Preclinical medical student satisfaction of Team-based learning in Chiang Mai University
Submitted: 9 February 2023
Accepted: 22 March 2023
Published online: 3 October, TAPS 2023, 8(4), 36-39
https://doi.org/10.29060/TAPS.2023-8-4/SC3000
Komson Wannasai1, Wisanu Rottuntikarn1, Atiporn Sae-ung2, Kwankamol Limsopatham2, Wiyada Dankai1
1Department of Pathology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 2Department of Parasitology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Abstract
Introduction: Global medical and healthcare education systems are increasingly adopting team-based learning (TBL). TBL is an interactive teaching programme for improving the performance, clinical knowledge, and communication skills of students. The aim of this study is to report the learning experience and satisfaction of participants with the TBL programme in the preclinical years of the Faculty of Medicine, Chiang Mai University.
Methods: Following the implementation of TBL in the academic year 2022, we asked 387 preclinical medical students, consisting of 222 Year 2 and 165 Year 3 medical students who attended the TBL class to voluntarily complete a self-assessment survey.
Results: Overall, 95.35% of the students were satisfied with the structure of the TBL course and agreed to attend the next TBL class. The overall satisfaction score was also high (4.44 ± 0.627). In addition, the students strongly agreed that the TBL programme improved their communication skills (4.50 ± 0.796), learning improvement (4.41 ± 0.781), and enthusiasm for learning (4.46 ± 0.795).
Conclusion: The survey findings indicated that students valued TBL-based learning since it enabled them to collaborate and embrace learning while perhaps enhancing their study abilities. However, since this is a pilot study, further investigations are warranted.
Keywords: Team-based Learning, Small Group Interaction, Medical Education, Implementation
I. INTRODUCTION
Team-based learning (TBL) is a form of small-group teaching which can improve student performance, clinical knowledge, and communication skills. It has been employed in medical and healthcare education in the US, Australia, Austria, Japan, South Korea, and Singapore (Burgess et al., 2014; Michaelsen & Sweet, 2008). Since 2000s, this model has been used in medical education to foster deep learning across a variety of subjects and educational contexts, benefiting teachers and helping academically weak and strong students achieve the same or better results than with conventional methods (Parmelee et al., 2012). In addition, it is more effective for engaging students than lecturing in a large class with few teachers (Burgess et al., 2020b).
The key elements of TBL include pre-class preparation to encourage self-study, teamwork, and instant feedback. These key elements promote active learning and critical thinking (Burgess et al., 2020a; Parmelee et al., 2012). The steps in TBL include pre-class preparation, individual readiness assurance test (iRAT), team readiness assurance test (tRAT), feedback, and team application (Burgess et al., 2014). In the tRAT and team application phase, students work in small groups to demonstrate the use of teamwork for problem-solving. Clinical problem-solving exercises by students lead to class discussions and instructor comments (Burgess et al., 2020a; Michaelsen & Sweet, 2008). The teacher’s feedback can help clarify students’ responses by discussing their answers. In the academic year 2022, TBL was implemented on second- and third-year medical students in the Faculty of Medicine, Chiang Mai University, and self-assessment questionnaires were used to assess students’ satisfaction with the TBL model. This research aims to examine the impact of team-based learning on whether or not students were able to build their own learning processes, as well as to measure student satisfaction with teaching and learning in the TBL paradigm in order to improve further TBL classrooms in the faculty.
II. METHODS
A. Sampling and Participants
In 2022, 387 pre-clinic medical students from Chiang Mai University’s Faculty of Medicine were studied (222 from Year 2 and 165 from Year 3). Year 2 medical students studied human skin and the connective tissue system, while Year 3 medical students studied human haematology. Each TBL class consisted of 50 teams of mixed-gender and grades. Each team contained five members.
B. Structure and Components of TBL
The TBL programme was first implemented in the 2022 academic year, covering preclinical academic Years 2 and 3 at the Faculty of Medicine, Chiang Mai University. The TBL structure comprised two major phases: pre-class and in-class. The TBL topics included automated haematology and venomous snakes for Year 3 medical students. The skin infection topic was selected for Year 2 medical students.
After TBL, the non-researcher academic team informed medical students about the study and sought volunteers to avoid a conflict of interest between the instructors and the medical students. The non-researchers urged students interested in the experiment to complete a Google Forms questionnaire outlining the study’s relevance, including an explanation of the topic, data gathering, and the pros and cons of participation. If participants agreed to answer the questionnaire, they could complete the Google Form to consent and submit the questionnaire, with their personal information remaining anonymous.
For validity, a questionnaire to explore students’ views on TBL was prepared via a literature study, student review (two students), peer review (faculty members from two departments), and expert opinion (a TBL expert). It also examined students’ perceptions of teams and their beliefs and values in collaboration. The outcomes of the different years of student were then compared.
C. Data Collection and Analysis
Upon completing the TBL class, participant students were invited to voluntarily take the self-assessment survey to explore their thoughts on the assertions made in the TBL literature. The questionnaire was in Thai and we used a five-point Likert scale (1 = strongly dissatisfied, 2 = unsatisfied, 3 = neither satisfied nor dissatisfied, 4 = satisfied, 5 = strongly satisfied). Students were asked about the preparation for the TBL class, including student material, classroom, teaching content, self-preparation, orientation programme, class material, and the overall programme. The self-assessment survey also asked about promoting self-understanding, including communication skills, learning improvement, and enthusiasm in learning using a five-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree).
The TBL self-assessment survey data were analysed according to mean and standard deviation (SD) using STATA version 16 (STATA Corp., Texas, USA). The Pearson’s Chi-square test was used to analyze the difference between second- and third-year medical students’ percentages of satisfaction or agreement in each aspect. Statistical significance was accepted at p < 0.05. The reliability of the questionnaire was calculated using Cronbach’s alpha.
III. RESULTS
In years 2 and 3, Cronbach’s alpha of the medical students’ questionnaire was 0.869. In total, 369/387 (95.35%) participants appreciated the course structure and agreed to attend the next TBL session. Students rated the TBL class 4.44 ± 0.627 on a five-point Likert scale, with 1 being severely dissatisfied and 5 very pleased. Students also liked the classroom (4.48 ± 0.738), TBL structure (4.41 ± 0.771), and self-preparation (4.28 ± 0.780). The orientation programme, instructional material, pre-recorded video, and handouts were also well-received. Most students (69.25%, 268/387) spent 1–2 days self-preparing before the TBL class, followed by 3–4 days (24.55%, 95/387) and 5–7 days (5.43%, 21/387), while 0.78% (3/387) did not self-prepare.
On a five-point Likert scale from 1 to 5, students assessed their self-understanding progress, stating that TBL increased their communication, learning, and enthusiasm (4.50 ± 0.796, 4.41 ± 0.781, 4.46 ± 0.795).
