Enhancing the student experience through sustainable Communities of Practice
Submitted: 29 March 2021
Accepted: 28 September 2021
Published online: 4 January, TAPS 2022, 7(1), 102-105
https://doi.org/10.29060/TAPS.2022-7-1/SC2508
Mairi Scott & Susie Schofield
Centre for Medical Education (CME), School of Medicine, University of Dundee, Scotland, United Kingdom
Abstract
Introduction: The switch to online off-campus teaching for universities worldwide due to COVID-19 will transform into more sustainable and predictable delivery models where virtual and local student contact will continue to be combined. Institutions must do more to replace the full student experience and benefits of learners and educators being together.
Methods: Our centre has been delivering distance blended and online learning for more than 40 years and has over 4000 alumni across five continents. Our students and alumni come from varied healthcare disciplines and are at different stages of their career as educators and practitioners. Whilst studying on the programme students work together flexibly in randomly arranged peer groups designed to allow the establishment of Communities of Practice (CoP) through the use of online Discussion Boards.
Results: We found Discussion Boards encouraged reflection on learning, sharing of ideas with peers and tutors, reduce anxiety, support progression, and enable benchmarking. This led to a highly effective student sense of belonging to each other, our educators, and the wider University, with many highlighting an excellent student experience and maintaining a thriving CoP within the alumni body.
Conclusion: Despite being based on one large postgraduate programme in medical education, our CoP approach is relevant to any undergraduate programme, particularly those that lead to professional qualification. With our mix of nationalities, we can ‘model the way’ for enabling strong CoP’s to share ideas about best practice with a strong student and alumni network which can be shared across the international healthcare community.
Keywords: Communities of Practice, Sense of Belonging, Student Experience
I. INTRODUCTION
The sudden switch to online, dual delivery and on-campus/off-campus teaching for Universities worldwide will not be reversed at the end of the current COVID-19 crisis but will transform into a more sustainable and predictable delivery model where virtual and local student contact will continue to be combined. The switch, known as Emergency Remote Teaching (ERT) (Hodges et al., 2020) achieved much in a short timeframe but institutions need to do more to truly replace the full student experience and benefits of learners and educators being together on-site. The need for this new approach is acute in professional-based courses such as medicine where students need to learn complex skills within the context of healthcare delivery. These skills are acquired through multiple interactions with clinical colleagues in the workplace which, although often brief, are focused in real-time.
Given that the learning environment is dependent on the institutional ‘personality, spirit, and culture’ (Holt & Roff, 2004, pp. 553), human interaction is necessary to create that culture. We must develop new approaches to delivering medical education by merging established educational technologies with virtual approaches to establish on-line interaction with peers and senior colleagues such as can be achieved in Communities of Practice (CoPs) (Lave & Wenger, 1991). CoPs are social structures where people can share ideas, stories, and experiences relevant to the community’s activities. They help participants make sense of new knowledge and enable novices to benefit from working with experts, thus reducing anxiety, supporting progression, and enabling benchmarking. These components lead to the creation of a rich environment for information-sharing which has become increasingly important within healthcare delivery organisations during the COVID-19 pandemic.
We have built on over 40 years’ experience of delivering distance, blended and online Masters-level accredited medical education learning across five continents to ‘model the way’ to providing a strong student experience for online learners. Our students and alumni come from various interdisciplinary healthcare disciplines, at different stages of their career as educators and practitioners.
II. METHODS
Several Discussion Boards (DBs), usually one per study week plus one for assignment questions are created in each 12-week Moodle-based module. Students are randomly assigned to groups to work together flexibly within these peer groups. Each discussion has a ‘prompt’ linked to that week’s work, designed to create CoPs and a highly effective student sense of belonging (SoB) to each other and programme educators. In the first module students are actively encouraged to participate, with emphasis being on the ‘safe space’ created that allows them to learn effectively from and with each other. DB comments are used as part of programme enhancement and quality assurance. Students give informed consent to their evaluation comments within DBs being extracted for overall programme review.
III. RESULTS
As students move from legitimate peripheral participant to experienced member, they often express increased confidence that their posts will allow them to share their view and help colleagues. The forum posts have been analysed as part of a much larger study; the following diagram (Figure 1) highlights some of the benefits.
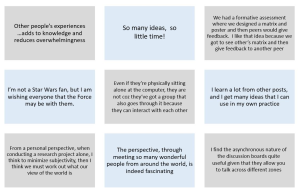
Figure 1. Sample of comments in DBs posts
Our experience over the last four years is that student levels of interaction increase the further into the programme they go, suggesting that they value and enjoy it. Overall, when asked specifically if that assumption is correct, feedback from students is exceptionally positive and they comment on their achievement of a SoB through engagement with the DBs. Many highlight the excellent student experience. Another indirect indication of success is that student module success rate averages 93% across the modules, which is high for an online learning programme.
The benefits of using DBs are threefold:
- They allow for reflection on learning in real-time due to regular module-specific weekly activities requiring students to reflect on that week’s educational materials and post their thoughts on the DBs.
- They allow sharing with peers and tutors, establishing CoPs: The DB posts create peer-to-peer dialogue, encouraging students to practise the language of the discipline in a safe, supported environment. Learning activities are based on the principle of linking previous experience with the interpretation of new knowledge, thus enabling an escalation of the complexity of questions to enhance deeper connection and dialogue. Although essentially (and importantly) it is the students as peers who are encouraged to respond to each other’s questions and comments, the tutors do monitor posts, providing input when necessary and desirable. In some modules, students are required to give peer feedback on draft assignments using a 1:4 ratio to encourage a range of views and expertise, increasing the depth and extent of their critical thinking and analysis. This also gives them practice in giving and receiving feedback, an essential skill for future medical educators.
- CoPs build trust in colleagues and a SoB within the learning environment, leading to an excellent learning experience. Students state that they value the tutor contribution as this increases the confidence they have in their own online comments, sometimes shifting the discussion to a more profitable area for new learning in a way that was not pre-planned or even at times expected.
IV. DISCUSSION
Our approach to the creation of CoPs is based on the principle that in order to establish student trust and a SoB DBs are an essential tool. Management research describes trust within organisations as being multifaceted, with the main components being capability, well-meaning intent, and integrity (Ridings et al., 2002). It is accepted that within our programmes both tutor and student capabilities have been established. Integrity is established by clearly explaining the expected mode of student behaviour at the outset and demonstrated as students work through the programme. Well-meaning intent is demonstrated by acts of positive reciprocation built up over time by asking students to give peer feedback frequently and around increasingly complex activities. Both integrity and well-meaning intent therefore need to have a continued focus during module design and delivery and throughout the assessment process.
Now that medical education has been forced to re-evaluate the place of online learning as a consequence of the COVID-19 crisis, it seems inevitable that many of the discovered benefits will lead to significant changes in the way we teach and learn. Davis (2018) explored a future medical school being one ‘without walls’ by which he meant that the artificial separation of the ‘classroom and the clinic’ would inevitably diminish as we embraced flipped classrooms and online collaborative learning.
If we adopt this approach for student learning it may also change the way we think about faculty development, as we could create extensive networks of faculty development special interest grouped CoPs beyond the ‘walls’ of our own schools. A recent study by Chan et al. (2018) in McMaster describes the creation of a Faculty Incubator – a virtual CoP which uses a longitudinal, asynchronous, online platform to deliver a one-year curriculum to support early-to mid-career educators from 30 different locations with their professional development. This widespread (geographically) collaborative approach was found to be well received, with lively interactions which broke down some of the boundaries that normally prevent early career academics from approaching unknown colleagues in different locations, colleagues they would normally never have met in person.
An additional challenge created by the COVID-19 pandemic was the necessity for healthcare professionals to make clinical decisions in an ‘evidence-poor’ disease by gathering emerging data (often by word-of-mouth) and treating patients without the certainty of a knowledge base built up over decades of robust randomised controlled trial (RCT) evidence. This is described by Rosenquist (2021, pp. 8) as a kind of “Bayesian fatigue”: a stress-induced dysphoria experienced when the corpus of knowledge that is the foundation of one’s work acquired over decades, becomes less important than information being gathered from disparate sources in real time.’ The ‘disparate sources’ referred to here are groups of widely dispersed practitioners (within current and new CoPs) who are sharing individual and collective rapid learning by experience that has become necessary when treating patients with COVID-19. These CoPs are based on the collective trust healthcare professionals express in valuing the views of colleagues struggling with similar challenges. This helps reduce that ‘Bayesian’ impact when it comes to making difficult clinical decisions in real time with limited evidence. However, trust within a CoP also comes from previous positive experience of being within other CoPs, and so it is important that we as medical educators enable our students to have experience of the value of sustainable CoPs in their own learning. Despite the limitations of the range of the study comments, we believe that given the extent of the sudden switch to ERT our findings of use of DBs to establish much appreciated CoPs justifies early dissemination through this short communication.
V. CONCLUSION
As medical educators we must have the skills necessary to establish strong and sustainable CoPs to educate current and future healthcare professionals in this effective way of learning from each other. This can be done as effectively with online learning as with on-campus interaction, allowing the possibility of the widespread creation of truly effective international CoPs sustainable for years to come.
Notes on Contributors
Professor Mairi Scott reviewed the literature, selected the data, wrote the manuscript, created the presentation and presented the materials virtually to the Conference. Dr Susie Schofield reviewed the literature, advised on the selection of the data and gave critical feedback on the manuscript. Both authors have read and approved the final manuscript.
Ethical Approval
Ethics approved was granted by School of Medicine & School of Life Sciences Research Ethics Committee, University of Dundee, Dundee, DD1 4HN on 03/05/19. Application Number: 19/41.
Data Availability
Ethical approval specified that raw data would not be made available for others out with the Centre ‘beyond the anonymised published or reported versions within the dissemination strategy’.
Acknowledgement
The authors would like to thank Dr Thillainathan Sathaananthan (PhD student) and Dr Linda Jones (PhD supervisor, Senior Lecturer) CME, University of Dundee, who produced some of the outcomes as part of research into student experiences with online learning and the use of Discussion Boards.
Funding
No grant or external funding was received for this work.
Declaration of Interest
Both authors have no conflict of interest to declare.
References
Chan, T. M., Gottlieb, M., Sherbino, J., Cooney, R., Boysen-Osborn, M., Swaminathan, A., Ankel, F., & Yarris, L. M. (2018). The ALiEM faculty incubator: A novel online approach to faculty development in education scholarship. Academic Medicine, 93(10), 1497–1502. https://doi.org/10.1097/ACM.0000000000002309
Davis, D. (2018). The medical school without walls: Reflections on the future of medical education. Medical Teacher, 40(10), 1004–1009. https://doi.org/10.1080/0142159X.2018.1507263
Hodges, C., Moore, S., Lockee, B., Trust, T., & Bond, A. (2020). The difference between emergency remote teaching and online learning. EDUCAUSE Review. https://er.educause.edu/%20articles/2020/3/the-difference-between-emergency-remote-teaching-and-online-learning
Holt, M. C., & Roff, S. (2004). Development and validation of the Anaesthetic Theatre Educational Environment Measure (ATEEM). Medical Teacher, 26(6), 553-558. https://doi.org/10.1080/01421590410001711599
Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation. Cambridge University Press.
Ridings, C. M., Gefen, D., & Arinze, B. (2002). Some antecedents and effects of trust in virtual communities: The Journal of Strategic Information Systems, 11(3-4), 271–295. https://doi.org/10.1016/S0963-8687(02)00021-5
Rosenquist, J. N. (2021). The stress of Bayesian medicine—Uncomfortable uncertainty in the face of COVID-19. New England Journal of Medicine, 384(1), 7-9. https://doi.org/10.1056/NEJMp2018857
*Mairi Scott
Centre for Medical Education,
University of Dundee
Email: m.z.scott@dundee.ac.uk
Submitted: 3 June 2021
Accepted: 4 October 2021
Published online: 4 January, TAPS 2022, 7(1), 76-86
https://doi.org/10.29060/TAPS.2022-7-1/OA2547
Nadia Greviana1,2, Dewi Anggraeni Kusumoningrum2, Ardi Findyartini1,2, Chaina Hanum1 & Garry Soloan1,3
1Medical Education Center, Indonesian Medical Education & Research Institute (IMERI) Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia; 2Department of Medical Education, Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia; 3Undergraduate Program in Medicine, Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia
Abstract
Introduction: As significant autonomy is given in a Massive Open Online Course (MOOC), online self-regulated learning (SRL) ability is crucial in such courses. We aim to measure the online SRL abilities of early-career medical doctors enrolled in a MOOC.
Methods: We performed a cross-sectional study using the Self-Regulated Online Learning Questionnaire-revised version (SOL-Qr). We conducted a three-stage cross-cultural validation of the SOL-Qr, followed by Confirmatory Factor Analysis (CFA). The online SRL ability of 5,432 medical doctors enrolled in a MOOC was measured using the validated SOL-Qr.
Results: The CFA of the cross-translated SOL-Qr confirmed its comparability to the original version, with excellent validity & reliability. Participants showed high levels of online SRL during their early careers. Despite high online SRL scores, MOOC completion rate was low. Male participants showed slightly better time management ability than female participants. Participants working in the primary epicentrum for COVID-19 in the country showed lower online SRL scores, while participants who graduated from higher accreditation levels showed better time management ability.
Conclusion: The SOL-Qr and its subscales are suitable and valid for measuring the online SRL abilities of medical doctors in a MOOC during their early-career period. Time management ability was associated with previous experience during the medical education period, while other online SRL subscales were mostly associated with workload. However, as the scores did not correlate with the time spent for learning in MOOC, the corresponding learning effort or time spent may be beyond just the commitment to the described MOOC.
Keywords: Self-Regulated Learning, MOOC, Online Learning
Practice Highlights
- It is important to take into account learners’ online SRL ability in MOOCs as it is dynamic across online learning contexts.
- The use of the SOL-Qr is beneficial for providing learners’ online SRL profiles in MOOC during medical doctors’ early career period.
- Understanding online SRL abilities helps MOOC developers to evaluate learning activities in MOOC and support learners’ online SRL ability.
I. INTRODUCTION
Massive Open Online Courses (MOOCs) are open academic platforms in which students can access learning resources interactively. The self-paced nature of MOOCs provides time-flexibility, facilitating deeper learning (Bullock & De Jong, 2013). MOOCs are useful for replacing direct interaction for knowledge transfer and learning processes during the ongoing pandemic because they utilise various formats, such as video lectures, reading resources, assignments, tests, and asynchronous discussion within the platform (Sandars & Patel, 2020). Because MOOC’s aim to give learners useful resources and empower teachers to provide vital knowledge, curation of the platform, with its copious information, it is beneficial for achieving high-quality content that fits the learning objectives and learners’ characteristics (Asarbakhsh & Sandars, 2013). As demand for technological solutions in education rise during the COVID-19 pandemic, MOOCs have been promoted as forms of disruption that accelerate adaptation to balance safety with the achievement of competencies by medical students and graduates (Hall et al., 2020; Liang et al., 2020).
MOOCs have generally been designed as open in access, location, pace, and time of completion; therefore, learners must control their learning process. Learning goals are usually set less strictly in MOOCs than in other courses. Unlike traditional, face-to-face teaching, MOOCs require highly engaged & strategic students. Learners must plan their study, set goals, evaluate their knowledge related to the course material, adapt their learning strategies, and assess their performance. They are solely responsible for managing their time and study environment (Jansen et al., 2017).
With high enrollment rates, the majority of learners fail to complete MOOCs, for various reasons: lack of time, insufficient prior knowledge, inadequate supervision, and difficulties in understanding the course materials (Hew & Cheung, 2014). Time management, effort regulation, metacognition, and critical thinking as part of Self-Regulated Learning (SRL) relate to success in online academic activities (Broadbent & Poon, 2015). Because MOOCs give students significant autonomy in completing the course, SRL is crucial for successful completion of MOOCs (Chung, 2015; Wong et al., 2018).
SRL encompasses a student’s ability to actively and constructively control their thoughts, acts, and emotions towards learning objectives (Jouhari et al., 2015), using the cycle of forethought, performance, and self-reflection phases, which should be implemented in an online learning environment (Panadero, 2017). Various external factors may interplay and affect self-regulated learning among students. This underscores the importance of a supportive family, helpful peers, and motivational, feedback-centered instruction methods; together, these factors support SRL (Jouhari et al., 2015).
Virtanen and Nevgi (2010) recognised gender as a factor affecting how SRL is perceived by students, especially during the forethought stage; they found that male students scored slightly higher on the sub-scale for self-efficacy, while female students demonstrated greater help-seeking strategies, performance anxiety, and beliefs in the value of studying. Bembenutty (2009) also found that female students perceive learning as a more valuable task in SRL than male students do.
Several instruments were developed to measure SRL, including structured interviews like the Self-Regulation Interview Schedule (SRLIS), questionnaires, teachers’ judgments, think-aloud techniques, and performance observations (Magno, 2011). The Motivated Strategies for Learning Questionnaire (MSLQ) is a common measure of SRL. It assesses two aspects: motivational orientation—encompassing values, expectations, and affective components—and the use of different learning strategies, e.g. cognitive and metacognitive strategies or resource management strategies (Pintrich et al., 1993). Another instrument for measuring students’ SRL in higher education is the Academic Self-Regulated Learning Scale (A-SRL-S), evaluating memory strategy, goal-setting, self-evaluation, seeking assistance, environmental structuring, learning responsibility, and planning and organising (Magno, 2011).
In the context of online learning, several instruments have been developed to measure students’ SRL, such as the Online Self-regulated Learning Questionnaire (OSLQ) and the Self-regulated Online Learning Questionnaire (SOL-Q). The OSLQ consists of six subscales: environment structuring, goal-setting, time management, help-seeking, task strategies, and self-evaluation (Barnard et al., 2009). However, this questionnaire cannot measure SRL activities in the appraisal or self-reflection phase. Meanwhile, the SOL-Q was developed by Jansen et al. (2017), using other existing SRL questionnaires to measure SRL activities, specifically in MOOCs, for all three SRL phases: preparatory, performance, and appraisal. The SOL-Q consists of five sub-scales: metacognitive skills, environmental structuring, help-seeking, time management, and persistence (Jansen et al., 2017). In 2018, a revision was made to split the metacognitive skills scale into three subscales: metacognitive activities before, during, and after a learning task. The revised questionnaire (SOL-Qr) demonstrated improved validity, usability, and reliability (Jansen et al., 2018).
Recognising the importance of learners’ during the use of MOOCs—and that SRL is affected by various factors—we attempted to measure the online self-regulated learning of early-career medical doctors enrolled in a MOOC that provides essential knowledge about COVID-19 to support medical doctors’ early careers during the COVID-19 pandemic. We seek to answer the following questions in this study:
- Is the Self-Regulated Online Learning Question (SOL-Qr) valid for use in our setting?
- What is the profile of students’ SRL scores, and are there any relationships between the SRL score, course completion, gender, respondents’ former medical school, and internship location
II. METHODS
A. Context
With approximately 270 million inhabitants across 34 provinces, Indonesia is one of the largest archipelagos in the world. According to a recent report, there is one medical doctor per 2500 people across the country (National Ministry of Health, 2020). Recently graduated medical doctors must undergo a one-year compulsory internship program upon graduation, where they serve as front-liners in primary health care settings across the country to serve in societies in very diverse sociocultural contexts and ethnicities. Those who graduated in 2020, mostly finished high school and entered medical schools in 2013–2014, completed their clinical stages and graduated from different medical schools in Indonesia at the beginning of the COVID-19 pandemic, during which some of the clinical duties in teaching hospitals were suspended and amended for safety reasons (Findyartini et al., 2020). A total of 93 public and private medical schools are distributed across Indonesia, all accredited by the National Accreditation Agency for Higher Education in Health with A-level as the highest accreditation indicating that the medical school has reached an established quality in teaching-learning processes and faculty members.
Considering the need for the newly graduated medical doctors serving as front liners to learn about the current pandemic situation and the importance of safety for both patients and healthcare workers, the Ministry of Health equipped these new graduates with essential COVID-19 knowledge before their involvement in patient management during the ongoing pandemic. Given the geographical reality of the country’s archipelago and the nature of the workplace setting during the internship program, the use of a Massive Open Online Course (MOOC) was preferred.
Little was known about COVID-19 at the beginning of the pandemic. Guidelines created by organisations (such as the CDC and WHO) are mostly amended living documents based on newly published articles, data, and clinical expertise. Studies on COVID-19 are being conducted on a massive scale worldwide, which may create information overload and overwhelm learners, especially those serving as front–liners (Poonia & Rajasekaran, 2020). A MOOC approach would facilitate a prompt response for equipping medical and health students, professionals, and the broader community to learn about the pandemic situation and prepare them to contribute to the pandemic response in community and hospital settings (Ortiz-Martìnez et al., 2021).
B. The COVID-19 MOOC Description
All internship doctors in Indonesia batch 3 and 4 in 2020, were compulsorily enrolled in an open course on COVID-19 at the beginning of their internship period. The open course was sequenced into two, sequentially accessed parts. The mandatory part A consists of fundamental knowledge on COVID-19 (such as COVID-19 screening, triage, infection control, management of patients, preventive strategy, etc); Part B consists of supplemental knowledge about COVID-19 (such as management of patients with comorbidity, ethics, and medicolegal aspects, perioperative management, etc); it is optional for participants to choose which topics to learn based on their interests and needs. Participants were encouraged to complete Part A during the first two weeks of their internship program to ensure sufficient knowledge before their service. However, participants were given full access to revisit the MOOC for up to 9–12 months of their internship programs. More details on the online course are reported elsewhere (Findyartini et al., 2021).
C. Study Design and Instruments
Our cross-sectional study uses the SOL-Qr (Jansen et al., 2018), which was adapted to Bahasa Indonesia, to assess online self-regulated learning ability in a Massive Open Online Course. Secondary data were obtained from the Moodle-based MOOC platform, including the total number of respondents, gender, internship location, former medical school, and course completion.
SOL-Qr measures seven aspects of SRL as mentioned in Table 1. Respondents answer each item on a 7-point Likert scale (1 for “not at all true for me” and 7 for “very true for me”). This questionnaire was translated to Bahasa Indonesia and back-translated to English to ensure similarity in meaning. Cognitive interviews with four respondents resembling the study participants were also conducted to obtain clarity of the items. The two respondents in this phase were final year medical school students from the authors’ institution (prospective participants of the national internship program) and the other two respondents were medical doctors who have just completed the national internship program.
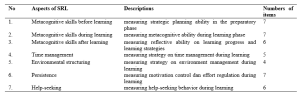
Table 1. Descriptions of SOL-Qr (Jansen et al., 2018)
Course completion, as analysed in this study, refers to the completion rate (in percentage) of the optional topics in part B that were accessed and completed by study participants in the open course.
D. Data Collection
Data were collected from the Moodle-based MOOC platform of the COVID-19 module from January to February 2021, two months after each course had started. This study uses a total sampling approach, with a minimum sample size of 204 respondents, calculated from standard deviation of 3.43 (Yen et al., 2016) and alpha (type I error) of 0.05 and beta (type II error) of 0.20 and 10% estimated drop out level.
All study participants were National Internship Medical Doctors in the year 2020 who were enrolled in the COVID-19 Open Course on the MOOC platform.
The SOL-Qr questionnaire was embedded in the evaluation questionnaire placed at the end of Part A, before participants moved forward to Part B. The questionnaire was completed voluntarily by participants who agreed to participate in this study. They were given adequate written information about the study and assured that there were no consequences of participation in regards to the course or the internship program evaluation. All data included in this study were collected from participants who signed and agreed upon the written consent embedded in the questionnaire. This study obtained ethical clearance from Faculty of Medicine Universitas Indonesia/ dr. Cipto Mangunkusumo General Hospital Research Ethics Committee Board (KET-1395/UN2.F1/ETIK/PPM.00.02/2020) in 2020.
E. Data Analysis
We conducted a three-stage validation process for the SOL-Qr, including the process of translation to Bahasa Indonesia by the research investigator, the back-translation process, and a review process by four newly graduated medical doctors who represented the characteristics of the study participants. This process ensured that the Bahasa Indonesia version of SOL-Qr was comparable to the original version. Furthermore, a Confirmatory Factor Analysis (CFA) was performed to confirm the model proposed by Jansen et al. (2018) as a fit model in the Bahasa Indonesia version compared to the original version. The fit model of CFA analysis determined whether normality, multicollinearity, residual values, and multivariate outliers were met. Furthermore, the Two-Index Presentation Strategy, the fit index combination of at least two indicators among the root mean square error of approximation (RMSEA), the standardised root mean square residual (SRMR), and the comparative fit index (CFI) all indicated the fit model of CFA analysis (Hu & Bentler, 1999; Schreiber et al., 2006). Internal consistency analysis of the Bahasa Indonesia version of SOL-Qr was also completed. Items were concluded as valid if the corrected item-total item correlation value was higher than 0.3. The questionnaire was considered reliable if alpha Cronbach ≥ 0.700; an alpha value higher than 0.900 indicates excellent internal consistency (Blunch, 2008).
All survey data obtained from the questionnaire were statistically analysed using IBM SPSS Statistic version 21. Demographic data were processed using descriptive statistics (proportion, mean, and standard deviation). Study participants were classified into two groups according to their internship location:
- Medical doctors who serve in Java- Bali Region, which was the primary epicenter of COVID-19 in the country in 2020.
- Medical doctors who serve in Outside Java- Bali Region.
We also classified participants according to their former medical school accreditation.
Bivariate analysis using the t-independent test was used to find relationships between the online self-regulated learning scores and gender, internship location, the former medical school, and the course completion. The Pearson correlation test was also used to analyse correlations between online SRL subscales and the course completion rate.
III. RESULTS
A. Validation of the SOL-Qr
The three stages of validation were conducted in the SOL-Qr instrument to ensure the content validity of the Bahasa Indonesia version of SOL-Qr. CFA was performed on the Bahasa Indonesia version of SOL-Qr, with the results showing the goodness-of-fit according to Hu and Bentler’s Two Index Presentation; the SRMR value was 0.056 (<0.08) while RMSEA value was 0.078 (<0.08). Meanwhile, the χ2/df value was < 0.001; the CFI value was 0.874 (Hu & Bentler, 1999). The model (Figure 1) also confirms the comparability of the subscales to the original SOL-Qr.
The Bahasa Indonesia version of SOL-Qr also shows excellent validity and reliability, with a Cronbach’s alpha of 0.974. The reliability of each subscale ranges from 0.971 to 0.975.
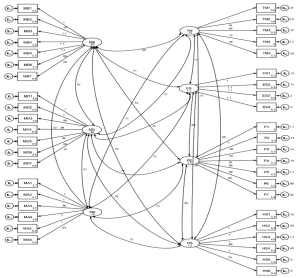
Figure 1. CFA results of the National Language Version of SOL-Qr (MB: Metacognitive Before, MD: Metacognitive During, MA: Metacognitive After, TM: Time Management, ES: Environmental Structuring, P: Persistence, and HS: Help Seeking)
B. Profile of Participants’ Online SRL Scores
A total of 5,846 internship doctors from all 34 provinces in Indonesia were enrolled and accessed the MOOC; as many as 5,432 participants, graduated from 74 medical schools (of which 46% are A-accredited while 54% are B-accredited), agreed to participate in the study (response rate of 92.9%). Details on the study participants are presented in Table 2.
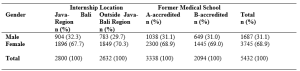
Table 2. Study participants (N = 5,432)
C. Relationship Between Online SRL Score, Course Completion, Gender, and Internship Location
Data on the online SRL scores and course completion were analysed according to gender, internship location, and medical school accreditation. The data are described in means and standard deviations, as they were normally distributed, as shown in Table 3.
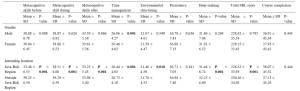

Table 3. Profile of online SRL and course completion according to gender, internship location, and medical school
According to Table 3, the average total scores of participants’ online self-regulated learning in all groups show high levels of online SRL (SRL score > 5). When comparing the male and female participants, the finding suggests that only the Time Management subscale shows a significant difference (p = 0.001). Male participants show higher scores in time management than female participants. Participants from the Outside Java-Bali Region had significantly higher online SRL scores in all subscales, except for the Persistence subscale (p = 0.181), than participants from the Java-Bali Region, which was the primary epicenter of COVID-19 in the country.
Meanwhile, the online SRL scores of participants who graduated from A-level versus B-level accredited medical schools mostly show similar online self-regulated learning scores, except in the time management scale (p = 0.009).
Although Table 3 shows no significant difference regarding course completion across gender, internship region, or former internship location, it does show a low course completion rate. Participants only completed less than approximately 40% of all optional topics in Part B.
The results of the Pearson correlation test show significant differences between the course completion rate and several SRL subscales, with very low correlation values (r < 0.1 in all subscales) for the SOL-Qr in the whole samples, as well as between the internship location and former medical education groups. Only the Time Management score was correlated to Course Completion in the Outside Java-Bali group, with a very low correlation value (r = 0.102). Therefore, the course completion rate does not correlate with the online SRL scores.
IV. DISCUSSION
Self-regulated learning is a dynamic process and may change while learners undergo various learning contexts (Barnard et al., 2009). The rapidly changing pandemic has accelerated the adaptation of new learning approaches and methods worldwide, including MOOCs that had gained popularity. Therefore, the use of the SOL-Qr is beneficial for providing MOOC learners’ SRL profiles (Jansen et al., 2018).
This study represents the first successful attempt to cross-culturally validate the SOL-Qr and determine the suitability of all its subscales for profiling online SRL of medical doctors in their early career. The three-stage validation process for the SOL-Qr was conducted as a form of cross-cultural adaptation of the instrument to facilitate its use in measuring self-regulated learning abilities in an online setting in the context of medical education—specifically in the MOOC used for continuing medical education and professional development programs for early-career, newly graduated medical doctors (Hambleton, 2005). The CFA conducted in this study also demonstrates a good fit, with excellent internal consistencies of the SOL-Qr and its subscales; this demonstrates the comparability of the instrument with the original SOL-Qr (Jansen et al., 2018).
The use of the SOL-Qr in this study demonstrates online SRL abilities during the transition phase in the early careers of medical doctors, from medical students to medical interns. This study demonstrates the high average level of online SRL ability among newly graduated medical doctors (SRL score > 5). Participants’ online SRL may increase due to the positive online learning experience obtained, considering that the knowledge on COVID-19 provided in this particular MOOC was vital and timely knowledge for these recent graduates. While participant perceptions of MOOCs have been reported elsewhere, it is known that positive perceptions of an online learning experience and environments are significantly correlated with the online SRL score (Abouzeid et al., 2021; Findyartini et al., 2020; Liaw & Huang, 2013).
The high scores for online SRL in our study were found in total and in most of the subscales, except for the metacognitive skills before learning (MB) scale in participants from the Java-Bali region. A similar finding on the low level of metacognitive ability was reported during the transition phase from preclinical to clinical learning, which was associated with previous clinical experience (Cho et al., 2017). Albeit being assessed using a different instrument, the decreased level of metacognitive skill in this study may also be affected by a similar factor. Since the Java-Bali Region had been the primary epicenter of COVID-19 in the country, with the greatest number of COVID-19 cases (69.41%) out of all other regions (National Ministry of Health, 2021), most interns in the Java-Bali Region may have experienced being removed from their duties at the beginning of the pandemic for safety reasons during their last clinical rotations as medical students (Findyartini et al., 2020). This may have caused discomfort because they felt useless and unable to contribute to patient care, further affecting their sense of competence and motivation, despite previous clinical experiences. Hence, this may have affected the process of goal-setting and reflecting on their prior knowledge during the transition to becoming medical interns (Dornan et al., 2014; Dubé et al., 2015).
Findings of this study demonstrate no significant correlation between online SRL and the number of optional topics achieved by participants. This result was supported by the fact that, despite the high level of online SRL ability depicted in this study, the duration of which participants accessed the compulsory Part A was lower than the expected minimum duration as estimated by course developers although we did not explore whether participants learned about COVID-19 from any other learning resources (Findyartini et al., 2021). The current study also supports the results of a previous study with similar findings regarding online SRL scores and academic achievement, although this study does report a significant relationship between online discussion and academic achievement (Abouzeid et al., 2021). The MOOC examined in this study does not provide two-way interactions among learners or between learners and instructors, which may affect the low number of optional courses completed.
Our study also shows that the online SRL scores of participants in the Outside Java-Bali Region were significantly higher (p < 0.001) across all scales than those of participants in the Java-Bali Region, except on the Persistence scale (p = 0.181). This suggests that participants in the Outside Java-Bali Region also have better time management, environmental structuring, and help-seeking abilities, which may relate to the workload at the internship locations. Participants in the Java-Bali Region face a higher workload and stress as front-liners in managing patients during the COVID-19 pandemic (as health educators, contact tracers, vaccinators, etc.). This aligns with other findings suggesting that an optimal workload determines the quality of students’ SRL in the early transition and adaptation phases (Barbosa et al., 2018).
Furthermore, the MOOC was given to the participants at the beginning of their internship programs, in which several orientations and patient management also took place. Hence, it is confirmed that the participants’ workload affected the time allocated to learn the MOOC (Eriksson et al., 2017). This study also suggests that the use of the MOOC for knowledge provision would preferably occur with sufficient time before immersion in other workplace-based learning experiences.
Hew and Cheung (2014) report few challenges in MOOC completion, including a lack of time and having other priorities to fulfill the course; therefore, time management ability remains crucial. The results of this study indicate that male participants had slightly better time management abilities than female participants. Although the absolute difference of the scores between groups is small, this study involved 5,432 respondents (much more than the minimum sample size), thus small differences in results can be statistically significant. As newly graduated doctors, study participants were interns who worked in a new environment hence new challenges regarding workplace relationships and workload may be faced. Previous studies show that female and male physicians may perceive these challenges differently (Babaria et al., 2009). Female physicians report that they feel uncertain and stressed when facing different clinical environments. Because they tend to need more time to adapt than male physicians (Malau-Aduli et al., 2020), completing a MOOC may not be their priority. Moreover, with masculinity/femininity level of cultural determinant, Indonesians have a clear cut between gender roles, thus affecting roles of female participants in most settings (Mangundjaya, 2013). Female participants may culturally face different roles in their personal lives, such as the expectation to perform housework and childcare, in addition to their internship obligation resulting in conflicting time and higher stress levels. The conflicting time and higher stress level in both work and personal life (Isaac et al., 2013) may influence female participants’ ability to commit time to learn and work and may explain the lower time management scores among female participants.
This study also highlights that, overall, the online SRL scores of participants graduating from the A-level and B-level of accredited medical schools show similar results, except on the time management scale (p = 0.009), where the participants from the higher level accredited schools show higher scores than the participants from the lower level accredited schools. Prior online learning experience has been reported as an important determinant of online learning success (Vilkova, 2019). For newly graduated doctors completing an internship program, prior online learning experience may be largely attributed to the use of online learning formally in their medical school’s curriculum. Our study suggests that the higher accredited medical schools may provide more online learning experiences, leading to better time management skills among the participants from this group. Furthermore, MOOC completion and the fulfillment of learning outcomes were determined by the forethought phase in the students’ SRL; thus, the goal-setting, self-efficacy, and task values should be emphasised by the participants and facilitated by the MOOC (Vilkova, 2019). Our study further indicates that time management in the use of the MOOC should be considered by learners in the forethought, performance, and self-reflection phases of their SRL; the planning stage of the MOOC development must determine the estimated completion time for the whole course and its sections about the course learning outcomes and the participant’s characteristics (Stracke et al., 2018).
Similar to the SRL ability in offline learning, our findings further imply the importance of accounting for learners’ online SRL abilities, which are dynamic across online learning contexts, including MOOCs. Certain characteristics of MOOCs, such as their open access and self-paced nature, stress the importance of online SRL ability, especially for MOOCs used in the transition phase in the early career of medicine. Therefore, using validated and reliable instruments, such as the SOL-Qr, to measure the online SRL abilities of MOOC participants would help course developers to identify whether the online learning context supports or hinders learners’ SRL abilities, thus helping course administrators further improve MOOC to provide further support for learners’ SRL (Barnard et al., 2009; Sandars & Patel, 2020).
V. LIMITATIONS OF THE STUDY
We identify several limitations of this study. As this study examined online SRL ability of participants using a self-reported questionnaire, it was unable to examine the actual online SRL ability, given the poor correlation with the course completion rate. Furthermore, as the evaluation of online SRL was only conducted once, it was not possible to observe changes in SRL ability throughout the use of the MOOC or in a longer period. With the data that we obtained, we were also unable to analyse whether participants used other online resources to learn about COVID-19 before the internship program or parallel with accessing the provided module as the marker of online SRL nor to explain any causal relationships between online SRL scores and the factors under investigation. However, measurement of online SRL ability using the cross-culturally validated SOL-Qr reveals that this instrument can be used for MOOCs on continuing medical education and professional development in the early-career context.
VI. CONCLUSION
Our study demonstrates the cross-cultural validity of the SOL-Qr and the suitability of its subscales for use in the medical and health fields. The results portray the online SRL ability of medical doctors as participants in a MOOC during the transition phase in their early career. We found that the time management ability was associated with previous experience during the medical education period, while other subscales were mostly associated with workload during the transition phase. However, as the scores did not correlate with the completion rate of MOOC, it can be concluded that the questionnaire is a possible valid tool to assess self-regulated learning in the MOOC environment. Yet, the corresponding learning effort or completion rate may be beyond just the commitment to the described MOOC.
Notes on Contributors
NG designed and led the study, led data collection and analysis, and led manuscript development. AF, DAK, and CH contributed in data collection, completed data analysis, and contributed to manuscript development. GS contributed in the data analysis and manuscript development. All authors approved the final version of the manuscript.
