Minor tweaks to tutorial presentation improved students’ perceptions of our mass tutorial
Submitted: 15 August 2022
Accepted: 20 December 2022
Published online: 4 July, TAPS 2023, 8(3), 54-57
https://doi.org/10.29060/TAPS.2023-8-3/SC2867
Seow Chong Lee & Foong May Yeong
Department of Biochemistry, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: In the first weeks of medical school, students learn fundamental cell biology in a series of lectures taught by five lecturers, followed by a mass tutorial session. In this exploratory study, we examined students’ perceptions of the mass tutorial session over two academic years to find out if they viewed the tutorials differently after minor tweaks were introduced.
Methods: Reflective questions were posted to the undergraduate Year 1 Medical students at the end of each mass tutorial session in 2019 and 2020. Content analysis was conducted on students’ anonymous responses, using each response as the unit of analysis. The responses were categorised under the learning objectives, with responses coded under multiple categories where appropriate. The distribution of the counts from responses in 2019 and 2020 was compared, and the tutorial slides used over the two years were reviewed in conjunction with students’ perceptions to identify changes.
Results: In 2019, we collected 122 responses which coded into 127 unique counts, while in 2020, 119 responses coded into 143 unique counts. Compared to 2019, we noted increases in the percentage of counts under “Link concepts” and “Apply knowledge”, with concomitant decreases in percentage of counts in “Recall contents”. We also found that the 2020 tutorial contained additional slides, including a summary slide and lecture slides in their explanations of answers to the tutorial questions.
Conclusion: Minor tweaks in the tutorial presentation could improve students’ perceptions of our mass tutorials.
Keywords: Mass Tutorials, Students’ Reflections, Apply Knowledge, Link Concepts, Minor Tweaks
I. INTRODUCTION
In the first few weeks of medical school, students learn about cell biology which is fundamental to what they need to know about tissues, organs, and the whole body in a series of lectures co-taught by five lecturers. In the lectures, efforts are made to highlight basic cellular processes, and illustrate how these are inter-connected in a cell. Where appropriate, how knowledge in the biomedical sciences underpins applications in clinical settings is also illustrated by the lecturers. At the end of the series of lectures, the lecturers will co-facilitate a mass tutorial session aimed at summing up the topics.
The mass tutorial session has several learning objectives. These include basic levels of learning such as recalling concepts, preparing for assessments, and building knowledge on topics, to higher levels of learning such as applying concepts to solve real life problems, and linking concepts between topics. Being the only teaching and learning activity that all lecturers co-teach, the mass tutorial provides the best opportunity to demonstrate links and apply the consolidated knowledge learnt during the different lectures.
Once the teaching and learning activities are completed, the coordinator of the lectures Foong May Yeong (YFM) reviews the curriculum to ensure that the teaching and learning activities delivered the intended learning objectives. Such reviews include students’ experiences of the curriculum (Erickson et al., 2008), which the coordinator (YFM) routinely collect through posting reflective questions at the end of the tutorial. In this exploratory study, we analysed students’ reflections from 2019 and 2020, and categorised them under different learning objectives of the tutorial. We noted an increase in percentage counts under “Apply knowledge” and “Link concepts” in 2020 compared to 2019. A review of the tutorial slides revealed the addition of summary and lecture slides in 2020. Our results suggest that minor tweaks to the tutorial presentation are sufficient to help students see the intended usefulness and relevance of tutorials.
II. METHODS
A. Format of Mass Tutorials
The mass tutorial was conducted after completion of the cell lectures. For 2019, this was a face-to-face session. For 2020, due to the COVID-19 pandemic, the tutorial was conducted online via Microsoft Teams. The class size was 281 for 2019, and 280 for 2020. Four out of five lecturers taught the same topics for both years. For both years, during the mass tutorial, each lecturer used Poll Everywhere to pose a mix of five to six recall and application questions linked to their topic. Identical questions were used in 2019 and 2020. Students discussed among themselves before answering these questions. The class responses were then revealed, after which the lecturer explained the solutions to their questions. The cycle was repeated until all the lecturers completed their parts.
B. Collection of Student Reflections
After each tutorial, the coordinator (YFM) posted two reflection questions on Poll Everywhere. The two questions were: 1. “What were the key points you learned in this session?”, 2. “Any questions?”. Answering these reflection questions were voluntary and anonymous. A waiver of informed consent was approved by Yong Loo Lin School of Medicine Medical Sciences Departmental Ethics Review Committee. The responses to question 1 obtained from students in 2019 and 2020 were analysed in this study.
C. Content Analysis
The responses to question 1 were coded and categorized into the different learning objectives of the mass tutorial, using each response as a unit of analysis. Each response could be coded into multiple categories when appropriate. The counts under each category were represented as a percentage of all counts coded from the responses. The tutorial slides used in 2019 and 2020 were also reviewed to understand students’ perceptions.
III. RESULTS
In 2019, we collected 122 responses which were coded into 127 unique counts. In 2020, we collected 119 responses which were coded into 143 unique counts. The number of responses and unique counts coded were largely similar between the two years. The unique counts were categorised into the five learning objectives and their percentage counts were presented in Figure 1. Supplemental data containing an overview of the categories and samples of students’ responses, as well as the counts under each category, are openly available in Tables 1 and 2 shared at Figshare at http://doi.org/10.6084/m9.figshare.20484498 (Lee & Yeong, 2022). The distribution of the counts differed between the two years. In 2019, majority of the counts were categorized to “Recall contents” (37.0%), with low numbers categorized as “Apply knowledge” and “Link concepts” (15.0% and 3.1% respectively). In comparison, in 2020, we observed a decrease in percentage of counts in “Recall contents” (to 21.0%), with an increased percentage in counts in “Apply knowledge” and “Link concepts” (to 22.4% and 15.4% respectively). Overall, there is a shift in distribution of counts, from a skewed distribution in 2019, to an even distribution in 2020.
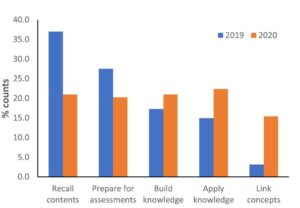
Figure 1. Categorisation of students’ responses into the learning objectives
Given that tutorial questions used in the two years were largely identical, we reviewed the tutorial slides used in these two years to look for possible differences. In 2020, firstly, a summary slide detailing the different aspects of the cell was added to the start of the tutorial slides. Secondly, lecture slides were included in the tutorial slides to explain the answers to the tutorial questions. The lecture slides could come from the lecturer teaching the topic of interest, or from other lecturers if connections across topics were important. These additions could have altered students’ perceptions of the mass tutorial session in 2020.
IV. DISCUSSION
In this study, we examined students’ reflections collected across two academic years to understand their perceptions of the mass tutorial sessions that capped the teaching of cell biology. One of the intentions of the lecturers when designing the tutorial questions was to demonstrate links across topics, and illustrate how questions can be solved using connections across topics. The decrease in percentage of counts under “Recall contents” in 2020 suggested an increase in students’ awareness of the usefulness and relevance of the tutorial sessions when minor changes were made in the presentation of the overview of the cell biology topic and the answers to the tutorial questions.
Both lecture and summary slides likely promoted links in different ways. The lecture slides represent theoretical knowledge for each topic, and also add visuals to the explanations of tutorial questions. Inclusion of lecture slides allow students to use both visual and audio channels to process the explanations, instead of using only the audio channel to listen to explanations when they were delivered verbally without visuals (Mayer, 2014). Using both channels could lower the cognitive load for students to learn and construct meaningful frameworks to solve problems. Summary slides juxtaposed different topics within a slide, allowing students to visualize connections between topics in the proper functioning of a cell (Bae & Watson, 2014). Adding these slides require little effort from the lecturers as the slides are readily available. Such small changes in improving the instructional approach could result in improvements in student learning (Lang, 2016).
There are several limitations to our study. Firstly, we only reviewed the tutorial slides, which covers part of the enacted curriculum. Secondly, the tutorial in 2019 was conducted face-to-face while the one in 2020 was conducted online. Online learning normally is not something students view positively, hence the improvements in student perceptions was surprising. Students prefer the social aspects of learning, which is abundant in face-to-face learning but greatly diminished in online learning (Siah et al., 2022). However, the diminished opportunities for peer-learning in online environment might contribute to increased attention diverted to lecturers for explanations.
V. CONCLUSION
Surveying and analysing students’ reflections at the end of mass tutorial proved to be informative in evaluating and improving our tutorials. In our preliminary analysis, a change in students’ perceptions of the tutorial from recalling of concepts to application of knowledge and linking concepts corresponded to minor tweaks in our tutorial presentation slides. Such minor tweaks, requiring little time, but yet are effective in helping students see the usefulness and relevance of tutorials, is an approach that even busy academics can do.
Notes on Contributors
Seow Chong Lee contributed to the analysis and interpretation of data, drafting and revising of the manuscript.
Foong May Yeong contributed to the conception and design of the study, interpretation of data, drafting and revising of the manuscript.
Ethical Approval
Ethics approval was obtained from Yong Loo Lin School of Medicine Medical Sciences Departmental Ethics Review Committee (Reference code: MSDERC-2022-006).
Data Availability
An overview of the categorization of responses into categories and samples of students’ responses, as well as the counts under each category are openly available in Figshare at https://doi.org/10.6084/m9.figshare.20484498.
Funding
This paper receives no funding from outside sources.
Declaration of Interest
The authors have no conflict of interest to declare.
References
Bae, J., & Watson, B. (2014). Toward a better understanding and application of the principles of visual communication. In W. Huang (Ed.), Handbook of Human Centric Visualization (pp. 179-201). Springer. https://doi.org/10.1007/978-1-4614-7485-2_7
Erickson, F., Bagrodia, R., Gook-Sather, A., Espinoza, M., Jurow, S., Shultz, J. J., & Spencer, J. (2008). Students’ experience of school curriculum: the everyday circumstances of granting and withholding assent to learn. In F. M. Connelly, M. F. He, & J. Phillion. (Eds.), The SAGE Handbook of Curriculum and Instruction (pp. 198-218). https://doi.org/10.4135/9781412976572.n10
Lang, J. M. (2016). Small Teaching: Everyday Lessons from the Science of Learning (1st ed.). Jossey-Bass.
Lee, S. C., & Yeong, F. M. (2022). Minor tweaks to tutorial presentation improved students’ perceptions of our mass tutorial. https://doi.org/10.6084/m9.figshare.20484498
Mayer, R. E. (2014). Multimedia instruction. In M. Spector, D. Merrill, J. Elen, & M. J. Bishop (Eds.), Handbook of Research on Educational Communications and Technology (pp. 385-399). https://doi.org/10.1007/978-1-4614-3185-5_31
Siah, C. R., Huang, C. M., Poon, Y. S. R., & Koh, S. S. (2022). Nursing students’ perceptions of online learning and its impact on knowledge level. Nurse Education Today, 112, Article 105327. https://doi.org/10.1016/j.nedt.2022.105327
*Foong May Yeong
MD4, 5 Science Drive 2,
S117545
+65 6516 8866
Email: bchyfm@nus.edu.sg
Submitted: 28 April 2022
Accepted: 9 February 2023
Published online: 4 July, TAPS 2023, 8(3), 50-53
https://doi.org/10.29060/TAPS.2023-8-3/SC2798
Olivia MY Ngan1,2, Jasmine YN Hui3 & Sihan Sun4
1Medical Ethics and Humanities Unit, School of Clinical Medicine, LKS Faculty of Medicine, The University of Hong Kong, HKSAR; 2Centre for Medical Ethics and Law, Faculty of Law and LKS School of Medicine, The University of Hong Kong; 3Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR; 4CUHK Centre for Bioethics, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR
Abstract
Introduction: Didactic pedagogy and passive learning in bioethics and medical humanities teaching are ineffective in engaging students and gauging learning interests. As a result, medical students are unaware of why and how bioethics and medical humanities relate to their learning and thus prioritising acquiring clinical knowledge in their medical education.
Methods: This project involves a teacher-student collaboration to develop a teaching approach, which bridges historical events and contemporary issues, acknowledging how ethics and humanities are interwoven in clinical and everyday life. The objectives are to (1) highlight landmark historical events in bioethics and medical humanities and (2) recognise the evolving nature of values and social norms that inform current practice.
Results: The three activities include the use of historical narratives, annual newsletter publications, and social media to augment didactic classroom teaching and learning. Video narratives of landmark events in bioethics were developed to strengthen historical knowledge and encourage self-reflection. The newsletter invited students to write about any topic in bioethics and medical humanities and enabled them to experience a peer-review process. It allowed students to critically appraise everyday issues. Social media engagement via Instagram offered a flexible and informal medium to diversify the traditional bioethics content taught in the classroom. The advantages and obstacles of each element are discussed.
Conclusion: A holistic approach using historical narratives, newsletters, and social media engages students’ learning and allows students to become conscious of how past events shape the present.
Keywords: Bioethics, Medical Ethics, Medical Humanities, Education, History, Curriculum Development, Social Media, Student as Partner, Newsletter
I. INTRODUCTION
With modern bioethics taking shape in the late 1960s, the introduction of formal bioethics teaching in medical schools developed slowly in Europe and Northern America over the subsequent decades. It was recognised that professional ability not only encompassed scientific knowledge and clinical skills, but also embodied a high standard of professional ethics, values, and moral conduct. A paradigm shift in how medical education shaped students’ moral compasses and holistic decision-making abilities was needed. In 1987, the Liaison Committee on Medical Education stated that medical schools must incorporate bioethics and medical humanities teaching into their curricula (Carrese et al., 2015). In 1993, the British General Medical Council published a white paper, Tomorrow’s Doctors, which outlined a blueprint for reforming the curriculum and affirmed that teaching ethics and law was an integral part of medical education (Mattick & Bligh, 2006).
Bioethics teaching started relatively late in Asia-Pacific and is strategically less developed in its teaching content, methodology, and assessment (Qian et al., 2018; Sim et al., 2019). There is little discussion on how to best deliver bioethics education through a multidisciplinary lens, as the disciplines of humanities (e.g., philosophy, history, and law), social sciences (e.g., anthropology and sociology), and arts (e.g., literature) are extensive. Our team recognised that passive learning using conventional pedagogy (e.g., didactic lectures and tutorials) had significant drawbacks. Earlier studies showed that teachers adopting these methods struggled to engage and stimulate students’ reception to ethics learning (Ganguly et al., 2022; Ngan & Sim, 2021). They were unaware of why and how bioethics and medical humanities were related to their science background, called them “soft” subject, and thus prioritised acquiring clinical knowledge (Leo & Eagen, 2008).
This paper describes a new teaching approach that draws reference from the philosophy of history teaching, using the past to understand and predict present and future actions. We describe three activities, including using historical narratives, annual newsletter publications, and social media to augment classroom teaching and learning in hopes of promoting ethical sensitivity to students’ clinical and everyday life experiences. Our learners are medical students undertaking a six-year undergraduate medical degree programme. These activities were implemented to support pre-clinical year teaching, though also applicable to clinical year students.
II. DESCRIPTIONS OF THREE TEACHING ACTIVITIES
A. Historical Narratives
The adoption of historical narratives in bioethics teaching draws reference from the philosophy of history teaching, using the past to appreciate the present and the future. But its history is often neglected in the curriculum due to time constraints. Students perceived a disconnection between themselves and unethical events, struggling to understand the significance and effects specific past events may have had on present society (Ngan & Sim, 2021). Gerald L. Gutek (1995), History Educator, advocated that “[teaching] should illuminate the past in order to provide the perspective in time and place that we need to make reflective decisions on the [medical] education choices that face us today. Understanding the importance of bioethics history reminds ourselves about the wrongdoings in science, either due to procedural insensitivity or limited guidelines, and may also improve individual behaviour and organisational culture, re-enforcing a high standard of professional conduct. The video narratives reinforce historical knowledge and the ability to discern and scrutinize the similarities and differences between the past and present.
In this pilot project supported by the faculty’s teaching development grant, landmark historical events were developed as short video narratives that complemented the teaching curriculum topic. Table 1 is a non-exhaustive list of examples describing key events in ethics and how they relate to contemporary issues. In our experience, the video productions were well-received by students’ feedback evaluation. The high cost, however, would be a concern. Should the video improve students’ sensitivity towards bioethics, a comprehensive development of bioethics history video should be invested as an educational media to support teaching.
|
Historical Events |
Related Ethical Concerns |
Contemporary Issues |
|
Eugenics measures in the United States (1896- 1940), Germany (1933-45), and Japan (1948-1996) |
Eugenics |
Emerging technologies (e.g., gene-editing technologies, preimplantation diagnosis, and prenatal diagnosis) |
|
The “God” Committee: Rationing dialysis machines (1961) |
Equity, fair allocation approach, transplantation ethics |
Allocation of scarce resources (e.g., vaccine, ICU bed, funds) |
|
Tuskegee Syphilis Study, (1972) |
Research ethics (e.g., informed consent, exploitation of vulnerable populations) |
Research involving vulnerable populations (e.g., homeless, inmates) |
|
Stanford Prison Experiment (1971)
Milgram’s “destructive obedience” Study (1974) |
Unethical research conduct was uncovered (e.g., psychological harms, deception) |
Social and behaviour research illuminates the need for participant protection beyond the scope of biomedical studies. |
|
Table 1. Implications of Landmark Events on Present-day |
||
B. Bioethics Newsletter
In this pilot project, our team incepted a student-led bioethics newsletter aiming to draw ethical sensitivity in everyday life. Medical students were invited to contribute and write a commentary based on a topical issue of their interest; stimuli may have ranged from the news, movies, dramas, documentaries, plays, clinical ward experiences, and overseas observations. The opportunity provided students with a platform to voice and elucidate their opinions. It also allowed students to be more receptive to opposing ideas, developing a greater awareness of ethical dilemmas.
We published three annual newsletters and reflected on our experience. In the first issue, there was no peer-review process. We felt that the absence of a communication medium between the student writers and student editors hindered the quality of submissions. A peer-review process was implemented starting from the second issue, which was perceived to be beneficial as students were able to receive feedback and enhance intellectual rigour. More importantly, students were also exposed to the peer-reviewing process, which is useful for their future professional career development in academia.
Several obstacles relating to the submission process and the future sustainability of the newsletter were also met. In the first issue, interest was generated primarily through word-of-mouth and promotion on social media. In the second issue, prize incentives were given to best-written submissions. Participation gained momentum in the second and third issues, where we saw an average of 15-20 submissions. Sustainability was also a concern in terms of reader engagement and recruiting altruistic junior students to take over the project. To encourage multidisciplinary engagement, we aim to call for submissions in both written Chinese and English and accept entries from all students within the medicine faculty. We have a long-term goal of fostering a multidisciplinary collaboration across the Faculties.
C. Social Media
Given the generational influx of physicians and medical educators, the use of social media in medical education has seen rising popularity in recent years. Platforms like Twitter, Instagram, YouTube, and LinkedIn are easily accessible, user-friendly and encourage users’ interaction in a local and international setting. The flexibility of social media may also promote active learning pedagogies and personalised education, allowing students to build upon the knowledge they perceive to be interesting.
We started an Instagram page (IG: cubioethics) in June 2020 and curated content on a monthly basis. Content covered a broad range of bioethical topics, including several themed series: a news roundup named “Ethics in the News” and a series based on biotechnology seen in the sci-fi television series, Black Mirror. Each post consisted of a short synopsis on the topic and multiple discussion points were raised to incite critical thinking and reflection.
The flexibility and informal nature of Instagram allowed us to diversify the traditional bioethics content taught in the classroom. For example, it offered an experimental opportunity to teach through television and film. Moreover, the Instagram page allowed us to connect with students and professionals from local and international institutes. Engagement was reflected in post shares, likes, comments, and page follows. As the bioethics community on Instagram remains relatively small, it was easy to establish rapport. This community was able to help expand our audience via mutual post sharing and furthered the ethical debate raised in our posts.
Maintaining an Instagram page was not easy – content creation, the design process, and engaging with readers required careful planning and time. Also, from a cultural standpoint, it seemed as if there was a stronger tendency for international users to publicly participate in the conversation by commenting rather than local students. This may be due to worries about online criticism or the pervasive nature of social media and how it may no longer be viewed as a “safe space” for controversial discourse.
III. CONCLUSION
We reflected on our experience refining traditional didactic pedagogy by adopting three activities: historical narratives, newsletters, and social media. Each component presents unique educational benefits (e.g., recounting the evolution of today’s achievements, exposing students to peer-review publishing experience, cultivating sensitivities to everyday life) and operational barriers (e.g., budget constraints, altruistic students’ recruitment, time- and labour-intensive). Our teaching pedagogy may also be adopted in bioethics teaching in other disciplines, including biomedical and life sciences.
Notes on Contributors
OMYN conceived the study, developed the narration scripts, facilitated the newsletter peer-review as a teacher editor, reviewed the literature, and drafted the intellectual content of the manuscript.
JYNH led the newsletter peer-review as a student editor, managed the social media platform, and drafted the intellectual content of the manuscript.
SS reviewed newsletter entries and critically revised the manuscript for intellectual content. All authors are accountable for all aspects of the work and approve the final manuscript.
Ethical Approval
This study involves a theoretical discussion only and does not require ethical approval.
Data Availability
The data that support the findings of this study are openly available in the Figshare repository. http://doi.org/10.6084/m9.figshare.19768264
Funding
The study is supported by the Teaching Development and Language Enhancement Grant (TDLEG) for the 2019-22 Triennium. The funders had no role in the content review of the manuscript.
Declaration of Interest
The authors declare no conflict of interest.
References
Carrese, J. A., Malek, J., Watson, K., Lehmann, L. S., Green, M. J., McCullough, L. B., Geller, G., Braddock III, C. H., & Doukas, D. J. (2015). The essential role of medical ethics education in achieving professionalism: The Romanell Report. Academic Medicine, 90(6), 744–752. http://doi.org/10.1097/ACM.0000000000000715
Ganguly, B., D’Souza, R., & Nunes, R. (2022). Challenges in the teaching–learning process of the newly implemented module on bioethics in the undergraduate medical curriculum in India. Asian Bioethics Review. https://doi.org/10.1007/s41649-022-00225-2
Gutek, G. L. (1995). A history of the western educational experience (2nd ed.). Waveland Press, Inc.
Leo, T., & Eagen, K. (2008). Professionalism education: The medical student response. Perspectives in Biology and Medicine, 51(4), 508–516. https://doi.org/10.1353/pbm.0.0058
Mattick, K., & Bligh, J. (2006). Teaching and assessing medical ethics: Where are we now? Journal of Medical Ethics, 32(3), 181–185. http://doi.org/10.1136/jme.2005.014597
Ngan, O. M. Y., & Sim, J. H. (2021). Evolution of bioethics education in the medical programme: A tale of two medical schools. International Journal of Ethics Education, 6, 37–50. https://doi.org/10.1007/s40889-020-00112-0
Qian, Y., Han, Q., Yuan, W., & Fan, C. (2018). Insights into medical humanities education in China and the West. Journal of International Medical Research, 46(9), 3507–3517.
Sim, J. H., Ngan, O. M. Y., & Ng, H. K. (2019). Bioethics education in the medical programme among Malaysian medical schools: Where are we now? Journal of Medical Education and Curricular Development, 6.
*Olivia M.Y Ngan
Medical Ethics and Humanities Unit,
School of Clinical Medicine,
Li Ka Shing Faculty of Medicine,
The University of Hong Kong, Pokfulam,
Hong Kong Island, Hong Kong SAR
Email: olivian1@hku.hk
Submitted: 30 Nov 2022
Accepted: 30 Jan 2023
Published online: 4 July, TAPS 2023, 8(3), 45-49
https://doi.org/10.29060/TAPS.2023-8-3/SC2921
Sasikala Devi Amirthalingam1, Shamala Ramasamy2 & Sharifah Sulaiha Hj Syed Aznal3
1Department of Family Medicine, International Medical University, Kuala Lumpur, Malaysia; 2Department for Psychology, International Medical University, Kuala Lumpur, Malaysia; 3Department of Obstetrics and Gynaecology, International Medical University, Kuala Lumpur, Malaysia
Abstract
Introduction: Introduction to Health Profession (IHP) was designed to teach first-year medical students the importance of self-directed learning, accountability, and teamwork in healthcare. Due to the COVID 19 pandemic, the course was delivered virtually, incorporating elements of gamification.
Methods: Gamification features included collaborative teamwork to simulate and record the roleplay for assignments based on crisis management scenarios. The syllabus involves knowledge checks to promote self-directed learning and personal accountability as well as online questionnaires to identify personality traits followed by discussion. Games like Chinese whispers and charades were introduced to identify listening skills. Additional gamification features include progress mechanics for collecting badges upon successful completion of knowledge checks / assessments and completing collaborative teamwork activities.
