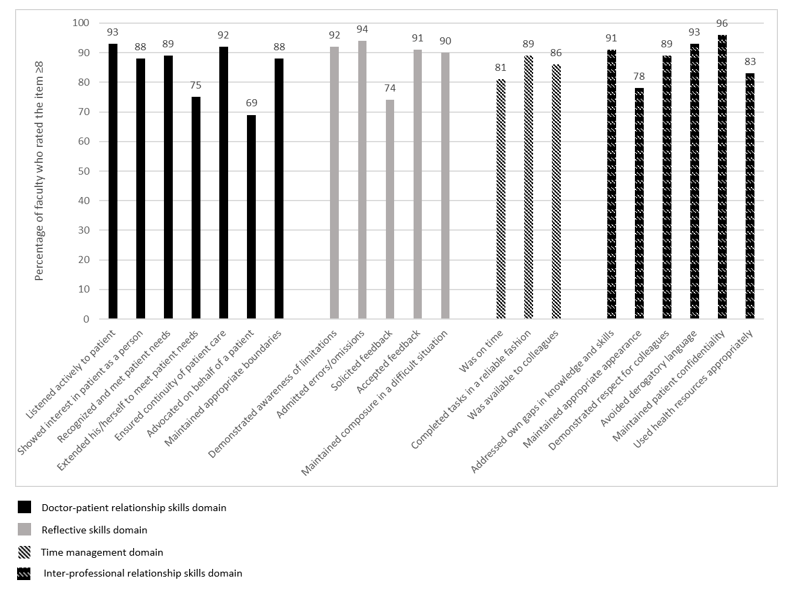
Figure 1: Percentage of faculty (n=555) who rated the item ≥8 on the relevance of the item in assessment of medical professionalism using a 0-10 numerical rating scale (0 representing not relevant, 10 representing very relevant).
B. Feasibility
There were 333 respondents for the question “In your opinion, is a P-MEX form with 21 items too long, making it not feasible for routine use? If so, which items should be removed?”, of which 34% (n=113) felt that there were too many questions in the P-MEX assessment form. The top four items chosen to be removed were “solicited feedback” (n=36), “extended his/herself to meet patient needs” (n=27), “advocated on behalf of a patient” (n=25), and “maintained appropriate appearance” (n=23). 208 (62%) respondents felt that the number of questions in the P-MEX assessment form was appropriate.
C. Comprehensiveness
There were 307 respondents to the question “In your opinion, are there any missing items (observable actions of a medical professional) that should be included in this form? If so, what new items should be added?”, of which 28% (n=85) faculty felt that there were missing items. The most frequently mentioned missing items were regarding assessment of ‘collegiality’ (n=54) and assessment of ‘communication with empathy’ (n=12).
Examples of ‘collegiality’ provided by faculty— “Collaboration with other healthcare professionals in the patients’ best interest”, “Demonstration of collaborative behaviour”
Examples of ‘communication with empathy ‘provided by faculty— “Communicate with empathy and effectively to patient and family, taking into account their level of understanding, education and socioeconomic background”, “Communication skills…should embrace empathy, listening skills, discretion, sensitivity and intelligence… sufficient information, counselling, planning and advice regarding medical condition and options.”
207 respondents (67%) felt that the P-MEX was comprehensive for the assessment of medical professionalism.
IV. DISCUSSION
This study provides preliminary evidence on the relevance, feasibility and comprehensiveness of the P-MEX in the assessment of medical professionalism in an Asian city state. The current study is part of a larger project to culturally adapt and validate the P-MEX. Based on our knowledge, this is the first study to explore the faculty perception on relevance, feasibility and comprehensiveness of the P-MEX in the assessment of medical professionalism in a multi-cultural and multi-ethnic context.
There were four items that were deemed to be less relevant (extended his/herself to meet patient needs, advocated on behalf of a patient, solicited feedback, maintained appropriate appearance). These findings were also similar in a validation study performed in Canada, where the items ‘extended his/herself to meet patient needs’ and ‘advocated on behalf of a patient’ were also frequently marked as ‘not applicable’, suggesting that the two items may be less relevant (Cruess, McIlroy, Cruess, Ginsburg, & Steinert, 2006). Qualitative methods can be used to explore the reasons why these items were deemed to be less relevant. About one-third of faculty felt that P-MEX was too long. Further study is warranted to evaluate the possibilities for shortening the P-MEX to reduce response burden and enhance routine use of the P-MEX.
In addition, our study revealed a need for greater emphasis on the assessment of collegiality. Some faculty felt that ‘collegiality’ was missing in the P-MEX despite the presence of items such as ‘demonstrated respect for colleagues’ and ‘avoided derogatory language’. This suggests that collegiality may encompass actions other than demonstrating respect and avoiding derogatory language in the local context, and further reinforces the emphasis of interprofessional collaborative practice.
Faculty also felt that there was also a lack of assessment of ‘communication with empathy’ in the P-MEX. The importance of empathetic communication is also supported by a study in Indonesia, a country in the same region, which found that patients considered communication as the most important attribute of medical professionalism (Sari, Prabandari, & Claramita, 2016).
This study has some limitations. The non-response rate raises concern about possible selection bias. Non-responders may have been less enthusiastic about the assessment of medical professionalism. Medical professionalism is affected by socio-cultural factors, therefore the findings from this study may not be entirely generalizable to another socio-cultural context. In addition, we were unable to elucidate the reasons for disagreement with the relevance of some of the items in the P-MEX as many faculty did not provide feedback and comments. Nevertheless, the findings of this study can serve as basis for future research, especially in countries with similar multicultural backgrounds.
V. CONCLUSION
Faculty agreed that most of the items in the P-MEX were relevant in the assessment of medical professionalism. Majority of the faculty also felt that the P-MEX was feasible to be used routinely in the assessment in medical professionalism. There may be a need for greater emphasis on the assessment of collegiality and communication with empathy in the modified P-MEX.
Notes on Contributors
Warren Fong reviewed the literature, designed the study, collected data, analysed data, and wrote manuscript. Yu Heng Kwan reviewed the literature, designed the study, collected data, analysed data, and wrote manuscript. Sungwon Yoon advised the design of study, analysed data, and gave critical feedback to the writing of manuscript. Jie Kie Phang collected data, analysed data, and wrote manuscript. Julian Thumboo advised the design of study, and gave critical feedback to the writing of manuscript. Swee Cheng Ng advised the design of study, collected data, analysed data, and gave critical feedback to the writing of manuscript. All authors have read and approved the final manuscript.
Ethical Approval
Ethical approval for this was granted by the SingHealth Institutional Review Board (Reference Number: 2016/3009).
Acknowledgement
The authors wish to thank all the study participants for contributing to this work.
Funding
This research was supported by SingHealth Duke-NUS Medicine Academic Clinical Programme Education Support Programme Grant (Reference Number: 03/FY2017/P2/03-A47). Funder was not involved in the design, delivery or submission of the research.
Declaration of Interest
The authors declare that they have no competing interests.
References
Avouac, J., Fransen, J., Walker, U., Riccieri, V., Smith, V., Muller, C., … Matucci-Cerinic, M. (2011). Preliminary criteria for the very early diagnosis of systemic sclerosis: Results of a Delphi Consensus Study from EULAR Scleroderma Trials and Research Group. Annals of the Rheumatic Diseases, 70(3), 476-481. doi:10.1136/ard.2010.136929
Cruess, R., McIlroy, J. H., Cruess, S., Ginsburg, S., & Steinert, Y. (2006). The professionalism mini-evaluation exercise: A preliminary investigation. Academic Medicine, 81(10), S74-S78.
Hodges, B. D., Ginsburg, S., Cruess, R., Cruess, S., Delport, R., Hafferty, F., . . . Ohbu, S. (2011). Assessment of professionalism: Recommendations from the Ottawa 2010 Conference. Medical Teacher, 33(5), 354-363.
Kwan, Y. H., Png, K., Phang, J. K., Leung, Y. Y., Goh, H., Seah, Y., . . . Lie, D. (2018). A systematic review of the quality and utility of observer-based instruments for assessing medical professionalism. Journal of Graduate Medical Education, 10(6), 629-638.
Sari, M. I., Prabandari, Y. S., & Claramita, M. (2016). Physicians’ professionalism at primary care facilities from patients’ perspective: The importance of doctors’ communication skills. Journal of Family Medicine and Primary Care, 5(1), 56-60. https://doi.org/10.4103/2249-4863.184624
*Warren Fong
SingHealth Rheumatology,
Senior Residency Programme,
20 College Road,
Singapore 169856
Tel: +6563214028
Email: warren.fong.w.s@singhealth.com.sg
Submitted: 16 April 2020
Accepted: 21 July 2020
Published online: 5 January, TAPS 2021, 6(1), 119-121
https://doi.org/10.29060/TAPS.2021-6-1/PV2250
Annushkha Sharanya Sinnathamby
Department of Paediatrics, Khoo Teck Puat National University Children’s Medical Institute, National University Hospital, Singapore
I. INTRODUCTION
“To have striven, to have made the effort, to have been true to certain ideals – this alone is worth the struggle.”
William Osler
The word “values” is heard frequently in healthcare. From the moment we step into medical school, we are challenged to reflect what our intrinsic values are, or how we can “add value” to a department during the residency application.
With time, and in going through the system, our definitions of the word “values” may change. To me, values are those things which are right and wrong, and which are important in life. In other words, values include not only what is important to my profession and to being a good doctor, but also to what is important to being a good person.
The philosopher Alasdair MacIntyre argues that one should reflect on the following three questions at the heart of moral thinking (Hinchman, 1989):
- Who am I?
- Who ought I to become?
- How ought I to get there?
In the context of understanding our values in healthcare, I wondered if the above can be translated into:
- What are my values?
- Which values should we value?
- How should we value those values?
In this article, I aim to touch on some of my view on values in the healthcare system, from the perspective of a junior doctor.
II. ARE OUR VALUES MISPLACED?
How often do we really ask ourselves what is important, what is good, or what is morally correct?
I asked a few junior doctors what values they think are important to being a good doctor. For some, the first response was classical, including “perseverance”, “compassion”, and “integrity”. However, the first thought of many others was not to be a kind or compassionate doctor, but an efficient or skilful one. I quote some of them verbatim:
“If my seniors don’t have to do anything, because I’ve done it all, then I’ve done my job.”
“No matter how much we value empathy and respect… I feel this doesn’t matter unless you have the competency to treat your patients.”
These doctors are far from unkind, dishonest, or cold. In fact, I know them personally to be some of the most good-hearted residents at work. Despite this, “typical” values such as kindness or integrity are not values which they instinctively identify with.
It is important to distinguish that being a “good” doctor may have more than one definition. “Good” as an adjective can mean being skilled and competent; on the other hand, it also means being morally upright, kind, and compassionate. Of course, it should be no argument that every doctor should be all of the above. Yet, I fear that we may be so increasingly fixated on the former, that we begin to lose sight of the latter.
As a case in point, I challenged some of our contemporaries to see how strongly they held on to an arguably core value—integrity. This value is often tested in a common daily scenario for our junior doctors: bargaining for a scan from our Radiology colleagues, where questionable tactics are sometimes employed to ensure a slot.
I asked every junior doctor working in the department two simple questions:
1) If they had ever lied to get a scan
2) If they had ever augmented the truth to get a scan
I had assumed that not a single doctor would have outright lied to get a scan, but 7.1% admitted to having done so. Furthermore, 67.9% said they would augment the truth to get a scan. This implies that there is a spectrum from an exaggeration to an outright falsehood.
When asked to elaborate on the above question, many retrospectively regretted embellishing the truth. A senior medical officer described in detail his experience lying for a particular peripherally inserted central catheter as a house officer. Even after 4 years, he could cite shame at lying to a radiologist who could almost certainly see through the lie, and perhaps depriving another patient who needed the scan more of a slot.