Ethical Approval
This study obtained ethical clearance from Research Ethics Committee of Faculty of Medicine Universitas Indonesia/ dr. Cipto Mangunkusumo General Hospital (KET-1395/UN2.F1/ETIK/PPM.00.02/2020) in 2020.
Data Availability
Data will be available upon request to corresponding author due to conditions of consent provided by respondents in this study and that it should abide data sharing policy from the authors’ institution and the Republic of Indonesia Ministry of Health.
Acknowledgement
The authors would like to acknowledge the Ministry of Health Republic of Indonesia for the trust that has been given to develop and organise the MOOC for the national internship program participants. We would also like to thank all national internship program participants for participation in this study and to Vernonia Yora Saki for assisting the authors with statistical analysis of the study. The preliminary results of this study were presented in Niigata Meeting 2020.
Funding
The development of MOOC and data analysis has been supported by the Ministry of Health Republic of Indonesia through a direct appointment decree to our institution.
Declaration of Interest
All authors state no possible conflicts of interest, including financial, consultant, institutional, and other relationships that might lead to bias or a conflict of interest.
References
Abouzeid, E., O’Rourke, R., El-Wazir, Y., Hassan, N., Ra’oof, R. A., & Roberts, T. (2021). Interactions between learner’s beliefs, behaviour and environment in online learning: Path analysis. The Asia Pacific Scholar, 6(2), 38-47. https://doi.org/10.29060/TAPS.2021-6-2/OA2338
Asarbakhsh, M., & Sandars, J. (2013). E-learning: The essential usability perspective. The Clinical Teacher, 10(1), 47-50. https://doi.org/10.1111/j.1743-498X.2012.00627.x
Babaria, P., Abedin, S., & Nunez-Smith, M. (2009). The effect of gender on the clinical clerkship experiences of female medical students: Results from a qualitative study. Academic Medicine, 84(7), 859-866. https://doi.org/10.1097/ACM.0b013e3181a8130c
Barbosa, J., Silva, Á., Ferreira, M. A., & Severo, M. (2018). Do reciprocal relationships between academic workload and self-regulated learning predict medical freshmen’s achievement? A longitudinal study on the educational transition from secondary school to medical school. Advances in Health Sciences Education, 23, 733-748. https://doi.org/10.1007/s10459-018-9825-2
Barnard, L., Lan, W. Y., To, Y. M., Paton, V. O., & Lai, S.-L. (2009). Measuring self-regulation in online and blended learning environments. The Internet and Higher Education, 12(1), 1-6. https://doi.org/10.1016/j.iheduc.2008.10.005
Bembenutty, H. (2009). Academic delay of gratification, self-regulation of learning, gender differences, and expectancy-value. Personality and Individual Differences, 46(3), 347-352. https://doi.org/10.1016/j.paid.2008.10.028
Blunch, N. J. (2008). Introduction to structural equation modelling using SPSS and AMOS. SAGE.
Broadbent, J., & Poon, W. L. (2015). Self-regulated learning strategies & academic achievement in online higher education learning environments: A systematic review. The Internet and Higher Education, 27, 1–13. https://doi.org/10.1016/j.iheduc.2015.04.007
Bullock, A., & De Jong, P. G. M. (2013). Technology-enhanced learning. In T. Swanwick (Ed.), Understanding medical education: Evidence, theory, and practice (2nd ed., pp. 149-160). Wiley Blackwell. https://doi.org/10.1002/9781118472361.ch11
Cho, K. K., Marjadi, B., Langendyk, V., & Hu, W. (2017). Medical student changes in self-regulated learning during the transition to the clinical environment. BMC Medical Education, 17(59). https://doi.org/10.1186/s12909-017-0902-7
Chung, L.-Y. (2015). Exploring the effectiveness of self-regulated learning in massive open online courses on non-native English speakers. International Journal of Distance Education Technologies, 13(3), 61-73. https://doi.org/10.4018/ijdet.2015070105
Dornan, T., Tan, N., Boshuizen, H., Gick, R., Isba, R., Mann, K., Scherpbier, A., Spencer, J., & Timmins, E. (2014). How and what do medical students learn in clerkships? Experience based learning (ExBL). Advances in Health Sciences Education, 19(5), 721-749. https://doi.org/10.1007/s10459-014-9501-0
Dubé, T. V., Schinke, R. J., Strasser, R., Couper, I., & Lightfoot, N. E. (2015). Transition processes through a longitudinal integrated clerkship: A qualitative study of medical students’ experiences. Medical Education, 49(10), 1028-1037. https://doi.org/10.1111/medu.12797
Eriksson, T., Adawi, T., & Stöhr, C. (2017). “Time is the bottleneck”: A qualitative study exploring why learners drop out of MOOCs. Journal of Computing in Higher Education, 29, 133-146. https://doi.org/10.1007/s12528-016-9127-8
Findyartini, A., Anggraeni, D., Husin, J. M., & Greviana, N. (2020). Exploring medical students’ professional identity formation through written reflections during the COVID-19 pandemic. Journal of Public Health Research, 9(s1). https://doi.org/10.4081/jphr.2020.1918
Findyartini, A., Greviana, N., Hanum, C., Husin, J. M., Sudarsono, N. C., Krisnamurti, D. G. B., & Rahadiani, P. (2021). Supporting newly graduate medical doctors in managing COVID-19: An evaluation of Massive Open Online Course in a limited-resource setting. PLoS ONE, 16(9), e0257039. https://doi.org/10.1371/journal.pone.0257039
Hall, A. K., Nousiainen, M. T., Campisi, P., Dagnone, J. D., Frank, J. R., Kroeker, K. I., Brzezina, S., Purdy, E., & Oswald, A. (2020). Training disrupted: Practical tips for supporting competency-based medical education during the COVID-19 pandemic. Medical Teacher, 42(7), 756-761. https://doi.org/10.1080/0142159X.2020.1766669
Hambleton, R. K. (2005). Issues, designs, and technical guidelines for adapting tests into multiple languages and cultures. In R. K. Hambleton, P. F. Merenda, & C. D. Spielberger (Eds.), Adapting educational and psychological tests for cross-cultural assessment (pp. 3–38). Lawrence Erlbaum.
Hew, K. F., & Cheung, W. S. (2014). Students’ and instructors’ use of massive open online courses (MOOCs): Motivations and challenges. Educational Research Review, 12, 45–58. https://doi.org/10.1016/j.edurev.2014.05.001
Hu, L.-t., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
Isaac, C., Petrashek, K., Steiner, M., Manwell, L. B., Carnes, M., & Byars-Winston, A. (2013). Male spouses of women physicians: Communication, compromise, and carving out time. The Qualitative Report, 18(52), 1-12. https://doi.org/10.46743/2160-3715/2013.1423
Jansen, R. S., van Leeuwen, A., Janssen, J., & Kester, L. (2018). Validation of the revised self-regulated online learning questionnaire. In V. Pammer-Schindler, M. Pérez-Sanagustín, H. Drachsler, R. Elferink, & M. Scheffel (Eds.), Lifelong Technology-Enhanced Learning (pp. 116-121). Springer. https://doi.org/10.1007/978-3-319-98572-5_9
Jansen, R. S., van Leeuwen, A., Janssen, J., Kester, L., & Kalz, M. (2017). Validation of the self-regulated online learning questionnaire. Journal of Computing in Higher Education, 29, 6-27. https://doi.org/10.1007/s12528-016-9125-x
Jouhari, Z., Haghani, F., & Changiz, T. (2015). Factors affecting self-regulated learning in medical students: A qualitative study. Medical Education Online, 20(1). https://doi.org/10.3402/meo.v20.28694
Liang, Z. C., Ooi, S. B. S., & Wang, W. (2020). Pandemics and their impact on medical training: Lessons from Singapore. Academic Medicine, 95(9), 1359-1361. https://doi.org/10.1097/ACM.0000000000003441
Liaw, S.–S., & Huang, H.–M. (2013). Perceived satisfaction, perceived usefulness and interactive learning environments as predictors to self-regulation in e-Learning environments. Computers & Education, 60(1), 14-24. https://doi.org/10.1016/j.compedu.2012.07.015
Magno, C. (2011). Validating the academic self-regulated learning scale with the Motivated Strategies for Learning Questionnaire (MSLQ) and Learning and Study Strategies Inventory (LASSI). The International Journal of Educational and Psychological Assessment, 7(2), 56-73.
Malau-Aduli, B. S., Roche, P., Adu, M., Jones, K., Alele, F., & Drovandi, A. (2020). Perceptions and processes influencing the transition of medical students from pre-clinical to clinical training. BMC Medical Education, 20, 279. https://doi.org/10.1186/s12909-020-02186-2
Mangundjaya, W. L. H. (2013). Is there cultural change in the national cultures of Indonesia? In Y. Kashima, E. S. Kashima, & R. Beatson (Eds.), Steering the cultural dynamics: Selected papers from the 2010 Congress of the International Association for Cross-Cultural Psychology. https://scholarworks.gvsu.edu/iaccp_papers/105/
National Ministry of Health. (2020, December 31). Health care workforce statistics database in Indonesia. Retrieved May 10, 2021, from http://bppsdmk.kemkes.go.id/info_sdmk/info/index?rumpun=101
National Ministry of Health. (2021, April 23). Current situations of the development of novel coronavirus (COVID-19). Retrieved May 10, 2021, from https://covid19.kemkes.go.id/situasi-infeksi-emerging/situasi-terkini-perkembangan-coronavirus-disease-covid-19-23-april-2021
Ortiz-Martìnez, Y., Castellanos-Mateus, S., Vergara-Retamoza, R., Gaines-Martìnez, B., & Vergel-Torrado, J. A. (2021). Online medical education in times of COVID-19 pandemic: A focus on Massive Open Online Courses (MOOCs), Educación Médica, 22, S40. https://doi.org/10.1016%2Fj.edumed.2020.12.001
Panadero, E. (2017). A review of self-regulated learning: Six models and four directions for research. Frontiers in Psychology, 8, Article 422. https://doi.org/10.3389/fpsyg.2017.00422
Pintrich, P. R., Smith, D. A. F., Garcia, T., & Mckeachie, W. J. (1993). Reliability and predictive validity of the Motivated Strategies for Learning Questionnaire (MLSQ). Educational and Psychological Measurement, 53(3), 801-813. https://doi.org/10.1177%2F0013164493053003024
Poonia, S. K., & Rajasekaran, K. (2020). Information overload: A method to share updates among frontline staff during the COVID-19 pandemic. Otolaryngology-Head and Neck Surgery, 163(1), 60-62. https://doi.org/10.1177%2F0194599820922988
Sandars, J., & Patel, R. (2020). The challenge of online learning for medical education during the COVID-19 pandemic. International Journal of Medical Education, 11, 169-170. https://doi.org/10.5116/ijme.5f20.55f2
Schreiber, J. B., Nora, A., Stage, F. K., Barlow, E. A., & King, J. (2006). Reporting structural equation modelling and confirmatory factor analysis results: A review. The Journal of Educational Research, 99(6), 323–338. https://doi.org/10.3200/JOER.99.6.323-338
Stracke, C. M., Tan, E., Moreira Texeira, A., do Carmo Pinto, M., Vassiliadis, B., Kameas, A., Sgouropoulou, C., & Vidal, G. (2018). Quality Reference Framework (QRF) for the Quality of Massive Open Online Courses (MOOCs): Developed by MOOQ in close collaboration with all interested parties worldwide. MOOQ. http://www.mooc-quality.eu/QRF
Vilkova, K. A. (2019, May 20-22). Self-regulated learning and successful MOOC completion [Europeaan MOOCs Stakeholders Summit 2019 Conference]. Proceedings of EMOOCs: Work in Progress Papers of the Research, Experience and Business Tracks.
Virtanen, P., & Nevgi, A. (2010). Disciplinary and gender differences among higher education students in self-regulated learning strategies. Educational Psychology, 30(3), 323-347. https://doi.org/10.1080/01443411003606391
Wong, J., Baars, M., Davis, D., Van Der Zee, T., Houben, G.-J., & Paas, F. (2018). Supporting self-regulated learning in online learning environments and MOOCs: A systematic review. International Journal of Human-Computer Interaction, 35(4-5), 356-373. https://doi.org/10.1080/10447318.2018.1543084
Yen, C.-J., Tu, C.-H., Sujo-Montes, L., & Sealander, K. (2016). A predictor for PLE management: Impacts of self-regulated online learning on students’ learning skills. Journal of Educational Technology Development and Exchange, 9(1), 29-48. https://doi.org/10.18785/jetde.0901.03
*Nadia Greviana
Faculty of Medicine Universitas Indonesia,
Jalan Salemba 6 Central Jakarta, Indonesia,
Email: nadiagreviana@ui.ac.id/ nadia.greviana@gmail.com
Submitted: 19 May 2021
Accepted: 26 August 2021
Published online: 4 January, TAPS 2022, 7(1), 66-75
https://doi.org/10.29060/TAPS.2022-7-1/OA2521
Lay Ling Tan1, Pim W. Teunissen2, Wee Shiong Lim3, Vanessa Wai Ling Mok1 & Hwa Ling Yap1
1Department of Psychological Medicine, Changi General Hospital, Singapore; 2School of Health Professions Education (SHE), Maastricht University, Netherlands; 3Cognition and Memory Disorders Service, Tan Tock Seng Hospital, Singapore
Abstract
Introduction: Development of expertise and counselling skills in psychiatry can be mastered only with effective supervision and mentoring. The conceptualisations of educational supervision amongst supervisors and residents were explored in this study to understand how supervisory roles may have been affected by the adoption of competency-based psychiatry residency training.
Methods: A qualitative research approach with thematic analysis was adopted. Individual in-depth interviews using a semi-structured interview guide with a purposive sample of six supervisors and six newly graduated residents were conducted. Transcripts of the interview were analysed and coded using the Atlas Ti software.
Results: Four major themes emerged from analysis of the transcripts: (1) Meaning and definition of supervision; (2) Expectations and responsibilities of the educational supervisor; (3) Elusiveness of mentoring elements in educational supervision and (4) Personal and professional development of residents in supervision. Supervisors and residents perceived educational supervision narrowly to be transactional with acquisition of knowledge and skills, but residents yearned for more relational interactions.
Conclusion: This study showed that the roles and functions of supervisors in educational supervision were unclear. It also highlighted the lack of a mentoring orientation in supervision in the psychiatry residency training program. An emphasis on assessment of competencies might have contributed to tension in the supervisory relationship and lack of a mentoring role, with concerns on residents’ personal and professional identity development in their psychiatry training.
Keywords: Psychiatry, Mentoring, Educational Supervision, Competency-Based Medical Education, Professional Identity Development
Practice Highlights
- Supervision in psychiatry has been described to encompass more than just a teaching and learning relationship but also a supportive and mentoring one.
- Educational supervision has been purported to offer the unique opportunity for effective mentoring within supervision.
- This qualitative study highlighted significant differences in definitions, roles and expectations of educational supervision.
- The conflict between mentoring and appraisal of competency needs to be addressed.
- Roles and expectations of the educational supervisor must be articulated clearly to both supervisors and residents.
I. INTRODUCTION
Postgraduate medical education (PGME) in Singapore underwent tremendous changes in the last decade. Before 2009, Singapore’s PGME was structured around time frames and curricular processes, in contrast to competency-based medical education (CBME) (Frank et al., 2017). In 2008, Singapore’s Ministry of Health (MOH) raised concerns of the lack of clear learning objectives and absence of measurable standards of training and outcomes with the medical schools and teaching hospitals. MOH recognised a need to ensure that every PGME graduate is prepared for clinical practice with the necessary competencies. With that vision in mind, MOH collaborated with the United States (US) Accreditation Council for Graduate Medical Education (ACGME) to revamp the PGME structure and accreditation system in 2009 (Chay, 2019). This move has resulted in major changes in the psychiatry postgraduate program. The 5-year National Psychiatry Residency Training Program was launched with a main teaching site and six sponsoring institutions. It also instituted the educational supervision framework where an assigned educational supervisor meets the supervisee regularly during the whole duration of training.
A. Concepts of Supervision
Supervision originated in professions outside of medicine (Launer, 2013) and is a distinct professional practice with specific articulated competence and training (Falender & Shafranske, 2007). It has been considered as a combination of various elements and is not a uniform concept (Carroll, 2006). Supervision is critical for ensuring effective professional practice of the healthcare sector (Tebes et al., 2011), particularly in psychiatry, where counselling skills can be developed only with effective supervision and mentoring.
1) Clinical supervision: Clinical supervision is subcategory to the wider concept of supervision. One definition is “provision of guidance and feedback on matters of personal, professional and educational development in the context of a trainee’s experience of providing safe and appropriate care” (Kilminster et al., 2007). There is consensual acceptance of the basic functions of clinical supervision: formative, supportive and managerial (Kilminster et al., 2007). These functions overlap depending on the context, problems emphasised and supervision goals (Kadushin, 1985).
2) Educational supervision: Educational supervision, on the other hand, has been described as regular supervision occurring in the context of a training program to determine learning needs and review progress of the supervisee (Passi, 2016). There has been extensive research done in clinical supervision (Kilminster et al., 2007; Patel, 2016) but educational supervision is under-researched with very few such studies conducted in psychiatry. It can be considered to be the most complex and challenging form of supervision as there are a number of overlapping and at times conflicting roles which need to be fulfilled (Launer, 2013). Aside from having to facilitate learning, there is also the need to evaluate the supervisee’s performance, which may result in confusion in the supervisory roles. Educational supervision has been purported to offer the unique opportunity for effective mentoring within supervision (Passi, 2016), which ideally should be recognised as an important component of the whole supervisory framework (Driessen et al., 2011).
B. Conceptual Framework for Educational Supervision in Postgraduate Psychiatry Training
Clinical and educational supervision are essential for development of health professionals and widely recognised as crucial for effective learning (Pront et al., 2016) and reflective practice (Schon, 1987). Learning in educational supervision can be conceptualised from experiential and social learning theory. Experiential learning is a key concept of the developmental-educational model of educational supervision (Kolb, 1984/2014). Learning is also a social process, where the supervisee is influenced by the cultural system of social knowledge and learns the trade with the guide of a more experienced colleague (Vec et al., 2014), a particularly important component in the field of psychiatry, a discipline closely related to the social sciences. Thus, there has been frequent reference to this apprenticeship model in supervision, although there is no clear definition of the term in the context of psychiatry training (MacDonald, 2002).
Supervision in psychiatry has its roots in psychoanalysis (Torby et al., 2015). Supervision in the context of general psychiatry training was mentioned infrequently and the concepts of supervision of the psychotherapeutic work of trainees were often transferred directly into the setting of general clinical supervision as if the two situations were identical (MacDonald, 2002). The supervisor can be seen as fulfilling the role of the analyst of the supervisee’s analytic ego (Akhtar, 2009). This necessitates a trusting relationship between the supervisor and supervisee, very much akin to that of informal mentoring, which has been described as psychosocial in nature and serves to enhance the supervisee’s self-esteem through interpersonal dynamics of the relationships, the emotional bonds they form and the work they accomplish together (Hansman, 2001). Supervision has also been frequently conceptualised as a development process or a process of identification (MacDonald, 2002). This is the transformation of a trainee through the acquisition of requisite knowledge, skills, attitudes, values, and attributes; from doing the work of a psychiatrist to being a psychiatrist (Wald, 2015). This active, constructive and transformative process has been referred to as professional identity formation (Wald, 2015). This continuous process requires the fostering of personal and professional growth through mentorship and self-reflection (Holden et al., 2015). The provision of guidance and mentoring with respect to personal and professional identity development would arguably be more critical in supervision in psychiatry. The personal aspects and the development of better self-awareness in the supervisee and the ‘internalised supervisor’ has been considered by some to be the fundamental goal of supervision (Kadushin, 1985). However, this will require the training program to allow sufficient time and opportunity to build and develop the supervisor-supervisee relationship.
With ACGME setting up collaborative initiatives with other countries and a trend towards a competency-based training approach, a better understanding of the impact of CBME on the supervision process and structure will be relevant to our international educators. The mentoring element in educational supervision has the potential to ensure that learning is not guided entirely by assessment and evaluation but is supplemented by the periodic guidance of a trusted mentor and addressing the personal and professional components in clinical supervision (Kilminster et al., 2007). With the implementation of the ACGME training framework, understanding the complexity and barriers of developing a mentoring relationship in educational supervision will be crucial. The research questions which this study aimed to answer were:
1. What are supervisors’ and residents’ perceptions on the educational supervisory role in the psychiatry residency program?
2. How do supervisors and residents perceive the supervisor’s mentoring roles in their educational supervision experience?
II. METHODS
A. Design
This was a qualitative research strategy where individual in-depth interviews with a purposive sample of six supervisors and six residents were conducted, the intent of which was to understand the participants’ meanings of the phenomenon of educational supervision (Creswell, 2014). Ethics approval was sought from the Institutional Review Board (CIRB Ref: 2017/2319) and informed consent was received from all participants.
B. Setting
The residency training program instituted the educational supervision framework by ACGME where an assigned educational supervisor meets the supervisee weekly of at least an hour duration. The educational supervisor is responsible for completion of the resident’s evaluation reports based on feedback gathered from the resident’s clinical supervisors and offer recommendations for the supervisee’s training progress. Clinical supervisors in the residency program are consultants managing patients together with the residents in the ward and clinic settings. Work-placed based assessments in the form of mini-clinical evaluations (mini-cex) and 360-degree feedback evaluations are done by both the educational and clinical supervisors.
There are six teaching sites in the psychiatry residency program and the researcher’s teaching site is one of the largest, with 18 supervisors overseeing nine to 12 residents posted in their various years of training. The setting of the research was the teaching site where the PI (Principal Investigator) served as Associate Program Director (APD).
C. Subjects
Six supervisors with two each from the Associate Consultant, Consultant and Senior Consultant group, and one male and one female from each group were invited to participate. For the residents, those who had just graduated from the residency program were invited. A total of six recently graduated residents (three males and three females) were sampled. This was to minimise biases related to fear of negative evaluation or power differentials while still undergoing residency training. It was hoped that with this purposive sampling, a relevant mix of supervisory experiences from the participants would be achieved.
D. Data collection
One-to-one semi-structured interviews were conducted by the PI using an interview guide (Appendix 1). The interview guide was developed by the PI with inputs from the research team. The interviews were audio-recorded with informed consent of the participants. Due attention was paid to the content of the participants’ sharing and the emerging themes during the interview and analysis process such that consideration of including more participants in the study would be taken if there was a need for further varied views to be elicited (Creswell, 2014).
E. Analysis
A qualitative research approach with thematic analysis was adopted. The Atlas Ti (version 8) software was used to code and analyse the data. Coding of all the data was made by the PI before a coding structure was created. There was a reiterative development and re-development of the coding structure such that all the data were appropriately accounted for. Codes were added and revised as more interviews were conducted. All the data were coded according to the study objectives and were classified into categories that reflected the emerging themes. Based on further readings in medical education literatures, the themes were grouped and sub-grouped in a logical fashion to form a thematic template. The raw data were revisited regularly throughout the analytic process to ascertain that the codes and resulting themes were grounded in the data. To ensure adequate coding and to improve the research reliability, we performed investigators’ triangulation. The co-investigator (LWS) was invited to analyse the first three interviews independently. The PI and co-investigators (TLL, VM, YHL) discussed regarding the main themes developed and differences were addressed and reconciled. To further improve credibility and transferability of the research data and its analysed results, member checking was used and participants’ comments regarding the developed themes were solicited. There was general agreement with the results generated from their interviews.
III. RESULTS
Six supervisors and six supervisees completed the study. As the research progressed, there was the progressive realisation of an overarching pattern emerging around the supervisory process, namely, the heterogeneity of the concept of supervision and the tension and conflicts amongst its various roles and functions.
Four major themes emerged:
- Meaning and definition of supervision
- Expectations and responsibilities
- Elusiveness of mentoring elements in educational supervision
- Personal and professional development in supervision
A. Meaning and Definition of Supervision
1) Supervisor’s perspectives: Supervisors defined supervision as “observing”, “helping”, “guiding”, “teaching”, “grading” and “assessing” the residents such that they could be certified to fulfil the program requirements. These descriptors suggested a supervisor-centric definition.
“Someone in a position of experience or age supervises, in other words…observe…teaches, impact knowledge and skills to the supervisee…is like watching somebody”
(S1)
2) Residents’ perspectives: Residents referred to supervision as an “apprenticeship”, “guiding and checking on progress” and promoting the “maturation as a clinician”. There was the repeated emphasis on the supervisor attending to the resident’s “growth”, “personal well-being” and to “encourage” and “commend”.
“…essentially is in line with the whole practice of medicine where there is apprenticeship, someone has to guide…to encourage, commend, growth…”
(R1)
B. Expectations and Responsibilities
1) Supervisor’s perspectives: Supervisors expected residents to be able to exhibit the attitude of being “able to talk about things and not being afraid of being judged”; “to pay attention to personal development so that the resident is more real as a person”; “to be ready to give feedback about supervision” and “being comfortable, open and trusting of the supervisor’s intentions”.
In practice, however, faculty observed that residents were “not expecting beyond helping them with clinical work”; “does not talk about struggles and frustrations” and were “not used to opening up”. Although engaging the resident with regards to their struggles was identified to be important, it was highlighted as “not the culture or consistently practiced” and that “residents may not appreciate why we want them to talk about their feelings”.
Faculty viewed discussing about resident’s personal issues as intrusive and a violation of the boundaries in supervision.
“We also have to keep some boundaries… we are careful not to go beyond certain boundary especially if it is something which the supervisee is not very comfortable with”
(S1)
Table 1 illustrates our faculty’s understanding of the roles and functions of the educational supervisor.
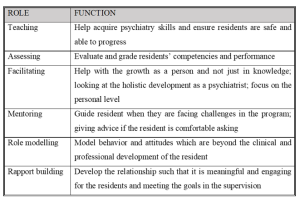
Table 1: Faculty’s understanding of the roles and functions of the educational supervisor
2) Residents’ perspectives: Residents’ expected the educational supervisor to be “approachable and open”, “easy to talk to”, “relaxed”, “able to attend to personal growth”, “helping to reflect” and “build rapport”. Residents thus expected a more relational as opposed to transactional interaction with the supervisor.
“…apart from the bread and butter clinical aspects of work…talk to you a bit more about your personal stage in life, how things are coming along… It is this stuff that I find it hard to find in textbooks or anywhere along the clear training roadmap”
(R1)
Residents tended to see the educational supervisor’s role as conflictual in view of the attendant assessor function, and how boundaries between the two roles are often not clearly delineated.
“Ultimately is quite hierarchical in the system…. so if a supervisee has a lot of problems and come to the supervisor for advice…the supervisor might negatively evaluate the supervisee”
(R2)
C. Elusiveness of Mentoring Elements in Educational Supervision
1) Supervisor’s perspectives: Faculty viewed mentoring as “broader”, “longer term” and “beyond clinical and professional development”. “Trust” and “special” characterised a mentoring relationship but the focus was more on “professional development” rather than “personal development”. Faculty did not see themselves as fulfilling a mentoring role but generally agreed that there could be opportunities in offering elements of mentoring in educational supervision and to “contribute to the growth of residents beyond the short-term focus on clearing examinations”.
“…take about certain other aspects you know…mentorship if possible…beyond the pure clinical and professional development”
(S1)
Supervisors alluded to their roles in educational supervision as “facilitating the growth as a person”; “giving advice” and “role modelling” but they did not consider these as mentoring roles even though these were generally accepted as mentoring in nature.
“…never seen myself in a mentoring position…mentoring goes beyond just the supervisor-supervisee relationship…but I don’t think it has really extended beyond that”
(S3)
2) Residents’ perspectives: There was a similar reference to mentoring as “adopting a broader view of the development of the resident” over “a longer period of time”. Residents described mentoring as having a “deeper emotional connect” and “beyond the clinical development”. The evaluator role was viewed as potentially inhibiting the development of a mentoring relationship.
“So, it muddles the role…when they are so tied up to assess…they may not be able to mentor as much…”
(R1)
D. Personal and Professional Development of Residents
1) Supervisor’s perspectives: Professional development was referred to as the “professional attitudes and motivation”, “duty of care”, “ethical boundaries” and the attributes which are more “formal” as contrasted to personal development. The latter being referred to as “one’s character”, “temperament”, “personality”; “the way we see things”; “development of self-awareness and self-actualisation” and the “need to know yourself and what problems you have in order to be able to help your patients struggling with personal problems”. Faculty also referred to personal development as “developing as a person and handling of stress”, “how to handle complaints”, and “how to juggle various roles to have a work-life balance”. Other views of personal development included “extracurricular activities outside of psychiatry” and “some hobbies” which some faculty opined as “more important in psychiatry because of the importance for self-care”.
However, some faculty held the opposing view that personal development should not be the focus of educational supervision. Lapses in personal development would only be brought up during supervision if there were “negative effects on professional roles and clinical practice and impeding progress” for risk of being accused of “prying into the residents’ personal lives and being nosy”.
“…but I don’t focus so much unless they hinder the work side of things. But maybe we should…”
(S3)
The reluctance of some residents to discuss issues of personal development were interpreted as an “Asian thing”, for instance being “uncomfortable” talking about personal struggles and “residents not expecting it”’.
2) Residents’ perspectives: Residents’ referred to personal developmental aspects as “be as a person”, “religious growth”, “personal well-being”, “how you are getting on with life as a whole”, “finding out about the person’s preferences”, “strengths and weaknesses” and “outside of the career”.
There was the fear of the lack of confidentiality and of being evaluated negatively if residents were to portray themselves as having personal struggles.
“though resident want to grow and develop but exposing these shortcomings could be very sensitive…”
(R1)
Residents considered personal aspects of their development to be “more private”; “should not be covered unless interferes with professional development”; “not so important”; “not fair for the supervisee and supervisor” and “something you should sort out on your own”. They perceived supervision to be formal and mainly moments of assessment for their professional development and so it would be inappropriate to discuss about personal struggles. Some residents also held the view that “personal and professional lives are separate” and the “supervisor may not be interested”.
“…to say that the supervisor should cover personal growth I don’t think that is very fair as well”
(S4)
IV. DISCUSSION
A. Conceptualisation of Educational Supervision
The concept of educational supervision was alien to both residents and supervisors. Supervision was seen mainly as teaching the residents to acquire knowledge and clinical skills with a focus on the transactional aspects. Our residents preferred a more relational supervisory interaction. The finding of psychiatry trainees valuing a supervisor’s emotional supportiveness more highly than clinical competence was also reported in another study (Chur-Hansen & McLean, 2007).
Our results showed that roles of teaching and assessing were more consistently endorsed by the supervisors. Relational roles like facilitating, role modelling, rapport building, and mentoring were considered important but cited less frequently by both groups. Participants tended to attribute this to the training’s emphasis on evaluation and assessment such that the focus of the supervision was more on the transactional rather than the relational components. This might have resulted in tension within the supervisory relationship as expectations for assessment of competencies take precedence (Julyan, 2009). This phenomenon was both ironic and worrying as the original intention for setting up the supervisory framework in the psychiatry residency program was to ensure that the training and learning would be supplemented by the presence of an educational supervisor with a mentoring role, entrusted with the fostering of the personal and professional components in clinical supervision (Kilminster et al., 2007).
B. Assessor Role of Supervisors
Although residency assessments were mainly formative, residents in our study still harbored concerns about the supervisor fulfilling the assessor role and determining their readiness to progress. If assessments were to be perceived as high stake in our examination-oriented training environment, the role of the teacher as helper might be compromised (van der Vleuten et al., 2012). As highlighted by the data in our study, combining the roles of helper and judge could confront the supervisor with a conflict of interest (Cavalcanti & Detsky, 2011). There might be situations either of inflation of judgement (Govaerts et al., 2007) or trivialisation of the assessment process (Dudek et al., 2005), which would potentially impair the professional development of the residents.
C. Personal and Professional Development
There was a common reference by both faculty and residents to the growth of the resident. Based on our data, there appeared to be some overlap of the concept of personal and professional development of residents in psychiatry training. Supervisors viewed the ability to handle stress and developing resilience not only as aspects of personal development but a reflection of the professional competence as well. But supervisors also opined that within the current supervisory framework, they would not be able to support the personal development of the residents. Although residents indicated their desires for supervisors to facilitate their holistic development and growth towards becoming a psychiatrist, they did not expect supervisors to be interested in their personal development but to focus more on the professional development of their clinical competencies.
There was avoidance by supervisors and residents to discuss personal struggles and frustrations in our study. This would be of concern if in the context of educational supervision in psychiatry, the personal aspects and development of better self-awareness could not be achieved, bearing in mind that this had been considered by some to be the fundamental goal of supervision in counselling (Kadushin, 1985). Concerns of boundary violations within the supervision relationship were raised by both groups of participants. In our study, the supervisors’ strict adherence to the boundaries as accustomed to in psychotherapeutic practice might deter self-disclosure. In contrast, our data suggested that sharing of clinical experiences by their supervisors were very much welcomed by the residents. Research has shown that there might be improvement in alliance when supervisors disclosed relevant past clinical experiences (Matazzoni, 2008). Self-disclosure by the supervisor usually normalised clinical struggles experienced by the residents and could enhance the supervision relationship (Knox et al., 2011). In our study, supervisors held fairly rigid boundaries within supervision, which had been shown to hinder the development of authentic emotional relationships or deeper mentoring relationships (Kozlowski et al., 2013).
Supervisors in our study reflected that it might have been cultural or an ‘Asian thing’ for residents to avoid discussion of personal struggles. Eastern cultures were noted to appreciate a larger power distance than Western cultures (Hofstede, 2011). Cultural value theory also opined that Eastern cultures tended to be more conservative and hierarchical and valued mastery to a lesser extent than the West (Schwartz, 1999). In our predominantly Asian context, the perception of a hierarchical training system might result in supervisors maintaining a stricter teacher-student boundary, or residents being more reluctant to share personal frustrations, particularly with the more senior supervisors. The evaluator role of the supervisor might also result in the resident erecting certain boundaries in the supervisory relationship. This would have implications for nurturing the personal and professional growth of the residents, which require guidance through mentorship and self-reflection within a trusting relationship (Holden et al., 2015).
D. Psychological Safety Within a Trusting Supervisory Relationship
Previous research has shown that any feedback which invoked the self potentially carried with it social judgements which might threaten the educational alliance (Pugh & Regehr, 2016; Telio et al., 2015) and there was a tendency for both supervisors and supervisees to interpret performance assessments as part of a judgement of personal worth (Hawe, 2003). The psychological safety within the supervisory relationship would be particularly important as awareness of the residents’ own inadequacies might be unpleasant and threatening as they faced their imperfect understanding and subjective theories (Vec et al., 2014). As such, the goals of supervision would be best attained with a trusting supervisor-supervisee relationship. However, our study showed that residents are unwilling to reveal too much of their inadequacies as this was too threatening for them, considering that their supervisors also evaluated their overall work performance and ability to deal with stress. This had resulted in tension in the supervisory relationship. The failure to pay heed to this, whether it was inherent to the training program or secondary to the supervisors’ lack of awareness, might further hinder and jeopardise the supervisory process.
The tension between assessment for support and assessment for high stakes decision-making will continue to challenge supervisors. The conflict between mentoring and appraisal of competency would need to be addressed. It would be important for residency training programs to create opportunities to allow the fostering of trusting supervisory relationships. Roles and expectations of the educational supervisor would need to be articulated clearly to both supervisors and residents. Supervisor training would need to focus not only on supervisor ability and competencies but more importantly, supervisor motivation. There should be the emphasis on instilling awareness of internal values and beliefs encompassing competency assessment, accountability, potential role conflicts, feedback delivery and “skills for establishing trusting, open and non-defensive yet problem–confronting relationships” (Govaerts et al., 2007).
E. Limitations of the Study
In our study, newly graduated residents who were agreeable to participate were recruited. The views of the ‘unwilling’ participants regarding supervision which might be more diverse and contentious might be inadvertently excluded. The content of the interview guide used was also not validated. Another limitation concerned the dual roles of researcher and APD. The view of the resident group might be subjected to biases and undue influence due to power differentials (Kotter, 2010). The researcher had minimised such potential biases by being reflexive and addressed concerns of imposing on the participants’ views openly during the interview (Creswell & Miller, 2000).
V. CONCLUSION
The mentoring role in supervision was found to be lacking in our current residency training. The residency program structure, with its focus on assessments of competencies and examinations, might have the unintended consequences of encouraging a transactional supervisory structure at the expense of a relational and mentoring relationship. This qualitative study highlighted significant differences in definitions, roles and expectations of educational supervision. It was our intention that this research endeavor contribute towards better appreciation of the dynamics within educational supervision in a competency-based residency training framework and further inform developments in the mentoring component of supervisory practices in the other training programs as well.
Notes on Contributors
Dr Lay Ling Tan formulated the research question and designed the research methodology. She conducted the semi-structured interviews and wrote the first draft of the manuscript.
Prof Pim W. Teunissen provided guidance for the research methodology and data analysis. He was also involved with the revision of the manuscript drafts.
Dr Wee Shiong Lim provided guidance for the research methodology, assisted with the initial analysis of the first three interviews independently as well as the revision of the manuscript drafts.
Both Dr Vanessa Wai Ling Mok and Dr Hwa Ling Yap were involved with recruitment of participants and data analysis.
Ethical Approval
Ethics approval was sought from the Institutional Review Board (CIRB Ref: 2017/2319) and informed consent was received from all participants.
Data Availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Acknowledgement
We would like to acknowledge the contributions of the National Psychiatry Residency Program Supervisors and Residents for their willingness to participate.
Funding
We did not receive any funding for this research study.
