Vertical integration of anatomy and women’s health: Cross campus blended learning
Submitted: 9 May 2022
Accepted: 11 October 2022
Published online: 4 April, TAPS 2023, 8(2), 89-92
https://doi.org/10.29060/TAPS.2023-8-2/CS2806
Vidya Kushare1,2, Bharti M K1, Narendra Pamidi1, Lakshmi Selvaratnam1, Arkendu Sen1 & Nisha Angela Dominic3
1Jeffrey Cheah School of Medicine & Health Sciences (JCSMHS), Monash University, Malaysia; 2Department of Anatomy, Faculty of Medicine, Universiti Malaya, Malaysia; 3Clinical School Johor Bahru (CSJB), Monash University, Malaysia
I. INTRODUCTION
For safe practice of medicine, proficiency in anatomy is important. Anatomy is mainly taught in the pre-clinical years. Knowledge retention decreases over time and this will affect clinical and practical application during clinical years (Jurjus et al., 2014; Zumwalt et al., 2007). Literature shows that integrating relevant anatomy with clinical teaching will reinforce the basic concepts and fill these knowledge gaps. Rajan et al. (2016) in their study show that integrating neuroanatomy refresher sessions to clinical neurological case discussions was effective in building relevant knowledge.
Monash University practices a vertically integrated curriculum to promote meaningful learning. In a vertically integrated curriculum, clinical and basic sciences are integrated throughout the program, to provide relevance to basic sciences for clinical practice (Malik & Malik, 2010; Wijnen-Meijer et al., 2020).
As part of the clinical skills development, the Women’s Health (WH) team at Monash university Malaysia in 2010 started episiotomy workshops. Episiotomy is a procedural skill, as future doctors working in Malaysia are expected to know. To perform and repair this surgical procedure safely as well as to identify potential complications, an in-depth knowledge of perineal anatomy is essential.
In 2019, the Anatomy and WH team came together to integrate a refresher anatomy component to the ongoing episiotomy workshops. The objective was to reinforce anatomy relevant to the episiotomy procedure to promote meaningful and lifelong learning.
The anatomy component was integrated virtually because the clinical and preclinical campus are located at different sites about 300km apart. The preclinical Sunway campus is located at Bandar Sunway and the Clinical School Johor Bharu (CSJB) campus is located at Johor Bahru.
Our aim was to see if this approach of virtually integrating refresher anatomy components with the episiotomy workshops will be relevant and beneficial to student learning.
II. METHODS
This cross-campus, blended learning approach, a combination of online (anatomy review session) and face-to-face (episiotomy workshops) sessions, was started in 2019 before the COVID-19 pandemic. These integrated sessions were conducted for year 5 medical students during their O&G rotation with each group attending the session only once. The anatomy sessions were remotely conducted by the anatomy team. All practical hands-on training workshops were conducted in the clinical skills lab (CSJB campus) by the WH team for the students attending onsite. The two sites were connected via a web conferencing platform/ application (Zoom).
Before the pandemic, the online anatomy sessions and the hand-on workshops were conducted synchronously. The anatomy session was in the form of a 30-minute lecture demo-presentation using various models, cadaveric plastinated specimens and images. This lecture-demo was broadcast virtually from the Monash Anatomy and Pathology e-Learning (MAPEL) Lab in Sunway campus to the clinical skills lab at CSJB. This was followed by the practical training on performing and repairing episiotomy on mannequins supervised by the WH team (see Appendix A).
During the COVID-19 pandemic, we altered the delivery format of the anatomy component due to the restrictions. The real time virtual anatomy demo-presentation was replaced by a pre-recorded video lecture uploaded to a Moodle learning management system for students to view asynchronously, before attending the workshop. During the workshop, a knowledge assessment quiz (using online polling application) was remotely conducted by the anatomy team. Each question was discussed in detail with explanation and feedback provided by both teams. This was followed by the practical, hands-on training for students attending onsite in the clinical skills lab at CSJB (see Appendix A).
At the end of the sessions, students responded to a voluntary, anonymised online survey questionnaire. The questionnaire consisted of both quantitative questions based on 5-point Likert scale and qualitative open-ended questions.
III. RESULTS
In 2021, we conducted seven integrated workshops, with a total of 59 students attending. Thirty-two students (54%) responded to the survey questionnaire, out of whom the majority (87.5%) had either observed or assisted an episiotomy procedure on real patients. Based on their feedback, most students had viewed the pre-recorded video lectures and found them useful.
As shown in Figure 1 below, 96% agreed that organization and content of pre-learning materials were effective in achieving the learning outcomes, 96% agreed that this approach refreshed their anatomy knowledge, 91% felt that the anatomy sessions were relevant to the episiotomy workshop, 96% agreed that this approach of integrating anatomy was beneficial and 93% found that this approach was effective in their understanding and application in real time practice.
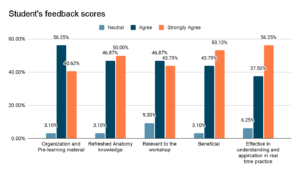
Figure 1. Student responses in evaluating impact (based on a 5-point Likert scale) of virtual integration of relevant anatomy in the episiotomy workshop
Qualitatively, the responses to open-ended questions were grouped as either most or least beneficial. Most beneficial to the students was that it helped them to revise and correlate relevant anatomy, consolidate and highlight the important concepts. Least beneficial to students were the non-clinical aspects, overlapping content between the uploaded lecture video and the real time zoom session, insufficient models and the lack of online engagement. Overall, the students responded positively towards this learning approach.
IV. DISCUSSION
Based on student feedback, more than 90% responded positively towards this virtual integrated approach of reviewing relevant anatomy during the hands-on workshop. This just-in-time’ review approach, even when conducted virtually, allows them to focus on applying only pertinent knowledge to the hands-on session and subsequently when dealing with real-time episiotomy repair on patients.
The limitations of the study include the internet network bandwidth at the two distant sites and the restrictions posed by the ongoing COVID-19 pandemic. Replacing the live anatomy demonstrations, time constraints, social distancing and the use of face shields/face masks made online interactions more challenging.
V. CONCLUSION
This is an ongoing project, requiring further evaluation to assess the impact of this pre-internship training strategy on key procedural skills learning and future practice that is expected in obstetrics.
To conclude, incorporating relevant, refresher anatomy sessions into clinical teaching, even when held virtually, can benefit students to review the core concepts of basic sciences and apply it to clinical practice. This allows for the development of clinical skill competency and ultimately safe patient care.
Notes on Contributors
Vidya Kushare initiated and designed the project, conducted the virtual anatomy review sessions, prepared the video, the quiz and the feedback questionnaire, performed the data collection and data analysis, wrote the manuscript and presented this in a conference.
Bharti M K was involved in the design of the project, conducted the virtual anatomy review sessions, prepared the video and edited the manuscript.
Narendra Pamidi was involved in the design of the project, editing the manuscript and providing references.
Lakshmi Selvaratnam was involved in the planning and development of the project, providing references, providing feedback, writing and editing the manuscript.
Arkendu Sen was involved in the design of the project, providing feedback, editing the manuscript and providing references.
Nisha Angela Dominic initiated and designed the project, conducted the hands-on workshop sessions, prepared the quiz and the feedback questionnaire, performed the data collection, editing the manuscript and providing references.
All the authors have read and approved the final manuscript.
Acknowledgement
The authors acknowledge the technical teams from both campuses: Mr Mah, Ms Nurul, Ms Zafrizal & Mr Abisina.
Funding
The authors received no financial support for this study.
Declaration of Interest
The authors have no conflict of interest.
References
Jurjus, R. A., Lee, J., Ahle, S., Brown, K. M., Butera, G., Goldman, E. F., & Krapf, J. M. (2014). Anatomical knowledge retention in third-year medical students prior to obstetrics and gynecology and surgery rotations. Anatomical Sciences Education, 7(6), 461–468. https://doi.org/10.1002/ase.1441
Malik, A. S., & Malik, R. H. (2010). Twelve tips for developing an integrated curriculum. Medical Teacher, 33(2), 99–104. https://doi.org/10.3109/0142159x.2010.507711
Rajan, S. J., Jacob, T. M., & Sathyendra, S. (2016). Vertical integration of basic science in final year of medical education. International Journal of Applied & Basic Medical Research, 6(3), 182–185. https://doi.org/10.4103/2229-516X.186958
Wijnen-Meijer, M., van den Broek, S., Koens, F., & ten Cate, O. (2020). Vertical integration in medical education: The broader perspective. BMC Medical Education, 20(1). https://doi.org/10.1186/s12909-020-02433-6
Zumwalt, A. C., Marks, L., & Halperin, E. C. (2007). Integrating gross anatomy into a clinical oncology curriculum: The oncoanatomy course at Duke University School of Medicine. Academic Medicine, 82(5), 469–474. https://doi.org/10.1097/acm.0b013e31803ea96a
*Vidya Kushare
Jln Profesor Diraja Ungku Aziz,
50603 Kuala Lumpur,
Wilayah Persekutuan, Malaysia
+60162440142
Email: vidyakusharee@gmail.com / vidyakushare@um.edu.my
Submitted: 4 May 2022
Accepted: 16 August 2022
Published online: 4 April, TAPS 2023, 8(2), 86-88
https://doi.org/10.29060/TAPS.2023-8-2/SC2804
Sok Mui Lim1,2 & Chun Yi Lim2,3
1Centre for Learning Environment and Assessment Development (CoLEAD), Singapore Institute of Technology, Singapore; 2 Health and Social Sciences, Singapore Institute of Technology, Singapore; 3Department of Child Development, KKH Women’s and Children’s Hospital, Singapore
I. INTRODUCTION
Interactive oral assessment has been identified as a form of authentic assessment that enables students to develop their professional identity, communications skills, and helps promote employability (Sotiriadou et al., 2020). It simulates authentic scenarios where assessors can engage students in genuine and unscripted interactions that represents workplace experiences (Sotiriadou et al., 2020). Unlike written examinations, interactive oral questions are not rigidly standardised as students and assessors role-play using workplace scenarios, enabling students to respond to the conversational flow and achieve authenticity (Tan et al., 2021). Using Villarroel et al. (2018) four-step ‘Model to Build Authentic Assessment’, this paper will present the use of oral interactive with first year occupational therapy students. This is within the context of a module named “Occupational Performance Across Lifespan” and students learn about children’s developmental milestones.
II. METHODS
The first step of the Model by Villarroel et al. (2018) is to consider the workplace context. It is important to identify key transferable skills that are needed at typical workplace scenarios. In the job of occupational therapists, they need to meet with caregivers and address their concerns. The key transferable skills include determining whether there is delay in a child’s developmental milestones, communicating with empathy and articulating practical suggestions for caregivers. Thinking critically and communicating persuasively and empathetically, especially in dynamic situations, are important graduate attributes for our students to prepare themselves for the clinical workforce.
The second step of the Model is to design authentic assessment, which involves (1) drafting a rich context; (2) creating a worthwhile task; and (3) requiring higher order skills. In our assessment, students were given a scenario and asked to discuss developmental milestones with parents, identify whether there were areas of concerns from what was reported and provide suggestions if appropriate.
To do this, we trained standardised “actors” / “parents” to share their concerns and correspond with the student individually. As the assessment took place during the pandemic, we used Zoom for corresponding, like therapists conducting teleconsultations. To promote employment opportunities, we included persons with disability as standardised parents. The students were unaware of the disability such as spinal cord injury, as it was conducted on an online platform. We followed the guide on inclusion of persons with disabilities as standardised patients (Lim et al., 2020). The academic staff took the role of the examiner and focused on listening in to the answers provided and writing down feedback for each student.
The third step involves developing the assessment criteria and standard in the form of rubrics and familiarising students with them. To prepare the students, five weeks before the actual assessment, we explained what oral interactive assessments were and introduced the rubrics. They watched videos of one high performing student and one who struggled from previous cohort (with permission sought). They discussed what went well and where the gaps were, followed by pairing up to practice. This helped the students to understand the expected standard, visualise how the oral interactive will take place and learn to evaluate. Three weeks before the assessment, students were given some mock scenarios to practice, and suggestions from the previous cohort on how best to prepare for the assessment.
The fourth step relates to feedback. Feedback can enable students to judge future performances and make improvements within the context of individual assessment. After the assessment, each student was given individual written feedback. The cohort was given group feedback on what they did well and some of the common mistakes. Students who needed more detailed feedback were also given the opportunity to be coached by the Module Lead. At coaching-feedback sessions, the student will watch their video, pause, coached on what they notice, what was done well, and how they can do differently in future. Such feedback sessions are viewed as a coachable moment for educators to develop students in their competency (Lim, 2021).
III. RESULTS
We conducted oral interactive assessments with persons with disability as standardised parents for two cohorts of students (n>200). From the anonymous module feedback, we learnt that students appreciated the assessment as it has real world relevance and enable them to gain professional skills. Some appreciated the opportunity to experience what it felt like interacting with caregivers at their future workplaces. We also noted some students expressed they were more anxious preparing for the oral interactive compared to other forms of assessments. Students shared that they prepared the assessment by remembering the developmental milestones and practise verbalising the concepts out loud with their peers.
IV. DISCUSSION
Students need time to be prepared for a new form of assessment as they may be more familiar with pen and paper examination or report. A few recommendations are suggested:
1) To reduce their anxiety, early preparation is important. Performance anxiety was a common stumbling block. Supporting students in learning strategies to manage performance anxiety can help.
2) For the assessment conversation to be natural, it is important to train the standardised actors on reactions for hit and missed responses from the students.
3) To maintain integrity of the assessment, different scenarios of similar level of difficulties were needed. Educators emphasised the value of learning from the assessment and individualised feedback, such that experience itself becomes intrinsically rewarding.
4) The educator plays the role of the examiner and concentrates to note down the quality of the answers and writes down feedback for each student.
5) Scaffolding students for continuous practice towards workplace competence is important. It is recommended to plan other authentic assessments in the later years of the curriculum such as OSCE.
V. CONCLUSION
Oral interactive assessment provides students with the opportunity to practice and be assessed on workplace competency. While students find themselves more anxious in preparing, they appreciate the real-world relevance and the opportunity to gain professional skills. It is worthwhile to spend effort in designing the assessment in detail, planning authentic scenarios, and preparing students for the experience. As an educator, it is rewarding to witness students developing the ability to demonstrate their competency in a professional manner.
Notes on Contributors
Associate Professor Lim Sok Mui (May) contributed to the conception, drafted and critically revised the manuscript.
Dr Lim Chun Yi contributed to the execution of the assessment, drafting and reviewing the manuscript.
All authors gave their final approval and agree to be accountable for all aspects of the work.
Acknowledgement
We would like to acknowledge the help of Mr Lim Li Siong, Dr Shamini d/o Logannathan and Miss Elisa Chong for their help in supporting the oral interactive assessments and Miss Hannah Goh for assisting to proofread this manuscript.
Funding
There is no funding involved in the preparation of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Lim, S. M. (2021, May 27). The answer is not always the solution: Using coaching in higher education. THE Campus Learn, Share, Connect. https://www.timeshighereducation.com/campus/answer-not-always-solution-using-coaching-higher-education
Lim, S. M., Goh, Z. A. G., & Tan, B. L. (2020). Eight tips for inclusion of persons with disabilities as standardised patients. The Asia Pacific Scholar, 5(2), 41-44. https://doi.org/10.29060/TAPS.2020-5-2/SC2134
Sotiriadou, P., Logan, D., Daly, A., & Guest, R. (2020). The role of authentic assessment to preserve academic integrity and promote skill development and employability. Studies in Higher Education, 45(11), 2132–2148. https://doi.org/10.1080/03075079.2019.1582015
Tan, C. P., Howes, D., Tan, R. K., & Dancza, K. M. (2021). Developing interactive oral assessments to foster graduate attributes in higher education. Assessment & Evaluation in Higher Education. https://doi.org/10.1080/02602938.2021.2020722
Villarroel, V., Bloxham, S., Bruna, D., & Herrera-Seda, C. (2018). Authentic assessment: Creating a blueprint for course design. Assessment & Evaluation in Higher Education, 43(5): 840–854. https://doi.org/10.1080/02602938.2017.1412396
*May Lim Sok Mui
Singapore Institute of Technology,
10 Dover Drive,
Singapore 138683
+65 6592 1171
Email: may.lim@singaporetech.edu.sg
Submitted: 31 August 2022
Accepted: 27 September 2022
Published online: 4 April, TAPS 2022, 8(2), 83-85
https://doi.org/10.29060/TAPS.2023-8-2/PV2874
Janet Grant1,2
1Centre for Medical Education in Context (CenMEDIC), United Kingdom; 2University College London Medical School, United Kingdom
I. TO BEGIN WITH MY VIEW
Medical education is a social science which addresses how people learn and teach medicine. The practice of education and training is therefore fundamental to its epistemology, whereby knowledge, and so scholarship, derives from practice. Where that practice is subject to social, contextual and cultural factors, we must question whether the tenets that are put forward are generalisable beyond the context from which they were derived (Fendler & Cole, 2006). This lack of automatic generalisability has implications for both the scholarship of the medical educationalist, and for the relationship between medical educationalist and teacher. Where educational practice is primary, and is contextually informed, then the teacher, the practitioner of medical education, must be the leader in developing scholarship, while the medical educationalist can support that development by enabling each teacher, context or culture, to tell their own truth well (Grant & Grant, 2022).
II. WHY IS THIS MY VIEW?
A. Scholarship and the Primacy of Practice
The term ‘scholarship’ implies special knowledge that is derived from research or academic analysis. While we can argue that learning has a research basis in educational and cognitive psychology, the same cannot be said of teaching. We can think, for example, of the churn of new teaching methods (sometimes erroneously presented as new ideas about learning) that sweep into medical education, find little evidence of consistent effect, and fade into the ever-expanding menu of teaching options. We can think of problem-based, task-based, case-based, resource-based, peer-assisted, blended, team-based, and e-learning, the flipped classroom, and more broadly, active learning and learner-centred learning. And there are more, changing with fashion and social values.
Are these changes based on generalisable knowledge derived from robust research? Although there might be published papers, they rarely constitute a consistent body of scholarly knowledge that enables claims about predictable effects of different teaching methods in different contexts. That is the nature of social science (Fendler & Cole, 2006). It is this lack of generalisability of the social practice of teaching that places the epistemology of medical education not in theories or fashion, but in widely variable, and contextually tailored, practice.
Although the practice of teaching is socially bound, we can say that the fundamental cognitive basis of learning, how knowledge is effectively organised in memory and accessed when needed, is the same for everyone. Knowing that short-term, working memory should not be overloaded, and that long-term memory should be well-organised with structured, generalisable and accessible knowledge, is the simple baseline against which a medical educationalist can ensure that teaching and learning methods are designed and judged. Many which demand complex processes (sometimes termed ‘learner-centred’) would fail that test.
There is a parallel literature demonstrating that the social, personal and interpersonal processes that cause knowledge to be stored and used effectively, and motor and cognitive skills to develop, are different depending on culture, content and context. Teaching that seems applicable and relevant in one cultural or content context may not apply in another. So it seems important to begin from practice, observe successes and problems, and build theories, if that seems helpful.
These uncertainties underpin our practice-based epistemology, where the teacher is the key person. Accordingly, we have argued (Grant & Grant, 2022) that medical education is not an academic discipline at all, but is an examination of instrumental practice, trying to relate educational activities to purposes, making its means relate to its ends, and making decisions about that on the basis of context and judgement.
This view places the teacher at the heart and in the vanguard of relevant medical education development. This is social science where generalisable scholarship in teaching is difficult to attain. So, there is an ethical responsibility borne by those who claim to know what effective teaching is.
This leads to the next question.
B. What might be the Relationship Between the Teacher and the Medical Educationalist?
Definitionally, I take a medical educationalist to be someone who claims special expertise by virtue of, for example, having completed a Master’s degree in health professions education. Some teachers have done this too, but most have not. Teachers, here, are the subject specialists who actively help others to acquire necessary knowledge and skill.
What might be the relationship between these two?
To answer this, we turn to Lawrence Stenhouse, a British educational thinker who sought to promote an active role for teachers in educational research and curriculum development. Stenhouse argued that the teacher might lead quality development, becoming an ‘extended professional’, supported by trained technical expertise: ‘It is not enough that teachers’ work should be studied: they need to study it themselves’ (Stenhouse, 1976, p143).
In this endeavour, the medical education specialist is a resource, knowing the theories and fashions, and their critiques, summarising where there is and is not evidence, guiding analysis, offering options in relation to the teacher’s practice. The teacher is an equal partner in this ‘mutually supportive co-operative research’ (Stenhouse, 1976, p159), learning to be a researcher, simply because knowledge comes from and is tested in its performance. The medical educationalist will be a crucial support in this process.
