A comparison of four models of professionalism in medical education
Submitted: 25 May 2020
Accepted: 30 December 2020
Published online: 13 July, TAPS 2021, 6(3), 24-31
https://doi.org/10.29060/TAPS.2021-6-3/RA2314
Maria Isabel Atienza
Curriculum and Instruction, College of Medicine, San Beda University, Philippines
Institute of Pediatrics & Child Health, St. Luke’s Medical Center, Global City, Philippines
Abstract
Introduction: The prevailing consensus is that medical professionalism must be formally included as a programme in the undergraduate medical curriculum.
Methods: A literature search was conducted to identify institutions that can serve as models for incorporating professionalism in medical education. Differences and similarities were highlighted based on a framework for the comparison which included the following features: Definition of professionalism, curricular design, student selection, teaching and learning innovations, role modelling and methods of assessment.
Results: Four models for integrating professionalism in medical education were chosen: Vanderbilt University School of Medicine (VUSM), University of Washington School of Medicine (UWSOM), University of Queensland (UQ) School of Medicine, and Mayo Clinic and Mayo Medical School. The task of preparing a programme on medical professionalism requires a well-described definition to set the direction for planning, implementing, and institutionalising professionalism. The programmes are best woven in all levels of medical education from the pre-clinical to the clinical years. The faculty physicians and the rest of the institution’s staff must also undergo a similar programme for professionalism.
Conclusion: The development of all scopes of professionalism requires constant planning, feedback and remediation. The students’ ability to handle professionalism challenges are related to how much learning situations the students encounter during medical school. The learning situations must be adjusted according to the level of responsibilities given to students. The goal of learning is to enable students to grow from a novice to a competent level and afterwards to a proficient and expert level handling professionalism challenges in medicine.
Keywords: Medical Professionalism, Medical Curriculum, Role Modelling in Medical Education, Culture of Medical Professionalism
Practice Highlights
- A programme on medical professionalism in education starts with a working definition of the term.
- The culture of professionalism must be articulated in the school’s vision and mission.
- The professionalism programme must be woven through the four years of medical education.
- Role models are essential in teaching medical professionalism.
- For teaching medical professionalism, a nurturing environment is preferable over punitive actions.
I. INTRODUCTION
There is a prevailing sentiment that professionalism must be taught formally and explicitly in all medical schools (Cruess & Cruess, 2006). This review aims to highlight some exceptional models for incorporating professionalism in the curriculum of medical education. The models were chosen based on the consensus among medical educators that medical schools need to respond to the following observations and recommendations from the vast literature on this subject:
1. Society expects physicians to act professionally (Lynch et al., 2004; Mueller, 2009; O’Sullivan et al., 2012).
2. There is a link between unprofessional behaviour in medical school and subsequent practice (Mueller, 2009; O’Sullivan et al., 2012; Parker et al., 2008).
3. Professionalism is associated with improved medical outcomes (Mueller, 2009).
4. Professionalism needs to be taught in the undergraduate medical institutions (O’Sullivan et al., 2012).
5. The teaching and learning must be coupled with a carefully constructed means of assessment of professionalism and professional behaviour (O’Sullivan et al., 2012).
6.Students must be supported in developing the skills for continuing professional development throughout their career (O’Sullivan et al., 2012).
This review aims to utilise these assumptions as a framework for reviewing and comparing models for the incorporation of medical professionalism in the curriculum of medical schools. This paper aims to provide answers to this question: Among medical schools that have incorporated professionalism in the medical curriculum, what are the salient features of the programmes that may be adopted by other institutions in need of such curricular innovations?
II. METHODOLOGY
A literature search was conducted to search for relevant institutions that have established a programme for incorporating professionalism in their medical schools. There was no attempt to review all published reports but to focus on the schools that can serve as models for other institutions in need of such curricular innovations. All information concerning the programmes were taken from the published journal articles which were authored by the faculty members in charge of the respective programmes on professionalism. An independent appraisal was done using a framework adopted from a systematic review by Passi and co-workers which included the following criteria: institutional definition of professionalism, curricular design, student selection, teaching and learning innovations, role modelling and assessment (Passi et al., 2010).
III. RESULTS
The review of literature on undergraduate medical programmes on professionalism revealed four notable models that describe how their institutions have integrated the teaching and assessment of professionalism among medical students, namely, Vanderbilt University School of Medicine (VUSM), University of Washington School of Medicine (UWSOM), University of Queensland (UQ) School of Medicine, and Mayo Clinic School of Medicine.
A. Vanderbilt University School of Medicine (VUSM)
A model applied at the VUSM focused on an Academic Leadership Programme (ALP) established to address unprofessional and disruptive behaviours of students (Hickson et al., 2007). The ALP is a programme designed for leaders and administrators tasked to identify and tackle unprofessional behaviours. A four-level graduated intervention programme was designed to deal with the incident cases occurring in the school. The tenets of professionalism are introduced to the medical students through a discussion of case vignettes dealing with unprofessional behaviour. The faculty are also asked to sign a creed and a commitment to be role models of professional behaviour for graduates and medical students.
A so-called “disruptive behaviour pyramid” serves as a guide for identifying and assessing variable degrees of unprofessional behaviour with their corresponding intervention. Surveillance systems have also been put in place to detect unprofessional behaviour of students and physicians from patients, visitors, and health care team members (Hickson et al., 2007).
B. University of Washington School of Medicine (UWSOM)
The UWSOM introduced their professionalism curriculum through the development of the Colleges programme for the preclinical medical students. Outstanding faculty-clinicians are selected and trained to teach and model clinical skills with small groups of students at the bedside from the second-year level until the time of their graduation. The institution recognises these faculty as role model physicians working closely with students in the care of patients (Goldstein et al., 2006).
The school promotes an “ecology of professionalism” in the campus and provides an environment for group discussions, role modelling and reflection among the different year levels of medical education. Professionalism is an institution wide concern such that both students and the faculty are required to undergo training on professionalism. In order to make the programme more meaningful, the institution added the “Patients as Teachers” project whereby the patients are asked to provide feedback and to offer advice to the medical students. The loop of learning involving the faculty, the students, and the patient is deemed as a “safe” and respectful educational environment that encourages professionalism as an institutional-wide responsibility (Goldstein et al., 2006).
C. University of Queensland (UQ) School of Medicine
The programme of the University of Queensland integrates medical ethics, law and the professionalism curriculum with a “Personal and Professional Development” process (Parker et al., 2008). Throughout the four-year levels of undergraduate medical education, topics of ethics and professional development are taught and assessed through written tests and objective structured clinical examinations. A document called “Commitment to Professionalism” is signed by every student at the start of their first-year level to reinforce the principles and their acceptance of the expectations of the school, including attendance.
A “Pyramid of Professionalism” serves as a model to identify the students that require supervision and eventually pass or fail the programme. Students are assessed at several levels with a committee providing support, feedback and remediation. Professional conduct ultimately affects the student’s promotion to the next year level (Parker et al., 2008).
D. Mayo Clinic School of Medicine
The Mayo Clinic incorporated professionalism into medical education by first articulating its culture through a statement of the institution’s primary value: “The needs of the patient come first”. Their mission statement declares that “Mayo will provide the best care to every patient every day through integrated clinical practice, education, and research.” This culture is expressed in all the institution’s policies and procedures (Mueller, 2009).
Mayo has adopted a framework for professionalism which places clinical competence, communication skills and sound understanding of ethics at its foundation (Mueller, 2015). Built on this foundation are the pillars or the key attributes of accountability, altruism, excellence and humanism. With this framework and the culture that Mayo promotes, professionalism teaching and assessment programmes have been implemented involving all levels of learners of the Mayo Clinic School of Medicine. An intensive bioethics courses and a leadership and professionalism course is given to the first-year medical students. For the second-year level, the “Advance Doctoring” professionalism reflective writing programme is given. For the third-year level, the “Safe Harbor” professionalism programme and an intensive bioethics course is applied (Mueller, 2009; Mueller, 2015).
More professionalism and ethics teaching are incorporated into different courses and clinical rotations throughout the four-year curriculum. Other interesting features include an elective course in Professionalism and Ethics related to the students’ career interest. Professionalism assessments are carried out by way of formative and summative feedback and professionalism “portfolios” which are summarized for their future applications for further training (Mueller, 2009; Mueller, 2015).
The Mayo Clinic faculty physicians also have their share of professionalism modules. The new physician staff are required to attend a complete series of professionalism courses. All faculty physicians have to take a complete web-based, interactive module on professionalism in order to maintain their status as practicing physicians. They also undergo a 360-degree review to identify and address lapses in professionalism. The non-physician allied healthcare staff of the institution also have their own professionalism programme to support Mayo’s service philosophy (Mueller, 2009; Mueller, 2015).
The core value of professionalism continues to guide the clinic in its leadership practices and management strategies. The value-based culture serves as a positive hidden curriculum that promotes the achievement of desired educational outcomes among the health care professionals (Viggiano et al., 2007).
E. Institutional Definitions of Medical Professionalism
The lack of a universal definition of medical professionalism has resulted in medical schools formulating what is suitable to their context (O’Sullivan et al., 2012). Among the four curricular models, Mayo clearly expounded on their definition of medical professionalism. This institution defined professionalism by embracing seven patient care-related and seven practice environment-related attributes as summarised in the Mayo Clinic Model of Care (Mueller, 2009).
In the case of UQ, while no clear-cut definition of professionalism was described in the journal article, the institution instead presented a list of topics of medical ethics and professional development for formal training and instruction. A review of the UQ listing shows that most of the elements of professionalism covered were related to the theme of public or societal professionalism, such as Medical Practice and the Law, Accountability and Self-Regulation, Inappropriate Practice and Medical Over servicing, and Commercialization of Medicine (Parker et al., 2008).
A second list of elements of professionalism was prepared by the UQ faculty, and this list contained attributes related to intrapersonal and interpersonal professionalism. This list served as their guide to identify students who required support, feedback or remediation through the process called the Pyramid of Professionalism (Parker et al., 2008).
The VUSM also did not state the elements of professionalism in their model. Instead, the institution focused on defining the unprofessional or disruptive behaviours that required case discussions in particular year levels of medical education. These were the same unacceptable behaviours that were used to identify students who needed immediate intervention ranging from non-punitive interventions up to the imposition of disciplinary processes if needed (Hickson et al., 2007).
The UWSOM developed a list of elements of professionalism that served as benchmarks for preclinical students, namely, the principles of altruism, honour and integrity, compassion, communication, respect, accountability and responsibility, scholarship, excellence and leadership. Despite this listing, the faculty received feedback from the students that the idea of professionalism and cultural competency remained unclear to them. This feedback came with a request from the students that the teaching of professionalism should be “more specific, clinically relevant, and challenging” (Goldstein et al., 2006).
F. Comparison of Programme Implementation
A systematic review (Passi et al., 2010) was done with the aim to summarise the evidence on methods used by medical schools to promote medical professionalism. Five main strategic areas to promote the development of professionalism in medical education were identified from the review: Curriculum design, student selection, teaching and learning methods, role modelling and assessment methods. These five areas can be used as guideposts in reviewing school programmes on professionalism. Table 1 shows a comparison of the four models presented earlier.
G. Similar Features in the Four Models
These are the features common to all four models: (1) Commitment of the leadership of the institution to embark on integrating professionalism into the curriculum, (2) Built-in programme for training of faculty for teaching and modelling of clinical skills, and (3) Vertical integration of the programme of professionalism from preclinical to clinical years.
These features are significant means to heighten the attention of both students and faculty to the need for growth in the area of professionalism. This will also help institutionalize professionalism. The journals on the models did not mention any policy regarding the screening for unprofessional behaviour during the student selection process.
H. Differences in the Four Models
Major differences are evident in the approach to teaching professionalism in the four curricular models.
1) The formal teaching and learning experience of the students of the four schools were varied in terms of duration and delivery of instruction: UWSOM and Mayo incorporates a formal course throughout the four years of medical education. In Mayo, all faculty physicians are trained and involved in the training of students for professionalism. UWSOM, on the other hand, has a select group of thirty faculty assigned for this purpose. UQ described a formal course on professionalism in the first two years of medical education. After the first 2 years, UQ proceeds to the clinical years of medical education using the personal and professional development (PPD) process of identifying personal and professional shortcomings among the students.
The approach taken by VUSM is more interventional in nature. Although short problem-based discussions are provided in the four-year levels of medical education, the main thrust of the programme is on identifying and rectifying incident cases of unprofessional behaviour. Its basis rests on the idea that “failing to address unprofessional behaviour simply promotes more of it.” The VUSM model mentions four graduated interventions as a disciplinary measure to address unprofessional behaviour.
2) The four schools also differed in their assessment methods: VUSM focuses on immediate recognition and grading using the “disruptive behaviour pyramid” to determine the appropriate intervention. UWSOM uses reflection and feedback in the preclinical years followed by a “closed loop” system of obtaining feedback from patients and faculty. Deficiencies in professional behaviour are identified so that remediation may be provided to ensure that only students who are ready will graduate or advance to the next year (Hickson et al., 2007).
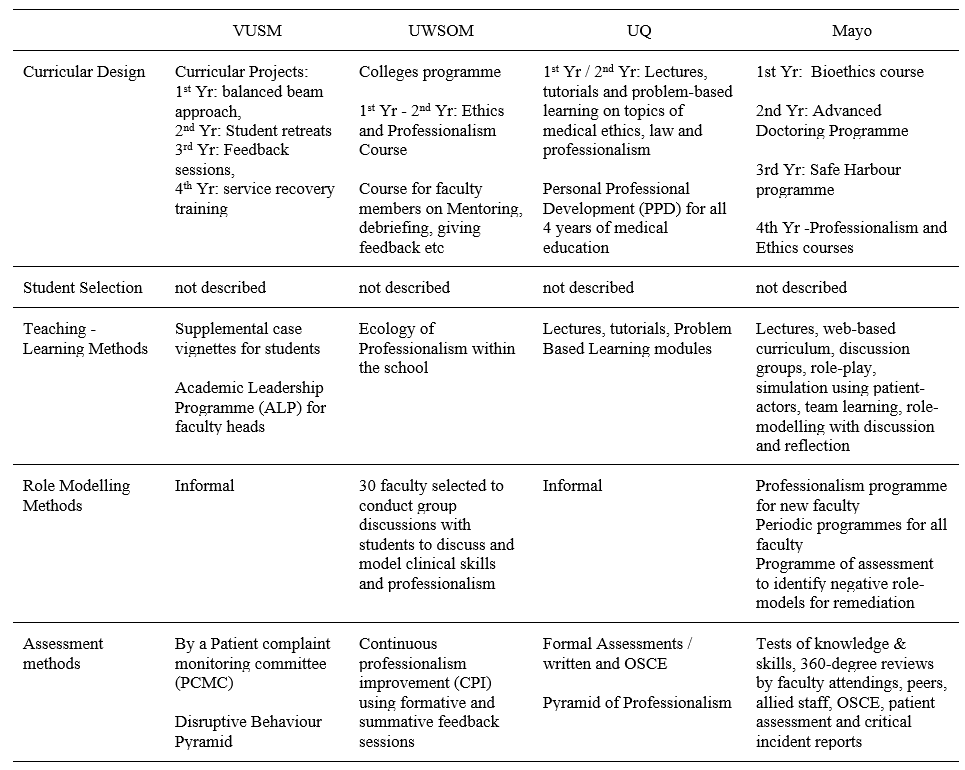
(Goldstein et al., 2006; Hickson et al., 2007; Mueller, 2009; Mueller, 2015; Parker et al., 2008)Table 1. Comparative Summary of Four Models of Educational Programme for Teaching Medical Professionalism
UQ focuses more on written tests and objective structured clinical examinations (OSCE) in the preclinical years. Because the school recognises that these assessment methods may not necessarily measure actual attitudes, the personal and professional development (PPD) process serves as a means directed towards identifying students with problems who are then referred to a committee for support and remediation (Parker et al., 2008).
Mayo has a more comprehensive assessment method by including a 360-degree review from faculty attendings, peers, allied staff and patients to complement the written tests and OSCE (Mueller, 2009).
3) Role modelling: On the area of role modelling, UWSOM has developed a formal programme to train select faculty members to promote role modelling as a means of teaching students. The programme to promote an “ecology of professionalism” within the institution is unique to UWSOM. This is the school’s way of making professionalism an institution-wide responsibility and yet maintains a “safe” educational environment for learning and improvement (Goldstein et al., 2006).
Mayo, on the other hand, has required all faculty and staff physicians to attend and successfully complete a series of modules on professionalism, physician-patient communication, self-awareness, and diversity. Maintaining the culture of professionalism in the Mayo Clinic is a result of a continuing process of allowing ethics and professionalism to be woven into the courses and clinical rotations (Mueller, 2009).
I. Professionalism in Medical Education in the Future
Much progress has been attained in the last decade when various models for incorporating professionalism in medical education have been disseminated in various journals. The Bioethics Core Curriculum introduced by the UNESCO also declared that bioethical principles and human rights must be taught early to medical students and that Medical Ethics, which is a branch of Bioethics, must be taught in all levels of education (United Nations Educational, Scientific and Cultural Organization, 2008).
The Medical Ethics Manual released by the World Medical Association (WMA) provided a basic and universally used curriculum for the teaching of medical ethics. The WMA curriculum includes professionalism as a key component needed for the inclusion of Medical Ethics and Human Rights as an obligatory course for medical schools worldwide (Williams, 2015).
It has been observed that professionalism taught through time-based training might not be sufficient to address the changing healthcare environment and new learners. For the current generation of learners, specialty training must now be aligned with global standards such as that of Accreditation Council for Graduate Medical Education (ACGME). The ACGME standards incorporates professionalism and system-based practice as core components of the curriculum that begins with acquisition of medical knowledge and clinical skills.
Moving forward to the future necessitates the development of methods of assessment of professionalism as a means to successfully teach these professional behaviours (Chay, 2019).
Another key step in the future includes the teaching of professionalism as part of health professions education. Future academic health centres will need more medical educators who can pursue further education and help foster an environment that supports educator development. This key step will help in the attainment of long-term goals and to adapt to the changes in medical education (Dickinson et al., 2020).
Providing doctors with professional models as they move from novice to expert in their professional career will be instrumental as a framework for education. One clear example is the professional identity model that incorporated leadership, followership and team-working roles A more rounded and mature professional identity eventually develops that would set these doctors as models of professionalism for other health workers (McKimm et al., 2017).
IV. CONCLUSION
The unresolved definition of medical professionalism has made the incorporation of programmes on professionalism quite challenging. Any programme that will be implemented must be well thought of and tailored to the needs of the institution and all stakeholders. Analysing unique contexts of the curricular programme will be the key to keep any programme on professionalism relevant and viable.
The fact is that there are few curricular models for the incorporation of medical professionalism into the medical curriculum. This process is not an easy task and needs a strong institutional commitment and resolve for it to be successfully implemented. The four models were amazing attempts to incorporate professionalism in medical education. No formal evaluation has been published concerning this. Based on the comparative analysis of the four models, certain aspects should be highlighted so that we could possibly learn from them:
1. The task of preparing a programme on medical professionalism would be more systematic if the institution starts with a working definition of professionalism. This was seen in Mayo where a well-described definition set the direction for planning, implementing and institutionalising professionalism.
2. The culture of professionalism needs to be articulated institutionally and incorporated in the institution’s vision, mission, goals and policies. Mayo’s declaration of its primary value that “the needs of the patient come first” sets the stage for an atmosphere that is conducive to serving with professionalism.
UWSOM also opened its door to a culture of professionalism by declaring an “ecology of professionalism”. However, its implementation may have been limited when the Colleges programme for the purpose of institutionalising professionalism was limited to thirty designated faculty and role models.
3. The professionalism programme must be woven in all levels of medical education from the pre-clinical to the clinical years. Just like any competency, acquiring the values and skills and putting it into practice requires constant learning and reinforcement throughout the years of education.
Mayo and VUSM have prepared programmes for all the four years of medical education. Both institutions have crafted programmes for the pre-clinical years and have provided teaching and learning activities such as lectures, problem-based learning, small group discussions and feedback. Mayo engaged their students in the clinical years in elective experiences in professionalism and ethics and a “professionalism portfolio” for all students. VUSM designed a programme for the clinical year that was limited to a service recovery training for the purpose of addressing actual patient complaints.
4. Role models are essential in teaching professionalism because they can greatly influence attitudes and behaviours. Unprofessional physician behaviours such as disrespect and abuse of medical personnel, and refusal to complete duties must be corrected. If left unchecked, the observing medical students may consider such behaviours as normal (Mueller, 2009). These are among the ill effects of a hidden curriculum that occurs when an institution lacks role models. For a programme on professionalism to be successful, the faculty physicians and the rest of the healthcare team and institution’s staff need to undergo professionalism programmes applicable to their needs and roles.
In the case of UWSOM, a group of 30 selected faculty underwent training while in Mayo, all faculty underwent a professionalism programme.
5. Based on the curricular models described, it appears that a nurturing environment is preferable over punitive actions. The development of all scopes of professionalism from the intrapersonal to interpersonal to societal professionalism requires constant discussion, feedback and remediation. Although repetitive unprofessional behaviours may have consequences, the medical trainee will need to go through the nurturing process in order to fully imbibe the heart and soul of a medical professional.
6. The ability to handle professionalism challenges follows a learning curve as well. The levels of difficulty of professionalism challenges are related to how much learning situations a student may have encountered. The goal is to move from novice to competent to proficient and hopefully to an expert level of handling professionalism challenges just like all other aspects of learning in medicine.
