What’s in a name? Research learning outcomes in primary medical education
Submitted: 14 July 2020
Accepted: 16 September 2020
Published online: 13 July, TAPS 2021, 6(3), 99-103
https://doi.org/10.29060/TAPS.2021-6-3/PV2343
Colleen Cheek1,2, Richard Hays3 & Janie Smith2
1Education and Research, Tasmania Health Service North West, Australia; 2Faculty of Health Sciences and Medicine, Bond University, Australia; 3Centre for Rural & Remote Health, James Cook University, Australia
I. INTRODUCTION
Research ability is considered important in preparing medical graduates for their future work roles, providing openness to critical inquiry and astute information management (Frenk et al., 2010). The role of knowledge integrator, facilitator, and advisor, incorporating finely-tuned judgement, reasoning and decision-making, are important in achieving the leadership expected of the profession (Frenk et al., 2010). Engaging medical students in research training has historically proven challenging, and there is variable understanding of the level expected in primary medical training.
Most medical schools in Australia have now adopted a Master’s Level ‘Medical Doctorate’ (MD) for primary medical training. Both the Australian Qualifications Framework (2013) requirements (pertaining to the level of qualification) and the Australian Medical Council (AMC) standards (pertaining to the profession) expect graduates of an MD to have understanding of research principles, process and methods, and to be able to apply these to professional practice (Australian Medical Council Limited, 2012). Many schools have interpreted this as a requirement for more intensive research training. While research knowledge and skills are integrated throughout curricula, there is substantial variation in the way these are taught, and little evidence of effective learning exists.
Varying approaches to align courses internationally may have muddied the situation further. For example, in the UK, primary medical training is considered to meet the requirements of a UK Level 7 Master’s Degree, although most programmes have retained historical titles of Bachelor of Medicine, Bachelor of Surgery, abbreviated as BM BS or MBChB. In Canada, graduates of primary medical training are awarded the degree of Doctor of Medicine (MD) but are considered to have achieved academic outcomes at Bachelor level. In the US, graduates of primary medical training are awarded the degree of Doctor of Medicine (MD) and widely assumed to achieve Master’s level learning outcomes. European medical schools, through conformance with the Bologna Declaration, are tending toward a 2nd cycle, or Master’s degree. In the Asia-Pacific region, Singapore retains a Bachelor of Medicine, Bachelor of Surgery (MBBS), as do Malaysia (a Level 6 Bachelor degree), Japan and New Zealand. In Australia, there are some Bachelor (Level 7) programmes but most medical schools have adopted a Master’s Degree (Extended) (Level 9E) for primary medical training, conferring a ‘Medical Doctorate’ (MD). In these examples there is little correlation between learning outcome levels and programme duration, which ranges from four to six years.
A. Defining Learning Outcomes and the Level of Understanding Required
The most recent standards of the World Federation for Medical Education promote ‘constructively aligned’ medical education. That is, teaching activities and assessment aligned with student-centred learning outcomes where the type of knowledge, whether declarative (book knowledge) or functional (professional know-how required in the workplace), and the level of understanding required are clear.
The level of understanding can be mapped from taxonomies of action verbs. The Structure of Observed Learning Outcomes (SOLO) is one taxonomy (Biggs & Collis, 2014). It consists of five levels of understanding that reflect increasing learning complexity. The first is pre-structural (no understanding); through uni-structural and multi-structural (representing two stages of qualitative comprehension) to relational and extended abstract. The verbs ‘order’ and ‘compute’ might describe learning action at uni- and multi-structural stages, whereas ‘construct’ and ‘extrapolate’ describe learning action at relational and extended abstract stages. Once learning outcomes are explicit, decisions about teaching activities that will allow the student to achieve the learning outcomes can be made. For example, functional knowledge verbs e.g. ‘assess’ or ‘reflect’, reflects activity performed in the workplace (ideally), or an authentic simulated environment.
Here we provide a perspective of the research knowledge and skills required of graduates of an Australian MD to promote shared understanding of the level of learning and the key elements for orientating teaching to medical practice.
II. METHODS
To define the Individual Learning Outcomes (ILO) relating to research competency in Australia, the Level 9E Australian Qualifications Framework (AQF) criteria and descriptors (Australian Qualifications Framework, 2013) and the AMC standards and graduate outcomes (Australian Medical Council Limited, 2012) that pertained to research knowledge and skills were collated (Appendix 1). Using the SOLO taxonomy (Biggs & Collis, 2014), the types of knowledge and the required level of understanding was determined (Appendix 2).
III. RESULTS
Three issues emerged. The first was that the highest levels of understanding required (extended abstract), pertain to functional knowledge such as critically analysing information, reflecting on and applying theory. Graduates are expected to have ‘expert’ knowledge and abilities in this area based on ‘research, experience or occupation’. This may imply that achieving the higher-level learning outcomes requires a substantial research experience, such as a completed project that engages students in all aspects of planning, conducting, and reporting research. This reflects what happens during the AQF Level 10 (doctoral level) research training and may be difficult to achieve during a Level 9E programme.
The second was that a high level of functional knowledge (relational) is required to plan and execute project work, reflecting the more traditional, Master’s (Research) programme. This should be achievable during Master’s (extended) programmes if the learning takes place over time and provides ‘reasonable’ experience in aspects of research. For this to fit in with the clinical immersion learning experience, such projects should engage students with healthcare delivery.
The third was that a fairly high, but lower level of declarative knowledge (multi-structural and relational) is required pertaining to scientific methods, ethical and privacy principles, and these should be heavily grounded in application to the profession. This is consistent with the inclusion of research training modules in coursework, but without a requirement to complete a research project.
IV. DISCUSSION
Medical curricula should constantly evolve to meet the perceived needs of the changing population and health systems. Cooke et al. (2010) tell us that the virtues of being curious, of being open to further learning, taking time to consider different perspectives and weigh up the options are metacognitive skills that should be developed early in medical training to cultivate lifelong learning and drive for continuing improvement in health systems. The emphasis in current medical education commentary is to provide options and electives for flexible, student-led approaches to learning.
The AMC graduate outcomes (Australian Medical Council Limited, 2012) affirm that a critical component of developing competency as a doctor is the opportunity to hone generic skills such as communication and teamwork and apply developing knowledge through authentic experience in the clinical setting. Functional knowledge is demonstrated through project work conducted (ideally) in real work settings. This experience provides opportunities to learn to adapt to unforeseen medical problems and to learn interactive and reflective skills important in achieving both specialist professional performance and life-long learning. Fostering knowledge and skills in seeking information, considering alternatives, collaborating, making decisions, planning and executing the plan may better prepare medical professionals for leadership roles that are required of responsive health systems where emerging technology and global forces are likely to drive adaptation and reform. Facets of critical inquiry, such as recognising a knowledge gap, seeking information, seeing multiple perspectives, taking time to consider alternatives and then make a judgement, are also qualities of an adaptive leader. Achieving all of this through a completed research project during primary medical education is challenging. Performing one component well may be enough if it is known how the component fits as part of the whole.
Specific requirements for knowledge and skills in research and their application are still inherent in both AQF and AMC standards. Expertise in defining a searchable question and finding and assessing the evidence are realistic and useful goals for primary medical training and are professionally relevant to the work of doctors in the 21st century. Conducting literature reviews about topics that matter to the local community can be achieved in primary training. There are models of collaboration within healthcare settings where medical students are supported in a community of practice with more senior doctors overseeing local quality improvement projects. Quality improvement projects in Primary Care offer further opportunity.
There may be other ways of achieving Master’s level learning outcomes that do not require research experience, as some students are not ready for this. Examples include project work in professional and capstone settings, where students performed skills associated with developing leadership and management competency in a range of different contexts.
V. CONCLUSION
Achieving higher-order thinking by the end of primary medical education is emerging as crucial to graduating doctors who are better prepared for managing the future challenges of healthcare. Integration of research thinking with work-based experience may be the critical attribute to foster this and may also be achieved through professional and capstone projects. There is a case for providing stronger guidance on just what is intended and achievable within the constraints of contemporary medical education. It is unlikely that the move to Master’s level programmes in Australia will on its own result in more research capable graduates; more important may be how students are introduced to research knowledge and practical experiences. However, adopting Master’s level outcomes as the endpoint may improve consistency in achievement of higher-level thinking and the inferred ability to find solutions to challenges as healthcare evolves.
Notes on Contributors
Colleen Cheek developed the methodological framework for the study, performed data collection and data analysis as part her PhD research project, and wrote the manuscript, collated edits and approved the final manuscript.
Richard Hays reviewed the study design and interpretation and developed the manuscript, read and approved the final manuscript.
Janie Smith reviewed the design of the study and gave critical feedback to the writing of the manuscript, read and approved the final manuscript.
Funding
No funding source was required.
Declaration of Interest
We have no conflict of interest to declare.
References
Australian Medical Council Limited. (2012). Standards for assessment and accreditation of primary medical programs by the Australian Medical Council. https://www.amc.org.au/wp-content/uploads/2019/10/Standards-for-Assessment-and-Accreditation-of-Primary-Medical-Programs-by-the-Australian-Medical-Council-2012.pdf
Australian Qualifications Framework. (2013). Australian Qualifications Framework (2nd ed.). https://www.aqf.edu.au/sites/aqf/files/aqf-2nd-edition-january-2013.pdf.
Biggs, J. B., & Collis, K. F. (2014). Evaluating the quality of learning: The SOLO taxonomy (Structure of the observed learning outcome). Academic Press.
Cooke, M., Irby, D. M., & O’Brien, B. C. (2010). Educating physicians: A call for reform of medical school and residency (Vol. 16). John Wiley & Sons.
Frenk, J., Chen, L., Bhutta, Z. A., Cohen, J., Crisp, N., Evans, T., Fineberg, H., Garcia, P., Ke, Y., Kelley, P., Kistnasamy, B., Meleis, A., Naylor, D., Pablos-Mendez, A., Reddy, S., Scrimshaw, S., Sepulveda, J., Serwadda, D., & Zurayk, H. (2010). Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. The Lancet, 376(9756), 1923-1958. https://doi.org/10.1016/S0140-6736(10)61854-5
*Colleen Cheek
ADON Education and Research,
Tasmania Health Service North West
PO Box 258, Burnie 7320
Email: Colleen.Cheek@ths.tas.gov.au
Submitted: 17 August 2020
Accepted: 30 September 2020
Published online: 13 July, TAPS 2021, 6(3), 111-113
https://doi.org/10.29060/TAPS.2021-6-3/PV2375
Nicholas Beng Hui Ng1, Terri Chiong1, Perry Yew Weng Lau1 & Marion M Aw1,2
1Khoo Teck Puat – National University Children’s Medical Institute, National University Health System, National University Hospital, Singapore; 2Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
I. INTRODUCTION
The Coronavirus Disease (COVID-19) pandemic caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) virus has led to significant disruptions globally with alarming mortality rates and increasing economic burden. For the medical community, aside from massive changes in workflow, healthcare worker fatigue and direct risk of infection, COVID-19 has also resulted in significant disruptions to medical training. During a pandemic, it is not surprising that manpower, financial resources and time are allocated fully to contain the disease. We believe however, that structured teaching activities amidst this crisis play an important, if not pivotal role, in keeping the medical community united and informed of the rapidly changing evidence surrounding this disease. Our department instituted measures to ensure that disruptions to post-graduate training were minimised amidst the clinical workflow changes. In this article, we share our experience of how teaching activities were sustained through implementing various strategies. We also discuss the benefits derived from ongoing teaching during this pandemic.
II. EXECUTION AND EXPERIENCE
When Singapore first announced the escalation of the Disease Outbreak Response System Condition (DORSCON) alert level from yellow to orange in response to increasing community spread of COVID-19, all healthcare institutions immediately put in place protocols and workflow to cope with the demands of COVID-19 (A Singapore Government Agency Website, 2020). Our department, a paediatric department in a university hospital, followed suit with plans for team segregation and clinical workflow protocols for children with respiratory illnesses. At the same time, all face-to-face teaching activities and meetings were suspended, in an attempt to minimise gatherings of clinicians.
The Residency Programme Director quickly formed a dedicated Education Task Force (ETF) to look into adapting the post-graduate teaching activities to take into account clinical service needs, as well as team segregation. Prior to the pandemic, our post-graduate teaching (in additional to clinical learning on the job) were largely based on face-to-face large group sessions, as well as small group clinical bedside teaching. As the department adjusted to the new COVID-19 clinical workflow, the ETF effectively morphed the delivery of post-graduate education to cater to the education needs of residents and faculty.
Our teaching sessions have been transformed from in-person to on-line delivery via the Zoom video-conferencing platform. This has allowed residents (interns, medical officers, senior residents) from different clinical locations, who are not allowed to meet physically, to attend. An added benefit is that residents off-site may also choose to attend these teaching activities. In addition, faculty members who would previously not attend resident teaching have also been able to attend these sessions and collectively contribute to the teaching and learning process. We have been able to conduct almost all our continued medical education (CME) programmes via video-conferencing; journal clubs, mortality rounds, radiology rounds, topic reviews, history taking sessions, case-based discussions and importantly, COVID-19 clinical workflow updates.
The ETF outlined ground rules for the on-line teaching sessions at the outset: participants have to sign in with appropriate identification, unmute microphones only when speaking and respect the confidentiality of teaching materials without taking pictures or recordings unless explicit permission is obtained. In order to ensure the security of these video-conferencing sessions, each session is managed by a host, with controlled admission of participants.
A. Modified Clinical Teaching
During this pandemic, we have been able to continue clinical history-taking teaching sessions for residents with real patients via video-conferencing. In this format, one resident in the “hot-seat” takes the history from the patient remotely, while other participants observe the encounter via a live video stream from different locations. This “live” history-taking session is followed by a discussion between the resident and faculty on the patient’s clinical history as well as management. Other residents are also able to participate in the discussion. We have been extremely encouraged by the responses from patients and their families who have readily consented to these video-streaming teaching sessions. Our experience has reinforced the notion that patients are willing to participate in medical education as a means to give back to the medical community (Stacy & Spencer, 1999; Thomas et al., 1999). In a time of crisis like this, where the medical community has to quickly learn and rapidly adapt to new discoveries of COVID-19, the role of patient involvement in teaching and research cannot be better overstated.
B. Specific Mock Code Training
Aside from core teaching sessions for residents, the department quickly recognized the importance for on-the-go pandemic-preparedness training for the residents. Faculty from the critical care division has developed COVID-19 relevant mock code scenarios for residents using high fidelity simulation equipment. These sessions are conducted during designated time slots and adhere to the team segregation plans. The scenarios involve the use of powered air-purifying respirator (PAPR) equipment and personal protective equipment (PPE). Residents are given the opportunity to perform the initial clinical assessment, cardio-pulmonary resuscitation and intubation, as well as communicate with the rest of the clinical team whilst dealing with mock patient emergencies in negative-pressure isolation facilities. Many of the junior doctors as well as nurses quickly realized the added challenge of performing seemingly standard resuscitation in isolation facilities whilst in full PPE. Routine tasks such as communication between team members, preparation of drugs, use of resuscitation drug charts and even mobile phones while wearing PAPR and PPE can be extremely difficult. These simulation sessions highlighted to us that good planning, coordination and communication between healthcare workers are all the more crucial while resuscitating in a COVID-19 setting.
C. Increase Trainee Participation
An initial unanticipated benefit of this style of teaching and learning was increased trainee participation in these sessions. We noticed that a proportion of residents who would otherwise have remained silent in an open group teaching encounter were now more willing to ask and answer questions, either through their voice audio or using the chat function of the Zoom platform. What is most interesting is that when we compared our teaching attendance rates for residents at these video-conferencing CME compared to the usual face-to-face teaching, there was an increase from an average of 32% (pre-COVID-19) to 68% (during COVID-19) in daily attendance rates. This increase attendance was seen for both COVID-19 and non-COVID-19 related teaching sessions, suggesting that it was not only the COVID-19 updates that drew participation for these sessions. Contributing factors could include the ease of access afforded by learning from various (remote) locations, particularly for residents posted off-site who are unable to travel back. In addition, the Zoom video-conferencing tool is readily available on a variety of platforms, including laptops, tablets and mobile phones.
D. Limitations and Challenges
The main issue raised had been that of internet connectivity in certain areas around the hospital, but this has been rectified with specific locations allocated as “teaching hubs”.
Another shortcoming of the on-line teaching programme is that bedside teaching for clinical skills has not been possible, in the interest of staff and patient safety. The ETF has since explored other innovative approaches; using video clips of clinical signs, as well as preparing pre-taped clinical examination signs with patient and caregiver consent.
III. THE RECIPE TO SUCCESS
The feedback received from residents for this on-line delivered teaching has been extremely positive, with 42 of 46 residents rating it positively on a feedback survey. Many of our residents look forward to attending these sessions, not only as a means to learn, but also as an opportunity to connect with fellow colleagues.
We believe that our success in maintaining a relevant teaching programme during the COVID-19 pandemic is attributed also to the following factors:
- Strong teaching culture with a mission of ensuring that residents are appropriately trained.
- Faculty realising the importance of pandemic-preparedness training for residents.
- The ability to innovate and the flexibility to adjust the delivery of medical education to meet the needs of the current pandemic situation.
- The availability of reliable resources and use of latest educational technology such as the Zoom Video-Conferencing to allow delivery of web-based teaching.
IV. CONCLUSION
As our health workers continue to brave the frontline battling against COVID-19, we are frequently reminded of the importance that flexibility and adaptability is crucial during this pandemic. While we continue to deliver the best possible patient-centred care and ensure the safety of our healthcare workers amidst this COVID-19 pandemic, structured teaching in our department continues to be an important part of our daily routine. We experienced first-hand the benefits of web-based learning and would retain some of these sessions post-pandemic. The deliberate strategies taken by our department to ensure that teaching activities continue has allowed learning to persist in a structured and relevant way. Importantly, on-the-go training for pandemic-preparedness for residents is a highly valuable skill to teach during this time. We are very proud to be able to continue to learn and keep abreast the latest developments on COVID-19 as a department. As former United States First Lady, Abigail Adams so eloquently said, “Learning is not attained by chance, it must be sought for with ardour and attended to with diligence”.
Notes on Contributors
Ng Nicholas Beng Hui contributed in design, analysis and interpretation of data, drafting the article, and final approval of the version to be published. Chiong Terri contributed in analysis and interpretation of data, revising it critically for important intellectual content, and final approval of the version to be published. Lau Perry Yew Weng contributed in conception and design, and interpretation of data, revising it critically for important intellectual content, and final approval of the version to be published. Aw Marion M contributed in conception and design, and interpretation of data, revising it critically for important intellectual content, and final approval of the version to be published.
Acknowledgement
We thank Dr Dimple Rajgor for helping with in editing, formatting and in submission of the manuscript for publication.
Funding
No funding is required for this paper.
Declaration of Interest
The authors have no conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
A Singapore Government Agency Website. (2020). Additional measures introduced with DORSCON Orange Singapore. Retrieved March 10, 2020, from https://www.gov.sg/article/additional-measures-introduced-with-dorscon-orange
Stacy, R., & Spencer, J. (1999). Patients as teachers: A qualitative study of patients’ views on their role in a community‐based undergraduate project. Medical Education, 33(9), 688-694.
Thomas, E. J., Hafler, J. P., & Woo, B. (1999). The patient’s experience of being interviewed by first-year medical students. Medical Teacher, 21(3), 311-314. https://doi.org/10.1080/01421599979608
*Ng Nicholas Beng Hui
Khoo Teck Puat-National University
Children’s Medical Institute,
National University Health System,
1E Kent Ridge Road,
NUHS Tower Block Level 12,
Singapore 119228
Email: nicholas_bh_ng@nuhs.edu.sg
Submitted: 19 July 2020
Accepted: 7 October 2020
Published online: 13 July, TAPS 2021, 6(3), 67-74
https://doi.org/10.29060/TAPS.2021-6-3/OA2347
Tess Lin Teo, Jia Hao Lim, Choon Peng Jeremy Wee & Evelyn Wong
Department of Emergency Medicine, Singapore General Hospital, Singapore
Abstract
Introduction: Singapore experienced the COVID-19 outbreak from January 2020 and Emergency Departments (ED) were at the forefront of healthcare activity during this time. Medical students who were attached to the EDs had their clinical training affected.
Methods: We surveyed teaching faculty in a tertiary teaching hospital in Singapore to assess if they would consider delivering clinical teaching to medical students during the outbreak and conducted a thematic analysis of their responses.
Results: 53.6% felt that medical students should not undergo clinical teaching in the ED and 60.7% did not wish to teach medical students during the outbreak. Three themes arose during the analysis of the data – Cognitive Overload of Clinical Teachers, Prioritisation of Clinical Staff Welfare versus Medical Students, and Risk of Viral Exposure versus Clinical Education.
Conclusion: During a pandemic, a balance needs to be sought between clinical service and education, and faculty attitudes towards teaching in high-risk environments can shift their priorities in favour of providing the former over the latter.
Keywords: Disease Outbreak, Pandemic, Faculty, Medical Students, Attitudes, Clinical Teaching, Emergency Medicine
Practice Highlights
- In a pandemic, a balance needs to be sought between clinical education and risking learner exposure to the virus.
- A crisis situation can affect educators’ priorities and attitudes towards the provision of clinical education, in favour of providing crucial clinical services.
I. INTRODUCTION
Since the first reported cases of COVID-19 infections in Wuhan, in December 2019, the month of January 2020 saw Singapore’s Ministry of Health (MOH) issue guidelines and implement a series of calibrated defensive measures to reduce the risk of imported cases and community transmission (Lin et al., 2020; WHO, 2020). Singapore has a Disease Outbreak Response System Condition (DORSCON) framework, which guides the nation’s response to various emerging infectious diseases outbreaks. The four-level colour-coded system of Green, Yellow, Orange and Red, describes the increasing severity of the outbreak in the community (Quah et al., 2020).
The Department of Emergency Medicine (DEM) of Singapore General Hospital saw 130 000 visits in 2019 (SGH, 2019). It hosted 158 medical students (MS) through the year. Aside from some elective students, the majority were in their second year of clinical postings. Formal clerkships consisted of four weeks of clinical exposure in which they were expected to clerk and present cases to teaching faculty and perform minor procedures such as intravenous cannulation and insertion of bladder catheters etc., with about nine hours of classroom tutorials.
In early January 2020, DORSCON yellow was declared, indicating either a severe outbreak outside Singapore or that the disease was contained locally with no significant community spread (Quah et al., 2020). All DEM staff were required to wear personal protective equipment (PPE). Hospital elective surgeries were postponed. Other outbreak measures included setting up new isolation areas for patients. DEM staff had their leave embargoed to ensure that there was adequate manpower to staff these areas in anticipation of a gradually worsening outbreak (Chua et al., 2020).
On 7 February 2020, the outbreak alert rose to DORSCON Orange (DO) as there were cases of community transmissions (Quah et al., 2020). Based on previous experience managing the Severe Acute Respiratory Syndrome (SARS) outbreak 17 years prior, the DEM transitioned to an Outbreak Response Roster, where physicians and nurses of the DEM were split into teams that worked 12 hour shifts, with no overlapping shifts, hence limiting staff contact to only those within their teams (Chua et al., 2020). With DO in effect, the department needed to come to a rapid decision about whether or not to accept MS in the ED. A group of 12 MS that the DEM was supposed to host this April already had their clerkship cancelled due to concerns of breaching infection control and safe distancing measures. There have been no studies to date on faculty attitudes towards clinical teaching of MS during a pandemic, although papers have been published about students’ attitudes towards clinical training during disease outbreaks. The Clerkship Director conducted a short and focused survey amongst the faculty between the 27th-29th of March, amidst rising public concerns that the country might soon be locked down, to explore their attitudes on having MS clerkships during the COVID-19 pandemic. The results of this survey allowed the Director to quickly understand the sentiments of the faculty and thus decided that an entirely remote, online teaching program would be created instead. 9 days after the survey, on the 7th of April, the Singapore government officially announced the implementation of a lockdown, known locally as a ‘circuit breaker’ (Quah et al., 2020).
