Combination of Teddy Bear Hospital and Virtual Reality Training increases empathy of medical students
Submitted: 5 January 2022
Accepted: 24 February 2022
Published online: 5 July, TAPS 2022, 7(3), 33-41
https://doi.org/10.29060/TAPS.2022-7-3/OA2739
Javier Zheng Huan Thng1, Fion Yun Yee Tan1, Marion Margaret Hui Yong Aw1,2 & Shijia Hu3
1Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Paediatrics, Khoo Teck Puat-National University Children’s Medical Institute, National University Health System, Singapore; 3Faculty of Dentistry, National University of Singapore, Singapore
Abstract
Introduction: In paediatric practice, healthcare professionals are required to connect with the child and interact at his/her level. However, it can be very difficult for medical students to put themselves in the shoes of the young child, to empathize and understand how a child actually feels while being treated. The Teddy Bear Hospital (TBH) can serve as a platform for medical students to learn how to communicate and empathise with children. Additionally, virtual reality (VR) can be used to portray a child’s viewpoint. This study aims to assess how TBH and VR can improve learning outcomes for medical students.
Methods: A cohort study was conducted on 20 first-year medical students taking part in TBH sessions. The medical students did a Pre-, Post- and 1-year Post-intervention Jefferson Scale of Empathy to assess their empathy levels. They also completed a 1-year Post-intervention quantitative and qualitative survey on their experience.
Results: There was a significant increase in Jefferson score compared to Pre-intervention (116.95 ± 8.19) for both Post-intervention (121.65 ± 11.03) and 1-year Post-intervention (123.31 ± 8.86). More than 80% believed that participating in TBH improved their confidence and ability to interact with children, while 50% felt that VR scenarios helped prepare them for the TBH. Thematic analysis of qualitative responses described (1) Personal development, (2) Insights into interacting with children, and (3) Structure and curriculum.
Conclusion: TBH improved empathy and communication with children among pre-clinical medical students and the use of VR can be used to augment sessions.
Keywords: Education, Medical Student, Simulation Training, Teddy Bear Hospital, Virtual Reality
- The Teddy Bear Hospital sessions, consisting of physical simulation of medical scenarios with children, increased empathy of medical students.
- The use of virtual reality scenarios to portray the viewpoint of a child can augment the teaching of the Teddy Bear Hospital.
- The Teddy Bear Hospital and virtual reality sessions improved the comfort, increased confidence, and self-perceived ability of interacting with children in medical students.
I. INTRODUCTION
In paediatric practice, healthcare professionals are required to connect with the child and interact at his/her level. This is especially important, when the child is encountering new and unfamiliar situations or when they are unwell and face potentially challenging and painful procedures (Mead & Bower, 2002). However, it can be very difficult for new practitioners to put themselves in the shoes of the young child, to empathise and understand how a child actually feels while being treated (Dwamena et al., 2012). This is particularly true for medical students, who not only have to grapple with the unfamiliar medical aspects of pediatric disease, but may also need to manage a frightened and uncooperative child at the same time (MacDonald-Wicks & Levett-Jones, 2012). Furthermore, having limited interaction with children means that most medical students have a difficult time empathising with them.
Empathy is an important element in a physician-patient relationship, as it has shown to improve communication and therapeutic goals (Mercer & Reynolds, 2002). However, several studies have shown significant decrease in empathy over the course of medical school (Neumann et al., 2011). Although there have been numerous methods and approaches developed to enhance empathy in medical students (Batt-Rawden et al., 2013), including interventions based around the patient narrative (e.g. creative writing, blogging, drama, poetry, fiction, and film), problem-based learning, interpersonal skills training, patient interviews, and experiential learning (simulation of patient experience). Among these interventions, experiential (immersive) learning experiences have shown promising results (Halton & Cartwright, 2018). These scenarios can be conducted either physically or virtually. It can involve the learner completing a simulated task or experience a scenario from the point of view of someone else so as to put themselves in someone else’s shoes.
The advent and advancement of virtual reality (VR) media provide the opportunity for the portrayal of different viewpoints (Lok et al., 2006). A recent study found that empathy in medical students was improved with VR portraying the viewpoint of an older patient with conditions such as macular degeneration and hearing loss (Dyer et al., 2018). However, there has not been any research done on the use of VR to simulate the point of view of a child in a medical setting. The power of immersive media can be harnessed to simulate interactions between a child and healthcare professionals, exhibiting both positive and negative examples. More importantly, it can be used to introduce an inexperienced practitioner to the viewpoint of a child patient. This will help foster empathy and drive home the effectiveness of behaviour management skills (Stewart et al., 2013).
The Teddy Bear Hospital (TBH) is an international initiative, carried out by students from Medical Faculties, aimed at reducing children’s anxiety around medical environments, procedures and professionals (Bloch & Toker, 2008; Santen & Feldman, 1994; Siegel et al., 2018). TBH simulates the different medical environments and clinical situations which children may encounter in a friendly manner using they own toys (such as teddy bears). This simulation takes the form of multi-station role-plays, which could include a check-up by the doctor, watching a doctor applying a cast for a limb fracture or performing a procedure (e.g., taking a blood sample), or receiving an injection (all performed on teddy bears, who are the patients). In addition to reducing anxiety in young children, the TBH has also been used to teach medical students communication with children in a medical setting (Nheu et al., 2018; Ong et al., 2018). Although the qualitative feedback from medical students have been generally positive (Nheu et al., 2018; Ong et al., 2018), there have not been objective measures of the effect of the TBH on the empathy of medical students.
Both VR and TBH are immersive interventions that can potentially increase the empathy of medical student, they can also improve the learning experience by allowing students to experience effective techniques to interact with children and practice those techniques. However, each intervention has inherent disadvantages. VR usually follows a scripted scenario that does not allow students to practice and interact in real-time. While TBH is time and resource intensive, and cannot be conducted is situations such as a pandemic. Therefore, evaluating the effects of a combination of the 2 techniques can inform on the individual effectiveness as well as in combination.
This study aims to determine the effect of virtual and physical simulation on the empathy and learning experience of medical students. This will be done through a combination of VR instruction and practical simulation in a TBH experience, in which medical students are exposed to and educated on the positive interactions with a child patient in various medical scenarios.
II. METHODS
This is a cohort study of first year medical students who took part in TBH sessions in January 2020 and were followed up in January 2021. Subjects were recruited from volunteers who signed up to participate in TBH sessions. Subjects were reassured that their responses are strictly confidential and will have no impact on their grades or teaching received. Medical students who have participated in previous TBH sessions were excluded. Written informed consent was taken prior to participation. This study was approved by the Institutional Review Board (NUS-IRB Reference Number: S-19-151) and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
As this was a pilot study, no sample size calculation was conducted prior to study initiation.
A. Survey Content and Timing
The Jefferson Scale of Empathy (Sidney Kimmel Medical College, Thomas Jefferson University, PA, USA) was used to assess the level of empathy (Hojat et al., 2018). It is a 20-item scale that was developed specifically to measure empathy in health professions education, including medical students. The S-version of the survey, for medical students, was administered in this study. The survey forms were purchased from Thomas Jefferson University, Center for Research in Medical Education and Health Care. The Jefferson scores were calculated out of a maximum of 140. The survey was conducted in its original English version as the language medium for education in Singapore is English and all participants are proficient.
1) Pre-intervention: Prior to the TBH session, the subjects completed the Jefferson Scale of Empathy to assess baseline empathy scores. The subjects then underwent a small group teaching session of one hour including viewing of two VR scenarios, conducted by the same instructors (JT & FT). The small group teaching sessions covered topics pertaining to doctor-patient relationship, and the developmental and psycho-affective challenges of interacting with children. The two VR scenarios depicted a child’s point of view in the setting of getting an injection (mooc vid, Scenario 1, 2019) and visiting the dentist (mooc vid, Scenario 2, 2019). The scenarios are interactive and the point of view can be manipulated by the viewer. After watching the VR scenarios, discussions where subjects can critique the healthcare providers’ actions and share their learning points were carried out. During this session, the subjects were also briefed about the different scenarios in the TBH session, including the content to be covered.
2) TBH session: The TBH session consisted of 5 scenarios namely: (1) Orthopedic Specialist: Meet Mr. Bones, (2) Respiratory Therapist: Help Teddy Breathe, (3) Family Medicine: Help Teddy Stay Healthy, (4) Personal Hygiene: Help Teddy Stay Clean, (5) Operating Theatre: Teddy has a Painful Tummy. The injection process and dental procedures were incorporated into scenarios 3 and 4 respectively. The medical students were divided into teams of 2 to 3, each interacting with a group of 5 to 8 children of the same age. Each team rotated through the different scenarios for 10 minutes. At each scenario, the medical students explained the task to the children and conducted hands-on simulation.
3) Post-intervention: After their first TBH session, the subjects completed a second Jefferson Scale of Empathy.
4) 1-year Post-intervention: One year after the TBH session, students completed a third Jefferson Scale of Empathy, along with a self-administered survey regarding the long-term impact of TBH sessions and the effectiveness of the VR scenarios.
To assess the long-term impact of TBH sessions and the effectiveness of the VR scenarios, a 1-year Post-intervention survey was administered in December 2020. The survey was adapted from a previous study (Ong et al., 2018) and piloted for understanding and readability.
The 1-year Post-intervention impact of TBH sessions was assessed using five questions on a 5-point Likert scale (strongly disagree, disagree, neutral, agree, strongly agree) regarding the effect of TBH sessions on improving the medical student’s ability, confidence and comfort level in communicating with children, and ability to empathize with children’s fear in the healthcare environment. Similarly, the effectiveness of the VR scenarios was assessed using three questions on a 5-point Likert scale, regarding the effect of the VR scenarios on preparation for TBH session, as well as improving the comfort level and confidence in engaging children. The remaining two questions obtained qualitative feedback regarding any difficulties faced as well as takeaways obtained during the TBH session.
B. Data Collection
The subjects completed the TBH sessions in small groups of up to eight volunteers, with up to 30 children, aged between 4 to 8 years old, in each session. It was explained to the children that they were participating in an activity to teach them about what happens during visits to a doctor. These sessions were conducted at the participating pre-schools with medical instruments and teddy bears as simulated patients.
Due to the COVID-19 pandemic situation and restrictions, the survey was collected via an online survey, instead of a planned Focused Group Discussion.
C. Data Analysis
Normality of data was checked using the Shapiro-Wilk test, data analysis of the Jefferson Scale of Empathy score was done via Paired samples correlation, Cohen’s d score and Paired Samples T test using Statistical Package for Social Sciences (SPSS) software (IBM SPSS Statistics 26, Armonk, NY, USA). Descriptive statistics were presented for the survey on learner experience.
Qualitative analysis was done on the medical students’ open-ended responses regarding the long-term impact of TBH sessions and the effectiveness of the VR scenarios. Using thematic content analysis and a qualitative descriptive framework (Creswell & Poth, 2019), emerging themes and illustrative quotes for each theme were extracted. The codes and themes were first done independently by two of the authors (JT & FT), any discrepancies were discussed and reconciled. After which, 2 other authors (SH & MA) reviewed and verified the finalised codes and themes, which were mapped for interpretation. Descriptive summaries and illustrative quotes were used to describe each theme.
III. RESULTS
A. Study Demographics
In total, 20 first time participants were recruited and consent was taken. All 20 were first year medical students; 9 males and 11 females. All participants (n=20) completed the Pre-intervention and Post-intervention survey while 16 completed the 1-year Post-intervention survey, with 4 participants declining to participate in the follow-up. The data that support the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.figshare.17973662 (Hu, 2022).
B. Jefferson Scale of Empathy
There was a significant (p=0.026) increase in the Jefferson score between the Pre-intervention (116.95 ± 8.19) and Post-intervention (121.65 ± 11.03). Similarly, there was a significant (p=0.002) increase from the Pre-intervention to 1-year Post-intervention (123.31 ± 8.86). (Figure 1) However, there was no difference between the Post-intervention and 1-year Post-intervention scores.
Cohen’s d score was used to determine the effect size of the intervention on the mean difference between the Pre- and Post-intervention score (0.48), and the Pre- and 1-year Post-intervention score (0.72). This corresponds to a medium effect of the intervention on the mean differences.
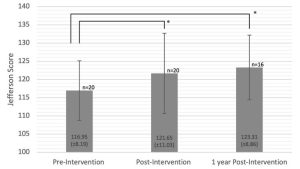
Figure 1. Jefferson Scale of Empathy Score before, immediately after and 1 year after TBH. Error bars represent the standard deviation. Asterisk (*) indicate significant differences between the groups, p<0.05.
C. Quantitative Survey
Quantitative responses from the survey on learner experience were categorised into positive responses (agree, strongly agree) and negative/neutral responses (neutral, disagree, strongly disagree). The total number of responses collected was 16 at 1-year Post-intervention (Table 1).
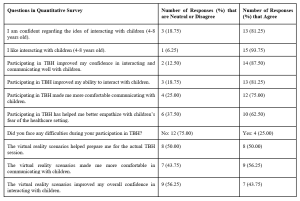
Table 1. Subject’s perception towards their TBH experience
The subjects were generally confident (75%) and enjoyed interacting with young children (94%). More than 80% believed that participating in TBH improved their confidence and ability to interact with children, and 75% felt that participating in TBH made them more comfortable communicating with children. 63% felt that TBH helped improve their ability to empathize with children’s fears of the healthcare setting. Overall, 75% of subjects did not face difficulties during the TBH sessions. In terms of the VR scenarios, around 50% felt that it was effective in preparing for the actual TBH session, with 56% feeling more comfortable and 44% feeling more confident interacting with children.
D. Qualitative Survey
Three major themes were generated from the analysis of the open-ended responses from 16 of the 20 subjects: (1) Personal development, (2) Insights into interacting with children and (3) Structure and curriculum of TBH. These themes were further categorised into sub-themes as shown in Table 2.
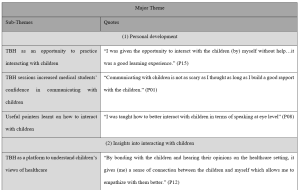
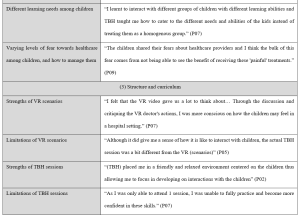
Table 2. Major themes, sub-themes and transcript highlights of qualitative survey
1) Personal development
TBH provided an opportunity for medical students in this study to interact with children in a safe and stress-free environment. These students would otherwise have limited experience communicating with children in that age-group, until actual clinical interactions with sick children.
“I was given the opportunity to interact with the children (by) myself without help…it was a good learning experience.” (P15)
The experience gave these medical students more confidence and reduced their anxiety about interacting with children, as they realized that it was not as difficult as they thought to communicate with children.
“Communicating with children is not as scary as I thought as long as I build a good rapport with the children.” (P01)
Medical students also learnt useful pointers on how to interact and communicate with children, which alleviated their worries and improved their confidence. These pointers include using simpler words, hand actions, speaking at eye level and being more expressive.
“(TBH) allowed me to practice how I interact with children (by) using easier words (and) hand actions” (P01)
“I was taught how to better interact with children in terms of speaking at eye level” (P08)
2) Insights into interacting with children
TBH was a unique platform to understand children’s learning needs and empathize with their views towards healthcare. This was achieved via interactions with the children.
“By bonding with the children and hearing their opinions on the healthcare setting, it gives (me) a sense of connection between the children and myself which allows me to empathize with them better.” (P12)
These interactions allowed medical students to learn how to adapt their teaching styles to suit the different needs of each individual child.
“I learnt to interact with different groups of children with different learning abilities and TBH taught me how to cater to the different needs and abilities of the kids instead of treating them as a homogenous group.” (P07)
These interactions also taught medical students that the children have different levels of fear towards healthcare. While some children were apprehensive, others were unafraid of the TBH sessions.
“The children shared their fears about healthcare providers and I think the bulk of this fear comes from not being able to see the benefit of receiving these ‘painful’ treatments.” (P09)
“The children seemed to be really excited during the TBH sessions, I don’t recall that the children expressed any fear about their experiences” (P16)
In addition to understanding the children’s fears towards healthcare, medical students learnt how to manage these fears by acknowledging them and putting themselves in the children’s shoes.
“We should never downscale a child’s fear towards healthcare. There is a need to try to understand where they are coming from, (and) to comfort and encourage them to the best of our ability.” (P13)
3) Structure and curriculum
To understand the impact of the newly added VR scenarios, feedback regarding its strengths and limitations were collated. One strength is that the students experienced various case studies through the VR scenarios. This allowed them to be better prepared for the TBH sessions and become more aware of the children’s emotions during their interaction.
“I felt that the VR video gave us a lot to think about… Through the discussion and critiquing the VR doctor’s actions, I was more conscious on how the children may feel in a hospital setting.” (P07)
Another strength is that during the training, medical students were also asked how they would respond to the hypothetical scenarios. By putting them in the hot seat, they were able to exchange ideas and learn from one another.
“The volunteer trainers asked us questions during the volunteer training, when I answered correctly it gave me more confidence and when I listen to other people’s answers, I feel more equipped to handle different situations too” (P15)
The VR scenarios were limited in terms of application to the actual TBH sessions. The scenarios only showed how to engage an individual child, which was different from actual TBH sessions, in which medical students had to teach a group of children.
“Although it did give me a sense of how it is like to interact with children, the actual TBH session was a bit different from the VR (scenarios)” (P05)
Feedback was also collated regarding the strengths and limitations of the TBH sessions.
One strength was the established curriculum so participants did not have to worry about the content but can instead focus on honing their communication skills. The fact that this was a student-run program, and that medical students had their peers as fellow participants, put them at ease and made it a more conducive environment.
“(TBH) placed me in a friendly and relaxed environment centred on the children thus allowing me to focus in developing on interactions with the children” (P02)
A limitation of the TBH sessions was that it was challenging for participants to balance teaching the children and empathising with them.
“I think it’s … difficult to see from the children’s perspective during the session… We are usually more focused on imparting rather than listening because of the inability to elicit responses from all of them.” (P13)
Another limitation of the TBH sessions was that participants are usually able to attend only one session. This may have held them back from being fully adept in their interactions with children.
“As I was only able to attend 1 session, I was unable to fully practice and become more confident in these skills.” (P07)
Finally, there were disagreements about whether the ratio of medical students to children was suitable. While some felt that it was appropriate, others had trouble managing the children.
“The ratio (of) facilitators to children were just nice (and) not overwhelming for either parties” (P15)
“It was just too chaotic and hard to manage so many of them especially since they’re so bubbly and curious” (P16)
IV. DISCUSSION
This was the first study to examine objectively and subjectively, the effect of TBH and VR training on the empathy levels of medical students. There was a statistically significant improvement in the medical student’s level of empathy immediately after the TBH session, which persisted 1 year after the TBH session. The outcomes of this study revealed that the medical students who participated in TBH augmented by VR training assisted them to better empathize with the children they worked with.
Compared with the previous work by Ong et al in the same institution, involving only traditional lecture preparation for TBH (Ong et al., 2018), it appears that the addition of VR training showed an increase in medical students’ perceived improvement in both interacting and teaching children. In that study conducted without the use of VR scenarios, 53% reported improvement in interacting with children and 39% reported improvement in teaching children, compared to the present study of 88% and 75% respectively. Moreover, VR training alone achieved improvements of 44% and 50% which is similar to TBH session alone. A recent study found that VR simulation alone improved the empathy of dental students when managing children (Hu & Lai, 2022), this is encouraging since the VR intervention was not as time and resource intensive as the TBH. Although the cohorts of medical students were different, each cohort is from the same year of training (i.e., first year medical students) and the TBH teaching was done with a standardised protocol and thus relatively similar across the cohorts. It appears that a combination of the 2 methods of training provided a greater magnitude to the student’s perceived improvement in interacting and teaching children. This suggests that although the VR training cannot replace the real TBH interaction with children, it can be used to augment the learning experience of students in communicating with children. Moreover, it can be deployed on a much larger scale to the entire cohort, instead of smaller groups like the labour intensive TBH teaching.
According to the qualitative analysis, the TBH is a good platform for medical students to practice and develop their communication skills with children. Through TBH, they pick up techniques on how to better communicate with children both from the trainers and their peers. Similar to previous studies, TBH has also been described to be a useful avenue to gain insights into children’s perspectives of the healthcare setting and therefore trains them to be better attuned to the needs and feelings of children (Nheu et al., 2018; Ong et al., 2018). Nonetheless, the medical students suggested some areas of improvements. For example, it was pointed out that the VR scenarios did not depict the actual TBH session, as such, it did not help in teaching children during TBH. However, the goal of the TBH session is to increase medical student’s empathy through teaching rather than training them to be educators. Therefore, the VR scenarios can still bring the desired benefits in terms of the medical student’s ability to empathize and communicate with children. Additionally, some felt that they are unable to fulfil both a teaching and learning role simultaneously and were overwhelmed. This may hinder them from achieving the desired outcome of increasing their empathy. A potential solution would be to expand the existing course material to further help those who struggle with engaging the children or having fewer children paired to each medical student teacher.
There were some limitations to this study. As there was no control group to compare against, it was difficult to determine if the improvements seen from Pre-intervention to Post-intervention were due to the VR training and participation in the TBH session alone. Future studies could consider including a control group in addition to the intervention group. The observed maintenance of the level of empathy from Post-intervention to 1-year Post-intervention could have been confounded by factors such as varying levels of clinical exposure. Additionally, the quantitative survey on learner experience was done 1 year after the TBH session and may be at risk for recall bias, future studies should consider collecting data at multiple time points to evaluate any difference between immediate and long-term effects of the interventions. However, all respondents provided feedback that were very detailed and informative, suggesting that they were able to recall the experience well. Moreover, due to the COVID-19 pandemic situation and restrictions, the survey was collected via an online survey, instead of the planned Focused Group Discussion, resulting in the inability to ask follow-up or clarifying questions. Lastly, the study was conducted on a small group of volunteers who may have biases due to interest in the discipline. However, a significant improvement was still noted in this small pilot study. Expansion of the program into the general curriculum to include a more diverse group of students will be needed to ascertain the effect of TBH on medical students in general.
V. CONCLUSION
In conclusion, the TBH experience for medical students was effective in increasing their levels of empathy and confidence in interacting and teaching children as it provides an opportunity for medical students to interact with children and understand their views of healthcare. The use of VR can augment the TBH experience or be used in situations where the student is unable to attend TBH sessions in person.
Notes on Contributors
JT and FT are considered co-first authors. JT participated in data collection, conducted the data analysis and interpretation, led the writing, and revised the manuscript for important intellectual content. FT participated in data collection, conducted the data analysis and interpretation, led the writing, and revised the manuscript for important intellectual content. MA conceived the idea and revised the manuscript for important intellectual content. SH conceived the idea, conducted the data analysis and interpretation, led the writing, and revised the manuscript for important intellectual content.
Ethical Approval
This study was approved by the Institutional Review Board (NUS-IRB Reference Number: S-19-151) and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Data Availability
The data that support the findings of this study are openly available in Figshare repository, https://doi.org/10.6084/m9.figshare.17973662.
Acknowledgement
The authors would like to thank Dr Lee Shuh Shing and Ms Lim Yih Lin for their help with the statistical analysis and Manzalab for the help in creating the virtual reality scenarios.
Funding
This work was supported by the USPC-NUS Joint Innovative Projects in Higher Education grant (USPC-NUS 2018 SoM).
Declaration of Interest
The authors declare that they have no competing interests.
References
Batt-Rawden, S. A., Chisolm, M. S., Anton, B., & Flickinger, T. E. (2013). Teaching empathy to medical students: An updated, systematic review. Academic Medicine, 88(8), 1171-1177. https://doi.org/10.1097/ACM.0b013e318299f3e3
Bloch, Y. H., & Toker, A. (2008). Doctor, is my teddy bear okay? The “Teddy Bear Hospital” as a method to reduce children’s fear of hospitalization. Israel Medical Association Journal, 10(8-9), 597-599.
Creswell, J. W., & Poth, C. N. (2019). Qualitative inquiry & research design: Choosing among five approaches. SAGE.
Dwamena, F., Holmes‐Rovner, M., Gaulden, C. M., Jorgenson, S., Sadigh, G., Sikorskii, A., Lewin, S., Smith, R. C., Coffey, J., & Olomu, A. (2012). Interventions for providers to promote a patient‐centred approach in clinical consultations. Cochrane Database of Systematic Reviews, (12).