Declaration of Interest
Dr Lay Ling Tan is the Associate Program Director and the PI of this research. Dr Hwa Ling Yap and Dr Vanessa Mok are both teaching faculty of the teaching site. They have a vested interest in ensuring the quality of supervision of residents. The other authors have no other conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Akhtar, S. (2009). Comprehensive dictionary of psychoanalysis. Routledge.
Carroll, M. (2006). Counselling supervision: Theory, skills and practice. SAGE.
Cavalcanti, R. B., & Detsky, A. S. (2011). The education and training of future physicians: Why coaches can’t be judges. JAMA, 306(9), 993-994. https://doi.org/10.1001/jama.2011.1232
Chay, O. M. (2019). Transformation of medical education over the years – A personal view. The Asia Pacific Scholar, 4(1), 59–61. https://doi.org/10.29060/TAPS.2019-4-1/PV1076
Chur-Hansen, A., & McLean, S. (2007). Trainee psychiatrists’ views about their supervisors and supervision. Australasian Psychiatry, 15(4), 269-272.
Creswell, J. W. (2014). Research design: Qualitative, quantitative, and mixed method approaches (4th ed.). SAGE.
Creswell, J. W., & Miller, D. L. (2000). Determining validity in qualitative inquiry. Theory Into practice, 39(3), 124-130. https://doi.org/10.1207/s15430421tip3903_2
Driessen, E. W., Overeem, K., & van der Vleuten, C. P. M. (2011). Get yourself a mentor. Medical Education, 45(5), 438-439. https://doi.org/10.1111/j.1365-2923.2011.03948.x
Dudek, N. L., Marks, M. B., & Regehr, G. (2005). Failure to fail: The perspectives of clinical supervisors. Academic Medicine, 80(10), S84-S87.
Falender, C. A., & Shafranske, E. P. (2007). Competence in competency-based supervision practice: Construct and application. Professional Psychology: Research and Practice, 38(3), 232–240. https://doi.org/10.1037/0735-7028.38.3.232
Frank, J. R., Snell, L., Englander, R., & Holmboe, E. S. (2017). Implementing competency-based medical education: Moving forward. Medical Teacher, 39(6), 568–573. https://doi.org/10.1080/0142159x.2017.1315069.
Govaerts, M. J., van der Vleuten, C. P., Schuwirth, L. W., & Muijtjens, A. M. (2007). Broadening perspectives on clinical performance assessment: rethinking the nature of in-training assessment. Advances in Health Sciences Education Theory Practical, 12(2), 239-260. https://doi.org/10.1007/s10459-006-9043-1
Hansman, C. A. (2001). Mentoring as continuing professional education. Adult learning, 12(1), 7–8. https://doi.org/10.1177/104515950101200104
Hawe, E. (2003). “It’s Pretty Difficult to Fail”: The reluctance of lecturers to award a failing grade. Assessment & Evaluation in Higher Education, 28(4), 371–382. https://doi.org/10.1080/0260293032000066209
Hofstede, G. (2011). Dimensionalizing Cultures: The Hofstede Model in Context. Online Readings in Psychology and Culture, 2(1), 1–26. https://doi.org/10.9707/2307-0919.1014
Holden, M. D., Buck, E., Luk, J., Ambriz, F., Boisaubin, E. V., Clark, M. A., Mihalic, A. P., Sadler, J. Z., Sapire, K. J., Spike, J. P., Vince, A., & Dalrymple, J. L. (2015). Professional identity formation: Creating a longitudinal framework through TIME (Transformation in Medical Education). Academic Medicine, 90(6), 761–767. https://doi.org/10.1097/acm.0000000000000719
Julyan, T. E. (2009). Educational supervision and the impact of workplace-based assessments: a survey of psychiatry trainees and their supervisors. BMC Medical Education, 9(1), 51. https://doi.org/10.1186/1472-6920-9-51
Kadushin, A. (1985). Supervision in social work. Columbia University Press.
Kilminster, S., Cottrell, D., Grant, J., & Jolly, B. (2007). AMEE Guide No. 27: Effective educational and clinical supervision. Medical Teacher, 29(1), 2–19. https://doi.org/10.1080/01421590701210907
Knox, S., Edwards, L. M., Hess, S. A., & Hill, C. E. (2011). Supervisor self-disclosure: Supervisees’ experiences and perspectives. Psychotherapy, 48(4), 336–341. https://doi.org/10.1037/a0022067
Kolb, D. A. (2014). Experiential learning: Experience as the Source of Learning and Development (2nd ed.). Pearson Education, Inc. (Original work published 1984).
Kotter, J. P. (2010). Power and influence. Simon and Schuster.
Kozlowski, J. M., Pruitt, N. T., DeWalt, T. A., & Knox, S. (2013). Can boundary crossings in clinical supervision be beneficial? Counselling Psychology Quarterly, 27(2), 109–126. https://doi.org/10.1080/09515070.2013.870123
Launer, J. (2013). Supervision, mentoring and coaching. In Swanwick. T (Ed.), Understanding medical education. Evidence, theory and practice (2nd ed., pp 111-122). Wiley Blackwell. https://doi.org/10.1002/9781118472361.ch8
MacDonald, J. (2002). Clinical supervision: A review of underlying concepts and developments. Australian & New Zealand Journal of Psychiatry, 36(1), 92-98. https://doi.org/10.1046/j.1440-1614.2002.00974.x
Matazzoni, T. A. (2008). The influence of supervisor self-disclosure on the supervisory working alliance in beginning and advanced therapists-in-training [Doctoral dissertation]. ProQuest.
Passi, V. (2016). The importance of mentoring during educational supervision. Perspectives on Medical Education, 5, 195-196.
Patel, P. (2016). An evaluation of the current patterns and practices of educational supervision in postgraduate medical education in the UK. Perspectives on Medical Education, 5(4), 205-214. https://doi.org/10.1007/s40037-016-0280-6
Pront, L., Gillham, D., & Schuwirth, L. W. (2016). Competencies to enable learning-focused clinical supervision: a thematic analysis of the literature. Medical Education, 50(4), 485–495. https://doi.org/10.1111/medu.12854
Pugh, D., & Regehr, G. (2016). Taking the sting out of assessment: is there a role for progress testing? Medical Education, 50(7), 721-729.
Schon, D. A. (1987). Educating the reflective practitioner: Toward a new design for teaching learning in the professions. John Wiley.
Schwartz, S. H. (1999). A theory of cultural values and some implications for work. Applied psychology, 48(1), 23-47. https://doi.org/10.1111/j.1464-0597.1999.tb00047.x
Tebes, J. K., Matlin, S. L., Migdole, S. J., Farkas, M. S., Money, R. W., Shulman, L., & Hoge, M. A. (2011). Providing competency training to clinical supervisors through an international supervision approach. Research on Social Work Practice, 21(2), 190-199. https://doi.org/10.1177/1049731510385827
Telio, S., Ajjawi, R., & Regehr, G. (2015). The “educational alliance” as a framework for reconceptualizing feedback in medical education. Academic Medicine, 90(5), 609-614. https://doi.org/10.1097/acm.0000000000000560
Torby, A., Turner, M. B., Kinzie, J. M., & Usher, C. (2015). What we talk about when we talk about supervision: The clear and the confusing in graduate psychiatric education. Journal of the American Psychoanalytic Association, 63(5), NP7-NP12. https://doi.org/10.1177/0003065115609724
van der Vleuten, C. P. M., Schuwirth, L. W. T., Driessen, E. W., Dijkstra, J., Tigelaar, D., Baartman, L. K. J., & van Tartwijk, J. (2012). A model for programmatic assessment fit for purpose. Medical Teacher, 34(3), 205-214. https://doi.org/10.3109/0142159X.2012.652239
Vec, T., Rupnik Vec, T., & Žorga, S. (2014). Understanding how supervision works and what it can achieve. In Watkins C. E. &. Milne D. I (Eds.) The Wiley International Handbook of Clinical Supervision (pp 103-127). Wiley. https://doi.org/10.1002/9781118846360.ch5
Wald, H. S. (2015). Professional identity (trans) formation in medical education: Reflection, relationship, resilience. Academic Medicine, 90(6), 701-706.
*Lay Ling Tan
2 Simei Street 3 S529889
Email: tan.lay.ling@singhealth.com.sg
Submitted: 23 January 2021
Accepted: 11 August 2021
Published online: 4 January, TAPS 2022, 7(1), 55-65
https://doi.org/10.29060/TAPS.2022-7-1/OA2475
Marcus A Henning1, Vanamali Joseph1, Roger J Booth2, Christian U Krägeloh3 & Craig S Webster1
1School of Medicine, University of Auckland, New Zealand; 2Department of Medical Science, University of Auckland, New Zealand; 3Department of Psychology and Neuroscience, Auckland University of Technology, New Zealand
Abstract
Introduction: This study investigates psychological distress and quality of life (QoL) amongst first year premedical and health science students. The primary aim of this study was to investigate potential differences in QoL and psychological distress between students who sought entry into a medicine programme when compared to those opting for a non-medicine career.
Methods: We examined participant responses to measures of QoL, psychological distress, and course preference (medicine or other). A structural equation model was conducted to consider the interrelationships among future course preference, gender, QoL, depression, anxiety and stress.
Results: Three hundred and sixty-five students completed the online survey. An a priori conceptual model was developed and then evaluated using a structural equation model. The values obtained for RMSEA (0.027), CFI (0.999), and SRMR (0.016) indicated an excellent model fit. The overall model fit statistic, chi-square (χ2 = 7.626, df=6, p= .267), confirmed a good model fit. Students aiming to enrol in medicine generated higher psychological health and environmental QoL scores compared to their non-medicine oriented peers. In addition, physical QoL and psychological health QoL scores significantly predicted psychological distress measures.
Conclusion: The study raises a potential debate regarding placing students with mixed career intentions into the same course and the potential implications this may have on teaching in interprofessional and large student groups in relation to wellbeing, pedagogy, equity, and expenditure. The findings clearly indicated that medical students are not as adversely impacted upon in terms of QoL and psychological distress compared with their non-medical peers.
Keywords: Medical and Health Science Students, Quality of Life, Psychological Distress, Course Preference
Practice Highlights
- Students focusing on medicine report higher levels of psychological health and environmental QoL.
- Course preference is associated with psychological QoL and psychological distress.
- Issues with psychological QoL are more common among females.
- QoL and learning in large lecture theatres requires further investigation.
I. INTRODUCTION
At the University of Auckland, the Biomedical Common Year or Overlapping Year 1 (BCY) programme is a first-year syllabus and the gateway for many students aiming to enrol into either medicine or other healthcare disciplines (e.g., nursing, optometry, or pharmacy). The requirements for entry into medicine is highly competitive such that approximately 700 students who study in BCY aim to apply for medicine out of which only 250 students are chosen (Henning et al., 2017b). Entry into other healthcare disciplines (e.g., nursing, optometry, or pharmacy) is less competitive and selection is thus likely less distressing (Al Alwan et al., 2013). However, the large class sizes within the pre-medical and health science year (of approximately 1,300 students) containing students applying for either medicine or non-medicine programmes may also create a marginalising learning dynamic that may hinder the motivation and wellbeing of non-medicine students (Henning et al., 2017a). Hence, the aim of this research was to assess whether those students aiming for selection into medicine were more at risk of poor quality of life (QoL) and psychological distress relative to those students aiming for selection into other healthcare disciplines.
Numerous studies have researched the areas of QoL and psychological distress amongst medical students (Lovibond & Lovibond, 1995; Szabó, 2010; Wickramasinghe et al., 2019). In their systematic review, Dyrbye et al. (2006) reported concerning rates of depression, anxiety and general psychological distress among medical students, citing for example in one report that 37% of medical students in their first year of study experienced mental health issues of some kind. The adverse impact of distress among students can contribute to problems associated with academic attainment, professional development, academic honesty, substance abuse, cynicism, humanitarian attitude, and development of empathy. Moreover, psychological distress appears to be more of a concern among female medical students. The implication underlying the research investigating QoL and psychological distress suggests that medical students are more compromised than their non-medical peers.
Our conceptual model for the present study was developed in accordance with self-determination theory (Ryan & Deci, 2000). According to this theory, the act of choosing can positively affect motivation, well-being and learning if the needs for autonomy, relatedness, and competence in the individual are high. In this study, students were free to choose their course of study and hence freedom of choice was perceived as equivalent to the notion of course preference. According to this theory, students can be intrinsically motivated (engaged in their studies because of inherent enjoyment) and extrinsically motivated with a focus on outcome (Vansteenkiste et al., 2006). Extrinsic motivation, however, can be differentiated into aspects of regulation dependent upon the degree of autonomy. Therefore, there are facets of autonomous motivation (which involves volition and choice) versus that of controlled motivation (feeling pressured or coerced) (Vansteenkiste et al., 2006). Hence, intrinsic motivation and well-intentioned aspects of extrinsic motivation are considered autonomous, whilst the poorly internalised form of extrinsic motivation are less well incorporated into an individual’s sense of self. In our proposed model, we suggest features of choice with links to QoL.
We cannot assume that the medical or non-medical students differ in terms of their intrinsic or extrinsic motivation, but we do know that the majority of non-medical students at this university (e.g. nursing and pharmacy) have been given conditional entry into their courses on the proviso that they pass their courses in the BCY. However, medical students do not have this luxury and are in a more competitive mode of action. They are, thus, likely intrinsically and extrinsically motivated, and their extrinsic motivation could be either autonomous or controlled. Our assumption is that the non-medical students are also likely to be intrinsic and extrinsically motivated, but their extrinsic motivation is likely more autonomous as they have conditional entry. Therefore, non-medical students would likely experience more heightened levels of QoL than medical students who are experiencing higher levels of competition (Katz & Assor, 2007; Ryan & Deci, 2000). If this is not true another more pressing variable may be affecting the QoL outcome, such as mixing high numbers of students together from different disciplines into one course (Hornsby & Osman, 2014). In addition, given the established empirical evidence (Haist et al., 2000; Henning et al., 2013; Naylor et al., 2018; Ramsbottom-Lucier et al., 1995), we argued that gender would likely moderate choice and QoL. Therefore, the first stage of our conceptual model proposes that, once students have chosen a particular course of study (medicine or other) this will directly impact their QoL given the increased expectation associated with the decision process (Katz & Assor, 2007). Therefore, those students aiming for a programme (i.e., medicine) requiring higher stakes will likely be more at risk of ill-health.
The next element of our argument proposes that QoL will likely impact psychological distress. For example, if a student experiences good health-related physical QoL they are then likely to have lowered risk of psychological distress (Burris et al., 2009). In their study of first year medical students, Verger et al. (2009) reported that psychological distress was moderated by gender and influenced by wellbeing protective factors, such as social support, coping with academic pressure, and socio-economic factors. Consequently, we suggest that there is likely a follow-on effect such that those students with compromised QoL will likely experience more psychological distress (Dyrbye et al., 2006). Nonetheless, the causes of poor QoL are likely complex and vary substantially between individuals given that some studies have shown that students aiming to study medicine may be more motivated and experience higher levels of QoL (Henning et al., 2017a).
The primary aim of this study was to empirically investigate potential differences in QoL and psychological distress between students who sought entry into a medicine programme when compared to those opting for a non-medicine career. The issue of follow-on effects from QoL to psychological distress has not been studied within this learning context. To illustrate potential differences between the two groups, we scrutinised conceptual links between choice, gender, QoL and psychological distress in reference to students’ course preference (medicine or other) whilst studying in the BCY programme.
II. METHODS
A. Participants
All students (N=1277) studying within the BCY programme were invited to participate in this survey. Students aiming to study in any health-related course at the University of Auckland first enrol in the BCY programme in preparation for formalised entry into degrees for Bachelor of Health Science, Bachelor of Pharmacy, Bachelor of Optometry or Bachelor of Medicine (The University of Auckland, 2019).
B. Procedure
Ethics approval for the collection and use of data was obtained from the University of Auckland Human Participants Ethics Committee (Ref. 021985).
Students were informed about the study by email in late July (2018), and two reminder emails were sent out. The anonymous survey was conducted prior to final course completion in Semester 2 (2018), but after grades for the first semester had been released. Informed consent was implied given that study participants received a participant information sheet prior to the start of the questionnaire. Data were collected online using a Google Forms questionnaire (Google.com, 2015), which requires respondents to fully complete the survey before they are able to submit it.
C. Measures
Demographic and background details were obtained to assess the representativeness of the sample included: (1) Age in years; (2) Gender; (3) Future course preference (medicine or other); (4) Enrolment status (international or domestic); and (5) Ethnicity.
Quality of life was measured using the New Zealand version of the WHOQOL (NZ WHOQOL-BREF) questionnaire (Krägeloh et al., 2016). It has four domains (physical QoL, psychological health QoL, social relationships QoL and the environmental QoL) and contains 31 items. In this study, physical QoL had six items, psychological health QoL had 10 items, social relationships QoL had four items and environmental QoL had eight items (The NZ WHOQOL Group, 2017). Questions 1 and 2 are global QoL and health items and, thus, not included in the scoring of the four quality of life domains. Question 3 was deemed to have little relevance with respect to the research question and had been previously identified as having a ceiling effect in early career medical students (Krägeloh et al., 2011). All items utilised a 5-point Likert scale with varying anchors (the scores for two items were reversed). High scores indicated higher levels of QoL.
Psychological distress was measured using the Depression, Anxiety and Stress Scale (DASS-21), which captures respondents’ emotional states in reference to three domains: depression, anxiety and stress (within the past seven days). Each domain is comprised of seven items. The DASS-21 instrument has been developed from a previous 42-item version (Lovibond & Lovibond, 1995), and has undergone psychometric investigation among a variety of populations (Le et al., 2017; Medvedev et al., 2018; Szabó, 2010; Yıldırım et al., 2018). Each item utilises a 4-item Likert scale. Higher scores indicate more frequency and severity in the experience of negative emotions.
D. Data Analysis
First, the response rate (n/N) was calculated as a percentage measure, and the details of the participants were described. Second, descriptive statistics (means and standard deviations (SDs)) were computed for the two self-reported questionnaires measures (NZ WHOQOL-BREF and DASS-21). These measures were computed for each of the questionnaire domains with respect to course preference (medicine; other) and gender (male; female). A multivariate analysis of variance (ANOVA) approach was used to assess levels of significance for the independent variables, course preference and gender, with respect to the aforementioned dependent variables.
Lastly, one structural equation model (SEM) was developed to consider the interrelationships among course preference, gender, and QoL and DASS-21 domain measures. This SEM was developed using the software AMOS v25 (Arbuckle, 2017). The primary goodness-of-fit indices used to assess the model fit were inspection of the model chi-square value, root mean square error of approximation (RMSEA), comparative fit index (CFI), and standardised root mean square residual (SRMR). Model fits were considered acceptable if they met the following recommendations: (1) RMSEA < 0.06; (2) SRMR < 0.08; and (3) CFI close to 0.95 or higher (Hu & Bentler, 1998). Additionally, using maximum likelihood bootstrapping with 1,000 samples, regression weights were computed, and bias-corrected 95% confidence intervals were determined (Byrne, 2010).
III. RESULTS
A. Response Rate and Participant Data
Three hundred and sixty-five students (n = 365) fully completed the online survey resulting in a response rate of 29%. The average age of participants was 19 years (SD = 1.84) with 75% of respondents being female. Table 1 provides the demographic profile for the sample, and upon examination, the distributions of the sample data appeared representative of the population profile. In this study, more than 75% of participants stated a preference to study medicine as opposed to other non-medicine health options, which is a rate higher than that found elsewhere (Henning et al., 2017b). The data that support the findings of this study are openly available in Figshare at https://figshare.com/articles/dataset/_/1405 0463 (Henning et al., 2021).
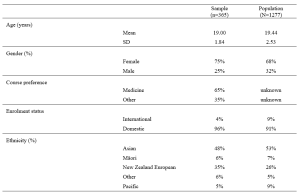
Table 1. Demographic and academic achievement details of the sample versus the population.
The means and standard deviations for the variables of interest are shown in Table 2. The NZ WHOQOL-BREF questionnaire means for these participants are marginally lower than those found elsewhere (Henning et al., 2017b). No comparable New Zealand medical student reference values for the DASS-21 are available for this population. In reference to internal consistency coefficients computed for each of the measures (Table 2), all Cronbach’s alpha values were equal to or greater than 0.70 thus meeting ‘acceptable’ requirements (Field, 2005).
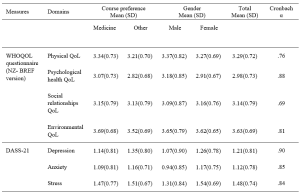
Table 2. Means, standard deviations (SD) and internal consistency scores (Cronbach alpha) of the measures used in the study.
Note: Using a multivariate ANOVA approach, significant differences (p<.05) for course preference (medicine vs. other) were noted for psychological health QoL, environmental QoL, and depression. In addition, significant differences (p<.05) for gender (male vs. female) were noted for psychological health QoL, depression, anxiety and stress.
B. Structured Equation Modelling
Based on previous literature (Dyrbye et al., 2006) and self-determination theory (Katz & Assor, 2007; Ryan & Deci, 2000), an a priori conceptual model was developed and tested using a SEM framework. The primary criterion variable was the students’ course preference (medicine, scored as 1 vs. other, scored as 0). The values obtained for RMSEA, SRMR, and CFI indicated that the model fit was excellent, that is, RMSEA = 0.027, CFI = 0.999, and SRMR = 0.016. As a secondary check, the overall model fit determined by the chi-square (χ2 = 7.626, df=6. p= .267) also indicated the model fitted very well. We noted that some of the error variances within measures of the NZ WHOQOL-BREF and DASS-21 were required to be correlated.
Figure 1 shows the path diagram for all the data collected (n = 365). The path coefficients are shown for significant relationships only (p < .05). The bias-corrected 95% confidence intervals for the regression weights (path coefficients) obtained using the maximum likelihood bootstrapping method were generated (Table 3) to ensure the accuracy and stability of the parameter estimates (Byrne, 2010).
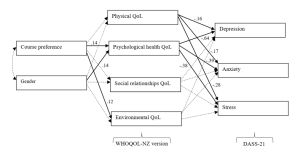
Figure 1. Path diagram of the tested structural equation model for all study participants.
Note. The path standardised regression weight estimates were shown only when statistically significant (p<.05). For non-significant relationships, directive arrows are shown with dashed lines (see Table 3 for details). Errors for all pertinent measures were removed to improve clarity of the figure. Error variances among the WHOQOL- NZ version and DASS-21 domian measures were were allowed to be correlated. No other error variances were correlated. Key fit indices and chi-square calculations were standardised RMR = .016, CFI = .999, RMSEA = .027, χ2 = 7.626, df=6. p= .267
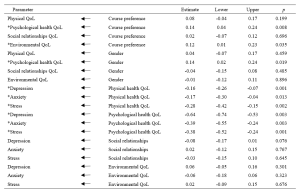
Table 3. Standardised regression weights: Lower and upper ends of bias-corrected 95% confidence intervals of the regression weights of the directional paths of the SEM.
Note. * p<.05
Table 3 and Figure 1 indicated the following relationships. The standardised regression weights determined that course preference significantly predicted psychological health QoL and environmental QoL. More specifically, those students preferring a medical course will likely have higher psychological health QoL and environmental QoL. Gender did not influence course preference but had a significant association with psychological health QoL. In turn, physical QoL and psychological health QoL scores significantly predicted depression, anxiety and stress (DASS-21 measures). The two remaining QoL measures (social relationships QoL and environmental QoL) did not significantly predict the DASS-21 measures.
When inspecting Table 2 and Figure 1, we can make certain assertions related to the differences between the two groups (medical and other students) with respect to QoL and psychological distress. Figure 1 indicates two significant associations between course preference and psychological health QoL and environmental QoL. Therefore, students indicating a preference for enrolling in a medical course were likely to experience greater psychological health QoL and environmental QoL. The findings in Table 2, clarify that students aiming to study medicine have higher levels of QoL in these two domains, compared to students aiming to study in non-medicine courses. In addition, the multivariate analyse indicate that depression is more of a concern for non-medical students than intending medicine students.
IV. DISCUSSION
The known health concerns associated with first year students (Naylor et al., 2018; Tinto, 2009) appear consistent with the current findings. The actual values (Table 2) for three of the four QoL domains from the NZ WHOQOL-BREF -psychological health QoL, social relationships QoL, and environmental QoL – are lower than previously published values for year 4 and 5 students at the same university (Henning et al., 2012), although the physical QoL score was higher. This indicates that year 1 students at this university appear to have relatively lower QoL than their year 4 and 5 peers and are consequently lower than the general population norms, particularly in the areas of psychological health QoL, social relationships QoL, and environmental QoL (Henning et al., 2012). In addition, the values for all domains are lower than those acquired from a 2015 first-year cohort (overall) studying in the same programme (Henning et al., 2017b).
Similarly, the DASS-21 findings (Table 2) show that this group scored higher on the domains of depression and anxiety compared to early career doctors also graduating from the same university (Henning et al., 2014). In comparison to a Malaysian student group, the mean values for the present study show distinct similarity in terms of stress and anxiety scores, but a marked lower score for depression (Yusoff et al., 2013). Therefore, we have provided good evidence to suggest that this group of students, irrespective of choosing either medicine or other as their preferred course option, studying in the BCY programme are experiencing relatively lower levels of QoL and higher levels of psychological distress compared to previous cohorts studying at the same university. However, their experiences may not differ greatly when compared to those students’ psychological distress perceptions in other universities.
In reference to the conceptual model, the findings also confirm that preference for course of study is linked with aspects of QoL. This in turn influences psychological distress, suggesting a feedback loop. Both of these associations were confirmed by the path analysis resulting in an excellent model fit for the SEM (Figure 1). The first part of the model considered how the preferred course option (medicine versus other) could directly impact QoL measures and the second part of the model considered the flow-on (indirect) effects to psychological distress (depression, anxiety and stress).
A. Choosing to Study medicine and Its Impact on Quality of Life
Figure 1 clearly shows that choosing to study medicine has an influence on aspects of QoL, although gender was not found to be significantly correlated with course preference. The decision to choose to study medicine was directly and significantly associated with psychological health QoL and environmental QoL (with higher scores noted for intending medicine students), but did not influence either physical QoL or social relationships QoL. In Table 2, we noted that psychological health QoL and environmental QoL for those vying for a place in the medical programme was higher than students’ scores for other health options (e.g., nursing, pharmacy, or optometry). The direction of the arrows in the model implies that the act of deciding to study medicine is likely influencing QoL on these two domains. These findings can be interpreted in several ways.
First, it is likely that students who aim for admission to medicine may be more psychologically robust to begin with. The psychological health QoL domain of the New Zealand version of the WHOQOL encompasses 10 facets (Krägeloh et al., 2016; WHOQoL Group, 1998). The facets that likely emphasise the difference between those applying for medicine and those applying for another degree are self-esteem, perception of negative or positive feelings, concentration, ability to meet expectation, and management of personal circumstances. In a previous study (Henning et al., 2017b), perceived stress was found to be highly correlated with psychological QoL and also noted to be a strong predictor of course preference (medicine versus other), with potential medical students scoring higher than their other heath professional peers.
Second, the aspects of cognitive capacity, personal management, and mental wellbeing need to be weighed in comparison to environmental QoL (measured in perceived access to resources, i.e., finance, health care, transport, security, technology, and housing) (WHOQoL Group, 1998). The current findings confirm previous research linking course preference to environmental QoL, suggesting that those students who come from affluent and supportive backgrounds will likely have more interest in pursuing a medical degree (Henning et al., 2017b).
B. Impact of Quality of Life on Psychological Distress
The SEM also revealed an interesting flow-on effect suggesting that those students not choosing medicine will have more issues with psychological wellbeing than those choosing to pursue medicine, which translates to greater risk of psychological distress in the form of depression, anxiety and stress for non-medical students. Furthermore, intending medicine students generated significantly lower depression scores than their non-medicine peers. Even though physical QoL is also directly connected with psychological distress factors, this association was not influenced by course preference. Hence, the key issues linked to course preference are related to psychological health QoL, which is incidentally linked to gender. Environmental QoL appears to have no flow-on psychological distress effects.
These findings indicate that some perceptions of QoL are likely linked to choice and ultimately psychological distress factors. The flow-on effect suggests that those students who struggle with psychological health QoL tend to further struggle with psychological distress. The point of difference between the two groups (medical and other) is that the intending medical students appear less affected by depression than their non-medical peers. The concept of choice has been established as a key component in motivation and wellbeing, for example, the perceived expectancies and values regarding a task are influenced by weighing up the benefits and costs associated with the forthcoming task (Katz & Assor, 2007). Hence, in the medical context the preferred choice of medicine likely has a powerful impact on motivation, learning and wellbeing (Katz & Assor, 2007). The current findings indicate that students focussing on medicine have higher psychological health QoL and lower psychological distress (particularly in the area of depression) than non-medicine students in the same year. This may imply that the current programme is more suited to those aiming for a medical career than those heading for a non-medicine health-related vocation, although this proposition requires further investigation.
C. Implications for Learning and Wellbeing
There are two clear implications associated with these results.
First, the findings indicate that intending medical students are more likely to have good access to environmental resources. The elevation of environmental QoL scores for students intending to study medicine as compared to students in other disciplines is consistent with findings reported elsewhere (Collins et al., 1993; Henning et al., 2012; Ng et al., 2009), suggesting that these students likely have better access to the needed resources. Equity arguments regarding selection of medical students is a global concern and impacts areas related to communication, empathetic listening, and shared understandings between clinician and patient (Rao & Flores, 2007). The resources differential suggests a clear argument that students who prefer to study medicine may not equitably mirror the less-resourced population at large and thus may have difficulty relating to large proportions of society. It is important to also emphasise that equity initiatives at the university in which this study was conducted are in place, although the complexity of the issues are multifaceted and may require further development (Curtis et al., 2015; Poole et al., 2009).
Second, the findings in this study clearly indicate that intending medical students are more likely to experience higher levels of psychological health QoL. Therefore, they are more likely to have a different wellbeing outcome than those students who aim for an alternative health sciences career, which may warrant investigating the rationale for placing students aiming for different health professions in one course of study. An argument for placing all health-career students together is likely based on the idea of interprofessional learning (Salamonson et al., 2009). Some of the benefits include improved knowledge gains especially for those students preparing for non-medical courses and positive attitudinal shifts regarding each profession (Carpenter, 1995). The findings in this study revealed that one lecturer was able lecture to 1277 students at one time (using asynchronous technology), suggesting this is a cost effective teaching option. Nonetheless, the findings in this study do indicate that the implication of large classes (or ‘massification’) in reference to wellbeing gains requires further investigation (Hornsby & Osman, 2014).
It has been established that students preferring medicine to other health science options will lead to greater academic attainment. For example, Henning et al. (2017b) reported that those students preferring to pursue medicine attained a bioscience grade average of 6.77 which was significantly higher than the non-medical comparison cohort which attained a grade average of 4.42. Therefore, creating smaller, discipline-specific groups could create more equitable learning, as well as engendering more opportunities for staff-student engagement, more engagement with relevant content, and greater likelihood of motivation for learning (Hornsby & Osman, 2014). However, in the context of pre-medical courses, such as the BCY programme, even though there are clear differences in resulting grade achievement, more research is required to tease out the subtle learning and wellbeing interconnections and to further investigate whether one group is more disadvantaged in their learning than the other (in this case the non-medicine group).
A limitation of this study is the relatively low response rate, although this is comparable with other studies using online questionnaires (Nulty, 2008) and the participants engaged in this study had similar characteristics to the total population (Table 1). Moreover, the response rate is within the range considered acceptable for surveys of representatives of organisations (36%±13%) – a category arguably appropriate for students entering their respective professions (Baruch, 1999). A further limitation of the study is that the research design is cross-sectional suggesting that the links between variables cannot infer temporal causality. Lastly, we acknowledge that it was outside the scope of the study to fully explore some of the speculations raised in this paper, such as whether choice of course of study was influenced by either intrinsic or extrinsic factors (i.e., degree of autonomy).
V. CONCLUSION
The main implication of this study is the direct relationships between course preference (medicine versus other) and psychological health QoL and environmental QoL, as well as the further indirect or flow-on effects to psychological distress via the psychological QoL pathway. Thus, indicating that medical students are not as adversely impacted upon in terms of QoL and psychological distress compared with their non-medicine peers. Lastly, the study findings provide useful debate and scope for further research in the areas of pedagogy, educational equity, career aspiration, and financial cost related to interprofessional education and teaching in large student groups.
Notes on Contributors
Marcus A. Henning is an associate professor in the Centre for Medical and Health Sciences Education at the University of Auckland, New Zealand. MAH was involved in the conceptualisation of the idea, data curation, formal analysis, developing the design of the study, writing the original draft and ongoing editing.
Vanamali Joseph was, at the time of this study, a third year medical student studying in the Faculty of Medical and Health Sciences at the University of Auckland, New Zealand. VJ was involved in the conceptualisation of the idea, data curation, developing the design of the study and ongoing editing.
Roger J. Booth is an associate professor in molecular medicine and pathology, in the Faculty of Medical and Health Sciences at the University of Auckland, New Zealand. RB was involved in the conceptualisation of the idea, data curation, developing the design of the study and ongoing editing.
Christian U. Krägeloh is an associate professor in the Department of Psychology at AUT University, New Zealand. CUK was involved in the conceptualisation of the idea, formal analysis and ongoing editing.
Craig S. Webster is an associate professor in the Centre for Medical and Health Sciences Education at the University of Auckland, New Zealand. CSW was involved in the conceptualisation of the idea, data curation, formal analysis, developing the design of the study, writing the original draft and ongoing editing.
Ethical Approval
Ethics approval for the collection and use of data was obtained from the University of Auckland Human Participants Ethics Committee (Ref. 021985).
Data Availability
The anonymised data that supports the findings of this study are openly available in the Figshare repository, https://figshare.com/articles/dataset/_/14050463
Funding
No funding source required for this study.
Declaration of Interest
The authors declare no conflicts of interest.
References
Al Alwan, I., Al Kushi, M., Tamim, H., Magzoub, M., & Elzubeir, M. (2013). Health sciences and medical college preadmission criteria and prediction of in-course academic performance: A longitudinal cohort study. Advances in Health Sciences Education, 18(3), 427-438. https://doi.org/10.1007/s10459-012-9380-1
Arbuckle, J. L. (2017). IBM® SPSS® Amos™ 25 User’s Guide. https://usermanual.wiki/Document/IBMSPSSAmosUserGuide.2983928102/view
Baruch, Y. (1999). Response rate in academic studies- A comparative analysis. Human Relations, 52(4), 421-438. https://doi.org/10.1177/001872679905200401
Burris, J. L., Brechting, E. H., Salsman, J., & Carlson, C. R. (2009). Factors associated with the psychological well-being and distress of university students. Journal of American College Health, 57(5), 536-544. https://doi.org/10.3200/JACH.57.5.536-544
Byrne, B. M. (2010). Structural Equation Modeling with AMOS: Basic concepts, applications and programming (2nd ed.). Routledge.
Carpenter, J. (1995). Interprofessional education for medical and nursing students: Evaluation of a programme. Medical Education, 29(4), 265-272. https://doi.org/10.1111/j.1365-2923.1995.tb02847.x
Collins, J., Jones, J., & White, G. (1993). Demographic variables in Auckland medical students. New Zealand Medical Journal, 106(960), 306-308.
Curtis, E., Wikaire, E., Jiang, Y., McMillan, L., Loto, R., Airini., & Reid, P. (2015). A tertiary approach to improving equity in health: Quantitative analysis of the Māori and Pacific admission scheme (MAPAS) process, 2008–2012. International Journal for Equity in Health, 14(1), 1-15. https://doi.org/10.1186/s12939-015-0133-7
Dyrbye, L. N., Thomas, M. R., & Shanafelt, T. D. (2006). Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Academic Medicine, 81(4), 354-373. https://doi.org/10.1097/00001888-200604000-00009
Field, A. P. (2005). Discovering statistics using SPSS : And sex, drugs and rock’n’roll (2nd ed.). SAGE.
Google.com. (2015). Homepage. https://www.google.co.nz/forms/about/
Haist, S. A., Wilson, J. F., Elam, C. L., Blue, A. V., & Fosson, S. E. (2000). The effect of gender and age on medical school performance: An important interaction. Advances in Health Sciences Education: Theory and Practice, 5(3), 197-205. https://doi.org/10.1023/A:1009829611335
Henning, M. A., Joseph, V., Booth, R. J., Krageloh, C. U., & Webster, C. S. (2021). Biomedical students’ course preference and links with quality of life and psychological distress [Data set]. Figshare. https://figshare.com/articles/dataset/_/14050463
Henning, M. A., Krägeloh, C. U., Hawken, S. J., Zhao, Y., & Doherty, I. (2012). The quality of life of medical students studying in New Zealand: A comparison with non-medical students and a general population reference group. Teaching and Learning in Medicine, 24(4), 334-340.https://doi.org/10.1080/10401334.2012.715261
Henning, M. A., Krägeloh, C. U., Booth, R., Hill, E. M., Chen, J., & Webster, C. S. (2017a). Biomedical students in their first year of study: Factors explaining performance in a high stakes examination. Medical Science Educator, 27(4), 633–643. https://doi.org/10.1007/s40670-017-0444-y
Henning, M. A., Krägeloh, C. U., Booth, R., Hill, E. M., Chen, J., & Webster, C. S. (2017b). Profiling potential medical students and exploring determinants of career choice. The Asia Pacific Scholar, 2(1), 7-15. https://doi.org/10.29060/TAPS.2017-2-1/OA1019
Henning, M. A., Krägeloh, C. U., Manalo, E., Doherty, I., Lamdin, R., & Hawken, S. J. (2013). Medical students in early clinical training and achievement motivation: Variations according to gender, enrolment status, and age. Medical Science Educator, 23(1), 6-15. https://doi.org/10.1007/BF03341798
Henning, M. A., Sollers, J., Strom, J. M., Hill, A. G., Lyndon, M. P., Cumin, D., & Hawken, S. J. (2014). Junior doctors in their first year: Mental health, quality of life, burnout and heart rate variability. Perspectives in Medical Education, 3, 136-143. https://doi.org/10.1007/s40037-013-0075-y
Hornsby, D. J., & Osman, R. (2014). Massification in higher education: Large classes and student learning. Higher Education Research & Development, 67(6), 711-719. https://doi.org/10.1007/s10734-014-9733-1
Hu, L.-t., & Bentler, P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424-453. https://doi.org/10.1037/1082-989X.3.4.424
Katz, I., & Assor, A. (2007). When choice motivates and when it does not. Educational Psychology Review, 19(4), 429. https://doi.org/10.1007/s10648-006-9027-y
Krägeloh, C., Henning, M., Hawken, S., Zhao, Y., Shepherd, D., & Billington, R. (2011). Validation of the WHOQOL-BREF quality of life questionnaire for use with medical students. Eductaion for Health, 24(2), 545.