Ultimately, I think this boils down to our personal yardstick of our own integrity, and how willing each of us is to allow ends to justify means. Though the change of phrasing in the question I asked led to a big change in statistics, this does not change the fact that for some doctors, “augmenting the truth” strays dangerously far from what the truth really is.
Perhaps, it is then relevant to examine what would make a junior doctor re-order their priorities, and inadvertently compromise their own core values. In an increasingly busy environment, one reason we may lose sight of our core values is burnout. Studies in Singapore have described that between 55.1%-80.7% of residents reported burnout in some form, higher than their US counterparts (Lee, Loh, Sng, Tung, & Yeo, 2018; See et al., 2016). Furthermore, it was postulated that there was a negative correlation between burnout and empathy levels, and that overnight calls and low degrees of respect from colleagues were associated with increased stress levels. Burnout and emotional fatigue may cause us to erroneously weigh our values, and this could be why some junior doctors prioritise efficiency, meticulousness, or even keeping their seniors happy, to the extent of losing sight of their core values.
III. WHAT VALUES SHOULD WE VALUE?
It is no secret that a career in medicine is highly competitive. At every stage of training, medical student’s face a barrage of rigorous series of assessments that continue on into their professional careers. Therefore, it is important to examine the criteria we use to measure our doctors. Grading systems increasingly put emphasis on the softer side of medicine such as compassion and integrity, but more can be done to help our doctors value themselves and their own values more.
I recently filled up a typical grading form for my house officer. For 22 questions about his daily work, there was only one about his values and professionalism. It was a shame, as I strongly believe that an emphasis on our values should be a learning outcome, even if it is not a graded criterion. I was once taught that a patient may never remember your management, but will always remember your kindness—words that resonate with me even today.
On an institutional level, it is also important to have an emphasis on values. The institution I work in advocates the TRICEPS core values, a catchy acronym for Teamwork, Respect, Integrity, Compassion, Excellence, and Patient-Centeredness. While these values were probably established as a guideline to attract like-minded individuals to the institution, I also think these are a good set of values to emulate.
IV. HOW SHOULD WE VALUE OUR VALUES?
A system is only as great as its people. It is difficult to change a huge system, but it is easy to start the change from within ourselves, and those around us. It is also beneficial to ensure junior doctors are mindful of their values. In our daily practice, this means empowering them to self-reflect.
A simple way I do this is to ensure that after every night call, I debrief each member of my on-call team to highlight things I noticed they did well. I try not to focus solely on their medical decisions, but also the small things: staying beyond hours just to let a teenage patient with a chronic condition sleep in before blood taking, sitting with an anxious parent, or sacrificing rest time to offer moral support to a colleague doing a difficult procedure. My hope in doing this is to allow junior doctors to recognise good traits in themselves, so that they can further nurture them along their journey of medicine, and in turn inspire the people around them.
My second suggestion is for each of us to take a minute to remember what values brought us into medicine in the first place. For me, when I am at my most fatigued, feel most apathetic, or when something had gone wrong at work, I read the personal statement I wrote for my medical school application more than 10 years ago, and try to remember that inside me, my core values are still the same as the overly enthusiastic teenager who wrote them—though perhaps more mature, and hopefully slightly wiser too.
After all, it is only if we are certain of what we value, that we can inspire and encourage those around us to value their values too.
Note on Contributor
Annushkha is a Paediatrics Senior Resident. She has an interest in medical education, and is currently in the National University Health System’s Medical Education Residency Programme. She conceptualised and gathered information and drafted the initial manuscript, critically reviewed the manuscript for important intellectual content and revised the manuscript.
Acknowledgements
The author would like to thank A/Prof Marion Aw and A/Prof Quah Thuan Chong for providing her with inspiration and guidance in writing this article.
Funding
There was no funding involved in writing this article.
Declaration of Interest
The author declares no conflicts of interest, including financial, consultant and institutional relationships that might lead to bias or a conflict of interest.
References
Hinchman, L. P. (1989). Virtue or Autonomy: Alasdair MacIntyre’s Critique of Liberal Individualism. Polity, 21(4), 635-654.
Lee, P. T.,Loh, J., Sng, G., Tung, J., & Yeo, K. K. (2018). Empathy and burnout: A study on residents from a Singapore institution. Singapore Medical Journal, 59(1), 50-54.
See, K. C., Lim, T. K., Kua, E. H., Phua, J., Chua, G. S., & Ho, K. Y. (2016). Stress and burnout among physicians: Prevalence and risk factors in a Singaporean internal medicine programme. Annals, Academy of Medicine, Singapore, 45(10), 471-474.
*Annushkha Sharanya Sinnathamby
Address: 1E Kent Ridge Rd,
National University Health System,
Singapore 119228
Email: annushkha_sharanya_sinnathamby@nuhs.edu.sg
Submitted: 12 July 2020
Accepted: 18 August 2020
Published online: 5 January, TAPS 2021, 6(1), 122-124
https://doi.org/10.29060/TAPS.2021-6-1/PV2339
Hirohisa Fujikawa1, Daisuke Son1,2 & Masato Eto1
1Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, The University of Tokyo, Japan; 2Department of Community-based Family Medicine, School of Medicine, Tottori University Faculty of Medicine, Japan
I. INTRODUCTION
Many countries enforce limits on the number of hours that medical residents work. For example, in the United States, regulations about duty hours were instituted by the Accreditation Council of Graduate Medical Education as early as in 2003, reinforcing those limits in 2011 and again in 2017 (Accreditation Council for Graduate Medical Education, 2017). These reforms triggered discussion in medical education literature about their wide-ranging effects on resident education, resident wellness, and patient care (Bolster & Rourke, 2015).
In Japan, restrictions on working hours will be implemented for physicians in April 2024 (Shibuya & Unno, 2019). Because of its rapidly shifting demographics to being a super-aged society with a low birth rate, Japan is now facing issues with residents’ learning and working that other countries will need to confront in the near future as their populations shift as well (as of late 2020). Here we report on the history and current situation of postgraduate medical education in Japan, which are highly relevant to re-evaluating postgraduate training in other countries.
II. INTRODUCTION OF WESTERN-STYLE MEDICAL EDUCATION TO JAPAN
Up to and throughout the Edo period (1603–1868), there were no qualifications required for someone to become a physician; they learned in apprenticeship or learned by reading medical books on their own (Izumi & Isozumi, 2001).
At the beginning of the Meiji era (1868–1912), the Japanese government introduced German medicine to the medical education system in Japan. In 1871, the government invited German medical teachers to the precursor of the University of Tokyo (Daigaku To-ko) (Izumi & Isozumi, 2001). In the years that followed, many graduates from that school were in charge of medical education at medical schools nationwide. The German-style medical education system, therefore, spread throughout Japan and the German impact on the Japanese system of medical education is still evident. For example, Japan’s current six-year undergraduate medical educational system has Germanic origin. Thus, although Japan introduced Western-style medical education, there was no systematic system of postgraduate medical education in this era.
III. EARLY INTERNSHIP PROGRAMME AND DEVELOPMENT OF NEW POSTGRADUATE MEDICAL TRAINING SYSTEM
From the end of World War II until the 1980s, the Japanese medical education system was reconstructed as a result of Japan coming under American influence. In 1946, the present national licensing system for physicians and first medical internship system were implemented. The educational content of this early internship programme, however, was lacking, as were the financial arrangements for the interns. Trainees had no guarantee of their status, and the first-year residents were required to work as volunteers before taking the national medical license examination (Shukan Igakukai Shimbun, 2004).
In the late 1960s, protests by medical students at the University of Tokyo for the improvement of interns’ working conditions progressively intensified and spread to other universities as well. Students across the country boycotted the medical license test and those in Tokyo occupied the Yasuda Auditorium (a symbol of the University of Tokyo) in protest. There was recognition that the internship programme as it was, with its overworked trainees, could lead to patient safety issues related to possible errors by the fatigued interns. This problem of patient safety is still a topic of discussion worldwide, and led to the limit of 80 hours of work per week for residents in U.S. training programmes mentioned in the introduction.
As a result of the protest, the internship system was discontinued in 1968, and a postgraduate medical training system was introduced to replace it. In this system, students took the medical license examination following graduation, and then received specific training for at least two more years. This strengthened the quality of the education compared to the previous system, but the status and pay of the trainees remained unstable (Shukan Igakukai Shimbun, 2004). Graduate students were forced to work part-time jobs during their training. They also raised issues related to the content of their education, inadequate guidance system, and insufficient evaluation of the training received.
In 2004, a new two-year mandatory postgraduate medical training system was implemented in all training programmes (Shukan Igakukai Shimbun, 2004). In this system, all medical school graduates spend two years rotating through the seven specialties (internal medicine, surgery, emergency medicine or anaesthesiology, paediatrics, psychiatry, community-based medicine, and obstetrics and gynaecology). Then only after the two-year training, can young physicians enter specialty-based residencies. Owing to this reform, the average resident salary has increased, and residents are paid sufficiently to concentrate on their training. Moreover, with respect to learning, this system has enabled residents to obtain more experience and become more confident about their clinical skills and the efficiency of their general knowledge (Nomura et al., 2008).
IV. WORK STYLE REFORM
The Japanese economy grew dramatically after World War II. At that time, ideal workers were considered to be those who spent all their time working. The epitome of this attitude is captured in the phrase “Can you work for 24 hours?” which became popular after originating from a Japanese TV advertisement for an energy drink. Japan was notorious for its long working hours, and because it also became an aging society, where a relatively small number of working-age people must support a large senior population, there was a need to raise productivity. Death by overworking was so frequently occurring in Japan that it even had its own name, Karoshi, which literally means “death by overwork.” As a result, work-life balance started to get a lot of attention as the solution to avoid this social problem.
Medical care in Japan has long been supported by the self-sacrificing work of physicians, especially young doctors in their twenties and thirties (Shibuya & Unno, 2019). According to an investigation performed by the Ministry of Health, Labour and Welfare (MHLW), 40% of physicians exceed the norm for hours worked by workers in other sectors. More than 10% of physicians work more than 1860 hours of overtime per year (Ministry of Health, Labour and Welfare, 2019). Because of this, the MHLW drew up a contentious plan to restrict physicians’ working hours through a regulation that will take effect in 2024. In particular, physicians’ overtime hours will be restricted to 960 hours per year, to keep hours below what is called the “Karoshi Line” (the number of hours beyond which a death is presumed to be related to overwork). There will still be allowances in the regulation for some physicians to work up to 1,860 hours yearly overtime, far above the Karoshi Line, if necessary to maintain community health care or to work intensively for the purpose of learning and becoming specialists.
V. RESIDENT AS LEARNER OR WORKER?
In Japan, the view of residents has vacillated over time between the perspective of “resident as learner” and that of “resident as worker.” Until the repeal of the early internship system in 1968, the viewpoint of “resident as learner” was dominant, and trainees were obliged to work unpaid. In the course of abolition of the early internship system, the standpoint of “resident as worker” was enhanced. The perspective of “resident as learner” was revisited through the process of the new two-year postgraduate training system implementation in 2004.
Nowadays, the viewpoint of “resident as worker” draws attention because physicians and residents are still forced to work for prolonged hours. Because of this, burnout among medical residents has become a critical problem, and several studies have been conducted on the mental health of residents in Japan. This suggests that the pendulum has swung too far and the perspective of “resident as learner” is now lacking. We must develop and implement resident education that emphasises their roles as both learners and workers, for the sake of the patients they care for and for society’s sake.