Results: Results from the descriptive study on the educational usefulness of the IHP module was found to be satisfactory. The feedback was encouraging as >95% of students gave positive feedback that the IHP activities enabled them to understand the value of teamwork, effective communication, professional behavior and enabled them to be resilient and adaptable. 92% agreed that the IHP activities helped to make connections and network with their peers during the pandemic
Conclusion: Gamification of IHP course was successful in terms of practicality and usefulness in promoting communication, collaborative work, experiential learning, and teamwork. Students were empowered to take charge of their own learning of both content and development of interpersonal skills and teamwork through gamification. The isolation caused by the pandemic was alleviated by the networking that occurred during collaborative group activities.
Keywords: Gamification, Self-directed Learning, Collaborative Learning
I. INTRODUCTION
Introduction to Health Profession (IHP) course was initiated during Covid-19 pandemic and conducted at the beginning of our medical program enrolment to introduce freshmen to the real world and value systems of health professional. The learning activities were designed to provide real life experiences, exposing to communication skills within the community and peers, professionalism including teamwork and ethics, and the value of self-reflecting practice. The isolation caused by the pandemic was alleviated by networking that occurred during collaborative group activities and online interactive discussion with invited speakers of health professionals. The group activities were gamified to make learning fun, memorable, engaging and motivating. It is designed to promote a sense of accomplishment while learning through discovery and during the social interaction.
Gamification in education has existed since time immemorial but with the advent of wireless technology, it has given rise to unique ways to improve student engagement (Dodson, 2021) in learning. Gamification is defined as “the craft of deriving all the fun and addicting elements found in games and applying them to real-world or productive activities” (Chou, 2012). There is growing evidence for gamification in a wider pedagogical context and the concept is gaining traction within the medical education community. These “fun and addicting elements” include progress mechanics such as badges, narrative structure and immediate feedback. The gamification features introduced in the IHP module are badges, immediate feedback, challenges in the form of knowledge checks and roleplay in virtual reality in crisis management scenarios.
II. METHODS
Collaborative group activities were conducted by dividing 171 first year students into 16 small groups. Activities were carried out using synchronous and asynchronous virtual platforms to accommodate about 40 % of international students who were still in their home countries. Lessons in IHP consisted of recognising personality traits, application of communication skills, ethics and professionalism and recognising teamwork as intrinsic requirements for delivery of effective healthcare.
Asynchronous sessions required students to individually go through the prepared learning materials followed by knowledge checks. Test repetition without penalty is allowed within an allotted time frame until learners reach a satisfactory result. Following successful completion of knowledge check, students would earn their badge of completion.
Activities like ‘discovering personality traits’ are conducted as online synchronous workshops and facilitated by a group of psychologists. Self-administered questionnaire was administered to determine personality traits, followed by a psychologist-led group discussion to share feedback and reflection. Having the session on a virtual platform provided the students with a degree of anonymity, which enabled them to share profound reflections and feedback. Through the questionnaire responses, the psychologists were able to identify red flags and reach out to the students.
During the online ‘communication skills’ workshop, games such as Chinese whispers and charades were used to cultivate active listening skills and understand nonverbal communication. Students were assigned to group works comprising of preparing oral presentations on scenarios involving ethics and professionalism. In addition, they were tasked to solve issues in selected crisis management scenarios using role-plays and virtual reality. Creativity is highly encouraged and weighted with high percentage. This encourages social interaction and influences learning by creating a subjective sense of presence to facilitate virtual experiential learning.
Upon completion of the IHP activities, students are required to complete a self-administered questionnaire to feedback on the efficacy of the module, hence implied consent is given. The questionnaire measured whether the gamification of IHP achieved the learning outcomes of enabling the understanding of the value of teamwork, effective communication, professional behaviour and to be adaptable and resilient. In addition, the questionnaire inquired if participation in IHP activities helped them create contacts and network with their peers. Open comments are sought after for thematic analysis.
III. RESULTS
51.4% of the cohort responded to the self-administered online questionnaire. Feedback was encouraging as >95% of students gave positive feedback. They felt IHP activities enabled them to understand the value of teamwork, effective communication, professional behaviour and being resilient and adaptable. Most agreed IHP activities helped to make connections and network with peers during the pandemic. Many agreed they developed some insight about themselves during IHP activities. Several themes were drawn from the collected feedback. The primary theme is teamwork where students demonstrate co-operation in working together in teams to attain mutual goals and learn leadership qualities. Majority felt they developed skills in active listening, organisation, patience, self-confidence, and showing empathy. Other characteristics learnt were resilience building, controlling emotions, adaptation, overcoming challenges, professionalism and ethical behaviour.
Common comments on areas to improve are their lack of confidence and discomfort in expressing one’s thoughts. Both being too rigid and overly flexible were commented. Other comments were not feeling at ease with working in a team, becoming overwhelmed, paying excessive attention to detail, and becoming frustrated. Being shy and quiet as well as not being assertive were among the constructive feedback (See Table 1). A copy of the survey questions and the additional tables of survey results are openly available at https://doi.org/10.6084/m9.figshare.21656864.
|
Student Feedback for the Introduction to Health Profession (IHP) module Total number of respondents: 88 |
|||
|
NO. |
THEMES |
OPEN FEEDBACK FROM STUDENTS |
|
|
Majority of the positive responses are as follows: |
Common comments on areas to improve self: |
||
|
1 |
Teamwork |
|
|
|
2 |
Effective Communication |
|
|
|
3 |
Professional Behavior |
|
|
|
4 |
Adaptability and resilience |
|
|
|
5 |
Making connections and networking with peers |
|
|
|
6 |
Insight to self |
|
|
|
Table 1. Student Feedback from IHP Cohort ME121 |
|||
IV. DISCUSSION
IHP is a new course with the objectives of introducing students to the real world and value systems of the health professional, focusing on communication skills, medical ethics, teamwork, and the importance of self-reflective practice. The learning is mainly facilitated by group work and formative assessment through immediate provision of feedback and self-reflection. Due to pandemic-related restrictions, the initial plans for real life experience and exposure in IHP course had to be converted to the online platform. An instructional method such as gamification was selected to help retain student engagement and encourage participation (Chou, 2012). Applying the design elements and principles found in games to education was useful in sparking student interest and motivation (Chou, 2012).
Knowledge checks challenged the minds, improved cognition and knowledge retention (Singhal et al., 2019). Progress mechanics in the form of earning ‘a badge on completion’ of assigned activities, going through the provided learning material and completing the knowledge check to an acceptable level, promoted self-directed learning, created a sense of achievement and retained student engagement. This reward system fosters student participation, as it is a tangible reward (Dodson, 2021).
The seclusion from real life interaction is feared to mentally and psychologically affect students. A study in Switzerland has shown a significant impact on the mental health of learners due to the lockdown in 2020 (Elmer et al., 2020). In another study, social interaction is recognised as an important factor for enhancing learning especially in areas of critical thinking and problem solving (Hurst et al., 2013). The group works in the IHP course, though set virtually, have assisted students in networking and socialising during the pandemic. This was agreed by majority of the students who participated in IHP activities.
Effective leadership is essential in delivering high standards of clinical practice. The students learnt leadership skills through organising group work, delegating roles and responsibilities among team members. Among the examples of group work are problem- solving scenarios like managing a fire in CCU or multiple vehicle accident on the highway. The instructional content was related to the teamwork and roles and responsibilities of the different health professionals involved in managing the crisis and it was gamified by adding elements of game fiction such as the different themes, settings and characters. As students had to self- produce scripts after some brief research of relevant contents, they had some autonomy over the depth and breadth of their learning. Working in teams towards common goals lead to improved productivity and self-esteem and created supportive relationships during the collaborative learning (Singhal et al., 2019). Narrative synthesis and role playing in scenarios managing crisis situations stimulated reflective practice whilst integration of cause and effect enabled experiential learning.
Overall feedback was encouraging as almost all students enjoyed the activities and found them both educational and engaging. They discovered characteristics in themselves that helped them to improve team spirit and communication. The groupwork on the various projects developed learning communities and promoted interpersonal skills, integrating diverse learner types with a wide range of knowledge, skills, past experiences and personal attributes. This was effectively utilized in the groupwork and collaborative learning.
Some setbacks occurred when both the faculty and students were unfamiliar with online gamification. The synchronous sessions with international students in different time zones, made group discussions challenging. Support from the Information Technology team is valuable but poses an exorbitant cost. Students having expectations of medical school learning to be more didactive, instead had to adapt to being adult learners, for more extensive self- directed learning and reflective practice.
V. CONCLUSION
In conclusion, gamification of IHP module encouraged student engagement, teamwork and collaborative learning. IHP course was accessible virtually, which was a boon for our international students who could interact virtually with peers and access and take part in the lessons. The gamification features used were reproducible. Gamification is useful in medical education and can be pursued as a method to deliver lessons and engage students. It is a tool to allow learning in depth and for experiential learning on the virtual platform.
Notes on Contributors
Dr Sasikala Devi Amirthalingam is the first author, contributing to the abstract, introduction, discussion and literature review. She agrees to be accountable for all aspects of the work.
Dr Shamala Ramasamy is the second author, contributing to methodology, results and literature review. She agrees to be accountable for all aspects of the work.
Prof Sharifah Sulaiha Hj Syed Aznal is the third author, contributing to abstract, introduction, discussion and revising it critically for important intellectual content. She agrees to be accountable for all aspects of the work.
Ethical Approval
The dean of School of Medicine, International Medical University has given a letter to say that there is no objection to sharing of findings for educational purpose.
Data Availability
The data that support the finding are openly available in the Figshare repository. https://doi.org/10.6084/m9.figshare.21656864
Acknowledgement
We would like to acknowledge Fareeza Marican Bt Abu Backer and Norhasliza Binti Hashim from E Learning Department from International Medical University for the technical assistance in the gamification features to the module.
Funding
There is no financial support or any financial relationships that may pose a conflict of interest.
Declaration of Interest
There is no conflicting interest to any parties concerned.
References
Chou, Y. K. (2012). What is gamification. Yukai Chou: Gamification and Behavioral Design. https://yukaichou.com/gamification-examples/what-is-gamification/
Dodson, K. R. (2021). Can gamification drive increased student engagement? Educause Review. https://er.educause.edu/articles/sponsored/2021/10/can-gamification-drive-increased-student-engagement
Elmer, T., Mepham, K., & Stadtfeld, C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE, 15(7), Article e0236337. https://doi.org/10.1371/journal.pone.0236337
Hurst, B., Wallace, R., & Nixon, S. B. (2013). The impact of social interaction on student learning. Reading Horizons: A Journal of Literacy and Language Arts, 52(4), Article 5. https://scholarworks.wmich.edu/reading_horizons/vol52/iss4/5
Singhal, S., Hough, J., & Cripps, D. (2019). Twelve tips for incorporating gamification into medical education. MedEdPublish, 8(3), Article 216.
*Sasikala Devi Amirthalingam
International Medical University,
Kuala Lumpur, Malaysia
+60133513435
Email: SasikalaDevi@imu.edu.my
Submitted: 30 May 2022
Accepted: 7 December 2022
Published online: 4 July, TAPS 2023, 8(3), 35-44
https://doi.org/10.29060/TAPS.2023-8-3/OA2876
Rachel Jiayu Lee1*, Jeannie Jing Yi Yap1*, Abhiram Kanneganti1, Carly Yanlin Wu1, Grace Ming Fen Chan1, Citra Nurfarah Zaini Mattar1,2, Pearl Shuang Ye Tong1,2, Susan Jane Sinclair Logan1,2
1Department of Obstetrics and Gynaecology, National University Hospital, Singapore; 2Department of Obstetrics and Gynaecology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
*Co-first authors
Abstract
Introduction: Disruptions of the postgraduate (PG) teaching programmes by COVID-19 have encouraged a transition to virtual methods of content delivery. This provided an impetus to evaluate the coverage of key learning goals by a pre-existing PG didactic programme in an Obstetrics and Gynaecology Specialty Training Programme. We describe a three-phase audit methodology that was developed for this
Methods: We performed a retrospective audit of the PG programme conducted by the Department of Obstetrics and Gynaecology at National University Hospital, Singapore between January and December 2019 utilising a ten-step Training Needs Analysis (TNA). Content of each session was reviewed and mapped against components of the 15 core Knowledge Areas (KA) of the Royal College of Obstetrics & Gynaecology membership (MRCOG) examination syllabus.
Results: Out of 71 PG sessions, there was a 64.9% coverage of the MRCOG syllabus. Four out of the 15 KAs were inadequately covered, achieving less than 50% of knowledge requirements. More procedural KAs such as “Gynaecological Problems” and those related to labour were poorly (less than 30%) covered. Following the audit, these identified gaps were addressed with targeted strategies.
Conclusion: Our audit demonstrated that our pre-pandemic PG programme poorly covered core educational objectives i.e. the MRCOG syllabus, and required a systematic realignment. The COVID-19 pandemic, while disruptive to our PG programme, created an opportunity to analyse our training needs and revamp our virtual PG programme.
Keywords: Medical Education; Residency; Postgraduate Education; Obstetrics and Gynaecology; Training Needs Analysis; COVID-19; Auditing Medical Education
Practice Highlights
- Regular audits of PG programmes ensure relevance to key educational objectives.
- Training Needs Analysis facilitates identification of learning goals, deficits & corrective change.
- Mapping against a milestone examination syllabus & using Delphi technique helps identify learning gaps.
- Procedural-heavy learning goals are poorly served by didactic PG and need individualised assessment.
- A central committee is needed to balance the learning needs of all departmental CME participants.
I. INTRODUCTION
Postgraduate medical education (PG) programmes are an important aspect in meeting core Specialty Trainees’ (ST) learning goals in addition to other modalities of instruction such as practical training (e.g. supervised patient-care or simulator-based training) (Bryant‐Smith et al., 2019) and workplace-based assessments (e.g. case-based discussions and Objective Structured Clinical Examinations [OSCEs] (Chan et al., 2020; Parry-Smith et al., 2014). In academic medical centres, PG education may often be nestled within a wider departmental or hospital Continuing Medical Education (CME) programme. While both PG and CME programmes indirectly improve patient outcomes by keeping clinicians abreast with the latest updates, reinforcing important concepts, and changing practice (Burr & Johanson, 1998; Forsetlund et al., 2021; Marinopoulos et al., 2007; Norman et al., 2004; Raza et al., 2009; Sibley et al., 1982), it is important to balance the learning needs of STs with that of other learners (E.g. senior clinicians, scientists and allied healthcare professionals). This can be challenging as multiple objectives need be fulfilled amongst various learners. Nevertheless, just as with any other component of good quality patient care, it is amenable to audit and quality improvement initiatives (Davies, 1981; Norman et al., 2004; Palmer & Brackwell, 2014).
The protracted COVID-19 pandemic has disrupted the way we deliver healthcare and conduct non-clinical services (Lim et al., 2009; Wong & Bandello, 2020). In response, the academic medical community has globally embraced the use of teleconferencing platforms such as ZoomⓇ, Microsoft TeamsⓇ and WebexⓇ (Kanneganti, Sia, et al., 2020; Renaud et al., 2021) as well as other custom-built solutions for the synchronous delivery of didactics and group discourse (Khamees et al., 2022). While surgical disciplines have suffered a decline in the quality of “hands-on” training due to reduced elective surgical load and safe distancing (English et al., 2020), the use of simulators (Bienstock & Heuer, 2022; Chan et al., 2020; Hoopes et al., 2020; Xu et al., 2022), remote surgical preceptorship, and teaching through surgical videos (Chick et al., 2020; Juprasert et al., 2020; Mishra et al., 2020) have helped mitigate some of these. Virtual options that that have been reproducibly utilised during the pandemic and will be a part of the regular armamentarium of post-graduate medical educationists include online didactic lectures, livestreaming or video repositories of surgical procedures, (Grafton-Clarke et al., 2022) and virtual case discussions and grand ward rounds (Sparkes et al., 2021). Notably, they facilitate the inclusion of a physically wider audience, be it trainer or trainee, and allow participants to tune in from different geographical locations.
At the Department of Obstetrics and Gynaecology, National University Hospital, Singapore, the forced, rapid transition to a virtual CME format (vCME) (Chan et al., 2020; Kanneganti, Lim, et al., 2020) provided an impetus to critically review and revamp the didactic component of our PG programmes. A large component of this had been traditionally baked into our departmental CME programme which comprises daily morning meetings covering recent specialty and scientific updates, journal clubs, guideline reviews, grand round presentations, surgical videos, exam preparation, topic modular series, and research and quality improvement presentations. The schedule and topics were previously arbitrarily decided by a lead consultant one month prior and were presented by a supervised ST or invited speaker. While attendance by STs at these sessions was mandatory and comprised the bulk of protected ST teaching time, no prior attempt had been made to assess its coverage of core ST learning objectives and in particular, the syllabus for milestone ST exams.
Our main aim was to conduct an audit on the coverage of our previous PG didactic sessions on the most important learning goals with the aim of subsequently restructuring them to better meet these goals.
II. METHODS
We audited and assessed our departmental CME programme’s relevance to the core learning goals of our STs by utilising a Training Needs Analysis (TNA) methodology. While there are various types of TNA used in healthcare and management (Donovan & Townsend, 2019; Gould et al., 2004; Hicks & Hennessy, 1996, 1997; Johnston et al., 2018; Markaki et al., 2021), in general they represent systematic approaches towards developing and implementing a training plan. The common attributes can be distilled into three common phases (Figure 1). Importantly for surgical and procedurally-heavy disciplines, an dimension that is not well covered by didactic sessions alone are assessments for procedural skill competency. These require separate attention that is beyond the scope of this audit.
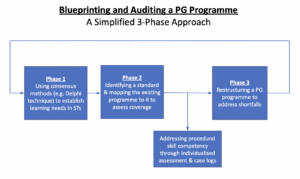
Figure 1. A simplified three phase approach to blueprinting, mapping, and auditing a Postgraduate (PG) Education Programme
A. Phase 1: Identifying Organisational Goals and Specific Objectives
The overarching goal of a specialty PG education programme is to produce well-balanced clinicians with a strong knowledge base. Singapore’s Obstetrics and Gynaecology specialty training programmes have adopted the membership examinations for the Royal College of Obstetricians and Gynaecologists (MRCOG) (Royal College of Obstetricians and Gynaecologists, 2021) of the United Kingdom as the milestone examination for progression from junior to senior ST.
First, we adapted a ten-step TNA proposed by Donovan & Townsend (Table 1) to crystallise our our core learning goals, identify deficiencies, and subsequently propose steps to address these gaps in a systematic fashion that is catered to our specific context. While most aspects were followed without change, we adapted the last aspect i.e. Cost Benefit Analysis. As a general organisational and management tool, the original TNA primarily looked at the financial costs of implementing a training programme. At an academic medical institution, the “cost” is mainly non-financial and mainly refers to time taken away from important clinical service roles.
As part of formulating what were deemed to be core learning goals of an ideal PG programme (i.e. Steps 1 to 4), we had a focused group discussion comprising key stakeholders in postgraduate education, including core faculty (CF), physician faculty (PF), and representative STs. The discussions identified 18 goals specific to our department. We then used a modified Delphi method (Hasson et al., 2000; Humphrey-Murto et al., 2017) to distil what CF, PFs, and STs felt were important priorities for grooming future specialists. Three rounds of priority ranking were undertaken via an anonymised online voting form. At each round, these 18 goals were progressively ranked and distilled until five remained. These were then ranked from highest to lowest priority and comprised 1) exam preparedness, 2) clinical competency, 3) in-depth understanding of professional clinical guidelines, 4) interpretation of medical research literature, and 5) ability to conduct basic clinical research and audits.
|
Training Needs Analysis |
||
|
1 |
Strategic objectives |
|
|
2 |
Operational outcome |
|
|
3 |
Employee Behaviours |
|
|
4 |
Learnable Capabilities |
|
|
5 |
Gap Assessment |
|
|
6 |
Prioritise Learning and Training Needs |
|
|
7 |
Learning Approaches |
|
|
8 |
Roll-out Plan |
|
|
9 |
Evaluation Criteria |
|
|
10 |
Cost Benefit Analysis |
|
Table 1. 10-step Training Needs Analysis
Table adapted from Donovan, Paul and Townsend, John, Learning Needs Analysis (United Kingdom, Management Pocketbooks, 2019)
MRCOG: Member of the Royal College of Obstetricians and Gynaecologists, O&G: Obstetrics and Gynaecology
CREOG: Council on Resident Education in Obstetrics and Gynecology
ACGME: Accreditation Council for Graduate Medical Education,
PG: Post-Graduate Education
B. Phase 2: Identifying a Standard and Assessing for Coverage against This Standard
As with any audit, a “gold-standard” should be identified. As the focus group discussion and Delphi method identified exam preparedness as the highest priority, we created a “blueprint” based on the syllabus of the MRCOG examination (Royal College of Obstetricians and Gynaecologists, 2019). This comprised more than 200 Knowledge Requirements organised more than 200 knowledge requirements into 15 Knowledge Areas (KAs) (Table 2). We mapped the old CME programme against this blueprint to understand the extent of coverage of these KAs. We analyse the session contents between January and December 2019. We felt the best way to ensure systematic coverage of these KAs would be through sessions with pre-identified areas of topical focus conducted during protected teaching time as opposed to opportunistic and voluntary learning opportunities that may not be widely available to all STs. In our department, this applied to morning CME sessions which indeed formed the bulk of protected teaching time for STs, required mandatory attendance, and comprised sessions covering pre-defined topics. Thus, we excluded didactic sessions where 1) the content of the presentations was unavailable for audit, 2) they covered administrative aspects and did not have a pre-identified topical focus where learning was opportunistic (e.g. risk management meetings, labour ward audits), and 3) where the attendance was optional.
Mapping was conducted independently by two members of the study team (JJYY and CYW) with conflict resolved by a third member (RJL). The number of knowledge requirements fulfilled within a KA were expressed as a percentage.
|
Core knowledge areas |
|
Clinical skills |
|
Teaching and research |
|
Core surgical skills |
|
Post operative care |
|
Antenatal care |
|
Maternal Medicine |
|
Management of Labour |
|
Management of delivery |
|
Postpartum problems |
|
Gynaecological problems |
|
Subfertility |
|
Sexual and reproductive health |
|
Early pregnancy care |
|
Gynaecological Oncology |
|
Urogynaecology & pelvic floor problems |
Table 2. RCOG Core Knowledge Areas (Royal College of Obstetricians and Gynaecologists, 2019)
C. Phase 3: Restructuring a PG Programme
The final phase i.e. the restructuring of a PG programme, is directed by responses to Steps 7-10 of the 10-step TNA (Table 1). As the focus of our article is on the methodology of auditing the extent of coverage of our departmental didactic sessions over our core ST learning goals i.e. the MRCOG KAs, these subsequent efforts are detailed in the discussion section.
III. RESULTS
Altogether, 71 presentations were identified (Table 3) of which 12 CME sessions (16.9%) were unavailable and, thus, excluded from the mapping exercise. The most common types of CME sessions presented clinical updates (31.0%), original research (29.6%), journal clubs (16.9%), and exam-preparation sessions (e.g. Case Based Discussion and OSCE simulations) (12.6%). The overall coverage of the entire syllabus was 64.9% (Figure 2). The KAs demonstrating complete coverage (i.e. 100% of all requirements) were “Teaching and Research”, “Postoperative Care” and “Early Pregnancy Care”. Three KAs had a coverage of 75-100% in the CME programme i.e. “Clinical Skills” (89%), “Urogynaecology and Pelvic Floor” (82%), and “Subfertility” (77%) while three were covered below 50% i.e. “Management of Labour”, “Management of Delivery”, “Postpartum Problems”, and “Gynaecological Problems”. These were more practical KAs that were usually covered during ward covers, operating theatre, clinics, and labour ward as well as during practical skills training workshops and grand ward rounds where clinical vignettes were opportunistically discussed depending on in-patient case mix. Nevertheless, this “on-the-ground” training is often unplanned, unstructured and ‘bite-sized’, thus complicating integration with the deep and broad guideline and knowledge proficiency that may be needed to train STs to adapt to complex situations.
|
Type of presentation |
Number of sessions |
Percentage breakdown |
|
Clinical Updates |
22 |
31.0% |
|
Presentation of Original Research |
21 |
29.6% |
|
Journal Club |
12 |
16.9% |
|
Case Based Discussion |
5 |
7.0% |
|
OSCE practice |
4 |
5.6% |
|
Others* |
2 |
2.8% |
|
Audit |
2 |
2.8% |
|
Workshops |
3 |
3.0% |
|
Total |
71 |
100% |
|
*Others: ST Sharing of Overseas Experiences and Trainee Wellbeing |
||
Table 3. Type of CME presentations
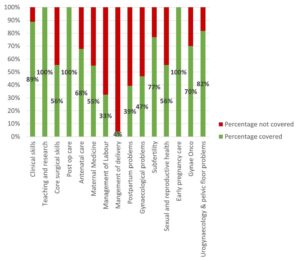
Figure 2. Graph showing the percentage coverage of knowledge areas
IV. DISCUSSION
Our audit revealed a relatively low coverage of the MRCOG KAs with only 64.9% of the syllabus covered. While the morning CME programme caters to all members of the department, the sessions are an important didactic component for ST education and exam preparation as they are deemed “protected” teaching time. There had been no prior formal review assessing whether it catered to this very important section of the department’s workforce. We were also able to recognise those KAs which had exceptionally low coverage were those with a large amount of practical and “hands-on” skills (i.e. “Gynaecological Problems”, “Management of Labour”, “Management of Delivery”, and “Postpartum Problems”). As a surgical discipline, this highlighted that these areas needed directed solutions through other forms of practical instruction and evaluation. In the pandemic environment, this may involve virtual or home-based means (Hoopes et al., 2020). These “hands-on” KAs likely require at least semi-annual individualised assessment by the CF through verified case logs, Objective Structured Assessment of Technical Skills, Direct Observation of Procedural Skills, and Non-Technical Skills for Surgeons (NOTSS) (Bisson et al., 2006; Parry-Smith et al., 2014). This targeted assessment was even more crucial during the recovery “catch-up” phase due to de-skilling because of reduced elective surgical caseload (Amparore et al., 2020; Chan et al., 2020) and facilitated the redistributing of surgical training material to cover training deficits.