II. METHODS
Clinical teachers of the DEM were issued an anonymous survey over a period of three days via an online survey tool, SurveyMonkey (www.surveymonkey.com). Participants were informed prior to completing the survey that it was anonymous, and by proceeding with the survey they consented to the results being used for research purposes. The data collected included their professional appointments in the department and two yes/no questions: “Do you think medical students should be performing their EM clerkship during DO?” and “Are you keen on teaching MS clinically during DO?”. Participants answering “No” to the latter were asked to elaborate. All participants were asked to write about any concerns they had about having MS in the emergency department (ED) during DO. No other personal identifying information was sought. The survey was deliberately kept short and easy to answer to promote staff participation within the short timeframe the DEM had to make the decision about accepting students. Informed consent was waived as per the Institutional Review Board (IRB).
A simple descriptive quantitative analysis of responses to the 1st two yes-no questions identified the overarching sentiment of the department towards hosting MS during DO and was followed by a thematic analysis of the free-text answers to the last two open-ended questions (Braun & Clarke, 2006).
As many participants used the last question (‘any other comments?’) to emphasise or elaborate on the preceding question (‘why aren’t you keen to teach?’), the majority of the qualitative data gathered pertains to the issues of having MS in the department during DO. There was a paucity of data detailing why participants were in favour of teaching MS, as the survey did not specifically ask this. Hence, the authors chose to focus on analysing the responses of participants who were not keen to teach during this time. This analysis yielded three different themes. However, a small number of respondents supportive of MS felt strongly about teaching and volunteered their reasons in response to the last question. While this data is insufficient to support a robust thematic analysis, a small section is included at the end in order to present as complete a discussion as possible.
III. RESULTS
A. Participant Background
Participants consisted of Emergency Medicine (EM) specialists, permanent registrars or middle grade staff and EM senior residents. These groups were chosen because they each hold significant roles, such as being named supervisors or clinical instructors of MS, and have considerably more contact time with MS in the DEM as opposed to nursing staff or junior doctors.
B. Quantitative Results
A total of 28 out of 45 (62.3%) responses were recorded. Except for two individuals, all other respondents in favour of hosting MS in the ED during DO (46.4%) were also keen to teach them. About two-thirds of the participants (60.7%) were not keen to teach MS during DO. However, of this latter group, 23.5% of respondents offered (without prompting) a compromise – where they proposed teaching only during the relatively less busy night shifts, in their response to ‘Any other comments?’ Table 1 shows the breakdown of responses.
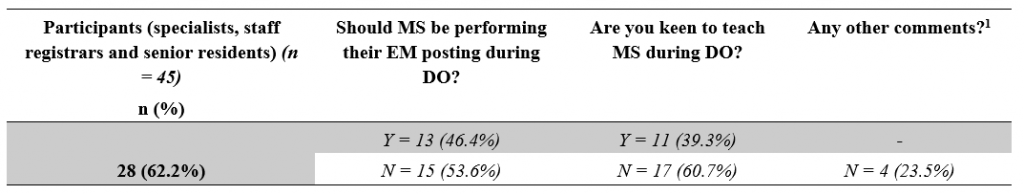
Table 1: Responses broken down by question.
[1]Number of participants who offered the compromise of teaching during the relatively less busy night shifts despite indicating they were not keen to teach MS.
C. Qualitative Results – Reasons Against
Each of the three themes presented here begins with a short paragraph that describes the situational context in which this survey took place, followed by a series of selected statements, and ends with a general summary and discussion of the responses within the respective theme. In order to maintain the authenticity of the data, each response is reproduced verbatim, sometimes in Singlish, the local colloquial variety of Standard Singaporean English (Bokhorst-Heng, 2005). Any edits to the text for clarification purposes have been clearly identified.
1) First theme: Cognitive overload of clinical teachers– There is only so much one can handle: Emergency physicians are no strangers to high stress environments, and are aware that as frontline workers they will be at the forefront in dealing with any emerging infectious disease. The move into DO represented the shifting of the local virus epidemiology from predominantly imported cases that could be easily identified and isolated, into the community-at-large. With this shift came changes to existing workflows and the re-arrangement of department space to form isolation areas for treating potential infectious cases. The implementation of a strict team-based roster described earlier meant that almost half the entire department would not physically meet the other half, and a surge in manpower requirements saw many junior doctors from other departments being rotated into the ED to help tackle the increased clinical load. Being new to the DEM, these new doctors required more supervision and assistance in adapting to the unfamiliar work environment. Responses that supported this theme include:
“High clinical load, long hours. Already cognitively overloaded. Not conducive for teaching. New [junior doctors] need to be taught also.”
Participant #6, Specialist
“Focus on daily evolving challenge first.” and in response to the last question “Please no.”
Participant #2, Senior Resident
“During DORSCON ORANGE we are in stress, if clinical teaching sessions start then other [doctors’] stress and workload level will increase.”
Participant #25, Staff registrar
“May be more a hassle if we have to look after the new [junior doctors] rotating and students [as well].”
Participant #4, Specialist
“We are also in a 12-hour outbreak roster which is physically, emotionally and mentally draining. Teaching students in this environment is far from ideal” and in response to the last question “Am fairly strongly against this idea”.
Participant #8, Specialist
“Day shifts no bandwidth to teach […] also can’t pay attention to [medical students] during day shifts, too tiring and too busy […] but I feel I can’t do [medical students] justice because I can’t debrief after a shift either, too tired.”
Participant #17, Specialist
Many of these responses conveyed a sense of exhaustion, reflecting the toll that constant workflow changes, longer work hours and relative social isolation was taking on the faculty. Teaching and supervising MS appeared to be viewed as a “hassle” or “extra work”, an additional drain to a clinical faculty’s energy during a busy and stressful shift.
This brought the department to a discussion on the provision of clinical services versus clinical education – whether teaching the next generation of future doctors was as important as treating the patient in front of us. One school of thought held that as clinician educators, physicians should – as the name implies – be clinicians first before educators. However, the interplay between these two roles is likely dependent on the faculty’s attitudes towards learners, as will be described later. Being cognitively overloaded naturally results in a shuffling of One’s priorities, which is seen next.
2) Second theme: Prioritisation of staff welfare – whose welfare is more important, staff or students? : It is well known that mental health can be adversely affected in crisis situations, and as the COVID-19 situation unfolded, boosting morale and maintaining the welfare of all staff became an important consideration (Matsuishi et al., 2012; McAlonan et al., 2007). At the forefront of this effort was the need to provide the staff with a supply of good quality personal protective equipment (PPE) so the staff would feel safe and confident in existing infection control measures. Although Singapore had yet to experience a shortage of PPE, there was still a concerted effort made by all hospitals to conserve these resources. Staff wellness was a theme seen in several responses:
“[I] can’t do the [junior doctors] justice because having a [medical student] attached to them is another stressor in an already stressful shift.”
Participant #17, Specialist
“Having to keep our doctors and nurses safe takes up a lot of energy. Students are young and naïve and will require even more time and resources to ensure they are safe.”
Participant #22, Specialist
“Furthermore, they will need to use PPE and again this should be conserved during the period of the outbreak.”
Participant #27, Specialist
“Medical students are important for future but I feel staff currently working in the department should be look after well.”
Participant #25, Staff registrar
“Waste PPE.”
Participant #20, Specialist
The importance of conserving PPE during a pandemic is undisputed and the concern that MS would use them up is valid. It was interesting to note in these responses hints of an “us-versus-them” mentality, where MS were seen as competition for the limited resources of PPE, time, and energy. Students were not viewed as part of the DEM team and perceived more as “stressors”, who required attention because they were “young and naïve”, and their use of PPE was viewed as a “waste”. This identification of an “in-group” of staff and an “out-group” of students led to a prioritisation or favouring of the former over the latter. This behaviour can be explained by the Social Identity Theory (SIT), which states that part of an individual’s self-image or self-concept is derived from the social groups to which they perceive themselves to belong to (Hogg & Reid, 2006; Tajfel & Turner, 1979). Thus, in order to maintain a positive self-image, there is a tendency for people to favour the in-group and discriminate against the out-group. This phenomenon was famously demonstrated by Tajfel et al in their Minimal Group Paradigm studies, which essentially showed that the mere perception of belonging to one of two distinct groups was enough to trigger social discrimination between the groups (Tajfel et al., 1971). Behaviour like this is indicative that a significant number of the department hold the belief that there is a distinct divide between students and staff, rather than seeing MS as belonging to the wider group of the medical fraternity. Creating such a divide between staff and student is problematic because it hinders effective teaching, especially because MS will eventually transition from the “out-group” of students to the “in-group” of staff upon graduation, and clinician educators are responsible for providing a safe environment for them to learn in. However, beyond this discussion of intergroup competition, there were concerns amongst the faculty with regards to the appropriateness of siting clinical learning in the high-risk, front-line location of the ED in a pandemic, as discussed in the next theme.
3) Third Theme: Risk of viral exposure vs clinical education – What is the price to pay and who pays it?: During the initial period of DO, medical schools pulled MS out of the clinical environment and moved to online learning, with the aim of protecting them from unnecessary exposure to the virus and for safe distancing. However, when they proposed that students be allowed back into the hospitals after undergoing PPE training, this risk of exposure had not changed, as the number of positive cases was rising daily still. Responses that reflected this theme included:
“Don’t think it’s appropriate to have students around in a high-risk environment.”
Participant #4, Specialist
“Having medical students around not only will expose them to infection it will also compromise the rest of the staff in the event of a breach in infection [protocols]. Also, them just hanging around & not allowed to have hands-on [participation] in the procedures, clerking, [patient] contact etc will not be of any benefit [to them] at this time.”
Participant #7, Senior Resident
“Student safety issue. No minder to ensure students’ adherence to strict PPE as Doctors and Nurses will be busy with clinical service.”
Participant #11, Specialist
“I think medical students are not providing clinical care to patients and having them in the ED increases risk to patients (without the attendant benefits) and increases risk to themselves (without the moral obligation to do so as doctors) and their family.”
Participant #27, Specialist
“Can students be [held] responsible for their own health? Or the school or the department? As doctors, we know it as our duty and occupational hazard. But as students – their duty is to learn (best done in a safe environment), not put their health at risk.”
Participant #6, Specialist
Responses that addressed the risk of virus exposure in the ED could be divided into two groups –those that were predominantly concerned about the students themselves catching the virus, and those that were more concerned about the consequences of such an event. The risk of catching the virus was seen as too high a cost – one that was borne not only by the individual student but by the patients and the staff as well. The benefits of clinical bedside instruction were called into question, as students’ movements would be restricted to low or medium-risk areas only. More than one participant raised the potential issue of students breaching infection control protocol or needing supervision in donning their PPE, despite reassurances given that schools would send MS for PPE training. This reflected a lack of trust in MS – themselves adult learners – who could be reasonably expected to understand the importance of infection control protocols. It begs the question of how big a role the educator plays in the personal safety of a MS and that of the patients and staff they interact with.
D. Qualitative Results – Reasons For
The survey design did not specifically ask responders about their reasons for supporting teaching MS during this pandemic. However, some participants felt strongly enough about this to advocate for clinical postings. Their reasons are shared below.
1) Theme: For the sake of tomorrow – In defence of teaching amidst a crisis:
“I feel we can still provide a meaningful learning experience for these students. We just need to lay out clear instructions and precautions for them to follow. It is a good opportunity to show to students how emergency medicine is adaptive, versatile, and for them to appreciate how quickly workflows can change, or how triage works in a disaster setting.”
Participant # 15, Specialist
“The way it is done has to be different […] the traditional method of teaching, where the students look to the seniors and may expect some form of spoon feeding […] Only when this mind-set is removed, will the tutors […] look at them as part of the team and incorporate them […], and will students see […] themselves as Drs to be [sic], practice safe habits from the very start and protect themselves as the patient’s doctor. This sense of ownership, accountability, professionalism can be started from that stage as a medical student. This is the perfect opportunity to state that this is what is expected and groom them likewise.”
Participant #19, Specialist
“I feel that the teaching should as much as possible be a simulation of working life and that working in high-risk areas such as these gives a semblance of pressure which cultivates good habits such as mindfulness of hand hygiene, donning of PPE etc.”
Participant #26, Senior Resident
The responses share a commonality of seeing the pandemic as an opportunity for modelling positive attitudes that would benefit the student in the future. This point of view advocates for the acknowledgement of the realities of being a doctor and assumes that students are already part of the “in-group” of the medical team rather than the “out-group” as seen in the earlier discussion.
IV. DISCUSSION
A. Limitations
This study has its limitations, chiefly being the lack of qualitative data representing the opinions of those who were keen to teach MS as the initial survey was conducted with the purpose of gauging whether or not the department would be open to receiving MS during DO. This lack of data meant that this study is at best a one-sided representation of the department’s opinion.
Additionally, all four of the authors have a keen interest in the education of MS and two of the authors are actively involved in faculty development. They were all both participants in the study as well as its evaluators. Prior to evaluation of results, the authors themselves suspected that majority of the faculty would be too overwhelmed with the changes the pandemic wrought to want to teach students, which may have contributed to confirmation bias in the analysis of the data. However, throughout the analysis, every attempt was made to ensure that the themes uncovered remained true to the data, and much of the original data was reproduced here faithfully to maintain transparency, such that the reader may draw their own conclusions.
Another limitation of the study was that the survey was unable to measure shifts in the attitudes of faculty as the pandemic evolved, which would have allowed us to understand the amplitude of the effect of the pandemic itself more clearly.
B. New Insights
It was worth noting that nearly two-thirds of the department did not want to teach MS during DO, despite each participant having taught MS routinely prior to this pandemic. Initial analysis of the reasons given for this refusal revealed three distinct themes of Cognitive Overload of Teachers, the need to Prioritise Staff Welfare and the Risk of Viral Exposure to Students – themes that are transferrable to many departments involved in pandemic response, regardless of locality.
Expounding further on this topic, it can be seen in some of the responses detailed under the themes of Cognitive Overload and Prioritising Staff Welfare, that there was a perceived increase in the need to supervise the new junior doctors rotating into the department on short notice (as opposed to the junior doctors who were already in the middle of their rotation and thus more familiar with the department’s protocols). This supervision is an important component of the continuing clinical education of junior doctors, which in itself is part of a larger debate surrounding the competing aims of clinical service versus clinical education that has been ongoing for many years (Woods, 1980). It is often the case in EM that when overwhelmed with patients, clinical education is sacrificed for clinical service without much short-term complications. Indeed, even amongst EM residents, more research is needed to define the optimal balance between service and education (Quinn & Brunett, 2009). However, a pandemic presents a rather unique situation in that most junior doctors will not have worked in a pandemic before. Thus, the need to educate junior doctors on both pandemic response and the importance of personal safety – with its direct impact on patient safety – now cannot be sacrificed without directly affecting the provision of clinical service.
It is beyond the scope of this paper to comment on whether educating MS on pandemics through clinical immersion programs during a pandemic better prepares them for future outbreaks, or in the broader sense, whether the clinical education of today’s MS by immersive learning can bolster the clinical service of tomorrow’s junior doctors. In fact, it seems almost premature to consider this question given the paternalistic attitude many of our faculty appeared to have towards students, perceiving them as learners to be looked after – to the extent that they could not even be trusted with their own safety and that of the patients and staff they interact with. Interestingly, this view seems to be shared by MS themselves – an electronic survey conducted at one of Singapore’s medical schools showed that a third of currently enrolled MS were concerned that they might introduce possible risks to the patient should they return to the clinical setting (Compton et al., 2020). These findings are indicative of a more deeply rooted mindset in which the social hierarchy draws a clear line between Teacher and Student. This becomes clearer when one considers that in Confucian Heritage Cultures such as Singapore (Biggs, 1998), the teacher holds great authority and students brought up in such cultures tend to defer to such authority as a matter of course (Ho, 2020). Given the multiple factors that contribute to this debate, it is unlikely that we will be able to arrive at a clear answer without further research, but what is certain is that medical students are not essential workers and, in a pandemic, medical schools need to balance their educational needs and ethical obligations to keep students safe (Menon et al., 2020).
Within our paper, it is heartening that many participants who were not keen to teach still tried to offer a compromise of teaching during the relatively less busy night shifts instead, and that 46% of our department were willing to accept MS during this period. COVID-19 allowed us to uncover some of the underlying attitudes towards MS and to consider them in the context of Singapore’s cultural heritage. These attitudes are important for us to address if we are to improve the delivery of medical education in the ED and we would like to invite the reader to consider whether the same uncovering has occurred in their respective departments.
V. CONCLUSION
The balance between clinical service and clinical education is a precarious one that appears to shift quickly in favour of the former in the high-risk environment of an evolving pandemic, which presents significant challenges even for experienced educators to overcome. As seen in our paper, cognitive overload of educators and the need to prioritise the welfare of junior staff inexperienced in pandemic response takes clear precedence over the education of MS. The paternalistic view that majority of our faculty hold leads to doubts about the ability of MS to keep themselves and their patients safe from virus exposure, doubts that are surprisingly shared by MS as well, and is indicative of the social hierarchy deeply ingrained in Confucian Heritage Cultures such as Singapore and surrounding countries in the region, where students tend to defer to authority as a matter of course. In order to improve as medical educators, we must place further effort into uncovering the underlying attitudes of both faculty and MS and address them in ways specific to our cultural heritage.
Notes on Contributors
Author Teo TL analysed the transcripts, conducted the primary thematic analysis and wrote the manuscript. Author Lim JH co-wrote the manuscript. Author Wee JCP conducted the literature review and developed the manuscript. Author Wong E designed and conducted the study, performed the data collection and developed the manuscript. All the authors have read and approved the final manuscript.
Ethical Approval
IRB approval for this study was obtained (SingHealth CRIB reference number 2020/2134).
Acknowledgement
The authors would like to acknowledge all participants of the survey.
Funding
No funding sources are associated with this study.
Declaration of Interest
All authors work in SGH DEM and answered the survey as participants.
References
Biggs, J. (1998). Learning from the confucian heritage: So size doesn’t matter? International Journal of Educational Research, 29(8), 723–738. https://doi.org/10.1016/S0883-0355(98)00060-3
Bokhorst-Heng, W. D. (2005). Debating singlish. Multilingua, 24(3), 185–209. https://doi.org/10.1515/mult.2005.24.3.185
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Chua, W. L. T., Quah, L. J. J., Shen, Y., Zakaria, D., Wan, P. W., Tan, K., & Wong, E. (2020). Emergency department ‘outbreak rostering’ to meet challenges of COVID-19. Emergency Medicine Journal, 37(7), 407–410. https://doi.org/10.1136/emermed-2020-209614
Compton, S., Sarraf-Yazdi, S., Rustandy, F., & Radha Krishna, L. K. (2020). Medical students’ preference for returning to the clinical setting during the COVID-19 pandemic. Medical Education, 54(10), 943–950. https://doi.org/10.1111/medu.14268
Ho, S. (2020). Culture and learning: Confucian heritage learners, social-oriented achievement, and innovative pedagogies. In C. Sanger & N. Gleason (Eds.), Diversity and inclusion in global higher education (pp. 117–159). Palgrave Macmillan. https://doi.org/10.1007/978-981-15-1628-3
Hogg, M. A., & Reid, S. A. (2006). Social identity, self-categorization, and the communication of group norms. Communication Theory, 16(1), 7–30. https://doi.org/10.1111/j.1468-2885.2006.00003.x
Lin, R. J., Lee, T. H., & Lye, D. C. B. (2020). From SARS to COVID-19: The Singapore journey. The Medical Journal of Australia, 212(11), 497-502.e1. https://doi.org/10.5694/mja2.50623
Matsuishi, K., Kawazoe, A., Imai, H., Ito, A., Mouri, K., Kitamura, N., Miyake, K., Mino, K., Isobe, M., Takamiya, S., Hitokoto, H., & Mita, T. (2012). Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry and Clinical Neurosciences, 66(4), 353–360. https://doi.org/10.1111/j.1440-1819.2012.02336.x
McAlonan, G. M., Lee, A. M., Cheung, V., Cheung, C., Tsang, K. W. T., Sham, P. C., Chua, S. E., & Wong, J. G. W. S. (2007). Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Canadian Journal of Psychiatry, 52(4), 241–247. https://doi.org/10.1177/070674370705200406
Menon, A., Klein, E. J., Kollars, K., & Kleinhenz, A. L. W. (2020). Medical students are not essential workers: Examining institutional responsibility during the COVID-19 pandemic. Academic Medicine, 95(8), 1149–1151. https://doi.org/10.1097/ACM.0000000000003478
Quah, L. J. J., Tan, B. K. K., Fua, T. P., Wee, C. P. J., Lim, C. S., Nadarajan, G., Zakaria, N. D., Chan, S. J., Wan, P. W., Teo, L. T., Chua, Y. Y., Wong, E., & Venkataraman, A. (2020). Reorganising the emergency department to manage the COVID-19 outbreak. International Journal of Emergency Medicine, 13(1), 32. https://doi.org/10.1186/s12245-020-00294-w
Quinn, A., & Brunett, P. (2009). Service versus education: Finding the right balance: A consensus statement from the council of emergency medicine residency directors 2009 academic assembly “Question 19” working group. Academic Emergency Medicine, 16(SUPPL. 2), 15–18. https://doi.org/10.1111/j.1553-2712.2009.00599.x
SGH. (2019). Hospital Overview – Singapore General Hospital. Retrieved August 17, 2020, from https://www.sgh.com.sg/about-us/corporate-profile/Pages/hospital-overview.aspx
COVID-19 (Temporary Measures) Act 2020. (2020). https://sso.agc.gov.sg/Act/COVID19TMA2020
Tajfel, H., Billig, M. G., Bundy, R. P., & Flament, C. (1971). Social categorization and intergroup behaviour. European Journal of Social Psychology, 1(2), 149–178. https://doi.org/10.1002/ejsp.2420010202
Tajfel, H., & Turner, J. C. (1979). An integrative theory of intergroup conflict. In W. G. Austin & S. Worchel (Eds.), The social psychology of intergroup relations (pp. 33–47). Brooks/Cole.
WHO. (2020). IHR emergency committee for pneumonia due to the novel coronavirus 2019-nCoV transcript of a pressing briefing. Retrived January 30, 2020, from https://www.who.int/docs/default-source/coronaviruse/transcripts/ihr-emergency-committee-for-pneumonia-due-to-the-novel-coronavirus-2019-ncov-press-briefing-transcript-30012020.pdf?sfvrsn=c9463ac1_2
Woods, D. (1980). Service and education in residency programs. A question of balance. Canadian Medical Association Journal, 123(1), 44.
*Evelyn Wong
Department of Emergency Medicine,
Singapore General Hospital
Outram Road
Singapore 169608
Email: evelyn.wong@singhealth.com.sg
Submitted: 30 August 2020
Accepted: 9 December 2020
Published online: 13 July, TAPS 2021, 6(3), 56-66
https://doi.org/10.29060/TAPS.2021-6-3/OA2440
Gayathri Devi Nadarajan1, Kirsty J Freeman2, Paul Weng Wan1, Jia Hao Lim1, Abegail Resus Fernandez2 & Evelyn Wong1
1Department of Emergency Medicine, Singapore General Hospital, Singapore; 2Office of Education, Duke-NUS Medical School, Singapore
Abstract
Introduction: COVID-19 challenged a graduate medical student Emergency Medicine Clinical Clerkship to transform a 160-hour face-to-face clinical syllabus to a remotely delivered e-learning programme comprising of live streamed lectures, case-based discussions, and telesimulation experiences. This paper outlines the evaluation of the telesimulation component of a programme that was designed as a solution to COVID-19 restriction.
Methods: A mixed methods approach was used to evaluate the telesimulation educational activities. Via a post-course online survey student were asked to rate the pre-simulation preparation, level of engagement, confidence in recognising and responding to the four clinical presentations and to evaluate telesimulation as a tool to prepare for working in the clinical environment. Students responded to open-ended questions describing their experience in greater depth.
Results: Forty-two (72.4%) out of 58 students responded. 97.62% agreed that participating in the simulation was interesting and useful and 90.48% felt that this will provide a good grounding prior to clinical work. Four key themes were identified: Fidelity, Realism, Engagement and Knowledge, Skills and Attitudes Outcomes. Limitations of telesimulation included the inability to examine patients, perform procedures and experience non-verbal cues of team members and patients; but this emphasised importance of non-verbal cues and close looped communication. Additionally, designing the telesimulation according to defined objectives and scheduling it after the theory teaching contributed to successful execution.