The student t-tests revealed no significant differences between students in years 2 and 3. Except time for preparation (Pearson’s Chi-square test; p < 0.005), medical students in years 2 and 3 had similar self-assessment survey scores. In addition, Year 3 medical students also scored better in enthusiasm for studying than Year 2 medical students in increasing self-understanding (Student t-test; p = 0.023) (Table 1).
|
|
Year 2 |
Year 3 |
p-value |
|
Student satisfaction towards the TBL class |
|||
|
Agree to attend the next TBL class: % (n) |
95.95% (213/222) |
94.55% (156/165) |
0.519 |
|
Classroom: mean (SD) |
4.49 (0.671) |
4.47 (0.823) |
0.903 |
|
TBL structure: mean (SD) |
4.38 (0.73) |
4.45 (0.822) |
0.377 |
|
Orientation programme: mean (SD) |
4.46 (0.628) |
4.40 (0.810) |
0.417 |
|
Teaching material: mean (SD) |
4.67 (0.568) |
4.56 (0.578) |
0.064 |
|
Student preparation time: mean (SD) |
4.20 (0.788) |
4.40 (0.755) |
0.012 |
|
Time for preparation: % (n) 1–2 days 3–4 days 5–7 days No preparation |
80.18% (178/222) 14.41% (32/222) 4.50% (10/222) 0.90% (2/222) |
54.55% (90/165) 38.18% (63/165) 6.67% (11/165) 0.61% (1/165) |
< 0.005 |
|
Promotion of learning skills |
|||
|
Communication skills: mean (SD) |
4.46 (0.734) |
4.56 (0.674) |
0.154 |
|
Understanding of the topics: mean (SD) |
4.36 (0.729) |
4.47 (0.845) |
0.180 |
|
Enthusiasm for learning: mean (SD) |
4.38 (0.797) |
4.56 (0.783) |
0.023 |
|
Cronbach’s alpha |
0.869 |
0.869 |
|
Table 1. Comparison between the satisfaction of medical students in years 2 and 3 towards the TBL class and agreement to the promotion of self-understanding
IV. DISCUSSION
TBL changes how students learn by encouraging them to become more accountable by preparing for the team assurance test and application exercise (Burgess et al., 2020a). Teacher-directed pre-class preparation for advanced tasks may involve reading textbooks, reference articles, or instructor-created material while the readiness assurance test enhances students’ enthusiasm for TBL (Parmelee et al., 2012). However, students may resist TBL or active learning because it varies from passive lecture-based learning. Teachers must be aware of this and advocate TBL-style learning to improve ability and encourage students to be more prepared. This research examines the attitudes of medical students towards the two courses post-TBL and provides valuable input on TBL strategies, regardless of the course schedule.
Student feedback can improve teaching and student satisfaction. Students agreed that TBL can improve communication, learning, and passion. Second-year medical students were less motivated than third-year (p = 0.023), implying they need to focus on the core content of the preclinical module rather than TBL preparation, while third years have more time management experience for pre-class self-study. Students liked the teaching material because, in addition to textbooks, the instructors prepared PowerPoint presentations, recorded VDOs, and documentation, allowing those with different learning styles to make the appropriate choice.
Interestingly, both classes found the TBL structure and location less satisfying, possibly because first-time students could not comprehend group activities. Students can further grasp the TBL framework and enjoy the structured process with a revamped instructional layout and additional classes. As for the classroom, the seat layout may prevent suitable group conversations, with a small-group or smart classroom being more appropriate for TBL.
The preparation time satisfaction results are significantly difference, with Year 2 students being considerably less satisfied than Year 3 (p = 0.012). Most second-year medical students spent one to two days planning, and third years one to four (p = 0.005), primarily because the third-year course was longer. Second-year medical students attended a two-week course on human skin and the connective tissue system with a TBL class in the second week, whereas third years took a five-week haematological system course with a TBL class in the fourth week. Both classes received course material on Mondays, while the TBL was on Fridays in the same week. Second-year medical students may need to study the basic science aspects and be unable to independently assess the pre-class material, whereas third-year students had more time. Accordingly, a TBL course should last at least three to four weeks to allow medical students to understand the basic TBL instructional material and independently assess it.
This study has limitations. The questionnaire was expert-evaluated without instructor facilitation. In addition, our study focused on students’ satisfaction with TBL, hence we didn’t include academic outcomes to prove the value of TBL.
V. CONCLUSION
The survey showed that students appreciated TBL-based learning since it helped them to work together and embrace learning, while potentially improving their study skills. A diversity of pre-class material allows students to choose learning tactics depending on their individual abilities. Students found the activity venue inadequate and classroom improvements would boost their satisfaction level.
Notes on Contributors
KW reviewed the literature, designed the study, analysed data, co-wrote the manuscript, critically reviewed and edited the manuscript, and then read it through prior to final approval.
WD reviewed the literature, analysed the data, co-wrote the manuscript, and critically reviewed and edited the manuscript.
WR gave critical feedback on the writing of the manuscript.
AS and KL provided scientific insight and advice, and critically reviewed and edited the manuscript.
Ethical Approval
This research was approved by the institutional ethics committee of the Faculty of Medicine at Chiang Mai University (Study code: PAT-2565-09243).
Data Availability
On reasonable request, the corresponding author will provide data to support the conclusions of this study. Due to privacy and ethical considerations, the data cannot be made public.
Acknowledgement
The authors wish to express their sincere appreciation to Ms. Naorn Sriwangdang for assisting with the preparation of the research proposal.
Funding
This study was supported by the Faculty of Medicine, Chiang Mai University, grant no. 062-2566.
Declaration of Interest
The authors confirm they have no potential conflicts of interest.
References
Burgess, A., Bleasel, J., Hickson, J., Guler, C., Kalman, E., & Haq, I. (2020a). Team-based learning replaces problem-based learning at a large medical school. BMC Medical Education, 20, Article 492. https://doi.org/10.1186/s12909-020-02362-4
Burgess, A., van Diggele, C., Roberts, C., & Mellis, C. (2020b). Team-based learning: Design, facilitation and participation. BMC Medical Education, 20(Suppl 2), Article 461. https://doi.org/10.1186/s12909-020-02287-y
Burgess, A. W., McGregor, D. M., & Mellis, C. M. (2014). Applying established guidelines to team-based learning programs in medical schools: A systematic review. Academic Medicine, 89(4), 678–688. https://doi.org/10.1097/ACM.0000000000000162
Michaelsen, L. K., & Sweet, M. (2008). The essential elements of team-based learning. New Directions for Teaching and Learning, 2008(116), 7–27. https://doi.org/10.1002/tl.330
Parmelee, D., Michaelsen, L. K., Cook, S., & Hudes, P. D. (2012). Team-based learning: A practical guide: AMEE Guide No. 65. Medical Teacher, 34(5), e275–e287. https://doi.org/10.3109/0142159X.2012.651179
*Komson Wannasai
Department of Pathology,
Faculty of Medicine,
Chiang Mai University,
110 Inthavaroros road, Sriphume
Meaung, Chiang Mai, 50200
+6653935442
Email: komson.wanna@gmail.com
Submitted: 9 February 2023
Accepted: 15 May 2023
Published online: 3 October, TAPS 2023, 8(4), 23-35
https://doi.org/10.29060/TAPS.2023-8-4/OA3006
Sethapong Lertsakulbunlue1, Kaophiphat Thammasoon2, Kanlaya Jongcherdchootrakul3, Boonsub Sakboonyarat3 & Anupong Kantiwong1
1Department of Pharmacology, Phramongkutklao College of Medicine, Thailand; 2Department of Personnel Administration Division, Phramongkutklao College of Medicine, Thailand; 3Department of Military and Community Medicine, Phramongkutklao College of Medicine, Thailand
Abstract
Introduction: Although medical research (MR) is constantly promoted, a global deficit of medical researchers has been noted. We aimed to explore the relationship among practice, perceptions, attitudes, barriers and motivation toward MR and its impacts on MR publication.
