How do factors in fixed clinical teams affect informal learning among Emergency Medicine Residents
Submitted: 28 July 2022
Accepted: 12 October 2022
Published online: 3 January, TAPS 2023, 8(1), 25-32
https://doi.org/10.29060/TAPS.2023-8-1/OA2850
Choon Peng Jeremy Wee1, Mingwei Ng1 & Pim W. Teunissen2
1Department of Emergency Medicine, Singapore General Hospital, Singapore; 2School of Health Professions Education (SHE), Faculty of Health Medicine and Life Sciences, Maastricht University, Maastricht, The Netherlands
Abstract
Introduction: This study was performed to understand how fixed clinical teams affected informal learning in Emergency Medicine Residents. Better understanding the effects of team dynamics on informal learning may help to optimise learning and improve performance.
Methods: From 8th February 2020 till 27th September 2020, the Singapore General Hospital Emergency Department adopted a fixed team system. Zoom interviews were carried out amongst Emergency Medicine Residents who worked in the fixed team system using a semi-structured iterative interview guide. A qualitative content analysis was used for this exploratory study. The interviews were transcribed verbatim, anonymised and coding via template analysis performed. Data collection and analysis were performed until data sufficiency.
Results: The themes identified centred around relationship dynamics, team composition and motivation for learning. The first was how improved relationships led to improved trust, communications and camaraderie among team members. This improved peer learning and clinical supervision and provided a more personalised learning experience. A balanced team composition allowed learners to be exposed to experts in various subspecialties. Finally, there was an initial increase in motivation, followed by a decrease with time.
Conclusion: In postgraduate medical education, working in a fixed team system with balanced members had positive effects on informal learning by strengthening relationships and communications.
Keywords: Informal Learning, Workplace Learning, Fixed Teams, Medical Education, Postgraduate
Practice Highlights
- Fixed teams can strengthen relationships between members through better trust, familiarity and communication.
- A balanced fixed team with members having different areas of expertise allows a variety of perspectives.
- Rotation of team members may achieve a balance between the stronger relationship and familiarity of the members of fixed teams and the greater variance in perspectives from a non-fixed team system.
I. INTRODUCTION
Fixed teams (FT) and non-fixed teams (NFT) exist in medicine because of differing service requirements and manpower resources. Examples of FTs can exist in ward round teams and operating surgical teams (Eddy et al., 2016; Stepaniak et al., 2012) where personnel stay within the same work team for long periods. In other areas of healthcare like the Emergency Departments (ED), a NFT system is usually employed where teams are formed according to the personnel rostered to work on that shift and team members change every shift. This allows a more flexible system for the team members as they can request off days and leave according to their personal schedule and yet allows for 24-hour coverage in the ED.
High levels of performance are required of medical teams, both fixed and non-fixed, to achieve good patient outcomes. Therefore, team members should learn how to work effectively together to deliver the best patient care. There are studies, both within healthcare and other industries, which showed mixed results when FT were compared with NFT with regards to team performance. A systematic review on minimal invasive surgical teams found that the FTs had better teamwork and had reduced rates of technical mistakes compared to NFTs (Gjeraa et al., 2016). However, an aviation study showed that FTs made more minor errors compared to NFTs due to FT members being too familiar with each other and overlooking errors (Barker et al., 1996). Although it is unclear how transferable specific research findings from non-healthcare domains are, what is clear is that FTs and NFTs are different in the way teams were formed and the amount of time team members spend working together. There is a lack of understanding if and how these differences affect the way learning takes place in FT and NFTs; which could translate to the performance of the team and its members.
Workplace learning occurs through informal learning by experiencing work challenges and via interpersonal relationships. Informal learning can be supported through learner engagement by encouraging active participation in work activities and aligning learners’ interests with that of the organisation’s objectives towards improving the individuals’ and organisation’s capabilities (Billett, 2007). Informal learning is now widely accepted as a form of workplace learning that occurs out of a formal planned teaching program. It usually occurs during work activities which are not primarily aimed towards education, with learning objectives not planned beforehand (Callanan et al., 2011; Rogoff et al., 2016; Watkins et al., 2018). Although informal learning had been studied, there are very few studies looking at how being in FTs affects informal learning. A review on the involvement of employees in workplace learning (Kyndt & Baert, 2013) revealed that there was a paucity of literature on whether any team system improves the involvement of employees in informal learning. Thus, it remains to be studied what effects working in a FT system has on informal learning especially of the more junior team members.
An integrative literature review on informal learning found that some of the important components of informal learning within members of a team and between teams included interpersonal relationships, feedback, networking and leadership (Jeong et al., 2018). Therefore, there may be differences in interpersonal relationships and feedback between the different team systems. It is known that good interpersonal relationships include good supervisor and peer support and both affect whether what is learnt is applied at the workplace (Burke & Hutchins, 2016), there was little published data on whether supervisor and peer support or even the supervisory relationship were affected by the amount of time spent together. Within some healthcare systems both FTs and NFTs consists of members with varying levels of experience, differing expertise and roles. In a FT, the learners are only supervised by supervisors within that team; therefore, each learner’s supervised time is divided within a small group of supervisors as compared to a NFT system where each learner’s supervised time is spread amongst a larger number of supervisors. Thus, despite this increased time spent together in a FT, it is not clear if working in a FT impacts supervisory or interpersonal relationship.
Having a good trusted learner-supervisor relationship can result in the establishment of an “Educational Alliance” (Telio et al., 2015). This is because feedback from a credible trusted source was more readily accepted and feedback is another important component of effective informal learning within a team (Jeong et al., 2018).
Furthermore, a study among social work students and their supervisors in a rotational placement model, found that the longer the amount of time they spent with each other the greater the trust between them (Vassos et al., 2017). On the other hand, being in a FT could restrict networking and socialisation to a smaller group of people as contact with other teams’ members could be reduced however it is not known how this could affect informal learning.
Understanding how informal learning takes place within FT and NFT may allow optimisation of learning within each and perhaps even configure teams to enhance learning and thus ultimately improve performance. Our study aimed to fill this gap in the literature by exploring how fixed clinical teams affected the experience of informal learning for Emergency Medicine (EM) Residents. By doing so we hope to understand how informal learning can be supported via the appropriate implementation of team systems especially where high performance is expected from the teams.
II. METHODS
To study how being in fixed clinical teams affected the experience of informal learning for EM Residents we conducted an exploratory qualitative study based on a constructivism research paradigm using content analysis of individual interviews. This is because informal learning could not be quantified with specific learning outcomes.
A. Setting
EDs teams manage a large number of critically ill patients who may need time sensitive interventions. These teams would comprise of experienced Emergency Physicians (EPs) and more junior Medical Officers (MOs) and Residents. The Residents are postgraduate doctors who are training to graduate as EPs; therefore, informal workplace learning is a crucial part of their training. Hence the residents would be good study subjects to investigate the effect of team systems on informal learning.
The Singapore General Hospital (SGH) ED functioned via NFTs where the composition and number of members in the team differed with each 8 hour shifts accordingly to the anticipated patient load. The COVID-19 pandemic provided a naturalistic setting where the effect of a FT system can be compared to a NFT system which had existed before hand. After COVID-19 was declared a pandemic by the World Health Organisation (WHO) on the 11th March 2020 (World Health Organisation, 2020). There was an emphasis on infection control to contain the pandemic. Many countries had instituted social distancing measures which included curfew-like measures and travel restrictions (Lake, 2020). Similarly, the Singapore government had instituted legislative measures to limit face-to-face interactions. In the ED of SGH, measures were put in place to limit the spread of COVID-19.
Thus, from 8th February till 27th September 2020, as part of infection control measures, doctors were organised into 5 FTs, each having between 5-7 Consultants, 3-5 EM Senior Residents, 2-3 EM Junior Residents and 7-9 non-EM Medical Officers (MO) (Liu et al., 2020; Quah et al., 2020). The Senior Emergency Physicians (SEPs) consisted of certified specialists in EM (Associate Consultants, Consultants and Senior Consultants); they played supervisory and educational roles to the junior doctors (JD) which included MOs, Junior Residents and Senior Residents. Each FT worked 12-hour shifts. Interactions between teams were kept to a minimum and members from different teams were not allowed to mingle. Thus, the residents were only supervised by their team’s SEPs. Informal learning would now occur within these FTs.
Formal learning was converted to a remote online platform because of infection control measures. Lectures and tutorials were held and recorded using software which enabled online asynchronous access e.g. Zoom (Zoom, 2016) as not all residents could be given protected learning time together. Sessions which could not be transferred onto an online platform (e.g. hands on simulation and procedure skills training) were cancelled. Formal summative examinations were also cancelled.
B. Interviews
Interviews were conducted and recorded via Zoom (Zoom, 2016) to maintain social distancing. The primary investigator performed 11 interviews and a coinvestigator performed the remaining 4 out of a total of 15 interviews. A semi-structured iterative interview guide was developed based on Eraut’s typology on informal learning which included team activities, tasks and enabling/disabling factors (Eraut, 2010) was used, and the interviews were audio-recorded and transcribed verbatim and anonymised. The interviews allowed positive and negative aspects to be explored and being semi structured the questions asked varied according to the interviewees’ responses. This helped to focus the interviewees to what informal learning was with examples when it could occur within team activities. The guide was iteratively amended with each interview to enhance clarity which helped to obtain more in-depth data in later interviews.
C. Participants
Twenty-four ED residents were working in the FT system in the ED of SGH during COVID-19. Fifteen were Junior Residents and 9 were Senior Residents. Purposive sampling was carried out with at least two Residents from each team being sampled. This is to ensure that there was good representation for all of the fixed clinical teams. All 24 residents were invited to participate via email and WhatsApp messaging platform with written consent being obtained. Fifteen individual interviews were conducted before data sufficiency was achieved where no new data would change the outcome of the study, thus no further interviews were conducted beyond data sufficiency (Varpio et al., 2017). Eleven interviewees were Junior Residents (4 females and 7 males) and 4 were Senior Residents (3 females and 1 male).
D. Data Analysis
Data analysis was performed via template analysis by the primary and coinvestigator independently (Brooks et al., 2015). Eraut’s typology developed from his research on informal learning was used as a priori themes in the initial coding template (Eraut, 2010). Coding template modifications were made as the analysis of the transcripts continued. Themes were categorised into hierarchical clusters and relationships between them were studied and defined. After final modifications, the coding template was applied to the entire data set. Coding themes were compared and discussed between the primary investigator and the coinvestigator until consensus was reached.
E. Ethics
Waiver for approval was granted by the Singhealth Institutional Ethics Board. The primary investigator was a core faculty within the Singhealth Emergency Medicine Residency Program and although the interview was conducted among EM residents the primary investigator did not conduct the interviews when the interviewees were from the same team as the primary investigator. These were conducted by the coinvestigator. The coinvestigator was an EM Senior Resident who was not involved in the FT system. A reflexivity diary was kept, and peer debrief was done.
III. RESULTS
Three main themes emerged on how working in FTs affected informal learning amongst our participants (Figure 1). These included changes in relationship dynamics between members, effect of FT composition on informal learning of the participants and influence on motivation.
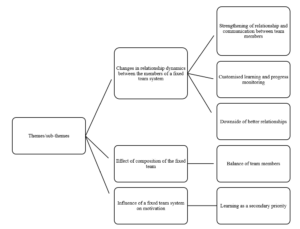
Figure 1. Themes and sub-themes
Theme 1: Changes in Relationship Dynamics between FT Members
From the interviews, the participants felt that the FT system resulted in more familiarity, trust, teamwork and improved communications between team members including SEPs, Residents and MOs. Interviewees felt that this strengthened the relationship dynamics between FT members as compared to a NFT. This meant that FT members were able to coordinate and exchange information better. It led to an increase in familiarity in knowing each member’s style of practice and way of thinking. The team members could understand each other better and how they reasoned.
The strengthened relationship between residents and SEPs changed with dynamics. Having a “closer rapport” and “deeper bond” allowed the residents to “tag along” with SEPs “more often” and gave the residents more insight as to why the SEPs behaved in a certain way as to “how they had practiced medicine” and the rationale behind each step was “more easily communicated to the residents who were tagging along” (Resident A), resulting in residents having a deeper understanding of why things were done in addition to how things were done. This strengthened relationship was also present between the residents and their peers. Therefore, peer learning improved within the FTs as junior residents reported feeling less reservation in asking each other questions.
Resident D felt that peer learning was better within FTs because of the improved relationship, there were less reservations which had prevented him from asking his peers questions in a NFT setting.
He elaborated:
“Fixed team [was] definitely better for peer learning. For the same reasons, because you know each other better, you’re more familiar. We don’t only talk to each other about work… after a while, when you go for meals together… or rather like resting together and no cases around you sit and talk. So there’s a lot more familiarity with the person you’re working with, and… you’re just more comfortable with asking questions… you don’t feel like this is somebody who’s going to judge you if [you] asked a stupid question”
This was not just amongst the residents but also with SEPs. Resident G felt that it was easier for the residents to speak to the SEPs because of familiarity and resulted in less workplace stress:
“Over the time as we knew each other better … the workplace stress was much lower… so I could… work with less stress at workplace… Because if you didn’t really know the consultant you tend to be afraid to talk to them; then of course your stress levels will be higher. But if you know that consultant and you know what kind of person, he or she is then you could be more comfortable to talk to them…”
“…It is more comfortable to… approach the senior because you know every day… we have a fixed team so naturally we feel that our relationship is closer…”
“… so, I won’t be too afraid to speak out or to talk to them to discuss with them.”
Contributing to additional ways of informal learning, communication within FTs even during work took on a more “friendly [and] social” form with greater congeniality and via more “communication platforms” (WhatsApp and Tiger Text) which continued even “outside of work” (Resident H). These platforms were also used as learning tools to facilitate case discussions, share learning points and experiences. This was not previously present in the NFTs. The residents felt that learning was more customised because of the change in relationship dynamics. In FTs, there was closer supervision of residents by SEPs. The residents “spent more time” with the same group of supervisors, thus the supervisors were able to better “assess both strengths, weaknesses and address any particular loopholes” of the residents (Resident A).
However, there were some adverse effects of this change in relationship dynamics. Some residents felt that with a closer relationship between team members, supervisors sometimes were more tolerant of the learners’ shortcomings and be less likely to point it out because of not wanting to affect the relationship. This closer relationship could result in residents taking “shortcuts” and “flying under the radar” because they knew the SEPs could tolerate or would not scrutinise the learners closely once “trust” was established (Resident L). Resident H gave an example of how familiarity could lead to less critical thinking by the learner:
“If… the senior always does like… [Rapid Sequence Intubation] … even though I question the first time I saw him do that… subsequently … every time I work with him I will do [it] this way. I won’t really think does the patient really need this way [of management] or will the patient benefit in a different way… if you are working with different bosses then every case you need to restart your thinking…”
Theme 2: Effect of Composition of the FT
All interviewees felt that the composition of the FT had affected informal learning, and that having a balanced team in terms of a wide range of years of practice amongst both the SEPs as well as the JDs would help improve informal learning. Having a team where the JDs were of differing seniorities of practice could help with peer learning because the senior ones could help the junior ones more. This also applied to the SEPs as that provided a wider perspective to clinical issues due to having different clinical experience and expertise in different subspecialties. Furthermore, if the JDs in a FT were of a similar level of practice, Resident C expressed that they could be “competing with each other for cases and procedures” which adversely affected informal learning with fewer opportunities to perform procedures. In a NFT the members would be constantly changing and it would be unlikely its JD would be always of the same level of practice.
The interviewees expressed concern that within a FT system that, although residents had close contact with a fixed group of supervisors, they lacked contact with the other teams’ SEPs. Many residents felt that this had adversely impacted informal learning because the SEPs were experts in different subspecialties (e.g., Trauma, Toxicology, Ultrasound, etc). By not interacting with many SEPs, residents were unable to learn from them. Furthermore, different supervisors had different perspectives and approaches to patients which the residents may not be exposed to if they were not in the same team as these seniors. However, this was mitigated by having a team with a balanced variation in the areas of specialty of the seniors. Resident F summarised this:
“…a team with… people from different seniorities are essential… (even) juniors can teach seniors… the way that my team was composed… it was a good mix… there are people from different… specialties… from different seniorities even within the juniors … like first posting to… [senior post graduate years]… offers different perspectives, learning of different things… people from different [subspecialties] can offer insight into the systems-based learning or component from other parts of the institution…”
Theme 3: Influence of a FT System on Motivation
Many residents felt that having FTs increased their motivation to learn. This resulted from their supervisors being able to inspire them and follow up with their learning progress more closely. Resident M was motivated to learn because his “friends (FT members) were very motivating” and “enthusiastic”; this encouraged him to learn more. Furthermore, resident C felt more motivated to learn in a FT because he “always sees the same senior” and this more frequent contact results in him being “more likely to take their feedback and opinion more seriously and work harder”
However, “after some time everyone is comfortable with each other” and some participants feared that their motivation “might go down” (Resident N). This was because there was a feeling of complacency as time went on within a FT, hence the motivation to learn started to dwindle after an initial increase.
Other reasons for this decline were related to COVID-19, the focus was more on facing the threat rather than learning and the priority to learn was secondary. The motivation to learn “was a bit less” as “the mood was more to survive than to learn”; Resident L was “less driven to learn” because there was a “general bleakness in the whole situation of [COVID-19] which made his “inner desire to learn… wane a bit”
IV. DISCUSSION
This study explored how working in fixed clinical teams affected informal learning for EM Residents. There are many pros and cons to fixed team rostering however the focus of this study is on informal learning. The findings highlighted the importance of having a balanced team composition where team members were able to establish trust and a strong bidirectional relationship because of the longer time spent working together. Motivation to learn increased initially; however after some time, some felt a decrease. This was consistent with prior work which highlighted team dynamics and commitment and that feedback which was given often and in a socially interactive environment were factors which helped to enable effective work-based learning (Attenborough et al., 2019; Jeong et al., 2018; Kyndt et al., 2016). Unlike in Attenborough’s work where team leadership was one of the factors identified; our respondents did not mention the effect of team leadership on informal learning. Their focus was more on the relationships between the different team members. From this study the predominant factors which positively affected informal learning included teamwork, collaborative task performance, where good communication was needed between different people, and personal development especially in building interpersonal relationships and group decision making.
Limited studies were done on how FTs affect informal learning. Our study found that FTs resulted in more (informal) communication channels (e.g. WhatsApp) being formed which was not present in NFTs, resulting in more learning activities including sharing ideas, resources and experiences. These sharing activities were some of the major forms of informal learning activities identified in the literature (Lohman, 2006). FTs resulted in open communication and quality feedback which was well received, and were found to be beneficial towards informal learning (Jeong et al., 2018). Our study showed that working in a FTs led to more customised learning. Findings of improved communications and strengthened relationships in a bidirectional manner involving teacher and learner alike, supports a shift from a predominantly teacher to learner type of dynamics to a team learning dynamics where all team members can learn with and from one another. This is important because informal learning takes place effectively when learning from past mistakes and feedback exchange occurs, involving both cognitive and social interactions (Jeong et al., 2018).
FTs had negative effects on informal learning as well. Familiarity resulted in supervisors being more tolerant of shortcomings and FTs limited learners’ contact with other teams’ supervisors and adversely affected informal learning. This was because informal learning also takes place when there is sharing of ideas, expertise and experience (Lohman, 2006) and limiting the number of supervisors limits the variance of shared viewpoints.
Our study has limitations. Firstly, interviewee recall bias was possible because 6 months had passed after the FT system was stopped before the interviews. Therefore, some details may not have been accurately recalled given this period which could affect the trustworthiness of results. Secondly, the participants were likely to be comparing their experiences in the FT system during COVID-19 to a NFT system without a pandemic. Thus, some of the experienced changes may be because of the pandemic rather than purely due to the FT system. Thirdly, there are many pros and cons to FTs however the focus of this study is on informal learning thus other factors not investigated with this study may affect the feasibility of FT. Lastly there could be power differential effects between the interviewers and the interviewees because the interviewers performed supervisory and roles to the residents. However, to mitigate this, a reflexivity diary was kept, and peer debrief between the two interviewers was performed. Furthermore, the interviewers did not interview members who had been in the same team as them.
V. CONCLUSION
In conclusion, FTs impact informal learning by building strong relationships with improved team communications and adding a social dimension for learning. A balance of team members as well as rotating the residents across different FTs may be beneficial for improving informal learning for EM Residents.
Notes on Contributors
Dr Wee Choon Peng Jeremy submitted the CIRB application, (with the help of the last author) conceptualised the study and its design. He performed the literature review, recruited and interviewed the participants, collected and transcribed the data, performed the thematic analysis of the data and wrote the manuscript.
Dr Ng Mingwei helped to recruit and interview some of the participants, transcribed and collected the data. Dr Ng helped perform the thematic analysis of the data and helped edit the manuscript.
Prof. Dr. Pim Teunissen was central to the conceptualisation of the study, advised on the design of the study and gave critical feedback to the writing of the manuscript and edited the manuscript extensively
All the authors have read and approved the final manuscript.
Ethical Approval
We have included the letter for waiver of CIRB via email. Ethics approval for waiver of written informed consent was obtained from the Singhealth Institutional Review Board (CIRB Ref: 2020/3114).
Data Availability
As the data set is qualitative in nature, we are not able to upload that in any public repository.
Funding
There is no funding for this paper/study.
Declaration of Interest
The authors report there are no competing interests to declare.
References
Attenborough, J., Abbott, S., Brook, J., & Knight, R. A. (2019). Everywhere and nowhere: Work-based learning in healthcare education. Nurse Education in Practice, 36, 132-138. https://doi.org/10.1016/j.nepr.2019.03.004
Barker, J. M., Clothier, C. C., Woody, J. R., McKinney, E. H., Jr., & Brown, J. L. (1996). Crew resource management: A simulator study comparing fixed versus formed aircrews. Aviation, Space, and Environmental Medicine, 67(1), 3-7.
Billett, S. (2007). Constituting the workplace curriculum. Journal of Curriculum Studies, 38(1), 31-48. https://doi.org/10.1080/00220270500153781
Brooks, J., McCluskey, S., Turley, E., & King, N. (2015). The utility of template analysis in qualitative psychology research. Qualitative Research in Psychology, 12(2), 202-222. https://doi.org/10.1080/14780887.2014.955224
Burke, L. A., & Hutchins, H. M. (2016). Training transfer: An integrative literature review. Human Resource Development Review, 6(3), 263-296. https://doi.org/10.1177/1534484307303035
Callanan, M., Cervantes, C., & Loomis, M. (2011). Informal learning. Wiley Interdisciplinary Reviews Cognitive Science, 2(6), 646-655. https://doi.org/10.1002/wcs.143
Eddy, K., Jordan, Z., & Stephenson, M. (2016). Health professionals’ experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. JBI Database of Systematic Reviews Implementation Reports, 14(4), 96-137. https://doi.org/10.11124/JBISRIR-2016-1843
Eraut, M. (2010). Informal learning in the workplace. Studies in continuing education, 26(2), 247-273. https://doi.org/10.1080/158037042000225245
Gjeraa, K., Spanager, L., Konge, L., Petersen, R. H., & Ostergaard, D. (2016). Non-technical skills in minimally invasive surgery teams: A systematic review, Surgical Endoscopy, 30(12), 5185-5199. https://doi.org/10.1007/s00464-016-4890-1
Jeong, S., Han, S. J., Lee, J., Sunalai, S., & Yoon, S. W. (2018). Integrative literature review on informal learning: Antecedents, conceptualizations, and future directions. Human Resource Development Review, 17(2), 128-152. https://doi.org/10.1177/1534484318772242
Kyndt, E., & Baert, H. (2013). Antecedents of employees’ involvement in work-related learning. Review of Educational Research, 83(2), 273-313. https://doi.org/10.3102/0034654313478021
Kyndt, E., Vermeire, E., & Cabus, S. (2016). Informal workplace learning among nurses. Journal of Workplace Learning, 28(7), 435-450. https://doi.org/10.1108/JWL-06-2015-0052
Lake, M. A. (2020). What we know so far: COVID-19 current clinical knowledge and research. Clinical Medicine, 20(2), 124-127. https://doi.org/10.7861/clinmed.2019-coron
Liu, Z., Teo, T. L., Lim, M. J., Nadarajan, G. D., Segaram, S. S. C., Thangarajoo, S., Wee, L. E., Wee, J. C. P., & Tan, K. B. K. (2020). Dynamic emergency department response to the evolving COVID-19 pandemic: The experience of a tertiary hospital in Singapore. Journal of the American College of Emergency Physicians Open, 1(6),1395-1403. https://doi.org/10.1002/emp2.12264
Lohman, M. C. (2006). Factors influencing teachers’ engagement in informal learning activities. Journal of Workplace Learning, 18(3), 141-156. https://doi.org/10.1108/13665620610654577
Quah, L. J. J., Tan, B. K. K., Fua, T. P., Wee, C. P. J., Lim, C. S., Nadarajan, G., Zakaria, N. D., Chan, S. J., Wan, P. W., Teo, L. T., Chua, Y. Y., Wong, E., & Venkataraman, A. (2020). Reorganising the emergency department to manage the COVID-19 outbreak. International Journal of Emergency Medicine, 13(1), Article 32. https://doi.org/10.1186/s12245-020-00294-w
Rogoff, B., Callanan, M., Gutiérrez, K. D., & Erickson, F. (2016). The organization of informal learning. Review of Research in Education, 40(1), 356-401. https://doi.org/10.3102/0091732×16680994
Stepaniak, P. S., Heij, C., Buise, M. P., Mannaerts, G. H., Smulders, J. F., & Nienhuijs, S. W. (2012). Bariatric surgery with operating room teams that stayed fixed during the day: A multicenter study analyzing the effects on patient outcomes, teamwork and safety climate, and procedure duration. Anesthesia and Analgesia, 115(6), 1384-1392. https://doi.org/10.1213/ANE.0b013e31826c7fa6
Telio, S., Ajjawi, R., & Regehr, G. (2015). The “Educational Alliance” as a framework for reconceptualizing feedback in medical education. Academic Medicine, 90(5), 609-614. https://doi.org/10.1097/ACM.0000000000000560
Varpio, L., Ajjawi, R., Monrouxe, L. V., O’Brien, B. C., & Rees, C. E. (2017). Shedding the cobra effect: Problematising thematic emergence, triangulation, saturation and member checking. Medical Education, 51(1), 40-50. https://doi.org/10.1111/medu.13124
Vassos, S., Harms, L., & Rose, D. (2017). Supervision and social work students: Relationships in a team-based rotation placement model. Social Work Education, 37(3), 328-341. https://doi.org/10.1080/02615479.2017.1406466
Watkins, K. E., Marsick, V. J., Wofford, M. G., & Ellinger, A. D. (2018). The evolving Marsick and Watkins (1990) theory of informal and incidental learning. New Directions for Adult and Continuing Education, 2018(159), 21-36. https://doi.org/10.1002/ace.20285
World Health Organisation. (2020). World Health Organisation emergencies press conference on coronavirus disease outbreak – 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
Zoom. (2016). Security guide. Zoom Video Communications Inc.