Conclusion: Telesimulation is an effective alternative when in-person teaching is not possible and if used correctly, can sharpen non-tactile aspects of clinical care such as history taking, executing treatment algorithms and team communication.
Keywords: Telesimulation, COVID-19, Emergency Medicine, Programme Evaluation
Practice Highlights
- Telesimulation doesn’t replace but can be an effective alternative when in-person teaching is not possible.
- When implemented correctly, it can sharpen non-tactile aspects of clinical care.
- It is possible to achieve a level of fidelity and realism in a telesimulation environment.
- Simulation faculty needs to be skilled in debriefing techniques that enable the learner to reflect.
- Limitations of telesimulation can be reframed as learning opportunities.
I. INTRODUCTION
COVID-19 brought about unexpected challenges to medical education, especially to student clinical clerkships where medical students would spend time within a clinical discipline, interacting with clinicians and learning from patients. Healthcare institutions restricted student movement within clinical environments and barred students from entering the high-risk frontline areas to reduce exposure risk.
Prior to COVID-19, students undertaking an Emergency Medicine (EM) Clinical Clerkship, would have the opportunity to manage and deliver care to high acuity patients, with bedside teaching, small group tutorials, problem-based learning and simulation modalities. With COVID-19, students were not permitted into the Emergency Department (ED) and face-to-face teaching activities were halted. Hence this clerkship had to be conducted remotely. The EM clerkship was transformed from a 160-hour clinical programme to a remotely administered programme comprising 40 hours of e-learning, 40 hours of interactive live online session and 15 hours of telesimulation. As part of this programme, we decided to utilise telesimulation to help students achieve some of the objectives of a clinical clerkship.
Telesimulation is defined as the “Process by which telecommunication and simulation resources are utilised to provide education, training and/or assessment to learners at an off-site location” (McCoy et al., 2017). By allowing simulation to be conducted through devices such as the computer and phone, it mitigates the problem of physical proximity. Though telesimulation has existed for about a decade, its utilisation appears limited to the rural settings and studies mainly describe its usage for learning skills (Mikrogianakis et al., 2011; Naik et al., 2020; Okrainec et al., 2010) rather than for emergency management of patients. With the need to adapt teaching to remote experiences, telesimulation is gaining popularity (Sa-Couto & Nicolau, 2020).
A. Programme Overview
This remote learning programme was developed in a tertiary ED in Singapore which receives both undergraduate and postgraduate medical students for their EM clerkship. There were 58 postgraduate medical students undertaking their 4-week EM clerkship in June 2020. The EM core clinical training curriculum was taught by EM faculty via online modules and interactive classroom sessions delivered via the video conferencing platform, Zoom. The learners spent the mornings in interactive online sessions with faculty, and afternoons in self-study as part of a flipped classroom learning, using provided learning materials. The telesimulation session was scheduled in the last week, over five days. The students were split into ten groups each comprising of five to six students, where two groups participated in one telesimulation session each day.
Our objectives for this telesimulation programme was to ensure that the students could take a focused clinical history from the simulated patients, communicate with them, construct a list of differentials and manage them accordingly in the emergency setting. The secondary objectives were to train them to prioritise the investigations and management of critically ill patients and to communicate and work effectively within a team. Using Kern’s six step approach, the team of simulation and clinical educators’ planned and implemented the telesimulation activity to achieve these outcomes (Harden et al., 1999; Smith & Dollase, 1999) during their EM clerkship.
As medical students, the learners are at a novice stage according to The Dreyfus Model of Skill Acquisition (Benner, 2004; Dreyfuss & Dreyfus, 1980). Hence, the deliberate attempt not to assess skills such as intubation or defibrillation through telesimulation as it may create unnecessary anxiety and feelings of incompetence (Papanagnou, 2017). Furthermore, it was deemed challenging to conduct procedural skill teaching through this modality. Instead, the focus was on clinical reasoning and patient management. The clinical students fall under the category of “show how” within the Miller’s pyramid, with regards to history taking, clinical reasoning and management. As adult learners, a problem centred (Knowles, 1990), experiential learning approach (Kolb, 1984) would be more valuable. Hence telesimulation was an appropriate modality.
Each telesimulation session was conducted by two simulation and one physician faculty. There was a total of four scenarios for each session, where one group, consisting of five to six students, will participate in the scenario, while the other group observes, before switching. This allowed each group of students to participate in two clinical scenarios. The topics chosen for telesimulation were Anaphylaxis, Cardiac Arrest, Meningitis, and Syncope where the theory was covered in the core topics in the preceding weeks. Each of these scenarios began with the students taking a history from the simulated patient, before the patient progressively deteriorated and required resuscitation. Figure 1 shows a summary of the scenarios. The scenarios were selected as they did not require much procedure-based interventions (e.g. chest tube insertion in a poly trauma victim) which would be difficult to assess via Zoom.
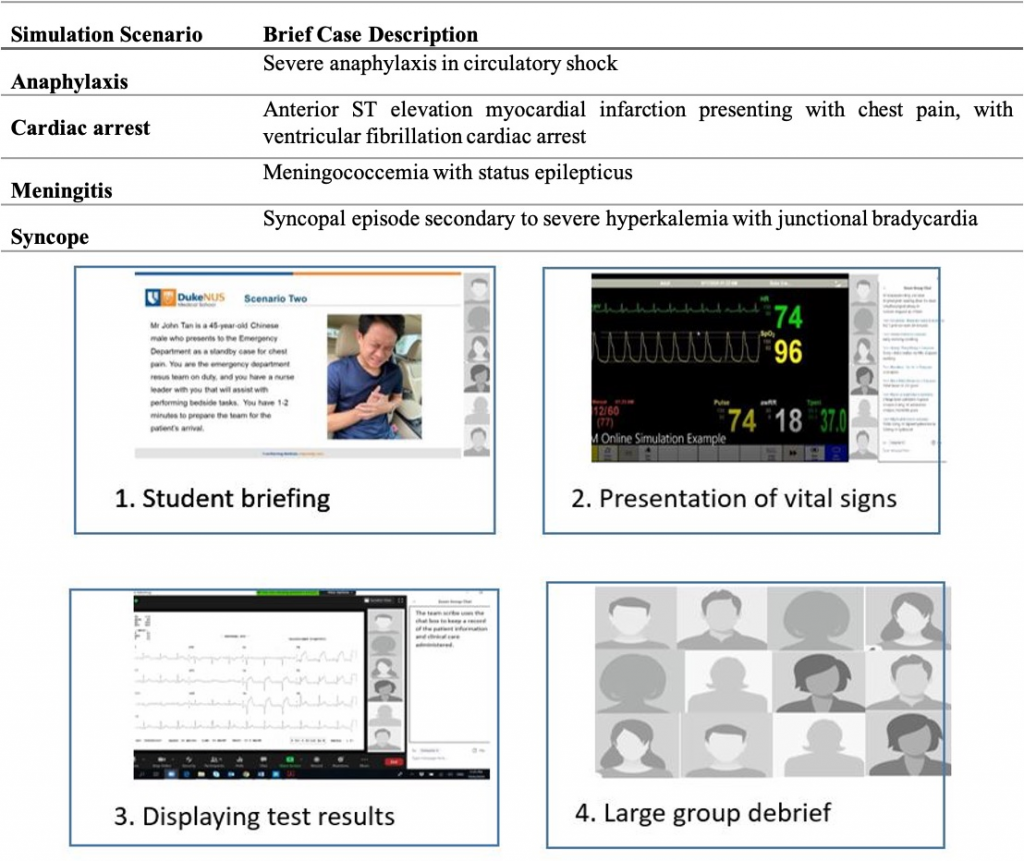
Figure 1. Brief case description of simulation scenarios and visual presentation of the flow of the telesimulation experience
The sessions commenced with a briefing where the students were orientated to the online environment, including the use of video and microphones. As depicted in Figure 1, using the share screen feature, the simulation technician switched between different views. The briefing included a photo of the patient as a visual cue, along with the text of the presenting case. One of the simulation faculty played the circulating nurse, providing prompts to aid students’ engagement and asking participants to clarify their statements or orders as the scenario progressed. Using existing mannequin software and ensuring sharing of screen sounds, real-time patient monitoring was provided to the learners when requested. Upon request, additional visual cues of investigation results would be displayed, reverting back to either a picture of the patient or the patient monitoring. With their video off, the clinical faculty voiced the patient. At the conclusion of the scenario, all participants and faculty turned their video and microphones back on to participate in the large group debrief before proceeding on to the next scenario.
The objective of this paper is to describe the students’ experience of telesimulation as part of an online clerkship programme and how such techniques can be used to meet learning outcomes (Harden et al., 1999) in various settings. At the time of writing, there is no literature describing evaluation of the use of a telesimulation programme within the ED for medical student education, with this paper aiming to address this gap.
II. METHODS
A mixed methods approach was used to evaluate the introduction of telesimulation to the EM online clerkship, and to gain students’ perspective on learning through telesimulation. Programme evaluation research aligns with a mixed methods approach as the collection of both quantitative and qualitative data provide a deeper understanding of the student experience (Cohen et al., 2011).
A. Participants, Data Collection and Analysis
58 final year medical students who participated in the EM Online Clerkship programme were invited to participate in a post-telesimulation activity evaluation survey. Using a 5-point Likert scale, students were asked to indicate their agreement on 11 items addressing pre-simulation preparation, their level of engagement, confidence in recognising and responding to the four clinical presentations and telesimulation as a tool to prepare for working in the clinical environment. Seven open-ended questions were asked to enable the students to describe their experience in greater depth. 24hrs after completing the telesimulation session, students received an email with a link to the survey. Qualtrics online survey software was used to build, distribute and collect the survey responses. Voluntary consent was assumed by participation in the anonymised online evaluation. A statement outlining the purpose of the survey was included at the start of the survey and require an agreement before the survey could be commenced. Completion of the survey therefore implied consent. The survey took between three and five minutes to complete, all responses were anonymous, with no identifiable data collected.
Descriptive statistics was used to analyse the responses to the Likert scale questions, with thematic analysis of the open-ended survey questions. Author one (GN) and author two (KF) reviewed the transcripts separately, making note of key phrases, outline possible categories or themes. Both authors then jointly rearranged and renamed the codes, developing higher order themes. NVivo 12™ was used to store, code and manage the qualitative data.
III. RESULTS
Of the 58 students who were invited to participate in the survey, 42 complete responses were received, a response rate of 72.4%. As seen in table 2, the results demonstrated that 97.62% of respondents agreed/strongly agreed that participating in the telesimulation session was interesting and useful to their learning. In relation to the use of visual and auditory cues, 93% of respondents felt that these helped them engage in the simulation. In relation to their level of preparedness to participate in the telesimulation experience, nearly 17% of respondents reported that the pre-session handout did not adequately preparing them for what to expect in the session.
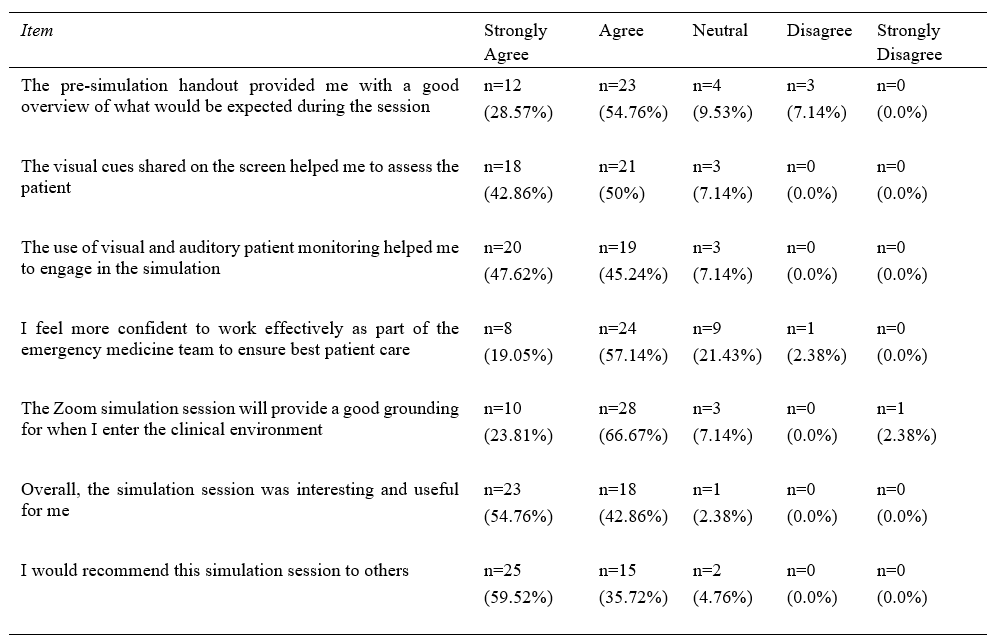
Table 1. Results of the student responses to the Likert scale items
When asked to rate if they felt more confident recognising and responding to the four clinical presentations (anaphylaxis, cardiac arrest, meningitis, and syncope), between 90% and 93% agreed/strongly agreed that participating in the telesimulation sessions resulted in them feeling more confident in recognising and responding to the specific clinical presentations (Figure 2).
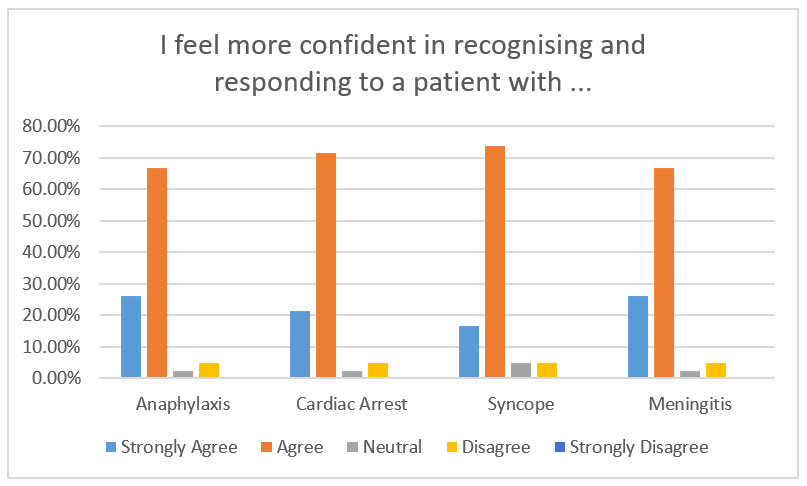
Figure 2. Student rating to the question “I feel more confident in recognising and responding to a patient with …”
Four key themes were identified following the data analysis of the open-ended survey questions, describing around the telesimulation experience of the respondents: 1) Fidelity; 2) Realism; 3) Engagement; and 4) Outcomes. As demonstrated in Figure 3, the themes do not exist in isolation, but intersect as they describe the telesimulation experience that the students had. The students feedback reflected the benefits and limitations which fall under these main themes.
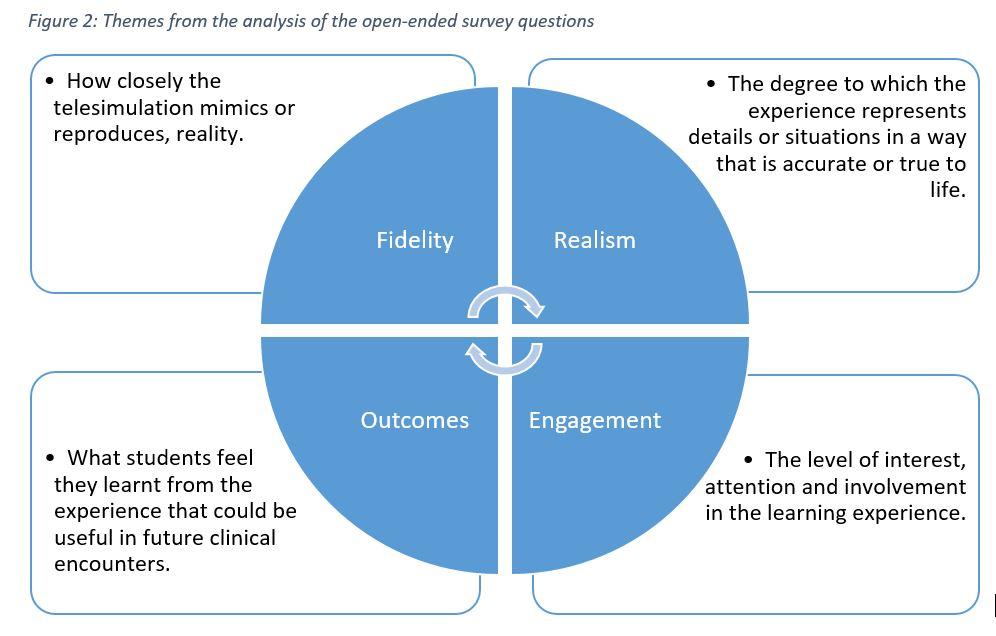
Figure 3. Themes reflecting the students experience with telesimulation
A. Fidelity – Physical, Psychological and Conceptual
The theme Fidelity reflects how closely the telesimulation mimics or reproduces, reality. Subthemes of conceptual, physical and psychological fidelity were also reflected. The students’ feedback reflected limitations in physical fidelity while conceptual and psychological fidelity was present mostly.
They reported that the auditory and visual stimulus from the dynamic display of investigations and real-time vital signs monitoring, provided a high level of physical fidelity.
“Auditory and visual information on patients’ vitals and results were really helpful in generating the differential list.”
Student 37
“The noise and sights is a good proxy for real life cases in a virtual environment.”
Student 4
“Seeing the vitals of the patient in real-time allows us to experience the importance of time in managing critically ill patients”
Student 20
However, aspects of physical fidelity, particularly related to the patient assessment, were reported as challenging via telesimulation. With the patient represented as a static picture, voiced by the clinical faculty, students shared how the lack of non-verbal and visual cues from the patient impacted their ability to perform a physical assessment of their patient.
“….we don’t get to observe the body language of the patient as much as we would like”
Student 12
“More difficult than in real life. Seeing and hearing a real patient gives much information”
Student 15
“I think what is lacking is being able to visually evaluate the patient”
Student 21
In terms of the level of psychological fidelity, the auditory cues from the ‘patient’ and the real-time vital signs monitoring simulated the ED resuscitation room, which appears to have instilled a similar sense the stress and the need to think under pressure, as reflected by the students’ feedback.
“Have to work around the distractions of beeping monitors, seizing patient, teammates asking questions/suggestions.”
Student 33
“It’s dynamic and gives us the opportunity to think under pressure.”
Student 13
“Stressful but probably close to reality?”
Student 35
The students’ statements reflected the subtheme of conceptual fidelity, where they felt the context and sequence was similar to what they would encounter in the ED, where they are required to deliver timely and lifesaving treatment. This was possibly because the faculty made deliberate attempts to ensure that events during the simulation would unfold as it usually would in the ED room, based on the learners’ actions.
“It simulates a clinical environment with real time updates of vitals and test results in addition to the history and communications.”
Student 5
What the students did report struggling with however, was the limitations of the platform in terms of multiple actions occurring simultaneously. Unlike in real life, multiple tasks could not be performed at the same time over the online platform, and this impeded the conceptual fidelity.
“In reality, multiple interventions would be carried out in tandem.”
Student 35
“More challenging to perform tasks concurrently over Zoom.”
Student 36
“…many things cannot occur concurrently.”
Student 2
B. Realism
The theme Realism captures the degree to which the experience represented details or situations in a way that is accurate or true to life. Students reported that aspects of the telesimulation experience represented what they thought an actual ED encounter would be like.
“I think the process is similar to the actual clinical environment, it is difficult, especially when the patient is deteriorating in front of you, and your team are waiting for you to make the decisions.”
Student 41
“The pictures/videos and the beeping of the monitor, they make it more real”.
Student 42
“It was realistic as getting the differentials was time sensitive”.
Student 13
The students also acknowledged the limitations in achieving realism presented by telesimulation as the various team members could not perform tasks simultaneously and take in cues from the patient to assess the outcome of their actions.
“Harder to communicate with my teammates compared to real life because only one person could speak at a time while in real life, multiple conversations could be occurring”
Student 3
“More difficult than taking a history in real life – more technical issues (can’t hear properly), Can’t see the patient”
Student 8
C. Engagement
The theme Engagement relates to the level of interest, attention and involvement in the learning experience. The level of fidelity and realism impacts the level of engagement of the learners. Most students were able to immerse themselves and fully engage in the scenarios, possibly because aspects of fidelity and realism were deliberately given close attention during the preparation phase.
“I actually forgot that the patient was being voiced by the clinical tutor”
Student 41
“My heart was racing doing the simulation – what will I be like when I am there for real?”
Student 41
However, on the downside, without being together in the same place, some felt that the scenario was too “messy” and “chaotic” and found it difficult to follow.
“It was a little hectic with the many other ongoing tasks in the background”
Student 6
“Easier to detach oneself from the patient (less affected by patient’s appearance, tone of voice, blood, gore, suffering etc.)”
Student 28
At the same time, some students faced technical difficulties, such as small or flickering screen, poor internet connection or poor audio, which were barriers to their engagement.
“…there were some issues hearing the faculty clearly which may affect the quality of learning.”
Student 6
By addressing the concepts of realism and fidelity, the students reported increased levels of engagement, although it appears that technical barriers unique to telesimulation provide challenges for some students achieving a greater level of engagement.
D. Outcomes- Knowledge, Skills and Attitudes
The theme Outcomes encompasses what students feel they learnt from the experience that could be useful in future clinical encounters. Under outcomes, there were sub-themes of knowledge, skills and attitudes. From a knowledge perspective, students reported that the telesimulation reinforced their clinical reasoning to arrive at a differential list.
“It was very useful and helped with our clinical reasoning. It was also useful in learning how to generate differential diagnoses as a team and going down the path of a working differential diagnosis while keeping others in mind.”
Student 32
Whilst the lack of hands-on practice was acknowledged, the telesimulation environment required them to practice the skills of prioritisation, leadership, teamwork and effective, close loop communication to manage the patient and this accounted for their skills gained.
“I will be able to apply the concept of teamwork, thinking on my feet, thinking broad, and constant reassessment of the unstable patient in my clinical training over the next few months”
Student 6
“Stay calm, go back to first principles, have the approach at your fingertips, make an effort to remember drug doses and administration route”
Student 2
IV. DISCUSSION
In relation to Kirkpatrick’s model for evaluating educational outcomes, the results of this study (table 1) demonstrate achievement of both level one (reactions) and level two (learning) outcomes (Kirkpatrick & Kirkpatrick, 2009). Whilst these findings may not determine the effectiveness of telesimulation, it does however provide insight into the learners’ experience that have highlighted the strengths and limitations of telesimulation, which the authors of this paper believe provides a foundation upon which others can build.
It is well documented in the simulation literature that fidelity and realism are important concepts that need to be considered when planning simulation-based education (Oliver, 2002). And this was an initial concern by the educators. The lack of a physical ‘patient’ on which to carry out procedures and physical examination could limit the effectiveness of the telesimulation experience. To address this limitation, faculty briefed the learners about the limitations and the strategies, such as the use of a ‘nurse confederate’ to provide clinical information, as well as having visual cues such as pictures and videos to trigger their actions. Interestingly, the feedback suggests that the lack of a physical ‘patient’ to examine, resulted in more emphasis being placed on the audio and visual cues during the session. This allowed the learners to proactively compensate for the lack of tactile cues with audio and visual ones, reinforcing the importance of clinical alerts and alarms. The inability to perform a physical examination provided an opportunity for the debriefer to emphasise the importance of the skill in clinical care.
There was a deliberate attempt to create scenarios that were commonly seen in the ED in as much details as possible to achieve realism in the virtual space. This limited the scenarios that could be used as we had to use ensure procedures were not required for the patient management to progress (for example, trauma was deemed inappropriate). The faculty feel that the typical, non-complex ED scenarios compounded with the sequence of events as it would occur in real life possibly contributed to the student’s perception of realism during the telesimulation.
Instructional scaffolding was key to student engagement. The faculty configured the telesimulation session to be held after three weeks of interactive and didactic sessions on Zoom. This allows the learners to acquire essential knowledge which they can then apply during the telesimulation session. With the background baseline knowledge, the telesimulation setup and audio and visual prompts of a real ED environment, the faculty felt that they were able to immerse the students within the scenario rather than conducting it as an online Problem-Based-Learning session. This may have contributed to their engagement.