The implication of this is that we will need to educate residents effectively and efficiently within a limited number of work hours. The duty hour restrictions will raise the number of trainees caring for a particular patient on any given day, and will push up the demand for meaningful and efficient transfer of information. We will have to teach “new professionalism.” New professionalism derives from sharing responsibility for patient care, as contrasted with nostalgic professionalism, which is defined as continuously giving priority to a patient’s needs over one’s own personal needs (Arora, Farnan, & Humphrey, 2012). Trainees have to be taught a new view of their responsibilities and new skills for directing team-based care. More specifically, they should be taught the skills of quickly summarising and communicating pertinent sign-out information at the end of shifts to support patient care. The model of continuity-enhanced handovers may be useful (Arora, Reed, & Fletcher, 2014).
It is our responsibility as educators and leaders to seek breakthrough solutions to promote an educational system that emphasises both the perspective of “resident as learner” and that of “resident as worker.” It is time for change.
Notes on Contributors
Hirohisa Fujikawa contributed to the acquisition, analysis and interpretation of the data and the drafting of the manuscript. He approved the final manuscript, and agreed to be accountable for all aspects of the work in ensuring that questions related to any part of the work are appropriately investigated and resolved.
Daisuke Son contributed to the conception and design of the study, and the revision of the manuscript. He approved the final manuscript, and agreed to be accountable for all aspects of the work in ensuring that questions related to any part of the work are appropriately investigated and resolved.
Masato Eto contributed to the conception and design of the study, and the revision of the manuscript. He approved the final manuscript, and agreed to be accountable for all aspects of the work in ensuring that questions related to any part of the work are appropriately investigated and resolved.
Acknowledgement
The authors wish to express sincere appreciation to Ms. Kayo Kondo, School of Politics, Philosophy, Language and Communication Studies, University of East Anglia, who assisted us in translating the manuscript.
Funding
The authors have no funding to report.
Declaration of Interest
The authors declare no conflicts of interest associated with this manuscript.
References
Accreditation Council for Graduate Medical Education. (2017). Common Program Requirements Section VI with Background and Intent [PDF file]. Retrieved from https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_Section%20VI_with-Background-and-Intent_2017-01.pdf.
Arora, V. M., Farnan, J. M., & Humphrey, H. J. (2012). Professionalism in the era of duty hours: Time for a shift change? JAMA, 308(21), 2195–2196. https://doi.org/10.1001/jama.2012.14584
Arora, V. M., Reed, D. A., & Fletcher, K. E. (2014). Building continuity in handovers with shorter residency duty hours. BMC Medical Education, 14(Suppl 1), S16. https://doi.org/10.1186/1472-6920-14-S1-S16
Bolster, L., & Rourke, L. (2015). The effect of restricting residents’ duty hours on patient safety, resident well-being, and resident education: An updated systematic review. Journal of Graduate Medical Education, 7(3), 349–363. https://doi.org/10.4300/JGME-D-14-00612.1
Izumi, Y., & Isozumi, K. (2001). Modern Japanese medical history and the European influence. The Keio Journal of Medicine, 50(2), 91–99. https://doi.org/10.2302/kjm.50.91
Ministry of Health, Labour and Welfare. (2019). On the upper limit for overtime among doctors (in Japanese). Document 2 presented at the 19th Committee on the Work Style Reform of Doctors [PDF file]. Retrieved from https://www.mhlw.go.jp/content/10800000/000481338.pdf
Nomura, K., Yano, E., Aoki, M., Kawaminami, K., Endo, H., & Fukui, T. (2008). Improvement of residents’ clinical competency after the introduction of new postgraduate medical education program in Japan. Medical Teacher, 30(6), e161–e169. https://doi.org/10.1080/01421590802047307
Shibuya, K., & Unno, N. (2019). Unpaid doctors in Japanese university hospitals. The Lancet, 393(10176), 1096–1097. https://doi.org/10.1016/S0140-6736(19)30472-6
Shukan Igakukai, Shimbun. (2004). The History of clinical training in Japan (in Japanese) [PDF file]. Retrieved from http://www.igaku-shoin.co.jp/nwsppr/n2004dir/n2566dir/n2566_02.pdf
*Hirohisa Fujikawa
The University of Tokyo,
7-3-1 Hongo, Bunkyo-ku,
Tokyo 113-0033, Japan
Tel: +81-3-5841-3480
Email: hirohisa.fujikawa@gmail.com
Submitted: 1 April 2020
Accepted: 26 May 2020
Published online: 5 January, TAPS 2021, 6(1), 128-131
https://doi.org/10.29060/TAPS.2021-6-1/PV2240
Sonia Kumar, Rachel Browne, Jeffrey Wu & Simon Tso
Department of Dermatology, South Warwickshire NHS Foundation Trust, Warwick, United Kingdom
I. FACTORS INFLUENCING MOTIVATION TO PURSUE GRADUATE-ENTRY MEDICINE
The decision to pursue medicine is a significant step for individuals, particularly those for whom this involves a career change. While medicine in the UK has traditionally been an undergraduate course, graduate-entry medicine (GEM) programmes were introduced in 2000 and offer an accelerated course for suitably qualified candidates with a Bachelor’s degree. Students have a variety of motivations for undertaking a GEM programme (Carter & Peile, 2007), and we herein explore the factors that influence this range of motivations.
Literature suggests that students of GEM programmes can broadly be categorised into two groups: individuals who do not consider medicine when choosing their first degree, or individuals who selected a degree subject that would keep medicine open as a career (Sulong et al., 2014). Key motivating factors to pursue GEM include prior health service experience (as a patient or as a health professional), professional autonomy, and influence from others. The most frequently cited factor influencing the decision was a desire to help people (Sulong et al., 2014). Other literature suggests a lack of job satisfaction and limited career development opportunities are key factors drawing individuals away from their original career paths and into medicine.
The other group includes individuals who had previously failed to gain entry to medical school at the undergraduate level, studying alternative subjects but maintaining a goal of studying medicine. These individuals have demonstrated motivation by completing a degree that was not their first choice, and this can continue throughout their medical studies. A comparison of Leicester Medical School GEM and undergraduate-entry medicine (UEM) students found higher general pass rates for GEM students with a biomedical science background when compared to their UEM peers (Carter & Peile, 2007).
II. STUDENT EXPERIENCES
A semi-structured interview-based study exploring the experiences of twenty-one students from the University of Warwick GEM programme was conducted by the author Simon Tso as part of his doctoral research thesis (Tso, 2017). Students were asked to describe their motivations to pursue GEM. Three broad groups of student journeys into GEM were identified: ‘medicine as an end goal’, ‘career indecision’ and ‘career switchers’. The ‘medicine as an end goal’ group represented students within the study and students in this group recalled a longstanding ambition to pursue medicine. The ‘career indecision’ group consisted of students who had previously considered medicine as a potential career but instead chose an alternative path. The ‘career switchers’ comprised of students who left their previous career to pursue GEM.
A. Why Pursue Medicine as a Career?
Motivations to pursue GEM were attributed to a combination of ‘pull’ and ‘push’ factors. ‘Pull’ factors included those that the students regarded as positive experiences or perceived incentives of choosing medicine as a career. A few, however, experienced negative ‘pull’ factors, recalling pressure and expectation from family to pursue medicine simply because they were good at science. Often, the reassurance of a guaranteed job following the degree influenced this pressure.
A key theme for motivations reported by this group was their general interest in human health, a desire to improve people’s lives and to do “meaningful work”. In most instances, many had received positive encouragements from other individuals who supported and positively influenced their career choice. One student, however, recalled a negative experience in secondary school when he expressed an interest in applying for UEM to a teacher. This teacher subsequently discouraged application expressing that they did not believe the student would meet the expected entry requirements. The student felt that extra support from their teachers rather than discouragement could have guided them to have studied UEM rather than having to apply for a GEM programme later in life.
‘Push’ factors were reasons why some students chose to cease continuing on their original career path and consider alternative careers instead. Reasons given highlighted the disillusionment they felt with certain aspects of their original career path and therefore felt pushed to consider an alternative career. These included lack of career progression opportunities, lack of job satisfaction and lack of autonomy in their roles. The students perceived that medicine could offer the opportunities they desired from a career.
III. OUR REFLECTIONS
A. What Factors Influence Motivation to Study GEM?
The Self Determination Theory devised by Ryan and Deci (2000) can be applied to the understanding of why people choose to study GEM. The Self Determination Theory suggests that three factors are required for psychological growth: autonomy, competence and connection. Although thought to be innate, these factors are affected by environmental interactions and can influence our proactivity or passivity. The degree of self-determination is also influenced by whether the factors that motivate us are:
- Intrinsic–where an activity is done for the pleasure or enjoyment of the activity itself.
- Extrinsic–where a task is performed for a possible reward or fear of punishment.
- In some instances, factors that make us demotivated–the lack of desire to act or, act without intent.
Typical intrinsic factors recalled as motivations for pursuing GEM were the desire to do something fulfilling or to help others. For others it was the desire to commit to lifelong learning or a career where their interest in biological sciences could be applied to human physiology.
Extrinsic factors such as family pressures or socioeconomic background also have been known to impact career choice and journey. In some cultures, professions such as medicine, engineering or pharmacy are held in high esteem and children from these backgrounds can be encouraged to pursue these subjects at university. These careers are often associated with job and financial stability, factors that may be of high importance to individuals from a disadvantaged or low socioeconomic background. In these instances, a career in medicine can be perceived as a mode of upwards social mobility.
B. What Factors Contribute to Career Indecision?
Gati, Krausz and Osipow (1996) describe a theoretically driven taxonomy of career decision that can be applied to the career indecisions reported by the medical students in their study. The taxonomy was categorised into three broad clusters; lack of readiness, lack of information, and inconsistent information, all of which can explain why individuals may be hesitant or indecisive when considering a career in medicine.
Typically, students in the United Kingdom consider a career in medicine aged 16-18, applying to medical school in the second year of the A-Level programme. The decision to pursue medicine is difficult, and some may be lacking the required information to adequately prepare them, both to apply and to succeed in the application process. This is particularly relevant to students from disadvantaged backgrounds or resource-poor schools that may find it challenging to support the aspirations of their students and prepare them for medical school interviews.
Widening participation (WP) is an umbrella term referring to coordinated efforts that encourage and support individuals from underrepresented or disadvantaged backgrounds to consider pursuing academic careers such as engineering, medicine and law. The idea behind the programmes is to ensure that all students have access to equal opportunities, regardless of their background. These schemes often provide interview support, work experience schemes and checking of personal statements. They can provide further insight into the career, and also provide workshops on the special entrance tests required for medical school admission.
A medical student in our study was supported by a WP scheme to gain admission into her first degree which served as a stepping-stone into a GEM programme. An increase in provision and access to WP schemes would seek to level the playing field in the application process to medical school at both UEM and GEM level. The provision of extra support and information would enable these students to make informed career choices and make the medical school application process fairer.
IV. CONCLUSION
GEM programmes provide individuals the opportunity to pursue medicine as a career at a later stage, and their additional life and work experience can engender a more diverse and experienced cohort of graduates (Carter & Peile, 2007). WP schemes at the university level could further contribute to this diversity, and it would be interesting for future studies to explore whether students who were unsuccessful or did not attempt to gain entry at the UEM level could have benefited from secondary school WP programmes.
It is clear that there are multiple reasons individuals decide to pursue GEM, whether as a long-term ambition from school age or as a career change. These multifactorial motivations consist of both intrinsic and extrinsic factors and more work is needed to understand their influence on students’ motivations. Identifying common themes allows for more effective recruitment and teaching of these non-traditional students who will eventually contribute to a more diverse medical workforce.