Dyer, E., Swartzlander, B. J., & Gugliucci, M. R. (2018). Using virtual reality in medical education to teach empathy. Journal of the Medical Library Association, 106(4), 498-500. https://doi.org/10.5195/jmla.2018.518
Halton, C., & Cartwright, T. (2018). Walking in a patient’s shoes: An evaluation study of immersive learning using a digital training intervention. Frontiers in Psychology, 9, 2124. https://doi.org/10.3389/fpsyg.2018.02124
Hojat, M., DeSantis, J., Shannon, S. C., Mortensen, L. H., Speicher, M. R., Bragan, L., LaNoue, M., & Calabrese, L. H. (2018). The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Advances in Health Sciences Education, 23(5), 899-920.
Hu, S. (2022). Raw Jefferson Scores. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.17973662
Hu, S., & Lai, B. W. P. (2022). Increasing empathy for children in dental students using virtual reality. International Journal of Paediatric Dentistry. https://doi.org/10.1111/ipd.12957
Lok, B., Ferdig, R. E., Raij, A., Johnsen, K., Dickerson, R., Coutts, J., Stevens, A., & Lind, D. S. (2006). Applying virtual reality in medical communication education: Current findings and potential teaching and learning benefits of immersive virtual patients. Virtual Reality, 10(3-4), 185-195.
MacDonald-Wicks, L., & Levett-Jones, T. (2012). Effective teaching of communication to health professional undergraduate and postgraduate students: A systematic review. JBI Evidence Synthesis, 10(28), 1-12. https://doi.org/10.11124/jbisrir-2012-327
Mead, N., & Bower, P. (2002). Patient-centred consultations and outcomes in primary care: A review of the literature. Patient education and counseling, 48(1), 51-61.
Mercer, S. W., & Reynolds, W. J. (2002). Empathy and quality of care. British Journal of General Practice, 52(Suppl), S9-S12.
mooc vid. (2019, September 13). Scenario 1 [Video]. YouTube. https://www.youtube.com/watch?v=4f6bZ_Kc2xw
mooc vid. (2019, September 13). Scenario 2 [Video]. YouTube. https://www.youtube.com/watch?v=oz4dm45Imkw
Neumann, M., Edelhäuser, F., Tauschel, D., Fischer, M. R., Wirtz, M., Woopen, C., Haramati, A., & Scheffer, C. (2011). Empathy decline and its reasons: A systematic review of studies with medical students and residents. Academic Medicine, 86(8), 996-1009. https://doi.org/10.1097/ACM.0b013e318221e615
Nheu, L., Uahwatanasakul, W., & Gray, A. (2018). Medical students’ experience of a Teddy Bear Hospital as part of a paediatric curriculum. Focus on Health Professional Education: A Multi-disciplinary Journal, 19(3), 40.
Ong, L., Chua, K. H., Soh, J. Y., & Aw, M. M. H. Y. (2018). Healthcare encounters in young children: Impact of Teddy bear Hospital, Singapore. The Asia Pacific Scholar, 3(3), 24-30. https://doi.org/10.29060/TAPS.2018-3-3/OA1055
Santen, L., & Feldman, T. (1994). Teddy bear clinics: a huge community project. MCN: The American Journal of Maternal/Child Nursing, 19(2), 102-106.
Siegel, B., Lewis, H., Bryan, L., & Batisky, D. (2018). The Teddy Bear Hospital as an outreach tool for reducing medical anxiety: A randomized trial. (2018). Pediatrics, 142(1_MeetingAbstract), 783. https://doi.org/10.1542/peds.142.1MA8.783
Stewart, M., Brown, J. B., Weston, W., McWhinney, I. R., McWilliam, C. L., & Freeman, T. (2013). Patient-centered medicine: Transforming the clinical method. CRC press.
*Shijia Hu
Faculty of Dentistry,
National University of Singapore
9 Lower Kent Ridge Road #10-01
National University Centre for Oral Health,
Singapore 119085
Email: denhus@nus.edu.sg
Submitted: 10 January 2022
Accepted: 22 April 2022
Published online: 5 July, TAPS 2022, 7(3), 23-32
https://doi.org/10.29060/TAPS.2022-7-3/OA2742
Tun Tun Naing1, Yuriko Minamoto2, Ye Phyo Aung1 & Marlar Than1
1Department of Medical Education, Defence Services Medical Academy, Myanmar, 2Meiji University, Tokyo
Abstract
Introduction: With the evolution of healthcare needs for the community and the changing trends in medical education in the 21st century, medical educators need to be prepared for their tasks in the coming decades. Medical educator training is crucial but other factors can also affect the development of their competency. This study aims to measure the impact of the medical educators’ training course and find out the key challenges encountered by the medical educators in Myanmar.
Methods: A retrospective quantitative design was conducted on 45 respondents by four levels of Kirkpatrick’s model assessment consisting of 39 statements and 9 items of key challenges, using five-point Likert scale. The item scores were analysed as mean and standard deviation, ‘t’ test and ANOVA were used for relationship between impact of training and demographic background.
Results: There was significant association between the impact of training and the educational background (p=0.03), job position (p=0.02), and academic year attended (p=0.03). The respondents distinctly agreed that the training increased their knowledge and attitudes and that they could apply the learnt lessons practically in their workplace (minimum 3.75±0.60 and maximum 4.28±0.50). Regarding the key challenges, respondents viewed that their institution needed to support more scholarship opportunities and academic recognition; encourage networking and strengthen ICT-based medical education system (minimum 2.55±0.84 – maximum 4.17±0.71).
Conclusion: This study indicates that enhancing the competency of medical educators with medical educator training programs is effective and useful; but inadequacy of institutional support for faculty development and internet facilities posed challenges in the overall faculty development.
Keywords: Medical Education, Faculty Development, Impact of Medical Educator’s Training, Kirkpatrick’s Model, Key Challenges
Practice Highlights
- Medical educator training program is crucial for enhancing competency in medical educators.
- Medical educator training program inspires medical educators to apply their knowledge and skills in their daily departmental activities.
- Beyond training, medical schools must address a balance of capacity for teaching, research and service functions for their faculty.
- Encouraging institutional support such as reward, recognition, and appreciation for their performance should be encouraged as an admirable institutional culture.
- Inadequacy of institutional support for faculty development and internet facilities posed challenges in the overall faculty development.
I. INTRODUCTION
Nowadays, with the evolution of healthcare needs for the community and changes in medical education trends, faculty development in medical education is challenging. Sheets and Schwenk (1990) explained that any activity that enhances the knowledge and skills of individual faculty members are very fundamental to their performance in a department or residency program such as teaching skills, clinical skills, research and administrative skill (Sheets & Schwenk, 1990). Developing the skills of faculty members is not effortless. The ability to teach is not inborn, although the graduate from medical school is supposed to be capable of teaching (McLean et al., 2008). Besides content, teaching involves ‘process,’ and to develop the ‘art’ of teaching, academics required to support (Benor, 2000).
The present-day teacher must be aware of and become part of the far- reaching changes taking place in medical education. Accordingly, in the 21st century, many changes can be found, such as teachers’ conventional roles being shifted to different roles, such as facilitators, curriculum planners, resource developers, educational administrators, and researchers (Crosby, 2000). Significant trends in underpinned theories of medical education are now focusing on patient-centred and culturally competent medical doctors and the ultimate aim of medical education is to improve the patient and community outcomes by promoting competent and caring practitioners (competent medical doctors) (McLean et al., 2008).
According to Harden and Laidlaw (2017), the competencies and attributes expected of an effective teacher includes not only mastery of the content area but also the technical competencies necessary to serve as an information provider, a role model, a facilitator of learning, a curriculum planner, an assessor, a manager and a scholar” (p. 9). Most medical schools worldwide have been implementing specific training for medical educators to develop the necessary skills as medical educators. The study conducted by Steinert (2014), pointed out that nowadays, most medical schools and educational organisations offer various programs and activities in response to educational trends in teaching and assessment for helping faculty members improve their skills as teachers and educators. Additionally, the World Federation of Medical Education (WFME) entails that for a basic standard of staff development: “the medical school must have a staff policy that addresses a balance of capacity for teaching, research and service functions. It also encourages ensuring recognition of meritorious academic activities, with appropriate emphasis on both research attainment and teaching qualifications” (World Federation for Medical Education, 2015).
In Myanmar, there are five civilian medical schools and one military medical school (Defence Services Medical Academy); however, no private medical school exists yet. Defence Services Medical Academy (DSMA), was established on 19th November 1992 in Mingalodon, Yangon and is listed in the World Directory of Medical Schools. The Ministry of Health and Sports, Myanmar, established a medical educator’s training program in 2003 for the medical educators from the civilian medical schools; likewise, the Directorate of Medical Services under the Ministry of Defence also started the medical educator training program for the military medical school in 2011. Both these medical educators’ training programs emphasize on developing the competent skills of medical educators.
Although medical educator training is crucial to improve medical educators’ quality in medical school, other influencing factors can affect the competency of medical educators. The impact of training depends not only on the program design of the training program but also on other factors such as learner characteristics and educational environment (Iqbal & AlSheikh, 2018). In a study conducted by Peeraer and Van Petegem (2012), the faculty members were able to apply teaching strategies and methods in their teaching activities after the faculty development training. Nevertheless, they faced some challenges, such as time constraints and scarce resources that impede their behavioural changes from becoming sustainable.
The medical educator training program in DSMA is a distance learning, diploma course with four face-to-face hands-on workshops. Individual written assignments are given on 10 fundamental modules that provide medical educators with the knowledge and skills about educational psychology, curriculum design and planning, objectives and contents, teaching-learning strategy, teaching-learning media, assessment and evaluation, educational leadership, communication skills, as well as conducting an educational workshop and educational research: throughout the one-year course. Since 2011, nine successive medical educator training courses have been conducted, and approximately 200 medical teachers from DSMA have successfully completed these courses and graduated.
Currently, there is no published evidence-based research investigating the crucial issues to develop competent medical educators in Myanmar. This study intends to focus on the training perspectives and the commitment of institutional support for the development of the medical skills. Therefore, the main objective of this study is to find out the impact of the medical educator’s training course conducted in the military medical school and to explore the key challenges encountered by the trainees.
II. METHODS
A. Research Design
A retrospective design was used to investigate the impact of the medical educator training course and the medical educators’ perception regarding their key challenges. By applying the program theory, a logic model for training program was applied, illustrated in Figure 1.

Figure 1. Logic model for training evaluation Adapted from (Rossi, et al., 2004)
B. Kirkpatrick’s Model
To investigate the impact of the training, the Kirkpatrick evaluation measurement tool was utilized (Appendix 1). The four-levels in the Kirkpatrick’s model are: 1) Reaction evaluation, Learning evaluation Behaviour evaluation and Result evaluation (Kirkpatrick & Kirkpatrick, 2006).
C. Research Framework

Figure 2. Research framework
D. Data Collection
Survey questionnaires were formulated in three sections. The first session aimed to get demographic information, the second one intended for Kirkpatrick’s evaluation by 39 evaluation questions, and the last was constructed by nine items to explore the critical challenges for medical educators. Questionnaires were developed based on the contents and expected outcomes of the medical educator training course that has been to delivered throughout the courses. These are related to the knowledge, attitude and skills that gained after the course regarding educational psychology, curriculum design and planning, objectives and contents, teaching-learning strategy & media, assessment and evaluation, educational leadership, communication skills, conducting an educational workshop and educational research. Moreover, questionnaires attributed to possible challenges that have been encountered by medical educators were adapted from the research outcomes of Huwendiek et al. (2010). All evaluation questions were self-administered and had the five-point Likert scale items ranging from 5 (strongly agree) to 1 (strongly disagree). Informed verbal consent was obtained from the respondents in respective of respondents’ autonomy before data collection. Ethics approval was obtained from the Ethical Review Committee of the Defence Services Medical Academy, Yangon, Myanmar.
E. Sampling Procedure
Every medical educator is eligible if they had already completed the training and currently engaging in the undergraduate and postgraduate medical education programs at the military medical school, in Myanmar. Among the 120 persons who meet eligibility, approximately 30% of the population (45 participants) responded to the evaluation survey and convenience sampling was practiced.
F. Data Analysis
Data obtained from the survey was entered in Microsoft Excel files and analysed by SPSS software. The item scores of each evaluation were analysed as descriptive analysis such as mean and standard deviation to compare the response rate. The t-test and ANOVA analysis were used to determine the relationship between respondents’ demographic characteristics and Kirkpatrick’s four-level evaluation results. Descriptive analysis was used to explore the key challenges of medical educators.
III. RESULTS
Forty-five medical educator attendees who satisfactorily completed one of the medical education courses held at DSMA between 2011 and 2019, individually expressed their views on the impact of the medical educator training courses and disclosed the key challenges regarding faculty development in medical education. The data that support the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.figshare.17074637 (Naing et al., 2021).
There were 39 evaluation questions, and each evaluation level has specific items, respectively. The internal consistency of each of the scales was examined by using Cronbach’s alpha. The alpha score was satisfactory: 0.65 for reaction evaluation (11 items), 0.86 for learning evaluation (10 items), 0.81 for behavioral evaluation (11items), and 0.84 for result evaluation (7 items).
A. Demographic Characteristics
Of the demographic characteristics, three factors (age, gender, and expertise), had no significant association with the impact of the training, but the respondents’ educational background (p=0.03), job’s position (p=0.02), academic year they attended (p=0.03) showed statistically significant association with the impact of training (Table 1). However, the proportionally unequal number of respondents in each group may affect the results.
|
Demographic Characteristics |
Reaction Evaluation |
Learning Evaluation |
Behavioral evaluation |
Result Evaluation |
|
Mean ± SD |
Mean ± SD |
Mean ± SD |
Mean ± SD |
|
|
Age(N=45) |
||||
|
<=40 (N=26) |
4.05±0.20 |
4.08±0.27 |
3.93±0.26 |
4.00±0.35 |
|
41-50 (N=11) |
4.10±0.27 |
4.30±0.44 |
3.99±0.22 |
4.22±0.39 |
|
>= 50 (N=8) |
4.06±0.28 |
4.12±0.38 |
4.01±0.44 |
4.10±0.40 |
|
‘F’ value |
0.17 |
1.55 |
0.28 |
1.30 |
|
‘p’ value |
0.83 |
0.22 |
0.75 |
0.28 |
|
Gender(N=45) |
||||
|
Male(N=33) |
4.06±0.23 |
4.10±0.31 |
3.93±0.26 |
4.07±0.39 |
|
Female(N=12) |
4.09±0.24 |
4.26±0.41 |
4.04±0.36 |
4.08±0.33 |
|
‘t’ value |
-0.474 |
-1.44 |
-1.16 |
-0.07 |
|
‘p’ value |
0.63 |
0.15 |
0.24 |
0.94 |
|
Education(N=45) |
||||
|
Master(N=31) |
4.05±0.27 |
4.09±0.31 |
3.90±0.27 |
3.99±0.37 |
|
Doctoral(N=14) |
4.09±0.20 |
4.25±0.39 |
4.09±0.28 |
4.25±0.32 |
|
‘t’ value |
-0.50 |
-1.49 |
-2.18 |
-2-23 |
|
‘p’ value |
0.61 |
0.14 |
0.03* |
0.03* |
|
Expertise in medical Sciences(N=45) |
|
|||
|
Basic Sciences(N=14) |
4.04±0.26 |
4.10±0.33 |
3.86±0.30 |
4.06±0.33 |
|
Paraclinical(N=16) |
4.09±0.19 |
4.25±0.33 |
4.09±0.24 |
4.20±0.36 |
|
Clinical(N=9) |
4.02±0.28 |
4.03±0.33 |
3.90±0.29 |
3.96±0.40 |
|
Others(N=6) |
4.15±0.21 |
4.10±0.41 |
3.90±0.32 |
3.92±0.45 |
|
‘F’ value |
0.45 |
0.95 |
1.94 |
1.19 |
|
‘p’ value |
0.71 |
0.42 |
0.13 |
0.32 |
|
Job Position (N=45) |
|
|||
|
Assistant lecturer(N=27) |
4.04±0.21 |
4.07±0.27 |
3.93±0.26 |
3.99±0.35 |
|
Lecturer(N=11) |
4.04±0.24 |
4.16±0.35 |
3.90±0.18 |
4.12±0.38 |
|
Associate Professor(N=3) |
4.33±0.29 |
4.70±0.30 |
4.33±0.29 |
4.38±0.35 |
|
Professor(N=4) |
4.11±0.30 |
4.15±0.52 |
4.02±0.56 |
4.25±0.45 |
|
‘F’ value |
1.49 |
3.47 |
2.02 |
1.47 |
|
‘p’ value |
0.23 |
0.02* |
0.12 |
0.23 |
|
Teaching experience (N=45) |
|
|||
|
< = 5 Years(N=17) |
4.02±0.24 |
4.11±0.37 |
3.88±0.27 |
4.13±0.45 |
|
(6-10) Years(N=15) |
4.15±0.19 |
4.12±0.24 |
4.03±0.23 |
4.01±0.32 |
|
(11-15) Years(N=7) |
4.00±0.23 |
4.11±0.28 |
3.90±0.44 |
4.08±0.29 |
|
> = 6 Years(N=6) |
4.07±0.28 |
4.31±0.54 |
4.06±0.24 |
4.04±0.39 |
|
‘F’ value |
1.00 |
0.55 |
1.05 |
0.24 |
|
‘p’ value |
0.41 |
0.64 |
0.37 |
0.86 |
|
Year of Services (N=45) |
|
|||
|
< = 10 Years(N=5) |
4.05±0.13 |
4.16±0.15 |
3.96±0.18 |
4.08±0.27 |
|
(11-15) Years(N=16) |
4.08±0.23 |
4.04±0.29 |
3.90±0.29 |
3.96±0.37 |
|
(16-20) Years(N=12) |
4.08±0.28 |
4.25±0.39 |
4.01±0.27 |
4.16±0.39 |
|
> = 21 Years(N=12) |
4.04±0.23 |
4.16±0.40 |
3.98±0.35 |
4.13±0.40 |
|
‘F’ value |
0.08 |
0.83 |
0.35 |
0.77 |
|
‘p’ value |
0.97 |
0.48 |
0.78 |
0.51 |
|
Academic Year (N=45) |
|
|
|
|
|
2011-2013(N=11) |
4.03±0.25 |
4.25±0.35 |
4.00±0.31 |
4.10±0.32 |
|
2014-2016(N=9) |
4.00±0.34 |
3.93±0.35 |
3.78±0.34 |
3.79±0.45 |
|
2017-2019(N=25) |
4.11±0.17 |
4.17±0.32 |
4.00±0.24 |
4.16±0.33 |
|
‘F’ value |
0.94 |
2.47 |
2.09 |
3.64 |
|
‘p’ value |
0.40 |
0.10 |
0.13 |
0.03* |
(*) means 0.05 level of significant
Table 1. Relationship between demographic characteristics and Kirkpatrick’s evaluation
B. Kirkpatrick’s Four Level of Evaluation
When looking at the reaction evaluation, most of the respondents gave favourable agreement on the management of training, teaching skills of the trainers, and training methods, however, there was relatively weakness in the proper preparation of training contents by facilitators (3.86±0.45), providing training materials (3.88±0.53). Looking upon the learning evaluation responses, all of the respondents expressed a high level of satisfaction on their understandings and awareness. Regarding learning behaviour, majority agreed that they can apply their learning to their workplace but comparatively lower response score was found in planning educational research (3.84±0.56), how to apply educational theories in medical education practices (3.84±0.52) and arrange an educational workshop programme (3.75±0.60). Although the medical educator training affects the respondents to get better improvement in most faculty development activities, there is still a need to develop the participation of respondents in research development activities with comparatively lowest evaluation scores of (3.80±0.66).
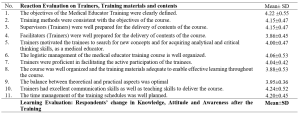



Table 2. Kirkpatrick’s Four Level of Evaluation of Medical Educator Training
C. Key Challenges in Faculty Development
It was found that majority of the evaluation scores for the statement items in the faculty development area were much lower than the scores for the items in the training’s impact. The most noticeable and lowest scores were found in the item of financial investment of medical educators (2.68±0.73), research collaboration in other universities (2.60±0.88) and networking with the international university for career development of medical educators (2.55±0.84). However, they agreed that the currently used undergraduate curriculum of the institution is appropriate for them to practically apply their pedagogic skills gained from the training course(4.17±0.71).
|
No. |
Statement |
Mean±SD |
|
1. |
Depending on the performance in faculty development activities, our institution appreciates rewards for medical educators as an institutional policy. |
2.80±0.75 |
|
2. |
Medical educators in our university have the opportunity to apply the Institutional scholarship program for research and carrier development. |
2.84±0.79 |
|
3. |
The financial investment for medical educators in our institution is acceptable in the current situation. (e.g. teaching-learning materials, research facilities, ICT based technology) |
2.68±0.73 |
|
4. |
There are adequate networks and collaboration with an international university to promote the carrier development of medical educators. (e.g. MOU) |
2.60±0.88 |
|
5. |
ICT based medical education system in our university is well functioned and applicable. |
2.73±0.80 |
|
6. |
The number of medical educators in our university is sufficient to achieve the mission of our university. |
2.71±0.84 |
|
7. |
The institutions’ current undergraduate curriculum is appropriate for us to practically apply the pedagogic skills gained from the training course. |
4.17±0.71 |
|
8. |
Research development activities of our university, including research funding, research skills of medical educators, and research facilities, are well functioning. |
2.80±0.78 |
|
9. |
The research collaboration with other universities or research centers to promote research innovation is acceptable. |
2.55±0.84 |
Table 3. Key Challenges in faculty development in medical education by respondents
IV. DISCUSSION
This study investigates the medical educator training program, which aims to develop the competency skills of medical educators who are involved in the faculty development activities at DSMA, Myanmar. Regarding the overall impact of the training, the respondents expressed their positive perception on the organisation of the program; the training improved their knowledge and attitudes as a medical educator; and it was practically applicable in their daily work. The positive perception of the training was not surprising because most of the trainees voluntarily attended the course and were highly motivated to accomplish self- improvement after attending the course. The findings are consistent with another study where ‘overall satisfaction with faculty development programs was high, and they consistently found the program helpful, enjoyable and relevant to their objectives’ (Steinert et al., 2016, p.779). Similarly, another study done by Yolsal et al. (2003) showed that the participants who enrolled in the similar training of trainers (TOT) course explored positive perception, and they agreed it was required to be acquainted with those kinds of instructional practices (Yolsal et al., 2003). The possible reason for the respondents’ satisfaction with the impact of training in the current study, could also be due to the organized training preparation and training context and, the course itself used mainly a distance learning format with flexible training schedules for them when compared to other full-time courses in other specialties. It was also found that significant improvements in self-efficacy of medical educators in the domain of the teaching relevant subject contents and developing creative ways to cope with system constraints after experiencing 12 months faculty development program in Bhutan (Tenzin et al., 2019).
In this study, for learning evaluation, most respondents believed that they gained in terms of knowledge, attitude, and skills and that it had an impact on the teaching effectiveness. It revealed that most of the medical educators gained benefits after the training, and the increase in confidence facilitated them to become more involved in participating in faculty development activities and curriculum planning activities. Similarly, F.J. Ciller and N. Herman explained that as a goal of an educational development program, changes in attitudes and perception serves as a foundation for further changes in behaviour (Cilliers & Herman, 2010).Even more, the review articles of Steinert et al. (2016) highlighted most of the faculty development interventions focus on teaching effectiveness by improving their teaching skills, assessment skills, designing curriculum, and educational leadership skills (Steinert et al., 2016).
When analysing the relationship between the various demographic background and impact of the training, it was revealed that the job position, educational background, and difference in academic year among the respondents were significantly associated with the impact of training. There might be many possible reasons why this was significant. For example, the course preparation, the changes in placement of trainers in several years might also be a possible issue, and variation in individual performance also considered. However, in this survey, those factors were not explored. Fishbein et al. (2003) explained that interpersonal variation and the organization’s favorable situation could be impact factors for behavioural change at the organization level (Fishbein et al., 2003).
In this study, although the self-reported changes showed self-actualization in individual performance to some extent, respondents are not contented with their learning environment in terms of institutional support. Institutional support plays a vital role in faculty development in medical education and every institution can meet its institutional mission and goals by enabling its faculty member to fulfil their particular purposes as teachers, scholars, and leaders according to the research outcome (Boucher et al., 2006). Moreover, Steinert pointed out that many factors are impeding the faculty development, such as unsupportive leadership, resistance to change, lack of faculty motivation, and the unwillingness of faculty to acquire the teaching skills and knowledge (Steinert, 2000).