Krägeloh, C. U., Billington, D. R., Hsu, P. H.-C., Feng, X. J., Medvedev, O. N., Kersten, P., Landon, J., & Siegert, R. J. (2016). Ordinal-to-interval scale conversion tables and national items for the New Zealand version of the WHOQOL-BREF. PLOS ONE, 11(11), e0166065. https://doi.org/10.1371/journal.pone.0166065
Le, M. T. H., Tran, T. D., Holton, S., Nguyen, H. T., Wolfe, R., & Fisher, J. (2017). Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PLOS ONE, 12(7), e0180557. https://doi.org/10.1371/journal.pone.0180557
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335-343.
Medvedev, O. N., Krägeloh, C. U., Titkova, E. A., & Siegert, R. J. (2018). Rasch analysis and ordinal-to-interval conversion tables for the Depression, Anxiety and Stress Scale. Journal of Health 25(10–11), 1374–1383. https://doi.org/10.1177/1359105318755261
Naylor, R., Baik, C., & Arkoudis, S. (2018). Identifying attrition risk based on the first year experience. Higher Education Research & Development, 37(2), 328-342. https://doi.org/10.1080/07294360.2017.1370438
Ng, C. L., Tambyah, P. A., & Wong, C. Y. (2009). Cost of medical education, financial assistance and medical school demographics in Singapore. Singapore Medical Journal, 50(5), 462-467.
Nulty, D. D. (2008). The adequacy of response rates to online and paper surveys: What can be done? Assessment and Evaluation in Higher Education, 33(3), 301-314. https://doi.org/10.1080/02602930701293231
Poole, P. J., Moriarty, H. J., Wearn, A. M., Wilkinson, T. J., & Weller, J. M. (2009). Medical student selection in New Zealand: looking to the future. New Zealand Medical Journal, 122(1306), 88-100.
Ramsbottom-Lucier, M., Johnson, M. M., & Elam, C. L. (1995). Age and gender differences in students’ preadmission qualifications and medical school performances. Academic Medicine, 70(3), 236-239. https://doi.org/10.1097/00001888-199503000-00016
Rao, V., & Flores, G. (2007). Why aren’t there more African-American physicians? A qualitative study and exploratory inquiry of African-American students’ perspectives on careers in medicine. Journal of the National Medical Association, 99(9), 986-993.
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68-78. https://doi.org/10.1037/0003-066X.55.1.68
Salamonson, Y., Everett, B., Koch, J., Wilson, I., & Davidson, P. M. (2009). Learning strategies of first year nursing and medical students: A comparative study. International Journal of Nursing Studies, 46(12), 1541-1547. https://doi.org/10.1016/j.ijnurstu.2009.05.010
Szabó, M. (2010). The short version of the Depression Anxiety Stress Scales (DASS-21): Factor structure in a young adolescent sample. Journal of Adolescence, 33(1), 1-8. https://doi.org/10.1016/j.adolescence.2009.05.014
The NZ WHOQOL Group. (2017). WHOQOL tools. Auckland University of Technology. https://cpcr.aut.ac.nz/new-zealand-whoqol
The University of Auckland. (2019). Biomedical Science. https://www.auckland.ac.nz/en/study/study-options/find-a-study-option/biomedical-science.html
Tinto, V. (2009). Taking student retention seriously: Rethinking the first year of university. FYE curriculum design symposium. Queensland University of Technology, Australia.
Vansteenkiste, M., Lens, W., & Deci, E. L. (2006). Intrinsic versus extrinsic goal contents in self-determination theory: Another look at the quality of academic motivation. Educational Psychologist, 41(1), 19-31. https://doi.org/10.1207/s15326985ep4101_4
Verger, P., Combes, J.-B., Kovess-Masfety, V., Choquet, M., Guagliardo, V., Rouillon, F., & Peretti-Wattel, P. (2009). Psychological distress in first year university students: Socioeconomic and academic stressors, mastery and social support in young men and women. Social Psychiatry and Psychiatric Epidemiology, 44(8), 643-650. https://doi.org/10.1007/s00127-008-0486-y
WHOQoL Group. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28(3), 551-558. https://doi.org/10.1017/S0033291798006667
Wickramasinghe, D. P., Almeida, I. S., & Samarasekera, D. N. (2019). Depression and stressful life events among medical students during undergraduate career: Findings from a medical school in South Asia. The Asia Pacific Scholar, 4(1), 42-47. https://doi.org/10.29060/TAPS.2019-4-1/OA2025
Yıldırım, A., Boysan, M., & Kefeli, M. C. (2018). Psychometric properties of the Turkish version of the Depression Anxiety Stress Scale-21 (DASS-21). British Journal of Guidance & Counselling, 46(5), 582-595. https://doi.org/10.1080/03069885.2018.1442558
Yusoff, M. S. B., Rahim, A. F. A., Baba, A. A., Ismail, S. B., Pa, M. N. M., & Esa, A. R. (2013). Prevalence and associated factors of stress, anxiety and depression among prospective medical students. Asian Journal of Psychiatry, 6(2), 128-133. https://doi.org/10.1016/j.ajp.2012.09.012
*Marcus A. Henning
The University of Auckland,
Private Bag 92019,
Auckland 1142, New Zealand
Tel: 0064 923 7392
Email: m.henning@auckland.ac.nz
Submitted: 26 January 2021
Accepted: 25 June 2021
Published online: 4 January, TAPS 2022, 7(1), 44-54
https://doi.org/10.29060/TAPS.2022-7-1/OA2471
Mitsumi Masuda1, Machiko Saeki Yagi2 & Fumino Sugiyama3
1Nagoya City University, Nagoya, Aichi, Japan; 2Jichi Medical University, Shimotuke, Tochigi, Japan; 3National College of Nursing, Japan, Kiyose, Tokyo, Japan
Abstract
Introduction: Simulation-based learning (SBL) is a practical and efficient learning method that involves the replacement of a portion of clinical education with quality simulation experiences. It has been utilised in various countries, such as the United States, Canada, and South Korea. However, based on current regulations in Japan, clinical education cannot be replaced with simulation experience. For future curriculum integration, it is necessary to clarify the current use of SBL and tackle systematic educational strategies of SBL. Therefore, this national survey aimed to clarify the prevalence and practices of SBL in undergraduate nursing education programs in Japan.
Methods: This article presents the results of our national survey in Japan. It presents the questionnaire based on the International Nursing Association for Clinical Simulation and Learning Standards of Best Practice and demonstrates the use of simulation-based learning in Japanese undergraduate nursing programs.
Results: Overall, the schools using simulation-based education (SBE) comprised 346 schools (82.4%) of the sample. Those equipped with high-fidelity simulators were 146 schools (27.6%); the rest owned medium-fidelity simulators. Almost all undergraduate nursing education systems were equipped with simulators, however, the frequency of use was low. SBL was incorporated into the curriculum at many undergraduate nursing education institutions, and awareness of the INACSL Standard of Best Practice: SimulationSM was extremely low.
Conclusion: This study shows that SBL is not properly utilised in undergraduate nursing programs, even though many schools are equipped with simulators. Thus, further study on barriers to simulator use is needed.
Keywords: Simulation-based Learning, Curriculum, International Nursing Association for Clinical Simulation and Learning Standard of Best Practice: SimulationSM, Japan, Undergraduate Nursing Education
Practice Highlights
- Almost all undergraduate nursing education programs use SBL.
- The frequency of use of SBL was low in almost all undergraduate nursing education systems.
- SBL was incorporated into the curriculum at many undergraduate nursing education institutions.
- Awareness of the INACSL Standard of Best Practice: SimulationSM was extremely low.
I. INTRODUCTION
A. Use of Simulation-based Learning in Undergraduate Nursing Education
Simulation-based learning (SBL) is a practical and efficient learning method developed in various countries, such as the United States (Zarifsanaiey et al., 2016), Canada (Chiniara et al., 2013), and South Korea (Kim et al., 2016; Shin et al., 2015), that allows aspiring practitioners to experience realistic clinical situations in a safe environment. An overview of past studies on SBL shows that it facilitates high satisfaction, confidence, critical thinking, clinical reasoning, and communication skills in nursing students (Adamson, 2015; Boling & Hardin-Pierce, 2016; Carter et al., 2016). Pal et al. (2018) study showed that learning had progressively improved with each session of simulation with corresponding decrease in stress. Further, the landmark National Council of State Boards of Nursing (NCSBN) National Simulation Study provided evidence that up to 50% of traditional clinical experience can be substituted by simulation in prelicensure nursing programs (Hayden et al., 2014). The results of this study provide substantial evidence that similar outcomes in nursing knowledge, clinical competency and National Council Licensure Examination-Registered Nurse (NCLEX-RN®) pass rates are observable in comparison to 10%, 25% and 50% substitution by simulation (Hayden et al., 2014). As a result, many educators in the United States are examining and revising regulations to allow replacement of a proportion of clinical education with quality simulation experiences (Breymier et al., 2015). The NCSBN study states that substituting simulation for clinical hours requires the use of high-quality simulations (Hayden et al., 2014). Therefore, the NCSBN developed the International Nursing Association for Clinical Simulation and Learning (INACSL) Standards of Best Practice: SimulationSM (Alexander et al., 2015). The INACSL Standard of Best Practice: SimulationSM (the INACSL Standards), provides guidelines for simulation design, outcomes and objectives, and professional integrity (INACSL Standards Committee, 2016), among other aspects, providing a strong foundation for simulation-based education when developing, implementing, and evaluating SBL.
B. Use of Simulation-based Learning in Japan
In Japan, although there have been many studies on individual educators’ simulation-based education practices, the research has been largely exploratory (Inagaki et al., 2018; Inukai & Nagosi, 2018; Yagi, 2018). In addition, there are very few examples of instructions based on set standards like the INACSL standards. The spread of SBL and the increase in nursing schools have caused the following problems: lack of educators with SBL experience, difficulty ensuring an appropriate learning environment, and procuring quality educators, among others. For future curriculum integration, learning program reviews and the current use of SBL must be identified. Therefore, this national survey aimed to clarify the prevalence and practices of SBL in undergraduate nursing education in Japan.
II. METHODS
A. Research Period
Data were collected from November 1, 2019, to January 31, 2020.
B. Subjects
This study constituted a survey that was conducted on the nursing specialties of all nursing schools in Japan. The research subject institutes were a total of 730 nursing schools in Japan, including 263 universities or colleges awarding a baccalaureate degree, 18 junior colleges awarding an associate degree, and 449 vocational schools awarding a diploma. The research subjects were 5,110 individuals consisting of a sample of coordinators in seven nursing specialties per school, namely foundations of nursing, adult nursing, geriatric nursing, pediatric nursing, maternal nursing, psychiatric nursing, and home nursing. The inclusion criteria of our study were the respondents nominated by the head of the education / research institution, nursing department, or nursing vocational school corresponding to the seven specialties. The criteria for nomination were those most involved in SBL in that particular specialty, and those responsible for exercises, if unknown. Thus, the individual and nursing specialty means the same. Out of the total number of 5110 individuals, the calculation of sample size was done with an acceptable error of 5%, a confidence level of 95%, and a response rate of 50%. It indicated that at least 358 respondents were required to fulfil the objectives of this study. The total number of respondents in our study was 420.
C. Data Collection
An independently created, anonymous, self-administered online questionnaire survey (survey) was conducted via Survey Monkey. The head of the education/research institution, nursing department, or nursing vocational school at each of the 730 nursing schools in Japan was sent a request for research participation, the access code necessary for the survey, and contact information of the researchers. Responses were then requested from seven individuals nominated by the head of the education/research institution, nursing department, or nursing vocational school corresponding to the seven specialties. The research subjects accessed Survey Monkey using the access code provided.
D. Survey Content
In the questionnaire, school characteristics and the status of SBL used were created independently based on previous research. The main items in the questionnaire were developed following the INACSL Standards. (Beroz, 2017; Gore et al., 2012; Hayden, 2010; Utsumi et al., 2017). Each item was discussed by the research members and the validity of the content was confirmed. In addition, a pilot test was conducted on several faculty members at the authors’ institution. The target faculty members for this pilot test were selected and requested to be non-responders to this survey. As a result of the pilot test, the wording of the items was corrected and explanations were added to simulation-specific terms such as S.M.A.R.T (specific, measurable, assignable, realistic, and time related) (Doran, 1981), cue, and professional integrity.
1) School characteristics: This section comprised three items including the facility type of the subject’s affiliated school, the respondent’s primary specialisation, and the number of faculty members.
2) The status of SBL use: This section comprised 11 items including the status of simulation-based education use, whether the school was equipped with a simulator, frequency of simulator use, and adoption in the curriculum.
3) The status of the INACSL Standards application: Each item of the INACSL Standards was incorporated as a question resulting in a total of 41 questions. Permission to use a Japanese version of the INACSL Standards was granted by the developer.
E. Data Analysis
Descriptive statistics were used to analyse school characteristics and survey forms. Excel 2019 and SPSS Statistics (Version 24.0) was used to manage data collection and conduct analysis.
F. Ethical Considerations
When providing an explanation and acquiring consent from survey respondents, it was made clear that subjects could decide whether to participate according to their own free will, that there would be no disadvantages for nonparticipation, and that withdrawal from participation after submission would not be feasible as it would be impossible to match individuals to any one anonymous online survey, as no personal identifiable data were collected. Respondents were sent the survey via Survey Monkey and communication was protected. The consent form was added to Survey Monkey and respondents had to consent prior to accessing it. Concerning the security of Survey Monkey, the service used for this study, communications were protected through SSL/TLS encryption, and access was restricted for all ports aside from 80 and 443 (https) using a firewall.
III. RESULTS
A. School Characteristics
Requests were sent to 5,110 individuals (one for each of the seven specialties at 730 schools) and 639 responses were received (response rate 12.5%). Of these, 420 respondents completed the entire survey (8.2%). The respondents’ affiliated schools included 132 universities and colleges (31.4%), 7 junior colleges (1.7%), and 281 vocational schools (66.9%). Thus, over half of the respondents were affiliated with vocational schools as shown in Table 1 (Masuda, 2021).
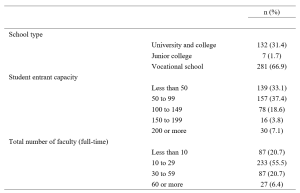
Table 1. School type, entrant capacity, and number of faculty
B. SBL Use
1) SBL use and equipping a high-fidelity and a medium-fidelity simulator and task trainer use: Concerning the status of SBL use, 346 schools (82.4%) responded that they are using SBL, while 74 schools (17.6%) responded that they are not. Among all schools surveyed, 346 (82.4%) were equipped with a simulator for medical/nursing education, while 74 (17.6%) were not. Concerning simulator types, the most common high-fidelity simulator capable of modelling biological reactions and pathology and performing drug administration and other procedures was the SimMan®, which was owned by 27 schools (6.4%) followed by a delivery simulator owned by 25 schools (6.0%). SCENARIO was also common (21 schools, 5.0%). SCENARIO is a high-fidelity simulator similar to SimMan® which hit the market in Japan in 2017 but is cheaper than SimMan®. Meanwhile, roughly 70% of schools (304 schools, 72.4%) were not equipped with a high-fidelity simulator. There were 361 schools (86.0%) equipped with at least one type of medium-fidelity simulator, allowing control of the creation of biological responses such as breath sounds, consciousness, and blood pressure. Regarding virtual reality (VR), 409 schools (97.4%) did not have VR facilities. VR refers to a computer-generated simulation in which a person can interact within an artificial three-dimensional environment using electronic devices, such as special goggles with a screen or gloves fitted with sensors. In this simulated artificial environment, the user is able to have a realistic-feeling experience. Concerning standardised patient (SP) simulation, 164 schools (39.0%) reported that they used SP while 254 schools (60.5%) did not, as shown in Table 2 (Masuda, 2021).
|
n (%) |
n (%) |
||||||||
|
Foundation |
Adult |
Pediatric |
Maternal |
Geriatric |
Psychiatric |
Home |
|||
|
Using simulation-based education (schools) |
|||||||||
|
Yes |
346 (82.4) |
||||||||
|
No |
74 (17.6) |
||||||||
|
Using simulation-based education (specialties) |
|||||||||
|
Yes |
223 (53.1) |
58 (16.8) |
55 (15.9) |
44 (12.7) |
48 (13.9) |
57 (16.5) |
45 (13.0) |
39 (11.3) |
|
|
No |
197 (46.9) |
22 (11.2) |
27 (13.7) |
20 (10.2) |
19 (9.6) |
40 (20.3) |
43 (21.8) |
26 (13.2) |
|
|
Equipped with a simulator for medical/nursing education (schools) |
|||||||||
|
Yes |
346 (82.4) |
||||||||
|
No |
74 (17.6) |
||||||||
|
Equipped with a high-fidelity simulator*1 (may select multiple answers) |
|||||||||
|
SimMan® |
27 (6.4) |
6 (22.2) |
4 (14.8) |
4 (14.8) |
2 (7.4) |
7 (25.9) |
3 (11.1) |
1 (3.7) |
|
|
iStan® |
2 (0.5) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (50.0) |
0 (0.0) |
0 (0.0) |
1 (50.0) |
|
|
Apollo™ |
1 (0.2) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (100.0) |
|
|
BabySim® |
11 (2.6) |
2 (18.2) |
1 (9.1) |
3 (27.3) |
1 (9.1) |
2 (18.2) |
1 (9.1) |
1 (9.1) |
|
|
Delivery simulator |
25 (6.0) |
3 (12.0) |
3 (12.0) |
1 (4.0) |
7 (28.0) |
4 (16.0) |
3 (12.0) |
4 (16.0) |
|
|
SCENARIO |
21 (5.0) |
7 (33.3) |
5 (23.8) |
2 (9.5) |
2 (9.5) |
2 (9.5) |
3 (14.3) |
0 (0.0) |
|
|
Equipped with other high-performance simulator |
59 (14.0) |
13 (22.0) |
9 (15.3) |
10 (16.9) |
5 (8.5) |
9 (15.3) |
8 (13.6) |
5 (8.5) |
|
|
Not equipped with a high-fidelity simulator |
304 (72.4) |
44 (14.5) |
45 (14.8) |
34 (11.2) |
43 (14.1) |
54 (17.8) |
38 (12.5) |
46 (15.1) |
|
|
Equipped with a medium-fidelity simulator*2 (may select multiple answers) |
|||||||||
|
Physiko |
265 (63.1) |
61 (23.0) |
50 (18.9) |
21 (7.9) |
25 (9.4) |
44 (16.6) |
26 (9.8) |
38 (14.3) |
|
|
Nursing Anne® |
46 (11.0) |
7 (15.2) |
11 (23.9) |
3 (6.5) |
6 (13.0) |
5 (10.9) |
7 (15.2) |
7 (15.2) |
|
|
SimManALS® |
13 (3.1) |
4 (30.8) |
3 (23.1) |
0 (0.0) |
0 (0.0) |
1 (7.7) |
4 (30.8) |
1 (7.7) |
|
|
Other |
37 (8.8) |
10 (27.0) |
5 (13.5) |
9 (24.3) |
9 (24.3) |
2 (5.4) |
1 (2.7) |
1 (2.7) |
|
|
Not equipped with a medium-fidelity simulator |
138 (32.9) |
7 (5.1) |
11 (8.0) |
18 (13.0) |
29 (21.0) |
28 (20.3) |
27 (19.6) |
18 (13.0) |
|
|
Equipped with a task trainer*3 |
|||||||||
|
Yes |
331 (78.8) |
62 (18.7) |
53 (16.0) |
42 (12.7) |
49 (14.8) |
50 (15.1) |
30 (9.1) |
45 (13.6) |
|
|
No |
89 (21.2) |
7 (7.9) |
11 (12.4) |
7 (7.9) |
9 (10.1) |
22 (24.7) |
22 (24.7) |
11 (12.4) |
|
|
Equipped with VR |
|||||||||
|
Yes |
11 (2.6) |
1 (9.1) |
3 (27.3) |
2 (18.2) |
0 (0.0) |
2 (18.2) |
1 (9.1) |
2 (18.2) |
|
|
No |
409 (97.4) |
68 (16.6) |
61 (14.9) |
47 (11.5) |
58 (14.2) |
70 (17.1) |
51 (12.5) |
54 (13.2) |
|
|
Using standardised patients in simulation (specialties) |
|||||||||
|
Yes |
164 (39.0) |
38 (23.2) |
30 (18.3) |
16 (9.8) |
22 (13.4) |
27 (16.5) |
10 (6.1) |
21 (12.8) |
|
|
No |
254 (60.5) |
31 (12.2) |
34 (13.4) |
33 (13.0) |
35 (13.8) |
45 (17.7) |
41 (16.1) |
35 (13.8) |
|
*1 High-fidelity simulator: The broad range of full body manikins that have the ability to mimic, at a very high level, human body functions (Lioce et al., 2020).
*2 Medium-fidelity simulator: The broad range of full body mannequins with installed human qualities such as breath sounds without chest rise (Smiley, 2019).
*3 Task trainer: A device designed to provide training in just the key elements of the procedure or skill being learned, such as lumbar puncture, or part of total system (Lioce et al., 2020).
Table 2. Simulation-based education use, equipping a high-fidelity and medium-fidelity simulator, and task trainer use
2) Frequency of simulator use and adoption in the curriculum: The application of SBL was infrequent with most schools (98 schools, 23.3%) using such programs once every year, followed by 97 schools (23.1%), which used SBL once every six months, and 72 schools (17.1%) using them once every two to three months, as shown in Table 3 (Masuda, 2021).
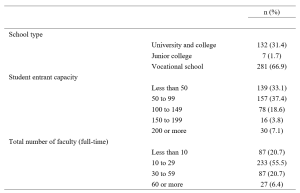
Table 3. Frequency of simulator use and adoption in the curriculum
C. The Status of INACSL Standards Application
Awareness of the INACSL Standards was low with over 90% of respondents stating, “I don’t know of them” (383 respondents, 91.2%) and only 8.8% (37 respondents) stating “I know of them.” Nonetheless, looking at specific items concerning simulation design, over half of the respondents reported using learning objectives, scenario design, methods for ensuring fidelity, learner levels and outcomes, and debriefing. However, rates of application were low for all other items, reaching only 20 to 30%, as shown in Supplementary Table S1 (Masuda, 2021).
IV. DISCUSSION
A. The Status of SBL Use
We surveyed the status of SBL use at nursing schools throughout Japan. The results revealed that 82.4% of those surveyed, use simulation-based education, validating that SBL is widespread in undergraduate nursing education. A nationwide survey in the United States in 2015 found the rate to be 99% (Breymier et al., 2015). Thus, although SBL is gaining popularity in Japan, the country continues to trail the United States in overall usage. Concerning the use of SBL by specialty, simulation is commonly used in foundation of nursing, followed by adult nursing and geriatric nursing. Meanwhile, simulation is used by less than 50% of schools for maternal nursing, pediatric nursing, psychiatric nursing, and home nursing. In countries such as the United States and South Korea, it is primarily used for specialties that require clinical practice in hospitals, such as adult nursing, and clinical nursing, but use for psychiatric and home nursing is limited (Kardong-Edgren et al., 2012; Shin et al., 2015). Thus, our findings were similar to those in these previous studies (Kardong-Edgren et al., 2012; Shin et al., 2015). The less frequent use of psychiatric and home nursing may be due to the inappropriate use of simulators such as SimMan® for medical field or the limited number of simulators in schools.
Concerning schools being equipped with simulators, roughly only 30% of schools had a high-performance simulator, but in comparison mid-level performance simulators were common, being present at approximately 80% of schools. Previous studies (Hayden, 2010; Smiley, 2019) and a meta-analysis (Kim et al., 2016) have shown that roughly 90% of schools implement programs, using either a high- or medium-fidelity simulator. It seems that Japan is catching up to countries with advanced SBL in terms of access to high- and medium-fidelity simulators. In addition, it is that the results were similar to 77.8% equipped with a task trainer of the schools. Nonetheless, the results of the present survey revealed that the frequency of use remains low. In other words, our findings suggest that although Japanese schools are sufficiently equipped with simulators, they are not optimally used.
Simulators are an expensive instructional tool, but it is not enough to simply purchase them. It is essential to further study the obstacles to their application and prepare an environment in which their use is possible. While high- and medium-fidelity simulators from Laerdal Medical were common, use of SCENARIO—a simulator put on the market by Kyoto Kagaku Co., Ltd. in 2017—is rapidly increasing. This rise may be influenced by the fact that SCENARIO is made in Japan. Moreover, not only is SCENARIO lightweight and relatively cheap, it also features native Japanese instructions reflecting the clinical situation, culture, and background of Japan rather than scenarios and an instruction manual written in English. Regarding simulator access by different specialties, it is only natural that the results matched those for the status of simulator-based education use, with foundation of nursing, adult nursing, and geriatric nursing having the most simulators. The rate of 39% of SP utilisation found in this survey was on par with the rate of 36% in bachelor’s programs in the United States (Kardong-Edgren et al., 2012), and a systematic review of 40 published studies from countries such as the United States, South Korea, UK, Australia, found that 25% used SPs (Kim et al., 2016). On the other hand, our results revealed that VR is virtually unused in undergraduate nursing education in Japan. This lags behind the US results of 25% for use in internet-based virtual hospitals and 34% for virtual intravenous injection programs (Kardong-Edgren et al., 2012).
Regarding the adoption of SBL into the curriculum, over half of the schools surveyed featured SBL in their present curriculum, and this inclusion can be expected to increase further as schools plan to transition to new curriculums shortly. Integration of simulation-based education into the curriculum is already in progress in the United States with studies finding that up to 50% of the time spent on clinical practice could be replaced with simulation-based learning with no change in learning outcomes (Hayden et al., 2014). Studies exploring how much of the curriculum has been replaced are also underway (Breymier et al., 2015; Gore et al., 2012; Hayden, 2010; Smiley, 2019). Based on current regulations of Ministry of Education, Culture, Sports, Science and Technology of Japan, the clinical experience cannot be replaced by simulation but is expected to become possible in the future as curriculum integration progresses. As such, integration of simulation into a curriculum requires a meticulous review of the program of study to identify gaps where simulation best fits to increase learning (Hodge et al., 2008). Additionally, past research on barriers to curriculum integration of simulation-based experience found that lack of time for faculty development was the primary barrier (Adamson, 2015; Sole et al., 2013). Therefore, it will be necessary to account for all obstacles to curriculum integration.
B. The Status of the INACSL Standards Application
Among the theoretical frameworks of SBLs, it was inferred that the Japanese version was the INACSL Standards to be developed and relatively known. Therefore, in this study, we investigated the awareness of the INACSL Standards. As a result, unfortunately, we found that awareness was extremely low and that these standards are not widespread in Japanese undergraduate nursing education. However, the results also suggested that over half of respondents implemented learning objectives, scenario design, methods for ensuring fidelity, learner levels and outcomes, and debriefing on simulation design. A survey of the status of simulation used by the INACSL found the use of conceptual frameworks and theories to be approximately 50% and described this result as extremely low (Beroz, 2017). The results of the present survey found an even lower rate with roughly 90% of respondents stating that they did not know of the INACSL Standards. However, even without having prior knowledge regarding the INACSL Standards, over half of the respondents were following the best practice standards in terms of simulation design. Therefore, it is imperative to correctly understand and apply theories and conceptual frameworks to teaching strategies rather than to know their official names. Nearly half of the educators surveyed were designing their simulation programs according to the INACSL Standards, which is considered a positive result. Despite these positive results for simulation design, other items were found to have low utilisation. It is thought that further popularisation of other items will lead to a comprehensive understanding of simulation program design.
C. Study Limitations
Online surveys are not yet widespread in undergraduate nursing education in Japan. It is also presumed that in Japanese undergraduate nursing educations, the coordinators of the nursing specialties are often held by professors or associate professors, and that the age groups of the subjects were relatively high. Therefore, it is considered that the participants may not be familiar with the online surveys. The inclusion criterion for subjects should have included someone familiar with on-line manipulations such as SurveyMonkey. In addition, it may be a deficiency in due to the lengthiness of the questionnaire, improper selection of respondents, response items or the data collection period has not been sufficiently taken. This aspect was the bias of this survey and may explain the low response rate.
In addition, the development of the questionnaire used in this study is limited to content validation, and no examination of construct validity has been conducted. Therefore, there is a limitation that the validity of the questionnaire is insufficient.
Regarding the classification of simulators, in our study, SimMan ALS® was included in a medium-fidelity simulator, and SimMan® was included in a high-fidelity simulator. However, SimManALS® can also be captured as a high-fidelity simulator. This may have influenced the scoring of “others”. In this study, a completed survey was conducted, and randomisation of confounders was not possible.
Therefore, based on the results obtained in this study, we will plan a more focused survey in the future. We suggest that the results of this study can be used to promote SBL in a more specific method.
Lastly, in 2020-21, opportunities for nursing students to complete practical training in medical facilities are limited as a result of the global pandemic of COVID-19. Hence, it can be said that SBL will play a major role in maintaining learning opportunities and clinical competence in students while ensuring the safety of patients, students, and medical staff. We plan to continue and expand upon our survey research to enable more educational institutions to begin practicing SBL.
V. CONCLUSION
In conclusion, this study provided an initial view of the current status of SBL in Japan. Our results suggested that while many schools are equipped with simulators, they are not properly utilised in the foundation of nursing programs in Japan. Thus, further study of barriers to simulator use is needed. Also, although awareness of INACSL Standards was extremely low, over half of the respondents were designing simulations following the standards, implying that they were making use of some theories or conceptual frameworks in their designs. Our results act as a foundational resource for studying strategies intended to systemise SBL in Japanese undergraduate nursing education. In the future, it will be necessary to specifically survey awareness and use of theories and conceptual frameworks to recommend methods for increasing their application and use in SBL.
Notes on Contributors
Dr. Mitsumi Masuda, PhD, RN, is an associate professor at the Graduate School of Nursing, Nagoya City University. She reviewed the literature, designed the study, performed data collection, data analysis and wrote the manuscript.
Dr. Machiko Saeki Yagi, MS, RN, is a lecturer at the School of Nursing, Jichi Medical University. She developed the methodological framework for the study, performed data collection, data analysis and gave critical feedback to the writing of the manuscript.
Dr. Fumino Sugiyama, PhD, RN, is an associate professor at the School of Nursing, National College of Nursing. She performed data collection and data analysis. All the authors have read and approved the final manuscript.
Ethical Approval
This research was approved by the research ethics review committee of the Nagoya City University, Graduate School of Nursing (Approval no.: 19019-2).
Data Availability
Datasets generated and/or analysed during the current study are available from the following DOI. https://doi.org/10.6084/m9.figshare.14010755.v1.
Acknowledgement
This study was completed with the support of The Murata Science Foundation (2019 No. 28). In addition, we would like to thank Editage (www.editage.com) for assisting with English language editing. We would like to offer our heartfelt thanks to the nursing schools across the country who participated in this study.
Funding
This study was completed with the support of The Murata Science Foundation (2019 No. 28).
Declaration of Interest
The authors declare that they have no competing interests.
References
Adamson, K. (2015). A systematic review of the literature related to the NLN/Jeffries simulation framework. Nursing Education Perspectives, 36(5), 281–291. https://doi.org/10.5480/15-1655
Alexander, M., Durham, C. F., Hooper, J. I., Jeffries, P. R., Goldman, N., Kardong-Edgren, S. S., Kesten, K. S., Spector, N., Tagliareni, E., Radtke, B., & Tillman, C. (2015). NCSBN simulation guidelines for prelicensure nursing programs. Journal of Nursing Regulation, 6(3), 39–42. https://doi.org/10.1016/S2155-8256(15)30783-3
Beroz, S. (2017). A statewide survey of simulation practices using NCSBN simulation guidelines. Clinical Simulation in Nursing, 13(6), 270–277. https://doi.org/10.1016/j.ecns.2017.03.005
Boling, B., & Hardin-Pierce, M. (2016). The effect of high-fidelity simulation on knowledge and confidence in critical care training: An integrative review. Nurse Education in Practice, 16(1), 287–293. https://doi.org/10.1016/j.nepr.2015.10.004
Breymier, T. L., Rutherford-Hemming, T., Horsley, T. L., Atz, T., Smith, L. G., Badowski, D., & Connor, K. (2015). Substitution of clinical experience with simulation in prelicensure nursing programs: A national survey in the United States. Clinical Simulation in Nursing, 11(11), 472–478. https://doi.org/10.1016/j.ecns.2015.09.004
Carter, A. G., Creedy, D. K., & Sidebotham, M. (2016). Efficacy of teaching methods used to develop critical thinking in nursing and midwifery undergraduate students: A systematic review of the literature. Nurse Education Today, 40, 209–218. https://doi.org/10.1016/j.nedt.2016.03.010
Chiniara, G., Cole, G., Brisbin, K., Huffman, D., Cragg, B., Lamacchia, M., Norman, D., Canadian Network For Simulation In Healthcare, & Guidelines Working Group. (2013). Simulation in healthcare: A taxonomy and a conceptual framework for instructional design and media selection. Medical Teacher, 35(8), e1380–e1395. https://doi.org/10.3109/0142159X.2012.733451
Doran, G. T. (1981). There’s a S.M.A.R.T. way to write management’s goals and objectives. Management Review, 70(11), 35-36.
Gore, T., Van Gele, P., Ravert, P., & Mabire, C. (2012). A 2010 survey of the INACSL membership about simulation use. Clinical Simulation in Nursing, 8(4), e125-e133. https://doi.org/10.1016/j.ecns.2012.01.002
Hayden, J. (2010). Use of simulation in nursing education: National survey results. Journal of Nursing Regulation, 1(3), 52–57. https://doi.org/10.1016/S2155-8256(15)30335-5
Hayden, J. K., Smiley, R. A., Alexander, M., Kardong-Edgren, S., & Jeffries, P. R. (2014). The NCSBN national simulation study: A longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. Journal of Nursing Regulation, 5(2), S3–S40. https://doi.org/10.1016/S2155-8256(15)30062-4
Hodge, M., Martin, C. T., Tavernier, D., Perea-Ryan, M., & Alcala-Van Houten, L. (2008). Integrating simulation across the curriculum. Nurse Educator, 33(5), 210–214. https://doi.org/10.1097/01.NNE.0000312221.59837.38
INACSL Standards Committee. (2016). INACSL standards of best practice: SimulationSM Simulation design. Clinical Simulation in Nursing, 12(S), S5–S12. https://doi.org/10.1016/j.ecns.2016.09.005
Inagaki, N., Inagaki, M., & Kobe, M. (2018). The perceptions of students concerning the changes in their thinking and exercise utilization caused by simulation exercises for critical care nursing practicums. Journal of Nursing Setanan University, 6(1), 3–11.
Inukai, T., & Nagosi, M. (2018). Students’ learning through a simulated seminar using SBAR.https://doi.org/10.15009/00002249
Kardong-Edgren, S., Willhaus, J., Bennett, D., & Hayden, J. (2012). Results of the national council of state boards of nursing national simulation survey: Part Ⅱ. Clinical Simulation in Nursing, 8(4), e117–e123. https://doi.org/10.1016/j.ecns.2012.01.003
Kim, J., Park, J.-H., & Shin, S. (2016). Effectiveness of simulation-based nursing education depending on fidelity: A meta-analysis. BMC Medical Education, 16, 152. https://doi.org/10.1186/s12909-016-0672-7
Lioce, L., Lopreiato, J., Downing, D., Chang, T. P., Robertson, J. M., Anderson, M., Diaz, D. A., Spain, A. E., & the Terminology and Concepts Working Group. (2020). Healthcare Simulation Dictionary -Second Edition. Retrieved from: https://doi.org/10.23970/simulationv2
Masuda, M. (2021). Materials (TAPS) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14010755.v1
Pal, B., Kumar, M. V., Kyaw Soe, H. H., & Pal, S. (2018). A study on the usefulness of high fidelity patient simulation in undergraduate medical education. The Asia Pacific Scholar, 3(1), 42-49.https://doi.org/10.29060/TAPS.2018-3-1/SC1059
Shin, S., Park, J.-H., & Kim, J.-H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Education Today, 35(1), 176–182. https://doi.org/10.1016/j.nedt.2014.09.009
Smiley, R. A. (2019). Survey of simulation use in prelicensure nursing programs: Changes and advancements, 2010-2017. Journal of Nursing Regulation, 9(4), 48–61. https://doi.org/10.1016/S2155-8256(19)30016-X
Sole, M. L., Betsy Guimond, M. E., & Amidei, C. (2013). An analysis of simulation resources, needs, and plans in Florida. Clinical Simulation in Nursing, 9(7), E265–E271. https://doi.org/10.1016/j.ecns.2012.03.003
Utsumi, M., Tokunaga, J., Hirano, S., Fujii, Y., Takamura, N., & Yamamoto, H. (2017). Status of clinical skills education in faculties of pharmaceutical sciences in Japan: A follow-up report. Journal of Japan Association for Simulation-based Education in Healthcare Professionals, 5, 9–16.