To hold this supporting role demands being critically informed about medical education theory and practice. Medical education seems replete with largely unexamined terms such as ‘adult learning’, ‘learner-centred’ or the oxymoronic ‘passive learning’; or with handy mnemonics, and frameworks that have ever-decreasing academic credibility such as ’learning styles’. Medical educationalists must be more securely rooted in the critical approach of social science, beyond the constantly metamorphosing rhetoric of medical education. That authenticity will be gained in equal partnership with teachers.
Stenhouse’s position is unequivocal: the expert is the teacher, the practitioner who understands the individual context. The ‘teacher as researcher’ was Stenhouse’s ground-breaking view of the basis of rational educational development (Stenhouse, 1976, pp. 142-165).
How different is the implication of this view of the teacher, not as a person to be studied or developed, but the person who should be the scholar, reaching, and sharing, their own conclusions in their own classroom. Agency then belongs to the teacher who enacts the curriculum.
In this model, the role of the medical education specialist is to provide knowledge of developmental potential, and of how to develop practice-based, contextual scholarship around methods of reflective action research, perhaps. The medical educationalist is no longer the primary source of knowledge, or the impartial researcher, but is the means of supporting authentic practice development, helping each teacher to find their own truth.
C. And What of the Scholarship of Teaching?
The literature on the scholarship of teaching addresses its derivation in research and reflection on practice, and its use in theory building and educational development. In that literature, the meaning of scholarship in relation to actual teaching is ill-defined.
The importance of this for medical education is that scholarship can easily be thought of as the domain of those who have taken medical education as their speciality, rather than the domain of the teacher who is primarily a scientist or a clinician. This creates a particular relationship where ideas such as ‘faculty development’ suggest that the scholarship of teaching is garnered elsewhere and then shared with the teacher.
But I have argued that the scholarship of teaching will come from the experience of the teachers. Others argued, before me, that knowledge comes from social practice, and then returns to serve and enhance that practice (Mao, 1937). In that, there must be a mechanism for gathering that knowledge derived from social practice and returning it to practice. This may be the role of the medical educationalist, or of medical educationalists collectively, pooling their knowledge gained through working with teachers, reflecting their experience.
This role of gathering together knowledge generated in practice, is especially important in these days when the controversial idea of ‘globalisation of education’ often passes without critique. But ‘Globalisation initiatives must be tempered by ‘cultural humility’ in recognition of the likelihood that, rather than there being one exclusive, universal and ‘superior’ model, there may be many models of effective teaching and learning in medical education around the world’ (Wong, 2011, p. 1218). For Wong, in opposition to the neo-institutionalist, perhaps neo-colonialist, view, ‘…the culturalist perspective focuses on the enduring ability of different cultures and ways of knowing to re-interpret, transform and hybridise education practices to best suit local context’ (Wong, 2011, p. 2010).
This view recognises those contextual imperatives: scholarship must derive from the domain of the teacher, supported, not driven, by the medical education specialist. This is true both of ideas on teaching methods, and of the theoretical and conceptual frameworks that shine and fade in parallel.
In this view, the teacher would become an extended professional who has ‘a capacity for autonomous professional self-development through a systematic self-study, through the study of the work of other teachers and through the testing of ideas by classroom research procedures’ (Stenhouse, 1976, p. 144). In other words, scholarship reverts to the teacher. Support for that scholarship belongs to the medical education specialist, working by the practitioner’s side, in the classroom, enabling that person to advance the contextual practice of medical education.
Note on Contributor
Janet Grant wrote the script, discussed it with Leo Grant and Professor Ahmed Rashid, and wrote the final version.
Acknowledgement
I would like to thank Leo Grant of CenMEDIC, London, and Professor Ahmed Rashid, of University College London Medical School, for their comments on this paper which helped me to express my personal view so much better than I could have done by myself.
Funding
There was no funding support accorded for this study.
Declaration of Interest
The author declares that there is no conflict of interest.
References
Fendler, L., & Cole, J. (2006). Why Generalisability is not Generalisable. Journal of Philosophy of Education, 40(4), 437–449. https://doi.org/10.1111/j.1467-9752.2006.00520.x
Grant, J., & Grant, L. (2022). Quality and constructed knowledge: Truth, paradigms, and the state of the science. Medical Education. https://doi.org/10.1111/medu.14871
Mao, Z. (1937). On Practice. https://www.marxists.org/reference/archive/mao/selected-works/volume-1/mswv1_16.htm
Stenhouse, L. (1976). An Introduction to Curriculum Research and Development. Heinemann.
Wong, A. K. (2011). Culture in medical education: Comparing a Thai and a Canadian residency programme. Medical Education, 45(12), 1209–1219. https://doi.org/10.1111/j.1365-2923.2011.04059.x
*Janet Grant
27 Church Street,
Hampton, Middlesex
TW12 2EB,
United Kingdom
Email: janet@cenmedic.net
Submitted: 15 July 2022
Accepted: 21 September 2022
Published online: 4 April, TAPS 2023, 8(2), 80-82
https://doi.org/10.29060/TAPS.2023-8-2/PV2842
Kevin Tan1,2, Yang Yann Foo2 & Nigel Choon Kiat Tan1,2
1Office of Neurological Education, Department of Neurology, National Neuroscience Institute, Singapore; 2Duke-NUS Medical School, Singapore
A program director of a one-year-old Singapore surgical residency programme reads a publication about a new model of feedback. The paper describes how a US medical school successfully trialled and implemented this new feedback model. Excited, she then tries to implement this new model in her residency programme. Unfortunately, this fails to change faculty and resident behaviour, with disgruntled faculty and residents, and poor take-up by the various surgical departments within her programme. Disappointed, she stops using the new feedback model after a year.
What happened? Why would an educational intervention about feedback, published as part of Scholarship of Teaching and Learning (SoTL) (Steinert, 2017), and successfully implemented in a US medical school, fail to take root in a Singapore surgical residency programme? Might failure to consider context have contributed? A review of the publication showed that while descriptions of the feedback model and the educational outcomes were rich, descriptions of the medical school environment and the broader educational context of the US were sparse.
Might a richer description of context in the publication have helped readers understand the social and educational milieu from which the novel feedback model developed? And with that understanding of context, might a subsequent analysis of contextual differences between the publication and the residency programme’s dissimilar contexts have helped avoid this education setback? Fundamentally, did the lack of contextual descriptions lead to a myopic view of the educational intervention?
Let’s first examine SoTL, which is defined as “the description and dissemination of effective and novel teaching methods and strategies, in a research presentation or publication” (Steinert, 2017). While standards for SoTL in health professions education (HPE) have been proposed (Glassick, 2000), including the need to describe goals, preparation, methods and results, there is scant mention of the need to describe the context within which the novel methods or strategies were operationalised or implemented. So while SoTL remains effective for disseminating novel teaching methods, the variable extent to which context is described (Bates & Ellaway, 2016) may result in challenges in implementing such methods in a different environment; key contextual enablers for successful implementation may have been inadequately described within the HPE SoTL literature. In contrast, the general education literature has long been aware of the importance of context in SoTL (Felten, 2013). There is therefore a blind spot in the HPE SoTL literature.
We next examine context. While we highlight rich descriptions of context for the value it brings to SoTL, we pause to reflect: how do we define context? Context can be difficult to define. A scoping review (Bates & Ellaway, 2016) concluded that one perspective was context as a “surrounding”, much like the layers of an onion, with a particular context playing a role as a mechanism influencing education outcomes. Employing these twin perspectives of “context as an environment surrounding an education activity”, and “context as a mechanism” (Bates & Ellaway, 2016) influencing said activity, we can then view context as surrounding and influencing the educational method, its implementation and its outcomes.
Given the many elements within the context that may influence outcomes, how do we then systematically identify and dissect these disparate elements? The analogy of an onion with surrounding layers (Bates & Ellaway, 2016) led us to consider Bronfenbrenner’s Ecological Systems theory (EST) (Bronfenbrenner, 1986). In EST, multiple systems (micro-, meso-, exo-, macro- and chrono-), much like layers of an onion, influence an individual’s learning. EST can be used to identify, dissect, and categorise contextual influences, and determine if they enable or inhibit educational activities.
In our scenario, the original SoTL work did not fully describe the context. Let us now imagine that the situation was clarified by us writing to the authors to learn more about their context. We are then rewarded with a rich, three-page description of their context. Using EST to dissect the differences between the US context of the intervention, versus the Singapore context of the residency programme, we now realise there were differences at multiple EST system levels, for example:
- Microsystem: medical students vs residents as learners and feedback recipients, university faculty vs clinician faculty as feedback providers
- Mesosystem: uniprofessional vs multiprofessional peers and colleagues, undergraduate vs postgraduate curricula
- Exosystem: university vs clinical training environment, academic workload vs clinical workload
- Macrosystem: cultures of medical school vs residency, cultures of university vs medical profession, societal cultures of the US vs Singapore
- Chronosystem: historical perceptions of feedback and utility of feedback in the US vs Singapore
With these different EST system levels in mind, one can identify enablers and inhibitors to successful implementation of the published feedback model in Singapore:
- Microsystem: residents and/or clinician faculty may be busy or distracted by concurrent clinical duties, thus less willing or able to deliver actionable feedback using the model, vs university lecturers who had dedicated time for feedback sessions
- Mesosystem: while feedback was institutionalised in the US medical school as a longitudinal aspect of the curriculum since 10 years ago, allowing easier integration of a new model into a mature curricular element, adding a new feedback model into a one-year-old programme’s curriculum and implementing it added more stress to a new programme still in flux
- Exosystem: the US medical school had several resources that the local programme did not. The American researchers had many dedicated teaching rooms for feedback provision to the medical students. In contrast, the surgical residents had to compete with other residents and users for fewer rooms in the local hospital that were also used for multiple clinical, administrative and research purposes. The university also had a mature e-portfolio system where faculty and students could review goals, milestones and progress to facilitate feedback provision, while the new residency programme did not.
- Macrosystem: feedback was viewed positively by university faculty and students as a key learning activity, with the school taking pride in providing actionable feedback as part of its culture and values. The school’s Dean also publicly affirmed support for the new feedback model. In contrast, the new residency faculty were still unused to providing structured feedback, or inviting reflection as part of feedback; some even viewed feedback as a chore rather than as a vehicle for learning and improvement. The nascent feedback culture of the residency faculty had not fully taken root yet, unlike in the US school.
- Chronosystem: Historical perceptions of feedback differed in the US vs Singapore, with feedback considered valuable for learning and improvement in the US. In Singapore however, feedback was viewed by some senior surgical faculty members as being useful only when mistakes were made by residents, whereupon forceful negative feedback was given by faculty to the resident in the name of patient safety, rather than for learning. These views from the local senior faculty were informed by their prior experiences as trainees in earlier training systems, leading to their rejection of the new feedback model as being “soft” and compromising patient safety.
With a rich description of context, and using EST as a tool, one can now see how the different system layers surround and envelope the faculty, residents and their feedback interaction. One can also see how contextual differences in these system layers (in the US vs Singapore) influenced the success or failure in implementation of the new feedback model. If rich contextual information was provided in the SoTL literature at the start then this information, considered with EST, might have helped the residency programme director avoid the implementation failure.
Successful understanding and application of SoTL in HPE thus relies not only on the six goals espoused by Glassick (Glassick, 2000), but also requires adequate descriptions of context. Readers can then understand contextual differences, use EST to compare and contrast it to their context, identify differences at various EST system layers and determine the potential influence of these differences.
Conversely, the general education literature emphasises that SoTL should be “grounded in context” (Felten, 2013). Felten explicitly states “… all SoTL is rooted in particular classroom, disciplinary, institutional, and cultural contexts” and that “any measure of good practice must account for both the scholarly and the local context where that work is being done” (Felten, 2013). The primacy of context is stated, clearly and unambiguously.
In summary, while we have made progress in SoTL in HPE, we have not adequately considered context in our SoTL guidance (Glassick, 2000) compared to our general education colleagues (Felten, 2013). This underemphasis on context may result in sparse descriptions of context in the HPE SoTL literature, leading HPE readers to be myopic and failing to see the myriad contextual influences affecting understanding and translation of the described SoTL methods to the reader’s context. If we had richer descriptions of context in the SoTL literature, however, we can then use the ‘context lenses’ to clearly view the surrounding layers that influence education outcomes (Bates & Ellaway, 2016). Finally, with visual clarity, we can then dissect and analyse these layers via mapping them to systems levels using EST (Bronfenbrenner, 1986), so that effective translation and implementation of the described SoTL methods can take place. It is time to correct our myopia by collectively advocating for the rich descriptions of context in our HPE SoTL literature.
Notes on Contributors
Dr Kevin Tan reviewed the literature and developed the manuscript. Dr Foo Yang Yann reviewed the literature and gave critical feedback to the writing of the manuscript. Dr Nigel Choon Kiat Tan reviewed the literature and gave critical feedback to the writing of the manuscript. All authors have read and approved the final manuscript.
Funding
The research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of Interest
Authors have no conflict of interest, including financial, institutional and other relationships that might lead to bias.
References
Bates, J., & Ellaway, R. H. (2016). Mapping the dark matter of context: A conceptual scoping review. Medical Education, 50(8), 807-816. https://doi.org/10.1111/medu.13034
Bronfenbrenner, U. (1986). Ecology of the family as a context for human development: Research perspectives. Developmental Psychology, 22(6), 723-742. https://doi.org/10.1037/0012-1649.2 2.6.723
Felten, P. (2013). Principles of Good Practice in SoTL. Teaching & Learning Inquiry: The ISSOTL Journal, 1(1), 121-125. https://doi.org/10.2979/teachlearninqu.1.1.121
Glassick, C. E. (2000). Boyerʼs expanded definitions of scholarship, the standards for assessing scholarship, and the elusiveness of the scholarship of teaching. Academic Medicine, 75(9), 877-880. https://doi.org/10.1097/00001888-200009000-00007
Steinert, Y. (2017). Scholarship in medical education. International Journal of Education and Health, 1(1), 3-4. https://doi.org/10.17267/2594-7907ijhe.v1i1.1657
*Kevin Tan
Office of Neurological Education,
Department of Neurology,
National Neuroscience Institute
11 Jalan Tan Tock Seng,
Singapore 308433
Email: kevin.tan@singhealth.com.sg
Submitted: 5 August 2022
Accepted: 2 November 2022
Published online: 4 April, TAPS 2023, 8(2), 76-79
https://doi.org/10.29060/TAPS.2023-8-2/SC2861
Poh-Sun Goh1 & Elisabeth Frieda Maria Schlegel2
1Department of Diagnostic Radiology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Department of Science Education, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hofstra University, United States
Abstract
Introduction: The aim of this short communication is to examine the journey of scholarship in health professions education (HPE).
Methods: We will focus on tangible small steps to start, sustain, and succeed along this journey. Through a proposed innovation in scholarship – micro-scholarship – we will describe how this is similar to and an extension of bite-size or micro-learning, and workplace micro-practice related to just-in-time (JiT) learning settings.
Results: We will demonstrate how the small steps for generating and engaging with micro-content can be similarly applied to micro-scholarship. Then, progressive and iterative refinement of output and practice of micro-scholarship can be combined and result in macro-scholarship after cycles of public engagement for final digital or print publication. This stepwise approach creates an accessible, sustainable strategy to achieve success as a scholar in HPE. We will elaborate on micro, macro, and meta matters and celebrate how these small steps encourage and allow broad participation in the creation, critique, and progressive refinement of scholarship.
Conclusion: Small, sustainable, steps leads to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Keywords: Micro-Scholarship, Micro-Learning, Just-In-Time (JiT) Learning, Community of Practice (CoP), Technology, Network Effects, Post-Publication Peer Review (PPPR)
I. INTRODUCTION
Modern changes in the pace and way we conduct and experience teaching and learning have resulted in production and consumption of smaller chunks of content. Succinct, bite-size content is easier to remember and consumes less cognitive bandwidth with reduced cognitive load. In addition, it is also significantly easier to share and engage with within a professional community of practice (CoP). Compact modular, bite-size content is also ideal for just-in-time (JiT) micro-learning and workplace micro-practice (Yilmaz et al., 2022), or on-demand learning and practice, with which we are all familiar. In this paper, we will extend this idea of micro-learning and micro-practice to scholarship, by examining the “new” idea of micro-scholarship – defined as “the process of making visible the smallest accessible and assessable steps that document a scholarly journey, which can then be assembled and presented as an outcome of academic scholarship” (Goh et al., 2021). Mobile technology tools and platforms support open display, access to, and iterative engagement with this content by a community of practice (CoP), both in learning and scholarship (Goh et al., 2021; Goh & Sandars, 2020; Schlegel, 2021).
II. MICRO-MATTERS
Just as a musical composition is made up of individual notes, a construction from its individual parts, and a meal of its individual ingredients, commonly accepted and acknowledged finished works of scholarship in HPE are composed of its individual parts. A conference presentation or journal paper, peer reviewed, read by and engaged with by a CoP, contains core components – e.g., the title (which includes key ideas); key words (which are defined and illustrated in the presentation or paper); and cited published work by earlier authors (from a review of the field, including takeaways from the author(s) that are relevant and that the authors intend to discuss, elaborate, and build upon). However, a close examination and reflection of these core parts of finished works of scholarship show that they not only form the ingredients of the final work, but that they also fall within the categories of scholarship proposed by Boyer, with evaluation criteria described by Hutchings and Shulman; (Goh et al., 2021; Goh & Sandars, 2020). Boyer’s model for scholarship includes (1) integration, (2) application, (3) teaching and learning, and (4) discovery.
Innovative JiT micro-content on mobile platforms is easily accessible for members of a CoP to engage with, evaluate, critique, and build upon. All online content, including, e.g., on Twitter, blogs, or modular courses, is subject to creative reader collectives, which post comments, repost, reshare, and create new meaning and value from individual posts of content, contributing to group engagement, which has many of the characteristics of scholarship (Schlegel & Primacio, 2021). We propose that these artefacts and activities illustrate examples of Boyer’s Scholarship categories, including demonstrating the Scholarship of Teaching and Learning SoTL. Digital and online content and platforms support and scale our efforts as learners and scholars, no different yet more facile as compared to in-person activities, with increased importance placed on being a public professional, and respecting intellectual property, shown by proper citation of digital content, and use of this content with permission where applicable, followed by data-driven dissemination (Arrington & Cohen, 2015; Kern et al., 2015). This public reaction and appraisal of content compares to wide audience post-publication peer review (PPPR) with the added value of a feedback-loop through responses on comments. Just as developing bite-size, short format, JiT digital, online content, has transformed and continues to transform our educational and professional practices, a similar process can now facilitate and support granular, open digital display and engagement of both our initial and subsequent steps when engaging in scholarship in HPE, similar to and an extension of micro-learning. Practicing micro-scholarship involves encountering a “new idea”; researching its meaning; adding relevance to specific discussion themes and takeaways; discovering key published and presented work; and then both taking note of and making notes on these findings during reflection and discussions within a local CoP. This micro-scholarship is subsequently made open and visible to a global readership or a CoP, through private, semi-private, and public engagement platforms. Micro-scholarship content gets progressively refined through iterative engagement with members of a CoP, through discussion, feedback, critique, and personal reflection. The relevance and usefulness of this content, as well as confidence in the authors of this micro- scholarship content, is progressively enhanced. We also learn how and where this content is best disseminated and presented, and best ways this might be combined and stacked. The iterative in- person and scalable digital conversations amplifying the spread and engagement with this material to create meaning, in step-by-step fashion, form the core practices of both micro-scholarship (Goh et al., 2021) and bite-size engagement with material (Schlegel, 2021). After refinement, these pieces can be combined into larger pieces of finished work of macro-scholarship. Thus, activities undertaken as part of micro-learning or micro-scholarship are accessible, independent, and sustainable small, step-wise efforts that can and do add-up. Progression along the developmental path of a scholar will include a variety of conversations within a CoP, such as the supportive networks of peers, senior practitioners, mentors and coaches, including collaborative (team)work and initially supervised instruction as part of a successful scholar’s journey. Conversations and engagement within a CoP do range from positive and helpful to (those that are or perceived to be) occasionally provocative and challenging. However, professional and good-natured discussion generally guide scholarly development similar to trial and error, and progressive improvement and iterative steps enable learning and growth.
