Remote physiology practical: Viable alternative to in-person practical in health sciences education?
Submitted: 7 December 2021
Accepted: 8 February 2022
Published online: 5 April, TAPS 2022, 7(2), 27-36
https://doi.org/10.29060/TAPS.2022-7-2/OA2718
Tan Charmaine1 & Ivan Cherh Chiet Low1,2
1Department of Physiology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Human Potential Translational Research Programme, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Practicals are core components of an undergraduate health sciences curriculum to promote experiential learning and motivation in students. With restrictions on traditional forms of face-to-face practicals during the COVID-19 pandemic, we designed and investigated the efficacy of remote practicals as a viable learning strategy in exercise physiology teaching.
Methods: Student volunteers were instructed to perform a graded exercise test in a remote setting and provide their collected data for subsequent discussion in an online lecture. The effectiveness of this remote practical in promoting students’ motivation and learning outcomes achievement was assessed via an anonymous questionnaire containing 29 closed-ended and 2 open-ended items. Continual Assessment (CA) results were also investigated. Unpaired student’s t-tests were performed for comparisons between interventions with significance level set at P<0.05.
Results: Sixty-one (out of 81; 75%) students responded to the questionnaires and 49 (60%) consented to the use of their CA results for this study. Results revealed that students were moderately motivated and attained strong achievement of learning outcomes. When compared to students who did not volunteer for the hands-on component of the remote practical, students who participated in the hands-on component reported significantly higher self-efficacy (P<0.05) in explaining the practical procedures to their peers. Qualitative analysis further revealed that experiential learning and real-life data analysis were the central reasons supporting the effectiveness of the remote practical. Students were generally satisfied and would recommend the remote practical to future students.
Conclusion: Our study highlights the potential of remote practicals as viable alternatives to traditional practicals.
Keywords: Remote Practical, Experiential Learning, Student Motivation, Learning Outcomes
Practice Highlights
- Remote practical aids in promoting experiential learning in exercise physiology teaching.
- Remote practical can promote motivation by enabling students to see the relevance of their learning.
- Students perceived that they could achieve the necessary learning outcomes via remote practicals.
I. INTRODUCTION
Laboratory work or practical classes are considered as core components of health sciences curriculum in higher education (Colthorpe & Ainscough, 2021; Dohn et al., 2016; Hofstein & Lunetta, 2004). Past studies have revealed the strong educational value of practical classes in promoting student motivation (Bruce, 1988; Dohn et al., 2016), student learning outcomes achievement (Brinson, 2015) as well as the ability to draw theory to practical applications (Neves et al., 2017).
One of the key subjects in undergraduate health sciences education is human physiology, a discipline seeking to understand the underlying mechanisms and dynamics of the human body (Lellis-Santos & Abdulkader, 2020). The role of practical classes in the teaching and learning of physiology is highly valued by educators and students alike (Dohn et al., 2016; Neves et al., 2017). Experiential learning in physiology practicals commonly takes the form of interactive hands-on activities, real-time data collection and analysis of physiological responses. When such practicals are carried out in a traditional face-to-face manner, students are able to utilise laboratory equipment in an authentic experimental setting and generate real-time data from their peers and/or themselves (Colthorpe & Ainscough, 2021). Data analysis and discussion following the hands-on component of practicals can further promote contextualised learning and facilitate the understanding of the theoretical content (Lewis & Williams, 1994). It has been reported that such an interactive learning approach in physiology enhances the achievement of learning outcomes and increases the level of motivation for students (Dohn et al., 2016).
The emergence of the COVID-19 pandemic has led to increasing safety management restrictions being imposed on physical classes in higher education institutes around the world (Ali, 2020). As such, educators were faced with the sudden need to switch from face-to-face lessons to online and remote teaching (Ali, 2020; Lellis-Santos & Abdulkader, 2020). Amidst the uncertainty of this transition, traditional face-to-face practicals have seen a sharp decline (Ray & Srivastava, 2020; Vasiliadou, 2020). As we examine these educational trends during crises, it becomes apparent that harnessing creativity to adapt and invent novel solutions is vital to maintain and even advance current standards of teaching and learning. Lellis-Santos and Abdulkader (2020) rightfully exemplify this notion by proposing the use of smartphone applications as a creative teaching approach to enable scientific data collection and practical learning from home even during social isolation. Along similar lines, we have designed a remote practical for students to carry out hands-on experiments outside of a traditional laboratory environment as an innovative alternative to circumvent the restrictions on face-to-face practicals and to provide them with experiential learning opportunities on cardiovascular concepts in exercise physiology.
To the best of our knowledge, there are few studies conducted to date regarding the efficacy of such remote practicals, particularly in the field of life sciences and exercise physiology. Therefore, our study aims to address this research gap by evaluating the effectiveness of our remote exercise physiology practical on (1) student learning outcomes, (2) student motivation and (3) students’ perceptions on the effectiveness and relevance of the remote practical. In addition, we also compared the quantitative and qualitative responses between students who participated and did not participate in the hands-on component of the remote practical. The Continual Assessment (CA) results from these two groups of students were also compared to assess if differences in academic performance existed between the two groups.
II. METHODS
A. Description of the Module
LSM3212 Human Physiology: Cardiopulmonary System is a third-year module in Life Sciences conducted by the Department of Physiology, Yong Loo Lin School of Medicine at the National University of Singapore. A total of 81 undergraduate Life Sciences students were enrolled in the module in the Academic Year 2020/2021, Semester 2. Traditionally, both lectures and practicals are carried out in a face-to-face manner for this module. However, due to restrictions imposed by the COVID-19 pandemic, lessons were forced to go online. As a result, a remote practical was designed and conducted as an innovative alternative for this batch of students.
B. Description of the Remote Practical
The remote practical was designed to provide students with experiential learning on cardiovascular concepts in exercise physiology. Conventionally, the practical involved a treadmill-based graded exercise test performed by a student volunteer equipped with specialised electrocardiogram-based heart rate monitors to illustrate how the cardiovascular system changes with increasing exercise stress. For the remote practical, however, students were given a set of practical handouts comprising a novel graded exercise protocol developed by the authors and could choose to perform it in their own time asynchronously, or not carry it out at all. In the graded exercise protocol, students were instructed to carry out a series of graded knee raise exercises and record their heart rate measured via a smartphone application together with other subjective exercise prescription ratings (ratings of perceived exertion and talk test ratings) after each set of exercise. The graded exercise protocol was developed with the intent to encourage contextualised learning from the practical content to real-life exercise routines. The consolidated data was subsequently used for discussion in a virtual lecture to illustrate how heart rate responses and cardiovascular adaptations may differ across individuals, as well as how the consolidated data may serve to guide exercise prescription. Participation in the hands-on component (knee raise exercises) of the remote practical was optional. However, participation in the analysis and discussion of the collated data in the virtual lecture conducted after the graded exercise was made compulsory. Via this design, the remote practical (comprising both the graded exercise and post-exercise discussion) not only replicated the pedagogy of the original in-class practical, but also augmented the opportunity for students to volunteer and take part in the graded exercise component of the practical.
C. Instruments
After the virtual lecture, students completed an anonymous (no informed consent required) questionnaire containing 29 closed-ended and 2 open-ended items. The purpose of this self-report questionnaire was to evaluate students’ perceived effectiveness of the remote practical on their motivation and achievement of learning outcomes of the virtual lecture.
Student motivation was measured by the Lab Motivation Scale (Dohn et al., 2016) containing 21 closed-ended statements based on three aspects – student interest, effort and self-efficacy. Multiple instruments had previously been employed to assess dimensionality and reliability of the validated Lab Motivation Scale (Dohn et al., 2016). A set of six closed-ended items were employed to measure students’ perception on whether they had achieved the intended learning outcomes of the remote practical. Lastly, two closed-ended items were included to elicit a general satisfaction score from students regarding the remote practical and/or the virtual lecture. All the closed-ended statements in the questionnaire were scored on a 5-point Likert Scale, ranging from 5 (strongly agree) to 1 (strongly disagree).
Furthermore, there were two open-ended questions focusing on the effectiveness of the remote practical and the relevance of the remote practical to students’ daily lives. The first question was posed to uncover specific reasons supporting the analysis of the closed-ended items, while the second question aimed to encourage contextualisation of concepts learnt through the remote practical in students’ daily lives.
Finally, the CA results of students who participated in the hands-on component of the remote practical were compared with students who did not participate. To ensure a fair comparison, we took into consideration only the CA result from the questions corresponding to the content covered in the remote practical and virtual lecture. The questions taken into consideration made up 40% of the entire examination score.
D. Analysis
A mixed method approach was employed in analysing the questionnaire responses. An initial 66 questionnaire responses were collected but five incomplete responses were excluded, leaving a total of 61 responses that were included in the final analysis. Responses to the closed-ended items were coded accordingly to a 5-point Likert scale, ranging from strongly agree (5) to strongly disagree (1). Scores were reversed for statements phrased in a negative manner (items 9, 15 and 18). All closed-ended responses were presented in the form of mean ± standard deviation. As a measure of internal consistency, Cronbach’s α was used as an instrument and measured across all scales. Unpaired student’s t-tests were carried out to find out if differences between students who participated and did not participate in the hands-on exercise component were significant with significance level set at P < 0.05. All data analysis and statistical tests were performed using Microsoft Excel 2016.
Open-ended responses were analysed in a 3-part process: informal reviewing, open coding and thematic analysis. Firstly, all responses were informally reviewed to familiarise with general ideas and main themes were identified. Next, open coding was performed where each response was analysed in detail and coded to the most appropriate theme (Braun & Clarke, 2006). Finally, thematic analysis was carried out through ranking themes according to frequency and analysing the results (Braun & Clarke, 2006). The open-ended questions were made optional, and all responses collected were subsequently analysed.
III. RESULTS
Out of the 61 participants, 29 (48%) participated in the hands-on exercise component of the remote practical while 32 (52%) did not participate. Both groups attended the compulsory virtual lecture conducted after the remote practical, where the data collected from the remote practical was consolidated and discussed with the entire class.
Internal consistency was calculated using Cronbach’s α and the reliability coefficient was found to be 0.95 across all closed-ended items, indicating an excellent level of interrelatedness across the overall scale (Cronbach, 1951). Individual scales of learning outcomes and motivation were also subjected to the analyses of Cronbach’s α. The alpha coefficient value was calculated to be 0.86 for perceived achievement of learning outcomes and 0.94 for motivation (Tables 1 & 2). Motivation was further divided into three individual subscales assessing student interest, effort and self-efficacy, with the reliability coefficients returning 0.85, 0.88 and 0.88 respectively (Table 1). These reliability coefficients correlate strongly with those of Dohn et al. (2016), hence providing support for the internal consistency of the Lab Motivation Scale. Data supporting these findings is openly available via Figshare at https://doi.org/10.6084/m9. figshare. 17170 964 (Low, 2021).
A. Remote Practical and Learning Outcomes
In general, students rated between “Agree” and “Strongly Agree” for perceived achievement of learning outcomes, with an overall mean score of 4.16 ± 0.68 on a 5-point Likert scale (Table 1). Students who participated in the hands-on component reported a mean score of 4.20 ± 0.54, which was similar to that rated by students who did not participate in the hands-on component (4.13 ± 0.68, P = 0.567; Table 1). For the first closed-ended statement: I have gained a stronger understanding of how heart rate responds to increasing exercise intensity, students who participated indicated a higher mean score of 4.52 ± 0.51 as compared to the lower mean score of 4.09 ± 0.59 (P = 0.004) for students who did not participate in the hands-on exercise component (Table 1).
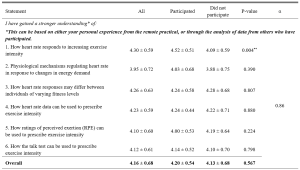
Table 1. Students’ perceived achievement of learning outcomes in cardiovascular physiology
n = 61. Responses were coded from 1 (Strongly Disagree) to 5 (Strongly Agree). All means are shown with ±SD of the mean. **P < 0.01.
B. Remote Practical and Student Motivation
Students generally rated between “Agree” and “Somewhat Agree/Somewhat Disagree” for student motivation, with an overall mean score of 3.66 ± 0.71 (Table 2). Students who participated in the hands-on component reported a mean score of 3.70 ± 0.64, which was similar to that rated by students who did not participate in the hands-on component (3.62 ± 0.78, P = 0.187; Table 2). Students rated between “Agree” and “Somewhat Agree/Somewhat Disagree” regarding the three aspects of student motivation, with a score of 3.92 ± 0.69 for interest, 3.66 ± 0.75 for effort and 3.50 ± 0.68 for self-efficacy respectively (Table 2). For statement 23, students who participated indicated a higher mean score of 3.68 ± 0.61 as compared to the lower mean score of 3.29 ± 0.71 (P = 0.031) for students who did not participate in the hands-on component (Table 2).
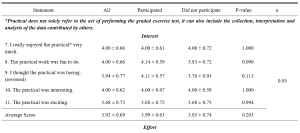
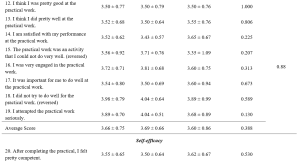
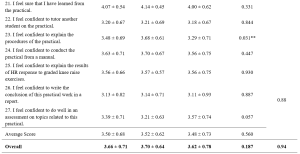
Table 2. Students’ perceived motivation towards the remote practical
n = 61. Adapted from the Lab Motivation Scale (Dohn et al., 2016). Responses were coded from 1 (Strongly Disagree) to 5 (Strongly Agree). Scores were reversed for statements phrased in a negative manner. All means are shown with ± SD of the mean. **P < 0.05.
C. Qualitative Explanations on Perceived Effectiveness and Relevance of Remote Practical
The first open-ended item sought to investigate the reasons underlying the perceived effectiveness or ineffectiveness of the remote practical in enhancing students’ learning. Of the 37 responses, 34 (92%) felt that the remote practical was effective while 3 (8%) felt it was ineffective and of little to no added value to them (Table 3). Experiential learning and real-life data emerged as the most common themes cited across all responses (n = 12), followed by reinforc(ing) concepts taught in lecture (n = 10; Table 3). Experiential learning was reflected as the most common response among students who participated in the hands-on component (n = 10) in comparison to real-life data indicated by students who did not participate in the hands-on component (n = 8; Table 3).
The aim of the second open-ended item was to investigate the relevance and application of the remote practical to students’ daily lives. Of the 36 responses, 29 (81%) felt the remote practical was relevant while 7 (19%) felt that it was irrelevant to their daily lives (Table 3). Overall, the remote practical was found to be most relevant in improving current exercise routine (n = 12), followed by understanding one’s own fitness level (n = 10) and understanding the importance of exercise (n = 7; Table 3). This trend was similar for both students who participated and did not participate in the hands-on component of the remote practical (Table 3).
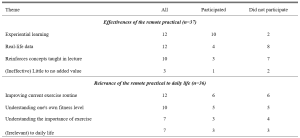
Table 3. Themes identified from the open-ended responses, ranked by frequency
D. Remote Practical and Satisfaction Score
Students rated close to “Agree” for satisfaction, with an overall mean score of 3.95 ± 0.75 (Table 4). Those who participated in the hands-on component reported a mean score of 4.11 ± 0.70, which was similar to that rated by students who did not participate in the hands-on component (3.81 ± 0.77, P = 0.054; Table 4).
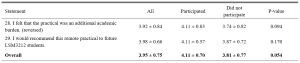
Table 4. Students’ satisfaction score
n = 61. Responses were coded from 1 (Strongly Disagree) to 5 (Strongly Agree). All means are shown with ± SD of the mean. **P < 0.05.
E. Remote Practical and Academic Performance
Out of the 49 students who consented to the use of their CA results for this research study, 30 (61%) participated in the hands-on component of the remote practical while 19 (39%) did not (Table 5). Only the questions corresponding to the content covered in the remote practical and relevant virtual lecture were taken into consideration for this study. The overall mean mark was 7.3 ± 1.64 out of 10 (Table 5). Students who participated in the hands-on component (7.3 ± 1.84) and did not participate in the hands-on component (7.3 ± 1.32) exhibited similar mean marks as well (P = 0.940; Table 5).

Table 5. Students’ CA results
n = 49. CA scores are shown as mean ± SD, with *P < 0.05 considered significant.
IV. DISCUSSION
This study sought to evaluate if remote physiology practicals could be viable alternatives to traditional face-to-face practicals, especially during emergency remote teaching in a pandemic. Our results demonstrated that the students who participated in the remote practical perceived that they could achieve the learning outcomes in cardiovascular and exercise physiology teaching with reasonable satisfaction, regardless of whether they participated in the hands-on component of the remote practical. However, students who had actively participated in the hands-on component (graded exercise) reported that the remote practical had particularly benefitted them in better achieving certain learning outcomes as compared to their classmates who did not participate in the graded exercise. Specifically, students indicated that their participation in the graded exercise allowed them to have a better grasp of the concepts concerning heart rate response to increasing exercise intensity. This finding was not unexpected as the remote graded exercise was specifically designed to provide experiential learning opportunities to better comprehend the concepts underlying this particular learning outcome.
Perceived scores for the achievement of learning outcomes were otherwise similar between the participated and non-participated group. This could be attributed to the fact that the remote practical was used as a complement to the virtual lecture, wherein the interpretation and analysis of data collected from the optional graded exercise was discussed with the whole class during the compulsory virtual lecture. The perception scores of learning outcome achievement were well supported by the students’ academic performance as all of them shared similar mean CA marks regardless of their participation in the remote practical. This similarity is especially prominent as the CA questions were set based on the principle of constructive alignment (Biggs, 1996; Bloom, 1956; Stamov Roßnagel et al., 2020).
Interestingly, open-ended responses revealed “experiential learning” as the key reason supporting the efficacy of the remote practical in students who participated in the graded exercise while “having real-life data which reinforces concepts taught in lecture” were key reasons indicated by students who did not participate in the hands-on component of the remote practical. These findings are in line with studies recommending experiential learning as one of the seven “principles of good practice” to achieve excellence in higher education (Chickering & Gamson, 2006). This is accomplished by generating real-life data to allow students to draw the link between theoretical content and practical applications, before applying it to analyse real-life situations in view of course material (Lewis & Williams, 1994). This suggests that the remote practical is able to foster environments which could encourage hands-on learning and real-time data generation to enhance student learning, even if not conducted in a traditional laboratory setting.
Overall, students were satisfied with the remote practical and/or virtual lecture, with those who participated in the hands-on component generally being more satisfied. Even though the remote practical was not compulsory, those who took part in the hands-on component generally did not view it as an additional academic burden and instead would recommend it to future batches of students. This reinforces the potential of such remote practicals in helping students to achieve learning outcomes without imposing unnecessary pressure on them.
With motivation being a strong indicator of self-directed learning and academic achievement (Cortright et al., 2013), it is crucial for educators to assess and understand the importance of motivating students. In fact, educators play a critical role in determining the motivation levels of their students through the nature of their classes and assignments (Cortright et al., 2013). Specifically, Dohn et al. (2016) states that students’ motivation could be negatively impacted by limited equipment or restricted time for practicals. Majority of students face similar limitations for a graded exercise test carried out in a traditional face-to-face practical. Typically, only one volunteer would carry out the actual exercise experimental protocol due to equipment and time constraints, while other students would passively watch and learn from the data collected. The novel remote practical proposed in this study could potentially overcome these limitations as students are able to personally experience the hands-on exercise component within their own spaces at home and at their own convenience, thereby possibly enhancing their motivation levels.
Our results indicated that overall motivation towards the remote practical and/or the virtual lecture ranged from 3 to 5, corresponding to “somewhat agree” and “strongly agree”, with a mean value of 3.62 ± 0.78. This is comparable to the motivation scores previously reported by Dohn et al. (2016) for in-class biomedical laboratory classes. The positive motivation score could be explained by the fact that majority of students (81%) could see the relevance (Table 3) of the remote practical in their daily lives. Learning activities which guide students towards finding ‘personal meaning and value’ in the educational content is known to positively influence their motivation levels (Cortright et al., 2013). By providing opportunities for students to reflect on, find meaning and draw relevance to their personal lives, such remote practicals can potentially address common limitations of traditional practicals and boost student motivation and learning.
Delving further into the three aspects of student motivation – interest, effort and self-efficacy, students rated the highest scores for interest, followed by effort and lastly self-efficacy. The score for effort placed into the practical could have been understandably affected due to the non-compulsory nature of the graded exercise. The exercise component of the practical could not be made compulsory as not all students were medically/physically fit enough to undergo a graded exercise test. Nonetheless, the similarity in perceived learning outcomes and academic results between students who did and did not participate in the graded exercise suggests that the follow up analysis and peer-based discussion of the tabulated data involving the entire class was sufficient to bridge the learning gap between the two groups of students. Overall, the favourable perceived learning outcomes (ranging from “agree” to “strongly agree”) and academic scores (corresponding to a grade of “A-” to “A”) reinforces the value of the remote practical as a teaching strategy to promote learning in exercise physiology, regardless of the students’ ability or interest to participate in strenuous physical activity. However, whether the remote practical is more effective than a conventional face-to-face practical or no practical at all remains an interesting question which necessitates future research as this cannot be addressed given the limitations of our current study design.
Notably, self-efficacy scores were rated the lowest amongst the three aspects of motivation. This could be due to the fact that students are not closely supervised during a remote practical, unlike face-to-face practicals. Without the physical presence and continuous guidance of an instructor, students could have faced uncertainty as to whether instructions were properly executed. Thus, strategies to enhance pre-practical instructions using asynchronous video instructions or the incorporation of remote supervision methods may aid to further enhance the effectiveness of the remote practical. Interestingly, participation in the hands-on component of the remote practical appeared to have nonetheless enhanced the confidence of students in explaining the procedures of the practical to their peers (Table 2). This finding is of particular importance, as the ability to teach and explain is an indication of higher order learning corresponding to the second and third levels of the Bloom’s taxonomy (Bloom, 1956).