Yagi, S. M. (2018). Simulation training for nurses in specified medical acts. The Journal of Japan Society for Clinical Anesthesia, 38(1), 83–87. https://doi.org/10.2199/jjsca.38.83
Zarifsanaiey, N., Amini, M., & Saadat, F. (2016). A comparison of educational strategies for the acquisition of nursing student’s performance and critical thinking: Simulation-based training vs. integrated training (simulation and critical thinking strategies). BMC Medical Education, 16(1), 294. https://doi.org/10.1186/s12909-016-0812-0
*Mitsumi Masuda
1, Kawasumi, Mizuho-cho,
Mizuho-ku, Nagoya,
467-8601, Japan.
Tel: +81-52-853-8063
Email: m.masuda@med.nagoya-cu.ac.jp
Submitted: 19 February 2021
Accepted: 17 June 2021
Published online: 4 January, TAPS 2022, 7(1), 33-43
https://doi.org/10.29060/TAPS.2022-7-1/OA2493
Chan Choong Foong*, An Jie Lye*, Che Rafidah Aziz, Wei-Han Hong, Vinod Pallath, Jessica Grace Cockburn, Siti Nurjawahir Rosli, Kuhan Krishnan, Prahaladhan Sivalingam, Noor Filzati Zulkepli & Jamuna Vadivelu
Medical Education & Research Development Unit (MERDU), Faculty of Medicine, University of Malaya, Malaysia
*Joint first authors
Abstract
Introduction: Medical schools universally responded by migrating teaching and learning to virtual learning environments (VLE) due to the impact of the COVID-19 pandemic. The use of virtual problem-based learning (PBL) in lieu of face-to-face sessions seems to be an appropriate response, but its effectiveness was understudied. The study compared the learning experiences of pre-clinical medical students at the beginning and completion of the virtual PBL.
Methods: The study was conducted at the University of Malaya, a public-funded university in Malaysia. A 12-item questionnaire was developed and validated to assess the learning experiences of students conducting virtual PBL sessions. Principal component analysis and test for internal consistency suggested that the questionnaire is valid and reliable. The questionnaire was administered to pre-clinical students (Year 1 and Year 2) twice: at the beginning and the end of the virtual PBL implementation. Their responses were compared for the domains “learning”, “confidence” and “concern”.
Results: Three hundred and forty-four pre-clinical students were recruited but only 275 students (80%) responded to both the initial and final questionnaires. Based on the responses, the learning experiences of students generally improved by the completion of the virtual PBL implementation. Students were most convinced that they obtained and understood the information given during the virtual PBL. However, they continued to be worried about passing the clinical examination and content acquisition.
Conclusion: The study supports the feasibility of virtual PBL as an acceptable alternative to replace face-to-face PBL during the COVID-19 pandemic.
Keywords: Problem-based Learning, COVID-19, Undergraduate Medical Education, Virtual Learning Environment
Practice Highlights
- The study compared the learning experiences of pre-clinical medical students in virtual Problem Based Learning (PBL).
- The learning experiences of students in virtual PBL generally improved.
- Students obtained and understood the information given during the virtual PBL.
- Students continued to be worried about passing the clinical examination and content acquisition.
- Virtual PBL could be an acceptable alternative to replace face-to-face PBL during the pandemic.
I. INTRODUCTION
The novel coronavirus disease, COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and characterised by pneumonia-like symptoms, was identified on January 7, 2020. The World Health Organization declared a pandemic on March 11, 2020, due to the rapid global increase in reported cases (World Health Organization, 2020). The first COVID-19 positive case in Malaysia was reported on January 25 and the first fatal case on March 17 of 2020 (Shah et al., 2020). A Movement Control Order (MCO) was issued by the Malaysian Government on March 18 to reduce the spread of COVID-19 in Malaysia (Shah et al., 2020). As mandated by the MCO, schools, and universities were closed to reduce the transmission of COVID-19.
The order to close the universities greatly affected the undergraduate medical program, particularly because students spend a large portion of time in physical classrooms, medical clinics, and face-to-face discussions. The University of Malaya was not isolated in this challenge, as the outbreak of COVID-19 affected medical schools worldwide (Ferrel & Ryan, 2020; Khalil et al., 2020; Reyna, 2020; Yusoff et al., 2020). Medical schools universally responded by migrating teaching and learning to virtual learning environments (VLE) to maintain planned 2019-2020 academic calendars as much as possible (Alkhowailed et al., 2020; Khalil et al., 2020). Most of the theoretical teaching and learning activities, such as lectures, seminars, and small group problem-based learning (PBL), were transferred to digital platforms to accommodate social distancing practices amidst the COVID-19 pandemic (Abbas, 2020; Alkhowailed et al., 2020). Online learning has increasingly complemented traditional face-to-face teaching in medical education in recent years (Ifediora, 2019), but the COVID-19 pandemic has expedited this transition in only months (Abedi & Abedi, 2020; Alkhowailed et al., 2020; Ebner et al., 2020; Tabatabai, 2020). Digitalisation has made the studies available for students regardless of their geographical locations and local circumstances (Laamanen et al., 2021).
It was a necessary assumption by medical education administrators that virtual PBL sessions would be an acceptable alternative to the planned face-to-face PBL sessions during the course of the COVID-19 pandemic. This included student participation from external locations using online platforms, such as Microsoft Teams and Zoom (Coiado et al., 2020), or customized information technology packages (Musal et al., 2017). This strategy ensured physical distancing practices were followed, as students remained isolated, while they were still able to actively participate in PBL discussions. Despite the change to a VLE, tutors and students were asked to adapt to the virtual environment to ensure that students could still practice communication, clinical reasoning, and presentation skills (Joseph et al., 2016). Additionally, course outcomes and student expectations, including positive interactions and participation, remained the same as those of face-to-face PBL sessions. However, the effect of the transition to virtual PBL sessions in the middle of a term on the development of these competencies was unknown. Research is therefore essential to assess the usefulness of those alternative plans for the COVID-19 pandemic (Foong, 2020). There are a few attempts to assess the effectiveness of fully online education amidst the COVID-19 pandemic, but these studies were generic to large-group learning, limited attempts explained the impacts on small-group interactive learning such as PBL (Hew et al., 2020; Schlenz et al., 2020).
Conveniently, administrators could draw on the results from studies that have reported on the implementation, effectiveness, and experiences of conducting planned virtual PBL sessions (Car et al., 2019; Musal et al., 2017; Valaitis et al., 2005). Virtual PBL sessions have shown to be effective as students have reported increased flexibility for learning, improved ability to process content, and improved access to valuable learning resources (Coiado et al., 2020; Valaitis et al., 2005). A systematic review also suggests that virtual PBL is not only as effective as traditional PBL but that it may be more effective at improving skills (Car et al., 2019). However, students have also reported technical difficulties, perceived increased workload, and asynchronous communication (Coiado et al., 2020; Musal et al., 2017; Valaitis et al., 2005). Overall, the use of virtual PBL in lieu of face-to-face sessions is an appropriate response, particularly facing the challenges of the COVID-19 pandemic.
Medical schools have globally responded to the COVID-19 pandemic by continuing programming by offering PBL in VLEs (Coiado et al., 2020; Khalil et al., 2020). It is necessary to measure the effectiveness and success of a transition to virtual PBL, particularly in environments where students were unfamiliar with the VLE at the beginning of their PBL sessions. The success of this transition may also indicate the success of the continued delivery of medical education using VLEs in other courses as well. This study aimed to assess the learning experiences of pre-clinical medical students on the implementation of the virtual PBL, in replacing the traditional in-person learning space. We compared the experiences of pre-clinical medical students at the beginning and completion of the virtual PBL since student perception is a measure of effectiveness and success of the curricula (Degtjarjova et al., 2018). This study helped to understand students’ experiences of an unexpected transition to the virtual PBL during the COVID-19 pandemic.
A. Theoretical Framework
We used the ACTIONS model (Access, Costs, Teaching and learning, Interaction and user-friendliness, Organisational issues, Novelty, and Speed) by Tony Bates to develop the VLE in a timely and resource-efficient manner (Boettcher & Conrad, 1999). We prioritised the consideration in Access and Costs since the University of Malaya was unable to provide unlimited internet subscriptions and access to all students and lecturers. This is, of course, required to establish an effective VLE. Teaching and learning and Interaction and user-friendliness were also important factors of the framework that were considered before finally selecting Microsoft Teams and OneNote. The software was able to support both the user demand and could host large and small group sessions. Finally, Microsoft Teams and OneNote were also able to satisfy the Organisational issues and Novelty and Speed properties of the VLE. The University of Malaya was able to provide appropriate information technology (IT) support by expanding online resources to be synchronised, aligned, and integrated. Ultimately, the university managed to provide a centralised platform for teaching and learning through Microsoft Teams and OneNote.
II. METHODS
The curriculum team, faculty development team, IT team, and programme evaluation team at the Medical Education Unit were involved in designing, implementing, and evaluating the virtual PBL.
A. Designing the Virtual PBL
The University of Malaya had been practicing face-to-face PBL weekly. There were eight students assigned to a group, and the discussion was facilitated by a trained tutor. In a PBL room, students discussed at a round table and scribed their points of discussion on the whiteboards. When the virtual teaching and learning modality commenced, students and tutors conducted their PBL in a virtual learning space using Microsoft Teams, and they used Microsoft One Note as the virtual whiteboard. All the required materials, such as the handbooks, were made available online. Students participated in the virtual PBL sessions at their primary residences (off-campus).
B. Setting up Microsoft Teams, Microsoft One Note (Virtual Whiteboard), and Users Onboarding
The customisation of the features was performed by the IT team. They created, set up and, organised the virtual classrooms and relevant resources (e.g., user distribution list, naming structure). The instruction was given to students to register for a Microsoft Teams account. Every student was supplied with an installation guide, a user manual, and a video guide by the IT team. Meanwhile, the user manual for tutors provided additional information. Selected features (e.g., raise the hand, initiate chat, share screen, scribe) were introduced to promote interactions with students. Tutors were also given operational access to record sessions. The recordings were stored in the Microsoft Streams for students to use for revision.
C. Training Tutors and Students
After the user manuals were distributed, training sessions and workshops were conducted to show the practical use of basic online interactive tools and the various features of Microsoft Teams and OneNote. In addition to this, a short session on experiencing virtual PBL was provided for tutors. Questions and concerns raised during each training session were resolved immediately by the IT team.
D. Implementation and Monitoring
The Medical Education Unit integrated student evaluation and tutor experiences in continually monitoring and improving the virtual PBL. The curriculum team monitored each of the allocated virtual PBL sessions to ensure the sessions were conducted as scheduled. Next, the faculty development team conducted a series of interviews with 20 tutors about the VLE. The information from these interviews was integrated into the future training of tutors. The faculty development team found that the tutors were able to navigate the VLE. The general attitude towards the VLE improved as tutors became more familiar with the platform. There were several reported issues, like poor connectivity and difficulty in navigating Microsoft Teams, these were all resolved by the IT team without affecting the delivery of the PBL materials. Finally, student feedback, through standardised evaluation forms, was collected by the programme evaluation team. The feedback was provided to tutors, and they were expected to integrate this feedback into the facilitation of subsequent virtual PBL sessions.
E. Assessing Learning Experiences of Students
A questionnaire was developed to measure the learning experiences of students in a transition to virtual PBL from face-to-face sessions. Items were designed using several resources: (1) the existing teaching criteria of the medical programme (e.g. based on the programme’s learning objectives) (Foong et al., 2015), (2) concerns raised by faculty lecturers prior to the implementation of virtual PBL (e.g. motivation, obtaining and understanding the information), (3) previous instruments in measuring the effectiveness of PBL (e.g. able to apply knowledge) (Yeo & Chang, 2017), (4) online learning (e.g. learn when I want) (Ngampornchai & Adams, 2016) and (5) education environment (e.g. confidence to pass the examination) (Roff, 2005). A pilot study was not possible due to limited time and the lack of a subject pool with experience with virtual PBL. As such, the programme evaluation team consisted of an educationist and two evaluation officers who reviewed the items. Ultimately, the instrument consisted of 13 items, with 5-point Likert-scale responses (1=strongly disagree, 2=disagree, 3=unsure, 4=agree, 5=strongly agree).
A prospective design was used to evaluate any change in experience between the beginning of implementation and the completion of all the virtual PBL sessions. The University of Malaya Research Ethics Committee (UM.TNC2/ UMREC-998) approved the instrument and design before the study was initiated. The questionnaire was distributed online to 344 pre-clinical (Year 1 and Year 2) medical students. Digital consent was obtained from students before they started to answer the online questionnaires. The first (initial) questionnaire was distributed to students one week after the implementation of the virtual PBL, May 4, 2020. One week later, students were sent one reminder. The same students were asked to complete the same questionnaire (final) a second time, after the completion of 13 virtual PBL sessions (i.e., two learning blocks). An invitation asking for participation was sent on July 27, 2020. Responses were initially opened for two weeks, and it was extended for another two weeks due to a low response rate. Initial and final questionnaire responses were matched using participant identities, after which responses were anonymised.
F. Data Analysis
All data were entered and analysed using IBM SPSS Statistics for Windows version 23.0. First, the construct validity and reliability of the questionnaire were assessed. A principal component analysis (PCA) was conducted on the 13-item instrument with varimax rotation. Overall, the Kaiser-Meyer Olkin (KMO) should be ≥ 0.7, and Bartlett’s Test measure of sampling adequacy should be significant at p= 0.05, to verify the appropriateness of using PCA (Bowling, 2009). For each component to exist, it should demonstrate an eigenvalue ≥ 1 in the Scree plot (Campbell et al., 2002). For items to be considered in components, the average communality after extraction should be greater than ≥0.6 for a sample size that exceeds 250 (Field, 2009). In addition, to consider the inclusion of an item for a component, the item should demonstrate factor loading ≥0.5 (Hair et al., 2009); an item with cross-loadings ≥0.5 should be excluded (Maskey et al., 2018). In terms of reliability, internal consistency using Cronbach’s alpha measure was analysed for the overall instrument and its domains. A Cronbach’s alpha coefficient of ≥0.5 would indicate an adequate internal consistency (Bowling, 2009; Verma et al., 2010). The corrected item-total correlation should be ≥ 0.2, and the effect of deleting an item on the Cronbach’s alpha coefficient is considered (Verma et al., 2010).
Second, descriptive statistics (e.g., frequencies, percentages, mean, standard deviation) were calculated for the demographics and each item. Next, the data followed non-normal distribution, so Wilcoxon signed-rank tests were used to compare item scores of the same students (paired samples) between the beginning and at the end of virtual PBL implementation. Third, the total score of the 12-item questions was compared between different years of study, genders, geographical locations, and online course experiences using the Mann-Whitney U test, respectively for initial and final questionnaires. Similarly, the total score was compared between different ages and household incomes using the Kruskal Wallis test, respectively for initial and final questionnaires.
III. RESULTS
A. Response Rate
Three hundred and forty-four students (N=344) (in 43 pre-assigned groups) began virtual PBL sessions when teaching and learning resumed on April 19, 2020. Students completed 13 PBL cases representing two learning blocks. Out of the 344 students, 293 students completed and submitted the initial questionnaire distributed at the beginning of the virtual PBL, and 317 students completed the final questionnaire distributed after completing the virtual PBL sessions. The number of students asked to participate was the same for both surveys. Upon matching the identities of respondents, 275 students (80%) responded to both the questionnaires, and whose data was used for further analysis. The remaining surveys were disregarded.
B. Psychometric Properties of the Questionnaire
A principal component analysis of 550 questionnaires produced the following results. During initial analysis, one item, ‘Overall, I believe that PBL using Microsoft Teams could replace face-to-face PBL sessions’, was excluded due to its factor loadings <0.5 in all components (Table 1). In the final analysis, the KMO measure for sampling adequacy was 0.85, and Bartlett’s test of sphericity produced an approximate chi-square of 4073.55, p< 0.01. Three components had eigenvalues >1.0 respectively, and in combination explained 71.42% of the variances (component 1 represents “Learning” = 27.80%; component 2 represents “Confidence” = 26.74%; component 3 represents “Concern” =16.89%). All the 12 items had factor loadings ≥0.5 and did not have cross-loading ≥0.5. An average communality after extraction of 0.65 was produced (max=0.90; min=0.55).
Internal consistency was measured using Cronbach’s alpha coefficient. Overall, the questionnaire produced a high and satisfactory coefficient (α= 0.897). The coefficient for each domain was also satisfactory such that the ‘Learning’ subsection produced a value of 0.869, the ‘Confidence’ subsection produced a value of 0.856, and the ‘Concern’ subsection produced a value of 0.900. All items had corrected item-total correlation coefficients of ≥ 0.2; while if any item was to be removed, the Cronbach’s alpha coefficient will be reduced (Table 1). In conclusion, the questionnaire is valid and reliable.
|
|
No |
Statement |
Factor Loadings |
Cronbach Alpha (Overall or by Domain) |
Corrected Item-Total Correlation |
Cronbach Alpha if Item Deleted |
|
All items |
0.897 |
|||||
|
‘Learning’ Domain |
L1 |
I am able to learn anytime or anywhere that I want through PBL using Microsoft Teams |
0.86 |
0.869 |
0.670 |
0.846 |
|
L2 |
I am able to learn according to my pace or ability through PBL using Microsoft Teams |
0.84 |
0.692 |
0.842 |
||
|
L3 |
I am motivated to participate in PBL using Microsoft Teams for my studies |
0.65 |
0.690 |
0.843 |
||
|
L4 |
I am able to obtain adequate information based on the learning objectives through PBL using Microsoft Teams |
0.61 |
0.702 |
0.843 |
||
|
L5 |
I am able to understand the given information through PBL using Microsoft Teams |
0.61 |
0.689 |
0.846 |
||
|
L6 |
Advantages of PBL using Microsoft Teams outweigh its disadvantages |
0.52 |
0.623 |
0.860 |
||
|
‘Confidence’ Domain |
‘C1 |
I am confident to pass my clinical examination after participating in PBL using Microsoft Teams |
0.84 |
0.856 |
0.665 |
0.836 |
|
C2 |
I am confident to pass my knowledge-based written examination after participating in PBL using Microsoft Teams |
0.81 |
0.741 |
0.799 |
||
|
C3 |
I am confident to perform skills that I have gained through PBL using Microsoft Teams |
0.78 |
0.741 |
0.799 |
||
|
C4 |
I am confident to apply knowledge that I have gained through PBL using Microsoft Teams |
0.66 |
0.667 |
0.832 |
||
|
‘Concern’ Domain |
W1 |
(Reversed) I am worried that I might acquire less content through PBL using Microsoft Teams, as compared to face-to-face PBL sessions |
0.94 |
0.900 |
0.818 |
NA |
|
W2 |
(Reversed) I am worried that I might acquire the content slower through PBL using Microsoft Teams, as compared to face-to-face PBL sessions |
0.92 |
0.818 |
NA |
NA=Not Applicable
Table 1. Psychometric properties of the questionnaire
A. Demographics
The distribution of demographics was representative of the Year 1 and Year 2 pre-clinical student population based on student records (Table 2).
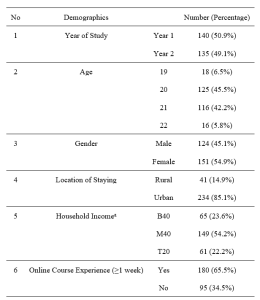
Note: aThe Malaysian government categorises its population into three income groups. T20 represents the top 20% income earners; M40 represents the middle 40% income earners; B40 represents the bottom 40% income earners.
Table 2. Demographics
A. Learning Experiences of Students
Student responses were assessed for their strength in agreement with each item in the initial and final questionnaires. The trends in response for items from each domain were also compared.
For the “Learning” domain, students reported learning experiences to be more positive than negative on a scale from 1.00 to 5.00 (Luciani et al., 2015) (Table 3). Many students indicated agreement for L1 to L5 (medianL1-L5=4.00), except for L6 (medianL6=3.00). In addition, students’ perceptions on learning through virtual PBL were significantly improved for items L2 (learn according to pace/ability) (p=.015), L3 (motivated) (p=.000), L4 (obtain adequate information) (p=.004), L5 (understand the information) (p=.003), and L6 (advantages outweigh disadvantages) (p=.041).
For the “Confidence” domain, students responded positively on average to all the items relating to confidence (medianC2-C4=4.00) except C1 (pass the clinical examination) (medianC4=3.00) (Table 3). Confidence of students was significantly higher at the end of the virtual PBL implementation in terms of C1 (pass the clinical examination) (p=.001), C2 (pass the knowledge-based written examination) (p=.000), and C4 (apply the gained knowledge) (p=.000); the increase in C3 (perform gained skills) was not significant (p=.067). Nevertheless, it is noted that students, while more agreed in the final questionnaire, remained mostly neutral towards their confidence to pass the clinical examination after participating in PBL using Microsoft Teams at the end of the implementation (medianinitial=3.00, medianfinal=3.00).
For the “Concern” domain, the results are summarised in Table 3. Their concerns in terms of W1 (might acquire less content) and W2 (might acquire content slower) slightly reduced, but the differences were not significant at p=0.05. Many students indicated neutrality, at the beginning and the end of the implementation (medianW1-W2=3.00). Further investigation into this trend showed that the initial median of 3.00 for W1 had a broad distribution of responses across the scale (12.4% students strongly disagreed, 21.1% students disagreed, 24.4% students were neutral, 28.0% students agreed, and 14.2% students strongly agreed). Similarly, the initial median of 3.00 for W2 was a result of 12.4% students strongly agreed, 20.4% disagreed, 23.6% students were neutral, 30.2% students agreed, and 13.5% students strongly agreed. These trends were similar for W1 and W2 from the final questionnaire where the distribution of response for W1 and W2 ranged from 11.3% to 26.5%. In summary, students’ concern was broadly represented in both the initial and final questionnaires.
Last, there were no significant differences in the total score comparing between different years of study, ages, geographical locations, and online course experiences, in both the initial and final questionnaires. However, the post-hoc test for the Kruskal Wallis test reported that students in households with a higher income (T20) had significantly higher total score than the lower-income students (B40) in both the initial (medianT20=43.0, medianB40=39.0, p=0.034) and final questionnaire (medianT20=46.0, medianB40=40.0, p=0.008). Whereas, male respondents indicated significantly more agreement in the initial questionnaire (medianmale=42.0, medianfemale=40.0, p=0.048); there was no significant difference between gender by the completion of PBL sessions.
|
Items |
Descriptive Statistics |
Wilcoxon Signed-Ranked Tests |
||||||
|
Initial Questionnaire
Median (IQR) |
Final Questionnaire
Median (IQR) |
|
N |
Mean Rank |
Sum of Ranks |
Z |
p |
|
|
L1 |
4.00(2) |
4.00(2) |
Negative Ranks |
73 |
76.10 |
5555.00 |
-1.582 |
.114 |
|
Positive Ranks |
87 |
84.20 |
7325.00 |
|||||
|
Ties |
115 |
|
|
|||||
|
L2 |
4.00(2) |
4.00(2) |
Negative Ranks |
61 |
82.25 |
5017.50 |
-2.431 |
.015 |
|
Positive Ranks |
98 |
78.60 |
7702.50 |
|||||
|
Ties |
116 |
|
|
|||||
|
L3 |
4.00(1) |
4.00(2) |
Negative Ranks |
55 |
74.89 |
4119.00 |
-3.868 |
.000 |
|
Positive Ranks |
102 |
81.22 |
8284.00 |
|||||
|
Ties |
118 |
|
|
|||||
|
L4 |
4.00(1) |
4.00(1) |
Negative Ranks |
52 |
70.04 |
3642.00 |
-2.896 |
.004 |
|
Positive Ranks |
88 |
70.77 |
6228.00 |
|||||
|
Ties |
135 |
|
|
|||||
|
L5 |
4.00(0) |
4.00(1) |
Negative Ranks |
51 |
68.38 |
3487.50 |
-3.017 |
.003 |
|
Positive Ranks |
87 |
70.16 |
6103.50 |
|||||
|
Ties |
137 |
|
|
|||||
|
L6 |
3.00(2) |
3.00(1) |
Negative Ranks |
73 |
81.04 |
5916.00 |
-2.043 |
.041 |
|
Positive Ranks |
96 |
88.01 |
8449.00 |
|||||
|
Ties |
106 |
|
|
|||||
|
C1 |
3.00(1) |
3.00(2) |
Negative Ranks |
67 |
84.04 |
5630.50 |
-3.330 |
.001 |
|
Positive Ranks |
109 |
91.24 |
9945.50 |
|||||
|
Ties |
99 |
|
|
|||||
|
C2 |
3.00(1) |
4.00(1) |
Negative Ranks |
47 |
80.29 |
3773.50 |
-4.642 |
.000 |
|
Positive Ranks |
111 |
79.17 |
8787.50 |
|||||
|
Ties |
117 |
|
|
|||||
|
C3 |
3.00(1) |
4.00(1) |
Negative Ranks |
67 |
82.83 |
5549.50 |
-1.832 |
.067 |
|
Positive Ranks |
95 |
80.56 |
7653.50 |
|||||
|
Ties |
113 |
|
|
|||||
|
C4 |
4.00(1) |
4.00(1) |
Negative Ranks |
52 |
74.81 |
3890.00 |
-3.690 |
.000 |
|
Positive Ranks |
99 |
76.63 |
7586.00 |
|||||
|
Ties |
124 |
|
|
|||||
|
W1 (Reversed) |
3.00(2) |
3.00(2) |
Negative Ranks |
86 |
94.38 |
8117.00 |
-.303 |
.762 |
|
Positive Ranks |
96 |
88.92 |
8536.00 |
|||||
|
Ties |
93 |
|
|
|||||
|
W2 (Reversed) |
3.00(2) |
3.00(2) |
Negative Ranks |
84 |
100.73 |
8461.00 |
-.579 |
.562 |
|
Positive Ranks |
104 |
89.47 |
9305.00 |
|||||
|
Ties |
87 |
|
|
|||||
Table 3. Item scores for initial and final questionnaire
IV. DISCUSSION
The rapid and widespread transmission of SARS-CoV-2 affected every nation and aspect of society, including medical education (Abbas, 2020; Rose, 2020; Sandhu & de Wolf, 2020; Wong, 2020). A universal response to reduce the spread of the virus was to implement physical distancing practices and elimination of any unnecessary interaction between contacts (Reyna, 2020). As such, competency-based medical programs, like the University of Malaya medical programme was particularly affected. The programme is designed to reflect clinical practice and to develop medical competencies, so group discussion and meeting in person is common practice (Frank et al., 2010). However, due to the closure of university campuses, medical schools were forced to respond by modifying the programme to be hosted in VLEs (Alkhowailed et al., 2020). An example of this comes from the University of Malaya who decided to transition PBL sessions to a VLE hosted by Microsoft Teams.
As with other medical schools (Coiado et al., 2020; Newman & Lattouf, 2020; Rose, 2020; Yusoff et al., 2020), the University of Malaya decided to offer the programme virtually, as the most effective means to continue programming with minimal disturbance. In this study, students’ experiences were generally improved by the end of the virtual PBL implementation. The following might be the contributing factors. First, a systematic approach using the ACTIONS framework was taken to develop an appropriate VLE. The Medical Education Unit chose Microsoft Teams and One Note as the most suitable online platform to deliver their courses and ensured that the key features of the traditional PBL sessions were translated to the VLE and virtual PBL sessions. Before implementing the virtual PBL, the faculty development team prepared guidebooks, conducted workshops, and answering questions to students and tutors. A strategy to identify and resolve problems as they arose was also implemented through tutor interviews and student evaluations.
The ability to translate students’ ability to learn in a VLE is a necessary component of virtual PBL particularly during the COVID-19 pandemic (Reyna, 2020). As such, we asked students about their opinions towards learning in the VLE. In general, students indicated a positive experience towards participating and learning from virtual PBL. Another important measure of educational success is the ability of students to translate their new knowledge into practice, applications, and assessments (Car et al., 2019; Robinson et al., 2015). Taken as a whole, students felt confident in their abilities to use the knowledge gained during the virtual PBL sessions.
Students were also asked about their concerns towards acquiring the appropriate amount of content and pacing of course material (items W1 and W2). The average response from students indicated a neutral opinion about these worries and there was no significant difference between the first and final questionnaires. Interestingly, the responses are broadly distributed across the scale for both items and in both the initial and final questionnaires. This may indicate that ‘concern’ may be interpreted differently between students as the level of tolerance to uncertainties varies among individuals (Hillen et al., 2017).
We also discovered some interesting trends between specific students in this study with their experiences conducting virtual PBL. Interestingly, students associated with the highest household income reported significantly higher scores in both the initial and final questionnaires. Higher household income may be indicative of accessibility to learning resources or increased confidence in performance (Thomson, 2018). Further investigation into this is necessary to understand whether the transition to VLE may provide inequitable education for all students. Additionally, males responded significantly higher than females in the initial questionnaire, but similarly in the final questionnaire. It would be interesting to investigate whether this trend is related to societal determinants of attitudes, which suggest that males are more technology-driven (Vázquez-Cano et al., 2017). Though interestingly, other studies suggest that there is no difference between the genders and attitudes towards e-learning (Gormley et al., 2009) or even show that males were less motivated to participate in PBL (Joseph et al., 2016). Regardless of the motivation for the responses, both genders had similar perceptions after completing the virtual PBL sessions.
In addition to the findings above, the questionnaire also provided insight into areas of improvement for the virtual PBL. Students were overwhelmingly positive towards the use of a VLE for PBL, suggesting that these sessions could remain virtual in the future. The biggest areas to improve are the confidence in passing clinical exams and the worry about content acquisition. More emphasis should be placed on the clinical applicability of the PBL sessions so that students may better see how to use the material in practice. Additionally, students must be reassured that participating in virtual PBL sessions is equivocal to in-person sessions in terms of the amount and pacing of content delivery.
A. Limitations of the Study
First, the study was conducted in a single institution, which limited the generalisability of its results. Second, a standard for expectations in conducting virtual PBL during the COVID-19 pandemic is not available (Schlenz et al., 2020). In this study, improvements in mean scores could only be considered as positive changes instead of meeting the standard of expectations, as there is no benchmark on the satisfactory mean score. Last, more investigations are needed before virtual PBL can be considered as an effective option post-pandemic. One of the future investigations would be accessibility to the internet and bandwidth in conducting virtual PBL.
V. CONCLUSION
A transition to virtual PBL was necessary during the MCO in Malaysia during the COVID-19 pandemic. In this study, the advantages of virtual PBL outweigh its disadvantages, as an acceptable alternative. Other medical schools could consider using virtual PBL to replace face-to-face PBL, and it would minimise disruption in medical training during the COVID-19 pandemic. Our experiences and lessons learnt may be helpful for medical schools moving towards digitising their PBL.
Notes on Contributors
VP, KK, and PS designed and developed the VLE. CCF, AJL, CRA designed and conceptualised this study with input from WHH, VP, and JV. CCF, AJL, and CRA worked on the acquisition and analysis of data. All the authors interpreted the data and drafted portions of the manuscript related to their roles in the Medical Education Unit. The manuscript has been read, revised, and approved for submission by all authors.
Ethical Approval
The authors had obtained ethical approval from the University of Malaya Research Ethics Committee (UM.TNC2/ UMREC-998) before the study was initiated.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to privacy and ethical concerns.
Acknowledgement
The authors would like to thank the students for participating in the study.
Funding
The authors received no financial support for this research.
Declaration of Interest
The authors declare that they have no competing interests.
References
Abbas, A. M. (2020). COVID-19 pandemic and medical education in a developing country. American Journal of Biomedical Science & Research, 9(4), 289-290. https://doi.org/10.34297/AJBSR.2020.09.001408
Abedi, M., & Abedi, D. (2020). A letter to the editor: The impact of COVID-19 on intercalating and non-clinical medical students in the UK. Medical Education Online, 25(1), 1771245.
https://doi.org/10.1080/10872981.2020.1771245
Alkhowailed, M. S., Rasheed, Z., Shariq, A., Elzainy, A., El Sadik, A., Alkhamiss, A., Alsolai, A. M., Alduraibi, S. K., Alduraibi, A., & Alamro, A. (2020). Digitalization plan in medical education during COVID-19 lockdown. Informatics in Medicine Unlocked, 20, 100432. https://doi.org/10.1016/j.imu.2020.100432
Boettcher, J., & Conrad, R.-M. (1999). Faculty guide for moving teaching and learning to the web. League for Innovation in the Community College.
Bowling, A. (2009). The psychometric properties of the older people’s quality of life questionnaire, compared with the CASP-19 and the WHOQOL-OLD. Current Gerontology and Geriatrics Research, 2009, 1-12. https://doi.org/10.1155/2009/298950
Campbell, S., Braspenning, J., Hutchinson, A., & Marshall, M. (2002). Research methods used in developing and applying quality indicators in primary care. Quality and Safety in Health Care, 11(4), 358-364. https://doi.org/10.1136/bmj.326.7393.816
Car, L. T., Kyaw, B. M., Dunleavy, G., Smart, N. A., Semwal, M., Rotgans, J. I., Low-Beer, N., & Campbell, J. (2019). Digital problem-based learning in health professions: Systematic review and meta-analysis by the digital health education collaboration. Journal of Medical Internet Research, 21(2), e12945. https://doi.org/10.2196/12945
Coiado, O. C., Yodh, J., Galvez, R., & Ahmad, K. (2020). How COVID-19 transformed problem-based learning at Carle Illinois College of Medicine. Medical Science Educator, 30(4), 1353-1354. https://doi.org/10.1007%2Fs40670-020-01063-3
Degtjarjova, I., Lapina, I., & Freidenfelds, D. (2018). Student as stakeholder: Voice of customer in higher education quality development. Marketing and Management of Innovations, 2, 388-398. https://doi.org/10.21272/mmi.2018.2-30
Ebner, M., Schön, S., Braun, C., Ebner, M., Grigoriadis, Y., Haas, M., Leitner, P., & Taraghi, B. (2020). COVID-19 epidemic as e-learning boost? Chronological development and effects at an Austrian University against the background of the concept of “e-learning readiness”. Future Internet, 12(6), 94. https://doi.org/10.3390/fi12060094
Ferrel, M. N., & Ryan, J. J. (2020). The Impact of COVID-19 on Medical Education. The Cureus Journal of Medical Science, 12(3), e7492. https://doi.org/10.7759%2Fcureus.7492
Field, A. (2009). Discovering statistics using SPSS (3rd ed.). SAGE publications.
Foong, C. C. (2020). Preliminary measures in the COVID-19 pandemic a trial for futuristic medical education. Journal of Research in Medical and Dental Science, 8(5), 77-78.
Foong, C. C., Hassan, H., Lee, S. S., & Vadivelu, J. (2015). Using students’ formative feedback to advocate reflective teaching. Medical Education, 49(5), 535. https://doi.org/10.1111/medu.12697
Frank, J. R., Snell, L. S., Cate, O. T., Holmboe, E. S., Carraccio, C., Swing, S. R., Harris, P., Glasgow, N. J., Campbell, C., & Dath, D. (2010). Competency-based medical education: Theory to practice. Medical Teacher, 32(8), 638-645. https://doi.org/10.3109/0142159x.2010.501190
Gormley, G. J., Collins, K., Boohan, M., Bickle, I. C., & Stevenson, M. (2009). Is there a place for e-learning in clinical skills? A survey of undergraduate medical students’ experiences and attitudes. Medical Teacher, 31(1), e6-e12. https://doi.org/10.1080/01421590802334317
Hair, J. F., Black, W. C., Babin, B. J., & Anderson, R. E. (2009). Multivariate data analysis (7th ed.). Pearson.