The ability of the future generation of physicians to serve society ultimately rests on how professionalism has been woven into the curriculum in medical education. How to incorporate professionalism will be a continuing challenge for all medical educators.
Note on Contributor
Dr. Maria Isabel M. Atienza, Professor, San Beda University College of Medicine, Philippines and Head, Institute of Pediatrics & Child Health, St. Luke’s Medical Center, Global City developed the methodological framework for the study and performed data collection and data analysis as part of her PhD research, and wrote and approved the manuscript.
Ethical Approval
This review article was not submitted for IRB/ethical approval.
Acknowledgement
The author would like to acknowledge the insightful suggestions of the Vice Dean of San Beda University College of Medicine: Dr Noel Atienza.
Funding
This review article did not receive any funding.
Declaration of Interest
There are no conflicts of interest to declare.
References
Chay, O. M. (2019). Transformation of medical education over the years – A personal view. The Asia Pacific Scholar, 4(1), 59-61. https://doi.org/10.29060/taps.2019-4-1/pv1076
Cruess, R. L., & Cruess, S. R. (2006). Teaching professionalism: General principles. Medical Teacher, 28(3), 205-208. https://doi.org/10.1080/01421590600643653
Dickinson, B. L., Chen, Z. X., & Haramati, A. (2020). Supporting medical science educators: A matter of self-esteem, identity, and promotion opportunities. The Asia Pacific Scholar, 5(3), 1-4. https://doi.org/10.29060/taps.2020-5-3/pv2164
Goldstein, E. A., Maestas, R. R., Fryer-Edwards, K., Wenrich, M. D., Oelschlager, A.-M. A., Baernstein, A., & Kimball, H. R. (2006). Professionalism in medical education: An institutional challenge. Academic Medicine, 81(10), 871-876. https://doi.org/10.1097/01.acm.0000238199.37217.68
Hickson, G. B., Pichert, J. W., Webb, L. E., & Gabbe, S. G. (2007). A complementary approach to promoting professionalism: Identifying, measuring, and addressing unprofessional behaviors. Academic Medicine, 82(11), 1040-1048. https://doi.org/10.1097/acm.0b013e3185761ee
Lynch, D. C., Surdyk, P. M., & Eiser, A. R. (2004). Assessing professionalism: A review of literature. Medical Teacher, 26(4), 366-373. https://doi.org/10.1080/01421590410001696434
McKimm, J., Vogan, C., & Mannion, H. (2017). Implicit leadership theories and followership informs understanding of doctors’ professional identity formation: A new model. The Asia Pacific Scholar, 2(2), 18-23. https://doi.org/10.29060/taps.2017-2-2/oa1022
Mueller, P. S. (2009). Incorporating professionalism into medical education: The Mayo clinic experience. The Keio Journal of Medicine, 58(3), 133-143. https://doi.org/10.2302/kjm.58.133
Mueller, P. S. (2015). Teaching and assessing professionalism in medical learners and practicing physicians. Ramban Maimonides Medical Journal, 6(2), e0011. https://doi.org/10.5041/rmmj.10195
O’Sullivan, H., van Mook, W., Fewtrell, R., & Wass, V. (2012). Integrating professionalism into the curriculum. Medical Teacher, 34(2), 155-157. https://doi.org/10/3109/0142159x.2011.595600
Parker, M., Luke, H., Zhang, J., Wilkinson, D., Peterson, R., & Ozolins, I. (2008). The pyramid of professionalism: Seven years of experience with an integrated program of teaching, developing, and assessing professionalism among medical students. Academic Medicine, 83(8), 733–741. https://doi.org/10.1097/acm.0b013e31817ec5e4
Passi, V., Doug, M., Peile, E., Thistlewaite, J., & Johnson, N. (2010). Developing medical professionalism in future doctors: A systematic review. International Journal of Medical Education, 1, 19-29. https://doi.org/10.5116/ijme.4bda.ca2a
United Nations Educational, Scientific and Cultural Organization. (2008). Bioethics core curriculum. Syllabus section 1: Ethics education programme. UNESCO. http://www.unesco-chair-bioethics.org/?mbt_book=bioethics-core-curriculum
Viggiano, T. R., Pawlina, W., Lindor, K. D., Olsen, K. D., & Cortese, D. A. (2007). Putting the needs of the patient first: Mayo clinic’s core value, institutional culture, and professionalism covenant. Academic Medicine, 82(11), 1089-93. https://doi.org/10.1097/acm.0b013e3181575dcd
Williams, J. R. (2015). Medical ethics manual (3rd ed.). World Medical Association. https://www.wma.net/what-we-do/education/medical-ethics-manual/
*Maria Isabel Maniego Atienza
San Beda University
College of Medicine,
Mendiola Street,
City of Manila,
Philippines 1005
Tel: 6329178668751
Email: mmatienza@sanbeda.edu.ph
Submitted: 23 July 2020
Accepted: 21 October 2020
Published online: 13 July, TAPS 2021, 6(3), 121-123
https://doi.org/10.29060/TAPS.2021-6-3/CS2361
Sandra E Carr, Katrine Nehyba & Bríd Phillips
Division of Health Professions Education, School of Allied Health, The University of Western Australia, Australia
I. INTRODUCTION
COVID-19 has caused a major disruption to medical education with many educators making rapid shifts to online teaching (Sandars et al., 2020). Many have had to make critical changes in their instructional delivery (Ferrel & Ryan, 2020; Perkins et al., 2020). These changes may have lasting effects on the shape of educational delivery impacting generations to come (Ferrel & Ryan, 2020). It is important to share these changes and innovations as “Students and educators can help document and analyse the effects of current changes to learn and apply new principles and practices to the future” (Rose, 2020, p. 2132). Our case study examined the transition of small group teaching from blended learning to an emergency remote teaching environment.
II. CONTEXT
At the University of Western Australia, medical students undertake a scholarly activity during the third and final years of their Doctor of Medicine that enables specialisations in research or coursework. Of these students, 27% (n=65) choose a specialisation in Medical Education and graduate having completed 75% of a graduate certificate in health professions education. The first unit, Principles of Teaching and Learning offers an introduction to educational theory, curriculum design, teaching and assessment with a focus on developing teaching skills in small and large group settings and applies blended learning strategies. The final assignment assesses small group teaching techniques and the application of peer assisted learning and feedback. This group assignment requires students to:
a. Develop, plan and deliver a face to face small group teaching activity.
b. Describe and assess the group work processes using an audio journal and group assessment rating.
c. Engage in Peer Observation of Teaching.
With the advent of COVID-19 a change in the assessment was required. The 65 students were informed that the group work would have to occur on line and the small group teaching activity would now be an online Video Presentation. Within the Blackboard learning management system, each group had access to a Discussion Board and a virtual meeting tool to support collaboration and teamwork. The marking rubric was not adjusted so the focus on application of small group teaching techniques remained. The video of the developed small group teaching activity was uploaded along with the audio journal and peer observation of teaching components of the assessment.
III. STUDENT EXPERIENCE
We undertook a thematic analysis of students’ audio journals and written responses to describe their experience in five broad themes (see Figure 1).
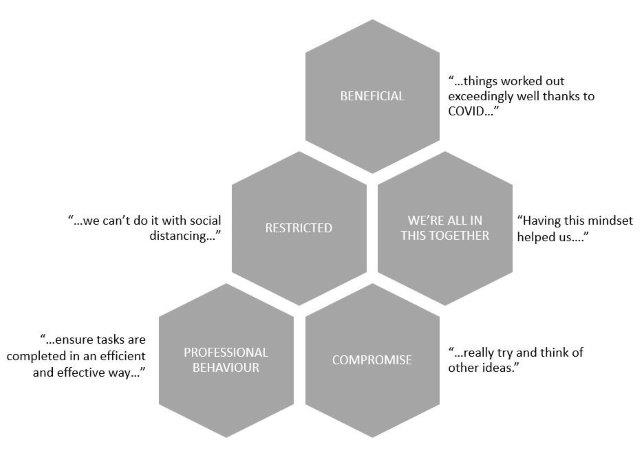
Figure 1. Student experiences of an online group assignment
Thirty percent of students reported aspects of working online as beneficial, and in some ways an improvement on face-to-face contact. For example, students who otherwise could have experienced difficulty meeting in person were able communicate and meet more easily:
“…we have already managed to organise our first meeting quite swiftly and with ease…”
(S1)
They also reported learning new skills:
“This group project taught me valuable skills when working in an online environment, including how to utilise and contribute in video meetings, share resources and regularly update the group…”
(S25)
“I have also learnt that filming or video is a great medium to communicate messages…once it is done, it can be a very effective tool.”
(S5)
However, not unexpectedly, some of the changes were seen as restrictions. The students talked of being “…banned from entering the hospital…” and of “…having no access…” to equipment or rooms, and “…we can’t do it with social distancing…” This led to feelings of disappointment and frustration, as they tried to find feasible options for the assignment.
“…all four of us were trying to actively brainstorm for an hour, trying to think of something…”
(S60)
“…we had fantastic plans…but unfortunately we didn’t have any of these options…”
(S25)
The perceived restrictions challenged the students’ persistence and adaptability (Ferrel & Ryan, 2020) and led them to compromise. One student, after their group changed their assignment idea from venepuncture to handwashing, said “…we…decided to try and make this idea work the best we could.” (S18). This adjustment and negotiation of ideas led to some innovative and varied submissions, using, for example, dolls; online role-plays; on-screen debate and custom virtual backgrounds.
Another theme that emerged was that of a shared experience, and a sense of we’re all in this together. The use of online communication platforms such as Zoom and Facebook Chat, and the use of shared documents meant that “…everyone could be involved, regardless…” There was evidence of a supportive environment and shared accountability, to ensure that they were “…giving everyone a chance…” and “…everyone seemed equally invested…”
Finally, despite the changes, restrictions and compromise, the students remained task-focussed and were able to plan, allocate, collaborate and communicate in their new online environment. The spread of grades for this assignment was consistent with previous cohorts, suggesting that the change in method was not detrimental to their performance. They were aware of potential dangers of working in this new, unknown way.
“…it will be important for us to be mindful of the risk of losing a professional mindset during our meetings, and divert away from the task at hand.”
(S1)
However, they described the same professional behaviours that would be expected in a face-to-face assignment, such as planning; delegation; effective communication; setting and meeting deadlines; and providing constructive feedback to other team members.
“…our team worked really well together. I suspect things worked out exceedingly well thanks to COVID and lockdown, which forced us to work online.”
(S8)
IV. CONCLUSION
Sklar states that during these unprecedented times “…it is important that our voices are loud about what we have experienced and learned” (Sklar, 2020, p. 9). In this case study we have described an experience of emergency remote teaching, in which a face-to-face small group teaching assignment was moved online. Our experience suggests that, even with its challenges, it was a success. Despite restrictions and compromise the students reported beneficial aspects to working online, and demonstrated a sense of comradery and professionalism while developing digital learning skills that are proving essential for learners and applicable for health professionals in the 21st century.
Notes on Contributors
Sandra Carr conceived the idea of the case study and contributed to the design of the work, gathered the qualitative data and interpretation of the findings. Katrine Nehyba contributed to the design of the case study, searched the supporting and relevant literature, undertook the thematic analysis of the data and constructed the Figure. Bríd Phillips contributed to the design of the work, searched the supporting and relevant literature to construct the rationale and introduction and contributed to the interpretation of the findings. All contributed to confirmation of the themes, the Discussion and Conclusion. All reviewed and contributed to each draft of the paper and approval the final submission.
Acknowledgement
This project was subject to ethical approval by the human ethics committee of the University of Western Australia. Consent was waived in line with the ethical approval obtained.
Funding
This work has not received any external funding.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Ferrel, M., & Ryan, J. (2020). The Impact of COVID-19 on Medical Education. Curēus, 12(3), e7492–e7492. https://doi.org/10.7759/cureus.7492
Perkins, A., Kelly, S., Dumbleton, H., & Whitfield, S. (2020). Pandemic pupils: COVID-19 and the impact on student paramedics. Australasian Journal of Paramedicine, 17(1), 1-4. https://doi.org/10.33151/ajp.17.811
Rose, S. (2020). Medical student education in the time of COVID-19. Journal of the American Medical Association, 323(21), 2131–2132. https://doi.org/10.1001/jama.2020.5227
Sandars, J., Correia, R., Dankbaar, M., de Jong, P., Goh, P., Hege, I., Masters, K., Oh, S., Patel, R., Premkumar, K., Webb, A., & Pusic, M. (2020). Twelve tips for rapidly migrating to online learning during the COVID-19 pandemic. MedEdPublish, 9(1), 82. https://doi.org/10.15694/mep.2020.000082.1
Sklar, D. (2020). COVID-19: Lessons from the disaster that can improve health professions education. Academic Medicine, 95(11), 1631–1633. https://doi.org/10.1097/ACM.0000000000003547
*Sandra Carr
Division of Health Professions Education
The University of Western Australia
35 Stirling Hwy,
Crawley WA 6009, Australia
Tel: +61 64886892
Email: Sandra.carr@uwa.edu.au
Submitted: 20 July 2020
Accepted: 6 November 2020
Published online: 13 July, TAPS 2021, 6(3), 14-23
https://doi.org/10.29060/TAPS.2021-6-3/RA2346
Claude Jeffrey Renaud1, Zhi Xiong Chen2,6, Heng-Wai Yuen3, Lay Ling Tan4, Terry Ling Te Pan5 & Dujeepa D. Samarasekera6
1Department of Medicine, Khoo Teck Puat Hospital, Singapore; 2Department of Physiology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Department of Otorhinolaryngology-Head & Neck Surgery, Changi General Hospital, Singapore; 4Department of Psychological Medicine, Changi General Hospital, Singapore; 5Department of Anaesthesiology, National University Health System, Singapore; 6Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: The Coronavirus-19 pandemic has had profound effects on health professions education (HPE) posing serious challenges to the continued provision and implementation of undergraduate, postgraduate and continuing medical education (CME). Across these HPE domains, the major disruptions included the exclusion of undergraduate learners from clinical learning environments, restricted intra-, inter-institutional and overseas movement of medical professionals, termination of face-to-face learner-educator interactions, deployment of postgraduate learners into non-scope service settings, and CME postponement.
Methods: In this review we report on how in Singapore various adaptive measures were instituted across the 3 HPE domains at institutional and national level to maintain adequate resources at the frontline to meet service exigencies, promote healthcare professionals’ wellbeing and safety as well as mitigate the spread of the pandemic.
Results: We identified several strategies and contingencies developed to address these challenges. These involved the use of online learning platforms, distributed and asynchronous learning, an undergraduate Pathway Programme, and use of innovative hands-on technology like simulation. Robust, well pre-planned pandemic preparedness, effective communication, as well as provision of psychological support resources ensured maintenance of service and academic continuity, trust and resilience within HPE. However, several challenges remain, namely the timing and manner of conducting formative and summative assessments, cybersecurity, and the indispensable hands-on, in-person experiential learning for surgical training.
Conclusion: Strong leadership with vision and planning, good communication, prioritising learners’ and educators’ wellbeing and safety, and harnessing existing and emerging online learning technologies are crucial elements for effective contingencies for HPE disruption during pandemics.
Keywords: Pandemic Preparedness, COVID-19, Curriculum Development, Online Learning and Assessment, Learner Wellbeing and Safety, Health Profession Education
Practice Highlights
- COVID-19 pandemic has caused profound disruption to medical education and Singapore is no exception.
- Health professions education community (undergraduate, residency and continuous professional development) had to rethink traditional learning approaches.
- There is a need for contingencies that integrate service and academic continuity and safety.
- Implementing contingencies requires coordinated national and institutional pandemic pre-preparedness.
- There remain uncertainties as to the long-term effectiveness of these contingencies on learning.
I. INTRODUCTION
Singapore had its first case of Coronavirus 19 (COVID-19) on 23rd January 2020 and scaled up its response from DORSCON (Disease Outbreak Response System Condition) Yellow to Orange 2 weeks later as the crisis evolved to pandemic proportion (Ashokka et al., 2020; J.E.L. Wong et al., 2020). This involved setting up a suite of strategies aimed at containing community transmission (Lee et al., 2020).
At the healthcare service and health profession education (HPE) level, these strategies centred on mobilising adequate resources at the frontline, mandating use of personal protective equipment (PPE) in high-risk areas and restricting healthcare workers’ movement (Ashokka et al., 2020; Lee et al., 2020; Liang et al., 2020; C. Wong et al., 2020; J.E.L. Wong et al., 2020). In addition, undergraduate medical education put a stop to clinical clerkships and large and small on-campus learning and restructured formative and summative assessments.
As the very stakeholders and resources required for HPE were diverted to fighting the pandemic, HPE faced extraordinary disruption. Educators and learners had to delicately balance service continuity, patients’ and learners’ wellbeing and safety versus maintaining a business-as-usual approach to learning. Moreso, the entire HPE community had to critically relook at the applicability of competency-based learning which is traditionally predicated on the principles of authentic supervised patient experience, programmatic assessment, learners as part of a community of practice and continuous professional development (CPD) (Harris et al., 2010; Iobst et al., 2010).
Previous public health emergencies like Severe Acute Respiratory Syndrome (SARS) have taught that such disruptions can provide unique opportunities for contingency planning in HPE especially when there is little time for wholesale programme redesign (Lim et al., 2009; Patil & Yan, 2003). This report thus describes the experience of 3 HPE domains in Singapore in mitigating the dissonance between optimal pandemic preparedness, unconstrained academic continuity and learners’ and educators’ well-being.
II. METHODS
A comprehensive review of the adaptive contingency strategies adopted at 1 undergraduate (Yong Loo Lin School of Medicine), Singapore residency programmes and across the CPD was made by looking at institutional and governmental programmes during the early phase of the pandemic and prevalent COVID-19 related literature on HPE. As this research is a description of events that have already happened and did not involve HPE stakeholders’ directly and interventionally, participants’ informed consent and internal review board approval were not required for its conduct.
III. RESULTS
Herein, is a detailed outline of the contingencies implemented across the 3 HPE domains which are also summarised in Table 1.
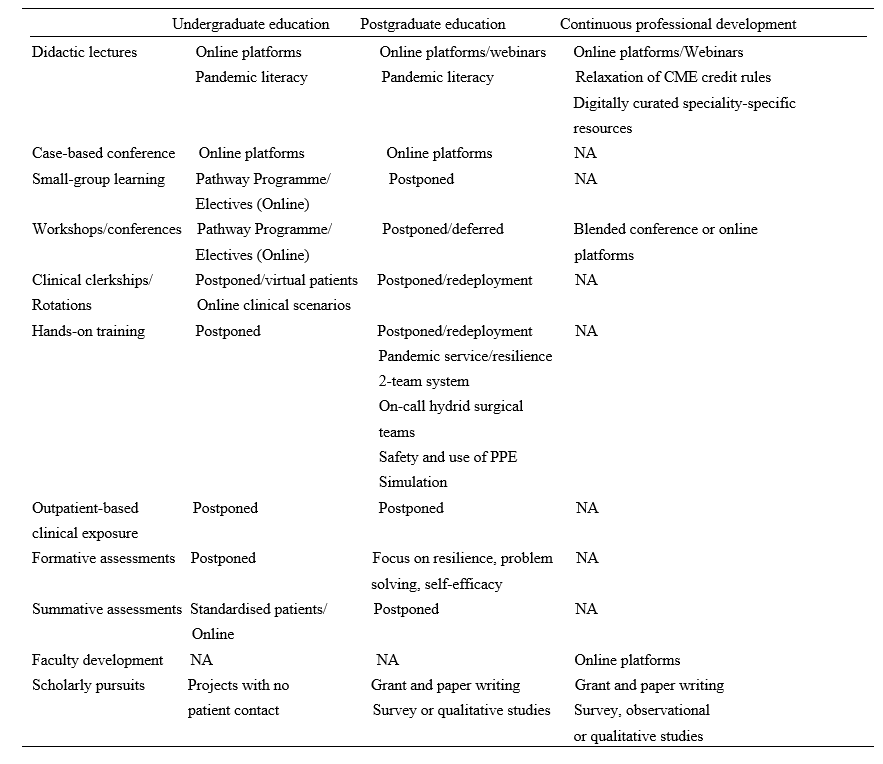
Table 1. Summary of disruptions and contingences across the health profession education spectrum during COVID-19 pandemic in Singapore.
Note: NA=not applicable; PPE= personal protective equipment
A. Contingencies in Undergraduate Medical Education: Experience of Yong Loo Lin School of Medicine
At the Yong Loo Lin School of Medicine which is the largest of the three medical schools in Singapore, the Education Team led by the Vice Dean (Education) started preparing in February 2020 for the possibility of loss of clinical teaching. Those most affected would be Phase 3 and 4 (Year 3 and 4) medical students. Phase 5 (Year 5) students were preparing for their Final Professional Examinations even though assessment was significantly disrupted across all Phases. Phase 1 and 2 (Year 1 and 2) students have relatively less clinical learning exposure and assessments, and were finishing their curricula and preparing for exams. Focusing on the Phase 3 and 4 students, first, their vacation and elective periods were brought forward respectively. Next, to give students meaningful learning opportunities that do not require patient contact, the Pathway Programme which had been launched before the pandemic was paced up (National University Singapore, Yong Yoo Lin School of Medicine, 2020).
The Pathway Programme consists of six Pathways. They are Health and Humanity, Health Informatics, Inquiry and Thinking, Medical Education and Medical Innovation and Entrepreneurship all led by a team of trained educationists. In addition, a non-Pathway initiative called Education Innovation completed the suite of new education offerings for the students. The sixth Pathway Behavioural and Implementation Science was partially offered under Inquiry and Thinking through a series of lectures on Health Economics. Below we describe what each Pathway is about.