On exploring the critical challenges of the medical educators, all the respondents believed that their institution should support more scholarship opportunity, academic recognition, networking with other universities in terms of research and professional development, and ICT-based medical education system. According to the survey of (Huwendiek et al., 2010) 806 medical educators from Association for Medical Education Europe (AMEE) revealed that the critical challenges of medical education were lack of academic recognition (40%), funding (36%), faculty development (24%), time for medical education issues (22%), and institutional support (21%) (Huwendiek et al., 2010).
Therefore, to accelerate the faculty development as a holistic approach, it is needed to consider not only training for faculty members but also other factors reward and recognition, ICT system, and networking. This requisite is not only in a military medical school, but internationally most medical schools are trying to support their faculty in accordance with the staff policy requirements as stated in the WFME Global standards for Quality improvement. However, the current research could gather only some self-reported changes in behaviour and whether the changes actually occurred in the workplace has not been proven by observation. Nevertheless, as the opinions were obtained from closed ended questionnaire statements, a further exploratory qualitative study is needed to obtain accurate information on the magnitude of the problem and the specific areas that needed further support from the institution.
V. CONCLUSION
This study revealed the medical educator training could improve their required knowledge, attitude, and skills to practice in the teaching environment, the fundamental need for educational leadership, educational research, and communication skills in the health-care setting. The medical educators who need to be competent could not be motivated only from the training without institutional support. The respondents believed that their institution should encourage institutional support in terms of reward, recognition, scholar allowance, and collaboration with other academic institutions to promote research culture and professional development, ICT-based medical education.
To conclude, the findings of this study exclusively show that military medical schools in Myanmar still need to emphasize the professional identities of medical educators by encouraging institutional support, not just by only focusing on the faculty development training as a mandatory by institutional policy.
Notes on Contributors
Tun Tun Naing reviewed the literatures and developed the conceptual framework and conducted the data analysis and wrote the discussion and conclusion. Finally, he developed the manuscript to submit to TAPS.
Yuriko Minamoto was involved in the formulation of research question and research framework to conduct the research systematically, application of evaluation tools and technique and, proofreading of original thesis and the manuscript.
Ye Phyo Aung participated in the research in the writing of research methodology session, conducted the data collection, and supported choosing research design, proper sampling methods and data collection tools and technique and proofreading of manuscript.
Marlar Than supported the construction of survey questionnaires which is the back bone of the evaluation research and contribute to proofreading of current manuscript.
Ethical Approval
Ethics approval was granted by the Ethical Review Committee of the Defence Services Medical Academy, Yangon, Myanmar. (7 / Ethics 2019).
Data Availability
The data that support the findings of this study are openly available in Figshare repository, http://doi.org/10.6084/m9.figshare.17074637
Acknowledgement
I would also like to express my gratitude to Japanese Government through the Japan International Cooperation Center (JICE) for their support to conduct this research project for completion of master thesis program at Meiji University.
I would like to express my special thanks to my colleagues, and without their support, the survey of my research would not have been achieved. I am indebted to all medical educators from Military Medical Service, Myanmar, who help me respond to my survey sharing with their valuable opinions and experience.
Funding
Conducting the research was operated during the study period supported by JDS Program under the JICA. For this publication , it is conducted for personal and professional development and no funding is involved.
Declaration of Interest
There is no conflict of interest in the current research.
References
Benor, D. (2000). Faculty development, teacher training and teacher accreditation in medical education: Twenty years from now. Medical Teacher, 22(5), 503-512. https://doi.org/10.1080/01421590050110795
Boucher, B., Chyka, P., Fitzgerald, W., Hak, L., Miller, D., Parker, R., Phelps, S., Wood, G., & Gourley, D. (2006). A comprehensive approach to faculty development. American Journal of Pharma- ceutical Education, 70(2), 27. https://doi.org/10.5688/aj700227
Cilliers, F., & Herman, N. (2010). Impact of an educational development programme on teaching practice of academics at a research‐intensive university. International Journal for Academic Development, 15(3), 253-267. https://doi.org/10.1080/1360144x.2010.497698
Crosby, R. (2000). AMEE Guide No 20: The good teacher is more than a lecturer – the twelve roles of the teacher. Medical Teacher, 22(4), 334-347. https://doi.org/10.1080/014215900409429
Fishbein, M., Hennessy, M., Yzer, M., & Douglas, J. (2003). Can we explain why some people do and some people do not act on their intentions? Psychology, Health &Amp; Medicine, 8(1), 3-18. https://doi.org/10.1080/1354850021000059223
Harden, R. M., & Laidlaw, J. M. (2017). Essential Skills for a Medical Teacher (2nd ed., pp. 9). Elsevier.
Huwendiek, S., Mennin, S., Dern, P., Ben-David, M., Van Der Vleuten, C., Tönshoff, B., & Nikendei, C. (2010). Expertise, needs and challenges of medical educators: Results of an international web survey. Medical Teacher, 32(11), 912-918. https://doi.org/10.3109/0142159x.2010.497822
Iqbal, M., & AlSheikh, M. (2018). Factors affecting the transfer of training to the workplace after a faculty development programme: What do trainers think? Journal of Taibah University Medical Sciences, 13(6), 552-556. https://doi.org/10.1016/j.jtumed.2018.11.001
Kirkpatrick, D., & Kirkpatrick, J. (2006). Evaluating Training Programs: The Four Levels (3rd ed.). Berrett-Koehler Publisher.
McLean, M., Cilliers, F., & Van Wyk, J. (2008). Faculty development: Yesterday, today and tomorrow. Medical Teacher, 30(6), 555-584. https://doi.org/10.1080/01421590802109834
Naing, T. T., Minamoto, Y., Aung, Y. P., & Than, M. (2021). Faculty development of medical educators: Training evaluation and Key Challenges. [Dataset].
Figshare. http://doi.org/10.6084/m9.figshare.17074637
Peeraer, J., & Van Petegem, P. (2012). The limits of programmed professional development on integration of information and communication technology in education. Australasian Journal of Educational Technology, 28(6), 1039-1056. https://doi.org/10.14742/ajet.809
Rossi, P., Lipsey, M., & Freeman, H. (2004). Evaluation: A Systematic Approach (7th ed.). Sage.
Sheets, K., & Schwenk, T. (1990). Faculty development for family medicine educators: An agenda for future activities. Teaching and Learning in Medicine, 2(3), 141-148. https://doi.org/10.1080/10401339009539447
Steinert, Y. (2000). Faculty development in the new millennium: key challenges and future directions. Medical Teacher, 22(1), 44-50. https://doi.org/10.1080/01421590078814
Steinert, Y. (2014). Faculty Development in Health Profession: A Focus on Research and Practice (1st ed.). Springer.
Steinert, Y., Mann, K., Anderson, B., Barnett, B., Centeno, A., Naismith, L., Prideaux, D., Spencer, J., Tullo, E., Viggiano, T., Ward, H., & Dolmans, D. (2016). A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Medical Teacher, 38(8), 769-786. https://doi.org/10.1080/0142159x.2016.1181851
Tenzin, K., Dorji, T., Choeda, T., & Pongpirul, K. (2019). Impact of faculty development programme on self-efficacy, competency and attitude towards medical education in Bhutan: A mixed-methods study. BMC Medical Education, 19(1), 468. https://doi.org/10.1186/s12909-019-1904-4
World Federation for Medical Education. (2015, January 1). Basic medical education WFME global standards for quality improvement. https://wfme.org/download/wfme-global-standards-for-quality-improvement-bme/.
Yolsal, N., Bulut, A., Karabey, S., Ortayli, N., Bahadir, G., & Aydin, Z. (2003). Development of training of trainer’s programmes and evaluation of their effectiveness in Istanbul, Turkey. Medical Teacher, 25(3), 319-324. https://doi.org/10.1080/0142159031000092779
*Tun Tun Naing
No. 94, D-1, Pyay Road,
Mingaladon Township
Yangon, Myanmar
Postal code – 11021
+95 95053402
Email: tuntunnaing@dsma.edu.mm, drhtun1984@gmail.com
Submitted: 30 May 2021
Accepted: 8 April 2022
Published online: 5 July, TAPS 2022, 7(3), 10-22
https://doi.org/10.29060/TAPS.2022-7-3/OA2539
Hanyi Li1, Elaine Li Yen Tan1,3, Mun Loke Wong2 & Marianne Meng Ann Ong1,3
1National Dental Centre Singapore, Singapore; 2Faculty of Dentistry, National University of Singapore, Singapore; 3Oral Health Academic Clinical Programme, Duke-NUS Medical School, Singapore
Abstract
Introduction: As young healthcare professionals (HCPs) enter the workforce, they find challenges adapting as academic training and workplace settings often do not mirror each other. Mentorship is a possible solution to help bridge this transition. The aim of this study was to gather information from HCPs with regards to their views towards mentorship as a strategy to help in the transition of newly qualified HCPs from study to work.
Methods: Two 3-hour interactive workshops entitled “Bridging the Study-Work Chasm” were organised, and participants were invited to complete a survey voluntarily after the workshop. The survey comprised questions regarding the benefits of mentorship, qualification of mentors, time commitment for mentoring, elements of an effective mentorship programme, and barriers to its effectiveness. The anonymised responses were analysed descriptively.
Results: Fifty-two out of 62 participants from various healthcare backgrounds completed the survey. 96.2% of respondents felt a study-work chasm exists in the healthcare workplace with 90.4% indicating that a mentorship programme would help to bridge the chasm. More than 70% of participants agreed or strongly agreed that mentoring would boost confidence, reduce anxiety, and aid in study-work transition. It was identified that to produce a more effective mentorship programme, time commitment, training, and proper organisation of the programme would be necessary.
Conclusion: It was perceived that a mentorship programme can help to bridge the study-work chasm in the healthcare landscape in Singapore, and will best serve mentors and mentees by committing the proper time and training to ensure its effectiveness.
Keywords: Training-Work Transition, Graduate, Healthcare Professionals, Mentorship
Practice Highlights
- Despite receiving extensive training during their education, healthcare professionals still experience many challenges as they enter the workforce.
- Globally it has been reported that differences in training and workplace demands, coupled with the need to take direct responsibility for patients, propagate anxiety and perceived incompetence in fresh graduates. This could result in compromised work performance and patient outcomes.
- A study-work chasm exists in the healthcare work space, and should be addressed.
- Mentorship was shown to be accepted as a popular solution amongst healthcare workers in Singapore, and the benefits were discussed.
- Elements of a good mentorship programme as well as challenges in setting one up were identified, laying the groundwork for future implementation of such programmes in local public healthcare institutions.
I. INTRODUCTION
Healthcare professionals (HCPs) are known to receive extensive training during their pre-qualification education. However, there still exists many challenges as they enter the workforce. These include increasing workload, encountering patients with more complex conditions, generational diversity in the workforce, performance anxiety, and bullying when transitioning to the workforce (Hofler & Thomas, 2016). While facing these challenges in a new working environment marks the beginning of a fresh process of learning, there are indications that this may be more than what newly qualified professionals can cope with (Teunissen & Westerman, 2011).
There are several contextual differences between pre-employment learning in the university and post-employment learning in the workplace. Fundamentally, the focus of education and real-world practice are different. The commonplace practice of test-taking in school focuses on knowledge retention, with minimal consideration for practical value in the workplace (Lave & Wenger, 1991). A good example of this is the learning of ethical guidelines, which can be easy to regurgitate in school assignments and tests, but are far more difficult to apply on the job (Le Maistre & Paré, 2004). In school, tasks and assignments follow a certain syllabus and scope, which are more structured and predictable than what is expected at the workplace. Similarly, these tasks and assignments in school are indicators of performance and avenues for feedback, while at the workplace such similar opportunities are limited (Wendlandt & Rochlen, 2008).
Healthcare training has had elements of practical application, but the adequacy of these exposures is questionable. Clinical shadowing and observation are known to be helpful, but cannot take the place of actual hands-on clinical experience (Brennan et al., 2010). With increased patient safety concerns, there has also been a shift towards simulation, which reduces meaningful contact with patients and poses challenges when students are expected to ultimately transfer their learning to real-life practice (Bleakley & Bligh, 2008).
The security of observing from a distance and the safe environment for experimentation and reflection that students experience in school have to be left behind as they enter the workplace, apply textbook knowledge in real-life situations, and deal with workplace systems and politics (Le Maistre & Paré, 2004). Efforts to prepare for this transition are misplaced (Kilminster et al., 2011), and the training and educational opportunities aimed to help with this transition, such as those in the transitional year, have been lacklustre and ineffective (Lambert et al., 2013). Therefore, a study-work chasm exists in many places, and is a pertinent and critical issue that requires addressing.
Among efforts to help in the transition of students to new HCPs at the workplace, mentorship has been seen as a possible solution (Andrews & Wallis, 1999; Dalgaty et al., 2017). Mentorship, as previously defined by The Standing Committee on Postgraduate Medical and Dental Education in the United Kingdom, is the guidance in “the development and re-examination of their own ideas, learning, and personal and professional development” by “listening and talking in confidence to the mentee” (Oxley & Standing Committee on Postgraduate Medical and Dental Education, 1998). It has also been built into medical practice guidelines, such as that in the UK (General Medical Council, 2012), as a key element in training and professional development.
Mentorship has been seen as a viable approach not only to address any gaps in professional skills, but also aid junior healthcare workers in personalised professional development in the workplace, to enhance job satisfaction, motivation, and self-esteem (Souza & Viney, 2014). The role of a mentor in medical education is to help mentees identify areas of strength and weaknesses in a comfortable and safe learning environment, offer guidance and advice, and motivate and support them to work towards their personal long-term goals (Burgess et al., 2018). Mentors have roles overlapping that of coaches and advisors in medical education. However, coaches tend to focus more on skills or knowledge-based content, and may have a relationship that is of shorter duration and of less depth than between mentors and mentees (Lin & Reddy, 2019). Advisors often oversee a group of individuals in an organisation. Therefore, they develop a more structured relationship compared to that between mentors and mentees, and tend to work towards an outcome based on the needs of the organisation (Hastings & Kane, 2018). Thus, mentoring has been a widely recognised method of helping young people learn, demonstrate their abilities and potential, as well as develop their identity (Fuller & Unwin, 1998). This is extensively explored and studied in many healthcare institutions and systems today.
The aim of this study was to gather information from HCPs about their views towards mentorship as a strategy to help in the transition of newly qualified HCPs from study to work.
II. METHODS
This was a descriptive study on the perceptions of the study-work chasm by HCPs. The protocols were sent to SingHealth Centralised Institutional Review Board (References: 2017/2687 and 2021/2044) and they were deemed exempt from review.
Two three-hour interactive workshops, entitled “Bridging the Study-Work Chasm”, were held in September 2017 and 2018. The workshops invited participation from HCPs in SingHealth, one of the three public healthcare clusters in Singapore.
Each 3-hour workshop comprised two short talks on ‘Is there a Chasm?’ and ‘Bridging the Chasm’, followed by small-group discussions, then sharing and discussions with the large workshop group. A round-up and summary was done by the respective facilitator after each large-group discussion.
The first talk on ‘Is there a Chasm?’ gave a definition of a study-work chasm and the small groups were then asked to describe how such a chasm manifested in the workplace with two questions: “How do we know if a study-work chasm exists?” and “What contributes to this study-work chasm?” After the sharing by the small groups with the large group and some discussion, the facilitator then summarised differences between learning in an academic setting versus learning in the workplace that could contribute to the study-work chasm.
The second talk on ‘Bridging the Chasm’ invited participants to think about and discuss in their small groups how they could bridge the study-work chasm and what were some of the anticipated barriers in doing this. These were then shared with the large group followed by a summary by the facilitator on how coaching and mentoring could be used to bridge the chasm. Facilitators finally concluded the workshop session with a summary of points, addressing questions and answers, and getting participants to complete the survey and workshop evaluation forms.
The survey was carried out by having the participants fill up either an online survey form via scanning a QR code, or a hardcopy version. Implied consent was obtained with the submission of the survey. The survey consisted of 26 items and two open-ended questions (Appendix 1). The first part utilised dichotomous questions to survey participants about their past and current experiences with mentoring, and their views towards whether a study-work chasm existed and whether mentoring could be a solution to bridge this gap. The second part comprised two open-ended questions, asking participants about the elements of an effective mentorship programme, and barriers to having one. The third part allowed participants to rate their level of agreement with 15 statements, related to the benefits of mentoring, the qualification of mentors, and time commitment for mentoring, on a Likert-like scale of 1-5 (1: Strongly Disagree; 5: Strongly Agree). Questions were adapted from a questionnaire that was developed and pilot-tested in a previous study (Lopez et al., 2010).
The anonymised survey data was collated and analysed descriptively. Common repetitive words that appeared in the responses to the open-ended questions were noted and these were grouped into key themes. The percentage of responses representing each theme was tabulated.
III. RESULTS
A. Respondents
Sixty-two participants comprising HCPs from various backgrounds – doctors, dentists, nurses, ancillary workers, and allied health professionals – attended both workshops. There were no repeat participants who attended the two workshops. The data that support the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.figshare.14740332 (Li et al., 2021). Among the 62 participants, 52 completed the survey, achieving a response rate of 83.9%. A majority (78.8%) of the respondents were females. Dentists were the largest healthcare group represented, comprising 42.6% of respondents, followed by doctors, comprising 21.2%. The age group of 30 to 39 years old had the strongest representation of 44.2%. Most respondents had more than five years of working experience, with 44.2% of respondents having six to 10 years of experience, and 51.9% of respondents having more than 10 years of experience (Figure 1). Among the respondents, 96.2% (50 out of 52) felt that a study-work chasm existed in the healthcare workspace, with 90.4% (47 out of 52) indicating that a mentorship programme would help to bridge the chasm, and a majority (90.4%) of respondents agreed that mentoring would be a viable strategy (the remaining 5 respondents were neutral). A good majority of respondents (67.3%) noted they did not have a mentor when they first started work.
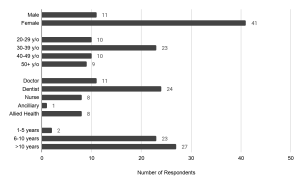
Figure 1. Demographics of survey respondents: gender, age, healthcare group, and number of years of working experience.
B. Key Features of An Effective Mentorship Programme
There was a total of 63 responses describing features of an effective mentorship programme, and the key themes were identified in Figure 2(a). Respondents raised attributes pertaining to the attitude and dynamics of the mentor and mentee, and the organisation of such a programme. Some respondents submitted multiple attributes.
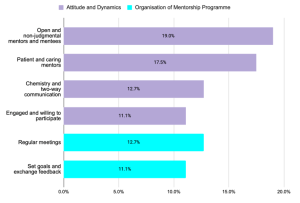
Figure 2(a). Key themes describing key features of an effective mentorship programme
Pertaining to attitude and dynamics, both the mentor and mentee must firstly be engaged and willing to participate in the programme (11.1% of responses). The mentor and mentee should have attributes of open-mindedness and humility (19.0% of responses), and the mentor also ought to be patient, caring, and non-judgmental (17.5% of responses). Finally, the mentor-mentee pair must have good two-way communication, and some degree of interpersonal “chemistry” to bond (12.7% of responses).
Pertaining to the organisation of a mentor-mentee programme, many (12.7% of responses) raised that there should be planned regular meetings, and participants should set goals and expectations and discuss timely feedback (11.1% of responses). However, there was no indication of an ideal frequency of meeting. Some other organisational features were also mentioned. Regarding mentor-mentee pairing, it was noted that the mentor-mentee ratio was an important factor, though there was no indication of a preferred ratio in the responses; others raised that both mentor and mentee should be from relevant fields, for instance from the same department. Some also mentioned that the mentorship programme could be built into the career progression pathway of the mentee to ensure continuation, and even to build it into licensing requirements, such as in the housemanship year for junior doctors.
C. Barriers to Effective Mentorship Programme
There was a total of 53 responses describing barriers to an effective mentorship programme, and the key themes were identified in Figure 2(b). Respondents acknowledged that several aspects of effective mentorship previously mentioned were difficult to achieve, many of which revolved around commitment and mentor-mentee dynamics. A lack of time was identified as the top barrier to implementing a mentoring programme (49.1% of responses). As mentorship can be time consuming, there might be difficulty getting sufficient mentors to willingly commit the time; similarly, it might be challenging to match the availability of mentors and mentees around hectic work hours. Furthermore, there was significant mention (41.5% of responses) about whether the seniority of mentors may result in difficulty breaking the ice with the mentees, or if cultural differences may hinder the understanding of differing perspectives. Some respondents also raised that not all mentors may have the personality, skills or willingness to render effective mentorship, as evidenced in 17.0% of the responses. Finally, some respondents questioned if and how the role of mentors and work supervisors should be differentiated in the workplace.
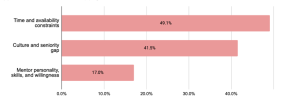
Figure 2(b). Key themes describing barriers to an effective mentorship programme.
Percentages represent the proportion of responses mentioning words related to the theme.
D. Mentorship Benefits and Commitment
On mentorship benefits and commitment, there was strong agreement (more than 70% of participants agreed or strongly agreed) that having a mentor would boost confidence, reduce anxiety, and aid in the transition from study to work (Figure 3). It was also strongly expressed that the participants would have liked a mentor in their first year in the workplace (82.6% agreed), and that the mentorship should extend beyond their first year of work as well – more than half (55.8%) disagreed that the mentorship should only be in the first year, and 90.4% agreed that mentorship would help even in the later years of work. In spite of this, and while a strong majority of 71.2% expressed that they would have liked a long-term mentor-mentee relationship, a large proportion of respondents (44.2%) was neutral towards expecting regular mentor-mentee contact while 38.5% expected mentors to meet regularly with mentees (Figure 4).
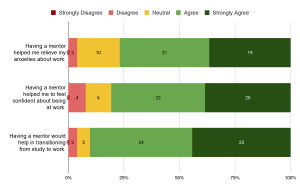
Figure 3. Responses on benefits of mentorship. Numbers in the chart indicate the number of respondents.
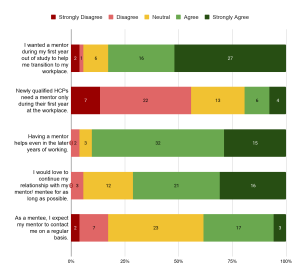
Figure 4. Responses on time commitment of mentorship. Numbers in the chart indicate the number of respondents.
E. Mentor Qualifications and Background
On mentor qualifications, more than half of the respondents agreed that they had adequate knowledge (59.6%) and skills (53.8%) to function as effective mentors. Most of those who agreed (74.2% for knowledge, 67.9% for skills) were HCPs with more than 10 years of experience. A significant proportion responded neutrally as well, with 28.8% and 34.6% for knowledge and skills, respectively. Majority of them (71.4% for knowledge, 52.9% for skills) had 6 to 10 years of work experience in healthcare. Nevertheless, many more (78.8%) agreed that receiving prior training or orientation in mentoring could increase their effectiveness as mentors. When asked about whether young professionals two to three years into their professions make the best mentors, there was strong neutrality in the response (46.1%, the largest proportion). It was noted that all the neutral responses were from HCPs with more than 5 years of experience, with a significant proportion of them (52.2%) having 6 to 10 years of work experience. All except two of the respondents who gave neutral responses had experience as a mentor. Majority (59.6%) preferred mentors to be paired with mentees with similar backgrounds; similarly, there was significant uncertainty around whether mentors from dissimilar professions could be effective, with the same proportion (38.5%) of respondents agreeing and holding a neutral stance towards this view (Figure 5).

Figure 5. Responses on qualification of mentors. Numbers in the chart indicate the number of respondents.
IV. DISCUSSION
The results from this study showed that there was a perceived study-work chasm among this cohort of HCPs. Given the wide range of backgrounds and years of work experience of the respondents, it is also evident that the chasm was perceived across different HCPs and batches of new HCPs entering the workforce.
Indeed, it was reported in the literature that newly qualified HCPs face challenges in the new workplace, indicating a study-work chasm. One such challenge is the lack of hands-on clinical skills. Junior doctors beginning practice and taking direct responsibility for patients found themselves undertaking clinical tasks for which they felt inadequately trained for (Lambert et al., 2013). As such, they expressed anxiety over their competence, especially in areas like prescribing (Brennan et al., 2010; Matheson & Matheson, 2009). It was also reported that new doctors lacked knowledge in pathology and therapeutics (Lempp et al., 2004). These gaps can bring dire consequences to clinical care, influencing assessment, treatment, and outcome of patients (Smith & Poplett, 2002).