Hew, K. F., Jia, C., Gonda, D. E., & Bai, S. (2020). Transitioning to the “new normal” of learning in unpredictable times: Pedagogical practices and learning performance in fully online flipped classrooms. International Journal of Educational Technology in Higher Education, 17(1), 1-22. https://doi.org/10.1186/s41239-020-00234-x
Hillen, M. A., Gutheil, C. M., Strout, T. D., Smets, E. M., & Han, P. K. (2017). Tolerance of uncertainty: Conceptual analysis, integrative model, and implications for healthcare. Social Science & Medicine, 180, 62-75. https://doi.org/10.1016/j.socscimed.2017.03.024
Ifediora, C. O. (2019). Online medical education for doctors: Identifying potential gaps to the traditional, face-to-face modality. Journal of Medical Education and Curricular Development, 6, 2382120519827912. https://doi.org/10.1177%2F2382120519827912
Joseph, N., Rai, S., Madi, D., Bhat, K., Kotian, S. M., & Kantharaju, S. (2016). Problem-based learning as an effective learning tool in community medicine: Initiative in a private medical college of a developing country. Indian Journal of Community Medicine, 41(2), 133-140. https://doi.org/10.4103/0970-0218.177535
Khalil, R., Mansour, A. E., Fadda, W. A., Almisnid, K., Aldamegh, M., Al-Nafeesah, A., Alkhalifah, A., & Al-Wutayd, O. (2020). The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: A qualitative study exploring medical students’ perspectives. BMC Medical Education, 20, 285. https://doi.org/10.1186/s12909-020-02208-z
Laamanen, M., Ladonlahti, T., Uotinen, S., Okada, A., Bañeres, D., & Koçdar, S. (2021). Acceptability of the e-authentication in higher education studies: Views of students with special educational needs and disabilities. International Journal of Educational Technology in Higher Education, 18(1), 1-17. https://doi.org/10.1186/s41239-020-00236-9
Luciani, E., van Dun, P. L., Esteves, J. E., Lunghi, C., Petracca, M., Papa, L., Merdy, O., Jäkel, A., & Cerritelli, F. (2015). Learning environment, preparedness and satisfaction in osteopathy in Europe: The PreSS study. PloS One, 10(6), e0129904. https://doi.org/10.1371%2Fjournal.pone.0129904
Maskey, R., Fei, J., & Nguyen, H.-O. (2018). Use of exploratory factor analysis in maritime research. The Asian Journal of Shipping and Logistics, 34(2), 91-111. https://doi.org/10.1016/j.ajsl.2018.06.006
Musal, B., Keskin, O., & Tuncel, P. (2017). Application of an electronic problem-based learning system in undergraduate medical education program. Journal of Health and Medical Informatics, 8(1), 1000246. https://doi.org/10.4172/2157-7420.1000246
Newman, N. A., & Lattouf, O. M. (2020). Coalition for medical education—A call to action: A proposition to adapt clinical medical education to meet the needs of students and other healthcare learners during COVID‐19. Journal of Cardiac Surgery, 35(6), 1174-1175. https://doi.org/10.1111%2Fjocs.14590
Ngampornchai, A., & Adams, J. (2016). Students’ acceptance and readiness for e-learning in Northeastern Thailand. International Journal of Educational Technology in Higher Education, 13(1), 34. https://doi.org/10.1186/s41239-016-0034-x
Reyna, J. (2020). Twelve tips for COVID-19 friendly learning design in medical education. MedEdPublish, 9(1), 103. https://doi.org/10.15694/mep.2020.000103.1
Robinson, G. F., Moore, C. G., McTigue, K. M., Rubio, D. M., & Kapoor, W. N. (2015). Assessing competencies in a master of science in clinical research program: The comprehensive competency review. Clinical and Translational Science, 8(6), 770-775. https://doi.org/10.1111%2Fcts.12322
Roff, S. (2005). The Dundee Ready Educational Environment Measure (DREEM)—A generic instrument for measuring students’ perceptions of undergraduate health professions curricula. Medical Teacher, 27(4), 322-325. https://doi.org/10.1080/01421590500151054
Rose, S. (2020). Medical student education in the time of COVID-19. Jama Network, 323(21), 2131-2132. https://doi.org/10.1001/jama.2020.5227
Sandhu, P., & de Wolf, M. (2020). The impact of COVID-19 on the undergraduate medical curriculum. Medical Education Online, 25(1), 1764740. https://doi.org/10.1080/10872981.2020.1764740
Schlenz, M. A., Schmidt, A., Wöstmann, B., Krämer, N., & Schulz-Weidner, N. (2020). Students’ and lecturers’ perspective on the implementation of online learning in dental education due to SARS-CoV-2 (COVID-19): A cross-sectional study. BMC Medical Education, 20, 354. https://doi.org/10.1186/s12909-020-02266-3
Shah, A. U. M., Safri, S. N. A., Thevadas, R., Noordin, N. K., Abd Rahman, A., Sekawi, Z., Ideris, A., & Sultan, M. T. H. (2020). COVID-19 outbreak in Malaysia: Actions taken by the Malaysian government. International Journal of Infectious Diseases, 97, 108-116. https://doi.org/10.1016/j.ijid.2020.05.093
Tabatabai, S. (2020). Simulations and virtual learning supporting clinical education during the COVID 19 pandemic. Advances in Medical Education and Practice, 11, 513-516. https://doi.org/10.2147/AMEP.S257750
Thomson, S. (2018). Achievement at school and socioeconomic background—An educational perspective. NPJ Science of Learning, 3, 5. https://doi.org/10.1038/s41539-018-0022-0
Valaitis, R. K., Sword, W. A., Jones, B., & Hodges, A. (2005). Problem-based learning online: Perceptions of health science students. Advances in Health Sciences Education, 10(3), 231-252. https://doi.org/10.1007/s10459-005-6705-3
Vázquez-Cano, E., Meneses, E. L., & García-Garzón, E. (2017). Differences in basic digital competences between male and female university students of social sciences in Spain. International Journal of Educational Technology in Higher Education, 14, 27. https://doi.org/10.1186/s41239-017-0065-y
Verma, S. K., Vidisha, S., Bhopal, M., & Jaloree, S. (2010). Pattern mining approach to categorization of students’ performance using Apriori Algorithm. International Journal of Computer Applications, 121, 36-39. https://doi.org/10.5120/21540-4550
Wong, R. Y. (2020). Medical education during COVID-19: Lessons from a pandemic. British Columbia Medical Journal, 62(5), 170-171.
World Health Organisation. (2020) WHO/Europe | Coronavirus disease (COVID-19) outbreak – About the virus. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov
Yeo, S., & Chang, B. H. (2017). Implementation of problem-based learning in medical education in Korea. Korean Journal of Medical Education, 29(4), 271-282. https://doi.org/10.3946/kjme.2017.73
Yusoff, M. S. B., Hadie, S. N. H., Mohamad, I., Draman, N., Al-Aarifin, I. M., Rahman, W. F. W. A., Pa, M. N. M., & Yaacob, N. A. (2020). Sustainable medical teaching and learning during the COVID-19 pandemic: Surviving the new normal. The Malaysian Journal of Medical Sciences, 27(3), 137-142. https://doi.org/10.21315/mjms2020.27.3.14
*Jamuna Vadivelu
Medical Education & Research Development Unit (MERDU),
Faculty of Medicine,
University of Malaya,
Lembah Pantai,
50603 Kuala Lumpur, Malaysia.
Email: jamuna@ummc.edu.my
Submitted: 19 May 2021
Accepted: 7 October 2021
Published online: 4 January, TAPS 2022, 7(1), 21-32
https://doi.org/10.29060/TAPS.2022-7-1/RA2537
Kirsty J Freeman1, Sandra E Carr2, Brid Phillips2, Farah Noya3 & Debra Nestel4,5
1Office of Education, Duke NUS Medical School, Singapore, Singapore; 2Division of Health Professions Education, The University of Western Australia, Perth, Australia; 3Faculty of Medicine, Pattimura University, Ambon, Indonesia; 4School of Clinical Sciences, Monash University, Clayton, Australia; 5Austin Precinct, Department of Surgery, University of Melbourne, Heidelberg, Australia
Abstract
Introduction: As healthcare educators undergo a career transition from providing care to providing education, their professional identity can also transition accompanied by significant threat. Given their qualifications are usually clinical in nature, healthcare educators’ knowledge and skills in education and other relevant theories are often minimal, making them vulnerable to feeling fraudulent in the healthcare educator role. This threat and vulnerability is described as the impostor phenomenon. The aim of this study was to examine and map the concepts of professional identity and the influence of impostor phenomenon in healthcare educators.
Methods: The authors conducted a scoping review of health professions literature. Six databases were searched, identifying 121 relevant articles, eight meeting our inclusion criteria. Two researchers independently extracted data, collating and summarising the results.
Results: Clinicians who become healthcare educators experience identity ambiguity. Gaps exist in the incidence and influence of impostor phenomenon in healthcare educators. Creating communities of practice, where opportunities exist for formal and informal interactions with both peers and experts, has a positive impact on professional identity construction. Faculty development activities that incorporate the beliefs, values and attributes of the professional role of a healthcare educator can be effective in establishing a new professional identity.
Conclusion: This review describes the professional identity ambiguity experienced by clinicians as they take on the role of healthcare educator and solutions to ensure a sustainable healthcare education workforce.
Keywords: Professional Identity, Impostor Phenomenon, Healthcare Educators, Health Professions Education, Scoping Review
Practice Highlights
- Professional identity ambiguity experienced when a clinician transitions to the role of healthcare educator is understudied relative to other professions.
- Professional identity ambiguity experienced when a clinician transitions to the role of healthcare educator is understudied relative to other professions.
- Creating communities of practice, whereby healthcare educators can interact with peers and experts, in both formal and informal settings, has a positive impact on professional identity construction.
- Faculty development activities that incorporate the beliefs, values and attributes of the professional role of a healthcare educator are effective in establishing a new professional identity or aligning multiple professional identities.
I. INTRODUCTION
Educating the current and future healthcare workforce relies on clinicians sharing their knowledge, skills and experience by teaching others. Some clinicians have a passion to educate and seek out this role. For others it is often their high level of clinical expertise that results in requests to take on an education role. This may result in an expansion of their current role as a clinician, or a transition from one role to another. There are many terms used to describe those teaching in healthcare including educator, teacher, and faculty. The term healthcare educators is used throughout this paper to describe clinicians educating in any environment. Changes in work roles can pose a threat to an individual’s identity (Barbulescu & Ibarra, 2008; Becker & Carper, 1956), as this requires the individual to develop a new sense of self (Conroy & O’Leary-Kelly, 2014). With this change in role comes a transition in professional identity.
Professional identity is defined as “the relatively stable and enduring constellation of attributes, beliefs, values, motives, and experiences in terms of which people define themselves in a professional role” (Ibarra, 1999, pp. 764). The formation of professional identity is centred on how an individual perceives themselves as a professional, their relationship with the profession, and how their knowledge, skills and attitudes align with the norms and culture of that profession (Sethi et al., 2018). Within healthcare there has been a call for professional identity formation to be explicitly addressed in the curriculum of future healthcare professionals, addressing both what it is to think, act and feel like a healthcare professional, and the processes by which that identity is formed (Cruess et al., 2019).
Individuals manage numerous identities during their lifespan, across personal, vocational, social and professional spheres. Van Gennep’s theory of rites of passage, where-by an individual transitions through three phases 1) ‘separation’ – letting go of the old self, 2) ‘liminality’ – middle phase, and 3) ‘aggregation’ – establishing a new identity, has been cited in the literature to describe career transition and formation of a new identity (Kulkarni, 2019; Mayrhofer & Iellatchitch, 2005; Petersen, 2017). It is in this middle phase of liminality where a clinician taking on the role of a healthcare educator may experience identity ambiguity. Given that literature from other industries show that professional identity can influence job satisfaction, feelings of accomplishment, and employment retention (Canrinus et al., 2012; Hutchins et al., 2018), it is essential that the formation of professional identity and potential identity ambiguity in healthcare educators is examined.
The term impostor phenomenon, also known as impostor syndrome, is used to describe negative feelings an individual experiences, despite achieving a level of competence, and the fear of being ‘found out’ by those around them (Clark et al., 2014). The concept of being exposed as a ‘fraud’ was coined impostor phenomenon by clinical psychologists Clance and Imes (1978). Literature suggests that despite external evidence of their competence, those exhibiting the phenomenon remain convinced that they are frauds and do not deserve the success they have achieved (Leonhardt et al., 2017; Neureiter & Traut-Mattausch, 2016; Vergauwe et al., 2015).
In their seminal work from the late 1970’s, Clance and Imes (1978) reported that impostor phenomenon is more prevalent in specific female populations. Recent studies however have shown that impostor phenomenon impacts individual regardless of gender, and occurs in a variety of contexts (Bernard et al., 2018; Chae et al., 1995). Prominent among high performing individuals, impostor phenomenon is experienced on a continuum from the occasional concern that the individual is not up to the task, to an extreme fear of being ‘found out’ as a fraud (Hibberd, 2019). Studies suggest that impostor phenomenon can have significant negative effects including an increase in work-family conflict (Crawford et al., 2016), and decreased job satisfaction (Cowman & Ferrari, 2002), with studies also reporting a link between impostor phenomenon and burnout (Villwock et al., 2016).
With impostor phenomenon well described in professions outside of healthcare, most literature published on impostor phenomenon within the healthcare professions has focused on students transitioning from study to the workplace (Aubeeluck et al., 2016; Dudău, 2014; Robinson-Walker, 2011), with very few studies examining current working professionals (Gottlieb et al., 2019; Hutchins et al., 2018). The aim of this study was to examine and map the concepts of professional identity and implications of impostor phenomenon in healthcare educators. By furthering our understanding of impostor phenomenon in healthcare educators and how it impacts professional identity, both individuals and organisations will be able to implement strategies that will assist in the development of a sustainable healthcare education workforce, addressing workforce capability, capacity, resilience and culture.
II. METHODS
The aim of a scoping review is to examine evidence, identify gaps in the literature, and clarify key concepts (The Joanna Briggs Institute, 2017). The objective of this scoping review is to examine and map the concepts of professional identity and impostor phenomenon in healthcare educators.
A. Review Questions
The primary review question was ‘how is professional identity and impostor phenomenon described in the literature about healthcare educators?’, with the secondary review question being ‘how is professional identity of healthcare educators influenced by imposter phenomenon?’. Tricco et al. (2016) identified 25 knowledge synthesis methods used across the health fields. We selected a scoping review methodology as it is the most appropriate to address our aim to map and summarise the literature, clarify working definitions and identify gaps. The framework that will guide the process is the five-step approach proposed by Arksey and O’Malley (2005). The steps are 1) identify the research question; 2) identify the relevant articles; 3) select the articles; 4) chart the data; and 5) collate and summarise the results.
B. Identifying Relevant Articles
Adopting the population, concept, and context (PCC) framework (Peters et al., 2020) informed the development of the search strategy as demonstrated in Table 1.
|
|
Main concepts |
|
|
|
|||
|
|
Population |
Concept 1 |
Concept 2 |
Context |
|||
|
|
Healthcare educators |
Professional identity |
Impostor phenomenon |
Healthcare education |
|||
|
Search Terms |
“healthcare educator.ti,ab,kw.” “nursing educator.ti,ab,kw.” “medical educator.ti,ab,kw.” “allied health educator.ti,ab,kw” “faculty.ti,ab,kw.” “facilitator.ti,ab,kw.” “educator.ti,ab,kw.” “*faculty, medical/ or *faculty, nursing/ or *health educators/” “clinical educator.ti,ab,kw.” “clinical teacher.ti,ab,kw.” |
“Professional identity.ti,ab,kw.” “Professional role*.ti,ab,kw.” “Professional competence.ti,ab,kw.” “Professional sociali*ation.ti,ab,kw.” “Professional identity formation.ti,ab,kw.” “*Professional Competence/” “*Professional Role/” “*Professionalism/” |
“impostor.ti,ab,kw.” “imposter.ti,ab,kw.” “fraud.ti,ab,kw.” “fake.ti,ab,kw.” “impost*rism.ti,ab,kw.” “intellectual fraud*.ti,ab,kw.” “(impost*r adj3 syndrome).ti,ab,kw.” “(impost*r adj3 phenomenon).ti,ab,kw.” “*Adaptation, Psychological/” “*Self Concept/” “*social identification/” “Self concept.ti,ab,kw.” |
“education, medical/ or *education, medical, continuing/ or *education, medical, graduate/ or *education, medical, undergraduate/” “*Education, Nursing/” “*Education, Allied Health/” “*Education, Clinical/” “education, medical/ or education, nursing/ or education, pharmacy/ or education, public health professional/” |
|||
Table 1: Key search terms
Note: ti = title; ab = abstract; kw = keyword
To identify potentially relevant articles, a literature search of six online databases was conducted on the November 6, 2020. These included MEDLINE, EMBASE, Joanna Briggs Institute EBP Database, CINAHL, PsycINFO, and ERIC. The search strategies were drafted in collaboration with an experienced librarian and further refined by the researchers. The search strategy conducted in MEDLINE is detailed in Table 2. The final search results were exported into Covidence systematic review software, a screening and data extraction tool (Covidence Systematic Review Software, 2019).
|
# |
Searches |
Results |
|
1 |
healthcare educator.ti,ab,kw. |
5 |
|
2 |
nursing educator.ti,ab,kw. |
51 |
|
3 |
medical educator.ti,ab,kw. |
164 |
|
4 |
allied health educator.ti,ab,kw. |
7 |
|
5 |
faculty.ti,ab,kw. |
46912 |
|
6 |
facilitator.ti,ab,kw. |
6518 |
|
7 |
educator.ti,ab,kw. |
5586 |
|
8 |
*faculty, medical/ or *faculty, nursing/ or *health educators/ |
14624 |
|
9 |
clinical educator.ti,ab,kw. |
119 |
|
10 |
clinical teacher.ti,ab,kw. |
279 |
|
11 |
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 |
66130 |
|
12 |
Professional identity.ti,ab,kw. |
1917 |
|
13 |
Professional role*.ti,ab,kw. |
2643 |
|
14 |
Professional competence.ti,ab,kw. |
1267 |
|
15 |
Professional sociali*ation.ti,ab,kw. |
376 |
|
16 |
Professional identity formation.ti,ab,kw. |
241 |
|
17 |
*Professional Competence/ |
11751 |
|
18 |
*Professional Role/ |
6495 |
|
19 |
*Professionalism/ |
836 |
|
20 |
12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 |
24196 |
|
21 |
impostor.ti,ab,kw. |
169 |
|
22 |
imposter.ti,ab,kw. |
148 |
|
23 |
fraud.ti,ab,kw. |
4102 |
|
24 |
fake.ti,ab,kw. |
1772 |
|
25 |
impost*rism.ti,ab,kw. |
16 |
|
26 |
intellectual fraud*.ti,ab,kw. |
7 |
|
27 |
(impost*r adj3 syndrome).ti,ab,kw. |
57 |
|
28 |
(impost*r adj3 phenomenon).ti,ab,kw. |
63 |
|
29 |
*Adaptation, Psychological/ |
43405 |
|
30 |
*Self Concept/ |
25641 |
|
31 |
*social identification/ |
5255 |
|
32 |
Self concept.ti,ab,kw. |
5240 |
|
33 |
21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 |
80945 |
|
34 |
20 and 33 |
597 |
|
35 |
education, medical/ or *education, medical, continuing/ or *education, medical, graduate/ or *education, medical, undergraduate/ |
108815 |
|
36 |
*Education, Nursing/ |
24454 |
|
37 |
*Education, Allied Health/ |
0 |
|
38 |
*Education, Clinical/ |
0 |
|
39 |
education, medical/ or education, nursing/ or education, pharmacy/ or education, public health professional/ |
96076 |
|
40 |
35 or 36 or 37 or 38 or 39 |
147396 |
|
41 |
11 and 34 and 40 |
17 |
Table 2: Search strategy conducted in Ovid MEDLINE on November 6, 2020
C. Eligibility Criteria
To be eligible for inclusion in the study, articles were required to satisfy the following criteria:
1. Population: This scoping review will consider literature that included educators within the healthcare context. Educators can include those of any age, gender, culture or geography.
2. Concept: There are two concepts that will be examined in this review, transition in professional identity and impostor phenomenon. This review will include the definition of the concepts, the theoretical, conceptual and the measurement of both concepts.
3. Context: This review will consider literature written in English, from any healthcare context with no restrictions on geographical location, or cultural factors.
D. Selection of Articles
One hundred and twenty-one articles were collated and citations, title and abstract were retrieved. An initial check identified one duplicate, which was removed. Titles and abstracts of the 120 articles were screened by three independent reviewers (KF, FN, BP) for assessment against the inclusion criteria for the review. Thirty-three articles were found to meet the inclusion criteria and progressed to full text review. Two researchers (KF, BP) conducted a full text review, recording reasons for exclusion. Disagreements were resolved through discussion, and consensus. Based on the Joanna Briggs Institute recommendations on scoping review methods, no critical appraisal of methodological quality was undertaken (The Joanna Briggs Institute, 2017).
E. Charting the Data
A data-charting form to determine which data to extract was jointly developed by two researchers (KF, SC). Two researchers (KF, BP) independently charted the data, then discussed the results and edited the data-charting form as required. A third researcher (FN) verified the data.
F. Collating, Summarising and Reporting the Data
Data was abstracted on article characteristics including country of publication, population of interest, study aim, sample size, study design, data collection methods, and findings related to the concepts of professional identity and impostor phenomenon.
III. RESULTS
One hundred and twenty-one abstracts were identified from six databases, 33 full text articles were reviewed, and 8 full text articles were analysed (See Figure 1). Of the included articles five were conducted in the USA (Cranmer et al., 2018; Heinrich, 1997; O’Sullivan & Irby, 2014; Stone et al., 2002; Talisman et al., 2015), and one in each of Australia (Higgs & McAllister, 2007), Canada (Lieff et al., 2012), and the United Kingdom (Andrew et al., 2009) (Table 3). In relation to the population of healthcare educators, four articles involved those working in medicine (Cranmer et al., 2018; O’Sullivan & Irby, 2014; Stone et al., 2002; Talisman et al., 2015), two in nursing (Andrew et al., 2009; Heinrich, 1997), one in speech pathology (Higgs & McAllister, 2007), and one involving healthcare educators from multiple professions (Lieff et al., 2012). Five studies adopted a qualitative approach, such as interviews or narrative responses, (Andrew et al., 2009; Higgs & McAllister, 2007; Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002), one employing a quantitative approach (Cranmer et al., 2018), one mixed methods (Talisman et al., 2015), and one article was a program description (Heinrich, 1997).

Figure 1: PRISMA flow diagram
|
Article |
Country |
Population |
Study aim |
Sample size (n) |
Study design |
Data collection method |
Findings |
|
Andrew et al. (2009) |
UK |
Nursing |
To explore online communities for novice educators to develop professional identity |
14 |
Qualitative content analysis |
Web blog |
Communities of practice can help in the development of professional identity |
|
Talisman et al. (2015) |
USA |
Medicine |
To explore the impact of teaching the mind-body medicine course on course facilitator’s professional identity |
50 |
Mixed Methods cross sectional design |
Survey including the FMI & PSS tools, & open-ended questions |
Participation as a facilitator in a mind-body medicine program has tangible positive outcomes for the professional identity of facilitators through improved communication, connection, empathy, and self-confidence. |
|
Stone et al. (2002) |
USA |
Medicine |
To examine factors that preceptors perceive as important to their identity as teachers |
10 |
Qualitative |
Semi-structured interviews |
Preceptors associate strong feelings with their identity as teacher. Four aspects of teacher identity are as follows: humanitarianism; adult learning principles; benefits and drawbacks, and image of self as teacher. Teacher identity was not associated with student learning. Faculty development can foster preceptor identity as teacher. |
|
O’Sullivan and Irby (2014) |
USA |
Medicine |
To examine identity formation of part time faculty developers |
29 |
Qualitative |
Semi-structured interviews |
Professional identity is fluid, and evolves over time. Faculty development, particularly developing others has a direct impact on this. |
|
Lieff et al. (2012) |
Canada |
Multiple professions |
To understand the factors that relate to the formation and growth of academic identity |
43 |
Qualitative case study approach |
Reflective paper and focus groups |
Academic identity formation is influenced by personal, relational and contextual factors, and that this identity the motivation, satisfaction, and productivity of health professional educators. |
|
Higgs and McAllister (2007) |
Australia |
Speech Pathology |
To examine the preparation and professional development of clinical educators based on research into the experiences of being a clinical educator |
5 |
Qualitative approach using hermeneutic phenomenology and narrative inquiry |
Interviews |
The model of The Experience of Being a Clinical Educator, emphasising six dimensions: a sense of self, of self-identity; a sense of relationship with others; a sense of being a clinical educator; a sense of agency or purposeful action; dynamic self-congruence; and the experience of growth and change, can be used as the basis for helping clinical educators to reflect on what it means to be a clinical educator Faculty development activities that include reflective strategies can assist the educator transition from novice to expert. |
|
Heinrich (1997) |
USA |
Nursing |
To describe an educational interventional designed to assist nurses who experience impostor phenomenon as they negotiate professional transitions |
Not stated |
Program description |
Faculty/author observation |
Impostor phenomenon is prevalent among nurses as they negotiate professional identity transformation, and that the use of metaphors in faculty development programs can be effective in aiding this transition. |
|
Cranmer et al. (2018) |
USA |
Medicine |
To describe the impact of a faculty mentoring program on the retention, promotion and professional fulfilment of junior faculty members |
23 |
Quantitative |
Survey |
Participation in a mentoring program has a positive effect on confidence, self-efficacy and skills, and that participation can assist new academic s develop their academic role and achieve professional fulfilment by fostering strong collegial and social relationships, ultimately leading to career satisfaction. |
Table 3. Summary of extracted data from the included articles
Articles identified several key influences when describing the professional identity of healthcare educators (Figure 2). Seven articles describe the healthcare educator’s interaction with others as having a positive influence on professional identity (Andrew et al., 2009; Heinrich, 1997; Higgs & McAllister, 2007; Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002; Talisman et al., 2015). Interactions with peers was identified as being key to clinicians successfully adopting an educator professional identity. One study found that by providing opportunities for informal discussions and social interactions amongst peers, healthcare educators reported a sense of belonging which was found to be essential in identity formation (Lieff et al., 2012). These findings were supported by Andrew et al. (2009) who found that online communities of practice were effective in supporting new educators in developing their professional identity.
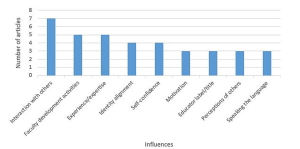
Figure 2. Key influences of professional identity
Interactions between the novice and expert educators were reported to have both a positive and negative influence on healthcare educators as they construct their educator identity. Two studies described the positive impact of formal mentoring programs, one as a means of maintaining a link to their clinical identity (Andrew et al., 2009), and the other as a tool to successfully negotiate the role transition (Cranmer et al., 2018). Lieff et al. (2012) reported that whilst certain individuals are motivated by experts, seeing them as role models, others were intimidated, discouraged, and overwhelmed by the interaction with the expert. Comparing oneself to others has the potential to reinforce or inhibit the development of the healthcare educator identity (Lieff et al., 2012).
The role of faculty development activities on educator professional identity was reported by five studies (Cranmer et al., 2018; Heinrich, 1997; Higgs & McAllister, 2007; Lieff et al., 2012; Stone et al., 2002). Three studies recommended that faculty development programs include content on fostering the development of identity as a healthcare educator (Higgs & McAllister, 2007; O’Sullivan & Irby, 2014; Stone et al., 2002). One study recommended using faculty development activities to remind clinicians of their existing role as educators to patients as a means of increasing their confidence and enhance educator identity (Stone et al., 2002). Another study identified the importance of faculty development programs in facilitating interactions with other healthcare educators with varying levels of expertise, that foster a sense of belonging (Lieff et al., 2012).
The perceptions of others was found to have an influence on professional identity (Andrew et al., 2009; Lieff et al., 2012; O’Sullivan & Irby, 2014). One study reported that an evolving identity can be strengthened when the educator was seen by others as an educator, validating the new identity. The opposite was also found to be true where the perceptions of others that one is an educator could place a high level of anxiety on the emerging identity not yet fully embraced (Lieff et al., 2012). The influence which holding the title of healthcare educator had on an emerging identity is also linked to the perceptions of others. When labelled and referred to by others as an educator two studies found that professional identity as an educator was reinforced (Lieff et al., 2012; Stone et al., 2002).
Three studies found that the ability to learn and speak the language of the healthcare educator influenced how individuals developed their professional identity (Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002). O’Sullivan and Irby (2014) found that sharing a common healthcare educator language increased deeper relationship between educators, with Lieff et al. (2012) reporting that acquiring the right language provided credibility and legitimacy. A strong sense of professional identity was linked to motivation to educate, with one study suggesting that a desire to teach correlated with satisfaction in the role (Stone et al., 2002).
Aspects of identity alignment was found to be key in a healthcare educator’s professional identity formation (Andrew et al., 2009; Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002). One study of novice nurse educators described the tension experienced when managing the dual identities of clinician and educator, and the stress that maintaining dual roles places on these nurses (Andrew et al., 2009). Another study looking at multiple healthcare professions highlighted this struggle, with participants facing the dilemma of how they can excel in both identities simultaneously (Lieff et al., 2012). Exploring physician educators, the study by Stone et al. (2002) found that the identities of clinician and educator were interwoven.
Four studies reported that as self-confidence developed so too did professional identity (Cranmer et al., 2018; Heinrich, 1997; Lieff et al., 2012; Talisman et al., 2015). Data from the study by Lieff et al. (2012) revealed that just as self-confidence ebbed and flowed during a healthcare educator’s role transition, so too did their identity, resulting in feeling like an impostor. Talisman et al. (2015) found that as self-confidence grew fear of rejection by colleagues became less, and that self-confidence in ones’ professional identity opened up opportunities to develop as a healthcare educator.
Only one study (Heinrich, 1997) made specific reference to the concept of impostor phenomenon, describing an educational program using metaphors as a corrective tool for those who experience feeling like a fraud. The authors do not provide any data on the prevalence of impostor phenomenon in the population of healthcare educators, nor do they provide any results on the impact of the educational program described.
IV. DISCUSSION
Healthcare educators manage multiple identities, from social and cultural, to gender and religious, however professional identity tends to contribute a large part of an individual’s overall identity. A change in professional identity brings with it inconsistencies between the old and the new, producing anxiety and discomfort, as the individual navigates this transition phase through which identity is reconstructed (Beech, 2010). In answering the review question, ‘How is professional identity and impostor phenomenon described in the literature about healthcare educators?’ the findings indicate that in relation to professional identity, clinicians who become educators experience identity ambiguity, in line with the theory of rites of passage described by Van Gennep (Kulkarni, 2019; Petersen, 2017). Characteristics of impostor phenomenon include anxiety, lack of self-confidence, depression, and frustration (Heinrich, 1997; Hibberd, 2019). While the literature describes the experiences of healthcare educators as they strive to solidify their professional identities, this review suggests that despite impostor phenomenon being described since the 1970’s, the reporting of the phenomenon in the healthcare literature has only occurred in recent years, impostor phenomenon is not being measured amongst healthcare educators.
For the secondary question in this review ‘How is professional identity of healthcare educators influenced by imposter phenomenon?’ we found that there are key influences (Figure 2) that can be harnessed, through faculty development activities, to assist individual’s transition to Van Gennep’s third phase, aggregation, which is the final step in transitioning to a new career and establishing a new professional identity.
Creating opportunities for interactions with others, both peers and experts, through formal and informal interactions, has a positive impact on professional identity construction (Lieff et al., 2012; O’Sullivan & Irby, 2014; Stone et al., 2002). A community of practice has been described as a collection of individuals who have a shared interest and who wish to deepen their knowledge, where participation provides members an opportunity to learn from one another (Wenger, 2010). The opportunity to engage in a community of practice enables the novice healthcare educator to construct their identity by comparing themselves with others, “boosting their confidence and solidifying their identities as educators” (Lieff et al., 2012; Wenger, 2010).
Communities of practice have been used in the healthcare sector in a variety of forms and with varying purposes (Dickinson et al., 2020; Ranmuthugala et al., 2011). Elements of social cognitive theory (Bandura, 1986) and social comparison theory (Bonifield & Cole, 2008) underpin the outcomes that result from participating in a community of practice, whereby members learn through observing the behaviour of others. If the purpose of a community of practice is to assist in professional identity formation, membership needs to be carefully cultivated as the findings of this study acknowledge the potential negative influence ‘experts’ can have, as other members compare themselves, possibly viewing themselves as inadequate (Lieff et al., 2012).
The formation of single-disciplinary communities of practice should be considered given that this study has revealed healthcare educators from nursing and medicine experience their identity alignment differently. Nurses were reported as struggling with managing the dual identities of clinician and educator (Andrew et al., 2009), whereas the physicians viewed them as interwoven (Stone et al., 2002).
Faculty development activities traditionally focus on providing healthcare educators with the knowledge and skill required to perform a new role. Adopting a new professional identity as a healthcare educator involves more than acquiring new skills, but also new behaviours and attitudes (Ibarra, 1999). The findings of this review support the addition of a specific focus on fostering professional identity as part of any faculty development program for new healthcare educators (O’Sullivan et al., 2021). Such inclusions to faculty development activities could be used to emphasize the skills that clinicians have as educators, skills that are transferable to their role in teaching emerging or current clinicians (Stone et al., 2002).
This review has revealed the tension that healthcare educators may experience as they transition from one professional identity to another, as well as the struggles in balancing dual identities. The impact of this identity misalignment on the individual could result in levels of stress that see the individual reverting to their clinical professional identity and withdrawing from the healthcare educator workforce. Healthcare training organisations need to ensure that strategies such as developing communities of practice and faculty development activities are engaged to support healthcare educators on their rite of passage to developing their healthcare educator identity.
Whilst several tools to measure impostor phenomenon exist, including the Clance Impostor Phenomenon Scale (CIPS), Harvey Impostor Scale, Perceived Fraudulence Scale and Leary Impostor Scale, Mak et al. (2019) report that no scales have been validated for use with healthcare educators, a finding supported by this review.
Our findings indicate a paucity of articles on the influence of impostor phenomenon on healthcare educators as they align their clinical and educator identities. This review has described the influences on professional identity that can be harnessed to address identity ambiguity, resulting in improved job satisfaction, employment retention, ensuring a sustainable healthcare education workforce.
A. Limitations of the Review
Six databases across health and education were included; it is possible that additional articles may have been identified if different databases were searched. We did not comprehensively search the gray literature beyond conference abstracts, protocols, and dissertations. By limiting our coverage of articles only published in English we may have missed important studies published in other languages, potentially resulting in a regional bias. As no critical appraisal of methodological quality was undertaken the reliability of some findings may be limited. With the ever-changing use of language the search terms selected related to the concepts of professional identity and impostor phenomenon may not be exhaustive.
V. CONCLUSION
The influence of impostor phenomenon on the professional identity alignment in healthcare educators has the potential to negatively impact the education of the current and future healthcare workforce. This review is a starting point for individuals and organisations involved in health professions education, and faculty development. It offers insight to the under examined understudied but potentially important prevalence and impact of impostor phenomenon in healthcare educators and the professional identity ambiguity experienced by clinicians as they take on the role of healthcare educator. This review highlights the need for further research into the prevalence of impostor phenomenon in healthcare educators across different settings, as well as exploring the experience and influence of impostor phenomenon on professional identity.
Notes on Contributors
KF led the design and conceptualisation of this work, drafted the protocol, developed the search strategy, and conducted the search, data extraction, analysis, discussion and conclusion. SC and DN were involved in the conceptualisation of the review design, specifically in establishing the review question as well as the inclusion and exclusion criteria, provided feedback on the manuscript. BP, FN and SC guided the conceptualisation and design of the study and participated in data analyses and have revised all drafts of the manuscript. All authors approve the publishing of this manuscript.
Ethical Approval
Ethics approval was granted by The University of Western Australia Human Research Ethics Committee: RA/4/20/5061.
Data Availability
All relevant quantitative data are within the manuscript.
Acknowledgement
The authors would like to acknowledge Terena Solomons, Faculty Librarian, for her support and guidance in the development of the search strategy.
Funding
This work has not received any external funding.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Andrew, N., Ferguson, D., Wilkie, G., Corcoran, T., & Simpson, L. (2009). Developing professional identity in nursing academics: The role of communities of practice. Nurse Education Today, 29(6), 607-611. https://doi.org/https://dx.doi.org/10.1016/j.nedt.2009.01.012
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methods, 8, 19-32. https://doi.org/10.1080/136455703200011961
Aubeeluck, A., Stacey, G., & Stupple, E. J. N. (2016). Do graduate entry nursing student’s experience ‘Imposter Phenomenon’?: An issue for debate. Nurse Education in Practice, 19, 104-106. https://doi.org/https://doi.org/10.1016/j.nepr.2016.06.003
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Prentice-Hall.
Barbulescu, R., & Ibarra, H. (2008). Identity as narrative: Overcoming identity gaps during work role transitions. INSEAD Working Papers Collection, 27, 1-39.
Becker, H. S., & Carper, J. W. (1956). The development of identification with an occupation. The American Journal of Sociology, 61(4), 289-298. https://doi.org/10.1086/221759
Beech, N. (2010). Liminality and the practices of identity reconstruction. Human relations (New York), 64(2), 285-302. https://doi.org/10.1177/0018726710371235
Bernard, D. L., Hoggard, L. S., & Neblett, E. W. (2018). Racial discrimination, racial identity, and impostor phenomenon: A profile approach. Cultural Diversity and Ethnic Minority Psychology, 24(1), 51-61. https://doi.org/10.1037/cdp0000161
Bonifield, C., & Cole, C. A. (2008). Better him than me: Social comparison theory and service recovery. Journal of The Academy of Marketing Science, 36(4), 565-577. https://doi.org/10.1007/s11747-008-0109-x
Canrinus, E. T., Helms-Lorenz, M., Beijaard, D., Buitink, J., & Hofman, A. (2012). Self-efficacy, job satisfaction, motivation and commitment: Exploring the relationships between indicators of teachers’ professional identity. European Journal of Psychology of Education, 27(1), 115-132. https://doi.org/10.1007/s10212-011-0069-2
Chae, J. H., Piedmont, R. L., Estadt, B. K., & Wicks, R. J. (1995). Personological evaluation of Clance’s imposter phenomenon scale in a Korean sample. Journal of personality assessment, 65(3), 468-485. https://doi.org/10.1207/s15327752jpa6503_
Clance, P. R., & Imes, S. A. (1978). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention. Psychotherapy, 15(3), 241-247. https://doi.org/10.1037/h0086006
Clark, M., Vardeman, K., & Barba, S. (2014). Perceived inadequacy: A study of impostor phenomenon among college and research librarians. College & Research Libraries, 75(3), 255-271. https://doi.org/10.5860/crl12-423
Conroy, S. A., & O’Leary-Kelly, A. M. (2014). Letting go and moving on: Work-related identity loss and recovery. The Academy of Management review, 39(1), 67-87. https://doi.org/10.5465/amr.2011.0396
Covidence Systematic Review Software. (2019). Veritas Health Innovation. https://covidence.org
Cowman, S. E., & Ferrari, J. R. (2002). “Am I for real?” Predicting impostor tendencies from self-handicapping and affective components. Social Behavior and Personality, 30(2), 119-125. https://doi.org/10.2224/sbp.2002.30.2.119
Cranmer, J. M., Scurlock, A. M., Hale, R. B., Ward, W. L., Prodhan, P., Weber, J. L., Casey, P. H., & Jacobs, R. F. (2018). An adaptable pediatrics faculty mentoring model. Pediatrics, 141(5), Article e20173202. https://doi.org/10.1542/peds.2017-3202
Crawford, W. S., Shanine, K. K., Whitman, M. V., & Kacmar, K. M. (2016). Examining the impostor phenomenon and work–family conflict. Journal of Managerial Psychology, 31(2), 375-390. https://doi.org/10.1108/JMP-12-2013-0409
Cruess, S. R., Cruess, R. L., & Steinert, Y. (2019). Supporting the development of a professional identity: General principles. Medical Teacher, 41(6), 641-649. https://doi.org/10.1080/0142159X.2018.153626
Dickinson, B., Chen, Z. X., & Haramati, A. (2020). Supporting medical science educators: A matter of self-esteem, identity, and promotion opportunities. The Asia Pacific Scholar, 5(3), 1-4. https://doi.org/10.29060/TAPS.2020-5-3/PV2164
Dudău, D. P. (2014). The relation between perfectionism and impostor phenomenon. Procedia – Social and Behavioral Sciences, 127, 129-133. https://doi.org/10.1016/j.sbspro.2014.03.226
Gottlieb, M., Chung, A., Battaglioli, N., Sebok‐Syer, S. S., & Kalantari, A. (2019). Impostor syndrome among physicians and physicians in training: A scoping review. Medical Education, 54(2), 116-124. https://doi.org/10.1111/medu.13956
Heinrich, K. T. (1997). Transforming impostors into heroes. Metaphors for innovative nursing education. Nurse educator, 22(3), 45-50. https://doi.org/10.1097/00006223-199705000-00018
Hibberd, J. (2019). The Imposter Cure: How to stop feeling like a fraud and escape the mind-trap of imposter syndrome. Aster.