A. Limitations
Our study sought to evaluate the effectiveness of a remote exercise physiology practical in promoting student motivation and learning in a cohort of Life Sciences undergraduates. However, the current study design does not permit immediate comparison with conventional face-to-face practicals as students could not be randomly allocated into different comparison groups (remote or face-to-face) owing to pandemic restrictions and ethical reasons. Also, we could only investigate the effects of practical participation on the effectiveness of the remote practical in enhancing student motivation and learning outcomes achievement using a quasi-experimental approach. This is so, for we were unable to randomly allocate students into two comparison groups given that not all students were medically/physically fit enough to undergo a graded exercise test for the hands-on component of the remote practical. Based on this study design, some degree of self-selection bias could have been present as physically active students who had volunteered to take part in the exercise component of the remote practical could have seen greater relevance to their daily lives and could have been more intrinsically motivated to partake and learn from the practical session. In spite of that, the overall student motivation score appeared comparable between the two groups of students who participated and did not participate in the exercise component of the practical, suggesting that the degree of self-selection bias may not be of significant concern in the present study.
V. CONCLUSION
Overall, students reported that experiential learning and real-life data were the main reasons supporting the effectiveness of the remote practical. With experiential learning and real-life data as key components of traditional practicals (Dohn et al., 2016; Randall & Burkholder, 1990), the present study demonstrates the potential of remote practicals as viable and innovative alternatives for face-to-face practicals in exercise physiology teaching. In cases of sudden shifts to emergency remote education, such alternatives offer the possibility of incorporating experiential learning even during social isolation.
Notes on Contributors
Tan conducted the study, analysed and interpreted the data, and drafted the manuscript. I.C.C. Low was involved in experimental conception and design, as well as critically reviewed and revised the manuscript. All authors have read and approved the final version of the manuscript.
Ethical Approval
All students were provided with a participant information sheet containing the purpose and details of the research study. The questionnaire was made completely anonymous. Informed consent was obtained from students for use of their CA results only after the release and confirmation of their results. Circulation of research materials was done virtually and students were never approached directly for recruitment. The study was approved by the National University of Singapore – Institutional Review Board (NUS-IRB) with study code NUS-IRB-2020-631.
Data Availability
Data supporting these findings is openly available via Figshare at DOI: https://doi.org/10.6084/m9.figshare. 17170964.
Acknowledgements
We greatly appreciate the study participants who have spent their time and effort to complete the questionnaires and have provided consent in the use of their results for research purposes.
Funding
There was no funding support accorded for this study.
Declaration of Interest
No potential conflict of interest was reported by the authors.
References
Ali, W. (2020). Online and remote learning in higher education institutes: A necessity in light of COVID-19 pandemic. Higher Education Studies, 10(3), 16-25. https://doi.org/10.5539/hes.v10n3p16
Biggs, J. (1996). Enhancing teaching through constructive alignment. Higher Education, 32(3), 347-364. https://doi.org/10.1007/BF00138871
Bloom, B. S. (1956). Taxonomy of educational objectives. Vol. 1: Cognitive domain. David McKay.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
Brinson, J. R. (2015). Learning outcome achievement in non-traditional (virtual and remote) versus traditional (hands-on) laboratories: A review of the empirical research. Computers & Education, 87, 218-237. https://doi.org/10.1016/j.compedu.2015.07.003
Bruce, R. H. (1988). Enhancing student motivation and learning: Experiences with a simple simulation. Higher Education Research & Development, 7(2), 103-110. https://doi.org/10.1080/0729436880070201
Chickering, A., & Gamson, Z. (2006). Seven principles of good practice in undergraduate education. New Directions for Teaching and Learning, 1991, 63-69. https://doi.org/10.1002/tl.37219914708
Colthorpe, K., & Ainscough, L. (2021). Do-it-yourself physiology labs: Can hands-on laboratory classes be effectively replicated online? Advances in Physiology Education, 45(1), 95-102. https://doi.org/10.1152/advan.00205.2020
Cortright, R. N., Lujan, H. L., Blumberg, A. J., Cox, J. H., & DiCarlo, S. E. (2013). Higher levels of intrinsic motivation are related to higher levels of class performance for male but not female students. Advances in Physiology Education, 37(3), 227-232. https://doi.org/10.1152/advan.00018.2013
Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297-334. https://doi.org/10.1007/BF02310555
Dohn, N. B., Fago, A., Overgaard, J., Madsen, P. T., & Malte, H. (2016). Students’ motivation toward laboratory work in physiology teaching. Advances in Physiology Education, 40(3), 313-318. https://doi.org/10.1152/advan.00029.2016
Hofstein, A., & Lunetta, V. N. (2004). The laboratory in science education: Foundations for the twenty‐first century. Science education, 88(1), 28-54. https://doi.org/10.1002/sce.10106
Lellis-Santos, C., & Abdulkader, F. (2020). Smartphone-assisted experimentation as a didactic strategy to maintain practical lessons in remote education: Alternatives for physiology education during the COVID-19 pandemic. Advances in Physiology Education, 44(4), 579-586. https://doi.org/10.1152/advan.00066.2020
Lewis, L. H., & Williams, C. J. (1994). Experiential learning: Past and present. New Directions for Adult and Continuing Education, 1994(62), 5-16. https://doi.org/10.1002/ace.36719946203
Low, I. C. C. (2021). Remote physiology practical: Viable alternative to in-person practical in health sciences education? [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.17170964
Neves, B. S., Altermann, C., Goncalves, R., Lara, M. V., & Mello-Carpes, P. B. (2017). Home-based vs. laboratory-based practical activities in the learning of human physiology: The perception of students. Advances in Physiology Education, 41(1), 89-93. https://doi.org/10.1152/advan.00018.2016
Randall, W. C., & Burkholder, T. (1990). Hands-on laboratory experience in teaching-learning physiology. Advances in Physiology Education, 259(6), S4-S7. https://doi.org/10.1152/advances.1990.259.6.s4
Ray, S., & Srivastava, S. (2020). Virtualization of science education: A lesson from the COVID-19 pandemic. Journal of proteins and proteomics, 11, 77-80. https://doi.org/10.1007%2Fs42485-020-00038-7
Stamov Roßnagel, C., Fitzallen, N., & Lo Baido, K. (2020). Constructive alignment and the learning experience: Relationships with student motivation and perceived learning demands. Higher Education Research & Development, 40(4), 838-851. https://doi.org/10.1080/07294360.2020.1787956
Vasiliadou, R. (2020). Virtual laboratories during coronavirus (COVID‐19) pandemic. Biochemistry and Molecular Biology Education, 48(5), 482-483. https://doi.org/10.1002/bmb.21407
*Ivan Cherh Chiet LOW
Department of Physiology,
Yong Loo Lin School of Medicine
Block MD9, 2 Medical Drive Level 4
Singapore 117593
Email: phsilcc@nus.edu.sg
Submitted: 6 April 2021
Accepted: 2 December 2021
Published online: 5 April, TAPS 2022, 7(2), 17-26
https://doi.org/10.29060/TAPS.2022-7-2/OA2510
Nicola Ngiam1,2, Kristy X Fu1,3 & Jacqueline SM Ong1,3
1Khoo Teck Puat- National University Children’s Medical Institute, National University Health System, Singapore; 2Centre for Healthcare Simulation, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Personal protection in aerosol-generating procedures is an important skill to safely deliver care to patients in the COVID-19 pandemic. This aim of this study was to evaluate the impact of “just-in-time” simulation training for airway management in a suspected COVID-19 patient.
Methods: This was a prospective mixed-method cohort study in a tertiary paediatric department. A mandatory “just-in-time” simulation training session for intubation of a suspected COVID-19 patient was conducted. Pre- and post-simulation questionnaires were administered. Participants were invited to attend focus group interviews to further delineate their experience. Quantitative and qualitative methods were employed to analyse the data.
Results: Thirty-three participants, including doctors, nurses and respiratory therapists attended the training. Self-confidence in intubation, managing and leading a resuscitation team and dealing with problems with intubation significantly improved. Simulation was valued for the experiential learning as well as for increasing confidence and awareness. Process improvement suggestions from both participants and trainers were raised. There was a small signal of skill translation to real life scenarios.
Conclusion: Simulation-based training is a useful tool for infectious disease outbreak preparedness. Further research will need to be done to determine the impact on actual clinical practice in pandemics.
Keywords: Simulation, COVID-19, Pandemic Preparedness, Training, Intubation
Practice Highlights
- The authors report their experience with “just-in-time” in situ simulation training for emergency preparedness in the face of an infectious disease outbreak.
- Simulation training was well received and improved the confidence as well as awareness of frontline staff in managing intubation and resuscitation in a suspected COVID-19 paediatric patient.
- Process improvement suggestions from participants and trainers was a useful by-product of the simulation training activity.
I. INTRODUCTION
Since the World Health Organization (WHO) declared the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) outbreak a public health emergency of international concern on 30 January 2020 (World Health Organization, 2020), the COVID-19 pandemic has now affected millions of people worldwide, with a wide range of case fatality rates amongst the 210 countries and territories affected (The Centre for Evidence-Based Medicine Nuffield Department of Primary Care Health Sciences University of Oxford, 2020). In Wuhan, China, one of the first epicentres of this international pandemic, out of 44672 confirmed cases of COVID-19, 1716 were healthcare workers (HCWs) (Wu & McGoogan, 2020). Of the confirmed cases among HCWs, 14.6% were classified as severe or critical, and 5 deaths were observed (The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020). Early reports suggest that modes of transmission of SARS-CoV-2 include droplet and contact (via the fecal-oral route and fomites); airborne transmission may occur during aerosol-generating procedures (World Health Organization, 2020).
During the 2003 SARS-CoV outbreak, despite the presence of existing safety protocols, up to half of the SARS-CoV cases in some centers were HCWs as a result of transmission within hospital units (Booth et al., 2003). Critical care and emergency care providers are often involved in high-risk aerosol-generating procedures such as oronasal suctioning, bag-valve-mask ventilation, non-invasive positive pressure ventilation, and endotracheal intubation in patients with COVID-19 with respiratory failure, and so must be prepared (Caputo et al., 2006; Wax & Christian, 2020; Zuo et al., 2020). The challenge for providers would be to provide high-quality and timely care to infected patients, without compromising their own safety. Apart from having adequate supplies of personal protective equipment (PPE), a safe environment for HCWs requires the provision of up-to-date information regarding the disease, smooth dissemination of protocols, and easy accessibility to portals reinforcing education and training in infection control procedures. Lau et al. (2004) reported that HCWs who underwent more than 2 hours of training were far less likely to be infected with SARS-CoV during the 2003 SARS-CoV outbreak in Hong Kong. In addition to PPE training, we felt that a simulated airway management scenario in a suspected COVID-19 patient was a vital component of training in order for staff to experience the profound challenges of performing high risk aerosol-generating procedures while in PPE and in isolation facilities. During the recent 2014 to 2016 West Africa Ebola outbreak, Grillet et al. (2015) with the use of simulation, found that commonly performed procedures in the intensive care unit becomes more complicated, more stressful and less comfortable in appropriate PPE. We were fortunate to find a window of opportunity close to the beginning of the COVID-19 outbreak in Singapore to prepare our healthcare teams using “just-in-time” in-situ simulation. The main objective of this study was to evaluate the impact of this training on our resuscitation teams when managing a respiratory emergency of a suspected COVID-19 pediatric patient.
II. METHODS
This was a prospective mixed-method cohort study in a paediatric department of a tertiary university hospital. Residents were put through a mandatory “just-in-time” simulation training session to prepare them for intubation of a suspected COVID-19 patient. The doctors involved were senior paediatric residents who regularly manage emergencies on call. Nurses and respiratory therapists were rostered to participate whenever available on shift. Participants worked in teams of 5 to 6 to manage a simulation scenario involving a patient with bronchiolitis who was suspected to have COVID-19. Each team comprised of participants from each of the healthcare professional groups listed above. Actual personal protective equipment (PPE) including powered air-purifying respirators (PAPR) were used in the simulation. Participants received training in the use of PPE and PAPR prior to the simulation session. The simulation was conducted in-situ in the paediatric intensive care unit (PICU) using a SimBaby (Laerdal). The scenario used can be found in the appendix. Each group participated in one scenario. Each scenario lasted 30 to 40 minutes. The end point was successful intubation of the patient. There were 2 instructors (paediatric intensive care clinicians) present, one in the anteroom and one in the patient’s room. Debriefing was conducted as a group by both instructors immediately after every simulation. Each debriefing session lasted 30 to 45 minutes and focused on technical and non-technical skills.
Anonymous pre-simulation and post-simulation questionnaires were administered. Questions focused on confidence levels with managing intubation in a COVID-19 suspect patient, using the PAPR, and anxiety levels. Responses were rated on a Likert scale of 1 to 5. Quantitative data was analysed using Microsoft EXCEL, 2016. Pre and post responses on the Likert scale were analysed using the paired t-test.
After the simulation and debriefing, participants were invited via email to attend focus group interviews to gain better insight into their responses and attitudes towards the simulation sessions. The format and logistics of the interviews were included in a participant information sheet in the email. Participation was voluntary. We aimed for maximal representation from the various groups of healthcare professionals who participated in the simulation. A semi-structured interview was conducted by 2 researchers (NN, JO) in groups of 3 to 5 and interviews were audio-recorded. Two focus group interviews were conducted. Participants were asked questions regarding how they felt, what they learnt and what the benefits of the simulation experience were. Each interview lasted 30 to 40 minutes and were conducted in a quiet room in the PICU. Audio recordings were transcribed verbatim and anonymised at the point of transcription. Participants were only identified by role in the transcript.
Thematic analysis of the transcripts was performed by the 2 interviewers using an inductive approach. Each interviewer coded the data independently, after which both interviewers discussed the codes and generated common themes together. Data was reviewed for commonality in responses, degree of specificity (detailed explanation), and extensiveness (number of different people who had similar responses). Where there was disagreement, review of the data and existing literature was used for resolution. Descriptive summaries were developed for each theme, and participant quotes provided further evidence for interpretation and recommendations made.
This study was approved by the institutional review board (National Healthcare Group, Domain Specific Review Board, NHG DSRB Ref. 2020/00234) and waiver of consent was obtained.
III. RESULTS
A. Pre- and Post-Simulation Questionnaire Responses
A total of 33 participants took part in the training and completed the pre- and post-simulation questionnaires. There were 19 doctors, 12 nurses and 2 respiratory therapists. Confidence, as assessed by the questionnaire, increased significantly after the simulation in the areas of intubation, use of the PAPR, airway management in a COVID-suspect patient, leading a team and dealing with problems that arise during resuscitation (p < 0.05). Regarding anxiety over intubating a COVID-suspect patient, most participants were less anxious after the simulation (p < 0.05). Interestingly, on looking more closely at the responses, 9% (n=3) of participants were more anxious after the simulation than before they started. 42% (n=14) reported no change in their level of anxiety. Table 1 shows the mean scores of the questions asked in the pre- and post-simulation questionnaire.

Table 1: Pre- and post-simulation responses
After the simulation training, 96% of participants agreed or strongly agreed that they were more aware of who to call for help and how to communicate effectively when wearing PPE or PAPR while in an isolation room and 93% agreed or strongly agreed that they were more able to anticipate problems. All participants agreed that simulation training was useful in preparing to deal with a similar situation while on call and in fact, 23% disagreed or strongly disagreed that 1 simulation session was sufficient. Figure 1 illustrates the perceived effectiveness of simulation training by participants.
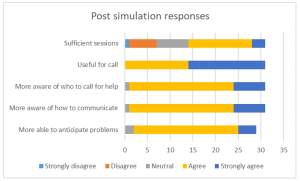
Figure 1: Post-simulation responses on effectiveness of simulation training
B. Focus Group Interviews
Eight participants agreed to focus group interviews, 4 doctors, 3 nurses and 1 respiratory therapist. Comments from the focus group interviews helped to further delineate the benefits and lessons learnt from this simulation exercise. Key benefits were grouped into the following themes:
1) Experiential learning: Participants commented that getting to put theory into practice during the simulation was key to understanding what to expect. Being able to practice before an actual patient encounter helped them to be more prepared. Even simple things like setting an intravenous cannula could not be accomplished with ease. Participants stated that they had to rethink the way that things needed to be done as how they were done previously would not work in this situation. This led to a paradigm shift in the clinical processes and also the application of knowledge. For example, a lesson learnt was that there is a lower threshold for intubation in COVID-19 patients. In the words of a participant about his experience:
“But the fact that you actually go through it, firstly you realize that it takes 3 times the length of the duration of what you would do, and the difficulties in communicating with the people around. So I thought that was the most…an awakening…. the most beneficial part.”
Participants appreciated that this was a complex scenario that was high stakes for the healthcare team as well as for the patient. Getting to practice this, even though it was likely to be an infrequent occurrence, helped with familiarity with protocols and equipment used. Participants also felt that more people should attend this training and that they needed more practice.
2) Increasing confidence: Participants felt that the simulation training was a timely intervention in light of the developing COVID-19 situation. This experience took away the “first-time” feeling and made the participants feel more comfortable with the protective equipment. This took away some of the anxiety and fear about their own safety and the safety of their COVID-19 patients. One participant stated that more practice in simulations may reduce the resistance to wearing the PAPR, which may in itself pose a safety issue if PAPRs are not used when required. They felt that this experience made them a more valuable member to the resuscitation team.
3) Increasing awareness: Participants appreciated the feedback and debriefing that came after the simulation. Experiencing the simulation made taught them to anticipate problems, plan ahead and to prioritize as resources were less accessible than usual. They developed insight into a possible “unconscious incompetence” as they expressed that if they had not gone through the simulation, they would not have known what they did not know and would be inappropriately confident in a real situation. Exploring resource management and considering aspects of waste reduction were thought to be beneficial for future encounters with similar situations. Some of our participants said:
“It really gives you…. the best kind of idea of what to expect in a real life scenario.”
“I would feel quite…. in a sense, bad for the patient that I was doing it for the first time on that patient. So I do feel that it is a responsible thing to do, as healthcare providers that we… that this was actually undertaken.”
“If we had not had this, I probably won’t even have that fear of how terrible it could have been……… But if I had not known, I would still be confident not knowing what I’m expecting.”
Some participants mentioned developing more empathy for colleagues caring for COVID-19 patients through this experience. However, one participant found herself more frustrated after going through the simulation as the experience of managing a resuscitation in this situation was worse than she had thought it would be.
4) Process improvement: In the focus group discussions, participants mentioned the need for process improvement that was discovered while encountering difficulties during the simulation scenario. Communication challenges were brought up multiple times and participants suggested making laminated signs for communication with staff outside the room when assistance was required, having pen, paper and drug labels in the room, as well as using intercoms or walkie-talkies for more efficient communication.
5) Translation: A couple of participants encountered a real subsequent clinical situation which required them to apply skills that they had learnt during the simulation training. The fact that they had gone through the training made them less anxious and more able to take control of the emergency situation. The respiratory therapist in the group expressed more confidence in the nurses that had gone through the simulation training when compared to those who had not when managing a COVID-19 patient. Participants also commented that the skills learnt could be translated to a different institution in the future and perhaps also to a different infective agent. Participants expressed the following:
“And so it would make you, I think… more valuable as a team member in providing care for a COVD patient or any other sort of respiratory pathogen X anywhere.”
“Because I observe that those nurses that attended the simulation, in the actual scenario or in the actual patient handling, they are more confident and competent in doing their PPE and flow of the sequence inside.”
“Because for me, for example, I actually had to initiate and help…coordinate initiation of ECMO for a COVID suspect patient and so I think if not for that…that mock… I would probably have been much more nervous and unsure.”
Key challenges encountered during the simulation were related to the simulation scenario and to the process of simulation itself. The most emphasised challenges encountered during the simulation were cognitive overload and communication barriers. Not only did the team have to deal with a deteriorating patient who was suspected to have COVID-19, they also had to deal with infection control protocols and the inherent challenges that it posed to the resuscitation process. As many tasks needed to be coordinated in a stressful situation, prioritisation was key. Communication barriers came in the form of restricted movement in and out of the isolation room, not being able to use their mobile devices, hearing impairment with the PAPR on and not being able to be heard clearly while wearing the N95 mask. Other challenges raised relating to the scenario were unfamiliarity with the safety equipment as it was not used frequently and having to wait a long time for orders to be carried out. An interesting challenge brought up was a tension between the patient’s safety or well-being and healthcare worker’s own safety. Healthcare professionals frequently put their patients first and in this unique situation, the need for donning personal protective equipment before entering the patient’s environment does not allow for as rapid a response to a deteriorating patient as they are used to:
“I feel like I need to go in as soon as possible but donning the PAPR takes some…. more time than I thought.”
Logistical challenges in planning for this simulation training included the availability and timely attendance of all frontline healthcare workers. With the developing crisis, healthcare professionals were kept busy with their clinical responsibilities, therefore this simulation training was seen as an unwelcome interruption. There was also a perceived resistance to participating by the nurses although the reasons are unclear.
Participants also commented on the design of this simulation training. Prior training in the process of intubation and use of PPE and PAPR were deemed necessary to optimize the benefits of this exercise. Participants appreciated that there were 2 trainers, 1 in the ante-room and 1 in the patient’s room, who were observing different processes and able to give valuable feedback during the debriefing. They also appreciated that the simulation exercise was done in-situ, and therefore was realistic in design.
Suggestions for improvement included providing a variety of clinical scenarios, training junior physicians so that the whole medical team is familiar with the processes, mimicking the typical manpower available on-call in the simulation exercise, and increasing the complexity of the scenarios to address resource allocation issues faced in a pandemic.
IV. DISCUSSION
With the development of the COVID-19 outbreak and patients requiring intensive care, our unit thought it would be imperative to train our frontline staff to be prepared to manage airway emergencies and to be able to resuscitate infected patients. Simulation provides a safe environment for mistakes to be made without compromising patient safety (Ziv et al., 2000). It also provides a platform for deliberate practice (Ericsson, 2004) and not allow for a chance clinical encounter to develop expertise in an area. Simulation has also been utilised in high consequence infectious outbreak training, resulting in improved self-efficacy, reduced anxiety and improved inter-professional teamwork (Marrs et al., 2019; O’Keeffe et al., 2016). As the consequences for patient and individual safety were high in the COVID-19 outbreak, we felt it was prudent to use simulation-based education as a platform for upskilling our staff.
Despite training in the use of personal protection equipment (PPE), including the powered air-purifying respirator (PAPR), Watson et al found that there was an inadequate adherence to the use of PPE and resuscitation guidelines in simulated cardiac arrest in paediatric influenza (H1N1) patients (Watson et al., 2011). Intensive care procedures have been found to be more difficult, stressful and uncomfortable when performed in PPE (Grillet et al., 2015). Simulation training has also been able to detect breaches in infection control procedures (Seet et al., 2009) and potentially improve compliance with infection prevention measures (Tan et al., 2021).