In addition, many professionals fresh from school experienced difficulties in communicating with patients. The immediate switch to a professional relationship with patients proved stressful for them, especially in the first few weeks of work (Lempp et al., 2004). The findings of the present study mirror this sentiment with a large proportion of the respondents citing their wish for a mentor in their first year or work. The difficulty was especially evident in such school-work transitions revolved around breaking bad news, dealing with difficult and violent patients, and communicating with people with mental illnesses. Despite active practice and drilling with simulated scenarios in school, fresh graduates still expressed that they were inadequately prepared for these in real life (Matheson & Matheson, 2009).
Mentorship was seen very favourably as a possible solution to bridging the chasm. Among these, more than half of the respondents (67.3%) had not experienced mentoring during their initial years of work, indicating that mentorship had not been widely implemented, and can be a new strategy for exploration in the local healthcare system. It is worthy to note that many of the respondents who had experienced mentorship had also viewed mentorship positively. Similarly, residents of a medical residency programme in Singapore viewed mentorship as being crucial and beneficial to their training, as mentors were able to provide guidance and encouragement, and create a more well-rounded learning environment (Chua et al., 2020). This implies that mentorship could potentially exert a positive impact on HCPs.
The benefits of mentorship have been well-reported worldwide. In particular, there have been reports emphasising its benefits on the emotional and psychological health of healthcare workers. For instance, in the United Kingdom, senior doctors as mentors and teachers helped train fresh graduates on the job, and reduced their stress (Brennan et al., 2010), increased motivation, and boosted self-esteem (Souza & Viney, 2014). In Saudi Arabia, use of coaching appeared to reduce depression and anxiety among HCPs in the short-term (Aboalshamat et al., 2015). A study in Denmark reported improved professional identity among their fresh doctors who had undergone group mentorship sessions, and participants developed new ways to deal with their new professional roles with increased awareness of their thinking, feelings, and reactions, making the stressful transition into their workplace more bearable (de Lasson et al., 2016). All these resonate well with the responses from this study, that mentorship can reduce anxiety and boost confidence in new HCPs.
Studies have shown attributes of an effective mentorship programme. Many of these attributes relate to the attitudes of mentors and mentees – trust and respect, responsibility, and taking initiative. The importance of having good communication, connection, and common values between mentors and mentees were also emphasised. These were consistent across countries, as seen in studies in North America (Straus et al., 2013) and the United Kingdom (Ssemata et al., 2017). Notably, these attributes were mentioned significantly in the responses collected in this study as well, specifically those relating to mentor-mentee dynamics.
Barriers to effective mentorship have also been brought up in several studies, and draw similarities to the responses obtained from this study. It was summarised that challenges can arise when there is a mismatch of goals, expectations, and time commitment between mentors and mentees. There can also be hindrances to communication due to generational and personality differences (Zerzan et al., 2009). Qualitative studies targeting students, junior faculty mentees and senior faculty members at healthcare institutions uncovered similar issues (Ssemata et al., 2017; Straus et al., 2013).
In this study, questions and uncertainties were raised pertaining to whether mentors should be supervisors as well, and how regular meetings should be held. It is noteworthy that in the United Kingdom, Ssemata et al. (2017) reported findings that there presented conflicts of interest when mentors were also supervisors. Such an arrangement posed problems with performance judgement, competition, and the amount of honesty in the mentor-mentee relationship. In the same study, it was noted that the mentor-mentee pairing could likely be better maximised if the pairing was selected mutually by the mentor and mentee, instead of being pre-assigned, as this would ensure better chemistry and as a result better commitment and motivation towards the relationship. Regular time commitment was generally agreed upon in literature; however, discussions on frequency were inconclusive, similar to the responses of this present study. It was reported in North America that the preferred frequency of meet-ups according to participating mentors and mentees ranged widely from monthly to half-yearly (Straus et al., 2013).
The literature has identified some other barriers to setting up of an effective mentorship programme not surfaced in our study that are worthy of note. In particular, factors relating to the organisation or system play a big part in the effectiveness of the mentorship programme. Geographical location, for instance, is one barrier identified in systems where mentors and mentees may be situated at different sites, such as different hospital campuses, and have difficulty meeting (Soklaridis et al., 2015). This can be the case when HCPs are posted to different clinical sites, or when HCPs across sites are linked up to increase diversity in mentorship. The strong focus by organisations on delivering clinical service may also have spared little resources and manpower for mentorship programmes (Ploeg et al., 2008), rendering such programmes inadequate support. For instance, the use of manpower and facilities for mentorship activities in job-specific areas such as a clinical simulation can be limited when these are dedicated to patient care (Morgan et al., 2018). Finally, a strong culture of hierarchy seen in healthcare settings, such as among nurses, can be a hindrance to the open-mindedness and non-judgemental nature of mentoring that the programme aspires to achieve (Morgan et al., 2018).
Nevertheless, it is clear from existing literature that a formalised mentorship programme would ensure the best outcomes, as time and resources can be dedicated to the programme to ensure better recruitment, matching and co-ordination between mentors and mentees, proper structure and guidelines so as to ensure mentorship outcomes are reviewed at adequate intervals and achieved within a desired timeframe, and adequate training for mentors to render support and guidance to their mentees. A proper programme can likely reduce the challenges to effective mentorship as raised by the respondents of this study, as well as in other studies. Lack of experience of mentors, for instance, was a main failure in mentoring relationships (Straus et al., 2013). Similarly, in this study, a significant finding was that there was a larger proportion of respondents with relatively fewer years of work experience who gave neutral responses towards statements on whether they had sufficient knowledge and skills to function effectively as mentors, compared to statements on benefits of mentorship and their preferences towards having a mentorship programme. This indicated a lower perceived confidence of these respondents in their effectiveness as mentors. In line with this, there was strong agreement that receiving training and orientation in mentoring would have been preferred prior to them assuming such mentoring roles, presumably regardless of their prior work experiences. This reinforces the need for proper training and resources for mentors in order for the mentorship programme to see positive effects.
This study presents with some limitations. Firstly, while there was a diverse range of backgrounds among the workshop participants, the proportions may not be representative of the healthcare landscape in Singapore. As such, this may introduce a potential source of bias towards views of predominant groups of participants such as the dentists. Nevertheless, the findings provide a useful baseline understanding of how other healthcare professionals view mentoring. This could, in turn, set the stage for more extensive work in this area among other healthcare professionals. Secondly, the respondents participated in the workshop prior to responding to this survey. The workshop raised awareness towards a study-work chasm and presented mentorship as one of the possible solutions. Therefore, it might have resulted in a stronger perception of this chasm among respondents, and induced more favourable views towards mentorship. Nevertheless, the participants’ positive views towards mentorship could be viewed as indications of the strong agreement they had towards mentorship as a solution highlighted in the workshop. In future workshops, qualitative focused-group discussions can be carried out, and questionnaires can be administered before and after the workshop, so as to establish a more accurate perception of study-work chasm among participants.
V. CONCLUSION
This study has shown that with a perceived presence of a study-work chasm in the healthcare landscape in Singapore, there were strong preferences for a mentorship programme in bridging this chasm. The benefits of a mentorship programme, and the attributes and challenges of setting up such an effective programme were identified, and echo the findings from existing studies from other regions and healthcare systems in the world. In particular, there were emphases on positive attitudes of mentors and mentees, and alignment of expectations between them. There was also strong indication that mentors require proper training. A formalised mentorship programme will best serve mentors and mentees by committing the proper time and resources to ensure its effectiveness.
This study lays the groundwork for future efforts to help fresh graduates better transition into the healthcare workplace using mentorship programmes. In particular, the study targeted healthcare professionals working in the healthcare system in Singapore and revealed their sentiments and opinions towards mentorship, paving the way for local efforts to improve healthcare education and mentorship. Moving forward, further studies can be carried out in an in-depth manner to investigate specific areas of concern pertaining to setting up an effective mentorship programme, such as mentor training, time commitment, and mentor-mentee pairing. Studies can be expanded to larger pools of participants, and targeted at specific sectors and participant groups, for example medical doctors in their housemanship year, to better cater to specific professional needs. Focused-group discussions can be carried out to collect more detailed, qualitative responses and feedback from potential mentors and mentees. Furthermore, this information can be used to engage stakeholders in public healthcare institutions in Singapore and the region, and execute pilot tests of formalised mentorship programmes tailor-made to the institution’s structure and the newly qualified HCPs’ needs.
Notes on Contributors
ELY Tan, ML Wong, and MMA Ong planned, developed, and conducted the workshops and data collection. H Li and ELY Tan, together with ML Wong and MMA Ong planned and wrote the manuscript. All authors read and approved the final manuscript.
Ethical Approval
The study protocols were sent to SingHealth Centralised Institutional Review Board (References: 2017/2687 and 2021/2044) and they were deemed exempt from review.
Data Availability
The data that support the findings of this study are openly available in Figshare with DOI: https://doi.org/10.6084/m9.figshare.14740332
Acknowledgement
The authors would like to thank the administrative team from SingHealth Duke-NUS Oral Health Academic Clinical Programme (Education) for their help and support in the smooth running of the workshops and collection of data.
Funding
No funding was sought for this study.
Declaration of Interest
The authors declare that they have no conflicts of interest, and do not foresee any future competing interests.
References
Aboalshamat, K., Hou, X.-Y., & Strodl, E. (2015). The impact of a self-development coaching programme on medical and dental students’ psychological health and academic performance: A randomised controlled trial. BMC Medical Education, 15(1), 134. https://doi.org/10.1186/s12909-015-0412-4
Andrews, M., & Wallis, M. (1999). Mentorship in nursing: A literature review. Journal of Advanced Nursing, 29(1), 201–207. https://doi.org/10.1046/j.1365-2648.1999.00884.x
Bleakley, A., & Bligh, J. (2008). Students learning from patients: Let’s get real in medical education. Advances in Health Sciences Education, 13(1), 89–107. https://doi.org/10.1007/s10459-006-9028-0
Brennan, N., Corrigan, O., Allard, J., Archer, J., Barnes, R., Bleakley, A., Collett, T., & De Bere, S. R. (2010). The transition from medical student to junior doctor: Today’s experiences of tomorrow’s doctors. Medical Education, 44(5), 449–458. https://doi.org/10.1111/j.1365-2923.2009.03604.x
Burgess, A., van Diggele, C., & Mellis, C. (2018). Mentorship in the health professions: A review. The Clinical Teacher, 15(3), 197–202. https://doi.org/10.1111/tct.12756
Chua, M. J., Foo, G. L., & Kwek, E. B. K. (2020). A tiered mentorship framework in an Orthopaedic Surgery Residency Programme. The Asia Pacific Scholar, 5(1), 54–60. https://doi.org/10.29060/TAPS.2020-5-1/OA2095
Dalgaty, F., Guthrie, G., Walker, H., & Stirling, K. (2017). The value of mentorship in medical education. The Clinical Teacher, 14(2), 124–128. https://doi.org/10.1111/tct.12510
de Lasson, L., Just, E., Stegeager, N., & Malling, B. (2016). Professional identity formation in the transition from medical school to working life: A qualitative study of group-coaching courses for junior doctors. BMC Medical Education, 16(1), 165. https://doi.org/10.1186/s12909-016-0684-3
Fuller, A., & Unwin, L. (1998). Reconceptualising apprenticeship: Exploring the relationship between work and learning. Journal of Vocational Education & Training, 50(2), 153–173. https://doi.org/10.1080/13636829800200043
General Medical Council. (2012, March 12). Leadership and management for all doctors. https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/leadership-and-management-for-all-doctors
Hastings, L. J., & Kane, C. (2018). Distinguishing mentoring, coaching, and advising for leadership development. New Directions for Student Leadership, 2018(158), 9–22. https://doi.org/10.1002/yd.20284
Hofler, L., & Thomas, K. (2016). Transition of new graduate nurses to the workforce. North Carolina Medical Journal, 77(2), 133-136. https://doi.org/10.18043/ncm.77.2.133
Kilminster, S., Zukas, M., Quinton, N., & Roberts, T. (2011). Preparedness is not enough: Understanding transitions as critically intensive learning periods. Medical Education, 45(10), 1006–1015. https://doi.org/10.1111/j.1365-2923.2011.04048.x
Lambert, T. W., Surman, G., & Goldacre, M. J. (2013). Views of UK-trained medical graduates of 1999–2009 about their first postgraduate year of training: National surveys. BMJ Open, 3(4), e002723. https://doi.org/10.1136/bmjopen-2013-002723
Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation (p. 138). Cambridge University Press. https://doi.org/10.1017/CBO9780511815355
Le Maistre, C., & Paré, A. (2004). Learning in two communities: The challenge for universities and workplaces. Journal of Workplace Learning, 16(1/2), 44–52. https://doi.org/10.1108/13665620410521503
Lempp, H., Cochrane, M., Seabrook, M., & Rees, J. (2004). Impact of educational preparation on medical students in transition from final year to PRHO year: A qualitative evaluation of final-year training following the introduction of a new Year 5 curriculum in a London medical school. Medical Teacher, 26(3), 276–278. https://doi.org/10.1080/248-0142159042000192046
Li, H., Tan, E. L. Y., Wong, M. L., & Ong, M. M. A. (2021). Tackling study-work chasm: Perceptions of the role of mentorship in the healthcare workplace [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14740332
Lin, J., & Reddy, R. M. (2019). Teaching, mentorship, and coaching in surgical education. Thoracic Surgery Clinics, 29(3), 311–320. https://doi.org/10.1016/j.thorsurg.2019.03.008
Lopez, N., Johnson, S., & Black, N. (2010). Does peer mentoring work? Dental students assess its benefits as an adaptive coping strategy. Journal of Dental Education, 74(11), 1197–1205. https://doi.org/10.1002/j.0022-0337.2010.74.11.tb04993.x
Matheson, C., & Matheson, D. (2009). How well prepared are medical students for their first year as doctors? The views of consultants and specialist registrars in two teaching hospitals. Postgraduate Medical Journal, 85(1009), 582. https://doi.org/10.1136/pgmj.2008.071639
Morgan, M. C., Dyer, J., Abril, A., Christmas, A., Mahapatra, T., Das, A., & Walker, D. M. (2018). Barriers and facilitators to the provision of optimal obstetric and neonatal emergency care and to the implementation of simulation-enhanced mentorship in primary care facilities in Bihar, India: A qualitative study. BMC Pregnancy and Childbirth, 18(1), 420. https://doi.org/10.1186/s12884-018-2059-8
Oxley, J., & Standing Committee on Postgraduate Medical and Dental Education. (1998). Supporting doctors and dentists at work: An enquiry into mentoring. SCOPME.
Ploeg, J., de Witt, L., Hutchison, B., Hayward, L., & Grayson, K. (2008). Evaluation of a research mentorship program in community care. Evaluation and Program Planning, 31(1), 22–33. https://doi.org/10.1016/j.evalprogplan.2007.10.002
Smith, G. B., & Poplett, N. (2002). Knowledge of aspects of acute care in trainee doctors. Postgraduate Medical Journal, 78(920), 335. https://doi.org/10.1136/pmj.78.920.335
Soklaridis, S., López, J., Charach, N., Broad, K., Teshima, J., & Fefergrad, M. (2015). Developing a mentorship program for psychiatry residents. Academic Psychiatry, 39(1), 10–15. https://doi.org/10.1007/s40596-014-0163-2
Souza, B. D., & Viney, R. (2014). Coaching and mentoring skills: Necessities for today’s doctors. BMJ, 348, g4244. https://doi.org/10.1136/bmj.g4244
Ssemata, A. S., Gladding, S., John, C. C., & Kiguli, S. (2017). Developing mentorship in a resource-limited context: A qualitative research study of the experiences and perceptions of the makerere university student and faculty mentorship programme. BMC Medical Education, 17(1), 123. https://doi.org/10.1186/s12909-017-0962-8
Straus, S. E., Johnson, M. O., Marquez, C., & Feldman, M. D. (2013). Characteristics of successful and failed mentoring relationships: A qualitative study across two academic health centers. Academic Medicine, 88(1), 82–89. https://doi.org/10.1097/ACM.0b013e31827647a0
Teunissen, P. W., & Westerman, M. (2011). Opportunity or threat: The ambiguity of the consequences of transitions in medical education. Medical Education, 45(1), 51–59. https://doi.org/10.1111/j.1365-2923.2010.03755.x
Wendlandt, N. M., & Rochlen, A. B. (2008). Addressing the college-to-work transition: Implications for university career counselors. Journal of Career Development, 35(2), 151–165. https://doi.org/10.1177/0894845308325646
Zerzan, J. T., Hess, R., Schur, E., Phillips, R. S., & Rigotti, N. (2009). Making the most of mentors: A guide for mentees. Academic Medicine, 84(1), 140–144. https://doi.org/10.1097/ACM.0b013e3181906e8f
*Eileen Lew
National Dental Centre Singapore
5 Second Hospital Avenue,
Singapore 168938
Email: elaine.tan.l.y@singhealth.com.sg
Submitted: 13 December 2021
Accepted: 22 April 2022
Published online: 5 July, TAPS 2022, 7(3), 1-9
https://doi.org/10.29060/TAPS.2022-7-3/OA2722
Claire Jing-Wen Tan1, Cathryn Cai2, Farida Ithnin2 & Eileen Lew2
1Department of Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Women’s Anaesthesia, KK Women’s and Children’s Hospital, Singapore
Abstract
Introduction: The COVID-19 pandemic has caused significant disruption to undergraduate medical education globally, with worldwide implementation of social distancing and lock-down measures. This systematic review aims to identify challenges in undergraduate medical education during the pandemic and report creative approaches that have been employed to ensure continuity of education.
Methods: A MEDLINE (PubMed) search was performed for articles published between 1 February 2020 and 1 September 2020, corresponding to the pandemic’s global upsurge. Studies, commentaries, perspectives, and correspondence reporting challenges, adaptations and innovations in undergraduate medical education were screened. Data was grouped in accordance with the research questions it sought to address and analysed qualitatively.
Results: 43 studies were included. The COVID-19 pandemic has resulted in lost opportunities for clinical exposure, reduced motivation, and heightened anxiety among medical students. Traditional teaching and assessment methods have transitioned to virtual platforms, harnessing video conferencing, social media, and virtual or augmented reality technologies. The long-term effectiveness of these solutions is uncertain, but immediate benefits conferred include increased access, improved time management, and cultivation of self-directed learning. The lack of authentic clinical experiences and patient interaction remains a major concern. Technical challenges and digital fatigue were also highlighted as pertinent challenges.
Conclusions: The COVID-19 pandemic has provided unexpected, yet invaluable opportunities to explore new pedagogies that may be instrumental in shaping medical education in the new norm. As future members of the healthcare workforce, medical students should be integrated into current healthcare systems to equip them with knowledge and skills to manage future pandemics.
Keywords: COVID-19, Education, Medical, Undergraduate, Medical Student, Telemedicine
Practice Highlights
- The COVID-19 pandemic has caused significant disruption to undergraduate medical education globally.
- Undergraduate medical students faced diminished clinical exposure, poor motivation, and isolation.
- The pandemic has provided unexpected yet invaluable opportunities to explore new teaching pedagogies.
- Institutions should continually adapt these strategies as methods of teaching in the new norm.
I. INTRODUCTION
The appearance of the novel coronavirus (SARS-CoV-2) was first reported in December 2019 (Huang et al., 2020). Since then, the COVID-19 outbreak has become a full-blown global health emergency, with more than 5.3 million deaths reported to date, disruptions in economies and education systems, and increased mental health issues amidst a climate of uncertainty (Torales et al., 2020).
Major disruptions to medical education and training have been experienced worldwide. At the height of the pandemic, universities and medical schools suspended in-campus learning and clinical training to curb the spread of infections (Murphy, 2020; Theoret & Ming, 2020). Non-essential health services were ceased to focus resources on managing the pandemic. With medical faculty deployed to the frontlines, little time and capacity was available for training and teaching. There were reservations deploying medical students in clinical areas, due to safety concerns and consumption of personal protective equipment (PPE) in the face of shortages (Hilburg et al., 2020).
Mitigating measures have challenged academic institutes to explore new pedagogies to sustain and bolster education efforts beyond the crisis. Creative approaches to ensure continuity of medical student education include the transition to e-learning and virtual clerkships, enabled through online video-conferencing platforms, social media, and virtual reality technology. Assessment formats have also been adapted to accommodate virtual evaluation of clinical competencies. While the effectiveness of these approaches remains to be proven, they are instrumental in allowing medical education to continue during the pandemic and into the new norm.
This qualitative systematic review aims to define the challenges associated with medical student education at the height of the COVID-19 pandemic, highlight creative approaches and innovations that were employed to sustain medical education in these unprecedented times, and review their limitations and effectiveness.
II. METHODS
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Page et al., 2021). Literature search was performed on MEDLINE (PubMed) using a combination of the following search terms: (COVID-19 OR pandemic) AND (undergraduate medical education OR undergraduate medical training). The search was tailored for the period of 1 February 2020 to 1 September 2020, to focus on the height of the pandemic.
Articles were included if they met the following criteria: published in English; reported challenges, strategies, and adaptations in conducting undergraduate medical education during the COVID-19 pandemic. To ensure comprehensive coverage, case reports, case and cohort studies, commentaries, perspectives, and correspondence were included. Articles pertaining to postgraduate medical education and non-medical education, non-English articles and systematic reviews were excluded.
Two reviewers (CJT and CC) independently screened the titles and/or abstracts of all articles and selected only articles that met inclusion criteria. Any disagreement was resolved by discussion with senior authors (FI and EL). Data extracted included: challenges encountered in the implementation of undergraduate teaching; innovations, strategies and adaptations employed to facilitate teaching and assessment; perceived limitations and effectiveness of described strategies; original authors’ conclusions. The data was collated on a spreadsheet, grouped by categories, and analysed qualitatively.
III. RESULTS
A total of 123 studies were identified using the search strategy, of which 43 studies eventually met inclusion criteria. The PRISMA study flow-diagram (Figure 1) demonstrates our research algorithm. The data that support the findings of this study are openly available in Figshare at http://doi.org/10.6084/m9.figshare.172968 56 (Tan et al., 2021).
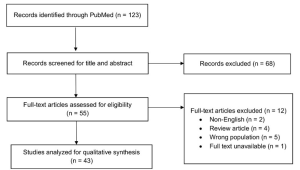
Figure 1: PRISMA flow-diagram of study selection
A. Challenges Arising from the COVID-19 Pandemic
1) Reduced clinical exposure:
Due to the enforcement of safe distancing measures, nearly all medical schools have suspended in-person classes and transitioned to online teaching. Scheduled summer and term breaks have been brought forward to provide a state of academic quarantine (Ashokka et al., 2020). Loss of patient interaction has been consistently cited as one of the biggest challenges in delivering clinical education during the pandemic. Across institutions, medical students have been withdrawn from clinical postings to protect them from infectious transmission and mitigate PPE shortages (Hilburg et al., 2020). With deployment of healthcare workers to the frontlines, clinicians focused attention and resources on patient care, with education taking a backseat (Hilburg et al., 2020; Tolsgaard et al., 2020).
Pre-clerkship medical students were less affected by the online transition, as preclinical contents can be easily adapted for digital learning (Newman & Lattouf, 2020). In contrast, students on clerkship rotations for procedural-based disciplines who rely heavily on patient interactions were severely impacted (Calhoun et al., 2020; Darras et al., 2021; Khalil et al., 2020). Without direct patient interaction, students cannot fully master physical examination skills, although history-taking and other communication skills can arguably be taught through virtual interactions with real or simulated patients. The development of professionalism and communication skills, including discussion of care plans in a multidisciplinary setting and presentation of academic work at professional platforms (Hammond et al., 2020; Rafi et al., 2020), have also been compromised.
2) Unpreparedness for the future:
With a truncated curriculum and migration to digital learning, some students have been disheartened by missed learning opportunities (Rallis & Allen-Tejerina, 2020). They felt incompetent (Hilburg et al., 2020) and unprepared for clinical examinations and patient encounters (Shahrvini et al., 2020). A survey study conducted across 33 medical schools in the United Kingdom reported that 49.5% of final-year students started work in hospitals ahead of anticipated schedule to meet increased manpower demands during the pandemic (Choi et al., 2020). Affected students admitted to feeling ill-equipped, due to the curtailing of final-year examinations and student assistantship programmes (Choi et al., 2020). There is concern that loss of training opportunities could disrupt the supply chain of specialists (Tolsgaard et al., 2020) and future workforce planning (Halbert et al., 2020).