Methods: A cross-sectional study included 262 senior medical students and interns. An electronic, standardised Likert scale questionnaire was used to collect the data. Binary logistic regression was used to determine the odds ratio between characteristics and MR publication. Confirmatory factor analysis was used to confirm the loading factor of each question, and structural equation modeling (SEM) was used to investigate the relationship between latent variables and MR publication.
Results: Cronbach’s alpha revealed a good internal reliability of 0.93. The accumulated grade point average did not differ between those who had published and those who had not. MR presentations were strongly associated with MR publication. SEM showed that attitudes (0.71, p<0.001) and perceptions (0.27, p<0.001) had a direct effect on practices. Practices (0.49, p<0.001) and attitudes (0.30, p<0.001) had a direct effect on motivation, while motivation had a total effect = 0.36, p<0.001 on MR publication through MR presentation as a mediator.
Conclusion: Positive attitudes and perceptions might lead to positivity in the intention to practice MR, which would lead to motivation and finally increase the odds of MR publication. Different approaches to promote excitement and perceptions in MR learning should be encouraged by teachers and faculty members.
Keywords: Medical Research, Students, Perceptions, Attitudes, Barriers, Motivation
Practice Highlights
- Enjoyment and excitement should be promoted while learning medical research.
- Medical research experiences enhanced publication, particularly medical research presentations.
- Extracurricular medical research activities should be routinely promoted.
- Facilitators in medical research might be tailor-made for each individual.
- Regular meetings regarding medical research with mentors or role models should be held.
I. INTRODUCTION
Health-related research is constantly promoted and has gained great importance over time (Sobczuk et al., 2022). However, a global shortage of medical researchers was noted despite an increasing demand for them (Funston et al., 2016). For example, in the US, the proportion of medical researchers has declined from approximately 4.7% to 1.5% in the 1980s and 2014, respectively (Carberry et al., 2021; Davila, 2016; Puljak, 2007). Several barriers toward conducting medical research (MR) have been reported among undergrads and postgraduates. For instance, lack of allotted time, lack of physician engagement in research early during medical students’ training, and lack of mentoring and guidance (Bonilla-Escobar et al., 2017; El Achi et al., 2020; Habineza et al., 2019; Okoduwa et al., 2018). To resolve these problems, medical education has globally incorporated research methods and epidemiology into its curriculum (Carberry et al., 2021). Nevertheless, only a minority of medical students had reached the primary goal of research, namely publishing (Bonilla-Escobar et al., 2017; Carberry et al., 2021; Laidlaw et al., 2012).
Factors associated with MR publication have been identified. Students from highly ranked undergraduate institutions were more likely to achieve publication. Mentors also played an important role in increasing the likelihood of publication. For example, a student working with a mentor with a PhD degree or a mentor with prior publication(s) with prior mentee(s) increases the chance of achieving publication (Parker et al., 2021). Medical students participating in an extracurricular scientific activity, such as the Scientific Society of Medical Students, or who take a scientific writing skills course, were also associated with greater odds of producing a scientific publication (Valladares-Garrido et al., 2022).
One of the main reasons researchers conduct a study is because of what they believe (Lev et al., 2010). Attitudes toward and barriers against health research influence research success (Lev et al., 2010; Memarpour et al., 2015; Osman, 2016). Attitudes and motivations toward a particular type of study also showed a positive relationship with achievement (Ma & Xu, 2004; Özer, 2020; Simpson & Oliver, 1990). Furthermore, a theory of success describes perception leading to passion, and the continuation of passion leading to obsession, which drives an individual to succeed (Dange, 2016; Schellenberg et al., 2022).
Previously, several studies reported descriptive data on attitudes, practices, knowledge levels, perceptions, motivation and barriers involving research among medical and science students (AlGhamdi et al., 2014; Al-Shalawy & Haleem, 2015; Arif et al., 2018; El Achi et al., 2020; Habineza et al., 2019; Memarpour et al., 2015; Osman, 2016; Pallamparthy & Basavareddy, 2019). Even though these factors are known to affect one’s behaviour, to our knowledge, research on whether these factors are associated with research publications among medical students is scarce.
Without research, no breakthroughs can be achieved in managing disease. Therefore, strategies to enhance medical students’ appreciation of research and publication should be promoted. As a step toward this goal, our study aimed to determine the relations between MR practices, perceptions, attitudes, barriers and motivation toward medical research and their effect on MR publications among senior medical students and internists graduated from Phramongkutklao College of Medicine, Thailand. Furthermore, we also explore the differences in the characteristics and MR experiences of the participants between the publishing group and the non-publishing group. The goal involved influencing future research and actions to increase research publications among physicians in the country and contribute to medical practices.
II. METHODS
A. Study Design and Subjects
A cross-sectional study based on a self-administered survey was conducted at Phramongkutklao College of Medicine (PCM), Bangkok, Thailand. The survey was distributed among senior medical students, including fourth-, fifth-, and sixth-year students and internists who graduated from PCM. The total number of senior medical students and internists was 292 and approximately 250 interns, respectively. The curriculum at PCM is spread out over six years, with the first three being pre-clinical years spent studying basic science and the last three being clinical years spent developing clinical experiences. An introductory module about MR is mandatory in three years of the curriculum in the third, fourth, and sixth years of medical school. Firstly, third-year medical students learn the basics of MR, such as basic study designs focusing on quantitative methods, data analysis, and research proposal development. Furthermore, students learn about public health aspects, including community participation. Secondly, fourth-year medical students learn more about advanced study designs and are more focused on conducting a study and multivariate analysis. Fourth-year students were divided into eight groups of approximately twelve to conduct a community-based research proposal before finalizing their project as a report. Finally, sixth-year medical students were divided into pairs or a group of three to conduct medical research to improve medical care in a community hospital setting. Then the research is presented, and a manuscript report is submitted. However, an MR publication was not mandatory. After they graduated, the students were sent to both Thai Army hospitals and government hospitals run by the Ministry of Public Health to work as interns.
The present study included senior medical students and internists due to their similar MR experiences. First, both groups were enrolled within the same curriculum paradigm. Second, the MR presentation and publications are according to the willingness of the student, as MR publications and presentations are not mundane. Finally, almost all the published research among the population is from projects developed during their fourth and sixth years as medical students. Therefore, several projects were published during the internship.