Communication skills were a common thread reported by the students, both positively and negatively in many of their statements. They described the shortcomings of communication over Zoom and felt that the session highlighted how non-verbal cues and the physical presence influences the way one communicates. At the same time, the absence of visual and tactile stimuli forced them to practice good communication to get their points across when managing the patients.
Interestingly, though many students scored high on the Likert scale about feeling confident in managing emergencies, with the open-ended questions, they reflected feelings of nervousness, fear and a lack of confidence to working in the ED, showing that perhaps this cannot replace patient contact.
Cognisant of the limitations of telesimulation, most of the learners enjoyed the session. This may have been due to the novelty of it and ED room mimics such as the beeping of the monitors and the realistic scenarios. Faculty also realise that the limitations of telesimulation and used them as discussion points to highlight elements that one may take for granted during their patient encounters, such as the non-verbal cues and the tactile stimuli.
Key to this successful telesimulation session was establishing realistic and focused objectives (Harden et al., 1999). Failing to recognise that telesimulation differs from conventional simulation and therefore emphasising on tactile skills such as procedures and physical examination will minimise the effectiveness of the session. Knowing the inherent limitations helped faculty to prepare holistically for the session. Learning objectives focused on non-tactile aspects, such as history taking and executing treatment algorithms. In addition, as tactile cues are limited in the telesimulation setting, all other cues such as visual and audio were optimised.
Debriefing during the telesimulation sessions has an even more vital role in student learning compared to conventional simulation sessions (Fanning & Gaba, 2007). The debriefer not only has to highlight salient clinical points regarding the case, but also probe learners to think about limitations of the telesimulation modality. Therein, understanding the importance of highlighting tactile and visual feedback. For example, one learner recognised that he was “unable to visually observe and direct the teammate”; another came to the conclusion that “being able to see the patient and physical expression of fellow doctors/nurses is crucial”. This allows the educator to discuss the importance of situational awareness and non-verbal cues in enhancing team dynamics. However, if the debriefer fails to address this limitation, the learners may leave the session feeling dissatisfied or inadequate with their performance at the session. The uniqueness of telesimulation adds another facet to debriefing where the debriefer needs to be able to address the limitations of telesimulation and relate it back to clinical relevance. Therefore, there might be a need to provide additional training for educators in debriefing telesimulation sessions.
Simulation-based training is an effective modality to teach procedural skills, put into practice treatment algorithms and hone soft-skill relevant to team dynamics. (Lateef, 2010; Sirimanna & Aggarwal, 2014). As demonstrated through this innovative programme, it has an important role to play in medical education during such a pandemic where it might be used to mitigate the negative educational impact of no patient contact, team-based training and protocol development and testing (Chaplin et al., 2020; Dieckmann et al., 2020). All this is done within a psychologically and physically safe environment.
Based on the feedback collected, a conceptual framework below (Figure 4) was drawn, showing the relationship between the concepts of fidelity and realism in the telesimulation experience to the level of engagement and therefore outcomes perceived by the learners. This is supported by the objectives, experiential learning and a safe learning environment.
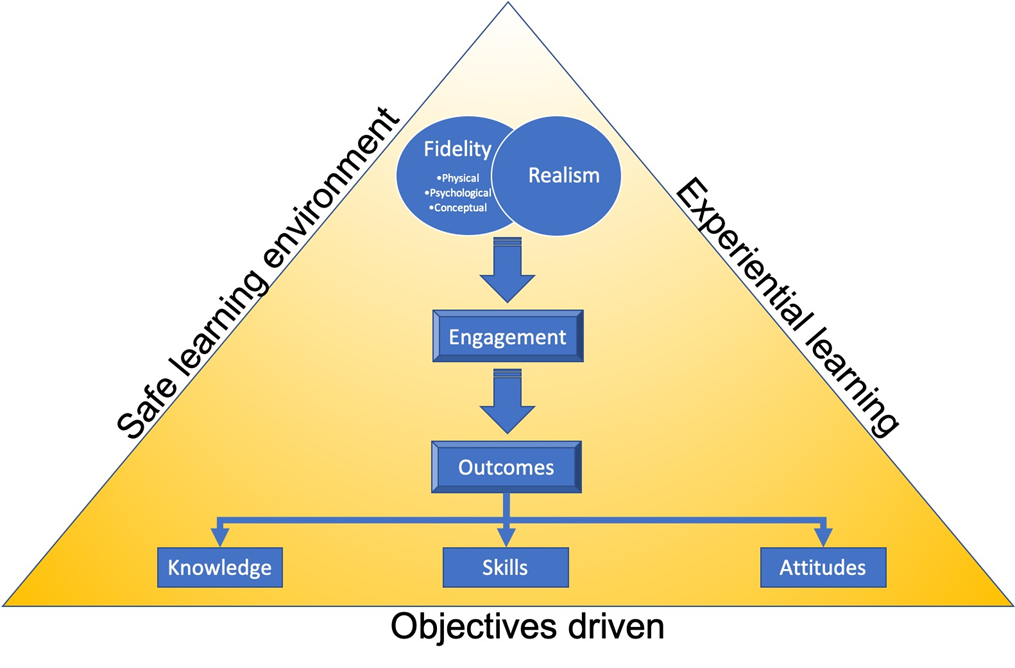
Figure 4. Conceptual framework
V. CONCLUSION
The role of face-to-face interactions with patients and immersing oneself in the acute care environment in bridging the theory to practice gap experienced by all healthcare students is essential to their clinical training. The restrictions encountered due to COVID-19 have required clinical educators to be agile and innovative in their approach the clinical clerkships. The EM clerkship telesimulation programme set out to provide an avenue for medical students to hone their clinical skills (history taking) and clinical reasoning (deriving differential diagnosis) in a safe environment. The evaluation of this programme has highlighted key areas of telesimulation which educators need to consider when planning to use it. The feedback from the students is promising and it highlights certain teaching points which may not be reflected upon during in-person simulation. Educators who wish to implement a telesimulation programme should pay particular attention to the learning objectives and debriefing methods. Whilst this paper has outlined how telesimulation can be implemented during a pandemic, it is envisaged that educators from other healthcare disciplines could use these findings to support the adoption of telesimulation in a variety of educational contexts. Telesimulation is a good alternative in settings such as this pandemic or during distance training programmes and may be a convenient way to hone history taking, clinical reasoning and communication skills without the use of an expensive simulation laboratory. The modality needs to meet the learning objectives and the debriefing should be adopted for telesimulation. However, the authors/faculty feel it cannot replace the full benefits of in-person simulation or learning from direct patient contact.
Notes on Contributors
Gayathri Devi Nadarajan and Kirsty J Freeman conceptualised the article, undertook the thematic analysis, contributed to article sections, and reviewed and revised manuscript based on suggestions from the other authors.
Lim Jia Hao, Wan Paul Weng and WONG Evelyn contributed to the conceptualisation of the paper, contributed to the article sections, reviewed and revised drafts.
Abegail Resus Fernandez undertook the quantitative analysis, and reviewed drafts.
All authors were involved in the development and delivery of the EM Clerkship Telesimulation Programme. All the authors have read and approved the final manuscript.
Ethical Approval
The SingHealth Centralised Institutional Review Board (CIRB) granted an exemption, CIRB Ref. No.: 2020/2719, as this study was assessed as a quality improvement project.
Data Availability
All relevant data are within the manuscript.
Acknowledgement
We would like to thanks the students who participated in this unit and their willingness to adapt to the online platform with grace and enthusiasm.
Funding
This work has not received any external funding.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Benner, P. (2004). Using the dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bulletin of Science, Technology and Society, 24(3), 188–199. https://doi.org/10.1177/0270467604265061
Chaplin, T., McColl, T., Petrosoniak, A., & Hall, A. K. (2020). Building the plane as you fly: Simulation during the COVID-19 pandemic. Canadian Journal of Emergency Medicine, 22(5), 576–578. https://doi.org/10.1017/cem.2020.398
Cohen, L., Manion, L., & Morrison, K. (2011). Research methods in education. Routledge. https://doi.org/10.4324/9780203720967
Dieckmann, P., Torgeirsen, K., Qvindesland, S. A., Thomas, L., Bushell, V., & Langli Ersdal, H. (2020). The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: Practical tips and resources from Norway, Denmark, and the UK. Advances in Simulation, 5(1), 1–10. https://doi.org/10.1186/s41077-020-00121-5
Dreyfuss, S. E., & Dreyfus, H. L. (1980). A five-stage model of the mental activities involved in directed skill acquisition. Berkeley. https://apps.dtic.mil/dtic/tr/fulltext/u2/a084551.pdf
Fanning, R. M., & Gaba, D. M. (2007). The role of debriefing in simulation-based learning. Simulation in Healthcare, 2(2), 115–125. https://doi.org/10.1097/SIH.0b013e3180315539
Harden, R. M., Crosby, J. R., & Davis, M. H. (1999). AMEE Guide No. 14: Outcome-based education: Part 1 – An introduction to outcome-based education. Medical Teacher, 21(1), 7–14. https://doi.org/10.1080/01421599979969
Kirkpatrick, D. L., & Kirkpatrick, J. D. (2009). Evaluating: Part of a ten-step process. In evaluating training programs. Berrett-Koehler Publishers.
Knowles, M. S. (1990). The adult learner: A neglected species. Gulf Publishing Co.
Kolb, D. A. (1984). The process of experiential learning. Experiential learning: Experience as the source of learning and development (pp. 20-38). Prentice Hall.
Lateef, F. (2010). Simulation-based learning: Just like the real thing. Journal of Emergencies, Trauma, and Shock, 3(4), 348. https://doi.org/10.4103/0974-2700.70743
McCoy, C. E., Sayegh, J., Alrabah, R., & Yarris, L. M. (2017). Telesimulation: An innovative tool for health professions education. Academic Emergency Medicine Education and Training, 1(2), 132–136. https://doi.org/10.1002/aet2.10015
Mikrogianakis, A., Kam, A., Silver, S., Bakanisi, B., Henao, O., Okrainec, A., & Azzie, G. (2011). Telesimulation: An innovative and effective tool for teaching novel intraosseous insertion techniques in developing countries. Academic Emergency Medicine, 18(4), 420–427. https://doi.org/10.1111/j.1553-2712.2011.01038.x
Naik, N., Finkelstein, R. A., Howell, J., Rajwani, K., & Ching, K. (2020). Telesimulation for COVID-19 Ventilator management training with social-distancing restrictions during the coronavirus pandemic. Simulation and Gaming, 51(4), 571–577. https://doi.org/10.1177/1046878120926561
Okrainec, A., Henao, O., & Azzie, G. (2010). Telesimulation: An effective method for teaching the fundamentals of laparoscopic surgery in resource-restricted countries. Surgical Endoscopy, 24(2), 417–422. https://doi.org/10.1007/s00464-009-0572-6
Oliver, R. G. (2002). Simulation-based medical education. In R. M. Harden & J. A. Dent (Eds.), A practical guide for medical teachers (4th ed., Vol. 29, Issue 2, pp. 226–233). Churchill Livingstone.
Papanagnou, D. (2017). Telesimulation: A paradigm shift for simulation education. Academic Emergency Medicine Education and Training, 1(2), 137–139. https://doi.org/10.1002/aet2.10032
Sa-Couto, C., & Nicolau, A. (2020). How to use telesimulation to reduce COVID-19 training challenges: A recipe with free online tools and a bit of imagination. MedEdPublish, 9(1), 1–7. https://doi.org/10.15694/mep.2020.000129.1
Sirimanna, P. V., & Aggarwal, R. (2014). Patient safety. In Levine, A., DeMaria, S., Jr., Schwartz, A. D., & Sim. A. J. (Eds.). The comprehensive textbook of healthcare simulation. Springer.
Smith, S. R., & Dollase, R. (1999). AMEE guide No. 14: Outcome-based education: Part 2 – Planning, implementing and evaluating a competency-based curriculum. Medical Teacher, 21(1), 15–22. https://doi.org/10.1080/01421599979978
*Gayathri Devi Nadarajan
Department of Emergency Medicine
Singapore General Hospital
1 Outram Road, Singapore 169608
Tel: +65 96804724
Email: gayathri.devi.nadarajan@singhealth.com.sg
Submitted: 28 July 2020
Accepted: 23 December 2020
Published online: 13 July, TAPS 2021, 6(3), 104-107
https://doi.org/10.29060/TAPS.2021-6-3/PV2363
Tushar Hari1, Dennis Hathey1, Sonia Kumar2, Ilona Blee2, Rachel Browne3 & Simon Tso3
1Buckingham Medical School, United Kingdom; 2South Warwickshire National Health Service Foundation Trust, United Kingdom; 3Jephson Dermatology Centre, South Warwickshire National Health Service Foundation Trust, United Kingdom
I. INTRODUCTION
We live in unprecedented times with the COVID-19 pandemic disrupting our normal way of life. First identified in December 2019, the novel SARS-CoV-2 strain has brought about vast devastation. According to the World Health Organisation (WHO), as of 21st November 2020, there are 56.9 million confirmed cases and 1.3 million deaths worldwide. The government approach to control the spread of COVID-19 in the United Kingdom (UK) is underpinned by social distancing measures; to limit the spread and prevent the inundation of National Health Service (NHS).
Social distancing impacts society on both an individual and population level. Across the country, virtual learning has become the new normal. It is our experience at Buckingham Medical School that students saw their clinical placements suspended. Educational resources were shared via online platforms and final year examinations done remotely to fast-track the transition to newly qualified doctors with an interim registration with the UK General Medical Council (GMC).
In this opinion piece, a diverse panel of two medical students, two doctors-in-training and two educators, including individuals with international student status, learning and sensory difficulties, chronic diseases, and dependents, discussed the impact on undergraduate medical education for individuals who may risk being left behind if efforts towards widening participation are not considered amidst this crisis and its aftermath. The focus group was held as an online asynchronous unstructured discussion through emails over a three-month period, moderated by a consultant, who regularly posted questions for the groups to discuss. This was supplemented by face-to-face discussion between the participants to summarise key outcomes and then circulated the conclusions to the panel before manuscript inclusion. Verbal consent was obtained from participants.
II. OVERVIEW: THE CHANGING LANDSCAPE OF UNDERGRADUATE MEDICAL TRAINING IN THE UK
What was once a curriculum encompassing face-to-face clinical teaching to deliver a degree in medicine, has now become reliant on the virtual learning environment (VLE).
In the UK, medical teaching methods vary between institutions. Under such unprecedented times, these long-established methods of education have required immediate reform, with VLE taking over and clinical teaching being significantly reduced or temporarily paused (Taha et al., 2020).
The use of VLE in UK medical schools has increased within the last decade. Many already utilise VLE for lecture recording, uploading learning materials, or online assessments. Challenges with virtual teaching existed before COVID-19, particularly the lack of time for educators to become familiar with and implement online learning. Some educators view virtual teaching negatively and thus engage poorly with these platforms (O’Doherty et al., 2018). These learning platforms may also be perceived as expensive. However, need is a big driver for change. With the COVID-19 pandemic forcing the need for socially distant learning, many institutions have become more receptive to this change and many students are benefitting from the flexibility of engaging with the material remotely.
Since the start of the pandemic, medical schools have begun to disseminate pre-recorded or live lectures using online platforms such as Microsoft Teams or Zoom. Simulations of the clinical setting are being recreated to accommodate for the loss of practical experience and provide medical students in the early stages an introduction to the clinical environment. Reduced opportunity for workplace-based clinical learning, suspension of rotational training and medical electives could also potentially impact on career choices due to a lack of exposure.
Student pastoral care is vital during this pandemic, with new anxieties and stresses arising daily. This can be continued on these virtual platforms, either as one-to-one sessions or in tutorial groups. However, members of our focus group expressed how they found video conferencing less personal, and difficulty with internet connections can make it hard to discuss personal problems.
III. INCLUSIVITY AND WIDENING PARTICIPATION CONSIDERATIONS
The GMC states that: “a diverse population is better served by a diverse workforce” (General Medical Council, 2018). Much effort has gone into widening access to medicine and focusing on inclusivity and diversity within medicine. This work must not be forgotten amidst this crisis.
A. Our International Community of Medical Students in the UK
An international UK medical student from our focus group explained that governments are advising their citizens abroad to return home. COVID-19 has impacted countries to varying degrees and many students have been recalled to help with national efforts such as volunteer work and contact tracing. With medical school teaching resuming via VLE in the UK, the challenge of now balancing voluntary commitments at home, family life and university work is made more difficult by differing time zones. Educators in the UK should bear in mind that these factors could impact on students’ level of engagement and learner satisfaction with online synchronous learning opportunities. Furthermore, access to certain learning resources such as the electronic British National Formulary and NICE (National Institute for Health & Care Excellence) guidelines is restricted outside the UK, causing difficulties with revision for some. Many have expressed concern regarding the future of their degrees; with questions around when respective governments will change travel advice so that they can return to the UK, and implications of the pandemic on their visas and degree duration. This uncertainty and stress are impacting some international students’ focus on their degrees. International students have also found positives to the new methods of teaching. Many students shared that online learning is more engaging compared to live classes and easier to access, ensuring standardised availability of resources for all, regardless of location. Also, many are content to be home with family support during a time of international crisis.
B. Students with Sensory Disability, Learning Differences and Chronic Diseases
In 2016/2017 the proportion of students with a declared disability was 9.3%, rising to 10.4% in 2017/2018 (General Medical Council, 2021). In the time of COVID-19, having a disability or chronic disease presents an additional barrier to effective workplace-based learning. Specific learning differences could impact on students’ ability to assist on ward round activities such as documentation. Documentation in medical notes at our institution is now performed away from patients’ bedside following completion of daily ward rounds due to infection control considerations. This presents student scribers with difficulties in working memory or other specific learning differences, the additional challenge of recalling large volumes of complex information after an event. In our real-life example, the clinician supported and debriefed the student after the ward round, and ensured the student had adequate time to document the plan in the patient notes, demonstrating a positive example of inclusivity.
Medical students with hearing impairment require lip-reading as a communication adjunct. Unfortunately, implementation of using face masks in the clinical setting limits this and there is a lack of availability of medical grade transparent face masks. Therefore, considerations on using appropriate debriefing and non-verbal communication skills such as hand gestures and written forms of expression can be vital in delivering a complete learning experience for students.
Many vulnerable students are concerned about their risks of contracting COVID-19 and thus their ability to complete their degree in the original timeframe. High-risk individuals have been advised to avoid clinical areas or even isolate at home. Students must fulfil time-based and performance-based criteria to be awarded a GMC-recognised medical degree, but the loss of time and clinical experience in a compact degree programme could put into question their ability to complete on time.
C. Students with Dependents
Students with dependents and those balancing part-time work with medicine to ease the financial burden of their degree could also require additional support. Universities and Colleges Admissions Service (UCAS) guidelines state, a student who holds responsibility for a child aged 17 or younger, should have access to additional support with studies (Universities and Colleges Admissions Service [UCAS], 2021). Students with dependents face many challenges during their degree due to personal obligations. The VLE offers students with dependents an opportunity to maintain their learning at a time when access to schools and care facilities are restricted during the lockdown, but this also presents the challenge of learning and completing coursework while simultaneously caring for their dependents. For some, a distinction between the place of study and the home environment was key to maintaining an effective work-life balance. The availability of care facilities, financial health of students and access to university hardship grants and support systems, would be key to maintaining this group of students’ participation in studying medicine.
IV. CONCLUSION
From our experience, the COVID-19 pandemic has changed the delivery of undergraduate medical education at the current time – whether these changes persist remains to be seen. Educators should be considerate about student support in this new way of working, to benefit all students. This applies especially to those with undeclared or undiagnosed learning difficulties, disability, chronic disease, and those with dependents, to encourage their full participation in all available workplace and online-based learning activities and integrate them into the clinical team. It is also important to implement the perceived advantages of VLE in future medical curricula. Further literature is required to see if these changes have truly made a positive impact on learning. Such inclusion is crucial to not deter students from continuing medicine. Neglecting the demands for these groups can hinder our previous efforts at widening participation within the NHS.
Notes on Contributors
Tushar Hari was involved mainly with creating the first draft of the paper and leading the focus group. He contributed some of his experiences as an international student. He participated in revising the paper prior to submission.
Dennis Hathey was involved with initially drafting the paper and helped organise the focus group. He was involved with designing the focus group questions and gathering various perspectives. He took part in final approval of the published version as did all the other authors.
Dr Sonia Kumar contributed to shaping the paper in the later stages and added input on all aspects of the paper. She helped with data collection and critical appraisal of the final draft of the submitted paper.
Dr Ilona Blee added input into the needs of disabled students and overall shaped the paper to its final draft. She played an important role in approving the final copy and contributed to data analysis and interpretation.
Dr Rachel Browne contributed to final changes made to the draft and made final approval of the paper along with the other authors.
Dr Simon Tso contributed to the final approval of the paper and helped supervise the conception and progression of the paper and focus group.
In summary, all authors fulfill the four criteria stated for authorship.
Acknowledgement
We would like to express our gratitude to our focus group participants for their contributions.
Funding
No funds were required for this paper.
Declaration of Interest
We have no conflicts of interest to disclose.
References
General Medical Council. (2018). Medical school reports. https://www.gmc-uk.org/education/reports-and-reviews/medical-school-reports.
General Medical Council. (2021). Who is a disabled person. https://www.gmc-uk.org/education/standards-guidance-and-curricula/guidance/welcomed-and-valued/health-and-disability-in-medicine/who-is-a-disabled-person.
O’Doherty, D., Dromey, M., Lougheed, J., Hannigan, A., Last, J., & McGrath, D. (2018). Barriers and solutions to online learning in medical education – An integrative review. BMC Medical Education, 18(1), 130. https://doi.org/10.1186/s12909-018-1240-0
Taha, M., Abdalla, M., Wadi, M., & Khalafalla, H. (2020). Curriculum delivery in Medical Education during an emergency: A guide based on the responses to the COVID-19 pandemic. MedEdPublish, 9(1), 69. https://doi.org/10.15694/mep.2020.000069.1
Universities and Colleges Admissions Service. (2021). Students with parenting responsibilities. https://www.ucas.com/undergraduate/applying-university/individual-needs/students-parenting-responsibilities
*Tushar Hari
Buckingham Medical School
Yeomanry House, Hunter Street,
University of Buckingham
Buckinghamshire, UK, MK181EG
Email: 1606656@buckingham.ac.uk
Submitted: 14 August 2020
Accepted: 6 November 2020
Published online: 13 July, TAPS 2021, 6(3), 45-55
https://doi.org/10.29060/TAPS.2021-6-3/OA2377
Nathalie Khoueiry Zgheib1, Ahmed Ali2 & Ramzi Sabra1
1Department of Pharmacology and Toxicology, American University of Beirut Faculty of Medicine, Beirut, Lebanon; 2Medical Education Unit, American University of Beirut Faculty of Medicine, Beirut, Lebanon
Abstract
Introduction: The forced transition to online learning due to the COVID-19 pandemic has impacted medical education significantly.
Methods: In this paper, the authors compare the performance of Year 1 and 2 classes of medical students who took the same courses either online (2019-2020) or face-to-face (2018-2019), and compare their evaluation of these courses. The authors also present results of three survey questions delivered to current Year 1 medical students on the perceived advantages and disadvantages of online learning and suggestions for improvement.
Results: Performance and evaluation scores of Year 1 and 2 classes was similar irrespective of the mode of delivery of the course in question. 30 current (2019-2020) Year 1 students responded to the survey questions with a response rate of 25.4%. Some of the cited disadvantages had to do with technical, infrastructural and faculty know-how and support. But the more challenging limitations had to do with the process of learning and what facilitates it, the students’ ability to self-regulate and to motivate themselves, the negative impact of isolation, loss of socialisation and interaction with peers and faculty, and the almost total lack of hands-on experiences.
Conclusion: Rapid transition to online learning did not affect student knowledge acquisition negatively. As such, the sudden shift to online education might not be a totally negative development and can be harnessed to drive a more progressive medical education agenda. These results are particularly important considering the several disadvantages that the students cited in relation to the online delivery of the courses.
Keywords: Online Learning, COVID-19 Pandemic, Medical Students
Practice Highlights
- The authors report on the forced transition to online learning due to the COVID-19 pandemic.
- The performance and evaluation scores were similar in online delivery vs face-to face.