The sense of inadequacy among students is compounded by widespread cancellation of summer elective placements and research programs, originally intended to provide avenues for further enrichment (Rallis & Allen-Tejerina, 2020). Consequently, students have missed out on opportunities to explore interests and immerse in rigorous clinical and research environments to guide them in making informed residency choices (Go & Rajasekaran, 2020).
3) Loss of motivation:
With the move to online learning and cancellation of examinations in some universities, students reported diminished motivation to study (Khalil et al., 2020), exacerbated by inexperience in distant-based learning, poor technical skills and frequent technical difficulties (Muflih et al., 2020). Students have also expressed frustration at the lack of clear communication with faculty members regarding curriculum and assessment plans, fueling negative learning attitudes (Shehata et al., 2020).
4) Socio-emotional isolation:
With loss of social interaction, medical students felt increasingly disconnected from their peers. Interruptions in normal routines and pressure from stay-home orders further fuelled feelings of isolation, apprehension and uncertainty about the future (Shahrvini et al., 2020). An increase in mental health issues was reported among medical students during the pandemic (Shahrvini et al., 2020). To address this, institutions have strengthened peer support systems (Ashokka et al., 2020) and initiated coaching programmes to impart coping skills and help students pursue personalised goal setting (Maini et al., 2020).
B. Innovations, Adaptations, and Strategies Employed in Undergraduate Medical Education
1) Online learning platforms:
Traditional face-to-face teaching has been largely replaced by online learning. ‘Live’ synchronous learning conducted over video-conferencing platforms, including Zoom, Microsoft Team, Google Hangouts, Skype, and WebEx, incorporate functions like screen-sharing, virtual whiteboards, mind-mapping tools, and polling for an interactive experience (Shahrvini et al., 2020). ‘Break-out’ room functions allow students to be further divided into smaller groups for interactive discussions (Darras et al., 2021; Ferrel & Ryan, 2020). Students can also ask and answer questions using the chat function or microphones (Singh et al., 2020). Synchronous tutorial sessions can also be recorded for future reference (Atreya & Acharya, 2020). Some institutions have adopted a flipped classroom approach, with learning material provided to students in advance of online discussions (Naidoo et al., 2020; Singh et al., 2020). Asynchronous lectures, on the other hand, are pre-recorded and have the distinct advantage of cultivating self-directed learning (Farooq et al., 2020).
Furthermore, learning management systems, like Google Classroom, Blackboard, Impartus, and Slack provide centralised platforms for tutors to share teaching materials and multimedia resources, with plug-ins to track students’ progress (Singh et al., 2020). Medical schools have also collaborated to share online resources, through OnlineMedEd, Geeky Medics, Oxford Medical Simulation, and Aquifer (Schaffir et al., 2020).
2) Social media:
Taking advantage of its popularity, tutors have turned to social media platforms for the dissemination of class schedules and learning materials during the pandemic (Iqbal et al., 2020). In one medical college, Telegram was used to create class groups and upload educational resources (Iqbal et al., 2020). At another institution, ophthalmology faculty members created Whatsapp student groups to upload quizzes, reference materials, and teaching videos (Sud et al., 2020).
The use of social media successfully enhanced student participation and collaborative learning (Naidoo et al., 2020). The ability to stay anonymous gave students the confidence to discuss topics without fear of being judged by their peers (Iqbal et al., 2020). As the complex technical interfaces, information overload and digital fatigue could cause distractions (Iqbal et al., 2020), its use should be moderated.
3) Virtual laboratory sessions:
Traditional anatomy classes, using ‘live’ cadaveric dissections, have been discontinued and substituted by novel online formats at some institutions (Darras et al., 2021). Students have been taught to appreciate anatomy via three-dimensional (3D) computer models (Remtulla, 2020) and virtual dissections on digital applications (Longhurst et al., 2020). Comprehensive learning materials have also been uploaded on Virtual Learning Environments (Ashokka et al., 2020; Longhurst et al., 2020; Naidoo et al., 2020). Institutions also conducted real-time tutorials and ‘live’ dissection sessions online (Longhurst et al., 2020). The University of Hong Kong implemented a web-based programme to provide basic surgical skills training to final-year undergraduate students. Tutors demonstrated surgical skills on ‘live’ camera, while students practised suturing at home using kits that were distributed in advance (Co & Chu, 2020).
4) Virtual clinical experience:
Technological advancements have enabled the use of simulations and virtual reality to address gaps associated with distance learning (Remtulla, 2020). Students have been able to learn history taking, clinical reasoning and communication skills via remote role-play with simulated patients (Mukhtar et al., 2020). Videos demonstrating communication, physical examination and procedural skills have also been utilised as teaching aids (Sam et al., 2020). Some universities have even implemented virtual placements with live-streamed ward rounds, empowering students to participate remotely in discussions and case presentations (Sam et al., 2020). At one university, students on virtual surgical electives could observe surgeries remotely, as attending surgeons wore head-mounted cameras to capture the surgical field (Chao et al., 2021).
With the ramp-up of telemedicine services during the pandemic, students have had opportunities to facilitate patient care through telephone or video consultations, enabling them to develop to cultivate interpersonal skills. Students have been roped in to provide virtual updates to patients’ families (Hilburg et al., 2020) and assist in scribing during virtual consultations (Rallis & Allen-Tejerina, 2020). Time pressures (Oki et al., 2021) and breaches in patient confidentiality (Rallis & Allen-Tejerina, 2020) were highlighted as potential concerns. With telemedicine being increasingly integrated into mainstream health services in the new norm, it is imperative to incorporate telemedicine training into the medical curricula to produce a telehealth-ready workforce (Iancu et al., 2020).
Although virtual clinical clerkships cannot fully substitute for hands-on clinical experiences (Nic Dhonncha & Murphy, 2021; Rafi et al., 2020; Roskvist et al., 2020; Sud et al., 2020), they have a role in promoting student engagement with tutors and patients, and helping students develop indispensable clinical skills (Chao et al., 2021).
5) Assessments:
Due to logistical, manpower and technical constraints, some universities have cancelled semester assessments (Tokuç & Varol, 2020). Others have adopted alternative methods to evaluate competencies. A study conducted at 14 medical universities in the United Kingdom and Republic of Ireland revealed that 7% of universities cancelled written examinations, 14% eliminated summative practical assessments and a further 36% cancelled assessments altogether (Longhurst et al., 2020). Only 21% of schools implemented online digital spotter or open-book examinations (Longhurst et al., 2020). Institutions that eliminated examinations altogether laid claim to facing difficulties adapting traditional examination formats to online assessments, and cited the lack of experience and training as underlying factors (Farooq et al., 2020).
Open-book examinations were implemented at some universities and were associated with reduced pressure among students (Hilburg et al., 2020; Nic Dhonncha & Murphy, 2021). Due to its initial success, there are now calls for widespread adoption of open-book examination formats (Hammond et al., 2020). Other institutions have opted for continuous formative assessment in place of scheduled summative assessments (Choi et al., 2020; Shehata et al., 2020).
For strict proctoring to maintain academic integrity during online examinations, web cam and screen capture functions have been harnessed (Hilburg et al., 2020; Mukhtar et al., 2020). Grading systems for examinations have also been modified. Instead of assigning specific grades based on performance, fourth-year medical students on elective courses at the University of Washington School of Medicine were assessed on a pass/fail basis, significantly alleviating students’ stress (Calhoun et al., 2020).
Clinical examinations have been more challenging to administer in compliance with enforced risk mitigation measures. Some schools have chosen to focus on theory assessments instead, while others successfully conducted virtual Objective Structured Clinical Examinations (OSCE), focusing on practical skills and communication capabilities (Naidoo et al., 2020).
C. Barriers and Limitations Associated with Innovations and Adaptations
1) Reduced tutor-student interaction:
Some reports suggest that switching to online learning platforms has compromised student engagement and collaboration (Ashokka et al., 2020; Ferrel & Ryan, 2020; Longhurst et al., 2020). Unlike face-to-face tutorials that facilitate vibrant discussion, online tutorials involve tutors speaking to a blank screen (Atreya & Acharya, 2020; Khalil et al., 2020; Roberts et al., 2020; Sud et al., 2020). The absence of visual cues may lead to communication gaps and loss of personal touch (Khalil et al., 2020; Mukhtar et al., 2020). Specifically, tutors have claimed to face difficulty in gauging students’ understanding (Hilburg et al., 2020; Mukhtar et al., 2020).
Furthermore, it was observed that some students have adopted passive learning attitudes (Sandhaus et al., 2020). It has become exceedingly difficult to engage students in virtual rooms and to retain their attention over prolonged periods (Atreya & Acharya, 2020; Farooq et al., 2020; Roberts et al., 2020). A handful of students were observed to switch off their cameras and mute their microphones, while others claimed they did not feel comfortable to speak up (Roberts et al., 2020).
Strategies have been formulated to increase student participation. Tracking of attendance has been proposed as a means to improve attendance rate, although it remains possible that students may log on but engage in their own activities without paying attention (Atreya & Acharya, 2020). Some tutors have incorporated interactive online quizzes during tutorials (Farooq et al., 2020), while others have decreased tutorial group sizes to optimise engagement (Joseph et al., 2020).
2) Reduced quality of instruction:
With short notice for curricular re-design, universities have faced struggles to obtain the resources necessary for a smooth transition, resulting in disruption to students’ learning in the interim (Oki et al., 2021) and reduced quality of instruction (Shahrvini et al., 2020). Medical students at one university experienced teaching disruption for four weeks during the transition to new teaching methods (Roberts et al., 2020). Tutors have also reported knowledge gaps and time constraints in creating new online educational content, amidst competing professional and personal duties during the pandemic (Newman & Lattouf, 2020).
3) Digital fatigue:
Long hours spent in front of devices have led to exhaustion, poor concentration, and loss of engagement (Shahrvini et al., 2020; Singh et al., 2020). Students also provided feedback on the excessive numbers of lectures and inappropriately long lessons (Khalil et al., 2020; Rafi et al., 2020).
4) Technical challenges:
With the growing reliance on technology, technical issues could compromise the quality of learning and affect learners’ and tutors’ experiences (Atreya & Acharya, 2020; Farooq et al., 2020; Khalil et al., 2020; Sud et al., 2020). Online lectures have often been conducted without real-time technical support (Longhurst et al., 2020), as most institutions lack a dedicated information technology (IT) department (Farooq et al., 2020). Given the steep learning curve with IT (Remtulla, 2020), it is not surprising that students have reported a lack of confidence in completing online assignments (Muflih et al., 2020). Institutions should provide basic computer literacy courses to students and tutors (Muflih et al., 2020).
With families staying home during lockdowns, students often had to share devices (Sud et al., 2020) and internet access (Atreya & Acharya, 2020; Roskvist et al., 2020) with household members. Online learning has also been adversely impacted by limited internet connectivity at remote geographical locations (Cruess et al., 2014; Farooq et al., 2020; Remtulla, 2020; Roskvist et al., 2020) and electrical interruptions from bad weather (Atreya & Acharya, 2020). Although the subscription of costly internet data bundles could circumvent these challenges, socioeconomic disparities could result in the less privileged students falling through the cracks. Hence, institutions must ensure the benefits of online education can be shared equitably by all students (Muflih et al., 2020).
D. Effectiveness of Innovations and Adaptations in Delivering Medical Education
1) Effectiveness of digital learning:
Overall, medical students expressed satisfaction with digital learning during the pandemic (Sandhaus et al., 2020), and reported ample opportunities for clarification (Singh et al., 2020) and communication with classmates and tutors (Muflih et al., 2020). Synchronous virtual lessons were reportedly well-attended, with active student participation (Nic Dhonncha & Murphy, 2021). Not only have online classes been viewed as a viable substitute for in-person teaching (Sud et al., 2020), a significant proportion of pre-clinical students have expressed a preference for online learning over traditional teaching (Khalil et al., 2020), leading to calls for online learning to be retained as a teaching modality post-pandemic. It might be worthwhile to consider the introduction of a hybrid model, comprising both online webinars and face-to-face teaching, in the medical curriculum (Hammond et al., 2020).
2) Access to learning:
With intermittent lock-down and return of international students to their native countries, online teaching platforms facilitated worldwide access to learning resources (Mukhtar et al., 2020). Medical students have also reported benefits arising from flexibility of learning in the comfort of their homes at their own pace (Cruess et al., 2014; Farooq et al., 2020), and feeling empowered to adopt an individualised approach to learning (Loh & Nalliah, 2010).
3) Time efficiency:
Online learning reduces commute time (Mukhtar et al., 2020; Shahrvini et al., 2020; Sud et al., 2020) and campus-based distractions (Sud et al., 2020). With better utility of time, students have had capacity to engage in concurrent activities like volunteering in COVID-19 relief efforts, thereby contributing to their holistic development (Shahrvini et al., 2020). There is also potential for improved academic performance due to efficient time management, better sleep patterns and reduced anxiety associated with learning within comfort zones (Khalil et al., 2020). Some students have also reported satisfaction of having more family bonding time (Sud et al., 2020).
4) Increased self-directed learning and student-led initiatives:
Sudden cessation of traditional, classroom-based teaching has presented a serendipitous opportunity for students to cultivate active learning behaviours and initiate student-led teaching to their peers (Newman & Lattouf, 2020; Roberts et al., 2020). At the Bristol Medical School, a student-led society delivered peer-led teaching sessions via video conferencing platforms (Roberts et al., 2020). These sessions not only helped mentees master content and clarify misconceptions, but also helped mentors reinforce foundational concepts. Students also leveraged on the prevailing volatility, uncertainty, complexity and ambiguity (VUCA) to learn coping skills and develop resilience and versatility, in preparation for their future careers (Ferrel & Ryan, 2020).
5) Opportunities for faculty development:
The COVID-19 pandemic has provided opportunities for universities to strengthen their current curricula by developing new relevant resources, exploring novel blended learning techniques, and developing alternative assessment methods (Longhurst et al., 2020). In a Strengths, Weaknesses, Opportunities and Threats (SWOT) analysis, 71% of British universities identified opportunities to develop new online resources, while 50% cited avenues for academic collaboration between universities (Joseph et al., 2020). Faculty members have also reported opportunities to upskill in new technologies, incorporate innovative software into current curricula and boost their confidence in navigating virtual learning platforms.
IV. DISCUSSION
The COVID-19 pandemic has caused major disruptions to medical education globally and left students feeling incompetent, unmotivated, and anxious. It has also challenged medical schools to explore novel ways of teaching and training that mitigate the risks associated with the pandemic. Insights gathered in this review could inform a strategy for the development of medical curricula in the post-pandemic era, integrating digital technology and novel pedagogy. As there is a paucity of good-quality studies, the effectiveness of virtual learning remains to be proven. However, online teaching cannot substitute for authentic clinical experiences. Modules using simulations and virtual or augmented reality may bridge the gap in procedural skills training, but the loss of inter-professional interactions could affect students’ ability to internalise the core values of medical professionalism – a fundamental component in medical education. Professionalism is traditionally taught through observation of inter-professional interactions, experiential learning, and role-modelling (Cruess et al., 2014; Loh & Nalliah, 2010). Hence, it is important that clerkship rotations are maintained with risk mitigation measures in place so that students can continue to learn and internalise the attributes of medical professionalism, mentored by their tutors.
The present review also revealed the mind shift of medical educators saddled with a protracted pandemic. Early inclination to exclude medical students from all forms of clinical work at the start of the pandemic has progressed to a collective resolve to equip them with the skills and knowledge to manage a pandemic as the future healthcare workforce (Halbert et al., 2020; Tolsgaard et al., 2020). The cautious re-introduction of clinical training has been facilitated by the availability of vaccination and regular testing. To further mitigate risks, students could be embedded in smaller care teams with close supervision. Clinical rotations could also be shortened to the minimum required to achieve competence, with provision for extension of training if students fail to attain proficiency. The opportunity to participate in the pandemic and show courage and altruism by fighting alongside other healthcare workers could go a long way to bolster their confidence and cultivate a shared sense of purpose among students (Chandratre, 2020).
Mental health issues have taken a toll on medical students, stemming from social isolation, lack of work-life balance, experience of illness and death among colleagues and families, and perceptions of inadequacy. However, there is a paucity of published studies on effective measures to address mental health issues during the COVID-19 pandemic. As a group, medical students have a higher prevalence of mental health issues (Molodynski et al., 2021; Schwenk et al., 2010), and are less likely to seek help (Molodynski et al., 2021). Thus, it is imperative to increase surveillance for this at-risk group and strengthen peer support and engagement channels. Further research should seek to delineate the range of mental health conditions faced by medical students in this pandemic, the influence of socio-cultural factors and effective strategies for surveillance and support.
Nonetheless, this systematic review has its limitations. The search was conducted using PubMed for its comprehensive coverage of indexed journal articles, including “in process” citations and links to related citations. However, this could have led to the exclusion of journals not cited by PubMed and the presentation of a more restricted view. References in non-English languages were not analysed. As we have confined our literature search to 1 February 2020 to 1 September 2020 to capture the challenges and innovations in undergraduate medical education at the height of the pandemic, we were unable to report the adaptations to medical education emerging after 1 Sep 2020.
V. CONCLUSION
The COVID-19 pandemic has provided unexpected, yet invaluable opportunities to explore new pedagogies that may be instrumental in shaping medical education in the new norm. Institutions should continue to evaluate and refine these new teaching techniques and content to ensure that the medical curriculum stays relevant and robust. As future members of the healthcare work force in the post-pandemic era, medical students should be integrated into current health systems to equip them with the knowledge, skills, and experience to manage future pandemics. This would also help forge a collective sense of purpose in these uncertain times.
Notes on Contributors
CJT performed the literature search and synthesis, wrote part of the manuscript, and prepared the figure. CC helped with the literature search and wrote part of the manuscript. FI helped in the resolution of disagreements in the literature search and constitution of the manuscript. EL helped in the planning the study, resolution of disagreements in the literature search and constitution of the manuscript.
Ethical Approval
As this study is a systematic review, ethical approval and IRB application was not required.
Data Availability
The data that support the findings of this study are openly available in Figshare repository http://doi.org/10.6084/m 9.figshare.17296856.
Funding
All authors have no funding sources to declare.
Declaration of Interest
All authors declare that they have no competing interests.
References
Ashokka, B., Ong, S. Y., Tay, K. H., Loh, N. H. W., Gee, C. F., & Samarasekera, D. D. (2020). Coordinated responses of academic medical centres to pandemics: Sustaining medical education during COVID-19. Medical Teacher, 42(7), 762-771. https://doi.org/10.1080/0142159x.2020.1757634
Atreya, A., & Acharya, J. (2020). Distant virtual medical education during COVID-19: Half a loaf of bread. The Clinical Teacher, 17(4), 418-419. https://doi.org/10.1111/tct.13185
Calhoun, K. E., Yale, L. A., Whipple, M. E., Allen, S. M., Wood, D. E., & Tatum, R. P. (2020). The impact of COVID-19 on medical student surgical education: Implementing extreme pandemic response measures in a widely distributed surgical clerkship experience. The American Journal of Surgery, 220(1), 44-47. https://doi.org/10.1016/j.amjsurg.2020.04.024
Chandratre, S. (2020). Medical students and COVID-19: Challenges and supportive strategies. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520935059
Chao, T. N., Frost, A. S., Brody, R. M., Byrnes, Y. M., Cannady, S. B., Luu, N. N., Rajasekaran, K., Shanti, R. M., Silberthau, K. R., Triantafillou, V., & Newman, J. G. (2021). Creation of an interactive virtual surgical rotation for undergraduate medical education during the COVID-19 pandemic. Journal of Surgical Education, 78(1), 346-350. https://doi.org/10.1016/j.jsurg.2020.06.039
Choi, B., Jegatheeswaran, L., Minocha, A., Alhilani, M., Nakhoul, M., & Mutengesa, E. (2020). The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: A national survey. BMC Medical Education, 20(1), 206. https://doi.org/10.1186/s12909-020-02117-1
Co, M., & Chu, K. M. (2020). Distant surgical teaching during COVID-19 – A pilot study on final year medical students. Surgical Practice, 24(3), 105– 109. https://doi.org/10.1111/1744-1633.12436
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2014). Reframing medical education to support professional identity formation. Academic Medicine, 89(11), 1446-1451. https://doi.org/10.1097/acm.0000000000000427
Darras, K. E., Spouge, R. J., de Bruin, A. B. H., Sedlic, A., Hague, C., & Forster, B. B. (2021). Undergraduate radiology education during the COVID-19 pandemic: A review of teaching and learning strategies. Canadian Association of Radiologists Journal, 72(2), 194-200. https://doi.org/10.1177/0846537120944821
Farooq, F., Rathore, F. A., & Mansoor, S. N. (2020). Challenges of online medical education in Pakistan during COVID-19 pandemic. Journal of the College of Physicians and Surgeons Pakistan, 30(6), 67–69. https://doi.org/10.29271/jcpsp.2020.Supp1.S67
Ferrel, M. N., & Ryan, J. J. (2020). The impact of COVID-19 on medical education. Cureus, 12(3), e7492. https://doi.org/10.7759/cureus.7492
Go, B., & Rajasekaran, K. (2020). Effect of COVID-19 in selecting otolaryngology as a specialty. Head & Neck, 42(7), 1409-1410. https://doi.org/10.1002/hed.26251
Halbert, J. A., Jones, A., & Ramsey, L. P. (2020). Clinical placements for medical students in the time of COVID-19. Medical Journal of Australia, 213(2), 69-69. e61. https://doi.org/10.5694/mja2.50686
Hammond, D., Louca, C., Leeves, L., & Rampes, S. (2020). Undergraduate medical education and Covid-19: Engaged but abstract. Medical Education Online, 25(1), 1781379. https://doi.org/10.1080/10872981.2020.1781379
Hilburg, R., Patel, N., Ambruso, S., Biewald, M. A., & Farouk, S. S. (2020). Medical Education During the Coronavirus Disease-2019 Pandemic: Learning From a Distance. Advances in Chronic Kidney Disease, 27(5), 412-417. https://doi.org/10.1053/j.ackd.2020.05.017
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., Zhang, L., Fan, G., Xu, J., Gu, X., Cheng, Z., Yu, T., Xia, J., Wei, Y., Wu, W., Xie, X., Yin, W., Li, H., Liu, M., . . . Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet, 395(10223), 497-506. https://doi.org/10.1016/S0140-6736(20)30183-5
Iancu, A. M., Kemp, M. T., & Alam, H. B. (2020). Unmuting medical students’ education: Utilizing telemedicine during the COVID-19 pandemic and beyond. Journal of Medical Internet Research, 22(7), e19667. https://doi.org/10.2196/19667
Iqbal, M. Z., Alradhi, H. I., Alhumaidi, A. A., Alshaikh, K. H., AlObaid, A. M., Alhashim, M. T., & AlSheikh, M. H. (2020). Telegram as a tool to supplement online medical education during COVID-19 crisis. Acta Informatica Medica, 28(2), 94-97. https://doi.org/10.5455/aim.2020.28.94-97
Joseph, J. P., Joseph, A. O., Conn, G., Ahsan, E., Jackson, R., & Kinnear, J. (2020). COVID-19 pandemic-medical education adaptations: The power of students, staff and technology. Medical Science Educator, 30(4), 1355-1356. https://doi.org/10.1007/s40670-020-01038-4
Khalil, R., Mansour, A. E., Fadda, W. A., Almisnid, K., Aldamegh, M., Al-Nafeesah, A., Alkhalifah, A., & Al-Wutayd, O. (2020). The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: A qualitative study exploring medical students’ perspectives. BMC Medical Education, 20(1), 285. https://doi.org/10.1186/s12909-020-02208-z
Loh, K. Y., & Nalliah, S. (2010). Learning professionalism by role-modelling. Medical Education, 44(11), 1123. https://doi.org/10.1111/j.1365-2923.2010.03827.x
Longhurst, G. J., Stone, D. M., Dulohery, K., Scully, D., Campbell, T., & Smith, C. F. (2020). Strength, Weakness, Opportunity, Threat (SWOT) Analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the Covid-19 pandemic. Anatomical Sciences Education, 13(3), 301-311. https://doi.org/10.1002/ase.1967
Maini, A., Saravanan, Y., Singh, T. A., & Fyfe, M. (2020). Coaching skills for medical education in a VUCA world. Medical Teacher, 42(11), 1308-1309. https://doi.org/10.1080/0142159x.2020.1788713
Molodynski, A., Lewis, T., Kadhum, M., Farrell, S. M., Lemtiri Chelieh, M., Falcão De Almeida, T., Masri, R., Kar, A., Volpe, U., Moir, F., Torales, J., Castaldelli-Maia, J. M., Chau, S. W. H., Wilkes, C., & Bhugra, D. (2021). Cultural variations in wellbeing, burnout and substance use amongst medical students in twelve countries. International Review of Psychiatry, 33(1-2), 37-42. https://doi.org/10.1080/09540261.2020.1738064
Muflih, S., Abuhammad, S., Karasneh, R., Al-Azzam, S., Alzoubi, K. H., & Muflih, M. (2020). Online education for undergraduate health professional education during the COVID-19 pandemic: Attitudes, barriers, and ethical issues. Research Square. https://doi.org/10.21203/rs.3.rs-42336/v1
Mukhtar, K., Javed, K., Arooj, M., & Sethi, A. (2020). Advantages, limitations and recommendations for online learning during COVID-19 pandemic era. Pakistan Journal of Medical Sciences, 36(Covid19-s4), S27-S31. https://doi.org/10.12669/pjms.36.COVID19-S4.2785
Murphy, B. (2020). COVID-19: How the virus is impacting medical schools. Retrieved 18 Dec, 2020, from https://www.ama-assn.org/delivering-care/public-health/covid-19-how-virus-impacting-medical-schools
Naidoo, N., Akhras, A., & Banerjee, Y. (2020). Confronting the challenges of anatomy education in a competency-based medical curriculum during normal and unprecedented times (COVID-19 Pandemic): Pedagogical framework development and implementation. JMIR Medical Education, 6(2), e21701. https://doi.org/10.2196/21701
Newman, N. A., & Lattouf, O. M. (2020). Coalition for medical education—A call to action: A proposition to adapt clinical medical education to meet the needs of students and other healthcare learners during COVID-19. Journal of Cardiac Surgery, 35(6), 1174-1175. https://doi.org/10.1111/jocs.14590
Nic Dhonncha, E., & Murphy, M. (2021). Learning new ways of teaching and assessment: the impact of COVID-19 on undergraduate dermatology education. Clinical and Experimental Dermatology, 46(1), 170-171. https://doi.org/10.1111/ced.14364
Oki, O., Shah, S., Scrivens, L., & Guckian, J. (2021). COVID-19: Challenges and solutions for the future of UK dermatology undergraduate curriculum delivery. Clinical and Experimental Dermatology, 46(1), 171-173. https://doi.org/10.1111/ced.14386
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., . . . Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
Rafi, A. M., Varghese, P. R., & Kuttichira, P. (2020). The pedagogical shift during COVID 19 pandemic: Online medical education, barriers and perceptions in Central Kerala. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520951795
Rallis, K. S., & Allen-Tejerina, A. M. (2020). Tele-oncology in the COVID-19 era: Are medical students left behind? Trends Cancer, 6(10), 811-812. https://doi.org/10.1016/j.trecan.2020.08.001
Remtulla, R. (2020). The present and future applications of technology in adapting medical education amidst the COVID-19 pandemic. JMIR Medical Education, 6(2), e20190. https://doi.org/10.2196/20190
Roberts, V., Malone, K., Moore, P., Russell-Webster, T., & Caulfield, R. (2020). Peer teaching medical students during a pandemic. Medical Education Online, 25(1), 1772014. https://doi.org/10.1080/10872981.2020.1772014
Roskvist, R., Eggleton, K., & Goodyear-Smith, F. (2020). Provision of e-learning programmes to replace undergraduate medical students’ clinical general practice attachments during COVID-19 stand-down. Education for Primary Care, 31(4), 247-254. https://doi.org/10.1080/14739879.2020.1772123
Sam, A. H., Millar, K. R., & Lupton, M. G. F. (2020). Digital clinical placement for medical students in response to COVID-19. Academic Medicine, 95(8), 1126. https://doi.org/10.1097/acm.0000000000003431
Sandhaus, Y., Kushnir, T., & Ashkenazi, S. (2020). Electronic distance learning of pre-clinical studies during the COVID-19 pandemic: A preliminary study of medical student responses and potential future impact. The Israel Medical Association Journal, 22(8), 489-493.