For the above reasons, healthcare professionals who worked in the paediatric intensive care unit were put through a mandatory simulation-based training session on airway management of a deteriorating patient who was suspected to have COVID-19 infection. An in-situ model was chosen as it could be used to evaluate system competence and identify latent conditions that predispose to medical error (Patterson et al., 2013). In this study, in situ simulation provided a means to identify areas for process improvement and knowledge gaps. It provided the ability to test the actual clinical care system, including equipment, processes, and staff response. This form of “just-in-time” training takes place in close proximity to the clinical encounter in a focused concise manner (Itoh et al., 2019). This provides the participants with contextually relevant hands-on experience in dealing with an impending low-frequency event before it actually happens. This has shown to improve confidence levels and clinical skills (Sam et al., 2012).
As expected, there was improvement in self-efficacy as shown in the improvement in pre- and post-simulation responses for all questions relating to management of the patient and clinical team. This has been shown in many previous studies using simulation as a methodology (McLaughlin et al., 2019; Secheresse et al., 2020). Evidence does suggest that clinicians have a limited ability for self-assessment of competence (Davis et al., 2006) and self-assessment. From the Kirkpatrick levels of evaluation, this would be a level 2 evaluation of knowledge, skills and attitudes (Kirkpatrick & Kirkpatrick, 2006). From the qualitative data, the benefits that were emphasised where related to experiential learning and increasing confidence as well as awareness. Kolb’s framework of experiential learning includes the phases of concrete experience and reflective observation (Kolb, 1984). These phases were evident in the simulation experience. Participants reflected that theoretical knowledge does not guarantee perfect execution in real life. The cognitive load of managing a high consequence, low incidence event along with the concomitant risk of exposure to a highly infectious agent makes clinical decision making harder. Although the participants underwent prior PPE training, they appreciated the opportunity to put it all into practice.
There was a definite signal for increased self-efficacy and confidence. This is seen in the literature on simulation-based healthcare education across disciplines (Bragard et al., 2018; Cohen et al., 2013; Fisher et al., 2011; Fouilloux et al., 2019). A study on influenza pandemic preparedness showed that simulation improved staff confidence and also demonstrated that many tasks and procedures took longer to complete with the implementation of guidelines (Phin et al., 2009). This was similarly evident in our participants as they became more aware of the challenges and the additional time needed for most resuscitative actions due to infection control requirements. Going through the simulated scenario and debriefing made them feel more prepared for an actual emergency. In addition, participants highlighted that the simulation experience alleviated anxiety as it successfully removed the “first-time” feeling for them, and felt that it was the responsible thing to do for healthcare workers in the midst a public health crisis. Lessons learnt by the participants included anticipatory planning, prioritisation and resource management. We had a small signal that the skills learnt translated to real life as one participant had a clinical encounter that required initiating extracorporeal life support in a patient with suspected COVID-19. She reported feeling relieved that she had the simulation experience before the real-life clinical encounter, and felt she was less nervous because of her prior stimulated experience. A respiratory therapist also observed that the nurses who he worked with in the PICU who had gone through the simulation seemed more confident and more aware of the necessary processes when intubating suspected COVID-19 patients.
An interesting phenomenon was the signal that there was an increase in anxiety levels after participants went through the simulation as seen in the pre- and post-simulation response. A possible explanation could be what participants brought up in the interviews about the simulation and debriefing revealing their “unconscious incompetence”. This made them more aware of the complexity and so increased their anxiety with dealing with intubation in a COVID-19 patient. Other studies in the literature generally report a reduction in anxiety after simulation (Bragard et al., 2019; Shrestha et al., 2019, 2020). This may not be a negative impact arising from the simulation experience itself as it may reflect increased awareness in an uncommon, yet stressful and complex clinical situation for our healthcare workers. Anxiety levels in frontline healthcare workers in a pandemic may also be due to other factors such as being at higher risk of exposure to COVID-19 at work and the possibility of bringing the infection home to their family (Holmes et al., 2020; Shanafelt et al., 2020).
Another benefit derived from running this simulation-based training is the process improvement suggestions made by the participants. This is a known benefit of simulation (Paige et al., 2018) and was utilised during the 2003 SARS-CoV outbreak (Abrahamson et al., 2005). The main challenge faced by participants during this scenario was the communication barrier which arose from not being able to communicate with personnel outside the room and the presence of the PPE and PAPR physically obstructing hearing and clarity of speech. Also, restriction of movement in and out of the patient’s room experienced during simulation highlighted the need to rethink resuscitation practices when dealing with COIVD patients. These systemic issues surfaced allowed us to brainstorm for practical solutions as a unit, and some have been implemented in our PICU. We have trialled the use of infant monitors as a 2-way communication device. Pre-packed resuscitation drug kits containing intravenous adrenaline and intravenous atropine as well as pre-packed intravenous cannulation disposables have been put in every isolation room so that these would be easily accessible in an emergency. As suggested by the participants, we have also extended the simulation training to include all junior doctors in the department, more nurses and all respiratory therapists in the PICU to facilitate better teamwork. We are also exploring the provision of a dedicated COVID-19 crash cart to minimise waste and prevent cross-contamination.
There are several limitations to this study. Firstly, the sample size is small and selection bias is possible due to the study design. Next, focus group interviews were conducted with a small subset of the participants who agreed to participate, and therefore our findings may not have been representative of the entire cohort. However, we are reassured by the fact that each healthcare professional group that took part in the simulation training was represented in the focus groups. As this simulation exercise was designed to be “just in time” training and we were limited by the urgency of the situation as well as the need to train as many staff in the shortest amount of time, we could only conduct a one-time simulation scenario specific to the highest risk procedure in resuscitating a suspected COVID-19 patient. We were therefore not able to assess the impact of this training on the subsequent performance of the participants either in another simulated scenario or a real life one.
V. CONCLUSION
Simulation-based training is a useful tool for infectious disease outbreak preparedness for the healthcare team. It improves confidence and awareness around managing emergencies while maintaining personal protection through deliberate practice in a safe environment. It also provides an opportunity for process improvement in a new and evolving pandemic situation. It was well-received by the participants and perhaps more sessions are needed for adequate practice. This is limited by the resource-intensive nature of in-situ simulation and the heavy clinical workload at this time of crisis. Further research will need to be done to determine if simulation-based training has a significant impact on actual clinical practice
Notes on Contributors
Nicola Ngiam conceptualised and designed the study, collected data, analysed and interpreted it, drafted the manuscript and approved the final version submitted.
Kristy X Fu did the background work and literature review, assisted in drafting the manuscript and critically revised the manuscript for important intellectual content and approved the final version submitted.
Jacqueline SM Ong designed the study, collected data, interpreted it, critically revised the manuscript for important intellectual content and approved the final version submitted.
Ethical Approval
Ethical approval has been granted by National Healthcare Group Domain Specific Review Board (Ref: NHG DSRB Ref. 2020/00234)
Data Availability
Transcripts from the interviews are confidential and the authors do not have consent to upload onto a repository. Data from questionnaires can be made available on request.
Acknowledgement
We would like to thank Dr Dimple Rajgor for helping with formatting, and submission of the manuscript for publication.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Interest
The Authors declare that there is no conflict of interest.
References
Abrahamson, S. D., Canzian, S., & Brunet, F. (2005). Using simulation for training and to change protocol during the outbreak of severe acute respiratory syndrome. Critical Care, 10(1), R3. https://doi.org/10.1186/cc3916
Booth, C. M., Matukas, L. M., Tomlinson, G. A., Rachlis, A. R., Rose, D. B., Dwosh, H. A., Walmsley, S. L., Mazzulli, T., Avendano, M., Derkach, P., Ephtimios, I. E., Kitai, I., Mederski, B. D., Shadowitz, S. B., Gold, W. L., Hawryluck, L. A., Rea, E., Chenkin, J. S., Cescon, D. W., Poutenan, S.M. & Detsky, A. S. (2003). Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA, 289(21), 2801-2809. https://doi.org/10.1001/jama.289.21.JOC30885
Bragard, I., Farhat, N., Seghaye, M.-C., Karam, O., Neuschwander, A., Shayan, Y., & Schumacher, K. (2019). Effectiveness of a high-fidelity simulation-based training program in managing cardiac arrhythmias in children: A randomized pilot study. Pediatric Emergency Care, 35(6), 412-418. https://doi.org/10.1097/PEC.0000000000000931
Bragard, I., Seghaye, M.-C., Farhat, N., Solowianiuk, M., Saliba, M., Etienne, A.-M., & Schumacher, K. (2018). Implementation of a 2-day simulation-based course to prepare medical graduates on their first year of residency. Pediatric Emergency Care, 34(12), 857-861. https://doi.org/10.1097/PEC.0000000000000930
Caputo, K., Byrick, R., Chapman, M., Orser, B., & Orser, B. (2006). Intubation of SARS patients: Infection and perspectives of healthcare workers. Canadian Journal of Anaesthesia, 53(2), 122-129. https://doi.org/10.1007/BF03021815
Cohen, E. R., Barsuk, J. H., Moazed, F., Caprio, T., Didwania, A., McGaghie, W. C., & Wayne, D. B. (2013). Making July safer: Simulation-based mastery learning during intern boot camp. Academic Medicine, 88(2), 233-239. https://doi.org/10.1097/ACM.0b013e31827bfc0a
Davis, D. A., Mazmanian, P. E., Fordis, M., Van Harrison, R., Thorpe, K. E., & Perrier, L. (2006). Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA, 296(9), 1094-1102. https://doi.org/10.1001/jama.296.9.1094
Ericsson, K. A. (2004). Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine, 79(10), S70-S81. https://doi.org/10.1097/00001888-200410001-00022
Fisher, N., Eisen, L. A., Bayya, J. V., Dulu, A., Bernstein, P. S., Merkatz, I. R., & Goffman, D. (2011). Improved performance of maternal-fetal medicine staff after maternal cardiac arrest simulation-based training. American Journal of Obstetrics and Gynecology, 205(3), e1-e5. https://doi.org/10.1016/j.ajog.2011.06.012
Fouilloux, V., Gran, C., Guervilly, C., Breaud, J., El Louali, F., & Rostini, P. (2019). Impact of education and training course for ECMO patients based on high-fidelity simulation: A pilot study dedicated to ICU nurses. Perfusion, 34(1), 29-34. https://doi.org/10.1177/0267659118789824
Grillet, G., Marjanovic, N., Diverrez, J., Tattevin, P., Tadié, J., & L’Her, E. (2015). Intensive care medical procedures are more complicated, more stressful, and less comfortable with Ebola personal protective equipment: A simulation study. The Journal of Infection, 71(6), 703-706. https://doi.org/10.1016/j.jinf.2015.09.003
Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Silver, R. C., & Everall, I. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry, 7(6), 547-560. https://doi.org/10.1016/S2215-0366(20)30168-1
Itoh, T., Lee-Jayaram, J., Fang, R., Hong, T., & Berg, B. (2019). Just-in-Time Training for Intraosseous Needle Placement and Defibrillator Use in a Pediatric Emergency Department. Pediatric Emergency Care, 35(10), 712-715. https://doi.org/10.1097/PEC.0000000000001516
Kirkpatrick, D., & Kirkpatrick, J. (2006). Evaluating training programs: The four levels (3rd ed.). Berrett-Koehler Publishers.
Kolb, D. (1984). The experiential learning theory of development. Experiential Learning: Experience as the Source of Learning and Development (pp. 132-160). Prentice Hall, Englewood Cliffs, NJ, 132-160.
Lau, J., Fung, K., Wong, T., Kim, J., Wong, E., Chung, S., Ho, D., Chan, L., Lui, S., & Cheng, A. (2004). SARS transmission among hospital workers in Hong Kong. Emerging Infectious Diseases, 10(2), 280-286. https://doi.org/10.3201/eid1002.030534
Marrs, R., Horsley, T. L., Hackbarth, D., & Landon, E. (2019). High consequence infectious diseases training using interprofessional simulation and TeamSTEPPS. American Journal of Infection Control, 48(6), 615-620. https://doi.org/10.1016/j.ajic.2019.10.007
McLaughlin, C., Barry, W., Barin, E., Kysh, L., Auerbach, M. A., Upperman, J. S., Burd, R. S., & Jensen, A. R. (2019). Multidisciplinary simulation-based team training for trauma resuscitation: A scoping review. Journal of Surgical Education, 76(6), 1669-1680. https://doi.org/10.1016/j.jsurg.2019.05.002
O’Keeffe, D., Bradley, D., Evans, L., Bustamante, N., Timmel, M., Akkineni, R., Mulloy, D., Goralnick, E., & Pozner, C. (2016). Ebola Emergency Preparedness: Simulation Training for Frontline Health Care Professionals. MedEdPORTAL, 12, 10433-10433. https://doi.org/10.15766/mep_2374-8265.10433
Paige, J. T., Fairbanks, R. J. T., & Gaba, D. M. (2018). Priorities related to improving healthcare safety through simulation. Simulation in Healthcare, 13(3S), S41-S50. https://doi.org/10.1097/SIH.0000000000000295
Patterson, M., Geis, G., Falcone, R., LeMaster, T., & Wears, R. (2013). In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Quality & Safety, 22(6), 468-477. https://doi.org/10.1136/bmjqs-2012-000942
Phin, N., Rylands, A., Allan, J., Edwards, C., Enstone, J., & Nguyen-Van-Tam, J. (2009). Personal protective equipment in an influenza pandemic: a UK simulation exercise. Journal of Hospital Infection, 71(1), 15-21. https://doi.org/10.1016/j.jhin.2008.09.005
Sam, J., Pierse, M., Al-Qahtani, A., & Cheng, A. (2012). Implementation and evaluation of a simulation curriculum for paediatric residency programs including just-in-time in situ mock codes. Paediatrics & Child Health, 17(2), e16-20. https://doi.org/10.1093/pch/17.2.e16
Secheresse, T., Pansu, P., & Lima, L. (2020). The impact of full-scale simulation training based on Kolb’s learning cycle on medical prehospital emergency teams: A multilevel assessment study. Simulation in Healthcare, 15(5), 335-340. https://doi.org/10.1097/SIH.0000000000000461
Seet, R., Lim, E., Oh, V., Ong, B., Goh, K., Fisher, D., Ho, K., & Yeoh, K. (2009). Readiness exercise to combat avian influenza. QJM : Monthly Journal of the Association of Physicians, 102(2), 133-137. https://doi.org/10.1093/qjmed/hcn159
Shanafelt, T., Ripp, J., & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA, 323(21), 2133-2134. https://doi.org/10.1001/jama.2020.5893
Shrestha, R., Badyal, D., Shrestha, A., & Shrestha, A. (2020). In-situ simulation-based module to train interns in resuscitation skills during cardiac arrest. Advances in Medical education and Practice, 11, 271-285. https://doi.org/10.2147/AMEP.S246920
Shrestha, R., Shrestha, A. P., Shrestha, S. K., Basnet, S., & Pradhan, A. (2019). Interdisciplinary in situ simulation-based medical education in the emergency department of a teaching hospital in Nepal. International Journal of Emergency Medicine, 12(1), 19. https://doi.org/10.1186/s12245-019-0235-x
Tan, K. W., Ong, H. K., & Mok, U. S. (2021). Using simulation and inter-professional education to teach infection prevention during resuscitation. The Asia Pacific Scholar, 6(1), 93-108. https://doi.org/10.29060/TAPS.2021-6-1/OA2229
The Centre for Evidence-Based Medicine Nuffield Department of Primary Care Health Sciences University of Oxford. (2020). Global Covid-19 case fatality rates. https://www.cebm.net/covid-19/global-covid-19-case-fatality-rates/. Accessed April 26, 2020.
The Novel Coronavirus Pnuemonia Emergency Response Epidemiology Team. (2020). The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly, 2(8), 113-122. https://doi.org/10.46234/ccdcw2020.032
Watson, C., Duval-Arnould, J., McCrory, M., Froz, S., Connors, C., Perl, T., & Hunt, E. (2011). Simulated pediatric resuscitation use for personal protective equipment adherence measurement and training during the 2009 influenza (H1N1) pandemic. The Joint Commission Journal on Quality and Patient Safety, 37(11), 515-523. https://doi.org/10.1016/S1553-7250(11)37066-3
Wax, R. S., & Christian, M. D. (2020). Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Canadian Journal of Anesthesia/Journal canadien d’anesthésie, 67(5), 568–576. https://doi.org/10.1007/s12630-020-01591-x
World Health Organization. (2020). Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019- nCoV). Retrieved 6 April, 2021, from https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
Wu, Z., & McGoogan, J. (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA, 323(13), 1239-1242. https://doi.org/10.1001/jama.2020.2648
Ziv, A., Small, S. D., & Wolpe, P. R. (2000). Patient safety and simulation-based medical education. Medical Teacher, 22(5), 489-495. https://doi.org/10.1080/01421590050110777
Zuo, M., Huang, Y., Ma, W., Xue, Z., Zhang, J., Gong, Y., & Che, L. (2020). Expert recommendations for tracheal intubation in critically ill patients with Noval Coronavirus Disease 2019. Chinese Medical Sciences Journal, 35(2), 105–109. https://doi.org/10.24920/003724
*Nicola Ngiam
Centre for Healthcare Simulation,
National University of Singapore,
14 Medical Dr,
Singapore 117599
Email: nicola_ngiam@nuhs.edu.sg
Submitted: 5 July 2021
Accepted: 13 September 2021
Published online: 5 April, TAPS 2022, 7(2), 6-16
https://doi.org/10.29060/TAPS.2022-7-2/OA2654
Ming-Jung Ho1,2, Yu-Che Chang3,4,5 & Steven L. Kanter6
1Center for Innovations and Leadership in Education, Georgetown University Medical Center (CENTILE), Washington, D.C., United States; 2Department of Family Medicine, Georgetown University School of Medicine, Washington D.C., United States; 3Chang Gung Medical Education Research Centre (CG-MERC), Chang Gung Medical Foundation, Taoyuan, Taiwan; 4Chang Gung University College of Medicine, Taoyuan, Taiwan; 5Department of Emergency Medicine, Chang Gung Memorial Hospital, Linkou, Taoyuan, Taiwan; 6Association of Academic Health Centers, Washington, D.C., United States.
Abstract
Introduction: The COVID-19 pandemic forced medical schools worldwide to transition online. While there are ample reports about medical education adaptations to this crisis, there are limited studies evaluating the impact.
Methods: This study includes a case study of how Taiwanese medical school deans maintained in-person education during the COVID-19 pandemic. Additionally, it demonstrates how SWOT analyses can help medical educators reflect on adaptations during the COVID-19 pandemic and future crises. This study employed two online surveys and a semi-structured interview regarding curricular adaptations. Eligible participants were deans or associate deans of all medical schools in Taiwan.
Results: Through a SWOT analysis, this study identified Strengths as strong leadership, prior experience with SARS, and ability to promptly adapt curriculum; Weaknesses as lack of faculty confidence in online education, limited numbers of administrative staff, and inability to rapidly add new topics; Opportunities as centralised anti-epidemic policies, inter-institutional collaborations, and educational innovations; and Threats as concerns from parents, patients, and teaching hospitals. It is reported that the quality of education was maintained as students’ evaluations of courses, performances in written exams, clerkship supervisors’ assessments, national OSCE, and national board exams remained comparable to pre-COVID times. Strengths and Opportunities such as strong leadership and centralised anti-epidemic policies can overcome Weaknesses and Threats, such as lack of confidence in online education and familial pressure to suspend hospital-based education.
Conclusion: This study recommends that medical school leaders conduct SWOT analyses as early as possible to plan strategies to continue safe and quality medical education during COVID-19 and future crises.
Keywords: SWOT Analysis, Adaptation, Medical School, COVID-19, Pandemic, National Survey, Medical Education, Taiwan
Practice Highlights
- Medical school deans in Taiwan documented critical observations made during a global pandemic.
- SWOT analysis can help us reflect on medical education adaptations during the pandemic and crises.
- Strong leadership and centralised anti-epidemic policies can aid in overcoming weaknesses/threats.
- Schools can benefit from using SWOT analyses to plan for continuing education during emergent crises.
I. INTRODUCTION
The novel coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China at the end of December 2019 evolved rapidly into a global pandemic and upended almost every aspect of our lives, including school closures across the world (UNICEF, 2021; Zhu et al., 2020). Medical schools are no exception (B. Choi et al., 2020; Harries et al., 2021). Almost all medical schools in the United States transitioned to online teaching by mid-March 2020 and tried to restart teaching on campuses and in hospitals safely in Fall 2020 (Frieden, 2020) . There is a growing literature on how to transition medical education online during the COVID-19 pandemic (Ahmed et al., 2020; Al-Balas et al., 2020; Journal of the Association of American Medical Colleges, 2021; Keegan & Bannister, 2021; Medical Education, 2020). Medical education associations also developed websites and offered webinars to share best practices and innovations focused on online education rather than in-person education (Association for Medical Education in Europe, 2020; Association of American Medical Colleges, 2021; International Association of Medical Science Educators, 2020). Most of the literature reflects the important perspectives of teachers and students with voices from medical school leadership and the forces impacting their decisions relatively limited (Abbas et al., 2020; Al-Balas et al., 2020; Compton et al., 2020; Gordon & Cleland, 2021; Lazarus et al., 2021; Soled et al., 2020). Furthermore, most of the publications are based on lessons learned from English-speaking countries. As non-English-speaking countries encountered COVID-19 and started to reopen medical schools earlier than English-speaking countries, lessons from non-English-speaking medical schools can be valuable to the global medical education community. This study addresses the above gaps in literature by surveying Taiwanese medical school deans on how they adapted their curricula and continued face-to-face medical education on campus and in hospitals amid this historical moment.
Located 81 miles from mainland China, and with over a hundred daily flights in between, Taiwan was predicted to have the second highest number of COVID-19 cases according to early modeling in January 2020 (Gardner, 2020). Having learnt a hard lesson from the severe acute respiratory syndrome (SARS) epidemic in 2003, the Taiwanese government, health system, general public, and medical educators were better prepared to respond to this new pandemic early and proactively (Wang et al., 2020). Before the first confirmed case in Taiwan, the Taiwan Centers for Disease Control began to monitor passengers returning from Wuhan, China, since on January 21, 2020 and set up the Central Epidemic Command Center to coordinate responses to COVID-19, including surveillance and testing, border control, community transmission control, medical system response, personal protective equipment (PPE) and other medical supplies stockpile and distribution, as well as health education and disinformation management (Taiwan Center for Disease Control, 2020).