*Wee Choon Peng Jeremy
Outram Road,
Singapore 169608
Email: jeremy.wee.c.p@singhealth.com.sg
Submitted: 26 November 2021
Accepted: 21 July 2022
Published online: 3 January, TAPS 2023, 8(1), 33-42
https://doi.org/10.29060/TAPS.2023-8-1/OA2712
Jaime Maria Tan1, Junaidah Binte Badron1 & Sashikumar Ganapathy1,2
1Department of Emergency Medicine, KK Women’s & Children’s Hospital, Singapore; 2Duke-NUS Medical School, Singapore
Abstract
Introduction: Perceptions towards the working and learning environment as well as coping mechanisms have been studied across different healthcare sectors. They have shown to reduce stress and burnout. However, perceptions of the work environment in the Emergency Department (ED) setting have not been studied in depth. The literature surrounding coping mechanisms also mostly focuses on their impacts rather than the mechanisms utilised. In addition, these were often investigated using surveys. This study aimed to use a phenomenological approach to explore the perceptions and coping strategies of junior doctors working in a paediatric ED.
Methods: Sixteen junior doctors working in the Paediatric ED were recruited. Semi-structured interviews were conducted after conducting literature reviews. Data was collected until saturation point. All interviews were recorded and transcribed verbatim manually and subsequently analysed.
Results: The greatest fears of junior doctors starting their paediatric emergency posting were lack of knowledge due to inexperience in the subspecialty; fear of the work environment due to unfamiliarity as well as workload and the intrinsic high-stress environment. The main coping strategies were ensuring clinical safety, obtaining psychosocial support from loved ones and colleagues, and placing focus on spirituality and wellbeing.
Conclusion: In this study, the perceptions and coping strategies of the junior doctors in the Paediatric ED were explored. The findings from this study will help to structure and improve the support given to future junior doctors who rotate to the department as well as better orientate them to allay their pre-conceived notions.
Keywords: Coping Behaviours, Perceptions, Paediatric Emergency Department, Stressors, Interviews
Practice Highlights
- Participants worried about knowledge, workload and responsibilities prior to starting their posting.
- Perceptions were mostly of an anticipatory nature, influenced by seniors’ past experiences.
- In work, support from senior staff was helpful in allaying their fears and increasing patient safety.
- Participants felt psychosocial support, spirituality and wellness were useful coping strategies.
- Maladpative coping strategies did not come up as a main theme in our study.
I. INTRODUCTION
Perceptions toward the work and learning environment can strongly impact experiences and even lead to large amounts of stress (Chan et al., 2016). A poorer perception of the learning environment is also associated with greater levels of burnout (Chew et al., 2019; Sum et al., 2019). Conversely, a positive perception of the work environment helps to alleviate stress (Abraham et al., 2018). Workers’ perception of their work environment contributes significantly to their overall experiences.
Main factors contributing to stress in the ED include heavy workload and critically ill patients. Workplace violence, trauma, abuse and morbidity also add to the stress and burnout experienced (Burbeck et al., 2002; Copeland & Henry, 2018; Healy & Tyrrell, 2011; Xu et al., 2019). In the paediatric setting, added stressors include dealing with sexual abuse and non-accidental injury as well as death and the inability to provide optimal care for children (Alomari et al., 2021; Basu et al., 2016; Durand et al., 2019; Greenslade et al., 2019; Shanafelt et al., 2012; Watson et al., 2019).
Given these significant stressors, individuals utilise different coping mechanisms to mediate these experiences (Howlett et al., 2015).
Some coping strategies discussed in previous studies include socialising with friends and family (Gribben et al., 2019). Focusing on physical wellbeing, clinical variety, reflectivity, and organizational activities were also helpful in alleviating burnout in other areas of healthcare (Barham et al., 2019; Koh et al., 2015).
Several studies also found that the use of maladaptive coping mechanisms, such as alcohol use and self-blame increased with the frequency of burnout (Jackson et al., 2016; Oreskovich et al., 2015; Ryali et al., 2018; Talih et al., 2018).
While many studies studied stressors and the effectiveness of the coping mechanisms used, the actual components of coping mechanisms were not well studied. In studies that did look at coping mechanisms and their effectiveness, these studies were also often done via the survey method and were only evaluated on the surface.
Most studies looked at healthcare workers in general. Few studies looked solely at the doctor population. This makes conclusively evaluating the doctor component of coping mechanisms and their effects difficult.
While other studies looked at an adult emergency perspective, there were also few studies looking at the paediatric ED. It has been reported that dealing with paediatric emergencies causes more stress compared to their adult equivalents. Some of the contributing factors are related to the nature of working with children. These, in itself, are unmodifiable (Guise et al., 2017). Therefore, it is important to study how the paediatric context can affect the experiences of the doctors who care for them.
In our study, we studied the perceptions of junior doctors at the beginning of their posting. We subsequently explored their coping mechanisms in the Singaporean context.
The element of stress in the ED among junior doctors is significant as the ED is often part of many specialist training pathways (Mason et al., 2015). During the time of training, the doctors are still learning and developing. Hence, many doctors experience sharp learning curves during their postings. This brings about more stress (McPherson et al., 2003). In some cases, the stress can even lead to doctors thinking about leaving clinical practice altogether (Degen et al., 2014).
In the Singaporean context, paediatric emergency postings are part and parcel of speciality training for junior doctors (especially for those in emergency medicine and family medicine training). Because of this, junior doctors spend the majority of their paediatric postings in the paediatric emergency. As such, a Singapore-specific context would give light on the challenges of this sizable group.
The nature of the healthcare system in Singapore is unique. Up to 60% of the consultations in the paediatric ED were for nonurgent conditions due to the overall perception of the severity of symptoms and parental preference towards paediatric specialist facilities (Ganapathy et al., 2015). This would lead to an increased workload for the paediatric ED. The distribution in workload may also differ compared to a global perspective, with the load of severe paediatric trauma in Singapore being low (Pek et al., 2019).
These subtleties in the paediatric ED in Singapore can influence the experiences of junior doctors differently. With these key differences in mind, we aimed to investigate the perceptions of junior doctors towards their paediatric ED posting in Singapore and how they subsequently coped with the challenges faced.
II. METHODS
A. Design
In this study, we examined the experiences of doctors in their paediatric ED rotation and how their thoughts and actions influenced their stress during their rotation. We deemed the phenomenological approach to be the most appropriate for this study. Phenomenology is defined as the study of how individuals see and experience a phenomenon and what this means to the individuals in their own experience (Neubauer et al., 2019; Smith, 2021).
The approach we chose was that of an interpretive phenomenological analysis in which we aimed to investigate the experience through the participants’ own experiences and perceptions. With the help of the various participants’ accounts, themes and ideas bound by their experiences were explored (Tuffour, 2017).
B. Methods
The members of the study performed a preliminary literature review on the topic and explored plausible methods of data collection. The study team decided on semi-structured interviews as it promotes sharing and would allow for sufficient privacy.
The team members included a senior consultant, a staff physician and a medical officer. Together, after discussions about concepts that the team was keen to explore, an interview guide was drawn up.
Subsequently, a proposal was submitted to the Hospital Centralised Institutional Review Board for approval.
One-on-one interviews were conducted with the participants by investigator A, a medical officer who was rotating within the department at the time of the study. This was done to reduce the power differential. Interviews were conducted at a location and time convenient to the participant.
Prior to the interviews, consent was sought and all interviews were recorded and subsequently transcribed verbatim. The interviews were conducted over a 1-month period in December 2019.
Questions were open-ended and allowed participants to share ideas that they were keen to raise with no restrictions to the topics brought up. Interview questions were tweaked alongside subsequent interviews so that they were easier to understand and would encourage sharing. Additional questioning in subsequent interviews was adopted to improve clarity. For example, one of the questions that featured early in the interviews was ‘What are some of the coping mechanisms you use?’ During subsequent interviews we noticed some participants utilised coping mechanisms before work to prepare themselves, some used other strategies during work to cope with the stress, while others dealt with their stressors after getting off work. We tweaked the question to include ‘during the shift or outside of the shift’ to help participants widen their perspective about certain coping methods they may have used but were not immediately conscious of when answering the questions. No new questions referring to particular themes were inserted although interviewers were aware of the themes that had been highlighted in previous interviews. This was done in addition to the initial interview guide and ensured the broad nature of questioning was not compromised and the breadth of interviews was maintained.
Themes were identified from the interviews until data saturation was reached. Data saturation was noted at the 12th interview. The team continued to learn from subsequent interviews, with interviews contributing additional depth to the issues explored. Further interviews were conducted to confirm that no new theme was being identified.
The interviews were then transcribed and de-identified. They were subsequently reviewed by 2 reviewers (Investigator A and Investigator B). Data was analysed using a step-by-step thematic analysis method (Braun & Clarke, 2006). Investigators A and B independently analysed the transcripts, identified themes and later reported the common themes. These themes were discussed for concurrence. When any differences in opinion arose, these would be reviewed by investigator C to resolve any disagreement.
C. Setting
The research was conducted within the Paediatric ED in KK Women’s and Children’s Hospital, a tertiary paediatric hospital.
The Children’s Emergency of KK Women’s and Children’s Hospital is the largest paediatric emergency unit in Singapore. During the time of the interviews, the department treated over 400 patients daily. The Children’s Emergency sees all children under the age of 18 years for all medical complaints.
The department is staffed by over 60 junior doctors at a single time. These junior doctors come from various backgrounds and pass through the department for varying amounts of time. Thus, their experience can be very heterogeneous.
The job scope and responsibilities of all the junior doctors are primarily the same despite the different levels of experience. They are expected to treat the patients that present to the ED. These doctors can seek advice from the senior doctors who are on the ground. However, for the majority of the time, they would be tasked to treat patients on their own.
D. Participants
Participants were recruited through an email that was circulated to all junior doctors in the department. Participation in the study was voluntary and participants were not remunerated.
A total of 16 junior doctors were recruited and interviewed over a 1-month period. Due to the busyness of the ED and the limited time frame in which the interviews were conducted, only 16 interviews were conducted. Convenience sampling was chosen for the sampling method. The first 16 volunteers who had volunteered were interviewed. However, it was noted that saturation point was reached prior to the conclusion of the interview process.
The variety within the ED was well represented. The details of participant breakdown are elaborated on in Table 1.
|
Experience & Training Information |
|
|
|
|
|
Mean post-graduate year, 3.6 (2-6)* |
|
|
|
|
|
|
Emergency Medicine |
Family Medicine |
Paediatric Medicine |
Not in a training program at time of study |
|
Training Program (n=16) |
5 |
2 |
1 |
8 |
|
Epidemiological Data |
|
|
|
|
|
|
Chinese |
|
Indian |
|
|
Race (n=16) |
13 |
|
3 |
|
|
|
Male |
|
Female |
|
|
Gender (n=16) |
6 |
|
10 |
|
Table 1: Characteristics of Participants
*Mean (Range)
E. Analysis
All transcripts were reviewed by JT and SG. Coding was done manually using Microsoft Word. During the process, themes were identified and substantiating quotes were recorded. Iterative data analysis was done so that interviewers were aware of themes that were previously mentioned. However, the themes were not specifically explored unless brought up by the subsequent interviews.
III. RESULTS
Through the interviews, we collected information about the experiences within the ED. Interview transcripts collected as a part of this study are openly available on Figshare at http://doi.org./10.6084/m9.figshare.19204761 (Tan et al., 2022). From the interviews conducted, the experience was divided into the initial perceptions and coping mechanisms.
A. Perceptions
The perceptions of the paediatric emergency rotation in the ED were largely contributed by the experiences of the individuals who had previously worked in the department. This was achieved through consultation with friends or colleagues prior to starting the posting to find out more about the rotation.
“Before I started doing the posting, I asked some people who have done or were currently doing the posting…to find out what I was getting myself into”
(P7)
The broad themes elicited about the perceptions and inherent worries of the incoming medical officers were that of being unprepared due to ‘inadequate knowledge’ or ‘unfamiliarity’, as well as the impending ‘work load’ and ‘work factors’.
1) Fear of subject matter: Participants who were not familiar with the paediatric content were worried about their competency and adequacy in treating children. Oftentimes, participants cited that exposure to the paediatric subject matter may have been inadequate or dated and as a result, resulted in fears of being unprepared or being unsafe.
“I’ve not done any paediatric postings before as a doctor so that was a bit worrying.”
(P4)
“I’ve never dealt with paediatrics before so it was quite scary to come onto the posting”
(P14)
In participants who did however have some background in paediatrics, additional fears of specialised emergency knowledge also emerged with participants feeling nervous about the posting.
“Some of the things included technical skills such as doing back slabs, manipulation and reduction, and I guess managing trauma and more complicated acute conditions such as diabetic ketoacidosis and haemophilia and oncological and metabolic related conditions.”
(P11)
“When I started I learnt about resuscitation cases which I felt was a bit nerve-wracking to start with”
(P12)
2) Unfamiliarity: Even though participants may have been at different time points in their careers during the posting, they were all expected to perform mostly the same duties and responsibilities. As a result, a section of the participants cited worries about adjusting to the roles and environment that they may have been new to. These included concerns about being new to the system used. These added to the worries that participants often had about starting a new posting and made participants even more fearful.
“Coming from the UK, this was my first job in Singapore as a MO and thus had close to 0 experience of working in Singapore”
(P8)
“I was also not very familiar with the system. It added to the fear and unpreparedness before starting the posting.”
(P9)
3) Work factors: As a place with high turnover and workload, the picture painted to many of the participants was that it may be difficult to cope with the high workload. This would result in participants being overloaded and overwhelmed. A level of uncertainty was also described. Many participants were left feeling fearful, apprehensive and unsure of what to expect during the upcoming posting. Some were also worried about the expectations they may have to live up to and the nature of the environment being extremely stressful.
“I just heard that it can be quite busy with many patients and at the beginning, it can feel a bit of a throw into the deep end as we often don’t know what to expect and the learning curve can be quite steep”
(P12)
“I was also a bit apprehensive as I heard how busy the posting could get”
(P10)
“It’s quite a stressful working environment because the seniors have a certain working expectation and if you can’t live up to the expectations.”
(P16)
Practically, participants were also worried about the potential to get sufficient rest. Many participants heard that manpower may be tight and would result in having fewer or insufficient off days and would run the risk of feeling tired and burnt out.
“I heard that it was also difficult to get leave that you want and that you would also be really tired during the posting”
(P13)
B. Coping Mechanisms
We then explored the different ways the participants utilised to cope with their experiences in the ED. Participants used a variety of means that we broadly classified into broad themes of ensuring clinical safety, psychosocial support and spirituality.
1) Clinical safety: Participants were inevitably worried about competency and had inherent fears of patient safety in their practice. Coping strategies in this realm could be divided into preparation, senior supervision and collegial opinion.
Preparation was often seen in speaking to doctors who had previously rotated through the posting to allow junior doctors to prepare themselves mentally.
“I asked around and tried to mentally prepare myself for what people told me to expect”
(P3)
In addition, the perceived knowledge gaps and lack of experience were dealt with by many participants through studying and reading up to cover these gaps as well as to prevent them from feeling out of depth.
“I had actually read the guidelines prior especially for the things that I was not familiar with.”
(P10)
On the ground, participants found the availability and approachability of help and support from senior colleagues helpful in easing the worry and anxiety experienced in the emergency department. This also helped participants feel more safe and secure in their practices in the emergency department.
“I appreciate the nice seniors. Most of the seniors are approachable and they treat us like fellow colleagues. They respect our opinions and try to keep it in mind”
(P10)
“I feel very safe at work and very well supported by the seniors. In general, it is easy to ask for help from most of the seniors.”
(P8)
In addition, many participants also felt that their fellow medical officer colleagues were also important in ensuring safety in their practice. With different levels of experience, they could bounce ideas off each other and get a second opinion from their peers. Furthermore, their colleagues also helped to pick up the workload when they felt overwhelmed.
“Everyone is willing to help out when you get stuck. Help is useful and it is easy to come by”
(P1)
“I feel like I have a good relationship with them (peers) and that helps me and I can also get second opinions from them if I’m unsure.”
(P9)
2) Psychosocial support: In the high-strung environment of the emergency department, there is a lot of stress and emotions that come with the job. We found that many participants shared about the social component involved in unpacking these emotions and relieving their stress. The components of the collegial environment and support from loved ones appeared to be crucial coping mechanisms that helped participants.
The work climate was cited to be collegial and relationships between co-colleagues were described as friendly. Many participants felt comfortable with their co-colleagues such that they could ventilate their emotions and experiences with one another. These helped participants process and debrief their experiences.
“We generally laugh about the situation together and it gets better. Sometimes they give advice based on what they have seen and how to avoid such circumstances and we try and help each other.”
(P7)
“It’s useful amongst colleagues because we go through the same things and we get to exchange ideas and I feel we get to debrief this way as well. That helps because we don’t feel like we go through it alone because we have similar experiences.”
(P8)
Apart from the work environment, supportive loved ones and close friends also helped participants cope with difficult days. Participants cited that out of work encounters helped them to get through tough days and relieve their stress.
“Sometimes I also talk about it with someone. Usually that helps and my stress doesn’t usually last beyond the same day.”
(P6)
“I guess these 3 things, my family, friends and colleagues help me with tough days.”
(P7)
3) Spirituality and wellness: Spirituality and wellbeing were also important in dealing with the experiences and stressors the participants faced. Apart from dealing with the clinical stressors and unpacking the experiences with others, participants also spoke about coming to terms with their experiences and emotions on their own. This involved components of religion and reflexivity. Participants also spoke about the role of maintaining their wellbeing with leisure and self-care activities.
Participants spoke about reflecting and reviewing the good as well as the bad moments at work. These helped the participants make sense of their experiences and as a result, helped them improve and learn.
“I usually pray and reflect on my day and think about what are the good points I can get out of the day.”
(P9)
Religion also featured as a means of coping with emotions in the sometimes chaotic environment seen in the ED. These helped participants work better and feel more focused at work.
“I feel like I’m stable when I pray … and I think more thoughts are more ordered. That helps me.”
(P15)
Focusing on physical wellbeing also helped to reduce the stress experienced. Participants cited different activities – food, sleep, exercise, self-care and hobbies that helped them take their minds off work and help them get rejuvenated before the next working day.
“Eating and relaxing help me after a tough day”
(P4)
“I find exercising is helpful, and it helps me feel fresher and less sleepy”
(P3)
“Listening to music and watching videos and just going about non-work related normal daily life.”
(P11)
“I ensure that I have a good work-life balance… I go for a massage, go for a buffet, watch a movie and enjoy myself.”
(P13)
“I draw, I paint. I learn languages. Sometimes I travel. These things help me relax and cope with stress.”
(P16)
IV. DISCUSSION
We sought to understand the perceptions of junior doctors starting out in the emergency department as well as the subsequent coping strategies they undertook for challenges that they faced. During the process, we interviewed sixteen junior doctors who spoke in detail about their experiences.
The perceptions that the junior doctors in our study described consisted mainly of their worries and concerns prior to the start of the posting. Most of the perceptions and worries were centred on knowledge, workload and responsibilities that came with the posting.
A large proportion of participants expressed worry regarding competency and personal comfort levels in managing children. As the ED is a broad one and knowledge is inexhaustible, the concerns in lack of competency are seen in the other elements of emergency care and not strictly paediatric emergency (Jelinek et al., 2013; Kennelly et al., 2012; Yong & Ng, 2016).
Many of the worries described by the participants were of an anticipatory nature, from hearing their predecessors’ experiences. Anticipation of negative experiences can lead to anxiety and stress in individuals (Carlson et al., 2010; Grupe & Nitschke, 2013). Participants had anxiety about the workload and certain work factors prior to the start of the posting. While predecessors’ recounts are helpful in preparing doctors for their upcoming experience, the anxiety that comes with this preparation may not be. Positive effects can also be seen when a positive picture is painted of the upcoming experience (Gangwal et al., 2014; Luo et al., 2018). As it is difficult to balance the negative anxiety and the positive effects of preparation, it may be helpful for junior doctors to receive a formal handover from existing doctors who themselves have had a positive experience so as to prevent excessive anxiety.
We next explored the coping strategies involved to help the participants through the difficult parts of their experiences.
In areas of safety, participants commented on how the support from the senior staff helped allay their fears and increase patient safety at work. Other studies showed similar themes with HCWs expressing the desire for support, professional help and preventive action in the ED (Mikkola et al., 2019; Povedano-Jimenez et al., 2020; Ruotsalainen et al., 2015). In situations where support was provided, these corresponded to higher levels of satisfaction at work (Hunsaker et al., 2015). This is especially so in HCWs who were exposed to traumatic situations (Zhao et al., 2015).
Social support is an important factor in dealing with stressful situations (Gribben et al., 2019). In our cohort, our participants also engaged in social interactions with family, friends and colleagues in an attempt to deal with stressors in the ED. The collegial environment was also beneficial in dealing with stress and helping participants better process their experiences (Povedano-Jimenez et al., 2020).
Apart from expressing emotions and stressors, participants also sought to ensure mental and physical wellness of oneself. This was done by focusing on their spirituality as well as physical wellness and self-care. These strategies utilised were similar to those seen in other studies (Gribben et al., 2019; Hoonpongsimanont et al., 2013; McPherson et al., 2003; Palmer Kelly et al., 2020; Xu et al., 2019).
Maladaptive coping strategies did not come up as a main theme in our interviews.
A. Limitations
The study was conducted in a single ED at a single time point. Efforts were taken to diversify the population interviewed with participants experiencing different durations within the department. However, interviews of participants who had experienced the ED at different time points could have brought about different views and themes.
The primary investigator was also working within the same department during the time of the study. As the investigator was also a junior doctor during the study, a power dynamic effect was minimised.
The setting was limited to a single centre in the Singapore setting and thus, was extremely specific. Singapore is a city-state with easy access to healthcare. In addition, due to strict legislation, violence is minimal compared to other areas. As such, the patient load and patient type may differ from other ED and may raise the question of applicability in a different setting.
In addition, this study was conducted prior to the COVID-19 pandemic and the findings were representative of the climate at that time. The pandemic has led to multiple changes in workflow and work culture in the paediatric ED, and these may affect the applicability of our findings.
B. Future Research and Practical Implications
The study is the first qualitative in-depth study looking at perceptions and coping strategies in a paediatric emergency setting among junior doctors in a single centre. It is the first study to explore the individual perceptions and coping mechanisms of doctors, with a focus on the subset of junior doctors. The group was relatively small and conducted at a single time point. As such, the study can be expanded to include a larger group of participants across different time points and centres to illustrate a bigger picture.
Many of the participants also talked about the challenges they experienced in the paediatric emergency. They also raised possible improvements that could be made to help with stressors and challenges in the ED. This could be studied further and future research could focus on how we could target these factors and how effective these adjustments can be.
The findings of this research echoed the findings of prior studies. This study also sheds light and gives us more depth in terms of the early perceptions prior to the start of the postings and the coping strategies that were used.
These findings can also help future doctors rotating through the ED picture the experience. This would give doctors an opportunity to decide how best to prepare themselves. It could also help the doctors feel united with their current colleagues and predecessors in their challenges. And that they are not alone in their experiences.
V. CONCLUSION
In this study, the perceptions of junior doctors and coping strategies of junior doctors in an Asian Paediatric ED were studied. We looked at the perceptions and coping strategies utilised. Many factors were established in contributing to the experience. Improvements and suggestions to improve the experience were also brought up. Other HCWs can also understand how to best work with the junior doctors to facilitate an effective and pleasant working environment.
Notes on Contributors
Jaime Tan undertook literature reviews, conducted and analysed interviews and drafted the manuscript. Junaidah Badron reviewed the interviews and drafted and reviewed the manuscript. Sashikumar Ganapathy conceived the idea of the study, reviewed and analysed interview transcripts and advised the manuscript design. All authors have read and approved the final manuscript.
Ethical Approval
This project was submitted to the Centralised Institutional Review Board for approval (CIRB Ref 2019.2772). All participants consented to the research study.
Data Availability
All data collected in this study are openly available on Figshare repository, http://doi.org/10.6084/m9.figshare.19204761
Acknowledgement
We would like to thank all participants for volunteering their time and agreeing to participate in this study.
Funding
No funding was involved in this study.
Declaration of Interest
The authors declare that they have no conflicts of interest.
References
Abraham, L. J., Thom, O., Greenslade, J. H., Wallis, M., Johnston, A. N., Carlström, E., Mills, D., & Crilly, J. (2018). Morale, stress and coping strategies of staff working in the emergency department: A comparison of two different-sized departments. Emergency Medicine Australasia, 30(3), 375-381. https://doi.org/10.1111/1742-6723.12895
Alomari, A. H., Collison, J., Hunt, L., & Wilson, N. J. (2021). Stressors for emergency department nurses: Insights from a cross‐sectional survey. Journal of Clinical Nursing, 30(7-8), 975-985. https://doi.org10.1111/jocn.15641
Barham, D., De Beer, W., & Clark, H. (2019). The role of professional supervision for palliative care doctors in New Zealand: A quantitative survey of attitudes and experiences. The New Zealand Medical Journal, 132(1501), 10–20.