Higgs, J., & McAllister, L. (2007). Educating clinical educators: Using a model of the experience of being a clinical educator. Medical Teacher, 29(2-3), e51-e57. https://doi.org/10.1080/01421590601046088
Hutchins, H. M., Penney, L. M., & Sublett, L. W. (2018). What imposters risk at work: Exploring imposter phenomenon, stress coping, and job outcomes. Human Resource Development Quarterly, 29(1), 31-48. https://doi.org/10.1002/hrdq.21304
Ibarra, H. (1999). Provisional selves: Experimenting with image and identity in professional adaptation. Administrative Science Quarterly, 44(4), 764-791. https://doi.org/10.2307/2667055
Kulkarni, M. (2019). Holding on to let go: Identity work in discontinuous and involuntary career transitions. Human Relations, 73(10), 1415-1438. https://doi.org/10.1177/0018726719871087
Leonhardt, M., Bechtoldt, M. N., & Rohrmann, S. (2017). All impostors aren’t alike – Differentiating the impostor phenomenon. Frontiers in Psychology, 8, 1505. https://doi.org/10.3389/fpsyg.2017.01505
Lieff, S., Baker, L., Mori, B., Egan-Lee, E., Chin, K., & Reeves, S. (2012). Who am I? Key influences on the formation of academic identity within a faculty development program. Medical Teacher, 34(3), e208-215. https://doi.org/10.3109/0142159x.2012.642827
Mak, K. K. L., Kleitman, S., & Abbott, M. J. (2019). Impostor phenomenon measurement scales: A systematic review. Frontiers in Psychology, 10, 671. https://doi.org/10.3389/fpsyg.2019.00671
Mayrhofer, W., & Iellatchitch, A. (2005). Rites, right? The value of rites de passage for dealing with today’s career transitions. Career Development International, 10(1), 52-66. https://doi.org/10.1108/13620430510577628
Neureiter, M., & Traut-Mattausch, E. (2016). Inspecting the dangers of feeling like a fake: An empirical investigation of the impostor phenomenon in the world of work. Frontiers in Psychology, 7, 1445. https://doi.org/10.3389/fpsyg.2016.01445
O’Sullivan, P. S., & Irby, D. M. (2014). Identity formation of occasional faculty developers in medical education: A qualitative study. Academic Medicine, 89(11), 1467-1473. https://doi.org/10.1097/ACM.0000000000000374
O’Sullivan, P. S., Steinert, Y., & Irby, D. M. (2021). A faculty development workshop to support educator identity formation. Medical Teacher, 43(8), 916-917. https://doi.org/10.1080/0142159X.2021.1921135
Peters, M. D. J., Godfrey, C., McInerney, P., Munn, Z., Tricco, A. C., & Khalil, H. (2020). Scoping Reviews. In E. Aromataris., & Z. Munn (Eds.), JBI Manual for Evidence Synthesis, JBI. https://doi.org/10.46658/JBIMES-20-12
Petersen, N. (2017). The liminality of new foundation phase teachers: Transitioning from university into the teaching profession. South African Journal of Education, 37(2), 1-9. https://doi.org/10.15700/saje.v37n2a1361
Ranmuthugala, G., Plumb, J. J., Cunningham, F. C., Georgiou, A., Westbrook, J. I., & Braithwaite, J. (2011). How and why are communities of practice established in the healthcare sector? A systematic review of the literature. BMC Health Services Research, 11, 273. https://doi.org/10.1186/1472-6963-11-273
Robinson-Walker, C. (2011). The imposter syndrome. Nurse Leader, 9(4), 12-13. https://doi.org/https://doi.org/10.1016/j.mnl.2011.05.003
Sethi, A., Schofield, S., McAleer, S., & Ajjawi, R. (2018). The influence of postgraduate qualifications on educational identity formation of healthcare professionals. Advances in Health Sciences Education, 23(3), 567-585. https://doi.org/10.1007/s10459-018-9814-5
Stone, S., Ellers, B., Holmes, D., Orgren, R., Qualters, D., & Thompson, J. (2002). Identifying oneself as a teacher: The perceptions of preceptors. Medical Education, 36(2), 180-185. https://doi.org/10.1046/j.1365-2923.2002.01064.x
Talisman, N., Harazduk, N., Rush, C., Graves, K., & Haramati, A. (2015). The impact of mind-body medicine facilitation on affirming and enhancing professional identity in health care professions faculty. Academic Medicine, 90(6), 780-784. https://doi.org/10.1097/acm.0000000000000720
The Joanna Briggs Institute (Ed.). (2017). Joanna Briggs Institute Reviewer’s Manual. https://reviewersmanual.joannabriggs.org/
Tricco, A. C., Soobiah, C., Antony, J., Cogo, E., MacDonald, H., Lillie, E., Tran, J., D’Souza, J., Hui, W., Perrier, L., Welch, V., Horsley, T., Straus, S. E., & Kastner, M. (2016). A scoping review identifies multiple emerging knowledge synthesis methods, but few studies operationalize the method. Journal of Clinical Epidemiology, 73, 19–28. https://doi.org/10.1016/j.jclinepi.2015.08.030
Vergauwe, J., Wille, B., Feys, M., De Fruyt, F., & Anseel, F. (2015). Fear of being exposed: The trait-relatedness of the impostor phenomenon and its relevance in the work context. Journal of Business and Psychology, 30(3), 565-581. https://doi.org/10.1007/s10869-014-9382-5
Villwock, J. A., Sobin, L. B., Koester, L. A., & Harris, T. M. (2016). Impostor syndrome and burnout among American medical students: A pilot study. International Journal of Medical Education, 7, 364-369. https://dx.doi.org/10.5116%2Fijme.5801.eac4
Wenger, E. (2010). Communities of practice and Social Learning Systems: The career of a concept. In C. Blackmore (Ed.), Social Learning Systems and Communities of Practice (pp. 179-198). Springer. https://doi.org/10.1007/978-1-84996-133-2_11
*Kirsty J Freeman
Duke-NUS Medical School
8 College Road,
Singapore 169857
Tel: +65 89219676
Email: kirsty.freeman@duke-nus.edu.sg
Submitted: 1 March 2021
Accepted: 13 September 2021
Published online: 4 January, TAPS 2022, 7(1), 9-20
https://doi.org/10.29060/TAPS.2022-7-1/RA2460
Cindy Shiqi Zhu1, Ryan Kye Feng Yap2,3, Samuel Yong Siang Lim2,3, Ying Pin Toh2,4 & Victor Weng Keong Loh1,2
1Department of Family Medicine, National University Health System, Singapore; 2Division of Family Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Ministry of Health Holdings, Singapore; 4HCA Hospice, Singapore
Abstract
Introduction: Humanistic values lie at the heart of medicine. In the wake of professional breaches among health care professionals, the place of humanistic values in medical training has been the subject of much debate and development in the literature. This scoping review aims to map the current understanding of how humanism in the Asian socio-cultural context may be understood and applied, and how the strengthening of humanistic values may be further integrated into medical schools in Asia.
Methods: Arksey and O’Malley’s approach to scoping reviews was used to guide the study protocol. Databases PubMed, ERIC, EMBASE, Scopus, CINAHL, and Web of Science were searched for articles on humanism and medical education in Asia. Data charting and thematic analysis were performed on the final articles selected.
Results: Three hundred and six abstracts were retrieved, 93 full-text articles were analysed, and 48 articles were selected. Thematic analysis revealed four themes on the need to strengthen humanistic values, the challenge of finding a common framework and definition, opportunities in medical school for curriculum design and training, and the need for validated tools in program evaluation in Asia.
Conclusion: Themes highlighted in this review show an increasing recognition amongst Asian medical educators of the importance of inculcating humanistic values into medical training. Further research and ongoing discussion are needed to develop culturally relevant, effective, and integrative curricula in order to promote humanistic attitudes and behaviours among medical students and physicians in Asia.
Keywords: Humanism, Asia, Medical Education, Medical Students, Admission, Curriculum, Mentorship, Assessment, Medical Humanities, Humanistic Values
Practice Highlights
- This review maps how medical schools in Asia impart humanistic values.
- There is a pressing need to strengthen humanistic values among medical students in Asia.
- The outcomes of current strategies are varied; mentorship and reflection on experience are crucial.
- There is much scope for further research in culturally relevant pedagogy that may impart humanism.
- Validated tools need to be developed for evaluating interventions to impart humanism in healthcare.
I. INTRODUCTION
Humanistic values lie at the heart of medicine. Humanism in health care has been defined as “an intrinsic set of deep-seated convictions about one’s obligations toward others”, and “devotion to human welfare”, characterised by a respectful and compassionate relationship between physicians, their patients, and other members of the healthcare team (Cohen, 2007; Gold, 2018).
Recent increased interest in the development of humanism in medical education (Maheux et al., 2000; Moyer et al., 2010; Wald et al., 2015) may be in response to concerns regarding the erosion of humanistic qualities among medical professionals (Haque & Waytz, 2012; Thibault, 2019). The push for medical humanism gained momentum through various advocacy movements, such as the Arnold P. Gold foundation in the United States, where the ‘IECARES’ framework was created to facilitate systematic discourse and study of humanism (Gold, 2018).
Medical educators in Asia have long recognised that humanistic traits are key to the art of medicine. They recognise that humanistic values have a positive effect on the patient-physician relationship, correlate positively with patient satisfaction, positively influence treatment outcome and adherence, and help maintain harmony in the working environment (Asai et al., 2007; Chiu et al., 2009; Saw, 2018; Song et al., 2017; Tokuda et al., 2008). Training in humanistic attitudes may therefore provide ballast to the thorny relationships sometimes seen in medical practice. In China, for example, more than 70% of doctors have experienced medical violence in hospitals, and strengthening humanistic values during medical training has been proposed as an urgent and important strategy to counteract this phenomenon (Hu, 2016).
Published studies from Asian medical training contexts that examine the perception, pedagogy, and assessment of humanistic values, and how humanism education frameworks derived from Western sociocultural contexts resonate with the cultural values, social history, and healthcare infrastructure in Asia are however relatively scarce.
As a social construct (Cohen, 2007; Kelly & Dornan, 2016; Rios, 2016), the discourse on humanism in Asian medical education and medical practice must consider cultural and contextual distinction from the main body of current literature that stems mainly from the West (Claramita et al., 2013; Schouten & Meeuwesen, 2006; Tsai, 2001). This study aims to explore how humanism has been understood and applied in medical education in the Asian sociocultural context by scoping current knowledge and evidence.
II. METHODS
A preliminary literature review revealed that existing literature on humanism in medical education in Asia was heterogeneous and limited. As such, a scoping review methodology was selected (Thomas et al., 2017). Arksey and O’Malley’s approach to scoping reviews was used to guide the study protocol (Arksey & O’Malley, 2005). Ethics approval was not required for this study, as it does not involve human subjects or data.
A. Identifying the Research Question and Relevant Studies
This study aims to provide an overview of the current knowledge on humanism in Asian medical education, identify successes and deficiencies in current practice, and guide further research.
The PICOS format was used to structure the research question for the literature search (Table 1). While alternate frameworks of humanism such as the Interactive Heart and Head model (Montgomery et al., 2017) and the outcome-oriented approach (Ferry-Danini, 2018) were considered, the authors decided that the Gold Foundation’s IECARES framework which knit together different strands of the humanism construct into a meaningful cohesive unit was most suited as a scaffold for our search terms. We thus included studies of any design on humanism and its core characteristics (Integrity, Excellence, Compassion & Collaboration, Altruism, Respect & Resilience, Empathy, and Service) as defined by the Gold Foundation’s IECARES framework), among medical students and educators in Asia. We excluded articles in foreign languages, on non-Asian populations, and allied health professionals (e.g. dentistry, pharmacy, nursing students). The search strategy was formulated through discussions between the authors and a medical librarian (A.C). Comprehensive search terms were constructed to expansively identify studies containing any synonyms or variation of three key concepts: humanism, medical education, and Asian countries and regions as defined by the United Nations Statistical Division (United Nations Statistics Division, n.d.). Six databases – PubMed, ERIC, EMBASE, Scopus, CINAHL, and Web of Science were searched.
|
PICOS Table |
Inclusion Criteria |
Exclusion Criteria |
|
Population |
Medical students and practising physicians including residents in Asia |
Allied health specialities such as nursing, pharmacy and physiotherapy. Non-medical specialities such as dentistry. Studies from non-Asian countries and regions |
|
Intervention |
Studies on humanism and its core characteristics (integrity, excellence, compassion, altruism, respect, empathy, and service) as defined by the GOLD foundation |
|
|
Comparison |
N/A |
N/A |
|
Outcome |
Definition of humanism Similarities and differences between Asian and Western concepts of humanism Perceptions on the integration of humanism as a subject/concept in medical education Methods of teaching humanism Assessment of humanistic characteristics and behaviour Suggested time point in training for teaching humanism |
|
|
Study Design |
All study designs and article types were included (observation studies, cross-sectional studies, nominal group studies, Delphi study, literature review, and scoping review) |
Studies published in a non-English language |
Table 1: PICOS Table of Inclusion and Exclusion Criteria
B. Study Selection
The selection process for articles is summarised in the PRISMA format (Moher et al., 2015) in Figure 1. Three hundred and six abstracts were identified through the initial search and reviewed after the removal of duplicates. Ninety-three full-text articles were examined to determine suitability for inclusion according to the selection criteria. Forty-eight full-text articles were included in the final review for thematic analysis.
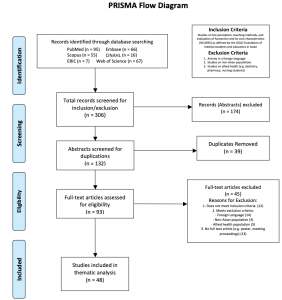
Figure 1. PRISMA Flowchart
C. Data Charting
Braun and Clarke’s inductive approach to reflective thematic analysis was utilised (Braun & Clarke, 2013, pp. 248-273). Two researchers (CZ and RY) independently reviewed the studies. Articles were read and analysed in detail, and key ideas were recorded into a data abstraction coding sheet (Zhu et al., 2021a). Frequently discussed ideas were identified and generated into a list of initial themes, which were added to a data extraction form (Zhu et al., 2021b). The researchers iteratively reviewed the independently extracted themes for agreement. This entailed a familiarisation with the depth and breadth of current knowledge through literature review and immersion in the derived data. The researchers subsequently ensured consistency in data extraction by applying the same coding sheet and data extraction forms on the entire data set, forming a template that included all the key ideas that were coded. Sessions for peer debriefing were set up to discuss more complex ideas by discussing each researchers’ interpretation all the while ensuring relevance to the research question.
D. Collating, Summarising, and Reporting Results
Codes and initial themes from the data abstraction sheet were reviewed and summarised into four final themes based on semantic and conceptual similarity. The themes were refined during the abstraction phase, and multiple discussions were conducted amongst all authors to achieve consensus on their definition and content. The results are reported in figures and narrative form below.
III. RESULTS
The final articles included in this review consisted mainly of cross-sectional studies of survey-based quantitative or mixed-method design and commentaries/essays by medical educators. There were a smaller number of nominal group studies, literature reviews, one Delphi study, and one scoping review on medical professionalism (Figure 2). East Asian studies (China, Taiwan, Japan, and Korea) comprised 58.33% of the articles included, South Asian (India, Pakistan, and Bangladesh) studies accounted for 16.7%, while studies from West Asia (Israel, Lebanon, Saudi Arabia) and Southeast Asia (Malaysia, Singapore, and Thailand) each accounted for 12.5% (Figure 3). The articles ranged in publication date from 1995 to 2018. Notably, there was a steady increase in the number of articles over this period (Figure 4). Thematic analysis revealed the following themes on humanism in Asian medical education (Zhu et al., 2021a, 2021b).

Figure 2. Graphical representation of article types included in the current review
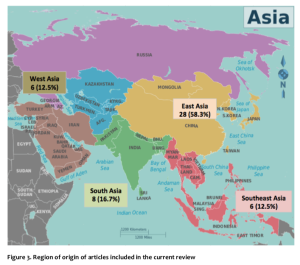
Figure 3. Region of origin of articles included in the current review
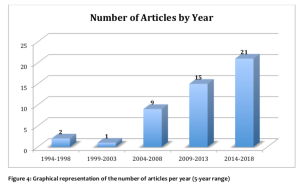
A. Training in Humanistic Values: A Pressing Need in Asian Medical Schools
The common refrain of concern for the current state of medical students’ and physicians’ humanistic qualities was highlighted in many articles from several Asian countries and regions. Issues related to breaches of professional and ethical behaviour among medical students and young physicians were widespread and of serious concern to medical educators and the general public in Japan (Tokuda et al., 2008). Taiwanese educators lamented a lack of dedication and personal commitment among young Taiwanese physicians compared to their predecessors (Chiu et al., 2010). In Pakistan, concerns regarding the deterioration of humanism and professional values in medicine were raised, with students overestimating the self-rated quality of their bedside manner compared to objective assessments (Farooq et al., 2013). Bhatia et al from India indicated that humanistic traits such as empathy, caring, altruism, and compassion were often underdeveloped in medical students and doctors (Bhatia et al., 2013). In China, medical students were described to be lacking in humanistic concerns, humanistic knowledge (cultural, geographical, historical), and awareness of the importance of humanism education (Liu & Li, 2012). A cross-sectional study of emergency physicians in Singapore found that they were perceived to be weak in humanistic traits including patient communication, holistic management, and professional relationship with colleagues (Fones et al., 1998). There was a clear and pressing need to foster humanistic values in medical training in Asian medical schools (Asai et al., 2007; Chiu et al., 2009; Hu, 2016; Saw, 2018; Song et al., 2017; Tokuda et al., 2008).
B. “Seeking the Welfare of the Other”: Unity Amidst Diversity of Meanings of Humanistic Values
Studies on Asian medical humanism adopted definitions and frameworks from the West, such as the Gold Foundation’s IECARES framework, and ABIM’s charter of physician professionalism (Chiu et al., 2009; Tsai et al., 2007). However, the direct application of these definitions and frameworks in Asia has been questioned (Chiu et al., 2009; Wang et al., 2016){Chiu, 2009 #53}. It has been recognised that the interpretations of medical humanism may vary due to the influence of local cultural, religious and philosophical systems, as well as difficulties in translating abstract concepts such as “ethics” that have been derived from a Western context (Ho et al., 2014; Pan et al., 2013; Qian et al., 2018; Zhang & Cheng, 2000).
While Western notions of humanism dichotomised physicians’ professional and personal lives, studies found that the collectivism imbued in East Asian physicians underpinned by Confucian cultural traditions blurred the lines between one’s personal and societal roles (Ho et al., 2014). Pan et al. (2013) commented that healthcare professionals in China considered the Western-derived term of “ethics” as being external to the individual, and thus ranked it low on the list of desired professional values in deference to “moral character” which was perceived to be more innate. The Confucian collectivistic slant could further be gleaned in concepts such as guanxi – the fostering of social relationships through the mutual exchange of favours, renai – “humane love” and gongxin or “public-spiritedness”. Traditional Chinese medical ethics, while influenced by two other major traditions – Taoism which leaned toward the pursuit of longevity, and Buddhism whose goal was the transcendence of the endless cycles of rebirth through non-attachment and garnering of merit, nonetheless had Confucianism as its core position (Zhang & Cheng, 2000).
While Jiang and Liu from mainland China proposed a narrative definition of humanistic medicine as “an interdisciplinary science that synthesizes knowledge concerning medical philosophy, medical ethics, medical law, medical history, medical sociology, medical logic, and doctor-patient communication” (Jiang & Liu, 2014), Wong from Taiwan has proposed the same to be “[a service environment where] patient welfare, patient autonomy, and social justice take primacy, and [practitioners] offer charitable and dignified treatment” (Wong et al., 2012). Among Asians of the Muslim tradition, Al-Eraky et al. (2014) described a four-gates model that pointed to four relationships the Muslim-Arab medical professional did well to align him/herself with; these include right relationships with the self – self-awareness, with the task-at-hand – excellence and reflective practice, with others – respect of patients and team members, and with God – self-awareness and right relationship with the Divine (Al-Eraky et al., 2014). Meanwhile, the perspective of patients in Singapore and Israel while highlighting the importance of moral-humanistic traits such as empathy highly, nonetheless ranked professional expertise above all other traits (Fones et al., 1998; Schattner et al., 2004).
Amid the broad differences in individual differences in how humanistic values were articulated regionally – for instance, the reference to collectivism in the East Asian context, and the reference to the divine in the Arab-Muslim context – these expressed how each sociocultural context sought that common humanistic goal of “seeking the welfare of the other.” We propose that the universal attributes of the IECARES framework (Gold, 2018) arguably encompasses these values.
C. Humanistic Values in Medical Training
1) Select for humanistic values:
For medical admissions to successfully select candidates that would become humanistic and competent medical professionals at the end of training, any process for entry into medical school based narrowly on academic criteria was inadequate. Authors argued that in addition to academic performance, medical admissions processes should include involvement in community work, extra-curricular activities, and the consideration of recommendation letters to better reflect the humanistic attributes of candidates that academic performance alone would not capture (Chiu et al., 2009; Lee & Ahn, 2004; Tokuda et al., 2008)
2) An afterthought in planning:
As a non-traditional curricular item, the introduction of humanism learning activities into already heavily packed curricula would often be met with resistance and/or inertia, be ranked lower in priority (Rao & Rao, 2007; Tokuda et al., 2008) and thereby poorly integrated into Asian medical school curricula (Liu & Li, 2012; Rao & Rao, 2007). When these existed in the curriculum, humanism courses were usually of short duration, offered as an elective (Liu & Li, 2012; Qian et al., 2018; Wang et al., 2016), and scheduled at unfavourable time slots (Kosik et al., 2014; Notzer et al., 2005). Students were often hard-to-manage and poorly motivated (Tsai et al., 2007; Woratanarat, 2014), and faculty would often have variable credentials (Liu & Li, 2012). Compounding this was the common experience of observing humanistic values being sidelined by busy healthcare providers on entering the workforce (Tsai et al., 2007).
Caught where holistic care is valued. Humanistic values would be best caught in specialities that prioritised the holistic care of individuals and families such as Family Medicine. Authors lamented how paternalistic medical cultures (Farooq et al., 2013) prioritised the draw of cutting-edge technologies and hospital specialities in the curriculum (Akhund et al., 2014) over disciplines where humanistic biopsychosocial (Engel, 1977) care was explicitly valued (Biderman, 2003; Iqbal, 2010; Rao & Rao, 2007).
3) Begin early, continue longitudinally:
Asian medical educators generally agreed that learning humanistic values should start early, and continue into post-graduate education, with contextualisation of how these could be applied at different workplace settings (Biderman, 2003; Karunakaran et al., 2017; Kosik et al., 2014; Qian et al., 2018; Singh & Talwar, 2013; Wang et al., 2016). The Medical Council of India recommended that humanistic values be introduced in the early pre-clinical years to students who often harboured ideals and a sense of duty to their home communities before these sentiments waned with further training (Karunakaran et al., 2017). These learning opportunities should then extend longitudinally into post-graduate years when values may be challenged in the face of real-world challenges in clinical practice (Biderman, 2003; Singh & Talwar, 2013; Wang et al., 2016).
4) Learning methods: Experiences and reflection:
A range of teaching methods has been tried in the attempt to impart humanistic values in Asia. In addition to lecture-based learning, it was recommended that interactive experiential learning activities where humanistic attributes were practised should be designed into the curriculum (Wang et al., 2016). The Silent Mentor Program where students met and interacted with the families of human cadaver donors, listened to their narratives, and respectfully participated in culturally and religiously appropriate ceremonies, was an example of a successful program where students learnt to integrate humanistic values as they learnt about human anatomy (Karunakaran et al., 2017; Rao & Rao, 2007; Saw, 2018). Other teaching activities include the use of art in Hong Kong to prompt self-awareness and empathy (Potash & Chen, 2014), the use of film and photography (Kosik et al., 2014; Lee & Ahn, 2004; Nakayama, 2009; Woratanarat, 2014), and training in communications skills that integrated interpersonal- and clinical- skills training (Biderman, 2003; Kaga & Asakage, 2007; Yazigi et al., 2006), narrative medicine (Chiu et al., 2009) and community humanitarian work (Chen & Chou, 2015; Wang et al., 2016). Courses in the humanities and social sciences, such as history, literature, ethics, law, and medical social studies have also become part of some medical curricula; they provide insight into the human condition and have been successfully used to foster humanistic qualities in medical students (Fones et al., 1998; Lee & Ahn, 2004; Liu & Li, 2012; Song & Tang, 2017). The co-design and co-facilitation of medical humanities course of home-faculty based basic scientists or clinicians with social scientist colleagues as opposed to having social scientists running a programme solo was a promising curriculum strategy that legitimised and contextualised the importance of learning the medical humanities (Rider et al., 2014; Singh & Talwar, 2013).
5) Mentorship and role-modelling crucial:
Fostering strong and dedicated mentor-mentee relationships is crucial for the development of humanistic traits through positive role-modeling (Bhatia et al., 2013; Islam et al., 2014). Positive attributes in mentors motivated learners to model their humanistic behaviour (Bhatia et al., 2013; Chiu et al., 2009; Farooq et al., 2013; Islam et al., 2014; Singh & Talwar, 2013), whereas negative behaviours in the informal and hidden curriculum constituted a formidable counter-influence (Akhund et al., 2014; Salam et al., 2012; Wong et al., 2012). Authors highlighted the importance of faculty development where faculty learnt to internalise their responsibility as role models; strengthened awareness of their learner’s needs, expectations, and feelings; and recognised how as mentors they unwittingly enabled or hindered the positive development of humanistic attitudes among learners (Biderman, 2003; Liu & Cheng, 2017; Notzer et al., 2005; Rao & Rao, 2007).
D. Program Evaluation: Need for Validated Tools
A small number of articles in this review examined how humanism was evaluated in Asian medical schools. Most used self-assessment tools developed in Western contexts. For example, the Jefferson Scale of Physician Empathy (JSPE) has been validated in several Asian cultures and languages and has a version for medical students (Mostafa et al., 2014). Taiwanese educators have translated and applied a 32-item self-administered questionnaire reflecting students’ perception of seven characteristics of professionalism defined by the American Board of Internal Medicine, many of which overlap with humanistic traits (Tsai et al., 2007). A novel instrument to measure students’ perception of personal attributes including honesty, respectfulness, and compassion was developed and validated by Malaysian educators, which included both a Likert scale and open-ended questions (Salam et al., 2012).
Few observer-rated and arguably more objective methods of humanistic behaviours were identified in this review. In a limited number of studies, the 360-degree peer evaluation was well received for evaluation of humanistic skills among physician trainees and residents (Tham, 2007; Wang et al., 2016), whereas the Defining Issues Test (DIT) may be a better tool for medical students with little working experience (Wang et al., 2016).
The need to develop validated methods to assess humanistic attributes was recognised, both to evaluate the effectiveness of teaching at the programmatic level (Tsai et al., 2007), as well as to identify students who required remediation and guidance in their professional development (Liu & Cheng, 2017).
IV. DISCUSSION
The current article presents a scoping review of peer-reviewed publications on humanism in Asian medical education. The four themes identified include the need to strengthen humanistic values among Asian medical students and physicians; the challenge of finding a common conceptual framework for operationalising humanistic values in Asia; opportunities in medical school to foster humanistic values at admissions, in curriculum planning, implementation within disciplines which teach holistic care, the use of different pedagogies, the role of mentorship, and fourthly the need for validated tools in program evaluation.
This review encompassed a diversity of types of articles and broad geographical representation.
Several findings of this review resonate with international literature. Both Western and Asian literature highlighted the importance of imparting humanistic values in medical training (Bombeke et al., 2010; Rios, 2016; Wald et al., 2015).
There was a lack of a common definition of humanistic medicine in this review, and that it was often conflated with other education concepts such as professionalism (Cohen, 2007; Hauck et al., 1990; Thibault, 2019; Tsai et al., 2007). We found nonetheless that the Gold foundation’s IECARES framework provided a broad enough scaffold to encompass the key notions of humanistic values in the Asian context. One of the key discrepancies between Asian and Western notions of humanism that surfaced in this review was that while humanistic medicine in the Western context often referred to a set of physician attributes, most commonly compassion, respect, and empathy toward patients, the therapeutic relationship in Asia may have distinct priorities. This would include the role of the patient in relation to his/her family, community, and society given the more collectivistic stance of the Asian patient. In addition, the notion of physician expertise may need to be more explicitly articulated (Fones et al., 1998; Ho et al., 2014; Schattner et al., 2004). In addition, the notion of relationship with self and the divine was highlighted in the West Asian four doors framework that is not explicitly mentioned in IECARES.
Much like educators in the West, Asian educators in this review describe the challenges associated with teaching humanism alongside the existing rigorous medical curricula for acquiring scientific and clinical skills, which often overshadows the humanistic aspect of medical education (Doran, 1983; Mostafa et al., 2014; Singh & Talwar, 2013). Nevertheless, some of the current methods used to impart humanism in Asian medical schools show promise in improving students’ humanistic attitudes. For example, medical-themed films were rated highly by students in their ability to enable understanding of humanistic and social aspects of medicine (Lee & Ahn, 2004), art-mediate learning increased students’ empathy on the State Empathy Scale (Potash & Chen, 2014), and the Silent Mentor Program nurtured the sense of responsibility and compassion within students as shown in their personal reflections (Lin et al., 2009). It remains a challenge for both Asian and Western medical educators to develop tools to objectively evaluate humanistic attitudes and behaviours (Buck et al., 2015; Shrank et al., 2004; Wang et al., 2016), which would be valuable in both assessing the effectiveness of teaching methods as well as motivate trainees to foster an active learning attitude (Pacifico et al., 2020).
Furthermore, methods to impart humanism must evolve along with students’ level of medical training. A qualitative study conducted in Singaporean found that medical trainees at different stages of their training valued different types of teachers, preferring a didactic approach in their earlier years, in contrast to more role-modelling and feedback once they step into clinical practice (Ooi et al., 2021).
This study has several limitations. Firstly, the term “humanism” and its conjugations were used in our search strategy to identify articles on humanistic attitudes and behaviours as a collective concept rather than its parts. However, there may be articles focused on one or more aspects of humanism education, such as empathy or compassion alone, which may not have been identified in the search. Furthermore, the inclusion criteria were constructed using Gold Foundation’s ‘IECARES’ framework, while it was later revealed through inductive thematic analysis that culturally relevant definitions should be developed to explore humanism in Asian medical education. Secondly, only English language databases were searched, and foreign language articles were excluded for practical purposes. Thirdly, there were notable intra-continental differences between various Asian countries represented, and there were a larger proportion of articles from East Asia in this review with Confucianism-based cultural origins. As such, conclusions drawn from these regions may be internally similar but require further adaptation for regions with differing religious or cultural origins.
V. CONCLUSION
Though Asia has been the cradle of many humanistic traditions since the dawn of civilisation, the explicit introduction of humanism education into the discourse of Asian medical schools is a recent phenomenon. This scoping review unveiled themes on key contentions around why, when, and how humanism should be integrated into the curriculum, and how this may impact the professional development of students, physicians and their relationship with their patients. Many of these topics are exciting areas of research that deserves greater attention.
Culturally validated frameworks and definitions of Asian medical humanism are lacking, and the agreed-upon frameworks may need to consider the sociocultural contexts of the different regions. What is clearly agreed upon is that the humanistic qualities of Asian medical students and physicians are in pressing need of improvement. Progress has been stifled by a slow start, the inertia from existing traditions that constrain changes, and differing opinions regarding the need for change. Various approaches to teaching humanism have been devised, such as elective humanities courses, participatory learning, mentorship, and the hidden curriculum. Authors called for improved quantity and quality of humanities courses, learning experiences outside of the classroom, and positive role-modeling in a longitudinal manner with constant integration back to the learner’s evolving clinical setting.
The current review presents an exciting growing body of literature advocating for the development of medical humanism in Asia. Further research, especially longitudinal studies, is needed to evaluate medical school admission processes, teaching and evaluation strategies in the instillation of humanistic medicine in Asia.
Notes on Contributors
TYP and VL designed and conceived the study. CZ and SL constructed search terms. CZ and RY conducted the literature review. CZ wrote the draft of the manuscript. CZ and VL co-edited the final draft. All authors have reviewed and approved the manuscript.
Ethical Approval
Ethics approval is not application for this review, as it does not involve human subjects or data.
Data Availability
The manuscript’s data is available at Figshare and may be accessed via the following public digital object identifier:
- Coding Sheet https://doi.org/10.6084/m9.figshare.14245850.v1
- Data Abstraction Sheet https://doi.org/10.6084/m9.figshare.14245991.v1
Acknowledgement
The authors wish to thank Ms. Annelissa Chin Mien Chew for her assistance with search terms and database search.
Funding
This research received no specific grant or funding from any agency in the public, commercial, or not-for-profit sectors.
Declaration of Interest
All authors certify that they have no affiliations with any organisation or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
References
Akhund, S., Shaikh, Z. A., & Ali, S. A. (2014). Attitudes of Pakistani and Pakistani heritage medical students regarding professionalism at a medical college in Karachi, Pakistan. BMC Research Notes, 7, 150. https://doi.org/10.1186/1756-0500-7-150
Al-Eraky, M. M., Donkers, J., Wajid, G., & van Merrienboer, J. J. G. (2014). A Delphi study of medical professionalism in Arabian countries: The Four-Gates model. Medical Teacher, 36 (Suppl 1), S8-S16. https://doi.org/10.3109/0142159X.2014.886013
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19-32. https://doi.org/10.1080/1364557032000119616
Asai, A., Ohnishi, M., Bito, S., Furutani, N., Ino, T., Kimura, K., Imura, H., Hayashi, A., & Fukui, T. (2007). Humanistic qualities of physicians: A view of Japanese residents. Medical Teacher, 29(4), 414. https://doi.org/10.1080/01421590701288523
Bhatia, A., Singh, N., & Dhaliwal, U. (2013). Mentoring for first year medical students: Humanising medical education. Indian Journal of Medical Ethics, 10(2), 100-103. https://doi.org/10.20529/IJME.2013.030
Biderman, A. (2003). Family medicine as a frame for humanized medicine in education and clinical practice. Public Health Reviews, 31(1), 23-26.
Bombeke, K., Symons, L., Debaene, L., De Winter, B., Schol, S., & Van Royen, P. (2010). Help, I’m losing patient-centredness! Experiences of medical students and their teachers. Medical Education, 44(7), 662-673. https://doi.org/10.1111/j.1365-2923.2010.03627.x
Braun, V., & Clarke, V. (2013). Successful Qualitative Research: A practical guide for beginners. SAGE.