In contrast to medical schools around world closing campus in the spring semester due to the COVID-19 pandemic, Taiwanese medical schools stayed open except for delaying the start of spring semester one or two weeks later than the originally scheduled date of February 17, 2020.
In addition to exploring how Taiwanese medical schools adapted their curriculum to continue on-campus and workplace-based education at the program level during the COVID-19 pandemic, this study addresses the gap in the literature regarding evaluation of these programmatic changes (Reid & Sam, 2021). This study employed a SWOT analysis (Ghazinoorya et al., 2011; Topor et al., 2018), a method widely used to analyse an organisation’s internal strengths and weaknesses, as well as external opportunities and threats in the environment to examine what medical education leaders critically consider in order to maintain in-person medical education amid the COVID-19 pandemic. This study surveyed and interviewed Taiwanese medical school deans in order to answer the following four research questions:
1. What curricular adaptations have been made in response to the COVID-19 pandemic?
2. What were the impacts of the curricular adaptations?
3. What were the strengths, weaknesses, opportunities, and threats of the curricular adaptations?
4. What are the lessons learned to be applied to the future?
II. METHODS
This study consists of two online surveys and a follow-up individual semi-structured interview. Eligible participants were deans or associate deans of all 13 medical schools in Taiwan. To encourage participation, we emailed invitations with information about study purpose, data confidentiality, and a weblink to the online survey. Participation was voluntary without incentives offered. Following the initial email, reminders were sent periodically. If the dean of a medical school was not available to complete the survey, we invited the associate dean to do so. We collected survey responses and conducted interviews about curricular adaptations between April 29 and May 18, 2020. A follow up survey on the impacts of curricular adaptation was conducted between August 27 and September 10. The online written surveys and follow-up semi-structured interviews were conducted in Chinese (written) and Mandarin (spoken) and translated to English by the first author (MJH). This study was approved as exempt by the Georgetown University Institutional Review Board (STUDY00002812). Since the study poses no greater than minimal risk to subjects, a waiver of written consent was granted, and verbal consent was obtained before data collection began. All methods were carried out in accordance with relevant guidelines and regulations.
A. Study Design
The survey questions were developed based on a review of relevant literature and consultations with international research collaborators in Italy, Japan and Korea, where similar surveys will be conducted. Open-ended survey questions can be found in Supplemental Digital Appendix 1.
In addition to the online survey, each participant was offered an opportunity to be interviewed by the first author (MJH) videoconference in the ensuing two weeks to provide further details about their survey responses. If a participant accepted the interview invitation, a semi-structured interview was conducted, in which the participant was prompted to elaborate on their answers in the surveys. Clarifying questions were asked for survey responses as needed. For example, a participant responded to a survey question by stating that an OSCE exam had been cancelled. During the ensuing interview, the interviewer asked “In the survey, you wrote that an OSCE was cancelled. What was the OSCE for? How did you make up for the cancelled OSCE?”
B. Data Analysis
The free text responses to the open-ended questions in the survey, as well as recordings of the interviews, were analysed by the researchers using a qualitative thematic analysis approach (Braun & Clarke, 2006). One researcher identified themes that emerged from the qualitative data; then, a second researcher determined if they agree or disagree with the analysis. For each point of disagreement, the two researchers discussed the data and reached consensus. Data analysis was initially inductive. After the themes emerged, we used a SWOT analysis framework to group themes into four categories: strengths internal to the institution, weaknesses internal to the institution, opportunities external to the institution, and threats external to the institution (Ghazinoorya et al., 2011; Topor et al., 2018).
III. RESULTS
All 13 medical schools in Taiwan completed the survey for a response rate of 100%. Eleven deans and two associate deans filled out the survey. Three deans and one associate dean agreed to participate in a follow-up interview by videoconference. Characteristics of the medical schools are listed in Table 1. In the first part of results, we will describe curricular adaptations and present themes with representative quotes of curricular adaptations in Table 2. Then Table 3 will summarise the SWOT analysis followed by descriptions of key themes in strengths, weaknesses, opportunities, and threats.
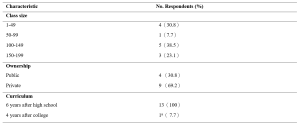
Table 1. Characteristics of Survey Schools
aOne medical school had both 6-year program for high school graduates and 4-year program for college graduates.
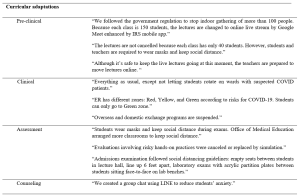
Table 2. Themes and quotes of curriculum adaptations
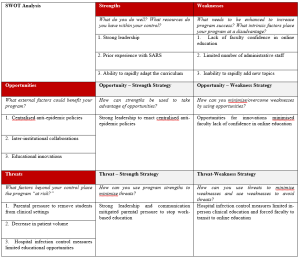
Table 3. SWOT Analysisb
b This table is created using the blank SWOT form from Topor et al.21
A. Curricular Adaptations
1) Pre-clinical curriculum adaptations:
Taiwanese medical schools rapidly adapted their curricula to comply with government policy on social distancing prohibiting indoor gatherings of more than 100 individuals. Whereas a school with a small student body and sufficient classroom capacity did not have to transition online, a school with a large student body and insufficient classroom capacity moved almost all pre-clinical classes online. Some schools went partially online, converting only lectures with more than 100 students to online learning and capping the number of students in the classroom, with live stream available for those not in the classroom. While schools adapted different modalities for lecture-based courses, all schools made efforts to keep laboratory courses face-to-face. Some schools shared how they adjusted laboratory sessions to maintain social distance, including simultaneously using more lab rooms or holding lab sessions in different time slots.
2) Clinical curriculum adaptations:
In contrast to approaches in the United States suspending clinical rotations in spring semester recommended by AAMC (Association of American Medical Colleges, 2021), all medical schools in Taiwan continued clinical rotations while protecting the safety of students. Several strategies were implemented rapidly: Orientation to clinical rotations articulated pandemic prevention and included online modules required by the hospital. Clinical students were provided with surgical masks. In the emergency room, students were given N95 respirators each day. Exposure to suspected and confirmed COVID-19 cases was avoided for students replacing rotations in specialties with high risk of COVID-19 exposure. To prevent cross infection, inter-institutional and overseas exchange programs were cancelled. Students rotated in only one of the affiliated hospitals. Social distancing is also mentioned in clinical rotation adjustments. Several respondents mentioned that the number of students in outpatient clinics, in classrooms, and in conferences was reduced. One school reported an increase of clinical teachers to meet social distancing demands.
3) Assessment adaptations:
Eight schools replied that they did not change the assessment of students by written examinations in classrooms but arranged empty seats between students to keep social distance and protected students from airborne droplet transmissions by requiring everyone to wear a mask. Some schools decreased the use of written exams in classrooms by substituting reports, reflections, online exams, online presentations, and other approaches. Some evaluations involving hands-on practices were cancelled or replaced by simulation. One school reported that their admission exams included tests in laboratories. To prevent face-to-face transmission of airborne droplets, transparent acrylic partitions were installed on the benches in front of each student.
B. Impact of curricular adaptations
Medical school deans tried to evaluate the impact of curricular adaptions by comparing student performance in the 2020 spring semester with previous years. Most deans reviewed the passing rate of courses and reported no statistical differences. They also reported monitoring students’ performances in national board exams in July and national OSCE clinical skills exam held before graduation. The deans were relieved to see that the national exam scores were comparable to previous years and felt that curricular adaptations didn’t impact student competencies negatively.
C. Strengths
The strengths of Taiwanese medical schools’ responses to COVID-19 can be summarised into three themes: strong leadership, prior experience with SARS, and ability to rapidly adapt the curriculum.
1) Strong leadership: The key strength most Taiwanese deans cited in their medical schools’ response to COVID-19 is the strong leadership in the early deployment of epidemic prevention measures. The guidelines from the Central Epidemic Command Center were implemented on each campus, including requiring students to wear masks, to maintain social distance, to monitor temperature and symptoms of COVID-19, and to quarantine international students in separate dormitory areas. Communication also was highlighted by respondents as manifesting strong leadership. Furthermore, two deans made videos in collaboration with students to promote anti-epidemic measures (Chang Gung University, 2020; Fu Jen Catholic University, 2020).
2) Prior experience with SARS: Another strength most respondents noted was the experience of SARS. When COVID-19 spread to Taiwan, most clinical teachers had experienced SARS and were able to share critical lessons to face new emerging infectious diseases with the younger generation. The experience of SARS also prepared medical educators to deal with professionalism and ethics issues such as distribution of limited medical resources. Many participants mentioned that SARS had a great impact on the medical education system in Taiwan because it exposed the lack of primary care workforce with medical school graduates entering specialty training directly after medical school. After SARS, a postgraduate year program was established with one year of required general medicine training prior to specialty training programs with the goal of producing more physicians competent in general medicine to respond to emergent infectious diseases.
3) Ability to rapidly adapt the curriculum: All schools reported rapid curricular adaptations when spring semester started one or two weeks later than the scheduled time. Different strategies were employed in pre-clinical and clinical curricula to prevent and control the spread of COVID-19 as described in 3.1 curricular adaptation.
D. Weaknesses
The weaknesses of Taiwanese medical schools’ responses to COVID-19 can be summarised into three themes: lack of faculty confidence in online education, limited number of administrative staff, and inability to rapidly add new topics.
1) Lack of faculty confidence in online education: All respondents mentioned online teaching as challenging to teachers. Many voiced concerns about the effectiveness of online learning and found assessment of online learning challenging. Online learning is also considered challenging to students. Some respondents mentioned that online learning requires self-directed learning, which is not a strength of Taiwanese students since didactic teaching and rote memorisation is the norm of the K-12 education system.
2) Limited number of administrative staff: In response to the question about weaknesses of their medical schools’ responses to the COVID-19 pandemic, administrative challenges were mentioned frequently. Although Taiwan did not experience high burdens of COVID-19, all schools were preparing for large-scale outbreaks with frequent scenario planning, describing these planning activities using the military metaphor of “military sand table planning” and “early deployment.”
3) Inability to rapidly add new topics: The pandemic also revealed the need for medical educators to engage in some topics traditionally not articulated in medical curricula. It was challenging to add new topics in the ongoing 2020 spring semester curricula but respondents suggested to add the following topics in the future: infectious disease control, emergent infectious disease, crisis management and communication, public policy and ethical issues related to pandemics such as distribution of medical resources, and government control and restrictions on human rights vs quarantine policy.
E. Opportunities
Taiwanese medical school deans highlighted three opportunities which enabled them to continue to open medical schools during the COVID-19 pandemic: centralised anti-epidemic policies, collaborations among medical schools, and educational innovations.
1) Centralised anti-epidemic policies: Taiwanese deans all reported that the policies from the central government are helpful in their implementation of anti-epidemic measures. Several deans shared the policy guidelines issued by the Ministry of Education with clear guidelines to follow the principles of infection containment. Although each university has the flexibility to decide how to comply with the guidelines, there was external oversight to ensure compliance. For example, when a teaching hospital had an intra-hospital transmission of COVID-19, the medical school had to work with the Central Epidemic Command Center and Ministry of Education in its response.
2) Inter-institutional collaborations: Collaborations among medical schools through the Taiwan Association of Medical Education (TAME) also helped Taiwanese medical school deans to adapt to COVID-19. For instance, the deans worked together at TAME to ensure that final-year students graduated on time. Every year, TAME organises a national OSCE examination required for graduation for final year Taiwanese medical students. Medical schools and teaching hospitals collaborated to administer these exams at OSCE centers in selected teaching hospitals with infection mitigating measures.
3) Educational innovations: All respondents mentioned that the COVID-19 pandemic provided opportunities to engage in innovations in medical education, especially online education. Online education was quickly implemented in some schools because access to internet is prevalent in Taiwan and they utilised the technology developed before the pandemic. One school reported an innovation using the Interactive Response System (IRS) developed three years ago and is now applied to enhance online teaching amid COVID-19. Another school adapted communication software instead of face-to-face counseling meetings. One school reported using “LINE” (a messaging app widely used in Taiwan) for a group chat for students to reduce student anxiety related to COVID-19.
F. Threats
Three themes were identified during the COVID-19 pandemic as threats to medical education, but external to medical schools: parental pressure to remove students from clinical settings, decrease in patient volume, and hospital infection control measures limited educational opportunities.
1) Parental pressure to remove students from clinical settings: Several deans mentioned that students’ parents reached out to them, pressuring them to discontinue clinical rotations. One respondent stated, “Parents are more worried than teachers and students. They are concerned that clinical rotations in the hospitals are risky for students. However, parents accepted our explanation that clinical rotations will not proceed unless there is adequate PPE and infection control measures.”
2) Decrease in patient volume: Another threat commonly mentioned was the decrease in patient volume. A participant explained, “Our hospital experienced a 30% decrease in patient volume. It is inconvenient for patients to come to the hospital due to tightened entrance control. The restriction on patients’ family visits is another factor. We are not letting students rotate on wards with suspected COVID-19 patients.” The limited patient encounters are perceived as potential threat to students’ clinical competence.
3) Hospital infection control measures limited educational opportunities: Finally, another threat reported was associated with infection control measures by the teaching hospitals. Deans expressed concerns that students’ clinical learning opportunities were compromised during the pandemic due to cancelled bedside teaching in high-risk specialties, cancelled presentations in conferences, cancelled interdepartmental grand rounds, and suspension of exchange programs both domestically and internationally. Some mentioned that reduced clinical exposures might result in less role modeling.
IV. DISCUSSION
During this historical event, medical schools around the world are challenged to navigate a path forward to meet missions of education, research, and patient care during an ongoing pandemic. As many countries are loosening or tightening restrictions after their curves of infection have flattened or resurged, medical schools globally are at various stages of deliberating when and how to resume campus-based and hospital-based medical education (Blaaza et al., 2020; Cleland et al., 2020; Tolsgaard et al., 2020). A systematic rapid review of published reports of medical educational developments in response to the COVID-19 pandemic concluded that most papers lacked evaluation data and focused on transitioning online and removing students from the clinical contexts (Gordon et al., 2020). The review suggested that medical schools learn from a few postgraduate papers reporting how face-to-face patient contact could be maintained while mitigating risk using PPE and social distancing (G. Choi et al., 2020; Hanel et al., 2020; Kang et al., 2020). Our study of medical school deans in Taiwan on how they continued in-person medical education throughout the COVID-19 pandemic offers lessons for the medical education community to engage medical students in campus-based and workplace-based learning with evaluation of impacts.
This study offers a conceptual advance by demonstrating how SWOT analysis can help us reflect on medical education adaptations to COVID-19 pandemic and future crises. Our analysis of the strengths, weaknesses, opportunities and threats in Taiwanese medical school adaptations to COVID-19 highlights certain strategies to leverage strengths and opportunities to overcome weaknesses and threats. A critical factor in the decision to continue face-to-face medical education, clearly identified by the opportunity-strength strategy in Table 3, was the early deployment of epidemic prevention measures under centralised government policies and strong medical school leadership. Epidemic prevention measures were deployed at all levels of schools in Taiwan as students returned to campus for spring semester in February 2020. To enact anti-epidemic policies in different contexts, this study presented various preventive measures to keep the recommended social distance in classrooms, laboratories, and teaching hospitals. To implement these measures, transparent communication and administrative support from medical school leadership are essential.
SWOT analysis on opportunity-weakness and threat-weakness strategies offers lessons on how to overcome the weakness of lack of faculty confidence in online education. Although online education is an important curricular adaptation to maintain social distance in campus-based medical education, our survey shows that respondents found online teaching challenging to faculty and are concerned about the effectiveness of online education. Strategies identified to overcome this weakness is to take advantage of the educational technology readily available and to transform the threats from hospital infection control to suspend hospital-based education into opportunities for integrating innovative online education. It is important to leverage innovative online education in workplace learning in the context of reduced patient case exposures before the pandemic subsides (B. Choi et al., 2020; Lo et al., 2020). There is sufficient evidence in the education literature that well-designed online education is as effective as traditional classroom teaching and shows equivalent or better learning outcomes (George et al., 2014; Jung & Rha, 2000; Khalil et al., 2020). We hope that the evaluations reported in the fall semester survey showing equivalent outcomes of online adaptations during COVID-19 would encourage medical educators to take advantage of innovations reported by this study, existing literature on online education in general, and the growing literature about innovative online medical education (Ahmed et al., 2020; Medical Education, 2020).
This study highlighted that another enabling factor for Taiwanese medical educators to continue face-to-face medical education was the experience of SARS. The Taiwanese population became accustomed to anti-epidemic measures, including wearing masks after SARS, which facilitated the implementation of anti-epidemic measures in schools during COVID-19. Taiwanese health providers were severely challenged during the 2003 SARS epidemic. 103 of 318 confirmed cases (Centers for Disease Control and Prevention, 2003) and 11 of 60 deaths (including two first-year residents) (Taiwan Centers for Disease Control, 2013) were healthcare workers. Medical education leaders had a difficult decision to make regarding the final year students who were working as interns in hospitals (Lai, 2020). Following closures of clinics and resignation of healthcare providers, there were heated debates about physician duties to treat patients while being at risk of exposure to a deadly infectious disease and of being stigmatised by society (Lee, 2003). After SARS, not only were curricula on ethics and infection control strengthened, but the medical education system was reformed to convert the final-year of medical school to a formal post-graduate year program (Ho et al., 2017). In addition, as articulated by the respondents of the survey, SARS prepared Taiwanese medical educators and clinical teachers to be confident and competent to perform their educational and clinical duties in the time of COVID-19.
Although this study has many lessons to offer both conceptually and practically, there are some limitations to be considered. We conducted the survey with open-ended questions to explore diverse perspectives. The reported theme frequencies should be considered with caution since some respondents record more comprehensive answers than others. While the most frequently mentioned themes might be most important to the respondents, the least frequently given answer might be valuable due to its innovative nature. Another limitation of an open-ended questionnaire is that respondents might not have the time to enter answers in detail. To overcome this limitation, we invited the respondents to participate in a follow-up interview. However, only about one-third of deans were available to be interviewed during the study period. The four interviews conducted nonetheless enriched the study with more context and details. Finally, this study only surveyed medical school deans. It would be interesting to conduct further studies comparing these results to the perspectives of students and faculty members.
V. CONCLUSION
This nationwide study of all medical schools in Taiwan documents critical observations of top medical school leaders during an active pandemic. This case study demonstrated that strengths and opportunities such as strong leadership and centralised anti-epidemic policies can overcome weaknesses and threats such as faculty lack of confidence in online education and parental pressure to stop hospital-based education. We recommend that medical school leaders conduct SWOT analyses as early as possible to plan strategies to continue safe and quality medical education during COVID-19 and forthcoming emergencies. Similar to the impact of SARS, which led to reform of the Taiwanese postgraduate training system, there is hope that thoughtful reflection on medical education adaptations to the COVID-19 pandemic will improve medical education in general and lead to better preparation for future crises.
Notes on Contributors
MH contributed to the conception, acquisition and analysis of data, drafted the article, and approved the final version; YC contributed to the design, acquisition and analysis of data, drafted the article, and approved the final version; SK contributed to analysis and interpretation of data, revised the article critically, and approved the final version.
Ethical Approval
This study was approved as exempt by the Georgetown University Institutional Review Board (STUDY00002812). Since the study poses no greater than minimal risk to subjects, a waiver of written consent was granted. . We emailed invitations with information about study purpose, data confidentiality, and a weblink to the online survey. A verbal consent was obtained before data collection began. Participation was voluntary without incentives offered. All methods were carried out in accordance with relevant guidelines and regulations.
Data Availability
It is not possible to share data since we did not get consent from participants to share all data collected. They agreed to have results reported in a summary format with selected quotes.
Acknowledgement
The authors wish to thank survey respondents and interviewees for providing insights on the research topic. Fred Hafferty and Carrie Chen provided useful feedback to improve the manuscript.
Funding
This study did not receive any funding.
Declaration of Interest
The authors declare that they have no competing interests.
References
Abbas, M., Dhane, M., Beniey, M., Meloche-Dumas, L., Eissa, M., Guerard-Poirier, N., El-Raheb, M., Lebel-Guay, F., Dubrowski, A., & Patocskai, E. (2020). Repercussions of the COVID-19 pandemic on the well-being and training of medical clerks: A pan-Canadian survey. BMC Medical Education, 20(1), 385. https://doi.org/10.1186/s12909-020-02293-0
Ahmed, S. A., Hegazy, N. N., Abdel Malak, H. W., Cliff Kayser, W., 3rd, Elrafie, N. M., Hassanien, M., Al-Hayani, A. A., El Saadany, S. A., Ai-Youbi, A. O., & Shehata, M. H. (2020). Model for utilizing distance learning post COVID-19 using (PACT)TM a cross sectional qualitative study. BMC Medical Education, 20(1), 400. https://doi.org/10.1186/s12909-020-02311-1
Al-Balas, M., Al-Balas, H. I., Jaber, H. M., Obeidat, K., Al-Balas, H., Aborajooh, E. A., Al-Taher, R., & Al-Balas, B. (2020). Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: Current situation, challenges, and perspectives. BMC Medical Education, 20(1), 341. https://doi.org/10.1186/s12909-020-02257-4
Association for Medical Education in Europe. (2020). COVID-19. Retrieved April 1, 2021, from https://amee.org/covid-19
Association of American Medical Colleges. (2021). Coronavirus (COVID-19) resource hub. Retrieved April 1, 2021, from https://www.aamc.org/coronavirus-covid-19-resource-hub
Blaaza, M., Akhtar, H. N., & Tanzim, U. (2020). Returning to clinics amidst COVID-19: A student response to Compton et al. Medical Education, 54(12), 1193. https://doi.org/10.1111/medu.14282
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative research in psychology, 3(2), 77-101.
Centers for Disease Control and Prevention. (2003). Severe acute respiratory syndrome–Taiwan, 2003. Morbidity and mortality weekly report, 52(20), 461‐466.