While there is significant literature on how to organise a robust PG didactic programme (Colman et al., 2020; Harden, 2001; Willett, 2008), little has been published on how to evaluate an established didactic programme’s coverage of its learner’s educational requirements (Davies, 1981). Most studies evaluating the efficacy of such programmes typically assess the effects of individual CME sessions on physician knowledge or performance and patient outcomes after a suitable interval (Davis et al., 1992; Mansouri & Lockyer, 2007), with most citing a small to medium effect. We believe, however, that our audit process permits a more holistic, reproducible, and structured means of evaluating an existing didactic programme and finding deficits that can be improve upon to brings value to any specialty training programme.
At our institution, safe distancing requirements brought on by the COVID-19 pandemic required a rapid transition to a video-conferencing-based approach i.e. vCME. As milestone examinations were still being held, the first six months were primarily focused on STs as examination preparation remained a high and undisputed priority and learning opportunities had been significantly disrupted by the pandemic. During this phase, our vCME programme was re-organised into three to four sessions per week which were peer-led and supervised by a faculty member. Video-conferencing platforms encouraged audience participation through live feedback, questions posed via the chat box, instantaneous online polling, and directed case-based discussions with ST participants. These facilitated real time feedback to the presenter in a way that was not possible in previous face-to-face sessions due to reasons such as shyness and difficulty conducting polls. Other useful features included being able to record presentations for digital storage in a hospital-based server for access on-demand for revision purposes by STs.
A previously published anonymised questionnaire within our department (Chan et al., 2020) found very favourable opinions of vCME as an effective mode of learning amongst 28 junior doctors (85.7%) and nine presenters (100%) with 75% hoping for it to continue even after normalisation of social distancing policies. Nevertheless, common issues reported included a lack of personal interaction, difficulties in engaging with speakers, technical difficulties, and inaccurate attendance confirmation as shared devices for participating on these vCME sessions sometimes failed to identify who was present. While there is altered teacher and learner engagement due to physical separation across a digital medium, studies have also found that the virtual platform provided a useful means of communication and feedback and created a psychologically safe learning environment (Dong et al., 2021; Wasfy et al., 2021).
While our audit focused primarily on STs, departmental CME programmes need to find balanced in catering to the educational outcome of various groups of participants within a clinical department (e.g. senior clinicians, nursing staff, allied healthcare professionals, clinical scientists). Indeed, as these groups started to return to the CME programme after about six months following the vCME transition, we created a core postgraduate committee comprising members representing the learning interests of each party i.e. Department research director, ST Programme Director and Assistant Director, and a representative senior ST in the fifth or sixth year of training, so that we could continue to meet the recommendations set in our TNA while rebalancing the programme to meet the needs of all participants. Out of an average of 20 CME sessions per month, four were dedicated to departmental and hospital grand rounds each. Of the remaining 12 sessions, two were dedicated towards covering KAs, four scientific presentations, three clinical governance aspects, and one journal club. The remaining two sessions would be “faculty wildcard” sessions to be used at the committee’s discretion of the committee to cover poorly covered, more contemporary, “breaking news” topics, or serve as a buffer in the event of cancellations of other topics. Indeed, the same TNA-based audit methodology can be employed any other group of CME participants.
A key limitation in our audit method is that it focused on the breadth of coverage of learning objectives, but not the quality of the teaching and its depth. Teaching efficacy is also important in the delivery of learning objectives (Bakar et al., 2012) and needs more specific assessment tools (Metheny et al., 2005). Evaluating the quality of PG training could take several forms and may be direct e.g. an evaluation by the learner (Gillan et al., 2011), or could be indirect e.g. charting the learner’s progress through OSCEs and CEXs, scheduled competency reviews, and ST examination pass rates (Pinnell et al., 2021). Importantly, despite the rise of virtual learning platforms, there is little consensus on the best way to evaluate e-learning methods (De Leeuw et al., 2019). Nevertheless, our main audit goal was to assess the extent of coverage of the MRCOG syllabus which is a key training outcome. Future audits, however, should incorporate this element to provide additional qualitative feedback to assess this dimension as well. Further research should be carried out in terms of evaluating the effects of optimising a PG didactic programme on key outcomes such as ST behaviour, perceptions, and objective outcomes such as examination results.
Finally, while these were the results of an audit conducted in a single hospital department and used a morning CME programme as a basis for evaluation, we believe that this audit methodology based on a ten-step TNA and also utilising the Delphi method and syllabus mapping techniques (Harden, 2001) can be reproduced to any academic department that has a regular didactic programme as long as a suitable standard is selected. The Delphi method can easily be conducted via online survey platforms (e.g. Google Forms) to crystallise the PG programme goals. Our audit shows that without a systematic evaluation of past didactic sessions, it is possible for even mature CME programme to fall significantly short of ameeting the needs of its learners and that PG didactic sessions need deliberate planning.
V. CONCLUSION
Just as any other aspect of healthcare delivery, CME and PG programmes are amenable to audits and must adjust to an ever-changing delivery landscape. Rather than curse the darkness during the COVID-19 pandemic, we explored the potential of reformatting the PG programme and adjusting course to better suit the needs of our STs. We demonstrate a method of auditing an existing programme, distilling important learning goals, comparing it against an appropriate standard (i.e. coverage of the MRCOG KAs), and implementing changes utilising reproducible techniques such as the Delphi method (Humphrey-Murto et al., 2017). This process should be a regular mainstay of any mature ST programme to ensure continued relevancy. As continual outbreaks, even amongst vaccinated populations (Amit et al., 2021; Bar-On et al., 2021; Bergwerk et al., 2021) auger a future of COVID-19 endemicity, we must accept a “new-normal” comprising of intermittent workplace infection control policies such as segregation, shift work, and restrictions for in-person meetings (Kwon et al., 2020; Liang et al., 2020). Through our experience, we have shown that this auditing methodology can also be applied to vCME programmes.
Notes on Contributors
Rachel Jiayu Lee participated in the data collection and review, the writing of the paper, and the formatting for publication.
Jeannie Jing Yi Yap participated in the data collection and review, the writing of the paper, and the formatting for publication.
Carly Yanlin Wu participated in data collection and review.
Grace Chan Ming Fen participated in data collection and review.
Abhiram Kanneganti was involved in the writing of the paper, editing, and formatting for publication. Citra Nurfarah Zaini Mattar participated in the editing and direction of the paper.
Pearl Shuang Ye Tong participated in the editing and direction of the paper.
Susan Jane Sinclair Logan participated in the editing and direction of the paper.
Ethical Approval
IRB approval for waiver of consent (National Healthcare Group DSRB 2020/00360) was obtained for the questionnaire assessing attitudes towards vCME.
Data Availability
There is no relevant data available for sharing in this paper.
Acknowledgement
We would like to acknowledge the roles of Mr Xiu Cai Wong Edwin, Mr Lee Boon Kai and Ms Teo Xin Yue in the administrative roles behind auditing and reformatting the PG medical education programme.
Funding
There was no funding for this article.
Declaration of Interest
The authors have no conflicts of interest in connection with this article.
References
Amit, S., Beni, S. A., Biber, A., Grinberg, A., Leshem, E., & Regev-Yochay, G. (2021). Postvaccination COVID-19 among healthcare workers, Israel. Emerging Infectious Diseases, 27(4), 1220. https://doi.org/10.3201/eid2704.210016
Amparore, D., Claps, F., Cacciamani, G. E., Esperto, F., Fiori, C., Liguori, G., Serni, S., Trombetta, C., Carini, M., Porpiglia, F., Checcucci, E., & Campi, R. (2020). Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urologica e Nefrologica, 72(4), 505-509. https://doi.org/10.23736/s0393-2249.20.03868-0
Bakar, A. R., Mohamed, S., & Zakaria, N. S. (2012). They are trained to teach, but how confident are they? A study of student teachers’ sense of efficacy. Journal of Social Sciences, 8(4), 497-504. https://doi.org/10.3844/jssp.2012.497.504
Bar-On, Y. M., Goldberg, Y., Mandel, M., Bodenheimer, O., Freedman, L., Kalkstein, N., Mizrahi, B., Alroy-Preis, S., Ash, N., Milo, R., & Huppert, A. (2021). Protection of BNT162b2 vaccine booster against Covid-19 in Israel. New England Journal of Medicine, 385(15), 1393-1400. https://doi.org/10.1056/NEJMoa2114255
Bergwerk, M., Gonen, T., Lustig, Y., Amit, S., Lipsitch, M., Cohen, C., Mandelboim, M., Levin, E. G., Rubin, C., Indenbaum, V., Tal, I., Zavitan, M., Zuckerman, N., Bar-Chaim, A., Kreiss, Y., & Regev-Yochay, G. (2021). Covid-19 breakthrough infections in vaccinated health care workers. New England Journal of Medicine, 385(16), 1474-1484. https://doi.org/10.1056/NEJMoa2109072
Bienstock, J., & Heuer, A. (2022). A review on the evolution of simulation-based training to help build a safer future. Medicine, 101(25), Article e29503. https://doi.org/10.1097/MD.0000000000029503
Bisson, D. L., Hyde, J. P., & Mears, J. E. (2006). Assessing practical skills in obstetrics and gynaecology: Educational issues and practical implications. The Obstetrician & Gynaecologist, 8(2), 107-112. https://doi.org/10.1576/toag.8.2.107.27230
Bryant‐Smith, A., Rymer, J., Holland, T., & Brincat, M. (2019). ‘Perfect practice makes perfect’: The role of laparoscopic simulation training in modern gynaecological training. The Obstetrician & Gynaecologist, 22(1), 69-74. https://doi.org/10.1111/tog.12619
Burr, R., & Johanson, R. (1998). Continuing medical education: An opportunity for bringing about change in clinical practice. British Journal of Obstetrics and Gynaecology, 105(9), 940-945. https://doi.org/10.1111/j.1471-0528.1998.tb10255.x
Chan, G. M. F., Kanneganti, A., Yasin, N., Ismail-Pratt, I., & Logan, S. J. S. (2020). Well-being, obstetrics and gynaecology and COVID-19: Leaving no trainee behind. Australian and New Zealand Journal of Obstetrics and Gynaecology, 60(6), 983-986. https://doi.org/10.1111/ajo.13249
Chick, R. C., Clifton, G. T., Peace, K. M., Propper, B. W., Hale, D. F., Alseidi, A. A., & Vreeland, T. J. (2020). Using technology to maintain the education of residents during the COVID-19 pandemic. Journal of Surgical Education, 77(4), 729-732. https://doi.org/10.1016/j.jsurg.2020.03.018
Colman, S., Wong, L., Wong, A. H. C., Agrawal, S., Darani, S. A., Beder, M., Sharpe, K., & Soklaridis, S. (2020). Curriculum mapping: an innovative approach to mapping the didactic lecture series at the University of Toronto postgraduate psychiatry. Academic Psychiatry, 44(3), 335-339. https://doi.org/10.1007/s40596-020-01186-0
Davies, I. J. T. (1981). The assessment of continuing medical education. Scottish Medical Journal, 26(2), 125-134. https://doi.org/10.1177/003693308102600208
Davis, D. A., Thomson, M. A., Oxman, A. D., & Haynes, R. B. (1992). Evidence for the effectiveness of CME: A Rreview of 50 randomized controlled trials. Journal of the American Medical Association, 268(9), 1111-1117. https://doi.org/10.1001/jama.1992.03490090053014
De Leeuw, R., De Soet, A., Van Der Horst, S., Walsh, K., Westerman, M., & Scheele, F. (2019). How we evaluate postgraduate medical e-learning: systematic review. JMIR medical education, 5(1), e13128.
Dong, C., Lee, D. W.-C., & Aw, D. C.-W. (2021). Tips for medical educators on how to conduct effective online teaching in times of social distancing. Proceedings of Singapore Healthcare, 30(1), 59-63. https://doi.org/10.1177/2010105820943907
Donovan, P., & Townsend, J. (2019). Learning Needs Analysis. Management Pocketbooks.
English, W., Vulliamy, P., Banerjee, S., & Arya, S. (2020). Surgical training during the COVID-19 pandemic – The cloud with a silver lining? British Journal of Surgery, 107(9), e343-e344. https://doi.org/10.1002/bjs.11801
Forsetlund, L., O’Brien, M. A., Forsén, L., Mwai, L., Reinar, L. M., Okwen, M. P., Horsley, T., & Rose, C. J. (2021). Continuing education meetings and workshops: Effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews, 9(9), CD003030. https://doi.org/10.1002/14651858.CD003030.pub3
Gillan, C., Lovrics, E., Halpern, E., Wiljer, D., & Harnett, N. (2011). The evaluation of learner outcomes in interprofessional continuing education: A literature review and an analysis of survey instruments. Medical Teacher, 33(9), e461-e470. https://doi.org/10.3109/0142159X.2011.587915
Gould, D., Kelly, D., White, I., & Chidgey, J. (2004). Training needs analysis. A literature review and reappraisal. International Journal of Nursing Studies, 41(5), 471-486. https://doi.org/10.1016/j.ijnurstu.2003.12.003
Grafton-Clarke, C., Uraiby, H., Gordon, M., Clarke, N., Rees, E., Park, S., Pammi, M., Alston, S., Khamees, D., Peterson, W., Stojan, J., Pawlik, C., Hider, A., & Daniel, M. (2022). Pivot to online learning for adapting or continuing workplace-based clinical learning in medical education following the COVID-19 pandemic: A BEME systematic review: BEME Guide No. 70. Medical Teacher, 44(3), 227-243. https://doi.org/10.1080/0142159X.2021.1992372
Harden, R. M. (2001). AMEE Guide No. 21: Curriculum mapping: A tool for transparent and authentic teaching and learning. Medical Teacher, 23(2), 123-137. https://doi.org/10.1080/01421590120036547
Hasson, F., Keeney, S., & McKenna, H. (2000). Research guidelines for the Delphi survey technique. Journal of Advanced Nursing, 32(4), 1008-1015. https://doi.org/10.1046/j.1365-2648.2000.t01-1-01567.x
Hicks, C., & Hennessy, D. (1996). Applying psychometric principles to the development of a training needs analysis questionnaire for use with health visitors, district and practice nurses. NT Research, 1(6), 442-454. https://doi.org/10.1177/174498719600100608
Hicks, C., & Hennessy, D. (1997). The use of a customized training needs analysis tool for nurse practitioner development. Journal of Advanced Nursing, 26(2), 389-398. https://doi.org/https://doi.org/10.1046/j.1365-2648.1997.199702 6389.x
Hoopes, S., Pham, T., Lindo, F. M., & Antosh, D. D. (2020). Home surgical skill training resources for obstetrics and gynecology trainees during a pandemic. Obstetrics and Gynecology 136(1), 56-64. https://doi.org/10.1097/aog.0000000000003931
Humphrey-Murto, S., Varpio, L., Wood, T. J., Gonsalves, C., Ufholz, L.-A., Mascioli, K., Wang, C., & Foth, T. (2017). The use of the Delphi and other consensus group Methods in medical education research: A review. Academic Medicine, 92(10), 1491-1498. https://doi.org/10.1097/ACM.0000000000001812
Johnston, S., Coyer, F. M., & Nash, R. (2018). Kirkpatrick’s evaluation of simulation and debriefing in health care education: a systematic review. Journal of Nursing Education, 57(7), 393-398. https://doi.org/10.3928/01484834-20180618-03
Juprasert, J. M., Gray, K. D., Moore, M. D., Obeid, L., Peters, A. W., Fehling, D., Fahey, T. J., III, & Yeo, H. L. (2020). Restructuring of a general surgery residency program in an epicenter of the Coronavirus Disease 2019 pandemic: Lessons from New York City. JAMA Surgery, 155(9), 870-875. https://doi.org/10.1001/jamasurg.2020.3107
Kanneganti, A., Lim, K. M. X., Chan, G. M. F., Choo, S.-N., Choolani, M., Ismail-Pratt, I., & Logan, S. J. S. (2020). Pedagogy in a pandemic – COVID-19 and virtual continuing medical education (vCME) in obstetrics and gynecology. Acta Obstetricia et Gynecologica Scandinavica, 99(6), 692-695. https://doi.org/10.1111/aogs.13885
Kanneganti, A., Sia, C.-H., Ashokka, B., & Ooi, S. B. S. (2020). Continuing medical education during a pandemic: An academic institution’s experience. Postgraduate Medical Journal, 96, 384-386. https://doi.org/10.1136/postgradmedj-2020-137840
Khamees, D., Peterson, W., Patricio, M., Pawlikowska, T., Commissaris, C., Austin, A., Davis, M., Spadafore, M., Griffith, M., Hider, A., Pawlik, C., Stojan, J., Grafton-Clarke, C., Uraiby, H., Thammasitboon, S., Gordon, M., & Daniel, M. (2022). Remote learning developments in postgraduate medical education in response to the COVID-19 pandemic – A BEME systematic review: BEME Guide No. 71. Medical Teacher, 44(5), 466-485. https://doi.org/10.1080/0142159X.2022.2040732
Kwon, Y. S., Tabakin, A. L., Patel, H. V., Backstrand, J. R., Jang, T. L., Kim, I. Y., & Singer, E. A. (2020). Adapting urology residency training in the COVID-19 era. Urology, 141, 15-19. https://doi.org/10.1016/j.urology.2020.04.065
Liang, Z. C., Ooi, S. B. S., & Wang, W. (2020). Pandemics and their impact on medical training: Lessons from Singapore. Academic Medicine, 95(9), 1359-1361. https://doi.org/10.1097/ACM.0000000000003441
Lim, E. C., Oh, V. M., Koh, D. R., & Seet, R. C. (2009). The challenges of “continuing medical education” in a pandemic era. Annals Academy of Medicine Singapore, 38(8), 724-726. https://www.ncbi.nlm.nih.gov/pubmed/19736579
Mansouri, M., & Lockyer, J. (2007). A meta-analysis of continuing medical education effectiveness. Journal of Continuing Education in the Health Professions, 27(1), 6-15. https://doi.org/10.1002/chp.88
Marinopoulos, S. S., Dorman, T., Ratanawongsa, N., Wilson, L. M., Ashar, B. H., Magaziner, J. L., Miller, R. G., Thomas, P. A., Prokopowicz, G. P., Qayyum, R., & Bass, E. B. (2007). Effectiveness of continuing medical education. Evid Rep Technol Assess (Full Rep), 149, 1-69. https://www.ncbi.nlm.nih.gov/pubmed/17764217
Markaki, A., Malhotra, S., Billings, R., & Theus, L. (2021). Training needs assessment: Tool utilization and global impact. BMC Medical Education, 21(1), Article 310. https://doi.org/10.1186/s12909-021-02748-y
Metheny, W. P., Espey, E. L., Bienstock, J., Cox, S. M., Erickson, S. S., Goepfert, A. R., Hammoud, M. M., Hartmann, D. M., Krueger, P. M., Neutens, J. J., & Puscheck, E. (2005). To the point: Medical education reviews evaluation in context: Assessing learners, teachers, and training programs. American Journal of Obstetrics and Gynecology, 192(1), 34-37. https://doi.org/10.1016/j.ajog.2004.07.036
Mishra, K., Boland, M. V., & Woreta, F. A. (2020). Incorporating a virtual curriculum into ophthalmology education in the coronavirus disease-2019 era. Current Opinion in Ophthalmology, 31(5), 380-385. https://doi.org/10.1097/icu.0000000000000681
Norman, G. R., Shannon, S. I., & Marrin, M. L. (2004). The need for needs assessment in continuing medical education. BMJ (Clinical research ed.), 328(7446), 999-1001. https://doi.org/10.1136/bmj.328.7446.999
Palmer, W., & Brackwell, L. (2014). A national audit of maternity services in England. BJOG, 121(12), 1458-1461. https://doi.org/10.1111/1471-0528.12973
Parry-Smith, W., Mahmud, A., Landau, A., & Hayes, K. (2014). Workplace-based assessment: A new approach to existing tools. The Obstetrician & Gynaecologist, 16(4), 281-285. https://doi.org/10.1111/tog.12133
Pinnell, J., Tranter, A., Cooper, S., & Whallett, A. (2021). Postgraduate medical education quality metrics panels can be enhanced by including learner outcomes. Postgraduate Medical Journal, 97(1153), 690-694. https://doi.org/10.1136/postgradmedj-2020-138669
Raza, A., Coomarasamy, A., & Khan, K. S. (2009). Best evidence continuous medical education. Archives of Gynecology and Obstetrics, 280(4), 683-687. https://doi.org/10.1007/s00404-009-1128-7
Renaud, C. J., Chen, Z. X., Yuen, H.-W., Tan, L. L., Pan, T. L. T., & Samarasekera, D. D. (2021). Impact of COVID-19 on health profession education in Singapore: Adoption of innovative strategies and contingencies across the educational continuum. The Asia Pacific Scholar, 6(3), 14-23. https://doi.org/10.29060/TAPS.2021-6-3/RA2346
Royal College of Obstetricians and Gynaecologists. (2019). Core Curriculum for Obstetrics & Gynaecology: Definitive Document 2019. https://www.rcog.org.uk/media/j3do0i1i/core-curriculum-2019-definitive-document-may-2021.pdf
Sibley, J. C., Sackett, D. L., Neufeld, V., Gerrard, B., Rudnick, K. V., & Fraser, W. (1982). A randomized trial of continuing medical education. New England Journal of Medicine, 306(9), 511-515. https://doi.org/10.1056/NEJM198203043060904
Sparkes, D., Leong, C., Sharrocks, K., Wilson, M., Moore, E., & Matheson, N. J. (2021). Rebooting medical education with virtual grand rounds during the COVID-19 pandemic. Future Healthc J, 8(1), e11-e14. https://doi.org/10.7861/fhj.2020-0180
Wasfy, N. F., Abouzeid, E., Nasser, A. A., Ahmed, S. A., Youssry, I., Hegazy, N. N., Shehata, M. H. K., Kamal, D., & Atwa, H. (2021). A guide for evaluation of online learning in medical education: A qualitative reflective analysis. BMC Medical Education, 21(1), Article 339. https://doi.org/10.1186/s12909-021-02752-2
Willett, T. G. (2008). Current status of curriculum mapping in Canada and the UK. Medical Education, 42(8), 786-793. https://doi.org/10.1111/j.1365-2923.2008.03093.x
Wong, T. Y., & Bandello, F. (2020). Academic ophthalmology during and after the COVID-19 pandemic. Ophthalmology, 127(8), e51-e52. https://doi.org/10.1016/j.ophtha.2020.04.029
Xu, J., Zhou, Z., Chen, K., Ding, Y., Hua, Y., Ren, M., & Shen, Y. (2022). How to minimize the impact of COVID-19 on laparoendoscopic single-site surgery training? ANZ Journal of Surgery, 92, 2102-2108. https://doi.org/10.1111/ans.17819
*Abhiram Kanneganti
Department of Obstetrics and Gynaecology,
NUHS Tower Block, Level 12,
1E Kent Ridge Road,
Singapore 119228
Email: abhiramkanneganti@gmail.com
Submitted: 30 June 2022
Accepted: 31 October 2022
Published online: 4 July, TAPS 2023, 8(3), 26-34
https://doi.org/10.29060/TAPS.2023-8-3/OA2834
Noorjahan Haneem Md Hashim1, Shairil Rahayu Ruslan1, Ina Ismiarti Shariffuddin1, Woon Lai Lim1, Christina Phoay Lay Tan2 & Vinod Pallath3
1Department of Anaesthesiology, Faculty of Medicine, Universiti Malaya, Malaysia; 2Department of Primary Care Medicine, Faculty of Medicine, Universiti Malaya, Malaysia; 3Medical Education Research & Development Unit, Dean’s Office, Faculty of Medicine, Universiti Malaya, Malaysia
Abstract
Introduction: Examiner training is essential to ensure the trustworthiness of the examination process and results. The Anaesthesiology examiners’ training programme to standardise examination techniques and standards across seniority, subspecialty, and institutions was developed using McLean’s adaptation of Kern’s framework.