Basu, S., Yap, C., & Mason, S. (2016). Examining the sources of occupational stress in an emergency department. Occupational Medicine, 66(9), 737–742. https://doi.org/10.1093/occmed/kqw155
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
Burbeck, R., Coomber, S., Robinson, S. M., & Todd, C. (2002). Occupational stress in consultants in accident and emergency medicine: A national survey of levels of stress at work. Emergency Medicine Journal, 19(3), 234–238. https://doi.org/10.1136/emj.19.3.234
Carlson, J. M., Greenberg, T., Rubin, D., & Mujica-Parodi, L. R. (2010). Feeling anxious: Anticipatory amygdalo-insular response predicts the feeling of anxious anticipation. Social Cognitive and Affective Neuroscience, 6(1), 74–81. https://doi.org/10.1093/scan/nsq017
Chan, C. Y. W., Sum, M. Y., Lim, W. S., Chew, N. W. M., Samarasekera, D. D., & Sim, K. (2016). Adoption and correlates of Postgraduate Hospital Educational Environment Measure (PHEEM) in the evaluation of learning environments – A systematic review. Medical Teacher, 38(12), 1248–1255. https://doi.org/10.1080/0142159x.2016.1210108
Chew, Q. H., Ang, L. P., Tan, L. L., Chan, H. N., Ong, S. H., Cheng, A., Lai, Y. M., Tan, M. Y., Tor, P. C., Gwee, K. P., & Sim, K. (2019). A cross-sectional study of burnout and its associations with learning environment and learner factors among psychiatry residents within a National Psychiatry Residency Programme. BMJ Open, 9(8), e030619. https://doi.org/10.1136/bmjopen-2019-030619
Copeland, D., & Henry, M. (2018). The relationship between workplace violence, perceptions of safety, and professional quality of life among emergency department staff members in a Level 1 Trauma Centre. International Emergency Nursing, 39, 26–32. https://doi.org/10.1016/j.ienj.2018.01.006
Degen, C., Weigl, M., Glaser, J., Li, J., & Angerer, P. (2014). The impact of training and working conditions on junior doctors’ intention to leave clinical practice. BMC Medical Education, 14(1). https://doi.org/10.1186/1472-6920-14-119
Durand, A. C., Bompard, C., Sportiello, J., Michelet, P., & Gentile, S. (2019). Stress and burnout among professionals working in the emergency department in a French university hospital: Prevalence and associated factors. Work, 63(1), 57–67. https://doi.org/10.3233/wor-192908
Ganapathy, S., Lim, S. Y., Kua, J. P., & Ng, K. C. (2015). Non-urgent paediatric emergency department visits: Why are they so common? A Singapore perspective. Annals of the Academy of Medicine, Singapore, 44(7), 269–271. https://doi.org/10.47102/annals-acadmedsg.v44n7p269
Gangwal, R. R., Rameshchandra Badjatia, S., & Harish Dave, B. (2014). Effect of exposure to positive images of dentistry on dental anxiety among 7 to 12 years old children. International Journal of Clinical Pediatric Dentistry, 7(3), 176–179. https://doi.org/10.5005/jp-journals-10005-1260
Greenslade, J. H., Wallis, M., Johnston, A. N. B., Carlström, E., Wilhelms, D. B., & Crilly, J. (2019). Key occupational stressors in the ED: an international comparison. Emergency Medicine Journal, 37(2), 106–111. https://doi.org/10.1136/emermed-2018-208390
Gribben, J. L., Kase, S. M., Waldman, E. D., & Weintraub, A. S. (2019). A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in paediatric critical care physicians in the United States*. Paediatric Critical Care Medicine, 20(3), 213–222. https://doi.org/10.1097/pcc.0000000000001803
Grupe, D. W., & Nitschke, J. B. (2013). Uncertainty and anticipation in anxiety: An integrated neurobiological and psychological perspective. Nature Reviews Neuroscience, 14(7), 488–501. https://doi.org/10.1038/nrn3524
Guise, J. M., Hansen, M., O’Brien, K., Dickinson, C., Meckler, G., Engle, P., Lambert, W., & Jui, J. (2017). Emergency medical services responders’ perceptions of the effect of stress and anxiety on patient safety in the out-of-hospital emergency care of children: A qualitative study. BMJ Open, 7(2), e014057. https://doi.org/10.1136/bmjopen-2016-014057
Healy, S., & Tyrrell, M. (2011). Stress in emergency departments: Experiences of nurses and doctors. Emergency Nurse, 19(4), 31–37. https://doi.org/10.7748/en2011.07.19.4.31.c8611
Hoonpongsimanont, W., Murphy, M., Kim, C. H., Nasir, D., & Compton, S. (2013). Emergency medicine resident well-being: Stress and satisfaction. Occupational Medicine, 64(1), 45–48. https://doi.org/10.1093/occmed/kqt139
Howlett, M., Doody, K., Murray, J., LeBlanc-Duchin, D., Fraser, J., & Atkinson, P. (2015). Burnout in emergency department healthcare professionals is associated with coping style: A cross-sectional survey. Emergency Medicine Journal, 32(9), 722–727. https://doi.org/10.1136/emermed-2014-203750
Hunsaker, S., Chen, H. C., Maughan, D., & Heaston, S. (2015). Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. Journal of Nursing Scholarship, 47(2), 186–194. https://doi.org/10.1111/jnu.12122
Jackson, E. R., Shanafelt, T. D., Hasan, O., Satele, D. V., & Dyrbye, L. N. (2016). Burnout and alcohol abuse/dependence among U.S. medical students. Academic Medicine, 91(9), 1251–1256. https://doi.org/10.1097/acm.0000000000001138
Jelinek, G. A., Weiland, T. J., Mackinlay, C., Gerdtz, M., & Hill, N. (2013). Knowledge and confidence of Australian emergency department clinicians in managing patients with mental health-related presentations: Findings from a national qualitative study. International Journal of Emergency Medicine, 6, Article 2. https://doi.org/10.1186/1865-1380-6-2
Kennelly, S. P., Morley, D., Coughlan, T., Collins, R., Rochford, M., & O’Neill, D. (2012). Knowledge, skills and attitudes of doctors towards assessing cognition in older patients in the emergency department. Postgraduate Medical Journal, 89(1049), 137–141. https://doi.org/10.1136/postgradmedj-2012-131226
Koh, M. Y. H., Chong, P. H., Neo, P. S. H., Ong, Y. J., Yong, W. C., Ong, W. Y., Shen, M. L. J., & Hum, A. Y. M. (2015). Burnout, psychological morbidity and use of coping mechanisms among palliative care practitioners: A multi-centre cross-sectional study. Palliative Medicine, 29(7), 633–642. https://doi.org/10.1177/0269216315575850
Luo, Y., Chen, X., Qi, S., You, X., & Huang, X. (2018). Well-being and anticipation for future positive events: Evidences from an fMRI Study. Frontiers in Psychology, 8. https://doi.org/10.3389/fpsyg.2017.02199
Mason, S., O’Keeffe, C., Carter, A., & Stride, C. (2015). A longitudinal study of well-being, confidence and competence in junior doctors and the impact of emergency medicine placements. Emergency Medicine Journal, 33(2), 91–98. https://doi.org/10.1136/emermed-2014-204514
McPherson, S., Hale, R., Richardson, P., & Obholzer, A. (2003). Stress and coping in accident and emergency senior house officers. Emergency Medicine Journal, 20(3), 230–231. https://doi.org/10.1136/emj.20.3.230
Mikkola, R., Huhtala, H., & Paavilainen, E. (2019). Development of a coping model for work‐related fear among staff working in emergency department in Finland – Study for nursing and medical staff. Scandinavian Journal of Caring Sciences, 33(3), 651–660. https://doi.org/10.1111/scs.12658
Neubauer, B. E., Witkop, C. T., & Varpio, L. (2019). How phenomenology can help us learn from the experiences of others. Perspectives on Medical Education, 8(2), 90–97. https://doi.org/10.1007/s40037-019-0509-2
Oreskovich, M. R., Shanafelt, T., Dyrbye, L. N., Tan, L., Sotile, W., Satele, D., West, C. P., Sloan, J., & Boone, S. (2015). The prevalence of substance use disorders in American physicians. The American Journal on Addictions, 24(1), 30–38. https://doi.org/10.1111/ajad.12173
Palmer Kelly, E., Hyer, M., Payne, N., & Pawlik, T. M. (2020). A mixed-methods approach to understanding the role of religion and spirituality in healthcare provider well-being. Psychology of Religion and Spirituality, 12(4), 487–493. https://doi.org/10.1037/rel0000297
Pek, J. H., Ong, Y. K. G., Quek, E. C. S., Feng, X. Y. J., Allen, J. C., Jr., & Chong, S. L. (2019). Evaluation of the criteria for trauma activation in the paediatric emergency department. Emergency Medicine Journal, 36(9), 529–534. https://doi.org/10.1136/emermed-2018-207857
Povedano-Jimenez, M., Granados-Gamez, G., & Garcia-Caro, M. P. (2020). Work environment factors in coping with patient death among Spanish nurses: A cross-sectional survey. Revista Latino-Americana de Enfermagem, 28. https://doi.org/10.1590/1518-8345.3279.3234
Ruotsalainen, J., Verbeek, J., Mariné, A., & Serra, C. (2015). Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews, 2015(4), CD002892. https://doi.org/10.1002/14651858.cd002892.pub5
Ryali, V. S. R., Sreelatha, P., & Premlal, L. (2018). Burnout and coping strategies among residents of a private medical college in South India: A cross-sectional study. Industrial Psychiatry Journal, 27(2), 213-218. https://doi.org/10.4103/ipj.ipj_53_18
Shanafelt, T. D., Boone, S., Tan, L., Dyrbye, L. N., Sotile, W., Satele, D., West, C. P., Sloan, J., & Oreskovich, M. R. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377-1385. https://doi.org/10.1001/archinternmed.2012.3199
Smith, D. W. (2021). Stanford Encyclopaedia of Philosophy. https://plato.stanford.edu.
Sum, M. Y., Chew, Q. H., & Sim, K. (2019). Perceptions of the learning environment on the relationship between stress and burnout for residents in an ACGME-I accredited national psychiatry residency program. Journal of Graduate Medical Education, 11(4s), 85–90. https://doi.org/10.4300/jgme-d-18-00795
Talih, F., Daher, M., Daou, D., & Ajaltouni, J. (2018). Examining burnout, depression, and attitudes regarding drug use among Lebanese medical students during the 4 years of medical school. Academic Psychiatry, 42(2), 288–296. https://doi.org/10.1007/s40596-017-0879-x
Tan, M. Y., Ng, N. B. H., Aw, M. M., & Lin, J. B. (2022). Perceived stress & sentiments of housemen starting work during the COVID-19 Pandemic in Singapore. The Asia Pacific Scholar, 7(2), 56–60. https://doi.org/10.29060/taps.2022-7-2/sc2686
Tuffour, I. (2017). A critical overview of interpretative phenomenological analysis: A contemporary qualitative research approach. Journal of Healthcare Communications, 2(4). https://doi.org/10.4172/2472-1654.10009
Watson, A. G., Saggar, V., MacDowell, C., & McCoy, J. V. (2019). Self-reported modifying effects of resilience factors on perceptions of workload, patient outcomes, and burnout in physician-attendees of an international emergency medicine conference. Psychology, Health & Medicine, 24(10), 1220–1234. https://doi.org/10.1080/13548506.2019.1619785
Xu, H. G., Johnston, A. N., Greenslade, J. H., Wallis, M., Elder, E., Abraham, L., Thom, O., Carlström, E., & Crilly, J. (2019). Stressors and coping strategies of emergency department nurses and doctors: A cross-sectional study. Australasian Emergency Care, 22(3), 180–186. https://doi.org/10.1016/j.auec.2018.10.005
Yong, A. M. Y., & Ng, J. (2016). Assessing the level of knowledge of emergency department physicians in recognition of common skin lesions. Annals of Clinical and Laboratory Research, 4(1). https://doi.org/10.21767/2386-5180.100073
Zhao, S., Liu, H., Ma, H., Jiao, M., Li, Y., Hao, Y., Sun, Y., Gao, L., Hong, S., Kang, Z., Wu, Q., & Qiao, H. (2015). Coping with Workplace Violence in Healthcare Settings: Social Support and Strategies. International Journal of Environmental Research and Public Health, 12(11), 14429–14444. https://doi.org/10.3390/ijerph121114429
*Jaime Maria Tan
KK Women’s and Children’s Hospital,
100 Bukit Timah Road,
Singapore 229899
+6590303124
Email: jaime.tan@mohh.com.sg
Submitted: 19 May 2022
Accepted: 21 September 2022
Published online: 3 January, TAPS 2023, 8(1), 3-12
https://doi.org/10.29060/TAPS.2023-8-1/OA2817
Junji Haruta1,2, Ayumi Takayashiki2, Ryohei Goto2, Takami Maeno2, Sachiko Ozone2 & Tetsuhiro Maeno2
1Medical Education Center, School of Medicine, Keio University, Japan; 2Department of Primary Care and Medical Education, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan
Abstract
Introduction: The pandemic caused by the novel coronavirus (COVID-19) has produced dramatic changes in the learning environment for clinical practice in medical education, and the impact on medical students has been significant. However, few program evaluation studies involving professional identity, now emphasised in medical education, have compared current with pre-COVID-19 programs. Here, we compared the professional identity recognised by medical students in the years before and during COVID-19.
Methods: Medical students who participated in clinical practice were evaluated using the Japanese version of the Professional Self-Identity Questionnaire (PSIQ), a 9-item inventory rated using 7-point Likert scales. They answered on the first day of a 4-week clinical practice module within a community-based medical education (CBME) program and at graduation in 2018-2019 (pre-COVID-19 pandemic) and in 2019-2020 (during-COVID-19 pandemic). We compared the mean difference in total PSIQ score of the 2019-2020 students to those of the 2018-2019 students as a historical cohort using an unpaired t-test.
Results: Participants were 104 medical students in the 2018-2019 academic year and 92 in the 2019-2020 academic year. PSIQ was increased at graduation. Mean difference in total PSIQ score was statistically higher for the 2019-2020 students (13.5 ± 9.4) than for the 2018-2019 students (10.3 ± 8.1) (t =2.6, df =195, p = 0.01).
Conclusion: Although clinical practice was restricted by COVID-19, this had some positive impact on the strengthening of professional identity recognised by medical students. This finding may have been influenced by the imprinting of professional norms and changes in society.
Keywords: Novel Coronavirus Infection, Professional Identity, Clinical Practice, Questionnaire Survey, Program Evaluation
Practice Highlights
- Professional identity recognised by medical students in Japan was assessed by questionnaire.
- Changes during clinical practice were compared between two grades using a historical cohort.
- Medical students’ recognised professional identity scores improved after one year in both cohorts.
- Medical students experienced the COVID-19 pandemic showed some positive impact on professional identity.
- Medical students internalised their role as healthcare professionals owing to COVID-19 pandemic.
I. INTRODUCTION
The pandemic caused by the novel coronavirus (COVID-19) has caused unprecedented disruption to medical education systems around the world (Kaul et al., 2021; Khasawneh et al., 2020; Lucey & Johnston, 2020; Papapanou et al., 2021). In particular, the pandemic has made it difficult to continue medical educational programs, including regular lectures, and face-to-face lectures, experiments, and clinical practice involving patients (Al Samaraee, 2020; Emanuel, 2020; Shankar & Wilson, 2020). The Association of American Medical Colleges took the unprecedented decision to suspend clinical practice and issued guidance instructing medical students to avoid clinical practice involving direct patient contact (Association of American Medical Colleges, 2020). The many university hospitals in the U.S. have made it a priority to utilise students in controlling the spread of COVID-19 infection. Other countries followed this precedent. Medical students accordingly lost the opportunity to learn through patients in clinical practice. In Japan also, clinical practice was suspended at many universities.
Commonly implemented alternative teaching methods were online interactive discussions and video lectures (Chiodini, 2020; Mian & Khan, 2020). To prevent the spread of COVID-19 from medical students in clinical practice (Alsoghair et al., 2021), students were required to socially distance not only from patients but also from healthcare providers and faculty members. However, implementing the requisite changes to curricula, such as interrupting or drastically postponing clinical practice, was difficult, forcing faculties to develop curricula that provided students with opportunities to supplement their ongoing clinical practice as early as possible, while making use of online devices (Ross, 2020). These changes in the learning environment affected medical students’ learning. For example, a survey of 2nd-6th grade students at the University of Geneva found that 2/3 of the medical students experienced decreased motivation and concentration in distracting learning environments such as home, whereas some medical students who were exposed to clinical practice during the COVID-19 pandemic showed an increased sense of belonging to the profession (Wurth et al., 2022). A change in perception with remote learning in response to the COVID-19 pandemic among Canadian undergraduate students also revealed a significant decrease in students’ achievement goals, engagement, and perceptions of success, and an increase in perceptions of cheating (Daniels et al., 2021). Perceptions of learning due to changes in the curriculum due to COVID-19 have been investigated and controversially reported, but few reports have investigated professional identity as a foundation for becoming a physician.
To be effective clinicians, it is important that medical students acquire not only knowledge and skills but also professional identity formation (Cruess et al., 2014; Hafferty & Franks, 1994). Professional identity is defined as “attitudes, values, knowledge, beliefs, and skills shared with others in a professional group” (Crossley & Vivekananda-Schmidt, 2009). Professional identity formation is noted as an ongoing process influenced by several factors, including practice experience and professional socialisation (Adams et al., 2006). In this study, we adopted a theoretical framework which is based on a concept that illustrates the interplay of professional identity formation and socialisation through a complex conscious and unconscious process centered on role models, mentors, and the accumulation of individual experiences (Cruess et al., 2015). Because clinical practice is a period in which medical students meet role models and mentors and gain their first experiences as a healthcare provider, clinical practice is major contributor to the development of professional identity in medical students (Haruta et al., 2020).
Although studies have reported that medical education programs altered by the COVID-19 pandemic have affected medical students’ perceptions of the role of the physician and their learning strategies (Findyartini et al., 2020; Wurth et al., 2022), little is known about the influence of curricula changes on medical students with regard to their professional identity formation as physicians affected by role models, mentors, and individual experience (Stetson et al., 2020).
Here, we aimed to compare professional identity as a physician as perceived by medical students in clinical practice before and during COVID-19 using the Professional Self Identity Questionnaire (PSIQ).
II. METHODS
A. Setting
Japan first faced the challenge of the COVID-19 pandemic in January 2020, and a state of emergency was declared for all regions of Japan on April 16, 2020 (Prime Minister’s Office of Japan, 2020). During that time, some medical universities suspended clinical training and implemented online education instead. The COVID-19 Outline of Measures for COVID-19 formulated by the Japanese Ministry of Education, Culture, Sports, Science and Technology was sent to all higher education institutions, including medical schools, on June 5, 2020 (Hayashi et al., 2022), with the main advice that universities should operate in a resilient manner for experiential educational practices such as clinical practice. Under these circumstances, leaders of Japanese medical schools were asked to consult various stakeholders and make decisions on whether or not to continue clinical practice, often leaving detailed instructions to local operations managers in each field (Hayashi et al., 2022). In contrast, primary care physicians were forced to adapt to local conditions (Haruta et al., 2021).
Students enter medical school in Japan after graduating from high school, and the curriculum is six years long. Clinical training usually takes place in the fourth to sixth years. This schedule is also implemented at the University of Tsukuba in Japan: clinical training is divided into a first half from October of the fourth year to September of the fifth year and a second half from October of the fifth year to June of the sixth year, for a total of 78 weeks. After clinical training, medical students spend time studying for graduation and national exams, in addition to attending lectures.
The first phase of this clinical practice consists of a four-week rotation in basic departments such as internal medicine, surgery, obstetrics and gynecology, pediatrics, and emergency medicine, mainly at affiliated hospitals. The second phase incorporates some elective subjects and includes 4 weeks’ mandatory clinical practice in a CBME curriculum and a further 4 weeks’ clinical practice in a department of interest. Typically, 15 to 17 students rotate every 4 weeks through clinical practice in the CBME curriculum. This clinical training was conducted before the pandemic, but was discontinued in response to it at the end of March 2020. In March, medical students continued clinical training while all elementary and junior high schools were closed. All clinical training was then cancelled in April 2020 and replaced with report assignments only. These were replaced in May and June with online training and on-demand assignments. Sixth-year students in the class of 2020, and subsequently also in 2021 and 2022, were required to adhere to health observation recording and infection prevention behaviors in accordance with the University of Tsukuba Hospital staff behavior guidelines, which had not been previously followed. Similarly, they were also restricted from participating in training hospital tours and extracurricular activities, which were usually a part of their training.
B. Study Design
Training in clinical practice at the University of Tsukuba consists of a first phase for 4th and 5th year students and a second phase for 5th and 6th year students. CBME is included in the latter phase. Data from 5th-year medical students who participated in clinical practice in a 4-week community-based medical education (CBME) program from October 2019 to March 2020 and who graduated in March 2021 were compared to those of the previous year’s students (2018-2019) as a historical cohort. This cohort included 6th-year medical students who graduated in March 2020 and who had participated in a similar clinical practice program the previous year, from October 2018 to May 2019. As in the 2018-2019 academic year, a questionnaire was administered using the PSIQ in the 2019-2020 academic year. The PSIQ, conducted as part of program evaluation of the CBME program, was administered on the first day of the 4-week clinical practice of the program and at graduation. Study participants included 118 fifth- and sixth-year medical students who participated in clinical practice in the CBME program from October 2018 to May 2019 (pre-COVID-19 pandemic) and 100 fifth- and sixth-year medical students who participated from October 2019 to March 2020 (during-COVID-19 pandemic). The 35 participants from April-May 2020, when the 4-week clinical practice in the CBME program was switched to online practice due to COVID-19, were excluded because they could not be pre-evaluated.
C. Instrument: Japanese Version of the Professional Self Identity Questionnaire (PSIQ)
The Professional Self-Identity Questionnaire (PSIQ) is a 9-item inventory which is rated using 7-point Likert scales (Crossley & Vivekananda-Schmidt, 2009). This instrument measures the sense of students in identifying their current position on a continuum between ‘first-day student’ and ‘qualified doctor’ when engaged in each of nine domains of professional activity. These nine domains include “Teamwork,” “Communication,” “Conducting assessment,” “Cultural awareness,” “Ethical awareness,” “Using records,” “Dealing with emergencies,” “Reflection,” and “Teaching”. Each item is rated on a 7-point Likert scale. For this research, we set 1 point as “equivalent to the first day of clinical practice” and 7 points as “equivalent to the first day of initial residency”. The PSIQ is an assessment sheet form originally designed in English. The original study was validated in a sample of 496 medical students across multiple phases of education, and the overall internal reliability (Cronbach’s alpha) was reported to be 0.93 (Crossley & Vivekananda-Schmidt, 2009). Previously, we developed a Japanese version of the PSIQ and operationally defined PSIQ scores as professional identity as a physician as perceived by medical students. Cronbach’s alpha of the Japanese PSIQ was reported to be 0.93 (Haruta et al., 2021), which allows students to measure changes in their own professional identity by tracking each of the nine professional activities over time. We set the total score on this scale as the main outcome of this study. The study showed that this was a reliable and valid tool for program evaluation during clinical practice (Haruta et al., 2021).
D. Participants and Data Collection
In 2018-2019 (pre-COVID-19 pandemic) and 2019-2020 (during-COVID-19 pandemic), we assessed the professional identity of medical students from October of their fifth year to May of the sixth year using PSIQ. The survey was administered on the first day of clinical practice in the CBME program as PSIQ 1 (September 2018 to May 2019 and September 2019 to March 2020) and at graduation as PSIQ 2 (2020 January, and January 2021) (Figure 1).
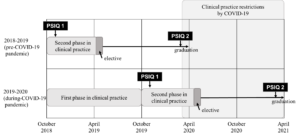
Figure 1. Timing in clinical practice and the PSIQ in 2018-2019 and 2019-2020
On the first day of clinical practice in the CBME program, the authors (JH, TaM, AT) explained the purpose of the study to the students. The authors informed the students that the study would be undertaken as a program evaluation and research, and that their grades would not be influenced in case they did not agree to participate. Those students who agreed to participate signed a consent form giving permission to use their data. Subsequently, the authors asked medical students to fill out the PSIQ as a paper-based, self-administered questionnaire, and to include their student ID number. At graduation, all medical students completed the PSIQ on the internet or on paper as a self-administered questionnaire, again with their student ID number. The study was approved by the Ethics Committee of the University of Tsukuba (No. 1329).
E. Data Analysis
To evaluate the differences in total PSIQ and scores for each item between the first day of clinical practice in the CBME program and the time of graduation, effect sizes (Cohen’s d) were determined for the total PSIQ and scores for each item. In addition, the Shapiro-Wilk test was performed to determine data distribution. For comparison of means for the difference in total PSIQ between 2018-2019 and 2019-2020, an unpaired t-test was applied. The Shapiro-Wilk test confirmed that data distribution for both PSIQ 1 and 2 were not normal. However, since the distribution of PSIQ 2-1 was consistent with normality, a t-test was employed. Missing values were excluded. Data analysis was conducted using SPSS ver. 26 with significance set at the p<0.05 level for total scores as the primary outcome of the PSIQ. Additionally, to deal with the possibility of multiplicity in the simultaneous assessment of each item score, significance levels were Bonferroni corrected, with p< 0.005 (Lee & Lee, 2018).
III. RESULTS
As shown in Table 1, participants analysed in the 2018-2019 academic year (pre-COVID-19 pandemic) included 104 medical students (response rate: 88.1%) who responded at both time points (first day of clinical practice in the CBME program and at graduation), 33 of whom were female. In the 2019-2020 academic year (during-COVID-19 pandemic), 92 medical students (response rate: 92.0%) who responded at both time points were included, 33 of whom were female. One student who did not give consent to have their data used in this study was excluded.
|
2018-2019 (pre-COVID-19 pandemic) |
2019-2020 (during-COVID-19 pandemic) (n=92) |
|
|
Age, mean ± standard deviation |
20.6±1.5 |
21.2±3.4 |
|
Gender, number of persons (%) |
||
|
Male |
66 (63.5) |
51 (55.4) |
|
Female |
33 (31.7) |
33 (35.9) |
|
Unknown |
5 (4.8) |
8 (8.7) |
Table 1. Characteristics of medical students included in the analysis
Table 2 shows that the means of total PSIQ scores and each PSIQ item for 2018-2019 and 2019-2020 were increased at graduation. A comparison of the mean for the difference using the unpaired t-test in total PSIQ score for 2018-2019 and 2019-2020 revealed that it was statistically higher for the 2019-2020 students (13.5 ± 9.4) than for the 2018-2019 students (10.3 ± 8.1) (t =2.6, df =195, p = 0.01). However, there were no statistically significant differences using the unpaired t-test with Bonferronni correction at a 0.005 level of significance in mean scores for 9 items of the PSIQ, namely “Teamwork” (t=0.96 df=195, p=0.341), “Communication” (t=1.84, df=195, p=0.068), “Conducting assessment” (t=2.31, df=195, p=0.24) “Cultural awareness” (t=1.41, df=195, p=0.022), “Ethical awareness” (t=2.25, df=195, p=0.161), “Using records” (t=2.67, df=195, p=0.026), “Dealing with emergencies” (t=2.33, df=195, p=0.008), “Reflection” (t=2.32, df=195, p=0.021) and “Teaching” (t=2.19, df=195, p=0.030). The effect size (Cohen’s d) for total PSIQ scores from the first day of clinical practice in the CBME program to graduation was Δ1.3 in 2018-2019 and Δ1.4 in 2019-2020. The effect size (Cohen’s d) for each item of the PSIQ was Δ1.4 in 2018-2019. Range for items was Δ0.8-1.1 in 2018-2019 and Δ0.9-1.2 in 2019-2020.
|
|
Fiscal year (usually April 1 to March 31) |
First day of the CBME program (1) |
At graduation (2) |
Mean difference in PSIQ (2)-(1) |
t score |
Df |
p-value |
Cohen’s d |
|
Total score (Main outcome) |
2018-2019 (pre-COVID-19 pandemic) |
28.5±7.6 |
38.8±8.5 |
10.3±8.1 |
2.60 |
195 |
0.01 |
1.3 |
|
2019-2020 (during-COVID-19 pandemic) |
28.0±6.6 |
41.6±9.2 |
13.5±9.4 |
1.4 |
||||
|
Sub-analysis |
|
|
||||||
|
Teamwork |
2018-2019 |
3.0±1.2 |
4.4±1.0 |
1.4±1.2 |
0.96 |
195 |
0.341 |
1.1 |
|
2019-2020 |
3.0±1.1 |
4.6±1.1 |
1.6±1.3 |
1.2 |
||||
|
Communication |
2018-2019 |
3.7±1.1 |
4.7±1.1 |
1.0±1.2 |
1.84 |
195 |
0.068 |
0.8 |
|
2019-2020 |
3.5±1.1 |
4.9±1.1 |
1.4±1.3 |
1 |
||||
|
Conducting assessment |
2018-2019 |
3.2±1.0 |
4.4±1.1 |
1.2±1.2 |
2.27 |
195 |
0.024 |
1 |
|
2019-2020 |
3.1±1.0 |
4.7±1.1 |
1.6±1.3 |
1.2 |
||||
|
Cultural awareness |
2018-2019 |
2.9±1.1 |
4.2±1.3 |
1.3±1.3 |
2.31 |
195 |
0.022 |
1 |
|
2019-2020 |
2.8±1.1 |
4.5±1.3 |
1.8±1.5 |
1.2 |
||||
|
Ethics awareness |
2018-2019 |
3.4±1.2 |
4.5±1.1 |
1.1±1.3 |
1.41 |
195 |
0.161 |
0.9 |
|
2019-2020 |
3.5±1.2 |
4.9±1.1 |
1.4±1.4 |
1 |
||||
|
Using record entries |
2018-2019 |
3.4±1.0 |
4.5±1.1 |
1.0±1.1 |
2.25 |
195 |
0.026 |
0.9 |
|
2019-2020 |
3.4±0.9 |
4.8±1.1 |
1.4±1.3 |
1.1 |
||||
|
Dealing with emergencies |
2018-2019 |
2.5±1.1 |
3.8±1.3 |
1.3±1.2 |
2.67 |
195 |
0.008 |
1.1 |
|
2019-2020 |
2.3±1.2 |
4.1±1.4 |
1.9±1.7 |
1.1 |
||||
|
Reflection |
2018-2019 |
3.3±1.1 |
4.3±1.1 |
1.0±1.3 |
2.32 |
195 |
0.021 |
0.8 |
|
2019-2020 |
3.2±0.9 |
4.6±1.3 |
1.4±1.5 |
1 |
||||
|
Teaching |
2018-2019 |
3.1±0.9 |
4.1±1.1 |
0.9±1.1 |
2.19 |
195 |
0. 030 |
0.8 |
|
2019-2020 |
3.2±1.0 |
4.5±1.2 |
1.3±1.4 |
1 |
Table 2. Unpaired t-test analysis and effect sizes for the Professional Identity Self-Assessment Form
IV. DISCUSSION
We found that the means of total and each PSIQ score of medical students who graduated during the COVID-19 pandemic were statistically increased compared to those of students graduating before the pre-COVID-19 pandemic. These findings indicate that, compared with students in the preceding year, the COVID-19 pandemic had a certain positive impact on professional identity formation in medical students with regard to clinical practice.