Chang Gung University. (2020, March 16). Chang Gung University COVID-19 anti-epidemic advanced adaptation measures [Video]. YouTube. https://www.youtube.com/watch?v=WyoOoShXVa8
Choi, B., Jegatheeswaran, L., Minocha, A., Alhilani, M., Nakhoul, M., & Mutengesa, E. (2020). The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: a national survey. BMC medical education, 20(1), 206. https://doi.org/10.1186/s12909-020-02117-1
Choi, G., Wan, W., Chan, A., Tong, S., Poon, S., & Joynt, G. (2020). Preparedness for COVID-19: In situ simulation to enhance infection control systems in the intensive care unit. British Journal of Anaesthesia, 125(2), e236-e239. https://doi.org/10.1016/j.bja.2020.04.001
Cleland, J., McKimm, J., Fuller, R., Taylor, D., Janczukowicz, J., & Gibbs, T. (2020). Adapting to the impact of COVID-19: Sharing stories, sharing practice. Medical Teacher, 42(7), 772-775. https://doi.org/10.1080/0142159X.2020.1757635
Compton, S., Sarraf-Yazdi, S., Rustandy, F., & Radha Krishna, L. K. (2020). Medical students’ preference for returning to the clinical setting during the COVID-19 pandemic. Medical Education, 54(10), 943-950. https://doi.org/10.1111/medu.14268
Frieden, J. (2020, May 9). Medical schools grapple with challenges for the coming year— Three-quarters hope to have students back by the end of July. MedPage Today. Retrieved April 1 fromhttps://www.medpagetoday.com/publichealthpolicy/medicaleducation/86416
Fu Jen Catholic University. (2020, February 16). COVID-19: Fu Jen Catholic University anti-epidemic promotion video. [Video]. YouTube. https://youtu.be/-n3KvlVHpzY
Gardner, L. (2020, January 31). Update January 31: Modeling the spreading risk of 2019-nCoV. Johns Hopkins University Center for Systems Science and Engineering. Retrieved April 1 from https://systems.jhu.edu/research/public-health/ncov-model-2/
George, P. P., Papachristou, N., Belisario, J. M., Wang, W., Wark, P. A., Cotic, Z., Rasmussen, K., Sluiter, R., Riboli-Sasco, E., Tudor Car, L., Musulanov, E. M., Molina, J. A., Heng, B. H., Zhang, Y., Wheeler, E. L., Al Shorbaji, N., Majeed, A., & Car, J. (2014). Online eLearning for undergraduates in health professions: A systematic review of the impact on knowledge, skills, attitudes and satisfaction. Journal of Global Health, 4(1), 010406. https://doi.org/10.7189/jogh.04.010406
Ghazinoorya, S., Abdia, M., & Azadegan-Mehr, M. (2011). SWOT methodology: A state-of-the-art review for the past, a framework for the future. Journal of Business Economics and Management, 12(1), 24-48. https://doi.org/10.3846/16111699.2011.555358
Gordon, L., & Cleland, J. A. (2021). Change is never easy: How management theories can help operationalise change in medical education. Medical Education, 55(1), 55-64. https://doi.org/10.1111/medu.14297
Gordon, M., Patricio, M., Horne, L., Muston, A., Alston, S. R., Pammi, M., Thammasitboon, S., Park, S., Pawlikowska, T., Rees, E. L., Doyle, A. J., & Daniel, M. (2020). Developments in medical education in response to the COVID-19 pandemic: A rapid BEME systematic review: BEME Guide No. 63. Medical Teacher, 42(11), 1202-1215. https://doi.org/10.1080/0142159X.2020.1807484
Hanel, E., Bilic, M., Hassall, K., Hastings, M., Jazuli, F., Ha, M., Trotter, B., Fraser, C., & Rutledge, G. (2020). Virtual application of in situ simulation during a pandemic. Canadian Journal of Eemergency Medicine, 22(5), 563-566. https://doi.org/10.1017/cem.2020.375
Harries, A. J., Lee, C., Jones, L., Rodriguez, R. M., Davis, J. A., Boysen-Osborn, M., Kashima, K. J., Krane, N. K., Rae, G., Kman, N., Langsfeld, J. M., & Juarez, M. (2021). Effects of the COVID-19 pandemic on medical students: A multicenter quantitative study. BMC Medical Education, 21(1), 14. https://doi.org/10.1186/s12909-020-02462-1
Ho, M.-J., Shaw, K., Shih, J., & Chiu, Y.-T. (2017). Mission and modernity: The history and development of medical education in Taiwan. In L. C. Chen, M. R. Reich, & J. Ryan (Eds.), Medical Education in East Asia: Past and Future (pp. 84-111). Indiana University press.
International Association of Medical Science Educators. (2020, April 22). #IAMSECafe Archives & COVID-19 resources for medical science educators. Retrieved April 1 from http://www.iamse.org/covid-19-resources-for-medical-science-educators/
Journal of the Association of American Medical Colleges. (2021). COVID-19 and medical education. Retrieved April 1 from https://journals.lww.com/academicmedicine/pages/collectiondetails.aspx?TopicalCollectionId=68
Jung, I., & Rha, I. (2000). Effectiveness and cost-effectiveness of online education: A review of the literature. Educational Technology, 40(4), 57-60.
Kang, Y., Deng, L., Zhang, D., Wang, Y., Wang, G., Mei, L., Zhou, G., & Shu, H. (2020). A practice of anesthesia scenario design for emergency cesarean section in patients with COVID-19 infection based on the role of standard patient. BioScience Trends, 14(3), 222-226. https://doi.org/10.5582/bst.2020.03066
Keegan, D. A., & Bannister, S. L. (2021). More than moving online: Implications of the COVID-19 pandemic on curriculum development. Medical Education, 55(1), 101-103. https://doi.org/10.1111/medu.14389
Khalil, R., Mansour, A. E., Fadda, W. A., Almisnid, K., Aldamegh, M., Al-Nafeesah, A., Alkhalifah, A., & Al-Wutayd, O. (2020). The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: A qualitative study exploring medical students’ perspectives. BMC Medical Education, 20(1), 285. https://doi.org/10.1186/s12909-020-02208-z
Lai, C. (2020, March 20). 2003 SARS: Reflections on Taiwanese medical education. UDN. https://health.udn.com/health/story/6631/4421448
Lazarus, G., Findyartini, A., Putera, A. M., Gamalliel, N., Nugraha, D., Adli, I., Phowira, J., Azzahra, L., Ariffandi, B., & Widyahening, I. S. (2021). Willingness to volunteer and readiness to practice of undergraduate medical students during the COVID-19 pandemic: A cross-sectional survey in Indonesia. BMC Medical Education, 21(1), 138. https://doi.org/10.1186/s12909-021-02576-0
Lee, M. (2003). SARS 風暴的啟示[Learning from the SARS event] [Editorial]. Journal of Medical Education, 7(1), 1-2.
Lo, H.-Y., Lin, S.-C., Chaou, C.-H., Chang, Y.-C., Ng, C.-J., & Chen, S.-Y. (2020). What is the impact of the COVID-19 pandemic on emergency medicine residency training: An observational study. BMC Medical Education, 20(1), 348. https://doi.org/10.1186/s12909-020-02267-2
Medical Education. (2020, May 7). Medical education adaptations. Retrieved April 1, 2020, from https://onlinelibrary.wiley.com/doi/toc/10.1002/(ISSN)1365-2923.med.adaptations.vi
Reid, M. D., & Sam, A. H. (2021). Reflections on assessment in the wake of change from the COVID-19 pandemic. Medical Education, 55(1), 128-130. https://doi.org/10.1111/medu.14368
Soled, D., Goel, S., Barry, D., Erfani, P., Joseph, N., Kochis, M., Uppal, N., Velasquez, D., Vora, K., & Scott, K. W. (2020). Medical student mobilization during a crisis: Lessons from a COVID-19 medical student response team. Academic Medicine, 95(9), 1384-1387. https://doi.org/10.1097/ACM.0000000000003401
Taiwan Center for Disease Control. (2020). Prevention and control of COVID-19 in Taiwan. Retrieved April 1, 2021, from https://www.cdc.gov.tw/Category/Page/0vq8rsAob_9HCi5GQ5jH1Q
Taiwan Centers for Disease Control. (2013). Severe acute respiratory syndrome (SARS). Retrieved April 1, 2021 from https://www.cdc.gov.tw/File/Get/InG8jagjxffXBDW1UexnrA
Tolsgaard, M. G., Cleland, J., Wilkinson, T., & Ellaway, R. H. (2020). How we make choices and sacrifices in medical education during the COVID-19 pandemic. Medical Teacher, 42(7), 741-743. https://doi.org/10.1080/0142159X.2020.1767769
Topor, D. R., Dickey, C., Stonestreet, L., Wendt, J., Woolley, A., & Budson, A. (2018). Interprofessional health care education at academic medical centers: Using a SWOT analysis to develop and implement programming. MedEdPORTAL, 14, 10766. https://doi.org/10.15766/mep_2374-8265.10766
UNICEF. (2021). COVID-19 Education: From disruption to recovery. Retrieved April 1, 2021, from https://en.unesco.org/covid19/educationresponse
Wang, C. J., Ng, C. Y., & Brook, R. H. (2020). Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. The Journal of the American Medical Association, 323(14), 1341-1342. https://doi.org/10.1001/jama.2020.3151
Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., Zhao, X., Huang, B., Shi, W., Lu, R., Niu, P., Zhan, F., Ma, X., Wang, D., Xu, W., Wu, G., Gao, G. F., & Tan, W. (2020). A novel coronavirus from patients with pneumonia in China, 2019. The New England Journal of Medicine, 382(8), 727-733. https://doi.org/10.1056/NEJMoa2001017
*Yu-Che Chang
No. 5, Fuxing St.,
Guishan Dist.,
Taoyuan City 333012,
Taiwan (R.O.C.)
Tel: +886-33281200 ext 3807
Email: changyuche@gmail.com
Submitted: 30 July 2021
Accepted: 4 October 2021
Published online: 5 April, TAPS 2022, 7(2), 1-5
https://doi.org/10.29060/TAPS.2022-7-2/GP2663
Mary Anne Reid1 & Kirsty Forrest2
1Senior Policy Officer, Medical Deans Australia and New Zealand, Australia; 2Dean of Medicine, Faculty of Health Sciences and Medicine, Bond University, Australia
Abstract
Introduction: This article summarises a report published in July 2021 by Medical Deans Australia and New Zealand (Medical Deans), the peak body representing the 23 medical programs in Australia and New Zealand. It explores how medical schools responded to the early impacts of COVID-19 in 2020, and how they might build on some of the changes to achieve fundamental improvements in medical education in Australia and New Zealand.
Methods: The Medical Deans report was based on: Responses to a survey midway through 2020 of its member schools about their experiences during the initial lockdowns; the contributions of presenters at the Medical Deans 2020 Annual Conference; subsequent discussions among communities of practice.
Results: Innovations introduced in response to the pandemic, included greater equity of learning opportunities across geographical locations; health services taking more responsibility for clinical placements; greater emphasis on competencies and less on clinical rotations in specific disciplines; strong collaboration between medical schools, and with providers in the medical training and research pipeline. Challenges include balancing the benefits of online learning with the need for human connection and a chronic lack of clinical training opportunities in community-based care.
Conclusion: While the impact of the pandemic on medical education and training was costly for all involved – both financially and personally – the scale of disruption provided a unique opportunity for step change. To fully realise this potential moving forward, medical schools will need to work in partnership with all those involved: students, health services, prevocational training, specialist colleges, regulators and governments.
Practice Highlights
- Equity of learning opportunities across rural, regional and urban locations using digital technology.
- Enhanced learning outcomes through a blend of remote and face-to-face teaching and assessment.
- Shared responsibility for medical students’ clinical placements as an essential part of the health system.
- More emphasis on student competencies and less on clinical rotations in specific disciplines.
- Strong collaboration between medical schools and across the training pipeline.
I. INTRODUCTION
Medical schools in Australia and New Zealand graduated close to the anticipated number of new doctors (3,800) at the end of 2020 – a significant feat given the size and number of shockwaves sent through the sector by the pandemic. Despite the immense stress COVID-19 placed on the sector, it was also the catalyst for significant innovation.
This article summarises the findings of a report published in July 2021 by the peak body representing the 23 medical schools in the two countries, Medical Deans Australia and New Zealand (Medical Deans). The report, Changing for good: What we learned in 2020 (Medical Deans Australia and New Zealand, 2021a), explored those innovations which occurred during the pandemic that medical schools want to retain and build on in the future. It also identified some critical gaps and problems highlighted by the pandemic that must be addressed moving forward.
II. METHODS
The report was authored on the basis of: responses to a survey run by Medical Deans Australia and New Zealand (MDANZ) midway through 2020; the contributions of presenters at the Medical Deans’ 2020 Annual Conference; subsequent discussions among Medical Deans’ communities of practice.
Where quotes are attributed to a particular person, they are drawn largely from the Annual Conference. Where quotes are attributed to a medical school rather than a person, they are drawn from the Medical Deans survey.
III. RESULTS
A. Innovation through Online Learning
As campuses closed early in 2020, schools employed a combination of pre-recorded sessions and interactive online lessons to deliver much of the non-clinical, and a small part of the clinical, medical curriculum to students. This created a sense of unity amongst students in different geographical locations as they all accessed the same lessons online – reducing disparities sometimes faced by those in regional and rural areas.
- University of Auckland: We have done much more synchronous learning across sites – we have eight sites in each clinical year across the north island – and we’re going to keep that.
- University of Newcastle: We’ve found that the expert facilitating a learning session can now be based anywhere and it works well.
- University of New South Wales: We have students at five metro hospitals and at least five rural ones, plus those in GP placements, who can now join each other in learning activities online. Prior to this, the rural students often felt left out of tutorials and activities that the metro students could get to.
The move out of the lecture theatre also allowed more flexibility for students in accessing lessons and interactivity, through online chat functions, and encouraged the use of advanced digital learning platforms. Small group tutorials used online tools to imitate some aspects of face-to-face clinical teaching and assessment, for example, Zoom rooms for interactions with actors or Objective Structured Clinical Examinations (OSCES).
- Sydney: The live Zoom component of the flipped classroom, with two experts (one monitoring chat), has proven very interactive and popular compared to a large lecture theatre. It also allows for more polling, which the students enjoy. With a cohort of 270, we saw increases from an average of 60-80 participants [25%] in lecture theatre mode to up to 210 participants on Zoom [75%].
However, there were also significant problems associated with delivering so much of the curriculum remotely. Online fatigue and the loss by students of a human connection with their peers and teachers was extremely stressful for many, particularly for international students, some of whom were far away from home for the first time. Another cohort at a particular disadvantage were the first-year students who did not get the chance to attend their university campus or make friends in this new phase of their life before the COVID lockdown.
Another issue for students was that access to adequate technology and learning space offsite was not always adequate, despite schools’ best efforts.
“The presumption in delivering medical training online is that all students have equal access to the technology, and that presumption is not correct,” said Professor John Fraser, University of Auckland’s Executive Dean of Medicine and Health Sciences. “Technology comes at a cost and not all students have enough resources to meet their technological needs. Also, the idea that each student has a space of their own to do their online learning is not always the case.”
Finally, medicine uses a very hands-on, apprentice-based educational approach, and there was only so much that could be done remotely.
Professor Fraser “There is so much subtlety in the way you learn in a clinical environment that it cannot be properly replicated online.”
The future of medical education lies in developing and refining the optimal blend of face-to-face and remote learning and assessment. Getting the balance right will be an ongoing priority for medical schools. By comparing approaches, medical schools have the best chance to determine the optimum mix of remote learning for their individual medical programs. This will be a continuing focus for medical schools, through the Medical Deans’ Medical Education Collaborative Committee (MECC). The University of Notre Dame Australia’s Dean of Medicine, Gervase Chaney, told the 2020 MDANZ Annual Conference that there was an opportunity to implement long-lasting change: “I think we’ve learned that if we are going to get value, we’re not going to be bringing our students on to campus four or five days every week. We’ll be looking at a more flexible learning approach and they can still be doing some clinical skills training – like the history-taking over Zoom or other online platforms. It’s a case of how we normalise this so that when students step into the clinical space, it’s a natural step for them.”
B. New Approaches to Clinical Learning
After an initial halt during the onset of the pandemic, clinical placements for later-year medical students were largely re-instated in 2020.
In Australia, one of the defining features of these new-style placements was the emphasis on shared responsibility between medical schools and health services. Medical schools collaborated as never before with each other and with health services on a range of clinical placement models and paid positions for medical students as part of the surge workforce. While remunerated roles already existed for final year students and pre-interns in other countries, including New Zealand, they were a first for Australia.
These new approaches to clinical placements and paid positions had the following features in common:
- the learning needs of the student were explicit and central
- the role of the student, and their scope of practice within the healthcare team, was more clearly defined and articulated
- medical schools and health services shared core responsibilities for students and the success of their placements
There was strong and widespread support from Australian medical schools for the benefits brought by this shared responsibility for medical students on placement or working within healthcare environments.
Another key shift in clinical training came about due to the need to minimise patient exposure to multiple healthcare workers: in many cases, students were placed for longer periods of time in general wards caring for patients with a range of medical conditions, and their rotations in some medical specialties were cancelled (e.g. obstetrics and gynaecology, intensive care). Students reported feeling more connected to the other health professionals they worked alongside during these longer placements and more able to make a valuable work contribution to patient care.
The Deputy Vice Chancellor, Tropical Health and Medicine at James Cook University, Richard Murray, believes this provided greater exposure for students to whole-of-patient care: “The clinical phase of medical education has traditionally been carved into different rotational experiences across medical disciplines and cemented in place through departments, budgets and staffing. COVID-19 has driven more learning around the integrated experience of patients. Rather than curriculum by a set of rotations, you have curriculum according to people of all ages and with all sorts of problems, which are often complex and interrelated. Learning is more integrated now.”
This discussion is furthered in the Medical Deans advocacy document Training tomorrow’s doctors – All pulling in the right direction (Medical Deans Australia and New Zealand, 2021b), with a number of recommendations for change. One of these is for regulators, medical schools and jurisdictional health service providers to build on the insights from the evaluation of the Assistants in Medicine role piloted in response to the pandemic in NSW in 2020 (New South Wales Health, 2021) and the New Zealand Trainee Intern model, to develop a shared and explicit understanding of what is needed to be prepared for practice; and to strengthen arrangements for students’ transition from medical school to employment.
C. Collaboration on Core Competencies
Also supporting this more generalist approach was the co-development by schools of an agreed set of core competencies needed for final-year medical students to progress to graduation.
This unprecedented collaboration between universities saw medical schools co-develop the common core competencies needed to graduate as a means of quality assuring the rapid and extensive changes made to their programs and placements due to the pandemic. Developed through the Medical Deans’ MECC, these core competencies were based on the schools’ own course outcomes and aligned with those required by the Australian Medical Council.
- Deakin University: We now have clear competencies mapped for internship – extended to the penultimate year. It is now less about the rotation and more about the competencies.
- University of Auckland: Based on our local graduate learning outcomes, we are emphasising core competencies over disciplinary learning outcomes. We are emphasising generic skills and capabilities.
The collaboration between medical schools during 2020 – culminating in the collaboration on core competencies – was amongst the most ranked highly ranked innovations of period which resulted in the Guidance statement: Clinical practice core competencies for graduating medical students (Medical Deans of Australia and New Zealand, 2020).
“The challenges of COVID made us create these dynamic and interactive education teams consisting of students, academics, professional support, design and IT staff all working together on re-developing format, content and assessments,” said University of NSW’s Associate Professor Torda. “At university level we did this across faculties; nationally, we worked more closely together, through Medical Deans in particular, to share and solve problems.” (Medical Deans Australia and New Zealand, 2021a)
D. Lack of Opportunities in Community-Based Care
A pre-existing lack of clinical training opportunities for medical students in community settings – in aged care in particular and, in some places, in general practice – only worsened during the COVID-19 pandemic.
National and international studies show that health systems which provide strong primary care are more cost-effective and associated with a more equitable distribution of healthcare across the population (Australian Department of Health, 2019). Yet GPs are not resourced in the same way as hospitals to provide clinical training for medical students, which fuels an over-emphasis on clinical training in hospitals. COVID-19 highlighted this problem, with GP placements becoming variable in 2020, as practices scrambled to secure the Personal Protective Equipment needed to provide patient services and tended to view medical students as an additional burden rather than as part of the health workforce response.
In the case of aged care, the limited training opportunities for clinical training that existed prior to the pandemic were lost completely in 2020, as facilities moved to shield their vulnerable elderly residents from COVID-19.
We know that the aging populations of Australia and New Zealand will increasingly require non-hospital-based care to manage the chronic and comorbidity conditions that typically occur in older populations (Australian Department of Health, 2019). Medical schools and health services must work together and with governments to ensure that more quality clinical training opportunities are available for students in both community-based aged care and general practice. In addition, to develop and implement solutions effectively there has to be continued and stronger collaboration right along the medical training and research pipeline, from medical schools to specialist training.
No single strategy will address this problem; it will require a coordinated effort. Medical Deans is advocating for Australian and New Zealand governments to establish a taskforce comprising the key stakeholders responsible for designing and delivering medical education and training across all stages of the continuum to:
- co-develop future training models that target the priority areas of workforce need; and
- explore the possibility of a “flipped” model for community-based PGY1 and PGY2 doctors where the majority of their experience occurs in a community-based setting, rotating into hospitals for training as required.
IV. CONCLUSION
While the impact of the pandemic on medical education and training in 2020 was costly – both financially and personally – the scale of disruption provided a unique opportunity for step change. In many cases, the sudden and massive changes created strong potential for lasting improvement. In other areas, the pandemic highlighted cracks that already existed within the health sector (e.g. lack of clinical placements in community healthcare settings), which will require coordinated effort beyond the medical education sector to fix.
Medical Deans has incorporated and built on these key learnings with the development of a number of advocacy positions and documents. In addition to those reports already mentioned, the learning has informed the student support document Creating a culture of support – For medical students transitioning to practice (Medical Deans Australia and New Zealand, 2021c), as well as the Medical Deans’ submission to the consultation for the Australian Medical Council’s Review of the Accreditation Standards for Primary Medical Programs.
Medical schools are looking to capitalise on the resourcefulness and innovation of 2020 in all the ways highlighted in this article and the full report by Medical Deans. To fully realise this potential, they will need to work in partnership with all those involved: students, health services, prevocational training, specialist colleges, regulators, and governments.