Methods: The programme was delivered through an online platform due to pandemic constraints. Key focus areas were Performance Dimension Training (PDT), Form-of-Reference Training (FORT) and factors affecting validity. Training methods included interactive lectures, facilitated discussions and experiential learning sessions using the rubrics created for the viva examination. The programme effectiveness was measured using the Kirkpatrick model for programme evaluation.
Results: Seven out of eleven participants rated the programme content as useful and relevant. Four participants showed improvement in the post-test, when compared to the pre-test. Five participants reported behavioural changes during the examination, either during the preparation or conduct of the examination. Factors that contributed to this intervention’s effectiveness were identified through the MOAC (motivation, opportunities, abilities, and communality) model.
Conclusion: Though not all examiners attended the training session, all were committed to a fairer and transparent examination and motivated to ensure ease of the process. The success of any faculty development programme must be defined and the factors affecting it must be identified to ensure engagement and sustainability of the programme.
Keywords: Medical Education, Health Profession Education, Examiner Training, Faculty Development, Assessment, MOAC Model, Programme Evaluation
Practice Highlights
- A faculty development initiative must be tailored to faculty’s learning needs and context.
- A simple framework of planning, implementing, and evaluating can be used to design a programme.
- Target outcome measures and evaluation plans must be included in the planning process.
- The Kirkpatrick model is a useful tool to use in programme evaluation: to answer if the programme has met its objectives.
- The MOAC model is a useful tool to explain why a programme has met its objective.
I. INTRODUCTION
Anaesthesiology specialist training in Malaysia comprises a 4-year clinical master’s programme. At the time of our workshop, five local public universities offer the programme. The course content is similar in all universities, but the course delivery may differ to align with each university’s rules and regulations. The summative examinations are held as a Conjoint Examination. Examiners include lecturers from all five universities, specialists from the Ministry of Health and external examiners from international Anaesthesiology training programmes. The examination consists of a written and a viva voce examination. The areas examined are the knowledge and cognitive skills in patient management.
A speciality training programme’s exit level assessment is an essential milestone for licensing. In our programme, the exit examination occurs at the end of the training before trainees practise independently in the healthcare system and are eligible for national specialist registration. Therefore, aligning the curriculum and assessment to licensing requirements is necessary.
Examiners play an important role during this high-stakes summative examination, making decisions regarding allowing graduating trainees to work as specialists in the community. Therefore, examiners must understand their role. In recent years, the anaesthesiology training programme providers in Malaysia have been taking measures to improve the validity of the examination. These include a stringent vetting process to ensure examination content reflects the syllabus, questions are unambiguous, and the examiners agree on the criteria for passing. However, previous examinations revealed that although examiners were clear on the aim of the examination, some utilised different assessment approaches, which were possibly coloured by personal and professional experiences, and thus needed constant calibration on the passing criteria. In addition, during examiner discussions, different examiners were found to have different skill levels in constructing focused higher-order questions and were not fully aware of potential cognitive biases that may affect the examination results.
These insights from previous examinations warranted a specific skill training session to ensure the trustworthiness of the examination process and results (Blew et al., 2010; Iqbal et al., 2010; Juul et al., 2019, Chapter 8, pp. 127-140; McLean et al., 2008). The examiners and the Specialty committee were keen to ensure that these issues were addressed with a training programme that complements the current on-the-job examiner training.
II. METHODS
An examiner training module was developed using McLean’s adaptation of Kern’s framework for curriculum development: Planning, Implementation and Evaluation (McLean et al., 2008; Thomas et al., 2015). A conceptual framework for the examiner training programme was drawn up from the programme’s conception stage to the evaluation of its outcome, as illustrated in Figure 1 (Steinert et al., 2016).
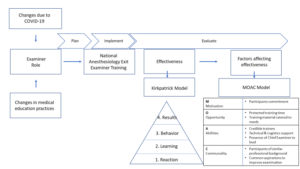
Figure 1: The conceptual framework for the examiner training programme and evaluation of its effectiveness
A. Planning
Three key focus areas were identified for the training programme: (1) Performance Dimension Training (PDT); (2) examiner calibration with Frame-Of-Reference Training (FORT); as well as (3) identifying factors affecting the validity of results and measures that can be taken to prevent them.
1) Performance dimension training (Feldman et al., 2012): The aim was to improve examination validity by reducing examiner errors or biases unrelated to the examinees’ targeted performance behaviours. Finalised marking schemes outlining competencies to be assessed required agreement by all the examiners ahead of time. These needed to be clearly defined and easily understood by all the examiners, and consistency was key to reducing examiner bias.
2) Examiner calibration with Frame-of-Reference Training (FORT) (Newman et al., 2016): Differing levels of experience among all the participants meant that there were differing expectations and performances among them. The examiner training programme needed to assist examiners in resetting expectations and criteria for assessing the candidates’ competencies. This examiner calibration was achieved using pre-recorded simulated viva sessions in which the participants rated candidates’ performances in each simulated viva session and received immediate feedback on their ability and criteria for scoring the candidates.
3) Identifying factors affecting the validity of results (Lineberry, 2019): Factors that may affect the validity of examination results may be related to construct underrepresentation (CU), where the results only reflect one part of an attribute being examined; or construct-irrelevant variance (CIV), where the results are being affected by areas or issues other than the attribute being examined.
An example of CU is sampling issues where only a limited area of the syllabus is examined, or an answer key is limited by the availability of evidence or content expertise.
Examples of CIV include the different ways a concept can be interpreted in different cultures or training centres, ambiguous questions, examiner cognitive biases, examiner fatigue, examinee language abilities, and examinees guessing or cheating. The examiner training programme was designed with the objectives listed in Table 1.
|
Malaysian Anaesthesiology Exit Level Examiner Training Programme |
|
1. Participants should be able to define the purpose and competencies to be assessed in the viva examination. |
|
2. Participants should be able to construct high-order questions (elaborating, probing, and justifying). |
|
3. Participants should be able to agree on anchors on rating scales of examination and narrow the range of ratings for the same encounter everyone observes. |
|
4. Participants should be able to calibrate the scoring of different levels of responses. |
Table 1: Objectives of the Faculty Development Intervention
B. Implementation
The faculty intervention programme was designed as a one-day online programme to be attended by potential examiners for the Anaesthesiology Exit Examination. The programme objectives were prioritised from the needs assessment and designed based on Tekian & Norcini’s recommendations (Tekian & Norcini, 2016). Due to time constraints, training was performed using an online platform closer to the examination dates after obtaining university clearance on confidentiality regarding assessment issues.
The structure and contents of the examiner training programme are outlined in Table 2 and is further elaborated in Appendix A.
|
General content |
Specific content |
|
Lectures |
1. Orientation to the examination regulations, objectives, structure and format of the final examination. |
|
|
2. Ensuring validity of the viva examination: elaborating on the threats present to the process and how to mitigate these concerns. |
|
|
3. Creating high-order questions based on competencies to be assessed and promoting appropriate examiner behaviours through consistency and increasing reliability. |
|
|
4. Utilising marking schemes, anchors and making inferences with:
|
|
Experiential learning sessions |
1. Participants discuss and agree on the competencies to be assessed. 2. Participants work in groups to construct questions based on a given scenario and competencies to be assessed. 3. Participants finalise a rating scale to be used in the examination. 4. Participants observe videos of simulated examination candidates performing at various levels of competencies and rate their performance. The discussion here focused on the similarities and differences between examiners. |
|
Participant feedback and evaluation |
A question-and-answer session is held to iron out any doubts and queries from the participants. |
Table 2: Contents and structure of the examiner training programme
Based on the objectives, the organisers invited a multidisciplinary group of facilitators. The group consisted of anaesthesiologists, medical education experts in assessment and faculty development, and a technical and logistics support team to ensure efficient delivery of the online programme.
A multimodal approach to delivery was adopted to accommodate the diversity of the examiner group (gender, seniority, subspeciality, and examination experience). Explicit ground rules were agreed upon to underpin the safe and respectful learning environment. The educational strategy included interactive lectures, hands-on practice using rubrics created and calibration using video-assisted scenarios. The programme objectives were embedded and reinforced with each strategy. Pre- and post-tests were performed to help participants gauge their learning and assist the programme organisers in evaluating the participants’ learning.
This would be the first time such a programme was held within the local setting. Participants were all anaesthesiologists by profession, were actively involved in clinical duties within a tertiary hospital setting and consented to participate in this programme. As potential examiners, they all had prior experience as observers of the examination process, with the majority having previous experience as examiners as well.
The programme was organised during the peak of the COVID-19 pandemic and was managed on a fully online platform to ensure safety and minimise the time taken away from clinical duties. In addition, participants received protected time for this programme, a necessary luxury as anaesthesiologists were at the forefront of managing the pandemic.
C. Evaluation
The Kirkpatrick model (McLean et al., 2008; Newstrom, 1995;) was used to evaluate the programme’s effectiveness described and elaborated in Figure 2.
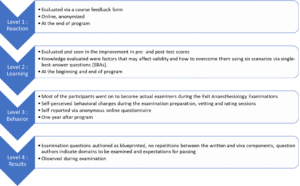
Figure 2: The Kirkpatrick model, elaborated for this programme
The MOAC model (Vollenbroek, 2019), expanded from the MOA (Marin-Garcia & Martinez Tomas, 2016) model by Blumberg & Pringle (Blumberg & Pringle, 1982) was used to examine factors that contributed to the effectiveness of the programme. Motivation, opportunity, ability, and communality are factors that drives action and performance.
III. RESULTS
Eleven participants attended the programme. These participants were examiners for the 2021 examinations from the university training centres and the Ministry of Health, Malaysia. Only one of the participants would be a first-time examiner in the Exit Examination. Four of the would-be examiners could not attend due to service priorities.
A. Level 1: Reaction
Seven of the eleven participants completed the programme evaluation form, which is openly available in Figshare at https://doi.org/10.6084/m9.figshare.20189309.v1 (Tan & Pallath, 2022). All of them rated the programme content as useful and relevant to their examination duties and stated that the content and presentations were pitched at the correct level, with appropriate visual aids and reference materials. The online learning opportunity was also rated as good.
All seven also aimed to make behavioural changes after attending the programme, as indicated below. Some of the excerpts include:
“I am more cognizant of the candidates’ understanding to questions and marking schemes”
“Yes. We definitely need the rubric/marking scheme for standardisation. Will also try to reduce all the possible biases as mentioned in the programme.”
“Yes, as I will be more agreeable to question standardisation in viva examination because it makes it fairer for the candidates.”
The participants also shared their understanding of the importance of standardisation and examiner training and would recommend this programme to be conducted annually. They agreed that the examiner training programme should be made mandatory for all new examiners, with the option of refresher courses for veteran examiners if appropriate.
B. Level 2: Learning
All 11 participants completed the pre-and post-tests. The data supporting these findings of this is openly available in Figshare at https://doi.org/10.6084/m9.figshare.20186582.v1 (Md Hashim, 2021). The participants’ marks in both tests are shown in Appendix B. The areas that showed improvement in scores were identifying why under-sampling is a problem and methods to prevent validity threats. Understanding the source of validity threat from cognitive biases showed a decline in scores (question 2 with scores of 11 to 8 and question 3 with scores of 10 to 8), respectively.
Comparing the post-test scores to pre-test scores, four participants showed improvement, four showed no change (one of the participants answered all questions correctly in both tests) and three participants showed a decline in test scores.
C. Level 3: Behavioural Change
Six participants responded to the follow-up questionnaire, which is openly available in Figshare at https://doi.org/10.6084/m9.figshare.20186591.v2 (Md Hashim, 2022). This questionnaire was administered about a year after the examiner training programme and after the completion of two examinations. Only one respondent did not make any self-perceived behavioural change while preparing the examination questions and conducting the viva examinations. Two respondents did not make any changes while marking or rating candidates.
The specific changes in the three areas of behavioural change that were consciously noted by the respondents were explored. Respondents reported increased awareness and being more systematic in question preparation, making questions more aligned to the curriculum, preparing better quality questions, and being more cognizant of candidates’ understanding of the questions.
They also reported being more objective and guided during marking and rating as the passing criteria were better defined and structured.
Regarding the conduct of the viva examination, respondents shared that they were better prepared during vetting and felt it was easier to rate candidates as the marking schemes and questions were standardised and could ensure candidates could answer all the required questions to pass.
D. Level 4: Results
The examiners who attended the training programme were able to prepare questions as blueprinted and were able to identify areas to be examined and provided recommended criteria for passing each question. This has led to a smooth vetting process and examination.
E. Factors Affecting Effectiveness
Even though the programme was not attended by all the potential examiners, those who did were committed to the idea of a fairer and more transparent examination process. This formed the motivation aspect of the model.
In terms of opportunity, protected training time is important, followed by prioritising the content of the training material according to the most pressing needs.
The ability aspect encompassed the abilities of the facilitators and participants. To emphasise the learning process, credible trainers were invited to this programme to facilitate the lectures and experiential learning sessions. In this aspect, the Faculty Development team comprised an experienced clinician, a basic medical scientist, and an anaesthesiologist, all with medical education qualifications and were vital in ensuring the success of this programme. The whole team was led by the Chief Examiner who focused on the dimensions to be tested and calibrated, while simultaneously managing the expectations of the examiners and their abilities to give and accept feedback. Communication and the skill to be receptive to the proposed changes were also crucial to make the intervention work.
In terms of communality, all the participants were of similar professional backgrounds and shared the common realisation that this training programme was essential and would only yield positive results. Hence this ensured the programme’s overall success.
IV. DISCUSSION
The progressive change seen in this attempt to improve the examination system is aligned with the general progress in medical education. Training of examiners is important (Holmboe et al., 2011), as it is not the tool used for assessment, but rather the person using the tool, that makes the difference. As it is difficult to design the ‘perfect tool’ for performance tests and redesigning a tool only changes 10% of the variance in rating (Holmboe et al., 2011; Williams et al., 2003), educators must now train the faculty in observation and assessment. It is not irrational to extrapolate this effect on written and oral examinations. Holmboe et al. (2011) also share the reasons for a training programme for assessors, which are changing curriculum structure, content and delivery and emerging evidence regarding assessment, building a system reserve, utilising training programmes as opportunities to identify and engage change agents and allow the faculty to form a mental picture of how changes will affect them and improve practice. Enlisting the help and support of a respected faculty member during training will promote the depth and breadth of change.
Khera et al. (2005) described their paediatric examination experiences, in which the Royal College of Paediatrics and Child Health defined examiners’ competencies, selection process and training programme components. The training programme included principles of assessment, examination design, writing questions, interpersonal skills, professional attributes, managing diversity, and assessing the examiners’ skills. They believe these contents will ensure the assessment is valid, reliable, and fair. As Anaesthesiology examiners have different knowledge levels and experiences, it had been crucial to assess their learning needs and provide them with appropriate learning opportunities.
In the emergency brought on by the COVID-19 pandemic, online training was the safest and most feasible platform for conducting this programme. Online faculty development activities have the perceived advantages of being convenient, flexible, and allowing interdisciplinary interaction and providing an experience of being an online student(Cook & Steinert, 2013). Forming the facilitation team together with the dedicated technical and logistics team and creating a chat group prior to conducting the programme were key in anticipating and handling communication and technical issues (Cook & Steinert, 2013).
Though participants were engaged and the results of the workshop were encouraging, the programme delivery and the content will be reviewed based on the feedback received. The convenience of an online activity must be balanced with the participant engagement and facilitator presence of a face-to-face-activity. Since the results of both methods of delivery differs (Arias et al., 2018; Daniel, 2014; Kemp & Grieve, 2014), the best solution may to ask the participants what would best work for them, as they are adult learners and experienced examiners. The programme must be designed with participants involvement, with opportunities to participate and engaging facilitators and support teams that would be able to support the participants’ learning need (Singh et al., 2022).
At the end of the programme, the effectiveness of the programme was measured by referencing the Kirkpatrick model. The Kirkpatrick model (Newstrom, 1995; Steinert et al., 2006) was the most helpful in helping us identify the success of the intervention, which included behavioural change. Measuring behavioural change and impact on the examination results, organisational changes and changes in student learning may be difficult and may not be directly caused by a single intervention (McLean et al., 2008). The key, is perhaps to involve examiners, students and other stakeholders in the evaluation process, using various validated tools, and to ensure that the effort is ongoing, with sustained support, guidance and feedback (McLean et al., 2008).
To explain the overall effectiveness of the programme (with regards to reaction, learning and behavioural change), the MOAC model (Vollenbroek, 2019) expanded from the original MOA model was used. The MOAC model not only describes factors that affect an individual’s performance in a group, but also the group behaviour.
Motivation is an important driving force of action, and members are more motivated when a subject becomes relevant on a personal level, leading to action. The motivation to be informed and to improve has led to active participation in the knowledge sharing session, processing new information presented in the programme and adopting changes learnt during the programme. Presence of a group of motivated individuals with the same goals supported each other’s learning.
Opportunity, especially time, space and resources, must be allocated to reflect the value and relevance of any activity. Work autonomy, allows professionals to engage in what they consider relevant or important, and be accountable for their work outcomes. Facilitating conditions, for example, technology, facilitators, and a platform to practise what is being learnt are also important aspects of opportunity. Allowing protected time with the appropriate facilitating conditions, indicates institutional support and has enabled participants to fully optimise the learning experience.
Ability positively affects knowledge exchange and willingness to participate. Having prior knowledge improves a participant’s ability to absorb and utilise new knowledge. The programme participants, being experienced clinical teachers and examiners are fully aware of their capabilities and are able to process and share important information. Experienced faculty development facilitators who are also clinical teachers and examiners were able to identify areas to focus and provide relevant examples for application.
Communality is the added dimension to the original MOA model. Participants of this programme are members in a complex system, who already know each other. Having shared identity, language and challenges have allowed them to develop trust while pursuing the common goal of improving the system they were working in. This facilitated knowledge sharing and behavioural change.
The limitation in our programme is the small sample size. However, we believe that is important to review the effectiveness of a programme, especially with regards to behavioural change, and to share how other programmes can benefit from using the frameworks we shared. The findings from this programme will also inform how we conduct future faculty development programmes. With pandemic restrictions lifted, we hope to conduct this programme face-to-face, to facilitate engagement and communication.
V. CONCLUSION
For this faculty development programme to succeed, targets for success must first be defined and factors that contribute to its success need to be identified. This will ensure active engagement from the participants and promote the sustainability of the programme.
Notes on Contributors
Noorjahan Haneem Md Hashim designed the programme, assisted in content creation, curation and matching learning activities, moderated the programme, and conceptualised and wrote this manuscript.
Shairil Rahayu Ruslan participated as a committee of the programme, assisted as a simulated candidate during the training sessions, as well as contributed to the conceptualisation, writing, and formatting of this manuscript. She also compiled the bibliography and cross-checked the references for this manuscript.
Ina Ismiarti Shariffuddin created the opportunity for the programme (Specialty board and interdisciplinary buy-in, department funding), prioritised the programme learning outcomes, chaired the programme, and contributed to the writing and review of this manuscript.
Woon Lai Lim participated as a committee member of the programme and contributed to the writing of this manuscript.
Christina Phoay Lay Tan designed and conducted the faculty development training programme, and reviewed and contributed to the writing of this manuscript. She also cross-checked the references for this manuscript.
Vinod Pallath designed and conducted the faculty development training programme, and reviewed and contributed to the writing of this manuscript.
All authors verified and approved the final version of the manuscript.
Ethical Approval
Ethical approval was applied for the follow-up questionnaire that was distributed to the participants, which was approved on the 6th of May 2022 (Reference number: UM.TNC2/UMREC_1879). The programme evaluation and pre- and post-tests are accepted as part of the programme evaluation procedures.
Data Availability
De-identified individual participant data collected are available in the Figshare repository immediately after publication without an end date, as below :
https://doi.org/10.6084/m9.figshare.20189309.v1
https://doi.org/10.6084/m9.figshare.20186582.v1
https://doi.org/10.6084/m9.figshare.20186591.v2
The authors confirm that all data underlying the findings are freely available for view from the Figshare data repository. However, the reuse and resharing of the programme evaluation form, pre- and posttest questions, as well as followup questionnaire, despite being easily accessible from the data repository, should warrant a reasonable request from the corresponding author out of courtesy.
Acknowledgement
The authors would like to acknowledge Dr Selvan Segaran and Dr Siti Nur Jawahir Rosli from the Medical Education, Research and Development Unit (MERDU) for their logistics and technical support in all stages of this programme; Professor Dr Jamuna Vadivelu, Head, MERDU for her insight and support; Dr Nur Azreen Hussain and Dr Wan Aizat Wan Zakaria from the Department of Anaesthesiology, UMMC and UM, for their acting skills in the training videos; and the Visibility and Communication Unit, Faculty of Medicine, Universiti Malaya for their video editing services.
Funding
There is no funding source for this manuscript.
Declaration of Interest
There are no conflicts of interest among the authors of this manuscript.