Buck, E., Holden, M., & Szauter, K. (2015). A methodological review of the assessment of humanism in medical students. Academic Medicine, 90(11 Suppl), S14-S23. https://doi.org/10.1097/ACM.0000000000000910
Chen, S.-S., & Chou, P. (2015). The implication of integrated training program for medical history education. Biomedical Journal, 38(1), 90-94. https://doi.org/10.4103/2319-4170.132885
Chiu, C.-H., Arrigo, L. G., & Tsai, D. (2009). Historical context for the growth of medical professionalism and curriculum reform in Taiwan. Kaohsiung Journal of Medical Sciences, 25(9), 510-514. https://doi.org/10.1016/S1607-551X(09)70558-3
Chiu, C.-H., Lu, H.-Y., Arrigo, L. G., Wei, C.-J., & Tsai, D. (2010). A professionalism survey of medical students in Taiwan. Journal of Experimental & Clinical Medicine, 2(1), 35-42. https://doi.org/10.1016/S1878-3317(10)60006-X
Claramita, M., Nugraheni, M. D. F., van Dalen, J., & van der Vleuten, C. (2013). Doctor-patient communication in Southeast Asia: A different culture? Advances in Health Sciences Education, 18(1), 15-31. https://doi.org/10.1007/s10459-012-9352-5
Cohen, J. J. (2007). Viewpoint: Linking professionalism to humanism: What it means, why it matters. Academic Medicine, 82(11), 1029-1032. https://doi.org/10.1097/01.ACM.0000285307.17430.74
Doran, G. A. (1983). Scientism vs humanism in medical education. Social Science & Medicine, 17(23), 1831-1835. https://doi.org/10.1016/0277-9536(83)90159-4
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129-136. https://doi.org/10.1126/science.847460
Farooq, Z., Mustaf, T., Akram, A., Khan, M., Amjad, R., Naveed, M., Azhar, A., Chaudhry, A. M., Khan, M. A. Z., & Rafiq, F. (2013). Bedside manners: Do we care? Journal Ayub Medical College Abbottabad, 25(1-2), 179-182.
Ferry-Danini, J. (2018). A new path for humanistic medicine. Theoretical Medicine and Bioethics, 39(1), 57-77. https://doi.org/10.1007/s11017-018-9433-4
Fones, C., Heok, K. E., & Gan, G. L. (1998). What makes a good doctor: Defining the ideal end-product of medical education. Academic Medicine, 73(5), 571-572. https://doi.org/10.1097/00001888-199805000-00029
Gold, A. P. (2018). Definition of humanism. Gold Foundation. Retrieved September 21, 2021, from https://www.gold-foundation.org/definition-of-humanism/
Haque, O. S., & Waytz, A. (2012). Dehumanization in Medicine: Causes, solutions, and functions. Perspectives on Psychological Science, 7(2), 176-186. https://doi.org/10.1177/1745691611429706
Hauck, F. R., Zyzanski, S. J., Alemagno, S. A., & Medalie, J. H. (1990). Patient perceptions of humanism in physicians: Effects on positive health behaviors. Family Medicine, 22(6), 447-452.
Ho, M.-J., Yu, K.-H., Pan, H., Norris, J. L., Liang, Y.-S., Li, J.-N., & Hirsh, D. (2014). A tale of two cities: Understanding the differences in medical professionalism between two Chinese cultural contexts. Academic Medicine, 89(6), 944-950. https://doi.org/10.1097/ACM.0000000000000240
Hu, X. (2016). Education as a starting point for preventing medical violence: Implications for medical violence in China. A commentary on Tan MF et al.” Nursing management of aggression in a Singapore emergency department: A qualitative study” Nursing & Health Sciences, 18(4), 539.
Iqbal, S. P. (2010). Family medicine in undergraduate medical curriculum: A cost-effective approach to health care in Pakistan. Journal Ayub Medical College Abbottabad, 22(4), 207-209.
Islam, M. Z., Salam, A., Helali, A. M., Rahman, Z., Wan, W. P. E., Ismail, S., Rahman, N. I. A., & Haque, M. (2014). Comparative study of professionalism of future medical doctors between Malaysia and Bangladesh. Journal of Applied Pharmaceutical Science, 4(4), 66-71.
Jiang, B., & Liu, H. (2014). Constructing the discipline of humanistic medicine on Mainland China. Chinese Education & Society, 47(3), 70-73.
Kaga, K., & Asakage, T. (2007). Medical education by bedside learning – Helping medical students to interact with patients who have head and neck cancer. Acta Oto-Laryngologica, 127(4), 408-410. https://doi.org/10.1080/00016480601011485
Karunakaran, I., Thirumalaikolundusubramanian, P., & Nalinakumari, S. D. (2017). A preliminary survey of professionalism teaching practices in anatomy education among Indian Medical Colleges. Anattomical Sciences Education, 10(5), 433-443. https://doi.org/10.1002/ase.1679
Kelly, M., & Dornan, T. (2016). Mapping the landscape or exploring the terrain? Progressing humanism in medical education. Medical Education, 50(3), 273-275. https://doi.org/10.1111/medu.12967
Kosik, R. O., Huang, L., Cai, Q., Xu, G.-T., Zhao, X., Guo, L., Tang, W., Chen, Q., & Fan, A. P.-C. (2014). The current state of medical education in Chinese Medical Schools: Humanities and medical ethics. Chinese Education & Society, 47(3), 74-87. https://doi.org/10.2753/CED1061-1932470308
Lee, Y.-M., & Ahn, D.-S. (2004). Medical-themed film and literature course for premedical students. Medical Teacher, 26(6), 534-539. https://doi.org/10.1080/01421590412331282318
Lin, S. C., Hsu, J., & Fan, V. Y. (2009). “Silent virtuous teachers”: Anatomical dissection in Taiwan. BMJ, 339(b5001). https://doi.org/10.1136/bmj.b5001
Liu, S., & Li, Y. (2012). Analysis of the status quo of humanistic quality-oriented education in medical colleges and universities. International Education Studies, 5(1), 216-220. https://doi.org/10.5539/ies.v5n1p216
Liu, Y., & Cheng, X. (2017). An upcoming program for medical humanities education in Fudan University’s School of Basic Medical Sciences. BioScience Trends, 11(2), 152-153. https://doi.org/10.5582/bst.2017.01094
Maheux, B., Beaudoin, C., Berkson, L., Côté, L., Des Marchais, J., & Jean, P. (2000). Medical faculty as humanistic physicians and teachers: The perceptions of students at innovative and traditional medical schools. Medical Education, 34(8), 630-634. https://doi.org/10.1046/j.1365-2923.2000.00543.x
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., Stewart, L. A., & PRISMA-P Group (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4, 1. https://doi.org/10.1186/2046-4053-4-1
Montgomery, L., Loue, S., & Stange, K. C. (2017). Linking the heart and the head: Humanism and professionalism in medical education and practice. Family Medicine, 49(5), 378-383.
Mostafa, A., Hoque, R., Mostafa, M., Rana, M. M., & Mostafa, F. (2014). Empathy in undergraduate medical students of bangladesh: Psychometric analysis and differences by gender, academic year, and specialty preferences. ISRN Psychiatry, 2014, 375439. https://doi.org/10.1155/2014/375439
Moyer, C. A., Arnold, L., Quaintance, J., Braddock, C., Spickard, A., Wilson, D., Rominski, S., & Stern, D. T. (2010). What factors create a humanistic doctor? A nationwide survey of fourth-year medical students. Academic Medicine, 85(11), 1800-1807. https://doi.org/10.1097/ACM.0b013e3181f526af
Nakayama, D. K. (2009). Professionalism in Kurosawa’s medical dramas. Journal of Surgical Education, 66(6), 395-398. https://doi.org/10.1016/j.jsurg.2009.06.001
Notzer, N., Abramovitch, H., Dado-harari, R., Abramovitz, R., & Rudnick, A. (2005). Medical students’ ethical, legal and cross-cultural experiences during their clinical studies. Israel Medical Association Journal, 7(1), 58-61.
Ooi, S. B. S., Tan, C. W. T., & Frambach, J. M. (2021). Who is an effective clinical teacher from the perspectives of medical students and residents? The Asia Pacific Scholar, 6(1), 40-48. https://doi.org/10.29060/TAPS.2021-6-1/OA2227
Pacifico, J. L., Villanueva, J. A. S., Heeneman, S., & van der Vleuten, C. (2020). How perceptions of residents toward assessment influence learning: A qualitative study. The Asia Pacific Scholar, 5(1), 46-53. https://doi.org/10.29060/TAPS.2020-5-1/OA2080
Pan, H., Norris, J. L., Liang, Y.-S., Li, J.-N., & Ho, M.-J. (2013). Building a professionalism framework for healthcare providers in China: A nominal group technique study. Medical Teacher, 35(10), e1531-e1536. https://doi.org/10.3109/0142159X.2013.802299
Potash, J., & Chen, J. (2014). Art-mediated peer-to-peer learning of empathy. The Clinical Teacher, 11(5), 327-331. https://doi.org/10.1111/tct.12157
Qian, Y., Han, Q., Yuan, W., & Fan, C. (2018). Insights into medical humanities education in China and the West. Journal of International Medical Research, 46(9), 3507-3517. https://doi.org/10.1177/0300060518790415
Rao, K. H., & Rao, R. H. (2007). Perspectives in medical education 5. Implementing a more integrated, interactive and interesting curriculum to improve Japanese medical education. Keio Journal of Medicine, 56(3), 75-84. https://doi.org/10.2302/kjm.56.75
Rider, E. A., Kurtz, S., Slade, D., Longmaid, E., Ho, M.-J., Pun, J. K., Eggins, S., & Branch, W. T. (2014). The international charter for human values in healthcare: An interprofessional global collaboration to enhance values and communication in healthcare. Patient Education and Counseling, 96(3), 273-280. https://doi.org/10.1016/j.pec.2014.06.017
Rios, I. C. (2016). The contemporary culture in medical school and its influence on training doctors in ethics and humanistic attitude to the clinical practice. International Journal of Ethics Education, 1(1), 173-182. https://doi.org/10.1007/s40889-016-0012-0
Salam, A., Chew, O. S., Mazlan, N. F., Hassin, H., Lim, S. L., & Abdullah, M. H. (2012). Professionalism of future medical professionals in universiti kebangsaan Malaysia (ukm) medical centre. International Medical Journal, 19(3), 224-228.
Saw, A. (2018). A new approach to body donation for medical education: The silent mentor programme. Malaysian Orthopaedic Journal, 12(2), 68-72. https://doi.org/10.5704/MOJ.1807.015
Schattner, A., Rudin, D., & Jellin, N. (2004). Good physicians from the perspective of their patients. BMC Health Services Research, 4(1), 26. https://doi.org/10.1186/1472-6963-4-26
Schouten, B. C., & Meeuwesen, L. (2006). Cultural differences in medical communication: A review of the literature. Patient Education and Counselling, 64(1-3), 21-34. https://doi.org/10.1016/j.pec.2005.11.014
Shrank, W. H., Reed, V. A., & Jernstedt, C. (2004). Fostering professionalism in medical education: A call for improved assessment and meaningful incentives. Journal of General Internal Medicine, 19(8), 887-892. https://doi.org/10.1111/j.1525-1497.2004.30635.x
Singh, M., & Talwar, K. K. (2013). Putting the humanities back into medicine: Some suggestions. Indian Journal of Medical Ethics, 10(1), 54-55. https://doi.org/10.20529/IJME.2013.013
Song, P., Jin, C., & Tang, W. (2017). New medical education reform in China: Towards healthy China 2030. BioScience Trends, 11(4), 366-369. https://doi.org/10.5582/bst.2017.01198
Song, P., & Tang, W. (2017). Emphasizing humanities in medical education: Promoting the integration of medical scientific spirit and medical humanistic spirit. Bioscience Trends, 11(2), 128-133. https://doi.org/10.5582/bst.2017.01092
Tham, K.-Y. (2007). 360 Degrees feedback for emergency physicians in Singapore. Emergency Medicine Journal, 24(8), 574-575. https://doi.org/10.1136/emj.2007.047530
Thibault, G. E. (2019). Humanism in Medicine: What does it mean and why is it more important than ever? Academic Medicine, 94(8), 1074-1077. https://doi.org/10.1097/ACM.0000000000002796
Thomas, A., Lubarsky, S., Durning, S. J., & Young, M. E. (2017). Knowledge syntheses in medical education: Demystifying scoping reviews. Academic Medicine, 92(2), 161-166. https://doi.org/10.1097/ACM.0000000000001452
Tokuda, Y., Hinohara, S., & Fukui, T. (2008). Introducing a new medical school system into Japan. Annals of the Academy of Medicine Singapore, 37(9), 800-802.
Tsai, D. F.-C. (2001). How should doctors approach patients? A Confucian reflection on personhood. Journal of Medical Ethics, 27(1), 44-50. https://doi.org/10.1136/jme.27.1.44
Tsai, T.-C., Lin, C.-H., Harasym, P. H., & Violato, C. (2007). Students’ perception on medical professionalism: The psychometric perspective. Medical Teacher, 29(2-3), 128-134. https://doi.org/10.1080/01421590701310889
United Nations Statistics Division. (n.d.). UNSD — Methodology. United Nations. Retrieved September 23, 2021, from https://unstats.un.org/unsd/methodology/m49/
Wald, H. S., Anthony, D., Hutchinson, T. A., Liben, S., Smilovitch, M., & Donato, A. A. (2015). Professional identity formation in medical education for humanistic, resilient physicians: Pedagogic strategies for bridging theory to practice. Academic Medicine, 90(6), 753-760. https://doi.org/10.1097/ACM.0000000000000725
Wang, X., Shih, J., Kuo, F.-J., & Ho, M.-J. (2016). A scoping review of medical professionalism research published in the Chinese language. BMC Medical Education, 16(1), 300. https://doi.org/10.1186/s12909-016-0818-7
Wong, Y. F., Lin, S. J., Cheng, H. C., Hsieh, T. H., Hsiue, T. R., Chung, H. S., Tsai, M. Y., & Wang, M. R. (2012). The formation and performance of medical humanities by interns in a clinical setting. Tzu Chi Medical Journal, 24(1), 5-11.
Woratanarat, T. (2014). Higher satisfaction with ethnographic edutainment using YouTube among medical students in Thailand. Journal of Educational Evaluation for Health Professions, 11. https://doi.org/10.3352/jeehp.2014.11.13
Yazigi, A., Nasr, M., Sleilaty, G., & Nemr, E. (2006). Clinical teachers as role models: Perceptions of interns and residents in a Lebanese medical school. Medical Education, 40(7), 654-661. https://doi.org/10.1111/j.1365-2929.2006.02502.x
Zhang, D., & Cheng, Z. (2000). Medicine is a humane art. The basic principles of professional ethics in Chinese medicine. The Hastings Center Report, 30(4), S8-S12.
Zhu, C., Yap, R., Lim, S., Toh, Y., & Loh, V. (2021a). Coding sheet (Humanism in Medical Education – A Scoping Review) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14245850.v1
Zhu, C., Yap, R., Lim, S., Toh, Y., & Loh, V. (2021b). Data Abstraction Sheet for Thematic Analysis (Humanism in Medical Education – A Scoping Review) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14245991.v1
*Cindy Shiqi Zhu
National University Health System,
1E Kent Ridge Road,
Singapore 119228
Email: Shi_Qi_ZHU@nuhs.edu.sg
Submitted: 14 June 2021
Accepted: 22 July 2021
Published online: 4 January, TAPS 2022, 7(1), 3-8
https://doi.org/10.29060/TAPS.2022-7-1/GP2655
Nagisa Shinagawa1, Tomoaki Inada2, Harumi Gomi3, Haruko Akatsu3, Motofumi Yoshida3 & Yutaka Kawakami3
1Graduate School of Medicine, International University of Health and Welfare, Japan; 2International Center, Jumonji University, Japan; 3School of Medicine, International University of Health and Welfare, Japan
Abstract
Introduction: The International University of Health and Welfare (IUHW) School of Medicine was founded in 2017 with the intention of providing medical content in English a historical first in Japan. Twenty international medical students have been accepted annually, with the majority possessing less than beginner level Japanese language proficiency at the time of enrolment. However, proficiency in Japanese, especially in the context of medicine is required for academic success and program completion. To address this, the IUHW School of Medicine has developed a course in medical Japanese with the objective of facilitating international students’ acquisition of medical Japanese and reinforcing such acquisition through various listening, speaking, reading, and writing activities. This study aims to describe the Japanese language education program for international students at the IUHW School of Medicine, with particular focus on the development of the curriculum and course content.
Methods: The course is designed based on the following educational strategies and their applications: (a) Synchronisation of both medical and Japanese contents; (b) Collaborative learning; (c) Japanese output of medical content learned in English; (d) Practical output through making/giving a presentation and discussion with medical experts; (e) Detailed language feedback from language experts; (f) Reinforcing the vocabulary knowledge by writing; and (g) Building up vocabulary and expressions with relevant contents.
Results: Our observations suggest that our international students have been able to continue their medical education in Japanese smoothly.
Conclusion: The content-based instructional design that includes second language acquisition strategies may also be applicable to other Asian languages such as Korean and Chinese.
Practice Highlights
- We have developed a medical Japanese language course to facilitate international students’ acquisition of Japanese medical language and to reinforce such acquisition through various listening, speaking, reading, and writing activities.
- According to the course design, Japanese language teachers introduce medical vocabulary and expressions into their lessons, and medical teachers determine their application by checking for errors in their Japanese-language presentation of medically-related content.
- This is the first effort in Japan to systematically teach medical Japanese to international students at the elementary level at a medical school.
- This approach has had a positive effect on international students’ acquisition of medical Japanese.
I. INTRODUCTION
International medical students’ need for linguistic educational support has been well reported by researchers in various countries. Many international students in Europe and the United States who have passed the language proficiency tests of their host institutions and are judged to have high language proficiency reportedly continue to have language-related problems in their academic and clinical work at medical schools (Michalski et al., 2017). To address this issue, educational courses for international students studying medicine in a second or third language are being implemented (Huhn et al., 2018). Although reports of such efforts in Chinese medical schools have surfaced in recent years (Zhang et al., 2019), no reports on systematic Japanese language education for international medical students have been published, in part due to the small number of international students in Japanese medical schools.
At the International University of Health and Welfare (IUHW) School of Medicine in Japan, 20 international medical students have been accepted annually since its foundation in 2017. However, the majority of admitted international students have possessed less than beginner level Japanese language proficiency at the time of enrolment. Notably, although international students have been accepted at university medical schools in Japan in the past, most of them have had high levels of Japanese language proficiency at the time of admission.
IUHW School of Medicine’s admission policy is as follows:
“Students must have achieved outstanding grades, outstanding English capability, a future-oriented and global outlook, and be strongly resolved to contribute to the development of the fields of health, medicine, and welfare in both their home country and the global community, in response to medical needs in Japan and overseas.”
This policy of accepting international students with limited Japanese proficiency is to facilitate the acceptance of outstanding students from Asia regardless of their Japanese ability and thus train them to become international medical doctors.
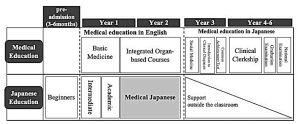
Figure 1. Medical Education Curriculum (top row) and Japanese Education Curriculum (bottom row) at International University of Health and Welfare School of Medicine, Japan
Figure 1 presents a simplified version of the curriculum of IUHW School of Medicine as well as the Japanese language education curriculum. At IUHW, medical education is carried out in English during the first two years of the six-year curriculum. International students come to Japan three to six months prior to entering medical school and attend several intensive pre-admission Japanese language courses. It is a condition of admission that students must acquire a beginner’s level of general Japanese before entering medical school. After enrolment, international students learn medicine together with Japanese students in English, while simultaneously continuing to learn Japanese. From the third year onwards, they learn medicine in Japanese and take the Common Achievement Tests (CAT) in Japanese; these comprise computer-based testing (CBT) for medical knowledge and an objective structured clinical examination (OSCE) on clinical skills. Both components are national tests that determine progression to the following year of study. All medical students in Japan must pass the CAT to proceed to a clinical clerkship. Essentially, passing the CAT is the prerequisite for passing the National Medical Licensure Examination, required to practice medicine as a physician in Japan.
To date, medical Japanese has rarely been research on the efficiency and methods of teaching medical Japanese to foreign students is rare due to the relatively small number of international medical students and foreign doctors in Japan. However, in recent years, research has revealed that medical Japanese is a distinct language that includes grammar and expressions that differ from general Japanese, with 80% of the vocabulary not covered in general Japanese language education curricula (Yamamoto et al., 2018).
Considering the precedents of other countries mentioned above, the Japanese language is not an exception for international medical students in Japan. However, if only general Japanese language classes are conducted, students will not only fail to acquire the knowledge and operational skills of medical Japanese but will be furthermore unable to acquire and retain the vast quantities of medical terminology they will encounter. As such, the IUHW School of Medicine has developed its own course in medical Japanese.
This study aims to describe the Japanese language education program for international students at the IUHW School of Medicine, with particular focus on the development of the “medical Japanese” course and its content. It is hoped that this paper will contribute to the development of educational curriculums for international medical students especially those from Asian countries who plan to study medicine in a second or third language.
II. SCOPE AND BACKGROUND INFORMATION
IUHW School of Medicine’s international students are currently, from Vietnam, Myanmar, Cambodia, Indonesia, Laos, Malaysia, Mongolia, Korea, China, and the United States (As of 2020). Most are from Southeast Asian countries, and, as noted, they arrive in Japan three to six months before beginning formal medical study with little or no Japanese language skills. At the IUHW School of Medicine, they begin learning Japanese from the “Hiragana”, a sort of Japanese language alphabet similar to the ABCs of English. After completing the beginner level course, they begin the formal study of medicine, and they will continue studying Japanese along with medicine in all years of study. The first and second semesters of the first year are dedicated to intermediate level study and the third term of the first year to the third term of the second year, they learn medical Japanese.
The objectives of the medical Japanese course are facilitating students’ acquisition of medical language through various listening, speaking, reading, and writing activities, reinforcing such acquisition, and developing their ability to deliver presentations in Japanese based on medical knowledge acquired in English. It was designed to provide content-based instruction (Grabe & Stoller, 1997) and was developed using various approaches to second language acquisition, such as collaborative learning and output-based activities.
Adult learning theory is the theoretical background for the development of this course. “A need to know” is an important element of adult learning theory. As students aim to become physicians in Japan, they often feel a strong need to acquire Japanese language skills and academic proficiency in Japanese. Particularly, since they know they will be studying medicine in Japanese from their third year on, they feel they must acquire medical Japanese before that time. As such, using medical content for Japanese language learning can satisfy this need and assist them in maintaining their internal motivation to learn. This leads us to “motivation to learn,” another important element of adult learning theory.
Adult learning theory focuses on self-directed learning involving the teaching of adults to be in control of their learning. Since students study medicine in English daily during their first two years of medical education, synchronising medical content with Japanese medical language learning facilitates their learning of medical terms, expressions, and phrases in Japanese using their existing knowledge. As they transit to studying medicine in Japanese from the third year onwards, international students become more autonomous inside and outside the classroom. Moreover, they work together with their Japanese classmates to utilise their content knowledge from the first two years to promote efficient acquisition of Japanese medical terms. From their third year of medical education onwards, since no additional formal Japanese language instruction is offered, international students are expected to primarily act as autonomous learners.
At the IUHW School of Medicine, from the third term in the first year to the end of the second year, the following 13 Integrated Organ-based Courses are provided: the Cardiovascular System, the Respiratory System, the Digestive System, the Endocrine System, the Renal System including Urology, the Gynecological System including the Mammary Gland, the Motor and Dermatological System including Connective Tissue, the Neurological System including Psychiatry, the Sensory Organ System, the Hematological System, Development and Abnormalities from Foetus to Child, Infectious Diseases, and Oncology including Radiotherapy and Palliative Care.
In the medical Japanese course, the units are aligned with the abovementioned specialties (see Figure 2). Group presentations are delivered on specific themes within those specialties. The composition of one unit is presented in Table 1. The teacher (hereafter “medical teacher”) of each organ-system subject selects four themes for each unit. For each theme, the key points to be learned in the second year are stipulated. For example, the Cardiovascular System medical teacher presents the key points, including pathology, epidemiology, diagnosis, treatment, and prognoses for various diseases (themes) such as hypertension, acute myocardial infarction, atrial fibrillation, and aortic stenosis.
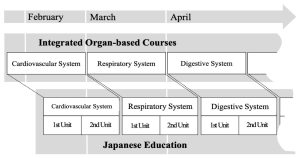
Figure 2. Linkage with Specialties
|
Time period |
Contents |
Details of Activities |
|
1 |
Vocabulary and contents learning |
Learning the vocabulary and contents of the theme using textbook. |
|
2 |
Presentation preparation |
Making the slides and the script |
|
3 |
Presentation rehearsal |
Check the slides and the script |
|
4 |
Presentation 1 |
・Presentation of the two groups ・Q&A session ・Plenary formative feedback session |
|
5 |
Presentation 2 |
・Presentation of the two groups ・Q&A session ・Plenary formative feedback session |
|
6 |
Presentation feedback |
・Individual feedback ・Overall general feedback ・Mini-reports |
|
7 |
Reading comprehension |
Reading the computer-based testing (CBT) workbook |
Table 1. Composition of One Unit
III. EDUCATIONAL STRATEGIES AND THEIR APPLICATIONS
We constructed the course based on educational strategies such as, synchronised medical contents and Japanese terms, small group discussion, and extensive reading, as detailed below.
A. Synchronisation of Both Medical and Japanese Contents
We intentionally synchronise the medical content and Japanese medical vocabulary to promote contextual learning for our students. The first hour of the session is preparatory time where the vocabulary and contents related to the particular theme. During this time, the vocabulary and expressions that are essential to the presentation are self-learned, after which class activities are carried out to reinforce understanding and apply content knowledge. As for the class activities, we conduct a variety of quizzes using interactive applications, such as Kahoot™ and Quizlet™. The Japanese language has three different sets of characters used in writing, and thus some medical terms are not easy for students to read. We use these interactive quiz applications to check for ability to read and comprehend each medical term.
B. Collaborative Learning
To promote deeper learning, group work for collaborative learning has been implemented.
In the second hour, students are divided into four groups, and presentation preparation is conducted. When the group leader initiates a review of the first session, the content of the theme is reconfirmed, along with the flow of the presentation and how the presentation frames should be distributed among the teammates.
Subsequently, students prepare the slides and presentation scripts individually, and then check with each other.
C. Japanese Output of Medical Content Learned in English
In the third hour, a rehearsal of the presentation is conducted, and two Japanese teachers listen to two group presentations (each 30 minutes per group). They write down any noteworthy points on a whiteboard and provide their feedback. They also check the slides for mistaken “Kanji” (Chinese characters in Japanese written format), for missing source references and pronunciation errors.
D. Practical Output through Making/Giving a Presentation, and Discussion with Medical Experts
In the fourth and fifth hours, presentations are made. In each hour, two groups deliver 15-minute presentations, each of which is followed by a 10-minute question and answer (Q&A) session and a 5-minute plenary formative feedback session. The medical teachers who teach the covered content in English listen to the presentations, answer questions, provide supplementary explanations, and correct students’ presentation as needed. The medical teachers use various categories to assess the presentations, such as the overall structure and appropriate application of medical knowledge. Simultaneously, the Japanese teachers assess the presentations for grammar and pronunciation.
E. Detailed Language Feedback by Language Experts
In the sixth hour, students will be given two types of feedback for the presentation: “individual feedback” and “feedback to everybody“. For the “individual feedback”, the students individually review their video-recorded presentations, based on a “presentation feedback sheet” created by the Japanese teachers. More specifically, this sheet includes comments about any pronunciation/expression errors made by the students. During “feedback to everybody”, the Japanese teacher explain and describe the Japanese expressions used by the students in the presentations and used by the medical teachers in the plenary formative feedback session, and the students further reflect on their Japanese.
F. Reinforcing the Vocabulary Knowledge by Writing
After receiving this feedback, the students write a mini-report. They are asked to summarise the contents of their presentations in a report, which is then reviewed by a Japanese teacher who corrects it and gives individual feedback later. It is generally desirable to learn specialised terms in the context of specialised subjects. It is also important to be exposed to the same words multiple times to acquire and retain vocabulary. By writing the summary related to the presentation contents, the students are given the opportunity to come into contact with medical terms multiple times.
G. Building Up Vocabulary and Expression with Relevant Content
In the seventh hour, extensive reading is conducted. Materials include the questions and commentaries for the 8–10 questions related to the presentation themes; these are selected by the medical teachers for each organ-system subject from a commercially available computer-based testing (CBT) workbook (Question Bank CBT, MEDIC MEDIA Co., Ltd.). It is important to note that the objective is not to answer comprehension questions but rather to understand the characteristic medical expressions, reinforce that understanding, and build vocabulary. Furthermore, the purpose is to familiarise the students with the question format in anticipation of the CBT examination they will undertake in their third year.
IV. DISCUSSION
This paper described the development of a medical Japanese course at the IUHW School of Medicine aiming to foster international students’ mastery of medical Japanese through various listening, speaking, reading, and writing activities.
Our observations suggest that IUHW School of Medicine’s international students have been able to continue their medical education in Japanese smoothly. The course assessment is based on the following two points: a vocabulary test for each Integrated Organ-based Course, and a rubric assessment by medical teachers and Japanese teachers at the time of presentation. In addition, we conducted questionnaires and interviews every end-of-semester with students. From the questionnaires, we could see that the students feel that this course will surely be useful for the medical school classes given in Japanese after the third year. The following compilation of comments from the interviews are illustrative: “I was able to reconstruct the fragmented knowledge in my mind by presenting in Japanese in this class what I learned in other medical courses in English.” “Since this class was synchronised with the medical courses, I was not only interested in giving my own presentation, but also in listening to other groups’ presentations.” “There were things that I did not understand in the medical courses that I was able to understand after listening to the presentations in this class.”
These results indicate that the Japanese medical course promotes students simultaneous learning of language forms (vocabulary, grammar, etc.) and medical content.
V. CONCLUSION
The content-based instructional design of our Japanese medical language course applies second language acquisition strategies simultaneously with adult learning theories such as contextual learning and collaborative learning. It is a teaching format for learning medical knowledge through the medium of English, and simultaneously learning another language other than English. In this case, the method was applied to Japanese language acquisition, specifically Japanese medical language acquisition. The method also offers scaffolding for international students to prepare them to continue their medical learning in Japanese on their own after the course. Having observed the Japanese language course over the three years since its implementation, we speculate that this method is applicable not only to the study of Japanese but also to the study in other Asian languages such as Korean and Chinese.
Notes on Contributors
NS reviewed the literature, designed the study and wrote the manuscript. TI advised the design of the study, gave critical feedback to the writing of the manuscript. HG gave scientific insight and advice, critically reviewed and edited the manuscript. HA, MY and YK have read and approved the final manuscript.
Acknowledgement
The authors wish to express sincere appreciation to Ahmed E. Hegab, Yuko Shiima, and Florescu M. Cosmin, International University of Health and Welfare, Medical School, for their constructive discussions and feedback during the preparation of this manuscript.
Funding
There is no funding for this paper.
Declaration of Interest
None of the authors have any competing interests.
References
Grabe, W., & Stoller, F. L. (1997). Content-Based Instruction: Research Foundations. https://carla.umn.edu/cobaltt/modules/principles/grabe_stoller1997/foundation.pdf (Accessed 7 April 2021).
Huhn, D., Al Halabi, K., Alhalabi, O., Armstrong, C., Castell Morley, A., Herzong, W., & Nikendei, C. (2018). Interactive peer-guided examination preparation course for second-year international full-time medical students: Quantitative and qualitative evaluation. GMS Journal for Medical Education, 35(5). https://doi.org/10.3205%2Fzma001203
Michalski, K., Farhan, N., Motschall, E., Vach, W., & Boeker, M. (2017). Dealing with foreign cultural paradigms: A systematic review on intercultural challenges of international medical graduates. PLOS ONE, 12(7), e0181330. https://doi.org/10.1371/journal.pone.0181330
Yamamoto, K., Inada, T., & Shinagawa, N. (2018). Ishikokkashikenno meishigoino taisuuyuudohini motozuku bunsekito kyoozaikaihatuno kanousei [Log-likelihood Analysis of Nouns in the National Examination for Medical Practitioners and the Development of Teaching Materials for International Medical Students]. Nihongo / Nihongo kyouiku. [Japanese/Japanese Education], (9), 245-260.
Zhang, J., Cheng, M., Guo, N., Xing, A., & Xu, L. (2019). ‘Standardized patients’ in teaching the communication skill of history-taking to four-year foreign medical undergraduates in the department of obstetrics and gynaecology. BMC Medical Education, 19(108). https://doi.org/10.1186/s12909-019-1541-y
*Nagisa Shinagawa
International University of Health and Welfare,
4-3 Kouzunomori, Narita,
Chiba 286-8686 Japan
Tel: +81-476-20-7701
Email: sinagawa@iuhw.ac.jp
Published online: 4 January, TAPS 2022, 7(1), 1-2
https://doi.org/10.29060/TAPS.2022-7-1/EV7N1
The practice of medicine has been rooted strongly in traditions. Discipline-based academies, colleges, societies, and associations regularly practice “rituals” based on context-specific traditional norms and cultural practices. Medical education and training are no different. Being part of a larger, higher education institution and preparing graduates for a future profession, they too have deeply embedded rituals such as the whitecoat ceremony, the silent mentor appreciations, oath taking, and the commencement. These practices have a strong influence of the institutions in which the programs are conducted giving each of these practices not only the professional but the context and institution specific angle and colours.
It is important to explore further why the traditions and heritage are important elements in training a future healthcare professional. The practice of medicine is intertwined with people’s values, beliefs, and culture. Patients and their families’ understanding of health and illness, their illness management and treatment preferences are all significantly impacted by the society they live in, and their cultural practices and traditions. The eastern cultures belief that some foods are heaty, plain or that some others are cold, therefore either good or bad for certain illnesses, stem from the ancient eastern philosophy of “Ying and Yang”. (Xie et al., 2020). This can have a direct effect on illness and care outcomes. (Kindig et al., 2004; Petri et al., 2015). This has to be incorporated into medical training early in the curriculum, to highlight its significance to the students and trainees.
Another area where the institutional and professional traditions and heritage play a part is in the development of professional identity of the learner (Wahid et al., 2021). This is critical in medicine to develop a sense of belonging to their future profession and to the institution from a very early stage of the student or trainee program. This will enable them to understand that they are part of an institution and a profession that strive to alleviate human suffering and improve lives. This will enable them to be resilient and develop their grit to successfully face the rigours of their challenging profession in the future. (Samarasekera & Gwee, 2021). This is important in the present context where, due to the pandemic, we are seeing an unprecedent number of doctors and other healthcare professionals leaving the profession or getting burnout, leading to a severe negative impact on providing quality care to our patients and communities (Kisa, 2020).
Another interesting aspect is how these context-specific cultural practices, norms, and traditions impact one’s development and conceptualization of patient empathy. There is evidence that students in medical programs from different localities show differences in the development of empathy (Ponnamperuma et al., 2019).
As professionals, when we engage with fellow colleagues, in public or during patientcare, we exhibit our learnings from role models and our cultural beliefs and practices that are deeply rooted in the institutional heritage. This is the reason why those activities during educating and training the future healthcare workforce become important in shaping the next generations of doctors and healthcare professionals. It is difficult to practise medicine and provide healthcare efficiently and effectively without having a good understanding of the traditions and cultural practices of the institution in which they trained and the profession to which they belong as well as the communities they care for. In all systems of healthcare practice, the place of training and the practice settings become important for the new practitioners to enhance their skills (Buckley et al., 2010). Therefore, it is important for the healthcare training institutions to place much emphasis on incorporating core values rooted in the institutional traditions. This could be an ideal platform to build new cultural norms and practices aligned to the 21st century society and clinical practice. Whether we are conscious of it or not, our beliefs, values and traditions shape the way we behave and practice. It forms the practice culture of our graduates and determine the quality of care. Therefore, providing a good foundation of cultural understanding will assist the future practitioner to embrace the challenges they may face in a rapidly changing, dynamic clinical practice without losing the notion of one’s identity, self-worth, or getting burnout in providing care. Furthermore, the training institutions could use examples from their rich traditions and heritage to imbibe a strong sense of servant leadership, an excellent service culture as well as to develop learner and, subsequently, practitioner grit. These measures will help improve efficiency and quality healthcare.
Dujeepa D. Samarasekera & Matthew C. E. Gwee
Centre for Medical Education (CenMED), NUS Yong Loo Lin School of Medicine,
National University Health System, Singapore
Buckley, J. D., Joyce, B., Garcia, A. J., Jordan, J., & Scher, E. (2010). Linking residency training effectiveness to clinical outcomes: A quality improvement approach. The Joint Commission Journal on Quality and Patient Safety, 36(5), 203-208. https://doi.org/10.1016/s1553-7250(10)36033-8
Kindig, D. A., Panzer, A. M., & Nielsen-Bohlman, L. (Eds.). (2004). Health literacy: A prescription to end confusion. National Academies Press.
Kisa, S. (2020). Burnout among physicians and nurses during COVID-19 pandemic. European Journal of Environment and Public Health, 4(2), Article em0055. https://doi.org/10.29333/ejeph/8447
Petri, R. P., Jr., Delgado, R. E., & McConnell, K. (2015). Historical and cultural perspectives on integrative medicine. Medical Acupuncture, 27(5), 309-317. https://doi.org/10.1089/acu.2015.1120
Ponnamperuma, G., Yeo, S. P., & Samarasekera, D. D. (2019). Is empathy change in medical school geo‐socioculturally influenced? Medical Education, 53(7), 655-665. https://doi.org/10.1111/medu.13819
Samarasekera, D. D., & Gwee, M. C. E. (2021). Adapting to change during challenging times. The Asia Pacific Scholar, 6(1), 1-2. https://doi.org/10.29060/TAPS.2021-6-1/EV6N1
Wahid, M. H., Findyartini, A., Soemantri, D., Mustika, R., Felaza, E., Steinert, Y., Samarasekera, D. D., Greviana, N., Hidayah, R. N., Khoiriyah, U., & Soeselo, D. A. (2021). Professional identity formation of medical teachers in a non-Western setting. Medical Teacher, 43(8), 868-873. https://doi.org/10.1080/0142159X.2021.1922657
Xie, A., Huang, H., & Kong, F. (2020). Relationship between food composition and its cold/hot properties: A statistical study. Journal of Agriculture and Food Research, 2, Article 100043. https://doi.org/10.1016/j.jafr.2020.100043
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