- The sudden shift to online education might not be a totally negative development despite the several disadvantages that students cited.
I. INTRODUCTION
The COVID-19 pandemic has impacted medical education significantly. Students were sent home and many schools were forced to shift their teaching, almost overnight, from face-to-face encounters to virtual, online delivery, in many cases without having had substantial previous experience with this mode of delivery. This disruption spanned the clinical and preclinical years. In previous events, researchers prioritised the synthesis of available evidence in terms of training medical students to respond and mitigate the effects of different types of disasters (Ashcroft et al., 2020). While there was more attention to find solutions for medical education in difficult settings (McKimm et al., 2019), including few examples that came to light after the outbreaks of H1N1 and H5N1 influenza, the severe acute respiratory syndrome (SARS) (Patil et al., 2003), and most recently, Ebola (Woodward & McLernon-Billows, 2018), there is paucity of literature that could inform adaptations of medical education methods during or post disasters, conflicts, or outbreaks. Recent articles have reflected on these changes and challenges and have suggested means of responding to the new reality, and offered advice on adopting new tools to ensure the best possible delivery of the curriculum (Daniel, 2020; Fawn et al., 2020; Liang et al., 2020; Ross, 2020; Sandars et al., 2020).
A recent meta-analysis that compared offline and online undergraduate medical education (under normal circumstances) revealed either no difference in outcomes on knowledge tests or a slightly higher performance for those who received online learning (Pei & Wu, 2019). In addition, a review of the literature showed that the adoption of E-Learning, in comparison with mostly traditional and other means of learning, expands access to education and increases the pool of faculty, in low resource settings (Frehywot et al., 2013). These data suggest that for preclinical education, there might not be a major negative impact of moving to online learning. It should be noted, however, that the situation brought about by the COVID-19 pandemic, which necessitated an abrupt transition to online education, may not be identical to that in which online delivery was a, planned and well-designed method to deliver at least part of the curriculum of the medical school; thus, the outcomes in knowledge acquisition during the recent COVID-19- forced transition to online teaching cannot be confidently predicted (Lim et al., 2009).
The American University of Beirut Faculty of Medicine (AUBFM), which follows the American model of medical education, suspended all in-person physical classes and assessments for years 1 and 2 on March 12, 2020. Thus, faculty, students and staff had to shift to online learning practically immediately. In this paper, we report our experience with this forced transition to online learning, specifically addressing Year 1 and 2 students’ perceptions of and response to it, and examining whether this transition affected their knowledge acquisition as reflected by their performance on written examinations.
II. METHODS
This is not a research study, as confirmed by our Institutional Review Board (IRB), since our purpose was to describe our experience with the delivery of the medical school curriculum after the sudden shift to online education, and whether that affected the students’ performance on their examinations and their evaluation of the courses. This was neither a planned intervention nor a systematic approach to test a specific hypothesis.
A. Setting
We analysed data from Year 1 and 2 classes of medical students who took the same courses either online (2019-2020) or face-to-face (2018-2019). We examined student performance in two courses, one for first year medical students (115 Class of 2022 students as face-to-face in 2018-2019 versus 118 Class of 2023 students as online in 2019-2020) entitled The Blood, and the other for second year medical students (114 Class of 2021 students as face-to-face in 2018-2019 versus 115 Class of 2022 students as online in 2019-2020) entitled Human Development and Psychopathology. Both courses are integrated modules that cover the histology, pathology, physiology, biochemistry, pathophysiology, pharmacology of the blood and lymphatic system and of neuropsychiatry, as well as the clinical, social, ethical, and behavioural aspects of related disorders.
Both courses extend over four weeks and end with a final summative examination. The main teaching activities consist of lectures and team-based learning (TBL) sessions, along with other small or large group discussions sessions dealing with epidemiology, evidence-based medicine, medical ethics, and social determinants of health relevant to the medical topics being covered.
The transition to online learning with the current medical students (2019-2020) was as follows: The didactic lectures were delivered either as asynchronous Voice-Over-PowerPoint (VOP) recordings or synchronous live lectures using Webex, which were recorded live. These recordings were made available to students on Moodle, the learning management system used at AUBFM. Faculty chose which of the two modes best suited them. As for the TBLs and group discussion sessions, they were run live using either Webex or Zoom applications. The latter was particularly appropriate for TBL sessions as it allowed virtual breakout rooms for team discussions.
The Respondus lockdown browser, with camera recordings serving as a virtual proctor, was adopted for written assessments, which included the individual Readiness Assurance Tests (i-RAT) of the TBLs as well as the final examinations. All these assessments utilise single-best answer multiple choice questions. Previous to the transition to online learning in 2018-2019, all i-RATs and group-RATs (g-RATs) were paper-based with physical proctoring, while the final course examinations, which used single best answer multiple choice questions, were computer-based, and were run on American University of Beirut (AUB) secure computers, also with physical proctoring.
Prior to COVID-19, final examinations were a hybrid of locally generated questions and National Board of Medical Examiners (NBME) customised examinations. During the COVID-19 pandemic, NBME examinations were not available and final examinations were totally locally generated. With regard to TBL’s, during the online transition, no g-RATs were performed due to our inability to ensure their security; thus, automatic feedback, which was an integral part of the TBL process, was not possible, and was replaced by a brief review of the questions by the TBL preceptor.
In addition, and in order to reduce the potential for cheating and communication among students, we reduced the time allotted for final examinations from 1.2 minutes per question to 1 minute per question. Reducing the on-line time during examinations was also done in order to minimise connectivity problems that arise due to the poor internet infrastructure in Lebanon and due to the frequent cuts in electricity.
B. Students’ Attitudes
At AUBFM, at the end of every course, students are expected to anonymously fill an online course evaluation form. This form includes twelve statements on various aspects of the course with which the students express a level of agreement (Sup. Table 1). Scores are assigned to their responses as follows: 1: Strongly disagree, 2: Disagree, 3: Neither agree nor disagree, 4: Agree, 5: Strongly agree. One of the items on that form (# 4) addresses the effectiveness of the teaching methods. An overall course rating is calculated as the average score for all 12 items. We compared the scores on both item #4 and the overall rating for the course given online (2019-2020) for both Year 1 and 2 medical students with the scores for the same course when delivered face-to-face (2018-2019).
Due to the lack of survey items that are specifically tailored to online teaching in the regular course evaluation forms, we asked the students to respond to 3 additional open-ended questions. This part was administered only to the current (2019-2010) first year medical students who had completed the Blood course and were the following:
1) In your opinion, what are the advantages of online teaching and learning over face-to-face teaching and learning?
2) In your opinion, what are the disadvantages of online teaching and learning over face-to-face teaching and learning?
3) Please provide suggestions for improvement of the online teaching and learning process.
C. Performance on the Final Examinations
Overall performance in the same courses was compared between the current classes (online) and the previous year’s classes (face-to-face). Thus, for the current Year 1 class (Class of 2023) the comparator class was the current Year 2 class (Class of 2022), and for the latter the comparator class was the current Year 3 class (Class of 2021). We restricted the comparisons of final examination grades to performance of the various classes on the locally generated questions.
In order to ensure that any two classes being compared did not differ in terms of academic or cognitive abilities, we also compared the performance of the current and the previous year’s classes according to: 1) their scores on the Medical College Admissions Test (MCAT) taken prior to admission to medical school; and 2) their overall grades in other courses that were given face-to-face during the current year (i.e. in the earlier part of the 2019-2020 academic year); these courses included one entitled Cellular and Molecular Basis of Medicine (CMM) given during year 1, and another entitled The Kidney and Urinary System given during year 2; these were the first courses to be delivered during the current year.
In comparing grades and scores on courses and examinations, we took into account the passing standards set for each. At AUBFM, we use criterion based absolute passing grades for every assessment. For written assessments such as final examinations using multiple choice questions, the Angoff method is utilised to set the passing grade. Similarly, the passing grade for a course is calculated based on the weighting of the individual assessment tools in that course. Thus, for any two courses or examinations that we compared, we first did the analysis using the raw grades, and then, when needed, we also compared the adjusted grades after equalising the passing grades.
D. Data Analysis
For the three survey questions, answers were downloaded on excel for systematic and iterative thematic analysis. Answers were manually coded by one of the authors. The compiled codes were then discussed, compared and consolidated into themes by two of the authors over 3 meetings. The focus was on main themes, commonalities and conflicting views of participants, and relationships between themes. Findings were tabulated with relevant quotes. For the evaluation scores and performance on exam, data were available on excel and statistical comparisons were conducted using the Student’s unpaired t-test.
III. RESULTS
A. Students’ Attitudes
Twenty-six of the 118 current medicine one student filled the survey, and four more sent an email to the course coordinator, the response rate is hence 24.5%. Several themes emanated for each of the three questions especially concerning disadvantages of online learning; these are tabulated in Table 1 with representative quotes. The main advantages of online learning were the time flexibility with asynchronous learning coupled with better overall well-being as a result of staying at home. VOPs were valued because they allowed students to control their learning pace.
As for disadvantages, there were several. These included: the loss of motivation, the potential for procrastination, the problems arising from a bad internet connection leading to greater internet costs, inadequacy of the home environment for learning, less interaction with teachers and students, paucity of immediate feedback, loss of hands on experiences, and struggles because of the faculty’s deficiencies in the area of information technology in general, and in online teaching, in particular.
The students made several suggestions to improve the process, and these included proposals for faculty development, and provision of better technical support and knowhow. In addition, they proposed to decrease or cancel synchronous lectures and provide all didactic lectures as VOPs, to be followed by synchronous online sessions for questions and feedback. They also proposed to imbed questions within the VOPs to stimulate students to think (akin to audience response polls used in live lectures), as well as forum discussions to increase interactions with peers and faculty. Students also insisted that they receive more detailed feedback on their performance on examinations and i-RAT questions.
Despite the many disadvantages cited and the clear room for improvement for online teaching and learning, the overall course ratings as well as the evaluation of teaching for the online courses were not different from their face-to-face counterparts (Tables 2 and 3).
|
Survey question |
Theme |
Quote |
|
Advantages of online teaching and learning in comparison to face to face teaching and learning |
Time flexibility with asynchronous learning |
“Better scheduling that allows us to sleep and rest at night in order to wake up better prepared to ace those PowerPoints” (S9) “Easier to manage our time” (S18) |
|
Control of learning pace with VOP |
“Being able to speed through slides/concepts we already understood and pausing and replaying concepts that we have trouble with makes the whole learning process a lot more efficient and focused” (S27) |
|
|
More wellbeing |
“Less time to commute which allows more time to rest and take care of oneself” (S9) “Having a very healthy diet with my family in the village” (S12) “The [exam] performance is better and stress in minimal” (S23) |
|
|
Disadvantages of online teaching and learning in comparison to face to face teaching and learning |
Potential for procrastination and loss of motivation |
“Less motivation, harder to follow the schedule, requires strong time management skills” (S5) “Face to face teaching helps me organize my day better” (S4) “Being at university with other students around studying during the day motivated me” (S26) |
|
Bad internet connection |
“Internet connection in our country is not stable to hold a class or an exam, so we are resorting to 3g/4g. This leads to a lot of extra expense” (S3) “Time consuming” (S2) and “Sessions would run for more than their original allocated time” (S3) “Longer exams might coincide with the times of the electricity shut offs. This would automatically freeze Respondus and the student will have to restart their computer and so on. Although we are given extra time this adds a lot of stress to an already stressful situation” (S19) “Asking questions are much more difficult and needs much more time” (S7) “WebEx needed a stronger Wi-Fi in some sessions which leads to a harder way to grasp the information” (S18) “The internet connection everywhere in Lebanon is not the best, sometimes we have trouble listening. Sometimes it also gets really crowded when everyone wants to talk at the at the same” (S21) |
|
|
Home environment less conducive to learning |
“Not everybody has the privilege of adjusting their environments to their liking, whether that be because of their dog barking or their family members not respecting their study time” (S28) “This experience helped my appreciate how much I concentrate better in the library” (S9)
|
|
|
Loss of interaction with teachers |
“No direct interaction, harder to communicate directly with professors” (S2) “Face to face interaction was lost: no clues to non-verbal clues, no gestures seen” (S17) “It is true that we can always email the doctors for any additional questions but that does not compare to in person interactions” (S19)
|
|
|
Loss of interaction with students |
“not being able to interact with my friends” (S12) “Students lose their social skills as they interact less with each other-more into introversion” (S17) “You feel there is a barrier between you and the students” (S17) |
|
|
Lack of immediate feedback |
“One problem is during exams not being able to see my mistakes” (S15) “Not correcting our exam and not seeing our mistakes was a huge disadvantage for the online learning” (S18) “Restricting questions to only emails” (S11) and “some professors don’t respond to emails” (S16) and “the response may be delayed” (S29) |
|
|
Loss of hands on experiences |
“No hands-on experience for courses like clinical skills” (S3) “Mainly missing out on clinical skills” (S22) |
|
|
Faculty’s lack of IT knowhow or experience |
“Professors have different abilities and effectiveness in knowing how to do a VOP/online lecture” (S11) “Most Drs. don’t know how to use zoom or WebEx” (S6) “Many instructors are not technically inclined or are outright aversive to it” (S13) “So much time is wasted on technical issues” (S19) “Professors sometimes don’t see the raised hands and sometimes it doesn’t even work. In some lectures we had to wait for the professor to give us access, so we spent time waiting while they didn’t see that some people are trying to access the lecture” (S21) “One of the disadvantages is using the live WebEx sessions. Some professors are losing their recordings, others have a poor connection” (S23) |
|
|
Effect on faculty’s teaching skills |
“Some professors …just read instead of teaching” (S7) “Many professors are not exactly cooperative in terms of explaining mainly because they read their PowerPoints” (S23) “Can’t explain a topic and be passionate about it if talking to a screen or microphone” (S23) |
|
|
Suggestions to improve the current online teaching |
Technical support and knowhow |
“Train the staff on the proper way of utilising the platforms” (S2) “Make IT staff more readily available to help instructors” (S16) “Agree on one way to give the lecture via WebEx as some professors used WebEx team, where we had to ask permission for access, and it was kind of chaotic. It would also be better if the professor agreed on one way to have the questions asked to avoid interruptions and multiple people talking at the same time” (S21) |
|
More VOPs and less WebEx for lectures |
“I think VOP is a much safer option and a less tiring one” (S23) “Revert from live WebEx sessions to VOP” (S3) |
|
|
More interaction and immediate feedback |
“Open forums for discussion” (S3) “Adding analytical questions in PowerPoints” (S9) “See exams and mistakes” (S15) “If the professors want to use WebEx … then they should allow questions at all times and not only at the end of the session” (S11) “Include small assessment questions (clicker like questions) at the end of each major concept so that the students can assess their understanding” (S19) “Recording voice over PowerPoint for lectures, with every group of lectures followed by a WebEx session where the professor answers questions” (S24) “Review/Q&A session once a week” (S25) |
Table 1. Themes Generated from the Three Survey Questions with Selected Representative Quotes
VOP: Voice Over PowerPoint
|
Medicine class of |
2022 |
2023 |
P-value |
|
Academic Year 1 |
2018-2019 |
2019-2020 |
|
|
Number of students |
115 |
118 |
|
|
|
Baseline performance |
||
|
MCAT scores |
509±6 |
510±6 |
0.119 |
|
Class average on the final exam of the CMM course |
82.6±6.1 |
84.3±7.4 |
0.011 |
|
Passing grade for the final exam of the CMM course |
64.1 |
64.7 |
|
|
Adjusted grade for the final exam of the CMM coursea |
83.2±6.1 |
84.3±7.4 |
0.065 |
|
|
Performance in The Blood course |
||
|
Course delivery |
Face to Face |
Online |
|
|
Number of questions on the final exam |
50 |
77 |
|
|
Class average on the final exam |
83±9 |
81±9 |
0.043 |
|
Passing grade for the final exam |
65 |
61 |
|
|
Adjusted grade for the final exama |
83±9 |
85±9 |
0.091 |
|
|
Student Evaluation of The Blood Course |
||
|
Rating of teaching methods |
4.0±0.8 |
4.0±1.0 |
0.920 |
|
Overall course rating |
4.0±0.7 |
4.1±0.8 |
0.754 |
Table 2. Comparison of Performance of Year 1 Students in Various Courses and Examinations and Their Evaluation of the Blood Course
Data are presented as Mean ± Standard Deviation
P-values were generated by Student’s unpaired t-test
MCAT: Medical College Admissions Test; CMM: Cellular and Molecular Basis of Medicine
aadjusted after equalizing the passing grades on the examinations in the 2 different years
|
Medicine class of |
2021 |
2022 |
P-value |
|
Academic Year 2 |
2018-2019 |
2019-2020 |
|
|
Number of students |
114 |
115 |
|
|
|
Baseline performance |
||
|
MCAT scores |
509±5 |
509±6 |
0.842 |
|
Class average on the final exam of the CMM course |
83.8±6.4 |
82.6±6.1 |
0.156 |
|
Passing grade for the final exam of the CMM course |
65.3 |
64.1 |
|
|
Adjusted grade for the final exam of the CMM coursea |
82.6±6.4 |
82.6±6.1 |
0.455 |
|
Performance on the final exam of The Kidney course |
78.1±7.9 |
78.7±7.2 |
0.558 |
|
Passing grade for the final exam of The Kidney course |
62.2 |
62.3 |
|
|
|
Performance in the Human Development and Psychopathology course |
||
|
Course delivery |
Face to Face |
Online |
|
|
Number of questions on the final exam |
45 |
75 |
|
|
Class average on the final exam |
83.7±7.4 |
83.5±6.8 |
0.892 |
|
Passing grade for the final exam |
68.0 |
64.8 |
|
|
Adjusted grade for the final exama |
83.7±7.4 |
86.7±6.8 |
0.002 |
|
|
Student evaluation of the Human Development and Psychopathology course |
||
|
Rating of teaching methods |
4.2±0.9 |
4.1±0.9 |
0.426 |
|
Overall course rating |
4.3±0.7 |
4.1±0.8 |
0.251 |
Table 3. Comparison of Performance of Year 2 Students in Various Courses and Examinations and Their Evaluation of the Human Development and Psychopathology Course
Data are presented as Mean ± Standard Deviation
P-values were generated by Student’s unpaired t-test
MCAT: Medical College Admissions Test; CMM: Cellular and Molecular Basis of Medicine
aadjusted after equalizing the passing grades on the examinations in the 2 different years
B. Performance of Students in the Courses and Examinations
As shown in Tables 2 and 3, there were no statistically significant differences in the MCAT scores between any two classes that were compared. The performance of the Year 1 students on the CMM course during the current academic year (online) was higher than that of students during the previous year (face-to-face); however, the passing grade for the two courses was slightly different. When the passing grades were equalised, there was no longer a difference between the two classes. Similarly, there was no difference in the performance of the Year 2 students on either the CMM course they took in Year 1, or on The Kidney and Urinary System course between the current class and the previous year’s class (all face-to-face).
With regard to The Blood course, the grade on the final examination was significantly lower for current students (online) relative to their predecessors (face-to-face); however, the passing grades on these examinations were different, with the current year’s examination having a lower passing grade than last year’s. When the passing grades were equalised, there was no longer a difference in the performance on the final examination.
The performance of the students in the Human Development and Psychopathology course’s final examination was almost identical in the online group compared with their predecessors (all face-to-face). Interestingly, the passing grade on this year’s examination was lower than that on last year’s examination, such that when the passing scores were equalized, the current class had better performance on the final examination than last year’s class.
IV. DISCUSSION
Medical education scholars have been increasingly disseminating opinions about sudden transitioning to online education to COVID-19 and the adaptations that are being implemented. Few studies have documented the actual institutional experiences, the perspectives of students, and the lessons learned in different medical courses or curricula such as TBL (Gaber et al., 2020), anatomy (Srinivasan, 2020) and continuing medical education in obstetrics and gynaecology (Kanneganti et al., 2020). Only one report from Wuhan, China, evaluated nursing interns’ outcomes on emergency medicine theoretical and practical examination scores (Zhou et al., 2020). The current paper is the first to examine the impact of this abrupt transition to online learning, which occurred in numerous countries worldwide, on the performance of our medical students in knowledge-based examinations. It reveals that the sudden shift to full online learning that our medical school had to adopt did not have a negative influence on the students’ knowledge acquisition as judged by their performance on final examinations. It also did not affect their overall reception and evaluation of the courses. These results are particularly interesting and important considering the many disadvantages that the students cited in relation to the online delivery of the courses.
Many of the limitations and disadvantages of online education cited by students had to do with technical and infrastructural matters and with faculty know-how and IT support. These are problems that can, theoretically, be easily remedied. The more challenging, however, limitations had to do with the process of learning, what facilitates or hampers it, the students’ ability to self-regulate and to motivate themselves, the negative impact of isolation, loss of socialisation and interaction with peers and faculty, and the almost total lack of hands-on experiences.
These limitations did not affect the students’ ability to achieve learning, at least in the domain of knowledge acquisition and application. It is clear that students in the three classes that were examined had, at baseline, a similar level of achievement meaning that any differences in student performance in the courses that were given online this year cannot be ascribed to differences in the academic performance or ability of the students. Therefore, the lack of difference in performance between classes taking the course online versus those taking it face-to-face suggests a consistency in performance that was not affected adversely by the sudden transition to online learning.
One reason for this lack of difference in performance between online and face-to-face delivery of the courses may be that the outcomes that were being sought and assessed were essentially knowledge acquisition and knowledge application. This agrees with the overall results of multiple studies that compared online vs offline learning in medical school, and which, in fact, tended to favour online learning (Pei & Wu, 2019). Indeed, even before our sudden shift to total online education, many of our students had adopted their own approaches to achieve the knowledge learning outcomes. Even though lectures were not available online, attendance at face-to-face lectures (which was not mandatory) was never complete, and for the majority of students, the rate of attendance ranged between 25% and 75% (unpublished data). In fact, the students indicated that they depended instead on notes and voice recordings made during the lecture that were shared by their classmates or predecessors, and that they used several Web-based resources. In contrast, attendance at TBL exercises and other interactive and small group sessions is mandatory at our school, and students uniformly participated in them, as they did in the online Zoom-based sessions. Thus, our students were probably well prepared for this sudden shift. In line with this view, Ferrel and Ryan (2020), in a recent editorial on the impact of COVID-19 on medical education, predicted that many medical students in their didactic years may perceive little change in their study schedule, since many of them already use outside resources and watch school lectures after they have been presented.
The lack of significant differences in scores and attitudes may also attest to our – and indeed all – medical students’ resilience and adaptability to difficult situations, for they are high-achieving and resourceful students who have been selected from among an exceedingly competitive group of applicants, and likely have the cognitive powers and non-cognitive qualities to meet such challenges. Ferrel and Ryan (2020) also emphasised the need for medical students to adapt and be innovative during the pandemic, and to devise ways by which they can exhibit their skills, work ethics and teamwork. In fact, one of the advantages of the online shift that our students cited was the flexibility this approach afforded them in managing their time, setting their schedules, controlling their pace of learning and achieving better self-care. Nevertheless, some of them found it challenging to do so, and to regulate their environment and motivate themselves; rather, they seemed to require external cues or assistance to get into a learning mode, and found difficulty in establishing boundaries between work and home, as suggested recently by Rose (2020). In this context, it is noteworthy that our students preferred asynchronous to synchronous learning, and this is consistent with Daniel’s recommendation to use this approach because it gives teachers “flexibility in preparing learning materials and enables students to juggle the demands of home and study” (Daniel, 2020).
Our findings also raise questions about certain assumptions regarding student learning and the optimal teaching approaches for knowledge-based objectives, such as the value and benefits of face-to-face interactions among students and with faculty in a didactic context. Our results suggest that students can achieve these knowledge objectives without the personal interaction and contact with faculty. This, of course, does not address the non-cognitive learning outcomes that might be negatively affected by pure online learning. As summarised by Fawn et al. (2020), while content may be covered well in such abrupt transitions to online learning, we cannot be sure that the valuable non-cognitive learning that happens as a result of the “social activity, the relationship-building, the problem-solving, the dialogue and generation of ideas and the students’ own discovery of other content that has not been pre-defined by the teacher” has been achieved.