B. Data Collection
We used an electronic standardised questionnaire, including six parts: short answer questions for obtaining demographic data; a 5-score Likert scale questionnaire on practice, perceptions, attitudes, barriers, and motivation toward MR. The questionnaire was translated using related published work that is relevant to this paper, as well as the investigators’ experience and context of PCM (El Achi et al., 2020; Funston et al., 2016; Habineza et al., 2019; Ichsan et al., 2018; Kamwendo, 2002; Okoduwa et al., 2018; Pallamparthy & Basavareddy, 2019). In addition, five expert professors examinedthe content validity and reliability of the questionnaire; pilot testing was conducted among 66 first year medical students and Cronbach’s alpha score ranged from 0.74-0.93.Then the questionnaire was launched in November and December of 2022 as a Google Form and advertised via social media to the study population. Information sheets, objectives, and methods of the study were provided on the first page of the Google Form, which participants were asked to read carefully before agreeing to participate. The questionnaire was then self-completed and took, on average, about 10–15 minutes to complete. The finalised Cronbach’s alphas were 0.83, 0.84, 0.74, 0.89, 0.88, and 0.93 for practices, perceptions, attitudes, barriers, motivation and overall questions, respectively.
Practice was defined as their willingness or intention to practice MR (El Achi et al., 2020). Perceptions are how the student perceives the importance of MR, while attitude is how they feel about conducting MR (El Achi et al., 2020; Funston et al., 2016). Barriers are defined as what the students perceive as being resistant to conducting MR; on the other hand, motivations are what they perceive as facilitating conducting MR (Habineza et al., 2019; Okoduwa et al., 2018).
C. Statistical Analysis
All data were downloaded from Google Forms, and data analyses were performed using StataCorp, 2021, Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC. A frequency distribution of demographic characteristics was performed to describe the study subjects. Categorical data were presented as percentages, and continuous variables were presented as means and standard deviations (SD). Univariable and multivariable logistic regression analysis was used to determine the odds ratio (OR) and adjusted odds ratio (AOR) with a 95% confidence interval (CI) of the association between the characteristics and MR experiences of the participants and the MR publication. All statistical tests were two-sided, and a p-value less than 0.05 was considered statistically significant.
The structural equation modeling (SEM) using maximum likelihood extraction was done to find out how the latent variables, including practice, perceptions, attitudes, barriers, and motivation, were related and what effect it had on MR publications. The procedure is comprised of two steps. The first is validating the measurement model, which is carried out primarily using confirmatory factor analysis (CFA), and the other is fitting the structural model, which is achieved primarily through path analysis of latent variables. CFA was applied to demonstrate the impact of each question (observed variable) on different beliefs toward MR (latent variable) and presented as a lambda. Questions with a low factor loading (below 0.60) were excluded from the SEM. During the SEM construction, questions with factor loadings below 0.60 were also removed. In the final model, there are 17 observed variables included within the SEM. The samples/observed variable were 15.41, which is more than 10, indicating adequate sample size for SEM (Wolf et al., 2013). The SEM was carried out to investigate the relationship among latent variables and their impact on MR publication