Notes on Contributors
Dr Sonia Kumar is a graduate of the University of Warwick graduate-entry medicine degree programme and is a newly qualified Foundation Year 1 doctor at the South Warwickshire NHS Foundation Trust. Dr Kumar made substantial contributions to the conception, design, editing of this piece and approval of the final manuscript.
Dr Rachel Browne completed a Masters in Medical Education at the University of Warwick. She is a Speciality Registrar in Dermatology and former Clinical Education Fellow at the South Warwickshire NHS Foundation Trust. Dr Browne contributed to the design and editing of this piece including approving this final manuscript.
Dr Jeffrey Wu is a graduate of the University of Warwick graduate-entry medicine programme and former undergraduate Teaching Assistant at the University of California, San Diego. He is training in Internal Medicine at South Warwickshire NHS Foundation Trust. Dr Wu contributed to the design, edit and approval of this manuscript.
Dr Simon Tso completed a doctoral (MD) degree at the University of Warwick. He is a Fellow of the Higher Education Academy and Consultant Dermatologist at the South Warwickshire NHS Foundation Trust. Dr Tso made substantial contribution to the conception, data analysis/interpretation editing and authorising the final manuscript.
Ethical Approval
This study was part of a larger study investigating the experience of graduate-entry medicine degree programme students, which has received ethical approval from the University of Warwick Biomedical Research Ethics Sub-Committee (Reference: 169-01-2012).
Acknowledgements
The authors would like to thank Asim Yousuf, Nina Owen, Mike Smith and Dr Jane Kidd for their assistance with the design and development of the study.
Funding
This study was part of a larger study investigating the experience of graduate-entry medicine degree programme students, which was funded by the Institute for Advanced Teaching and Learning, University of Warwick, United Kingdom.
Declaration of Interest
The authors have no conflict of interest, including no financial, consultant, institutional and other relationships that might lead to bias.
References
Carter, Y. H., & Peile, E. (2007). Graduate entry medicine: High aspirations at birth. Clinical Medicine, 7(2), 143–147. https://doi.org/10.7861/clinmedicine.7-2-143
Gati, I., Krausz, M., & Osipow, S. H. (1996). A taxonomy of difficulties in career decision making. Journal of Counselling Psychology, 43(4), 510–526. https://doi.org/10.1037/0022-0167.43.4.510
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68–78. https://doi.org/10.1037/0003-066X.55.1.68
Sulong, S., McGrath, D., Finucane, P., Horgan, M., O’Flynn, S., & O’Tuathaigh, C. (2014). Studying medicine – A cross-sectional questionnaire-based analysis of the motivational factors which influence graduate and undergraduate entrants in Ireland. JRSM Open, 5(4), 204253331351015. https://doi.org/10.1177/2042533313510157
Tso, S. H. Y. (2017). The graduate-entry medical student: Challenges to transition through medical school (Doctoral dissertation, University of Warwick, Coventry, United Kingdom). Retrieved from http://wrap.warwick.ac.uk/99890/
*Sonia Kumar
Lakin Road, CV34 5BW
South Warwickshire NHS Foundation Trust,
Warwick, United Kingdom
Email: Sonia.kumar@doctors.org.uk
Submitted: 21 February 2020
Accepted: 3 June 2020
Published online: 5 January, TAPS 2021, 6(1), 125-127
https://doi.org/10.29060/TAPS.2021-6-1/PV2228
Chooi Peng Ong, Cindy Shiqi Zhu, Desmond SL Ong & Ying Pin Toh
Family Medicine Residency, National University Health System, Singapore
I. INTRODUCTION
Family medicine training encompasses the need to develop a diverse skillset and the ability to practice in different settings. During three years of training, family medicine residents from National University Health System (NUHS) rapidly transit through many hospital rotations with varying specialty-specific competency requirements. Throughout this period, each resident is rostered to run a half-day primary care clinic on the same day each week and is assigned a dedicated faculty member to supervise him during the session. Each faculty member is assigned up to four to six residents for the half-day sessions every week. There is a need to contextualise what is learnt in hospital to primary care, and to effectively integrate knowledge across disciplines. We describe here a tool that the NUHS family medicine residency has used to bring together faculty and residents of varying seniorities and locations for discussion, reflection, and growth.
II. METHODS
A. What We Did
Over the past few years, learners’ groups have been created by residency faculty and residents on a voluntary basis, using an internet-based group messaging platform. As described here, the group is defined by a common supervising faculty member and is formed for the duration of the academic year. The supervisor is also the group administrator and main facilitator.
The platform described here is the WhatsApp messaging platform. It was chosen because of the ubiquity of its use by the faculty and resident bodies as well as the closed nature of the groups, in that membership is by invitation, and messages are encrypted (WhatsApp Inc., n.d.). An additional benefit was that, unlike some dedicated healthcare messaging applications, the messages and shared resources are not automatically deleted (Geron, 2011) after a period of time.
The WhatsApp group chat functions as a virtual community board for clinical learning, questions, answers, and clarification. Topics discussed usually arise from residents’ clinic encounters, and the emphasis of discussion is on contextualising knowledge from books and hospital learning to real-life primary care practice. For example, a patient is seen for chronic disease management and is noted to smoke cigarettes. The post-consultation debrief may include a suggestion to read up on nicotine replacement strategies (NRT), following which the resident may upload an update on NRT to the chat group. Case-based discussion proceeds asynchronously and is facilitated by the supervisor and contributed to by all group members. Notably, case discussions involving patients are anonymised, and the use of unique personal identifiers is prohibited. Additionally, the group platform allows discussion and opinion to evolve on current issues relating to professionalism and ethics. Over time, the group chat messages become a useful depository of contextualised, opportunistic, experiential learning for the group.
III. DISCUSSION
A. Potential Pitfalls
The commonest pitfall is the tendency for resources shared to be comprehensive textbook-like knowledge updates, whereas the more useful type of update is a distilled, pragmatic one that can be directly applied to practice. It is often noted that group participation tends to wane as the year progresses, possibly due to an increase in coursework and examination preparation. Some group members tend to participate more freely than others. Unlike a face-to-face group, the quiet members may be virtually forgotten by others over the course of the year unless effort is made to engage them.
The openness of the discussion can be affected by traditional medical hierarchies and the facilitator may need to intentionally address this. It is important to recognise that the richness of discourse is largely dependent on the quality of moderation and on participant engagement. Finally, as topics for discussion are identified opportunistically, the same topics may be repeatedly identified.
B. Tips for Managing the Group
The tone and culture of the group will greatly affect the efficacy of group interactions. It is important to set ground rules of courtesy, freedom to question, and expectations of participation early in the group’s life cycle. Also, while the facilitator needs to encourage active participation with provocative questioning, the senior residents need to help set the tone of egalitarian discussion, in order for younger participants to feel sufficiently comfortable to contribute willingly. Having a co-facilitator who is another faculty member or a resident who was a member of a past-year group has helped in establishing the group’s openness and activeness, with varying degrees of success.
It is important for the facilitator to have an idea of what broad topics ought to be discussed over the lifespan of the group, which is often the duration of the academic year. This ensures that discussions are guided beyond the strictly opportunistic. The length of contributions should not exceed the attention span of those reading. As a suggestion, the length of an uploaded update should not exceed the size of a smartphone screen, the emphasis being on curated pearls.
It is important to emphasise an academic focus, to ensure the group does not devolve into a social support group. This is not because social support is secondary, but because these WhatsApp groups, as described here, were set up to further academic objectives. Social greetings are therefore largely relegated to alternative message boards and private messages. Nevertheless, it is recognised that a functional group will have social elements, and that social greetings may be an indicator of group cohesion and viability (Salas, Grossman, Hughes, & Coultas, 2015).
As with any group that interacts over time, an informal curriculum (Rogoff, Callanan, Gutiérrez, & Erickson, 2016) will run in parallel with the explicit curriculum and will eventually impact on learner attitudes and even values. It is important for the facilitator to reflect on the elements of his informal/implicit curriculum and to intentionally drive it. Examples of these elements may include personal integrity, collegiality, or independent questioning.
IV. CONCLUSION
The WhatsApp chat groups described here have allowed us to extend study group discussions beyond the clinic. This is particularly useful in family medicine training where the contextualization of a broad knowledge base needs to be constant and relentless, and opportunities for face-to-face meetings are limited by logistics. The extended virtual discussion is also a useful platform by which to teach affective domain skills, such as attitudes and values. Because of the iterative nature of clinic sessions intercalated with online discussions, learning can be reflected on and applied and may be postulated to occur at up to Kirkpatrick level 3 (Kirkpatrick & Kirkpatrick, 2006). Finally, by bringing together learners of varying seniorities, role modelling, mentoring, camaraderie, and certain emotional support are happy by-products.
Notes on Contributors
Ong Chooi Peng is a faculty member of the NUHS family medicine residency program. She runs several virtual groups, reviewed the literature, and wrote the manuscript.
Desmond Ong is a faculty member of the NUHS family medicine residency program. He also runs virtual groups and helped edit the manuscript.
Cindy Zhu Shi Qi and Toh Ying Pin are residents within the NUHS family medicine residency program. They belong to virtual groups and helped edit the manuscript.
Acknowledgements
The authors acknowledge the generations of NUHS family medicine residents who have contributed to the development and evolution of the virtual groups, to the current form of WhatsApp groups described here.
Funding
The authors received no funding for this work.
Declaration of Interest
The authors declare no conflict of interest.
References
Geron, T. (2011, June 15). TigerText secures (and erases) your text messages. Retrieved January 20, 2020, from https://tigerconnect.com/newsroom/tigertext-secures-and-erases-your-text-messages/
Kirkpatrick, D. L., & Kirkpatrick, J. D. (2006). Evaluating Training Programs. New York, NY: Macmillan Publishers.
Rogoff, B., Callanan, M., Gutiérrez, K., & Erickson, F. (2016). The organization of informal learning. Review of Research in Education, 40(1), 356-401. https://doi.org/10.3102/0091732×16680994
Salas, E., Grossman, R., Hughes, A., & Coultas, C. (2015). Measuring team cohesion. Human Factors: The Journal of the Human Factors and Ergonomics Society, 57(3), 365-374. https://doi.org/10.1177/0018720815578267
WhatsApp Inc. (2020, January 20). WhatsApp Security: Privacy and Security is in our DNA. Retrieved from http://www.whatsapp.com/security/
*Cindy Shiqi Zhu
1E Kent Ridge Road,
Singapore 119228
National University Health System (NUHS)
Email: Shi_Qi_ZHU@nuhs.edu.sg
Submitted: 20 April 2020
Accepted: 29 April 2020
Published online: 1 September, TAPS 2020, 5(3), 88
https://doi.org/10.29060/TAPS.2020-5-3/LE2252
Wenqi Chiew
Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Dear Editor,
I read with great interest your editorial “Grit in healthcare education and practice” published on The Asia Pacific Scholar (Dujeepa & Gwee, 2020). I agree that grit is an important trait to develop in healthcare, especially for patient care. In addition to focusing on grit at the institutional level, we could look at it on an individual level. The question henceforth is that–How do we develop or strengthen the grit in ourselves? Angela Duckworth proposed 5 ways to develop grit–pursue what interests you; practice; find purpose; have hope; and join a gritty group (Barker, 2016). Personally, I feel that finding purpose plays a large role in developing passion and perseverance.
I would like to share this poem that I wrote after my first attempt on blood taking on a patient. Amidst hectic schedules and difficult tasks in medical school, this promise that I made years ago helped kept my passion and perseverance alive.
With shaking hands and a sweaty palm
I slide the needle in and try to calm
And I heave a sigh of great relief
As I watch the backflow fill beneath
Just minutes before, my mentor had asked
“Do you mind if my student try this task?”
With trusting eyes and a reassuring grin,
The patient said, “go ahead, do your thing.”