We cannot make definite, long-term conclusions from this single account that is restricted to 2 courses in the preclinical years, a brief period of time, and one institution, and a low response rate for the survey questions, but the results are encouraging, and may have implications for educational practice. The lack of decline in cognitive performance may suggest that the sudden shift to online education might not be a totally negative development. If our findings are reproduced or generalised, one can use them to validate what progressive medical educators have been advocating for years, that: online educational technology must change the way we educate our students; didactic lecturing should give way to flipped classrooms; and valuable teacher time must be expended to help students apply knowledge rather than to simply transfer information in scheduled lectures. Quoting Ezekiel Emanuel (2020), who in a recent article stated that the reconfiguration of medical education, fuelled by online educational technology, seemed inevitable, Wolanskyj-Spinner (2020) suggested that the coronavirus epidemic appears to be an inflection point that is forcing a disruption in how we teach medicine. At AUBFM, we have long pressed the faculty who teach medical students to record their lectures and use the scheduled class time thus saved to implement flipped classrooms, employing small-group-based, problem-solving and interactive sessions. While many responded, many also hesitated, objected, and even resisted. The following two additional comments provided by two students illustrate their frustration with the resistance of faculty and their hopes to move in that direction:
“I really hope we can make online learning standard coming out of this phase … There was an attempt a few years ago but many instructors refused to be recorded or to fiddle with computers; we must seize the opportunity now.”
“Please never stop recording lectures, regardless of the status of live classes!”
Ahmed et al. (2020) recently reported that during the 2003 SARS epidemic in China, novel online problem-based learning techniques had to be implemented in one medical school that proved to be so popular that they were applied as part of the regular curriculum in later years. We believe that medical educators can harness the current disruption in how we teach medical students, and make use of to implement novel and sound educational practices and adopt a wide variety of valid approaches and tools that, otherwise, might have been resisted by unwilling individuals with entrenched ideas.
V. CONCLUSION
In conclusion, rapid transition to online learning did not affect student knowledge acquisition negatively. As such, the sudden shift to online education might not be a totally negative development and can be harnessed to drive a more progressive medical education agenda. These results are particularly important considering the several disadvantages that the students cited in relation to the online delivery of the courses.
Notes on Contributors
Nathalie Zgheib developed the concept, collected and analysed data, and wrote the first draft of the manuscript. Ahmed Ali also developed the concept, performed the literature review, and revised the manuscript write-up. Ramzi Sabra also developed the concept, collected and analysed data, and revised the manuscript write-up. The three authors read and approved the final version of the manuscript.
Data Availability
The data that support the findings of this manuscript are available from the corresponding author upon reasonable request.
Ethical Approval
This is a report of experience with educational practices. It was confirmed by our Institutional Review Board (IRB) that the activities described in this article do not constitute human subject research.
Acknowledgments
The authors wish to thank AUBFM faculty and medical students for their support, diligence and flexibility during the COVID-19 pandemic.
Funding
This study did not receive any funding.
Declaration of interest
The authors do not have any conflict of interest to declare.
References
Ahmed, H., Allaf, M., & Elghazaly, H. (2020). COVID-19 and medical education. The Lancet Infectious Diseases, 20(7), 777-778. https://doi.org/10.1016/S1473-3099(20)30226-7
Ashcroft, J., Byrne, M. H. V., Brennan, P. A., & Davies, R. J. (2020). Preparing medical students for a pandemic: A systematic review of student disaster training programmes. Postgraduate Medical Journal, Advance online publication. https://doi.org/10.1136/postgradmedj-2020-137906
Daniel, S. J. (2020). Education and the COVID-19 pandemic. Prospects, 49, 91-96. https://doi.org/10.1007/s11125-020-09464-3
Emanuel, E. J. (2020). The inevitable reimagining of medical education. Journal of the American Medical Association, 323(12), 1127-1128. https://doi.org/10.1001/jama.2020.1227
Fawn, T., Jones, D., & Aitken, G. (2020). Challenging assumptions about “moving online” in response to COVID-19, and some practical advice. MedEdPublish, 9(1), 83. https://doi.org/10.15694/mep.2020.000083.1
Ferrel, M. N., & Ryan, J. J. (2020). The impact of COVID-19 on medical education. Cureus, 12(3), e7492. https://doi.org/10.7759/cureus.7492
Frehywot, S., Vovides, Y., Talib, Z., Mikhail, N., Ross, H., Wohltjen, H., Koumare, A. K., & Scott, J. (2013). E-learning in medical education in resource constrained low- and middle-income countries. Human Resources for Health, 4(11), 4. https://doi.org/10.1186/1478-4491-11-4
Gaber, D. A., Shehata, M. H., & Amin, H. A. A. (2020). Online team-based learning sessions as interactive methodologies during the pandemic. Medical Education, 54(7), 666-667. https://doi.org/10.1111/medu.14198
Kanneganti, A., Lim, K. M. X., Chan, G. M. F., Choo, S. N., Choolani, M., Ismail-Pratt, I., & Logan, S. J. S. (2020). Pedagogy in a pandemic – COVID-19 and virtual continuing medical education (vCME) in obstetrics and gynecology. Acta Obstetetricia et Gynecologica Scandinavica, 99(6), 692-695. https://doi.org/10.1111/aogs.13885
Liang, Z. C., Ooi, S. B. S., & Wang, W. (2020). Pandemics and their impact on medical training: Lessons from Singapore. Academic Medicine, 95(9), 1359-1361. https://doi.org/10.1097/ACM.0000000000003441
Lim, E. C., Oh, V. M., Koh, D. R., & Seet, R. C. (2009). The challenges of “continuing medical education” in a pandemic era. Annals of Academic Medicine Singapore, 38(8), 724-726.
McKimm, J., Mclean, M., Gibbs, T., & Pawlowicz, E. (2019). Sharing stories about medical education in difficult circumstances: Conceptualizing issues, strategies, and solutions. Medical Teacher, 41(1), 83-90. https://doi.org/10.1080/0142159X.2018.1442566
Patil, N. G., Chan, Y., & Yan, H. (2003). SARS and its effect on medical education in Hong Kong. Medical Education, 37(12), 1127-1128. https://doi.org/10.1046/j.1365-2923.2003.01723.x
Pei, L., & Wu, H. (2019). Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Medical Education Online, 24(1), 1666538. https://doi.org/10.1080/10872981.2019.1666538
Rose, S. (2020). Medical student education in the time of COVID-19. Journal of the American Medical Association, 323(21), 2131-2132. https://doi.org/10.1001/jama.2020.5227
Ross, D. (2020). Creating a “quarantine curriculum” to enhance teaching and learning during the COVID-19 pandemic. Academic Medicine, 95(8), 1125-1126.
Sandars, J., Correia, R., Dankbaar, M., de Jong, P., Sun Goh, P., Hege, I., Oh, S., Patel, R., Premkumar, K., Webb, A., & Pusic, M. (2020). Twelve tips for rapidly migrating to online learning during the COVID-19 pandemic. MedEdPublish, 9(1), 82. https://doi.org/10.15694/mep.2020.000082.1
Srinivasan, D. K. (2020). Medical students’ perceptions and an Anatomy teacher’s personal experience using an e-learning platform for tutorials during the Covid-19 crisis. Anatomical Sciences Education, 13(3), 318-319. https://doi.org/10.1002/ase.1970
Wolanskyj-Spinner, A. (2020). COVID-19: The global disrupter of medical education. ASH Clinical News, https://www.ashclinicalnews.org/viewpoints/editors-corner/covid-19-global-disrupter-medical-education/
Woodward, A., & McLernon-Billows, D. (2018). Undergraduate medical education in Sierra Leone: A qualitative study of the student experience. BMC Medical Education, 18(1), 298. https://doi.org/10.1186/s12909-018-1397-6
Zhou, T., Huang, S., Cheng, J., & Xiao, Y. (2020). The distance teaching practice of combined mode of massive open online course micro-video for interns in emergency department during the COVID-19 epidemic period. Telemedicine Journal and E-Health, 26(5), 584-588. https://doi.org/10.1089/tmj.2020.0079
*Ramzi Sabra
Department of Pharmacology and Toxicology,
Faculty of Medicine,
American University of Beirut,
PO. Box 11-0236, Riad El Solh,
Beirut, Lebanon
Tel: +961-1-350000 Ext: 4848
Email: rsabra@aub.edu.lb
Submitted: 20 July 2020
Accepted: 30 September 2020
Published online: 13 July, TAPS 2021, 6(3), 108-110
https://doi.org/10.29060/TAPS.2021-6-3/PV2369
Kimberly Hires1 & Colleen Davis2
1Lewis College of Nursing and Health Professions, Georgia State University, United States of America; 2Leadership Development, Vuselela Davis, South Africa
I. INTRODUCTION
Historically, health professional education has focused on the development of clinical expertise over leadership skills that enable practitioners to lead dynamic teams who can adapt and pivot rapidly in a crisis. Clinical acumen and the ability to lead effectively are not mutually exclusive within healthcare systems. Leadership development is vital for health professionals as it allows them to lead patients and health systems, adapt to rapidly changing healthcare environments, and elicit optimal performance from their teams—all of which lead to improved health outcomes. The COVID-19 crisis highlights an opportunity to innovate health professional education to create practitioners who can treat and lead with excellence.
In December 2019, the Wuhan Municipal Health Commission reported four cases of pneumonia of an unknown origin. The cluster of cases were the first sign of COVID-19. COVID-19 is caused by a novel coronavirus that can spread from person to person. Within six months, the virus spread to 231 countries and infected over 13 million people worldwide. In attempts to slow the spread of the virus, countries issued emergency shutdowns, schools were closed, global travel was prohibited, and every industry was affected. One industry most affected by COVID-19 is the healthcare industry. Healthcare infrastructures are facing unprecedented challenges to meet the demands for care related to COVID-19. Providers are battling burnout, insufficient supply of personal protective equipment, depression, anxiety, job dissatisfaction and in some cases increased rates of suicide (Greenberg et al., 2020). To identify the contributing factors to challenges faced by health professionals during COVID-19, leaders must go to the root: health professional education.
Current health professional education competencies prioritize the development of hard skills that focus on clinical performance or evidence-based practice over the development of soft skills that facilitate building healthy interpersonal relationships, self-awareness, communication, leadership skills and effective coping (Albarqouni et al., 2018). Health professions encompass art and science. Current health professional education rewards the science of healthcare but starves the art of leadership. The COVID-19 pandemic, has created a collective trauma within the global community for which current leaders are not equipped to respond (Greenberg et al., 2020). The evidence for COVID-19 is constantly changing and leaders do not have the confidence and care algorithms to which they have grown accustomed. Due to COVID-19, health care workers worldwide have experienced an increase in depression, anxiety, and other forms of psychological distress. Health professionals already experience higher levels of burnout and job dissatisfaction than other professions; COVID-19 has amplified existing challenges for healthcare leaders who were struggling with employee recruitment and retention prior to the global pandemic.
As COVID-19 becomes a critical component of the world’s new normal, this is the optimal time for health professional education to innovate and prepare graduates who can lead in the midst of the new normal. This paper draws on experience of the two authors and their work with students enrolled in health professional programmes at the initial level and the specialist level, as well as the post-academic level in the United States and South Africa. This paper aims to introduce a new model of leadership development informed by over three decades of observations from combined experiences in health professional education, hospital learning and development, and leadership coaching.
II. DISCUSSION
Top down, traditional styles of leadership with an emphasis on self-sacrifice do not have a future in 21st century healthcare leadership. Leaders who are highly aware, connected, and genuinely compassionate experience success in productivity, high performing teams, cost effectiveness, strategy, innovation and employee retention. Just as health professional education relies on evidence-based practice, the Human-based leader (HBL) Model was developed to explain how effective leadership skills are developed. The HBL model utilizes an ecological framework. Ecological systems theory was developed by Urie Bronfenbrenner and posits that development is guided by interactions between an individual and the surrounding environment; this interaction populates a system (Bronfenbrenner, 1979). Bronfenbrenner’s original system is comprised of four systems represented as four concentric circles: the individual/microsystem (the core), mesosystem (second sphere), exosystem (third sphere), and macrosystem (fourth sphere) (Bronfenbrenner, 1995).
The HBL is comprised of three concentric circles. At the core is phase I. The goal of phase I is the development of self-awareness. The microsystem (the individual/leader) is housed within this sphere. The next sphere is phase II which houses the mesosystem (relationships with others such as family, friends, team members, peers) and the exosphere (additional factors related to the organization including patients and the community). In phase II leaders develop an awareness of others. The third sphere, phase III, houses the macrosystem (factors related to the profession, population, values, and cultural customs). Development of this phase allows the health professional leader to contribute to the building of a global community. The HBL makes the following assumptions: (1) Leadership development is a dynamic process that is influenced by exchanges between the individual (the leader) and the environment. (2) Leadership development is a continuous process. (3) Leadership success is not limited to job related competencies. Success includes healthy organizational culture, employee job satisfaction, recruitment, retention, customer/client satisfaction, and work-life balance as well as profit and loss.
Historically, health professional education focuses on team development and neglects teaching students how to understand their own experiences and worldview. Engaging in reflective practices are vital for professional identity development, however, current practices limit the reflection to clinical experiences (Wald, 2015). This approach ignores the very rich and varying life experiences students bring with them into a health professional programme. These life experiences follow students well into practice. Healthcare leaders with decades of experience are often surprised to find how influential their worldview is on patient care and working within teams. In this phase, it is vital for the individual to be able to answer, “Who am I?” beyond the professional identity. As individuals reflect on who they are, they can identify triggers, motivators and fears. Seeing the Self and helping a leader understand the Why behind behaviour is fundamental to healing and growth for the leader and the organization. Leaders who are self-aware in a crisis, such as a pandemic, can move dynamically as the environmental norms shift.
Current practices in health professional education emphasizes teamwork, however, by ignoring phase I, health professional educators make a fallible assumption that self-awareness is not vital to working effectively in teams. If individuals are unable to see the humanness in themselves (self-awareness) to value their own stories, challenges, and uniqueness, then they will fail to see it in others (peers, staff). In this phase, leaders gain a clear understanding of how to connect with and motivate each member of the team for optimal performance and retention. Failure to successfully achieve this phase results in poor performance, increased risk for medical errors, and high turnover.
Once leaders have an awareness of self and an appreciation for others, then they can graduate to the macrosystem or global sphere. The COVID-19 pandemic has illustrated the power of globalization. Within six months, healthcare systems experienced a global rate of infection that needed a swift, fluid, innovative and agile response. It is imperative that health professional education helps students and future leaders develop a global paradigm that sees beyond local hospitals and communities. A healthy worldview facilitates an easier transition into a global macrosystem.
The HBL can be adapted and implemented at various levels of health professional education and practice. It can be incorporated as learning modules in existing courses at the initial level and as a formal coaching programme at the specialist and post-academic levels. At the initial level of health professional education, the HBL was implemented with students in their final semester of a health professional (baccalaureate) programme at a research institution in the United States. The model was integrated into a leadership and management course as learning modules, case-studies, and self-development activities to equip students with skills needed to successfully progress through phases I, II, and III. At the specialist level, health professional students in the United States benefited from a formal coaching programme comprised of individual and group coaching sessions delivered over 12 weeks. At the post-academic level, the HBL model was implemented with practitioners in the United States and South Africa. At the post-academic level, practitioners benefit from a formal, customised coaching programme comprised of individual coaching sessions or a combination of individual and group coaching sessions delivered over 12 to 16 weeks. The greatest challenge with implementing the HBL at the specialist and post-academic levels is facilitating the unlearning of maladaptive leadership behaviours that lead to unhealthy organizational culture.
III. CONCLUSION
As demands for quality health care increase, health professional education is charged with meeting the supply. COVID-19 has provided a unique disruption for global health professional education to pivot from a rigid, process-driven and task-oriented model towards a model of a self-aware, empathetic leader. The Asia Pacific health care market was significantly impacted by COVID-19. Building this model into health professional education curriculums now will result in increased resilience and retention among providers. The HBL model can be adapted to regional needs to provide guidance for health professional educators to help students embrace their unique worldview and experience, teach lifelong reflective processes, be effective members of teams, and significantly contribute to improving population health.
Notes on Contributors
Assistant Professor Kimberly Hires reviewed the literature, designed the manuscript, developed the conceptual framework, and wrote the manuscript. Colleen Davis developed the conceptual framework, developed the manuscript, gave critical feedback to the writing of the manuscript. All the authors have read and approved the final manuscript.
Acknowledgements
The authors thank all students, faculty, colleagues, and clients who have informed our model.
Funding
No funding was used for the development of this personal view.
Declaration of Interest
The authors declare no conflict of interest concerning any aspect of this research.
References
Albarqouni, L., Hoffmann, T., Straus, S., Olsen, N. R., Young, T., Dragan, I., Shaneyfelt, T., Haynes, R., Guyatt, G., & Glasziou, P. (2018). Core competencies in evidence-based practice for health professionals: Consensus statement based on a systematic review and Delphi Survey. Journal of the American Medical Association Network Open, 1(2), e180281. https://doi.org/10.1001/jamanetworkopen.2018.0281
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard university press.
Bronfenbrenner, U. (1995). Developmental ecology through space and time: A future perspective. In P. Moen, G. H. Elder, Jr., & K. Lüscher (Eds.), Examining lives in context: Perspectives on the ecology of human development. (pp. 619–647). American Psychological Association. https://doi.org/10.1037/10176-018
Greenberg, N., Docherty, M., Gnanapragasam, S., & Wesseley, S. (2020). Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. British Medical Journal, 368, m1211. https://doi.org/10.1136/bmj.m1211
Wald, H. S. (2015). Professional identity (trans)formation in medical education: Reflection, relationship, resilience. Academic Medicine, 90(6), 701-706. https://doi.org/10.1097/ACM.0000000000000731
*Kimberly A. Hires
Georgia State University
Atlanta, GA 30302,
United States
Email: khires@gsu.edu
Submitted: 28 August 2020
Accepted: 3 March 2021
Published online: 13 July, TAPS 2021, 6(3), 32-44
https://doi.org/10.29060/TAPS.2021-6-3/OA2385
Judy McKimm1, Subha Ramani2 & Vishna Devi Nadarajah3
1Swansea University Medical School, United Kingdom; 2Harvard Medical School, United States of America; 3International Medical University, Malaysia
Abstract
Introduction: The COVID-19 pandemic has caused huge change and uncertainty for universities, faculty, and students around the world. For many health professions’ education (HPE) leaders, the pandemic has caused unforeseen crises, such as closure of campuses, uncertainty over student numbers and finances and an almost overnight shift to online learning and assessment.
Methods: In this article, we explore a range of leadership approaches, some of which are more applicable to times of crisis, and others which will be required to take forward a vision for an uncertain future. We focus on leadership and change, crisis and uncertainty, conceptualising ‘leadership’ as comprising the three interrelated elements of leadership, management and followership. These elements operate at various levels – intrapersonal, interpersonal, organisational and global systems levels.
Results: Effective leaders are often seen as being able to thrive in times of crisis – the traditional ‘hero leader’ – however, leadership in rapidly changing, complex and uncertain situations needs to be much more nuanced, adaptive and flexible.
Conclusion: From the many leadership theories and approaches available, we suggest some specific approaches that leaders might choose in order to work with their teams and organisations through these rapidly changing and challenging times.
Keywords: Leadership, Followership, Management, Health Professions Education, Change, Crisis, Uncertainty, Emotional Intelligence, COVID-19 Pandemic, Universities
Practice Highlights
- In rapid change and uncertainty, different leadership approaches are needed.
- Primal leadership and emotional intelligence are essential.
- Followers need to feel safe, physically and psychologically.
- Authentic and inclusive leadership draws from diverse views.
- Adaptive and regenerative leadership acknowledges interrelated systems.
I. INTRODUCTION
The COVID-19 pandemic has caused huge change and uncertainty for universities and their stakeholders around the world. For many health professions education (HPE) leaders, the pandemic has caused an unforeseen crisis, the ripples from which will probably be felt for years to come. Effective leaders are often seen as being able to thrive in times of crisis – the traditional ‘hero leader’ – however, leadership in rapidly changing, complex and uncertain situations need to be much more nuanced and flexible. In this article we explore leadership approaches, some of which are more applicable to times of crisis, and others which will be required to take forward a vision for the ‘new normal’ to ensure that we learn from our experiences during the pandemic.
In this article we focus on leadership and change. We start with an overview of the leadership triad, a discussion of the educational challenges imposed by the COVID-19 pandemic, followed by detailed discussion of effective leadership styles and competencies during challenging situations, approaching these through three lenses: Intrapersonal, referring to characteristics that successful leaders possess; interpersonal, referring to leadership styles and approaches leaders can adopt when they interact with others; and system level, which refers to leadership attributes to effectively lead organisations during a crisis. We conceptualise ‘leadership’ as comprising three interrelated elements: leadership, management, and followership (see Figure 1), which we call the ‘leadership triad’ (McKimm & O’Sullivan, 2016).

Figure 1: The Leadership Triad
Note: From “When I say … leadership,” by J. McKimm, and H. O’Sullivan, 2016, Medical Education, 50(9), 896–897. https://doi.org/10.1111/medu.13119
Leadership is about change and movement, putting the power and energy into a system or initiative, whereas management provides the means of enacting the leadership vision and making change happen. Leadership is always about ‘people’ (motivating them towards goals or activities) whereas management is about systems, processes and policies and we structure the article around this approach (Scouller, 2011). Followership provides the leadership with the ‘people power’ to enact the change; without followers, leadership cannot happen as leaders cannot do everything themselves. Even the most senior leaders do not ‘lead’ all the time, in ‘real life’ we move around these three elements as we lead, manage, and follow in various situations.
As leaders in HPE ourselves (Refer to Appendix A), we reflect and ask, what can a leader do during this period to ensure the best interest of all stakeholders? What lessons can we offer from our own experiences and the experiences of other leaders to those who need guidance to weather and even thrive after the crisis? The approach we have taken is to first examine the major challenges facing health professions’ leaders during this crisis, we then offer specific leadership approaches that can effectively address these challenges, concluding with change management approaches required to prepare and sustain the new normal.
II. CRISIS AND CHALLENGES FOR HEALTH PROFESSIONS EDUCATION
2020 has been a hugely challenging year for all higher education leaders across the world. From managing the rapid switch to online learning, answering student calls for some form of refund or reduction in fees, to expanded support for students and staff including emotional support, the COVID-19 pandemic has forced educational leaders to manage a different type of crisis altogether.
HPE leadership has been hugely tested during the pandemic ‘crisis’ which is very different from leading in ‘normal’ times. How do we define a crisis? A crisis is any event that could lead to an unstable, difficult and/or dangerous situation affecting an individual, group, community, or whole society. It means that difficult or important decisions must be made amidst great uncertainty and lack of information about what the future might hold. In the middle of a crisis everything can feel like it is failing or impossible. The pandemic accelerated and exacerbated many of the challenges already being experienced in HPE, including the rising costs of operating universities, increase in tuition fees and accessibility to higher education, and competition from commercial and online learning providers. Leaders in HPE face additional and different sets of challenges, as they service and are dependent on both the education and health care sectors for student education and postgraduate training. The crisis is not only experienced at organisational or team level, but the pandemic has also impacted individuals (students, academic faculty, clinical teachers, and healthcare staff) whose normal coping mechanisms may be insufficient.
However, this is not all negative and leaders need to tap into a growth mind-set, which has been defined as one that views failure and challenges as learning opportunities (Dweck, 2016). For example, Kanter (2020) suggests that it is possible to come out of a crisis stronger than before if leaders operate with a ‘people first culture’ and pay ‘attention to three things: establish clear accountability in the leadership ranks; develop a nuts-and-bolts, collaborative plan for getting through the crisis; and appoint a separate group in charge of defining the “new normal,” when the worst is over’.
It is also important to recognise that the pandemic (set alongside climate change and causes related to systemic social injustices) has foregrounded and increased awareness on inequalities across the globe in many areas, including HPE. Leadership in these times needs to pay close attention to this and seize the moment to facilitate and mobilise real change within their institutions or communities. Perhaps more so when such institutions train future health professionals and develop future leaders, who need to believe that a positive change is possible and that their own cultural context can be celebrated.