in our study population.The six following indices were used to evaluate model fit: (1) the chi-square test, χ2; (2) the chi-square test over degree of freedom (df), χ2/df (3) the comparative fit index, CFI; (4) the Tucker–Lewis index, TLI (5) the root-mean square error of approximation, RMSEA; and (6) the root-mean square residual, (SRMR). All these indices indicated a proposed fit for SEM data. A χ2/df lower than 2, CFI greater than 0.95, TLI greater than 0.95, RMSEA less than 0.06 and SRMR less than 0.06 each indicated a good fit between the data and the hypothesised model.
III. RESULTS
A. Characteristic of Participants
Table 1 demonstrates the characteristics of participants stratified by MR publishing. A total of 139 senior medical students and 123 interns participated in the survey. The response rate was 47.6% and 49.2% for senior medical students and interns, respectively. Over one-fifth (22.1%) of the participants had published MR and were mostly internists (81.0%). Approximately 60% of the participants were male, corresponding to an enrolment at PCM of 60 male and 40 female students. The accumulated grade point average (GPAX) was approximately the same at 3.4±0.3 among both published and those who had not published. Regarding, MR experience or roles served during medical student years, being a group leader (AOR: 2.12, 95% CI: 0.97 to 4.64, p=0.06) was associated with MR publishing. Finally, those having experience in MR presentation, whether oral or poster, and international or national presentation, were strongly associated with MR publishing, with adjusted odds ratios of 4.34 (p<0.001) shown in Table 2.
|
Characteristics |
Non-Published |
Published |
|
n (% of 204) |
n (% of 58) |
|
|
Demographics |
||
|
Sex |
||
|
Male |
119 (58.3) |
37 (63.8) |
|
Female |
85 (41.7) |
21 (36.2) |
|
Educational level |
||
|
Clinical year |
128 (62.7) |
11 (19.0) |
|
Intern |
76 (37.3) |
47 (81.0) |
|
Accumulated grade point average (GPAX) |
||
|
Mean ± SD |
3.4±0.3 |
3.4±0.3 |
|
Medical research participation |
||
|
MR elective |
59 (28.9) |
15 (25.9) |
|
Time spent on MR (hours/week) |
||
|
<1 |
119 (58.3) |
27 (46.6) |
|
1-5 |
56 (27.5) |
17 (29.3) |
|
5-10 |
15 (7.4) |
7 (12.1) |
|
>10 |
14 (6.9) |
7 (12.0) |
|
Extra curriculum research activity |
39 (19.1) |
23 (39.7) |
|
Academic club activity |
30 (14.7) |
13 (22.4) |
|
MR experience during medical student |
||
|
Group leader |
45 (22.1) |
24 (41.4) |
|
Design MR |
89 (43.6) |
34 (58.6) |
|
Proposal writing |
142 (69.6) |
45 (77.6) |
|
Data enter |
126 (51.5) |
41 (70.7) |
|
Data analysis |
99 (48.5) |
34 (58.6) |
|
Literature review |
125 (61.3) |
42 (72.4) |
|
Manuscript writing |
76 (37.3) |
33 (56.9) |
|
None |
7 (3.4) |
2 (3.4) |
|
National MR presentation |
||
|
Oral presentation |
23 (11.3) |
22 (37.9) |
|
Poster presentation |
22 (10.8) |
22 (37.9) |
|
International MR presentation |
||
|
Oral presentation |
7 (3.4) |
8 (13.8) |
|
Poster presentation |
9 (4.4) |
15 (25.9) |
|
Published national MR |
0 (0) |
29 (50.0) |
|
Published international MR |
0 (0) |
37 (63.8) |
MR: Medical Research
Table 1. Characteristics of participants stratified by medical research publishing experience (N=262)
|
Characteristics |
Non-Published |
Published |
OR |
95% CI |
p-value |
AOR |
95% CI |
p-value |
|
n (% of 204) |
n (% of 58) |
|||||||
|
Sex |
||||||||
|
Male |
119 (58.3) |
37 (63.8) |
ref |
ref |
||||
|
Female |
85 (41.7) |
21 (36.2) |
0.79 |
0.43-1.45 |
0.455 |
0.76 |
0.37-1.56 |
0.458 |
|
Educational level |
||||||||
|
Clinical year |
128 (62.7) |
11 (19.0) |
ref |
ref |
||||
|
Intern |
76 (37.3) |
47 (81.0) |
3.09 |
1.74-5.50 |
<0.001 |
6.67 |
3.12-14.28 |
<0.001 |
|
Accumulated grade point average (GPAX) |
||||||||
|
Mean±SD |
3.4±0.3 |
3.4±0.3 |
1.02 |
0.40-2.59 |
0.971 |
0.417 |
0.12-1.41 |
0.159 |