Schaffir, J., Strafford, K., Worly, B., & Traugott, A. (2020). Challenges to medical education on surgical services during the COVID-19 pandemic. Medical Science Educator, 30(4), 1667–1671. https://doi.org/10.1007/s40670-020-01072-2
Schwenk, T. L., Davis, L., & Wimsatt, L. A. (2010). Depression, stigma, and suicidal ideation in medical students. JAMA, 304(11), 1181-1190. https://doi.org/10.1001/jama.2010.1300
Shahrvini, B., Baxter, S. L., Coffey, C. S., MacDonald, B. V., & Lander, L. (2020). Pre-clinical remote undergraduate medical education during the COVID-19 pandemic: A survey study. Research Square. https://doi.org/10.21203/rs.3.rs-33870/v1
Shehata, M. H., Abouzeid, E., Wasfy, N. F., Abdelaziz, A., Wells, R. L., & Ahmed, S. A. (2020). Medical education adaptations post COVID-19: An Egyptian reflection. Journal of Medical Education and Curricular Development, 7. https://doi.org/10.1177/2382120520951819
Singh, K., Srivastav, S., Bhardwaj, A., Dixit, A., & Misra, S. (2020). Medical education during the COVID-19 pandemic: A single institution experience. Indian Pediatrics, 57(7), 678-679. https://doi.org/10.1007/s13312-020-1899-2
Sud, R., Sharma, P., Budhwar, V., & Khanduja, S. (2020). Undergraduate ophthalmology teaching in COVID-19 times: Students’ perspective and feedback. Indian Journal of Ophthalmologyy, 68(7), 1490-1491. https://doi.org/10.4103/ijo.IJO_1689_20
Tan, J. W. C., Cai, C., Ithnin, F., & Lew, E. (2021). Challenges and innovations in undergraduate medical education during the COVID-19 pandemic – A systematic review [Data set]. Figshare. http://doi.org/10.6084/m9.figshare.17296856
Theoret, C., & Ming, X. (2020). Our education, our concerns: The impact on medical student education of COVID-19. Medical Education, 54(7), 591-592. https://doi.org/10.1111/medu.14181
Tokuç, B., & Varol, G. (2020). Medical education in Turkey in time of COVID-19. Balkan Medical Journal, 37(4), 180-181. https://doi.org/10.4274/balkanmedj.galenos.2020.2020.4.003
Tolsgaard, M. G., Cleland, J., Wilkinson, T., & Ellaway, R. H. (2020). How we make choices and sacrifices in medical education during the COVID-19 pandemic. Medical Teacher, 42(7), 741-743. https://doi.org/10.1080/0142159x.2020.1767769
Torales, J., O’Higgins, M., Castaldelli-Maia, J. M., & Ventriglio, A. (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry, 66(4), 317-320. https://doi.org/10.1177/0020764020915212
*Eileen Lew
KK Women’s and Children’s Hospital,
100 Bukit Timah Road
Singapore 229899
Telephone: +65 6394 2422
Email: eileen.lew@singhealth.com.sg
Submitted: 17 September 2021
Accepted: 4 October 2021
Published online: 5 April, TAPS 2022, 7(2), 61-62
https://doi.org/10.29060/TAPS.2022-7-2/LE2691
Gabriela González & Mildred Lopez
Tecnologico de Monterrey, Escuela de Medicina y Ciencias de la Salud, Mexico
Although there have been many calls for dental education to move to comprehensive training, many have remained in rhetoric. However, recently the strategic analysis of the American Dental Association of Education recommended a curriculum transformation to engage students in life-long learning and nurturing an educational community with well-qualified teachers to mentor students and model the values of the profession (Formicola et al., 2018).
Reimagining dental education demands a curriculum that considers the unique characteristics of learners. The generation to come has grown in a globalised world where information about what is happening in remote geographical places is quickly available, which has shaped their cultural and political points of view. Their idealism and advocacy have marked how they relate to patients. As part of the inherent characteristics, students thrive in experiential learning and rely on the internet and multimedia content. Therefore, incorporating technology is a must for engaging them in meaningful learning activities.
Instead of theory-oriented education, institutions should foster learning environments that depict the immediate community’s health challenges, for example, childhood caries, poor access to dental care, and the increase in the number of people with untreated oral conditions. A starting point is to transition to context-rich educational experiences where students can make a positive social impact. While doing so, they honour their social commitment to patients and families and transform into health advocates.
Additionally, this comprehensive approach needs to nurture a professional that can work within a health system. Dentists that are successful in practice are immersed in a community and have an interdisciplinary approach to deliver quality care. To achieve this competence undergraduates, need more opportunities to develop critical thinking skills, engage in self-assessment of performance, provide, and receive feedback to spark growth, and practice evidence-based decision-making (Kornegay et al., 2021).
Considering the evolution of technologies and the emergence of diseases, it is impossible to think that dental training has not changed. However, the unique profile of the new generation of students demands that we accelerate the change process. Learners have raised to the challenge and have demonstrated their will to positively impact their communities and society. The call for action for educational institutions is to embrace a new vision for a wide comprehensive dental education model where students learn from dental sciences and medicine to advocacy and ethics.
Notes on Contributors
Gabriela Gonzalez prepared first draft; literature review; writing and Mildred Lopez revised the final version of the manuscript. ML wrote and revised the final version of the manuscript.
Funding
There is no funding for this study.
Declaration of Interest
Authors declare no conflict of interest.
References
Formicola, A. J., Bailit, H. L., Weintraub, J. A., Fried, J. L., & Polverini, P. J. (2018). Advancing dental education in the 21st century: Phase 2 report on strategic analysis and recommendations. Journal of Dental Education, 82(10), eS1–eS32. https://doi.org/10.21815/JDE.018.109
Kornegay, E. C., Jackson, T. H., LaGarry‐Cahoon, A., Reside, J. M., Wolcott, M. D., & Quinonez, R. B. (2021). “I don’t think the problem’s the student… I think it’s us”: Engaging faculty in curriculum innovation. Journal of Dental Education, 85(4), 582-588. https://doi.org/10.1002/jdd.12495
*Gabriela González
Tecnologico de Monterrey,
Escuela de Medicina y Ciencias de la Salud
Av. Morones Prieto 3000 Pte
64710 Monterrey, N.L. México
Tel: 52/81 8888 2254
Email: dra.gabrielaglzl@gmail.com
Submitted: 23 August 2021
Accepted: 28 October 2021
Published online: 5 April, TAPS 2022, 7(2), 56-60
https://doi.org/10.29060/TAPS.2022-7-2/SC2686
Mae Yue Tan, Nicholas Beng Hui Ng, Marion Margaret Aw & Jeremy Bingyuan Lin
Khoo Teck Puat -National University Children’s Medical Institute, National University Health System, Singapore
Abstract
Introduction: The transition from medical student to houseman is well recognised as a stressful period for newly qualified doctors. This stress is likely to be heightened when the transition occurs during a pandemic. We aimed to evaluate the perceived stress levels of housemen as they begin housemanship and explore their sentiments and preparedness in starting work amidst the coronavirus disease 2019 (COVID-19) pandemic.
Methods: Housemen starting work at a tertiary institution in Singapore in May 2020 completed the following: (1) Perceived Stress Scale, (2) open-ended questions on perceived challenges and concerns and (3) questionnaire on preparedness and confidence in starting work. Descriptive statistics were used to analyse quantitative data and modified thematic analysis performed for qualitative data.
Results: Sixty-one housemen participated. Thirty-five (57.4%) reported high perceived stress. The themes for perceived challenges in this transition included coping with constant change, lack of reliable information from authorities, dealing with disappointment, physical fatigue, and loss of autonomy. The themes for concerns in beginning housemanship elicited relate to clinical competence, transitioning into new responsibilities, risk of infection with COVID-19, senior expectations, physical fatigue and training-related concerns. Despite these challenges and concerns, housemen were prepared to begin work during this pandemic.
Conclusion: Housemen transitioning during this pandemic experienced additional stressors and unique challenges pertaining to working in a pandemic. Encouragingly, they remain prepared to start work. Institutions and departments should be mindful of the specific concerns and challenges so that appropriate support can be put in place to support these junior doctors.
Keywords: COVID-19, Junior Doctor, Intern, Pandemic, Challenges, Preparedness
I. INTRODUCTION
Newly graduated doctors are a particularly vulnerable group of healthcare workers as they start work as housemen amidst the COVID-19 pandemic. The transition from student to doctor is already notorious for steep learning curves and increased stress (Sturman et al., 2017). Moreover, housemen in Singapore experienced drastic changes during their final year of medical school, a time which coincided with the surge of the pandemic in Singapore. Not only was clinical training was disrupted, this batch also experienced a modified form of final examinations, an earlier start to housemanship, and changes to posting selections, as manpower allocation was done centrally based on manpower demands. With that, we aimed to evaluate the perceived stress among housemen and explore their perceived challenges, concerns and preparedness just before they started work.
II. METHODS
We performed a cross-sectional anonymous survey on housemen at our institution on their first day of housemanship, in May 2020. The survey was administered before the hospital orientation by an independent institutional representative not part of the investigating team. Consent was implied through voluntary participation.
The Perceived Stress Scale (PSS) (Cohen et al., 1983) was used as a measure of stress. This tool is designed to assess how unpredictable, uncontrollable, and overloaded respondents find their lives. We also administered structured open-ended questions to elicit perceived challenges and major concerns while transitioning from medical school to starting work as a houseman. Participants also completed 7-point Likert rating scale modelled after an existing military instrument (Zagelbaum et al., 2014) to evaluate perceived preparedness and confidence in starting work.
Quantitative data was analysed using IBM SPSS (Version 23.0), with descriptive analysis. The qualitative data was analysed using modified thematic analysis, with NVivo software. All transcripts were coded independently by three authors. The coding method involved an inductive (ground up) method, looking at generating the unit of meanings, categorising the data and developing themes until data saturation was achieved. The kappa coefficient score for the qualitative data analysis was 0.87, indicating good agreement.
III. RESULTS
Sixty-one housemen participated (response rate 100%). A significant proportion (57.4%) rated high stress on the PSS.
Key themes of perceived challenges reported by the housemen transitioning from medical school to the workforce during the COVID-19 pandemic included: (1) coping with constant change, (2) lack of timely reliable information, (3) dealing with disappointment, (4) physical fatigue, (5) loss of autonomy (Fig 1). Examples of last-minute changes to examinations, work commencement and posting-related information were quoted as a major cause for significant uncertainties. Additionally, some had quoted the lack of timely nor reliable dissemination of the information, coming from third-party sources rather than relevant authorities. The shortened break between end of examinations and housemanship meant that typical traditions of personal and post-graduation plans, had to be cancelled, resulting in disappointment and reduced rest. Many also felt that the central distribution of manpower with increased rotations to pandemic heavy departments meant a loss of autonomy in selecting a posting or institution of choice.
The themes for perceived concerns about starting work during the pandemic included (1) clinical competence as a junior doctor, (2) transitioning into new responsibilities, (3) risk of infection, (4) failing to meet expectations of seniors, (5) physical fatigue and (6) training-related concerns. The lack of competence in patient management, “call” duties, and managing emergencies were a huge concern. This extended from concerns of manpower constraints and reduced supervision during pandemic times. Navigating the new job as a doctor with new responsibilities were also raised, with concerns on the long hours and overnight “calls” leading to burnout. There were also examples given on failing to meet the expectations of senior colleagues. Pandemic-specific concerns included the risk of contracting and transmitting COVID-19 to loved ones. Many had also expressed apprehension about the possible impact that the pandemic may have on their clinical training and career progression.
In terms of preparedness to start work amidst a pandemic, 82.0% (n = 50) housemen shared that they were mentally prepared to start work. Majority (86.8%) felt that their medical school had prepared them adequately to be a junior doctor. Three-quarters (75.4%) agreed that their medical school has prepared them adequately to deal with the pandemic and its related clinical demands. Majority (83.6%) felt confident in their clinical competency to effectively work as a junior doctor, and 77.0% felt confident in their clinical competency in dealing with the pandemic as a junior doctor. Interestingly, when asked about their confidence in managing stress, 80.3% reported being confident of dealing with stressors faced by a junior doctor while 77.0% felt confident in managing pandemic-related stress.

Figure 1. Perceived challenges in the transition period, and perceived concerns of new housemen just before starting their housemanship. The size of the boxes corresponds to the frequencies of the themes with examples of verbatim responses transcribed.
IV. DISCUSSION
Our results show that a significant proportion of housemen starting work in the current pandemic have high perceived stress; this appeared to be higher than what is reported in literature for medical students and house officers in non-pandemic settings (Drachev et al., 2020), and higher than healthcare workers during this pandemic (Chen et al., 2020). As such, we believe that this is a significant finding warranting attention.
The challenges of transitioning from medical school to housemanship is well established: not only do housemen have to cope with the responsibility of being a full-fledged doctor, there is also increased physical fatigue and professional expectations that need to be met. Some of these challenges specific to transitioning have also been raised by our housemen.
The sentiments of housemen transitioning during a pandemic are not unique to this group alone: dealing with frequent and constant change and the lack of reliable and timely information are challenges that have also been reported among other healthcare workers. However, there were specific points unique to this group of junior doctors we had studied, particularly the perceived insecurity over their qualifications due to disrupted student clinical training and modified final examinations. This we feel is an important point that medical schools should be aware of; in the event of disruptions or sudden changes to the process of assessment or accreditation, it is important that these be conveyed clearly to the student body, with appropriate engagement, opportunities for clarification and reassurance on any insecurities which they may result from these changes.
Significant pandemic-specific concerns included fears of contracting the COVID-19 infection and transmitting this to others. This fear is not uncommon among healthcare workers and has been reported in recent literature. There was also the additional concern of postgraduate training disruption, which was not unexpected given the disruptions to teaching, deployment to pandemic areas and the lack of choices in the selection of their postings.
We were encouraged to find that despite the higher perceived stress, reported challenges and concerns shared, the majority had felt that their medical schools had prepared them adequately to be a junior doctor, and to deal with pandemic related demands. Additionally, despite the concerns about starting work earlier, majority still reported being ready to start work and felt confident to work effectively – their response to readiness meant that they were not shying away from the call of duty during this pandemic.
Our study is not without limitations. Open-ended questions instead of interviews that were done in line with social distancing restrictions limited the depth of the qualitative data. That said, the 100% response rate provided us which rich data that could be analysed. Additionally, the use the modified questionnaire on preparedness not only lacked external validation; we are also aware that self-reported preparedness may not correlate with actual readiness.
We believe that the key sentiments we have reported on housemen starting work in a pandemic are likely to be universal and not unique to our institution alone. These data would be informative for institutions to provide targeted support for new housemen amidst the pandemic. These include:
- Providing clear and effective information transfer particularly on rapidly changing protocols.
- Emphasis on training on personal protection and infection prevention throughout their postings.
- If manpower resources permit, institutions may consider first deploying housemen to non-pandemic services with initial job-shadowing before sending them to pandemic areas.
- Close clinical supervision from immediate seniors.
- Specific teaching program catering to the learning needs of housemen during the pandemic.
- Enforcing strict work-rest cycles to ensure adequate rest.
- Dedicated mentors for housemen to share concerns and grievances. These mentors have the responsibility of identifying housemen who are struggling such that early support can be rendered.
- Appropriate resources for housemen who require additional support.
V. CONCLUSION
Newly qualified doctors beginning their housemanship during the COVID-19 pandemic have high perceived stress with specific pandemic-related concerns and challenges on top of the usual stressors in transitioning. That said, there is encouraging data on housemen preparedness in starting work during this time. Institutions should ensure that support systems are in place to support junior doctors in these likely protracted extraordinary times. A successful transition from medical school to workplace is the cornerstone that allows these junior doctors to integrate effectively to contribute to the workforce in the pandemic, and the long journey beyond.
Notes on Contributors
Mae Yue Tan contributed to analysis and interpretation of data, drafting and critical revising of the article.
Nicholas BH Ng contributed to analysis and interpretation of data, drafting and critical revising of the article.
Marion M Aw contributed to interpretation of data, drafting and critical revising of the article.
Jeremy BY Lin contributed to conception and design, interpretation of data, drafting and critical revising of the article.
All authors gave final approval of the version to be published.
Ethical Approval
Ethics approval was obtained from from the NHG Domain Specific Review Board (DSRB), with NHG DSRB reference number of 2020/00392.
Data Availability
The data for this study can be found at https://doi.org/10.6084/m9.figshare.16399107 and https://doi.org/10.6084/m9.figshare.16399419. The access to these datasets are available for use subject to approval of the authors of this article.
Acknowledgement
The authors would like to thank the housemen who participated in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Interest
All authors have no conflict of interest to declare.
References
Chen, B., Li, Q. X., Zhang, H., Zhu, J. Y., Yang, X., Wu, Y. H., Xiong, J., Li, F., Wang, H., & Chen, Z. T. (2020). The psychological impact of COVID-19 outbreak on medical staff and the general public. Current Psychology, 1–9. https://doi.org/10.1007/s12144-020-01109-0
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behaviour, 24(4), 385-396.
Drachev, S. N., Stangvaltaite-Mouhat, L., Bolstad, N. L., Johnsen, J. K., Yushmanova, T. N., & Trovik, T. A. (2020). Perceived stress and associated factors in Russian medical and dental students: A cross-sectional study in North-West Russia. International Journal of Environmental Research and Public Health, 17(15), 5390. https://doi.org/10.3390/ijerph17155390
Sturman, N., Tan, Z., & Turner, J. (2017). “A steep learning curve”: Junior doctor perspectives on the transition from medical student to the health-care workplace. BMC Medical Education, 17(1), Article 92. https://doi.org/10.1186/s12909-017-0931-2
Zagelbaum, N. K., Heslin, K. C., Stein, J. A., Ruzek, J., Smith, R. E., Nyugen, T., & Dobalian, A. (2014). Factors influencing readiness to deploy in disaster response: Findings from a cross-sectional survey of the department of veterans affairs disaster emergency medical personnel system. BMC Emergency Medicine, 14, Article 16. https://doi.org/10.1186/1471-227X-14-16
*Tan Mae Yue
1E Kent Ridge Road,
NUHS Tower Block Level 12,
Singapore 119228
Tel: +65 6772 5555
Email: mae_yue_tan@nuhs.edu.sg
Submitted: 11 November 2021
Accepted: 27 January 2022
Published online: 5 April, TAPS 2022, 7(2), 51-55
https://doi.org/10.29060/TAPS.2022-7-2/SC2710
Rintaro Imafuku, Kaho Hayakawa & Takuya Saiki
Medical Education Development Center, Gifu University, Japan
Abstract
Introduction: Personal statements are important documents in the admission and programme application processes, including international elective programmes, in medical education. However, writing these is challenging for international applicants not only because of their unfamiliarity with this genre but also their English academic writing skills. This study aims to explore the organisation and elaboration of text in personal statements written by Japanese medical students for international elective programme application.
Methods: Drawing on genre analysis, the first draft of personal statements written by eight fifth-year medical students at a Japanese university were analysed. The text data were deductively classified into moves and steps, using Chiu’s framework of the personal statement genre.
Results: In the introduction, Japanese medical students commonly described the context and issues of healthcare in Japan and the future goals for physicians. In the move of the relevant background, it was notable that six out of eight personal statements showed personality. Although a range of moves was covered when writing about the reasons for applying, only two students described their understanding of programmes and institutional attributes. In the move of conclusion, they focused more on writing their goals of future success and contribution to the course. Furthermore, no applicant expressed self-promotion and praise for academics, programmes, and institutions.
Conclusion: The findings of this study can provide a springboard for the development of support for Japanese students’ academic writing in English in medical education across cultures.
Keywords: Medical Education, International Electives, Personal Statement, Genre Analysis, Discourse, Rhetorical Patterns, Written Communication
I. INTRODUCTION
The personal statement, as a promotional academic genre, is an important document in the admission process for higher education. However, numerous applicants face difficulties while preparing application materials because of their unfamiliarity with the genre of discourse and audience expectations (Ding, 2007). In medical education, particularly institutions in Western countries, several instances require the submission of personal statements for application to, for instance, medical schools, international electives, residency programmes, and research programmes.