Considering the framework we used, in which the interaction and reflection of role models, mentors, and individual experiences are key, we believe that all participants were influenced by COVID-19. In addition, professional identity formation is reported to be strongly influenced by environment, context, and other personal variables. (Jarvis-Selinger et al., 2012) The increase in total PSIQ score from the previous year’s medical students may have been due not only to changes in clinical practice, but also to changes in what is expected of medical students by the university hospital and society. In light of these factors, medical students had fewer opportunities to acquire the knowledge and skills required of physicians in the clinical setting directly from role models and mentors, but may nevertheless have been affected by compliance with COVID-19 control measures conducted by the university hospital, and thereby followed the norms of medical professionals communicated through intentional and unintentional messaging. In addition, with the all-engrossing impact of the COVID-19 pandemic throughout society, we speculate that at least some of the students in the COVID-19 group were consulted by family and social contacts as experts and authorities on a daily or more frequent basis, and that such constant reinforcement might also have encouraged PIF. That is, medical students under the COVID-19 pandemic may have internalised the values and norms of the medical professional (Kinnear et al., 2021). Since professional identity formation involves social and relational factors, it is possible that the students’ life and social changes due to COVID-19 reinforced their recognised professional identity (Goldie, 2012).
The more uncertain and ambiguous the period, the more important reflection becomes in PIF. To cope with such uncertainties as the transition from the classroom curriculum to online platforms, rapid changes in the clinical practice environment, and the isolation caused by social distancing, medical students need a well-formed professional identity and socialisation practices (Costello, 2005). Poor PIF is reported to manifest in burnout (Abedini et al., 2018), and depression and anxiety disorders have increased in COVID-19 (Daniels et al., 2021). Since a core component of PIF is the acceptance of uncertainty and ambiguity, medical educators may have provided reflection opportunities for medical students to consciously consider the social factors manifested in COVID-19, such as individual and professional duties, resource priorities, and health disparities, all of which have a positive impact on PIF and socialisation (Stetson et al., 2020). Alternatively, emotion-focused coping strategies (e.g., arts engagement) and problem-solving strategies (e.g., volunteering) to reduce medical students’ anxiety, fear, and stress may be effective (Moula et al., 2022). Students require time and space to reflect on their emergent identity as professionals in these crisis situations (Moula et al., 2022). The extended time for independent learning may have allowed the students to subconsciously reflect on their professional identity, taking seriously the changes in society caused by COVID-19. PIF scores may have accordingly increased in this study.
In general, medical teachers should have made efforts to promote medical students’ professional identity formation even during the COVID-19 pandemic (Goldhamer et al., 2020). Professional identity formation is not a process that should be left to chance; it should be explicitly supported through systematic support and curriculum initiatives (Cruess et al., 2015; Schumacher et al., 2012). In reality, it is necessary to require rapid changes in clinical practice to prevent infection caused by COVID-19, and it has been difficult to promote systematic support for professional identity formation for medical students. However, COVID-19 might not have negatively affected the professional identity recognised by medical students who were in clinical practice immediately after the pandemic. The efforts of Japanese medical educators to implement online and other types of learning to replace clinical practice, and the well-considered efforts of faculty to make clinical practice as feasible as possible may have served as role models or mentors, and influenced medical students’ professional identity formation.
This study has three limitations. First, because there was a difference of 8-17 months between the first day of clinical practice in the CBME program and graduation, given that more clinical practice experience may strengthen the professional identity recognised by medical students, it is possible that differences in clinical practice experience may have affected PSIQ scores. Second, extrapolation from this study should be done with care, since it is a comparison of a one-year questionnaire survey at a single university. Third, a degree of response bias may be present due to the self-reporting design, with inclusion of student ID number. Fourth, evaluation at three or more points may allow a more precise comparison of changes, given that professional identity formation is a dynamic process. Even allowing for these limitations, our findings provide meaningful feedback to medical students and faculty, particularly given the paucity of studies evaluating and comparing changes in professional identity formation – which consists of multiple factors – before and during the COVID-19 pandemic. For the future of medical education, it is imperative to track the professional identity recognised by physicians whose student experience in clinical practice was restricted under the COVID-19 pandemic, and was accordingly significantly changed compared with other years.
V. CONCLUSION
Comparison of the professional identity recognised by medical students whose experience of clinical practice was affected by the COVID-19 pandemic to that of students in the previous year showed some positive impact on professional identity. This lack of negative difference in recognised professional identity even under restricted clinical practice may have been influenced by the imprinting of professional norms and changes in society.
Notes on Contributors
JH, AT, SO, TaM and TeM were involved in the conception and design of this study. JH, AT, and TaM collected the data. JH and RG conducted data analysis. JH mainly wrote the paper. AT, SO, TaM and TeM gave critical feedback on the manuscript. All authors have read and approved the final manuscript.
Ethical Approval
This study was approved by the Ethics Committee of the University of Tsukuba’s Faculty of Medicine and Medical Sciences (No. 1329). All participants have given written consent for their data to be used in the research and for publication.
Data Availability
It is not possible to share data since we did not obtain consent from participants to share all data collected.
Acknowledgement
We thank the faculty staff members Shoji Yokoya, Hisashi Yoshimoto, Shogen Suzuki, Naoto Sakamoto, Yu Yamamoto, Yoshihiro Kataoka, Shoichi Masumoto, Haruka Kuno, Takashi Inaba, Shuhei Hamada, Shogo Kawada, and Sayaka Nin of the Department of Primary Care and Medical Education, Faculty of Medicine, University of Tsukuba. Additionally, we thank the healthcare staff who taught the medical students at the CBME program sites in clinical practice.
Funding
This study was funded by the education/research fund of Department of Primary Care and Medical Education, Faculty of Medicine, University of Tsukuba.
Declaration of Interest
There are no companies or other entities with which the authors have conflict of interest relationships that should be disclosed in relation to the content of the paper.
References
Abedini, N. C., Stack, S. W., Goodman, J. L., & Steinberg, K. P. (2018). “It’s not just time off”: A framework for understanding factors promoting recovery from burnout among internal medicine residents. Journal of Graduate Medical Education, 10(1), 26–32. https://doi.org/10.4300/JGME-D-17-00440.1
Adams, K., Hean, S., Sturgis, P., & Clark, J. M. (2006). Investigating the factors influencing professional identity of first-year health and social care students. Learning in Health and Social Care, 5(2), 55–68. https://doi.org/10.1111/j.1473-6861.2006.00119.x
Al Samaraee, A. (2020). The impact of the COVID-19 pandemic on medical education. British Journal of Hospital Medicine, 81(7), 1-4. https://doi.org/10.12968/HMED.2020.0191
Alsoghair, M., Almazyad, M., Alburaykan, T., Alsultan, A., Alnughaymishi, A., Almazyad, S., Alharbi, M., Alkassas, W., Almadud, A., & Alsuhaibani, M. (2021). Medical Students and COVID-19: Knowledge, preventive behaviors, and risk perception. International Journal of Environmental Research and Public Health, 18(2), 842. https://doi.org/10.3390/ijerph18020842
Association of American Medical Colleges. (2020). Guidance on medical students’ participation in direct in-person patient contact activities. https://www.aamc.org/system/files/2020-08/meded-August-14-Guidance-on-Medical-Students-on-Clinical-Rotations.pdf
Chiodini, J. (2020). Online learning in the time of COVID-19. Travel Medicine and Infectious Disease, 34, Article 101669. https://doi.org/10.1016/j.tmaid.2020.101669
Costello, C. Y. (2005). Professional identity crisis: Race, class, gender, and success at professional schools. Vanderbilt University Press.
Crossley, J., & Vivekananda-Schmidt, P. (2009). The development and evaluation of a professional self identity questionnaire to measure evolving professional self-identity in health and social care students. Medical Teacher, 3(12), e603–e607. https://doi.org/10.3109/01421590903193547
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2014). Reframing medical education to support professional identity formation. Academic Medicine, 89(11), 1446–1451. https://doi.org/10.1097/ACM.0000000000000427
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2015). A schematic representation of the professional identity formation and socialization of medical students and residents: A guide for medical educators. Academic Medicine, 90(6), 718–725. https://doi.org/10.1097/ACM.0000000000000700
Emanuel, E. J. (2020). The inevitable reimagining of medical education. JAMA, 323(12), 1127–1128. https://doi.org/10.1001/jama.2020.1227
Findyartini, A., Anggraeni, D., Mikhael Husin, J., & Greviana, N. (2020). Exploring medical students’ professional identity formation through written reflections during the COVID-19 pandemic. Journal of Public Health Research, 9(s1), 1918. https://doi.org/10.4081/jphr.2020.1918
Goldhamer, M. E. J., Pusic, M. V., Co, J. P. T., & Weinstein, D. F. (2020). Can covid catalyze an educational transformation? Competency-based advancement in a crisis. New England Journal of Medicine, 383(11), 1003–1005. https://doi.org/10.1056/NEJMP2018570
Goldie, J. (2012). The formation of professional identity in medical students: Considerations for educators. Medical Teacher, 34(9), e641–e648. https://doi.org/10.3109/0142159X.2012.687476
Hafferty, F. W., & Franks, R. (1994). The hidden curriculum, ethics teaching, and the structure of medical education. Academic Medicine, 69(11), 861–871. https://doi.org/10.1097/00001888-199411000-00001
Haruta, J., Maeno, T., Takayashiki, A., Goto, R., Ozone, S., & Maeno, T. (2021). Validation of the professional self-identity questionnaire for medical students during clinical practice in Japan. International Journal of Medical Education, 12, 160–165. https://doi.org/10.5116/ijme.610d.104b
Haruta, J., Ozone, S., & Hamano, J. (2020). Doctors’ professional identity and socialisation from medical students to staff doctors in Japan: Narrative analysis in qualitative research from a family physician perspective. BMJ Open, 10(7), e035300. https://doi.org/10.1136/bmjopen-2019-035300
Hayashi, M., Saiki, T., Kanter, S. L., & Ho, M. J. (2022). Leaders’ perspectives and actions to manage challenges in medical education presented by the COVID-19 pandemic: A nationwide survey of Japanese medical colleges. BMC Medical Education, 22(1), 144. https://doi.org/10.1186/s12909-022-03193-1
Jarvis-Selinger, S., Pratt, D. D., & Regehr, G. (2012). Competency is not enough: Integrating identity formation into the medical education discourse. Academic Medicine, 87(9), 1185–1190. https://doi.org/10.1097/ACM.0b013e3182604968
Kaul, V., Gallo de Moraes, A., Khateeb, D., Greenstein, Y., Winter, G., Chae, J. M., Stewart, N. H., Qadir, N., & Dangayach, N. S. (2021). Medical education during the COVID-19 pandemic. CHEST, 159(5), 1949–1960. https://doi.org/10.1016/j.chest.2020.12.026
Khasawneh, A. I., Humeidan, A. A., Alsulaiman, J. W., Bloukh, S., Ramadan, M., Al-Shatanawi, T. N., Awad, H. H., Hijazi, W. Y., Al-Kammash, K. R., Obeidat, N., Saleh, T., & Kheirallah, K. A. (2020). Medical students and COVID-19: Knowledge, attitudes, and precautionary measures. A descriptive study from Jordan. Frontiers in Public Health, 8, 253. https://doi.org/10.3389/fpubh.2020.00253
Kinnear, B., Zhou, C., Kinnear, B., Carraccio, C., & Schumacher, D. J. (2021). Professional identity formation during the COVID-19 pandemic. Journal of Hospital Medicine, 16(1), 44–46. https://doi.org/10.12788/jhm.3540
Lee, S., & Lee, D. K. (2018). What is the proper way to apply the multiple comparison test? Korean Journal of Anesthesiology, 71(5), 353-360. https://doi.org/10.4097/KJA.D.18.00242
Lucey, C. R., & Johnston, S. C. (2020). The transformational effects of COVID-19 on medical education. JAMA, 324(11), 1033–1034. https://doi.org/10.1001/jama.2020.14136
Mian, A., & Khan, S. (2020). Medical education during pandemics: A UK perspective. BMC Medicine, 18(1), 100. https://doi.org/10.1186/s12916-020-01577-y
Moula, Z., Horsburgh, J., Scott, K., Rozier-Hope, T., & Kumar, S. (2022). The impact of COVID-19 on professional identity formation: An international qualitative study of medical students’ reflective entries in a global creative competition. BMC Medical Education, 22(1), 545. https://doi.org/10.1186/s12909-022-03595-1
Papapanou, M., Routsi, E., Tsamakis, K., Fotis, L., Marinos, G., Lidoriki, I., Karamanou, M., Papaioannou, T. G., Tsiptsios, D., Smyrnis, N., Rizos, E., & Schizas, D. (2021). Medical education challenges and innovations during COVID-19 pandemic. Postgraduate Medical Journal, 98, 321-327. https://doi.org/10.1136/postgradmedj-2021-140032
Prime Minister’s Office of Japan. (2020). [COVID-19] Declaration of a state of emergency in response to the Novel Coronavirus Disease. https://japan.kantei.go.jp/ongoingtopics/_00020.html
Ross, D. A., & the members of National Neuroscience Curriculum Initiative “Quarantine Curriculum” Committee (2020). Creating a “Quarantine Curriculum” to enhance teaching and learning during the COVID-19 pandemic. Academic Medicine, 95(8), 1125–1126. https://doi.org/10.1097/ACM.0000000000003424
Schumacher, D. J., Slovin, S. R., Riebschleger, M. P., Englander, R., Hicks, P. J., & Carraccio, C. (2012). Perspective: Beyond counting hours: The importance of supervision, professionalism, transitions of care, and workload in residency training. Academic Medicine, 87(7), 883–888. https://doi.org/10.1097/ACM.0b013e318257d57d
Shankar, P. R., & Wilson, I. G. (2020). The COVID-19 pandemic and undergraduate medical student teaching-learning and assessment. Canadian Medical Education Journal, 12(1), e190–e191. https://doi.org/10.36834/cmej.70800
Stetson, G. V., Kryzhanovskaya, I. V., Lomen-Hoerth, C., & Hauer, K. E. (2020). Professional identity formation in disorienting times. Medical Education, 54(8), 765–766. http://doi.org/10.1111/medu.14202
Wurth, S., Sader, J., Cerutti, B., Broers, B., Nadia Bajwa, M., Carballo, S., Escher, M., Galetto-Lacour, A., Grosgurin, O., Lavallard, V., Savoldelli, G., Serratrice, J., Nendaz, M., & Audétat-Voiro, M. C. (2022). Correction to: Medical students’ perceptions and coping strategies during the first wave of the COVID-19 pandemic: Studies, clinical implication, and professional identity. BMC Medical Education, 22(1), Article 232. https://doi.org/10.1186/s12909-022-03307-9
*Junji Haruta
35 Shinanomachi Shinjukuku Tokyo
160-8582, Japan
Email: junharujp@keio.jp
Submitted: 12 May 2022
Accepted: 3 August 2022
Published online: 3 January, TAPS 2023, 8(1), 13-24
https://doi.org/10.29060/TAPS.2023-8-1/OA2810
Audrey Lim1, Vicki Xafis2 & Clare Delany3
1Health and Social Sciences Cluster, Singapore Institute of Technology (SIT), Singapore; 2Graduate School of Humanities and Social Sciences, University of Melbourne, Melbourne, Australia; 3Department of Medical Education, School of Medicine, University of Melbourne, Melbourne, Australia
Abstract
Introduction: Workplace contexts, including political and sociocultural systems influence health professions’ perception and experience of ethical issues. Although established health ethics principles are relevant guiding values, they may be experienced and interpreted differently within different health contexts. How should ethics education account for this? This paper presents ethical dilemmas and concerns encountered by physiotherapists practicing in Singapore and discusses the implications for ethics education.
Methods: Qualitative methods informed by interpretivism and phenomenology were employed. In-depth interviews with 42 physiotherapists from different workplace settings in Singapore were conducted. Participants described everyday ethical challenges they encountered. Inductive content analysis was used to analyse the interview transcript data.
Results: Ethical issues occurred within and across three spheres of ethics: micro, meso and macro. Ethical issues at the micro sphere centered around physiotherapist-patient relationships, interactions with colleagues, and therapists’ feelings of moral distress. In the meso sphere, ethical challenges related to influences arising from the organizational resources or systems. In the macro sphere, ethical challenges developed or were influenced by sociocultural, religious, economic, and political factors.
Conclusion: The findings reflect current literature indicating that context can influence ethical situations, as experienced and perceived by physiotherapists in their unique settings. Such empirical data might inform the development of ethics curricula to ensure that universal ethical principles are situated within the realities of clinical practice. Locally relevant and realistic ethical case studies will better enable students to recognise and address these situations.
Keywords: Ethics, Physiotherapy, Health Professions Education, Ethics Education, Asian Context, Singapore, Healthcare Principles, Health Ethics Principles
Practice Highlights
- Context can influence the ethical situations experienced and interpreted by healthcare professionals.
- Contextualised cases studies need to be developed to make ethics real and relevant to students.
- Ethics education should incorporate local context and not focus only on ethics epistemic knowledge.
- Ethics education should incorporate the dynamic influence of macro, meso and micro factors.
I. INTRODUCTION
The established health ethics principles articulated by Beauchamp and Childress (2001): autonomy, beneficence, non-maleficence, and justice guide healthcare practice, including physiotherapy (Carpenter & Richardson, 2008; Edwards, Delany, et al., 2011). Although these principles were originally proposed as universally relevant and foundational to health ethics, health professionals interpret them differently, depending on their professional and personal background, their values, and the culture of the community and settings in which they work (Fuscaldo et al., 2013). In physiotherapy ethics scholarship, there is growing recognition that the universal nature of principlism as a supporting ethical decision-making framework, may not be a sufficient guide for physiotherapists in their ethical decision-making, because of the plurality of values and diverse contexts of healthcare practice (Carpenter, 2010; Carpenter & Richardson, 2008; Edwards, Wickford, et al., 2011; Fryer et al., 2021; Greenfield, 2006; Hudon et al., 2019; Oyeyemi, 2011; Souri et al., 2020; Sturm et al., 2022). Consequently, there is increasing pedagogical interest in using case studies drawn from everyday practice to bring authenticity and contextual relevance to ethics education (Aguilar-Rodríguez et al., 2019; Fuscaldo et al., 2013).
In physiotherapy, empirical studies have shown that different work contexts, political and sociocultural systems have a direct influence on physiotherapists’ perception and experience of ethical issues (Delany et al., 2018; Fryer et al., 2021; Sturm et al., 2022). A recent example is the study of ethical issues physiotherapists experienced by Sturm et al. (2022). The authors reported physiotherapists working in specific countries described having to compromise their professional integrity due to overt threats and intimidation by suppressive professional organisations or leaders. They were directed to follow the societal or organisational hierarchies or risk jeopardizing their careers. Studies of ethical experiences of physiotherapists practicing in the African nations (Aderibigbe & Chima, 2019; Chigbo et al., 2015; Nyante et al., 2020; Oppong, 2019; Oyeyemi, 2011) and the Greater Middle East region (Edwards, Wickford, et al., 2011; Qamar et al., 2014; Souri et al., 2020) similarly discussed how cultural influences, such as religion or spirituality can directly affect ethical practice and decision-making. Despite increasing empirical evidence globally, the influence of cultural and societal contexts on ethical decision-making and therapists’ interpretation of health values has not been examined in the East and Southeast Asian regions. There has also been little exploration of how societal and cultural context in which physiotherapy is practiced might be used to inform and shape curricula for ethics education.
In this paper, we present data about the ethical situations physiotherapists in Singapore encounter in their everyday clinical practice. Singapore is multi-racial, multi-religious and multi-cultural. The values of Singaporean people are very much rooted in their Asian heritage, with Confucianism as the prevailing social model (Ong, 2020; Tan, 1989; Yang et al., 2006). This research aims to contribute to knowledge about the influence of context on clinical ethical issues and decision-making, as interpreted by physiotherapists in Singapore. The empirical data will then be used to inform subsequent ethics curricula. Identifying and analysing the factors influencing ethical issues, as they are experienced and interpreted by physiotherapists in the Singaporean context, is an important pedagogical strategy to inform the development of health ethics curricula.
II. METHODS
We used a qualitative methodology drawing on the research paradigm of phenomenology and conducted in-depth interviews. We recruited physiotherapy clinicians using purposive (Palys, 2008) and snowball sampling (Holloway & Galvin, 2016). Written and verbal consent was obtained. Semi-structured interviews were conducted by AL and ranged from 44 to 123 minutes. Audio recordings were professionally transcribed verbatim and were reviewed by AL. Content analysis was used to analyse the transcribed data, with interviewer’s written field notes as supporting reference. Data was systematically coded and categorised with the aim of identifying themes, their frequency, and relationships, through both description and interpretation (Elo & Kyngäs, 2008; Hsieh & Shannon, 2005; Lindgren et al., 2020; Vaismoradi et al., 2013). Assisted by QSR NVivo 12 Software, the data analysis was organised into five steps (Figure 1). Although illustrated as a linear, chronological sequence, analysis occurred in a non-linear, iterative manner till there was clarity and meaning in the themes that were identified.