References
Arias, J. J., Swinton, J., & Anderson, K. (2018). Online vs. face-to-face: A comparison of student outcomes with random assignment. E-Journal of Business Education & Scholarship of Teaching, 12(2), 1–23. https://eric.ed.gov/?id=EJ1193426
Blew, P., Muir, J. G., & Naik, V. N. (2010). The evolving Royal College examination in anesthesiology. Canadian Journal of Anesthesia/Journal canadien d’anesthésie, 57(9), 804-810. https://doi.org/10.1007/s12630-010-9341-1
Blumberg, M., & Pringle, C. D. (1982). The missing opportunity in organizational research: Some implications for a theory of work performance. The Academy of Management Review, 7(4), 560–569. https://doi.org/10.2307/257222
Cook, D. A., & Steinert, Y. (2013). Online learning for faculty development: A review of the literature. Medical Teacher, 35(11), 930–937. https://doi.org/10.3109/0142159X.2013.827328
Daniel, C. M. (2014). Comparing online and face-to-face professional development [Doctoral dissertation, Nova Southeastern University]. https://doi.org/10.13140/2.1.3157.5042
Feldman, M., Lazzara, E. H., Vanderbilt, A. A., & DiazGranados, D. (2012). Rater training to support high-stakes simulation-based assessments. Journal of Continuing Education in the Health Professions, 32(4), 279–286. https://doi.org/10.1002/chp.21156
Holmboe, E. S., Ward, D. S., Reznick, R. K., Katsufrakis, P. J., Leslie, K. M., Patel, V. L., Ray, D. D., & Nelson, E. A. (2011). Faculty development in assessment: The missing link in competency-based medical education. Academic Medicine, 86(4), 460–467. https://doi.org/10.1097/ACM.0b013e31820cb2a7
Iqbal, I., Naqvi, S., Abeysundara, L., & Narula, A. (2010). The value of oral assessments: A review. The Bulletin of the Royal College of Surgeons of England, 92(7), 1–6. https://doi.org/10.1308/147363510×511030
Juul, D., Yudkowsky, R., & Tekian, A. (2019). Oral Examinations. In R. Yudkowsky, Y. S. Park, & S. M. Downing (Eds.), Assessment in Health Professions Education. Routledge. https://doi.org/10.4324/9781315166902-8
Kemp, N., & Grieve, R. (2014). Face-to-face or face-to-screen? Undergraduates’ opinions and test performance in classroom vs. online learning. Frontiers in Psychology, 5. https://doi.org/10.3389/fpsyg.2014.01278
Khera, N., Davies, H., Davies, H., Lissauer, T., Skuse, D., Wakeford, R., & Stroobant, J. (2005). How should paediatric examiners be trained? Archives of Disease in Childhood, 90(1), 43–47. https://doi.org/10.1136/adc.2004.055103
Lineberry, M. (2019). Validity and quality. Assessment in Health Professions Education, 17-32. https://doi.org/10.4324/9781315166902-2
Marin-Garcia, J. A., & Martinez Tomas, J. (2016). Deconstructing AMO framework: A systematic review. Intangible Capital, 12(4), 1040. https://doi.org/10.3926/ic.838
McLean, M., Cilliers, F., & Van Wyk, J. M. (2008). Faculty development: Yesterday, today and tomorrow. Medical Teacher, 30(6), 555–584. https://doi.org/10.1080/01421590802109834
Md Hashim, N. H. (2021). Pre- and Post-test [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.20186582.v1
Md Hashim, N. H. (2022). Followup Questionnaire [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.20186591.v2
Newman, L. R., Brodsky, D., Jones, R. N., Schwartzstein, R. M., Atkins, K. M., & Roberts, D. H. (2016). Frame-of-reference training: Establishing reliable assessment of teaching effectiveness. Journal of Continuing Education in the Health Professions, 36(3), 206–210. https://doi.org/10.1097/CEH.0000000000000086
Newstrom, J. W. (1995). Evaluating training programs: The four levels, by Donald L. Kirkpatrick. (1994). San Francisco: Berrett-Koehler. 229 pp., $32.95 cloth. Human Resource Development Quarterly, 6(3), 317-320. https://doi.org/10.1002/hrdq.3920060310
Singh, J., Evans, E., Reed, A., Karch, L., Qualey, K., Singh, L., & Wiersma, H. (2022). Online, hybrid, and face-to-face learning through the eyes of faculty, students, administrators, and instructional designers: Lessons learned and directions for the post-vaccine and post-pandemic/COVID-19 World. Journal of Educational Technology Systems, 50(3), 301–326. https://doi.org/10.1177/00472395211063754
Steinert, Y., Mann, K., Anderson, B., Barnett, B. M., Centeno, A., Naismith, L., Prideaux, D., Spencer, J., Tullo, E., Viggiano, T., Ward, H., & Dolmans, D. (2016). A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Medical Teacher, 38(8), 769-786. https://doi.org/10.1080/0142159x.2016.1181851
Steinert, Y., Mann, K., Centeno, A., Dolmans, D., Spencer, J., Gelula, M., & Prideaux, D. (2006). A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Medical Teacher, 28(6), 497–526. https://doi.org/10.1080/01421590600902976
Tan, C. P. L., & Pallath, V. (2022). Workshop Evaluation Form [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.20189309.v1
Tekian, A., & Norcini, J. J. (2016). Faculty development in assessment : What the faculty need to know and do. In M. Mentkowski, P.F. Wimmers (Eds.), Assessing Competence in Professional Performance across Disciplines and Professions (1st ed., pp. 355–374). Springer Cham. https://doi.org/10.1007/978-3-319-30064-1
Thomas, P. A., Kern, D. E., Hughes, M. T., & Chen, B. Y. (2015). Curriculum development for medical education : A six-step approach. John Hopkins University Press. https://jhu.pure.elsevier.com/en/publications/curriculum-development-for-medical-education-a-six-step-approach
Vollenbroek, W. B. (2019). Communities of Practice: Beyond the Hype – Analysing the Developments in Communities of Practice at Work [Doctoral dissertation, University of Twente]. https://doi.org/10.3990/1.9789036548205
Williams, R. G., Klamen, D. A., & McGaghie, W. C. (2003). SPECIAL ARTICLE: Cognitive, social and environmental sources of bias in clinical performance ratings. Teaching and Learning in Medicine, 15(4), 270–292. https://doi.org/10.1207/S15328015TLM1504_11
*Shairil Rahayu Ruslan
50604, Kuala Lumpur,
Malaysia
03-79492052 / 012-3291074
Email: shairilrahayu@gmail.com, shairil@ummc.edu.my
Submitted: 23 August 2022
Accepted: 3 January 2023
Published online: 4 July, TAPS 2023, 8(3), 15-25
https://doi.org/10.29060/TAPS.2023-8-3/OA2871
Iroro Enameguolo Yarhere1, Tudor Chinnah2 & Uche Chineze3
1Department of Paediatrics, College of Health Sciences, University of Port Harcourt, Nigeria; 2Department of Anatomy, University of Exeter, United Kingdom; 3Department of Education and Curriculum studies, University of Port Harcourt, Nigeria
Abstract
Introduction: This study aimed to compare the paediatric endocrinology curriculum across Southern Nigeria medical schools, using reports from learners. It also checked the learners’ perceptions about different learning patterns and competency in some expected core skills.
Methods: This mixed (quantitative and qualitative) study was conducted with 7 medical schools in Southern Nigeria. A multi-staged randomized selection of schools and respondents, was adopted for a focus group discussion (FGD), and the information derived was used to develop a semi-structured questionnaire, which 314 doctors submitted. The FGD discussed rotation patterns, completion rates of topics and perceptions for some skills. These themes were included in the forms for general survey, and Likert scale was used to assess competency in skills. Data generated was analysed using statistical package for social sciences, SPSS 24, and p values < 0.05 were considered significant
Results: Lectures and topics had various completion rates, 42.6% – 98%, highest being “diabetes mellitus”. Endocrinology rotation was completed by 58.6% of respondents, and 58 – 78 % perceived competency in growth measurement and charting. Significantly more learners, 46.6% who had staggered posting got correct matching of Tanner staging, versus learners who had block posting, 33.3%, p = 0.018.
Conclusion: Respondents reported high variability in the implementation of the recommended guidelines for paediatric endocrinology curriculum between schools in Southern Nigeria. Variabilities were in the courses’ completion, learners’ skills exposure and how much hands-on were allowed in various skills acquisitions. This variability will hamper the core objectives of human capital development should the trend continue.
Keywords: Paediatric Endocrinology Curriculum, Perception, Compliance, Completion Rate, Learners
Practice Highlights
- Medical and dental council of Nigeria has a recommended benchmark for minimum academic standards in all medical schools to which total compliance is expected.
- Evaluation of paediatric endocrinology curriculum content and training methods was conducted using reports from learners.
- Variability in the content, and training methods of the intended competency were reported across medical schools.
- Compliance rate of the recommended curriculum was less than 50% in some contents and some learners reported low skill performance training.
- The lack of uniformity can prevent achievement of the overarching objective of the curriculum in Nigeria with wide variations in competence among graduating doctors.
I. INTRODUCTION
The primary aim of the Medical and Dental council of Nigeria (MDCN) undergraduate curriculum is “to train doctors and dentists who can work effectively in a health team to provide comprehensive health care to individuals in any community in the nation, and keep up to date on issues of global health” (Federal Ministry of Health of Nigeria, 2012). In Nigeria today, there are 49 federal, 59 states and 111 private universities, and 44 of these have full or partially accredited medical schools and while these schools have a prescribed curriculum, some are not following explicitly (Federal Ministry of Health of Nigeria, 2012). This curriculum advocates for universities to develop syllabus to meet the benchmark for minimum academic standards (BMAS) across schools, however there is no uniform template developed for assessing graduates to know how their competence converge as is applicable in United States of America (USA), Canada and United Kingdom (UK) (Santen et al., 2019; Shah et al., 2020; Sosna et al., 2021). Diabetes mellitus, thyroid disorders, puberty, rickets and growth abnormalities are topics included in the MDCN paediatric curriculum under endocrinology which learners are expected to acquire competence in cognitive and psychomotor skills to diagnose and treat or refer appropriately children presenting with these diseases.
A. Problem
Most deaths from diseases in Nigeria and other resource-limited countries are consequent upon general public ignorance of disease, late presentation to the health care systems, poverty and lack of funds to access healthcare facilities and reduced knowledge of some disease patterns by the healthcare providers (Yarhere & Nte, 2018). Addressing the gaps in reduced knowledge can be done by developing competency-based curriculum for all graduating doctors to have as near-similar competence as possible but achieving this may not be feasible. Training activities are not uniform throughout medical schools in Nigeria and elsewhere, and depend on schools’ vision, mission and objectives, and the structures and processes put in place. There are barriers to positive implementation across schools including but not limited to individual school’s determination of what is relevant in the curriculum, access to the materials needed to teach the curriculum content and getting trainers to use these curriculums (Polikoff, 2018). The lack of uniformity of curriculum across universities may not be contending issues, but when the graduating doctors have varying degree of competencies in skills and cognition, then a template for imparting uniform and up to date knowledge and to evaluate this is needed to find ways of reducing the variability (McManus, 2003; McManus et al., 2020; Rimmer, 2014).
The curriculum uniformity across schools is one way of improving competency and thus, healthcare standards, and there is need to explore this uniformity or diversity within the paediatric undergraduate training. In some countries, there is a uniform board certification examination before doctors can practice and this is also done for doctors immigrating into these countries (Hohmann & Tetsworth, 2018; Puri et al., 2021; Tiffin et al., 2017; van Zanten et al., 2022) but Nigeria is exempt from this uniform exit examination. This uniform exit board examination makes these schools align course contents, and therefore reduces the variabilities between medical schools and undergraduate training.
B. Curriculum Evaluation for Change or Improvement
Curriculum evaluation is a means by which educators understand whether the curriculum used to train learners is working as intended, and whether there is need to change the entire programme or redesign aspects (Burton & McDonald, 2001; Ornstein & Hunkins, 2009). It is also a way of identifying deficiencies in training syllabus across universities, (Rufai et al., 2016) or whether compliance to a curriculum is being achieved (Grant, 2014; Olson et al., 2000). Kirkpatrick’s curriculum evaluation method is widely acceptable in medical education using the 4 steps; learners’ reaction or satisfaction, knowledge, behavioural changes and results or impact, and in Nigeria, for paediatric endocrinology, this has not been done (Alsalamah, 2021; Bates, 2004).
Universities have variabilities in organisation, students’ numbers in classes, duration of specific posting, posting types and whether the courses are elective or core. In medical schools in Nigeria, paediatric postings are undertaken in the 5th or 6th year of a 6-year programme. While some stagger the posting to be done within the last 2 years, others do theirs in the 5th or the 6th year exclusively, and the extent of these variabilities and how they affect the training processes and products has not been evaluated in Nigeria and this can be done using learners’ or graduates’ perceptions.
The aim of this research was to evaluate learners’ report and perception of some aspects of the paediatric endocrinology curriculum contents and learning methods across Southern Nigeria medical schools. Endocrinology was taken from the paediatric course to reduce the volume of information to be analysed.
II. METHODS
This was a cross sectional study design with qualitative and quantitative data analyses, evaluating learners’ report and their perception of the curriculum being used by various medical schools in Southern Nigeria to deliver the MDCN paediatric endocrinology curriculum. Survey was conducted across 10 medical schools in Southern Nigeria that have learners who have either completed their final year, or are doing their internship. Two steps were used to retrieve the information needed; a focus group discussion of sampled learners, and a questionnaire survey sent out to randomly selected respondents and these 2 methods complemented each other. The focus group discussion was used to explore in depth, the minds of the respondents and what they perceived was being done well and what needed to be changed in the syllabus in their respective schools. The questionnaire survey was then used to collect reports and perceptions from a wider set of learners who had completed their paediatric posting within the past 6 – 12 months. Some of these were already doing their internship and others were in their final year in preparation for their final examinations.
Sample size for respondents will be calculated using the formula:
N = (Z score)2 x SD x (1 – SD)
(CI)2
Z score = 1.96, SD (standard deviation of the mean) = estimated at ± 0.5, Confidence interval = 0.05
= 384 respondents, with an attrition rate of 10% will be added 10% of 384 = 38
384 + 38 = 422 respondents.
A. Sampling Technique
Multi-staged sampling technique was used to determine the schools, and respondents that participated in the study. There are 29 Southern Universities with medical / health colleges and 16 of these had more than 50 learners in their final year or had graduated. Ten schools were randomly selected using the excel formula [= rand ()], and a proportionate stratified sampling was done using the matriculation numbers of the students in each school to arrive at 422 respondents. Total number of learners that studied paediatrics in various institutions was 800; Ibadan 150, Port Harcourt, 128, Lagos 128, Niger delta University 69, UNN Enugu 128, University of Benin 128, Others 69. From the total number of learners in each school, selected learners and interns were sent the questionnaire using their email addresses. Selection for the FGD was done using simple random sampling from each school and these were sent separate emails with details for the meeting.
B. Focus Group Discussions Process
Focus group discussion was conducted with the respondents using zoom video platform, and the process lasted for 2 hours, 30 minutes. Ten learners’ representatives from the selected schools were contacted for this FGD, however, 7 (70%) agreed to participate after several email reminders. The interview was semi-structured with a flexible topic guide, which covered issues relating to the respondents’ views and opinions on the curriculum in paediatric endocrinology; description of posting type in each school, whether block, or staggered, topics received and/or completed, perception of their competence in a key psychomotor skill. The focus group interview discussions were recorded in the zoom meeting platform and transcribed verbatim. The data were analysed using the thematic framework content analyses method. The themes generated were categorised into; 1. Lecture contents and completion rate, 2. Types of paediatric rotation and posting, 3. Skill competence acquisition and clinical postings. Their perceptions about these themes were also sought and discussed. The transcription of the groups’ discussions was reviewed by IY and TC to help categorise the data and pull-out important quotes used.
C. Questionnaire Survey
Following thematic analyses of the FGD, the themes generated were converted to questions in a survey for a larger sample population. Themes generated were the type of paediatric posting, rotations through units in the departments and paediatric endocrinology topics, training methods and competency acquired. Demographic characteristics of responders such as level/year of study, age, gender and university of study were collected. The respondents were also asked to select topics from a poll, included in their paediatric endocrinology syllabus, with result in Figure 1, and to state the various methods used to learn growth and growth disorders in their schools. A means of assessing cognitive (recall) skills of the learners was conducted using animated pictures of Tanner staging and matching-type multiple choice, and the responses were crossmatched with the type of posting learners were exposed to, i.e. block posting or staggered posting. Tanner staging was chosen as it cuts across general paediatrics and endocrinology as part of growth and puberty (endocrinology).
Data retrieved were analysed statistically by using chi-square test, and Pearson correlation for categorical variables. The level of competence perceived by learners in height measurement and charting on growth chart was retrieved using 5-point Likert scale (where 1 = not competent; 2 = low competence; 3 = neutral; 4 = competent; and 5 = proficient). The association between level of competence and whether learners rotated through paediatric endocrinology was checked using Pearson’s correlation test. For all statistics, p value < 0.05 was considered significant.
D. Ethics
The research commenced after the Research Ethics committee of the University of Port Harcourt granted approval (UPH/CEREMAD/REC/MM80/056). Verbal informed consent was obtained from the participants during the focus group discussion, who also gave consent for video and recording of the process. Informed consent was also obtained from all participants who filled and submitted the online survey. The focus group discussants received N3,000 ($10) for internet data only as monetary compensation.
III. RESULTS
There were 314 learners from the 422 calculated sample size, responded to the questionnaire survey, giving a response rate of 74.4%. There were more final year respondents than early career doctors and more of the respondents were in the age bracket 20 – 24 years, with a mean of 25.02 ±2.71 years. The male: female ratio was 1:1.01, and the data that support the findings of this study are available in Figshare at https://doi.org/10.6084 /m9.figshare.20730937.v1 (Yarhere et al., 2022).
|
RESPONDENTS |
Frequency |
Percentage |
|
|
Year of study |
|
|
|
|
Early career doctor (graduate/intern) |
130 |
41.4 |
p = 0.002 |
|
Final year |
184 |
58.6 |
|
|
University attended (calculated cohort) |
|
|
|
|
University of Port Harcourt (63) |
62 |
19.7 |
|
|
Niger Delta University (54) |
54 |
17.2 |
|
|
University of Ibadan (76) |
50 |
15.9 |
|
|
University of Benin (65) |
44 |
14.0 |
|
|
University of Lagos (65) |
40 |
12.7 |
|
|
University of Nigeria (65) |
42 |
13.4 |
|
|
Other western Universities (34) |
22 |
7.0 |
|
|
Age |
|
|
|
|
20-24 |
140 |
44.6 |
|
|
25-29 |
162 |
51.6 |
|
|
>=30 |
12 |
3.8 |
|
|
Mean |
25.02 ± 2.71 |
|
|
|
Gender |
|
|
|
|
Male |
152 |
48.4 |
p = 0.612 |
|
Female |
162 |
51.6 |
|
Table 1. Demographic characteristics of all respondents and the universities attended
A. Evaluating Contents of Lecture Topics and Completion of Lectures
The syllabus lecturers use to teach courses are supposed to be descriptive with all learning outcomes stated in the handbook or in the log books given to them before the start of the academic year. The prescribed topics for paediatric endocrinology as stated below were not completely taught to learners or learners did not attend the lectures. In the discussion, some agreed that they did not have the full complement of lectures suggested by the BMAS. One respondent said she and her group mates did not receive diabetes mellitus lectures in their final paediatric posting. This fact was corroborated in the questionnaire survey as 2% of the respondents revealed not having diabetes mellitus lectures, and more than 40% did not learn genetics in their paediatric endocrinology training as shown in Figure 1.
Diabetes had almost 100% lecture recipient while genetic had the least. In some schools, genetics were placed under endocrine disorders while in others, genetics were left for the pathology and basic medicine classes.
“I was taught, I personally received 4 lectures in Paed Endo including ambiguous genitalia, “CAH” congenital adrenal hyperplasia, hypothyroidism, and puberty.”
Participant 3
“So, you did not get to do calcium and rickets?”
Facilitator
“No, I was not taught calcium and rickets.”
Participant 3
“What about growth and short stature?”
Facilitator
“Yes, I received introductory lectures in my young (sic), junior posting, yes I did in my 400 level, but not in my senior posting and it was not part of endocrinology but general paediatrics.”
Participant 3
“I did not take lectures in diabetes mellitus because it was rescheduled several times until we finally had to sit for our exams. In the end, many of us just took notes from our seniors and other students who had theirs when it was scheduled.”
Participant 2
“Why were the classes rescheduled? I mean what did the lecturer tell you?”
Facilitator
“The lecturer kept traveling or was indisposed most of our time in the senior posting.”
Participant 2
Participant 4 shared:
Dr. xxxxxx taught us diabetes mellitus and the topic was quite extensive. We learnt the different types, pathophysiology, aetiology, DKA, precipitating factors, risk factors, management. Our lecturers even made us do presentations on DKA, we monitored patients that were being managed for DKA, checking their urine samples for ketones, glucose and their blood pressure.
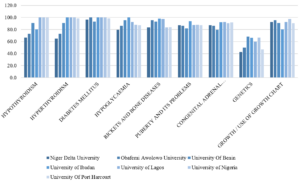
Figure 1: Percentage of learners in various schools who received/attended specific endocrinology lectures in their universities
B. Types of Paediatric Posting and Rotation and Perception of Learners Relating to Task Completion
There were basically 2 modes of paediatric posting in the institutions sampled; 4-months block posting where respondents have a month of didactic lectures and 3 months of clinical rotations through various units in the Paediatric departments, and 4 months of staggered rotations with junior and senior postings in the clinical classes. While some learners rotated through all the units (core and electives) in the departments, some went through core units, emergency and neonatal units, and 2 other units randomly selected for the respondents by the departments.
C. Learners’ Responses to Rotation through Paediatrics and Posting Types
Participant 2 shared:
The way it works in University of xxxx, we rotate through 2 elective postings with core (CHEW and SCBU) postings in the junior and senior postings. These elective postings are randomly selected by the department (meaning heads or coordinators). I did neurology and gastroenterology in my junior posting and haemato-oncology and I really can’t remember the other one in my senior posting.
“Will I be wrong to say you did not see a patient with Diabetic keto acidosis?”
Facilitator
“I saw a child with diabetic keto acidosis in the ward but it wasn’t my unit managing the patient. I only went to the ward to do some other thing.”
Participant 2
“If you were given the opportunity to design a curriculum or programme for your university, will you prefer what is being practiced now, or will you rather have every student go through every unit and get titbits from each unit?”
Facilitator
Participant 2 responded:
Yes, I will prefer that situation where you get to be exposed to every unit in the department but …. emmm, that creates a problem because you may be in a unit for a week, and no patient comes in but the next group rotating to the unit gets to see many patients. I would want to suggest that perhaps, instead of focusing on more of clinical posting, that a unified tutorial class which will expose everyone to the core diseases in the various disciplines.
Table 2 corroborates the information given by the focus group discussants. Testing the competency outcome in either method can give some estimated guess as to which is better, however, there are several confounding factors that will not allow fair comparison (See Table 3).
|
Variable |
Frequency |
Percent (%) |
|
|
Paediatric posting in your university |
|
|
|
|
Staggered posting into Junior and senior paediatrics |
176 |
56.1 |
c2 = 4.59, |
|
Block posting of 4 months total |
138 |
43.9 |
p = 0.032 |
|
Paediatric rotations through various units in universities |
|
|
|
|
I rotated through all units in the department |
162 |
51.6 |
c2 = 0.318, |
|
I rotated through CHEW, neonatal unit, and 2/3 other units |
152 |
48.4 |
p = 0.573 |
|
Rotate through paediatric endocrinology unit in your university |
|
|
|
|
Yes |
184 |
58.6 |
c2 = 7.48, |
|
No |
130 |
41.4 |
p = 0.006 |
Table 2. Paediatric posting and unit rotations in the departments (n=314)
Though there were differences in the mode of paediatric postings where staggered or block, c2 = 4.59, p = 0.032. the difference in proportion of respondents who had core and selected elective posting as against all units posting was not significant, c2 = 0.318, p = 0.573.
|
|
Block posting of 4 months |
Staggered junior and senior paediatrics |
|
|
Correct |
Count |
46 |
82 |
|
% within paediatric posting |
33.3% |
46.6% |
|
|
% of Total |
14.6% |
26.1% |
|
|
Wrong |
Count |
92 |
94 |
|
% within paediatric posting |
66.7% |
53.4% |
|
|
% of Total |
29.3% |
29.9% |
|
|
Total |
Count |
138 |
176 |
|
% within correct response |
43.9% |
56.1% |
|
|
% of Total |
43.9% |
56.1% |
|
Table 3: Comparing correct response to animated picture of Tanner stage (pubic hair) in females, and the type of paediatric rotation learners were exposed to
In the 2×2 table above where recall was tested in the learners based on their paediatric posting type, higher percentage of those who had staggered posting got the correct matching of Tanner stage, and the difference was significant, c2 = 5.630, p = 0.018. However, the total number of respondents with the correct response was low.
D. Perception of Core Competency Skill in Growth Measurement and Charting by Learners
One of the most important courses in paediatrics is growth and development and training future medical doctor to acquire skills and competence in growth and management is a key component of the BMAS. While growth measurement may seem easy to the uninformed, the whole task is daunting especially in children with complex growth abnormalities and malformation, and for more complex skills like arm span. Which of the more complex skills should the learner be expected to be competent in, will be debated in an expert forum of trainers.
“So, did you do anthropometric measures?”
Facilitator
Participant 1 shared:
Yes, anytime we clerk a patient, we must check the weight and height and interpret using age-appropriate charts, but we did not plot them in the charts. We carry the age-appropriate chart and interpreted our patients, as this is a requirement.
Using the chart may not be emphasised by all paediatric lecturers, so learners can be smart to know those lecturers who will request this skill from them during the clerkship period or the unit rotations.
“We did not quite get the concept of mid parental height, height percentile, it was just mentioned in passing. I never saw a severely short child that needed growth hormone. I was only told by a classmate of mine.”
Participant 3
The charting and interpretation of weight and height measurements of children was not done in all schools as shown in Table 4 below, which tells that only 65.8% of total respondents were taught interpretation of measured and charted growth parameters. The level of competence in these tasks will also be varied as seen in Appendix 1. Two hundred and thirty-eight (75.8%) learners perceived they had competency/ proficiency in height measures using stadiometer, and 44.6 % of the learners with these perceptions actually had paediatric endocrinology clinical rotation (Appendix 1).
|
Variable |
Frequency n = 314 |
Percent (%) |
|
How was growth and growth disorders taught in your school (Multiple response applicable) |
|
|
|
Didactic lectures |
272 |
86.6 |
|
Measurement of children using standardised stadiometer |
230 |
73.2 |
|
Charting of growth measurements in CDC/WHO growth charts |
203 |
64.6 |
|
Measurement of children using improvised height rules |
157 |
50.0 |
|
Interpretation of measured and charted growth parameters |
203 |
64.6 |
|
Ward clerkship and presentation |
230 |
73.2 |
|
Measurements of children using bathroom spring balance |
140 |
44.6 |
|
Use of bone age X radiographs |
78 |
24.8 |
|
Use of orchidometer |
90 |
28.6 |
Table 4: Methods used to teach growth and growth disorders in various institutions
Bone age and orchidometers are used to assess skeletal maturation and puberty, which are advanced for the undergraduate learners and certainly not compulsory, but some respondents were taught with the tools showing the variabilities in contents and skills delivery between these schools. From Table 4 above, framers of the syllabus for endocrinology aspect of paediatrics curriculum are unlikely to include use of orchidometer and bone age during the undergraduate paediatric endocrinology rotation as the skill is complex, and not necessary for their level of development.