III. MACRO-MATTERS
Simply put, a finished larger work is made up small pieces that have been selected and refined, through an iterative process of reflection and feedback, by engaging with a CoP or specialised collective of readers. Open (digital) practice from an early stage, the platforms (places and readers) we engage in, and our active participation in professional CoP of global specialised readers provide both “informed” and “critical” feedback – and review of these “early” and “small” or “micro” pieces of work – from a (much wider) audience. The key distinction is who engages with this work, from as wide a spectrum of professional practice, experience, and expertise as possible, and from a diversity of points of view. Digital tools and practices facilitate and scale this process. This is similar to the work of artists, who engage in open sketching, including showcasing early drafts and ideas, prototyping, drawing, and artistic creation in open studios. When members of a CoP engage through digital platforms the impact from their individual and collective input can scale exponentially through network effects (Azhar, 2021).
IV. META-MATTERS
The process of scholarship mirrors the stepwise, sequential, cumulative process of learning, and training for proficiency and mastery in any area of practice. Our roles as practitioners, educators and scholars are all informed by learning science. Digital devices, tools, platforms, and practices exponentially scale up the impact of our efforts through applied network theory and interactions. Ultimately, we live and practice professionally within our CoP, which provides both the audience and peer reviewers of our public work, thus driving a fruitful evolution of our profession. Our ultimate aim is to engage a CoP in conversations, including broader participation in the production, refinement, and consumption of products of scholarship, in form and format, and through processes accessible for all. Micro-scholarship is a starting point that allows wider participation and engagement in the process of scholarship. The components of micro-scholarship, when refined and confidently presented, are contained within published finished macro-scholarship outputs. Then, micro-scholarship and macro-scholarship add collaboration and value within a larger scholarship ecosystem and professional CoP, a meta-level practice or meta-system, within which micro- and macro- level activities occur. An explicit example of the outputs and process of moving from micro, through macro, to meta practice illustrated https://www.slideshare.net/dnrgohps/illustrated-stacked-microscholarship-steps-along-academic-path-of-educational-scholar.
Another example of enhancing scholarship of teaching and learning SoTL across different levels might include, e.g. a remote consultation with members of scholarly project teams, prompting to publish a themed blog post, which, in return, becomes now a generalizable, transferrable offering to the global CoP, moving from the meta-system to the macro-level, as evidenced by comments from different institutions and subsequent implementation of ideas (Arrington & Cohen, 2015).
V. CONCLUSION
In this paper, we have examined, showcased, and celebrated the small sustainable steps to success as a scholar in HPE, describing micro, macro, and meta matters and illustrating how combining small components of scholarship is an effective strategy for dissemination, access, engagement, conversation and collaboration within a CoP in HPE.
Notes on Contributors
Poh-Sun Goh pitched initial idea, was involved in active discussion and brainstormed with co-author iterative refinement of core message(s), wrote first draft, and actively revised series of subsequent drafts, and submitted final draft. This manuscript built on previous collaborative work, cited in article on Micro-Scholarship and Digital Scholarship.
Elisabeth Schlegel was involved in active discussion and brainstormed with co-author iterative refinement of core message(s), and actively revised series of subsequent drafts, and including and approving final draft. This manuscript built on previous work, cited in article including on bite-sized learning.
Ethical Approval
As this manuscript is a description of an innovative approach to scholarship, ethical approval and IRB application was not required.
Data Availability
There is no additional data separate from available in cited references.
Acknowledgement
No technical help and/or financial and material support or contributions was received in preparation of this manuscript.
Funding
Both authors have no funding source to declare.
Declaration of Interest
Both authors declare that there are no possible conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
References
Arrington, N. M., & Cohen, A. L. (2015). Enhancing scholarship of teaching and learning through micro-level collaboration across two disciplines. International Journal of Teaching and Learning in Higher Education, 27(2), 194.
Azhar, A. (2021). The exponential age: How accelerating technology is transforming business, politics and society. Diversion Books.
Goh, P. S., Roberts-Lieb, S., & Sandars, J. (2021). Definition of Micro-Scholarship. https://microscholarship.blogspot.com/
Goh, P. S., & Sandars, J. (2020). Rethinking scholarship in medical education during the era of the COVID-19 pandemic. MedEdPublish, 9(97). https://doi.org/10.15694/mep.2020.000097.1
Kern, B., Mettetal, G., Dixson, M., & Morgan, R. K. (2015). The role of SoTL in the academy: Upon the 25th anniversary of Boyer’s scholarship reconsidered. Journal of the Scholarship of Teaching and Learning, 15(3), 1-14. https://doi.org/10.14434/josotl.v15i3.13623
Schlegel, E. (2021). (Not only) for medical students: Get involved in medical education research & scholarship. https://elisabeth-fm-schlegel.weebly.com/elearning-bites/not-only-for-medical-students-get-involved-in-medical-education-research-scholarship
Schlegel, E., & Primacio, J. (2021). Blogging for the continuum of medical education: Engaging diverse communities of learners. MedEdPublish, 10, Article 136. https://doi.org/10.15694/mep.2021.000136.1
Yilmaz, Y., Papanagnou, D., Fornari, A., & Chan, T. M. (2022). The learning loop: Conceptualizing Just-in-Time faculty development. AEM Education and Training, 6(1), e10722. https://doi.org/10.1002/aet2.10722
*Poh-Sun Goh
Department of Diagnostic Radiology
National University Hospital,
Main Building, Lobby F, Level 4
#04-398, DDI Library
5 Lower Kent Ridge Road, Singapore 119074
+6567724211
Email: dnrgohps@nus.edu.sg
Submitted: 28 April 2022
Accepted: 19 August 2022
Published online: 4 April, TAPS 2023, 8(2), 70-75
https://doi.org/10.29060/TAPS.2023-8-2/SC2802
Sok Mui Lim, Ramesh Shahdadpuri & Ching Yee Pua
Centre for Learning Environment and Assessment Development (CoLEAD), Singapore Institute of Technology, Singapore
Abstract
Introduction: Coaching has gained acceptance in the education field as a way to enable learners to achieve their fullest potential. In the endeavor to set up a coaching ecosystem in our university, we started by equipping our educators with fundamental coaching skills and techniques. Our training workshop, Coaching As An SIT Educator, covers the key coaching competencies and is highly practice focused. Participants get hands-on skills practice using contextualised scenarios that are based on realistic academic, workplace and clinical placement settings.
Methods: To address concerns on time-effectiveness, we adopt a solution-focused approach to coaching. We want to create a mindset shift for educators, from subject experts providing advice and solutions, to coaches asking powerful coaching questions that help students make discoveries and work towards their goals. We encourage our educators to engage students holistically by finding coachable moments in their daily student interactions.
Results: Competency-based assessments are conducted to determine achievement of the learning outcomes, articulated by the knowledge, attitude, and demonstration of coaching skills with students. Assessments consist of a reflection, multiple-choice question (MCQ) quiz, and scenario-based coaching role plays. Participants achieved the learning outcomes as demonstrated from the assessments.
Conclusion: The coach training workshop is the major pillar of our coaching initiative. Beyond the workshop, ongoing coaching development is supported through other activities and resources, including community of practice, coaching circle and knowledge repository. Opportunities for continuous learning and conversation platforms for sharing coaching experiences are part of the growing coaching ecosystem at SIT.
Keywords: Assessments, Coaching Competencies, Coaching Conversations, Coaching Ecosystem, Coachable Moments, Faculty Development, Feedback, Holistic Development, Solution-Focused
I. INTRODUCTION
Coaching has gained greater awareness and wider acceptance in the education field in the past decade, led by the efforts of innovative educators and more evidence-based research. Coaching has been described as a very powerful approach that facilitates personal and professional change through deep level listening, questioning, setting the right challenges and providing support along the process (Griffiths, 2005). More specifically, academic coaching is defined as individualised practice of asking students reflective, motivation-based questions, providing opportunities for formal self-assessment, sharing effective strategies, and co-creating a tangible plan that promotes accountability (Deiorio et al., 2017).
In traditional educational settings, communication tends to be mostly directive, where the educator is the subject expert who gives instructions, solutions or advice to students. From this “telling” or “pushing” stance where the focus is on problem solving and advice giving, shifting to coaching conversations requires an “asking” or “pulling” communication approach. Engaging in coaching conversations involves the educator coaching students through powerful questioning, active listening and guiding them to explore possibilities so as to discover new ideas and find solutions for themselves.
In 2020, Singapore Institute of Technology (SIT) introduced internal coach training for all academic staff with the aim to build educators’ capability to work with students at a deeper level. This highly contextualised academic coaching training was made mandatory for all educators. This was essential for the creation of a strong coaching ecosystem in the university and adopting coaching practices across a variety of learning contexts, such as providing assignment feedback, consultations on projects and supervising students at the workplace. In working with students towards their preferred futures, SIT educators can help the students develop confidence and self-efficacy, enabling them to achieve their fullest potential.
II. METHODS
This section highlights the critical elements of the faculty development programme.
A. Solution-focused Approach
One of the top concerns of many educators is time. There are underlying concerns on whether coaching students will take up too much time, and what happens if they uncover student issues that they cannot deal with. A solution-focused coaching approach alleviates some of these concerns. The basic principle of the solution-focused approach is to help coachees reflect and design their solutions, rather than go down the path of root cause analysis. Its forward-oriented solution approach contrasts with other traditional psychological techniques, which tend to look back at the past or are problem-focused (Grant & Gerrard, 2020).
The solution-focused approach is known for its simplicity, attention to language and time effectiveness. The conversation is steered to a preferred future of the issue at hand without dwelling on the troubled past. The coach encourages the coachee to focus on their strengths and positive resources, to think about their resourceful past, and to draw on positive lessons from when they have been at their best. After identifying their desired outcomes and considering their options in the context of present realities, the coach guides the coachee to think about the next steps to progress towards their preferred future.
B. Mindset Shift
In higher education, many coachable opportunities outside the formal contact hours can be easily missed. For example, instead of merely deducting marks for repeated late submissions of assignments, the educator could coach the student on improving time management. In clinical fieldwork, when a student complains about limited interaction with the busy clinical educator, the university supervisor can coach the student on how best to schedule time for feedback. Our daily encounters and interactions with students present many coachable moments that offer just-in-time and authentic learning opportunities to support students in their development to become work-ready graduates.
Students may initially find coaching sessions difficult as it is easier to just ask for solutions than to discover solutions for oneself. However, with time, students will realise the value of coaching as they witness their progress. In an Asian context, where many students are respectful and value advice from authoritative figures, such as professors, coaching can require a mindset shift for both students and faculty (Lim, 2021).
C. Tailoring the Coaching Training to Education Context
The Coaching As An SIT Educator workshop is an in-house designed 2-day program. It is highly contextualised for the needs of SIT academic staff, to equip them to be versatile and agile educators, performing the role of Teacher-Coach-Mentor. The workshop covers the key coaching fundamentals and is highly practice-oriented. The programme design was intended for participants to develop hands-on coaching skills with contextualised role play scenarios (see Appendix A for an example), so that they can apply what they have learnt with their students immediately after the workshop.
While we do not intend to train credentialed professional coaches, the key International Coaching Federation (ICF) coaching competencies were referenced to guide the design of the SIT workshop. The GROW model (Whitmore, 2019) was introduced as a framework for the participants to organise and manage the flow of the coaching conversation. Drawing on inputs from academic staff, realistic student-centric scenarios were created for class discussions and role plays. The coaching practice sessions are conducted in dyad, triad, and hot seat formats. The workshop design and facilitation ensure that there is psychological safety, providing a trusting space for constructive debriefing, feedback sharing and open questions and answers to take place.
To manage the workshop time and resources effectively, e-learning content was developed in-house, specifically to complement the interactive classroom session. A week before the start of the workshop, the participants can access materials in the form of an asynchronous pre-recorded webinar. The webinar consists of five micromodules, covering topics such as Mindset, Motivation, Emotional Intelligence, and Feedback Skills (refer to Appendix B for more details). As many participants may already be familiar with these topics, this self-learning component serves as a good refresher to prepare participants for the coaching workshop.
Please refer to Table 1 for details of the Coaching as An SIT Educator workshop.
|
Workshop: Coaching As An SIT Educator |
|
|
Learning Outcomes By the end of this course, participants will be able to:
|
|
|
Topics Covered |
|
|
Pre-Workshop: eLearning
|
Workshop Day 1:
Workshop Day 2:
|
|
Assessments (Day 2) |
|
|
Role Plays: Standardised Students & Assessors Scenarios (each – 20 minutes):
|
Quiz: Multiple Choice Questions (MCQs)
|
Table 1. Coaching As An SIT Educator Workshop
III. EVALUATION OF COACHING COMPETENCY
To assess the attainment of the learning outcomes and development of the participants’ coaching competence (knowledge, skills, attitude), assessments and reflection exercises are incorporated into the workshop. As this is not a certification program, assessments are formative in nature, with focus on providing the educators quality feedback. Coaching knowledge is assessed through a multiple-choice question (MCQ) quiz. Attitude and mindset shift is evaluated through pre- and post- workshop surveys, and reflection questions.
Coaching skills are assessed via role plays (with standardised students). The role play format involves two 20-minute coaching sessions with the participant (playing the role of an educator) having a coaching conversation with standardised students (who act as coachees) and are conducted virtually in real time over the Zoom platform, using breakout rooms. The role plays that are based on common scenarios in university and workplace supervision settings. An invaluable part of the learning in this assessment comes from the feedback conversation between the participant (coach) and assessor, who observes the coaching conversation. Many participants regard the skills assessment and individualised feedback on their coaching skills as the highlight of the training programme.
IV. DISCUSSION
Many readily available coaching materials or vendor-run workshops are geared towards executive or corporate scenarios. While the skills of coaching may be transferable, it is difficult for educators to draw relevance to student engagement. Therefore, Coaching As An SIT Educator workshop focuses on case studies of university scenarios, and supervision for work-integrated learning (e.g., internship, clinical placement). Participants get to work with fellow learners in group work and discussions, to engage in personal reflection, and takeaway practical knowledge and skills on their learnings in a safe space.
For a sustained effort to practice coaching and build an on-going coaching culture, a mandatory workshop is inadequate. Other coaching resources are available to support coaching practice and promote continuous learning in SIT:
- Community of Practice: Coaching Conversations @SIT (offered to any interested academic staff)
- Coaching Circle (offered to all alumni of the coaching workshop)
- Coach Academy (knowledge repository with academic and coaching industry resources).
V. CONCLUSION
In coaching, there lies great potential for students to be developed holistically if we tap on coachable moments in higher education. A contextualised, well-developed coaching development programme is an enabler for this potential to be fulfilled. Drawing on evidence-based research from academia and professional practice, a practice-oriented programme which focuses on developing hands-on coaching skills will be impactful, as educators can put these skills into action in their interaction with students.
Notes on Contributors
Associate Professor Lim Sok Mui (May) led the Center for Learning Environment and Assessment Development (CoLEAD) and spearheaded the coaching initiative in the university, contributed to the conception, drafted and critically revised the manuscript.
Ramesh Shahdadpuri is the senior educational developer in CoLEAD and plays the role of the coaching trainer for the faculty training program. reviewed the literature, contributed to the conception and assisted in revising the manuscript.
Pua Ching Yee is the learning analyst in CoLEAD and plays the role of coordinating the coaching training and assessment of the participants. She assisted in critically reviewing, revising and formatting the manuscript.
All authors gave their final approval and agree to be accountable for all aspects of the work.
Ethical Approval
This is a narrative review related to coaching training program with no data presented and no ethical approval is required.
Data Availability
This paper is a narrative review with no data analysis.
Acknowledgement
The authors would like to thank Miss Cherine Foo for her significant contribution of the coaching program.
Funding
There is no funding involved in the preparation of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Deiorio, N. M., Skye, E., & Sheu, L. (2017). Introduction and definition of academic coaching. In N. M. Deiorio & M. M. Hammoud (Eds.), Coaching in medical education: A faculty handbook (pp. 1-5). American Medical Association.
Grant, A. M., & Gerrard, B. (2020). Comparing problem-focused, solution-focused and combined problem-focused/solution-focused coaching approach: solution-focused coaching questions mitigate the negative impact of dysfunctional attitudes. Coaching: An International Journal of Theory, Research and Practice, 13(1), 61-77. https://doi.org/10.1080/17521882.2019.1599030
Griffiths, K. (2005). Personal coaching: A model for effective learning. Journal of Learning Design, 1(2), 55–65. http://dx.doi.org/10.5204/jld.v1i2.17
Lim, S. M. (2021, May 27). The answer is not always the solution: using coaching in higher education. Times Higher Education. https://www.timeshighereducation.com/campus/answer-not-always-solution-using-coaching-higher-education
Whitmore, J. (2019). Coaching for performance: The principles and practice of coaching and leadership (5th ed.). Nicholas Brealey Publishing.
*Lim Sok Mui
Singapore Institute of Technology,
10 Dover Drive, Singapore 138683
+65 65921171
Email: may.lim@singaporetech.edu.sg
Submitted: 4 October 2022
Accepted: 5 December 2022
Published online: 4 April, TAPS 2023, 8(2), 66-69
https://doi.org/10.29060/TAPS.2023-8-2/SC2894
Simon Field1, Pat Croskerry2, Susan Love3, & Peggy Alexiadis Brown4
1Undergraduate Medical Education and Emergency Medicine, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada; 2Critical Thinking Program, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada; 3Faculty Development, Continuing Professional Development, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada; 4Dalhousie Medicine New Brunswick, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada
Abstract
Introduction: For all clinical providers in healthcare, decision-making is a critical feature of everything they do. Every day physicians engage in clinical decision-making where knowledge, evidence, experience, and interpretation of clinical data are used to produce decisions, yet, it is fair to say that most do not have an explicit insight or understanding of this complex process. In particular, few will have training in teaching and assessing the cognitive and affective factors that underlie clinical decision-making.
Methods: To foster an increased awareness and understanding of these factors, the Dalhousie Critical Thinking Program was established with the mandate to develop and deliver curriculum for critical thinking in the 4-year undergraduate program. To assist teaching faculty with the goal and objectives of the program, the Teaching and Assessing Critical Thinking Program (TACT) was introduced.
Results: Using the dual process model as a platform for decision-making, this program introduces general principles of critical thinking and provides tools to teach learners how to strengthen their critical thinking skills. To offer flexible learning, an online approach was chosen for delivery of the program.
Conclusion: To date, we have offered eleven iterations of Part 1 to a total of 261 participants and six iterations of Part 2 to a total of 89 participants. Evaluations show the online approach to content delivery was well received and the content to be of practical use.
Keywords: Critical Thinking, Clinical Decision-Making, Faculty Development, Asynchronous Learning
I. INTRODUCTION
This paper provides a review of a two-part Teaching and Assessing Critical Thinking (TACT) program which was developed to help faculty understand vulnerability to bias and the role of metacognitive processes in clinical decision-making. The objective of the TACT program is to better prepare faculty to teach learners these important skills. In this paper, we describe how it was implemented, how participants perceived the program, and what changes were needed to address this important hidden ‘soft’ skill within the clinical setting.
II. METHODS
Physicians are constantly required to interpret information when they interact with patients, communicate with colleagues, review medical histories and laboratory reports, conduct physical exams, review the medical literature, and attend rounds. All of these clinical activities demand a sustained level of accuracy, clarity, and especially rationality. Critical thinking (CT) does not guarantee rationality but is one of its more important features and is essential for the role of physician.
Reliable and accurate diagnosis is the barometer of good clinical decision-making and will have a direct impact on treatment outcomes and patient safety. One in 20 (or roughly 12 million) American adult outpatients are affected by diagnostic errors every year. The overall number of fatalities associated with diagnostic failure is not known, but it is estimated that 40,000 – 80,000 deaths occur annually in hospitalised patients in the USA due to diagnostic failure.
A number of studies have shown that training in the development of CT skills in undergraduate students is effective. (Abrami et al., 2015) However, given that most faculty in medical schools today will not have had explicit CT training, specific initiatives in teaching it seem appropriate, not only for the faculty themselves but, importantly, for the students they teach.
To better prepare learners, Dalhousie’s Faculty of Medicine established the Critical Thinking Program in 2012. The program incorporated principles from the Foundation for Critical Thinking into a general model of clinical reasoning (Croskerry, 2018). The Dalhousie critical thinking curriculum reflects a consensus in the current medical literature that the dual process model (System 1 and System 2) is the most appropriate platform for reviewing the clinical decision-making process (See Figure 1).
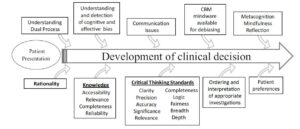
Figure 1. The Dalhousie University model for clinical decision making. (Reproduced with Permission)
A key component in the delivery of this curriculum is helping faculty develop the skills they will need to teach and mentor critical thinking in the clinical environment. Most educators have limited understanding of the advances in medical decision-making and how to best teach critical thinking and clinical reasoning.