The trust that you have given to me
Even though I may now be unworthy
Inspires me and greatly spurs me on
To be a better doctor hereupon.
Notes on Contributors
Wenqi Chiew is listed as the first author and she wrote this paper.
Funding
There is no funding provided.
Declaration of Interest
There is no conflict of interest, including financial, consultant, institutional or otherwise for the author.
References
Barker, E. (2016). This is how to increase grit, according to research. Retrieved from TIME, https://time.com/4323260/how-to-increase-grit-perseverance/
Dujeepa, D. S., & Gwee, M. C. E. (2020). Grit in healthcare education and practice. The Asia Pacific Scholar, 5(1), 1-2. https://doi.org/10.29060/TAPS.2020-5-1/EV5N1
*Wenqi Chiew
Yong Loo Lin School of Medicine,
1E Kent Ridge Road,
National University of Singapore,
Singapore 119228
Email: wenqi@u.nus.edu
Submitted: 17 March 2020
Accepted: 3 April 2020
Published online: 1 September, TAPS 2020, 5(3), 83-87
https://doi.org/10.29060/TAPS.2020-5-3/SC2238
Cristelle Chow1, Cynthia Lim2 & Koh Cheng Thoon3
1General Paediatrics Service, Department of Paediatrics, KK Women’s and Children’s Hospital, Singapore; 2Nursing Clinical Services, KK Women’s and Children’s Hospital, Singapore; 3Infectious Disease Service, Department of Paediatrics, KK Women’s and Children’s Hospital, Singapore
Abstract
Background: Effective communication between doctors and patients leads to better compliance, health outcomes and higher doctor and patient satisfaction. Although in-person communication skills training programs are effective, they require high resource utilisation and may provide variable learner experiences due to challenges in standardisation.
Objective: This study aimed to develop and implement an evidence-based, self-directed and interactive online communication skills training course to determine if the course would improve learner application of communication skills in real clinical encounters.
Methods: The course design utilised the Kalamazoo Consensus framework and included videos based on common paediatric clinical scenarios. Final year medical students in academic year 2017/2018 undergoing a two-week paediatric clerkship were divided into two groups. Both groups received standard clerkship educational experiences, but only the intervention group (88 out of 146 total students) was enrolled into the course. Caregiver/patient feedback based on students’ clinical communication was obtained, together with pre- and post-video scenario self-reported confidence levels and course feedback.
Results: There were minimal differences in patient feedback between intervention and control groups, but the control group was more likely to confirm caregivers’/patients’ agreement with management plans and provide a summary. However, caregivers/patients tended to feel more comfortable with the intervention compared to the control group. Median confidence levels increased post-video scenarios and learners reported gains in knowledge, attitudes and skills in paediatric-specific communication.
Conclusion: Although online video-based communication courses are useful standardisation teaching tools, complementation with on-the-job training is essential for learners to demonstrate effective communication.
Keywords: Online Learning, Undergraduate Medicine, Professionalism, Communication Skills, Patient Feedback
I. INTRODUCTION
Effective doctor-patient communication leads to better compliance, health outcomes and higher doctor and patient satisfaction. Online video-based communication skills courses can be feasible, with learners reporting increased confidence in key communication skills (Kemper, Foy, Wissow, & Shore, 2008). However, these evaluation methods have been limited to the Kirkpatrick levels of “reaction” and “learning”, instead of “behaviour” and “results”, which are more reflective of applied learning.
While in-person communication skills training programs simulate clinical environments, they can have inconsistent delivery because facilitators and standardised patients provide variable training experiences. In order to replace traditional role-play sessions, this study aimed to develop and implement a pilot online communication skills course to provide standardised, video-based scenarios in a self-directed interactive learning format using an evidence-based framework.
Our research questions are as follows:
- Would an online communication course improve the application of communication skills in real clinical encounters?
- What is the impact of an online communication course on learner-rated confidence levels in paediatric-specific clinical communication encounters?
- What are the self-reported aspects of learning that participants of an online communication course experience?
II. METHODS
This course design utilised the Kalamazoo Consensus framework (Makoul, 2001) which included the essential elements of clinical communication: Open the discussion, gather information, understand patient’s perspective, share information, reach agreement and provide closure.
Through Bandura’s social learning theory, people learn through observing others’ behaviour. The attitudes and outcomes of those behaviours then guide subsequent actions. This course therefore utilised videos featuring positive doctor-caregiver interactions, to encourage modelling through observation. The 3-5-minute video scenarios acted by practicing healthcare professionals were based on commonly encountered general paediatric clinical situations.
The course was designed using Articulate© software. “Pop-up” prompts highlighting important clinical or communication points, a pre- and post-test and in-video multiple-choice questions were included to increase learner engagement. To evaluate the impact of the course on learner-rated confidence levels, students were shown a clinical vignette, and asked to rate their self-confidence on a 4-point Likert scale before and after each video. Each video concluded with a summary, emphasising the utilisation of the Kalamazoo Consensus Framework.
|
Q1: Did the student introduce his/ her name? |
Q2: Did the student allow you to express your concerns? |
|
⃝ Yes ⃝ No ⃝ Not sure |
⃝ Yes, ALL my concerns ⃝ Not really, only SOME of my concerns ⃝ No, NONE of my concerns |
|
Q3: How much was the student interested in your point of view (e.g. expectations, ideas, beliefs, values) when he/she was asking you questions? |
Q4: How much was the student interested in your point of view (e.g. expectations, ideas, beliefs, values) when he/she was planning and explaining things? |
|
⃝ Very interested ⃝ Somewhat interested ⃝ Somewhat uninterested ⃝ Not interested at all |
⃝ Very interested ⃝ Somewhat interested ⃝ Somewhat uninterested ⃝ Not interested at all |
Q5: Did you feel that the student listened to you? |
Q6: How well do you feel the student explained things to you? |
|
⃝ Listened all the time ⃝ Listened sometimes ⃝ Did not listen at all |
⃝ Very well – I understood all the explanation ⃝ Fairly well – I understood some of the explanation ⃝ Not well at all – I did not understand all of the explanation |
|
Q7: Did the student check if you were agreeable with the management plan? |
Q8: Did the student provide a summary of the problem/ plans at the end of the conversation? |
|
⃝ Yes ⃝ No ⃝ Not sure |
⃝ Yes ⃝ No ⃝ Not sure
|
|
Q9: Overall, how comfortable were you interacting with the student? |
Q10: What do you think this student could improve in? E.g. Be more courteous/ respectful, speak or explain more clearly, listen more, check my understanding, answer my queries etc. |
|
⃝ Very comfortable – I would like to have him/ her be my/ my child’s doctor ⃝ Somewhat comfortable ⃝ Somewhat uncomfortable ⃝ Not comfortable at all – I do not want him/ her to be my/ my child’s doctor |
|
Table 1. Caregiver/Patient Feedback Form
To evaluate the self-reported learning points from the course, students were asked upon course completion to provide course feedback, including free-text completion of the phrase: “Things I have learnt include…” To evaluate whether the course improved the application of communication skills in real clinical encounters, caregiver/patient feedback was obtained towards the end of the paediatric clerkship for all students, regardless of course participation (Table 1). This form was modified based on course content from a family feedback instrument utilised in a paediatric setting (Zimmer, Solomon, Siberry, & Serwint, 2008). Implied informed consent was obtained from all participants.
Final year medical students from a five-year Singapore undergraduate medical program were enrolled over one academic year (2017/2018). Alternate batches (2nd, 4th, 6th, 8th) were enrolled into the course. Each student was provided a unique username and password for course access on any internet-enabled device throughout his/her 2-week paediatric clerkship and course participation was strongly recommended. Students from other batches (1st, 3rd, 5th, 7th) were analysed as controls. All students integrated into paediatric clinical teams, participated in ward rounds and communicated plans to patients/caregivers.
Statistical analysis was performed using SPSS© Statistics version 25.0 and chi-square analysis was used for patient feedback analysis.
This study was exempted from formal Centralized Institutional Review Board review and implied informed consent was granted by the SingHealth Centralized Institutional Review Board.
III. RESULTS
A total of 146 students were posted to the study institution in academic year 2017/2018 and 88 students were enrolled into the course. There were 80 (90.9%) attempts at the course, of which 76 (95%) students provided course feedback. The median time needed for course completion was 59 minutes. Patient feedback was successfully collected for 94 students, of which 44 (46.8%) attempted the course. Main reasons for unsuccessful collection were fast patient turnovers and patients/caregivers rejecting the request to provide feedback, usually due to perceived insufficient student contact time.
A. Application of Communication Skills – Evaluated via Patient Feedback
Although there were generally no differences in patient feedback between intervention and control groups, the control group was more likely to check with caregivers/patients whether they were agreeable with the management plan (76.0% vs. 56.8%, p<0.05) and provided a summary to the caregiver/patient (74.0% vs. 47.7%, p<0.05). Approaching statistical significance was the finding that caregivers/patients were more likely to feel very comfortable with the intervention compared to the control group (65.9% vs. 48.0%, p=0.062).
B. Course Impact on Self-Reported Confidence Levels
For scenario 1, the median confidence level increased from 3 (“somewhat confident”) to 4 (“very confident”). For the subsequent scenarios, this increased from 2 (“a little confident”) to 3 (“somewhat confident”).
C. Self-Reported Learning Points –Evaluated via Course Feedback
1) Knowledge: The majority of students mentioned learning about the clinical management and discharge advice for gastroenteritis and urinary tract infection, and the need for procedural sedation in uncooperative young children. Students reported that they had learnt general frameworks and principles for communication, and concepts of consent-taking. Students also frequently mentioned “practical”, in terms of “practical knowledge” and “practical tips” for communication.
2) Attitude: Students mentioned that they learnt about the importance of empathy. They also reported important aspects of patient-centred care, such as understanding the parent’s or patient’s perspective to formulate a treatment plan together and ensuring mutual understanding via “checking back to ensure the parent truly understands” and “to have a closed loop at the end of each communication”.
3) Skills: On a broader perspective, students described that they had learnt “how to properly structure communication with a patient’s parents” and “how to better communicate with parents using the various strategies”. Almost all students reflected that they had learnt specific communication skills, particularly with regards to dealing with challenging situations such as “how to approach parents who may not be cooperative/willing to listen to you” and “how to address angry parents” as well as “how to address their concerns and manage their expectations”. Two students also mentioned that they may not have been exposed to similar scenarios in their daily work: “… handle scenarios which are often not taught within lectures.”
IV. DISCUSSION
Computer-based communication courses have shown to improve students’ self-efficacy in performing communication tasks and assessments of students’ perceptions and practice of communication skills (Kemper et al., 2008), which was also demonstrated in this study’s improvement in self-reported confidence levels. It is however, expected that most students would experience increased confidence immediately after receiving new information about an unfamiliar topic.
This study provides an example of how a course that is traditionally delivered face-to-face can be designed to be delivered online, utilising less time and manpower resources while providing standardised teaching instruction in an evidence-based manner.
The qualitative findings in this study have not been replicated elsewhere, and provide an interesting perspective to student course perception. Students gained practical knowledge which is not readily available in clinical clerkships due to patient case variability and gained insight into an applicable framework for future clinical communication encounters. It is possible that the interactive nature of the course increased student presence and participation, resulting in improved learning outcomes in this aspect (Ammenwerth et al., 2019). Empathy, an important professional skill not easily taught but reflected as a learning point, was likely acquired through non-verbal communication demonstrated in the videos. Although it is not guaranteed that self-reported knowledge, skills and attitudes will translate into practice, future e-learning communication courses can be designed as pre-course material for traditional role-play facilitators to enhance learning experiences.