IV. DISCUSSION
This study has highlighted differences in course contents and training methods across medical schools in Southern Nigeria. While many schools have used the BMAS prescribed by the MDCN, the syllabus used are different and the intended learning outcomes are diverse based on the respondents’ reports. Some learners reported not having diabetes lectures in their school through no fault of theirs, as lecturer rescheduled the lectures and never gave them. While learners have the responsibility to attend lectures, trainers are also obligated to be present at their scheduled lectures or transfer this to their teacher-assistants, or use technologies (Grant, 2014; Ruiz et al., 2006). Some learners had little participation in the Emergency Room, others participated fully in DKA management, learning empathy, specialised skills and communication. The intended competencies to be acquired can be achieved through shadowing and participation, bed-side teaching, and tutorial to improve the cognitive and psychomotor skill, and these opportunities must be created for them in experiential settings (Ryan et al., 2020; Shah et al., 2020).
More learners had staggered postings, going through junior and senior paediatric postings in what may be considered as integrated learning departing from the traditional method (Patel et al., 2005; Watmough et al., 2006, 2009). In the staggered posting type of rotation, we noticed that not all learners went through paediatric endocrinology unit posting, and like one of the discussants said, they would rather everyone went through each unit getting bits of everything and having opportunity to study specific and prevalent diseases in paediatric units rather than leaving them with the possibility of not learning important disorders. As it is not always possible to encounter specific diseases like DKA during entire posting in the schools that use staggered posting types, the likelihood of exposure was higher in schools that had block posting from the FGD conducted, but this did not translate to better retention of skills or cognitions as depicted in the Tanner staging matching question.
Having learners train in all special postings may not be the best approach in undergraduate medicine because the specialised skills may not be utilised in general practice and even in general paediatrics should the learners plan paediatric specialisation (Bindal et al., 2011). While some trainers may argue that all information and skill should be taught to the learners, the time to acquire and achieve mastery may be short for the learners (Jensen et al., 2018; Offiah et al., 2019). This study can be referenced in curriculum designing and implementation so the framers understand what society needs should be filled at any time. The concept of cognitive overload has actually reduced the duration of core specialty in clinical medicine while increasing the duration for others with emphasis on psychomotor, affective skills and professionalism. Some medical schools have core paediatric posting of 7 – 8 weeks, but Nigeria is still fixed with the traditional 3 – 4 months. In some schools in South Africa, the clinical posting is run as modular block for 3 years, with paediatric curriculum running from year 4 through year 6 (Dudley & Rohwer, 2015). With the long duration in the Nigeria curriculum, skills competencies are still deficient, so there is need to revamp the curriculum to make it more competency driven. It is excusable that more sophisticated competence like use of orchidometer were not known by more than half the learners, but if some were taught, the level of confidence in these skills at this stage of their learning should also be assessed as was done for diabetes by George et al. (2008).
Medical schools in Nigeria and other countries will have to continually evolve and produce curricula that are competency based, using problem-based learning, simulations, mannikin training for skills as is done in other countries (Watmough et al., 2006). Diabetes, thyroid, ambiguous genitalia with congenital adrenal hyperplasia, short stature and calcium disorders are common in Nigeria and should be taught in structured and integrated formats. Integrated curriculum where skills are graded from simple to complex can also be tested e g, skills of height measurements and charting using the stadiometer and growth charts can be taught in the 1st clinical year, and then the mid parental heights, target height calculation and bone age may be taught in the 2nd and 3rd clinical years. (Brauer & Ferguson, 2015; Grant, 2014).
A. Strength of the Research
Articulating the perceptions of learners is not always easy as they are varied and subjective, but getting them to come together, discuss and give suggestions on how curriculum can be designed and achieved increases the strength of this research. There was no sense of victimisation of the learners as many had already graduated from their schools, and the discussants admitted to not missing classes, or clinical learning. They spoke freely, with courtesy to others and there was little or no argument among them.
B. Limitations of the Research
As this research is based on past experiences of the cognitive and psychomotor skills achieved during the learners’ training period, the possibility of recall bias is high, and respondents may underestimate or exaggerate their skills. Using respondents who had just concluded their paediatric postings was an attempt at reducing this limitation. The best time to evaluate a programme is usually soon after the programme has been concluded however, as there has been no report of this type of evaluation, there was need to embark on it and make recommendations.
V. CONCLUSION
Respondents reported high variability in the implementation of the recommended guidelines for paediatric endocrinology curriculum between schools in Southern Nigeria. Variabilities were in the courses’ completion, learners’ skills exposure and how much hands-on were allowed in various skills acquisitions. This variability will hamper the core objectives of human capital development should the trend continue.
A. Area of Future Research
Noting the differences exist between schools, curriculum strategists and implementation teams in universities should commission a DELPHI study by experts, where core competencies and objectives for paediatric endocrinology will be agreed on and sent to the regulatory bodies for endorsement and implementation.
Notes on Contributors
IY conceived, designed, planned, executed and conducted interviews and the research. He also collected the data, analysed it and wrote the manuscript.
TC helped in designing the methodology for the data colllection and analyses, and reviewed the manuscript.
CU gave critical appraisal of the manuscript and all authors have approved the final manuscript.
Ethical Approval
The research ethics committee of the Univeristy of Port Harcourt gave ethical approval before the start of the study with the number: UPH/CEREMAD/REC/MM80/056.
Data Availability
The data supporting this research is available for publication purposes, without editing. Data can be shared only with express permission from the corresponding author as deposited in Figshare repository, using the private url:
https://figshare.com/articles/dataset/Copy_of_CURRICULUM_STUDENTS_xls/21154396
Acknowledgement
We acknowledge the early career doctors and final year students who participated in the online survey especially the selected ones who took part in the focus group discussion.
Declaration of Interest
Authors declare that there are no conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest.
Funding
There was no funding for this survey.
References
Alsalamah, A., & Callinan, C. (2021). Adaptation of Kirkpatrick’s four level model of training criteria to evaluate training programmes for head teachers. Education Science, 11(116), 1-25. https://doi.org/10.3390/educsci11030116
Bates, R. (2004). A critical analysis of evaluation practice: The Kirkpatrick model and the principle of beneficence. Evaluation and Program Planning, 27, 341-347. https://doi.org/10.1016/j.evalprogplan.2004.04.011
Bindal, T., Wall, D., & Goodyear, H. M. (2011). Medical students’ views on selecting paediatrics as a career choice. European Journal of Pediatrics, 170(9), 1193-1199. https://doi.org/10.1007/s00431-011-1467-9
Brauer, D. G., & Ferguson, K. J. (2015). The integrated curriculum in medical education: AMEE Guide No. 96. Medical Teacher, 37(4), 312-322. https://doi.org/10.3109/0142159X.2014.970998
Burton, J. L., & McDonald, S. (2001). Curriculum or syllabus: Which are we reforming? Medical Teacher, 23(2), 187-191. https://doi.org/10.1080/01421590020031110
Dudley, L. D., Young, T. N., Rohwer, A. C., Willems, B., Dramowski, A., Goliath, C., Mukinda, F. K., Marais, F., Mehtar, S., & Cameron, N. A. (2015). Fit for purpose? A review of a medical curriculum and its contribution to strengthening health systems in South Africa. African Journal Health Profession Education, 7(1), 81-84. https://doi.org/10.7196/AJHPE.512
Federal Ministry of Health of Nigeria, Health Systems 20/20Project. (2012). Nigeria undergraduate medical and dental curriculum template. Health systems 20/20 Project, Abt Associates Inc.
George, J. T., Warriner, D. A., Anthony, J., Rozario, K. S., Xavier, S., Jude, E. B., & Mckay, G. A. (2008). Training tomorrow’s doctors in diabetes: Self-reported confidence levels, practice and perceived training needs of post-graduate trainee doctors in the UK. A multi-centre survey. BMC Medical Education, 8, Article 22. https://doi.org/10.1186/1472-6920-8-22
Grant, J. (2014). Principles of curriculum design. In T. Swanwick, K. Forrest, B. C. O’Brien (Eds.), Understanding medical education evidence, theory and practice Sussex, UK: Wiley Blackwell, 31-46.
Hohmann, E., & Tetsworth, K. (2018). Fellowship exit examination in orthopaedic surgery in the commonwealth countries of Australia, UK, South Africa and Canada. Are they comparable and equivalent? A perspective on the requirements for medical migration. Medical Education Online, 23(1), Article 1537429. https://doi.org/10.1080/10872981.2018.1537429
Jensen, J. K., Dyre, L., Jørgensen, M. E., Andreasen, L. A., & Tolsgaard, M. G. (2018). Simulation-based point-of-care ultrasound training: a matter of competency rather than volume. Acta Anaesthesiology Scandanavia, 62(6), 811-819. https://doi.org/10.1111/aas.13083
McManus, I. C. (2003). Medical school differences: beneficial diversity or harmful deviations. BMJ Quality and Safety in Health Care, 12(5), 324-325. https://doi.org/10.1136/qhc.12.5.324
McManus, I. C., Harborne, A. C., Horsfall, H. L., Joseph, T., Smith, D. T., Marshall-Andon, T., Samuels, R., Kearsley, J. W., Abbas, N., Baig, H., Beecham, J., Benons, N., Caird, C., Clark, R., Cope, T., Coultas, J., Debenham, L., Douglas, S., Eldridge, J., . . . Devine, O. P. (2020). Exploring UK medical school differences: the MedDifs study of selection, teaching, student and F1 perceptions, postgraduate outcomes and fitness to practise. BMC Medicine, 18(1), Article 136. https://doi.org/10.1186/s12916-020-01572-3
Offiah, G., Ekpotu, L. P., Murphy, S., Kane, D., Gordon, A., O’Sullivan, M., Sharifuddin, S. F., Hill, A. D. K., & Condron, C. M. (2019). Evaluation of medical student retention of clinical skills following simulation training. BMC Medical Education, 19(1), Article 263. https://doi.org/10.1186/s12909-019-1663-2
Olson, A. L., Woodhead, J., Bekow, R., Kaufman, N., & Marshal, S. (2000). A national general pediatric clerkship curriculum: The process of development and implementation. Pediatrics, 160(S1), 216 -222. https://doi.org/10.1542/peds.106.S1.216
Ornstein A, H. F., & Hunkins, F. P. (2009). Curriculum: Foundations, principles and issues (5th Ed.). Pearson.
Patel, V. L., Arocha, J. F., Chaudhari, S., Karlin, D. R., & Briedis, D. J. (2005). Knowledge integration and reasoning as a function of instruction in a hybrid medical curriculum. Journal of Dental Education, 69(11), 1186-1211. https://www.ncbi.nlm.nih.gov/pubmed/16275683
Polikoff, M. S. (2018). The challenges of curriculum materials as a reform lever Evidence Speaks Reports, 2, 58
Puri, N., McCarthy, M., & Miller, B. (2021). Validity and reliability of pre-matriculation and institutional assessments in predicting USMLE STEP 1 success: Lessons from a traditional 2 x 2 curricular model. Frontiers in Medicine (Lausanne), 8, Article 798876. https://doi.org/10.3389/fmed.2021.798876
Rimmer, A. (2014). GMC will develop single exam for all medical graduates wishing to practise in UK. BMJ, 349, g5896. https://doi.org/10.1136/bmj.g5896
Rufai, S. R., Holland, L. C., Dimovska, E. O., Bing Chuo, C., Tilley, S., & Ellis, H. (2016). A national survey of undergraduate suture and local anesthetic training in the United Kingdom. Journal of Surgical Education, 73(2), 181-184. https://doi.org/10.1016/j.jsurg.2015.09.017
Ruiz, J. G., Mintzer, M. J., & Leipzig, R. M. (2006). The impact of E-learning in medical education. Academic Medicine, 81(3), 207-212. https://doi.org/10.1097/00001888-200603000-00002
Ryan, A., Hatala, R., Brydges, R., & Molloy, E. (2020). Learning with patients, students, and peers: Continuing professional development in the solo practitioner workplace. Journal of Continuing Education in the Health Profession, 40(4), 283-288. https://doi.org/10.1097/CEH.0000000000000307
Santen, S. A., Feldman, M., Weir, S., Blondino, C., Rawls, M., & DiGiovanni, S. (2019). Developing comprehensive strategies to evaluate medical school curricula. Medical Science Educator, 29(1), 291-298. https://doi.org/10.1007/s40670-018-00640-x
Shah, S., McCann, M., & Yu, C. (2020). Developing a national competency-based diabetes curriculum in undergraduate medical education: A Delphi study. Canadian Journal of Diabetes, 44(1), 30-36. https://doi.org/10.1016/j.jcjd.2019.04.019
Sosna, J., Pyatigorskaya, N., Krestin, G., Denton, E., Stanislav, K., Morozov, S., Kumamaru, K. K., Jankharia, B., Mildenberger, P., Forster, B., Schouman-Clayes, E., Bradey, A., Akata, D., Brkljacic, B., Grassi, R., Plako, A., Papanagiotou, H., Maksimović, R., & Lexa, F. (2021). International survey on residency programs in radiology: similarities and differences among 17 countries. Clinical Imaging, 79, 230-234. https://doi.org/10.1016/j.clinimag.2021.05.011
Tiffin, P. A., Paton, L. W., Mwandigha, L. M., McLachlan, J. C., & Illing, J. (2017). Predicting fitness to practise events in international medical graduates who registered as UK doctors via the Professional and Linguistic Assessments Board (PLAB) system: a national cohort study. BMC Medicine, 15(1), Article 66. https://doi.org/10.1186/s12916-017-0829-1
van Zanten, M., Boulet, J. R., & Shiffer, C. D. (2022). Making the grade: licensing examination performance by medical school accreditation status. BMC Medical Education, 22(1), Article 36. https://doi.org/10.1186/s12909-022-03101-7
Watmough, S., Garden, A., & Taylor, D. (2006). Does a new integrated PBL curriculum with specific communication skills classes produce Pre Registration House Officers (PRHOs) with improved communication skills. Medical Teachers, 28(3), 264-269. https://doi.org/10.1080/01421590600605173
Watmough, S., O’Sullivan, H., & Taylor, D. (2009). Graduates from a traditional medical curriculum evaluate the effectiveness of their medical curriculum through interviews. BMC Medical Education, 9, Article 64. https://doi.org/10.1186/1472-6920-9-64
Yarhere, I., Chinnah, T., & Uche, C. (2022). Learners’ report and perception of differences in undergraduate paediatric endocrinology curriculum content and delivery across Southern Nigeria. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.20730937.v1
Yarhere, I. E., & Nte, A. R. (2018) A ten-year review of all cause paediatric mortality in University of Port Harcourt Teaching Hospital, Nigeria (2006–2015). Nigerian Journal of Paediatrics, 45(4), 185-91.
*Iroro Enameguolo Yarhere
East/West Road,
PMB 5323 Choba,
Rivers State, Nigeria
+2347067987148
Email: iroro.yarhere@uniport.edu.ng
Submitted: 16 May 2022
Accepted: 3 January 2023
Published online: 4 July, TAPS 2023, 8(3), 5-14
https://doi.org/10.29060/TAPS.2023-8-3/OA2813
Bikramjit Pal1, Aung Win Thein2, Sook Vui Chong3, Ava Gwak Mui Tay4, Htoo Htoo Kyaw Soe5 & Sudipta Pal6
1Department of Surgery, Manipal University College Malaysia, Melaka, Malaysia; 2Department of Surgery, Manipal University College Malaysia, Melaka, Malaysia; 3Department of Medicine, Manipal University College Malaysia, Melaka, Malaysia; 4Department of Surgery, Manipal University College Malaysia, Melaka, Malaysia; 5Department of Community Medicine, Manipal University College Malaysia, Melaka, Malaysia; 6Department of Community Medicine, Manipal University College Malaysia, Melaka, Malaysia
Abstract
Introduction: The practice of high-fidelity simulation-based medical education has become a popular small-group teaching modality across all spheres of clinical medicine. High-fidelity simulation (HFS) is now being increasingly used in the context of undergraduate medical education, but its superiority over traditional teaching methods is still not established. The main objective of this study was to analyse the effectiveness of HFS-based teaching over video-assisted lecture (VAL)-based teaching in the enhancement of knowledge for the management of tension pneumothorax among undergraduate medical students.
Methods: A cohort of 111 final-year undergraduate medical students were randomised for this study. The efficacy of HFS-based teaching (intervention group) and VAL-based teaching (control group), on the acquisition of knowledge, was assessed by single-best answer multiple choice questions (MCQ) tests in the first and eighth week of their surgery posting. Mean and standard deviation (SD) for the total score of MCQ assessments were used as outcome measures. ANCOVA was used to determine the difference in post-test MCQ marks between groups. The intragroup comparison of the pre-test and post-test MCQ scores was done by using paired t-test. The P-value was set at 0.05.
Results: The mean of post-test MCQ scores were significantly higher than the mean of pre-test MCQ scores in both groups. The mean pre-test and post-test MCQ scores in the intervention group were slightly more than those of the control group but not statistically significant.
Conclusion: There was a statistically significant enhancement of knowledge in both groups but the difference in knowledge enhancement between the groups was insignificant.
Keywords: High-Fidelity Simulation, Video-Assisted Lecture, Simulation-Based Medical Education (SBME), Randomized Controlled Trial (RCT), Medical Education, Pre-test and Post-test Knowledge Assessments
Practice Highlights
- An RCT study to evaluate the effectiveness of HFS over video-assisted lecture teaching method.
- HFS seems to be not superior than VAL-based teaching for knowledge acquisition and retention.
- HFS may be used judiciously when the objectives are mainly knowledge based.
- Further research may determine curricular areas where HFS is superior and worth adopting.
I. INTRODUCTION
High-Fidelity Simulation (HFS) is an innovative healthcare education methodology that involves the use of sophisticated life-like mannequins to create a realistic patient environment. HFS can be considered an innovative teaching method that aids students in translating knowledge and psychomotor skills from the classroom to the actual clinical setting. Kolb’s Experiential Learning Cycle (Kolb, 1984) provides a basis for the integration of active learning of simulation with conventional teaching methods for a comprehensive learning experience in undergraduate medical education. HFS-based education is potentially an efficacious pedagogy that is now available for teaching. The usefulness of HFS has been recognized by the Accreditation Council of Graduate Medical Education (Accreditation Council of Graduate Medical Education [ACGME], 2020). HFS has the added benefit of increasing students’ confidence and their ability to care for the patients at the bedside (Kiernan, 2018). HFS-based education and video-assisted lecture-based teaching are both effective in achieving factual learning. Despite the increasing acceptance of HFS, there are limited studies to compare the usefulness of HFS with conventional teaching methods for factual learning among undergraduate medical students. At present, the different research studies have not provided enough evidence to establish HFS-based teaching’s superiority over traditional educational methods in the acquisition and retention of knowledge. There is inconsistent and variable outcome regarding the effectiveness of HFS on student learning (Yang & Liu, 2016). HFS-based education is both time-consuming and resource intensive. Its long-term merits in retaining knowledge and translating it into enhanced patient care need further research. As educators, we need to systematically evaluate the expensive newer teaching-learning modules like HFPS for their effectiveness by using rigorous research methodology and protocols. This is to ensure that we are providing the best learning opportunities conceivable for the students. Previous studies were mostly done in North America and, therefore, the generalisability of these results is guarded and might not be applicable in the context of Europe and Asia due to many differences in academic and curriculum aspects (Davies, 2008). The purpose of this study was to establish the feasibility of the use of HFS to deliver critical care education to final-year medical students and to find its efficacy in the enhancement of knowledge when compared to video-assisted lectures. The study compared the effectiveness of two methods of teaching pedagogy in the enhancement of knowledge acquisition using pre-test and post-test MCQ. This study was designed to provide insights that may be applied to the future development and improvement of HFS-based education among undergraduate medical students and its possibility of integrating it into course curricula.
II. METHODS
A. Study Design
Randomized Controlled Trial (RCT) with parallel groups and 1:1 allocation. Please see Appendix 1 for the Flow Chart.
B. Sample Size
G*Power software was used to calculate the sample size (Faul et al., 2007). Based on the preliminary RCT study of our institute done with the same protocol in 2018, the calculated sample size was 114 with a power of 0.95 for this study.
C. Inclusion and Exclusion Criteria
All male and female final-year undergraduate medical (MBBS) students in our institute were recruited after obtaining their written informed consent. All final-year students in the institute consented to the study. The participants were between the ages of 22-26 years.
The total number of participants recruited was 123.
The number of participants dropped out was 12 (9.77%).
Out of 111 participants who completed the study, 61 (54.95%) were female and 50 (45.05%) were male.
The study was conducted in the Clinical Skills Simulation Lab of Melaka Manipal Medical College (presently known as Manipal University College Malaysia).
The study period was from March 2019 to February 2020 (12 months).
D. Interventions
1) Description of HFPS-based teaching: It was an interactive session using a high-fidelity patient simulator demonstrating the management of tension pneumothorax by performing Needle Decompression on METIman (Pre-Hospital) following the Advanced Trauma Life Support Manual developed by the American College of Surgeons (ATLS Subcommittee et al., 2013).
2) Description of Hi-fidelity simulator: METIman Pre-Hospital HI-Fidelity Simulator (MMP-0418) was used for the simulation sessions. It was a fully wireless, adult High-Fidelity Patient Simulator (HFPS) with modelled physiology. It comes with extensive clinical features and capabilities designed specifically for learners to practice, gain experience, and develop clinical mastery in a wide range of patient care scenarios.
3) Description of video-assisted lecture-based teaching: It was a small group interactive session delivered face-to-face to the participants using a recorded video clip demonstrating the management of tension pneumothorax by performing Needle Decompression on METIman (Pre-Hospital) following the Advanced Trauma Life Support Manual developed by the American College of Surgeons (ATLS Subcommittee et al., 2013).
E. Outcome
The tool for measurement of knowledge was an identical set of single-best answer A-type MCQs. These MCQs were used for both Pre-test and Post-test knowledge assessments. MCQs were constructed based on the teaching sessions to assess their learning outcome.
The efficacy of HFPS-based teaching when compared to video-assisted lecture-based teaching is enhancement of knowledge for management of tension pneumothorax.
F. Recruitment
The students were recruited in the study during their final year surgical posting.
G. Randomisation
A cohort of 12 to 14 students from each rotation was randomised into intervention (HFPS-based teaching) and control (video-assisted lecture-based teaching) groups following random sequence generation method.
A computer-generated random sequence number was developed from randomizer.org. The independent randomiser was a biostatistician who did not participate in the delivery of interventions. The allocated interventions were then sealed in a sequentially numbered, opaque envelope.
Block randomisation with a block size of two was used to assign the students into intervention and control groups.
H. Implementation
A biostatistician generated the allocation sequence. One independent investigator enrolled the participants, and another independent investigator assigned the participants to interventions. The outcome assessor and the biostatistician were kept blinded to the randomisation.
I. Procedure for Data Collection
The participants who gave consent were enrolled in the study. Each session was conducted with a group of 12 to 14 participants. On the first day, the participants were briefed about the sessions and expected learning outcomes. As part of the briefing process, they were explained the confidentiality of the HFPS, the video-assisted lecture sessions and the ethical issues involved. All the participants were introduced to the high-fidelity patient simulator (METIman) in the clinical lab set-up to make them aware of its functions and familiarise them with the handling of the mannequin. An assurance was given to the students that the training course was not part of the evaluation process for the surgical curriculum. The briefing was followed by the first knowledge assessment (Pre-test MCQ) of all the participants. Pre-test MCQ was designed to collect the score of initial background knowledge about tension pneumothorax and its management following the ATLS protocol. The module for the aetiology, pathophysiology and clinical presentation of tension pneumothorax and its steps of management following the ATLS protocol was part of their final year course curriculum. It was taught before they participated in the study. After the Pre-test MCQ session, they were randomized into intervention and control groups consisting of 6 to 7 participants each. For the intervention group, an independent investigator used the high-fidelity simulator (METIman Pre-hospital) to demonstrate the diagnosis and management of tension pneumothorax (Needle Decompression) in an emergency setting. The demonstration time was 20 minutes followed by hands-on training for another 20 minutes. For the control group, a recorded video clip of the identical facilitated simulation session on the diagnosis and management of tension pneumothorax (Needle Decompression) was shown by another investigator. The video demonstration lasted for 20 minutes. This session was followed by a 20-minute interactive discussion session with the faculty. All the participants in both groups were apprised of the importance of aetiology, pathophysiology and clinical presentation in arriving at the diagnosis and management of tension pneumothorax during these interactive teaching sessions. The participants were encouraged to explore how they would manage the stated clinical situation through discussion. The faculty were instructed to emphasize the teaching points related to the outcome of the study. The total duration for both types of teaching was 40 minutes. There were no more additional hands-on practice or video-assisted lecture sessions for the participants during the course of the research study. In the seventh/eighth week, both the intervention and the control groups again participated in the second knowledge assessment (Delayed Post-test MCQ) to assess their gain and retention of knowledge. Delayed Post-test MCQ assessment may minimise the recall bias and test their retained memory better.