The TACT Program comprises two distinct courses: TACT 1 and TACT 2. The program is structured to develop a sound knowledge of critical thinking principles in TACT 1, followed by a focus on teaching and learning in TACT 2. TACT 1 centres on three main themes: How Physicians Make Decisions, Cognitive and Affective Biases, and Cognitive Debiasing Strategies. TACT 2 centres on two main themes: Fundamentals of Medical Education and Strategies for Teaching and Assessing CT. In TACT 2, participants choose one of four elective options: Evidence Based Medicine, Competency Based Medical Education, Medical Humanities, or Curriculum Development.
The TACT Program uses an asynchronous online approach to reach Dalhousie faculty who are distributed across the Canadian Maritime Provinces. This approach mediates potential barriers for participation such as distance and time constraints and allows for individualised learning experiences while building an interactive online community of practice experience (Cook & Steinert, 2013). We use a combination of curricular tools including online didactic lectures, independent study activities, webinars, and discussion boards.
To date (Winter 2022), we have held 11 iterations of TACT 1 and 6 iterations of TACT 2, with 163 of 261 participants completing TACT 1 and 78 of 89 registrants completing TACT 2.
Of those who completed TACT 1, 55 % went on to enrol in TACT 2.
We initially developed the TACT Program for Dalhousie faculty (primarily physicians); however, due to growing interest in the topic, we have opened enrolment to include participants from around the world, including the United States, Mexico, United Kingdom, Australia, New Zealand, Turkey and Brazil. We also opened enrolment to participants from a variety of health professions and other fields of study. By opening the program to participants with diverse backgrounds in practice and location we have increased the diversity of perspectives and the richness of reflections posted to the discussion boards.
Prior to starting the TACT Program, we asked participants to complete a survey measuring their current knowledge of teaching and assessing CT, and motivation for taking the course.
Participants reported little satisfaction with previous knowledge in CT (Mean: 2.67 ± 0.84 on a Likert Scale of 1 (not at all satisfied) to 5 (very satisfied)). The following themes were identified as motivators for taking the TACT Program — a desire to: learn, improve clinical reasoning by increasing knowledge, understand the impact of critical thinking, provide better clinical care, decrease diagnostic error, and become a better educator.
We administered a summative evaluation following both TACT 1 and TACT 2. For TACT 1, 75% (121/162) completed the final evaluation and for TACT 2, 90% (63/70). In the summative evaluation, we asked participants to rate their course in a number of areas from course delivery to the effectiveness of increasing their knowledge and comfort in teaching critical thinking. Consent to data collection was implied as part of the administration of the evaluation. We found that participants were very satisfied with delivery methods.
III. RESULTS
A. What Did We Learn about the Participants?
All participants taking the TACT Program shared a similar motivation: the intent to improve their critical thinking skills and to teaching others. Steinert et al. (2002) found that faculty are more likely to enrol in an online program if they believe it would meet a perceived need. Our participants identified a desire to improve their own practice, confidence and awareness, to make the unconscious conscious, and to develop the language to name, identify and act on cognitive biases and those circumstances that create biases. This enabled them to better teach and mentor CT.
Participants also identified the value of communicating with others who offered a different perspective on clinical work and life experiences.
Physicians may not readily share/disclose mistakes they make in the clinical setting. In medical training environments, overconfidence and reluctance to admit mistakes are often the norm, which may work against fostering a culture of reflection (Brezis et al., 2016). Due to the confidentiality of the discussion boards, our participants could freely reflect on what factors contribute to errors they have made/seen and share those lessons with peers without fear of loss of reputation and embarrassment.
B. What Did We Learn about the Delivery?
We found that the online delivery was successful in reaching a broad base of participants. Some participants appreciated the mode of delivery as well.
A benefit of online courses is the ease with which faculty can control their pace of instruction. When asked, we found that 97.4% of respondents identified they would do more faculty development programs online.
When we reviewed the online tracking statistics, we found that our participants were accessing materials at all hours. Participants, each with their own learning style, appreciated the mix of interactivity and self-study the online format offered.
IV. DISCUSSION
Ideally, we would like to know how effectively participants in the TACT program incorporated the teaching principles into their own practices in the real clinical world. However, it is very challenging methodologically to do this, and it appears the best we can do is to ask about participant impressions and insight into their experience.
It appeared that the TACT program provided a rich opportunity for participants to interact and share their quest to understand and refine the metacognitive aspects associated with their clinical decision-making and critical thinking processes. It also provided our participants with the language to describe and teach these processes to trainees.
V. CONCLUSION
In summary, the TACT program shows promise in engaging distributed faculty to further their curiosity and interest in how to improve, teach and foster critical thinking skills within medical education and in their own practice. We recognise that although this online asynchronous mode of delivery may not be appropriate to meet the diverse learning styles of all potential participants, the favourable reviews we have received from our program graduates highlighted that the flexible interactivity with the content contributed to the success of the TACT program.
Notes on Contributor
Simon Field assisted in the initial development of the TACT program and contributed to the data analysis and writing of the article.
Pat Croskerry was a founding member of the Critical Thinking Advisory Group, and contributed to the development of the TACT program and to the writing of the article.
Susan Love has been an active contributor to the running of the TACT program, designed the survey tools, collected and analyzed qualitative and quantitative data from the program evaluation, and contributed to the writing of the article.
Peggy Alexiadis Brown collected and analyzed qualitative and quantitative data from the program evaluation survey tools, and contributed to the writing of the article.
All authors have reviewed and approved the final manuscript.
Ethical Approval
The data gathered for this article was collected anonymously as part of Program Evaluation, and a written waiver has been obtained stating that it is exempt from full institutional Research Ethics approval.
Acknowledgement
We acknowledge the valuable support and contribution of Deirdre Harvey and other members of the Critical Thinking Advisory Group. For further information on how to implement a similar program in your region, please feel free to contact us.
Funding
There is no funding associated with this project.
Declaration of Interest
None of the authors have any conflicts of interest to declare, and they do not receive any financial assistance or funding for their participation in the TACT program.
References
Abrami, P. C., Bernard, R. M., Borokhovski, E., Waddington, D. I., Wade, C. A., & Persson, T. (2015). Strategies for teaching students to think critically: A meta-analysis. Review of Educational Research, 85(2), 275-314. https://doi.org/10.3102%2F0034654314551063
Brezis, M., Orkin-Bedolach, Y., Fink, D., & Kiderman, A. (2016). Does physician’s training induce overconfidence that hampers disclosing errors? Journal of Patient Safety, 15(4) 296-298. https://doi.org/10.1097/pts.0000000000000255
Cook, D. A., & Steinert, Y. (2013). Online learning for faculty development: a review of the literature. Medical Teacher, 35(11), 930-937. https://doi.org/10.3109/0142159X.2013.827328
Croskerry, P. (2018). A model for clinical decision-making in medicine. Medical Science Educator, 27(Suppl 1), S9-S13. https://doi.org/10.1007/s40670-017-0499-9
Steinert, Y. L., McLeod, P. J., Conochie, L., & Nasmith, L. (2002). An online discussion for medical faculty: An experiment that failed. Academic Medicine., 77(9), 939-940. https://doi.org/10.1097/00001888-200209000-00046
*Simon Field
Dept of Emergency Medicine,
Dalhousie University, Halifax,
Nova Scotia, Canada
Email: simonfield@dal.ca
Submitted: 16 March 2022
Accepted: 26 May 2022
Published online: 4 April, TAPS 2023, 8(2), 57-65
https://doi.org/10.29060/TAPS.2023-8-2/OA2778
Vijay Kautilya Dayanidhi1, Arijit Datta2, Shruti P Hegde3 & Preeti Tiwari4
1Department of Forensic Medicine, Medicine, Manipal Tata Medical College, MAHE, India; 2Department of Forensic Medicine, Medicine, Pramukhswamy Medical college, India; 3Department of Ophthalmology, Medicine, Manipal Tata Medical College, MAHE, India; 4Department of Community Medicine, Medicine, Pramukhswamy Medical college, India
Abstract
Introduction: Summative assessments play a major role in shaping the student’s learning. There is little literature available on validity of summative assessment question papers in Forensic Medicine & Toxicology. This study analyses 30 question papers from 6 reputed universities for content validity.
Methods: A retrospective cross-sectional record-based observational study was conducted where 30 university summative question papers in Forensic Medicine & Toxicology from 6 universities across India were evaluated for content validity. The learning domain assessed, the type of questions asked, and sampling of the content was compared and presented in the results.
Results: From the results of the study, it was noted that 80% weightage was allotted to recall in most papers and only one paper tested for application. 70 to 80% of the marks were allotted to Forensic Pathology leading to disproportionate sampling. Core areas in Toxicology and Medical Jurisprudence were sparsely assessed.
Conclusion: The content validity of the summative question papers in Forensic Medicine and Toxicology was unsatisfactory, emphasising the need for evaluation of the clarity and efficacy of the blueprints being used by the universities. Faculty training to motivate and influence a change in the mindset is necessary to bring about a course correction.
Keywords: Forensic Medicine & Toxicology, Summative Assessments, University Assessments, Blueprint, Content Validity, Learning Domains
Practice Highlights
- Content validity of the Forensic Medicine & Toxicology university exam question papers form six universities was studied.
- It was observed that certain subtopics like Forensic Pathology over time have been over value (80% Weightage).
- Core areas in Medical Jurisprudence and toxicology like substance abuse, environmental toxicology, and pharmaceutical toxicity have been undervalued.
- None of the QPs analysed tested for application. Most items in the assessment tested only recall.
- The blueprints for the paper setters, considering the competencies to be assessed must be designed and validated.
I. INTRODUCTION
Reflecting on our learning experience during MBBS, we realised that we have always had issues with the examination system. The questions are vague and clustered around few important topics. Undergraduate students look up to previous examination question papers as references to decide the stake to be allotted to the topics while preparing for examination. Invariable all students attempt to predict the examination pattern and allot appropriate time and efforts to different subjects, skills, and topics. This reiterates George E Miller’s quote “Assessment drives Learning”. Summative assessments need to be planned appropriately as medicine has high stakes (Amin et al., 2006). Properly designed and executed assessments are known to have a “positive steering effect on the student’s learning. They are also needed to evaluate the programs. Improper assessments can drive a hidden curriculum leading to a completely unintended outcomes (Amin & Khoo, 2003, pp. 260).
Competency Based Medical Education (CBME) model being adopted in India as per the new Graduate Medical Education Regulations 2019, has attempted to bring about a radical change in the educational process. Undergraduate examinations in India are shifting towards a criteria-based process (Aggarwal & Agarwal., 2017; Bhattacharya et al., 2017; Mehta & Kikani, 2019). Outcome based education demands that the examinations be designed to sample and evaluate specific competencies prescribed. The success of these models strongly depended on the validity of the examination process. Summative assessments require that the assessment tool be validated. Key outcomes need to be tested (Amin & Khoo, 2003, pp. 260; McAleer, 2001). Content validity and construct validity are two very important aspect that support the effectiveness of an assessment. Content validity tests the representativeness of the learning objectives in the assessment tool and construct validity represents the congruence of the assessment tool with the intended purpose (Amin & Khoo, 2003, pp. 260).
Forensic Medicine and Toxicology in India, trains the undergraduate to apply their knowledge gained in Medicine for the benefit of law. It is a culmination of Forensic Pathology, Medical Jurisprudence and Toxicology put together. Its key objective is to empower Indian Medical Graduates in handling Medical Legal issues and critically apply their medical skills in delivering justice. Emphasis is also placed on training in etiology, identification, and management of Poisoning ( Sharma et al., 2005). Studies on student perception suggest that teaching is significantly teacher centric and theory oriented. Skill training in Medical Jurisprudence and Toxicology is significantly neglected. Students allege though they value the subject, they spend less time as only select concepts are emphasised (Gupta et al., 2017; Parmar, 2018; Sharma et al., 2005; Sudhan & Raj, 2019). As the new CBME UG curriculum 2019 is being rolled out it is necessary that deficiencies in the traditional curriculum be identified in order to deliver an efficient and effective Forensic Medicine & Toxicology curriculum (National Medical Commission, 2018).
Summative theory exams inherently have a challenge with distribution of the items being tested (Aggarwal & Agarwal, 2017; Amin et al., 2006; Amin & Khoo, 2003, pp. 260; Bhattacharya et al., 2017). Validity of the content being tested in examination is always in question. Selecting appropriate questions, question types and domain can make all the difference in the validity of the examination (Amin et al., 2006; Amin & Khoo, 2003, pp. 260; McAleer, 2001). Particularly in Forensic Medicine which is purely application-based course, testing critical thinking and synthesis is necessary. This is found wanting in the traditional curriculum (Parmar, 2018; Sharma et al., 2005; Sudhan & Raj, 2019). Published literature on systematic analysis of summative assessment question papers in Forensic Medicine & Toxicology are sparsely available. In this study, we have analysed and compared undergraduate summative examination question papers of Forensic Medicine & Toxicology from six reputed universities all over India for the distribution of content tested, Domain of learning and Construct of the question.
II. METHODS
A retrospective cross-sectional record-based observational study was conduct at Government Medical College, Bharatpur after obtaining ethical approval from the Institutional Ethics Committee between October to December 2020. For the study, 30 summative exam question papers from six reputed medical universities were selected based on the availability of the University question papers in public domain. The last five-year (2016-20) undergraduate question papers in Forensic Medicine & Toxicology were collected from the university websites and the college records from constituent colleges after thorough web search. The names of the universities have been kept anonymous during the analysis of results. All the data was collected form sources in public domain hence explicit consent was not taken. Two of the selected universities were based in North India and four universities were based in South India. The identity of the Medical Universities was kept confidential during the analysis of the question papers.
The Summative theory examination in Forensic Medicine & Toxicology as per the Medical Council of India (MCI) regulations consists of one theory paper of minimum 40 marks. The question paper consists of essay type questions and objective questions like very short answer questions or Multiple-choice questions depending on the universities (National Medical Commission, 2018).
For analysis, the questions were categorised based on the question type as LEQ (Long Essay Question), SAQ (Short Answer Question) & VSAQ (Very Short Answer Question including MCQs). The Questions were also categorised based on the domain of learning as Recall Based, Comprehension Based and Application Based Questions.
The Topics in Forensic Medicine & Toxicology can be broadly subdivided into Medical Jurisprudence, Forensic Pathology and Toxicology. These were further subdivided as Six Categories as Legal Procedure, Medical jurisprudence, Forensic Pathology, Forensic Psychiatry, Lab Technique, emerging trends, and Toxicology (Medical Council of India, 1997). Percentage of marks allotted to each of these topics was analysed in each of the papers.
Further, Forensic Pathology was Sub divided into Subtopics like Identification, Postmortem Changes, Mechanical Injuries, Mechanical Asphyxia, Thermal Deaths, Sexual Offences and Medico Legal issues related to Pregnancy, Delivery, Abortion. Toxicology was Sub divided into General Toxicology, Chemical Toxicology, Drug, Pharmacy & Substance abuse Toxicology, Bio toxicology (Medical Council of India, 1997). Percentage allotment of Marks in each of the question papers was analysed for each of the subtopics.
The data thus collected was tabulated in an Excel Sheet and the percentage distribution of marks in various subtopics noted. The SPSS Statistical Software (IBM SPSS Statistics for Windows, Version 23.0) was used to analyse the data. Radar Graphs and line graphs were plotted to represent and compare pattern of distribution of marks in various topics in each question paper. The type of questions asked, the weightage allotted to the subtopics were compared keeping in mind the expected outcomes in the Forensic Medicine & Toxicology curriculum proposed by National Medical Commission and Medical Council of India for content validity (Medical Council of India, 1997; National Medical Commission, 2018). The learning domain targeted in the questions was compared for construct validity of the question papers.
III. RESULTS
In this study, five question papers(n=30) from each university(n=6) were analysed and compared. The data that supports the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.Fig share.19367864 (Kautilya et al., 2022).
As regulated the university Summative examination in Forensic Medicine & Toxicology consists of one theory assessment and one practical assessment (Medical Council of India, 1997; National Medical Commission, 2018). The theory paper is allotted a minimum of 40 marks. Five universities conducted exam for 40 marks and one university paper was of 100 marks. All question papers had three types of questions, namely Essay questions (Long Answer Questions-LAQs) of 8 to 10 marks each, short essays (Short Answer questions-SAQs) of 3-5 marks each and Objective questions (like Multiple choice questions-MCQs or Very short answer questions- VSAQs) of 1-2 marks each. Table 1 presents the percentage distribution of the marks allotted to each question type.
|
University
|
% Marks LAQ |
% Marks SAQ |
% Marks VSAQ/ MCQ |
|
U1 |
43 |
49.5 |
7.5 |
|
U2 |
25 |
50 |
25 |
|
U3 |
20.4 |
51.2 |
28.4 |
|
U4 |
25 |
50 |
25 |
|
U5 |
25 |
56 |
19 |
|
U6 |
42 |
40.5 |
17.5 |
Table 1. University vice distribution marks in the question papers based on the type of questions
Nearly 50% of the marks in all universities is allotted to Short Essay or Short Answer question types. This was followed by Long Answer questions and very short answer questions respectively. Relative to the number of marks allotted to each question type the university question papers consisted of 11 to 22 items or questions in every question paper.
A. Domain of the Learning Tested
Theory questions papers attempt to test the knowledge/ cognition of the students. Limiting the questions to just recall type affects the quality of the question paper. Medicine and Forensic Medicine, requires application of knowledge. Testing of higher order cognition is necessary for the assessment to be Valid. To evaluate this the questions were categorised into Recall type, Comprehension type and application type. The percentage distribution of marks in each question paper was also analysed and presented in the Line graph (Figure 1).
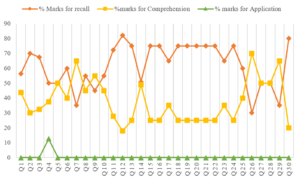
Figure 1. Comparison of percentage mark distribution based on the domain of learning
B. Distribution of Marks Based on the Subtopics
The Graduate Medical education regulation- 2019 further divide the subject of Forensic Medicine and Toxicology into Forensic Pathology, General Information and legal procedures, medical jurisprudence, Forensic Psychiatry, Toxicology, Lab investigations and general trends. The question papers were further analysed for the percentage distribution of marks among these six subtopics and presented in a radar graph in Figure 2.
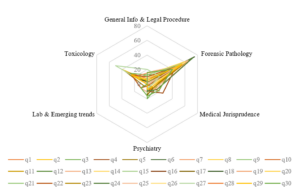
Figure 2. Topic wise distribution of marks (%) in the question papers
From the graph it is noted that Forensic Pathology receives the most attention in almost all the question papers from all the universities. Forensic pathology can further be divided into seven subtopics. From the total marks allotted in each paper for forensic Pathology, percentage marks allotted for each of these subtopics was calculated and presented as a separate radar graph in Figure 3.
Figure 3. Percentage distribution of marks in Forensic Pathology in the question papers
Toxicology can further be divided into subtopics like General Toxicology dealing with management of poisons, Chemical Toxicology, drug-pharmacy, and substance abuse dealing with pharmaceutical agents and banned substances, Bio and environmental toxicology dealing with snakebite, venomous stings, mushrooms, Food poisoning and plant toxicology etc. From the total marks allotted to toxicology, the percentage distribution of marks allotted to each of these subtopics was analysed and presented in Figure 4.
Figure 4. Percentage distribution of marks in Toxicology in the question papers
IV. DISCUSSION
The undergraduate medical education curriculum has been governed by the Graduate Medical Education Rule- GMR 1997 (Medical Council of India, 1997) framed by the Medical Council of India over the last two decades and in 2019, the National Medical Commission adopted a competency-based training model to revamp the medical education in India. The National Medical Commission in its series of reports and documents has attempted to identify the lacuna in the old curriculum. To be able to successfully implement this radically new proposal it is necessary that we understand the limitations of the current curriculum. The Graduate Medical Education Rules 1997, like the newer GMER 2019 provides a clear framework of the Undergraduate curriculum. It lays down guidelines on the standards of implementation. The curriculum framework is designed in a manner that there is significant room for the colleges and the Universities to plan and implement the same as they deem best suits them. This however is not the case always. It has been observed in various previous studies that universities and colleges sometimes fall short of the expectations (Medical Council of India, 1997; National Medical Commission, 2018; Sharma et al., 2005).
Previous studies attempting to gauge the student’s perception on the implementation of Forensic Medicine and Toxicology curriculum have raised serious doubts among the academicians. Kumar et al. (2018) in their study of student’s perception revealed that 20% of the students felt that autopsy was a mere formality and 64% felt the need for student involvement during the autopsy training. Mardikar and Kasulkar (2015) revealed that 89% of the Interns and 41% of the residents didn’t have any exposure to handling medico-legal cases. It was noted that only 14% of the Interns and 21% of the residents were aware of the proper preservatives to be used for body fluids in poisoning. Only 32% of the interns and 46% of the residents were aware of Medical Indemnity Insurance. Only 13% of the interns were aware of the consumer protection act. There is a serious disconnect between the proposed and the implemented curriculum in forensic medicine.