III. WHAT SORT OF LEADERSHIP IS NEEDED TO ADDRESS THESE CHALLENGES?
Inevitably changes are to be expected as the impact of the pandemic is unprecedented and is a matter of national security and public health. In most countries, governance and decision making during this crisis will be by National security councils with advisories or guidelines offered by ministries of health higher education, home affairs, or other relevant bodies. This means that universities and educational leaders who usually have autonomy in decision making are subject to stricter controls and frequent changes from authorities who are understandably making decisions at national and international levels. For people in leadership positions, this is unchartered territory and given the ‘traditional’ power and authority hierarchies and processes in higher education and health professions education, it is unsurprising that leaders may feel helpless during a crisis such as this. In Figure 2, we list four levels along which leadership needs to be enacted, and some suggested approaches to help leaders move out of this feeling of helplessness so that they can lead the people for whom they are responsible.
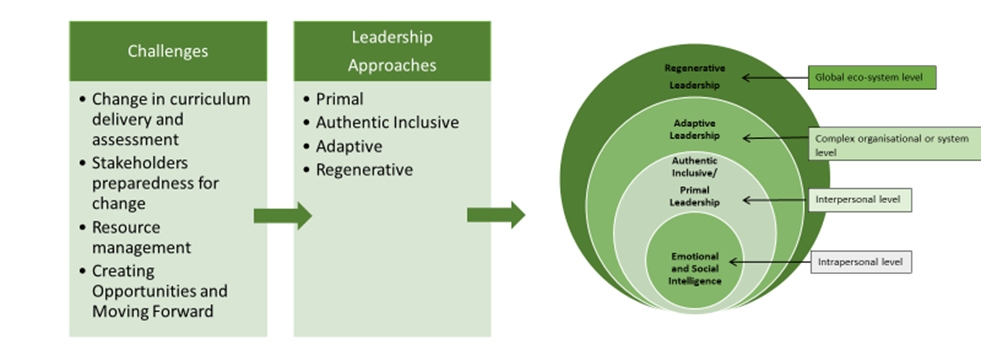
Figure 2: Four levels of leadership for addressing challenges during a crisis
Note: Drawing from “ABC of clinical leadership,” by T. Swanwick and J. McKimm, 2017, John Wiley & Sons.
A. The Intrapersonal Level: Working with Emotional and Social Intelligence
Challenging circumstances which force change, such as the COVID-19 pandemic, result in a range of emotional responses among leaders and all those for whom they are responsible.
In 1998, Daniel Goleman proposed that leadership skills such as toughness, vision, determination, and intelligence alone are insufficient. He stated that the most successful leaders also possess a high degree of emotional intelligence (EI) which includes the traits of self-awareness, self-regulation, motivation, empathy, and social skills (Goleman, 1998). Boyatzis and Goleman went to analyse the core attributes that were present in those identified by a variety of companies as their most successful leaders. As a result, twelve competencies of emotional and social intelligence were described under four domains and depicted in Figure 3. The four domains include: Self-awareness, self-management, social awareness, and relationship management; these are critical attributes for leaders to operate effectively through own and others’ emotions during challenging circumstances such as the COVID-19 pandemic. These competencies and behaviours help to simplify a complex construct such as EI and can facilitate leadership development in this area.
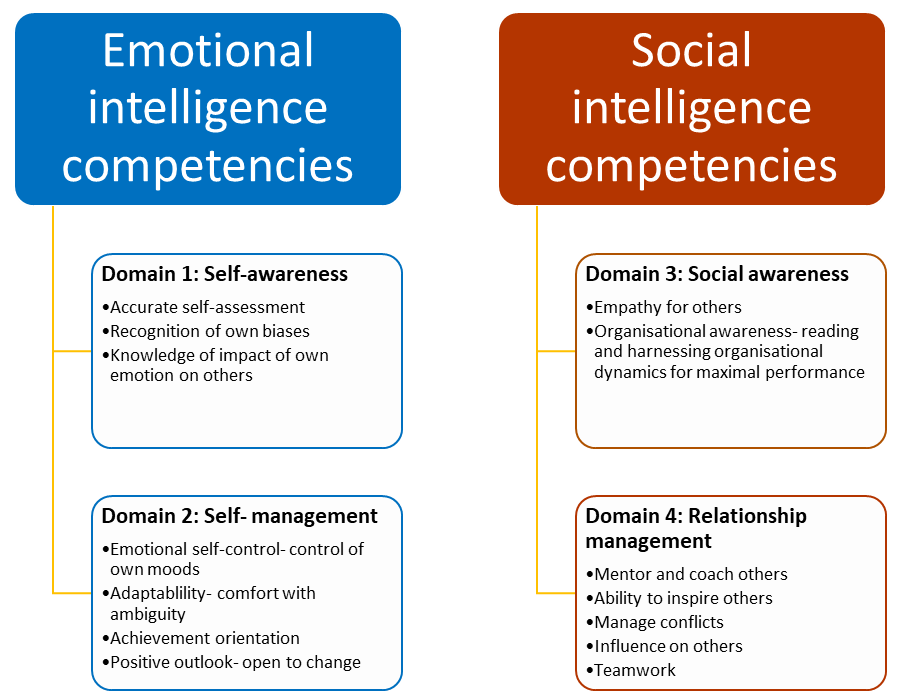
Figure 3: Intrapersonal leadership attributes: Emotional and social intelligence competencies essential to lead and manage change during challenging circumstances.
Note: Adapted from “Competencies as a behavioral approach to emotional intelligence,” by R. E. Boyatzis, 2009, Journal of Management Development, 28(9), 749–770. https://doi.org/10.1108/02621710910987647
While the construct of EI and competencies can serve as a useful guide to leaders in leading and managing change, the actual behaviours that are most effective depend on the organisational culture and the societal culture within which an organisation is situated. Moreover, at institutions which feature diversity in the composition of its leaders, staff and learners, leaders should recognise that individuals on a team might have different emotional reactions even when working towards a common goal. All four domains of EI competencies are essential for leaders to manage the groups of people they lead (See Table 1).
|
1. Self-awareness allows leaders to recognise their assumptions and biases, and how they affect their worldview. 2. Self-management promotes thought before action and ability to manage own emotions and reactions, important in reigning in negative emotion. 3. Social awareness allows leaders to understand the individuals who make up their team and recognise differences in viewpoints and personalities. 4. Relationship management is essential to welcome a variety of perspectives, nurture talent, and maximise the potential and productivity of individuals, teams, and the organisation. Mentoring and coaching skills fall under this domain.
|
Table 1: The impact of the four EI domains
A. The Interpersonal Level: Influencing Others and Drawing on Their Individual and Collective Strengths
In rapid change and uncertainty, what people want from their leaders is an authentic voice and to feel that leaders are listening, taking their concerns seriously and that they have the expertise and authority to lead and manage change. Leaders are created and maintained by how their followers see, relate to, and trust them (Uhl-Bien & Carsten, 2018). Simon Sinek talks about how followers will follow their leaders into highly unsafe situations (such as war) if they feel their leaders can keep them safe and that they are ‘in it’ together (Sinek, 2014). Whilst internally, leaders may feel as lost and at sea as those for whom they are responsible, they must draw on their own resilience and ‘grit’ (Duckworth & Duckworth, 2016) to step up and provide effective leadership. This involves displaying courage, putting personal interests aside to achieve what needs to be done and acting on convictions and principles even when it requires personal risk-taking. In crisis or uncertainty, followers need leaders who can communicate clearly, transparently, and regularly, who can make decisions (even if these are unpopular or later change) and who look out for and care for them (Paixão et al., 2020).
Primal leadership, described by EI experts, emphasises that leaders’ emotional affect and mood is a major driver of the mood and behaviours of others around them (Goleman et al., 2001). Thus, during a crisis, leaders need to be optimistic, yet, authentic and realistic. Positive emotion or resonance is critical to motivate people, allow them to be productive amidst chaos and preserve their wellbeing. As the pandemic spread around the world, some academic leaders demonstrated a highly person-centred approach in relation to staff and students, recognising their fears and anxieties, encouraging virtual education and work whenever possible, thus demonstrating primal leadership as well as cultural intelligence (Liao & Thomas, 2020; Velarde et al., 2020). If we want people to work interprofessional, pay attention to well-being and motivation, and work together to meet organisational goals, then flattening hierarchies is essential to generate ideas and functional collaboration (Barrow et al., 2011; Barrow et al., 2014) (Refer to Appendix B).
Whilst leaders may need to take a ‘command and control’ type of leadership in times of great crisis because important decisions must be taken and communicated quickly, after the immediate crisis other approaches will be helpful. For example, authentic, altruistic, person-centred, and inclusive leadership (Avolio & Gardner, 2005; Cardiff et al., 2018; Hollander, 2012; Sosik et al., 2009) approaches are very much focussed on the leader drawing from their own strengths and, through awareness and acknowledgement of their own weaknesses and biases, proactively seeking a range of perspectives on issues and demonstrating that they value and listen to those around them. When leaders are trying to make impactful decisions in times of uncertainty, having a range of views and ideas is essential. Leaders may also need to show intellectual humility – admitting mistakes, learning from criticism and different points of view, and acknowledging and seeking contributions of others to overcome limitations. As tasks are defined, leaders need to empower and demonstrate their confidence in people by delegating and holding them responsible for activities they can control.
B. The Complex Organisation or System Level: Adaptive Leadership
While conventional approaches to leadership and management have their place, as the pandemic elapsed around the world leaders needed to be highly adaptive and flexible, adjusting their outcomes and approaches based on rapidly changing information. Because we live in a VUCA (Volatile, Uncertain, Complex, Ambiguous)
(Worley & Jules, 2020) and RUPT (Rapid, Uncertain, Paradoxical, Tangled) (Till, Dutta, McKimm, 2016) world, leadership is needed that is flexible and agile enough to adapt to circumstances which most HPEs have not experienced before.
Adaptive leadership (Heifetz et al., 2009; Randall & Coakley, 2007) is specifically focussed on leadership in complex systems or situations and is helpful when thinking about how to respond to change, uncertainty, and crisis. Adaptive leaders do not simply work in a technical way (by just applying familiar management processes and ways of working) but involve people throughout the organisation to help solve ‘wicked’ problems, which may not have a clear solution and may require new ways of working. Adaptive leaders create the organisational conditions that enable dynamic networks and environments to achieve agreed goals in uncertain environments. Adaptive leadership focuses on four dimensions: Navigating organisational/system environments; leading with empathy; learning through self-correction and reflection and creating win-win solutions. These dimensions have many parallels with EI competencies. One of the most useful concepts in adaptive leadership which helps leaders to make decisions, is the ability to diagnose the ‘precious’ from the ‘expendable’ (Heifetz et al., 2009). What do we mean by this? The ‘precious’ is what is vitally important to the organisation; in education this is the learners themselves, the faculty, and the quality of educational provision – you do not want to lose the focus on these as you respond to crisis and change. What is ‘expendable’? Because of campus closures due to the pandemic, suddenly the large lecture theatres, shiny new buildings, and campuses that many universities see as artefacts of success and prestige, were expendable. Once the ‘new normal’ emerges, we will no doubt see a return to campuses and utilisation of buildings again, but adaptive leaders recognise what is precious and make sure that this is looked after and nurtured. We must remember this once the immediate crises are past (Refer to Appendix C).
C. The Global Eco-System Level: A Focus on Healing and Regeneration
The pandemic has highlighted starkly that the world, its countries, people, and structures are highly interconnected. In such times what affects one country, and actions (or inactions) cause ripples across the globe. We have already alluded to the need for leaders to work collaboratively and share practices, and during the pandemic we have seen multiple examples of international collaboration and the sharing of practice by HPEs everywhere. When we are all in the same boat, we need to sail in the same direction.
As well as being willing and proactive in collaborating on finding solutions to common challenges, leaders in HPE also need to consider the wider implications of the impact of climate change and human activities on health and health care. McKimm and McLean (2020) make the case for an ‘eco-ethical’ leadership approach which focuses leaders’ minds on the need for sustainable health professions’ education and practices. Another approach that is very relevant to HPE and its response to the pandemic is that of ‘regenerative’ leadership (Hutchins & Storm, 2019). In stimulating the recovery of health professions’ education and the organisations that provide it, leaders will need to pay attention to ensuring the conditions for healing, regeneration and thriving are present, so that people (faculty and students) feel safe to return to campuses and a more ‘normal’ way of working.
IV. PREPARING FOR A ‘NEW NORMAL’
A. Planning and Implementing Change
As countries, organisations and individuals start to look forward and prepare for mass returns to campus, leaders will need to support students and faculty for a ‘new normal’. This requires managing expectations as well as physical and psychological safety as discussed above. Management is all about maintaining stability and order (as Drucker (2007) says: ‘doing the thing right’) therefore, in addition to choosing appropriate leadership approaches, leaders will need to utilise a range of management tools to help plan how universities and their research, education programmes and other activities will function.
B. Risk Assessment
In an ideal world, all changes would be able to be planned for and there would be no surprises. However, successful organisations (and individuals) also plan for unforeseen circumstances to stay resilient and help mitigate risk. There are a few ways of assessing risks, with one of the most widely used being a ‘risk matrix’ (Ni et al., 2010). This is used during risk assessment to define the level of risk by considering the category of probability or likelihood against the category of consequence severity. This simple tool helps to increase the visibility of risks and assist management decision making. At university level as well as departmental and programme levels, a risk analysis should be carried out and updated regularly. In stable times, risk analysis helps the organisation keep aware of external and internal risk factors and put plans in place, but during the pandemic it is essential.
C. Managing Change
A widely used tool to lead, accelerate and manage change is Kotter’s (2007) eight-stage process (Refer to Appendix D).
The pandemic itself provided a sense of urgency as universities and teachers scrambled to respond, and leaders needed a good understanding of organisational resources, the external environment, and educational responses worldwide to develop meaningful and realistic strategies (Schwartzstein et al., 2008). The fluidity and volatility of the pandemic situation early on made any progress along Kotter’s steps difficult to see at either individual or institutional level. Whilst it can feel very unsettling to have to return to an earlier Step, after moving a few steps forward, it is often necessary to do so and Kotter’s model acknowledges that change is iterative, not linear. Kotter’s and similar models are very useful both for planning the changes needed as well as offering a framework for analysis of where change efforts are faltering or failing. A formal communications strategy is essential which provides consistent messages, opportunities for questions to be answered for all key stakeholders and celebrates ‘quick visible wins’, such as learners returning to their studies or a successfully run online assessment or graduation ceremony.
D. Focus on Outcomes
Across the world, universities (many of which had never provided online learning or assessment) suddenly had to decide how (or whether) they would (or could) provide educational opportunities for their students. Cameron and Green (2019) suggest that leaders responding to or stimulating change need to balance their efforts across three dimensions of any change: outcomes, interests, and emotions. In terms of ‘outcomes’, they stress that clear outcomes (deliverables) must be developed and implemented. Outcomes (goals, targets or objectives) need to be SMART (specific, measurable, achievable, realistic and time bound). In times of immediate crisis, some goals will need to be very short-term (e.g. ‘ensure all faculty are able and prepared to work from home by the end of next week’), whereas strategically, senior leaders have the responsibility to keep the longer terms outcomes in mind, e.g. ‘ensure that the university remains financially viable’. In terms of ‘emotions’, Cameron and Green (2019) suggest that the role of the leader is to enable people and the culture to adapt to the change and leaders also need to pay attention to (what may be competing) interests, here they need to mobilize their influence, authority and power to enact the change.
E. Planning and Implementation
McKimm and Jones (2018) suggest using project management techniques for operational planning and implementation. During the pandemic, plans will need to be devised and aligned in a range of areas (learning and teaching, student and faculty wellbeing, research, estates, finance etc.) and at many levels: whole university, department, and programme.
A project management approach sees activities as temporary, non-routine, acknowledging uncertainty and with a defined end point. Techniques taking a ‘linear’ view of change such as Lewin’s ‘freeze/unfreeze’ model (Cummings et al., 2016; Lewin, 1951) can be useful in framing the response into simple terms rather than getting bogged down in complexity. These look at the change process as comprising three steps: current state (how the university, schools and programmes ran pre-pandemic) – transitional state (how the university runs during the pandemic) – desired state (how might everything run after the pandemic, in the ‘new normal’). Once the broad elements and strategy have been agreed, then the detailed planning and implementation stages begin.
F. Sustaining Change
1) Recognising the dynamism of change: While crisis can bring about opportunities for real change, realistically there will be challenges sustaining the change. Buchanan et al. (2005) suggests organisational sustainability is contextual and dependent of various factors, including changes in market demands, financial viability, or political decisions. The drivers of sustainability will also differ based on organisational levels for example whether at the individual, managerial or leadership role. Given the uncertainties that leaders will face, an important step in sustaining change with positive outcomes would be an awareness that change, and sustainability is not static but is instead dynamic, requiring an improvement trajectory over time. This concept can also be described as dynamic stability: a process of continual, small, and possibly innovative changes that involve the modification or enhancement existing practices and business models (Hodges & Gill, 2014). When translated into practice, sustaining change requires as much attention from leaders as when developing and implementing change.
2) Supporting individuals at multiple levels: As sustainability of change is also dependent at the individual level, leaders should strongly promote and support initiatives that promote both individual professional and personal development. In the context of HPE, staff support is often interpreted as faculty development activities and more often is the form of workshops or, more recently, webinars. It is important for institutions to broaden the support activities to include non-faculty staff, provide activities other than workshops and implement initiatives for wellness and mental health wellbeing at the workplace. Another example of staff supports activities that has gained traction during this crisis are global community of practices. Given the similar challenges faced, global community of practices offer an opportunity to share strategies of mutual interest and benefit and build networks of educators across socio-cultural contexts (Thampy et al., 2020). As health professions’ leaders and educational organisations brace for the financial impact of the crisis, the case to reduce funding for staff support and investment in people maybe put forward. Leaders need to reflect and balance the impact reducing operating costs with enhancing the skills of staff to embrace, work with and sustain change.
3) Exchanging and co-creating global solutions: Sustaining change requires a vision for a new way of leadership and ways of working (McKimm & McLean, 2020). The recent COVID-19 crisis has highlighted that solutions to manage and sustain positive outcomes may not come from familiar local sources or authorities. The crisis also challenged the previously held assumptions of standards and readiness of healthcare systems and governance of it in some countries, suggesting much can be learned from successful approaches taken across the globe. Leaders in HPE should work collaboratively to acknowledge that solutions can come from across boundaries and draw from it lessons and guidelines for a global approach in the training of health professionals.
V. CONCLUSION
Although this paper provides a roadmap and suggested approaches for HPE leaders and followers alike to reflect on as they work through various waves of the pandemic, it is critical for leaders to be flexible and adaptive and adopt an emotionally intelligent and person-centred approach. Psychological safety is integral for professionals at all levels to successfully accomplish individual and institutional goals during challenging circumstances, along with leaders who provide stability and vision. What has become abundantly clear during the pandemic is that health professions’ educators from around the world have common as well as unique challenges and are increasingly seeking a diverse, multicultural global community of practice, sharing best practices and seeking to understand other cultural, regional and national educational context. These insights emphasise that health professions educators, regardless of their geographical location, cannot succeed in their leadership roles without a culturally sensitive, competent and grounded approach. No longer can experts from one group of countries impose their best practices on another region of the world without opening themselves to learning from other cultures and contexts.
Notes on Contributors
Judy McKimm conceptualised the idea for the article, wrote specific sections, and reviewed and edited the full article prior to submission.
Subha Ramani helped design the structure for this perspective, wrote content sections, edited, read and approved the final manuscript.
Vishna Devi Nadarajah helped design the structure for this perspective, wrote content sections, edited, read and approved the final manuscript.
Ethical Approval
No ethics approval was required as this is an opinion piece supported by a literature review and does not relate to primary research.
Funding
No funding sources are associated with this paper.
Declaration of Interest
I confirm that the manuscript is original work of authors which has not been previously published or under review with another journal.
I confirm that all research meets the legal and ethical guidelines.
I confirm that I have stated all possible conflicts of interest in my manuscript and explicitly stated even if there is no conflict of interest.
I am not using third-party material that requires formal permission.
References
Ashokka, B., Ong, S. Y., Tay, K. H., Loh, N. H. W., Gee, C. F., & Samarasekera, D. D. (2020). Coordinated responses of academic medical centres to pandemics: Sustaining medical education during COVID-19. Medical Teacher, 42(7), 762–771. https://doi.org/10.1080/0142159x.2020.1757634
Avolio, B. J., & Gardner, W. L. (2005). Authentic leadership development: Getting to the root of positive forms of leadership. The Leadership Quarterly, 16(3), 315–338. https://doi.org/10.1016/j.leaqua.2005.03.001
Barrow, M., McKimm, J., & Gasquoine, S. (2011). The policy and the practice: early-career doctors and nurses as leaders and followers in the delivery of health care. Advances in Health Sciences Education, 16(1), 17–29. https://doi.org/10.1007/s10459-010-9239-2
Barrow, M., McKimm, J., Gasquoine, S., & Rowe, D. (2014). Collaborating in healthcare delivery: Exploring conceptual differences at the “bedside.” Journal of Interprofessional Care, 29(2), 119–124. https://doi.org/10.3109/13561820.2014.955911
Boyatzis, R. E. (2009). Competencies as a behavioral approach to emotional intelligence. Journal of Management Development, 28(9), 749–770. https://doi.org/10.1108/02621710910987647
Buchanan, D., Ketley, D., Gollop, R., Jones, J. L., Lamont, S. S., Neath, A., & Whitby, E. (2005). No going back: A review of the literature on sustaining strategic change. International Journal of Management Review, 7 (3). https://doi.org/10.1111/j.1468-2370.2005.00111.x
Cameron, E., & Green, M. (2019). Making sense of change management: A complete guide to the models, tools, and techniques of organizational change. Kogan Page Publishers.
Cardiff, S., McCormack, B., & McCance, T. (2018). Person-centred leadership: A relational approach to leadership derived through action research. Journal of Clinical Nursing, 27(15–16), 3056–3069. https://doi.org/10.1111/jocn.14492
Cummings, S., Bridgman, T., & Brown, K. G. (2016). Unfreezing change as three steps: Rethinking Kurt Lewin’s legacy for change management. Human Relations, 69(1), 33-60.
Duckworth, A. (2016). Grit: The power of passion and perseverance (Vol. 234), Scribner. https://doi.org/10.1111/peps.12198
Dweck, C. (2016). What having a “growth mindset” actually means. Harvard Business Review, 13, 213-226.
Goleman, D. (1998). The emotionally competent leader. The Healthcare Forum Journal, 41(2), 36-38.
Goleman, D., Boyatzis, R., & McKee, A. (2001). Primal leadership: The hidden driver of great performance. Harvard Business Review, 79(11), 42-53.
Heifetz, R. A., Heifetz, R., Grashow, A., & Linsky, M. (2009). The practice of adaptive leadership: Tools and tactics for changing your organization and the world. Harvard Business Press.
Hodges, J., & Gill, R. (2014). Sustaining change in organizations (1st ed.). SAGE Publications.
Hollander, E. P. (2012). Inclusive leadership: The essential leader-follower relationship (Applied Psychology Series) (1st ed.). Routledge.
Hutchins, G., & Storm, L. (2019). Regenerative Leadership: The DNA of life-affirming 21st century organizations. Wordzworth Publishing.
Kanter, R. M. (2020). Leading your team past the peak of a crisis. Harvard Business Review
Kotter, J. (2007). Leading change: Why transformation efforts fail. Harvard Business Review, 86, 97-103.
Lazarus, G., Mangkuliguna, G., & Findyartini, A. (2020). Medical students in Indonesia: An invaluable living gemstone during coronavirus disease 2019 pandemic. Korean Journal of Medical Education, 32(3), 237–241. https://doi.org/10.3946/kjme.2020.165
Lewin, K. (1951). Field theory in social science: Selected theoretical papers (D. Cartwright, Ed.). Harpers.
Liao, Y., & Thomas, D. C. (2020). Conceptualizing Cultural Intelligence. In Cultural Intelligence in the World of Work (pp. 17-30). Springer.
McKimm, J., & Jones, P. K. (2018). Twelve tips for applying change models to curriculum design, development and delivery. Medical Teacher, 40(5), 520-526.
McKimm, J., & McLean, M. (2020). Rethinking health professions’ education leadership: Developing ‘eco-ethical’leaders for a more sustainable world and future. Medical Teacher, 42(8), 855-860.