Both Pre-test and Post-test knowledge assessments comprised 20 MCQs which were to be completed in 20 minutes. The single-best answer A-type MCQs with five options of answers were prepared following the guidelines framed by the National Board of Medical Examiners (Case & Swanson, 2001). For each correct response, a score of one point was awarded. No negative marking was awarded for incorrect response. Based on the learning objectives, the MCQs were constructed by 6 experts in the field of Surgery, Medicine and Medical Education who were not part of this research study. The MCQs covered the items on pathophysiology, diagnosis, and management of tension pneumothorax, and assessed for knowledge comprehension and knowledge application. The order of the questions was changed between the Pre-test and the Post-test. The MCQ answer sheets were scanned by Konica Minolta FM (172.17.5.12) scanner and graded by using Optical Mark Recognition (OMR) software (Remark Office OMR, version 9.5, 2014; Gravic Inc., USA). Before the main study, a preliminary study involving 56 students was conducted to explore the time management, feasibility, acceptability, and validation of the MCQs (Pal et al., 2021). In the preliminary study, the Pre-test and the Post-test were administered in the first week and the fourth week respectively to note the short-term retention of knowledge. This study is an extension of the preliminary study with a different cohort of students where the Pre-test and the Delayed Post-test were administered in the first week and the seventh/eighth week respectively to determine the medium-term retention of knowledge. The MCQs were reviewed based on the feedback from the preliminary study on the appropriateness of the content, clarity in wording, and difficulty level. The difficulty index and the bi-serial correlation for item discrimination of all MCQs were checked. The value between 30 and 95 in the difficulty index and the bi-serial correlation value > 0.2 were chosen as the accepted standard for this study.
At the end of the study, the participants in the intervention group were provided with access to the identical video-assisted lecture sessions as designed for the control group. Similarly, the participants in the control group were provided with access to the same HFS sessions. This is to ensure parity between the groups for their professional development of knowledge.
J. Statistical Analysis
SPSS software (version 25) was used for data analysis. The descriptive statistics such as frequency and percentage for categorical data and the mean and standard deviation for the total score of the assessments were calculated. ANCOVA was used to determine the difference in post-test MCQ marks between intervention and control groups with pre-test MCQ marks as a covariate. Intragroup comparison of pre-test and post-test MCQ marks was also done by calculating paired t-test. For intergroup comparison, the effect size – Partial Eta Squared was calculated in ANCOVA. Cohen’s dz was calculated for the comparison of dependent means. The level of significance was set at 0.05 and the null hypothesis was rejected when P < 0.05. We measured the scale-level content validity index (SCVI) and item-level content validity index (ICVI) for the validity and Cronbach alpha for the internal consistency (reliability) of the MCQs. The average values of SCVI and ICVI were 0.94 & 0.89 respectively. The value of Cronbach’s alpha was 0.78.
III. RESULTS
The data that support the findings this RCT study are openly available at https://doi.org/10.6084/m9.figshare.19932053 (Pal et al., 2022).
A. General Data Analysis
There was no difference in the highest Pre-test scores achieved by the participants in both intervention and control groups. The lowest scores recorded in the intervention group were better than the control group in both Pre-test and Post-test. There was a negligible difference between the highest Post-test scores among control and intervention groups (See Table 1).
|
Test score |
Intervention |
Control |
|
PRE-TEST |
||
|
Mean (SE) |
12.31 (0.34) |
12.23 (0.36) |
|
95% CI for Mean |
11.64 – 12.98 |
11.50 – 12.96 |
|
Min – Max |
6.0 – 18.0 |
6.0 – 18.0 |
|
POST-TEST |
||
|
Mean (SE) |
13.65 (0.27) |
13.60 (0.30) |
|
95% CI for Mean |
13.12 – 14.19 |
12.98 – 14.20 |
|
Min – Max |
8.0 – 18.0 |
7.0 – 17.0 |
|
Table 1. Highest, lowest and unadjusted mean MCQ scores among intervention and control groups |
||
|
SE – Standard Error CI – Confidence Interval Min – Minimum Max – Maximum |
||
B. Statistical Data Analysis
ANCOVA was used to determine the difference in Post-test MCQ scores among control and intervention groups after adjusting pre-test MCQ scores. There was a linear relationship between Pre-test and Post-test MCQ scores for each group, as determined by visual inspection of the scatterplot. The homogeneity of regression slopes was noted as the interaction term was not statistically significant, F (1, 107) = 0.889, P = 0.348. When assessed by Shapiro-Wilk’s test, standardized residuals were normally distributed (P > 0.05) in the intervention group, but not normally distributed in the control group (P < 0.05). Both homoscedasticity and homogeneity of variance were noted, as assessed by visual inspection of a scatterplot and Levene’s test of homogeneity of variance (P = 0.531), respectively. Data were adjusted with mean ± standard error unless otherwise stated. The effect size, Partial Eta Squared (Partial η2) was calculated in ANCOVA. A partial η2 value of 0.01 or less was considered to be small. For the comparison of dependent means, the effect size, Cohen’s dz was calculated; where the effect size of 0.5-0.8 was considered to be moderate (Ellis, 2010). Post-test MCQ score was higher in the intervention group but after adjustment for pre-test MCQ scores, there was no statistically significant difference in post-test MCQ scores between the control and intervention groups. The effect size was small (See Table 2).
|
Variable |
n |
Post-test MCQ score Mean (SE) |
Mean difference (95% CI) |
P-value |
Partial η2 |
|
Intervention |
55 |
13.65 (0.27) |
0.04 (-0.69, 0.77) |
0.917 |
0.0001 |
|
Control |
56 |
13.60 (0.30) |
|||
|
Table 2. Intergroup comparison of post-test MCQ scores between intervention and control groups after adjusting pre-test MCQ marks (ANCOVA) |
|||||
|
n: number of students SE: Standard error 95% CI: 95% confidence interval Partial η2: Partial Eta Squared |
|||||
There was a statistically significant difference between pre-test and post-test MCQ scores among the intervention and control groups. The mean of post-test MCQ scores was significantly higher than the mean of pre-test MCQ scores in both intervention and control groups. The effect size was moderate in both groups (See Table 3).
|
Variable |
n |
Mean (SD) |
Mean difference (95% CI) |
t (df) |
P-value |
Dz |
|
|
Pre-test MCQ scores |
Post-test MCQ scores |
||||||
|
Intervention |
55 |
12.31 (2.49) |
13.65 (1.99) |
1.34 (0.64, 2.05) |
3.841 (54) |
* < 0.001 |
0.518 |
|
Control |
56 |
12.23 (2.72) |
13.60 (2.26) |
1.36 (0.68, 2.04) |
3.998 (55) |
* < 0.001 |
0.534 |
|
Table 3. Intragroup comparison of pre and post MCQ scores among intervention and control groups (Paired t-test) |
|||||||
|
n: number of students * Significant SD: Standard deviation 95% CI: 95% confidence interval dz: Cohen’s dz |
|||||||
IV. DISCUSSION
Multiple studies have revealed slight to the modest enhancement of knowledge in simulation-based medical education (SBME) when compared to other instructional teaching methods (Cook et al., 2012; Gordon et al., 2006; Lo et al., 2011; Ray et al., 2012; Ten Eyck et al., 2009). Notwithstanding the increasing popularity of SBME, there is little evidence to conclude that it is superior to other small-group teaching modalities for the acquisition of knowledge (Alluri et al., 2016). The common perception is that knowledge lies at the lowest level of competence in Miller’s model of clinical acumen (Miller, 1990), but it is also important to note that knowledge is the basic foundation of competence and proficiency (Norman, 2009). Theoretically, SBME is advantageous for assessment of both knowledge and skills but there are few studies which directly evaluated the effectiveness of HFS in the assessment of knowledge (McGaghie et al., 2009; Rogers, 2008).
The mean scores of both Pre-test and the Post-test were higher in the intervention group in this study. In comparison, our preliminary study demonstrated that the control group had higher mean MCQ marks than the intervention group in Pre-test whereas at Post-test, the intervention group had higher mean MCQ marks than the control group (Pal et al., 2021).
In our study, there is significant enhancement of knowledge (P < 0.001) in both modes of teaching which corroborates the findings of Alluri et al. (2016). Their RCT study demonstrated that the participants in both the simulation and lecture groups had improved post-test scores (p < 0.05). The comparison of Pre-test and Post-test MCQ scores in our preliminary study also revealed significant higher mean MCQ scores at Post-test than Pre-test in both intervention and control groups (Pal et al., 2021). A study by Couto et al. (2015) showed improved post-test scores in both methods. Similar results were noted in the studies by Chen et al. (2017) and Vijayaraghavan et al. (2019). The finding of a study by Hall (2013) showed a slight increase in post-test scores in both the HFPS and control groups.
A systematic review by La Cerra et al. (2019) revealed that HFS was superior to other teaching methods in improving knowledge and performance. Significant higher scores for participants in the HFS group in the studies by Larsen et al. (2020) and Solymos et al. (2015) demonstrated that HFS may be superior to conventional teaching methods for factual learning. In another study by Bartlett et al. (2021), HFS showed a significant long-term gain in knowledge over traditional teaching methods, but short-term knowledge gain was insignificant. Our study revealed that the Post-test MCQ score was higher in the HFS group but after adjustment of pre-test scores, there was no significant difference in knowledge gain between the control and intervention groups. The findings were similar in our preliminary study where the intervention group had higher mean change score of MCQ scores than the control group but it was not statistically significant (Pal et al., 2021).
On the other hand, there was no significant knowledge improvement in both simulation and traditional teaching methods as observed in the studies (Corbridge et al., 2010; Kerr et al., 2013; Moadel et al., 2017). The findings of Alluri et al. (2016) also showed no difference in knowledge gain between simulation and lecture-based teaching. The studies by Morgan et al. (2002) and Tan et al. (2008), demonstrated equal efficacy between simulation and conventional lectures. The findings of a study by Kerr et al. (2013) demonstrated that SBME was not beneficial in acquisition and retention of knowledge. There was no significant improvement in knowledge after simulation-based education as revealed by the findings of three RCTs (Cavaleiro et al., 2009; Cherry et al., 2007; Kim et al., 2002).
Despite simulation being effective in acquisition of knowledge, it may not be the most efficient modality when compared to other traditional educational methods (Bordage et al., 2009). There is ample evidence that SBME usually leads to enhancement of knowledge and skills among undergraduate students but its superiority over other conventional teaching methods is yet to be defined (Nestel et al., 2015).
A. Limitations
There is a possibility of potential biases in the form of design, recruitment, sample populations and data analysis that could have influenced the findings. Due to randomization in blocks of two, the allocation of participants may be predictable which may result in selection bias. The confounding factors such as communication between the different groups of students prior to the second MCQ assessment, participants’ recall memory and preparation for the post-test after 7 – 8 weeks need to be considered. As it was a single-centre study which included final-year medical students only, the validity of the findings may not be applicable to other settings.
V. CONCLUSION
Conventional teaching modalities and HFS, when used in conjunction with bedside teaching, may complement clinical practice, leading to higher retention of knowledge. Therefore, more studies are required to measure the efficacy of simulation for a better understanding of the differences that it can make in the acquisition of knowledge. Our study revealed that the efficacy of high-fidelity simulation-based teaching was not superior to video-assisted lecture-based teaching in terms of knowledge acquisition and retention. The substantially higher cost and maintenance associated with HFS need to be considered before planning a teaching-learning activity. It may be used judiciously with conventional teaching when the objectives are mainly knowledge-based. More studies are required to determine its effectiveness and further evaluation as a teaching-learning tool in medical education.
Notes on Contributors
Bikramjit Pal was involved in Conceptualization, Formal Analysis, Literature Review, Methodology, Project administration & Supervision, Data Analysis and Writing (original draft & editing).
Aung Win Thein was involved in Formal Analysis, Literature Review, Methodology, Supervision and Writing (review & editing).
Sook Vui Chong was involved in Literature Review, Methodology, Supervision and Writing (review & editing).
Ava Gwak Mui Tay was involved in Formal Analysis, Literature Review, Supervision and Writing (review & editing).
Htoo Htoo Kyaw Soe was involved in Formal Analysis, Methodology, Data curation, Statistical Analysis and Validation.
Sudipta Pal was involved in Literature Review, Methodology, Formal Analysis, Data curation and Writing (review & editing).
Ethical Approval
Ethical approval was duly obtained from the Ethical Committee / IRB of Manipal University College Malaysia. Informed consent was taken from all the participants. All information about the participants was kept confidential.
Approval number: MMMC/FOM/Research Ethics Committee – 11/2018.
Data Availability
The data that supports the findings of this RCT study are openly available at Figshare repository, https://doi.org/10.6084/m9.figshare.19932053.v2 (Pal et al., 2022).
Acknowledgement
The authors would like to acknowledge the final year MBBS students of Manipal University College Malaysia who had participated in this research project, the faculty of the Department of Surgery, the lab assistants and technicians of Clinical Skills Lab and the Management of Manipal University College Malaysia.
Funding
The researchers had not received any funding or benefits from industry or elsewhere to conduct this study.
Declaration of Interest
The researchers had no conflicts of interest.
References
Accreditation Council for Graduate Medical Education. (2020, July 1). Program requirements for graduate medical education in general surgery. https://www.acgme.org/globalassets/pfassets/programrequirements/440_generalsurgery_2020.pdf.
Alluri, R. K., Tsing, P., Lee, E., & Napolitano, J. (2016). A randomized controlled trial of high-fidelity simulation versus lecture-based education in preclinical medical students. Medical Teacher, 38(4), 404–409. https://doi.org/10.3109/0142159X.2015.1031734
ATLS Subcommittee, American College of Surgeons’ Committee on Trauma, & International ATLS working group. (2013). Advanced trauma life support (ATLS®): The ninth edition. Journal of Trauma and Acute Care Surgery, 74(5), 1363–1366. https://doi.org/10.1097/TA.0b013e31828b82f5
Bartlett, R. S., Bruecker, S., & Eccleston, B. (2021). High-fidelity simulation improves long-term knowledge of clinical swallow evaluation. American Journal of Speech-Language Pathology, 30(2), 673–686.
Bordage, G., Carlin, B., Mazmanian, P. E., & American College of Chest Physicians Health and Science Policy Committee (2009). Continuing medical education effect on physician knowledge: Effectiveness of continuing medical education: American College of Chest Physicians evidence-based educational guidelines. Chest, 135(3 Suppl), 29S–36S. https://doi.org/10.1378/chest.08-2515
Case, S. M., & Swanson, D. B. (2001). Constructing written test questions for the basic and clinical sciences. 3rd ed. Philadelphia: National Board of Medical Examiners.
Cavaleiro, A. P., Guimarães, H., & Calheiros, F. (2009). Training neonatal skills with simulators? Acta Paediatrica, 98(4), 636–639.
Chen, T., Stapleton, S., Ledford, M., & Frallicciardi, A. (2017). Comparison of high-fidelity simulation versus case-based discussion on fourth- year medical student performance. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 18(5.1). https://escholarship.org/uc/item/5k73f4qc
Cherry, R. A., Williams, J., George, J., & Ali, J. (2007). The effectiveness of a human patient simulator in the ATLS shock skills station. Journal of Surgical Research, 139(2), 229–235. https://doi.org/10.1016/j.jss.2006.08.010
Cook, D. A., Brydges, R., Hamstra, S. J., Zendejas, B., Szostek, J. H., Wang, A. T., Erwin, P. J., & Hatala, R. (2012). Comparative effectiveness of technology-enhanced simulation versus other instructional methods: A systematic review and meta-analysis. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, 7(5), 308–320. https://doi.org/10.1097/SIH.0b013e3182614f95
Corbridge, S. J., Robinson, F. P., Tiffen, J., & Corbridge, T. C. (2010). Online learning versus simulation for teaching principles of mechanical ventilation to nurse practitioner students. International Journal of Nursing Education Scholarship, 7(1), Article 12. https://doi.org/10.2202/1548-923X.1976
Couto, T. B., Farhat, S. C., Geis, G. L., Olsen, O., & Schvartsman, C. (2015). High-fidelity simulation versus case-based discussion for teaching medical students in Brazil about pediatric emergencies. Clinics (Sao Paulo, Brazil), 70(6), 393–399. https://doi.org/10.6061/clinics/2015(06)02
Davies, R. (2008). The Bologna process: the quiet revolution in nursing higher education. Nurse Education Today, 28(8), 935–942. https://doi.org/10.1016/j.nedt.2008.05.008
Ellis, P. (2010). The essential guide to effect sizes: Statistical power, meta-analysis, and the interpretation of research results. Cambridge University Press. https://doi.org/10.1017/CBO9780511761676
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/bf03193146
Gordon, J. A., Shaffer, D. W., Raemer, D. B., Pawlowski, J., Hurford, W. E., & Cooper, J. B. (2006). A randomized controlled trial of simulation-based teaching versus traditional instruction in medicine: A pilot study among clinical medical students. Advances in Health Sciences Education , 11(1), 33–39. https://doi.org/10.1007/s10459-004-7346-7
Hall, R. M. (2013). Effects of high fidelity simulation on knowledge acquisition, self-confidence, and satisfaction with baccalaureate nursing students using the solomon-four research design [Doctoral dissertation, East Tennessee State University]. East Tennessee State University Higher Education Commons. https://dc.etsu.edu/etd/2281
Kerr, B., Hawkins, T. L., Herman, R., Barnes, S., Kaufmann, S., Fraser, K., & Ma, I. W. (2013). Feasibility of scenario-based simulation training versus traditional workshops in continuing medical education: a randomized controlled trial. Medical Education Online, 18(1), Article 21312. https://doi.org/10.3402/meo.v18i0.21312
Kiernan, L. C. (2018). Evaluating competence and confidence using simulation technology. Nursing, 48(10), 45–52. https://doi.org/10.1097/01.NURSE.0000545022.36908.f3
Kim, J. H., Kim, W. O., Min, K. T., Yang, J. Y., & Nam, Y. T. (2002). Learning by computer simulation does not lead to better test performance on advanced cardiac life support than textbook study. The Journal of Education in Perioperative Medicine, 4(1), Article E019.
Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development. Prentice Hall.
La Cerra, C., Dante, A., Caponnetto, V., Franconi, I., Gaxhja, E., Petrucci, C., Alfes, C. M., & Lancia, L. (2019). Effects of high-fidelity simulation based on life-threatening clinical condition scenarios on learning outcomes of undergraduate and postgraduate nursing students: A systematic review and meta-analysis. BMJ Open, 9(2), Article e025306. https://doi.org/10.1136/bmjopen-2018-025306
Larsen, T., Jackson, N., & Napolitano, J. (2020). A comparison of simulation-based education and problem-based learning in pre-clinical medical undergraduates. MedEdPublish, 9(1), Article 172.
Lo, B. M., Devine, A. S., Evans, D. P., Byars, D. V., Lamm, O. Y., Lee, R. J., Lowe, S. M., & Walker, L. L. (2011). Comparison of traditional versus high-fidelity simulation in the retention of ACLS knowledge. Resuscitation, 82(11), 1440–1443. https://doi.org/10.1016/j.resuscitation.2011.06.017
McGaghie, W. C., Siddall, V. J., Mazmanian, P. E., Myers, J., & American College of Chest Physicians Health and Science Policy Committee (2009). Lessons for continuing medical education from simulation research in undergraduate and graduate medical education: Effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest, 135(3 Suppl), 62S–68S. https://doi.org/10.1378/chest.08-2521
Miller, G. E. (1990). The assessment of clinical skills/competence/performance. Academic Medicine, 65(9), S63–S67. https://doi.org/10.1097/00001888-199009000-00045
Moadel, T., Varga, S., & Hile, D. (2017). A prospective randomized controlled trial comparing simulation, lecture and discussion-based education of sepsis to emergency medicine residents. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 18(5.1). https://escholarship.org/uc/item/0132981t
Morgan, P. J., Cleave-Hogg, D., McIlroy, J., & Devitt, J. H. (2002). Simulation technology: A comparison of experiential and visual learning for undergraduate medical students. Anesthesiology, 96, 10–16. https://doi.org/10.1097/00000542-200201000-00008
Nestel, D., Harlim, J., Smith, C., Krogh, K., & Bearman, M. (2015). Simulated learning technologies in undergraduate curricula: An evidence check review for HETI.
Norman, G. (2009). The American College of Chest Physicians evidence-based educational guidelines for continuing medical education interventions: a critical review of evidence-based educational guidelines. Chest, 135(3), 834–837. https://doi.org/10.1378/chest.09-0036
Pal, B., Chong, S. V., Thein, A. W., Tay, A. G., Soe, H. H., & Pal, S. (2021). Is high-fidelity patient simulation-based teaching superior to video-assisted lecture-based teaching in enhancing knowledge and skills among undergraduate medical students? Journal of Health and Translational Medicine, 24(1), 83-90. https://doi.org/10.22452/jummec.vol24no1.14
Pal, B., Thein, A. W., Chong, S. V., Tay, A., Htoo, H., & Pal, S. (2022). A randomized controlled trial study to compare the effectiveness of high-fidelity based teaching with video-assisted based lecture teaching in enhancing knowledge [Dataset]. Figshare. https://doi.org/10.6084/m9.figshare.19932053
Ray, S. M., Wylie, D. R., Shaun Rowe, A., Heidel, E., & Franks, A. S. (2012). Pharmacy student knowledge retention after completing either a simulated or written patient case. American Journal of Pharmaceutical Education, 76(5), 86. https://doi.org/10.5688/ajpe76586
Rogers, D. A. (2008). The role of simulation in surgical continuing medical education. Seminars in Colon and Rectal Surgery, 19(2), 108-114. https://doi.org/10.1053/j.scrs.2008.02.007
Solymos, O., O’Kelly, P., & Walshe, C. M. (2015). Pilot study comparing simulation-based and didactic lecture-based critical care teaching for final-year medical students. BMC Anesthesiology, 15, Article 153. https://doi.org/10.1186/s12871-015-0109-6
Tan, G. M., Ti, L. K., Tan, K., & Lee, T. (2008). A comparison of screen-based simulation and conventional lectures for undergraduate teaching of crisis management. Anaesthesia and Intensive Care, 36(4), 565–569.
Ten Eyck, R. P., Tews, M., & Ballester, J. M. (2009). Improved medical student satisfaction and test performance with a simulation-based emergency medicine curriculum: a randomized controlled trial. Annals of Emergency Medicine, 54(5), 684–691. https://doi.org/10.1016/j.annemergmed.2009.03.025
Vijayaraghavan, S., Rishipathak, P., & Hinduja, A. (2019). High-fidelity simulation versus case-based discussion for teaching bradyarrhythmia to emergency medical services students. Journal of Emergencies, Trauma, and Shock, 12(3), 176–178. https://doi.org/10.4103/JETS.JETS_115_18
Yang, Y., & Liu, H. P. (2016). Systematic evaluation influence of high-fidelity simulation teaching on clinical competence of nursing students. Chinese Nursing Research, 30(7), 809–814. https://caod.oriprobe.com/articles/47628779/Systematic_evaluation_influence_of_high_fidelity_s.htm
*Bikramjit Pal
RCSI & UCD Malaysia Campus (RUMC),
4 Jalan Sepoy Lines,
Georgetown, Penang, 10450, Malaysia
+6042171908-1908 (Ext)
Email: bikramjit.pal@rcsiucd.edu.my
Submitted: 15 October 2022
Accepted: 3 January 2023
Published online: 4 July, TAPS 2023, 8(3), 1-4
https://doi.org/10.29060/TAPS.2023-8-3/GP2903
Galvin Sim Siang Lin1, Yook Shiang Ng2 & Chan Choong Foong3
1Department of Dental Materials, Faculty of Dentistry, Asian Institute of Medicine, Science and Technology (AIMST) University, Malaysia; 2Conservative Dentistry Unit, School of Dental Sciences, Universiti Sains Malaysia, Health Campus, Malaysia; 3Medical Education and Research Development Unit (MERDU), Faculty of Medicine, Universiti Malaya, Malaysia
Abstract
Introduction: Dental materials science is one of the core courses for Malaysian undergraduate dental programmes, which has been primarily taught through a series of didactic lectures during the preclinical phase. In accordance with the newly revised national competency statement, Malaysian dental education is moving toward competency-based education, hence a reformation of the dental materials science curriculum is warranted.
Methods: Curriculum design including common teaching, learning and assessments methods for the Malaysian dental materials science were described and analysed. The common practices were reviewed and compared with latest national guidelines and literature.
Results: There is yet an initiative to establish a national curriculum for dental materials science. The use of traditional teaching strategies for this course also needs to be revamped from a teacher-centred to a student-centred approach. Furthermore, faculty members are facing significant challenges because the revamp requires them to explore cutting-edge pedagogical methods and develop appropriate learning opportunities, environments, resources, and assessments. Several recommendations are proposed, such as mapping the existing dental materials science curriculum to identify gaps, incorporating more hands-on sessions, implementing an integrated curriculum, introducing various formative and summative assessments, as well as recruiting faculty members with different areas of educational expertise.