Notes on Contributors
Mary Anne Reid developed the Medical Deans survey of members schools and collated its findings. She integrated these with elements of the presentations made at the 2020 Annual Conference, and other member discussions, to develop the structure and write the text.
Kirsty Forrest provided key editorial and supervisory input as the member of the Medical Deans Executive supporting the report.
Acknowledgement
The authors acknowledge the support of Helen Craig, Chief Executive Officer of Medical Deans, who came up with the idea for the report and provided guidance throughout.
Funding
There are no funding sources to declare.
Declaration of Interest
The authors declare that there is no conflict of interest related to this manuscript.
References
Australian Department of Health. (2019). National Medical Workforce Strategy Scoping Framework.
Medical Deans Australia and New Zealand. (2020). Guidance statement: Clinical practice core competencies for graduating medical students. Unpublished. Please contact Medical Deans to request a copy at admin@medicaldeans.org.au
Medical Deans Australia and New Zealand. (2021a, July). Changing for good: What we learned in 2020. https://medicaldeans.org.au/md/2021/07/Changing-for-Good-What-We-Learned-in-2020-Medical-Deans-report-July-2021.pdf
Medical Deans Australia and New Zealand. (2021b, September). Training tomorrow’s doctors – All pulling in the right direction. https://medicaldeans.org.au/resource/training-tomorrows-doctors-all-pulling-in-the-right-direction/
Medical Deans Australia and New Zealand. (2021c, October). Creating a culture of support – For medical students transitioning to practice.
New South Wales Health. (2021). Assistant in Medicine Evaluation Report.
https://www.health.nsw.gov.au/workforce/medical/Publications/aim-evaluation-report.pdf
*Mary Anne Reid
Medical Deans Australia and New Zealand,
19 Kent Street, Sydney, NSW 2000
Email: mreid@medicaldeans.org.au
Submitted: 2 June 2021
Accepted: 21 June 2021
Published online: 4 January, TAPS 2022, 7(1), 115-116
https://doi.org/10.29060/TAPS.2022-7-1/LE2546
Clement Luck Khng Chia1, Shaun Wen Yang Chan1, Priscilla Ng2 & Chee Chew Yip3
1Department of General Surgery, Khoo Teck Puat Hospital, Singapore; 2Department of Geriatrics, Khoo Teck Puat Hospital, Singapore; 3Department of Ophthalmology, Khoo Teck Puat Hospital, Singapore
Dear Editor,
Khoo Teck Puat Hospital held its first LOTTE (Learning Oriented Teaching in Transdisciplinary Education) elective program for Yong Loo Lin School of Medicine students in April 2021. The four-week program focuses on undergraduate medical education in an inter-professional collaborative setting through observation and presentation of complex clinical cases. Its teaching-learning activities are underpinned by the Learning Oriented Teaching (LOT) theory (ten Cate et al., 2004) to improve learning at the cognitive, affective and metacognitive levels with shared guidance between students and faculty.
At the cognitive level, students were encouraged to take ownership of learning, do literature review and present cases. Faculty critiqued and helped students to refine learning objectives and identify pertinent clinical aspects for elaboration and learning.
At the affective level, students were motivated to present cases on Zoom videoconferencing to classmates as they learned through active doing and attained peer recognition of their good effort. The teacher highlighted the importance of peer learning through discussing authentic, complex cases that required transdisciplinary holistic patient care.
At an interactive self and peer learning level, students used tools such as the Kahoot! game-based app for peer teaching to optimise learning and increase participation.
With a greying population, there is a need for transdisciplinary education to improve patient outcomes in the geriatric population (Chia et al., 2016). LOTTE provided an introduction to transdisciplinary education and highlighted importance of integrating competencies from various disciplines in preparation for future practice.
The first run of LOTTE consisted of seven transdisciplinary themes. An example of a transdisciplinary theme would be “Palliative Surgery” offered by both a palliative physician and an oncology surgeon. LOTTE differed from traditional “single discipline” electives as it emphasised inter-professional collaboration and collective learning involving the surgeon, physician and students. Students divided their time equally in both subspecialties, attending ward rounds, clinics, operating theatres and home visits. They encapsulated their learnings by presenting real-life complex cases via Zoom in the last week to their peers and faculty. Learning opportunities in two subspecialties were maximised with the student following through the patient journey from ‘Start to Finish’ (Chia et al., 2016).
Medical graduates face an increasingly complex healthcare landscape where management of co-morbidities may be beyond one’s expertise. LOTTE may be helpful to promote transdisciplinary collaboration for holistic management of complex geriatric patients and nurture the development of independent learning in medical undergraduates.
Notes on Contributors
Dr Clement Chia conceptualised and designed LOTTE framework, was a faculty in LOTTE and wrote the manuscript and approved the final version.
Dr Shaun Chan conceptualised and designed LOTTE framework, helped coordinate students, was a faculty in LOTTE and revised and approved the manuscript.
Dr Priscilla Ng conceptualised and designed LOTTE framework, was a faculty in LOTTE, revised and approved the manuscript.
A/Prof Yip Chee Chew conceptualised and designed LOTTE, revised and approved the manuscript.
Acknowledgement
We would like to thank all the transdisciplinary educators who made this inaugural run of LOTTE possible. They include A/Prof Tan Kok Yang, A/Prof Toh Hong Chuen, A/Prof Tavintharan Subramaniam, Dr Desmond Ooi, Dr Tan Mingyuan, Dr Tan Bo Chuan, Dr Ruth Chua, Dr Benjamin Lam, Dr Visnja Baksa Reynolds and Dr Gabriel Cher.
Funding
There is no funding for this study.
Declaration of Interest
Authors declare no conflict of interest.
References
ten Cate, O., Snell, L., Mann, K., & Vermunt, J. (2004). Orienting teaching toward the learning process. Academic Medicine, 79(3), 219-228. https://doi.org/10.1097/00001888-200403000-00005
Chia, C. L. K., Mantoo, S. K., & Tan, K. Y. (2016). ‘Start to finish trans-institutional transdisciplinary care’: A novel approach improves colorectal surgical results in frail elderly patients. Colorectal Disease, 18(1), O43–O50. https://doi.org/10.1111/codi.13166
*Clement Chia
Khoo Teck Puat Hospital,
90 Yishun Central,
Singapore 768828
Department of General Surgery
Tel: +6566022207
Email: chia.clement.lk@ktph.com.sg
Submitted: 28 May 2021
Accepted: 25 August 2021
Published online: 4 January, TAPS 2022, 7(1), 112-114
https://doi.org/10.29060/TAPS.2022-7-1/PV2544
Sok Ying Liaw & Siew Tiang Lau
Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
I. BACKGROUND
The coronavirus disease 2019 (COVID-19) has been declared as a pandemic. On 7 February 2020, the Ministry of Health (MOH), announced the suspension of all clinical postings. All healthcare students were ordered to withdraw from hospitals within hours after the announcement. Graduating year nursing students from the National University of Singapore (NUS) were into their final phases of clinical postings. The suspension of clinical postings greatly disrupted the students’ preparations in developing clinical competencies critical to their future nursing professions.
Across the world, healthcare policymakers and institutions have responded to nursing students’ clinical education in a variety of ways. One compelling argument for continuing the clinical education of graduating nursing students is to treat them as part of the healthcare teams and leverage their clinical skills to boost the capacity of care teams. However, as our nursing students were at an earlier stage of their final year clinical practicum and have yet to acquire the knowledge, skills and clinical experience of a qualified nurse, it may be argued that their involvement in patient care delivery would have primarily been for educational purposes. Thus, the potential of compromising patient safety due to lack of supervision by the overwhelmed trained staff, the risks of contracting the contagion and giving rise to psychological concerns might not overweigh their educational benefits.
In Singapore, healthcare policymakers and institutions face the challenge of balancing education, healthcare service and potential risks for students in the healthcare settings. The main reasons for the suspension of clinical postings were the unknown risk of COVID-19 at that timepoint and the need for hospitals to manage their resources to transform their facilities and manpower to care for infectious patients. The suspension of clinical postings affected the nursing students’ abilities to fulfil the required number of clinical hours set out by the Singapore Nursing Board (SNB) to be registered as a registered nurse. Academic nurses at the NUS had to react quickly by employing simulation strategies to replace clinical hours. This gave rise to a debate around evidence-based practice versus practicalities in designing simulation as a substitute for clinical practice in nursing clinical education.
II. SIMULATION TO REPLACE CLINICAL PRACTICE HOURS
In light of the suspension of clinical placements, the SNB has permitted the substitution of 160 out of 400 clinical hours (40%) of the final year students’ clinical practicums with simulation. This can be supported by existing evidences on the use of simulation as a substitute for clinical placement in prelicensure nursing programmes (Curl et al., 2016). In our plan to replace 160 clinical hours, we initially assumed a ratio of one hour of simulation to one hour of clinical time. However, we recognised the challenges to implement this 1:1 ratio for the training of 300 nursing students using the existing simulation facilities, along with the need to adhere to the safe distancing measures initiated by the university. We had to plan a class size of not more than ten persons in a simulation laboratory, including a facilitator and a simulated patient, in order to keep everyone at a safe distance of at least two metres apart. Given these resource implications, we equated a ratio of one hour of simulation to two hours of clinical practice.
There is no clear evidence on the substitution ratio for simulation hours to clinical placement hours. A study by Curl et al., (2016) evaluated the use of simulation experiences to replace 50% of clinical experiences by employing a ratio of a substitute of one hour of simulation to two hours of clinical experience. Bogossian et al. (2019) postulated that as a simulation can be both controlled and time-compressed, it should draw more than parity in clinical practice hours, which is an aspect worth future investigation.
III. TYPES OF SIMULATION MODALITIES
We had to work out different types of simulation modalities to meet the 80 hours of simulation learning as well as to achieve the learning outcomes based on the SNB’s competency domains for registered nurses. The 80 hours also included the simulation-based assessment on clinical performance and post simulation activities on reflective writing to provide evidence to SNB on the achievement of learning outcomes. Earlier studies focused mainly on the use of high-fidelity simulations to replace clinical practices (Bogossian et al., 2019; Curl et al., 2016). The adequacy of existing simulation facilities and their accesses were constraints that led us to explore a variety of simulation modalities, including simulated clinical immersion using high-fidelity simulations, procedural simulations and computer-based simulations.
We adopted and expanded our earlier developed evidence-based simulation program, known as SIMulated Professional Learning Environment (SIMPLE) to create simulated clinical immersion learning and assessments in the NUS Centre for Healthcare Simulation. The availability of the SIMPLE guide, which included learning objectives, details of scenarios, debriefing guides and scripts for simulated patient, prompted our quick planning and implementation of the facilitators’ briefing and simulation learning. A total of six simulation sessions were implemented based on themes related to common ward nursing practices. In each simulation session, we incorporated two patients (one high-fidelity simulator and one simulated patient) in a simulated general ward setting. Our earlier study provided evidence on the benefits of the SIMPLE programme in promoting nursing students’ transition-to-practice experiences (Liaw et al., 2015). We also put in place a contingency plan on the use of video-based simulations in case we could not conduct face-to-face simulations. The video-based simulations were conducted via video conferencing for a small group of students who were unable to attend face-to-face simulations.
In the simulated clinical immersion scenarios, the students were required to perform a set of clinical procedures related to patient care. Thus, we incorporated procedural simulations to provide opportunities for the students to revise the procedures and practise the technical skills that they had acquired in years one and two. As a result of a lack of simulation facilities and faculty resources, the self-direct practice approach was adopted for procedure simulation learning. The students were given case scenarios and a set of requisites, including a wound dressing set, an intravenous priming set and an indwelling catheterization set, to practise the clinical procedures innovatively at home. They were also instructed to develop and submit video recordings of their best ten performed procedures, selected from a list of core skills for registered nurses, to provide evidence of their time (e.g. 20 hours) in engaging self-directed learning as well as for instructor feedback. Apart from procedural simulation learning, we managed to implement procedural simulation assessments on donning and doffing personal protection equipment (PPE) at remote locations by leveraging telecommunication resources using Zoom’s video conference calls. This approach enabled direct observations of performance and feedback between a student and an assessor.
Earlier, we developed two computer-based simulations, e-RAPIDS (Rescuing A Patient In Deteriorating Situation) and CREATIVE (Create Real-time Experience And Teamwork In Virtual Environment), to allow the students to participate in experiential learning. These were considered valuable resources for students’ off-site learning for the development of non-technical skills. Using experiential learning approach, the e-RAPIDS provided a self-directed learning resource for students to develop clinical reasoning skills through the application of knowledge to problem solve deteriorating virtual patients with feedback from multiple scenarios. The CREATIVE provided nursing students opportunities to undertake simulation-based interprofessional education with medical students on nurse-doctor communication skills training. We evaluated the effectiveness of these computer-based screen simulations on students’ learning outcomes performance by comparing with high-fidelity simulation in the previous studies (Liaw et al., 2014, 2020). The non-inferiority outcomes of these simulations to high-fidelity simulations may justify the use of these computer-based screen simulations to replace some clinical hours.
IV. CONCLUSION
The COVID-19 outbreak posed a unique challenge to nursing clinical education. The cessation of clinical placements led to immediate concerns on nursing students’ clinical competencies, which necessitated the adoption of various simulation resources as an alternative means of delivering clinical education. The inadequacy of existing simulation resources and their limited accessibilities posed challenges in the replacement of clinical hours. Nonetheless, this COVID-19 pandemic has prompted us to embrace more innovative simulation initiatives, including video-based simulations and tele-simulations. These innovations inevitably gave rise to a debate around evidence-based practice versus practicalities for designing simulation as a replacement for nursing clinical practice. More evidence is warranted to justify the use of different types of simulation modalities to replace clinical practices in terms of learning outcomes and cost-effectiveness. Such evidence can inform future implementations and policy development on the regulation of using simulations to replace clinical practices to ensure student competency for the nursing workforce. We look forward to seeing more simulation innovations along with evaluation research for simulation technology amid the COVID-19 pandemic.
Notes on Contributors
Sok Ying Liaw designed and implemented the simulation and took the lead in writing the manuscript.
Siew Tiang Lau contributed to the planning of the simulation and aided the development of the manuscript.
Acknowledgement
The authors would like to thank the faculty staff of Alice Lee Centre for Nursing Studies for supporting the implementation of simulation. The authors would like to thank the National University Health System, Research Support Unit, for providing editing services to this manuscript.
Funding
The authors have no funding to report.
Declaration of Interest
The authors have no conflict of interests to declare.
References
Bogossian, F. E., Cant, R. P., Ballard, E. L., Cooper, S. J., Levett-Jones, T. L., McKenna, L. G., Ng, L. C., & Seaton, P. C. (2019). Locating “gold standard” evidence for simulation as a substitute for clinical practice in prelicensure health professional education: A systematic review. Journal of Clinical Nursing, 28(21-22), 3759-3775. https://doi.org/10.1111/jocn.14965
Curl, E. D., Smith, S., Chisholm, L. A., McGee, L. A., & Das, K. (2016). Effectiveness of integrated simulation and clinical experiences compared to traditional clinical experiences for nursing. Nursing Education Perspectives, 37(2), 72-77. https://doi.org/10.5480/15-1647
Liaw, S. Y., Chan, S. W.-C., Chen, F.-G., Hooi, S. C., & Siau, C. (2014). Comparison of virtual patient simulation with mannequin-based simulation for improving clinical performances in assessing and managing clinical deterioration: Randomized controlled trial. Journal of Medical Internet Research, 16(9), e214. https://doi.org/10.2196/jmir.3322
Liaw, S. Y., Ooi, S. W., Rusli, K. D. B., Lau, T. C., Tam, W. W. S., & Chua, W. L. (2020). Nurse-physician communication team training in virtual reality versus live simulations: Randomized controlled trial on team communication and teamwork attitudes. Journal of Medical Internet Research, 22(4), e17279. https://doi.org/10.2196/17279
Liaw, S. Y., Palham, S., Chan, S. W.-C., Wong, L. F., & Lim, F. P. (2015). Using simulation learning through academic-practice partnership to promote transition to clinical practice: A qualitative evaluation. Journal of Advanced Nursing, 71(5), 1044-1054. https://doi.org/10.1111/jan.12585
*Sok Ying Liaw
Alice Lee Centre for Nursing Studies,
Yong Loo Lin School of Medicine,
National University of Singapore
Level 2, Clinical Research Centre, Block MD11
Singapore 117597
Email: nurliaw@nus.edu.sg
Submitted: 8 June 2021
Accepted: 11 August 2021
Published online: 4 January, TAPS 2022, 7(1), 109-111
https://doi.org/10.29060/TAPS.2022-7-1/PV2558
Jimmie Leppink
Hospital virtual Valdecilla, Spain
I. INTRODUCTION
Single case designs (SCDs) comprise repeated measurements (time series) of the same variables of interest (Van de Schoot & Miocevic, 2020) to understand changes in knowledge, skill, attitude or other constructs in a defined time period that includes one or more events or developments that may affect that change. Possible units of analysis include individuals (e.g., individual skill development), teams (e.g., team dynamics), or settings (e.g., situational-contextual change). Whether the outcome variables are quantitative (e.g., time-on-task), qualitative (e.g., changes in habits or preferences), or some combination of the two (e.g., test scores and transitions in practice strategy), a range of parametric and nonparametric statistical models are available for analysis at the level of N = 1, and the outcomes of multiple N = 1 analyses can be combined using multilevel and meta-analytic models (for reviews and examples, see: Leppink, 2020; Van de Schoot & Miocevic, 2020). This makes SCDs useful for any sample size and, contrary to traditional randomised controlled experiments and other group comparison studies, can help health professions education (HPE) researchers and practitioners to (1) Respect the dynamic nature of learning, (2) Use no more resources than needed, (3) Bridge the research-practice gap, and (4) Appreciate diversity and approach challenges in the sector accordingly. Each of these advantages is explained in the following.
II. RESPECT THE DYNAMIC NATURE OF LEARNING
Although learning by definition involves time, the vast majority of traditional randomised controlled experiments and other group comparison studies focus on performance at a single occasion or at best at two occasions. SCDs can incorporate quantitative and qualitative information to understand the longitudinal and non-linear nature of learning, effects of interventions or events, and possibly the temporal order of changes. For example, in a five-year medicine program in which we assess knowledge, skill and attitude every 3-4 months in each year of the program, we can monitor change in each of these variables and study possible temporal orders in changes at the level of the individual student as well as – through multilevel and meta-analytic models that combine individual outcomes – at the level of a larger group (e.g., changes in attitude tending to precede changes in knowledge, or the other way around). Although a commonly perceived limitation of SCDs is a lack of generalisability to larger populations, generalisability is not always of interest in our field (e.g., ‘what is the level of competence of this resident at this point?’, or ‘does this simulation session contribute to more effective communication in this team in this hospital?’), and where it is of interest (e.g., under which conditions can the use of virtual reality games help to improve communication skills?), it can be increased through replication studies from different settings the findings of which are combined in multilevel and meta-analytic models.
III. USE NO MORE RESOURCES THAN NEEDED
While traditional randomised controlled experiments and other group comparison studies with a limited number of measurements (usually one or two) often require more than 100 participants, SCDs – through their use of series of repeated measurements – allow researchers and practitioners to investigate educationally interesting phenomena with any number of individuals, teams or situations including one (i.e., N = 1). This is great for example for institutions that do not have large numbers of students or residents (e.g., eleven students or six residents) and do not pretend that the outcomes of their study can be generalised to all of the rest of the world, and is one of the reasons why in some clinical areas (Van de Schoot & Miocevic, 2020) and some areas in education (Leppink, 2020) SCDs have already been used successfully for a while. In addition, not using more resources than needed is always important and even more so in times of enormous pressure on healthcare systems across the world. To use an example from assessment practice, decisions about the progression of individuals or teams usually require longer exams when performance is borderline (i.e., almost at the expected level with minor lapses that would not cause concerns for patient outcomes) compared to where performance is good or poor. In this context, SCDs can help us determine when we have sufficient information about the knowledge (how many questions?), techniques (how many tasks?), skills (how many stations?) or attitudes (how many portfolio reflections?) of a specific individual or team being assessed in order to make informed and confident decisions.
IV. BRIDGE THE RESEARCH-PRACTICE GAP
Most group comparison studies include the unethical and often practically nonsensical action of withholding an educational intervention from some participants (control group), whereas in SCDs the question is not if but when that intervention takes place. Just like in a study on skydiving one would never include a ‘control’ condition in which participants are not allowed to open their parachute (the question should be when not if one should open that parachute), in an educational context in which the use of for instance virtual reality technology which allows students or residents to practice with complex anatomy structures in 3D is an inherent part of an anatomy training programme, including a condition in which no virtual reality technology is offered does not make sense. A more appropriate question in this context is when to use the virtual reality technology. On a related note, in complex domains such as medicine, we tend to move from simple to complex because more complex tasks require one to be able to complete a series of simpler tasks. Sticking with simple tasks only or moving from complex to simple does not make sense in this practice, and it is therefore pointless to design experiments which incorporate such conditions (i.e., a no-complex-tasks control group or a group in which we start with complex and end with simple). SCDs which introduce (more) complexity at different points in time for different participants or teams make more sense, and if that starting point is randomised for different participants, we speak of a single case experimental design (SCED; Van de Schoot & Miocevic, 2020); experimental because like in traditional experiments we have both manipulation (here: simple vs. more complex) and randomisation. SCEDs can facilitate causal inference, although where effects of several interventions are considered the complexity of the design as well as the number (generally a higher demand) and timing of measurements (sufficient measurements in each of several stages of the study) will require very careful thought. Finally, HPE is ultimately about contributing to the best possible healthcare, hence research questions on possible effects of training on future healthcare performance (e.g., are we delivering good doctors?) are key (Nickson et al., 2021; Prideaux, 2019), and the longitudinal character of SCDs allows us to study these questions.