|
Extra curriculum research activity |
39 (19.1) |
23 (39.7) |
2.78 |
1.48-5.23 |
0.002 |
1.47 |
0.62-3.46 |
0.379 |
|
MR experience during medical student |
||||||||
|
Group Leader |
45 (22.1) |
24 (41.4) |
2.49 |
1.34-4.63 |
0.004 |
2.12 |
0.97-4.64 |
0.060 |
|
MR presentation |
||||||||
|
No |
170 (83.3) |
27 (46.6) |
ref |
ref |
||||
|
Yes |
34 (16.7) |
31 (53.5) |
5.74 |
3.05-10.82 |
<0.001 |
4.34 |
1.99-9.47 |
<0.001 |
MR: Medical Research, OR: Odds Ratio, AOR: Adjusted Odds Ratio, CI: Confidence interval
Table 2. Univariable and multivariable analysis of characteristics and medical research experiences by medical research publishing experience (N=262)
B. Confirmatory Factor Analysis of Practices, Perceptions, Attitudes, Barriers and Motivation toward Medical Research
Table 3 demonstrates the confirmatory factor analysis (CFA) of practices, perceptions, attitudes, barriers and motivation Likert scores and MR publishing experience. In the practice section, all questions had a loading factor of approximately 0.80. The loading factors for perception range from 0.74 to 0.79, except for two questions: (1) research or publication should be mandatory and (2) research experience should be a criterion for residency training. For the attitude section, the CFA found that MR is exciting and MR is enjoyable, with high impacts of 0.89 and 0.87, respectively, followed by MR being valuable and essential for the medical profession, with loading factors of 0.58 and 0.54, respectively. However, for the questions where MR is complicated and time-consuming, the loading factor was relatively low, under 0.30. Regarding barriers, lack of exposure and opportunities, training and support, mentoring and guidance, and lack of personal knowledge of the research process all had a high loading factor of over 0.70. Lack of statistical support, funding, and lack of rewards or motivations had relatively lower loading factors between 0.60 and 0.69. For motivation, pursuit of further education, pursuit of personal interest, improving their potential in research skills, having mentor guidance/role model and to be a part of solving medical problems in society had high loading factors over 0.70.
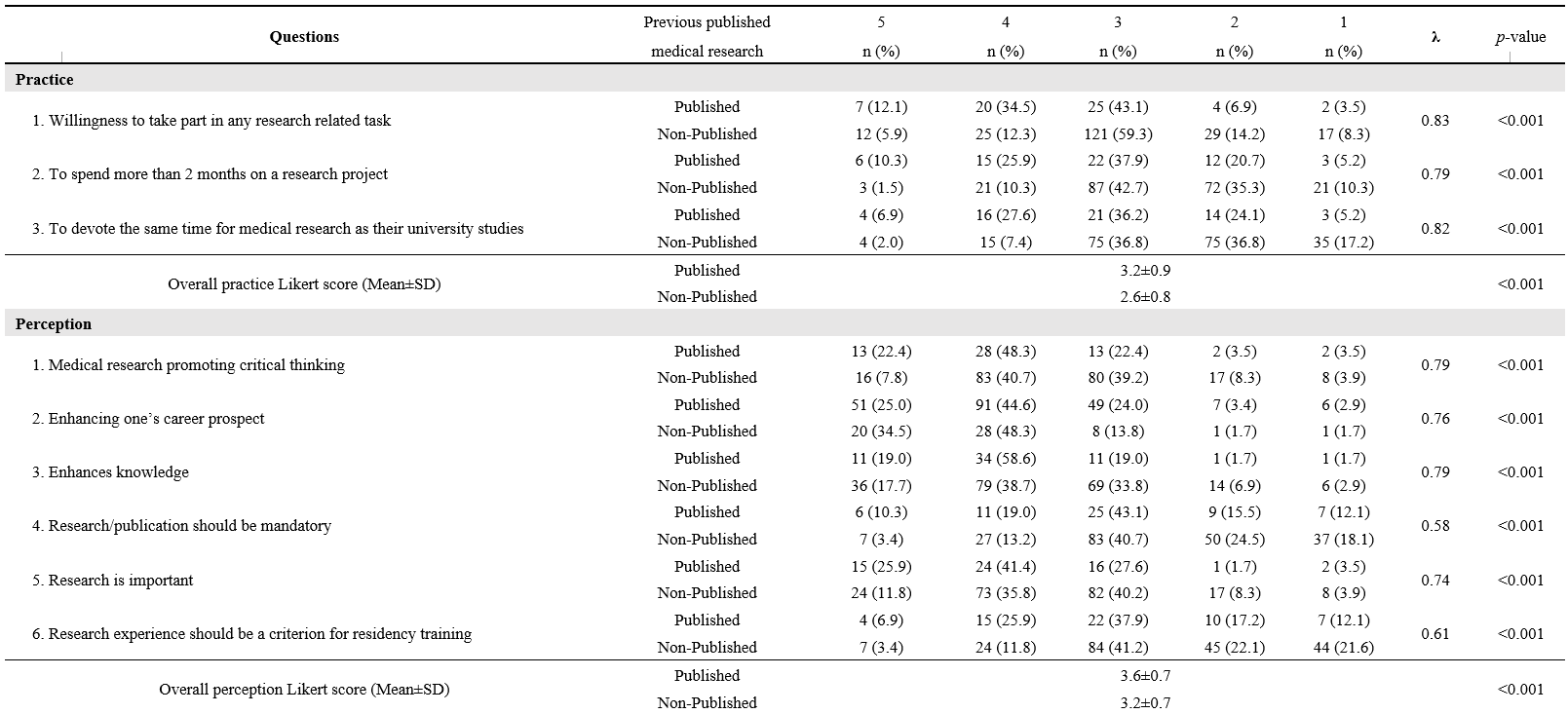
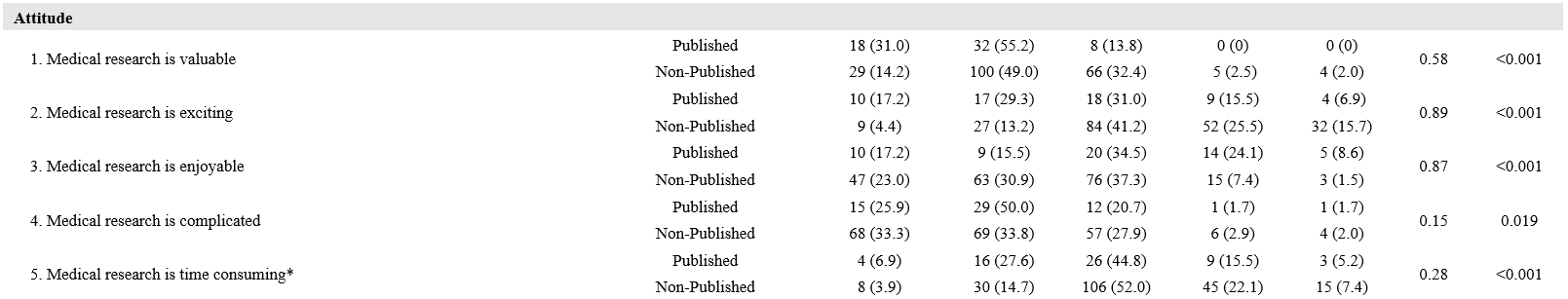
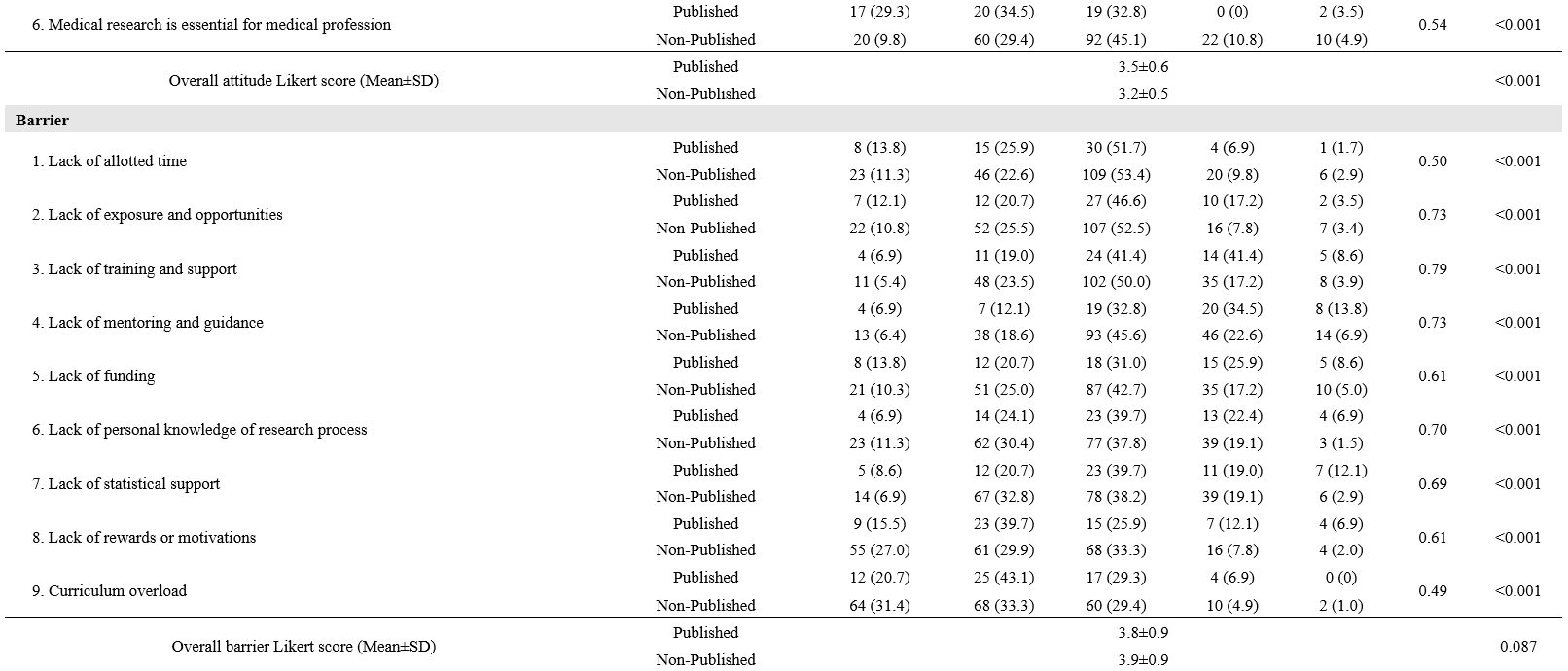
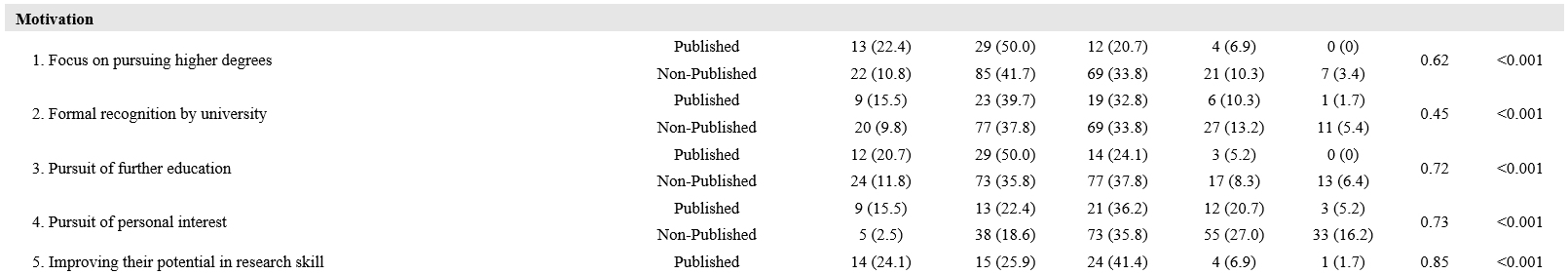
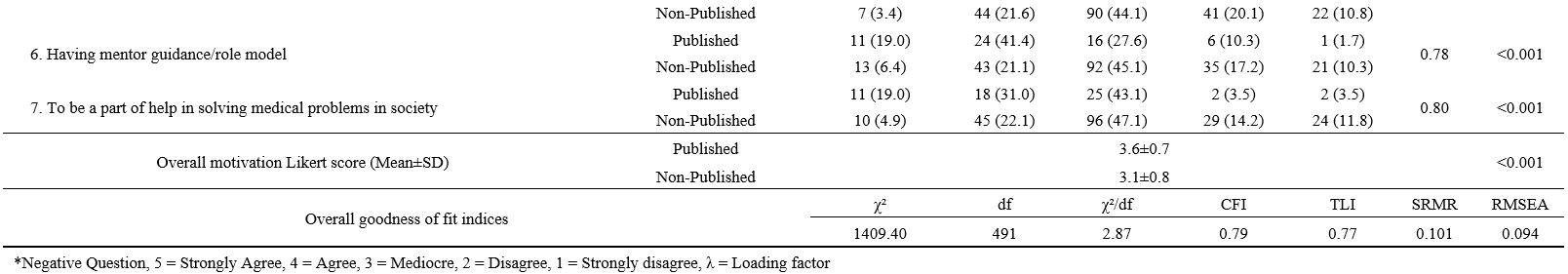
Table 3. Confirmatory factor analysis of practice, perception, attitude, barrier and motivation Likert-score and medical research publishing experience
C. SEM of Practices, Perceptions, Attitudes, Barriers and Motivation and MR Publishing
The SEM is developed from five latent variables, leading to the outcome, including medical research presentation and publication (Figure 1). We found that perception has a direct effect on both practices (0.27, p<0.001) and motivation (0.12, p= 0.087). Perceptions and attitudes also correlated (0.57, p<0.001). Practices and attitudes have a direct effect on motivation, 0.49 and 0.30, respectively (p<0.001 for both). The indirect effect of attitudes through practices on motivation was 0.71 * 0.49 = 0.35, all coefficients p<0.001. Practices also exhibited a direct negative effect on barriers (-0.13, p= 0.072). Regarding our primary outcome, both motivation and, surprisingly, barriers also revealed a positive direct effect on MR publishing (0.28, p<0.001 for motivation and 0.15, p= 0.014 for barriers). The MR presentation experience also showed a direct effect on MR publication (0.26, p<0.001). Furthermore, MR presentation also acted as a mediator for motivation, with an indirect effect of 0.08 and a total effect of motivation on MR publication of 0.36. The SEM model provided a good fit for the data (χ²/df= 1.67, CFI= 0.96, TLI= 0.95, RMSEA= 0.05, SRMR= 0.05).