McKimm, J., & O’Sullivan, H. (2016). When I say … leadership. Medical Education, 50(9), 896–897. https://doi.org/10.1111/medu.13119
Nadarajah, V. D., Er, H. M., & Lilley, P. (2020). Turning around a medical education conference: Ottawa 2020 in the time of COVID‐19. Medical Education, 54(8), 760–761. https://doi.org/10.1111/medu.14197
Ni, H., Chen, A., & Chen, N. (2010). Some extensions on risk matrix approach. Safety Science, 48(10), 1269–1278. https://doi.org/10.1016/j.ssci.2010.04.005
Paixão, G., Mills, C., McKimm, J., Hassanien, M. A., & Al-Hayani, A. A. (2020). Leadership in a crisis: Doing things differently, doing different things. British Journal of Hospital Medicine, 81(11), 1–9. https://doi.org/10.12968/hmed.2020.0611
Randall, L. M., & Coakley, L. A. (2007). Applying adaptive leadership to successful change initiatives in academia. Leadership & Organization Development Journal, 28(4), 325–335. https://doi.org/10.1108/01437730710752201
Schwartzstein, R. M., Huang, G. C., & Coughlin, C. M. (2008). Development and implementation of a comprehensive strategic plan for medical education at an academic medical center. Academic Medicine, 83(6), 550–559. https://doi.org/10.1097/acm.0b013e3181722c7c
Scouller, J. (2011). The three levels of leadership: How to develop your leadership presence, knowhow, and skill. Management Books 2000.
Sinek, S. (2014). Leaders eat last: Why some teams pull together and others don’t. Penguin.
Sosik, J. J., Jung, D., & Dinger, S. L. (2009). Values in authentic action. Group & Organization Management, 34(4), 395–431. https://doi.org/10.1177/1059601108329212
Swanwick, T., & McKimm, J. (2017). ABC of clinical leadership. John Wiley & Sons.
Thampy, H. K., Ramani, S., McKimm, J., & Nadarajah, V. D. (2020). Virtual speed mentoring in challenging times. The Clinical Teacher, 17(4), 430–432. https://doi.org/10.1111/tct.13216
Till, A., Dutta, N., & McKimm, J. (2016). Vertical leadership in highly complex and unpredictable health systems. British Journal of Hospital Medicine, 77(8), 471–475. https://doi.org/10.12968/hmed.2016.77.8.471
Uhl-Bien, M., & Carsten, M. (2018). Reversing the lens in leadership: Positioning followership in the leadership construct. In Leadership now: Reflections on the legacy of Boas Shamir. Emerald Publishing Limited.
Velarde, J. M., Ghani, M. F., Adams, D., & Cheah, J.-H. (2020). Towards a healthy school climate: The mediating effect of transformational leadership on cultural intelligence and organisational health. Educational Management Administration & Leadership. https://doi.org/10.1177/1741143220937311
Worley, C. G., & Jules, C. (2020). COVID-19’s uncomfortable revelations about agile and sustainable organizations in a VUCA world. The Journal of Applied Behavioral Science, 56(3), 279–283. https://doi.org/10.1177/0021886320936263
*Judy McKimm
Swansea University Medical School,
Swansea University
Swansea, UK, SA1 8PP
Email: j.mckimm@swansea.ac.uk
Submitted: 14 August 2020
Accepted: 14 October 2020
Published online: 13 July, TAPS 2021, 6(3), 114-117
https://doi.org/10.29060/TAPS.2021-6-3/PV2376
Meredith T. Yeung1, Melissa Y. Chan1, Clement C. Yan1,2 & Katherin S. Huang1
1Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore; 2Department of Physiotherapy, Sengkang General Hospital, Singapore
I. INTRODUCTION
Coronavirus Disease 2019 (COVID-19), which requires no introduction, is transmitted through droplet transmission and is highly contagious (del Rio & Malani, 2020; Guan et al., 2020; Sohrabi et al., 2020). After it was declared a pandemic on 11 March 2020, the Singapore government implemented a “circuit breaker” period, or partial lockdown, on 7 April 2020 (Ministry of Health, 2020). In spite of numerous initiatives for faculty to embrace technology-enhanced learning over the past years, it was a steep take-off for most programmes at institutes of higher learning. This short personal view intends to share our experience from the sole entry-level physiotherapy programme in Singapore.
II. ONLINE LESSONS
During the preliminary stages of the pandemic, faculty proactively switched all face-to-face lectures and tutorials that involved 50 or more students to online lessons. As the academic timetable had already been established, there was little to no disruption to lesson scheduling. Synchronous methods of e-learning occurred via video-conferencing software, such as Zoom and Microsoft Teams, and was used for lectures and tutorials. The virtual classroom allowed live interaction, and was especially useful for small group case study discussions when students were allocated into breakout rooms. Asynchronous methods of e-learning took the form of pre-recorded lectures, predominantly via Microsoft PowerPoint or iSpring, or recordings of live lectures. This promoted ubiquitous learning where the learner could learn at a time and place of their convenience, and which garnered positive feedback of over 60% from an unofficial survey of students. One student commented that “the online lectures were very useful, especially those that are pre-recorded so [that we] won’t miss out on what the professor is saying”.
While the move to online teaching was essential, it certainly had its challenges. Many of the faculty were not proficient with the advanced features of Zoom, resulting in initial hiccups in organising multiple lessons for over a hundred students. For example, being unfamiliar with the software, lack of stable Wi-Fi off-campus, and insufficient software accounts were some teething problems. Training workshops for the use of Zoom were initially planned prior to the pandemic, however these could not be realised due to sudden time constraints. Training and troubleshooting manuals were thus made available for all educators and students via an online portal, in addition to a phone helpdesk for further assistance. Furthermore, the other challenge we faced was the short amount of time available to produce and upload enough e-learning material, such as filming of teaching videos, organising self-directed packages, and modifying lecture material to suit live online or pre-recorded delivery. Students also faced challenges due to the multiple modules they were enrolled in during the academic term, having to keep track of up to five randomly-generated meeting identification numbers (ID) each day. The use of one meeting ID per module, set at a regular occurrence, was implemented to alleviate this burden.
One concern we had was over “Zoom fatigue” and general lack of engagement from students. One strategy we implemented was to insert stretching exercises and a rest period after each hour of lesson. Quiz apps, such as Kahoot and Socrative, was also used to poll content-specific questions, to promote student engagement and active participation. These strategies helped to sustain attention span and was deemed successful as reflected by near-100% participant responses and structured module feedback. One student commented that she was “quite happy that we can still continue lessons, although it is modified…and not have to worry about the uncertainty of lessons being cancelled”.
III. BLENDED FORMAT FOR PRACTICAL LESSONS
Physiotherapy students are highly dependent on skills-based learning and hands-on practice, which equips them with competencies to treat real patients in the clinical setting. Conducting practical lessons was met with additional challenges due to the strict rules on safe distancing, restrictions on human movement, and limits on class size and frequency. We approached this using video-augmented practicum. A pre-recorded demonstration of physiotherapy skills was disseminated to students via the learning management system (LMS) before each hands-on lesson. This strategy was useful for teaching of skills which require physical space and simulation, such as performing auscultation, manual handling, patient positioning and transfers, airway suctioning, or walking tests. To illustrate, in the teaching of cardiopulmonary exercise testing (CPET), we divided the content into several components: an introductory video and stepwise guide on how to conduct the exercise test; a self-directed learning package on CPET results interpretation with self-evaluation; and a hands-on practical session of performing the full CPET with peers in the human performance laboratory on university campus. Faculty then utilised the face-to-face practical sessions to provide critical feedback and correct students’ techniques. Students were further able to consult with faculty and receive real-time feedback on their performance of skills via video-conferencing, if requested.
IV. CONDUCTING ASSESSMENT DURING A PANDEMIC
Following the declaration of the pandemic, our programme converted all physical paper examinations to online examinations. Commercially available remote proctoring systems, such as Respondus® and Proctortrack by Verificient, allowed us to mitigate cheating in the virtual environment. The three-point identity check in these systems ensures that authentication is vigorous, while the manual or artificial intelligence proctoring technology enables remote invigilation. ‘Browser lock’ disables platform-sharing functions such as screen-sharing or remote desktop control that would otherwise allow a proxy to take the examination.
V. ONLINE VIVA VOCE
To assess the “thinking” portion of patient management, we conducted online viva examinations in lieu of physical examinations. To prepare for the large volume of online assessments, we underwent several trials of Zoom, tinkering with features such as the waiting room and breakout rooms. These trials enabled us to familiarise ourselves with the logistic flow, as well as troubleshoot issues such as interruptions during entrance and exit, transfer of host rights, and audio-visual glitches. Administrative coordinators were designated to manually allocate students into the breakout rooms, which was preferred over pre-allocation in order to reduce errors. In anticipation of potential lapses, we used a separate chat messaging software for assessors and coordinators to flag and resolve technical issues. A spreadsheet was used to schedule detailed information about switchover times and room allocation for each candidate, ensuring smooth transition from main room to breakout rooms, as well as to resolve any scheduling conflict. Advance dissemination of the examination schedule and login details was crucial in minimising technical issues. Marking rubrics with clear descriptors were developed, with time set aside for pre- and post-viva calibration amongst assessors. Students had access to the marking rubrics, and a mock run was held to familiarise students with the logistic flow of the assessment. With these preparations in place, we were able to conduct online viva examinations for over a hundred students successfully and efficiently.
VI. VIDEO SUBMISSION FOR SKILLS ASSESSMENT
To assess the “doing” portion of patient management, we utilised video-based assessment. The evidence for video-based assessment in healthcare education is at its infancy, with most evidence evolving around the idea of video-based peer feedback, assessment for communication skills, or the assessment of surgical skills. We tested this method in a final-year elective module that required learners to demonstrate manually-assisted cough—a skill that would traditionally be performed in front of an assessor and marked against a checklist. Casually dubbed the ‘open-book practical assessment’, faculty listed detailed requirements of the assessment, which gave students time to practise skills before recording and submission. The use of student-generated video assessment (mean marks 77.84 ± 4.59, class size of 30) to replace traditional skills assessment (mean marks 80 ± 3.88, class size of 25) was considered a success as there was no significant difference in the pass-fail ratio between the affected cohort and prior cohorts. In addition, we observed some unintentional benefits, such as the demonstration of digital capability and communication skills by the students, while aligned with the learning and assessment objectives – a finding consistent with the available literature (Walters et al., 2015).
The assessment of skills may also be performed real-time through video-conferencing. However, the logistics and time required to assess such a large number of students within a relatively short timeframe made it a task too immense for us to undertake. Nonetheless, with adequate manpower and resources, it could undoubtedly be feasible, perhaps even superior, as a form of video assessment.
VII. CONCLUSION
The unprecedented COVID-19 pandemic has forced us to refashion pedagogical approaches to our curriculum and to embrace positive changes for the future of physiotherapy education. Utilising aforementioned strategies, we were able to deliver our teaching effectively and almost entirely virtually, despite initial hiccups. Pragmatically, it would be ideal to formally evaluate the impact of a virtual curriculum on established learning outcomes, as well as the general acceptability of such a programme for both students and faculty. In the event of future similar state of emergencies, it may even be prudent to develop a blueprint of and stepwise approach to pedagogy escalating along the spectrum of face-to-face methods versus virtual technology. We hope that this short personal view will provide other educators with some solutions to coping with the challenges of teaching surrounding this exigent time.
Notes on Contributors
Meredith T. Yeung is an Associate Professor at the Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore. She contributed to the conception and revision of the manuscript critically for important intellectual content.
Melissa Y. Chan is an Associate Faculty at the Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore. She contributed to the conception and revision of the manuscript critically for important intellectual content.
Clement C. Yan is an Associate Professor at the Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore and Senior Principal Physiotherapist at the Department of Physiotherapy, Sengkang General Hospital, Singapore. He contributed to the conception and revision of the manuscript critically for important intellectual content.
Katherin S. Huang is an Associate Faculty at the Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore. She contributed to the conception and revision of the manuscript critically for important intellectual content.
Acknowledgements
The authors wish to thank all students and staff members from the Singapore Institute of Technology and the physiotherapy programme for all the support during this challenging time of COVID-19. All comments and module feedback referred to in this article were willingly and voluntarily provided by students.
Funding
This personal view did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Interest
The authors declare no form of possible conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
del Rio, C., & Malani, P. N. (2020). 2019 Novel coronavirus – Important information for clinicians. Journal of the American Medical Association, 323(11), 1039-1040. https://doi.org/10.1001/jama.2020.1490
Guan, W., Ni, Z., Hu, Y., Liang, W., Ou, C., He, J., Liu, L., Shan, H., Lei, C., Hui, D. S. C., Du, B., Li, L., Zeng, G., Yuen, K.-Y., Chen, R., Tang, C., Wang, T., Chen, P., Xiang, J., … Zhong, N. (2020). Clinical characteristics of Coronavirus Disease 2019 in China. New England Journal of Medicine, 382(18), 1708–1720. https://doi.org/10.1056/NEJMoa2002032
Ministry of Health (2020, April 7). Speech by Mr Gan Kim Yong, Minister for Health, at the second reading of COVID-19 (temporary measures) Bill, 7 April 2020 [Press release]. https://www.moh.gov.sg/news-highlights/details/speech-by-mr-gan-kim-yong-minister-for-health-at-the-second-reading-of-covid-19-(temporary-measures)-bill-7-april-2020
Sohrabi, C., Alsafi, Z., O’Neill, N., Khan, M., Kerwan, A., Al-Jabir, A., Iosifidis, C., & Agha, R. (2020). World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). International Journal of Surgery, 76, 71–76. https://doi.org/10.1016/j.ijsu.2020.02.034
Walters, S. R., Hallas, J., Phelps, S., & Ikeda, E. (2015). Enhancing the ability of students to engage with theoretical concepts through the creation of learner-generated video assessment. Sport Management Education Journal, 9(2), 102-112. https://doi.org/10.1123/smej.2014-0041
*Meredith T. Yeung
Singapore Institute of Technology,
10 Dover Drive,
Singapore 138683
Tel: +65 65928671
Email: Meredith.Yeung@SingaporeTech.edu.sg
Submitted: 16 July 2020
Accepted: 4 November 2020
Published online: 13 July, TAPS 2021, 6(3), 118-120
https://doi.org/10.29060/TAPS.2021-6-3/CS2392
Wai Keung Chui, Han Kiat Ho, Li Lin Christina Chai & Paul J. Gallagher
Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore
I. THE CHANGING LANDSCAPE IN PHARMACY PRACTICE
Pharmacy practice in Singapore is rapidly evolving with the advent of technological innovations and changes in patient demographics. For instance, the dispensing process in hospitals have been automated; telepharmacy has made access to pharmaceutical services more convenient in the community; an aging population has brought along complex co-morbidities, chronic diseases, polypharmacy and community-based pharmaceutical care services that will require clinical interventions by pharmacists. These examples have raised the question of the “relevance of pharmacists” in the evolving health system. To stay relevant, pharmacists must move from the traditional medication supply (product focus) role to curating the optimal use of medicines by patients (patient focus) in a technology and informatics driven health system. This paradigm shift can only be enabled if the education of pharmacists is suitably re-constructed with outcomes that will future-roof their capabilities in the new healthcare ecosystem. This prompted the Department of Pharmacy at the National University of Singapore (NUS) to make a commitment to review its present programme thereby turning the threats into opportunities for its future pharmacy graduates. This case study reports the approach taken by the Department to re-engineer its curriculum for modern pharmacy practice in the twenty-first century.
II. NEEDS ANALYSIS AND RECOMMENDATIONS
In late 2018, a needs analysis was conducted by the Department to inform the design strategies. This was done through structured interviews by informed consent of key opinion leaders, and focused group discussions with alumni and students. The data collected were coded and analysed thematically. Some main themes about the graduates that came through were the weakness in applying their knowledge, their lack of an understanding of the health system and their reluctance to take leadership role. Feedback on the present curriculum included a lack of connectivity between modules that were taught in silos and the structured experiential learning was scheduled too late in the curriculum. It was recommended that a competency-based and integrated curriculum (Husband et al., 2014; Pearson & Hubball, 2012) would help students achieve the necessary competence as a health professional and apply the multidisciplinary knowledge holistically to problem solve. An introduction of systems thinking, and a longitudinal experiential learning programme across the four years will help students understand their future work environment better.
III. PROGRAMME DESIGN
Based on these recommendations, the department had to deconstruct and re-organise the current traditional teaching approach where basic sciences are taught in separate modules in years 1 to 2 while topics in pharmacy practice and therapeutics are introduced from years 3 to 4; with work-place learning happening only after year three. A Curriculum Design Group (CDG) was established to dissect and develop the curriculum. The CDG adapted the key competencies listed in the Association of Faculties of Pharmacy in Canada Educational Outcomes for First Professional Degree Programs in Pharmacy (Association of Faculties of Pharmacy of Canada, 2017) as the basis for the competency-based curriculum. The students will learn to approach pharmacy practice by skilfully integrating sub-competencies of communicator, collaborator, leader-manager, scholar-innovator, health advocate and professional roles into an overarching care provider role. The scholar role is expanded to scholar-innovator role as innovation aligns well with the core value of NUS and is also a critical attribute to safeguard against future disruptions. The key competencies under each role are carefully mapped onto the learning outcomes of themed modules. The themed modules (based on physiological systems) are designed using a theoretical framework of integrating basic, clinical and systems sciences (Gonzalo et al., 2017) (Figure 1). To help students make sense of what they learn, experiential learning is incorporated longitudinally across the four years so that students can apply their theoretical studies at the workplace when they go on clinical placements (Figure 1). This 3-pillar educational framework has been successfully applied in medical education in the US to develop medical competencies and systems thinking among the physicians (Gonzalo et al., 2017); the CDG believed that the same framework would work for pharmacists in Singapore.
Pharmacy graduates must be prepared for a health system that is driven by informatics and technology. Joseph Aoun in his book “Robot-Proof: Higher Education in the Age of Artificial Intelligence” (Aoun, 2017) recommended undergraduate students to acquire technical, data and human literacies, which he collectively refers to as the “humanics”, for them to stay ahead of the technological revolution. Therefore, subjects such as medical sociology, computational thinking, health informatics are included to cultivate the humanics in the pharmacy students. It is envisaged that this approach can better prepare the graduates to work with patients, co-workers, data and technologies in providing quality care. Furthermore, instilling characteristics of a transformational leader and familiarising students to implementation science will take a step closer to grooming the student pharmacists into future leaders.
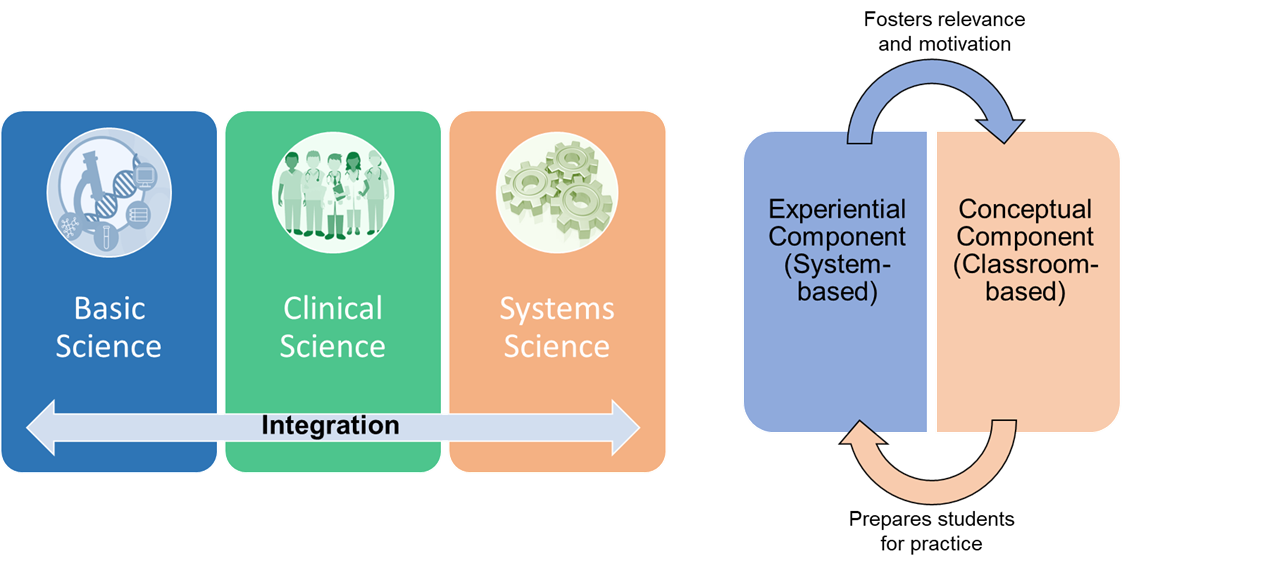
Figure 1: The theoretical framework of curricular integration. Adapted from Gonzalo et al. (2017) and Pearson and Hubball (2012).
In the new programme, students are made accountable of their own learning through pre-class preparations and interactive team-based learning (TBL) in the classroom. TBL sessions are facilitated by a scientist and a clinician who help students to use integrative thinking to solve the cases. In the laboratory, students will also work in teams to gather scientific data for inquiry-based learning. The impact of the new educational approach will be evaluated against all the four levels of the new world Kirkpatrick Model to determine the effectiveness of the curriculum.
IV. TRANSFORMING PHARMACY EDUCATION IN RESPONSE TO THREATS
The fourth industrial revolution has indeed caused disruptions to pharmacy practice. Pharmacists will have to step forward and be leaders of change when it comes to any matter related to medicines, be it optimising drug use, identifying drug-related problems or recommending cost-effective therapy. Therefore, it is the mission of NUS Department of Pharmacy to respond to the threats by transforming its professional pharmacy programme to one that can future proof its graduates who will be ready to seize new opportunities in a dynamic health system.
Notes on Contributors
Professor Christina Chai is the Head of the Pharmacy Department at NUS. She initiated the EduRx project by calling for the need to redesign the professional pharmacy degree curriculum to better prepare the graduates for the evolving healthcare landscape in Singapore.
Associate Professor Ho Han Kiat, in the capacity of the Deputy Head (Education), supported the curriculum design group in ensuring that the new pharmacy curriculum is closely aligned to both the NUS educational philosophy and the educational outcomes for pharmacy graduates.
Professor Paul Gallagher and Associate Professor Chui Wai Keung are co-leaders of the EduRx project who under their co-leadership worked with the curriculum design group to develop the competency-based and integrative pharmacy programme.
Acknowledgements
The authors would like to acknowledge the contributions made by the curriculum design group that comprises the following members: Chng Hui Ting, Fan Wenjie, Han Zhe, Priscilla How, Law Hwa Lin, Eugene Lim Zi Jie, Anson Lim Zong Neng, Tan Bee Jen, Matthias Gerhard Wacker, and Yeo Shao Jie.
Funding
There is no research funding source for the programme review project.
Declaration of Interest
The authors declare no conflict of interest concerning any aspect of this case study.
References
Aoun, J. (2017). Robot-proof: Higher education in the age of artificial intelligence. The MIT Press.
Association of Faculties of Pharmacy of Canada. (2017). AFPC educational outcomes for first professional degree programs in pharmacy in Canada 2017. https://afpc.info/system/files/public/AFPC-Educational%20Outcomes%202017_final%20Jun2017.pdf
Gonzalo, J. D., Haidet, P., Papp, K. K., Wolpaw, D. R., Moser, E., Wittenstein, R., & Wolpaw, T. (2017). Educating for the 21st-century healthcare system: An interdependent framework of basic, clinical and systems sciences. Academic Medicine, 92 (1), 35-39. https://doi.org/10.1097/ACM.0000000000000951
Husband, A. K., Todd, A., & Fulton, J. (2014). Integrating science and practice in pharmacy curricula. American Journal of Pharmaceutical Education, 78 (3), 63. https://doi.org/10.5688/ajpe78363
Pearson, M. L., & Hubball, H. T. (2012). Curricular Integration in Pharmacy Education. American Journal of Pharmaceutical Education, 76 (10), 204. https://doi.org/10.5688/ajpe7610204
*Wai Keung Chui
Department of Pharmacy,
Faculty of Science,
Block S4A, 18 Science Drive 4,
Singapore 117543.
Tel: +65 6516 2933
Email: phacwk@nus.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