Globalisation in medical education has promoted worldwide student mobility. Currently, many Asian medical students, including Japanese students, participate in international electives in Western countries. International electives provide several benefits to medical students, including cultural competence, communication skills, and clinical reasoning (Imafuku et al., 2021). However, because some institutions require the submission of personal statements for application to the international elective programme, it can be challenging for international applicants not only because of their unfamiliarity with the genre of discourse but also their English academic writing skills.
As the preparation of application materials, including personal statements, can be challenging for Asian medical students, educators must facilitate a more comprehensive pre-departure course, along with providing support for composing such documents. Specifically, a better understanding of the linguistic features of their personal statements is fundamental for developing academic writing support for their application documents. Therefore, this study used the genre analysis framework (Swales, 1990) to explore the organisation and elaboration of text in personal statements written by Japanese medical students for the international elective programme application. Specifically, the following research question was developed: What are the rhetorical characteristics of Japanese medical students’ personal statements written in English?
II. METHODS
A. Setting
International electives, which allow the students at the Gifu University School of Medicine to study overseas, are optional modules of either four or eight weeks in the final year of the clinical clerkship programme with the goals of observation, understanding and experiencing clinical practices in different cultural contexts. Through this programme, every year, 10–15 medical students study clinical medicine in a foreign country and gain cross-cultural experience in a clinical setting. As some highly competitive overseas institutions require the submission of personal statements, letters of recommendation, and curriculum vitae during the application, faculty members of the medical education division provide some support for their preparation, if required by the students. Although the guidebook for international electives briefly explains the definition and role of personal statements, the students are not officially given any sample or format of English personal statements.
B. Data Collection and Analysis
This study collected personal statements written in English by fifth-year medical students (n=8; Student A-H) at a Japanese university, from 2013 to 2017, as part of the application documents for international electives in institutions in the United Kingdom (UK) or the United States (US). Their TOEFL (Test of English as a Foreign Language) (iBT) score ranges from 90 to 101. Written informed consent to participate was obtained from them. Their first drafts were analysed through the lens of move analysis as an element of genre analysis (Swales, 1990) to reveal rhetorical patterns from a cultural perspective. The first draft, which has not been revised using feedback from others, directly reflects their cultural and linguistical influences regarding the rhetorical patterns. Text data were analysed by the first author, who has a background in applied linguistics and medical education. Subsequently, the preliminary findings of the text analysis were discussed by all the research team members to establish the credibility and dependability of the data analysis.
Genre analysis aims to describe the organisational patterns of text in a specific context, and genres are viewed as staged goal-oriented social processes of the written or spoken practice. For example, in written communication, reader expectations, document structure, and rhetoric development vary depending on the genre, such as research articles, invitation letters, and reminder emails. A move is an analytical unit defined as a rhetorical component shifting from one part of a text to another that performs a specific communicative function (Swales, 1990, p.140). Each move is subcategorised into one or more functional units called steps.
Specifically, this study applied Chiu’s (2016) framework of moves and steps in the context of personal statements for graduate school application to medical education. Drawing on this analytical framework that comprises five moves: introduction, relevant background, reasons for applying, extra-curricular information, and conclusion, the text data were deductively classified into moves and steps.
Ethical approval was obtained from the Gifu University Ethics Committee (No. 25–367). Students were assured of the confidentiality of the contents.
III. RESULTS
The average length of the personal statements was 535.5 words (range: 314–873 words). The deidentified data of personal statements by some participants who gave their consent to share the whole text that support the findings of this study are available in Figshare at http://doi.org/10.6084/m9.figshare.17030705. All the data set can be available from the corresponding author on reasonable request. Table 1 indicates the total number of personal statements that consists of any step of each move and shows the representative text in each move.
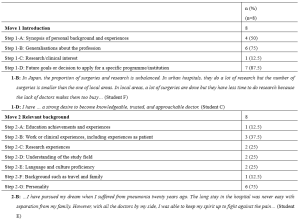

Table 1. Moves and steps of the personal statements for international electives written in English by Japanese medical students
As can be seen from Table 1, in the introduction, Japanese medical students commonly described the context and issues of healthcare in Japan (1-B) and future goals for physicians (1-D). Expressions of their research and clinical interests (1-C) were made the least in the introduction move. In the relevant background move, it is notable that six out of eight personal statements in this study showed personality (2-G), which is much higher than the rest of the other steps. In the reasons for applying move, six Japanese medical students made the rhetorical step of personal development and ambition, whereas only two students described their understanding of programmes and institutional attributes (3-C) and disciplinary and research reasons (3-E). Extra-curricular information (Move 4) was not provided by the applicants in this study. In the move of conclusion, Japanese medical students focused only on their future success goals (5-A) and contribution to the course (5-E). Furthermore, no applicant expressed self-promotion (5-B) and praise for academics, programmes, and institutions (5-D) in this study.
IV. DISCUSSION
Drawing on genre analysis (Swales, 1990), this study revealed the rhetorical patterns of personal statements written by Japanese medical students. Although the participants had high or adequate English proficiency, they seemed to struggle with personal statement writing due to the unfamiliar genre of discourse. Imafuku et al. (2021) found that the participants faced several difficulties related to linguistic, sociolinguistic, and sociocultural aspects during the international electives, whereas this study showed that the applicants had already experienced difficulties of cross-cultural communication at the pre-departure stage.
Genre analysis offers a useful theoretical framework and an analytical perspective of people’s communicative practices in a cultural context, especially allowing educators or researchers to examine how language is used in specific contexts for particular purposes, thus contributing to the knowledge of specific writing instructions (Ding, 2007). Writing a personal statement is a common issue not only in medical education but also in higher education. Personal statements are a type of promotional academic genre in admissions to higher education institutions or programmes that expects textual self-aggrandisement by applicants. Chiu (2016), who examined personal statements in the areas of educational policy, language and literacy, and higher education, demonstrated that self-promotion or evaluation is an important step in the conclusion move for graduate school applications in the UK and the US. As a response to Chiu’s (2016) study, the finding of this study that self-promotion or evaluation is not indicated in the move of conclusion by Japanese medical students suggests their need to learn not only the rhetorical structure and reader expectations but also ways of logically and effectively expressing their own strengths. The results of this study can be a useful learning resource to understand what rhetorically characterises a personal statement.
Reflecting on the rhetorical patterns of the students in a given genre is pivotal to communicative achievement in intercultural settings. In this sense, contrastive rhetoric studies have provided useful implications for a better understanding of writing patterns from a cross-cultural viewpoint. For example, contrastive rhetoric studies of Japanese and English to date have shown different discourse organisations of and approaches to writing in a variety of genres, such as newspaper columns, doctoral dissertations, and narrative essays (Connor, 1996). In the previous studies reviewed by Connor (1996), Japanese writing was characterised by a reader-responsible language and a deductive rhetorical pattern. Furthermore, the Japanese are oriented to share values of indirectness, and the reader is expected to interpret what the writer intended to convey. This study suggests that understanding the rhetorical features in the writer’s own cultural context is essential to writing in the target genre of discourse in different cultural contexts.
Although this study illuminates written communication across cultures through the text analysis of personal statements, investigation should be undertaken continuously for further data collection, as the sample size of text data from eight students is limited to a particular institution. Furthermore, follow-up interviews are worthwhile to explore students’ writer identity and cognitive process during writing.
V. CONCLUSION
There are increased opportunities for cross-cultural communication, including both spoken and written formats, in globalised contexts, such as medicine. For written communication, in the genre of personal statements in medical education, this study found that Japanese students shared limited information about the relevant background (Move 2) and did not express adequate self-promotion (Move 5). The findings can act as a springboard for the development of support for Japanese students’ academic writing in English in medical education across cultures.
Notes on Contributors
Rintaro Imafuku reviewed the literature, designed the study, conducted text analysis, and wrote the manuscript.
Kaho Hayakawa was involved in data collection and analysis of the text.
Takuya Saiki was involved in data collection and analysis of the text.
All the authors have read and approved the final manuscript.
Ethical Approval
This study was approved by the Gifu University Ethics Committees (No. 25–367). Consent was obtained from all participants for the research study. Confidentiality was assured for the contents of students’ writing. All participants have given written consent for their data to be used in the research and for publication.
Data Availability
Deidentified data of personal statements by the participants who gave their consent to share the whole text are openly available at http://doi.org/10.6084 /m9.figshare.17030705. The data are available from the corresponding author on reasonable request.
Funding
This work was supported by the JSPS KAKENHI [Grant number 20K10374].
Declaration of Interest
The authors report no conflicts of interest.
References
Chiu, Y.-L. T. (2016). ‘Singing your tune’: Genre structure and writer identity in personal statements for doctoral applications. Journal of English for Academic Purposes, 21, 48-59. https://doi.org/10.1016/j.jeap.2015.11.001
Connor, U. (1996). Contrastive rhetoric: Cross-cultural aspects of second language writing. Cambridge University Press.
Ding, H. (2007). Genre analysis of personal statements: Analysis of moves in application essays to medical and dental schools. English for Specific Purposes, 26(3), 368-392. https://doi.org/10.1016/j.esp.2006.09.004
Imafuku, R., Saiki, T., Hayakawa, K., Sakashita, K., & Suzuki, Y. (2021). Rewarding journeys: Exploring medical students’ learning experiences in international electives. Medical Education Online, 26(1), 1913784. https://doi.org/10.1080/10872981.2021.1913784
Swales, J. (1990). Genre analysis: English in academic and research settings. Cambridge University Press.
*Rintaro Imafuku
1-1 Yanagido, Gifu, Gifu, 501-1194
Email: rimafuku@gifu-u.ac.jp
Submitted: 30 July 2021
Accepted: 17 January 2022
Published online: 5 April, TAPS 2022, 7(2), 46-50
https://doi.org/10.29060/TAPS.2022-7-2/SC2662
Kheng Tian Lim1 & Bao Yun Koh2
1Department of General Surgery, Khoo Teck Puat Hospital, Singapore; 2Education Development Office, Khoo Teck Puat Hospital, Singapore
Abstract
Introduction: Medical students (MS) may lack the knowledge and experience in performing basic surgical skills (BSS) when they first commence their postgraduate surgical training. We conducted a pilot BSS workshop with specific learning outcomes for MS.
Methods: Our BSS workshop program consisted of reading the pre-workshop online modules, watching the instructional videos of skills demonstration, and completing the pre-workshop multiple-choice questions (MCQ). MS attended the onsite workshop a week later, which consisted of a basic surgical theory lecture, live demonstration of the skills by the teaching faculty and, supervised skills training coupled with feedback. Surgical skills taught were knot tying, suturing techniques, laparoscopic peg transfer, precision cutting, application of endoloop ties. A standardised surgical skills rubric was used to assess the competency and safety of BSS. A post-workshop MCQ was administered to assess the knowledge learned. The criteria for successful completion of BSS were a satisfactory grade in the surgical skills assessment and a pass score in the MCQ.
Results: All the participating MS achieved a satisfactory grade in the surgical skills assessment and passed the MCQ. Several pedagogical methods were used to enhance knowledge learning and practical skills competency including a flipped classroom in blended learning, technology-enhanced learning, kinesthetic learning, and providing effective feedback.
Conclusion: MS taught in BSS workshop can achieve competency in knowledge, skills, safe attitude and prepare them for future postgraduate surgical training. In the current COVID-19 pandemic, our challenge is to develop similar BSS in a safe environment using technology-enhanced tools such as online instructional videos and online feedback.
Keywords: Assessment, Basic Surgical Skills, Competency, Feedback, Medical Students, Outcome-based Education
I. INTRODUCTION
Medical students (MS) may lack the knowledge and experience in performing certain basic surgical skills (BSS) when they first commence their postgraduate surgical training in hospitals. Traditionally, BSS are usually not taught formally in the undergraduate medical curriculum until much later in the postgraduate level. The opportunity for teachers to teach BSS and for MS to learn is much dependent on the situation in operating rooms during assigned core surgical postings or student selective postings.
In Singapore, Yong Loo Lin School of Medicine, National University of Singapore (NUS) provides basic and advanced clinical procedural simulation training to undergraduate MS. Skills taught include gowning, scrubbing techniques, suturing, and knot-tying. Lee Kong Chian School of Medicine, Nanyang Technological University (NTU) teaches suturing and knot-tying skills in dry laboratory to undergraduate MS. All these stimulated practical skills and experience acquired by MS are transferrable to real patients’ environments. In addition, SingHealth Academy, an educational arm of SingHealth, provides BSS workshop training at the postgraduate level for interested learners. In the United Kingdom and Ireland, the BSS course is a curriculum-mandated course for postgraduate Core Surgical Training programmes.
Healthcare institution partners such as Khoo Teck Puat Hospital (KTPH), provide clinical training for MS of NUS and NTU. Our Department of General Surgery (GS) identifies the need in the learning outcomes for the graduating MS, to equip them with the competent foundation of BSS for postgraduate surgical training, although not a graduating competency requirement set by Singapore Medical Council. We conducted a small pilot workshop at our institution, aiming at educational quality improvement for our MS in three learning domains, namely surgical knowledge, practical surgical skills, and attitudes in safety that are common to all forms of surgery.
II. METHODS
A. Workshop organization, MS and Teaching Faculty, Teaching Materials
The Department of GS and Education Development Office (EDO), KTPH organised a 1-day BSS workshop for MS with the request from MS and was scheduled on 20th December 2019. Planning over three months was required to prepare the learning objectives and outcomes, workshop programme schedule, venue, teaching materials, surgical scrubs, sustenance, and coordination by the workshop director and EDO. Both the local and overseas MS were invited and recruited for training. Experienced local teaching faculty members were invited and briefed on the teaching methodology, feedback provision, and assessment criteria.
MS who agreed to participate were given instructions to read the pre-workshop fundamentals of the BSS document, watch the instructional video clips of the BSS demonstration and, complete pre-workshop multiple-choice questions (MCQ), all of which were provided online 1 week before the workshop. These pre-workshop activities may help to motivate the MS and provide an opportunity for self-assessment of their understanding of the BSS topics. MS were allowed to post questions to the workshop director for guidance. The course content and MCQ were prepared by the course director to be appropriate to the MS level.
The workshop was divided into morning and afternoon sessions to cater to a larger group of interested MS coming from overseas. The onsite workshop consisted of a short basic theory lecture, a live demonstration of the practical BSS, MS performing the practical BSS with direct supervision and corrective feedback. BSS taught were knot tying using one-hand, two-hand, and instrumental techniques. Suturing techniques taught included simple, mattress, interrupted, continuous suture. More advanced laparoscopic skills such as laparoscopic peg transfer, precision cutting, and application of endoloop ties were taught. A post-workshop MCQ was administered.
B. Assessment in Knowledge, Skills, and Attitudes
The surgical knowledge was assessed using the pre-and post-workshop MCQ, based on the course content prepared for MS.
The surgical skills assessment was carried out by direct observation of procedural skills (DOPS) using a standardised surgical skills rubric. Open surgery skills assessment included instrument selection and handling, knotting techniques, tissue handling, and suturing techniques. Laparoscopic surgery skills assessment included instrument selection and handling, peg transfer, precision cutting, and ligating loop. The overall summative assessment of global grading in the surgical skills domain by the teaching faculty was either satisfactory or unsatisfactory.
MS were assigned to work in pairs with the ratio of MS: teaching faculty as 2:1. Assessment in the attitude and behavior domain was based on direct observation in the safe handling of sharps and needles, general assisting, and laparoscopic camera assisting skills.
C. Feedback and Competency
The teaching faculty used DOPS to provide feedback on the practical BSS performed by the MS which allowed the MS to improve and progress from a novice to a competent learner level in the skills and attitude domains. The specific, timely, and purposeful feedback served as a channel for MS to improve and reflect on their learning outcomes in these domains.
The competency criteria for successful completion of the BSS workshop were set as a pass mark of 60% in the summative MCQ test and a satisfactory grade in the summative skills assessment by the teaching faculty. A Certificate of Attendance would be awarded to MS who have acquired the competency criteria.
III. RESULTS
Assessment and evaluation data gathered for this workshop and pre-workshop MCQ questions were uploaded to an online repository for archiving and validation purposes. It may be assessed through the following Digital Object Identifier (DOI): https://doi.org/10.6084/m9.figshare.16884877.v2 (Lim & Koh, 2021).
A total of 38 MS signed up for the BSS workshop with 1 dropout. Thirty-seven MS attended the workshop of which 25 were from overseas medical schools. Thirty-six MS attempted the pre-workshop MCQ (10 questions). Thirty-seven MS passed the post-workshop MCQ (15 questions). All MS achieved satisfactory grades in practical skills. There was no needle stick injury reported.
The BSS workshop program evaluation form was administered and completed anonymously for the quality improvement process after verbal consent was taken from the participants. (Table 1).
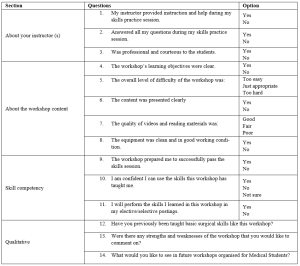
Table 1. BSS Workshop for MS Program Evaluation
IV. DISCUSSION
Bloom’s Taxonomy comprises three learning domains known as cognitive (knowledge), affective (attitude), and psychomotor (skills). Each domain has a hierarchy that corresponds to distinct levels of learning which is important for students to develop holistically. The learning objectives of the BSS workshop for MS are thus designed to fulfil these three domains, specifically to: 1) acquire the fundamental knowledge of BSS (knowledge), 2) demonstrate a variety of surgical knots and suturing skills effectively (skills) and, 3) handle and use of surgical instruments and tissue safely (attitude).
Harden et al. (1999) described an outcome-based education framework that comprises six levels of training to achieve the outcomes. These six levels of training are: 1) awareness of the procedure, 2) full theoretical understanding of the procedure, 3) observation of the procedure, 4) carrying out part of the procedure, 5) undertaking the procedure under the supervision and, 6) undertaking the procedure unsupervised. Similarly, the programme activities of the BSS workshop for MS were developed to cover these six levels of training. The learning outcomes of this workshop are to equip the MS with the competency of BSS for postgraduate surgical training. The teaching faculty members share their knowledge, demonstrate their expertise, advise MS, and provide feedback to improve technical skills and promote learning.
Effective feedback is necessary to enhance learning. Pendleton et al. (2003) described a four-step process for carrying out a feedback session. Ramani and Krackov (2012) described twelve tips for clinical teachers to provide effective feedback to undergraduate and graduate medical trainees. Our teaching faculty members were able to provide effective feedback to MS using these frameworks to establish a respectful learning environment, feedback on direct observation, make feedback timely, reinforce and correct observed behaviors, use specific language to focus on performance, confirm the learner’s understanding and conclude with an action plan.
The assessment for learning in the BSS workshop for MS was designed to align with the three learning domains using: 1) pre-and post-workshop MCQ to test surgical knowledge, 2) DOPS by the teaching faculty to test surgical skills and, 3) DOPS in the safe handling of sharps and needles, general assisting and laparoscopic camera assisting skills to test the attitude and behavior. A standardised surgical skills rubric was used for DOPS.
Technology-enhanced learning (TEL) intervention and enhancement can be characterised by 1) replicating existing teaching practices, 2) supplementing existing teaching or, 3) transforming teaching, learning processes, and outcomes (Kirkwood & Price, 2014). Several pedagogical methods were used in this BSS workshop to enhance knowledge learning and skills acquisition such as flipped classroom in blended learning, a mixture of the three characteristics of TEL, kinesthetic learning, and providing effective feedback. In the current COVID-19 pandemic, there are challenges to conducting such a practical workshop. TEL tools that combine online educational materials, instructional videos, feedback, and face-to-face online interaction such as Zoom, and Microsoft Teams are the new norm.
The limitation of this workshop includes the lack of MCQ standardisation process and the quality of the video clips which we intend to improve in the next workshop.
V. CONCLUSION
Conducting a BSS workshop for MS with specific learning outcomes is feasible where the MS can achieve competency in knowledge, skills, safe attitude and prepare them for postgraduate surgical training. In the current COVID-19 pandemic, our challenge is to develop similar BSS in a safe environment using TEL tools.
Notes on Contributors
Dr. Lim Kheng Tian designed the work, reviewed the literature, drafted the work, revised the content critically, and wrote the manuscript. Ms. Koh Bao Yun contributed to the design and administration of the work, gave critical feedback to the content, and revised the manuscript. All authors have read and approved the final manuscript.
Ethical Approval
This 1-day workshop program was conducted for educational quality improvement (QI) with approval from the Department of GS and EDO, KTPH. This article was submitted with Institutional Review Board/Ethical approval for exemption from full review. We have attached the local IRB waiver document NHG DSRB Ref: 2021/00888.
Data Availability
Inline to make research available to the scientific community for data replication and scientific progress, the dataset of this workshop may be found for free through the Figshare website: https://doi.org/10.6084/m9. figshare.16884877.v2
Acknowledgement
The authors want to thank all the MS and teaching faculty who participated in the workshop. We would like to acknowledge Dr. Lee Yao Zong, Associate Consultant of the Department of GS, KTPH for providing help in the laparoscopic educational content. We would like to acknowledge the technical help of Mr. Mohamad Sean Abdullah, former Experimental Surgical Services Development Executive of the Department of GS, KTPH. We would like to acknowledge equipment support from KARL STORZ Endoscopy Singapore Sales Pte Ltd for providing the reusable laparoscopic trainer and laparoscopic instruments. We also like to acknowledge NHG Education for linking up EDO, KTPH with the Singapore Medical Society of Australia and New Zealand (SMSANZ).
Funding
There is no funding for this paper. The suturing materials used in the workshop were funded by the Pre-Employment Clinical Training (PECT) Funds received by KTPH for local MS whilst overseas MS were self-funded. The funder was not involved in the design, delivery of the workshop, or submission of the paper.
Declaration of Interest
All authors declare no conflicts of interest, including financial, consultant, institutional, and other relationships that might lead to bias or a conflict of interest.
References
Harden, R. M., Crosby, J. R., Davis, M. H., & Friedman, M. (1999). AMEE Guide No. 14: Outcome-based education: Part 5-From competency to meta-competency: A model for the specification of learning outcomes. Medical Teacher, 21(6), 546–552. https://doi.org/10.1080/01421599978951
Kirkwood, A., & Price, L. (2014). Technology-enhanced learning and teaching in higher education: What is ‘enhanced’ and how do we know? A critical literature review. Learning, Media and Technology, 39(1), 6–36. https://doi.org/10.1080/17439884.2013.770404
Lim, K. T., & Koh, B. Y. (2021). Start small and aim big in conducting a basic surgical skills workshop for medical students—Repository data (p. 11710 Bytes) [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.16884877.v2
Pendleton, D., Schofield, T., Tate, P., & Havelock, P. (2003). The New Consultation. Oxford University Press.
Ramani, S., & Krackov, S. K. (2012). Twelve tips for giving feedback effectively in the clinical environment. Medical Teacher, 34(10), 787–791. https://doi.org/10.3109/0142159X.2012.684916
*Lim Kheng Tian
Department of General Surgery,
Khoo Teck Puat Hospital,
90 Yishun Central,
Singapore 768828.
Tel: +65 65558000
Email: lim.kheng.tian@ktph.com.sg
Submitted: 22 August 2021
Accepted: 28 December 2021
Published online: 5 April, TAPS 2022, 7(2), 42-45
https://doi.org/10.29060/TAPS.2022-7-2/SC2682
Lee Man Xin1*, Zhang Yuan Helen2* & Fatimah Lateef2,3
1Changi General Hospital Emergency Department, Singapore; 2Singapore General Hospital Emergency Department, Singapore; 3Singhealth Duke-NUS Institute of Medical Simulation (SIMS) Education Office, Singapore
*Joint first authors
Abstract
Introduction: Advanced Cardiac Life Support (ACLS) course is one of the mandatory certifications for the majority of medical as well as some nursing professionals. There are, however, multiple variations in its instruction model worldwide. We aim to evaluate the efficacy of traditional ACLS course versus a hybrid ACLS course utilised during the COVID-19 pandemic.
Methods: This retrospective study was carried out at SingHealth Duke-NUS Institute of Medical Simulation using course results of participants in the centre’s ACLS course between May to October 2019 for the traditional course were compared with participants attending the hybrid course from February to June 2021.
Results: A total of 925 participants were recruited during the study period. Of these, 626 participants were from the traditional group and 299 participants were from the hybrid learning group. There is no statistically significant difference between the two group (χ2=1.02 p = 0.313) in terms of first pass attempts; first pass attempt at MCQ (p=0.805) and first pass attempt at practical stations (p=0.408). However, there was statistically significant difference between the mean difference in results of traditional vs hybrid MCQ score, -0.29 (95% CI: -0.57 to -0.01, p=0.0409). Finally, senior doctors were also found to perform better than junior doctors in both traditional (p=0.0235) and hybrid courses (p=0.0309) at the first pass attempt of ACLS certification.