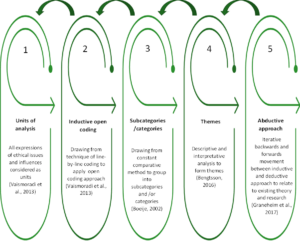
Figure 1. Sequence of data analysis
III. RESULTS
A total of 42 physiotherapists from four settings: acute, community, specialised institutions, and private practice participated (Table 1). All participants have been practicing physiotherapists in Singapore for the past three years, with 33.3 % in geriatrics and neuro rehabilitation, 45.3% in musculoskeletal and sports, and 21.4% in cardiopulmonary and other niche specialties. Thirty-six participants are Singaporeans and six are from Malaysia, Philippines, Hong Kong, New Zealand, and the UK. Ages ranged from 27 to 54 years old.
|
WORK SETTINGS |
ACUTE
Restructured public hospitals & subsidiaries |
COMMUNITY
Government supported intermediate & long- term care facilities |
SPECIALISED INSTITUTIONS
Government supported facilities for medical specialties/ niche populations
|
PRIVATE
Independent private physio clinics |
TOTAL (n) |
|
Number of Participants (n) |
16 |
13 |
6 |
7 |
42 |
|
Percentage (%) |
38.1 |
31.0 |
14.3 |
16.6 |
100 |
|
Gender (n) |
|
||||
|
Female |
9 |
12 |
5 |
2 |
28 |
|
Male |
7 |
1 |
1 |
5 |
14 |
|
Age Group in Years (n) |
|
||||
|
26-35 |
10 |
5 |
2 |
2 |
19 |
|
36-45 |
4 |
5 |
3 |
3 |
15 |
|
46-55 |
2 |
3 |
1 |
2 |
8 |
|
Professional Qualifications (n) |
|
||||
|
Diploma/Degree |
7 |
9 |
2 |
1 |
19 |
|
Postgraduate |
9 |
4 |
4 |
6 |
23 |
|
Number of Years in Healthcare (n) |
|
||||
|
< 10 |
9 |
6 |
1 |
2 |
18 |
|
10-20 |
5 |
5 |
4 |
3 |
17 |
|
> 20 |
2 |
2 |
1 |
2 |
7 |
n = number of participants
Table 1. Participants demographics
Six key themes were identified from the ethical situations described by the participants in their everyday physiotherapy practice: 1) managing healthcare resource constraints – encompassing ethical situations regarding the financial cost of healthcare, resource limitations and healthcare system inadequacies, 2) conforming to healthcare norms in Singapore – covering particular ethical challenges related to Singapore’s sociocultural context, including healthcare norms, 3) negotiating the complexity of the work environment – comprising challenges participants encountered in fulfilling their multiple obligations, especially in a negative work environment, 4) adapting to the intricacies of different healthcare settings – representing the unique ethical issues specific to the four different settings in Singapore, 5) balancing professional obligations and personal wellbeing – emerging from the participants’ struggle with their duty as moral agents, entrusted with the care of their patients while safeguarding their personal wellbeing and 6) advocating for patients: the predicament of relationships – exploring the relational aspects of a physiotherapist’s role, including defining professional boundaries, advocating for patients while managing their responsibilities to patients’ family and their colleagues. Complete quotes (QN1- QN18) illustrating the six themes are presented in Table 2.
|
Themes |
Quotations (QN) |
|
Managing healthcare resource constraints |
QN1: “I feel that these boundaries are set…because… at the end of the day it’s [healthcare] a business … we have to meet our finances. We have to balance our cheque books”. (P25) QN2: “If it’s something beyond our control, like the health system in Singapore itself, it can also be a potential barrier to our ethical practice. Because it’s not that we don’t want to do it. But … our hands are tied and it’s because of all these external factors that is affecting us.” (P38) |
|
Conforming to healthcare norms in Singapore |
QN3: “The subsidized cases actually are more complex than the private patients because private patients once they have a problem, they will get medical attention immediately… Whereas the subsidized patients…they usually drag…if they are being managed by a fresh grad that has no idea what is going on, then I think is unfair for them. And so, the cases that they [juniors] see, a lot of time is much more complex than the cases that the seniors see.” (P15) QN4: “I think insisting on certain types of equipment that we don’t feel or don’t agree with, that the patient really needs, but we do have to give because the doctor will keep on insisting on it, no matter how much we tell them that it may not be beneficial to the patient and all that. I think that’s one of the ethical things that I feel that I encounter.” (P33) QN5: “Breaking bad news seems to be also a bit of a two-way thing, where you have to go around to the family member first, before telling the patient even now. I mean, 20 years ago when I first started work it was like that, and I thought it would have moved on right? No. So I think is the education and is the perception of our Asian values, of the very paternalistic values that I think our families, or our patient’s families have.” (P09) |
|
Negotiating the complexity of the work environment |
QN6: “Because all you [i.e. the organisation] care about is earning money, all you [i.e. the organisation] care about is how many patients I can see a day and not caring whether I see it well, I’m seeing it correctly, whether I have provided value to the client.” (P13) QN7: “I see a patient, I read the history and I do the minimum, I do no harm. Patient may not get very well or recover as fast as they should…In terms of assessment, we need to be a bit more holistic, we need to assess thoroughly, but we don’t have the time…to me is clinically not ethical, but that’s how we’ve been working in a clinical setting because of time constraint, resources constraint.” (P22) QN8: “When I see something, I will just say it out to my superior, hoping that something can be done. And I can say it a few times, but once I see this is not going to work, because simply nobody responds to you, then just have to let it be, or if you really cannot take it, then you leave the organization.” (P15) |
|
Adapting to the intricacies of different healthcare settings |
QN9: “So, the proper procedure is that we refer them back to the doctor and get a new referral for the new problem. I find it quite silly to do that, the patient is right in front of me, and I know what’s the problem. I can instantly give a solution to the problem, why do I need to go and get a referral, and then delay for another three months before the patient can come back and see me for another problem?” (P26 – in acute setting) QN10: “If I make this person too mobile, family member cannot cope, he’s falling down, so this is my moral dilemma. I want him to be better, physically better. But he’s moving all over the place and he’s prone to fall and he’s much bigger size than the carer, (who) is only 40kg. I’m in a moral dilemma, how much should I give? How much should I train, or should I just give a little bit more just to maintain him? Must see from carer’s perspective. I don’t live with the person. I can come in once in a while, that one hour or just 45 minutes. But this person stays 24 hours, that’s where I’m stuck.” (P02 – in community setting) QN11: “However, then comes to work organisation that you need to understand the needs of the organisation and even the greater picture, therefore, you may not give the patient the best anymore.” (P03 – in specialised institution setting) QN12: “It’s very correlation or causation, or whatever. Often the treatment plan will miraculously be the same length as the [number] of sessions given by insurance, which you know is coincidence right? That it always happens to be the same length. You’ve got 10 sessions via insurance. That’s how long it’s going to take you to get better.” (P29 explained in a satirical manner – in private practice clinic) |
|
Balancing professional obligations and personal wellbeing
|
QN13: “Yes, so every day, we’ll carry him out on a chair for two hours… we’ll carry him back to bed and it’s two to three times max assist…this actually gave my senior some backache…because every day, is every day…because for such heavy patient, there’s no real technique already… So, this is a dilemma.” (P36) QN14: “Because I thought it was like part of my job. Probably he accidentally touched…when we do transfer, it tends to like, hands go flare anywhere. So, I thought never mind because I need to do my job. I need to transfer him. Of course, I don’t want him to fall down. So, I have to do all this contact.” (P34) QN15: “If it is a young female patient, then you try to have the female TA (therapy assistant) to be in as your chaperon. If it’s Ah Ma (older lady), then just keep the door open. It’s okay. I don’t know how is that right or wrong. But so far, it doesn’t give me any problem with that kind of practice. Usually, the Ah Ma doesn’t complain.” (P11) |
|
Advocating for patients: the predicament of relationships |
QN16: “Of course, the patient did give verbal consent. So, by right, by legal standpoint, it means that it’s fine. Then you start thinking a little bit deeper, sometimes when you’re in a clinic, patient will actually feel that they have to do that. If they don’t agree to your examination, then they are here for no purpose…Does it make the patient feel that we are coercing them? And they don’t really have a choice to really say, I don’t want it in that sense.” (P41) QN17: “I’m trying to fight for my client’s welfare. But a lot of times, if the family do not seek that welfare for the client, there is nothing I can do…. Do I train the caregiver who’s not willing to learn? Do I charge this family when the family has already expressed interest in no longer paying for equipment, or even therapy? Do I force it down their throat?” (P04)
QN18: “I guess maybe to me it really depends on the extent of that incident, how bad of that it is to the profession as a whole. If it is something that is minor and understandable, then probably I will not. But if it is something that is…pretty bad, maybe I would. I don’t know, it’s still a struggle, I can’t because it’s my fellow friends and colleagues. So, it’s a bit tough to be honest.” (P27) |
Table 2. Quotes to illustrate the six themes
A. Managing Healthcare Resource Constraints
Participants were aware of their ethical responsibility to act in the patient’s best interest in the provision of care but felt the pressure of finite resources and financial constraints (QN1). They described how they struggled to fulfill their professional obligations whilst at the same time managing patients’ expectations about availability of resources. Some therapists found loopholes to bypass government funding requirements. One participant (P26) summarised it as being a “discrepancy between the ideal care for the nation as a whole versus what is ideal for the patient’s health right before my eyes”. Some participants spoke about how key performance indicators (KPIs) intended to manage healthcare costs can drive change in organisational and clinician behaviour to practice defensively rather than using evidence-based practice to meet patients’ needs. Participant 09 described it as “funding drives behaviour” and gave the example of how a KPI that tracks fall rates may sway clinicians to be overly conservative to prevent falls, rather than challenging patients’ balance to maximise recovery. A lack of clear workflows and integration between different clinical settings was another ethical challenge preventing best available care for patient. Community and private practice physiotherapists indicated that they lack access to medical records and diagnostic results to seek clarity on a patient’s condition. This resulted in therapists feeling frustrated, as they had to delay treatment or proceed without a clear understanding of the patient’s medical status (QN2).
B. Conforming to Healthcare Norms in Singapore
For some participants, the allocation of only senior clinicians to private patients and junior clinicians to subsidised patients was viewed as unjust practice, where allocation of clinicians’ expertise is not based on the needs of patients. Participant 15 shared that the subsidised patients tended to be more complex cases as they may not have the resources to seek medical attention early (QN3). Most participants acknowledged this as an accepted practice in Singapore’s healthcare system and not just specific to physiotherapy, with participant 39 highlighting that “no one addresses it”. Adding to the social class differentiation, nearly all participants commented on the acceptance of hierarchical differentiation in healthcare with doctors at the top. Many participants spoke about paternalism being widely practiced and accepted by patients, and shared incidents where doctors dictated treatment plans, and even overrode patients’ wishes. Participants felt obliged to comply regardless of their own professional judgement (QN4).
Familialism may also compromise patients’ autonomy. Participants shared stories where family members dominated decision-making or demanded withholding information from patients. There were also geriatric patients who chose to relinquish their autonomy to their children. Many participants viewed this as an accepted part of Asian norms (QN5). A few participants stressed that many Singaporeans still hold conservative views and highlighted the importance of remaining sensitive to racial, religious, and cultural differences. For example, participant 22 disclosed that it is not accepted practice for male physiotherapists to place electrocardiogram (ECG) leads on a female patient even with the patient’s consent and a chaperon present.
C. Negotiating the Complexity of the Work Environment
Organisations have to manage the financial cost of patient care and ensure business sustainability. With resource limitations, clinicians face the challenge of conflicting obligations to their organisation and their patients. Participant 13 expressed her frustration and resentment that physiotherapy outcomes are determined by organisational financial values (QN6). Another participant (P31) shared how she had to discharge patients “prematurely” to meet organisational expectations. Other participants coped by settling for minimum treatment and doing no harm to patients (QN7).
Adding to this complexity was a negative work culture, expressed by participants as the pressure to conform to the organisation’s expectations, norms, and practices. Examples given included unreasonable workloads, biasness towards preferred staff, belittling remarks, fault-finding, and masked threats of poor appraisals. Staff were expected to conform and follow the rules, leading to a culture of fear, where safety incidents went unreported for fear of repercussions. This was further perpetuated by the lack of supervisors’ moral courage, who ignored such ethical infringements, thus normalizing ethical silence as accepted behaviour. Participant 13 disclosed her moral distress when her concerns regarding fraudulent behaviour by a colleague who falsely documented and charged for services, were disregarded by her seniors. Some participants dispiritedly added that often no action was taken and they either learnt to accept the status quo and found their own solutions or left the organisation (QN8).
D. Adapting to the Intricacies of Different Healthcare Settings
1) Acute settings: The different organisational structure and systems in each setting gave rise to specific ethical concerns. Many ethical issues in the acute settings related to the structured systems, established practices and workflows. One such practice was physiotherapists not being allowed as first contact practitioners in public institutions. Patients can only be seen with a referral from doctors and only be treated for the problem for which they were referred. This was ethically challenging for physiotherapists wanting to manage patients holistically (QN9). Several participants also raised concerns regarding minimal charging per session. In some acute settings, the on-call duty was rostered for all physiotherapists, regardless of their inpatient competency or speciality. Concerns were raised about whether this was ethically good clinical practice and in patients’ best interests.
2) Community settings: Some participants commented that community settings have varied and diverse services, making it difficult to implement guidelines that are applicable and fair to all services. This can encourage clinicians to circumvent the rules to benefit their patients. In integrating a patient back to their community, the patient’s psychological, social, and family issues can become the major consideration. Participant 02 shared her dilemma in having to factor in the caregiver’s coping ability when progressing a patient with mental health issues, who had little comprehension of fall risks, to independent mobility (QN10). A few participants commented that community physiotherapists generally have greater independence and flexibility in their work schedule, but this can engender accountability issues in terms of documentation and the standard of services provided. Some participants felt that the lack of awareness of community services available and an unsubstantiated perception that community physiotherapists are not as skilled, may deter some patients from continuing their care in the community and could have contributed to a shortage of community allied health professionals.
3) Specialised institutions: For some specialised institutions where healthcare is not the core business, physiotherapists reported being constrained by the organisational goals when caring for their patients. The needs of the organisation and the deliverables expected factored greatly in both the patient’s and clinician’s decision-making. Consequently, the best interest of the patient may not take precedence (QN11). Participants commented that the hierarchical order in such institutions tended to be more overt, with instructions directed by leaders in charge rather than team discussions.
4) Private practice clinics: Participant 27 described the business aspect of private practice as having to wear two hats: one as a clinician and one as a businessman. This can lead to maximising profits through overcharging, overservicing and maximising insurance claims. Participant 27 further disclosed that most people kept it hushed, “it’s one of those things that everyone knows is happening, but no one wants to rock the boat”. Participant 29 shared how he had to see post-op cases twice weekly, regardless of whether it was necessary, “because that’s just the way things are done” and how the cost of treatment or number of sessions needed for recovery consistently matched the insurance claim limits (QN12). Other participants raised issues which bordered on being illegal. One common example shared was fee-splitting, whereby commission was given for the referral of patients. Private clinicians commented that private practice is loosely regulated, with no standardisation or best practice guidelines and that there is little collaboration or accountability to the profession. They further elaborated that private practice is very competitive, with some clinicians making exaggerated claims about their skills or effectiveness of their treatment.
E. Balancing Professional Obligations and Personal Wellbeing
Participants described conflicts between their work responsibilities and their personal wellbeing. They shared their insecurities about whether they had positively fulfilled their professional obligations. Demanding expectations or long working hours imposed by organisations forced some participants to sacrifice their personal life, compromise their mental health and even sustain work-related injuries. Participants detailed episodes of transferring or ambulating patients without equipment or sufficient manpower (QN13). The nature of physiotherapy often requires close physical contact with patients. Participant 34 disclosed her distressing encounter with a patient with mental health issues, who repeatedly touched her inappropriately but denied it. On why she continued treatment, she replied that she needed to do her job and convinced herself that it was probably accidental (QN14). Participant 11 shared his dilemma with regard to treating female patients when there was a lack of chaperones. To protect staff from allegations of misconduct, it is accepted practice to leave the consultation room door open, leading to a possible violation of patients’ privacy (QN15). Participants also disclosed unethical and even illegal incidents which reflected the therapists’ conflict between protecting themselves and their professional responsibilities. These included false documentation of clinical notes, dishonesty about treatment errors, or not reporting safety violations.
Having self-doubt about one’s competency, whether it is due to inexperience, being out of practice or due to a lack of access to resources led some participants to question whether they had done patients a disservice or whether they were practicing beyond their capability. At times, clinicians also found it challenging to bill patients for physiotherapy services, especially if patients had financial difficulties.
F. Advocating for Patients: The Predicament of Relationships
Several participants highlighted the crossing of professional boundaries as an ethical concern. This included patients constantly calling or messaging, asking for free advice or personal favours. The nebulous zone where a professional relationship crossed over into friendship or even a dependency worried many participants. Numerous participants shared their turmoil when dealing with special populations such as patients with mental health conditions. The dilemma of overriding a patient’s autonomy became harder to resolve when the patient’s safety was at risk or where there was a possibility of detrimental consequences. Participant 41 pondered about the unspoken power differential between the patient and the healthcare professional, which can lead to patients feeling pressured to consent to treatment (QN16).
Another common dilemma expressed by participants was gaining caregivers’ and families’ support. Family members felt justified in their demands as the payer and viewed themselves as the spokesperson. Some participants expressed their helplessness with family members unwilling to pay for needed services or equipment (QN17).
Participants shared views about maintaining collegiality and not disrespecting colleagues’ viewpoints, specifically when there were conflicting patient management strategies. Some participants resented the loss of their professional autonomy but yielded to maintain harmony, and to avoid confusion for the patient. A number of participants reinforced this strong sense of fraternity, including unwillingness to expose wrongdoing even if colleagues had crossed ethical and legal boundaries (QN18). Some participants spoke about the move towards transdisciplinary practice in Singapore and the blurring of professional boundaries. One participant (P04) elaborated on resource limitations in home-based therapy, prompting her to take on other healthcare roles to prescribe home equipment and even change patients’ wound dressings. She expressed her dilemma in having to consider the patient’s perspective, her organisation’s views, and her own competency as well as the professional and legal implications of providing the wrong advice.
Further analysis revealed that the ethical challenges encountered mapped to the three overall spheres of ethics previously identified by Glaser (2005) and Sippel et al. (2015), namely the micro, meso and macro spheres. Ethical issues at the micro sphere centered around physiotherapist-patient relationships, physiotherapist’s interactions with colleagues and their own needs. The meso sphere consists of four quarters that represented the four settings, and issues included structural problems and challenges related to organizational resources or systems. The macro sphere comprises ethical issues rooted in the influence of cultural, sociological, religious, economic, and political contexts (Sippel et al., 2015). The modified illustration of spheres of ethics with the meso sphere encircling the micro sphere and the macro sphere encircling the meso sphere, show the connection and interdependence of all three spheres (Figure 2).

Figure 2. Spheres of ethics (six themes)
IV. DISCUSSION
This study is the first to report on the clinical ethics issues faced by physiotherapists practicing in Singapore. It also provides some insights into the influence of context in ethical decision-making. The six themes identified were further organised into micro, meso and macro spheres or contexts of ethics. The micro sphere themes included ethical issues that have previously been identified in other physiotherapy study findings (Delany et al., 2018; Fryer et al., 2021; Praestegaard & Gard, 2013; Sturm et al., 2022). The notable points of difference specific to Singapore were themes residing in the meso and macro spheres. These themes offered potential insights into the particular context of physiotherapy practice in Singapore. One example in the meso sphere is the influence of different healthcare settings (acute, community, specialised institutions, and private practice) on ethical dimensions of physiotherapy practice within Singapore’s healthcare system. There were differences in the predominance or perceived importance of certain ethical issues due to each setting’s unique organisational structure and systems. These findings appear to reflect current literature which reported on differences in physiotherapists’ ethical experiences due to the influence of healthcare settings (Cantu, 2018, 2019; Hudon et al., 2015).
At the macro sphere, participants reported that fulfilling government set KPIs or outcome measures which determined healthcare funding exerted indirect pressure on them. They grappled with patients’ expectations of advocacy on their behalf and societal expectations of cost containment (Dronberger, 2003). In meeting the requirements, participants had to balance their view about what was a good enough treatment constrained by the system, versus the best treatment available. The findings suggest that having to meet quantitative statistical numbers such as discharge rates was interpreted by some therapists as neglecting the quality of care and negatively affecting the therapist-patient relationship. This finding is consistent with that of Hudon et al. (2015), who highlighted institutional and economic influence on the quality of physiotherapy service and public trust. Another theme in the macro sphere concerned the negative effects of hierarchies and power differentials, which therapists believed led to paternalistic practice. Factors contributing to paternalism can include time limitations on treatment, patient’s literacy levels, societal values of respecting seniority and the accepted practice of patients handing over decision-making to authority or their family. Familialism is prevalent in Singaporean culture, where a family centric approach or interest will outweigh individual’s autonomy (Krishna, 2012). It is viewed as an accepted part of Asian values and needs to be acknowledged in order to provide the best possible care for the patient. Ethical issues related to familialism have also been reported by studies in the African context (Chigbo et al., 2015; Nyante et al., 2020; Sippel et al., 2015).
A. Relevance to Ethics Education
There is agreement that ethics cannot be taught independent of context, with a focus only on the epistemic knowledge, but that it needs to incorporate the dynamic influence of macro, meso and micro factors (Barradell, 2017; Cantu, 2018; Greenfield et al., 2015; Ladeira & Koifman, 2017). The themes in this study can directly inform the ethics curriculum, highlighting to students the influence of resource constraints, local healthcare norms, organisational culture, challenges of different settings, as well as balancing multiple obligations. Beyond awareness, students must be equipped with the abilities and skillsets to address and navigate these ethical situations. Elaboration on each theme’s implications for the local ethics curriculum is outlined in Table 3.
|
Spheres of ethics |
Themes |
How understanding of spheres of ethics can inform physiotherapy ethics curricula |
|
MACRO: Conflict of ethical principles versus societal expectations, culture, and practices |
Managing healthcare resource constraints |
· Incorporate understanding of financial aspects of healthcare and its influence on physiotherapy practice (Finch et al., 2005). · Learn to anticipate and navigate the potential conflicts between equitable use of resources (justice) and best care for each patient (beneficence). |
|
Conforming to healthcare norms in Singapore |
· Be consciously aware of local cultural and practices. Acknowledging and respecting both universal health ethics principles and culturally based differences in values by taking into account relevant contextual considerations in application of ethical principles (Fuscaldo et al., 2013). · Learn to reason and negotiate for common moral ground without compromising one’s moral integrity (Fuscaldo et al., 2013). |
|
|
MESO: Contention between ethical principles and organisational values and norms |
Negotiating the complexity of the work environment |
· Recognise the complexities of the work environment, including managing obligations to employers versus professional duty to their patients. · Develop strategies and skillsets to overcome negative work culture (e.g. by building an advisory support system and network within the organisation or the national professional body). |
|
Adapting to the intricacies of different healthcare settings |
· Understand the strengths and limitations of different workplace settings in Singapore and potential ethical challenges. |
|
|
MICRO: Conflict of ethical principles or the struggle between self-interest versus altruism |
Balancing professional obligations & personal wellbeing |
· Reinforce importance of personal integrity and learn coping strategies for self -care to prevent professional burn out or moral distress. |
|
Advocating for patients: the predicament of relationships |
· Appreciate that relational aspects of physiotherapy practice go beyond patient-therapist interactions to include colleagues and caregivers. · Emphasise physiotherapists’ role as a moral agent and advocate for patients. |
Table 3. Implications for ethics curricula
The study findings can be used to inform the development of realistic and contextualised case studies that have the potential to resonate with students’ clinical experience and improve the relevance of ethics education (Barnitt & Roberts, 2000; Fuscaldo et al., 2013; Triezenberg & Davis, 2000). The data in this study highlighted therapists’ emotions of frustration, anger, and concern. Disregarding contextual differences may create indifference, cynicism, or even moral distress when students begin practice and experience the realities of clinical practice (Greenfield & Jensen, 2010; Mohr & Mahon, 1996; Nalette, 2010). Students may dismiss ethics as irrelevant or feel disrespected that their culture and practices have not been considered in the materials taught (Fuscaldo et al., 2013).
Developing realistic case studies for ethics curricula has four possible effects: 1) it assists in dispelling the notion that ethics is based on abstract and idealist considerations (Seedhouse, 1995), 2) it can stimulate practical reflection and be action guiding to help students reason and navigate ethical challenges (Geddes et al., 2009; Swisher et al., 2012), 3) it can address the dissonance between what they learn in the classroom and what they experience in clinical practice (Dutton & Sellheim, 2017), 4) it can assist to increase ethics literacy and ethical courage. Case studies based on local experiences can provide the physiotherapy community with the ethical language to express their thoughts (Barnitt & Partridge, 1997). This shared language may enable students and clinicians to share experiences and learn how to speak up or seek help. Only when ethical issues that are pertinent to the local physiotherapy community are voiced, articulated, and discussed, can there be engagement of the community to confront identified ethical concerns, commit to creating change, and to strive towards ethical clinical practice.
B. Limitations
Participant recruitment and interviews were completed under the permeating influence of the global COVID crisis amidst shortage of healthcare staff. Due to the sensitivity of the topic, participants may have been guarded and not freely shared their views.
V. CONCLUSION
This study explored the ethical issues experienced and interpreted by physiotherapists across a range of practice settings in Singapore and examined how these experiences could inform ethics education. Our results have further substantiated current literature that context plays a critical influencing role on ethical situations, as they are experienced and perceived by physiotherapists in their unique geographical and clinical settings. The ability to act ethically has to be understood within the context and complexity of the sociocultural and political framework, along with the explicit and implicit influences, obligations, and commitments as part of a community, in order to directly address the everyday frustrations and concerns that clinicians face in trying to provide the best care for patients. With this knowledge, ethics educators and clinical supervisors will be better equipped to prepare students for clinical practice in Singapore.
Notes on Contributors
AL reviewed the literature, conceptualised and designed the study, conducted the interviews, analysed and interpreted the data, drafted the manuscript and wrote the final version submitted. This study is part of her PhD thesis.
CD is the first author’s primary PhD supervisor, who is involved in finalising the study and manuscript conceptualisation, and supervised the study from the beginning to the final version of the manuscript.
VX is the first author’s local PhD supervisor for data collection and supervised the study from the beginning to the final version of the manuscript.
Both CD and VX gave critical feedback on the direction and writing of the manuscript.
Ethical Approval
Ethics approval for this study was obtained from the University of Melbourne, Medicine and Dentistry Human Sub-Committee on 25 October 2019 (ID 1955123), and from the Singapore Institute of Technology, Institutional Review Board on 25 November 2019 (Project 2019146).
Data Availability
As the topic is of a sensitive nature and part of a larger PhD study, transcripts from the interviews are confidential and the authors do not have consent to upload onto a repository.
Acknowledgement
The authors would like to thank the 42 participants who have consented and graciously gave their time to participate in this study.
Funding
This study was completed with support from Singapore Institute of Technology (SIT) SEED grant (R-MOE-E103-C019).
Declaration of Interest
The authors declare that they have no competing interests.
References
Aderibigbe, K. S., & Chima, S. C. (2019). Knowledge and practice of informed consent by physiotherapists and therapy assistants in Kwazulu-Natal Province, South Africa. South African Journal of Physiotherapy, 75(1), a1330. https://doi.org/10.4102/sajp.v75i1.1330
Aguilar-Rodríguez, M., Marques-Sule, E., Serra-Añó, P., Espí-López, G. V., Dueñas-Moscardó, L., & Pérez-Alenda, S. (2019). A blended-learning programme regarding professional ethics in physiotherapy students. Nursing Ethics, 26(5), 1410–1423. https://doi.org/10.1177/0969733017748479
Barnitt, R., & Partridge, C. (1997). Ethical reasoning in physical therapy and occupational therapy. Physiotherapy Research International, 2(3), 178–194. https://doi.org/10.1002/pri.v2:3
Barnitt, R. E., & Roberts, L. C. (2000). Facilitating ethical reasoning in student physical therapists. Journal of Physical Therapy Education, 14(3), 35–41. https://doi.org/10.1097/00001416-200010000-00007
Barradell, S. (2017). Moving forth: Imagining physiotherapy education differently. Physiotherapy Theory & Practice, 33(6), 439–447. https://doi.org/10.1080/09593985.2017.1323361
Beauchamp, T. L., & Childress, J. F. (2001). Principles of biomedical ethics. Oxford University Press.