As per the guidelines framed by the Medical Council of India in the GMER-1997, a variety of essay questions and short answer questions are permitted. Objective question like Very Short Answer questions and MCQs are permitted to the extent of 20 % only (Medical Council of India, 1997). Most of the question papers analysed in this study conformed to this regulation. From the Table 1 it can be noted that nearly 50% of the marks were allotted for short essay/Answer questions (SAQ) requiring a descriptive answer. Long Answer Questions (LAQ) requiring an elaborate explanation of the concepts represented about 20% to 42 % of the question paper. The total marks allotted for the individual questions also varied with the LAQs being allotted between 8 to 10 marks each, SAQs being allotted 3 to 5 marks and VSAQs being allotted 1- 2 marks each. Thus, the Number of Items included in each question paper ranged from 11 to 22. This distribution is similar to the analysis published in papers of other subjects like microbiology, Pharmacology, anatomy, Physiology etc (Aggarwal & Agarwal , 2017; Ayub et al., 2013; Bhattacharya et al., 2017; Choudhary et al., 2012; Chowdhury et al., 2017; Mehta & Kikani, 2019; Pichholiya et al., 2021).
With the number of items being limited the chance of certain areas being missed increases. This has a profound influence on the sampling while making the blueprint (Raymond & Grande, 2019). In papers with only 11 Items, there is a definite probability of certain topics being left out compared to papers having 22 items. As Forensic Medicine and Toxicology has only one paper compared to other subjects which have two papers in the second year MBBS, some key topics get left out, adversely effecting its content validity.
A. Analysis of the Domain of Learning Tested
From the Figure No 1, it can be observed that in about 10 of the 30 papers, more than 75% of the questions/ Items tested recall. In only 7 of the 30 papers, more than 50% of the marks were allotted to comprehension. In only one paper the application was assessed to an extant of 12.5%. This is similar studies done in Anatomy, Physiology, Pharmacology, and microbiology (Aggarwal & Agarwal., 2017; Bhattacharya et al., 2017; Choudhary et al., 2012; Chowdhury et al., 2017; Mehta & Kikani, 2019).
This raises a serious doubt on the construct validity of the question papers. Forensic Medicine and Toxicology, an application-based course requires that higher order cognition like application is tested. The current papers fall short of assessing the right competency domains. The Regulations prescribed by the GMER-1997 require that the at least one long answer question (LAQ) of 10 marks (i.e., 25% of the Marks) testing application is asked in the theory question paper (Medical Council of India, 1997). The newer Competency based medical education Regulations prescribed in the GMER- 2019 document also reiterate this fact and in addition suggest that an application based question including Attitude, Ethics and communication skills module be included in every paper (National Medical Commission, 2018). This needs serious introspection in the times to come.
B. Content Validity of the Question Papers
The content validity of a test depends strongly on how well the sample is spread across the syllabus. From the analysis of the percentage distribution of marks allotted to different subtopics presented in figure no 2, it is very clear that in majority of the question papers the bulk of the questions asked are from forensic pathology. There is distinct skewing of the graph toward forensic pathology with an average allocation of 60% of the marks.
This is like studies in physiology with over 42% of the marks being allotted to Cardiovascular system. The observations in the figure no 2 classically suggest that the forensic medicine and toxicology curriculum is a victim of “Carcinoma of the Curriculum” (Abrahamson, 1978). Over a period, certain section of the curriculum takes precedence and are valued more than other equally relevant sections. Core areas like Toxicology and Medical Jurisprudence which are clinically more relevant to the undergraduate students, considering their role as a physician of the first contact, seem to have been blatantly missed and neglected. Faculty should reflect on the factors that might have caused this drift which over time has led to this dangerous disease of the curriculum.
The New Competency based UG curriculum being implemented by the National Medical Commission wonderfully provides a framework of competencies in forensic medicine and toxicology (National Medical Commission, 2018). They serve as guiding milestones to reorient and redistribute the weightage, time and value allotted to certain topics.
From the Percentage marks allotted to each of these subtopics in forensic pathology in Figure no 3 it clearly shows that over 60 to 70% of the marks allotted were distributed among just 3 key topics i.e., Post-Mortem Changes, Mechanical Injuries and Asphyxia. The source of the error in the assessment is this high value allotted to theoretical aspects related to Autopsy and Medical examination. The faculty and the student’s attention have shifted towards the conduct of postmortem examination which is generally a high stakes scenario. But only a handful of undergraduates end up doing autopsies in their career. The ability to do autopsy is no doubt an important competency for the Undergraduates but the competencies related to Medical Jurisprudence and Toxicology are equally Important. The competencies related to handling Medico- legal issues related to patient care are encountered more frequently by an undergraduate thus requiring additional attention in the undergraduate curriculum than Forensic Pathology which is a rare or chance encounter for an MBBS graduate in India (Kumar et al., 2018; Medical Council of India, 1997; National Medical Commission, 2018; Sharma et al., 2005).
An Indian Medical graduate needs to make accurate observation, logical deductions and take critical decisions applying medical ethics in patient care. He should be able to diagnose and manage the common cases of poisoning as a physician of the first contact (Kumar et al., 2018; Medical Council of India, 1997; National Medical Commission, 2018; Sharma et al., 2005).
Most of the competencies in Toxicology are covered in the Forensic Medicine curriculum rather than in General Medicine. Hence, the percentage marks allotted for various subtopics of toxicology was also analysed in figure no 4. From figure no 2 it can be noted that about 20% of the marks were allotted to toxicology. Further considering figure no 4 it can be observed that 60-80% of the marks for toxicology was allotted to general toxicology and chemical toxicology showing a skewing in the distribution of marks.
Assessments must complement the roles of the undergraduate after completion of the course. Snake bite, an occupational disease in India, is an emergency frequently encountered by physicians of first contact (Vijay & Hegde, 2019). Substance abuse and pharmaceutical toxicity are also some of the most encountered cases in clinical practice following pesticide abuse (Basu & Mattoo, 1999). As a curriculum planner it is imperative that these factors considered as core in the curriculum (Amin et al., 2006; Amin & Khoo, 2003, pp. 260; McAleer, 2001). The current UG curriculum is deficient as certain areas have been undervalued leading to poor perception about the subject. Students undervalue the subject as the core competencies tested are not relevant considering their role as physician of the first contact. Students allot little time to study as most assessments cover few topics leading deterioration in the quality of teaching and learning in the course (Sharma et al., 2005).
Adult learners value learning bases on its immediate applicability and its use in problem solving. Curriculum must value topic and skill that complement the roles the learner after the training. Medical jurisprudence and toxicology have not been sufficiently assessed in this curriculum.
V. CONCLUSION
From the above discussion, it is reiterated that the university assessments in Forensic Medicine and Toxicology need to be realigned with the curricular needs. Certain subtopics like Forensic Pathology have been over valued compared to Medical Jurisprudence and Toxicology which have been undervalued. The sampling in Forensic Medicine and Toxicology assessment is not ideal. Application must be tested instead of just recall.
Universities need to periodically Assess their question papers for validity and chalk down clear guidelines for the paper setters. The current blueprints being used must be revalidated to check if there is clarity and scope of improvement. Most importantly, training the faculty and the question paper setters to use the blueprint and value the competencies mandated by the Curriculum lies at the heart of the solution to this problem. Overtime, this curricular malignancy observed, has had a profound effect on the mindsets of the faculty trainers. Faculty Developments activities to motivate and influence these mindsets to bring change is indispensable. The Application centered regulations prescribed by the National Medical Commission provides an excellent opportunity to motivate positive changes leading to the required course correction.
Notes on Contributors
Dr Vijay Kautilya was instrumental in conseptualising the idea, designing the study, data collection, data analysis, drafting and reviewing the manuscript.
Dr Arijit Datta contributed in designing the study, data collection, data analysis, drafting and reviewing the manuscript.
Dr Shruti P Hegde was instrumental in designing the study, data analysis, drafting and reviewing portions of the manuscript.
Dr Preethi Tiwari, contributed in data collection, data analysis, drafting and reviewing portions of the manuscript.
Ethical Approval
Institutional Ethics committee approval was received from the IEC, Government Medical College, Bharatpur where the study was conducted (GMCB/IEC/2020/009 dated 26th September 2020).
Data Availability
Datasets generated and/or analysed during the current study are available from the following DOI.
https://doi.org/10.6084/m9.figshare.19367864
Acknowledgement
We wish to acknowledge the Faculty of Forensic Medicine and Toxicology at MTMC, Jamshedpur for assisting in procurement of the question papers.
Funding
No external funding was received for the conduct of this study.
Declaration of Interest
There is no conflict of Interests to the best of our knowledge.
References
Abrahamson, S. (1978). Diseases of the curriculum. Academic Medicine, 53(12), 951-957. https://doi.org/10.1097/00001888-197812000-00001
Aggarwal, M., & Agarwal, S. (2017). Analysis of undergraduate pharmacology annual written examination papers at Pt. B. D. Sharma University of health sciences Rohtak. National Journal of Physiology, Pharmacy and Pharmacology, 7(5), 509. https://doi.org/10.5455/njppp.2017.7.1236224012017
Amin, Z., Chong, Y. S., & Khoo, H. E. (2006). Practical guide to medical student assessment. World Scientific. https://doi.org/10.1142/6109
Amin, Z., & Khoo, H. E. (2003). Basics in Medical Education. World Scientific.
Ayub, M., Habib, M., Huq, A., Manara, A., Begum, N., & Hossain, S. (2013). Trends in covering different aspects of anatomy in written undergraduate MBBS course. Journal of Armed Forces Medical College, Bangladesh, 9(1), 75-83. https://doi.org/10.3329/jafmc.v9i1.18729
Basu, D., & Mattoo, S. K. (1999). Epidemiology of substance abuse in India: Methodological issues and future perspectives. Indian Journal of Psychiatry, 41(2), 145-153.
Bhattacharya, S., Wagh, R., Malgaonkar, A., & Kartikeyan, S. (2017). Analysis of content of theory question papers in preliminary examinations and marks obtained by first-year MBBS students in physiology. International Journal of Physiology, Nutrition and Physical Education, 2(2), 856-868.
Choudhary, R., Chawla, V. K., Choudhary, K., Choudhary, S., & Choudhary, U. (2012). Content validity of first MBBS Physiology examinations and its comparison with teaching hours devoted for different sub-divisions of physiology. Journal of Physiology and Pathophysiology, 3(1), 8-11.
Chowdhury, D. K., Saha, D., Talukder, M. H., Habib, M. A., Islam, A. S., Ahmad, M. R., & Hossin, M. I. (2017). Evaluation of pharmacology written question papers of MBBS professional examinations. Bangladesh Journal of Medical Education, 8(2), 12-17. https://doi.org/10.3329/bjme.v8i2.33331
Gupta, S., Parekh, U. N., & Ganjiwale, J. D. (2017). Student’s perception about innovative teaching learning practices in forensic medicine. Journal of Forensic and Legal Medicine, 52, 137-142. https://doi.org/10.1016/j.jflm.2017.09.007
Kumar, A., Kumar, S., Goel, N., Ranjan, S. K., Prasad, M., & Kumari, P. (2018). Attitude of undergraduate medical students towards medico-legal autopsies at IGIMS, Patna, Bihar. International Journal of Medical Research Professionals, 4(6), 132-135.
Kautilya, D. V., Datta, A., Hegde, S. P., & Tiwari, P. (2022). Evaluating the content validity of the undergraduate summative exam question papers of forensic medicine & toxicology from 6 medical universities in India. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.19367864
Mardikar, P. A., & Kasulkar, A. A. (2015). To assess the need of medicolegal education in interns and residents in medical institution. Journal of Evolution of Medical and Dental Sciences, 4(17), 2885-2889. https://doi.org/10.14260/jemds/2015/417
McAleer, S. (2001). Formative and Sumative assessment. In J. A. Dent, & R. M. Harden, A Practical Guide to Medical teachers (pp. 293-302). Edinbergh Churchill Livingstone.
Medical Council of India. (1997). Regulations on Graduate medical education, 1997. https://www.nmc.org.in/wp-content/uploads/2017/10/GME_REGULATIONS-1.pdf
Mehta, S., & Kikani, K. (2019). Descriptive analysis of II – MBBS university question papers of microbiology subject. Journal of Education Technology in Health Sciences, 6(2), 44-47. https://doi.org/10.18231/j.jeths.2019.011
National Medical Commission. (2018). Competency based undergraduate curriculum for the indian medical graduate. https://www.nmc.org.in/information-desk/for-colleges/ug-curriculum/
Parmar, P. (2018). Study of students’ perceptions towards case based learning in forensic medicine. Indian Journal of Forensic Medicine & Toxicology, 12(1), 154-160.
Pichholiya, M., Yadav, A., Gupta, S., Kamlekar, S., & Singh, S. (2021). Blueprint for summative theory assessment in pharmacology – A tool to increase the validity as per the new competency based medical education. National Journal of Physiology, Pharmacy and Pharmacology, 11(12), 1345-1355. https://doi.org/10.5455/njppp.2021.11.06170202107072021
Raymond, M. R., & Grande, J. P. (2019). A practical guide to test blueprinting. Medical Teacher, 41(8), 854-861. https://doi.org/10.1080/0142159x.2019.1595556
Sharma, B., Harish, D., & Chavali, S. (2005). Teaching, training and practice of forensic medicine in India-An overview. Indian Journal of Forensic medicine & Toxicology 27(4), 247-251.
Sudhan, S. M., & Raj, M. N. (2019). Current status of knowledge, attitude and awareness of medical students on forensic autopsy in Tumkur district of Karnataka. Indian Journal of Forensic Medicine & Toxicology, 13(1), 131-141.
Vijay, D. K., & Hegde, S. P. (2019). Study of snake bite and factors influencing snake bite among the rural population of Kancheepuram district. Journal of Punjab Academy of Forensic Medicine & Toxicology, 19(2), 142-146.
*Vijay Kautilya D
Kadani Road, Baridih,
Jamshedpur-831017
Jharkhand, India.
+919448651848
Email: kautilya.dacroo@gmail.com
Submitted: 19 August 2022
Accepted: 5 December 2022
Published online: 4 April, TAPS 2023, 8(2), 47-56
https://doi.org/10.29060/TAPS.2023-8-2/OA2869
Edyta Truskowska1, Yvonne Emmett2 & Allys Guerandel1
1Department of Psychiatry, Faculty of Medicine, University College Dublin, Ireland; 2National College of Ireland, Ireland
Abstract
Introduction: Digital Badges have emerged as an alternative credentialing mechanism in higher education. They have data embedded in them and can be displayed online. Research in education suggests that they can facilitate student motivation and engagement. The authors introduced digital badges in a Psychiatry module in an Irish University. Completion of clinical tasks during the student’s clinical placements, which were previously recorded on a paper logbook, now triggers digital badges. The hope was to increase students’ engagement with the learning and assessment requirements of the module.
Methods: The badges – gold, silver and bronze level – were acquired on completion of specific clinical tasks and an MCQ. This was done online and student progress was monitored remotely. Data was collected from the students at the end of the module using a questionnaire adapted from validated questionnaires used in educational research.
Results: The response rate was 68%. 64% of students reported that badges helped them achieve learning outcomes. 68% agreed that digital badges helped them to meet the assessment requirements. 61% thought badges helped them to understand their performance. 61% were in favour of the continuing use of badges. Qualitative comments suggested that badges should contribute to a higher proportion of the summative mark, and identified that badges helped students to structure their work.
Conclusions: The findings are in keeping with the literature in that engagement and motivation have been facilitated. Further evaluation is required but the use of badges as an educational tool is promising.
Keywords: Medical Education, Digital Badges, Students’ Engagement, Continuous Assessment Gamification, Health Profession Education
Practice Highlights
- Digital badges may enhance student engagement.
- Digital badges may promote motivation for learning.
- Evaluation of digital badges using a questionnaire with ordinal analysis of data and coding of free comments.
- Majority of students reported working harder than in a non-gamified module.
- Digital badges provided structure and direction to the student’s learning.
I. INTRODUCTION
Educational research recognises student engagement as valuable and as having significant impact on their learning (Mandernach, 2015). While searching for tools impacting on engagement, educators observed that games have been good at engaging players for decades, through their ability to sustain players’ attention and keep them motivated throughout the games (Przybylski et al., 2010). This level of engagement is desirable to both students and educators. This achievable level of engagement in gaming strategies has led to the exploration of its use in education. Elements from game design applied in non-game contexts to influence, engage and motivate individuals and groups have resulted in the development of a new field known as gamification (Deterding et al., 2011).
Digital badges are common tools of gamification (Barata et al., 2013). They are frequently used by game designers and in recent years also by educators. A digital badge used in education can be a validated symbol of academic achievement, accomplishment, skill, quality or interest (HASTAC, n.d.). Digital badges are digital images obtained through the completion of some pre-specified goals that are annotated with metadata and that can be displayed online (Hensiek et al., 2017). In higher education badges have been used to recognise a student’s participation in a learning activity, to help students explicitly and visually capture and monitor progress made on learning tasks, to recognise the achievement of skills and competencies and to serve as a means of certifying these achievements. They are reported to have a positive effect on the learners’ motivation if they are considered as awards or if they trigger competition among peers (Yildirim et al., 2016).
It appears that the value of digital badges depends on their design (when awarded, for what, and what they mean). For example, the use of badges as credentials only, has been criticised for focusing exclusively on extrinsic motivating factors, which have less impact on engagement than intrinsic ones (Seaborn & Fels, 2015). This is why combining the use of badges, as credentials as well as using them within the assessment process appears to be a better idea. Considering, that assessment has proven to have the most impact on effective learning, the use of badges during structured assessment has been favoured by educators (Abramovich, 2016; Rolfe & McPherson, 1995). The assessments that have potential to generate formative and summative feedback are presented as particularly useful (Armour-Thomas & Gordon, 2013). Digital Badges represent a viable alternative to existing methods of assessment in educational institutions and in the work environment (Dowling-Hetherington & Glowatz, 2017). It was also noted that access to regular feedback (broadly available in games) is helpful to learners. Students that are given opportunities to complete a task and learn from their mistakes do better in overall assessment. Games are a great example of the design where a player learns through feedback, gets better and eventually becomes successful (McGonigal, 2011). Similarly, the literature states that the use of badges has potential to offer a sort of “covert assessment”, meaning that students can approach a task as if it was a game. This helps to maintain the benefits of assessment while minimizing the potential for unhelpful levels of test anxiety (McGonigal, 2011) (Abramovich et al., 2013).
Another advantage given for the use of digital badges is their potential for remote monitoring of students’ progress and their difficulties by instructors and tutors (Huang & Soman, 2013). There is a growing momentum for the use of digital badges as an innovative instruction and credentialling strategy in higher education (Noyes et al., 2020).
In our University, Psychiatry is taught as a 10-credit module to both undergraduate and graduate entry students in the final stage of their degree in medicine. Typically, approximately 240 students are taught the module in four different groups: two groups in the spring and two groups in autumn, for six weeks at a time. Face to face teaching is centralized on Mondays and Fridays. Clinical teaching is delivered during the rest of the week and takes place in multiple different clinical centres. The overall assessment of this module comprised a continuous assessment with specific formative and summative tasks recorded in a paper logbook. The summative tasks were worth 20% of their overall assessment.
Standardising the student clinical experience, engaging them in their clinical placements and monitoring their attendance and progress can be challenging. The paper logbook/portfolio we were using was inadequate in that it did not allow for central monitoring of progress and often the difficulties students were encountering came to the attention of the teaching staff only when the logbook was handed over at the end of the module. Provision of feedback on progress was also limited. We felt that, in particular, students that were slow to progress were missing potential remediation before the summative assessments. We also encountered practical difficulties such as lost logbooks that affected the continuous assessment process.
We felt that digital badges offered a way of monitoring attendance and participation in tasks remotely, providing feedback, facilitating remediation and allowing students’ gauge how they are doing in relation to their peers while optimizing engagement in the clinical placements and structuring the learning to sustain progress through the module. We introduced and piloted the use of digital badges in the Psychiatry module as part of the continuous assessment. We carried out a descriptive study to appraise the potential usefulness of digital badges as part of our teaching strategy.
II. METHODS
A. Course Design
Students taking the 6-week Psychiatry module start their clinical placement on day 2 of the Module. Each week, students participate in their continuous assessment in order to collect their weekly badge. To acquire a badge, they need to complete and upload specific clinical tasks including formative clinical cases scheduled for them, to upload a Clinical Placement Form signed by the consultant on the team they are attached to and do an online multiple-choice question test at the end of the week. As all of this is done online their progress can be monitored remotely by the teaching team independent of the location of their clinical placement. Collecting their weekly badges provides them with 5% of their continuous assessment mark. The other marks for continuous assessment come from a summative clinical case (90%) and a reflective assignment (5%). Continuous assessment contributes to 20% of overall assessment mark.