1) Behavioral and implementation science: This pathway exposes medical students to principles of behavioural and implementation science, and applies this knowledge to effectively design and deliver healthcare in real-world settings, and lays the foundation for them to become active agents of change in clinical practice.
2) Health and humanity: This pathway aims to nurture emotionally resilient, socially conscious and globally minded health leaders through rekindling one’s love for medicine and humanity. Through experiential activities, inspirational workshops and hands-on project work in the community, students develop critical thinking skills in global health, teamwork and leadership skills to inspire health for all.
3) Health informatics: This pathway aims to enable students to gather and critically evaluate research and health informatics data, equipping them with the skills necessary to apply the principles of health informatics, summarise and visualise datasets to perform basic analyses, so they become data-science competent clinicians who can identify and analyse medical data to address clinical issues.
4) Inquiry and thinking: This pathway aims to inspire and motivate our medical students to develop a sense of curiosity so as to foster a habit of inquiry that is able to dynamically utilise a range of thinking methods, processes and skillsets to tackle questions and problems. The end goal of this pathway is to groom a pipeline of thinking doctors who can advance healthcare in any aspect they desire.
5) Medical education: This pathway exposes medical students to concepts and principles in HPE, to equip them with foundational skills in HPE, with a focus on educational innovation and scholarship of teaching and learning, so as to groom future clinical educators.
6) Medical innovation and entrepreneurship: This pathway aims to nurture medical students with the 6Cs attributes: Curiosity, Creativity, Compassion, Collegiality, Collaboration, and Commercial Intelligence. The programme gradually exposes medical students to concepts and principles in innovation, and the selective elements equip students with foundational skills in innovation and entrepreneurship.
With the elective period brought forward, Phase 4 students were exposed to the Pathway Programme from early-March to early-May 2020 through two weeks of front-loading online lectures, followed by four to eight weeks of projects. Most Pathways followed the general structure with slight variations between them. For Phase 3 students, they enjoyed an early vacation before encountering a shortened Pathway Programme from early-April to early-May 2020, comprising of 2 weeks of front-loading online lectures and 2 weeks of projects, which students had the option of continuing into Phase 4.
Using Inquiry and Thinking Pathway as an example, topics of front-loading online lectures included ‘Complexity and Systems Thinking’, ‘Habits of Inquiry and Critical Thinking’ and ‘Evidence-based Medicine and Search Methods’. More than 80 projects were offered by prospective supervisors with more than 70 students getting involved in projects. Each student was guided in the project by the supervisor as well as engaged in a one to two-hour weekly reflection sessions with a separate mentor or the supervisor who doubled up as a mentor. Students were required to submit a weekly reflection write-up of 50 words or more. At the end of the Pathway Programme, students submitted a single slide of their projects for evaluation. Top two projects from each Pathway were selected to present and compete in a Grand Finale on 8 May 2020 before the School’s leadership, a panel of judges, their peers and overseas observers. The Grand Finale attracted over 200 participants. Single slides of all projects were compiled into an e-book to be shared with students and faculty members.
B. Postgraduate Training: Experience of Residency Programmes across Singapore Three Sponsoring Institutions (SIs)
Since SARS, Singapore has steadily been bolstering critical resource reserves and expertise in pandemic preparedness, culminating in the setup of the 330-bed purpose-built National Centre for Infectious Diseases (NCID) at the National Healthcare Group (NHG) Novena campus (Lee et al., 2020; Seah, 2020). Concurrently, postgraduate medical education underwent significant transformation with the adoption of Accreditation Council for Graduate Medical Education (ACGME) styled competency-based learning, culminating in the setup of three residency SIs of which NHG is one (Huggan et al., 2012; Khoo et al., 2014). Thus during the build-up to COVID-19 pandemic, NCID, residents and faculty at NHG 27 residency programmes formed the initial frontliners in managing the pandemic before being later joined by the other two SIs (C. Wong et al., 2020).
Care delivery and learning had to be restructured so that adequate manpower could be redeployed at screening centres, emergency departments, outbreak wards and critical care units. Frontline residents had to endure long and exhausting shifts wearing PPEs and prolonged time away from family, not to mention postponed leaves. Residents and faculty also had to be segregated into independent two-team system with phased two-weekly rotations to avoid manpower attrition and service disruption as a result of staff infection, quarantine or burnout. Elective surgeries, continuity clinics, grand rounds, face-to-face case conferences, cross-institutional elective rotations, in-person programme selection interviews as well as summative assessment had to be deferred. Postgraduate specialty conferences, courses and workshops, whether local or international, also had to be postponed or cancelled due to travel restrictions, further limiting opportunities for learning.
As a result of these changes several resourceful strategies were implemented to balance the palpable tensions between service, wellbeing and learning.
The first was maintaining open and transparent communication between institutional and academic leaders, faculty and residents so that the rationale for a pandemic-mode centralised command-control leadership model could be accepted. This allowed residents to grasp the real sense of urgency brought in by COVID-19, thus facilitating speedier buy-in and compliance to ever changing human resource and education policies. In addition, this strategy helped build up trust in the institutional support structure and contain the spread of parallel distracting infodemics, allowing residents to focus on service delivery, learning and well-being.
The second strategy was the promotion of residents’ physical and psychological safety and wellbeing. This entailed ensuring all residents had adequate orientation to the proper use of PPEs and could easily access them. Well-being and resilience support resources like in-person or anonymous virtual outreach psychological crisis intervention counselling and peer support through online debriefing and feedback were put in place across all hospitals under the three SIs. The ancillary effect was that residents felt their safety, their families’ and patients’ was valued and that there was fair and equitable work and rest allocation. Further, ACGME cancelled all accreditation and Clinical Learning Environment Review site visits and took steps to reframe and relax some accreditation criteria (Nasca, 2020). This went a long way in allaying residents’ anxieties regarding clinical progression.
The third strategy was leveraging existing online tools to maintain some element of learning continuity without the need to invest in significantly expensive technologies, curricular redesign or faculty re-development. Programmes transferred their core didactic lectures, journal clubs and case-based discussions onto distributed learning platforms such as Zoom, Go to meeting, Google meet or WebEx for synchronous learning. Access to Webinars had the added advantage of providing opportunities for asynchronous learning. Zoom teleconferencing in particular, remains the most popular due to its affordable subscription, large participant capacity and easier accessible collaborative interface and a breakout feature that enables mounting learning models like team-based learning.
Residents from surgical residency programmes who rely on direct-patient encounter and hands-on experience for learning were more significantly impacted. Importantly, because non-emergency visits to hospitals were halted, elective procedures and surgeries were postponed or cancelled and, the number of patients and learning opportunities was thus greatly reduced. This was further aggravated by the shift of many training institutions and teaching hospitals to pandemic service (Liang et al., 2020). In many instances, surgical residents were redeployed to frontline areas, like screening centres, which are beyond their usual scope of practice (C. Wong et al., 2020).
Curriculum development contingencies thus went beyond online didactic content dissemination to embrace enhanced distributed learning approaches like videos, podcasts, virtual reality and simulated learning (C. Wong et al., 2020). Some programmes improvised by forming on-call hybrid surgical teams, which allowed surgical residents some measure of hands-on exposure to generic emergency or semi-elective cases during on calls but not necessarily within the scope of their area of interest.
C. Contingencies for Continuous Professional Development (CPD)
The disruption brought on by closure of higher educational institutions, scaling down of healthcare organisations and travel restrictions, compelled educators and health care professionals to adapt and embrace curricular changes and transition to virtual learning and use of technology for simulated learning.
Continuing medical education (CME) and CPD are integral parts of the development of a healthcare professional in providing optimal clinical care for his/her patient. CME is aimed at maintaining or updating the requisite knowledge, skills, professional performance and relationships and crucially, is a requirement for maintenance of certification in the discipline or specialty of the healthcare profession (Davis et al., 2008). CPD on the other hand caters to a broader range of competencies that reflect the healthcare profession attitudes towards learning and learning needs (Filipe et al., 2018). Every specialty and governing medical body has its stipulated requirements. In Singapore, the Singapore Medical Council (SMC) states that all fully and conditionally registered doctors are required to meet the compulsory CME requirements of 50 core points for the qualifying period before their practising certificate can be renewed (Singapore Medical Council, 2020a). While most CME activities involve attendance at local, regional or international scientific meetings or conferences, self-study, review and authorship of articles are also considered core CME points. Most hospitals hold regular Grand Ward Rounds, journal clubs and peer review learning sessions at departmental and institutional levels, which also contribute towards core CME points.
However, with Singapore moving to DORSCON Orange, many of these learning activities were immediately suspended as staff scrambled to reorganise clinical services amidst the pandemic imperative for team separation and safe distancing. Thus, traditional face-to-face meetings were replaced by online meetings and webinars facilitated by virtual platforms mentioned previously. In tandem the SMC relaxed requirements for CME credits by allowing healthcare professionals to log in attendance to online sessions, including webinars (Singapore Medical Council, 2020b). There was also an increase in allocation of CME credits for self-study (e.g., reading of referenced journals listed in PubMed). COVID-19-related CME activities were also considered core points for all doctors (Singapore Medical Council, 2020b).
While, much of the recent global CME content has primarily focused on increasing understanding of COVID-19 and its infectious nature across various medical disciplines, there has been lesser emphasis on its medical and psychological impact to health. It has nonetheless enabled healthcare professionals to better provide optimal care for patients while adopting best available evidenced practice relating to all aspects of this rapidly contagious disease. Thus, online information dissemination has been at an unprecedented high with multiple local, regional and international webinars and resource websites being made readily accessible. Professional societies have also made available to their members regularly curated digital speciality-specific resources on best practices pertaining to COVID-19 management (Academy of Medicine Singapore, 2020).
In addition to CME, healthcare professionals have traditionally relied on annual live face-to-face local, regional and international scientific conferences, symposiums, and educational workshops to network as a learning community and keep abreast of domain-specific advances. With strict travel restrictions these have been cancelled, postponed or moved online as webinars, interactive content, forums and chats.
Some conference organisers decided to still proceed to issue notices of acceptance of abstract submissions as ‘proof’ of scholarly work or allowed online presentation. Other creative ways of continuing with international conferences have included a “blended conference” approach with a mix of face-to-face and online content to support those attending onsite and online (Nadarajah et al., 2020). With careful attention paid to safe distancing for onsite participants, such “blended conferences” provide the all-important human face-to-face interactions which online webinars and conferences, though functional in most parts, sorely lack. They also provide the best of both worlds and may indeed be the new normal in the foreseeable future as COVID-19 further changes the HPE landscape relating to international travel and social interaction.
Similarly, Singapore’s three medical school curriculum development centres rapidly transited in-person to virtual faculty development sessions. This allowed educators openly dispersed by social distancing and clinical exigencies to continue tapping on the best pedagogic practices, interact and engage in interprofessional learning.
IV. DISCUSSION
The COVID-19 pandemic disruptions have reinforced the need for agency and adaptation in HPE. We have shown that through well-coordinated, multisectoral efforts, solutions can be harnessed to minimise their negative impact on learning. However COVID-19, unlike other recent coronavirus epidemics like SARS and Middle East Respiratory Syndrome (MERS) seems a more formidable crisis (Jones, 2020; Peeri et al., 2020). It may not go away quickly without the advent of effective vaccines and sustained infection control measures. These contingencies are therefore aimed at promoting service and academic continuity, safety and resilience. Whilst they are useful blueprints for pandemic preparedness and responsiveness in the short term, they may not be applicable in all contexts or in a crisis of attrition. Further, they have their own strengths and limitations.
A major strength is institutional and academic leaders’ sense of long-term planning and commitment to educators’ and learners’ safety through effective communication, being visible and providing programme and system support. In a rapidly evolving disruptive environment, this is crucial, as stakeholders remain engaged and trusting without having to anguish over under-resourcing or abandonment. Recent publications have alluded to the social capital returns of such an “integrative resilience approach” that amplifies individual and system wellbeing and minimises burn-out and contagion (Neufeld & Malin, 2020; Samarasekera et al., 2020; Schwartz et al., 2020; Wald, 2020).
Another strength is the adoption of adaptive online technologies which not only ensures academic continuity but also allows a smooth and rapid quarantine and pandemic curriculum development. Large virtual communities of learners can thus be rapidly mobilised without fundamentally affecting content, quality and institutional bottom lines. Indeed, this may have had the unintended consequences of unprecedentedly boosting attendance rates in medical schools, residency programmes and CPD sessions. Online migration also facilitates quick and mass standardised training and deployment of untrained or returning retired healthcare professionals in general and critical care medicine, allowing healthcare institutions to boost capacity in those critical areas during pandemics (Brunner et al., 2020; Li et al., 2020). More so, these emergent technologies hold a lot of promise for post-pandemic medical education and replication of authentic patient experiences. It is envisioned that they can be interfaced onto learning management systems (LMS) and into areas like virtual patient consults, telemedicine, adaptive learning and extended reality or avatar-like high fidelity simulation (Goh & Sandars, 2020). They are also important as a source of asynchronous learning whereby learners who are too busy with clinical duties or for surgical residents when there is a lack of critical hands- on training (Tolu et al., 2020).
A third strength, is that such crisis can open unintended opportunities for learners to develop competencies outside the core curricular knowledge and procedural skills sphere. For instance, the mere exposure of undergraduate learners not directly involved in patient care to pandemic-related content, volunteering in contact tracing or public awareness centres or restructuring of learning experiences like the Pathway Programme can nurture professional identity, pandemic literacy and doctor-ready qualities like service prioritisation, altruism and resilience (Bauchner & Sharfstein, 2020; Rose, 2020; Stetson et al., 2020). Indeed, the Pathway Programme succeeded in meaningfully engaging medical students at a time when clinical teaching and clinical elective opportunities were frozen. It gave time for the medical school to work out a safe and calibrated approach to resume clinical training in consultation with the relevant government bodies. The fact that it was conceptualised pre-pandemic demonstrates an extraordinary sense of prescience by the academic leadership. The advent of COVID-19 served to accelerate its implementation. It thus not only helped undergraduate medical education to cope with the pandemic but enrich the medical curriculum by catering to the diverse strengths and interests of each learner in order to nurture future-ready doctors for a post-COVID world.
As to residents’ learning, negotiating challenging pandemic duty rosters, making personal choices and sacrifices, navigating processes like resource allocation and public health measures and being deployed into non-core areas, can be just-in-time learning platforms for more nuanced ACGME competencies like professionalism, interpersonal and communication skills, system-based practice and practice-based learning (Hall et al., 2020; Nasca, 2020; Schwartz et al., 2020; Tolu et al., 2020; C. Wong et al., 2020). For surgical residents, there is also an added learning and safety benefit when hitherto straightforward surgical procedures like tracheostomy suddenly come with a myriad of precautions, criteria, and protocols (Givi et al., 2020). Clinic and elective surgery postponement can provide ample opportunities for self-directed learning, exit exams preparation and scholarly pursuits like grant, research ventures and quality improvement projects writing (Schwartz et al., 2020; Tolu et al., 2020). Additionally, prioritisation of public health emergency response training across the HPE spectrum can render healthcare institutions better prepared at handling future pandemics and burn-out (Yang et al., 2020).
Nevertheless, these contingencies have a number of limitations. Namely, moving medical education from the bedside to the ‘web-side’ cannot replace the real patient-centred clinical experience and case-mix learners derive from ward rounds, grand rounds and continuity clinics. Even the Pathway Programme was not without its challenges. With Singapore entering into Circuit Breaker phase of DORSCON Orange on 3rd April 2020, some projects were disrupted as access and movement became more limited (Ministry of Health Singapore, 2020).
Secondly, the utility of online learning is very much predicated on the vagaries of internet penetration and connectivity which makes this approach not always transferable to all socio-economic contexts (Cecilio-Fernandes et al., 2020). More so, for surgical residents, online learning or high-fidelity simulation cannot substitute for in-person learning. The technical skills, haptic feedback, the realism of live surgery, the experiential and contextual learning of ‘being there’ in a surgical team, and the non-cognitive domain skills like collaboration and resilience can be hard to simulate. Reduced contact time between residents and faculty also impacts adversely on opportunities for mentoring, role modelling and supervision. There is also always a danger of breaching learning principles such as cognitive overload when online content design is outside the hands of curriculum developers and programme directors (Kachra & Ma, 2020). As to health professionals, most of these online CME resources represent rather an amalgam of available information that may not have been well curated and pre-approved by accreditation organisations for relevancy.
Thirdly, the contingencies fail to address the enormous challenges in conducting clinical workplace-based assessments, without compromising their validity, reliability, defensibility and educational impact. Although high-stakes OSCE can be successfully conducted in a pandemic environment, its implementation comes with tremendous logistical and political manoeuvring to ensure students’, examiners’ and patients’ safety and assessment integrity are preserved (Boursicot et al., 2020). Cancelling both formative and summative assessments can delay learners’ progression or completion unless adjustments are made to previously established competency criteria. Undergraduates may fail to graduate on time to join the vital pool of medical workforce and residents may not be able to practise as independent practitioners. This can create anxiety and concern to both learners and educators about how to catch up post-pandemic with piling assessment and case and portfolio backlogs.
Lastly, reliance on third party software entities for online content dissemination contrary to institution-designed LMS or whole-sale programme information technology infrastructure redesign carries cybersecurity, privacy and data ownership risks (Fawns et al., 2020; Sandars et al., 2020). Not all faculty are tech savvy to handle the technical intricacies and the many options in the market. Predatory providers may thus seek to peddle behaviourist tactics onto users for their own corporate gains.
V. CONCLUSION
In summary, the COVID-19 pandemic has been a major threat to HPE in Singapore but it has also created opportunities for adaptive and flexible contingencies so that learning goes on safely with minimum constraints. While there is a need to celebrate these early successes, it is also imperative that we assess and learn from their limitations so that we can further refine and more successfully, collaboratively and iteratively apply them in a prolonged crisis. Furthermore, these experiences can serve as templates for adaptive and value-added learning at both regional and international HPE settings beset by larger service and academic disruption. But most importantly they foreshadow the resilience, reimagining and resourcefulness that are expected of HPE as it transits from the new normal of pandemic crisis management to the post-pandemic next normal of innovative technology-based learning.
Notes on Contributors
Adj Associate Professor Claude J Renaud is a senior consultant nephrologist at Khoo Teck Puat hospital Singapre and Associate Programme Director at the National Healthcare Group Renal Residency Programme. He conceptualised, drafted and revised article and wrote introduction, postgraduate medical education (PGME), discussion and conclusion sections.
Dr Zhi Xiong Chen is a Senior Lecturer in Physiology and Assistant Dean for Education at Yong Loo Lin School of Medicine, National University of Singapore. He conceptualised article and wrote the undergraduate medical education section.
Adj Associate Professor Heng Wai Yuen is senior consultant in the Department of Otorhinolaryngology-Head & Neck Surgery, Changi General Hospital, Singapore and Campus Director, SingHealth Duke-NUS Institute for Medical Simulation (SIMS). He wrote abstract and post graduate medical education sections and revised article.
Adj Associate Professor Tan Lay Ling is senior consultant in the Department of Psychological Medicine, Psychogeriatric Service, at Changi General Hospital (CGH). She wrote the section on continuous professional development and revised article overall.
Dr Terry Ling Te Pan is a Senior Consultant, Department of Anaesthesia, National University Hospital and Advisor, Education Technology Unit, Yong Loo Lin School of Medicine, National University of Singapore. He co-wrote the section on continuous professional development and revised article overall.
Dr Dujeepa D. Samarasekera, director at Centre for Medical Education (CenMED) Yong Loo Lin School of Medicine, National University of Singapore. conceptualised and revised article.
Ethical Approval
This study is a description of events and practices and therefore did not require approval from institutional review boards.
Funding
There is no external funding involved in this study.
Declaration of Interest
Other than Dr Dujeepa D Samarasekera who is Editor of TAPS, all authors have no conflict of interest, including financial, consultant, institutional and other relationships that might lead to bias.