Bengtsson, M. (2016). How to plan and perform a qualitative study using content analysis. NursingPlus Open, 2, 8–14. https://doi.org/10.1016/j.npls.2016.01.001
Boeije, H. (2002). A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Quality and Quantity, 36, 391–409. https://doi.org/10.1023/a:1020909529486
Cantu, R. (2018). Physical therapists’ perception of workplace ethics in an evolving health-care delivery environment: A cross-sectional survey. Physiotherapy Theory and Practice, 35(8), 724–737. https://doi.org/10.1080/09593985.2018.1457744
Cantu, R. (2019). Physical therapists’ ethical dilemmas in treatment, coding, and billing for rehabilitation services in skilled nursing facilities: A mixed-method pilot study. Journal of the American Medical Directors Association, 20(11), 1458–1461. https://doi.org/10.1016/j.jamda.2019.06.013
Carpenter, C. (2010). Moral distress in physical therapy practice. Physiotherapy Theory & Practice, 26(2), 69–78. https://doi.org/10.3109/09593980903387878
Carpenter, C., & Richardson, B. (2008). Ethics knowledge in physical therapy: A narrative review of the literature since 2000. Physical Therapy Reviews, 13(5), 366–374. https://doi.org/10.1179/174328808×356393
Chigbo, N. N., Ezeome, E. R., Onyeka, T. C., & Amah, C. C. (2015). Ethics of physiotherapy practice in terminally ill patients in a developing country, Nigeria. Nigerian Journal of Clinical Practice, 18(7), S40–S45. https://doi.org/10.4103/1119-3077.170826
Delany, C., Edwards, I., & Fryer, C. (2018). How physiotherapists perceive, interpret, and respond to the ethical dimensions of practice: A qualitative study. Physiotherapy Theory and Practice, 35(7), 663–676. https://doi.org/10.1080/09593985.2018.1456583
Dronberger, J. (2003). Fraud and negligence in physical therapy practice: A case example. Physiotherapy Theory and Practice, 19(3), 151–159. https://doi.org/10.1080/09593980307961
Dutton, L. L., & Sellheim, D. O. (2017). Academic and clinical dissonance in physical therapist education: How do students cope? Journal of Physical Therapy Education, 31(1), 61–72. https://doi.org/10.1097/00001416-201731010-00009
Edwards, I., Delany, C. M., Townsend, A. F., & Swisher, L. L. (2011). New perspectives on the theory of justice: Implications for physical therapy ethics and clinical practice. Physical Therapy, 91(11), 1642–1652. https://doi.org/10.2522/ptj.20100351.10
Edwards, I., Wickford, J., Adel, A. A., & Thoren, J. (2011). Living a moral professional life amidst uncertainty: Ethics for an Afghan physical therapy curriculum. Advances in Physiotherapy, 13(1), 26–33. https://doi.org/10.3109/14038196.2010.483015
Elo, S., & Kyngäs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. https://doi.org/10.1111/j.1365-2648.2007.04569.x
Finch, E., Geddes, E. L., & Larin, H. (2005). Ethically-based clinical decision-making in physical therapy: Process and issues. Physiotherapy Theory and Practice, 21(3), 147–162. https://doi.org/10.1080/09593980590922271
Fryer, C., Sturm, A., Roth, R., & Edwards, I. (2021). Scarcity of resources and inequity in access are frequently reported ethical issues for physiotherapists internationally: An observational study. BMC Medical Ethics, 22, Article 97. https://doi.org/10.1186/s12910-021-00663-x
Fuscaldo, G., Russell, S., Gillam, L., Delany, C., & Parker, M. (2013). Addressing cultural diversity in health ethics education: Final Report 2013. http://www.research-matters.com.au/publications/FinalReport.pdf
Geddes, E. L., Salvatori, P., & Eva, K. W. (2009). Does moral judgement improve in occupational therapy and physiotherapy students over the course of their pre-licensure training? Learning in Health and Social Care, 8(2), 92–102. https://doi.org/10.1111/j.1473-6861.2008.00205.x
Glaser, J. W. (2005). Three realms of ethics:An integrating map of ethics for the future. In R. B. Purtilo, G. M. Jensen, & C. B. Royeen (Eds.), Educating for moral action: A sourcebook in health and rehabilitation ethics (pp. 169-184). F.A. Davies.
Graneheim, U. H., Lindgren, B. M., & Lundman, B. (2017). Methodological challenges in qualitative content analysis: A discussion paper. Nurse Education Today, 56, 29–34. https://doi.org/10.1016/j.nedt.2017.06.002
Greenfield, B., & Jensen, G. M. (2010). Beyond a code of ethics: Phenomenological ethics for everyday practice. Physiotherapy Research International, 15(2), 88–95. https://doi.org/10.1002/pri.481
Greenfield, B. H. (2006). The meaning of caring in five experienced physical therapists. Physiotherapy Theory and Practice, 22(4), 175–187. https://doi.org/10.1080/09593980600822859
Greenfield, B. H., Jensen, G. M., Delany, C. M., Mostrom, E., Knab, M., & Jampel, A. (2015). Power and promise of narrative for advancing physical therapist education and practice. Physical Therapy, 95(6), 924-933. https://doi.org/10.2522/ptj.20140085
Holloway, I., & Galvin, K. (2016). Data analysis: Procedures, practices and use of computers. In Qualitative research in nursing and healthcare(4th ed., 287–302).Wiley-Blackwell.
Hsieh, H. F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687
Hudon, A., Drolet, M. J., & Jones, B. W. (2015). Ethical issues raised by private practice physiotherapy are more diverse than first meets the eye: Recommendations from a literature review. Physiotherapy Canada, 67(2), 124–132. https://doi.org/10.3138/ptc.2014-10
Hudon, A., Ehrmann Feldman, D., & Hunt, M. (2019). Tensions living out professional values for physical therapists treating injured workers. Qualitative Health Research, 29(6), 876–888. https://doi.org/10.1177/1049732318803589
Krishna, L. R. (2012). Best interests determination within the Singapore context. Nursing Ethics, 19(6), 787–799. https://doi.org/10.1177/0969733011433316
Ladeira, T. L., & Koifman, L. (2017). Interface entre fisioterapia, bioética e educação: revisão integrativa [Interface between physical therapy, bioethics and education: Integrative review]. Revista Bioética, 25(3), 618–629. https:/doi.org/10.1590/1983-80422017253219
Lindgren, B. M., Lundman, B., & Graneheim, U. H. (2020). Abstraction and interpretation during the qualitative content analysis process. International Journal of Nursing Studies, 108. https://doi.org/10.1016/j.ijnurstu.2020.103632
Mohr, W. K., & Mahon, M. M. (1996). Dirty hands: The underside of marketplace health care. Advances in Nursing Science, 19(1), 28–37. https://doi.org/10.1097/00012272-199609000-00005
Nalette, E. (2010). Constrained physical therapist practice: An ethical case analysis of recommending discharge placement from the acute care setting. Physical Therapy, 90(6), 939–952. https://doi.org/10.2522/ptj.20050399
Nyante, G. G., Andoh, C. K., & Bello, A. I. (2020). Patterns of ethical issues and decision-making challenges in clinical practice among Ghanaian physiotherapists. Ghana Medical Journal, 54(3), 179–185. https://doi.org/10.4314/gmj.v54i3.9
Ong, E. K. (2020). The impact of sociocultural influences on the COVID-19 measures—reflections from Singapore. Journal of Pain and Symptom Management, 60(2), e90–e92. https://doi.org/10.1016/j.jpainsymman.2020.04.022
Oppong, S. (2019). When the ethical is unethical and the unethical is ethical: Cultural relativism in ethical decision-making. Polish Psychological Bulletin, 50(1), 18–28. https://doi.org/10.24425/ppb.2019.126014
Oyeyemi, A. (2011). Ethics and contextual framework for professional behaviour and code of practice for physiotherapists in Nigeria. Journal of the Nigeria Society of Physiotherapy, 19(1–2), 49–53. https://academicjournals.org/journal/JNSP/article-full-text -pdf/0AA592B65221
Palys, T. (2008). Purposive sampling. In L. M. Given (Ed.), The sage encyclopedia of qualittaive research methods (Vol. 2, pp. 697–698). Los Angeles: Sage.
Praestegaard, J., & Gard, G. (2013). Ethical issues in physiotherapy – Reflected from the perspective of physiotherapists in private practice. Physiotherapy Theory & Practice, 29(2), 96–112. https://doi.org/10.3109/09593985.2012.700388
Qamar, M. M., Basharat, A., Rasul, A., Basharat, S., & Ijaz, M. J. (2014). Perception of physical therapy students and professionals about the importance of professional ethics. International Journal of Medicine and Applied Health., 2(2), 57–61. https://www.academia.edu/11604067/perception_of_physical_therapy_students_and_professionals_about_the_importance_of_professional_ethics
Seedhouse, D. (1995). There’s Logic, and then there’s what we do around here. Health Care Analysis, 3(2), 87–90. https://doi.org/10.1007/BF02198208
Sippel, D., Marckmann, G., Atangana, E. N., & Strech, D. (2015). Clinical ethics in Gabon: The spectrum of clinical ethical issues based on findings from in-depth interviews at three public hospitals. PLoS ONE, 10(7), e0132374. https://doi.org/10.1371/journal.pone.0132374
Souri, N., Moghadam, A. N., & Shahbolaghi, M. (2020). Iranian physiotherapists’ perceptions of the ethical issues in everyday practice. Iranian Rehabilitation Journal, 18(2), 125–136. https://doi.org/10.32598/irj.18.2.221.5
Sturm, A., Edwards, I., Elizabeth Fryer, C., & Roth, R. (2022). (Almost) 50 shades of an ethical situation-international physiotherapists’ experiences of everyday ethics: A qualitative analysis. Physiotherapy Theory and Practice. https://doi.org/10.1080/09593985.2021.2015812
Swisher, L. L., Kessel, G. V., Jones, M., Beckstead, J., & Edwards, I. (2012). Evaluating moral reasoning outcomes in physical therapy ethics education: stage, schema, phase, and type. Physical Therapy Reviews, 17(3), 167–175. https://doi.org/10.1179/1743288X12Y.0000000011
Tan, C. H. (1989). Confucianism and nation building in Singapore. International Journal of Social Economics, 16(8), 5–16. https://doi.org/10.1108/03068298910133106
Triezenberg, H. L., & Davis, C. M. (2000). Beyond the code of ethics: Educating physical therapists for their role as moral agents. Journal of Physical Therapy Education, 14(3), 48–58. https://doi.org/10.1097/00001416-200010000-00009
Vaismoradi, M., Turunen, H., & Bondas, T. (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing and Health Sciences, 15(3), 398–405. https://doi.org/10.1111/nhs.12048
Yang, S., Shek, M. P., Tsunaka, M., & Lim, H. B. (2006). Cultural influences on occupational therapy practice in Singapore: a pilot study. Occupational Therapy International, 13(3), 176–192. https://doi.org/10.1002/oti.217
*Audrey Lim
Health and Social Sciences Cluster
Singapore Institute of Technology (SIT)
10 Dover Road
Singapore 138683
+65 6592 3390
Email: Audrey.Lim@SingaporeTech.edu.sg
Submitted: 26 May 2022
Accepted: 10 June 2022
Published online: 4 October, TAPS 2022, 7(4), 86-87
https://doi.org/10.29060/TAPS.2022-7-4/LE2816
Tomoko Miyoshi1, Fumiko Okazaki2, Jun Yoshino3, Satoru Yoshida4, Hiraku Funakoshi5, Takayuki Oto6 & Takuya Saiki7
1Department of General Medicine, Kurashiki Educational Division, Graduate School of Medicine Dentistry and Pharmaceutical Sciences, Okayama University, Japan; 2Center for Medical Education, The Jikei University School of Medicine, Japan; 3Department of Physical Therapy, Faculty of Health and Medical Science, Teikyo Heisei University, Japan; 4Emergency and Critical Care Medical Center, Niigata City General Hospital, Japan; 5Department of Emergency and Critical Care Medicine Tokyobay Urayasu Ichikawa Medical Center, Japan; 6Department of General Dental Practices, Kagoshima University Hospital, Japan; 7Medical Education Development Center, Gifu University, Japan
Dear Editor,
We are delighted to report that the Japanese translated version of R2C2 (relationship, reaction, content, coaching) was published in the Journal of Medical Education in Japan, under kind permission of the author and Journal of Academic Medicine. The R2C2 model, developed by Sargeant et al. (2015), promotes behavior change through reflection and feedback, while incorporating coaching. The effectiveness and influencing factors have been demonstrated in supervisor–resident pairs in various residency programs (family medicine, psychiatry, internal medicine, surgery, and anesthesiology) in the U.S., Canada, and the Netherlands. The R2C2 model is fascinating since it emphasises the relationship and dialogue between the resident and the supervisor, and provides insights into the residents’ in-depth learning.
While we are interested in factors that influence feedback, common across different specialties and contexts, we hypothesise that national culture and health profession disciplines may affect the dialogue and impact of the R2C2 model, especially in bridging the gap between self-assessment and supervisor’s assessment.
Reports of such cultural differences demonstrate the Japanese learning more from their failures, while Westerners learning more from their successes, as well as differences in learners’ self-evaluation. In addition, Hofstede reports that the relationship between learners and teachers in East Asia, including Japan is hierarchical, and feedback is therefore likely to be one-sided. Regarding mentoring/coaching, we have revealed that Japanese physician–scientist relationships are dependent on trust in mentors, and the cultural influence of acceptance of paternalistic mentoring (Obara et al., 2021) suggests the need for building trusting relationships. Furthermore, we as multidisciplinary author teams are keen to explore how different health profession disciplines shape the different perspectives on effective feedback and supervisor–learner relationship. We expect this topic to become more apparent as modern health services are becoming more multi-professional and the discourse may develop in a multi-professional relationship.
The Japanese version has been cautiously translated and published to overcome any issue involving translation. Although we had successfully conducted the nationwide workshop on R2C2 in Gifu, Japan in 2021 to disseminate its philosophy, we realised variety of factors should affect when we conduct R2C2 in our context. Our future goal is to examine the utility of R2C2 model in cross-cultural settings as well as cross-disciplinary situations in order to generate findings that will contribute to the glocalisation of medical education and multi-disciplinary education.
Notes on Contributors
T Miyoshi conceptualised and wrote the manuscript and approved the final version.
F Okazaki conceptualised cultural difference of R2C2 and revised and approved the manuscript.
H Funakoshi conceptualised cultural difference of R2C2 and revised and approved the manuscript.
T Oto conceptualised different health profession disciplines of R2C2 and approved the manuscript.
J Yoshino conceptualised different health profession disciplines of R2C2 and approved the manuscript.
S Yoshida conceptualised different health profession disciplines of R2C2 and approved the manuscript.
Prof T Saiki supervised and edited the manuscript.
Acknowledgement
We would like to acknowledge Rintaro Imafuku, Kaho Hayakawa, Chihiro Kawakami in Gifu University Medical Education Development Center, for writing and editing the Japanese translated version of R2C2 collaboratively.
Funding
There is no funding provided.
Declaration of Interest
There is no conflict of interest, including financial, consultant, institutional or otherwise for the author.
References
Obara H, Saiki T, Imafuku R, Fujisaki K, & Suzuki Y. (2021). Influence of national culture on mentoring relationship: a qualitative study of Japanese physician-scientists. BMC Medical Education, 21, 300. https://doi.org/10.1186/s12909-021-02744-2
Sargeant J, Lockyer J, Mann K, Holmboe E, Silver I, Armson H, Driessen E, MacLeod T, Yen W, Ross K, & Power M. (2015). Facilitated Reflective Performance Feedback: Developing an Evidence- and Theory-Based Model That Builds Relationship, Explores Reactions and Content, and Coaches for Performance Change (R2C2). Academic Medicine, 90(12), 1698-1706. https://doi.org/10.1097/ ACM.0000000000000809
*Tomoko Miyoshi
2-5-1 Shikata-cho, Kita-ku,
Okayama, Japan, 700-8558
+81-86-235-7342
Email: tmiyoshi@md.okayama-u.ac.jp
Submitted: 9 May 2022
Accepted: 3 August 2022
Published online: 4 October, TAPS 2022, 7(4), 83-85
https://doi.org/10.29060/TAPS.2022-7-4/CS2808
Chi Sum Chong1 & Woei Yun Siow2
1Yong Loo Lin School of Medicine, National University of Singapore, Singapore, 2Raffles Hospital, Singapore
I. INTRODUCTION
The AO foundation aims to improve patient outcomes in the surgical treatment of trauma and musculoskeletal disorders and promote education and research. Yearly, approximately 30,000 Orthopaedics surgeons worldwide attend AO foundation courses. To ensure that the planned curriculum is delivered, the AO foundation requires its surgeon-faculty to attend the Faculty Education Program (FEP) before teaching at regional and international courses.
FEP participants are AO member-surgeons who are actively teaching within their own countries. They are selected by their local AO committees and invited to attend. Every participant is encouraged to teach at regional and international courses thereafter.
II. METHODS
Course structure:
- Five weeks of online learning
This includes a self-assessment. Thereafter, participants learn through reading assignments, case studies and peer discussion at their own pace. These provide a problem-based and collaborative approach to learning. Most participants experience the same planned curriculum. Participants from locations with poor internet signals require a modified delivery of the curriculum e.g. email and hard copies.
- One-and-a-half days of live event
This begins with a group discussion to derive the core principles of effective learning from one’s learning experiences. This is followed by an “introduction to the Pendleton method of giving and receiving feedback”. Thereafter, each participant presents a lecture, conducts a small group discussion and demonstrates teaching of a practical session through role playing. For each activity, each participant receives feedback from the other participants and the faculty (Benton & Young, 2018). The event concludes with feedback to evaluate the course. Face-to-face learning activities are contextual and allow for learning of knowledge and skills of teaching strategies in a collaborative fashion. The online and face-to-face curriculum follow the SPICES model and align with the learning outcomes (Harden et al., 1984).
- One week of online follow-up with a post-course self-assessment.
The learning outcomes are:
- Prepare and present a lecture
- Moderate a small group discussion
- Instruct in practical exercises
- Receive and give feedback
- Evaluate one’s own teaching
- Work with outcomes in teaching strategies
- Set expectations of a teaching or learning activity
- Use information about learners e.g. learners’ needs and cultural context in the educational process
- Motivate learners
- Encourage interaction among learners
The outcomes encompass knowledge and skills in teaching and awareness of best practice guidelines in teaching strategies i.e. attitudinal domain. They are specific, relevant and timely for the participants who are young surgeons interested in teaching (Harden et al., 1999).
Some outcomes are easily measurable e.g. prepare and present a lecture, moderate a small group discussion, instruct in practical exercises and receive and give feedback. Participant performance is measured against a set of guidelines (Kogan et al., 2009). Some outcomes are embedded within the learning activities e.g. set outcomes and expectations in learning activities, motivate learners and encourage interaction among learners and evaluate one’s own performance. Some outcomes are not easily measurable e.g. using learner information to plan learning activities. Overall, Kirkpatrick’s level three achievement is met in most outcomes.
For outcomes that cannot be easily measured during the course, longitudinal assessment of the participants will allow these outcomes to be measured i.e. when they teach at future AO courses after the FEP. Thus, entrustable professional activities from the FEP are aligned with the course outcomes (Shorey et al., 2019).
Feedback was gathered from participants attending the FEP courses where the author Siow was one of the faculty. All participants verbally consented to give feedback. A total of 103 participants attended six FEP courses between 2016 to 2019. The response rate was 100%. Achievement of course outcomes was measured using three categories ranging from “not achieved” to “fully achieved”. Faculty effectiveness, content relevance and overall course impact were assessed using five categories ranging from “not at all effective” to “very effective”.
According to the Canton Zurich Ethical commission, this study does not require an authorisation from the ethics committee (BASEC-Nr. Req-2022-00536).
III. RESULTS
Eighty percent or more of graduates agreed that the following outcomes were fully achieved: prepare and present a lecture, moderate a small group discussion, instruct in practical exercise, encourage interaction, work with outcomes in teaching strategies, set expectations and evaluate one’s own teaching.
Seventy-five to seventy-eight percent of graduates agreed that the following outcomes were fully achieved: motivate learners, receive and give feedback and manage time and logistics.
Sixty-six percent of graduates agreed that the following outcome was fully achieved: using learner’s information in the educational process.
Ninety-five to ninety-eight percent of graduates agreed that the faculty, the course content and the overall course impact were very effective.
IV. DISCUSSION
A large majority of the participants were able to fully achieve these outcomes: prepare and present a lecture, moderate a small group discussion, instruct in practical exercise, encourage interaction, work with outcomes in teaching strategies, set expectations and evaluate one’s own teaching. This is likely because these outcomes are more familiar to the participants.
Seventy-five to seventy-eight percent of graduates agreed that the following outcomes were fully achieved: motivate learners, receive and give feedback and manage time and logistics. The achievement rate for this group of outcomes is slightly lower than the previous group of outcomes possibly because these outcomes are less familiar to the participants. Furthermore, the AO method of giving and receiving feedback presents a new concept and practice to many participants.
Sixty-six percent of graduates agreed that the following outcome was fully achieved: using learner’s information in the educational process. One reason for this lower score may be because the application of this outcome was not specifically highlighted and explained to the participants. This outcome was strictly adhered to and applied in the planning and the execution of the very FEP course attended by the participants, but the manner in which participant’s information was used to do so was not clearly explained to the participants themselves.
V. CONCLUSION
The FEP is a rare opportunity for surgeon-educators to learn about scholarly teaching. Feedback from the courses support the continuation of these courses to help faculty improve their teaching skills.
Notes on Contributors
Chi Sum Chong reviewed the literature, performed data analysis and developed the manuscript. Woei Yun Siow reviewed the literature, designed the study, performed the data collection and wrote the manuscript. All authors read and approved the final manuscript.
Funding
This work has not received any external funding.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Benton, S. L., & Young, S. (2018). Best practices in the evaluation of teaching. IDEA paper No. 69.
Harden, R. M., Crosby, J. R., & Davis, M. H. (1999). AMEE Guide No. 14: Outcome-based education: Part 1-An introduction to outcome-based education. Medical Teacher, 21(1), 7-14. https://doi.org/10.1080/01421599979969
Harden, R. M., Sowden, S., & Dunn, W. R. (1984). Educational strategies in curriculum development: The SPICES model. Medical Education, 18(4), 284-297.
Kogan, J. R., Holmboe, E. S., & Hauer, K. E. (2009). Tools for direct observation and assessment of clinical skills of medical trainees. A systematic review. Journal of the American Medical Association, 302(12), 1316-1326.
Shorey, S., Lau, T. C., Lau, S. T., & Ang, E. (2019). Entrustable professional activities in health care education: A scoping review. Medical Education, 53(8), 766-777.
*Woei Yun Siow
Raffles Hospital,
585 North Bridge Road,
Singapore 188770
Email: siowwoeiyun@gmail.com
Submitted: 14 April 2022
Accepted: 3 August 2022
Published online: 4 October, TAPS 2022, 7(4), 76-82
https://doi.org/10.29060/TAPS.2022-7-4/CS2780
Eusni RM Tohit1, Fauzah A Ghani1, Hizmawati Madzin3, Intan N Samsudin1, Subashini C Thambiah1, Siti Z Zakariah2 & Zainina Seman1
1Department of Pathology, Faculty of Medicine & Health Sciences, Universiti Putra Malaysia, Malaysia; 2Department of Medical Microbiology, Faculty of Medicine & Health Sciences, Universiti Putra Malaysia, Malaysia; 3Department of Multimedia, Faculty of Computer Science & Information Technology, Universiti Putra Malaysia, Malaysia
I. INTRODUCTION
Twenty first century learning requires analytical thinking and problem solving; hence, medical educators must design suitable model to prepare learners for challenges in future. Medical teaching and learning are moving towards this direction and use of technology in education is embedded in the process. The role of laboratory testing in patients care is recognised as a critical component of modern medical care (Smith et al., 2010). Ability of practicing physicians to appropriately order and interpret laboratory tests is declining and little attention was given to appropriate medical student education in pathology (Smith et al., 2010).
Clinical Pathology (CP) is a module recently introduced in our medical programme. In depth learning of pathology requires learners to identify appropriate tests and specimen containers, interpret patients’ results with consideration of other factors that may influence them.
Design thinking skills (DTS) is a guided process of thinking where learners’ work in a team and work through to identify problems (patient case), analyse through collaborative learning, provide justification for investigation, interpretation of results, and outline relevant effective management. Experiential learning emphasises the central role of the learners in the educational process by allowing the learner to draw own conclusions and ruminate on meaning of the learned material (Clem et al., 2014). Blending DTS and experiential learning creates a holistic approach to the learning of CP.
II. METHODS
A pilot study was executed amongst year 3 medical students in the Faculty of Medicine and Health Sciences, University Putra Malaysia, Serdang, Selangor, Malaysia. The study was approved by Ethics Committee for Research Involving Human Subjects, Universiti Putra Malaysia, (JKEUPM-2019-387). It was conducted over a span of two months outside students’ formal teaching and learning. Inclusion criteria include students who in clinical years and never been expose to Clinical Pathology module. Students were divided into small groups of either 4 or 5 students, and all were equipped with the CP app (Appendix 1) in Android smartphone together with DTS task book. Each group had a clinical pathologist facilitating the four hybrid sessions (physical and online) due to the global pandemic. In brief, phases involved introduction to CP (empathy), case findings (define), laboratory workup (ideation), results interpretation (solution), case approach (prototype), critical analysis (reflection and post-mortem). [Details in Appendix 2]. These were then presented in the final phase of DTS in a simulated grand ward round. Learners went through pre and post-test in CP and were asked to evaluate their experiences using a modified 28 items questionnaire (Appendix 3) using Likert scale score; adapted from a validated experiential learning questionnaire (Clem et al., 2014).
III. RESULTS
Twenty students from Medicine and Surgery posting participated in this pilot study, conducted from 27th April 2021 to 26th June 2021. In general, students were very satisfied with the experiential learning project. Responses of experiential learning and score marks were tabulated in Table 1. The 28 items were divided into 4 subheadings; as for the type of environment used, 66% agreed to the hybrid approach used in running of the project. Seventy-five percent agreed on the active participation in different phases of DTS. Eighty-six percent agreed with the relevance of the content of CP in their teaching and learning towards being a medical professional. Over two third of respondents agreed on utility of the CP learning experience be adapted in their future learning. As per for students’ performance (n=20) in pre and post-test OSCE in pathology, students scored significantly higher mark in all items evaluated as seen in Table 1.
Encouraging responses were recorded from some of the respondents as stated below:
“I enjoyed it very much. I received a lot of clarity on how important clinical pathology is after the session. Even after all these sessions, I even read again and again the clinical pathology notes that I have. I feel I can slowly relate my prior knowledge when it comes to clinical.”
Respondent 1
“In my opinion, I think this research project has given me a lot of benefits such as I can know how to correctly fill in the form to order the lab investigation, understand how to choose the correct tube for each lab investigation. I like this project very much as it can help me in this medical field”
Respondent 2
“I am grateful for being part of this research since I learnt a lot from the sessions. I have learnt about the type of lab investigations and blood tube, the sequence of taking blood as well as the phlebotomy techniques from the sessions which may help me in my future medical career.”
Respondent 3
|
Subheading I |
Agree (%) |
Neutral (%) |
Disagree (%) |
|
|
On the environment of Clinical Pathology used in the experiential learning |
66 |
15 |
19 |
|
|
On the active participation and learning of Clinical Pathology |
75 |
14 |
11 |
|
|
On the relevance of the content of Clinical Pathology module |
86 |
3 |
11 |
|
|
On the utility of Clinical Pathology experience in future learning |
68 |
3 |
29 |
|
|
Subheading II |
Pre-test (/5) |
Post-test (/5) |
||
|
Correct selection of specimen container |
0.6 |
3.5 |
||
|
Correct order of blood draw |
2.5 |
4.0 |
||
|
Correct preanalytical variables identified |
0.3 |
3.0 |
||
|
Relevant information in the laboratory form |
2.3 |
4.0 |
||
|
Interpretation of laboratory tests |
3.5 |
4.5 |
||
Table 1. Responses to the questionnaire, pre and post-test score for OSCE in Clinical Pathology
IV. DISCUSSION
The pilot study conducted has shown to be beneficial for the clinical students who participated in the research.