V. APPRECIATE DIVERSITY AND ACT ACCORDINGLY
As eloquently formulated by Prideaux (2019), medical schools must “direct their activities to local priorities and to serving local health systems” (p. 25) and at the same time healthcare systems across the world share many challenges and can all benefit from solid theory on what works in which circumstances. SCD (or in experimental form called SCED) findings from different institutions or settings can be combined into meta-analyses (Van de Schoot & Miocevic, 2020) and systematic reviews, helping us to understand commonalities and diversity across institutions, to develop existing and new theory, and to approach sector challenges accordingly. Although where generalisability is of interest smaller samples tend to provide substantially less information than larger samples, many carefully performed smaller sample studies combined in meta-analyses and systematic reviews can make a more powerful and, in our field, much more useful end result than small numbers of larger sample studies. Besides, although the number of measurements needed depends on what we are measuring and not all models require large numbers of measurements (e.g., 10 measurements of the same individual for relatively simple conclusions about that individual), larger numbers of measurements – where that it is possible and makes sense in the context at hand – generally provide more information and allow for a study of more complex relations than smaller numbers of measurements.
VI. CONCLUSION
Nearly 17 years ago, Johnson and Onwuegbuzie (2004) published their immensely popular article “Mixed methods research: A research paradigm whose time has come”. SCDs allow researchers to adopt that mixed methods lens by integrating qualitative and quantitative information on complex phenomena such as learning and other types of development, to address the needs of educational and healthcare practice while using no more resources than what is needed (no more statistical power calculations for group experiments of more than 100 participants that include conditions that would never occur in educational practice), and to appreciate diversity (rather than to average where things should not be averaged). SCDs constitute a wonderful tool for research and practice in specific institutions as well as for multi-institution studies that are part of national or international collaborative projects. Recent years have resulted in parametric and nonparametric models for different types of data, which make SCDs useful regardless of the type of data we are considering. These questions and developments in combination make that the time for SCDs in HPE has come. Institutions and centres should be encouraged to use SCDs to answer local questions and serve local needs, and to document and publish findings arising from such SCDs so others can learn from these findings and design similar studies in their local contexts. Additionally, institutions and centres should consider the use of SCDs in multi-institution or multi-centre collaborations. Both ways can facilitate generalisability through meta-analysis and systematic review.
Note on Contributor
This manuscript has one author who wrote the full letter and meets all four criteria of authorship listed under International Committee of Medical Journal Editors (ICMJE); there were no other authors contributing to this letter.
Funding
No funds, grants or other support was received.
Declaration of Interest
No conflicts of interest are associated with this paper.
References
Johnson, R. B., & Onwuegbuzie, A. J. (2004). Mixed methods research: A research paradigm whose time has come. Educational Researcher, 33(7), 14-26. https://doi.org/10.3102/0013189X033007014
Leppink, J. (2020). The art of modelling the learning process: Uniting educational research and practice. Springer. https://doi.org/10.1007/978-3-030-21241-4
Nickson, C. P., Petrosoniak, A., Barwick, S., & Brazil, V. (2021). Translational simulation: From description to action. BMC Advances in Simulation, 6(6), 1-11. https://doi.org/10.1186/s41077-021-00160-6
Prideaux, D. (2019). The global-local tension in medical education: Turning ‘think global, act local’ on its head? Medical Education, 53(1), 25-31. https://doi.org/10.1111/medu.13630
Van de Schoot, R., & Miocevic, M. (2020). Small sample size solutions: A guide for applied researchers and practitioners. Routledge. https://doi.org/10.4324/9780429273872
*Jimmie Leppink
Avenida de Valdecilla,
s/n, 39008, Santander, Spain
Email: jleppink@hvvaldecilla.es
Submitted: 4 May 2021
Accepted: 22 July 2021
Published online: 4 January, TAPS 2022, 7(1), 106-108
https://doi.org/10.29060/TAPS.2022-7-1/PV2532
Shamalee Wasana Jayarathne1 & Lambert Schuwirth2
1Medical Education Unit, Faculty of Medicine and Allied Sciences, Rajarata University of Sri Lanka, Sri Lanka; 2Prideaux Centre for Research in Health Professions Education, Flinders University, Australia
Medical Professional Identity Formation (PIF) has been suggested as a fundamental outcome in medical education (Cruess et al., 2014). Medical professional identity is development of both personal and professional identity as a physician. PIF achieved in stages over time during which the characteristics, values, and norms of the medical profession are internalised, resulting in individual thinking, acting, and feeling like a physician (Cruess et al., 2014). It is basically not a process of learning to demonstrate professional behaviour but of change into a “professional being” or professional physician. Throughout the journey of PIF, moments of dissonance between personal values and professional values are likely to occur. So logically, there will be phases of learning and unlearning. Learning is generally well-defined, but unlearning has been conceptualised through different lenses both on the process of unlearning and the unlearnt content, leading to conflicting views.
Unlearning has been conceptualised through different lenses. Hislop et al. (2014) have described unlearning as “abandoning or giving up knowledge or behaviours without making any judgement on the status of the knowledge or behaviours being unlearned”. In addition, Macdonald (2002) has explained unlearning in terms of transformative unlearning, which is as a process of questioning, reflecting and giving up some core values, assumptions, knowledge and practices. On the other hand, some authors have given subjective value to unlearnt knowledge and practices. Srithika and Bhattacharyya (2009) have defined unlearning as a process that includes judging the knowledge, values or practices with current knowledge. If current knowledge is superior to previous knowledge, individuals do unlearn previous knowledge. In this background, we hypothesise unlearning to be a meta-cognitive process and not as a permanent loss of something. Instead, we recognise it as a person consciously discarding, abandoning, or giving up particular values, knowledge, or behaviour and consciously choosing not to continue using them; a meta-cognitive process.
Several authors have categorised unlearning in various ways, which leads to sometimes conflicting views on the characteristics of the process of unlearning. Rushmer and Davies (2004) have categorised unlearning into three categories namely, ‘fading’, ‘wiping’ and ‘deep unlearning’. Fading occurs due to lack of use and it occurs over time. Wiping is deliberate process, occurs due to external change or due to an experience. Wiping is a process in which unlearning of behaviours and complex social learning (beliefs, values, attitudes, assumptions, and interpersonal skills) happens. Deep unlearning was defined as a “sudden, unexpected, and potentially painful event that ruptures part of our way of being or deeply held understanding of the world” (Rushmer & Davies, 2004). They further explained that deep unlearning occurs in an unpredictable, disruptive way and it is less planned and less deliberate. It trigged by a sudden action or an event (Rushmer & Davies, 2004). Although, transformative unlearning is defined similar to the concept of deep unlearning, the characteristics of the process of unlearning are rather conflicting in deep unlearning and transformative unlearning. Transformative unlearning is conceptualised as a process of reflecting upon, questioning and giving up some values, assumptions and practices (Macdonald, 2002). This transformative unlearning process has three phases which are “receptiveness, recognition and grieving”. Hence, during this process a “person loses prior ways of seeing [which] until now had brought certainty and security”. However, this is a slow process.
There is a scarcity of empirical studies found in relation to individual unlearning process. One study in the UK explored health care managers’ engagement in unlearning and the impact of unlearning in decision making (Coombs et al., 2013). Authors distinguished two types of unlearning based on these health care managers’ experiences: “behavioural unlearning” and “cognitive unlearning”. Behavioural unlearning has similarities with wiping, whereas cognitive unlearning has similarities with deep unlearning. Behavioural unlearning is triggered by a deliberate process of change that had been externally imposed, while deep unlearning is triggered by questioning individuals’ basic assumptions due to an external event. Hence, the descriptions on characteristics of process of unlearning is conflicting in deep unlearning, transformative unlearning and cognitive unlearning and it is worth further exploration.
It is important to recognise the similarities and differences between to forgetting and unlearning. Some researchers tend to use unlearning and forgetting interchangeably (Rushmer & Davies, 2004). According to Rushmer and Davies (2004) fading occurs due to lack of use and it occurs over time. This is not an intentional action and it equals to forgetting. However, they have conceptualised fading under the concept of unlearning, which is questionable. Equally, several authors observed the contrasting nature of unlearning and forgetting. They distinguish the deliberate, conscious nature of unlearning (Coombs et al., 2013) from unintentional nature of forgetting. Our stance is that forgetting as loss of knowledge not necessarily planned or intended, which is distinct from unlearning.
Although there is conflicting conceptual literature, the concept of unlearning is worthwhile to explore; especially the different conceptual models of ‘transformative unlearning’ (Macdonald, 2002) ‘deep unlearning’ (Rushmer & Davies, 2004) and cognitive unlearning (Coombs et al., 2013) in relation to PIF in physicians. Unlearning is important in PIF process, because an inability to give up values, norms, practices when they no longer match the demand of one’s current perspectives inevitably leads to rigidity in thinking and lack of flexibility. It is plausible that individuals who enter into the career of medicine have their own personal values and assumptions or specific world views. But professional values of medicine are often a set of values defined by society and public. It is proven that, professional attributes are contextually depended. Physicians need to keep to these professional values based on the context in which they work. During the journey of PIF moments of dissonance between personal values and professional values are likely to occur. These can be struggling points for both medical students and physicians while they unlearn their worldviews and replace them by new or adapted ones. Also, there are still many unclear areas concerning PIF and unlearning. For instance, can individuals unlearn deep values and assumptions? would that process really entail deep unlearning or merely wiping? Why is this unlearning cognitively and emotionally challenging for some individuals? Exactly how does unlearning of deep values and assumptions of individuals occur during PIF of physicians is currently under-researched. Thus, understanding the process of professional identity formation in the light of unlearning of deep values and assumptions of individuals is important in medical education to support journey of PIF of physicians and medical students.
Notes on Contributors
YGSW Jayarathne, MBBS, PG Dip in MEd, MD in MEd is a Senior Lecturer in Medical Education and was involved the conceptual development, argument building, ethics application and the development of the manuscript.
Lambert Schuwirth, MBBS, MD, PhD, FANZHPE is a Professor of Medical Education and Director Prideaux Centre for Research in Health Professions Education, College of Medicine and Public Health, Flinders University and was involved the conceptual development, argument building and the development of the manuscript.
Acknowledgement
No acknowledgement is associated with this paper.
Funding
No funding sources are associated with this paper.
Declaration of Interest
There are no conflicts of interests related to the content presented in the paper.
References
Coombs, C. R., Hislop, D., Holland, J., Bosley, S. L. C., & Manful, E. (2013). Exploring types of individual unlearning by local health-care managers: An original empirical approach. Health Services and Delivery Research, 1(2), 1–146.
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2014). Reframing medical education to support professional identity formation. Academic Medicine, 89(11), 1446-1451. https://doi.org/10.1097/ACM.0000000000000427
Hislop, D., Bosley, S., Coombs, C. R., & Holland, J. (2014). The process of individual unlearning: A neglected topic in an under-researched field. Management Learning, 45(5), 540-560. https://doi.org/10.1177/1350507613486423
Macdonald, G. (2002). Transformative unlearning: Safety, discernment and communities of learning. Nursing Inquiry, 9(3), 170-178. https://doi.org/10.1046/j.1440-1800.2002.00150.x
Rushmer, R., & Davies, H. T. (2004). Unlearning in health care. BMJ Quality and Safety, 13(Suppl 2), 10-15. https://doi.org/10.1136/qshc.2003.009506
Srithika, T. M., & Bhattacharyya, S. (2009). Facilitating organizational unlearning using appreciative inquiry as an intervention. Vikalpa, 34(4), 67-78. https://doi.org/10.1177/0256090920090406
*YG Shamalee Wasana Jayarathne
Medical Education Unit,
Faculty of Medicine and Allied Sciences,
Rajarata University of Sri Lanka
Email: wasana@med.rjt.ac.lk, wjayaratna@yahoo.com
Submitted: 21 April 2021
Accepted: 7 October 2021
Published online: 4 January, TAPS 2022, 7(1), 87-97
https://doi.org/10.29060/TAPS.2022-7-1/OA2519
Nisakorn Deesaen1, Kongpop Sutantikorn1, Punyanuch Phonngoenchai1, Sakchai Chaiyamahapruk2 & Patcharada Amatyakul3
1Faculty of Medicine, Naresuan University, Thailand; 2Department of Community Medicine, Faculty of Medicine, Naresuan University, Thailand; 3Department of Obstetrics and Gynaecology, Faculty of Medicine, Naresuan University, Thailand
Abstract
Introduction: Pelvic examination of patients in the department of obstetrics and gynaecology (Ob–Gyn) is an important skill for medical students. Because it involves a physical assessment of the patients’ genitalia, patients may refuse medical students to participate in the examination, affecting the medical students’ clinical skills.
Methods: This cross–sectional study was conducted at Naresuan University Hospital to determine the factors that influence the acceptance of medical student participation in the pelvic examinations. A total of 198 out–patients from the Ob–Gyn department were included. A Likert scale questionnaire was designed which featured topics on patients’ attitudes and circumstances related to medical student involvement in gynaecological procedures.
Results: The majority of outpatients (71.7%) accepted the participation of medical students in pelvic examinations. Patients with prior experiences in physical and pelvic examination by medical students had a significant impact on the patients’ acceptance (P–value<0.001). The patients’ impressions had an influence on the decision to accept students in pelvic exam participation. Approximately 40% of patients were concerned about the breach of confidentiality. However, most patients strongly agreed that allowing medical students to perform pelvic examination would benefit their medical education.
Conclusion: Most of the participants permitted medical students to participate in pelvic examinations and preferred that the medical instructor be the one to request permission. The patients’ impressions of medical students were crucial factors that significantly influence their decision whether to allow or deny them to participate in the procedure. Disclosure of confidentiality was found to be matters of concern to most patients.
Keywords: Pelvic Examination, Medical Students, Acceptance, Performance, Clinical Teaching
Practice Highlights
- Most of the patients consent to a medical student participating in a pelvic examination.
- Medical instructors should ask for patients’ permission.
- Confidentiality and privacy of patients are critical issues that must be addressed.
- Patients’ impressions and prior examination experiences by medical students influence patients’ decisions.
I. INTRODUCTION
Medical students should learn how to perform pelvic examinations on patients during clinical years. History taking, physical examination, and pelvic examination are taught during the fourth to sixth year of medical training in our curriculum. Pelvic examination is defined as the assessment of external genitalia, speculum examination of the vagina and cervix, bimanual palpation of the uterus, adnexa and sometimes rectovaginal examination. This procedure is used to screen for gynaecological diseases and cancers in asymptomatic women and to diagnose gynaecological diseases in symptomatic women. Pelvic examination differs from other physical examinations because it involves an inspection of the genitalia, which, according to studies, commonly causes anxiety, fear, embarrassment (10–80% of women), pain, and discomfort (11–60% of women) (Bloomfield et al., 2014). Some factors why patients feel uncomfortable during a physical examination by medical students are concerns about privacy, confidentiality, and embarrassment (Rizk et al., 2002). As a result, patients may refuse to allow medical students to participate in the pelvic examination, affecting the learning experience and clinical skills of medical students. Furthermore, factors related to age, race, religion, cross–cultural differences, marital status, and previous delivery may also influence the patients’ decision to allow medical students in conducting pelvic examination (Anfinan et al., 2014; McLean et al., 2010). Compared to other ethnic and religious groups, Muslim women had a higher rate of refusing medical students, particularly male students (Nicum & Karoo, 1998). During intrapartum care, approximately 50% of Hindu and Muslim patients refused to accept medical students. Sikh and Muslim patients accepted only female medical students, 41% and 40%, respectively, whereas 59% of Christian patients accepted both female and male medical students (Nicum & Karoo, 1998). However, patients’ reasons for accepting and refusing medical student participation in pelvic examination have not been established in Southeast Asia because of limited investigation.
According to the patient’s bill of rights, patients have a right to accept or refuse the medical students’ participation. They should have the opportunity to decide if they want to contribute to the medical education or decline care from medical students (Teunissen, 2018). Approximately 26% of the patients refused to have a medical student perform a pelvic examination (Fortier et al., 2006). Previous study reported that the refusal rate increased as the level of student involvement increased, from observation to history taking to examinations and procedure, particularly with digital vaginal and rectal examination (Salah et al., 2015). In contrast, some patients accepted the medical students’ participation because they wanted to contribute to the clinical training in medical education. Because of the training process, the patients felt more confident that they would receive appropriate treatments. From the literature review, most studies were conducted in developed and some Arab countries. There are limited data from women in Southeast Asia countries on the factors and attitudes that influence their decision whether they allow or refuse medical students to participate in a pelvic examination. This research aimed at studying the patients’ characteristics, influencing factors and correlation with the acceptance of medical students, which may increase the Ob–Gyn patients to participate in clinical education.
II. METHODS
This cross–sectional descriptive study was conducted at the out–patient unit of the Department (OPD) of Obstetrics and Gynaecology, Naresuan University Hospital. Patients who visited Ob–Gyn department between November 2018 and May 2019 were included in the study. Patients under 20 years old, mentally or critically ill and unable to understand the questionnaire in Thai language were excluded in this study. All the participants were able to complete the consent forms and questionnaires independently, and were guaranteed anonymity.
The questionnaire was developed to evaluate 4 domains, as follows: (1) demographic and socio–economic data (age, gender, educational level, occupation and parity), (2) patient preference, (3) factors influencing patient receptivity of medical student involvement in pelvic examination (gender, hygiene, manner and demeanour, patients’ impressions of the medical students, prior experience in physical and pelvic examination), and (4) patients’ attitudes toward accepting medical students to conduct pelvic examination under supervision of medical instructors. Influencing factors and attitudes included in the questionnaire were modified based on a literature review. A 5–point Likert scale was used to determine the level of agreement (1= strongly agree; 2= agree; 3= neutral; 4= disagree; and 5= strongly disagree). The questionnaire was initially tested for content validity using the item-objective congruence (IOC) index, and then used in a pilot study on 30 patients who were not included in the study to ensure clarity and reliability.
A. Statistical Analysis
A Microsoft Excel spreadsheet was created for data entry and statistical analysis. Descriptive data was presented in the form of frequency, mode, and percentage. Chi-square test was calculated for proportions. The p–value of less than 0.05 was considered statistically significant.
B. Ethical Considerations
All collected data was kept confidential, and the information was used for research only. This study was approved by Naresuan University Institutional Review Board in compliance with the principles of the Helsinki Declaration.
III. RESULTS
During the study period, 236 participants were recruited from the out–patient department of Ob–Gyn, but only 198 completed the questionnaire. Most of them (99.0%) were aware that Naresuan University Hospital is a primary teaching hospital of the Faculty of Medicine, Naresuan University which provides clinical training for medical students and residents. The socio–demographic data of the study population are shown in Table 1. The data that supports the findings of this study are openly available at http://doi.org/10.17605/OSF.IO/HBV68 (Amatyakul, 2021).
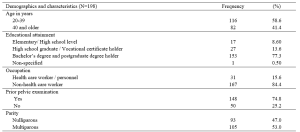
Table 1. Demographics and characteristics of the study population
From 198 participants, 71.7% accepted the medical students to participate in pelvic examination. Fifty–seven percent of the participants in the acceptor group allowed both male and female medical students, while 42.9% in the same group allowed only female medical students. The correlation between patients’ acceptance and refusal for the medical students to participate in pelvic examination showed that age, occupation and parity of the patients were not statistically different (p> 0.05). Thirty–one percent of bachelor’s degree holders and 37% of postgraduate degree holders refused the participation of medical students. The higher the patient’s educational attainment, the more likely they are to refuse a pelvic examination performed by medical students, as observed in this study. In the conduct of pelvic exam procedure, 69.3% of the patients in the acceptor group and 53.6% of the patients in the non-acceptor group felt comfortable with students present as observers. Before the students participate in a pelvic examination, most of the participants (81.4%) preferred that the medical instructors (56.6%) ask permission rather than the medical students (21.7%) or nurses (21.7%).
This research recorded 52.7% of the patients with prior experience of physical examination by medical students from other departments in Naresuan University Hospital. Thirty–two percent of the patients previously received pelvic examination by medical students (from our department or other medical training hospitals). Patients who had their physical examinations performed by medical students from other departments or had pelvic examinations performed by medical students had a statistically significant increase in allowing medical students to participate in pelvic examinations under the supervision of a medical instructor (Table 2).
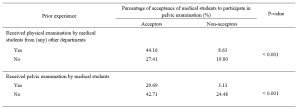
Table 2. The correlation between the acceptance of medical student participation in pelvic examination and prior experience of pelvic examination performed by medical students.
The participants’ decisions were influenced by their impressions of medical students. More than 90% of the participants believed that characteristics like manner, demeanour, cleanliness, hygiene, trustworthiness, and respect had a substantial impact on their attitudes and acceptance. Similarly, the gender of the medical students also influenced the decision of the participants (69.2%), which female students were preferred. The negative and positive attitudes of the patients related to medical student participation in pelvic examination are shown in Table 3.
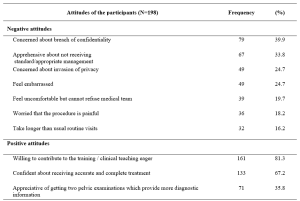
Table 3. The positive and negative attitudes of the participants about medical students’ participation in pelvic examination under the supervision of medical instructors.
IV. DISCUSSION
Our study demonstrated that 71.7% of the participants agreed to have their pelvic examinations performed by medical students. This result was comparable to the study of Western women that reported an acceptance rate ranging from 58 to 77% (Nicum & Karoo, 1998). Conversely, our acceptance rate was lower when compared to a study conducted in United Arab Emirates by Rizk et al. (2002), in which 87.1% of the out-patients in Ob-Gyn accepted the involvement of medical students. According to the results of our study, there were no statistically significant differences between acceptors and non-acceptors in terms of age, educational level, occupation, parity, or prior pelvic examination. Hartz and Beal (2000) also reported similar findings, stating that the age and education of the patients were not statistically different between the two groups. However, Rizk et al. (2002) stated that the acceptance of the patients with older age, higher parity, and higher education was statistically significant. Interestingly, there was a trend discovered in our research that patients who are highly educated were more reluctant to allow medical students in performing pelvic examination, even when supervised by medical instructors. This reluctance could be because of a strong concern for their privacy, which should be investigated further through an in-depth interview.
Prior experience of the patients receiving physical examination by medical students from other departments, and prior experience of the patients receiving pelvic examination performed by medical students significantly increased the rate of acceptance. These findings are consistent with those of Ghobain et al. (2016) who reported that a positive prior experience with a medical student was significantly related to giving medical students permission to perform a physical examination. This can be explained by the fact that these patients were already aware of the medical student involvement in performing physical examinations. Therefore, they are more likely to accept medical student participation in subsequent Ob-Gyn consultations.