References
Academy of Medicine Singapore (AMS) (2020, June 2). Resource site on COVID-19. https://www.ams.edu.sg/policy-advocacy/covid-19-resource-page
Ashokka, B., Ong, S. Y., Tay, K. H., Loh, N. H. W., Gee, C. F., & Samarasekera, D. D. (2020). Coordinated responses of academic medical centres to pandemics: Sustaining medical education during COVID-19. Medical Teacher, 42(7), 717-720. https://doi.org/10.1080/0142159X.2020.1757634
Bauchner, H., & Sharfstein, J. (2020). A bold response to the COVID-19 pandemic: Medical students, national service, and public health. The Journal of the American Medical Association, 323(18), 1790-1791, https://doi.org/10.1001/jama.2020.6166
Boursicot, K., Kemp, S., Ong, T. H., Wijaya, L., Goh, S. H., Freeman, K., & Curran, I. (2020). Conducting a high-stakes OSCE in a COVID-19 environment. MedEdPublish, 9(1), 54. https://doi.org/10.15694/mep.2020.000054.1
Brunner, M., Vogelman, B., & Smith, J. (2020). Rapid development of an outpatient‐to‐inpatient crash curriculum for COVID providers. Medical Education. Advanced online publication. https://doi.org/10.1111/medu.14244
Cecilio-Fernandes, D., Parisi, M. C. R., Santos, T. M., & Sandars, J. (2020). The COVID-19 pandemic and the challenge of using technology for medical education in low and middle income countries. MedEdPublish, 9(1), 74. https://doi.org/10.15694/mep.2020.000074.1
Davis, N., Davis, D., & Bloch, R. (2008). Continuing medical education: AMEE education guide No 35. Medical Teacher, 30(7), 652–666. https://doi.org/10.1080/01421590802108323
Fawns, T., Jones, D., & Aitken, G. (2020). Challenging assumptions about “moving online” in response to COVID-19, and some practical advice. MedEdPublish, 9(1), 83. https://doi.org/10.15694/mep.2020.000083.1
Filipe, H. P., Golnik, K. C., & Mack, H. G. (2018). CPD? What happened to CME? CME and beyond. Medical Teacher, 40(9), 914–916. https://doi.org/10.1080/0142159X.2018.1471200
Givi, B., Schiff, B. A., Chinn, S. B., Clayburgh, D., Iyer, N. G., Jalisi, S., Moore, M. G., Nathan, C. A., Orloff, L. A., O’Neill, J. P., Parker, N., Zender, C., Morris, L., & Davies, L. (2020). Safety Recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. The Journal of the American Medical Association Otolaryngology-Head & Neck Surgery, 146(6),579-584. https://doi:10.1001/jamaoto.2020.0780
Goh, P. S., & Sandars, J. (2020). A vision of the use of technology in medical education after the COVID-19 pandemic. MedEdPublish, 9(1), 49. https://doi.org/10.15694/mep.2020.000049.1
Hall, A. K., Nousiainen, M. T., Campisi, P., Dagnone, J. D., Frank, J. R., Kroeker, K. I., Brzezina, S., Purdy, E., & Oswald, A. (2020). Training disrupted: Practical tips for supporting competency-based medical education during the COVID-19 pandemic. Medical Teacher, 42(7), 756-761. https://doi.org/10.1080/0142159X.2020.1766669
Harris, P., Snell, L., Talbot, M., & Harden, R. M. (2010). Competency-based medical education: Implications for undergraduate programs. Medical Teacher, 32(8), 646–650. https://doi.org/10.3109/0142159X.2010.500703
Huggan, P. J., Samarasekara, D. D., Archuleta, S., Khoo, S. M., Sim, J. H. J., Sin, C. S. P., & Ooi, S. B. S. (2012). The successful, rapid transition to a new model of graduate medical education in Singapore: Academic Medicine, 87(9), 1268–1273. https://doi.org/10.1097/ACM.0b013e3182621aec
Iobst, W. F., Sherbino, J., Cate, O. T., Richardson, D. L., Dath, D., Swing, S. R., Harris, P., Mungroo, R., Holmboe, E. S., & Frank, J. R. (2010). Competency-based medical education in postgraduate medical education. Medical Teacher, 32(8), 651–656. https://doi.org/10.3109/0142159X.2010.500709
Jones, D. S. (2020). History in a crisis—Lessons for Covid-19. New England Journal of Medicine, 382(18), 1681–1683. https://doi.org/10.1056/NEJMp2004361
Kachra, R., & Ma, I. W. Y. (2020). Practical tips for faculty development workforce training under pressure in the time of COVID-19 pandemic. MedEdPublish, 9(1), 81. https://doi.org/10.15694/mep.2020.000081.1
Khoo, S. M., Lahiri, M., Huggan, P. J., Archuleta, S., Olszyna, D. P., Goh, W. P., Chua, S. W., & Ho, K. Y. (2014). When traditional model meets competencies in Singapore: Beyond conflict resolution. Annals of the Academy of Medicine Singapore, 43, 544–549.
Lee, V. J., Chiew, C. J., & Khong, W. X. (2020). Interrupting transmission of COVID-19: Lessons from containment efforts in Singapore. Journal of Travel Medicine, 27(3), 1-5. https://doi.org/10.1093/jtm/taaa039
Li, L., Xv, Q., & Yan, J. (2020). COVID-19: The need for continuous medical education and training. The Lancet Respiratory Medicine, 8(4), e23. https://doi.org/10.1016/S2213-2600(20)30125-9
Liang, Z. C., Ooi, S. B. S., & Wang, W. (2020). Pandemics and their impact on medical training: Lessons from Singapore. Academic Medicine, 95(9), 1359-1361. https://doi.org/10.1097/ACM.0000000000003441
Lim, E. C., Oh, V. M., Koh, D. R., & Seet, R. C. (2009). The challenges of “continuing medical education” in a pandemic era. Annals of the Academy of Medicine, Singapore, 38(8), 724–726.
Ministry of Health Singapore. (2020, June 1). Circuit breaker to minimise further spread of COVID-19. https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19
Nadarajah, V. D., Er, H. M., & Lilley, P. (2020). Turning around a medical education conference: Ottawa 2020 in the time of COVID‐19. Medical Education, 54(8), 760-67. https://doi.org/10.1111/medu.14197
Nasca, T. J. (2020). ACGME’s early adaptation to the COVID-19 pandemic: Principles and lessons learned. Journal of Graduate Medical Education, 12(3), 375-378. https://doi.org/10.4300/JGME-D-20-00302.1
National University of Singapore, Yong Yoo Lin School of Medicine. (2020, June 30). Curriculum structure and requirements. https://www.nus.edu.sg/nusbulletin/yong-loo-lin-school-of-medicine/undergraduate-education/degree-requirements/bachelor-of-medicine-and-bachelor-of-surgery-m-b-b-s/curriculum-structure-and-requirements
Neufeld, A., & Malin, G. (2020). Twelve tips to combat ill-being during the COVID-19 pandemic: A guide for health professionals & educators. MedEdPublish, 9(1), 70. https://doi.org/10.15694/mep.2020.000070.1
Patil, N. G., & Yan, Y. C. H. (2003). SARS and its effect on medical education in Hong Kong. Medical Education, 37(12), 1127–1128. https://doi.org/10.1046/j.1365-2923.2003.01723.x
Peeri, N. C., Shrestha, N., Rahman, M. S., Zaki, R., Tan, Z., Bibi, S., Baghbanzadeh, M., Aghamohammadi, N., Zhang, W., & Haque, U. (2020). The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? International Journal of Epidemiolology, 49(3), 717-720. https://doi.org/10.1093/ije/dyaa033
Rose, S. (2020). Medical student education in the time of COVID-19. The Journal of the American Medical Association, 323(21), 2131-2132. https://doi.org/10.1001/jama.2020.5227
Samarasekera, D. D., Goh, D., & Lau, T. C. (2020). Medical school approach to manage the current COVID-19 crisis. Academic Medicine: Journal of the Association of American Medical Colleges, 95(8), 1126–1127. https://doi.org/10.1097/ACM.0000000000003425
Sandars, J., Correia, R., Dankbaar, M., de Jong, P., Goh, P. S., Hege, I., Masters, K., Oh, S.-Y., Patel, R., Premkumar, K., Webb, A., & Pusic, M. (2020). Twelve tips for rapidly migrating to online learning during the COVID-19 pandemic. MedEdPublish, 9(1), 82. https://doi.org/10.15694/mep.2020.000082.1
Schwartz, A. M., Wilson, J. M., Boden, S. D., Moore, T. J., Bradbury, T. L., & Fletcher, N. D. (2020). Managing resident workforce and education during the COVID-19 pandemic: Evolving strategies and lessons learned. Journal of Bone & Joint Surgery Open Access, 5(2), 1-5. https://doi.org/10.2106/JBJS.OA.20.00045
Seah, I. (2020). Striving as a nation to become an academic leader in the COVID-19 crisis. Singapore Medical Journal, 61(7), 370-372. https://doi.org/10.11622/smedj.2020059
Singapore Medical Council (2020a, May 29). Continuing medical education (CME) for doctors. https://www.healthprofessionals.gov.sg/smc/continuing-medical-education-(cme)-for-doctors
Singapore Medical Council (SMC) (2020b, May 29). Fulfilling continuing medical education (CME) requirements via online platforms. https://www.healthprofessionals.gov.sg/docs/librariesprovider2/continuing-medical-education-(cme)-for-doctors/circular—fulfilling-cme-requirements-via-online-platforms.pdf
Stetson, G. V., Kryzhanovskaya, I. V., Lomen‐Hoerth, C., & Hauer, K. E. (2020). Professional identity formation in disorienting times. Medical Education, 54(8), 765-766. https://doi.org/10.1111/medu.14202
Tolu, L. B., Feyissa, G. T., Ezeh, A., & Gudu, W. (2020). Managing Resident Workforce and residency training during COVID-19 pandemic: Scoping review of adaptive approaches. Advances in Medical Education and Practice, 11, 527–535. https://doi.org/10.3171/2020.4.JNS201012
Wald, H. S. (2020). Optimizing resilience and wellbeing for healthcare professions trainees and healthcare professionals during public health crises—Practical tips for an ‘integrative resilience’ approach. Medical Teacher, 42(7), 744-755. https://doi.org/10.1080/0142159X.2020.1768230
Wong, C., Tay, W., Hap, X., & Chia, F. (2020). Love in the time of coronavirus: Training and service during COVID-19. Singapore Medical Journal, 61(7), 384-386. https://doi.org/10.11622/smedj.2020053
Wong, J. E. L., Leo, Y. S., & Tan, C. C. (2020). COVID-19 in Singapore—current experience: Critical global issues that require attention and action. The Journal of the American Medical Association, 323(13), 1243. https://doi.org/10.1001/jama.2020.2467
Yang, D.-Y., Cheng, S.-Y., Wang, S.-Z., Wang, J.-S., Kuang, M., Wang, T.-H., & Xiao, H.-P. (2020). Preparedness of medical education in China: Lessons from the COVID-19 outbreak. Medical Teacher, 42(7), 787-790. https://doi.org/10.1080/0142159X.2020.1770713
*Claude J Renaud
Department of Medicine,
Division of Renal Medicine,
Khoo Teck Puat Hospital,
90 Yishun Central, Singapore 768828
Email: jeffrey.renaud@ktph.com.sg
Submitted: 16 July 2020
Accepted: 12 August 2020
Published online: 13 July, TAPS 2021, 6(3), 124-127
https://doi.org/10.29060/TAPS.2021-6-3/CS2344
Kirsty J Freeman, Weiren Wilson Xin & Claire Ann Canning
Office of Education, Duke-NUS Medical School, Singapore
I. INTRODUCTION
The Duke-NUS Medical School Simulated Patient programme is instrumental in the development of clinical and behavioural skills in the future medical workforce of Singapore. Starting with a group of 20 passionate individuals in 2007, the Simulated Patient programme currently engages over 100 individuals, of which 58% are Female, 42% are Male; with 46% over 50 years of age. Simulated Patients (SPs) are individuals who are trained to portray a real patient in order to simulate a set of symptoms or problems used for healthcare education, evaluation, and research (Lioce et al., 2020). The SPs are engaged across the curriculum and are specifically trained to provide realistic and convincing patient-centred encounters, as well as identify and give feedback on key elements of interpersonal and communication skills in face-to-face interactions for a unique educational experience.
Medical students at Duke-NUS engage with SPs from their first year, as they learn the fundamental skills of clinical practice (FOCP), the skill of history taking being one of the cornerstones of the programme. Keifenheim et al. (2015) define history taking as “a way of eliciting relevant personal, psychosocial and symptom information from a patient with the aim of obtaining information useful in formulating a diagnosis and providing medical care to the patient”. Several studies have reported on the impact of engaging SPs to teach history taking (Hulsman et al., 2009; Nestel & Kidd, 2003).
The COVID-19 pandemic dramatically impacted the delivery of on-campus education, requiring medical educators to adapt teaching methods to reflect governmental and institutional restrictions. Whilst journals have been expedient in their ability to publish the experience of educators and students during the COVID-19 pandemic, the experience of other stakeholders are lacking. This paper will describe the experience of simulated patients in adopting telesimulation during a pandemic.
II. ADOPTING TELESIMULATION DURING A PANDEMIC
McCoy et al. (2017) define telesimulation as “a process by which telecommunication and simulation resources are utilised to provide education, training, and/or assessment to learners at an off-site location” (McCoy et al., 2017, p. 133). With staff, students and SPs in numerous off-site locations (their own homes), the telecommunication platform adopted for this experience was Zoom. The main reason behind this was it was the platform of choice by the institution when face-to-face teaching was shifted to e-learning, therefore staff and students were familiar with the functionality. To effectively engage our simulation resources, i.e. our SPs, it was essential that we provide an orientation programme that would educate them on the use of telesimulation. Through an online training session, seen in Figure 1, the SPs were introduced to the rationale behind the adoption of telesimulation and the functionality of the Zoom platform. Topics such as how to use the video and audio effectively to build rapport during the interaction as well as functions such as moving between breakout rooms were covered. A telesimulation orientation manual was emailed to all SPs after the session, summarising the online training session, with step by step instructions and screenshot examples on how to use Zoom. See Figure 2 for summary of the orientation programme.

Figure 1. Simulated patient large group telesimulation training
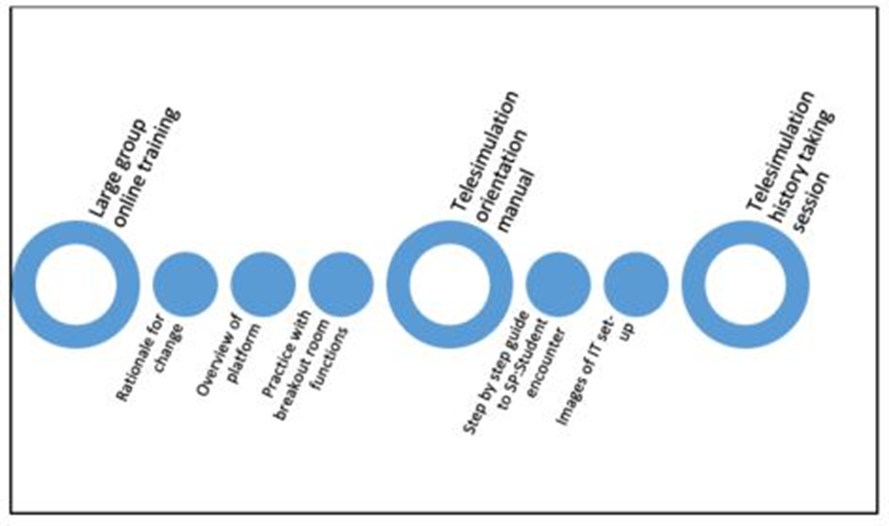
Figure 2. Summary of SP orientation to history taking telesimulation encounter
45 SPs participated in a series of tele-simulated history taking encounters for the class of 82 students. All SPs were invited to participate in a post tele-simulation history taking electronic questionnaire. Using a 5-point Likert scale SPs were asked to indicate their agreement on 13 items as seen in Table 1.
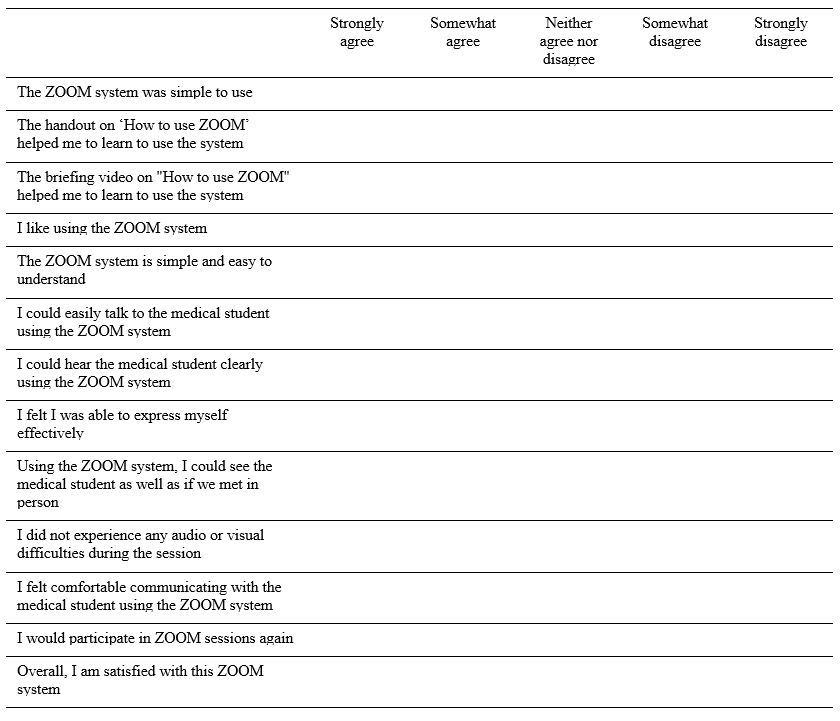
Table 1: Likert scale items form post-telesimulation evaluation questionnaire
III. THE SP EXPERIENCE
Of the 45 respondents 64% were male, 36% were female, with 93% stating that they had participated in previous face-to-face sessions with students. Aged between 21 and 71 years, half of the respondents were over 50. To participate in the telesimulation the majority of SPs (67%) utilised a laptop or desktop computer, with 71% reporting that they used a headset. 80% of the SPs had previous experience with video-based calls prior to this session.
Key to the history taking encounters is the ability to communicate clearly. While 11% of SPs did report some technical difficulties related to Wi-Fi connectivity, the majority of SPs (91%) could hear the student clearly and 89% felt they could express themselves effectively. 96% felt they could communicate easily with the student. On whether they could see the medical student as well as they would in a face-to-face interaction, responses were mixed, with SPs acknowledging that the limitations of the telesimulation experience is the non-verbal communication component of the interaction:
“Sometimes, the lighting is not good enough to see the expression on the student’s face”, and “I was not able to observe students’ body posture via zoom as such, I was unable to comment fully on students’ non-verbal communication skills”.
One of the themes that arose in the written feedback was that many SPs appreciated the travelling time saved by being off-site during the telesimulation:
“I used to take 45-60mins to arrive/return at/from a SP rehearsal/session. Now it only takes 15mins to be in the meeting – saves a lot of traveling time; and all is done in the comfort of my home :)”.
Whilst it was acknowledged that telesimulation could not replace the authenticity of face-to-face interactions, the SPs overwhelmingly rated the experience as extremely positive, noting that the online training session and handout helped in learning how to negotiate the online platform. An unexpected benefit that was shared was the sense of connection that the telesimulation experience provided the SPs during a time of lockdown, as they “got to see other SPs”. One respondent shared how they were able to integrate these new skills to maintain social connections:
“…even it has broadened my experience and now been using this app for communication with friends during this CB (circuit breaker)”.
IV. CONCLUSION
As the restrictions around face-to-face teaching due to COVID-19 continues to impact how health professional educators engage SPs in teaching and assessing, this paper demonstrates how to safely and effectively engage the SP workforce during a pandemic. By describing the experience of SPs in adopting telesimulation to teach history taking, we hope that fellow educators across the region can continue to engage SPs in their curriculum.
Notes on Contributors
Kirsty J Freeman is the main author, conceptualised, wrote and revised the manuscript based on comments and suggestions from the other authors. She contributed to the development and facilitation of the simulated patient telesimulation training programme, and conducted the data collection.
Xin Weiren Wilson developed and conducted the simulated patient telesimulation training programme, assisted with data collection, performed the data analysis, and developed the manuscript.
Claire Ann Canning assisted with data collection, and contributed to the conceptualisation of the manuscript, reviewed and revised drafts.
All the authors have read and approved the final manuscript.
Acknowledgements
We would like to thank all the simulated patients who took part in the telesimulation programme and were willing to share their experiences. We also wish to acknowledge the Clinical Faculty and Administrative Coordinators of the FOCP programme for adopting telesimulation into the programme.
Funding
This work has not received any external funding.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Hulsman, R. L., Harmsen, A. B., & Fabriek, M. (2009). Reflective teaching of medical communication skills with DiViDU: Assessing the level of student reflection on recorded consultations with simulated patients. Patient Education and Counseling, 74(2), 142-149. https://doi.org/10.1016/j.pec.2008.10.009
Keifenheim, K., Teufel, M., Ip, J., Speiser, N., Leehr, E., Zipfel, S., & Herrmann-Werner, A. (2015). Teaching history taking to medical students: A systematic review. BMC Medical Education, 15(159), 1-12. https://doi.org/10.1186/s12909-015-0443-x
Lioce L., Lopreiato J., Downing D., Chang T.P., Robertson J.M., Anderson M., Diaz D.A., Spain A.E., & Terminology and Concepts Working Group (2020). Healthcare Simulation Dictionary (2nd Ed.). Agency for Healthcare Research and Quality. https://doi.org/10.23970/simulationv2
McCoy, C. E., Sayegh, J., Alrabah, R., & Yarris, L. M. (2017). Telesimulation: An innovative tool for health professions education. Academic Emergency Medicine Education and Training, 1(2), 132-136. https://doi.org/10.1002/aet2.10015
Nestel, D., & Kidd, J. (2003). Peer tutoring in patient-centred interviewing skills: Experience of a project for first-year students. Medical Teacher, 25(4), 398-403. https://doi.org/10.1080/0142159031000136752
*Kirsty J Freeman
Duke-NUS Medical School
8 College Rd,
Singapore 169857
Email: kirsty.freeman@duke-nus.edu.sg
Submitted: 24 December 2020
Accepted: 10 March 2021
Published online: 13 July, TAPS 2021, 6(3), 10-13
https://doi.org/10.29060/TAPS.2021-6-3/GP2455
Young-Mee Lee1 & Hyunmi Park1,2
1Department of Medical Education, Korea University College of Medicine, Seoul, South Korea; 2Department of Brain Convergence Research Center, Korea University College of Medicine, Seoul, South Korea
Abstract
Introduction: We describe the circumstances and adaptations in the South Korean medical education during the COVID-19 pandemic and discuss areas in need of improvement in preparation of a worsening situation or for similar future public health crises.