This study’s use of patient feedback provides unique insight into applied learning. Interestingly, the control group fared better in the actions of checking with caregivers/patients about management plan agreement and providing caregivers/patients with a summary. As clerkships also provide opportunities to observe healthcare professionals conducting clinical communication, it is likely that the control group learnt these behaviours from real-life encounters. Caregivers/patients tended to feel more comfortable with the intervention group, which could be explained through unmeasurable, subtle behaviours that the group may have learnt from the course, such as empathy, attentiveness and appropriate body language. Although the use of standardised patients for comparing both groups might have shown different results, it is known that how learners behave in the classroom and with real patients when unobserved is often less reflective of true workplace behaviours (Malhotra et al., 2009).
This study is limited by small participant and patient feedback numbers. Culturally, many patients forget their healthcare providers and experiences. An ideal situation would be direct clinical encounter observation, but due to the Hawthorne effect, a less truthful version of student behaviour may be observed instead.
V. CONCLUSION
Although online video-based communication courses can be used as a standardised teaching tool to improve student self-reported confidence levels and self-perceived knowledge, skills and attitudes, it remains to be proven if they can result in a change in student behaviour. It is likely that on-the-job experiences also contribute to their ability to demonstrate effective communication, which supports the supplementation, rather than the replacement of such practical experiences with online video-based course material.
Notes on Contributors
CC, CL and TKC contributed to the conception and design of the work. CC, CL and TKC also analysed data and drafted the work . CC, CL and TKC approved the final published version and are agreeable to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. CC, CL and TKC collectively contributed equally to this paper.
Ethical Approval
This study was exempted from formal Centralized Institutional Review Board review by the SingHealth Centralized Institutional Review Board (CIRB Ref: 2017/2178).
Acknowledgements
The authors would like to acknowledge the SingHealth Paediatrics Academic Clinical Programme in providing the grant funding for this project.
Funding
The study was funded by the SingHealth Paediatrics Academic Clinical Programme Tan Cheng Lim Fund Grant which was awarded in 2017 (Grant Reference: PAEDACP-TCL/2017/EDU/001).
Declaration of Interest
All authors disclose that there are no potential conflicts of interest, including financial, consultant, institutional and other relationships that could have direct or potential influence or impart bias on the work.
References
Ammenwerth. E., Hackl, W. O., Dornauer, V., Felderer, M., Hoerbst, A., Nantschev, R., & Netzer, M. (2019). Impact of students’ presence and course participation on learning outcome in co-operative online-based courses. Studies in Health Technology and Informatics, 262, 87-90.
Kemper, K. J., Foy, J. M., Wissow, L., & Shore, S. (2008). Enhancing communication skills for paediatric visits through on-line training using video demonstrations. BMC Medical Education, 8, 8.
Makoul, G. (2001). Essential elements of communication in medical encounters: the Kalamazoo consensus statement. Academic Medicine, 76(4), 390-393.
Malhotra, A., Gregory, I., Darvill, E., Goble, E., Pryce-Roberts, A., Lundberg, K., & Hafstad, H. (2009). Mind the gap: Learners’ perspectives on what they learn in communication compared to how they and others behave in the real world. Patient Education and Counseling, 76(3), 385-90.
Zimmer, K. P., Solomon, B. S., Siberry, G. K., & Serwint, J. R. (2008). Continuity-structured clinical observations: assessing the multiple-observer evaluation in a pae1diatric resident continuity clinic. Pediatrics, 121(6), e1633-1645.
*Cristelle Chow
Department of Paediatrics,
KK Women’s and Children’s Hospital
100 Bukit Timah Road,
Singapore 229899
Email: cristelle.chow.ct@singhealth.com.sg
Submitted: 8 February 2020
Accepted: 9 April 2020
Published online: 1 September, TAPS 2020, 5(3), 71-82
https://doi.org/10.29060/TAPS.2020-5-3/OA2226
May Eng Loo1, Brenda Wong2, Yee Mun Lee3
1Health Outcomes and Medical Education Research (HOMER), National Healthcare Group, Singapore; 2Group Education, National Healthcare Group, Singapore; 3Department of Urology, Tan Tock Seng Hospital, Singapore
Abstract
In order to understand what constitutes unprofessional online behaviour from the perspectives of stakeholders, there have been studies that examine the perceptions of doctors and the public on hypothetical online postings. However, the considerations and reasoning of the participants when they evaluate online posts have not been explored in-depth. This project aimed to examine the main considerations and possible conflicting considerations of faculty and residents when they evaluate the appropriateness of Facebook posts, and how they might negotiate any conflicts. Faculty and residents from the National Healthcare Group – Alexandra Health Pte Ltd Residency in Singapore were randomly presented Facebooks posts as part of an online questionnaire, rated their appropriateness, and provided explanations for their ratings. Responses were coded for main considerations and responses with 2 or more conflicting considerations were further analysed to describe the conflict and the way they were negotiated. 182 faculty and residents rated the appropriateness of three out of six Facebook posts and explained their evaluation. Except for one post which was evaluated as ‘Neither appropriate nor inappropriate’ by the majority (37%) of the respondents, all other posts were rated as either ‘Very inappropriate’ or ‘Inappropriate’ by the majority of respondents (34%-69%). Despite similar evaluation of inappropriateness, faculty and residents take into account a wide range of considerations. These considerations tend to conflict with one another when the respondents considered freedom of expression of the poster and the educational purpose of a post. Understanding physicians’ negotiation of conflicting considerations provides insight into their outworking of professionalism in social media context.
Keywords: Professionalism, Social Media, Postgraduate Education
Practice Highlights
- Doctors within the same Residency do not necessarily have a uniform set of professional priorities regarding social media.
- They may also have to manage conflicting professional and personal values in different contexts.
- Educators of professional values could recognise the complexity of such conflicts and be sensitive to this in their teaching.
- We recommend creating platforms for doctors to have conversations on social media use.
I. INTRODUCTION
In June 2017, Mark Zuckerberg announced that the Facebook community was officially two billion people. While seeking to understand how social media can be maximised for good, Chief Product Officer Chris Cox was conscious of Facebook’s responsibility to ‘curtail any way that it can be misused or turned into something sad’ (Constine, 2017). In healthcare education and practice, social media has both the potential to be maximised for good (e.g. facilitating communication and improving knowledge) as well as the potential to be misused, compromising patient confidentiality and eroding public confidence in the medical profession (Greysen, Kind, & Chretien, 2010; Hamm et al., 2013). In their commentary, Chretien and Kind (2014) propose that in order to reap the benefits of social media use for healthcare, physicians need to be first aware of the risks of using social media and address concerns of unprofessional online behaviour.
In order to understand what constitutes unprofessional online behaviour from the perspectives of stakeholders, there have been studies that examine the perceptions of doctors and the public on hypothetical online postings (Chretien, Farnan, Greysen, & Kind, 2011; Dawkins, King, Boateng, Nichols, & Desselle, 2017; Greysen et al., 2013; Jain et al., 2014; Kesselheim, Batra, Belmonte, Boland, & McGregor, 2014; Kind, Greysen, & Chretien, 2012; Rocha & de Castro, 2014). These studies found that online behaviour that participants judged as unprofessional include patient privacy violations, patient content in general and negative comments about faculty and staff. However, the considerations and reasoning of the participants when they evaluate online posts have not been explored in-depth, and especially for posts that may be inappropriate but may not appear obviously unprofessional. Such ‘grey posts’ may include patient storytelling posts where, for example, a patient’s identity is not revealed but details are shared to encourage reflection or request support through social media (Wells, Lehavot, & Isaac, 2015). Professional or personal values may sometimes come into conflict when they seem equally important in such situations. However, not much is known about what these conflicting considerations are when doctors evaluate such online posts and how these conflicting considerations are resolved or negotiated.
In response to concerns about unprofessional behaviour on social media, guidelines have been published by medical associations in various countries like the USA, UK, Canada, Australia, New Zealand as well as Singapore (American College of Physicians Ethics, Professionalism, and Human Rights Committee, 2012; Australian Medical Association, 2010; Canadian Medical Association, 2011; General Medical Council, 2013; Singapore Medical Council, 2016). These existing guidelines are generally comprehensive, providing principles for social media use and examples of unprofessional behaviour to avoid. Regarding posting online, concerns about patient confidentiality, professionalism, collegiality and preserving patients’ and the public trust in the medical profession are key issues raised by the guidelines. In particular, the Singapore Medical Council gives a list of inappropriate posts, examples include ‘speaking and writing in an indiscreet, bigoted, rude, and obscene or profane manner’ and ‘posting personal or derogatory comments about patients or colleagues’ (Singapore Medical Council, 2016).
Our study seeks to explore the considerations and possible competing or conflicting considerations of faculty and residents in the National Healthcare Group – Alexandra Health Pte Ltd (NHG-AHPL) Residency program when they evaluate online postings, especially grey posts. This study also aims to examine how the participants resolve or negotiate these conflicting considerations. Identifying the considerations of faculty and residents when they evaluate the posts sheds light on what constitutes unprofessional online posts and provides a platform for further discussion on existing social media use guidelines. Furthermore, understanding how doctors negotiate at times conflicting norms and obligations also provides insight into how they perceive the outworking of professionalism in the social media context.
II. METHODS
Six Facebook posts deemed inappropriate were identified from an online search. One author (L.M.E.) searched Google News on 30th June 2016 using a Boolean search: (social media OR Facebook OR twitter OR blog OR online OR internet OR web) AND (doctor OR physician OR medical student OR hospital OR clinic OR ward) AND (inappropriate OR unprofessional OR wrong OR unethical). The search was restricted to the first 20 pages of results (10 hits/page) and four posts (Posts 1, 2, 4 and 5) that appeared inappropriate but were not clearly unprofessional were selected. The remaining two posts (Post 3 and 6) were re-used from a pilot phase of the study. The characteristics of the posts are described in Table 1 and the screenshots of the six posts can be found in Appendix A.
|
|
Content domain |
Poster’s seniority |
Possible issues |
|
Post 1 |
Work: patient-related |
Not stated |
Breach of confidentiality, privacy |
|
Post 2 |
Personal: interpersonal conflict |
Medical student
|
Harsh language bordering on criminal threat |
|
Post 3 |
Work: patient-related |
Doctor |
Negativity towards patient, breach of confidentiality |
|
Post 4 |
Personal: opinion |
Medical student |
Harsh language on a controversial topic |
|
Post 5 |
Work: patient-related |
Junior doctor |
Breach of confidentiality, insensitive language |
|
Post 6 |
Work: colleague-related |
Intern |
Negativity towards colleague |
Table 1. Characteristics of posts
As part of an online questionnaire administered between 8th September and 30th October 2016 on social media use, faculty and residents from the NHG-AHPL Residency program in Singapore were asked to rate the appropriateness of three of these posts and to explain their evaluation. All respondents provided informed consent at the start of the questionnaire. Considerations were identified using structural coding which is a question-based code that acts as a labelling and indexing device (Saldana, 2012). For example, the following response was coded ‘Purpose’, ‘Language’ and ‘Respect’ based on the question “What do respondents consider when they evaluate posts?”
Someone has just died. Instead of showing empathy to the family of the deceased who had just lost a loved one, she uses swear words in a callous, insensitive way. Even though her intentions might have been good to ask people to wear a crash helmet, the way she said it was offensive and highly inappropriate given the circumstances. (F5.3)
In the first round of coding, two authors (L.M.E, B.W.) coded each response independently and resolved coding discrepancies through discussions. Using a codebook developed from the first round of coding as a guide, each response was revisited and coded. Coding discrepancies were resolved through more extensive discussions. The second round of coding added new codes to the codebook. Responses with two or more conflicting considerations were further analysed to describe the conflict and the way they were negotiated. Conflicting considerations were identified based on the plain reading of the response, prompted by the use of conjunctions such as ‘but’, ‘even though’ and ‘while’. Appendix B gives a full description of the codes used. Ethics approval was obtained from the institution’s Domain Specific Review Board.