Using Kirkpatrick model (Kirkpatrick & Kirkpatrick, 2021), students in this pilot study achieved level 2 of the model outcome. As Clinical Pathology is a new subject in the amended curriculum, ‘sensitising’ the students to the importance of Clinical Pathology (CP) is achieved.
Small group teaching practised in this pilot study is in line with other schools who used small group teaching which resulted in close relationship between students & facilitator (Smith et al., 2010). The CP app provided self-directed learning on information about laboratory tests which able to improve students’ performance (Smith et al., 2010). When students worked through their own clinical case, this create inquisitive learners as they were able to do clinical correlation with the laboratory findings of their patients.
Disagreement showed by some of the students’ implied the need to improve implementation and running of the project. Students’ learning preferences varies from visual, aural, reading, and kinaesthetic (VARK) and a suitable approach need to be designed to suit spectrum of students.
Post-test OSCE scores showed improvement in common pathology knowledge required from students. This general knowledge will assist them in other clinical postings in future. CP app provided earlier will be useful as self-directed learning. However, there’s still challenges in developing a standardised approach to assessing students’ knowledge and skills in this area (Smith et al., 2010) which is an avenue for future research.
V. CONCLUSION
Students developed more confidence in CP which is useful for future learning experience in other disciplines and future career.
Notes on Contributors
ERT designed the research, developed the CP app storyboard, created the DTS task book, analysed the results, wrote the manuscript. HM developed the CP application, edited the manuscript. FAG, INS, SCT, SZZ, ZS revised the protocol, CP app story board, DTS task book, facilitated the project, edited the manuscript.
Acknowledgement
The authors would like to acknowledge Sufi Firdaus and Rubhan AL Chandran on technical help in assisting the development of CP application and DTS task book.
Funding
This work was supported by Geran Inovasi Pengajaran Pembelajaran2018 /Universiti Putra Malaysia/ Centre of Academic Development (800-2/2/15).
Declaration of Interest
All authors declared there is no conflict of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Clem, J. M., Mennicke, A. M., & Beasley, C. (2014). Development and validation of the experiential learning survey. Journal of Social Work Education, 50, 490-506. https://doi.org/10.1080/1043 7797.2014.917900
Kirkpatrick, J., & Kirkpatrick, W. K. (2021). Introduction to the New World Kirkpatrick model. Kirkpatrick Partners. Retrieved June 7, 2022, from https://www.kirkpatrickpartners.com/wp-content/uploads/2021/11/Introduction-to-the-Kirkpatrick-New-World-Model.pdf
Smith, B. R., Aguero-Rosenfeld, M., Anastasi, J., Baron, B., Berg, A., Bock, J. L., Campbell, S., Crookston, K. P., Fitzgerald, R., Fung, M., Haspel, R., Howe, J. G., Jhang, J., Kamoun, M., Koethe, S., Krasowski, M. D., Landry, M. L., Marques, M. B., Rinder, H. M., . . . Wu, Y. (2010). Educating medical students in laboratory medicine: A proposed curriculum. American Journal of Clinical Pathology, 133(4), 533–542. https://doi.org/10.1309/AJCPQCT9 4S FERLNI
*Eusni Rahayu binti Mohd.Tohit
Department of Pathology,
Faculty of Medicine & Health Sciences,
University Putra Malaysia,
43400 Serdang, Selangor
+60397692379
Email: eusni@upm.edu.my
Submitted: 11 March 2022
Accepted: 10 June 2022
Published online: 4 October, TAPS 2022, 7(4), 73-75
https://doi.org/10.29060/TAPS.2022-7-4/CS2783
Kiyotaka Yasui, Maham Stanyon, Yoko Moroi, Shuntaro Aoki, Megumi Yasuda, Koji Otani & Yayoi Shikama
Centre for Medical Education and Career Development, Fukushima Medical University, Fukushima, Japan
I. INTRODUCTION
Educational strategies that are effective in one culture may not elicit the expected response when transferred across cultures. For instance, discussion-based learning methods such as problem-based learning, which were developed in Western contexts to foster self-directed lifelong learning (Franbach et al., 2019), are not easy for Asian students to adapt to. The quietness of Asian students, noted in multi-national contexts, is not always due to linguistic or cultural literacy barriers (Remedios et al., 2008) and requires contextual deconstruction to enable effective solution generation. In a Japanese context, we have observed how quietness manifests through insufficient question generation and a lack of spontaneous opinion expression in class. Such attitudes may be interpreted by western standards as lacking initiative and critical thinking (Tavakol & Dennick, 2010) but are in line with Japanese social norms and traditional views of learning. Because effective learning through discussion requires cognitive conflict to facilitate conceptual transformation (De Grave et al., 1996), it is necessary to ease the psychological burden experienced by our students when deviating from inherited cultural habits so that they can comfortably express opinions to embrace such conflicts. In this case study we share how we created a supportive environment to enable Japanese medical students to embrace this behavioural change.
Through our understanding of Japanese cultural norms, we hypothesised that student quietness could be attributed to the following: 1) belief that their question is insignificant and a desire not to impose on the time of others; 2) reluctance to express different opinions which might cause conflict; and 3) risk aversion to making incorrect statements. Reasons 1) and 2) reflect Japanese social norms requiring people to always act with consideration for others, while 3) is related to a Confucian-affected traditional view of learning that values humility for one’s imperfection as a driving force to self-cultivation which potentially reinforces embarrassment when giving incorrect statements. We aimed to address the above points by introducing environmental changes to boost student confidence in the significance of their questions and minimise the psychological burden of expressing their opinions during a class on ethical dilemmas.
II. METHODS
The class was undertaken by 256 first-year medical students at Fukushima Medical University in 2018 and 2019, as shown in Figure 1.
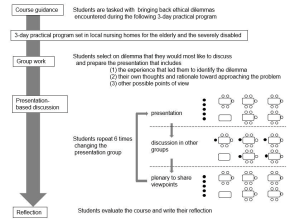
Figure 1. Flow diagram explaining the class: The closed circles represent the presenting group members and their interaction with the rest of the class (open circles) during the discussion and plenary session
A. Building Student Confidence
To minimise the risk aversion and associated anxiety of voicing incorrect opinions, we tasked students to reflect on ethical dilemmas with no clear answer, that they encountered during a 3-day placement in local nursing homes which was presented in groups of 5-6 to the rest of the class. Through removing the expectation of a right answer from the start, we created an atmosphere where students felt comfortable in generating multiple questions rather than being focused on reaching a single ‘correct’ answer.
B. A Conducive Environment for Cognitive Conflict
To break down the barriers of students seeking conformity and agreement during their presentations, we refocused the objective of the session onto the reasoning process of how they considered their ethical dilemma. This reframing supported students to embrace conflicting perspectives without worrying about achieving a consensus.
C. Nurturing a Diversity of Opinions
To facilitate the voicing of minority opinions, we harnessed a positive psychological trait in Japanese culture where pleasure is felt in acting as a collective. Therefore, when opinions were presented to the class, the entire group embraced ownership of the discussion, allowing the individuals who raised the points to remain anonymous. This reduced the potential for personal conflict and allowed diverse opinions to be aired without a loss of face.
At the end of the class, students were asked to evaluate the class using a 4-point Likert scale (good, fairly good, not so good, not good) and to write a reflection on the experience in one to two lines.
III. RESULTS
Out of the 245 students who submitted ratings, 89.9% evaluated the course as “good” or “fairly good”. About half mentioned their surprise at the diversity of opinions and their satisfaction with hearing them, acknowledging that hearing the different perspectives deepened their thoughts, broadened their perspectives, and created new ideas. Satisfaction with being able to express one’s thoughts was stated by a small number of students. Some of the students who chose “not so good” or “not good” pointed out that discussion was tough and required getting used to.
IV. DISCUSSION
When adopting a teaching method developed in a different culture, it should be delivered in the context of one’s own culture to optimise student learning. Once given a supportive environment, Japanese students, previously more content to listen than to actively contribute to discussions, exchanged their ideas and positively encountered cognitive conflict, rather than suffer from low confidence and an aversion to personal conflict. This demonstrates their potential to assimilate different perspectives and advance their thinking, akin to undergoing conceptual transformation. Through this work, we show that the standardisation of teaching methods does not equate to the globalisation of education, but how teaching must be adapted with clear implementation strategies and outcome definition, grounded in the culture to which the learners belong.
V. CONCLUSION
Generalising our adaptations outside of a Japanese context is limited, because of the cultural diversity within Asian countries that brings different challenges to discussion-based learning methods. However, vast numbers of students migrate across cultures in higher education and healthcare training. For universities and clinical training institutions with international students, understanding the barriers and supporting ‘quiet’ students to learn effectively through discussion alongside inherited cultural norms is a priority. This study aids in this understanding by providing an example from a Japanese medical undergraduate context.
Notes on Contributors
Kiyotaka Yasui designed and conducted the course, analysed the student reflections and wrote the manuscript.
Maham Stanyon analysed student reflctions and wrote the manuscript.
Yoko Mori conducted the course facilitation and supported the contextualisation of the results and discussion.
Shuntaro Aoki conducted the course facilitation and supported the contextualisation of the results and discussion.
Megumi Yasuda conducted the course facilitation and supported the contextualisation of the results and discussion.
Koji Otani conducted the course facilitation and supported the contextualisation of the results and discussion.
Yayoi Shikama planned and conducted the course as a course supervisor, analysed the student course ratings and reflections, and wrote the manuscript.
Acknowledgement
The authors would like to thank Dr. Rintaro Imafuku (Gifu University, Gifu, Japan) for constructive advice given during the medical education and research mentoring program sponsored by the Japan Society of Medical Education and Oliver Stanyon for editing a draft of this manuscript.
Funding
This study did not receive any funding.
Declaration of Interest
The authors have no conflict of interest to declare.
References
De Grave, W. S., Boshuizen, H. P. A., & Schmidt, H. G. (1996). Problem based learning: Cognitive and metacognitive processes during problem analysis. Instructional Science, 24, 321-341. http://doi.org/10.1007/BF00118111
Franbach, J. M., Talaat, W., Wasenitz, S., & Martimianakis, M. A. (2019). The case for plural PBL: An analysis dominant and marginalized perspectives in the globalization of problem-based learning. Advances in Health Sciences Education, 24, 931-942. http://doi.org/10.1007/s10459-019-09930-4
Remedios, L., Clarke, D., & Hawthorne, L. (2008). The silent participant in small group collaborative learning contexts. Active Learning in Higher Education 9(3), 201-216. http://doi.org/10.1177/1469787408095846
Tavakol, M., & Dennick, R. (2010). Are Asian international medical students just rote learners? Advances in Health Sciences Education, 15, 369-377. http://doi.org/10.1007/s10459-009-9203-1
*Kiotaka Yasui
1 Hikarigaoka,
Fukushima 960-1295,
Japan
Email: taka-y@fmu.ac.jp
Submitted: 23 November 2021
Accepted: 10 May 2022
Published online: 4 October, TAPS 2022, 7(4), 59-70
https://doi.org/10.29060/TAPS.2022-7-4/OA2714
Deepthi Edussuriya1, Sriyani Perera2, Kosala Marambe3, Yomal Wijesiriwardena1 & Kasun Ekanayake1
1Department of Forensic Medicine, Faculty of Medicine, University of Peradeniya, Sri Lanka; 2Medical Library, University of Peradeniya, Sri Lanka; 3Department of Medical Education, Faculty of Medicine, University of Peradeniya, Sri Lanka
Abstract
Introduction: Emotional Intelligence (EI) is especially important for medical undergraduates due to the long undergraduate period and relatively high demands of the medical course. Determining associates of EI would not only enable identification of those who are most suited for the discipline of medicine but would also help in designing training strategies to target specific groups. However, there is diversity of opinion regarding the associates of EI in medical students. Aim of the study was to determine associates of EI in medical students.
Methods: The databases MEDLINE, CENTRAL, Scopus, EbscoHost, LILAC, IMSEAR and three others were searched. It was followed by hand-searching, cited/citing references and searching through PQDT. All studies on the phenomenon of EI and/or its associates with medical students as participants were retrieved. Studies from all continents of the world, published in English were selected. They were assessed for quality using Q-SSP checklist followed by narrative synthesis on selected studies.
Results: Seven hundred and ninety-two articles were identified of which 29 met inclusion criteria. One article was excluded as its full text was not available. Seven articles found an association between ‘EI and academic performance’, 11 identified an association between ‘EI and mental health’, 11 found an association between ‘EI and Gender’, 6 identified an association between ‘EI and Empathy’ while two have found an association with the learning environment.
Conclusion: Higher EI is associated with better academic performance, better mental health, happiness, learning environment, good sleep quality and less fatigue, female gender and greater empathy.
Keywords: Emotional Intelligence, Associates of Emotional Intelligence, Medical Students, Mental Wellbeing, Empathy
Practice Highlights
- Higher emotional intelligence is associated with better academic performance.
- Higher emotional intelligence is associated with better mental health.
- Higher emotional intelligence is associated with female gender.
- Higher emotional intelligence is associated with greater empathy.
I. INTRODUCTION
Emotional intelligence (EI) is defined as “the ability to perceive emotions accurately, appraise, and express emotion; the ability to assess and/or generate feelings when they facilitate thought; ability to understand emotions and emotional knowledge, and to regulate emotions to promote emotional and intellectual growth” (Mayer & Salovey, 1997). Studies have found that there is a positive effect between EI and academic as well as professional success (Suleman et al., 2019). It has been reported that people and college students with good EI show better social functioning and interpersonal relationship and peers have identified them as less antagonistic and conflictual (Petrovici & Dobrescu, 2014).
Several tests and instruments that have been used to assess the Emotional intelligence of medical students were identified through the literature. These include standard EI tests, modified versions of standard EI tests, and authors’ assessment methods of their own. Schutte self-report EI test, TEIQue questionnaire and Bar-on’s emotional intelligence questionnaire ((EQ-i) 2.0) have been used frequently. Each of these instruments has different advantages and disadvantages of their own.
The Emotional Quotient Inventory (EQ-i) 2.0 is a revision of the EQ-I (Bar-On, 2004). The Emotional Quotient Inventory (EQ-I) 2.0 measures the interaction between an individual and their environment. Since the EQ-i 2.0 is a revision of the original Emotional Quotient Inventory (EQ-I) the standard platform of the EQ-i validation remains intact.
The Schutte Self-Report Emotional Intelligence Test (SSEIT) is a method of measuring general Emotional Intelligence (EI), using four sub-scales: emotion perception, utilising emotions, managing self- relevant emotions, and managing others’ emotions (Schutte et al., 1998). The SSEIT model is closely associated with the EQ-I model of Emotional Intelligence. It has a reliability rating of 0.90. The EI score, overall, is fairly reliable for adults and adolescents. However, the utilising emotions sub-scale has shown poor reliability (Ciarrochi et al., 2001). Also, they report a mediocre correlation of the SSREI with self-estimated EI, the Big Five EI scale, and life satisfaction (Petrides & Furnham, 2000). However, SSREI correlated poorly with well-being and EI criteria.
The Trait Emotional Intelligence Questionnaire (TEIQue), is an openly accessible instrument developed to measure global trait emotional intelligence. Based on the Trait Emotional Intelligence Theory, a significant number of research has been conducted regarding emotional intelligence (EI) (Mikolajczak et al., 2007). The TEIQue is available in long form and short forms. Internal consistency and test-retest both indicated scale reliabilities of 0.71 and 0.76. High correlations between the TEIQue with Shrink’s Emotional Intelligence Scale showed validity in measuring emotional intelligence and the “Big Five” Personality Traits.
Apart from those assessment methods, Genos Emotional Intelligence Assessment, Mayer-Salovey-Caruso Emotional Intelligence Test, TMMS-24 data and DASS-21 scale, Bradbury-Graves’s Emotional Intelligence and Siberia Schering’s Emotional Intelligence Questionnaire have also been used by the authors to assess the EI.
A comprehensive survey in medicine states that EI had a positive contribution in doctor-patient relationship, increased empathy, teamwork, communication skills, stress management, organisational commitment and leadership (Arora et al., 2010). EI is invariably important to medical professionals as it is associated with self-monitoring which would not only ensure adapting to clinical situations appropriately and having desirable interpersonal relations but also result in a favorable outcome for the patient and the wellbeing of the practitioner.
Few studies suggest that EI training can help medical students to build their leadership and empathy skills, as they enter the clinical years (Austin et al., 2005; Dolev et al., 2019). Literature surveys on emotional intelligence and medicine, and physician leadership qualities concludes that EI correlates with many of the competencies that modern medical curricula seek to deliver including leadership (Mintz & Stoller, 2014; Reshetnikov et al., 2020). Other studies indicate that age and gender are associated with emotional intelligence. However, some studies showed that EI at medical school admission could not reliably predict academic success in later years (Reshetnikov et al., 2020). These studies have all looked at the associates in an isolated sense. However, it would also be interesting to reflect on the concept of EI in a broader sense as it is inevitable that there would be an interaction of factors.
The medical course extends over a period of five years as opposed to most undergraduate degrees which are shorter. Medical training involves close interactions with different categories of people including patients, doctors of different grades and the paramedical staff. Training includes long hours of work in stressful environments where some situations could be emotionally challenging. This long undergraduate period and relatively high demands of the medical course would require medical students to possess a high degree of EI. As findings of different studies on EI are sometimes diverse in opinion, it would be useful to conduct a systematic review to identify the associates of EI in order to design training strategies which target specific groups.
Even though EI is considered a trainable trait, the extent of trainability depends on many personal and institutional factors (Mattingly & Kraiger, 2019). Völker (2020) expresses that trainability in emotional intelligence is subjected to acquired knowledge which is situational and may depend on accumulating relevant experience.
In the Sri Lankan context, the sole criteria for selection of students to a medical course is the academic excellence at the Advanced level examination, which alone may not reflect their suitability to follow a profession like medicine (University Grants Commission, 2022).
However, since EI is an essential trait especially for medical practice many universities worldwide use different tools to assess EI in their applicants. Furthermore, different universities adopt varying techniques to develop EI of their students throughout the course. It is envisaged that this review would not only help determine what additional factors could be considered in the selection of applicants for a medical course but would also help teachers design training strategies to target specific groups of students and also ensure a more enjoyable and productive learning experience for the students as a whole. There is no doubt that these selection and intervention programs would produce doctors with more favourable qualities which would not only produce greater benefits to the patient but would prevent burn out among doctors.
A. Objective
The objective of this study is to find out, the associates of Emotional Intelligence in Medical students based on available literature in English from 2015 to 2020.
II. MATERIALS AND METHODS
The research question was defined based on the PICOS (Population, Intervention, Comparison, Outcomes and Setting) format. The review protocol was developed according to PRISMA-P 2015 (Preferred reporting items for systematic review and meta-analysis protocols) statement (Moher et al. 2015) by all three authors DE, KM and SP and was registered in the PROSPERO Registry (CRD42021227877). The methodology for the systematic review (SR) followed the guidelines and standards of IOM (Institute of Medicine) (Eden et al., 2011) and PRISMA-2015 for reporting.
A. Search Strategy
A Systematic and comprehensive search was conducted by SP in April 2020 and references were managed using the software Mendeley. The search explicitly aimed to identify all published and unpublished relevant studies in order to limit bias in the searching process. The key search terms were identified with the aid of a search-term-harvesting table by KM and DE. A combination of relevant medical subject headings and search terms tagged with other appropriate search fields were used in the literature search. The following databases were searched:
CDSR (Cochrane Database of Systematic Reviews), DARE (The Database of Abstracts of Reviews of Effects), MEDLINE (1950- 2020) via Pubmed (See supplemental Appendix 1 for search strategy), CENTRAL (The Cochrane Central Register of Controlled Trials, 1948 – 2020), Scopus, EbscoHost, LILAC, IMSEAR (Index Medicus for South East Asian region) and WHO International Clinical Trials Registry Platform (ICTRP). In addition to electronic searches, two key journals (2015-2020) were hand-searched, and cited & citing references of all included studies were screened for further relevant articles. Searches were limited to studies published between the years 2015-2020. Searching other resources included grey literature such as PQDT (ProQuest Dissertations and Thesis database) and Global health (via WHO).
B. Selection Criteria
After removal of duplicates from the retrieved articles, the remaining articles with abstracts were uploaded to the Web application, Rayyan (Quzzani et al., 2016) for the purpose of screening. The criteria for selection of articles were based on the PICOS elements. The studies were from all continents of the world and limited to those published in English. All studies focusing on the phenomenon of EI and/or its associates with medical students as participants were considered for inclusion in the review.
The authors DE, KM, SP and KE independently screened the uploaded articles in Rayyan, using the above eligibility criteria. In the first phase, title and abstract of each article were reviewed by any of the two authors independently for its candidacy. Following this initial evaluation, the full text of all those selected articles were retrieved and further examined by KM and DE independently (second phase), for the final verification before inclusion in the review. Any disagreements regarding eligibility of studies were resolved by consulting a third author (SP). Reviews, systematic reviews, editorials, letters and comments were removed. Articles which met the eligibility criteria were selected for inclusion in the review. Excluded studies were marked with the ‘reason’ in Rayyan.
C. Data Extraction and Quality Assessment
Data from all included studies were extracted by the review authors YW and KM using a data extraction table developed for the purpose of this review (Appendix 2). Data extracted were cross-checked by SP for any errors. Information recorded included: study details (author, year, country of origin), participants (number of participants, gender, level of undergrad program, etc.), methods (study aim, design, total study duration, tools used), study type (phenomenon /context studied) and outcomes (all relevant findings related to primary and secondary outcomes).
SP and YW independently assessed the quality of those selected studies using Quality Assessment Checklist for Survey Studies in Psychology (Q-SSP) (Protogerou & Hagger, 2020) Results of the quality assessments were compared (Appendix 3); any disagreements were resolved by consensus. Articles which met the required quality criteria were selected for inclusion in the review.
D. Strategy for Data Synthesis
Due to the heterogeneity between the included studies, a quantitative synthesis was not considered. A narrative synthesis of the findings from individual included studies was carried out by DE, based on the characteristics of the targeted populations and the type of outcome such as association/correlation of EI with academic performance, professional success, social functioning, interpersonal relationship, empathy, teamwork spirit, communication skills, stress management, organizational commitment, leadership quality, self-monitoring, mental health and emotional well-being.
III. RESULTS
A total of 792 articles were retrieved during the literature search. After removing the duplicates, 752 articles were considered for screening using the eligibility criteria. Initial evaluation of articles through title and abstract resulted in only 29 articles meeting the selection criteria. During the full-text evaluation, one article (Parijitham, 2018) was removed, as its full-text article could not be found even after contacting the author. The data that support the findings of this study are openly available at https://doi.org/10.6084/m9.figshare.15564210 (Edussuriya et al., 2021). Twenty-eight articles were finally selected for quality assessment. Flow diagram of the selection of studies is shown in Figure 1.
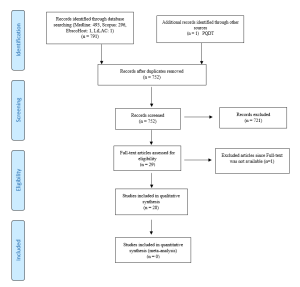
Figure 1. Flow diagram illustrating included and excluded studies in the systematic review
The study design of the selected studies comprised of 26 cross sectional (majority), one longitudinal and one quasi-experimental. However, all studies used standard validated survey questionnaires to collect data. Therefore, to assess the quality of selected studies, Quality Assessment Checklist for Survey Studies in Psychology (Q-SSP) was selected as the best, ‘applicable to all’ tool in this review, considering its relevance also to the trait emotional intelligence since emotions, thoughts and mental processes are aspects of psychology. The quality of the studies was determined by the extent to which the items on above checklist were met by each of the articles. There were 20 checklist items in the tool out of which one item (item-19 – Debriefing participants at the end of data collection) could be justifiably waived; one reason being none of the included studies used it in the methodology. Thus 19 items were considered to be applicable in this review (Appendix 4).
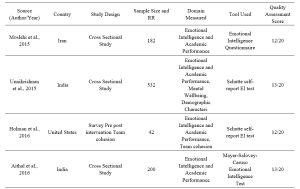



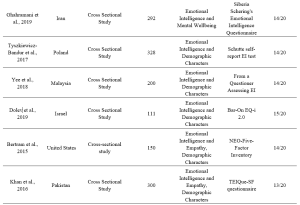

Table 1. Characteristics of included studies
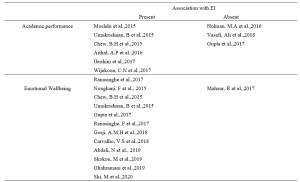

Table 2. Categorisation of findings of the studies
A. Findings of Studies and Data Analysis
1) EI and academic performance: According to studies, a positive correlation was identified between EI and academic performance (Aithal, et al., 2016, Ibrahim et al. 2017; Moslehi et al., 2015, Wijekoon et al., 2017) while (Ranasinghe et al., 2017; Unnikrishnan et al., 2015) also found a significant association between EI and academic performance. These studies indicated that students with higher EI intend to perform better in their academic work. A cross-sectional study done by Chew et al. (2015) showed that medical students with less emotional intelligence were largely unaware of their anxiety, which was associated with lower academic performance. According to studies done by Holman et al., 2016, Gupta et al., 2017 and Vasefi et al., 2018 there was no correlation of EI with academic performance. A study by Othman et al., 2020 revealed that EI showed a significant positive effect on intuitive decision-making style and a negative effect on avoidant and dependent decision-making styles which may explain better academic performance of medical students with high EI.
2) EI and mental health (emotional wellbeing): A direct relationship between EI and academic satisfaction was found in studies done by Rouhani et al., 2015, Unnikrishnan et al., 2015 and Carvalho et al., 2018. Further, Carvalho et al., 2018 reported that a positive relationship was observed between EI and academic-related well-being which accounts for both academic performance and mental health. It was seen that medical students with less emotional intelligence were largely unaware of their anxiety (Chew et al., 2015) and those with higher emotional intelligence perceived lesser stress (Gupta et al., 2017 and Ranasinghe et al., 2017). Shi and Du (2020) found that EI was strongly and negatively associated with Personal Distress. Heidari Gorji et al. (2018) identified a direct relationship between emotional intelligence and mental health while a study done by Mahaur et al. (2017) did not find a significant relationship between the two. Ghahramani et al. (2019) identified a significant positive relationship of EI with happiness while Abdali et al. (2019) showed a positive correlation with sleep quality and a negative correlation with general fatigue.