Methods: Literature reviews, focusing on research papers about medical educational changes in South Korea during the COVID-19 pandemic were performed. Selective data collected from a nationwide online survey by the Korean Association of Medical Colleges on the status of curricular changes in medical schools during the COVID-19 was presented.
Results: All lectures have moved online, but clinical students continued their hospital placements during the pandemic, except for the first 3-5 weeks during the first surge in 2020. Initial technical naivety of the faculty and lack of technical resources were short-lived and the medical students settled well showing a much higher than expected student satisfaction level over online education. Practical skills sessions which benefit most from onsite hands-on experiences such as anatomy dissection, were delivered through a blended approach in some medical school. Student evaluation is the area of least change, mainly due to the students’ lack of trust in online assessments.
Conclusion: South Korea’ underwent major changes in medical education brought upon COVID-19 and the readiness of the technology adoption has been much increased. Student evaluation is the area of least transformation. Adoption of a programmatic assessment system should be considered to enhance not only learning but also improve trust among stakeholders of medical schools.
Practice Highlights
- Medical education in South Korea has evolved rapidly due to COVID-19.
- Korea’s medical schools moved all its lectures online with positive student responses.
- Clinical placements continued under strict personal protection equipment.
- The readiness of technology adoption in education bore fruit during the current pandemic.
- Assessment is the area of least change, but to prepare for the future, adaptations are necessary.
I. INTRODUCTION
However, from the beginning of December 2020, the daily positive COVID-19 patients have steadily increased reaching the new 1,000 mark by mid-December. The government having raised its social distancing level up to 2.5 in the Seoul metropolitan area, is contemplating raising it to the maximum, which will become akin to the European lockdown with most non-essential businesses and institutions shutting down. At the time of writing this paper in the middle of December the whole country is trying hard to avoid lockdown.
In this paper, the authors described the circumstances and adaptations in the South Korean medical education during the COVID-19 pandemic with some specific examples and discuss areas in need of improvement in preparation of a worsening situation or for similar future public health crises.
II. OVERALL ADAPTATIONS IN MEDICAL SCHOOL WITH SPECIFIC EXAMPLES
On the 30th of January 2020, the Korean government, via the Central Disease Control Headquarters, raised the infectious disease alert level to three out of the four-tier system, and the Korean Association of Medical Colleges (KAMC) produced its first recommendation for its 40 medical schools. This recommendation included advice to medical schools to enhance its infection control measures, augment communication with the students and hospitals, and provide adequate personal protective equipment (PPE) to all students in the clinical hospital rotation. On the 23rd of February 2020, the Korean government raised its infectious disease alert to the highest level. On the 24th of February 2020, KAMC released its second guidance to all medical schools, relaying the advice from the ministry of education on delaying the school opening date for 2 weeks and suspending all clinical rotations.
To explore the overall adaptations in medical schools by the mid-May 2020, KAMC conducted a nationwide online survey which 37 deans out of the 40 medical schools in South Korea participated in. This survey showed that all 37 medical schools had changed to online education for their preclinical courses. Laboratory skills in basic science subjects moved online, but anatomy dissection laboratory varied: online e-Anatomy replaced them in 11 schools, and 14 schools delayed it to the end of semester, and 10 schools proceeded with on-campus cadaveric dissection under strict infection control measures when the government social distancing level decreased to level 2 (the daily new positive COVID-19 patient fell under 100). The early glitches derived from the technical naivety of the faculty and lack of technical resources did not last long, and all students, faculty and institutions adapted rapidly, which resulted in a much higher than expected student satisfaction level on online education. The area of least change was in the student assessment. The student assessment was mostly delayed, and held later in face-to-face format at the end of the semester.
The suspension of clinical rotations varied widely between schools, from the first week of March to the last week of May 2020, with a median of 21 days. 14 schools provided online teaching and one school provided alternative simulation lessons but without patient contact during the closure or delay of clinical rotations. Before making the decision on restarting clinical rotations, there were high tensions between medical schools and students and even parents who were concerned and nervous on the potential infection risk to students that the hospital rotations potentially posed. To reduce this anxiety, medical schools held a series of meetings with student representatives and after putting in place safeguards against the risk of COVID-19 infection including PPE, the clerkships restarted. KAMC’s great efforts in the procurement of masks for medical students was critical for restarting clinical rotations, and medical schools were able to provide five masks per student per week even during the period of extreme masks shortage (Park et al., 2020).
A. Blended Anatomy Learning: Does Students’ Satisfaction Equal Achievement of Intended Learning Outcomes?
In the authors’ medical school, the COVID-19 pandemic forced the anatomy course to change from the traditional large group lectures and cadaveric dissection to blended anatomy courses. The theory lectures were delivered entirely online and the anatomy dissection course, resulted in an inadvertent flipped learning effect. The e-Anatomyâ videos (Panmun Education, Seoul, Republic of Korea), and Complete Anatomyâ (Elsevier, Amsterdam, Netherlands) online platform were provided to students as home assignment while on-campus dissection sessions were suspended. At the end of April, face-to-face cadaver dissections recommenced following the infection prevention measures guidelines with the use of proper PPE.
Although the students’ responses to the online anatomy teaching were remarkably positive, the anatomy department faculty at the authors’ school were concerned about the effectiveness of the altered teaching methods in achieving the intended learning outcomes. Therefore, Yoo et al. (2021) examined the educational outcomes of the online and blended learning approach in anatomy, and the results showed the anatomy achievement scores of the blended learning group (the 2020 class) being higher than those of traditional lectures (2019 class). The authors of this study interpreted that in-advance self-study at home using online learning videos before the actual on-campus dissection labs induced a flipped learning effect, and online education let the students to achieve more self-study time and individual tailored learning.
B. Adaptations in Paediatric Clerkship Education
As described earlier, most university-based hospital rotations restarted around March 16th with limited patient contact in respiratory and primary community clinics. Although the reduced patient volume which students could come into contact was inevitable, this situation was most serious in paediatric clinical clerkships. Paediatric patients visiting primary clinics and even tertiary university hospitals drastically decreased down in South Korea during the COVID-19 pandemic. In addition, the paediatric parents’ refusal or complaints on being seen by medical students worsened and the number of medical students allowed into hospital rotations were restricted in some hospitals.
To overcome the shortcomings of paediatric clerkship education, the authors of the study (Lee, K. D. Park et al., 2020) created an actual patient encounter-based role play. One student within the student group (usually 3-4 students in one group) performed a history taking and physical examination of a hospitalised child with a guardian, who later played the role of the parent, with another student in the same group taking the doctor’s role, interacting with each other in front of faculty physicians, residents, and the rest of the peer students. This role play session facilitated the provision of feedback and discussion. The students’ responses to the alternative educational approaches were positive, but the students required more discussion, and detailed feedback from the faculty physicians on their performance.
C. Online Medical Education Seminar for Faculty
Although the advantages of webinars in higher education and professional training have already been proven, they have not been widely used in South Korea before the COVID-19 pandemic. However, currently webinars and online academic conferences have almost totally replaced onsite gatherings. The COVID-19 pandemic has forced the Faculty Academy of Medical Education (FAME) seminars at Korea University College of Medicine (KUCM) to go online (Lee, H. Park et al., 2020). The authors of this study reported that FAME was established to enhance the teacher’s educational competency and promote a positive educational culture, but the participation of faculty members in this seminar has not been very active. When FAME had to be abruptly changed to online, the authors moved the seminar format online with pessimistic expectations of further decrease in the number of participants. However, such expectations were thoroughly shattered on April 8th by the login attendance of 210 faculty members on the first webinar which was the highest attendance since its inception in 2012. Although the webinar for faculty development was launched successfully and received positive reviews, further studies should follow to examine its educational effectiveness.
D. Medical Licensing Examination
The Korean Medical licensing exam consists of two parts; the written test takes place annually in January and the clinical skills test is held the previous year usually between September and October. During the span of 35 days 3,100 participants are examined in one examination centre. This year, the clinical exam was planned to be held between September 1st and October 27th, at its usual centre under strict infection control measures. However, another unprecedented crisis was added on the present COVID-19 pandemic in South Korea. In August 2020 Korean doctors held a series of national strikes as the government tried to push new policies amidst a pandemic where healthcare workers have been working tirelessly over the previous half a year to maintain the COVID-19 cases at bay and protecting the public. The doctors’ national protest was triggered by a sudden governmental announcement on critical policy changes without any previous discussion or consultation to medical associations or medical education authorities. The policies included the foundation of a ‘public medical school’ funded by taxpayers’ money with a non-transparent admission criterion and an exemption from the standard accreditation process to accelerate its building. This policy only focused on increasing the total number of doctors with the hope to fill the currently essential specialties which residents undersupply without dealing with the core underlying problem.
The national doctors strike resulted in 86% of medical students forfeiting their application for the national licensing exams (Kim & Choi, 2020) with only around 400 students undertaking the clinical exam on site wearing masks. All the stations were carried out as before with only the oral cavity examination being replaced for a verbal explanation.
III. DISCUSSION
Korea has managed the COVID-19 situation relatively well and only the lectures were moved online, whilst exams were carried face-to-face, and almost near-normal clinical practice training ensued in medical education. This double edge sword situation might not have prepared us as a nation in the event of a worse pandemic in the future. Fortunately, we can learn from the published experiences of other countries such as virtual rounds, virtual patient encounters, clinical skills simulations through the use of information technology (IT), and from virtual or augmented reality experiences used in resident skills training.
Remarkable advances in the Korean medical education in recent decades, especially, the readiness of technology adoption in education bore fruit during the current pandemic. More importantly, the experiences gained by educators during COVID-19 have consolidated student-centred education which was previously a concept rather than an actioned need. Nevertheless, student evaluation is the area of least transformation. The main reason for the resistance by the students towards online assessments is the lack of trust in the security and fairness of such method. The students’ negative perceptions over online assessments are mainly due to their belief that no technical method can 100% prevent cheating. Some medical educators pointed out that having to consider using various devices to prevent cheating during online exams is born out of the schools’ mistrust towards students, a non-educational behaviour in need of reconsideration. However, in Korea, the distrust among student peers is a bigger issue than the mistrust between the schools and students. To reduce the distrust surrounding examination, we should reconsider the current competitive summative assessment system. We could aspire for a better model, which can promote student learning instead of focusing on achieving good grades only. It is time to discuss a transition to a programmatic assessment and investigate ways on its adaptation and incorporation in medical education.
The authors of this article described major changes in medical education brought upon COVID-19 and the lessons what we’ve learned in South Korea. Since each country has faced differing levels of the COVID-19 crisis, our experience in South Korea may not be directly transferrable to other countries or contexts. However, sharing eclectic experiences from differing countries the mounting literature that can be tapped into by countries who find themselves in similar situations as ours in the future. Medical educators should actively share their novel ideas, experiences and hardships encountered on medical education through the current health crisis, as such cooperation will prepare us all against the uncertain medical future.
Notes on Contributors
Young-Mee Lee is a professor at the Department of Medical Education, Korea University College of Medicine, Seoul, South Korea, reviewed the literature, developed the methodological framework for the study, performed data analysis and developed the manuscript, gave critical feedback to the writing of the manuscript.
Hyunmi Park, MBChB, FRCS, PhD, is a research professor at the Department of Brain Convergence Research Center, Korea University, Seoul, South Korea, reviewed the literature, analysed the data and was involved in the writing of the draft, review and editing of the manuscript.
Both authors have read and approved the final manuscript.
Acknowledgments
We, authors of this study, are very grateful to KAMC for sharing the national survey data so we could perform the analysis and interpretation of such data. We wish to show our deepest gratitude to every single one of the Korean medical school deans, who not only have taken their time to participate in our study, but have tirelessly worked during the worst pandemic in living memory to ensure the safety of students and staff whilst maintaining the highest of standards in medical education.
Funding
There are no funding sources to declare.
Declaration of Interest
No conflicts of interest to declare.
References
Kim, M., & Choi, H. (2020). S. Korean government to not let over 2,700 medical students another shot at medical licensing exam. Hankyoreh. http://english.hani.co.kr/arti/english_edition/e_national/961515.html
Lee, Y. -M., Park, H., Pyun, S. B., & Yoon, Y. W. (2020). Enforced format change to medical education webinar during the coronavirus disease 2019 pandemic. Korean Journal of Medical Education, 32(2), 101–102. https://doi.org/10.3946/KJME.2020.158
Lee, Y. – M., Park, K. D., & Seo, J. H. (2020). New paradigm of pediatric clinical clerkship during the epidemic of COVID-19. Journal of Korean Medical Science, 35(38), 1–5. https://doi.org/10.3346/JKMS.2020.35.E344
Park, J., Park, H., Lim, J. E., Rhim, H. C., & Lee, Y. -M. (2020). Medical students’ perspectives on recommencing clinical rotations during coronavirus disease 2019 at one institution in South Korea. Korean Journal of Medical Education, 32(2), 223–229. https://doi.org/10.3946/KJME.2020.170
Yoo, H., Kim, D., Lee, Y. -M., & Rhyu, I. J. (2021). Adaptations in anatomy education during COVID-19. Journal of Korean Medical Science, 36(1), e13. https://doi.org/10.3346/jkms.2021.36.e13
*Young-Mee Lee
Department of Medical Education,
Korea University College of Medicine,
73 Goryodae-ro, Seongbuk-gu,
Seoul, 02841, Republic of Korea
Email: ymleehj@korea.ac.kr
Submitted: 28 July 2020
Accepted: 3 December 2020
Published online: 13 July, TAPS 2021, 6(3), 75-82
https://doi.org/10.29060/TAPS.2021-6-3/OA2366
Kirsty J Freeman1 & Brid Phillips2
1Office of Education, Duke-NUS Medical School, Singapore; 2Health Professions Education Unit, The University of Western Australia, Australia
Abstract
Introduction: Healthcare requires its practitioners, policymakers, stakeholders, and critics to have empathetic awareness and skills in critical thinking. Often these skills are neglected or lost in current educational programs aimed at those interested in the field of health. Health humanities and, in particular narrative medicine, aim to redress this omission.
Methods: We used a mixed methods approach to explore the experience of health humanities students in creative writing and staged readings to foster empathic awareness and critical thinking. Data was collected from 20 second-year students enrolled in an undergraduate health humanities unit via a post-assessment survey, and thematic analysis of a reflective paper.
Results: 92.9% of the students felt that writing a creative piece helped them to understand the health topic from a different perspective, with 85.7% reporting that the use of creative writing helped to create emotional connections. From the reflective paper, six themes were elicited through the thematic data analysis: (1) The value of language; (2) Insights into the patient experience; (3) Giving voice to the patient; (4) Creating empathic exchanges; (5) Illness and emotion; and (6) Reflective practice.
Conclusion: By offering a mode of experiential learning involving both creative writing and staged readings, students develop empathic ways of thinking and being while deepening their critical engagement with a range of health topics. Students were able to understand the need to make humanistic sense of the health and well-being narrative, providing them with a range of transferable skills which will be an asset in any workplace.
Keywords: Narrative Medicine, Empathy, Critical Thinking, Staged Reading, Health Humanities
Practice Highlights
- Creative writing and staged readings are effective in fostering empathetic awareness and critical thinking.
- Narrative medicine techniques result in greater understanding about the perspectives of others.
- Developing creative language leads to enhanced communication skills and nuanced ways of thinking.
- Staged readings delivered online provide effective teaching and learning opportunities.
I. INTRODUCTION
Health humanities, and the attendant field of medical humanities, refer to the application of the creative or fine arts (visual arts, performing arts etc.) and humanities disciplines (literary studies, law, history, philosophy, etc.) to discussions and explorations on the nature of human health and well-being (Crawford et al., 2010). Within this broad umbrella lies the discipline of narrative medicine. The application of humanities to health has had a long pedigree, but the distinct disciplines of both narrative medicine and health humanities only began to emerge over the first decade of the 21st Century. In part, they emerged from a growing concern about an increasing lack of empathy in health professionals (Dean & McAllister, 2018; Lai, 2020). Narrative medicine with its interest in creativity and ambiguity strives to address this concern. Through narrative medicine, skills in thinking reflectively, listening actively, observing more closely and writing creatively can be developed. It has been shown that there is a positive impact on empathy and communication following narrative medicine education (Barber & Moreno-Leguizamon, 2017). This is important as the empathy conveying physician is more successful in promoting better clinical outcomes for patients. However, ‘[d]espite the centrality of stories to many of the tasks that clinicians perform it remains that explicit and formal teaching of knowledge and methods in narrative is relatively novel’ (Boudreau et al., 2012, p. 152).
One of the educational techniques embraced in narrative medicine is staged readings. A staged reading is an event which may have some rehearsal time, but the readers use scripts on stage. There is minimal staging, costuming, and props. This is pertinent as the use of theatre in academic teaching represents a new model of education that reminds students of the humanity of people (Baker et al., 2019). This form of engagement involves an emotional transaction through the spectacle of theatre which, as the Greeks understood it, was an occasion that provided recognition, catharsis, and release for both the individual and the wider community (Shapiro & Hunt, 2003). Health topics are also more easily understood through the medium of performance (Ünalan et al., 2009). Ünalan et al. (2009) also surmised that theatrical performance could increase empathy levels. There are similar benefits to be had from staged medical readings which foster introspection and reflection (Matharu et al., 2011). The purpose of this study was to determine whether the use of creative writing and staged readings could develop empathy and critical thinking in second year university students enrolled in an undergraduate health humanities unit of study. Student enrolment information confirms majority of students are on a pathway to studying medicine, pharmacy, dentistry, ophthalmology, or global health.
A. Context
In semester one of 2020, 20 second-year students were enrolled in a narrative medicine unit, as part of their undergraduate bachelor’s degree. By delivering an undergraduate unit in narrative medicine, the goal is to give students the opportunity:
- To dip their toes into the world of literary fiction.
- To present their own creative pieces relating to health topics.
- To gain an understanding of health issues from the perspective of others as this increases empathetic awareness.
Through a series of scaffolded assessments, students have a unique opportunity to develop empathetic awareness and critical thinking skills through creative presentations mimicking staged readings.
Two of the three assessments related to the staged reading, the second assessment was a creative piece and the third was a reflection on process of creating the piece and the health topic to which it related. The purpose of these assessments was to demonstrate different modes of narrative writing. This was achieved through the construction of a creative piece that explored a health topic using narrative medicine techniques including but not limited to short story writing, poetry, and play writing.
The unit involved supporting students to devise a short creative writing piece. Within the piece, themes of empathy, communication, cultural difference, and societal biases and assumptions around the students’ chosen health topics were explored. The piece was then to be presented as a staged reading by the students for an invited audience. The audience would include the wider university community of undergraduate and postgraduate students, staff, and invited guests such as health professionals to the reading. Immediately following their reading, the students, supported by academic staff, were to hold a guided discussion on the significance of health topics in the piece. This discussion would bring biases and assumptions into focus and heighten the individual’s awareness of emotional dynamics at work in the healthcare context while also offering insights into the perspective of others. Similar programs have been used to educate bioethical students, help them to develop discussion questions, and enhance their critical self-reflection (Kerr et al., 2020; Robeson & King, 2017).
Students were required to read a literary fiction novel, Extinctions (Wilson, 2020). The act of reading itself has demonstrated benefits of improving processing of experiences and developing empathy. Reading literature also improves our social awareness and our ability to see the perspectives of others (Fennelly, 2020; Kaptein et al., 2018). In the novel Extinctions, there are many discernible health topics such as traumatic brain injury, drug use, ageing, mobility issues, death and dying, and loss of independence. There is also a range of characters involved in these issues from a young girl with a drug problem to the protagonist, Fred, a man in his declining years. It was important to foster student engagement with the project by offering a fully scaffolded experience to allay performance anxieties. Scaffolding has been shown to support students as they negotiate a challenging environment and allow them to make meaning for themselves rather than have it imposed on them from an autocratic perspective (Wilson, 2016). Each week from the first week of semester, the seminar included both a close reading exercise and a creative writing exercise. The scaffolding also included several resource folders addressing the main genres the students were encouraged to explore – short story, poetry, drama. The folders contained videos, book chapters, blog posts, and journal articles that introduced the students to ways of writing creatively. There was also a dedicated workshop which explored these techniques and answered any questions the students had on creative writing.
Due to COVID-19 restrictions on social gatherings and the cancellation of face-to-face interactions, the presentation aspect had to be cancelled at short notice and instead, presentations took place online without the wider audience participation. The creative pieces were read in an online forum limited to students and the unit coordinator. The students had the opportunity to read their work to other participating students and to lead a short discussion on their health topic. This sharing is important as ‘representation is always a dialogue, in which, the receiver of the work contributes a necessary response to the creator of the work’ (Charon et al., 2016, p. 347). As the students based their pieces on fully rounded characters from the novel, this process shares similarities with verbatim theatre. Verbatim theatre has been shown to allow positive exploration of emotional behaviours (Scott et al., 2017). After this process, students were encouraged to incorporate feedback from the presentations into their pieces before submission of the creative piece.
The third assessment component of the unit required the students to submit a reflective essay on the experience where they discuss the creative process and their representation of the health topic which they had chosen. They had to discuss the significance of the health topic and examine their personal responses to the topic and how it was influenced by their research, the creative process, and the discussions which took place following the presentation of the piece. To support the reflective process, we developed a reflective writing toolkit which illustrates both the process and its importance.