III. RESULTS
A total of 182 respondents (36.8%)–64 faculty and 118 residents–rated the appropriateness of three out of six Facebook posts. 463 responses–169 responses from faculty and 294 responses from residents–were analysed. Table 2 provides a summary of the results for each post.
|
|
Evaluation of appropriateness |
Considerations |
Conflicting considerations |
|
Post 1 |
n=86 ‘Very inappropriate’ (34%)
‘Inappropriate’ (34%)
‘Neither appropriate nor inappropriate’ (30%).
‘Appropriate’ (1%)
‘Very appropriate’ (1%)
|
n=74 1. ‘Consent’ (n=41) 2. ‘Confidentiality’ (n=20) 3. ‘Context’ (n=11) 4. ‘Respect’ (n=10) 5.’Professionalism'(n=6) 6 ‘Purpose'(n=6) 7. ‘Consequences'(n=3) 8. ‘Language'(n=3) 9. ‘Safety'(n=3) 10. ‘Audience'(n=1) 11. ‘Behaviour'(n=1) 12. ‘Platform’(n=1) |
n=3 Positive tone of the post versus patient confidentiality, whether consent was taken, consequences and sensitivity towards the baby’s parents
|
|
Post 2 |
n=93 ‘Very inappropriate’ (39%)
‘Inappropriate’ (39%)
‘Neither appropriate nor inappropriate’ (18%)
‘Appropriate’ (3%)
|
n=77 1. ‘Platform’ (n=24) 2. ‘Behaviour’ (n=16) 3. ‘Freedom'(n=16) 4. ‘Professionalism’ (n=16) 5. ‘Lawfulness'(n=13) 6. ‘Method of resolution'(n=13). 7. ‘Language'(n=8) 8. ‘Reflection'(n=8) 9. ‘Audience'(n=3) 10. ‘Consequences'(n=2) 11. ‘Trends and norms'(n=2) 12. ‘Context'(n=1) 13. ‘Purpose'(n=1) 14. ‘Seniority'(n=1).
|
n=6 Personal nature of the post and the poster’s freedom to express his anger and how his anger is justifiable versus considerations of professionalism, the method used for resolution, consequences and lawfulness
Norms on the internet versus how the post reflects negatively upon the poster’s personality
|
|
Post 3 |
n=95 ‘Very inappropriate’ (36%)
‘Inappropriate’ (44%)
‘Neither appropriate nor inappropriate’ (20%)
‘Appropriate’ (0%)
‘Very appropriate’ (1%)*
|
n=81 1.‘Professionalism’ (n=48) 2. ‘Confidentiality’ (n=24) 3. ‘Platform’ (n=14) 4. ‘Consequences'(n=5) 5. ‘Language'(n=5) 6. ‘Reflection’(n=5) 7. ‘Boundary’(n=4) 8. ‘Freedom’(n=4) 9. ‘Purpose'(n=4) 10. ‘Behaviour'(n=2) 11. ‘Method of resolution'(n=2) 12. ‘Audience'(n=1)
|
n=4 Poster’s right to state a fact or express his feelings and poster posting in jest versus considerations of professionalism
|
|
Post 4 |
n=96
‘Very inappropriate’ (27%)
‘Inappropriate’ (28%)
‘Neither appropriate nor inappropriate’ (37%)
‘Appropriate’ (4%)
‘Very appropriate’ (1%)*
No response (1%)
|
n=79 1. ‘Freedom’ (n=33) 2. ‘Behaviour’ (n=14) 3. ‘Context’ (n=13) 4. ‘Platform’ (n=11) 5. ‘Language’ (n=8) 6. ‘Professionalism’ (n=7) 7.‘Boundary’ (n=6) 8. ‘Trends and norms’ (n=5) 9. ‘Consequences’ (n=3) 10. ‘Method of resolution’ (n=3) 11. ‘Anonymity’ (n=2) 12. ‘Respect’ (n=2) 13. ‘Audience’ (n=1) 14. ‘Confidentiality’ (n=1).
|
n=13 Poster’s freedom to express his personal opinion versus considerations, of professionalism, language, audience, behaviour, context, platform and consequences.
Norms on social media versus harsh language |
|
Post 5 |
n=91 ‘Very inappropriate’ (24%)
‘Inappropriate’(42%)
‘Neither appropriate nor inappropriate’ (24%)
‘Appropriate’(1%)
‘Very appropriate’ (9%)
|
n=79 1. ‘Confidentiality’ (n=38) 2. ‘Language’ (n=24) 3. ‘Purpose’ (n=23) 4. ‘Respect’ (n=17) 5. ‘Professionalism’ (n=10) 6. ‘Behaviour'(n=8) 7. ‘Platform'(n=7) 8. ‘Audience’(n=6) 9. ‘Consequences’(n=4) 10. ‘Freedom’(n=4) 11. ‘Boundary'(n=1) 12. ‘Context'(n=1) 13. ‘Reflection'(n=1) 14. ‘Trends and norms'(n=1)
|
n=15 Educational message versus considerations of language and tone, respect, platform, audience and consequences
Freedom of the poster to post what she wants without patient identifiers versus consideration of the language used |
|
Post 6 |
n=89 ‘Very inappropriate’(69%)
‘Inappropriate’ (20%)
‘Neither appropriate nor inappropriate’ (4%)
‘Appropriate’ (0%)
‘Very appropriate’ (2%)
No response (2%)
|
n=91 1.‘Platform’ (n=22) 2. ‘Collegiality’ (n=21) 3.’Method of resolution’ (n=20) 4. ‘Professionalism’ (n=18) 5. ‘Consequences’ (n=13) 6. ‘Language'(n=11) 7. ‘Lawfulness’(n=6) 8. ‘Confidentiality’(n=4) 9. ‘Behaviour’(n=3) 10. ‘Context'(n=3) 11.’Anonymity'(n=2) 12. ‘Freedom’ (n=1) 13. ‘Purpose’ (n=1) 14. ‘Respect'(n=1)
|
n=1 Consideration that the poster might be trying to resolve an issue versus considerations of the inappropriateness of the post in terms of collegiality |
Table 2. Summary of results for Posts 1-6
A. Evaluation and Considerations
Except for Post 4 which was evaluated as ‘Neither appropriate nor inappropriate’ by the majority (37%) of the respondents, all other posts were rated as either ‘Very inappropriate’ or ‘Inappropriate’ by the majority of respondents (34%-69%). In particular, Post 5 has a relatively high proportion of respondents (10%) rating it as either ‘Appropriate’ or ‘Very appropriate’. Respondents have a broad range of considerations with ‘Professionalism’, ‘Language’, ‘Behaviour’ and ‘Platform’ repeated across all six posts.
‘Platform’ was the main consideration for Post 2 and Post 6. Respondents considered the inappropriateness of posting on a public platform what should only be said or done in private, “FB is a public forum. People should settle personal grievances NOT online but privately” (R2.57; Post 2); “Publicly criticizing a colleague is inappropriate. Feedback should always be given in a private setting” (R6.33; Post 6).
For the other posts, the main considerations were ‘Consent’ (Post 1), ‘Professionalism’ (Post 3), ‘Freedom’ (Post 4) and ‘Confidentiality’ (Post 5). More than half of the respondents (55%) for Post 1 considered whether consent or permission was obtained before posting. For Post 3, more than half of the respondents (59%) considered professionalism generally or more specifically in terms of attitude. For Post 4, 42% of the respondents considered the freedom of speech of the poster including the freedom of the poster to post personal matters in a personal capacity, with personal accountability. Confidentiality and privacy of patients was considered by 24% of respondents on Post 5.
B. Negotiation of Conflicting Considerations
Among the six posts, Post 5 had the most number of respondents with conflicting considerations (n=15), followed by Post 4 (n=13).
For Post 5, fourteen respondents considered that the poster has an educational purpose versus other considerations and one respondent considered freedom of expression versus language. To negotiate the conflicting considerations for Post 5, six respondents reasoned that the educational message of the post and the poster’s good intentions need to be subjected to (or at least seen in the light of) considerations of confidentiality, language, professionalism and respect. For example, two faculty members, F5.3 and F5.5, thought that although the poster had good intentions and the message was educational, her language and tone were inappropriate.
Someone has just died. Instead of showing empathy to the family of the deceased who had just lost a loved one, she uses swear words in a callous, insensitive way. Even though her intentions might have been good to ask people to wear a crash helmet, the way she said it was offensive and highly inappropriate given the circumstances (F5.3).
F5.5 also considered the possible identification of the victim, “although message was ‘correct’ strong language including expletives used which is inappropriate timing and location of post may allow identification of victim” (F5.5).
However, there were nine respondents for Post 5 who considered educational purpose and freedom of expression at the same level of importance as other considerations. Rating Post 5 as ‘Neither inappropriate nor appropriate’, F5.6 reasoned that the possible breach in Professionalism/Confidentiality may be justified by educational purpose, “I don’t think it’s appropriate to talk about patient experiences on Facebook but I believe she has done so with the intention of encouraging others to wear helmets” while R5.39 reasoned that the inappropriate language use may also be justified by the freedom of the poster to say what she wants as long as there were no patient identifiers, “While her choice of words may not be the best, there were no patient identifiers. Again, she can say what she wants”.
For Post 4 which had 13 respondents with conflicting considerations, 12 respondents considered that the poster should have the freedom to express his personal opinion versus a variety of other considerations, including that of ‘Professionalism’,’ Language’, ‘Audience’,’ Behaviour’, ‘Context’, ‘Platform’ and ‘Consequences’. One respondent considered norms on social media versus the harsh language used.
To negotiate the conflicting considerations for Post 4, six respondents prioritised professionalism and other considerations like audience and consequences over freedom of expression. For example, a resident reasoned that while medical professionals can have their own political views, the poster should consider the possible consequences of such a post being seen by a wider audience and being used against him, “Everyone is entitled to his own view, medical professionals can have their own political views, but caution needs to be exercised if this information is used against him. might need to restrict to close friends only” (R4.43).
Seven respondents, however, considered freedom of expression and norms on social media at the same level of importance as other considerations. For example, respondents R4.51 and R4.60 rated Post 4 as ‘Neither inappropriate nor appropriate’. They reasoned that the harsh language used or the negative consequences of the post may be justified by the poster’s entitlement to freedom of expression, “He is entitled to his beliefs and freedom of speech about political and religious issues. Even though these comments are harsh and mean, we can’t possibly control how everyone speaks” (R 4.51); “Everyone is entitled to free speech and he has every right to say what he wants. But again this does not look good on his reputation” (R 4.60).
The number of respondents with conflicting considerations for the other posts ranged from 1 to 6. In general, respondents negotiated the conflicting considerations mainly by prioritising professionalism over and above the other considerations.
IV. DISCUSSION
A total of 182 faculty and residents (36.8%) from the NHG-AHPL Residency program in Singapore rated the appropriateness of Facebook posts and 463 evaluation responses were analysed. One of three postgraduate medical education programs in Singapore, the NHG-AHPL Residency comprises 27 residency programs within a few institutions including hospitals and nine polyclinics. Faculty and residents who explained their evaluation took into account a wide range of considerations and these considerations tended to conflict with one another when the respondents considered freedom of expression of the poster and the educational purpose of a post. These findings suggest that doctors within the same Residency do not necessarily have a uniform set of professional priorities and may have to manage conflicting professional and personal values in different contexts. The teaching and evaluation of professionalism should thus increasingly take conflict and context into consideration (Ginsburg et al., 2000). Educators of professional values could recognise the complexity of such conflicts and be sensitive to this in their teaching, whether formally or informally.