Conclusion: Participants in the hybrid ACLS course demonstrated at least equal overall proficiency in certification of ACLS as compared to the traditional instruction.
Keywords: Advanced Cardiac Life Support, Teaching Model, COVID-19, Hybrid Learning
I. INTRODUCTION
Cardiopulmonary resuscitation (CPR) represents an emergency lifesaving procedure for cardiac arrest patients. It is a core skillset for every licensed physician, graduating medical students and paramedics. It provides evidence-based algorithms to be executed to optimise the likelihood of survival in cardiac arrest patients. Cardiac arrest poses a major public health challenge. Worldwide, sudden and unexpected cardiac death is one of the most common causes of death. Given such a substantial disease burden, structured and continued training of physicians and first responders on advanced cardiac life support (ACLS) is extremely crucial. In Singapore, about 3000 people have a sudden cardiac arrest every year (Ong, 2020).
The first Advanced Cardiac Life Support (ACLS) course in Singapore, was started in late 1985 and traditionally it has been conducted over two days. It comprises of pre-reading from a manual outlining the procedure algorithms, a combination of face-to-face didactics and hands-on skills stations conducted by licensed providers and instructors, followed by multiple-choice theory and practical certification tests. It mainly focuses on technical knowledge and skills which needs to be recertified every two years (Anantharaman, 2017). Since the implementation of social distancing measures under DORSCON Orange in Singapore in response to the COVID-19 disease outbreak on 7th February 2020, ACLS teaching model has since been modified to multimedia lectures followed by small-group (maximum 5 people) practical lessons, which was further adjusted to include an online self-administered pre-lecture quiz from 18th February 2021 onwards. Limited evidence has shown that written evaluation is not a predictor for skills performance in an ACLS course and there is now, a growing body of advocates for high-fidelity mannequin-based simulation supplementing ACLS curricula. Multiple research studies have focused on the efficacy of various educational and instructional methods for ACLS teaching in terms of improvement to the resuscitation knowledge and clinical skills (Thorne et al., 2017).
We aim to retrospectively evaluate the efficacy of our new hybrid ACLS teaching model based on participants passing rate of both theory and practical tests as compared to the traditional ACLS instruction model. The primary goal is to provide enhanced insights into the way ACLS training should be conducted and further refine our courses as we evolve in the new norm of living with the COVID-19 pandemic. Institutional Review Board waiver has been obtained through Singapore Health Service (CIRB: 2021/2499).
II. METHODS
A. Study design and participants
This retrospective study was carried out at SingHealth Duke-NUS Institute of Medical Simulation (SIMS) using the course results of participants in the centre’s Advanced Cardiac Life Support (ACLS) course. A waiver of consent was approved by the institute’s CRIB committee as the results were anonymised.
The ACLS course traditionally comprises face-to-face didactic lecture components and practical skills stations culminating in MCQ and practical assessment. Successful completion of both MCQ and practical assessment results in certification or recertification for the participants.
In the hybrid ACLS learning model, the didactic lecture component has been replaced with an interactive online learning platform while maintaining the same practical skills stations with reduced instructor to student ratio because of safe distancing measures. To facilitate learning, a pre- and post-lesson quiz, with 25 MCQ questions, was administered on the online learning platform.
Course results of participants attending the traditional course from May to October 2019 were compared with participants attending the hybrid course from February to June 2021. No participants were found to have attended both the traditional and hybrid ACLS courses, to date. We did not differentiate between recertification and certification courses since there are no differences in assessments.
B. Outcome measures
Our primary outcome measure was the proportion of participants with successful first pass attempt at course certification between traditional and hybrid ACLS courses.
For secondary outcomes, we analysed the mean difference in MCQ scores and first pass attempts at practical stations between traditional and hybrid ACLS instructions. We also compared differences between pre- and post-lesson quiz scores administered during the hybrid learning to assess retention of theoretical knowledge. Lastly, we conducted a sub-group analysis comparing the proportion of senior doctors and junior doctors who pass the course at the first attempt, in both the traditional and hybrid learning groups. Here, senior doctors refer to individuals with specialist registration while junior doctors refer to all other registered medical practitioners.
C. Statistical analysis
A priori sample size estimation was carried out with the assumption that 90% of participants will pass with the first attempt in both traditional and hybrid ACLS teaching models. We used a non-inferiority margin of 10%. Taking α = 0.05 and a statistical power of 80%, we determined that would require at least 155 participants per group.
Statistical analysis was performed using Microsoft Excel 2019. T-test was used when comparing means, Chi-square test was used when comparing categorical variables.
III. RESULTS
A total of 925 participants were recruited during the study period. Of these, 626 participants were from the traditional group and 299 participants, from the hybrid learning group. No participants were excluded from the study. Table 1 shows the characteristics of both groups. The data supporting this study are openly available at https://doi.org/10.6084/m9.figshare.15131664.v1 (Lee et al., 2021).
For the traditional group, 87.7% (549 of 626) passed at the first attempt, whilst for the hybrid group, 90.0% (269 of 299) passed at first attempt (See Table 1). There was no statistically significant difference between the two groups (p = 0.313).
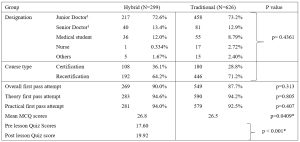
Table 1. Baseline Demographics of Participants for the ACLS Courses and comparison of primary and secondary outcome measures between the Hybrid and Traditional ACLS courses participants
1 Senior doctors are registered specialists under Singapore Medical Council. Junior doctors are all other registered medical practitioners under Singapore Medical Council.
There were no statistically significant differences between the two groups in terms of proportion of first pass attempt at MCQ (p=0.805) and first pass attempt at practical stations (p=0.408). There was however, a statistically significant difference, but with a very small effect size, between the mean difference in results of traditional vs hybrid MCQ score, -0.29 (95% CI: -0.57 to -0.01, p=0.0409).
We also compared the pre- and post-lesson quiz scores in the hybrid learning group. 21 participants were excluded from the analysis due to incomplete pre- or post- test results. We found a mean score difference of 2.32 (95% CI: 1.84 to 2.80, p < 0.001), out of a maximum score of 25, which was higher in post-test group.
Lastly, we compared the proportion of first pass test attempts between senior and junior doctors in both traditional and hybrid learning groups. Senior doctors consistently performed better than junior doctors in both traditional (96.3% vs 87.8% p=0.0235) and hybrid settings (100% vs 89.4% p=0.0309).
IV. DISCUSSION
ACLS is one of the most basic yet crucial skills of medical practitioners worldwide receiving special attention in the framework of various international and national resuscitation councils and societies (Thorne et al., 2017). Clinical educators must explore modalities and evolving technologies that can overcome the barriers of cost, access, and frequency of exposure, while balancing flexibility and applicability that follow deliverable sequelae. Thus far, participants of blended e-learning ACLS courses are known to demonstrate similar scores on the knowledge test, skills test and their final passing rate. The e-learning ACLS course also demonstrates equivalence to traditional face-to-face learning in equipping participants with ACLS skills when compared to the traditional course. This was demonstrated in our results as well. This is a value-added benefit, especially when considering factors such as increased autonomy, cost-effectiveness, decreased instructor burden and improved standardisation of course material (Thorne et al., 2017).
As we shift more towards andragogy among adult professionals, the principles for ACLS instruction should also focus more on self-directed, self-motivated and experiential instruction. Evidence does support that the form and content of these highly structured/model courses are important to transfer the clinical competence that is needed, especially in unstructured, emergencies (Rasmussen et al., 2013). Hence, exploring a sustainable model of ACLS knowledge translation is another important point since further research is needed to develop the optimal evaluation system for the ACLS training program which includes evaluation of the participants, the instructors, and the overall program. The goal should be to assess the degree to which the ACLS program is meeting its objective: to educate medical practitioners, first responders and rescuers.
The COVID-19 pandemic has affected simulation centres where ACLS courses are routinely held. Alternative education modalities have been employed, which include computer-based simulation where technology is used to enhance, augment or even at times, replace real-life simulation. It not only offers the professionals convenience but, complies with safe-distancing or ‘work-from-home’ restrictions put forth by regulatory bodies in many countries. Online modules of virtual reality have also been explored as these can be accessed anywhere electronically and can reduce the amount of face-to-face time that routine training normally requires.
V. CONCLUSION
Hybrid instruction of ACLS training for certification should be recommended as one of the main formats of course delivery as it is as effective compared to the traditional face-to-face training program. From our results it has performed well enough to allow for the safe transition and application of ACLS training in this new era.
Notes on Contributors
Lee Man Xin is involved in conceptualising the study, analysing and interpreting the data, drafting the above manuscript and approving the version to be published. He agrees to be accountable for all aspects of the work.
Zhang Yuan Helen is involved in conceptualising the study, interpreting the data, drafting the above manuscript and approving the version to be published. She agrees to be accountable for all aspects of the work.
Lateef Fatimah is involved in finalising the study conceptualisation and determining key elements for analysis. She is involved in the revision and final approval of the version to be published. She agrees to be accountable for all aspects of the work.
Ethical Approval
Institutional Review Board waiver has been obtained through Singapore Health Service (CIRB: 2021/2499).
Data Availability
The data supporting this study are openly available at figshare repository: https://doi.org/10.6084/m9.figshare.15131664.v1
Acknowledgement
The authors would like to thank Mr Billy Tee, Ms Suppiah Madhavi and Ms Angeline Ng from Singhealth Duke-NUS Institute of Medical Simulation (SIMS) Singapore for providing the data sets.
Funding
This paper receives no funding from outside sources.
Declaration of Interest
Authors have nothing to declare, nor any conflict of interests.
References
Anantharaman, V. (2017). The National Resuscitation Council, Singapore, and 34 years of resuscitation training: 1983 to 2017. Singapore Medical Journal, 58(7), 418–423. https://doi.org/10.11622/smedj.2017069
Lee, M. X., Lateef, F., & Zhang, H. Y. (2021). Hybrid ACLS model (version 1). [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.15131664.v1
Ong, M. E. (2020, October 2). Improving outcomes for Out-of-Hospital cardiac arrest victims. The Straits Times. https://www.singhealth.com.sg/rhs/news/research/improving-outcomes-for-out-of-hospital-cardiac-arrest-victims
Rasmussen, M. B., Dieckmann, P., Barry Issenberg, S., Østergaard, D., Søreide, E., & Ringsted, C. V. (2013). Long-term intended and unintended experiences after Advanced Life Support training. Resuscitation, 84(3), 373–377. https://doi.org/10.1016/j.resuscitation.2012.07.030
Thorne, C. J., Lockey, A. S., Kimani, P. K., Bullock, I., Hampshire, S., Begum-Ali, S., & Perkins, G. D. (2017). e-Learning in Advanced Life Support-What factors influence assessment outcome? Resuscitation, 114, 83–91. https://doi.org/10.1016/j.resuscitation.2017.02.014
*Lee Man Xin
Changi General Hospital Emergency Department
2 Simei Street 3, Singapore 529889
Email: Lee.Man.Xin@singhealth.com.sg
Submitted: 10 August 2021
Accepted: 28 October 2022
Published online: 5 April, TAPS 2022, 7(2), 37-41
https://doi.org/10.29060/TAPS.2022-7-2/SC2670
Qianhui Cheng1, Joanna Pearly Ti1,2, Wai Yung Yu1,2, Hui Ping Oh1, Yih Yian Sitoh1,2
1Department of Neuroradiology, National Neuroscience Institute, Singapore; 2Duke NUS Graduate Medical School, Singapore
Abstract
Introduction: Magnetic Resonance (MR) safety is critically important in any Radiology Department, and MR-related accidents are preventable. Serious games provide opportunities for learners to build MR safety awareness through play in an immersive learning environment by using simulated scenarios such as screening virtual patients and managing an MR-related accident.
Methods: We developed a serious game, in partnership with a game developer, introducing MR safety concepts to learners as they navigate through a virtual 3D Radiology department. Drag-and-drop minigames are incorporated to aid the learner to identify hazards in and around the MR environment. Virtual patients are placed in waiting areas to provide realism, and learners are tasked to screen them as part of MR Safety Screening checks. A simulation of an MR-related accident prompts learners to make decisions or take actions to ensure safety and mitigate further risks during the accident. The learner also role-plays as a Risk Officer to identify the multiple key incidents that led to the accident. These formative assessments, with instantaneous feedback, assesses the learners’ knowledge of MR safety.
Results: Pilot feedback of this serious game revealed that it is realistic, engaging and relatable. The instructions within the game were clear and aided learning. The game has also been scaled up and customised for the radiology departments of 3 other healthcare institutions.
Conclusion: Serious games provide a training solution to raise MR safety awareness by simulating real-life scenarios in an immersive learning environment. It supplements face-to-face training and is scalable to other healthcare institutions.
Keywords: Medical Education, Technology-Enhanced Learning, Gamification, MR Safety, Workplace Safety, Simulation
I. INTRODUCTION
Magnetic Resonance (MR) safety plays a critical role in any Radiology Department to ensure the safety of patients and healthcare workers. MR is an imaging tool that uses a magnetic field to acquire detailed images of the body for the investigation of diseases.
MR-related incidents are prevalent; for instance, the US Food and Drug Administration (US FDA) received 1568 adverse events reports for MR-related incidents over 10 years between 2008 and 2017 (Delfino et al., 2019). These reported adverse events included mechanical events (eg. crushed injuries) and projectiles that are caused by objects pulled in by the magnetic field.
Hence, caution must be taken as the MR scanner’s magnetic field is always on and poses safety risks when MR safety protocols are not adhered to. Ferromagnetic objects can become projectiles within or near the magnetic field and pose a danger to patients and staff members present within it. MR-related accidents are preventable and are caused by MR safety lapses, occasionally resulting in deadly outcomes. Hence, building MR safety awareness for all levels of healthcare staff, from ward staff to those who work in the radiology department, is crucial.
Today’s generation of learners, coined as ‘digital natives’ are accustomed and receptive to the digital world and game-based learning (Girard et al., 2013). Serious games refer to digital games with the specific purpose of training learners to meet an educational objective (Girard et al., 2013). It has been used as an educational tool to realistically simulate incidents for disaster risk management (DRM) and to raise awareness (Solinska-Nowak et al., 2018). Similarly, it has also been used as training tools in health professional education for patient safety (Ricciardi & De Paolis, 2014).
Serious games can virtually replicate the MR environment and simulate MR incidents that are too dangerous to re-enact in the real world, thus preparing the healthcare professionals for such scenarios. The serious game is an ideal training solution to complement face-to-face training of healthcare professionals on MR safety and can be incorporated into the standardised curriculum design. The intended learning outcomes can be achieved through the constructive alignment of learning activities (within the game and on-the-job) and coupled with assessment and in-game feedback.
Using a learner-centric approach, serious games provide learners with risk-free decision-making opportunities, enhancing MR safety competency through play within an immersive, yet safe, virtual learning environment. These allow learners to exercise the safety behaviours and actions required at the workplace to handle situations that they may encounter.
This short communication aims to describe how this serious game was developed and how the game was evaluated at the pilot stage.
II. METHODS
The team was awarded the Learning Technology Adoption Grant in January 2020 offered by SkillsFuture Singapore (SSG). It is a grant to fund medical education serious games in SingHealth. SingHealth Academy partnered the team with game developers, including instructional designers who helped with the game development.
MR safety lapses can be deadly, and the learning outcomes of the game are to gain knowledge of MR safety and accident risk management, and to be able to demonstrate understanding of these concepts by application of knowledge in the application scenarios within the game and at the workplace.
The target audience for this game includes radiology staff, healthcare staff or ancillary staff, such as housekeeping personnel, who may enter the MR environment and thus, are required to ensure MR safety in their line of work.
The game sets out in a virtual radiology department, modelled after the Neuroradiology department at the National Neuroscience Institute. The virtual world includes virtual patients, staff as player and non-player characters in institutional uniforms, and medical devices that mirror real-life equipment in the radiology department.
Two games were created in the MR safety series. In the first game, learners navigate as an avatar to interact with objects in the MR environment, such as medical devices and virtual patients. The learning outcome of the first game is to understand the key MR safety concepts which follow the American College of Radiology (ACR) guidelines (American College of Radiology, 2020).
The second game was modelled on an MR-related accident. Learners assess the accident scenario (Fig 1a) and consider strategies for risk management, evaluating their options within the game. Critical wrong decisions or actions made during the gameplay may trigger an abrupt end to the game. This emphasises the urgency of actions required in an MR-related accident when a life is in danger and the immediate steps required to be taken to reduce the risk for further injuries. Beyond the virtual accident, the learner role-plays as a Risk Officer to assess and identify several key incidents that led to the accident as part of a root cause analysis investigation.
Figure 1a (left): MR accident scenario within the serious game
Figure 1b (right): Application of MR safety labelling near the MR scanner
Minigames are used as formative assessments, and learners receive instantaneous in-game feedback from their attempts. By screening virtual patients and placement of medical devices in their appropriate location, as part of the MR safety screening checks, the game assesses learners’ ability to identify hazards in and around the MR environment (Fig 1b), with correct placement demonstrating their learning.
For the purpose of game development, beta testers from the Neuroradiology department were included to gather preliminary feedback about the game through implied consent. A survey was administered, and responses ranged on a Likert scale (1=Strongly disagree to 5= Strongly agree).
III. RESULTS
In the initial phase of game development, beta testing of the game was conducted on 11 staff, including radiographers, radiologists, radiography assistants, radiology nurses and administrative staff with differing years of MR work experience. Beta-testers were also selected for their experiences in playing games, ranging from none to some experience. Data reported below as ‘agreed’ is aggregated to reflect ‘agreed’ and ‘strongly agree’ responses (Cheng et al., 2021).
In terms of the learning instructions, all respondents (100%) were aware of the learning outcomes. 81.82% found the instructions clear, and they knew what to do at every stage.
In terms of the virtual game environment, respondents generally felt the game has realistic engagement regarding the design. All respondents (100%) agreed that the game environment was realistic; the avatars (player characters) and objects in the game resembled those at the workplace (100%), and the background sound aided the engagement with the game (81.82%). 90.91% of respondents could also relate to the main player character within the game.
On the contrary, some respondents had trouble operationalising the game mechanics; 27.27% had trouble using the controls, and 36.36% found it difficult navigating within the game.
Overall, 90.91% found the game was fun, and engaging (100%). 81.82% agreed that their past experience helped them to overcome some of the obstacles in the game. Furthermore, 81.82% agreed that the results are a fair reflection of their skill and competency in MR safety.
Arising from the positive preliminary feedback of this serious game, the game has been shared and further adopted by radiology departments from three other healthcare institutions [Singapore General Hospital (SGH), KK Women’s and Children’s Hospital (KKH) and Sengkang General Hospital (SKH)]. The respective teams are working with the game developers to customise and adapt the environment to the local site, including medical devices and safety labels in their local settings for MR safety education.
IV. DISCUSSION
The MR safety game is an educational tool to assess and align MR safety competency for healthcare staff. Furthermore, the game can be incorporated into the orientation curriculum of radiographers as part of a competency checklist onboarding package, supplementing face-to-face training.
Being accustomed to the digital games, ‘digital natives’ as the target generation of learners would find this mode of delivery more relatable, engaging and realistic (Girard et al., 2013). At the same time, it also incorporates a structured learning design, constructively aligned with clear learning outcomes, learning activities and assessment coupled with instantaneous in-game feedback.
However, we acknowledge that some learners may experience difficulties with navigation in a virtual world. Hence, clear instructions by the facilitator on gaming instructions need to be incorporated in the pre-briefing to learners for more effective engagement and outcomes.
As learners navigate the virtual environment, they pick up MR safety knowledge and apply them to game scenarios as part of active learning. Role-playing as a Risk Officer also makes them more aware of the possible safety lapses that may occur and lead to an MR-related accident. Post-game play feedback should also be incorporated for learners to align the behaviours expected of learners at the workplace.
Beyond the institution, it is scalable to staff from other radiology departments and hospital ward staff, such as nurses and doctors who have no prior knowledge of MR safety but would have adhoc opportunity to be in the MR environment, for example, accompanying a patient to the radiology department for an MR scan.
Finally, through experiential learning, the game emphasises that everyone plays a critical role in MR safety and that safety lapses can lead to accidents.
V. CONCLUSION
Purpose-built simulation serious games that mimic a virtual radiology department provide an ideal training solution for MR safety education. Serious games provide an immersive learning environment where simulated scenarios such as safety screening of virtual patients and MR-related accidents is made possible. Simulation of dangerous scenarios that are impossible to recreate in the real world provides opportunities to raise MR safety awareness and is also scalable to the wider healthcare community.
Notes on Contributors
Cheng Qianhui contributed to the conceptualisation and design of this serious game, drafting the manuscript and approved the final version to be published.
Joanna Pearly Ti contributed to the conceptualisation and design of this serious game, revised the manuscript for intellectual content and approved the final version to be published.
Yu Wai-Yung is a mentor to the team, revised the manuscript for intellectual content and approved the final version to be published.
Oh Hui Ping contributed to the conceptualisation and design of this serious game, revised the manuscript for intellectual content and approved the final version to be published.
Sitoh Yih Yian is a mentor to the team, revised the manuscript for intellectual content and approved the final version to be published.
Ethical Approval
Review not required as stipulated by CIRB (CIRB Reference No.: 2021/2397).
Data Availability
The beta testing evaluation data presented in this manuscript is available in the Figshare data repository: https://doi.org/10.6084/m9.figshare.14473074.v1
Acknowledgement
We would like to thank SingHealth Academy and Playware Studios for their tremendous contribution for the creation of this serious game. We are also thankful to NNI neuroradiology staff for their help with the pre-testing of the game, contributing to the game development through honest feedback. We are thankful to Serious Games Asia and Singapore University of Technology and Design (SUTD) for co-developing the survey evaluation. We sincerely thank our scale-up teams, the radiology departments from Singapore General Hospital (SGH), Sengkang General Hospital (SKH) and KK Women’s and Children’s Hospital (KKH) so that more staff across SingHealth can benefit from MR safety training through this serious game.
This project has been presented as Free Communication at the Asia Pacific Medical Education Conference 2021, and the author was awarded the Young Scholar Award Runner-up.
Funding
The game development and scale-up is funded by Learning Technology Adoption Grant (LTAG) offered under SkillsFuture Singapore (SSG), which SingHealth Academy has applied to jumpstart medical education serious games in SingHealth institutions. SingHealth Academy is the education arm in SingHealth to coordinate the application with SSG.
Declaration of Interest
The authors declare no conflict of interest.
References
American College of Radiology. (2020). ACR manual on MR safety. https://www.acr.org/-/media/ACR/Files/RadiologySafety/MRSafety/Manual-on-MR-Safety.pdf
Cheng, Q., Ti, J. P., Yu, W.-Y., Oh, H. P., & Sitoh, Y. Y. (2021). MR safety beta testing data [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.14473074.v1
Delfino, J. G., Krainak, D. M., Flesher, S. A., & Miller, D. L. (2019). MRI‐related FDA adverse event reports: A 10‐yr review. Medical Physics, 46(12), 5562–5571. https://doi.org/10.1002/mp.13768
Girard, C., Ecalle, J., & Magnan, A. (2013). Serious games as new educational tools: How effective are they? A meta-analysis of recent studies. Journal of Computer Assisted Learning, 29(3), 207–219. https://doi.org/10.1111/j.1365-2729.2012.00489.x
Ricciardi, F., & De Paolis, L. T. (2014). A comprehensive review of serious games in health professions. International Journal of Computer Games Technology, 2014, Article 787968. https://doi.org/10.1155/2014/787968
Solinska-Nowak, A., Magnuszewski, P., Curl, M., French, A., Keating, A., Mochizuki, J., Liu, W., Mechler, R., Kulakowska, M., & Jarzabek, L. (2018). An overview of serious games for disaster risk management – Prospects and limitations for informing actions to arrest increasing risk. International Journal of Disaster Risk Reduction, 31, 1013–1029. https://doi.org/10.1016/j.ijdrr.2018.09.001
*Cheng Qianhui
National Neuroscience Institution
11 Jalan Tan Tock Seng,
Singapore 308433
Singapore 117593
Email: qianhui_cheng@nni.com.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