II. METHODS
A cross-sectional mixed methods design was used to evaluate the experience of health humanities students in creative writing and staged readings to foster empathic awareness and critical thinking. 20 second-year students who were enrolled in a narrative medicine unit between January and June 2020 were invited to participate.
A. Data Collection and Analysis
Data was collected at two points over the semester, an online survey in week 10, and a reflective paper at the end of semester in week 13.
1) Creative writing and staged reading assessment student experience survey: All 20 undergraduate students enrolled in the unit in semester one, 2020, were invited to participate in an online survey examining the student experience of participating in the creative writing and staged reading assessment. The survey tool curated by author one (KF) was designed to collect basic demographic data about the student, along with information about their current enrolment. The survey was designed to evaluate the first two level of Kirkpatrick’s model of program evaluation, level one being reaction and level two learning (Frye & Hemmer, 2012). Given that this is the first time the program had been offered, the authors felt that the data collected would provide a baseline upon which further detailed evaluations can build upon. Students were asked to rate their experience with the staged reading project using a five-point Likert scale, as well as responding to open-ended questions designed to further expand on the students’ experience. A statement of voluntary consent was included at the start of the survey and the participant had to agree to the consent before the survey could commence. Thus participation in the anonymized online evaluation indicates consent. Descriptive statistics were calculated for the demographic data. Categorical data are presented as number and percentage. The analyses were performed using IBM SPSS Statistics Version 25.0. Thematic analysis of the open-ended questions was then undertaken. Researcher bias was minimised by having author one (KF), who was not involved in delivering the course, undertake the analysis of the survey data.
2) Staged reading reflective essay: The second data collection point was a reflective essay (n=20). Thematic analysis of the text was undertaken by both authors. Each author reviewed the transcripts separately, making note of key phrases, outline possible categories or themes. Discussion of our interpretations took place over teleconference, as we then jointly rearranged and renamed the codes, developing higher order themes. NVivo 12™ was used to manage the qualitative data (QSR International., 2018). This mixed methods design combines quantitative and qualitative data to provide a richer source of information about the experience of staged readings.
III. RESULTS
A. Creative Writing and Staged Reading Assessment Student Experience Survey
Of the 20 students enrolled in the unit, 14 completed the student experience survey, a response rate of 70%. Table 1 summarises the demographic characteristics of the respondents. As can be seen in Table 1, the students were enrolled in one of three bachelor degrees. The degree enrolled by majority of students in is science based, with only 1 respondent studying an Arts based degree. 92.8% of respondents had not previously completed an undergraduate degree. Three respondents spoke languages other than English at home.
When asked to rate their experience in the staged reading project 92.9% of the respondents felt that writing a creative piece helped them to understand the health topic from a different perspective; with 85.7% reporting that the use of creative writing helped to create emotional connections (Table 2).
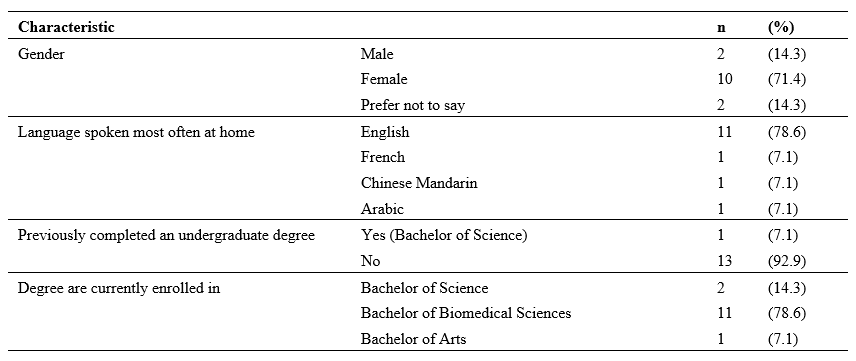
Table 1. Summary of demographic characteristics of respondents
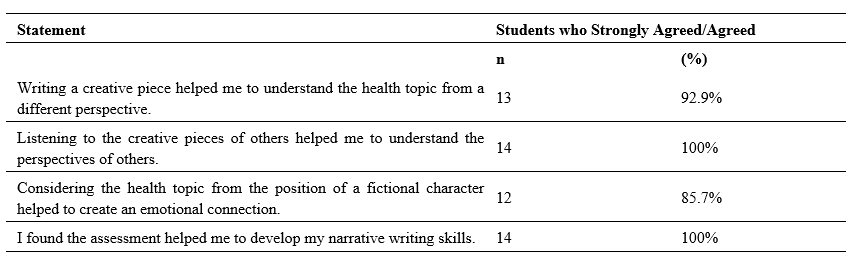
Table 2. Student rating of creative writing and staged reading assessment
When asked to describe their experience of the staged reading assessment in the free text survey questions students reported feeling daunted, nervous and apprehensive about the prospect of writing a creative piece, as many of them shared that they had little or no experience with creative writing. With several students describing to task as challenging, on reflection they expressed feeling fulfilled, enriched, sharing that they found the task rewarding.
A. Staged Reading Reflective Essay
The qualitative data analysis resulted in six themes being identified: (1) The value of language; (2) Insights into the patient experience; (3) Giving voice to the patient; (4) Creating empathic exchanges; (5) Illness and emotion; and (6) Reflective practice (Figure 2). These themes are described in this section, illustrated with representative quotes.
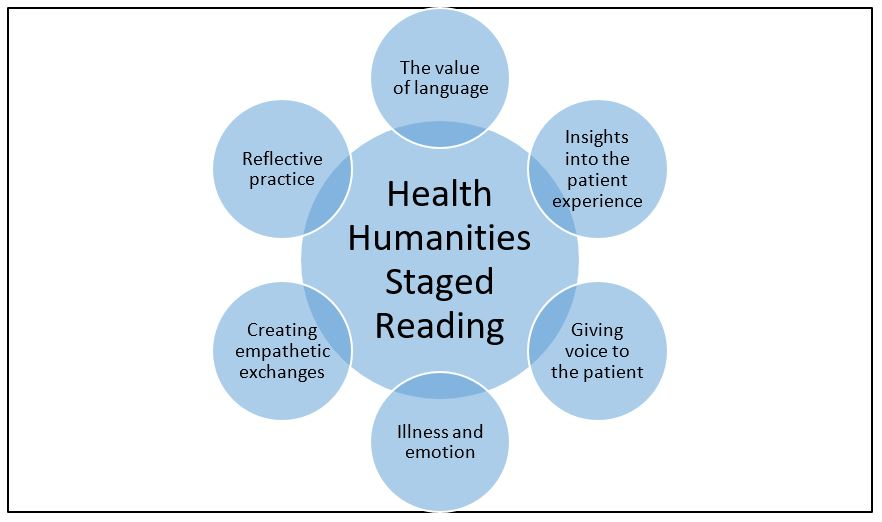
Figure 1. Overview of the staged reading themes
1) The value of language: as they worked through their creative piece, students discovered the value and power of language as a tool for expression and communication. Students commented on their appreciation of language:
Since I wanted to create a powerful and emotional piece, I experimented using literacy techniques to achieve a desperate and anxious tone.
Student 2
I learnt that the use of language is also vital in writing a creative piece, emphasising the importance of communication between the author and readers.
Student 14
2) Insights into the patient experience: Students developed an awareness of the value of research when trying to understand the issues surrounding health topics. Better equipped with quality knowledge and research, they were able to give more nuanced accounts of health experiences. Students learned the value of looking beyond the symptom to see the whole person and, thus the value and importance of person-centred care:
Acknowledging that my research and reflections had resulted in greater understandings of both the health topic and the importance of seeing a patient beyond their physical disease.
Student 2
It is very important to take into consideration all aspects of what a person is experiencing in order to make the best assessment and to come up with the best route of action to help the patient overcome whatever it is they are suffering from.
Student 1
3) Giving voice to the patient: Students gained an insight into the need to give a voice to patients in order to gain better understanding of the perspectives of others. They reflected on the powerlessness and silence that often surrounds certain conditions and situations:
I felt that I was able to give Katie an authentic voice, through which readers were then able to empathise with, and better understand, her struggles.
Student 4
Furthermore, the narratives of victims can empower them by giving them a voice in times when they are often silenced.
Student 7
4) Creating empathetic exchanges: Students gained an understanding of empathetic exchanges and in some instances understood the need to create opportunities for the development of empathy. The students did not always articulate the word empathy but instead alluded to the concept by talking about experiencing and understanding the emotions and perspectives of others:
I felt increased levels of empathy towards individuals dealing with the disorder as I now understand the many other challenges and hurdles that accompany eating disorders that I didn’t know prior to this assignment.
Student 8
When using these descriptions, I felt that I was able to build an emotional connection with Katie’s character, thus encouraging readers to also empathise with her situation.
Student 4
5) Illness and emotion: Students discovered that emotional transactions and states are intertwined with health and illness. They understood, through their work, the interconnectiveness of emotional responses and illness. Some of their observations included:
I have become more sensitive to the idea that human beings are inherently emotional and can be affectively moved when provided with an impetus.
Student 3
The purpose of the piece was unearthing the complex thoughts and emotions individuals with eating disorders and substance abuse go through.
Student 8
6) Reflective Practice: On topics where students previously had felt knowledgeable, deeper reflection and considerations revealed their own misconceptions and lack of knowledge. Within this paradigm, they also showed a maturation of habits and behaviours. Their comments were insightful:
I entered a phase of reflection where I realised that I would have previously contributed to these harmful views.
Student 2
I learnt and later researched further the differences in the perception of STEM women in both Western and Asian populations. This is something I would attempt to change. It was really interesting for me to discover that I had this unconscious bias forcing me to further expand my learning and knowledge in the area.
Student 18
IV. DISCUSSION
While the use of creative writing and staged readings is a developing area in health humanities, the findings of this study suggest that they are effective in fostering emotional awareness and critical thinking. McDonald et al. (2015) found that ‘[a]nalysis of the student’s writing showed that they demonstrated the ability to “stand in another’s shoes” and, interestingly, the students’ comments on their own writing showed that their ability to relate to characters they initially felt little affinity for deepened’ (McDonald et al., 2015, p. 9).
By taking part in the creative writing project and the accompanying reflection piece, students were exposed to an innovative and experiential form of learning that provided a unique pedagogical experience. Whilst the students reported being daunted at the thought of constructing a creative piece, the self-reflective processes and actively engaging with the perspectives of others, ensured students were able to enhance their critical thinking skills. In the creative writing and staged reading assessment student experience survey, 100% of students agreed, “Listening to the creative pieces of others helped me to understand the perspectives of others”. This accords with the work of Deloney and Graham who note “[e]xperiential learning activities increase student engagement and are a helpful tool to connect abstract ideas with concrete knowledge” (Deloney & Graham, 2003, p. 249).
The findings of this study highlight the value of language as a tool for expression and communication. Educators need to be mindful of their student population when contemplating incorporating creative writing and staged readings into their programs. For students to be accepted for enrolment at The University of Western Australia they must demonstrate a minimum level of English language proficiency necessary for academic studies. Whilst there has been several studies examining what Hyland calls “linguistics disadvantage in terms of a Native/non-Native divide” (Hyland, 2016, p. 61) in academic writing (Badenhorst et al., 2015; Bocanegra-Valle, 2014; Zhao, 2017), the impact of this linguistic divide in creative writing and staged readings has not been fully explored.
The students gained insights into holistic care relating to both themselves and others. As these are undergraduate students, many on a pathway to a career in health, insights into holistic care and self-care are valuable life lessons. There was also an indication that the process contributed to the social and cultural well-being of themselves and others. Nagji et al. (2013) note that theatre based programs/novel humanities based curriculum items contribute to student well-being, an increasingly important area for universities to address particularly during a pandemic. Although the student population participating in this unit are studying science-based degrees where creative writing is not commonplace, the learning strategies were structured in a way that enabled development of narrative writing skills.
By integrating the narrative medicine techniques of creative writing and staged readings the students were able to give more nuanced accounts of health experiences. Students learned the value of looking beyond the symptom to see the whole person and, thus the value and importance of person-centred care. This gave them valuable insights into the patient experience. During this process, students gained an insight into the need to give a voice to patients in order to gain better understanding of the perspectives of others. They learnt about the powerlessness and silence that often surrounds certain conditions and situations. In their responses, the students did not always articulate the word empathy but instead alluded to the concept by talking about experiencing and understanding the emotions and perspectives of others. Students gained an understanding of the power of empathetic exchanges and in some instances understood the importance of creating empathetic exchanges opportunities. Another important theme which was uncovered, was a growing awareness amongst students that emotional transactions and states are intertwined with health and illness. They understood, through their work, the interconnectiveness of illness and emotion. On topics where students previously had felt knowledgeable, deeper reflection and considerations revealed their own misconceptions and lack of knowledge. Within this paradigm, they also showed a maturation of habits and behaviours leading to improved reflective practices.
There were limitations with the project as we had to move from face-to-face to online teaching due to constraints placed upon teaching during the COVID-19 pandemic. However, the online format did have some unexpected benefits, with a number of students feeling less intimidated when presenting online compared to a face-to-face workshop. Despite the move to online teaching, the cohort remained present and engaged in the project. Many expressed regrets at losing physical contact and the incidental discussions that happen before and after classes but overall with support they adapted well.
V. CONCLUSION
This study has described the experience of students engaging in creative writing and staged readings as part of a narrative medicine unit. Students completing the unit and its attendant assessments developed useful life skills including critical thinking, understanding the perspectives of others, and the positive use of narrative in appreciating the experiences of others. The work engaged them in new and innovative ways evidenced by some statements which noted that their experience in this unit was unique in their university journey. Having autonomy over the health topic they chose, the character they explored, and the creative medium they used to express their thinking, enhanced the learning experience and allowed them to meet the learning outcomes of the unit.
Notes on Contributors
Kirsty J Freeman crafted the paper with her co-author, performed the data collection and analysis of the survey, and undertook thematic analysis of the reflective essays. Dr Brid Phillips crafted the paper with her co-author, conducted the literature search, and undertook thematic analysis of the reflective essays. All the authors have read and approved the final manuscript.
Ethical Approval
Ethics approval was granted by The University of Western Australia Human Research Ethics Committee: HREC RA/4/20/5254.
Data Availability
All relevant quantitative data are within the manuscript. The qualitative data collected for this manuscript originates from assessment items submitted as part of the participants’ academic studies. The authors do not have consent to upload this data into a data repository.
Acknowledgement
We would like to thanks the students who participated in this unit and their willingness to adapt to the online platform with grace and enthusiasm.
Funding
This work has not received any external funding.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Badenhorst, C., Moloney, C., Rosales, J., Dyer, J., & Ru, L. (2015). Beyond deficit: Graduate student research-writing pedagogies. Teaching in Higher Education, 20(1), 1-11. https://doi.org/10.1080/13562517.2014.945160
Baker, H. F., Moreland, P. J., Thompson, L. M., Clark-Youngblood, E. M., Solell-Knepler, P. R., Palmietto, N. L., & Gossett, N. A. (2019). Building empathy and professional skills in global health nursing through theatre monologues. The Journal of Nursing Education, 58(11), 653-656. https://doi.org/10.3928/01484834-20191021-07
Barber, S., & Moreno-Leguizamon, C. J. (2017). Can narrative medicine education contribute to the delivery of compassionate care? A review of the literature. Medical Humanities, 43(3), 199-203. https://doi.org/10.1136/medhum-2017-011242
Bocanegra-Valle, A. (2014). ‘English is my default academic language’: Voices from LSP scholars publishing in a multilingual journal. Journal of English for Academic Purposes, 13(1), 65-77. https://doi.org/10.1016/j.jeap.2013.10.010
Boudreau, J. D., Liben, S., & Fuks, A. (2012). A faculty development workshop in narrative-based reflective writing. Perspectives on Medical Education, 1(3), 143-154. https://doi.org/10.1007/s40037-012-0021-4
Charon, R., Hermann, N., & Devlin, M. J. (2016). Close reading and creative writing in clinical education: Teaching attention, representation, and affiliation. Academic Medicine, 91(3), 345-350. https://doi.org/10.1097/ACM.0000000000000827
Crawford, P., Brown, B., Tischler, V., & Baker, C. (2010). Health humanities: The future of medical humanities? Mental Health Review Journal, 15(3), 4-10. https://doi.org/10.5042/mhrj.2010.0654
Dean, S., & McAllister, M. (2018). How education must reawaken empathy. Journal of Advanced Nursing, 74(2), 233-234. https://doi.org/10.1111/jan.13239
Deloney, L. A., & Graham, C. J. (2003). Wit: Using drama to teach first-year medical students about empathy and compassion. Teaching and Learning in Medicine, 15(4), 247-251. https://doi.org/10.1207/S15328015TLM1504_06
Fennelly, B. A. (2020, May 15). What’s the use of reading? Literature and empathy [Video] . https://youtu.be/9nJv8sxpUKU
Frye, A. W., & Hemmer, P. A. (2012). Program evaluation models and related theories: AMEE guide no. 67. Medical Teacher, 34(5), e288-299. https://doi.org/10.3109/0142159x.2012.668637
Hyland, K. (2016). Academic publishing and the myth of linguistic injustice. Journal of Second Language Writing, 31, 58-69. https://doi.org/10.1016/j.jslw.2016.01.005
Kaptein, A., Hughes, B., Murray, M., & Smyth, J. (2018). Start making sense: Art informing health psychology. Health Psychology Open, 5(1), 205510291876004. https://doi.org/10.1177/2055102918760042
Kerr, A., Biechler, M., Kachmar, U., Palocko, B., & Shaub, T. (2020). Confessions of a reluctant caregiver palliative educational program: Using readers’ theater to teach end-of-life communication in undergraduate medical education. Health Communication, 35(2), 192-200. https://doi.org/10.1080/10410236.2018.1550471
Lai, C.-W. (2020). “Booster shots” of humanism at bedside teaching. The Asia Pacific Scholar, 5(2), 45-47. https://doi.org/10.29060/TAPS.2020-5-2/PV1085
Matharu, K. S., Howell, J., & Fitzgerald, F. (2011). Drama and empathy in medical education: Drama and empathy. Literature Compass, 8(7), 443-454. https://doi.org/10.1111/j.1741-4113.2011.00778.x
McDonald, P., Ashton, K., Barratt, R., Doyle, S., Imeson, D., Meir, A., & Risser, G. (2015). Clinical realism: A new literary genre and a potential tool for encouraging empathy in medical students. BMC Medical Education, 15(1), 112-112. https://doi.org/10.1186/s12909-015-0372-8
Nagji, A., Brett-MacLean, P., & Breault, L. (2013). Exploring the benefits of an optional theatre module on medical student well-being. Teaching and Learning in Medicine, 25(3), 201-206. https://doi.org/10.1080/10401334.2013.801774
QSR International. (2018). NVivo 12 [Software]. In https://qsrinternational.com/nvivo/nvivo-products/
Robeson, R., & King, N. (2017). Performable case studies in ethics education. Healthcare, 5(3), 57. https://doi.org/10.3390/healthcare5030057
Scott, K. M., Berlec, Š., Nash, L., Hooker, L., Dwyer, P., Macneill, P., River, J., & Ivory, K. (2017). Grace under pressure: A drama-based approach to tackling mistreatment of medical students. Medical Humanities, 43(1), 68. https://doi.org/10.1136/medhum-2016-011031
Shapiro, J., & Hunt, L. (2003). All the world’s a stage: The use of theatrical performance in medical education. Medical Education, 37(10), 922-927. https://doi.org/10.1046/j.1365-2923.2003.01634.x
Ünalan, P. C., Uzuner, A., Ifçili, S., Akman, M., Hancolu, S., & Thulesius, H. O. (2009). Using theatre in education in a traditional lecture oriented medical curriculum. BMC Medical Education, 9(1), 73-73. https://doi.org/10.1186/1472-6920-9-73
Wilson, J. (2020). Extinctions. UWA Publishing.
Wilson, K. (2016). Critical reading, critical thinking: Delicate scaffolding in english for academic purposes (EAP). Thinking Skills and Creativity, 22, 256-265. https://doi.org/10.1016/j.tsc.2016.10.002
Zhao, J. (2017). Native speaker advantage in academic writing? Conjunctive realizations in EAP writing by four groups of writers. Ampersand, 4, 47-57. https://doi.org/10.1016/j.amper.2017.07.001
*Kirsty J Freeman
Duke-NUS Medical School
8 College Road, Singapore 169857
Tel:+65 89219676
Email: kirsty.freeman@duke-nus.edu.sg
Submitted: 15 October 2020
Accepted: 17 February 2021
Published online: 13 July, TAPS 2021, 6(3), 5-9
https://doi.org/10.29060/TAPS.2021-6-3/GP2430
Wei-Han Hong1a, Vinod Pallath1b, Chan Choong Foong1, Christina Phoay Lay Tan2, Mary Joseph Marret3, Yang Faridah Abdul Aziz4 & Jamuna Vadivelu1
1Medical Education Research and Education Unit, Faculty of Medicine, Universiti Malaya, Malaysia; 2Department of Primary Care Medicine, Faculty of Medicine, Universiti Malaya, Malaysia; 3Department of Paediatrics, Faculty of Medicine, Universiti Malaya, Malaysia; 4Department of Biomedical Imaging, Faculty of Medicine, Universiti Malaya, Malaysia
a,bJoint first author
Abstract
Introduction: The article is a succinct summary of events and process for emergency digitisation and transition to remote teaching during the COVID- 19 pandemic. The challenges of such transition included the need for enhanced infrastructure facilities, compliance to directives from regulatory bodies, providing an equivalent learning experience in the virtual learning environment (VLE) and ensuring the end user capacity to utilise the VLE created.