B. Badges Design
Tutors in Psychiatry in conjunction with the University’s Teaching and Learning Department created Badges. It was part of an institution-wide digital badging pilot project (UCD Teaching and learning, 2017). It was agreed that there would be three types of badges -bronze, silver and gold – obtained and displayed on the university’s virtual learning environment (currently, Brightspace). As noted above students receive a digital badge on completion of assigned tasks, which are part of their continuous assessment. The type of badge awarded depends on the MCQ score and it is displayed on the student’s Blackboard profile. Figure 1 depicts the process. It shows that all badges are contributing to 5% of the module continuous assessment. Every week students receive information as to what percentage of the group has acquired a bronze, silver or gold badge so they have an idea of their performance in relation to that of the rest of the group.
Figure 1. Step-by-step the process of getting/awarding a badge
C. Questionnaire
The ‘Digital Badges Experience Survey’ questionnaire was designed based on previously described surveys: the ARCS Badge Motivation Survey (Foli et al., 2016) and the Badge Opinion Survey (Abramovich et al., 2013) with some additional questions suggested by the literature on digital badges. The authors and faculty members identified and agreed on the following constructs as being relevant to our teaching delivery and our study: previous knowledge of digital badges (items 1 & 2), their meaning and relevance to students (items 22, 13, 14, 12, 8 & 5) motivation and engagement (items 3, 4 & 23), relevance to assessment and feedback (items 11, 9, 10, 24, 18 & 19), their use in structuring learning (items 15, 6, 7 & 16), self-efficacy (items 17, 20, 21 & 25), social context implication (items 26, 27 & 28). Under each construct, items from the above questionnaires were discussed and agreement reached on the ones to be used, altered or added assessing relevance and acceptability for our aims and teaching context.
Our survey consisted of 30 items with answers displayed on a seven-point Likert Scale. The 31st (final) question required dichotomous (yes/no) answer with space for respondents to explain their reasons for it. We also provided for free commenting from students (Questionnaire is available in Table 1).
Please rate your agreement with each of the statements using the following scale:
|
Strongly Agree |
Agree |
Somewhat Agree |
Neutral |
Somewhat Disagree |
Disagree |
Strongly Disagree |
||
|
+3 |
+2 |
+1 |
0 |
– 1 |
-2 |
-3 |
||
|
Please circle one number for each statement |
Strongly Agree |
|
|
Strongly Disagree |
||||
|
1. I knew what digital badges were before I began this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
2. I have earned digital badges before beginning this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
3. I felt motivated to complete the module because I was earning digital badges. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
4. Compared to other modules on my programme, the digital badges motivated me to work harder. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
5. The digital badges helped me to understand the learning outcomes for this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
6. The digital badges helped me to achieve the learning outcomes for this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
7. The badge helped draw my attention to the clinical seminars. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
8. The digital badges helped me to understand the content of this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
9. The digital badges helped me to understand the assessment requirements for this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
10. I was more aware of the module continuous assessment requirements because I would be earning digital badges. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
11. Because I was earning digital badges, I knew the continuous assessment requirements were important. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
12. Earning digital badges made a difference in how I viewed completing the continuous assessment requirements. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
13. Earning badges made the assignments more significant to me. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
14. The badges increased how relevant the assignments were. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
15. The digital badges helped me to structure my work in this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
16. The digital badges helped me to meet the assessment requirements of this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
17. The badges increased my confidence that I could demonstrate the content of my knowledge. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
18. The digital badges helped me to understand my performance in this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
19. The digital badges helped me to understand my progress through the module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
20. The badges were symbols that I had mastered content. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
21. The badges increased my overall level of satisfaction with completing the continuous assessment requirements. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
22. By earning the badges I was more fulfilled as a student by completing the assessment requirements. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
23. The digital badges made me want to keep on working. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
24. I understand why I earned all of my badges. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
25. The badges I earned represent what I learned on this module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
26. I talked to others about the badges I earned. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
27. I compared the badges I earned with others’ on the module. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
28. The potential to earn digital badges at gold, silver and bronze levels made me feel competitive. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
29. I think digital badges are a good addition to the programme. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
30. I would like to earn digital badges in other modules on my programme. |
+3 |
+2 |
+1 |
0 |
-1 |
-2 |
-3 |
|
|
31. I think the badges are helpful and should be used in the coming years: tick as appropriate and give 3 reasons why |
Yes ☐ |
No ☐ |
||||||
|
32. Any other comments |
||||||||
Thank you for your participation
Table 1. Digital Badges Experience Survey
D. Participants
The questionnaires were distributed to all the students of final year of Medicine in our university at the beginning of the final or sixth week of the module and collected by their tutors. Informed verbal consent was obtained from study participants. As described above, the course was run four times in one academic year, and we collected data from all four groups of students: two in the spring and two in the autumn.
E. Data Collection and Analysis
As noted above, questionnaires were distributed and collected by tutors at the beginning of the sixth (last) week of the Psychiatry Course. The level of student’s agreement with various statements was marked on the 7-point Likert-type scale. Those data were uploaded to Excel. Data from Likert scales can be analysed as ordinal as well as interval data (Sullivan & Artino 2013), (Norman, G. 2010) and we have considered both options. We concluded that using descriptive statistics such as the mean in relation to students’ opinions had limited value (Sullivan & Artino 2013), (Knapp 1990). This is why we decided to analyse our data as ordinal. To simplify the answers, we organised them into three groups: “agreed”, “neutral”, “disagreed”.
Students’ comments were entered into an excel sheet and analysed by two independent researchers. The comments relating to the use of badges in teaching of Psychiatry were coded according to topics, which were identified and agreed upon by the two independent researchers (Johnson & LaMontagne, 1993), (Sundler et al., 2019). Topics were further codified as positive or negative. This way of coding is described and performed in more details in other studies (Quesenberry et al., 2011).
III. RESULTS
A. Demographics
161 out of 237 students completed questionnaires giving a 68% response rate. The response rate was 75% in the first half (from springtime) of the students and 61% in the second (autumn rotation).
B. Analysis of Answers
65% of students had no previous knowledge of digital badges and 93% had never earned a badge before the module as per items 1 & 2 of questionnaire.
1) Meaning and relevance: Item 22: 48% of respondents agreed that by earning the badges they felt more fulfilled as a student when completing the assessment requirements. 31% disagreed. 45% agreed and 39% disagreed that earning badges made the assignments more significant to them (item 13) and similarly only 42% felt the badges increased the sense of how relevant the assignments were, while 40 % disagreed with this view as per item 14.
Earning digital badges made a difference in how 59% of students viewed completing the continuous assessment requirements, (item 12). 29% disagreed with this. 68% students felt that the digital badges helped them to understand the content of this module and 18% disagreed, (item 8). 66% students agreed and 24% disagreed about the fact that digital badges helped them to understand the learning outcomes for this module (item 5).
2) Motivation and engagement: 51% of students that responded felt motivated to complete the module because they earned a digital badge (item 3). 33% did not agree with this. The possibility of earning a digital badge motivated 43% of respondents to work harder (item 4). 39% disagreed with this. The digital badges made 45% of students want to keep on working, while 29% were not impacted (item 23).
3) Assessment and feedback: Item 11: 50% felt that because they were earning digital badges, they knew that the continuous assessment requirements were important. 36% disagreed. The digital badges also helped 69% respondents to understand the assessment requirements for this module but not so for the 15% respondents (item 9). Out of all respondents, 78% were more aware of the module continuous assessment requirements because of the digital badges, and only 15% disagreed with that (item 10). Item 24: As many as 74% of all respondents did and 14% did not understand why they earned their badges. The digital badges helped 61% of students to understand their performance in this module (item18). 27% did not find that badges helped in that way. Similarly, the digital badges helped 61% of students to understand their progress through the module. 22% disagreed with this (item 19).
4) Structure: Out of all respondents 50% agreed and 33% disagreed that the digital badges helped them to structure their work in the module (item 15). 64% of respondents agreed and 21% disagreed that the digital badges helped them to achieve the learning outcomes for this module (item 6). Similarly, the badge helped draw attention to the clinical seminars for 57% of respondents, but not so for 25%. 68% of students (vs 19% who have disagreed) felt that the digital badges helped them to meet the assessment requirements of this module (item 16).
5) Self-efficacy: Item 17: 48% of students agreed (vs 33% who disagreed) that earning the digital badges made them more confident that they could demonstrate the content of their knowledge. Item 20: 41% of all respondents agreed that the badges were symbols of mastering the content of the module. A similar number (40%) of students disagreed and 17% stayed neutral. 59% found the badges increased their overall level of satisfaction with completing the continuous assessment requirements (item 21). 27% disagreed with this. 44% of students agreed and 41% disagreed with the statement that the badges they earned represented their learning in the module (item 25).
6) Social context and competitiveness: 42% of students did and 44% did not talk to others about the badges they earned (item 26). The potential to earn digital badges at gold, silver and bronze levels made 49% of students more competitive (item 28). 39% disagreed with this. 29% of students did and 56% did not compare the badges they earned with others on the module (item 27).
7) Overall: 56% agreed that digital badges were a good addition to the program. 61% of students found digital badges helpful and felt that they should be used in the future. 31% did not agree with the statement and 8% did not answer.
Students’ opinions: 136 students did and 25 students did not write any comment. Students’ comments related either to one or to several topics. Students were positive about the use of badges (in various topics) 134 times (See Figure 1) and negative/critical 106 times (See Figure 2). It is important to note however that as many as 67 out of the 106 negative comments related to the low value of the badges.
Figure 2 depicts information about positive topics included in students’ comments. 50 students liked the structure and focus that the badge system provided. Twenty-eight students found badges motivating and 24 valued feedback they received in the process. A number of students found the whole process enjoyable, rewarding and fun (See Figure 2). Figure 3 indicates the negative opinions. The most frequent topic of all was repeated 67 times as was related to the value of badges (See Figure 3). Figure 4 shows some comments made by students in the free comment box provided on the survey (See Figure 4).
Figure 2. Frequency of positive comment grouped by topic
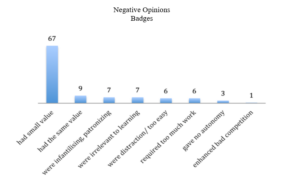
Figure 3. Frequency of negative comment grouped by topic
Figure 4. Comments written by students
In summary, the majority of the students liked the way Digital Badges were used in the teaching of Psychiatry, however both groups (those that liked and those that dislike badges) criticized them for their low value of the overall assessment.
IV. DISCUSSION
Students met digital Badges piloted in the teaching of Psychiatry to Medical Students of our university originally with apprehension. The majority of the students had never heard of digital badges and have never earned a digital badge before this module. However, data from the study looking at students’ perception of the use of digital badges in medical education provided encouraging results.
A. Sense of Reward
Students found badges rewarding yet complained about the small value of the badges. This reflected our design intention in which we wanted to support and engage students rather than focus on extrinsic motivating factors such as sense of reward.
As mentioned above the badge was awarded for completion of weekly tasks, and the acquisition of a badge was functioning more as a method of feedback to students rather than for grading. However, a number of students complained about this, and reported a sense of frustration and a lack of motivation to try harder when the assessment value of the badge was so low.
Nevertheless, our design was supported by other studies. One such study concluded that achievement of badges could influence students’ behaviour even if they do not interfere with grading (Hakulinen & Auvinen, 2014). It seems that competitiveness was triggered in those who wanted to do better anyway.
We were pleased to see learners’ comments about reduced stress during the module. We wanted our award system to potentiate a sense of safety around assessment, giving participants freedom to learn from their mistakes without influencing their final grade. This is a well-recognized principle in gamification as a facilitator of students’ engagement (De Byl & Hooper, 2013).
In addition, our design was guided by the fact that the best use of badges was linked with the recognition of already occurred learning, therefore more viewed as an assessment tool, providing feedback and possibly self-reflection (Reid et al., 2015).
B. Impact on Structure, Assessment and Feedback
We were pleased to note that students in our study felt that digital badges provided direction and structure to their learning. This was also reflected in their comments: students mentioned how badges impacted on their study structure, helping them to focus attention on important aspects of the seminars. These findings are consistent with a study that reported that students who enjoyed badges, found them helpful in giving them the direction they needed to work in (Abramovich et al., 2013). These students also praised the alignment between badge topics and course content (Abramovich et al., 2013).
We were also hoping that badges designed, as part of an assessment that generates formative feedback would help students know if they are progressing enough to meet the requirements of their class (HASTAC n.d.). Based on responses to items 24, 18 and 19 it appeared that students benefited somewhat from the potential guidance and feedback provided by the digital badges system.
It is important to remember that students were asked about the badges at their review seminar and few days prior to their exams. This timing could have influenced their answers. For example, students’ opinion was divided on the statement that earning a badge gave them a sense that they have mastered the course content. Similarly, opinion was divided on whether badges increased students’ confidence that they could demonstrate their knowledge, nevertheless more students felt that they had an impact. It would be interesting to see if students’ responses had been different after their exams. We know gamification has already been described as a powerful strategy that can help achieve learning objectives by affecting the way students behave (Huang & Soman, 2013).
C. Impact on Motivation and Engagement
In our study, a majority of students responded that they worked harder in this module compared to non-gamified modules. Similarly, about 30% more students stated that they were more motivated to work harder through the module because they were earning digital badges. Interestingly when they were given space to provide free comment, many have noted that they did feel more motivated, and a few felt more engaged. Previous studies also reported that students were more likely to engage in the game-like tasks providing rapid feedback (Thamvichai & Supanakorn-Davila, 2012). In other publications students also considered gamified courses to be more motivating, interesting and easier to learn as compared to other courses (Barata et al., 2013), (Dicheva et al., 2015), (Hakulinen & Auvinen, 2014). It is suggested that badges are most valued by learners who are extrinsically motivated and value external validation (Foli et al., 2016).
D. Impact on Outcomes
We did not compare outcomes in overall performance in assessment between students before and after implementation of badges. Having considered this, we decided against it. We felt there were too many variables influencing students’ performance and it would be difficult to definitely attribute potential change to the implementation of digital badges.
E. View of Badges and Learner Type
The impact of an educational tool could also depend on characteristics of the student as a learner. It is reported that students with high expectation for learning and those that value their learning tasks may view the badge as validating if designed as a performance assessment (having impact on intrinsic motivation), but it may devalue their learning if it was viewed as an external reward (Reid et al., 2015). On the other hand, badges used as an assessment model can have a negative impact on students with low expectancy values (Reid et al., 2015). Another study concluded that engagement in the gamified classroom was dependent on students’ playfulness (De Byl & Hooper, 2013). In this study, we have not addressed the learner types and other such specifications of the individuals in our group of students.
In a systematic review of digital badges in health care education, it is mentioned that digital badges represent an innovative approach to learning and assessment and evidence in further education literature demonstrates that their use increases knowledge, retention and motivation to learn. However, they also report a lack of empirical research investigating digital badges within the health care education context (Noyes et al., 2020).
F. Limitations
Our study is limited by the lack of demographic data from all participants. This reduces the potential for comparison between genders and undergraduate vs postgraduate students. As mentioned above, we have not addressed learner characteristics and types (intrinsic versus extrinsic motivation, playfulness). The timing of the data collection (students completed questionnaires before their exams, rather than after) may also be limiting factors. It is also important to remember that this study allowed only for assessment of subjective impact (via students’ opinions and experience) of the badges on students learning and did not perform objective measures of students’ overall performance.
V. CONCLUSION
This study was performed at the start of the implementation of the digital badges in the module and at the time, it was the only module with elements of gamification throughout the whole undergraduate medical curriculum in our university. Like most changes in the assessment process, the students greeted this with a level of apprehension. It would be interesting to see if students’ opinion has evolved after a few years of digital badges being integrated in the module and when other modules are using them. Nevertheless, our data shows that our group of students felt, that they benefited from the learning structure provided by the digital badges. The online process of obtaining the badges enabled tutors to provide timely feedback and monitor students’ progress. In addition, our findings are in keeping with the literature in that engagement and motivation have been facilitated by introducing the digital badges and as such, they indicate that the use of digital badges is a promising tool in education.
The use of digital badges in Medical Education is only starting and would benefit from more research in its judicious integration in higher education curriculum as appropriate.
Notes on Contributors
Dr Edyta Truszkowska did the literature search, collected and analysed the data and gave feedback on methodology and questionaire developed and wrote paper.
Dr Yvonne Emmett designed the methodology and developed questionaire. She gave feedback on the data analysis and edited the writing of the paper.
Prof Allys Guerandel suggested the implementation of digital badges and research project. She gave feedback on data analysis and wrting of paper making revisions to same.
All three authors have read and approved the final manuscript.
Ethical Approval
Our project has been exempted by ethics committee of our institution Human Research Ethics Committee – Sciences (Exemption number LS-E-17-56).
Data Availability
Data is available on reasonable request and data is shared in the institution.
Acknowledgement
We would like to acknowledge our institution psychiatry teaching team for their support in the implementation of the digital badges.
Funding
There are no sources of funding.
Declaration of Interest
There is no conflict of interest for any of the authors.
References
Abramovich, S. (2016). Understanding digital badges in higher education through assessment. On the Horizon, 24(1), 126-131. https://doi.org/10.1108/OTH-08-2015-0044
Abramovich, S., Schunn, C., & Higashi, R. M. (2013). Are badges useful in education? It depends upon the type of badge and expertise of learner. Educational Technology Research and Development, 61(2), 217-232. https://doi.org/10.1007/s11423-013-9289-2
Armour-Thomas, E., & Gordon, E. (2013). Toward an Understanding of Assessment as a Dynamic Component of Pedagogy. https://www.ets.org/Media/Research/pdf/armour_thomas_gordon_understanding_assessment.pdf
Barata, G., Gama, S., Jorge, J., & Gonçalves, D. (2013, September). Engaging engineering students with gamification. In 2013 5th International Conference on Games and Virtual Worlds for Serious Applications IEEE, UK (VS-GAMES) (pp. 1-8). https://doi.org/10.1109/VS-GAMES.2013.6624228
De Byl, P., & Hooper, J. (2013). Key attributes of engagement in a gamified learning environment. In ASCILITE-Australian Society for Computers in Learning in Tertiary Education Annual Conference, Australia (221-230). https://www.learntechlib.org/p/171232/
Deterding, S., Dixon, D., Khaled, R., & Nacke, L. (2011, September). From game design elements to gamefulness: defining” gamification”. In Proceedings of the 15th international academic MindTrek conference: Envisioning future media environments (pp. 9-15). https://doi.org/10.1145/2181037.2181040
Dicheva, D., Dichev, C., Agre, G., & Angelova, G. (2015). Gamification in education: A systematic mapping study. Journal of Educational Technology & Society, 18(3), 75-88. https://www.jstor.org/stable/jeductechsoci.18.3.75
Dowling-Hetherington, L., & Glowatz, M. (2017). The usefulness of digital badges in higher education: Exploring the student perspectives. Irish Journal of Academic Practice, 6(1), 1-28. https://researchrepository.ucd.ie/handle/10197/9691
Foli, K. J., Karagory, P., & Kirby, K. (2016). An exploratory study of undergraduate nursing students’ perceptions of digital badges. Journal of Nursing Education, 55(11), 640-644. https://doi.org/10.3928/01484834-20161011-06
Hakulinen, L., & Auvinen, T. (2014, April). The effect of gamification on students with different achievement goal orientations. In 2014 international conference on teaching and learning in computing and engineering, Malaysia (pp. 9-16). IEEE. https://doi.org/10.1109/LaTiCE.2014.10
HASTAC. (n.d.). Digital Badges. http://www.hastac.org/digital-badges
Hensiek, S., DeKorver, B. K., Harwood, C. J., Fish, J., O’Shea, K., & Towns, M. (2017). Digital badges in science: A novel approach to the assessment of student learning. Journal of College Science Teaching, 46(3), 28. https://www.proquest.com/scholarly-journals/digital-badges-science-novel-approach-assessment/docview/1854234735/se-2
Huang, W. H. Y., & Soman, D. (2013). Gamification of education. Report Series: Behavioural Economics in Action, 29, 11 -12.
Johnson, L. J., & LaMontagne, M. J. (1993). Research methods using content analysis to examine the verbal or written communication of stakeholders within early intervention. Journal of Early Intervention, 17(1), 73-79.
Knapp, T. R. (1990). Treating ordinal scales as interval scales: An attempt to resolve the controversy. Nursing Research, 39(2), 121-123.