One interesting finding from our study was the positive patient receptivity of medical students acting as observers during pelvic examination. Patients in approximately 70% of the acceptor group allowed other medical students to observe the examination process. Remarkably, 53.6% in the non-acceptor group was comfortable with medical students observing a pelvic examination performed by medical instructor. This would imply that even if students cannot perform pelvic examinations, they can still gain clinical knowledge through observation, and clinical instructors can take advantage of this valuable opportunity to educate their students.
Other major concern of patients is the requirement for students to obtain permission before participating in any procedures. The majority of the participants prefer that medical instructors be in charge of obtaining patient permission to allow students to perform physical examinations on their behalf. This tendency may lead to a higher rate of acceptance of student participation.
The characteristics and performance of the medical students in our study had a significant impact on patients’ decision. The external part of the female reproductive organ is a sensitive and the most private area for every woman, and patients would only allow medical students who practice good hygiene and cleanliness to participate in the examination. Furthermore, the appropriate manner and demeanour, including respectfulness and politeness toward patients, and trustworthiness of the medical students during the clinical procedure may increase the patients’ receptivity of medical students to conduct pelvic examination. Professional appearance reflecting cultural backgrounds also impacts patient preference and acceptance; therefore, medical students should dress properly (Aljoudi et al., 2016).
Several studies, including ours, found that participants felt more at ease with female students than with male students (Salah et al., 2015; Subki et al., 2018). Chang et al. (2010) reported that male students were refused by patients to participate in clinical interviews and physical examinations, including pelvic examinations. In a study conducted at Taibah University in India (Shetty et al., 2021), women significantly preferred female students during abdominal and genital examinations. As a result, it is difficult for obstetrics and gynaecology educators to consider methods of encouraging patients to accept participation of medical students, regardless of their genders.
Patients’ positive attitudes toward medical students’ participation contributed to clinical teaching, which is an important process for professional development. The patients agreed that they would receive more accurate and comprehensive treatment if they had two pelvic examinations. These details are consistent with the findings of a study conducted by Rizk et al. (2002), which revealed that 69.7% of the participants were willing to contribute to the education of students. Most participants were satisfied with the overall service because they were well informed about their care by the health care team and were actively involved in the treatment decision-making process. Like other literature (Nicum & Karoo, 1998), medical students also provided patients with useful medical information and support. Furthermore, patients strongly supported the idea that real patient encounters and practices under clinical supervision are more effective methods for improving student’s clinical skills than just mere observation or skill laboratory practice (Subki et al., 2018).
Patients’ main reasons for refusing medical students’ participation in pelvic examination were concerns about breaching their confidentiality and privacy, which were similar to a study conducted in London. According to the findings, the common reasons for patients’ uneasiness with participation of the medical students were related to privacy, receiving lower standard of care, examinations, lack of control over the student’s level of involvement, and a longer consultation time (Ryder et al., 2005). The participants in our study were also concerned about taking a longer than usual routine visit. Not only applicable in Ob-Gyn department, patients’ perceptions of students’ professionalism and respect for privacy were significantly related to the acceptance of medical students’ participation in surgical ward (Ghobain et al., 2016). Thus, all medical students must be informed about the doctor-patient relationship and the importance of maintaining patient confidentiality. Medical instructors must inform and reassure patients about their confidentiality. Before participating in any clinical teachings, medical instructors should explain to students their roles and responsibilities. To minimise patients’ feeling of discomfort, these roles and responsibilities should be conveyed and explained to them before asking for their approval.
This paper has highlighted the significance of patients’ attitudes toward medical students’ manner and demeanor, which greatly influences patients’ decision-making process. However, some limitations should be considered, such as the fact that all participants were Thai, and that the study was carried out in one of the Southeast Asia countries where data on the attitudes of female patients had not been thoroughly investigated. Since socio-demographic factors and cultural issues vary across Southeast Asia, the results of this research only represent the characteristics of the Thai population and not the entire region. Additionally, this cross-sectional study could not establish the reasons for patients’ negative attitudes toward student involvement in pelvic examination. Therefore, it is suggested that future research use in-depth interview methodology to gather more information from both the acceptor and non-acceptor groups.
V. CONCLUSION
Most of patients agreed to medical students participating in pelvic examinations and preferred medical instructors to be the persons to ask patients for permission. Essentially, patients’ confidentiality and privacy must always be safeguarded. The performance of medical students, and their observance of patient privacy and confidentiality are crucial factors in gaining the patient’s approval. Furthermore, the gender of the medical student influences the patient’s acceptance and comfort level in student’s involvement. Clinical instructors must effectively convince patients in gynaecology department to allow male medical students to perform gynaecologic procedures.
Notes on Contributors
Nisakorn Deesaen, Punyanuch Phonngoenchai, and Kongpop Sutantikorn contributed to the literature review, concept development, questionaire design, data collection, data analysis, and manuscript finalisation. Sakchai Chaiyamahapruk was involved in the study design, data analysis, and manuscript finalisation. Patcharada Amatyakul contributed to the literature review, concept development, study design, data analysis, and manuscript writing and finalisation.
Ethical Approval
Ethical approval for this study was obtained from the Naresuan University Institutional Review Board, Naresuan University, Thailand (Ethics approval number IRB 0653/60).
Data Availability
The data that support the findings of this study are publicly available in Open Science Framework repository, http://doi.org/10.17605/OSF.IO/HBV68.
Acknowledgement
The authors would like to express their gratitude to the nurses at the out-patient unit of the Department of Obstetrics and Gynaecology, Naresuan University Hospital, for their help in distributing and collecting questionnaires from the patients.
Funding
This research received no specific grant from any funding agency.
Declaration of Interest
The authors declare no conflict of interest.
References
Aljoudi, S. B., Alsolami, S. S., Farahat, F. M., Alsaywid, B., & Abuznadah, W. (2016). Patients’ attitudes towards the participation of medical students in clinical examination and care in Western Saudi Arabia. Journal of Family and Community Medicine, 23(3), 172‑178. https://doi.org/10.4103/2230-8229.189133
Amatyakul, P. (2021). Proposal for patients’ attitude and factors influencing the acceptance of medical students’ participation in pelvic examination. [Data set]. Open Science Framework. http://doi.org/10.17605/OSF.IO/HBV68
Anfinan, N., Alghunaim, N., Boker, A., Hussain, A., Almarstani, A., Basalamah, H., Sait, H., Arif, R., & Sait, K. (2014). Obstetric and gynecologic patients’ attitudes and perceptions toward medical students in Saudi Arabia. Oman Medical Journal, 29(2), 106-109. https://doi.org/10.5001/omj.2014.26
Bloomfield, H. E., Olson, A., Greer, N., Cantor, A., MacDonald, R., Rutks, I., & Wilt, T. J. (2014). Screening pelvic examinations in asymptomatic, average-risk adult women: An evidence report for a clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 161(1), 46–53. https://doi.org/10.7326/M13-2881
Chang, J. C., Odrobina, M. R., & McIntyre-Seltman, K. (2010). The effect of student gender on the obstetrics and gynecology clerkship experience. Journal of Women’s Health, 19(1), 87-92. https://doi.org/10.1089/jwh.2009.1357
Fortier, A. M., Hahn, P. M., Trueman, J., & Reid, R. L. (2006). The acceptance of medical students by women with gynaecology appointments. Journal of Obstetrics and Gynaecology Canada, 28(6), 526-530. https://doi.org/10.1016/S1701-2163(16)32179-X
Ghobain, M. A., Alghamdi, A., Arab, A., Alaem, N., Aldress, T., & Ruhyiem, M. (2016). Patients’ perceptions towards the participation of medical students in their care. Sultan Qaboos University Medical Journal, 16(2), 224–229. https://doi.org/10.18295/squmj.2016.16.02.014
Hartz, M. B., & Beal, J. R. (2000). Patients’ attitudes and comfort levels regarding medical students’ involvement in Obstetrics–Gynecology outpatient clinics. Academic Medicine, 75(10), 1010-1014. https://doi.org/10.1097/00001888-200010000-00018
McLean, M., Al Ahbabi, S., Al Ameri, M., Al Mansoori, M., Al Yahyaei, F., & Bernsen, R. (2010). Muslim women and medical students in the clinical encounter. Medical Education, 44(3), 306-315. https://doi.org/10.1111/j.1365-2923.2009.03599.x.
Nicum, R., & Karoo, R. (1998). Expectations and opinions of pregnant women about medical students being involved in care at the time of delivery. Medical Education, 32(3), 320-324. https://doi.org/10.1046/j.1365-2923.1998.00205.x.
Rizk, D. E. E., Al-Shebah, A., El-Zubeir, M. A., Thomas, L. B., Hassan, M. Y., & Ezimokhai, M. (2002). Women’s perceptions of and experiences with medical student involvement in outpatient obstetric and gynecologic care in the United Arab Emirates. American Journal of Obstetrics and Gynecololgy, 187(4), 1091-1100. https://doi.org/10.1067/mob.2002.126284.
Ryder, N., Ivens, D., & Sabin, C. (2005). The attitude of patients towards medical students in a sexual health clinic. Sexually Transmitted Infection, 81(5), 437–439. https://doi.org/10.1136/sti.2004.014332.
Salah, A. B., Mhamdi, S. E., Bouanene, I., Sriha, A., & Soltani, M. (2015). Patients’ attitude towards bedside teaching in Tunisia. International Journal of Medical Education, 6, 201-207. https://doi.org/10.5116/ijme.5669.ea24.
Shetty, P. A., Magazine, R., & Chogtu, B. (2021). Patient outlook on bedside teaching in a medical school. Journal of Taibah University Medical Sciences, 16(1), 50-56. https://doi.org/10.1016/j.jtumed.2020.10.002
Subki, A. H., Algethami, M. R., Addas, F. A., Alnefaie, M. N., Hindi, M. M., & Abduljabbar, H. S. (2018). Women’s perception and attitude to medical students’ participation in obstetrics and gynecology care. Saudi Medical Journal, 39(9), 902-909. https://doi.org/10.15537/smj.2018.9.22668
Teunissen, P. W. (2018). An inconvenient discussion. Medical education, 52(11), 1104-1110. https://doi.org/10.1111/medu.13689
*Patcharada Amatyakul
Department of Obstetrics and Gynaecology,
Faculty of Medicine, Naresuan University,
99 Thaphoe District, Muang,
Phitsanulok, 65000 Thailand
Tel: 66-86-397-3455
Email: pamatyakul@hotmail.com
Submitted: 14 April 2021
Accepted: 24 June 2021
Published online: 4 January, TAPS 2022, 7(1), 98-101
https://doi.org/10.29060/TAPS.2022-7-1/SC2517
Lean Heong Foo & Marianne Meng Ann Ong
Department of Restorative Dentistry, National Dental Centre Singapore, Singapore
Abstract
Introduction: Team-based learning (TBL) pedagogy is a structured, flipped classroom approach to promote active learning. In April 2019, we designed a TBL workshop to introduce the New Classification of Periodontal Diseases 2017 to a group of general dental practitioners (GDPs). We aimed to investigate GDPs feedback on learning this new classification using TBL pedagogy.
Methods: Two articles related to the 2017 classification were sent to 22 GDPs 2 weeks prior to a 3-hour workshop. During the face-to-face session, they were randomly assigned to five groups. They participated in individual and group readiness assurance tests. Subsequently, the GDPs had inter- and intragroup facilitated discussions on three simulated clinical cases. They then provided feedback using a pen-to-paper survey. Based on a 5-point Likert scale (1-strongly disagree to 5-strongly agree), they indicated their level of agreement on items related to the workshop and their learning experience.
Results: Majority (94.7%, 18 out of 19 GDPs) agreed the session improved their understanding of the new classification and they preferred this TBL pedagogy compared to a conventional lecture. All learners agreed they can apply the knowledge to their work and there was a high degree of participation and involvement during the session. They found the group discussion and the simulated clinical cases useful.
Conclusion: A TBL workshop is suitable for clinical teaching of the New Classification of Periodontal Diseases 2017 for GDPs. Its structure promotes interaction among learners with the opportunity to provide feedback and reflection during the group discussions. This model might be a good pedagogy for continuing dental education.
Keywords: Team-based Learning, General Dental Practitioners, New Classification of Periodontal Diseases
I. INTRODUCTION
Team-based learning (TBL) is a flipped classroom, structured learning pedagogy that was introduced by Larry Michaelsen and has gained popularity among healthcare educators recently. TBL is learner-centric and dialectic based, and practices logical discussion used for determining the truth of a theory or opinion (Michaelsen et al., 2008). It provides the opportunity for peer-teaching by group members and can assist weaker students in understanding course materials.
Several dental educators have utilised TBL in undergraduate dentistry programmes and observed higher engagement among learners, less student contact time and faculty time, and higher course grades (Haj-Ali & Al Quran, 2013). General dental practitioners (GDPs), unlike undergraduate dental students, juggle between busy dental practice and family life. Hence, GDPs might seek active learning with direct knowledge application to manage their continuing dental education needs efficiently. The World Workshop of Periodontology recently revamped the diagnosis of periodontal diseases and proposed a new classification of staging (Stage I-IV; based on severity of disease) and grading (Grade A-C; based on disease progression) for periodontitis (Tonetti et al., 2018). We aimed to investigate GDP feedback on learning this new classification using TBL pedagogy.
II. METHODS
This is a descriptive study on GDPs’ feedback on learning the New Classification of Periodontal Diseases 2017 using a TBL approach. 22 GDPs attended the TBL workshop in April 2019.
Two articles related to the new classification were sent to the GDPs 2 weeks prior to the 3-hour workshop. Five multiple-choice questions were crafted from the two articles (Individual Readiness Assurance Test, IRAT) to assess learners’ basic understanding of the new classification. Learners were divided into five groups to discuss IRAT and provide answers using the immediate feedback assessment technique card (Group Readiness Assurance Test, GRAT). Faculty then highlighted key elements of the new classification. Three clinical periodontal cases crafted based on the 4S framework principles i.e. same problem, significant problem, specific choice, and simultaneous reporting, were used in the application process (Michaelsen et al., 2008). The key question was to diagnose the periodontal condition based on the staging and grading criteria. Lastly, learners provided implied consent by answering an anonymous pen-to-paper survey voluntarily. They answered based on their level of agreement on a 5-point Likert scale (5 indicating strongly agree, 1 indicating strongly disagree). The survey comprising 13 education-related statements: two statements related to programme content, two to presentation, six to learning experience, and three about the workshop. Three qualitative questions in the survey were: “What do you like most about the workshop?”, “What aspects of the session could be improved?” and “Other comments and feedback”.
III. RESULTS
Nineteen out of the 22 GDPs who attended the TBL workshop responded to the survey (response rate 86.4%). Results are summarised in Figure 1. We conducted a reliability analysis on the perceived task values scale comprising two subscales (learning experience and workshop) with at least three items.
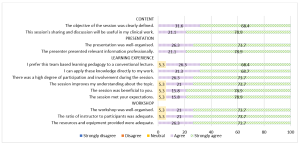
Figure 1. Learners’ feedback about the workshop
A. Content (Two items)
During the workshop, we highlighted the staging and grading criteria for the new classification. Learners provided a mean score of 4.74 (standard deviation, SD, 0.446; median 5) in two statements related to content. In general, 68.4% of them strongly agreed and 31.6% agreed the objective of the workshop was clearly defined. There were 78.9% and 21.1% of learners who strongly agreed and agreed respectively that the sharing and discussion during the workshop was useful to their clinical work.
B. Presentation (Two items)
Learners gave a mean score of 4.76 for presentation (SD 0.431; median 5). There were 73.7% learners who strongly agreed and 26.3% who agreed that the presentation was well-organised. In addition, 78.9% and 21.1% of the learners strongly agreed and agreed respectively that the presenter presented relevant information professionally.
C. Learning Experience (Six items)
Cronbach’s alpha for the learning experience subscale reached acceptable reliability at α = 0.81. The mean score for learning experience was 4.70 (SD 0.531; median 5). There were 68.4% learners who strongly agreed and 26.3% who agreed that they prefer TBL pedagogy to a conventional lecture. Also, 68.7% of the learners strongly agreed and 31.3% agreed they could apply the knowledge directly to their work. All learners agreed that there was a high degree of participation and involvement during the session. 18 learners (94.7%) agreed that the session met their expectations and improved their understanding about the topic.
D. Workshop (Three items)
The mean score for learners’ feedback on the workshop was 4.71 (SD 0.533; median 5). 18 learners (94.7%) agreed that the workshop was well organised with an adequate ratio of instructor to participants (2:22). There were 73.7% learners who strongly agreed and 26.3% who agreed that resources and equipment provided were adequate. Cronbach’s alpha for the workshop subscale reached acceptable reliability at α = 0.75.
E. Qualitative Feedback
The learners cited the following themes as their favourite component of the workshop: “group interaction and discussion” (4), “clinical case discussion” (3), “useful and relevant clinical cases” (1), “interesting readiness assurance test” (1), and “pre-reading material” (1). They also cited “active learning” (1), “correct wrong understanding” (1), “discussion improves my understanding” (1), and “great information and lecturer” (1) as positive learning experiences. Three different learners provided feedback of “best workshop ever attended”, “well done”, and “very good” respectively. One learner commented that the air-conditioning in the room was cold. One learner commented on small font size in dental charting and another learner suggested “less tests at the start”.
IV. DISCUSSION
The flipped classroom concept in TBL was suitable for GDPs to study the pre-reading articles at their own pace. The structured workshop enabled them to correct any misconception immediately and deepen their understanding about the new classification. This observation concurs with the finding that all GDPs agreed they could apply the knowledge to their work and preferred this pedagogy over a traditional lecture. This active learning process differs from a conventional didactic lecture, which is faculty-centric with less feedback and interaction. Hence, this pedagogy can be applied for some continuing dental education programmes by improving the delivery and application of new concepts. The 4S framework in the application cases are key elements to promote productive and logical discussion similar to a debate facilitated by faculty. The problem-solving aspect of TBL, along with the scaffolding and guidance by faculty, can enhance the metacognition process among learners (Hrynchak & Batty, 2012). Almost all learners agreed there was an adequate ratio of faculty to participants, emphasising the benefit of using TBL workshops to teach a large group of learners with less faculty. However, faculty needs to work more in planning and preparing the teaching materials, executing, and facilitating the session following the TBL structure and process. In addition, hurdles in conducting TBL include acceptance from faculty and learners, difficulty in supervising a large group, the customisation of the course content, and adequate training and expertise to conduct TBL effectively.
The learners also cited “group interaction and discussion” as their favourite component of the workshop. The learning theory underpinning TBL is the constructivist learning theory where the faculty exposes knowledge inconsistency during group discussion, subsequently allowing a new mental framework to be built upon the new understanding (Hrynchak & Batty, 2012). TBL is useful in healthcare education since it can promote good critical thinking and teamwork. In addition, the intra- and intergroup formal discussion provides the opportunity to reflect, give feedback, and enable peer-teaching. Self-reflection enables learners to make a judgement when modifying their existing knowledge. Peer-to-peer teaching in TBL enhances learning and aids weaker learners to understand the course material (Park et al., 2014).
Some limitations of our study were that the sample size was small, reporting participants’ self-perception on how they felt after attending the workshop and the lack of longitudinal follow-up on retention of knowledge. In addition, we did not have a separate didactic lecture on the new classification as a control group to truly compare the two different modes of teaching. Future recommendation includes having two groups of GDPs to collate their perceptions as well as include a pre and post assessment to investigate the difference in improvement and in knowledge retention comparing TBL workshop and traditional didactic lecture, and include peer evaluation in TBL to increase accountability among learners. Besides, ethnographic research method can be explored to provide insight to researchers to understand the essence of how dental professionals learn during TBL. It would be meaningful to follow up this group of GDPs to assess the accuracy of their periodontal diagnoses based on the new classification to investigate the effectiveness of the TBL workshop. Of note, TBL workshops can be adapted into an online format; this is particularly useful during the current COVID-19 pandemic to engage learners and promote active learning in an online setting.
V. CONCLUSION
In conclusion, TBL pedagogy may be another mode of teaching for GDPs in continuing dental education where participants are actively engaged, and direct application of knowledge gained can be made. During this pandemic, where face-to-face sessions are minimised, educators can consider adopting TBL pedagogy on an online platform to improve learning experience and engagement of their learners.
Notes on Contributors
Dr Lean Heong Foo is a Consultant Periodontist in Department of Restorative Dentistry and Head to the Dental Surgery Assistant Certification Programme in National Dental Centre Singapore. FLH reviewed the literature, contributed to study conception, data acquisition, data analysis, drafted and critically revised the manuscript.
Dr Marianne M. A. Ong is a Senior Consultant Periodontist & Director of Education in National Dental Centre Singapore. MO contributed to study conception, data acquisition and critically revised the manuscript. All authors gave their final approval and agreed to be accountable for all aspects of the work.
Ethical Approval
This study was exempted from formal Centralised Institutional Review Broad review by SingHealth Institutional Review Board (CIRB Ref: 2021/2133).
Data Availability
Data is deposited at Figshare. https://doi.org/10.6084/m9.figshare.14411858
Acknowledgement
The authors would like to thank Ms Safiyya Mohamed Ali for providing editorial support.
Funding
There was no funding involved in the preparation of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Haj-Ali, R., & Al Quran, F. (2013). Team-based learning in a preclinical removable denture prosthesis module in a United Arab Emirates dental school. Journal of Dental Education, 77(3), 351–357.
Hrynchak, P., & Batty, H. (2012). The educational theory basis of team-based learning. Medical Teacher, 34(10), 796–801.https://doi.org/10.3109/0142159X.2012.687120
Michaelsen, L. K., Parmelee, D. X., McMahon, K. K., & Levine, R. E. (2008). Team-based learning for health professions education: A guide to using small groups to improving learning. Stylus.
Park, S. E., Kim, J., & Anderson, N. K. (2014). Evaluating a team-based learning method for detecting dental caries in dental students. Journal of Curriculum and Teaching, 3(2), 100-105. https://doi.org/10.5430/jct.v3n2p100
Tonetti, M. S., Greenwell, H., & Kornman, K. S. (2018). Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. Journal of Periodontology, 89(Suppl 1), S159–S172. https://doi.org/10.1002/JPER.18-0006
*Foo Lean Heong
National Dental Centre Singapore,
5, Second Hospital Avenue,
168938 Singapore
Email: foo.lean.heong@singhealth.com
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