Methods: To accomplish this task a suitable instructional design and transition model was utilised to create an integrated Moodle and Microsoft Teams platform as the VLE. The curriculum was recreated in the VLE through review of existing infrastructure and resources, deconstructing the demands of the curriculum, reconstructing the learning experiences of curriculum in VLE and innovating to improve. The end user training was also provided using the same VLE created, which ensured capacity building. Virtual Clinical Assessments (VCA) were created to ensure the completion of assessment tasks.
Results: The utilisation of the ACTIONS transition model resulted in the evolution of instructional delivery from a Web Enhanced approach to a customised Web Centric approach and implementation of Virtual Clinical Assessments. Students expressed their satisfaction in the learning experience through VLE, but were anxious about their clinical training and connectivity issues.
Conclusion: This transition demonstrated the need of future directions in terms of learner readiness to be more self-directed and self-determined, design thinking for transformation to a Web Centric curriculum, faculty readiness to change and develop the competency of Technological Pedagogical Content Knowledge (TPACK).
Practice Highlights
- ACTIONS model is an appropriate design and transition model.
- Exigent transition is an opportunity to augment the capabilities of VLE and innovate.
- Ensure the recreation of an equivalent virtual learning experience to the onsite learning experience
- TPACK has emerged as an essential trainer competency.
I. INTRODUCTION
The COVID-19 pandemic has been a catalyst for extraordinary transformation in medical education. Malaysia underwent a form of lockdown under the Movement Control Order (MCO). The MCO was initiated on 18th March 2020 for two weeks and extended several times until 9th June 2020, with changing levels of restrictions in phases. With the designation of their usual clinical learning environment as a COVID Hospital, it was inevitable that medical students at the Universiti Malaya experienced major disruptions in clinical teaching.
The exodus of all students to their hometowns at the start of the MCO necessitated overnight conversion of teaching and learning processes into online delivery. With the emergence of the initial four weeks of the MCO as a fluid, unpredictable and undefined landscape, the medical faculty formulated a range of teaching and learning modalities adaptable to different conditions.
These adaptations were made while maintaining compliance with requirements of various regulatory bodies and policy makers, including the Ministry of Higher Education, Malaysian Medical Council, the Malaysian Qualifying Agency and university governance. This process of assimilation within a rapidly evolving milieu was a formidable challenge. This article aims to provide a succinct summary of events and processes for emergency digitisation and transition to remote teaching during the COVID-19 pandemic. This summary will function as a model for transformation on the run to manage the implementation and delivery of higher education programme during a major crisis or disaster.
II. METHODS
As events preceding the implementation of the MCO unfolded, sequential meetings were held to brainstorm on the safety, mode of delivery in emergency transition, preparation for training of students and staff, and evaluation of the changes. The faculty of medicine seized the opportunity to plan and implement a comprehensive online learning experience during the MCO period. Designated teams explored the various technologies available to support learning and shared best practices in an explosion of webinars. It became evident that dedicated teamwork to deal with sudden and enforced changes was crucial for this transition to be effective.
A. Theoretical Framework to Support the Digital Transition
An exigent digital transition like this required an instructional design model to affect a transition that was sustainable and future-ready. There was also a need to ensure that learning objectives envisaged for a physical face-to-face curriculum delivery model could be achieved with digital transition. The most practical model for such a transition was the ACTIONS model by Tony Bates (as cited in Boettcher & Conrad, 1999). ACTIONS is an acronym for Access, Costs, Teaching and learning, Interaction and user friendliness, Organisational issues, Operational and implementation expenses, Novelty and Speed.
B. The Development Approach – Review, Deconstruct, Reconstruct and Innovate
Recreating the entire learning experience in the VLE required the following steps
1) Review of existing e-resources and mapping them to curriculum: The existing e-resources available at Faculty of Medicine and Library were reviewed to analyse the need for additional resources. Contents of the e- resources were also mapped to the curriculum to understand the alignment of available resources with topics covered in different stages.
2) Deconstruct the existing curriculum and detailing its demands: The Universiti Malaya Medical Programme (UMMP) comprises five stages. Stages 1 and 2 (years 1 and 2) provide the preclinical and Stages 3. 1, 3.2 and 3.3 (years 3 to 5) provide the clinical learning experiences to students. The unique instructional demands of each stage were carefully analysed to clarify the possibilities and limitations of the VLE created. This step enabled categorisation of learning experiences which were suitable for delivery in the VLE and learning experiences which were not suited to a VLE with regard to the achievement of learning outcomes.
3) Reconstruct the learning experiences of curriculum in VLE: While contents of the curriculum were already available on a university learning management system (LMS) called Student Powered e- Collaborative Transforming UM (SPeCTRUM), the Moodle-based segment of the VLE, learning spaces had to be created within the Microsoft Teams segment to enable synchronous collaboration. The design principle adopted was to replicate physical facilities of Faculty of Medicine as closely as possible by providing virtual large and small group learning spaces (virtual classrooms) within Microsoft Teams. Each stage was denoted as a team. Designated channels were then created within each team for system-based blocks in preclinical stages and specialty-based postings in clinical stages. Small group teaching activity spaces including PBL rooms were created as separate channels within respective teams.
4) Innovate and improve: Although it was an exigent digital transition, the opportunity to innovate and improve could not be missed. Through deep linking of Moodle-based SPeCTRUM and Microsoft Teams, a seamless login and navigation experience was created. The learning spaces created in Microsoft Teams were provided with direct access to e-resources in the forms of ‘tabs’, simulating the existence of resource libraries within the learning spaces. OneNote was made available in these tabs as potential ‘white boards’. A complete transition to ‘flipped classes’ was also adopted by the faculty, replacing the traditional lectures.
C. Ensuring the Effective Utilisation of the VLE and Digital Instructional Delivery – The End User Training
Effective digital transition was enabled through utilisation of the VLE itself as the learning space for training of end-users. Detailed user guides were prepared. A series of synchronous hands-on sessions were also provided. All training sessions were recorded and accessible in the VLE for future reference. Continuous one-to-one support was provided on request for end-users. This dynamic transition support became an opportunity for upskilling faculty members and administrators.
D. Evaluation of Learning Experiences of the Students
A 13-item questionnaire was developed to examine learning experiences of students. The development considered existing institutional expectations of teaching, standards for problem-based learning and online learning, and generic criteria for learning environments. In addition, two open-ended questions were created for students to express what they liked and what did not work well. One week after commencement of the VLE, students were invited to relate their learning experiences via this questionnaire. This early feedback from the perspective of end-users was vital to identify aspects of the newly-constructed VLE which required adjustments.
III. RESULTS
A. The Challenge Made into an Opportunity – The Digital Transition
The school faced a huge hurdle as these sudden changes required augmented capabilities, stretching the existing connectivity infrastructure to its limits. As Information Technology (IT) professionals addressed the obvious task of ensuring good connectivity for all faculty members, administrators and students, others worked to transform mindsets of the eager and less-willing to adapt to the new norm of providing emergency online teaching to the students.
Universiti Malaya had an existing web-enhanced blended learning approach which utilised SPeCTRUM to support e-learning. The pandemic compelled transition from a Web-Enhanced approach with a physical classroom as the primary site of instruction to a web-centric approach with a virtual online platform as the primary site of instruction. To effect this change, capabilities of the existing LMS were enhanced to provide experiences of asynchronous and synchronous communication together with collaboration possibilities in a robust Virtual Learning Environment (VLE).
The ACTIONS model facilitated the evaluation of issues including uniform access to the selected web-based tools, adaptability of existing teaching learning methods to the VLE, organisational constraints and support needed for implementation, reliability and future-readiness of the VLE platform as well as the speed or ease with which the curriculum could be fully transitioned to a Web-Centric mode. Such planning resulted in the decision of deep linking and combining the capabilities of Moodle-based SPeCTRUM and Microsoft Teams as a VLE solution for the instantaneous digital transition.
B. Transition in Assessments
Assessment activities also had to be aligned with teaching and learning, taking into account guidelines of various regulatory bodies. During the MCO, existing written assessment components, which were in the form of single best answer (SBA) and extended matching type questions, were administered using online software in the SBA format.
Clinical end-of-rotations examinations posed a greater challenge. During the MCO, it was not possible to conduct examinations in the clinical environment with actual patients or a simulated clinical environment where both examiners and students could have face-to-face interaction with standardised patients. We therefore created Virtual Clinical Assessments (VCAs), writing clinical scenarios which could be used in a format similar to a structured oral examination online. Each VCA lasted 30 minutes with components of history-taking, physical examination, differential diagnoses, investigations and management along the lines of an “observed long case” clinical examination. Examiners or standardised patients were trained to role play for history-taking. De-identified clinical photographs were used for the physical examination component. Investigations such as biomedical images and laboratory results provided data for interpretation. An existing final-year examiner clinical assessment mark sheet with reference rubric was adapted for use, with components of history-taking, examination, clinical reasoning, management, knowledge, communication skills and professionalism. Specific trigger questions to assess these components were incorporated into each scenario. This assessment format could be utilised on a totally virtual platform or in a partially virtual assessment, combining face-to-face interaction with simulated patients/caregivers and clinical photographs or videos, complying with prevailing restrictions at different phases of the MCO.
C. Students’ Experiences of the Virtual Learning Environment
Students recognised and appreciated the Faculty’s efforts in establishing the online learning system for them to continue their studies. Students reported several aspects that worked well. These included pre-recorded teaching materials which allowed students to learn at their own pace. Students were also able to obtain adequate information and understood the information delivered during the virtual problem-based learning sessions. They were also less inhibited to ask questions from behind the screen during synchronous sessions.
However, there were also some areas of concern. Some students encountered internet stability issues. They needed time to adapt to the online learning platform, such as learning how to avoid speaking at the same time during the problem-based learning sessions. While acknowledging the usefulness of videos for some clinical exposure, they yearned to return to hands-on practice of clinical skills and receive feedback on their performance.
D. Prioritising Safety
With the relaxation of MCO restrictions in June to a “recovery MCO” when final year medical students were allowed back, guidelines and protocols were established to ensure safety of students, staff as well as patients. Students returned in batches and were provided with instructions to self-assess their risks before travelling. Subsequent orientation was given to perform risk assessments whenever they checked into their hostel, other buildings within the university campus, and into the hospital. The Occupational Safety, Health and Environment (OSHE) and hospital infection control teams developed a software application for the purpose of tracking the entry of patients, students and staff into the hospital premises. Students were placed on a staggered schedule within their clinical rotation to avoid overcrowding of wards and clinics. Students and staff were constantly reminded to adhere to social distancing and safety guidelines from the Ministry of Health.
IV. CONCLUSION- FUTURE DIRECTIONS
The COVID-19 pandemic has enhanced the use of technology-enhanced learning and instructional delivery as a medium for education. To adapt to this paradigm shift and ensure future readiness, the following areas require immediate attention:
A. Student Readiness
Ensuring readiness of learners to become self-directed and self-determined as they move from higher secondary/ high school to University education. Students should also be supported to develop effective online learning approaches.
B. Academic Faculty Readiness and TPACK as a competency
Academic faculty readiness to facilitate learning among the generation Z learners needs to be ensured. This essentially means that faculty members need to develop Technological Pedagogical Content Knowledge (TPACK, Figure 1) (Koehler & Mishra, 2009), as an essential competency to be effective in technology integration to facilitate learning. TPACK essentially represents the fundamental understanding of faculty members on effectively facilitating the learning process using technology, using appropriate pedagogical approaches to meet the instructional demands of each discipline/ specialty. The importance of up-skilling and re-skilling academic faculty members to equip them with latest tools available for teaching and learning is getting emphasised here.
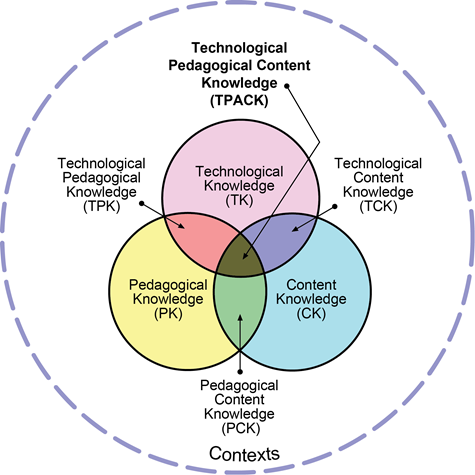
Figure 1: Technological Pedagogical Content Knowledge (TPACK). Reproduced by permission of the publisher (Koehler, 2011)
C. Infrastructure Development
Infrastructure planning, development and resource allocation to meet the future needs of technology-enhanced learning becomes a necessity to ensure the implementation of curriculum.
Notes on Contributors
Dr. Wei Han Hong involved in development of the concept, contributed to the creation of VLE through the inputs of curriculum requirements and ensured implementation, participated in the trials and troubleshooting of VLE, coordinated and contributed to the manuscript writing and approved the final version.
Associate Professor Dr. Vinod Pallath involved in conceptualising and development of the VLE, coordinated the development of VLE and lead the training of the faculty members through the VLE, contributed to manuscript writing and performed critical revisions to make the final version and approved the final version.
Dr. Chan Choong Foong involved in development of the concept, ensured the integration of quality requirements in the VLE, participated in the trials and troubleshooting of VLE, contributed to the manuscript and approved the final version.
Professor Dr. Christina Tan Phoay Lay involved in development of the concept, coordinated and contributed to development of assessments in the VLE, participated in the training, contributed to the manuscript and approved the final version.
Professor Dr. Mary Joseph Marret involved in development of the concept, coordinated and contributed to development of assessments in the VLE, participated in the training, contributed to the manuscript and approved the final version.
Professor Dr. Yang Faridah binti Abdul Aziz involved in development of the concept, supported the development of VLE in the capacity of Deputy Dean (undergraduate), ensured the demands of the curriculum are met through the VLE, contributed and critically reviewed the manuscript and approved the final version.
Professor Dr. Jamuna Vadivelu involved in development of the concept, supported the development of VLE in the capacity of Head of Unit, ensured the demands of the curriculum are met through the VLE, contributed and critically reviewed the manuscript and approved the final version.
Acknowledgement
Authors acknowledge the technical contributions and administrative support received from Medical Education and Research Development Unit and Dean’s Office, Faculty of Medicine, Universiti Malaya.
Funding Statement
There was no funding for the process described in the manuscript.
Declaration of Interest
The authors declare that there is no conflict of interest related to this manuscript.
References
Boettcher, J. V., & Conrad, R. M. (1999). Faculty guide for moving teaching and learning to the web. League for Innovation in the Community College.
Koehler, M. (2011, May 11). Using the TPACK image. TPACK.ORG. http://matt-koehler.com/tpack2/using-the-tpack-image/
Koehler, M., & Mishra, P. (2009). What is technological pedagogical content knowledge (TPACK)? Contemporary Issues in Technology and Teacher Education, 9(1), 60-70. https://doi.org/10.1177/002205741319300303
*Jamuna Vadivelu
Medical Education and Research Development Unit,
Faculty of Medicine,
University of Malaya,
50603 Kuala Lumpur, Malaysia.
Email: jamuna@ummc.edu.my
Published online: 13 July May, TAPS 2021, 6(3), 1-4
https://doi.org/10.29060/TAPS.2021-6-3/EV6N3
Lambert Schuwirth1 & Ardi Findyartini2
1Prideaux Centre for Research in Health Professions Education, College of Medicine and Public Health, Flinders University, Australia; 2Department of Medical Education, Faculty of Medicine, Universitas Indonesia, Indonesia
This quote is attributed to Nicolo Machiavelli, an Italian Renaissance political philosopher. And it may sound reasonable, but at a time where the Covid-19 pandemic is still very active around the world it is also callous to think of a crisis as an opportunity. We want to acknowledge this and we want to send our deepest sympathy to all those who have been personally affected by this pandemic.
Nevertheless, it is also fair to say that in many places in the world the pandemic has served as a catalyst for changes in a variety of human domains–not in the least in health professions education. When we say catalyst, we use the word very purposefully, because there are many developments that were already taking place prior to 2020 and which have already produced quite disruptive changes in society. This crisis is a catalyst, therefore, in the sense that it has heightened the awareness that such fundamental changes will be very soon have an impact on the way we educate future health professionals.
We could easily fill 20 thematic issues with examples of how medical schools around the world have rapidly adapted their educational processes to allow them to continue whilst complying with Covid-19 related restrictions. These changes were necessary and often quite successful. However, it also has to be stated that they were often merely the proverbial Plan B rather than really fundamental innovations. And while Plan B is a good solution for the short term it also has to be a steppingstone for more fundamental innovations. In other words, our attention should not only focus on ‘what where the changes and how were they made, but also ‘why did the changes take place and in what ways can they improve education’.
So, let us quickly reflect on what are these changes that are taking place in the world around us and conjecture about what they could mean for health professions education. Not surprisingly, many of these changes have to do with the rapid development in information and communication technology. These have opened up completely new ways of dealing with the important aspects of society and those in health professions education.
The first example concerns the way we conceptualise knowledge. This is quite different to what it was 50 years ago. Fifty years ago, knowledge was typically seen as the possession of the experts, and out of altruism or for a tuition fee, the expert was willing to share their knowledge with the learner. The typical business equivalent of this was the traditional encyclopaedia. In an encyclopaedia the knowledge of the group of experts is laid down and sold to clients. Nowadays, in contrast, knowledge/information is seen as something that can or even must be constructed collaboratively, by a community of people each adding small pieces to the whole ‘puzzle’. Such a re-conceptualisation has found its crystallisation in wikis, with Wikipedia as the most well-known example. There was a time when businesses tried to put the traditional encyclopaedia on a CD-ROM and made it more feasible to use. However, an encyclopaedia on a CD-ROM is just still a traditional encyclopaedia, just a technical delivery differs. Needless to state that this wasn’t a profitable business development; it wasn’t a real innovation but rather a sort of Plan B. It is therefore, plausible to assume that online lectures are a similar form of Plan B in health professions education.
Another important development concerns the way we manage trust. From a society that has institutionalised trust we are gradually moving into a society that relies on distributed trust (Botsman, 2017). In an institutionalised trust society, important transactions and the trust in those transactions are managed by a trusted institution. For example, we transfer large sums of money preferably via a bank, we negotiate house sales through a conveyancer, and so on. Many of these still exist, but increasingly trust is distributed. Previously, if you wanted to go out for fine dining and spend a lot of money on a fancy restaurant, you could consult the Michelin guide. In fact, this means that you ‘outsourced’ your trust in finding a good quality restaurant to a trusted organisation. Most people no longer used this guide; they just go online and read the long list of customer reviews and evaluate the way the restaurant has dealt with the reviews. This is an example of distributed trust, as a community with direct experience we collectively construct ‘quality’. Our universities still operate as trusted institutions, they provide the transaction–education–and the trust and transaction–academic degrees–in one. Of course, recognition of prior learning are early steps to disconnect the educational transaction from the management of trust, but there is still a long way to go.
For instance, in order to organise recognition of prior learning and the disentanglement of trust and transaction effectively, there is a need of a trusted dossier/portfolio that can be managed across educational phases and by different stakeholders in a fully authenticated way. Open ledger or block chain technology is very likely able to provide such systems, although much may still be under development (Mikroyannidis et al., 2018, June). It is not a huge leap of faith to imagine what this would mean for future employers. Instead of having to trust an academic transcript with only a few numbers or grades and with seals and signatures, an employer would have the opportunity to ‘interrogate’ an applicant’s whole dossier of learning, improvement and achievements. Such developments are likely to also severely disrupt the way accreditation works and probably influence how learners engage in more meaningful way to achieve competence in health professions education.
For the learner this means that they would easily be able to fill such a portfolio with a combination of course material, micro credentialing and elements obtained from the cognitive surplus (Shirky, 2010). ‘Cognitive surplus’ refers to the fact that, increasingly, knowledge is provided or shared for free in the Internet. The probably most well-known example of this is the Khan Academy (Khan Academy, n.d.). Tuition and learning that were previously only available to feepaying students, is now available for free. Of course, not all that is offered in the cognitive surplus is of high quality and there is a challenge for learners to distinguish between offerings of poor and of good quality, but it does mean that most modern learners are increasingly used and expecting to be able to access knowledge for free or for a negligible fee. This will place an increasing burden on universities to demonstrate their added value to a feepaying student’s learning, including in instilling students’ ability to critically think and reflect on the abundant information they can access freely. One could argue that the higher education industry is still highly regulated in most countries and the only way to achieve a credible degree in the health professions is by going through a university. Such industry which has to rely purely on a regulatory framework is vulnerable.
Finally, the development that most people are talking about are artificial intelligence and machine learning. It is very difficult to predict what the future will hold, but it is likely that artificial intelligence and machine learning will significantly augment or even substitute what currently is most doctors’ specific expertise; making a diagnosis and deciding on therapeutic management plans. The former is generally a categorisation task, something at which artificial intelligence is becoming better and better. The latter is becoming ever more patient specific, especially with the emergence of precision medicine, which will increasingly require decision support systems. This does not automatically mean that patients will not be needing somebody to care for them, to partner with them or to help them make meaning in periods of illness, angst and uncertainty. Obviously, this will require health professionals with more elaborate so-called ‘soft’ skills which enable them to develop empathetic and professional connections with their patients either for better cure or care.