Mandernach, B. J. (2015). Assessment of student engagement in higher education: A synthesis of literature and assessment tools. International Journal of Learning, Teaching and Educational Research, 12(2), 1-14.
McGonigal, J. (2011). Reality is broken: Why games make us better and how they can change the world. Penguin.
Norman, G. (2010). Likert scales, levels of measurement and the “laws” of statistics. Advances in health sciences education, 15(5), 625-632.
Noyes, J. A., Welch, P. A., Johnson, J. W., & Carbonneau, K. J. (2020). A systematic review of digital badges in health care education Medical Education, 54(7), 600-615. https://doi.org/10.1111/medu.14060
Przybylski, A. K., Rigby, C. S., & Ryan, R. M. (2010). A motivational model of video game engagement. Review of General Psychology, 14(2), 154. https://doi.org/10.1037/a0019440
Quesenberry, A. C., Hemmeter, M. L., & Ostrosky, M. M. (2011). Addressing challenging behaviors in Head Start: A closer look at program policies and procedures. Topics in Early Childhood Special Education, 30(4), 209-220. https://doi.org/10.1177/0271121410371985
Reid, A. J., Paster, D., & Abramovich, S. (2015). Digital Badges in undergraduate composition courses: effects on intrinsic motivation. Journal of Computers in Education, 2(4), 377-98. https://doi.org/10.1007/s40692-015-0042-1
Rolfe, I., & McPherson, J. (1995). Formative assessment: How am I doing? The Lancet, 345(8953), 837-839. https://doi.org/10.1016/S0140-6736(95)92968-1
Seaborn, K., & Fels, D. I. (2015). Gamification in theory and action: A survey. International Journal of Human Computer Studies, 1(74), 14-31. https://doi.org/10.1016/j.ijhcs.2014.09.006
Sullivan, G. M., & Artino, A. R. (2013). Analyzing and interpreting data from likert-type scales. Journal of Graduate Medical Education, 5(4), 541-542 https://doi.org/10.4300/JGME-5-4-18
Sundler, A. J., Lindberg, E., Nilssonn, C., & Palmer, L. (2019). Qualitative thematic analysis based on descriptive phenomenology. Nursing Open, 6(3), 733-739. https://doi.org/10.1002/nop2.275
Thamvichai, R., & Supanakorn-Davila, S. (2012). A pilot study: Motivating students to engage in programming using game-like instruction. Proceedings of Active Learning in Engineering Education. St Cloud University. https://nms.asee.org/wp-content/uploads/sites/47/2020/02/St_Cloud_2012_Conference_Proceedings.pdf#page=18
UCD Teaching and learning. (2017). UCD digital/open badges pilot 2016/2017. Implementation and evaluation report. UCD Teaching and Learning, 1-23. https://www.ucd.ie/t4cms/UCD%20Digital%20Badges%20Pilot%20Report.pdf
Yildirim, S., Kaban, A., Yildirim, G., & Celik, E. (2016). The effect of digital badges specialization level of the subject on the achievement, satisfaction and motivation levels of the students. Turkish Online Journal of Educational Technology- TOJET, 15(3), 169-182. https://eric.ed.gov/?id=EJ1106420
*Allys Guerandel
University College Dublin,
School of Medicine and Medical Sciences,
Belfield, Dublin 4, Ireland D04V1W8.
00353868590063
Email: allys.guerandel@ucd.ie
Submitted: 1 August 2022
Accepted: 1 November 2022
Published online: 4 April, TAPS 2023, 8(2), 36-46
https://doi.org/10.29060/TAPS.2023-8-2/OA2855
Marina C. Jenkins1, Caroline R. Paul2, Shobhina Chheda1 & Janice L. Hanson3
1School of Medicine and Public Health, University of Wisconsin-Madison, United States; 2Langone Health, Grossman School of Medicine, New York University, United States; 3School of Medicine, Washington University in St. Louis, United States
Abstract
Introduction: Increases in vaccine hesitancy continue to threaten the landscape of public health. Literature provides recommendations for vaccine communication and highlights the importance of patient trust, yet few studies have examined medical student perspectives on vaccine hesitancy in clinical settings. Therefore, we aimed to explore medical student experiences encountering vaccine hesitancy, mistrust, and personal biases, with the goal of informing medical student education.
Methods: A health disparities course including simulated clinical scenarios required students to complete a written reflection. We sorted reflections written in 2014-2016 to identify common topics and used inductive thematic analysis to identify themes relevant to vaccine hesitancy by group consensus.
Results: Our sample included 84 de-identified essays sorted into three non-exclusive topics: vaccine hesitancy (n=42), mistrust (n=34), and personal bias (n=39). We identified four themes within medical students’ reflections: 1) Building a Relationship, including emphasis on patient-centred approaches; 2) Preparedness and Need to Prepare for Future Encounters, including highlighting gaps in medical education; 3) Reactions to Encountering Hesitant Patients, including frustration; 4) Insights for Providing Information and Developing a Plan with Hesitant Patients, including approaches to presenting knowledge.
Conclusion: Reflections in the context of simulated encounters and discussion are useful in students identifying their preparedness for vaccine discussion with patients. Student reflections can assist educators in identifying missing educational frameworks for particular scenarios such as vaccine hesitancy. Without a structured framework regarding addressing vaccine hesitancy, students draw upon other skills that may contradict recommended practices.
Keywords: Medical Education, Vaccine Hesitancy, Reflective Writing, Bias, Mistrust
Practice Highlights
- Reflective writing can be a useful tool in medical education toward addressing vaccine hesitancy.
- Medical student reflective writing can be used to demonstrate curricular gaps.
- Medical students expressed feeling unprepared to care for vaccine hesitant patients.
- Without a framework for vaccine communication, students may draw on other inappropriate skills.
I. INTRODUCTION
Increases in vaccine hesitancy and refusal threaten public health (He et al., 2022; Hough-Telford et al., 2016; Kempe et al., 2020; Santibanez et al., 2020), especially with the COVID-19 pandemic introducing a need for quick and widespread uptake of a new vaccine (Hamel et al., 2022; Ognyanova et al., 2022). Patients, especially parents, are increasingly seeking alternative forms of health information, such as online sources that can include misinformation (Broniatowski et al., 2018; Hara & Sanfilippo, 2016; Jenkins & Moreno, 2020; Meleo-Erwin et al., 2017). Patient trust in their clinician and the health care system delivering the vaccine strongly influence vaccination decisions (Goldenberg, 2016; Kennedy et al., 2011; Larson, 2016). Trust remains the most important barrier to acceptance and uptake of the COVID-19 vaccine, with mistrust of government, medicine, and science presenting major barriers to vaccine uptake (Ognyanova et al., 2022). Vaccine hesitant patients may bring preconceptions and concerns from their own research to in-clinic vaccine communication. Thus, it is important for clinicians to be well-prepared to work with vaccine-hesitant patients and parents.
Existing recommendations for clinicians encountering vaccine hesitancy emphasise centring patient views and voice instead of a medical, academic perspective (Holt et al., 2016; Koski et al., 2019). Approaches including motivational interviewing, presumptive language around vaccine recommendations, and persistent vaccine reminders without pressuring or dismissing patients have been shown to be effective in addressing vaccine hesitancy in medical practice (Dempsey et al., 2018; Gagneur et al., 2018; Hofstetter et al., 2017), while correcting misinformation and offering evidence to patients have been found to be counterproductive (Holt et al., 2016; Koski et al., 2019). These pre-COVID recommendations remain the same for addressing COVID-19 vaccine hesitancy, and lack of physician preparedness for encountering these patients is still an important issue (Centres for Disease Control and Prevention, 2021). Physicians may have misconceptions about patients’ reasons for vaccine hesitancy, often assuming lack of understanding or information on the safety, effectiveness, and necessity of vaccines (Hough-Telford et al., 2016), rather than recognising the more central roles of trust and validation of concerns. If physicians do not learn approaches for centring patient voices in vaccine communication, these pre-conceived biases may present a barrier to vaccine uptake and patient-physician trust.
While valuable recommendations for addressing vaccine hesitancy in the clinical setting exist, current efforts center around informing practicing clinicians on these approaches and providing more educational resources to patients (Centres for Disease Control and Prevention, 2021). These may not represent a sufficient, long-term solution. Furthermore, resources available for healthcare workers may be inaccessible or overwhelming for physicians independently seeking tools (Karras et al., 2019). Incorporating vaccine hesitancy-centred curriculum into medical education may be the optimal, long-term solution to the lack of physician preparedness for these encounters, especially in the face of future pandemics and introduction of new vaccines. With curriculum renewal efforts incorporating early clinical experiences, students could encounter patients for whom vaccines are recommended, including vaccine hesitant patients, early in medical school. It would provide a better educational experience for students and a better health care experience for patients if students receive education to prepare them for these conversations. However, few studies have examined medical student perspectives on vaccine hesitancy in the clinical setting. Existing studies have found mixed findings around medical students’ reflections on their preparedness for encountering vaccine hesitant patients and highlight the need for expansion of related curriculum in medical education (Brown et al., 2017; Kernéis et al., 2017). While COVID vaccine hesitancy literature lacks exploration of medical student perspectives and preparedness, recent studies have highlighted an additional barrier of vaccine hesitancy among medical students in some settings (Lucia et al., 2021). These findings provide additional motivation for including vaccine hesitancy-specific curriculum in medical education.
Understanding medical students’ reactions to vaccine hesitancy is critical in preparing students to address vaccine hesitancy while maintaining patient trust. In the present study, which used a scholarship-of-teaching approach, we aimed to expand on existing research on medical student preparedness for encountering vaccine hesitancy to examine written reflections on mistrust and personal bias in clinical encounters more broadly and use a larger sample of student narratives. We analysed students’ structured reflections regarding assigned reading, simulated patient encounters, peer discussions, and faculty-facilitated discussions to evaluate medical students’ learning during a health disparities curriculum. Structured reflection on simulated encounters has been shown to be a useful tool for understanding student perspectives (Koski et al., 2018); this approach can inform development of medical curriculum for addressing vaccine hesitancy and may be a useful teaching tool as well for students to practice, discuss, and reflect on their own biases in an educational setting. Therefore, the purpose of this study was to explore medical student reflections on encountering vaccine hesitancy, patient mistrust, and personal biases, with the goal of informing medical student education.
II. METHODS
In this qualitative study, we analysed written reflections from a third-year medical student Skills to Impact Health Disparities course, to evaluate their learning about interacting with vaccine-hesitant patients and parents. This study was determined to be exempt by the relevant institutional review boards, including a waiver of informed consent.
From 2006-2018, a medical school at a U.S., Midwestern university required a one-day core session with the goal of developing learner skills to impact health disparities. Small groups of approximately six students went through five to six standardized patient scenarios, each designed to generate discussion and reflection about clinician bias that can unintentionally influence patient care. During the learning activity, each student spent 3-5 minutes interacting with a standardized patient who presented a challenge designed to provoke a level of discomfort in the learners to allow for discussion and reflection. One of these six scenarios included a parent with a history of vaccine refusal for their child expressing concerns about a recommended vaccine.
Following each case, students engaged in a 15-minute, non-facilitated discussion based on a list of focused questions. After all cases, students joined another group of six students for a 75-minute faculty-facilitated debrief. In addition, students were required to complete a brief critical reflection based on a theme of the core day activity using the LeAP framework (Aronson et al., 2012). This framework is modelled on a clinical framework, the SOAP note (Chief complaint, Subjective, Objective, Assessment, and Plan). Students were asked to consider a specific experience that led to concern or questions; describe the experience as fully as possible; reconsider the experience by getting other perspectives; synthesize learning; and make a plan to address future similar challenges. Students could choose to reflect on simulated or real clinical experiences.
Written reflective essays were available for analysis from years 2014-2016, providing qualitative data about students’ observations and experiences with health disparities and health equity. All available essays (n=292) from 2014, 2015, and 2016 that were submitted as a course requirement for the Skills to Impact Health Disparities Core Day required course were de-identified and organized by year.
To ascertain the topics that the students addressed, three investigators (two involved in this study and one from another study using the larger set of all essays) read all essays. Each investigator then designated each essay to a topic from a jointly-developed list of non-exclusive topics derived from the data. After individually assigning topics for a sample of essays, the investigators met to compare their sorting and reconcile any differences before they went on to sort through another set of essays. This process continued until all essays were assigned to one or more topics. Most topic labels matched topics of the simulated scenarios that the students encountered in the course, while others related to broader issues highlighted across scenarios. With the goal of selecting reflections relevant to the issue of vaccine hesitancy, all reflections designated under the topics of vaccine hesitancy, mistrust, and personal bias were gathered for qualitative data analysis. Literature review and initial reading of essays suggested essays on encountering mistrust and bias relate to students’ experiences when encountering vaccine hesitant patients, despite not all essays relating directly to vaccine hesitancy. Each essay was assigned an identifier with cohort year and an essay number. Individual essays were excluded based on group consensus on lack of relevance to vaccine hesitancy.
Inductive thematic analysis was used to identify codes and themes in the reflection data using a semantic, realist approach to identify explicit reactions from students grounded in clinical experiences to identify themes that could be directly applied to clinical practice (Braun & Clarke, 2006). Four investigators, including two involved in topic assignment (CRP, SC) and two additional investigators (MCJ, JLH), read and discussed six essays to develop a preliminary codebook, applied these codes to the same six essays, then met to discuss and revise the codebook. Subsequently, investigators coded the remaining essays in pairs using the revised codebook through four rounds of coding, making further iterative changes to the codebook and reconciling differences within pairs. The full team then met to discuss the coding, revise code descriptions, refine the grouping of the codes, and agree on descriptions of the groups. Any changes made to the codebook during the analysis process were retrospectively updated in all previous coding, so that all coding data reflected the final version of the codebook. Data were organized with qualitative analysis software (HyperResearch version 4.5.4). After all data were coded, investigators discussed and reached consensus on the themes.
III. RESULTS
A total of 90 reflections were collected from the Skills to Impact Health Disparities course across three cohorts of third-year medical students from 2014-2016 at one U.S., Midwestern university. Based on investigator consensus on lack of content relevance, six reflections were excluded from our study sample. Our final study sample included 84 de-identified reflections across three, non-exclusive topics: 42 categorized as relating to vaccine hesitancy, 34 as mistrust, and 39 as personal bias. We identified four major themes in medical students’ reflections on encountering vaccine hesitancy, mistrust and personal bias: 1) Building a Relationship, 2) Preparedness and Need to Prepare for Future Encounters, 3) Reactions to Encountering Hesitant Patients, and 4) Insights for Providing Information and Developing a Plan with Hesitant Patients. Representative quotes for each theme can be found in Table 1. Supplemental Table 1 lists each theme with the codes that informed the theme.
A. Building a Relationship
In our first theme, medical students recognized the importance of Building a Relationship with hesitant parents or patients as the foundation for discussions about vaccines or other care about which patients expressed hesitance. They focused on approaches such as building rapport, centring the parent/patient’s views during the discussion, acknowledging their efforts to gather information about their health decisions, expressing empathy, and avoiding direct confrontation of the patient’s viewpoint during the discussion. Many of these observations occurred during the core day experience. For example, one student wrote:
“I learned the importance of letting the patient try to teach the doctor what they know rather than the doctor jumping in and lecturing to the patient. In the future I will try to talk less and let the patient explain more about why they oppose vaccinations to better gauge what they understand about the literature before I try to explain why vaccinations are important and the facts about vaccinations.”
[Year3_61]
The students saw the importance of finding points of commonality between their perspectives and those of the patient and moving the conversation toward establishing goals that they could work together with the patient to accomplish.
One student described, “I learned that a big part of approaching this difficult conversation is establishing the correct approach: common goal, shared decision making.”
[Year3_65]
B. Preparedness and Need to Prepare for Future Encounters
Another major theme identified in medical student reflections on encountering hesitant patients was Preparedness and Need to Prepare for Future Encounters. This theme included discussion of whether the student expressed feeling ready for the encounter or whether they thought it was successful, as well as specific plans for preparing for similar encounters in the future. One way that students discussed their own feelings of preparedness was by recognizing their own biases upon reflection of the encounter. For example, one student wrote:
“I realized my own prejudices influenced my care of my patients more than I would have liked. … It was an eye opener that I am not as impartial as I would like to be and that it takes a lot more self-reflection and awareness to be the best care provider I can be.
[Year3_16]
When discussing a need to prepare for future encounters, many students referenced plans to independently seek additional resources, especially those referenced by patients in encounters.
Other students mentioned plans to practice patient interactions related to the reflection encounter; including, “For me, practicing acknowledging a patient’s views and concerns without endorsing or validating false information is paramount.”
[Year1_07]
Some students also referenced plans to request feedback or advice from more senior clinicians. Additionally, several students identified gaps in their medical school curriculum that contributed to their lack of preparedness or that needed to be filled to support future preparedness. Students specifically referred to needing more resources, support, and training for encountering hesitant patients. They sometimes called for system-wide changes to address this gap in knowledge.
C. Reactions to Encountering Hesitant Patients
One of the themes identified in the students’ self-reflection was related to their own and others’ Reactions to Encountering Hesitant Patients. While some students expressed frustration with patients/parents who expressed hesitance about vaccines, they acknowledged that they can be passionate about the topic of vaccines in their patient care, but ultimately, patients and parents make their own decisions.
One student shared, “I have always found it quite distressing when an otherwise healthy child goes unvaccinated, given the enormous amount of evidence in favour of vaccination efficacy and its effect on public health.”
[Year2_86]
Another student shared, “I knew I could not force the patient, and I knew that she ultimately was in control of what she would do.”
[Year3_78]
In some reflections patient and parents were labelled, for example, as “anti-vaxxers.” Some reflections described parents’ and patients’ bias towards the physician or clear messaging of a desire for a different doctor. In encountering standardized patients in our scenarios or in reflecting on patients seen in clinical settings, students acknowledged that these conversations were difficult, and they were able to self-assess their level of comfort with conversations.
This was well-summarized in one reflection: “It was remarkable to me how such a strong reaction from this patient’s mother elicited an equally strong reaction in me.”
[Year2_34]
At times students recognized a point where these difficult conversations could reach a dead end. One student stated, “No matter how hard I would try, nothing seemed to work.”
[Year2_03]
Especially in this context, students reflected ambivalence towards the patient’s decision. For example:
“I personally feel that providers allowing for healthy children on their patient panels to remain unvaccinated indirectly reinforces non-vaccination as being acceptable by the medical establishment. That said, I also see and appreciate that turning a child away from one’s practice because their parents refuse to vaccinate them not only does not solve the problem at hand, but it also leaves a child at a very critical developmental age with no health care at all until an alternative provider can be found. Ultimately, I found attempting to reconcile these seemingly incompatible sides of the issue of dealing with anti-vaccination quite confusing and uncomfortable.”
[Year2_86]
D. Insights for Providing Information and Developing a Plan with Hesitant Patients
A fourth theme centred on students’ insights regarding how to provide information appropriately to patients and how to create a plan with patients who were hesitant regarding the medical recommendations given to them. Medical students suggested a variety of ways to provide information to patients who were hesitant. They noted the importance of contributing relevant facts and evidence, stressing that such information and knowledge in general needed to be presented in an understandable manner.
As one student described, “Finding the appropriate words to use in such conversations with a patient is essential.”
[Year1_44]
Students often wrote that they needed to provide reputable information to inform the patient’s decision-making. Some suggested strategies for how to present information to patients, including the sharing of stories and the use of scary information to convey the level of seriousness of the medical recommendation and advice.
One student referenced storytelling in the literature, “…the use of storytelling, the same method used by the anti-vaccination movement, [can be] a way to counteract the barrage of misinformation regarding vaccines.”
[Year1_90]
Sharing these insights about how to present information, students also moved towards how to develop a plan with their patients with some deliberate suggestions. Some students felt they needed to be persistent in their recommendations for vaccines. Some students explained how intentional discussions on the risks and benefits of their recommendations can help in their negotiation about a care plan with their patients.
One student noted, “This draws along the line of patient autonomy, and as long as we are clear about the risks and benefits with the patient, then ultimately, it’s up to the patient to make the decision about which medications she will take.”