Freedom of speech or expression appears to be a recurrent consideration for posts not just in the personal domain (Posts 2 and 4) but also those in the work-related domain as well (Posts 3 and 5). Given that freedom of expression is not commonly encouraged or emphasised in Asian cultures (Kim & Sherman, 2007), it may be somewhat surprising that this was a recurrent consideration for doctors in Singapore. This consideration thus deserves more attention from developers of social media use guidelines and online professionalism course facilitators who can seek to start addressing these considerations by first recognising and acknowledging them. While existing social media guidelines could and should be tempered by recognising doctors’ right to free speech, doctors and medical students would also need to exercise critical judgment to consider whether their freedom of expression is appropriate in view of the guidelines (Farnan et al., 2009).
This study found that the post that elicited the most number of conflicting considerations was Post 5. This post by a junior doctor contained insensitive language and patient-related content but had an educational purpose. It is unclear whether if the post had been written more sensitively, it would elicit even more conflicting considerations. This may be a valid cause for concern given the potential negative consequences of such posts (Wells et al., 2015). Although the victim was not named, it is still possible that enough details are given for him to be identified. Such a post may also violate family members’ expectations of privacy. Public trust could also possibly be undermined because of the insensitivity and lack of empathy displayed by a doctor. It may be helpful for faculty to engage residents or students with such issues informally or formally during relevant courses and to explore alternative avenues for patient storytelling.
Based on the findings of our study, we recommend creating platforms for conversations on social media use to take place among faculty and residents. Using existing social media use guidelines and relevant findings from studies as material for discussion, faculty and residents could consider various perspectives, discuss how guidelines may moderate some considerations and explore further considerations arising from the conversation. Discussions like these require doctors to exercise critical judgments on ethical dilemmas and arrive at possible ways to negotiate conflicting considerations in various circumstances within the social media context. In her commentary on social media and medical professionalism, Fenwick (2014) discusses how doctors in contemporary practice must deal with conflicting priorities and urges a more pluralistic approach to understanding the notion of professionalism while thinking critically about social media’s current and future implications for practice. Such conversations can provide opportunities for the doctors to do so and perhaps more crucially, to consider how social media can be used creatively for better patient and health outcomes.
In a recent systematic review on the use of social media in graduate medical education, the authors found ten studies pertaining to resident professionalism (Sterling, Leung, Wright, & Bishop, 2017). However, most were exploratory, surveying residents about their social network behaviour and exploring how program directors use social media to monitor unprofessional behaviour of residents. Although our study was limited to the faculty and residents in one Residency in Singapore, to our knowledge, this is the first study to shed light on how residents as well as faculty negotiate conflicting considerations when evaluating online posts. Instead of hypothetical Facebook posts (whereby it would be possible to address potential biases by varying factors like the age or gender of the poster), we used authentic posts (except Post 6) which respondents might find more relevant and might be more motivated to evaluate and discuss them. Another limitation of the study was that we did not consider how factors like the respondents’ age, type of residency program or their actual usage of social media may influence their evaluation of the posts. However, we followed a systematic, transparent process for coding the written responses and we achieved a high interrater reliability through extensive discussions.
Future work should focus on understanding the complexities of how doctors negotiate conflicting professional values. In this study, respondents were asked to explain their evaluation after rating the appropriateness of the posts and the length of responses varied from one word to several sentences. Due to the limitation of such a study design, the reasoning process of some respondents could not be examined. Conducting interviews or focus groups could enable more in-depth analysis of how participants negotiate conflicting values. Research in moral psychology has shed light on how a person makes moral judgments. According to cognitive developmentalists a person may spontaneously have a new intuition that contradicts the initial intuitive judgment during the course of thinking about a situation (Kohlberg, 1969; Piaget, 1965). He/she comes to see a dilemma from more than one perspective and experiences competing intuitions. In particular, focus-group discussions could shed light on how the moral judgments of participants in the group might influence one another (Haidt, 2001). Studies designed to focus on examining how doctors resolve conflicting professional values can deepen our understanding of medical professionalism and what it constitutes, within the social media context and beyond.
V. CONCLUSION
This study aimed to explore the considerations and possible competing or conflicting considerations of faculty and residents in the NHG-AHPL Residency program when they evaluate online postings, especially grey posts. Faculty and residents who explained their evaluation took into account a wide range of considerations and these considerations tended to conflict with one another when the respondents considered freedom of expression of the poster and the educational purpose of a post. These findings suggest that doctors within the same Residency do not necessarily have a uniform set of professional priorities and may have to manage conflicting professional and personal values in different contexts. Educators of professional values could recognise the complexity of such conflicts and be sensitive to this in their teaching, whether formally or informally. We recommend creating platforms for conversations on social media use to take place among faculty and residents.
Notes on Contributors
Ms Loo May Eng is Research Analyst at Health Outcomes and Medical Education Research (HOMER), National Healthcare Group. She is the primary author of this manuscript and was involved in the study design, data collection and analysis of this project.
Dr Lee Yee Mun is Senior Consultant at the Department of Urology, Tan Tock Seng Hospital. He was involved in the conceptualisation of this project.
Ms Brenda Wong is Program Coordinator at Group Education, National Healthcare Group. She was involved in data collection and analysis.
Ethical Approval
Ethics approval was obtained from the institution’s Domain Specific Review Board (NHG DSRB Ref: 2015/00584).
Acknowledgements
The authors would like to thank all residents and faculty who participated in the questionnaire.
Funding
The research did not receive any specific grant from funding agencies.
Declaration of Interest
There is no conflict of interest to declare.
References
American College of Physicians Ethics, Professionalism, and Human Rights Committee. (2012). American College of Physicians Ethics Manual: Sixth edition. Annals of Internal Medicine, 156(1 Pt 2), 73–104. https://doi.org/10.7326/0003-4819-156-1-201201031-00001
Australian Medical Association. (2010). Social media and the medical profession. Retrieved from https://ama.com.au/article/social-media-and-medical-profession
Canadian Medical Association. (2011). Social media and Canadian physicians: Issues and rules of engagement. Retrieved from https://www.cma.ca/En/Pages/social-media-use.aspx
Chretien, K. C., Farnan, J. M., Greysen, S. R., & Kind, T. (2011). To friend or not to friend? Social networking and faculty perceptions of online professionalism. Academic Medicine, 86(12), 1545-1550. https://doi.org/10.1097/ACM.0b013e3182356128
Chretien, K. C., & Kind, T. (2014). Climbing social media in medicine’s hierarchy of needs. Academic Medicine, 89(10), 1318–1320. https://doi.org/10.1097/ACM.0000000000000430
Constine, J. (2017, June 27). Facebook now has 2 billion monthly users… and responsibility. Retrieved October 20, 2017, from TechCrunch website http://social.techcrunch.com/2017/06/27/facebook-2-billion-users/
Dawkins, R., King, W. D., Boateng, B., Nichols, M., & Desselle, B. C. (2017). Pediatric residents’ perceptions of potential professionalism violations on social media: A US national survey. JMIR Medical Education, 3(1). https://doi.org/10.2196/mededu.5993
Farnan, J. M., Paro, J. A. M., Higa, J. T., Reddy, S. T., Humphrey, H. J., & Arora, V. M. (2009). Commentary: The relationship status of digital media and professionalism: it’s complicated. Academic Medicine, 84(11), 1479–1481. https://doi.org/10.1097/ACM.0b013e3181bb17af
Fenwick, T. (2014). Social media and medical professionalism: Rethinking the debate and the way forward. Academic Medicine, 89 (10), 1331–1334. https://doi.org/10.1097/ACM.0000000000000436
General Medical Council. (2013). Doctors’ use of social media. Retrieved from http://www.gmc-uk.org/guidance/ethical_guidance/21186.asp
Ginsburg, S., Regehr, G., Hatala, R., McNaughton, N., Frohna, A., Hodges, B., … Stern, D. (2000). Context, conflict, and resolution: A new conceptual framework for evaluating professionalism. Academic Medicine, 75(Supplement), S6–S11.
Greysen, S. R., Johnson, D., Kind, T., Chretien, K. C., Gross, C. P., Young, A., & Chaudhry, H. J. (2013). Online professionalism investigations by state medical boards: First, do no harm. Annals of Internal Medicine, 158(2), 124–130. https://doi.org/10.7326/0003-4819-158-2-201301150-00008
Greysen, S. R., Kind, T., & Chretien, K. C. (2010). Online Professionalism and the Mirror of Social Media. Journal of General Internal Medicine, 25(11), 1227–1229. https://doi.org/10.1007/s11606-010-1447-1
Haidt, J. (2001). The emotional dog and its rational tail: A social intuitionist approach to moral judgment. Psychological Review, 108 (4), 814–834.
Hamm, M. P., Chisholm, A., Shulhan, J., Milne, A., Scott, S. D., Klassen, T. P., & Hartling, L. (2013). Social media use by health care professionals and trainees: A scoping review. Academic Medicine, 88(9), 1376–1383. https://doi.org/10.1097/ACM.0b013e31829eb91c
Jain, A., Petty, E. M., Jaber, R. M., Tackett, S., Purkiss, J., Fitzgerald, J., & White, C. (2014). What is appropriate to post on social media? Ratings from students, faculty members and the public. Medical Education, 48(2), 157–169. https://doi.org/10.1111/medu.12282
Kesselheim, J. C., Batra, M., Belmonte, F., Boland, K. A., & McGregor, R. S. (2014). New professionalism challenges in medical training: An exploration of social networking. Journal of Graduate Medical Education, 6(1), 100–105. https://doi.org/10.4300/JGME-D-13-00132.1
Kim, H. S., & Sherman, D. K. (2007). “Express yourself”: Culture and the effect of self-expression on choice. Journal of Personality and Social Psychology, 92(1), 1-11. https://doi.org/10.1037/0022-3514.92.1.1
Kind, T., Greysen, S. R., & Chretien, K. C. (2012). Pediatric clerkship directors’ social networking use and perceptions of online professionalism. Academic Pediatrics, 12(2), 142–148. https://doi.org/10.1016/j.acap.2011.12.003
Kohlberg, L. (1969). Stage and sequence: The cognitive development approach to socialization. In D. Goslin (Ed.), Handbook of socialization theory (pp. 347–480). Chicago: Rand McNally.
Piaget, J. (1965). The moral judgment of the child. Retrieved from http://archive.org/details/moraljudgmentoft005613mbp
Rocha, P. N., & de Castro, N. A. A. (2014). Opinions of students from a Brazilian medical school regarding online professionalism. Journal of General Internal Medicine, 29(5), 758–764. https://doi.org/10.1007/s11606-013-2748-y
Saldana, J. (2012). The Coding Manual for Qualitative Researchers. London: SAGE.
Singapore Medical Council. (2016). smc handbook on medical ethics. Retrieved from http://www.healthprofessionals.gov.sg/content/hprof/smc/en/topnav/guidelines/ethical_code_and_ethical_guidelines.html
Sterling, M., Leung, P., Wright, D., & Bishop, T. F. (2017). The Use of Social Media in Graduate Medical Education: A Systematic Review. Academic Medicine, 92(7), 1043–1056. https://doi.org/10.1097/ACM.0000000000001617
Wells, D. M., Lehavot, K., & Isaac, M. L. (2015). Sounding Off on Social Media: The Ethics of Patient Storytelling in the Modern Era. Academic Medicine, 90(8), 1015–1019. https://doi.org/10.1097/ACM.0000000000000668
*Loo May Eng
Health Outcomes and Medical Education Research,
National Healthcare Group
Tel: (65) 6359 6362
Email: may_eng_loo@nhg.com.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