Such changes to what makes a ‘good’ doctor will require changes to health professions education. On the one hand, education should equip students with data and technology literacies, but on the other, it should allocate sufficient resources for the development of human literacy (Aoun, 2017). Development of soft skills means the training of doctors who can partner with their patients, who can nurture them and help them make meaning. It also requires students who eventually will be able to embrace uncertainty and who will be equally comfortable with ‘knowing’ and with ‘not knowing’; which further highlights the importance of creativity and innovations, self-awareness, and lifelong learning skills.
Obviously, there are implications for health professions education. Firstly, a purely transactional process of passing on knowledge may not need to take a central role in a curriculum. The traditional lecture was an educational ‘technology’ that was designed to cater to students who did not have access to books. The lecturer, the reader, read the knowledge to the students who either were able to write it down or had to memorise it. The purely transactional process of passing on knowledge should no longer have a central role in the learning process, and it has implications for assessment as well. The assessment arm of it is the typical structured and standardised knowledge test in which the candidates reproduce the knowledge that they’ve been provided with. This no longer seems current nor relevant one of which because of a lot of changes and uncertainties this pandemic has taught us. Modern students, through their laptops, tablets or smart phones, have accesses to a whole world of information. This is quite recent because even in the early days of problem-based learning, the university had control over the quality of the resources students could use for their learning. Nowadays, there is a whole Internet of information–some relevant and some absolutely incorrect nonsense–that is absolutely not under the control of the University. It is under the control of the students, though, and they will use that information. In order to manage this huge affordance educationally, changes will have to be made to develop curricula that incorporate both the formal and informal educational spaces. To successfully combine those spaces, curricula may have to give more room to students and teachers to develop a dialogue in such a positive relationship that it better facilitates students’ critical thinking and professional identity formation.
Such changes cannot happen in an educational context in which the students are not allowed or supported to exhibit agency over their own learning, and as a consequence, over their own assessment. But changing this organisational mindset culture is probably the biggest challenge ahead of us. It requires a culture shift from distrust and control to one of trust and empowerment. Thinking about trust and empowerment is not idealism but we think it is pure necessity. The dramatic events in the world of online proctoring are a clear demonstration that the choice to go further down the pathway of distrust and control has not been the best use of what technology affords.
Furthermore, trust and empowerment are not only needed during training but also after graduation. Where in our time as students it could still be reasonably expected that upon graduation we were equipped with all the knowledge, skills, problem-solving ability and attitudes to last us for the rest of our career–bar some updating through Continuing Medical Education (CME)–it is now clear that the world, the healthcare environment and the expectations of patients are changing rapidly. No longer can we assume that upon graduation our students will be a complete ‘product’. Instead, they will have to continue to learn, to develop and probably to reinvent themselves continually. But if we as universities have never empowered them or allowed them to take agency over their own learning and assessment, it is implausible that our graduates would suddenly and magically be capable to do this after graduation. The implication for assessment is obvious. The notion of single moment assessments of final examinations is not in alignment with these views. Assessment will have to take on a more longitudinal and integrated form to be aligned with more than educational processes and the lifelong learning requirements.
A final point relates to the so-called affordances modern students have (Friedman & Friedman, 2008). There are several listed in the literature, but some are most pertinent in the short run. Through their laptops, tablets or smart phones, students are able to be in multiple communities and entertain multiple communications at the same time. They can be in a practical session working with one group of peers, but also texting to other members of the student cohort or more general friends about what they currently learning or even about completely unrelated issues. There are numerous examples of Information and Communications Technology (ICT) afforded learners–or academics for that matter–who entertain to communications with two communities at the same time. Everyone who has been in an online meeting and has used the chat function at the same time, has had experience with this. Of course, this rapid switching between communities and communications, this time slicing, comes at the expense of cognitive load, but it can also be used in a very enriching way for learning. The same applies to collaborations. Any student who is a tutorial group or even in a lecture hall and accesses the cognitive surplus or Wikipedia is in fact in two knowledge creation collaboratives at the same time.
Unfortunately, our students are not yet very well experienced in how to use these affordances well, but also most educational designers or curriculum developers are not able to incorporate them and take maximum advantage of what they enable the learner to do.
The challenge that lies ahead of us is to bring these developments to health professions education. One ramification is already inevitable, ICT in most contexts has dramatically reduced power asymmetries. In the example of the restaurant and the reviews, any customer now has the power to publicise their experience and restaurant owner would be wise to respond appropriately, in healthcare patients come to the consulting room prepared with Dr Google and whether what they found is relevant or not, they do have knowledge that the doctor will have to deal with, and finally in education students have point of care access to a whole world of information which will make them more equal partners in their education. Students who are well prepared for lectures are able to disagree with their lecturers or even be better informed on details than the lecturer. Universities may need to increase efforts to better engage students and to facilitate their personalised learning needs, as well as to enable more co-creation in knowledge development. Universities that do not acknowledge these changes run the risk of quickly becoming obsolete. But acknowledging this also means better preparation of teachers through more comprehensive faculty development programmes.
However, this editorial is not about doom and gloom or risks, it is about opportunities. All the affordances that are already or could be incorporated in modern health professions education make it possible to educate even better health professionals for the future, who are agile and optimally positioned to an ever-changing healthcare system and align better with their patients. The potential and opportunities are vast. Whether or not these disruptive changes give us those opportunities, will depend both on how we adapt for the short-term needs and how we prepare to embrace substantial and necessary changes in our health professions education for the future.
Lambert Schuwirth & Ardi Findyartini
Guest Editors &
International Editorial Board Members
The Asia Pacific Scholar (TAPS)
Botsman, R. (2017). Who can you trust?: How technology brought us together and why it might drive us apart. Hachette.
Mikroyannidis, A., Domingue, J., Bachler, M., & Quick, K. (2018, June 25-29). A learner-centred approach for lifelong learning powered by the blockchain. EdMedia+ Innovate Learning, Amsterdam, Netherlands.
Shirky, C. (2010). Cognitive surplus: Creativity and generosity in a connected age. Penguin Books.
Khan Academy. (n.d.). https://en.khanacademy.org/
Aoun, J. E. (2017). Robot-proof: Higher education in the age of artificial intelligence. The MIT Press.
Friedman, L. W. & Friedman, H. H. (2008). The new media technologies: Overview and research framework. Social Science Research Network. http://dx.doi.org/10.2139/ssrn.1116771
Submitted: 17 May 2020
Accepted: 2 September 2020
Published online: 4 May, TAPS 2021, 6(2), 91-93
https://doi.org/10.29060/TAPS.2021-6-2/CS2263
K. Anbarasi1 & Kasim Mohamed2
1Department of Dental Education, Sri Ramachandra Institute of Higher Education and Research, Chennai, India; 2Department of Maxillofacial Prosthodontics, Sri Ramachandra Institute of Higher Education and Research, Chennai, India
I. INTRODUCTION
Dental practitioners often encounter situations that require customising the prosthesis to satisfy the needs of patients. Artificial devices called dental appliances or prosthesis is custom fabricated for the functional, aesthetic, and psychological wellbeing of patients (Chu et al. 2013). The patient’s complaints may vary from missing natural teeth to extensive maxillofacial defects, and there is no single best rehabilitative therapy for these conditions. Designing our product is the choice, and this demands adaptive expertise, i.e., the ability to generate potential solutions (Mylopoulos et al. 2018). Maxillofacial Prosthodontics applies a variety of learning methods like systematic simulation laboratory exercises, See One, Do One, Teach One (SODOTO method), and supervised clinical practice to train the routine technical skills and clinical practice. To maximise the outcomes in the complex prosthetic treatment, the course specialists designed an “Interdisciplinary Device Development program (IDDP)”—a value-added course for the postgraduates in collaboration with the Biomedical Instrumentation Engineering Faculty of our Institution. IDDP is the first of its kind challenge-based learning model in Dentistry that uses innovations to deal with rehabilitation care beyond routine practice. This paper aims to present our IDDP model and programme outcomes.
II. METHODS
IDDP is structured in three stages referring to problem determination, design, and development. An abstract idea about the essential requirements and intellectual property protection is also included and is scheduled for 3 hours per week for 10 weeks’ (Table 1). The IDDP concept and curriculum were presented in the College Council meeting and subsequently in the Board of Studies and Academic Council. The proposal was approved and permitted implementation.
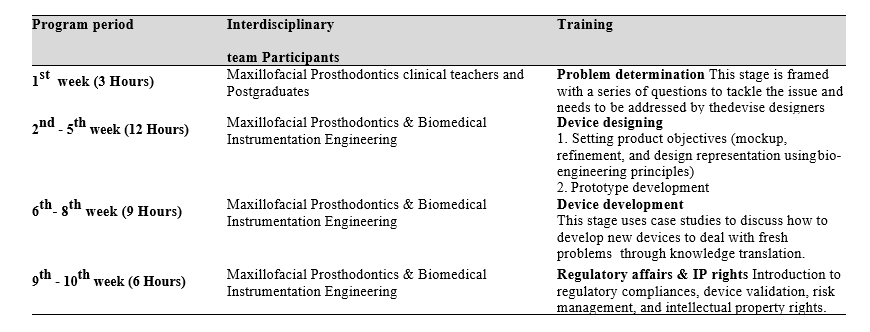
Table 1: IDDP curriculum framework
Participation in IDDP is mandatory for all postgraduates (PGs) of Maxillofacial Prosthodontics, but knowledge translation into practice is expected only when patients present with unique/challenging conditions. Chances of treating these patients are given for all PGs, but priority is given to those who showed valuable accomplishments in their regular clinical works. Once get allotted with such cases, the PG needs to work with their faculty in-charge, the primary consultant, a faculty member from biomedical engineering, and laboratory technicians.
The device designing demands advanced prosthodontic techniques and the attainment of competency depends on repeated practice. Skill assessment before accustoming it is not a safe practice hence the IDDP is not emphasising on assessments that reflect on summative grade, but performance assessment was made for the postgraduates who have undertaken the task to appraise their diligence, completeness, and problem-solving ability in a standard template, and supporting them to improve their learning.
III. INVENTIONS IN THE CLINICAL GROUNDS
A. Cheek Bumper
A Von Recklinghausen’s disease patient reported with a nodule on the left buccal mucosa and chewing difficulty. The patient expected non-surgical management, and there was a need for invention. Relieving the contact between the mucosal nodule and teeth was suggested as a solution and one PG student turned out the novel idea as an acrylic cheek bumper, an intraoral device that separated the growth 5mm away from the teeth surface. Wearing this appliance at mealtime solved the patient’s problem.
B. Training Pad for Jaw Reposition
A patient has undergone hemimandibulectomy on the right side. After a month, he reported aesthetic concern because of the deviation of the lower third of the face during jaw movements. Denture rehabilitation with a flange is a routine treatment to improve aesthetics. In our discussion, a PG student proposed to reposition the jaws before denture treatment to achieve the jaw compatibility for receiving the denture, hence optimising the success. The team accepted to transform the vision into reality. A prototype was prepared, and an intraoral acrylic pad with retainers was developed. Later the patient was treated with a prosthesis and he expressed his happiness in gaining back the chewing efficiency and confidence
C. Modified Impression Tray to Make Ear Prosthesis
To avoid the shape distortion and to get the adequate fine details in the replica, a postgraduate student in the existing tray pattern did a design modification and got an excellent result.
D. Compression Stent
A patient was referred for the management of a hypertrophic scar following ear piercing. The literature search revealed a solution of stent fabrication to cover the affected ear completely and wearing it full time for a year. The drawbacks like patient discomfort and long-time follow-up were highlighted and a PG student suggested redesigning the compression sent to cover only the scar region using claw type hair clip model. The patient was instructed to wear the stent for 10 to 12 hours per day. At the end of the fifth month, the scar was completely disappeared and she regained the ear lobe shape.
The devices in the process include:
- Mouth opening assisting device to treat trismus.
- Impression tray with size adjustable screws.
- Custom designed intraoral radio-productive device for patients receiving radiotherapy.
IV. STRENGTHS AND LIMITATIONS
A supportive curriculum always opens an avenue for innovation. Integration of Biomedical engineering solved the clinical problem by applying engineering principles, formulas, and materials in device designing as the dental specialty lacks the potential to practice the engineering domain. IDDP inspired our postgraduates to take part actively in treatment planning sessions. There is a positive shift in their clinical reasoning skill, describing the treatment options with their pros and cons, and finally specifying the target device by solving the limitations on the existing model or developing an alternative model.
The unresolved factors of IDDP include the struggle to tap the inventive potential of graduate students, their level of commitment, and time allocation. Formal assessment, patient satisfaction survey, student perception, and feedback should be considered.
V. MOVING FORWARD
Incorporating IDDP in the dental curriculum at the national level is the way forward.
VI. CONCLUSION
Our experience in IDDP evidences the innovation that happened on academic grounds. The structured training and opportunity to transform the learning into practice enhanced the confidence level of the clinicians to think out of the box, act as problem solvers, and shape the future health care industry.
Notes on Contributors
Dr. K. Anbarasi, MDS, PhD, devised the presented concept, framed the theoretical framework, wrote the manuscript, and agreed on its final form for submission.
Dr. Kasim Mohamed, MDS, involved in curriculum planning, conducted the programme, contributed to the final version of the manuscript, and agreed to its final form for submission.
Acknowledgment
The authors like to acknowledge the programme coordinators of IDDP.
Funding
The program was supported by the authors’ institution as an academic event.
Declaration of Interest
The authors have no conflict of interest.
References
Chu, K. Y., Yang, N. P., Chou, P., Chi, L. Y., & Chiu, H. J. (2013). Dental prosthetic treatment needs of inpatients with schizophrenia in Taiwan: A cross-sectional study. BMC Oral Health, 13(1), 8. https://doi.org/10.1186/1471-2458-10-482
Mylopoulos, M., Kulasegaram, K., & Woods, N. N. (2018). Developing the experts we need: Fostering adaptive expertise through education. Journal of Evaluation in Clinical Practice, 24(3), 674-677. https://doi.org/10.1111/medu.12893
*K. Anbarasi
Faculty of Dental Sciences,
Sri Ramachandra Institute of
Higher Education and Research,
Chennai, India.
Email: anbarasi815@gmail.com
Submitted:5 September 2020
Accepted: 11 January 2021
Published online: 4 May, TAPS 2021, 6(2), 94-96
https://doi.org/10.29060/TAPS.2021-6-2/CS2449
Y.G. Shamalee Wasana Jayarathne1,2, Riitta Partanen2 & Jules Bennet2
1Medical Education Unit, Faculty of Medicine and Allied Sciences, Rajarata University of Sri Lanka, Sri Lanka; 2Rural Clinical School, Faculty of Medicine, University of Queensland, Australia
I. INTRODUCTION
The mal-distributed Australian medical workforce continues to result in rural medical workforce shortages. In an attempt to increase rural medical workforce, the Australian Government has invested in the Rural Health Multidisciplinary Training (RHMT) program, involving 21 medical schools (RHMT program, 2020). This funding requires participating universities to ensure at least 25% of domestic students attend a year-long rural placement during their clinical years and 50% of domestic students experience a short-term rural clinical placement for at least four weeks.
Multiple factors influence selecting a rural medical career pathway. Four basic truths presented by Talley (1990) USA on successful medical career pathways are still pertinent today.
1. Students from rural origin are more likely to return to rural areas of practice.
2. Medical graduates who trained in rural areas are more likely to choose rural practice.
3. General practice is the key discipline of rural health care.
4. Doctors practice close to where they train.
The evidence shows the longer a student spends training in rural area, the more likely they are to work in a rural
area (Kwan et al., 2017; Talley, 1990). Repeated exposure of rural clinical practice promotes rural living and practice, enabling the development of professional and social networks within rural communities (Eley et al., 2008). However, there is a dearth of empirical data on whether brief rural clinical learning experiences increases medical students’ rural medical career intent.
We report a case study on the pilot project of Objective Simulated Bush Engagement Experience (OSBEE), a novel approach to promote rural medical careers to medical students, where second year (of a four year program) medical students participated in a series of rurally themed scenarios and skills stations set in a rural location, with near peer supervisors (The term bush in OSBEE refers to the forested setting where the stations were undertaken).
II. OBJECTIVE AND METHODS
The objective was to evaluate the introduction of a one day immersive rural clinical learning experience in the form of the OSBEE. Metropolitan-based students travelled 280km to attend OSBEE, set in a forested area on a large farm. The students rotated through a series of simulated rural emergency scenarios and skills stations with predominantly third and fourth year medical students as supervisors.
The participants of the study were second year medical students of The University of Queensland (UQ). These students would all be attending a UQ Rural Clinical School (UQRCS) for their third year. To evaluate the influence of this program on their rural medical career intent, on peer-assisted learning and the program itself, a mixed study using a focus group and questionnaire. A focus group discussion conducted by the principal investigator, where informed written consent was obtained from all participants, was audio recorded, verbatim transcribed and thematically analysed. All correspondence was anonymous, and confidentiality maintained. The online questionnaire was administered two weeks after the OSBEE. Frequencies were calculated for questionnaire items. Themes were identified for open ended questions.
III. RESULTS
Identified key themes and quotes from the focus group and open-ended questionnaire questions are presented in Table 1.
|
Key Themes |
Quotes |
|
“Overall a positive impression on OSBEE program”
|
“Awesome learning environment, everyone was so positive and enthusiastic” “I really liked – overall it was good, …” “I think this today is quite eye-opening for me to see what approaches to take when it comes to different scenarios” “For me it was a very collaborative, We could ask questions, it was very friendly” “It kind of was an exam scenario I suppose. But not in a bad way” |
|
About the OSBEE stations |
“I think it’s a lot of real-life scenarios that you could potentially face out in the bush,” “Snake bite was pretty fun” “I don’t know if you guys have heard, where students are actually thrown into these scenarios and they can actually practice their skills.” “There was a lot of clinical practice, but not much clinical reasoning” |
|
“Positive learning during OSBEE”
|
“So I think that really – the most useful part of the day was the similar-ish things but different problems and different contexts and different patients to facilitate memory retention…” “Supervisors were very supportive. Learned a lot from them.” “I feel like the debrief session is enough of a learning. Just enough to know what to do.” |
|
“Positive impression of rural practice” |
“Yeah, it really paints a picture of the typical things, the different situations you might find in a rural scenario.” |
Table 1: Key themes with quotes
The questionnaire response rate by the six study participants was 100 %. All students agreed: “OSBEE was a positive learning experience” and “enjoyed the program”. And 2/3 (4 students) felt “OSBEE encouraged them to consider working in rural context”.
IV. DISCUSSION
Maldistribution of medical workforce is a global concern. Different strategies to address this have been implemented and described in the global literature. Medical schools play an important role in implementing initiatives that best promote rural medical career to grow the rural medical workforce. The OSBEE program provided an enjoyable peer-assisted rural contextualised learning experience and inspired participants to consider rural practice. Although brief rural clinical immersions alone are unlikely to significantly increase rural practice intent, they may enhance the impact of short-term and year-long rural clinical placements on future rural medical workforce.
V. MOVING FORWARD
Whilst our study group was small, and limits the generalisability of our findings, we believe our findings infer brief immersive clinical learning experiences play a role in the promotion of rural medical careers, thus have continued to offer the OSBEE program to early program medical students. However further evaluations of brief (and frequent or repeated) immersive rural clinical learning experiences, on student perceptions of rural medical careers would be useful. Tracking of students involved in these brief rural experiences, as well as short-term and year-long clinical placements would provide valuable insights, to see if participants of the various rural learning experiences do subsequently work in rural areas. Our program and findings may help other medical schools focused on increasing rural medical workforce.
Notes on Contributors
YGSW Jayarathne, MBBS, PG Dip in MEd, MD in MEd was involved the conceptual development, ethics application, data collection including focus group facilitator for the OSBEE evaluation, analysis of the quantitative data, thematic analysis of the qualitative data and the development of the manuscript, including the final approval.
Riitta Partanen, MBBS, FRACGP, DRACOG, General Practitioner, Head of UQRCS was involved in the conceptual development, ethics application, data collection including focus group facilitator for the near peer supervisors, analysis of the quantitative data, thematic analysis of the qualitative data and the development of the manuscript, including the final approval.
Jules Bennet, RN, Masters of Clin Ed, Grad Cert Emerg Nursing, Grad Cert Healthcare Simulation, Lead Clinical Educator – Clinical Skills & Simulation, UQRCS Hervey Bay was involved the conceptual development, ethics application, quantitative data collection, analysis of the quantitative data and the development of the manuscript and final approval.
Funding
This study was supported by funding received from the RHMT grant.
Declaration of Interest
There are no conflicts of interests related to the content presented in the paper.
References
Australian Government Department of Health. Rural Health Multidisciplinary Training (RHMT) Program. Retrieved February 20, 2020, from https://www1.health.gov.au/internet/main/publishing.nsf/Content/rural-health-multidisciplinary-training
Eley, D. S., Young, L., Wilkinson, D., Chater, A. B., & Baker, P. G. (2008). Coping with increasing numbers of medical students in rural clinical schools: Options and opportunities. Medical Journal of Australia, 188(11), 669-671.
Kwan, M. M., Kondalsamy-Chennakesavan, S., Ranmuthugala, G., Toombs, M. R., & Nicholson, G. C. (2017). The rural pipeline to longer-term rural practice: General practitioners and specialists. PLoS One, 12(7), e0180394
Talley, R. C. (1990). Graduate medical education and rural health care. Academic Medicine: Journal of the Association of American Medical Colleges, 65(12 Suppl), S22-5.
*Y G Shamalee Wasana Jayarathne
Medical Education Unit,
Faculty of Medicine and Allied Sciences,
Rajarata University of Sri Lanka
Email: wasana@med.rjt.ac.lk
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