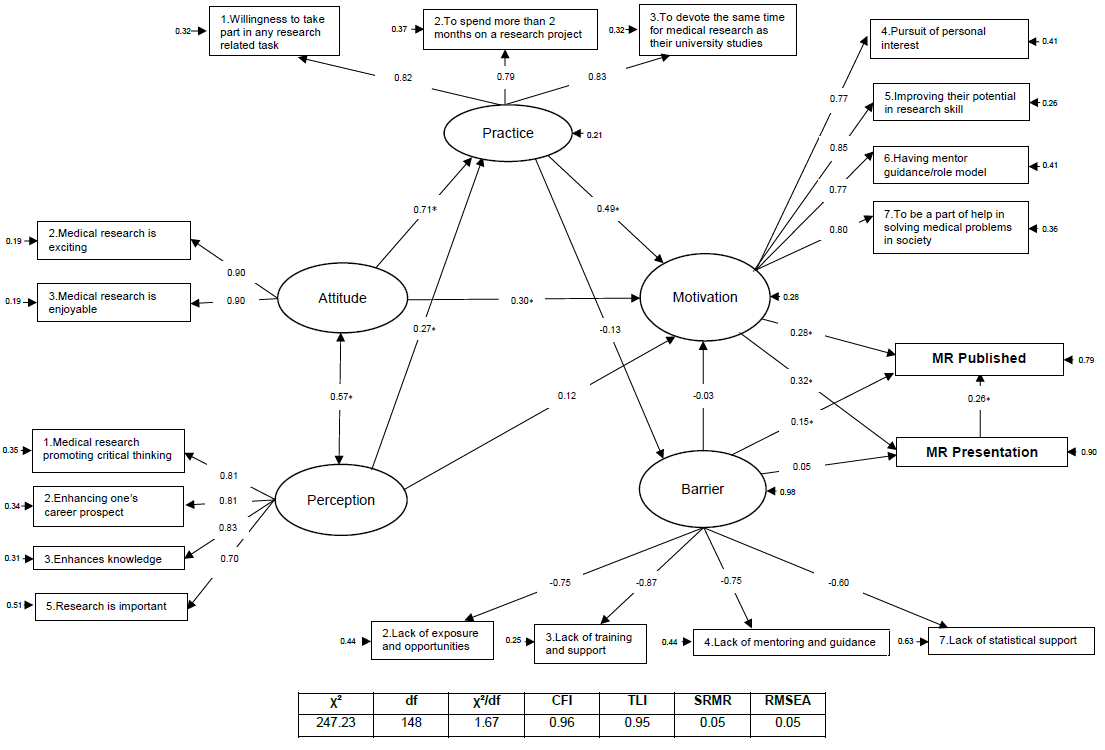
*= P<0.05
Figure 1. SEM of practices, perceptions, attitudes, barriers and motivation and MR publishing
IV. DISCUSSION
We successfully enrolled 139 PCM senior medical students, and 123 interns graduated from PCM. This study is the first to formulate a SEM on the relationship between practices, perceptions, attitudes, motivation and barriers to MR publication and presentation. We found that attitudes, practices and motivation significantly contribute to MR publication and presentation. The roles and experiences that medical students have in medical research during their medical student years are also important to the success of MR publications. However, because our population only includes those who have studied or are studying at PCM, additional external validation may be required.
This study described how baseline characteristics and MR experiences were associated with MR publication. Unsurprisingly, a higher proportion of interns had published MR. GPAX, on the other hand, were not associated with MR publication, which is a common factor in a relative study with positive associations toward perceptions, attitudes and practices (El Achi et al., 2020). A large study in China also reported that research engagement was associated with improving overall learning outcomes (Zhang et al., 2022). This controversy may be explained by two reasons. First, the time required for developing MR and publications is large and might interfere with normal curriculum activity. A study in Colombia noted that their students believed that they could obtain higher GPAs if they were not involved in research (Bonilla-Escobar et al., 2017). The latter is that MR skills and academic skills might not completely overlap. While MR engagement might improve science, scholarship, and professionalism, other domains, such as clinical practice, require more time and effort to learn (Zhang et al., 2022).
MR experiences and roles during MR learning also play an important part in MR publication. Experience in MR presentation was strongly associated with MR publication. This may be partially explained by the student’s readiness before the research presentation; students need to be highly knowledgeable about their own research, and knowledge is a key to success and behavioural change (Bettinghaus, 1986; Pengpid et al., 2016). Furthermore, presentation requires planning, preparation, creating visual aids, and practicing one’s presentation skills. The effort and time spent on this process might be motivation to achieve a higher goal, namely publication. Our study demonstrates that MR presentations, whether nationally, internationally, oral, or poster, are highly associated with MR publication. Thus, MR presentations should be promoted.
Those who had been group leaders had a higher chance of MR publication. During the PCM curriculum, the group leader for MR conduct was never assigned and was elected in each group. Northouse mentioned two forms of leadership: assigned and emergent. Those assigned leadership positions were given the role of group leader. When an individual is perceived as one of the most influential members of a group or organization, that person is exhibiting emergent leadership (Northouse, 2021). Medical leadership development was seen to improve outcomes at the individual, organizational and clinical levels (Lyons et al., 2021). Several leadership training programs in medicine and clinical practices were widely visible. However, to our knowledge, no curriculum focusing on medical research leadership was available.
Perception is described as a method for identifying and interpreting the environment and the meaning of sensual motivations. Cognition may influence perception, which can also occur subconsciously and without cognizance (Saini et al., 2020). Some literature has been carried out showing perceptions, attitudes, and motivation toward research among medical students, in which those with positive perceptions mostly had positive attitudes and motivation (AlGhamdi et al., 2014; El Achi et al., 2020; Osman, 2016). These were similar to our research showing that perception impacts positively on practices and motivation.
In line with the current study, the theory of planned behaviour describes that one’s attitude and how they perceive the behaviour directly affect their intention to perform the behaviour (Bosnjak et al., 2020). The SEM also demonstrated that perception and attitude directly affect the population’s intention to conduct MR (practice). Moreover, a study in Turkey on the predictiveness of attitude and motivation on achievement (vocational English course scores) found a significant positive relationship between attitude and motivation, attitude and achievement, and motivation and achievement (Özer, 2020). Therefore, a positive attitude may positively impact their motivation and their willingness to practice MR. The feeling that MR is exciting and enjoyable had the greatest impact on the attitude domain. Hence, activities that increase the excitement and joy of conducting MR should be encouraged.