3) EI and demographic characters: Higher EI in females compared to males was found (Aithal et al., 2016, Bertram et al., 2015, Ibrahim et al., 2017, Khan et al., 2016, Raut & Gupta, 2019 Sundararajan and Gopichandran, 2018, Tyszkiewicz-Bandur et al., 2017, Unnikrishnan et al., 2015 and Wijekoon et al., 2017). Irfan et al. (2019) suggests that female medical students had significantly higher empathic behavior and emotional intelligence than male students. However, Skokou et al. (2019) did not find any difference in EI in males and females. Vasefi et al. (2018) and Abe et al. (2018) too did not find a significant relationship between EI and gender. However, Abe et al. (2018) revealed that females showed significantly higher Neuroticism, Agreeableness and Empathy scores than males. According to Ibrahim et al. (2017) increasing age resulted in higher EI. However, Yee et al. (2018) did not find a significant association of EI with age. According to Yee et al. (2018) there was no significant association of EI with ethnicity.
4) EI and empathy: Significant correlation between EI and Empathy was identified (Bertram et al., 2015, Irfan et al., 2019 Khan et al., 2016; Sundararajan & Gopichandran, 2018). Shi and Du (2020) suggests that EI helps medical professionals to establish a better association with the patient.
5) Learning environment: Relationship between EI and academic background was identified by both Irfan et al. (2019) and Sundararajan and Gopichandran (2018). According to Sundararajan and Gopichandran (2018), students who attended government schools for high school education had greater emotional intelligence than students from private schools. But Irfan et al. (2019) suggests that medical students of private medical schools showed higher level of empathy as compared to public medical schools. Dolev et al. (2019) reveals that there are no differences in EI levels between first-year and sixth-year medical students.
IV. DISCUSSION
The review included studies conducted in South and Southeast Asian, European, Arabian, North American and South American countries. Majority of studies on Asian students revealed a high association between EI and academic performance. However, two studies on Asian students and one on US students failed to observe such associations. The impact of EI on academic performance may be explained by the fact that being aware of one’s anxiety relieved stress and those with high EI experienced greater mental wellbeing and satisfaction with their programs; which may contribute to better academic performance. Furthermore, the fact that EI showed a positive correlation with better mental health/wellbeing, less perceived stress/distress, happiness, good sleep quality and less fatigue may account for the better academic performance of students with high EI.
Empathy is an important aspect in the delivery of high-quality healthcare. Several researchers from different regions of the world reported strong association between empathy and high EI scores. Therefore, assessment of EI may be useful in admitting students for medical degrees. However, since EI is considered as a “trainable trait”, the role that EI plays in admitting students to medical schools is debatable. Therefore, all efforts must be taken by medical schools to include activities that enhance EI, during the medical course, irrespective of the EI levels of students on admission. The fact that EI did not improve with seniority does not purely support the fact that EI is not trainable but it maybe those students were not exposed to and not sensitised to activities which enhance EI.
Evidence indicated a positive association between high EI scores and female gender. It maybe postulated that the “nurturing and caring” role assigned by society to the females influence their upbringing. Thereby improving their emotional intelligence.
In conclusion it must be stated that since a majority of studies revealed that higher EI is associated with better academic performance, better mental health and greater empathy and since EI is considered a trainable trait, curricular need to be developed with a view to improving EI.
In order to develop EI, curricular should contain programs on general leadership development, self-care/ wellness and burn-out prevention (Monroe & English, 2013). Small-group experiential learning activities and meeting with trained mentors throughout the years would be helpful. Debriefing sessions and maintaining a journal are some other techniques that need to be considered. It may be helpful to discuss change management and quality improvement with students (Audra et al., 2020). Exposure of students to skills of self-awareness and self-management through discussion, exposure to theories of conflict management, mindfulness practice, leadership training, discussions on learning styles, discussions on power and influence, identification of team dynamics, exposure to high-functioning inter-professional teams, peer coaching, health care leader interview and shadowing of experienced clinicians are some techniques that could be adopted in attempting to develop EI among students (Kozlowski & Ilgen, 2006). It would be beneficial to evaluate acquisition based on completion of an EI inventory, feedback from peers and staff, project presentations, reflective writing, measurement of achievement of professional and personal development benchmarks and milestones, performance on simulated scenarios and small-group exercises (Pan & Allison, 2010).
During the study it was observed that there is paucity of longitudinal studies on Associates of EI. Therefor it would be beneficial to conduct longitudinal studies which may help identify some aspects with regard to the trainability of EI in medical students.
V. CONCLUSION
Through this review it was revealed that higher EI is associated with
- better academic performance,
- better mental health including less perception of stress and distress, happiness, good sleep quality and less fatigue,
- female gender, and
- greater empathy.
No significant association was found between age, ethnicity, and seniority in the medical course, and emotional intelligence. No conclusions could be made about the association between the nature of the educational institute (private or state) and emotional intelligence.
A. Limitations
In this review, it was found that authors of included studies which used several different tools to assess the EI of medical students. Each of these tools have their own advantages and disadvantages which cause comparison difficult. It could not be assumed that, each and every one of these methods provide results in the same level.
B. Recommendation
Since high EI has shown a positive correlation with academic performance and better mental wellbeing of students and since it has been identified as a “trainable trait” all efforts should be made to enhance EI of medical students during their undergraduate training.
Notes on Contributors
Edussuriya D.H (DE) was the Principal Investigator of the study. Protocol drafting, study selection, analysis and interpretation of data, synthesis of findings of individual studies and the drafting of manuscript was done by the author.
Perera S. (SP) facilitated the methodology, involved in drafting the protocol and retrieved selected articles, since the author has previous experience in conducting systematic reviews. Reference management in Mendeley and Rayyan, cross-checking the extracted data, assessed quality of selected studies and final review of draft was also done by the author.
Marambe K.N (KM) was involved in drafting the protocol, involved in article selection and extracted data from the selected articles.
Wijesiriwardena W.M.S.Y (YW) extracted data from selected articles, assessed the quality of selected articles and finalised the manuscript.
Ekanayake E.M.K.B (KE) has screened the uploaded articles in Rayyan.
Ethical Approval
The review is registered in PROSPERO – The International Prospective Register of Systematic Reviews under the registration number CRD42021227877 for the systematic review.
Data Availability
Data set that support the findings of this study are openly available in Figshare repository https://doi.org/10.6084/ m9.figshare.15564210
Acknowledgement
The authors acknowledge Information Officers of National Science Library and Resources Center, National Science Foundation, Sri Lanka for support in Scopus searches and staff of Medical Library of Faculty of Medicine, University of Peradeniya for the assistance in finding full text articles of the included studies in the review.
Funding
No funding sources are associated with this study.
Declaration of Interest
No conflicts of interest are associated with this paper.
References
Abdali, N., Nobahar, M., & Ghorbani, R. (2019). Evaluation of emotional intelligence, sleep quality, and fatigue among Iranian medical, nursing, and paramedical students: A cross-sectional study. Qatar Medical Journal, 2019(3), 15. https://doi.org/10.5339/qmj.2019.15
Abe, K., Niwa, M., Fujisaki, K., & Suzuki, Y. (2018). Associations between emotional intelligence, empathy and personality in Japanese medical students. BMC Medical Education, 18, Article 47. https://doi.org/10.1186/s12909-018-1165-7
Aithal, A. P., Kumar, N., Gunasegeran, P., Sundaram, S. M., Rong, L. Z., & Prabhu, S. P. (2016). A survey-based study of emotional intelligence as it relates to gender and academic performance of medical students. Education for Health, 29(3), 255–258.
Arora, S., Ashrafian, H., Davis, R., Athanasiou, T., Darzi, A., & Sevdalis, N. (2010). Emotional intelligence in medicine: A systematic review through the context of the ACGME competencies. Medical education, 44(8), 749–764. https://doi.org/10.1111/j.1365-2923.2010.03709.x
Audra, V. W., O’Brien, T. C., Varvayanis, S., Alder, J., Greenier, J., Layton, R. L., Stayart,C. A., Wefes, I., & Brady, A. E. (2020). Applying experiential learning to career development training for biomedical graduate students and postdocs: Perspectives on program development and design. CBE—Life Sciences Education, 19(3), 1-12. https://doi.org/10.1187/cbe.19-12-0270
Austin, E. J., Evans, P., Goldwater, R., & Potter, V. (2005). A preliminary study of emotional intelligence, empathy and exam performance in first year medical students. Personality and Individual Differences, 39(8), 1395-1405. https://doi.org/10.1016/j.paid.2005.04.014
Bar-On, R. (2004). The Bar-On Emotional Quotient Inventory (EQ-i): Rationale, description and summary of psychometric properties. In G. Geher (Ed.), Measuring Emotional Intelligence: Common Ground and Controversy (pp. 115–145). Nova Science Publishers.
Bertram, K., Randazzo, J., Alabi, N., Levenson, J., Doucette, J. T., & Barbosa, P. (2016). Strong correlations between empathy, emotional intelligence, and personality traits among podiatric medical students: A cross-sectional study. Education for Health (Abingdon), 29(3), 186–194.
Carvalho, V. S., Guerrero, E., & Chambel, M. J. (2018). Emotional intelligence and health students’ well-being: A two-wave study with students of medicine, physiotherapy and nursing. Nurse Education Today, 63, 35–42. https://doi.org/10.1016/j.nedt.2018.01.010
Chew, B. H., Hassan, F., & Zain, A. M. (2015). Medical students with higher emotional intelligence were more aware of self-anxiety and scored higher in continuous assessment: A cross-sectional study. Medical Science Educator, 25(4), 421-430. https://doi.org/10.1007/s40670-015-0168-9
Ciarrochi, J., Chan, A. Y., & Bajgar, J. (2001). Measuring emotional intelligence in adolescents. Personality and Individual Differences, 31(7), 1105-1119. https://doi.org/10.1016/S0191-8869(00)00207-5.
Dolev, N., Goldental, N., Reuven-Lelong, A., & Tadmor, T. (2019). The evaluation of emotional intelligence among medical students and its links with non-cognitive acceptance measures to medical school. Rambam Maimonides Medical Journal, 10(2), e0010. https://doi.org/10.5041/RMMJ.10365
Eden, J., Levit, L., Berg, A., & Morton. S. (2011). Finding what works in health care: Standards for systematic reviews. National Academies Press. https://doi.org/10.17226/13059
Edussuriya, D., Perera, S., Marambe, K., Wijesiriwardena, Y., & Ekanayake, K. (2021). Emotional intelligence systematic review (Version 3) [Data Set]. Figshare. https://doi.org/10.6084/m9.figshare.15564210.v3
Ghahramani, S., Jahromi, A. T., Khoshsoroor, D., Seifooripour, R., & Sepehrpoor, M. (2019). The relationship between emotional intelligence and happiness in medical students. Korean Journal of Medical Education, 31(1), 29–38. https://doi.org/10.3946/kjme.2019.116
Gupta, R., Singh, N., & Kumar, R. (2017). Longitudinal predictive validity of emotional intelligence on first year medical students perceived stress. BMC Medical Education, 17(1), 139. https://doi.org/10.1186/s12909-017-0979-z
Heidari Gorji, A. M., Shafizad, M., Soleimani, A., Darabinia, M., Goudarzian, A. H. (2018) Path analysis of self-efficacy, critical thinking skills and emotional intelligence for mental health of medical students. Iranian Journal of Psychiatry and Behavioral Sciences. 12(4), e59487. https://doi.org/10.5812/ijpbs.59487
Holman, M. A., Porter, S. G., Pawlina, W., Juskewitch, J. E., & Lachman, N. (2016). Does emotional intelligence change during medical school gross anatomy course? Correlations with students’ performance and team cohesion. Anatomical Sciences Education, 9(2), 143–149. https://doi.org/10.1002/ase.1541
Ibrahim, N. K., Algethmi, W. A., Binshihon, S. M., Almahyawi, R. A., Alahmadi, R. F., & Baabdullah, M. Y. (2017). Predictors and correlations of emotional intelligence among medical students at King Abdulaziz University, Jeddah. Pakistan Journal of Medical Sciences, 33(5), 1080–1085. https://doi.org/10.12669/pjms.335.13157
Irfan, M., Saleem, U., Sethi, M. R., & Abdullah, A. S. (2019). Do we need to care: emotional intelligence and empathy of medical and dental students. Journal of Ayub Medical College, Abbottabad: JAMC, 31(1), 76–81.
Khan, M. A., Niazi, I. M., & Rashdi, A. (2016). Emotional intelligence predictor of empathy in medical students. Rawal Medical Journal, 41(1), 121-124.
Kozlowski, SWJ., & Ilgen. D.R. (2006). Enhancing the effectiveness of work groups and teams. Psychological Science in the Public Interest, 7(3), 77-124. https://doi.org/10.1111/j.1529-1006.2006.00030.x
Mahaur, R., Jain, P., & Jain, A. K. (2017). Association of mental health to emotional intelligence in medical undergraduate students: Are there gender differences? Indian Journal of Physiology and Pharmacology, 61(4), 383-391.
Mattingly, V., & Kraiger, K. (2019). Can emotional intelligence be trained? A meta-analytical investigation. Human Resource Management Review, 29(2), 140-155. https://doi.org/10.1016/j.hrmr.2018.03.002
Mayer, J. D., & Salovey, P. (1997). What is emotional intelligence? Emotional development and emotional intelligence: Educational implications (pp. 3-31). Basic Books.
Mikolajczak, M., Luminet, O., Leroy, C., & Roy, E. (2007). Psychometric properties of the Trait Emotional Intelligence Questionnaire: Factor structure, reliability, construct, and incremental validity in a French-speaking population. Journal of Personality Assessment, 88(3), 338–353. https://doi.org/10.1080/00223890701333431
Mintz, L. J., & Stoller, J. K. (2014). A systematic review of physician leadership and emotional intelligence. Journal of Graduate Medical Education, 6(1), 21–31. https://doi.org/10.4300/JGME-D-13-00012.1
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., Stewart, L. A., & PRISMA-P Group (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), Article 1. https://doi.org/10.1186/2046-4053-4-1
Monroe, A. D., & English, A. (2013). Fostering emotional intelligence in medical training: The SELECT program. AMA Journal of Ethics, 13(6), 509-513. https://doi.org/10.1001/virtualmentor.2013.15.6.medu1-1306
Moslehi, M., Samouei, R., Tayebani, T., & Kolahduz, S. (2015). A study of the academic performance of medical students in the comprehensive examination of the basic sciences according to the indices of emotional intelligence and educational status. Journal of Education and Health Promotion, 4, 66. https://doi.org/10.4103/2277-9531.162387
Noughani, F., Bayat, R. M., Ghorbani, Z., & Ramim, T. (2015). Correlation between emotional intelligence and educational consent of students of Tehran University of Medical Students. Tehran University Medical Journal, 73(2), 110-116.
Othman, R., El Othman, R., Hallit, R., Obeid, S., & Hallit, S. (2020). Personality traits, emotional intelligence and decision-making styles in Lebanese universities medical students. BMC Psychology, 8(1), Article 46. https://doi.org/10.1186/s40359-020-00406-4
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan- A web and mobile app for systematic reviews. Systematic Reviews, 5(1), Article 210. https://doi.org/10.1186/s13643-016-0384-4
Petrides, K., & Furnham, A. (2000). On the dimensional structure of emotional intelligence. Personality and Individual Differences, 29(2), 313-320. https://doi.org/10.1016/S0191-8869(99)00195-6
Petrovici, A., & Dobrescu, T. (2014). The role of emotional intelligence in building interpersonal communication skills. Procedia-Social and Behavioral Sciences, 116, 1405-1410. https://doi.org/10.1016/j.sbspro.2014.01.406
Protogerou, C., & Hagger, M. S. (2020). A checklist to assess the quality of survey studies in psychology. Methods in Psychology, 3, 100031. https://doi.org/10.31234/osf.io/uqak8
Ranasinghe, P., Wathurapatha, W. S., Mathangasinghe, Y., & Ponnamperuma, G. (2017). Emotional intelligence, perceived stress and academic performance of Sri Lankan medical undergraduates. BMC Medical Education, 17(1), Article 41. https://doi.org/10.1186/s12909-017-0884-5
Raut, A. V., & Gupta, S. S. (2019). Reflection and peer feedback for augmenting emotional intelligence among undergraduate students: A quasi-experimental study from a rural medical college in central India. Education for Health (Abingdon, England), 32(1), 3–10. https://doi.org/10.4103/efh.EfH_31_17
Reshetnikov, V. A., Tvorogova, N. D., Hersonskiy, I. I., Sokolov, N. A., Petrunin, A. D., & Drobyshev, D. A. (2020). Leadership and emotional intelligence: current trends in public health professionals training. Frontiers in Public Health, 7, 413. https://doi.org/10.3389/fpubh.2019.00413
Schutte, N. S., Malouff, J. M., Hall, L. E., Haggerty, D. J., Cooper, J. T., Golden, C. J., & Dornheim, L. (1998). Development and validation of a measure of emotional intelligence. Personality and Individual Differences, 25(2), 167–177. https://doi.org/10.1016/S0191-8869(98)00001-4
Shi, M., & Du, T. (2020). Associations of emotional intelligence and gratitude with empathy in medical students. BMC Medical Education, 20(1), Article 116. https://doi.org/10.1186/s12909-020-02041-4
Skokou, M., Sakellaropoulos, G., Zairi, N. A., Gourzis, P., & Andreopoulou, O. (2019). An exploratory study of trait emotional intelligence and mental health in freshmen Greek medical students. Current Psychology, 40, 6057–6066. https://doi.org/10.1007/s12144-019-00535-z
Suleman, Q., Hussain, I., Syed, M. A., Parveen, R., Lodhi, I. S., & Mahmood, Z. (2019). Association between emotional intelligence and academic success among undergraduates: A cross-sectional study in KUST, Pakistan. PloS one, 14(7), e0219468. https://doi.org/10.1371/journal.pone.0219468
Sundararajan, S., & Gopichandran, V. (2018). Emotional intelligence among medical students: A mixed methods study from Chennai, India. BMC Medical Education, 18(1), Article 97. https://doi.org/10.1186/s12909-018-1213-3
Tyszkiewicz-Bandur M., Walkiewicz M, Tartas M, Bankiewicz-Nakielska J. (2017). Emotional intelligence, attachment styles and medical education. Family Medicine & Primary Care Review, 19(4), 404–407. https://doi.org/10.5114/fmpcr.2017.70127
University Grants Commission, Sri Lanka. (2022). University Admissions. Retrieved April 21, 2022, from https://www.ugc.ac.lk/index.php?option=com_content&view=article&id=25&Itemid=11&lang=en
Unnikrishnan, B., Darshan, B., Kulkarni, V., Thapar, R., Mithra, P., Kumar, N., Holla, R., Kumar, A., Sriram, R., Nair, N., Juanna, Rai, S., & Najiza, H. (2015). Association of emotional intelligence with academic performance among medical students in South India. Asian Journal of Pharmaceutical and Clinical Research, 8(2), 300-302.
Vasefi, A., Dehghani, M., & Mirzaaghapoor, M. (2018). Emotional intelligence of medical students of Shiraz University of Medical Sciences cross sectional study. Annals of Medicine and Surgery, 32, 26–31. https://doi.org/10.1016/j.amsu.2018.07.005
Völker, J. (2020). An examination of ability emotional intelligence and its relationships with fluid and crystallized abilities in a student sample. Journal of Intelligence, 8(2), 18. https://doi.org/10.3390/jintelligence8020018
Wei, P., & Joseph, A. (2011). Implementing and evaluating the integration of critical thinking into problem based learning in environmental building. Journal for Education in the Built Environment, 6(2), 93-115. https://doi.org/10.11120/jebe.2011.06020093
Wijekoon, C. N., Amaratunge, H., de Silva, Y., Senanayake, S., Jayawardane, P., & Senarath, U. (2017). Emotional intelligence and academic performance of medical undergraduates: A cross-sectional study in a selected university in Sri Lanka. BMC Medical Education, 17(1), Article 176. https://doi.org/10.1186/s12909-017-1018-9
Yee, K. T., Yi, M. S., Aung, K. C., Lwin, M. M., & Myint, W. W. (2018). Emotional intelligence level of year one and two medical students of University Malaysia Sarawak: Association with demographic data. Malaysian Applied Biology, 47(1), 203-208.
*Edussuriya D.H
Department of Forensic Medicine, Faculty of Medicine,
University of Peradeniya, Sri Lanka, 20400
+94711698916
Email: deepthi.edussuriya@med.pdn.ac.lk
Submitted: 27 May 2022
Accepted: 10 June 2022
Published online: 4 October, TAPS 2022, 7(4), 71-72
https://doi.org/10.29060/TAPS.2022-7-4/PV2819
Bhuvan KC1,2 & P Ravi Shankar3
1Faculty of Pharmacy and Pharmaceutical Sciences, Monash University, Parkville, Australia; 2College of Public Health, Medical and Veterinary Sciences, James Cook University, Townsville, Australia; 3IMU Centre for Education, International Medical University, Kuala Lumpur, Malaysia
I. INTRODUCTION
Healthcare systems and medicines operate in a complex landscape and constantly interact with individuals, the environment, and society. In such a complex healthcare delivery system, nonlinearity always exists, and treatments, different healthcare services, and medicines cannot be delivered without factoring in the uncertainty brought about by human, behavioural, system, and societal factors.
A medical doctor prescribes medication/s to treat diseases or healthcare problems following certain treatment protocols and guidelines. However, in the community, several factors affect the adherence and outcomes, such as adverse effects, lifestyle factors, socioeconomic aspects, attitudes, and belief systems, so it is difficult to entirely predict the success of a regimen. These factors that can influence the outcomes of therapy have not received adequate attention. Furthermore, the complexity of healthcare delivery is starker in the treatment of ageing populations or those with chronic diseases.
Our world is becoming increasingly complex. Many uncertainties affect the delivery of healthcare services today. There are inherent challenges within the healthcare system such as lack of adequate funding, ageing population, rising burden of chronic diseases, and overstretched health workforce. In addition, newer challenges such as the impact of climate change on health delivery, the use of digital health technologies, the emergence of new epidemics, and questions regarding sustainability make healthcare delivery complex and uncertain. Healthcare systems operate through a network of subsystems such as hospitals and health systems, clinics, primary healthcare networks, rehabilitation centres, pharmacies, hospices, care homes, families, and patients. They interact with each other in a complex way sometimes producing unintended consequences such as adverse reactions, medication errors, unintended hospitalisations, and hospital-acquired infections. Thus, if we view the health system as a complex entity we can appreciate its dynamic behaviour helping us in delivering health services in a self-organized way (Lipsitz, 2012).
There is an urgent need to teach complexity science to undergraduate and postgraduate health sciences students as it better prepares them to deliver healthcare services and medicines to a dynamic and complex society. The healthcare systems we work for and the communities and societies we deliver healthcare services and medicines are complex. Healthcare delivery is disrupted by access to funding and resources, information and communication technology (ICT) applications, healthcare professionals who keep moving in and out of the system, and the increasing burden of chronic diseases and elderly populations needing several healthcare services and medicines. It is difficult to predict the outcome of the healthcare services and medicines that are delivered via both primary and secondary healthcare systems. Furthermore, it is difficult to predict the impact of healthcare services and medicines on patients. A patient may develop an adverse drug reaction to a medication, patient may have different genetic polymorphisms affecting the metabolism of medication or factors such as socioeconomic conditions, education level, support system might affect the way they receive and use healthcare services and medicines. There has been a growing recognition of such complex needs and the biological, psychological, social, and cultural aspects of medicine in the healthcare sciences curriculum (Quintero, 2014). There is also a greater appreciation for the collaborative care and practice model that brings together medical doctors, pharmacists, nurses, and other healthcare professionals together for patient care (Blount et al., 2006). The collaborative care model attempts to implement change in small and manageable cycles, appreciating the complexity involved. We must introduce complexity in medicine and pharmacy teaching and learning by introducing concepts, terminology, and lexicons regarding complexity and uncertainty. Students’ engagement and appreciation of the complexity of healthcare systems and delivery can be assessed through reflective practice, clinical reasoning, and evidence-based practice.
Complexity recognises that relationships may be nonlinear and emphasises the relations and interconnections between different components. Flow, interdependence and the emergence of structures and patterns are emphasised. An acceptance of the non-linear cause and effect relationship is stressed. Evidence-based medicine is based on statistics derived from large populations. Applying the results to an individual patient requires caution. Diagnosis and treatment outcomes are probabilistically determined. With the advent of large data sets the probabilistic nature of medicine is becoming apparent. A particular set of signs and symptoms provides a set of differential diagnosis in either increasing or decreasing order of probability. A variety of social, emotional, and political factors can influence treatment decisions, access to care, and treatment outcomes.
Universities have begun to realise the importance of teaching complexity science to medicine and health sciences students. A study by Jorm et al. (2016) had shown how complexity theory can be used to guide interprofessional learning. It showed how complexity theory can be used to design cases, formats, and assessments and how it enabled students to achieve complex interprofessional learning outcomes (Jorm et al., 2016). Another study by Jorm and Roberts (2018) reported the use of complexity theory to design evaluations with a new focus on developing medical students as future change agents for the transformation of the health system and patients’ lives (Jorm & Roberts, 2018). Several institutions like the Santa Fe Institute (New Mexico, United States) have already begun training programs on complexity in medicine and health care systems. Such programs and training need to be developed and evaluated globally so that medicine and pharmacy students can better tackle the complexity of health systems and the uncertainty around delivering medicines and healthcare in a complex environment. Training students for complexity today can ensure they are better prepared for both current and future challenges.
Notes on Contributors
BKC contributed to the conceptualisation of the manuscript, wrote the first draft, revised the subsequent draft, and contributed to the final draft. PRS contributed to the conceptualisation of the manuscript and critically revised the first draft. The author contributed to the subsequent revision and finalisation of the manuscript.
Funding
No funding has been received for this article.
Declaration of Interest
The authors state that they do not have any conflicts of interest, including financial, consultant, institutional, and other relationships that might lead to bias or a conflict of interest.
References
Blount, A., DeGirolamo, S., & Mariani, K. (2006). Training the collaborative care practitioners of the future. Families, Systems, & Health, 24(1), 111-119. https://doi.org/10.1037/1091-7527.24.1.111
Jorm, C., Nisbet, G., Roberts, C., Gordon, C., Gentilcore, S., & Chen, T. F. (2016). Using complexity theory to develop a student-directed interprofessional learning activity for 1220 healthcare students. BMC Medical Education, 16(1), Article 199. https://doi.org/10.1186/s12909-016-0717-y
Jorm, C., & Roberts, C. (2018). Using complexity theory to guide medical school evaluations. Academic Medicine, 93(3), 399-405. https://doi.org/10.1097/ACM.0000000000001828
Lipsitz, L. A. (2012). Understanding health care as a complex system: The foundation for unintended consequences. JAMA, 308(3), 243-244. https://doi.org/10.1001/jama.2012.7551
Quintero, G. A. (2014). Medical education and the healthcare system-why does the curriculum need to be reformed? BMC Medicine, 12(1), Article 213. https://doi.org/10.1186/s12916-014-0213-3
*P Ravi Shankar
IMU Centre for Education
International Medical University+94711698916
126, Jln Jalil Perkasa 19, Bukit Jalil,
57000 Kuala Lumpur, Malaysia
Email: ravi.dr.shankar@gmail.co
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