Conclusion: It is hoped that this article offers a clearer pathway for Malaysian dental educators to pioneer new insight and transform the existing dental materials science curriculum.
I. INTRODUCTION
Malaysian dental curriculum is historically underpinned by the primary goal in nurturing clinically competent dentists to provide safe and high-quality oral healthcare treatment to the public. Although the curriculum has witnessed an array of revisions over the years, little has been done for dental materials science courses. In the present article, the authors outline an overview of the dental curriculum in Malaysia and describe how dental materials science courses are currently delivered. Subsequently, challenges and compelling needs are highlighted to envision the future curriculum.
II. OVERVIEW OF DENTAL CURRICULUM IN MALAYSIA
In May 1972, the Universiti Malaya established the country’s first dental school to offer a Bachelor of Dental Surgery (BDS) programme. Nowadays, dentistry has become one of the popular university programmes for high school leavers in Malaysia and the number of applicants has increased significantly over the past decades. Thirteen dental schools have been established of which six are public institutions and the remaining seven are private institutions. All dental schools in Malaysia operate independently as siloed institutions; there is no national standardised curriculum or licensing examination. Currently, each of these dental schools offers a five-year undergraduate dental programme leading to the conferment of BDS or Doctor of Dental Surgery (DDS), and all programmes are required to be accredited by the Malaysian Dental Council (MDC).
In general, undergraduate dental programmes in Malaysia are divided into two phases: preclinical and clinical phases. The preclinical phase encompasses the first two years of the undergraduate programmes. Undergraduate dental students are taught fundamental dental and medical concepts along with operative practical and laboratory skills through simulation exercises on mannequins or dummy heads. In the subsequent three years of the clinical phase, students are given the opportunities to manage and provide treatments to patients. At the end of the five-year programmes, dental students are expected to be clinically competent and practise evidence-based dentistry with ethics and professionalism.
III. DENTAL MATERIALS SCIENCE CURRICULUM IN MALAYSIA
A. Curriculum Content
Undergraduate dental programmes in Malaysia offer dental materials science courses as one of the core disciplines in the second year of preclinical phase. Dental materials science is a course that integrates underlying principles of chemical engineering and materials science into the practice of contemporary dentistry (Qazi et al., 2019). Typically, dental materials science is introduced as a stand-alone course distributed across several modules over the preclinical dental phase. The course usually starts with an introduction to dental materials and the properties of commonly used dental materials. In some dental schools, the course is divided into discipline-based such as dental materials used in conservative dentistry, prosthodontics, paediatric dentistry, orthodontics, or periodontics; whereas some schools divide the course into clinical-based and laboratory-based dental materials. Among the course content covered in clinical-based dental materials include amalgam, dental composite resin, glass ionomer cement and impression materials. On the other hand, denture-based polymers, dental ceramics, metal alloys, gypsum products as well as casting and investment materials are covered under laboratory-based dental materials. Additionally, most dental schools in Malaysia design and develop their dental materials science courses based on Bloom’s and Simpson’s taxonomies, with the bulk of the curriculum content lying within cognitive C1 (Remember) to C3 (Apply) and psychomotor P2 (Set) to P4 (Mechanism) levels.
B. Teaching, Learning and Assessment Methods
Dental materials science courses are usually delivered through a series of didactic lectures. Students are also exposed to practical hands-on sessions to examine the properties of commonly used dental materials and manipulate various dental materials. For instance, some dental schools in Malaysia introduce hands-on practical to evaluate the mechanical and viscoelastic properties of various dental materials as well as to mix clinical and laboratory-based dental materials, such as dental gypsum products, dental polymers, dental cement, and dental impression materials.
Nevertheless, since each dental school utilises a distinct set of course learning outcomes, it is infeasible to make a direct comparison between them. Moreover, students are required to meet the desired course learning outcomes upon completion of the courses. Most dental schools use either formative, summative, or a combination of both assessments to evaluate their students, though solely evaluating students based on formative assessment is rare. Students also might be evaluated through quizzes, presentation seminars, assignments, written assessments, and practical assessments such as objective-structured practical examinations (OSPE). Examples of written assessments include multiple-choice questions (MCQ) and short-answer questions (SAQ).
IV. CHALLENGES AND THE TURNING POINT
In June 2021, the Malaysian Dental Dean Council organised a workshop and proposed a revised national competency statement for future graduates in Malaysia, which was later endorsed by the Malaysian Dental Council in July 2021 (Malaysian Dental Council [MDC], 2021). The national competency statement was revised to align with the Malaysian Qualifications Framework version 2.0 competency-based education. Specifically, for dental materials science, the cognitive and psychomotor-related clusters have stated that future dental graduates should be able to justify the selection of dental materials based on the science and applications and related environmental issues (Cognitive: C4 Analyse) and to manipulate commonly used dental materials (Psychomotor: P5 Complex or overt response). Subsequently, Malaysian dental schools are prompted to revise their existing dental materials science curriculum to attain the intended learning outcomes. It is necessary to reform the dental materials science curriculum that is going to lead the attainment of cognitive and psychomotor competencies. Yet, there is no standardised national curriculum for dental materials science courses in Malaysia, despite there were a few attempts by faculty members from several dental schools.
Furthermore, pedagogical methods require improvement as dental materials science courses are often delivered via didactic lectures, whereby students claimed as a ‘dry’ subject (Soni et al., 2021). Implementation of traditional pedagogical methods does not only result in a lack of applications of pertinent knowledge, but these methods also reduce students’ interest and learning efficacies for the courses. Hence, the traditional pedagogical methods used to deliver dental materials science must be revamped to shift from teacher-centred approach to student-centred approach. There is a need to adopt diverse pedagogical methods in encouraging active students’ engagement during learning activities. This shift has posed a significant challenge to faculty members because not only do they need to explore innovative pedagogical methods that promote active learning, but they need to devise appropriate learning opportunities, learning locations, learning resources, and alternative assessments for students.
Different educational backgrounds of faculty members who teach dental materials courses are also a topic of discussion. Some Malaysian dental schools recruit experts with postgraduate degrees either in dental materials, conservative dentistry, prosthodontics, or restorative dentistry, while some schools might employ experts with a background in chemistry or material sciences. Students may miss the fundamental knowledge (if taught by BDS qualified) or fail to relate the clinical applications (if taught by scientists). At the present, teaching qualifications are encouraged but not mandatory for faculty members.
V. RECOMMENDATIONS FOR TOMORROW’S DENTAL MATERIALS SCIENCE CURRICULUM
The revised national competencies statement represents national advocacy for transformation in the dental curriculum. Hence, curriculum mapping is an initial step in transforming tomorrow’s dental materials science curriculum. Following curriculum mapping, dental educators can identify the gaps in the existing curriculum, suggest components to be maintained, revised, or removed with the purpose to achieve the desired cognitive and psychomotor competencies as listed in the national statement. Consequently, it also symbolises the significance to spur the call for the establishment of a designated dental education department in designing and developing comprehensive dental programmes in Malaysia. In hindsight, one may say that this notion served as the impetus for Malaysia to accomplish competency-based dental education in the 21st century.
Didactic lectures place a focus on the transmission of knowledge passively from lecturers to students. Students may find it difficult to understand the basic premises and practical applications of materials science and engineering due to its interdisciplinary nature in the field of dentistry. As students are required to comprehend and justify the selection of various dental materials, hands-on experience in their pre-clinical education is of utmost importance. For instance, practical sessions on manipulating different materials may be arranged following theoretical lectures. Thus, the ability to actively apply the theories of materials science to clinical content is what constitutes mastery in dental materials science courses, which goes beyond how well a student can recall and repeat factual information. In addition, to incorporate more hands-on sessions, the dental materials science curriculum should consider diverse pedagogical methods including but not limited to concept mapping, flipped classroom, micro-teaching, jigsaw, small-group discussions, and team-based learning. Although these methods are experimented in the literature, there is limited published evidence in Malaysia (Bhat et al., 2021).
The current discipline-based curriculum in Malaysian dental education consists of a stack of separate courses with their compartmentalised scopes and syllabus. Students may find it difficult to correlate theoretical knowledge and clinical application due to the lack of integration between preclinical and clinical courses. An integrated competency-based curriculum could overcome this dilemma by incorporating dental materials science into the list of courses that demand vertical and horizontal integration. Integrated curriculum as a visionary change could be regarded as one of the first instances in Malaysian dental education, where dental materials science is no longer viewed as a stand-alone course or under the aegis of a particular dental speciality. In fact, it will be divided into several subtopics that are integrated into several dental specialities across the preclinical and clinical phases. For instance, topics like amalgam and dental composite resin can be incorporated in conservative dentistry courses, whilst removable prosthodontics courses can cover dental materials like resin polymer and gypsum. As students are transitioning into clinical years, dental ceramics can be integrated into fixed prosthodontics courses.
A well-designed dental materials science curriculum must take assessments into consideration since it reflects how the documented curriculum is related to the outcomes (e.g., the student’s learning experiences, course learning outcomes and learning opportunities). If the dental materials science curriculum is to be revised to accommodate horizontal and vertical integrations, then a myriad of assessments should be utilised. Interdisciplinary care and evidence-based treatments with sound analytical and communication skills, are necessary for the successful and efficient delivery of tomorrow’s dental education. This justifies the need for assessment systems to be thorough and concrete enough to evaluate every stage of students’ progression. Although dental schools in Malaysia have been utilising written assessments (e.g., multiple choices questions, short answer questions) as the main assessment tool in dental materials science courses, alternative assessments such as modified Direct Observation of Procedural Skills (DOPS), peer- and self-assessments could be introduced in accordance with an integrated curriculum (Ferris & O’Flynn, 2015). These alternative assessments are valid and reliable in determining competencies and offering exceptional chances to combine summative and formative assessments. It is expected that students would be capable of recognising knowledge and skills, and they would value opportunities for improvement in their learning (i.e., self-reflection).
Moreover, Malaysian dental schools should consider recruiting faculty members with different areas of educational expertise in teaching dental materials science courses. Diversity of teaching staff will enhance and enrich the learning experiences of students. Experts with backgrounds in chemistry and materials science could involve in the teaching of fundamental principles of dental materials, while those with dental degrees may involve in translating the knowledge into practical applications. It is also worth noting that no single faculty member is recommended to cover the whole teaching and learning syllabus. Last, teaching qualifications are highly recommended for faculty members to apply and keep abreast with the latest instructional design. Nevertheless, the movement toward competency-based education (and moving away from traditional discipline-based or requirement-based education) would require more education research and academic discussions in Malaysia to rationalise and select appropriate teaching, learning and assessment methods as well as intellectual vibrancy, academic support, research, scholarship, and educational management in dental materials science courses.
VI. CONCLUSION
Malaysia is on the verge of advancing towards competency-based dental education along with the introduction of a diversity of teaching, learning and assessment methods. The path to change is not without obstacles and ambiguity. Thus, comprehensive education research and academic discussions among dental educators in Malaysia involved in the teaching of dental materials science are warranted to pioneer new insight to transform the existing dental materials science curriculum.
Notes on Contributors
GSSL and CCF was involved in conception and design of the study. GSSL and YSN reviewed the literature, collected the data, and wrote the original draft. CCF edited the original draft. All authors have read and approved the final manuscript.
Funding
No funding is required for this paper.
Declaration of Interest
All authors have no conflicts of interest.
References
Bhat, S., Madiyal, A., & Babu, G. S. (2021). Innovative teaching methods in dental education. Gülhane Medical Journal, 63, 8-13. https://doi.org/10.4274/gulhane.galenos.2020.1181
Ferris, H., & O’Flynn, D. (2015). Assessment in medical education; What are we trying to achieve? International Journal of Higher Education, 4(2), 139-144. https://doi.org/10.5430/ijhe.v4n2p139
Malaysian Dental Council. (2021). Competencies of new dental graduates, Malaysia-V2-2021. Retrieved September 23, 2022, from https://mdc.moh.gov.my/uploads/competencies_of_new_dental_grad_20222.pdf
Qazi, H. S., Ashar, A., & Ahmad, S. A. (2019). Impact of an innovative approach of teaching science of dental materials on the learning experiences of undergraduate students. Pakistan Armed Forces Medical Journal, 69, 582-588.
Soni, V., Kotsane, D. F., Moeno, S., & Molepo, J. (2021). Perceptions of students on a stand-alone dental materials course in a revised dental curriculum. European Journal of Dental Education, 25, 117-123.
*Galvin Sim Siang Lin
Department of Dental Materials,
Faculty of Dentistry,
Asian Institute of Medicine,
Science and Technology (AIMST) University,
08100, Bedong, Kedah, Malaysia
Email: galvin@aimst.edu.my
Submitted: 27 December 2022
Accepted: 13 March 2023
Published online: 4 July, TAPS 2023, 8(3), 70-71
https://doi.org/10.29060/TAPS.2023-8-3/LE2938
Hirofumi Kanazawa1 & Ikuo Shimizu2,3
1Shinshu University School of Medicine, Matsumoto, Japan; 2Safety Management Office, Shinshu University Hospital, Matsumoto, Japan; 3Department of Medical Education, Chiba University Graduate School of Medicine, Chiba, Japan
Medication errors are one of the most serious problems in healthcare, and their occurrence is due to a wide variety of causes. While almost all drug-related medical errors are potentially avoidable, the main obstacles are primarily health system vulnerabilities and human error. To remove those obstacles, the World Health Organization (WHO) suggested providing more education (World Health Organization, 2017), specifically by participating in medical care. Graduation competencies in many countries, which include activities about medication and patient safety, are consistent with the statement. In addition, it is known that more prescribing errors occur in the first postgraduate year. Learning about prescriptions during medical studentships must be enhanced.
Nevertheless, we are concerned that medication safety education is still insufficient in the current undergraduate curriculum because of license-based regulation. It is considered difficult for clinical students to incorporate prescribing and ordering medication as part of medical studentship. Such license-based regulation is typical in Asia, where authoritarian attitudes are strong. We would like to point out that invasive clinical procedures are handled differently from prescriptions, despite the fact that such procedures are also medical practices that can involve risk. While medical students have the opportunity to conduct invasive medical procedures in the workplace, they scarcely prescribe medication before graduation.
It is time for medical educators to take the WHO statement seriously and organise more opportunities to learn how to prescribe medications safely. We can transfer learning strategies from invasive clinical procedures, even in the context of strict regulations. For example, we can implement more simulation practices. Although the WHO Curriculum Guide for Patient Safety does not yet include scenario simulation, research suggests that education with appropriate feedback can be very effective (Motola et al., 2013). Simulation-based prescription practice, especially in situations where medication errors are likely to occur, would allow for focused practice in a zero-risk environment. Another concern is that there have been relatively few published studies on the effectiveness of medication safety in undergraduate education, including simulation. High-fidelity simulators are available in many medical schools, but the usability is still limited because they do not cover a wide variety of situations to use medications. A possible breakthrough can be the implementation of virtual or mixed reality environment. Enhancing the reality of prescribing and administrating medications through these educational strategies could be a very useful tool to apply not only in Asia but also in other contexts.
Notes on Contributors
Hirofumi Kanazawa conceptualised and wrote the manuscript.
Ikuo Shimizu wrote and supervised the manuscript.
All authors discussed and contributed to the final manuscript.
Funding
This work was supported by JSPS KAKENHI Grant Number 21H03161.
Declaration of Interest
There is no conflict of interest.
The main idea of this article was presented at The 17th Annual Congress of Japanese Society for Quality and Safety in Healthcare on November 27, 2022.
References
Motola, I., Devine, L. A., Hyun, S. C., Sullivan, J. E., & Issenberg, S. B. (2013). Simulation in healthcare education: A best evidence practical guide. AMEE Guide No. 82. Medical Teacher, 35(10), e1511-e1530. https://doi.org/10.3109/0142159X.2013.818632
World Health Organization. (2017, May 15). Medication Without Harm – Global Patient Safety Challenge on Medication Safety. https://www.who.int/publications/i/item/WHO-HIS-SDS-2017.6
*Ikuo Shimizu
Safety Management Office,
Shinshu University Hospital,
Matsumoto, Japan
3-1-1, Asahi, Matsumoto City,
Nagano, Japan, 390-8621
+81 263 37 3359
Email: qingshuiyufu@gmail.com
Submitted: 22 July 2022
Accepted: 5 December 2022
Published online: 4 April, TAPS 2023, 8(2), 93-96
https://doi.org/10.29060/TAPS.2023-8-2/CS2849
Mian Jie Lim1, Jeremy Choon Peng Wee2, Dana Xin Tian Han2 , Evelyn Wong2
1SingHealth Emergency Medicine Residency Programme, Singapore Health Services, Singapore; 2Department of Emergency Medicine, Singapore General Hospital, Singapore
I. INTRODUCTION
Singapore raised its Disease Outbreak Response System Condition (DORSCON) from yellow to orange on the 7th of February 2020 after it is first reported unlinked community COVID-19 case on the 6th of February 2020.
The Department of Emergency Medicine (DEM) of Singapore General Hospital (SGH) hosted clinical rotations for medical students (MS) from Duke-NUS Medical School. Their clinical rotations lasted four weeks, during which MS were expected to achieve competence in history taking, physical examination, formulating a management plan, and performing minor procedures.
The local curriculum relies heavily on clinical rotations, during which MS directly contacts patients to fulfil their learning objectives. During DO, clinical postings were postponed, and the term break was brought forward (Ashokka et al., 2020). Restricting MS from entering hospitals and having face-to-face interactions with patients resulted in significant changes to clinical learning. Learning sessions involving direct contact that could not be held over remote platforms were cancelled.
We aimed to discover how MS felt excluded from clinical teaching during the COVID-19 pandemic and how teaching could be improved to support their learning.
II. METHODS
A mixed method of qualitative content analysis and quantitative analysis was performed for this study. Purposive sampling was conducted among all the Duke-NUS MS whose clinical postings to SGH DEM were affected during the COVID-19 outbreak. The link for the online survey form was sent via email or WhatsApp® to 60 MS. Their preferences in learning were assessed by a simple descriptive quantitative analysis of the responses to multiple-choice questions and were followed by an open-ended question whereby template analysis was performed. The consent of each participant was obtained as part of the online survey. The sample of the survey is attached in Appendix A.
III. RESULTS
A. Quantitative Result
Twenty-five MS (42%) were keen to participate in all learning activities at all department areas during normal times if they were trained to wear adequate personal protective equipment (PPE). Twenty-one MS (35%) felt that all learning activities should only be in safe areas of the department with appropriate PPE. Twelve MS (20%) were not keen on having any patient contact.
B. Qualitative Results
1) What other areas of improvement department could introduce about learning during the current pandemic?
Identified main themes, subthemes, and quotes from the open-ended questionnaire questions are presented in Table 1.
|
Main themes /subthemes |
Quotes |
|
1) Balance of training needs with infection control Patient contact is integral to medical education, but it had to be balanced during this pandemic by reducing infection transmission risk. |
“… there is simply no substitute for actually seeing patients for the best learning….” “I think it would be more dangerous to let the students into the wards with a false sense of security (i.e., anticipating limited exposure) than to be fully prepared for all situations.” |
|
2) Respecting medical students’ choice Some respondents felt that MS are all adult learners and should be given the liberty o weigh the risk of infection and benefit of learning through direct patient contact and decide if they want full clinical exposure to patients. |
“should be allowed to choose – whether or not they wish to see patients.”
|
|
2.1) Competency and training needs By preventing all MS from seeing the patients, some felt that this would result in MS not achieving adequate competency as a doctor, subsequently affecting the future healthcare workforce. |
“…We should be allowed to participate in national efforts to quell this disease and to learn as part of this job the national defence expects of us in the future.” |
|
2.2) Compromise in patient safety If patients were to be managed by doctors who lack sufficient clinical exposure during their MS training, their care would be compromised. |
“…It’s helping no one and least of all the patients who will encounter a fresh batch of HOs [House Officers] with little practical experience.” |
|
3) Risk reduction methods Training MS to wear PPE correctly can reduce the risk of transmission significantly and prepare them for future pandemics. |
“To teach and equip students adequately as it would help students with clinical posting and understand the basic importance of PPE in the future as well be well prepared.” |
|
3.1) Remote learning is good but should be engaging and interactive One of the challenges of remote learning is the difficulty faced by MS in maintaining a constantly high level of attentiveness. Hence, it is crucial that remote learning is engaging and interactive. |
“interactive digital simulations” “using polls was a good way to interact.” |
Table 1. Themes, subthemes and medical students’ responses
IV. DISCUSSION
A multi-centre quantitative study was done in the USA by Harries et al. (2021) which showed that 83.4% of MS agreed to return to the clinical environment. These results were comparable with our study’s quantitative result, which showed that 77% of MS were willing to return to the clinical environment during a pandemic.
Spencer et al. (2000) showed that direct patient contact is essential for developing clinical reasoning, communication skills, professional attitudes, and empathy. The findings of this study showed that MS felt that not having direct clinical contact with patients during the pandemic had adverse effects on their learning. Although actual patient contact is desired, this may be countered by the risk of COVID-19 infection, reflected in the first theme of “balance of training needs with infection control” only if adequate risk reduction can patient contact be achieved within a low-risk environment.
MS are all adult learners and should be given liberty on the need for full clinical exposure to patients. However, barring MS from clinical areas also occurred in other countries, especially with the shortage of PPE during the initial emergence of COVID-19 (Rose, 2020).
PPE and infection control training for MS is crucial to ensure clinical teaching can be conducted safely during a pandemic outbreak. Norton et al. (2021) suggested that to avoid injury to patients and healthcare providers and reduce COVID-19-related anxiety among MS, better PPE and infection control training was essential.
A. Limitation
As our study is a mixed qualitative content analysis and quantitative analysis study of a single centre, it is therefore affecting the generalisability of our results. More multi-centre research could be conducted to understand MS’s opinions across Singapore better.
Secondly, another limitation is that our data was collected via an online survey, and we could not follow up with in-depth questions, unlike face-to-face interviews.
The study was done during the early phase of the COVID outbreak and was designed as an initial exploratory study. The results could be used to establish initial information that can help guide future studies.
V. CONCLUSION
From this study, it is essential that medical education needs to be more versatile in future pandemics and consider MS’s opinions. We recommend the incorporation of PPE and infection control training in the undergraduate curriculum, as well as the set-up of an effective online learning platform.
Notes on Contributors
Lim Mian Jie performed the literature review and the template analysis of the data and wrote the manuscript.
Wee Choon Peng Jeremy developed the methodological framework, performed the template analysis of the data, and gave critical feedback to the writing of the manuscript.
Dana Han Xin Tian submitted the CIRB application, recruited the participants, and collected the data.
Evelyn Wong conceptualised the study, collected the data, advised on the study’s design, and gave critical feedback to the writing of the manuscript.
All the authors have read and approved the final manuscript.
Ethical Approval
IRB exemption for this study was obtained (SingHealth CRIB reference number 2020/2134).
Acknowledgement
The authors would like to acknowledge the contributions of all the participants.
Funding
No funding is required for this study.
Declaration of Interest
There is no conflict of interest.
References
Ashokka, B., Ong, S. Y., Tay, K. H., Loh, N. H. W., Gee, C. F., & Samarasekera, D. D. (2020). Coordinated responses of academic medical centres to pandemics: Sustaining medical education during COVID-19. Medical Teacher, 42(7), 762–771. https://doi.org/10.1080/0142159X.2020.1757634
Harries, A. J., Lee, C., Jones, L., Rodriguez, R. M., Davis, J. A., Boysen-Osborn, M., Kashima, K. J., Krane, N. K., Rae, G., Kman, N., Langsfeld, J. M., & Juarez, M. (2021). Effects of the COVID-19 pandemic on medical students: A multi-centre quantitative study. BMC Medical Education, 21(1), Article 14. https://doi.org/10.1186/s12909-020-02462-1
Norton, E. J., Georgiou, I., Fung, A., Nazari, A., Bandyopadhyay, S., & Saunders, K. E. A. (2021). Personal protective equipment and infection prevention and control: A national survey of UK medical students and interim foundation doctors during the COVID-19 pandemic. Journal of Public Health, 43(1), 67–75. https://doi.org/10.1093/pubmed/fdaa187
Rose, S. (2020). Medical student education in the time of COVID-19. JAMA, 323(21), 2131. https://doi.org/10.1001/jama.2020.5227
Spencer, J., Blackmore, D., Heard, S., McCrorie, P., McHaffie, D., Scherpbier, A., Gupta, T. S., Singh, K., & Southgate, L. (2000). Patient-oriented learning: A review of the role of the patient in the education of medical students. Medical Education, 34(10), 851–857. https://doi.org/10.1046/j.1365-2923.2000.00779.x
*Lim Mian Jie
Singapore General Hospital,
Outram Road,
169608, Singapore
Email: mianjie.lim@mohh.com.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