[Year1_52]
|
Medical Students’ Experiences with Vaccine Hesitancy, Mistrust, and Bias |
|
|
Themes |
Exemplar Quotes |
|
Building a relationship |
“I felt it was most important that I listen to his story as much as I possibly could, before I spoke. So I let him talk. I said, ‘tell me your concerns.’” [Year3_18] “My feelings during this situation were somewhat of frustration but more of just desire for the patient to feel as though I was there to care for her child above all else and to come alongside her rather than combat with her.” [Year3_03] “One suggestion that my classmate said was to start out the conversation by validating how they are feeling more and that you understand that they are a good parent rather than jumping into facts about vaccinations which caused the patient to become defensive.” [Year3_61] |
|
Preparedness and need to prepare for future encounters
|
“I need more tools for dealing with these situations in the future.” [Year1_04] “My plan is to educate myself more on the materials available for parents regarding immunizations.” [Year3_03] “Ultimately it would be nice to see EMRs advance to the point where they can track a patient’s problem, not just on a list, but through stages of management and onto completion, with a provider responsible for follow-up.” [Year2_33] “I will seek feedback from my attendings and residents so that I can improve my motivational interviewing skills.” [Year3_81] |
|
Reactions to encounter-ing hesitant patients |
“Ultimately this is a decision of the parent and I can only offer my professional advice…I learned that this topic did elicit some emotion which I was surprised about.” [Year3_79] “I learned that I need to work on my bluntness (what I consider to be honesty), as well as increasing affirmation of patients’ fears, since telling someone they are wrong (in any facet of life) typically doesn’t work out that well.” [Year2_34] “I felt uncomfortable and offended at times during the conversation. The patient clearly was not interested in negotiating vaccination, and when I tried to discuss the validity of some of the studies and articles she had read, she became very defensive.” [Year2_82] “I dealt with a mother who had embraced the anti-vaccination movement. This is an issue that I have thought about a lot but despite my reflections, it is an issue that I do not know how to address well. This filled me with fear because I honestly didn’t know what the best approach was.” [Year1_90] |
|
Insights for providing information and creating a plan with hesitant patients
|
“From the debriefing session I learned that a promising approach for the anti-vaccine population is to continue to offer the vaccines at each well-child check-up without intensive counsel on the risks/benefits of vaccines.” [Year1_13] “I also learned about using pictures to get a visceral response from the parent which hopefully would change their mind about not getting a vaccine.” [Year3_69] “When I encounter this scenario in the future, as I’m sure I will, I will begin by teasing out whether the patient is interested in more information, in which case I can have resources and studies available, or if they have already made up their mind and at that point I need to negotiate the visit to ensure that they continue to see me for whatever care they are willing to receive, even if that doesn’t include all the preventive measures I would like.” [Year2_82] |
Table 1. Medical students’ experiences with vaccine hesitancy, mistrust, and bias—Themes and exemplar quotes
IV. DISCUSSION
In this qualitative study of a curricular activity designed to build medical students’ skills for interacting with patients toward reducing health disparities, we explored medical student reflections on real and simulated patient care encounters related to vaccine hesitancy, mistrust and personal bias, with the overall goal of informing medical student education. This allowed for evaluation of the utility of this curriculum framework, as well as highlighting gaps in medical curriculum around addressing vaccine hesitancy. Our analysis supports that medical student reflections across the areas of vaccine hesitancy, mistrust and personal bias share thematic structure and implications for informing medical curriculum regarding encounters with patients who resist medical advice, as well as recommendations for teaching approaches to communication with patients and parents who express hesitancy about vaccines.
This study highlights the benefits of reflections on simulated clinical encounters in the context of a Skills to Impact Health Disparities course. Reflections in the context of simulated encounters and discussion were successful in encouraging students assess their preparedness for vaccine discussions with patients. Review of written reflections, like those analysed in this study, can assist educators in identifying missing educational frameworks for particular patient care scenarios such as vaccine hesitancy. While efforts are growing to incorporate vaccine hesitancy information into medical curricula, especially now, in response to the COVID-19 pandemic (Kelekar et al., 2022; Onello et al., 2020; Real et al., 2017; Schnaith et al., 2018), there is little focus on recommending or evaluating these efforts on a large scale in the U.S. However, recent efforts to establish innovative curriculum of this kind have shown it to be feasible and effective for improving medical student preparedness in addressing vaccine hesitancy (Kelekar et al., 2022; Onello et al., 2020; Real et al., 2017; Schnaith et al., 2018). The curriculum structure assessed in this study may offer a strong approach to teach students valuable lessons related to vaccine hesitancy and evaluate existing progress in this area.
Findings from this study also highlight gaps in existing medical curriculum for preparing students to encounter hesitant patients. We found that without a structured and deliberate learning framework for addressing vaccine hesitancy, students will draw upon other skills that may not be appropriate and may be counterproductive. Students in this study often expressed feeling unprepared, aligning with prior studies (Brown et al., 2017; Kernéis et al., 2017). However, we found that using a structured framework for reflection encouraged planning future preparation for similar encounters. This included calling for system-wide changes to curriculum and availability of resources. Additionally, discussion with peers and reflection were cited as helping students to feel more prepared for future encounters with hesitant patients.
While discussion with peers as a learning strategy was widely recognized as helpful, outcomes of these discussions varied greatly and were directly related to the student’s overall reflection and plan for future preparation. This sometimes led to misguided solutions, highlighting the need for aligning education and training around similar encounters with evidence-informed recommendations. Many students referenced using an approach of centring patient views, either during the clinical encounter or after peer discussion and reflection, which aligns with recommendations (Centres for Disease Control and Prevention, 2021; Holt et al., 2016; Jarrett et al., 2015; Koski et al., 2019). However, many others referenced using only facts to correct knowledge, which is advised against in the vaccine hesitancy literature (Holt et al., 2016; Koski et al., 2019). In the context of these reflections, there would not be a space for students who came to misguided conclusions about approaching vaccine hesitancy to have this knowledge corrected based on recommended practices. Additional support and curriculum around vaccine hesitancy should be implemented alongside this framework of practice, peer discussion and reflection.
Previous research has shown that written reflections provide an effective tool for students to acknowledge their biases and the potential impact on patient care, as was seen in this study (Ross & Lypson, 2014). Physician biases related to perceptions of patient education, lifestyle, and identity have been documented and found to impact patient care and rapport (Forhan & Salas, 2013; Franz et al., 2021; Verbrugge & Steiner, 1981; Walls et al., 2015). There are concerns of physicians’ dismissal of patients expressing vaccine hesitancy from their care and physicians’ beliefs that patient hesitancy is due to lack of reliable information (Hough-Telford et al., 2016). Physician frustration may contribute to lack of willingness to bridge communication with hesitant patients; this has been seen even at the student-level, in this study and in previous research (Koski et al., 2018). Preparing students for these types of encounters by promoting reflection on frustrations and biases is important for addressing vaccine hesitancy.
Limitations of this study include that data were collected from a single institution. However, detailed, written reflections allowed for in-depth thematic analysis that may transfer to medical students more broadly. Additionally, reflections were from a course required for all medical students at the institution from cohorts over three years. Students’ reflections were written in 2014-2016, prior to the COVID-19 pandemic. However, vaccine hesitancy is an even more relevant topic now and reasons for vaccine hesitancy as well as strategies for addressing it are largely unchanged (Centres for Disease Control and Prevention, 2021). Indeed, vaccine hesitancy to the COVID-19 vaccine highlights the need for deliberate curricular efforts. Another limitation is that our sample only includes students who chose to discuss vaccine hesitancy, mistrust and bias in their reflections. However, this allowed us to analyse a fairly large sample of student reflections for a qualitative study, aiding in robust thematic saturation and providing insights that are relevant beyond vaccine hesitancy cases.
V. CONCLUSION
There are several meaningful implications of this study for medical education. Our findings illustrate benefits of learner reflection to build insights about communicating and building relationships to address vaccine hesitancy in medical education. Students found encounters with vaccine hesitant patients challenging, in part due to lack of preparedness, highlighting a gap in curriculum. Findings demonstrate varied familiarity with existing recommendations for addressing vaccine hesitancy, emphasizing the need to incorporate specific training into medical curriculum regarding specific skills gaps such as with communication. By focusing on mistrust and personal bias beyond vaccine hesitancy-specific cases, medical curriculum can better prepare students to approach these underlying issues with vaccine hesitant patients and patients expressing hesitancy to other medical recommendations in their future clinical practice. Finally, comprehensive efforts to improve vaccine hesitancy preparedness amongst learners are needed in our current climate of medical mistrust, given the prominence of vaccine hesitancy not just in paediatrics but also throughout clinical care in the context of the current COVID-19 pandemic. To improve vaccine confidence and decrease mistrust in the physician-patient relationship, medical educators must address medical student preparedness for encounters with vaccine-hesitant patients and parents through intentional learning strategies incorporated into medical school curriculum. We recommend that medical schools explore incorporating simulated patient encounters or role-play scenarios with structured reflection and discussion activities in response to encounters with hesitant patients, alongside didactic curriculum on evidence-based vaccine communication strategies, as research continues to evaluate best practices for preparing medical students to encounter vaccine hesitancy.
Notes on Contributors
Marina C. Jenkins BA was involved in the conceptual development of this qualitative analysis; analysis of reflective writings for development of themes; writing of introduction, results, methods and discussion and editing all sections and final approval of the manuscript.
Caroline R. Paul MD was involved in the original curriculum, the original sorting process of student reflective writing; the conceptual development of this qualitative analysis; analysis of reflective writings for development of themes; writing of results section and editing of all sections and final approval of the manuscript.
Shobhina Chheda MD MPH was involved in the original curriculum, the original sorting process of student reflective writing; analysis of reflective writings for development of themes; writing of results section and editing of all sections and final approval of the manuscript.
Janice L. Hanson PhD EdS MH was lead in the conceptual development of this qualitative analysis and organization of qualitative data; analysis of reflective writing; writing of results; writing of methods; and primary mentor to first author on writing of introduction and discussion; editing of all sections and final approval.
Ethical Approval
This study received exemption status from the Institutional Review Boards from the University of Wisconsin-Madison and the Washington University in St. Louis.
Data Availability
We do not have IRB permission to share our data in a data repository. The data are essays written by medical students during a required university course. While the essays are de-identified, it could be possible for someone who wrote an essay or participated in discussion groups with those who wrote the essays to identify an individual who wrote an essay.
Acknowledgement
We would like to acknowledge Andrea Maser, MS for her assistance in de-identifying student reflections and organization of student reflections from various student cohorts.
We would like to acknowledge Roberta Rusch, MPH for assistance in the original sorting of student reflections.
Funding
There is no funding source for this study.
Declaration of Interest
The authors have no conflicts of interest to disclose.
References
Aronson, L., Kruidering, M., Niehaus, B., & O’Sullivan, P. (2012). UCSF LEaP (Learning from your experiences as a professional): guidelines for critical reflection. MedEdPORTAL, 8, 9073. https://doi.org/10.15766/mep_2374-8265.9073
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
Broniatowski, D. A., Jamison, A. M., Qi, S. H., AlKulaib, L., Chen, T., Benton, A., Quinn, S. C., & Dredze, M. (2018). Weaponized health communication: Twitter bots and russian trolls amplify the vaccine debate. American Journal of Public Health, 108(10), 1378-1384. https://doi.org/10.2105/ajph.2018.304567
Brown, A. E. C., Suryadevara, M., Welch, T. R., & Botash, A. S. (2017). “Being persistent without being pushy”: Student reflections on vaccine hesitancy. Narrative Inquiry in Bioethics, 7(1), 59-70. https://doi.org/10.1353/nib.2017.0018
Centres for Disease Control and Prevention. (2021). COVID-19 vaccination field guide: 12 strategies for your community. United States Department of Health and Human Services. https://www.cdc.gov/vaccines/covid-19/downloads/vaccination-strategies.pdf.
Dempsey, A. F., Pyrznawoski, J., Lockhart, S., Barnard, J., Campagna, E. J., Garrett, K., Fisher, A., Dickinson, L. M., & O’Leary, S. T. (2018). Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination: A cluster randomized clinical trial. JAMA Pediatrics, 172(5), e180016. https://doi.org/10.1001/jamapediatrics.2018.0016
Forhan, M., & Salas, X. R. (2013). Inequities in healthcare: A review of bias and discrimination in obesity treatment. Canadian Journal of Diabetes, 37(3), 205-209. https://doi.org/10.1016/j.jcjd.2013.03.362
Franz, B., Dhanani, L. Y., & Miller, W. C. (2021). Rural-urban differences in physician bias toward patients with opioid use disorder. Psychiatric services, 72(8), 874-879. https://doi.org/10.1176/appi.ps.202000529
Gagneur, A., Gosselin, V., & Dubé, È. (2018). Motivational interviewing: A promising tool to address vaccine hesitancy. Vaccine, 36(44), 6553-6555. https://doi.org/10.1016/j.vaccine.2017.10.049
Goldenberg, M. J. (2016). Public misunderstanding of science? Reframing the problem of vaccine hesitancy. Perspectives on Science, 24(5), 552-581. https://doi-org/10.1162/POSC_a_00223
Hamel, L., Sparks, G., Lopes, L., Stokes, M., & Brodie, M. (2022). KFF COVID-19 Vaccine Monitor: January 2022 Parents And Kids Update. K. F. Foundation. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-january-2022-parents-and-kids-update/
Hara, N., & Sanfilippo, M. R. (2016). Co-constructing controversy: Content analysis of collaborative knowledge negotiation in online communities. Information Communication & Society, 19(11), 1587-1604. https://doi.org/10.1080/1369118x.2016.1142595
He, K., Mack, W. J., Neely, M., Lewis, L., & Anand, V. (2022). Parental perspectives on immunizations: Impact of the COVID-19 pandemic on childhood vaccine hesitancy. Journal of Community Health, 47(1), 39-52. https://doi.org/10.1007/s10900-021-01017-9
Hofstetter, A. M., Robinson, J. D., Lepere, K., Cunningham, M., Etsekson, N., & Opel, D. J. (2017). Clinician-parent discussions about influenza vaccination of children and their association with vaccine acceptance. Vaccine, 35(20), 2709-2715. https://doi.org/10.1016/j.vaccine.2017.03.077
Holt, D., Bouder, F., Elemuwa, C., Gaedicke, G., Khamesipour, A., Kisler, B., Kochhar, S., Kutalek, R., Maurer, W., Obermeier, P., & Seeber, L. (2016). The importance of the patient voice in vaccination and vaccine safety—Are we listening? Clinical Microbiology and Infection, 22, S146-S153. https://doi.org/10.1016/j.cmi.2016.09.027
Hough-Telford, C., Kimberlin, D. W., Aban, I., Hitchcock, W. P., Almquist, J., Kratz, R., & O’Connor, K. G. (2016). Vaccine delays, refusals, and patient dismissals: A survey of pediatricians. Pediatrics, 138(3), 9, Article e20162127.https://doi.org/10.1542/peds.2016-2127
Jarrett, C., Wilson, R., O’Leary, M., Eckersberger, E., & Larson, H. J. (2015). Strategies for addressing vaccine hesitancy–A systematic review. Vaccine, 33(34), 4180-4190. https://doi.org/10.1016/j.vaccine.2015.04.040
Jenkins, M. C., & Moreno, M. A. (2020). Vaccination discussion among parents on social media: A content analysis of comments on parenting blogs. Journal of Health Communication, 25(3), 232-242. https://doi.org/10.1080/10810730.2020.1737761
Karras, J., Dubé, E., Danchin, M., Kaufman, J., & Seale, H. (2019). A scoping review examining the availability of dialogue-based resources to support healthcare providers engagement with vaccine hesitant individuals. Vaccine, 37(44), 6594-6600. https://doi.org/10.1016/j.vaccine.2019.09.039
Kelekar, A., Rubino, I., Kavanagh, M., Lewis-Bedz, R., LeClerc, G., Pedell, L., & Afonso, N. (2022). Vaccine hesitancy counseling—an educational intervention to teach a critical skill to preclinical medical students. Medical Science Educator, 32(1), 141-147. https://doi.org/10.1007/s40670-021-01495-5
Kempe, A., Saville, A. W., Albertin, C., Zimet, G., Breck, A., Helmkamp, L., Vangala, S., Dickinson, L. M., Rand, C., & Humiston, S. (2020). Parental hesitancy about routine childhood and influenza vaccinations: A national survey. Pediatrics, 146(1). https://doi.org/10.1542/peds.2019-3852
Kennedy, A., LaVail, K., Nowak, G., Basket, M., & Landry, S. (2011). Confidence about vaccines in the United States: Understanding parents’ perceptions. Health Affairs, 30(6), 1151-1159. https://doi.org/10.1377/hltaff.2011.0396
Kernéis, S., Jacquet, C., Bannay, A., May, T., Launay, O., Verger, P., Pulcini, C., Abgueguen, P., Ansart, S., Bani-Sadr, F., Bannay, A., Bernard, L., Botelho-Nevers, E., Boutoille, D., Cassir, N., Cazanave, C., Demonchy, E., Epaulard, O., Etienne, M., & Wyplosz, B. (2017). Vaccine education of medical students: A nationwide cross-sectional survey. American Journal of Preventive Medicine, 53(3), e97-e104. https://doi.org/10.1016/j.amepre.2017.01.014
Koski, K., Lehto, J. T., & Hakkarainen, K. (2018). Simulated encounters with vaccine-hesitant parents: Arts-based video scenario and a writing exercise. Journal of Medical Education and Curricular Development, 5, 2382120518790257. https://doi.org/10.1177/2382120518790257
Koski, K., Lehto, J. T., & Hakkarainen, K. (2019). Physician self-disclosure and vaccine-critical parents׳ trust: Preparing medical students for parents׳ difficult questions. Health Professions Education, 5(3), 253-258. https://doi.org/10.1016/j.hpe.2018.09.005
Larson, H. J. (2016). Vaccine trust and the limits of information. Science, 353(6305), 1207-1208. https://doi.org/10.1126/science.aah6190
Lucia, V. C., Kelekar, A., & Afonso, N. M. (2021). COVID-19 vaccine hesitancy among medical students. Journal of Public Health, 43(3), 445-449. https://doi.org/10.1093/pubmed/fdaa230
Meleo-Erwin, Z., Basch, C., MacLean, S. A., Scheibner, C., & Cadorett, V. (2017). “To each his own”: Discussions of vaccine decision-making in top parenting blogs. Human Vaccines & Immunotherapeutics, 13(8), 1895-1901. https://doi.org/10.1080/21645515.2017.1321182
Ognyanova, K., Lazer, D., Baum, M., Perlis, R. H., Druckman, J., Santillana, M., Qu, H., Trujillo, K. L., Safarpour, A., Uslu, A., Quintana, A., Green, J., Pippert, C. H., & Shere, A. (2022). The COVID States Project# 82: COVID-19 vaccine misinformation trends, awareness of expert consensus, and trust in social institutions. Open Science Framework. https://doi.org/10.31219/osf.io/9ua2x
Onello, E., Friedrichsen, S., Krafts, K., Simmons, G., Jr., & Diebel, K. (2020). First year allopathic medical student attitudes about vaccination and vaccine hesitancy. Vaccine, 38(4), 808-814. https://doi.org/10.1016/j.vaccine.2019.10.094
Real, F. J., DeBlasio, D., Beck, A. F., Ollberding, N. J., Davis, D., Cruse, B., Samaan, Z., McLinden, D., & Klein, M. D. (2017). A virtual reality curriculum for pediatric residents decreases rates of influenza vaccine refusal. Academic Pediatrics, 17(4), 431-435. https://doi.org/10.1016/j.acap.2017.01.01
Ross, P. T., & Lypson, M. L. (2014). Using artistic-narrative to stimulate reflection on physician bias. Teaching and Learning in Medicine, 26(4), 344-349. https://doi.org/10.1080/10401334.2014.945032
Santibanez, T. A., Nguyen, K. H., Greby, S. M., Fisher, A., Scanlon, P., Bhatt, A., Srivastav, A., & Singleton, J. A. (2020). Parental vaccine hesitancy and childhood influenza vaccination. Pediatrics, 146(6), Article e2020007609. https://doi.org/10.1542/peds.2020-007609
Schnaith, A. M., Evans, E. M., Vogt, C., Tinsay, A. M., Schmidt, T. E., Tessier, K. M., & Erickson, B. K. (2018). An innovative medical school curriculum to address human papillomavirus vaccine hesitancy. Vaccine, 36(26), 3830-3835. https://doi.org/10.1016/j.vaccine.2018.05.014
Verbrugge, L. M., & Steiner, R. P. (1981). Physician treatment of men and women patients: Sex bias or appropriate care? Medical Care, 19(6), 609-632. https://doi.org/10.1097/00005650-198106000-00005
Walls, M. L., Gonzalez, J., Gladney, T., & Onello, E. (2015). Unconscious biases: Racial microaggressions in American Indian health care. The Journal of the American Board of Family Medicine, 28(2), 231-239. https://doi.org/10.3122/jabfm.2015.02.140194
*Marina C. Jenkins
Department of Paediatrics
University of Wisconsin-Madison
2870 University Ave., Suite 200
Madison, WI 53703
Email address: mcjenkins@wisc.edu
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