The main factors impacting MR publication are motivation, practices, attitudes and perceived barriers. Based on the health-belief model (HBM), providing motivation as needed might help students overcome the triggers of MR barriers so that correct thoughts and perceptions about MR will arise. Thus, techniques derived from motivational interviews might be a useful option for encouraging students toward MR publication (Tober, 2013). One of the most important motivations in our study is having a mentor or role model, and the lack of a mentor constitutes a high-impact barrier. Therefore, mentors should play an important role in guiding their students toward research success. Based on motivational interview techniques, active listening might be the key skill for mentors to better understand their students’ motivations and empower them toward success (Rollnick et al., 2010).
Surprisingly, our study showed that perceived barriers had a positive impact on MR publication. The perception of a barrier greatly influences the likelihood of an individual’s uptake of that behaviour (Becker & Maiman, 1975). Usually, a barrier is a resistance to achieving a goal, which negatively affects achievement. However, the barriers included in our study consisted of a lack of exposure and opportunities, training and support, mentoring and guidance, and statistical support. As a result, those who had not yet published any medical research may not have had the prestige of encountering these barriers, which is why they are perceived as insignificant.
The practice domain included three questions: (1) willingness to participate in any research-related task; (2) willingness to spend more than two months on a research project; and (3) willingness to devote the same amount of time to medical research as they did to their university studies, indicating a willingness to practice medical research. Willingness is the quality or state of being prepared to accomplish something. A study in China about speaking English demonstrated that the willingness to communicate is directly related to motivation and mastery approach (Turner et al., 2021). Furthermore, passion and obsession are what drive an individual to succeed (Dange, 2016).
In view of all the factors presented, mentors have an important role to play in guiding and facilitating the students’ acquisition of adequate experience in medical research during their medical school years. A good extracurricular MR learning environment might be needed to ensure statistical confidence and exposure to conducting research. Actively listening to students and empowering and motivating them to break through barriers may result in successful MR publications. In addition, a different approach to learning MR might be needed to promote attitudes, perceptions and motivations toward MR. According to Self-Determination Theory (SDT), when students perceive that the primary purpose of learning is to obtain external rewards, such as exam grades, they may perform less well due to a detrimental effect on their intrinsic motivation (Deci et al., 1999).
SDT revealed that three basic needs must be fulfilled to empower one’s attitude and motivation, including autonomy, competence, and a feeling of belonging (Deci et al., 1999). To promote these basic needs, faculty members could provide extracurricular research time, give choice to research topics and mentors, and hire students to be research assistants, if possible, to promote their autonomy (Rosenkranz et al., 2015). Competence could be enhanced by early research skills introduction and practical training (Rosenkranz et al., 2015). Research mentors may play a crucial role in fostering a sense of belonging toward MR by promoting well-functioning group work through guidance and evaluation (Dorrance et al., 2008). Furthermore, portfolios, logbooks and reflective journals are particularly useful to improve the students’ attitude and motivation (Taylor & Hamdy, 2013). Constant positive feedback from mentors during MR activities is encouraged to improve the learning environment (Peifer et al., 2020). A different approach to learning MR might also benefits the MR learning environment, for example, through game-based learning and other collaborative learning models (Blakely et al., 2009).
The present study encountered several limitations. First, the study included only senior medical students and interns who graduated from PCM, so the model might not be accurately applied to other universities with different curricula and further validation might be needed. Even though most participants who had published a MR were interns (81%), the medical research published was composed while they were medical students. Second, the study was a cross-sectional study, and causal relationships were unavailable. However, according to PCM curricula, for most participants, the MR presentation and their experience with medical research came before the MR publication. Furthermore, personal beliefs change over time, and recall bias might have affected the study results. (Seitz et al., 2017). The beliefs elicited by the questionnaire comprised the participants’ current beliefs, rather than beliefs formed during their participation in medical research publications. As a result, our study investigated only the participants’ current beliefs and their impact on the publication of medical research. A further prospective cohort or qualitative study on whether the students’ current beliefs toward MR are related to successful MR publication is encouraged. Finally, because only participants who volunteered to take part in the study were included, selection bias may also be a significant limitation of this study. Our study had considerable strengths, there had been no reports describing practices, perceptions, attitudes, motivation and barriers toward medical research. However, this is the first study to formulate a SEM model displaying factors related to MR publication.
V. CONCLUSION
Medical research experience and positive practices or willingness, perception, attitude, and motivation in medical research might pave the road to a successful MR publication. Medical research experience and extracurricular activities should be supported by both teachers and faculties through active policies. A different approach to medical research learning might also be needed to promote enjoyment and excitement. Finally, external validation needs to be explored to generalise the model.
Notes on Contributors
SL reviewed the literature, designed the study, collected the data, data analysis and wrote the manuscript. KT, KJ and BS collected the data, developed the methodology framework and developed the manuscript. AK reviewed the literature, designed the study, data analysis and wrote the first draft.
Ethical Approval
The study was approved by the Medical Department Ethics Review Committee for Research in Human Subjects, Institutional Review Board, Royal Thai Army (Approval no. S060q/65_Exp), according to the international guidelines including the Declaration of Helsinki, the Belmont Report, CIOMS Guidelines, and the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use – Good Clinical Practice (ICH-GCP). A documentation of informed consent was used, and was granted permission by the Institutional Review Board, RTA Medical Department.
Data Availability
The datasets used and/or analysed during the current are available from https://doi.org/10.6084/m9.figshare.22128725
Acknowledgement
We thank professors Mathirut Mungthin, Ram Rangsin Panadda Hattachote, Phunlerd Piyaraj and Picha Suwannahitatorn for validating our questionnaire and providing support. This work would not have been possible without the active support of Phramongkutklao College of Medicine and its academic leaders.
Funding
The authors report that there is no funding associated with the work featured in this article.
Declaration of Interest
The authors declare they have no competing interests.
References
AlGhamdi, K. M., Moussa, N. A., AlEssa, D. S., AlOthimeen, N., & Al–Saud, A. S. (2014). Perceptions, attitudes and practices toward research among senior medical students. Saudi Pharma- ceutical Journal, 22(2), 113–117. https://doi.org/10.1016/j.jsps.2013.02.006
Al–Shalawy, F. A.-N., & Haleem, A. (2015). Knowledge, attitudes and perceived barriers towards scientific research among undergraduate health sciences students in the central province of Saudi Arabia. Education in Medicine Journal, 7(1), e16-e21. https://doi.org/10.5959/eimj.v7i1.266
Arif, A., Siddiqui, M. A., Aziz, K., Shahid, G., Shiekh, A., & Fahim, M.F. (2018). Perception towards research among undergraduate physical therapy students. Biometrics & Biostatistics International Journal, 7(3), 171–175. https://doi.org/10.15406/bbij.2018.07.00206
Becker, M. H., & Maiman, L. A. (1975). Sociobehavioral determinants of compliance with health and medical care recommendations. Medical Care, 13(1), 10–24. https://doi.org/10.1097/00005650–197501000–00002
Bettinghaus, E. P. (1986). Health promotion and the knowledge–attitude–behavior continuum. Preventive Medicine, 15(5), 475–491. https://doi.org/10.1016/0091–7435(86)90025–3
Blakely, G., Skirton, H., Cooper, S., Allum, P., & Nelmes, P. (2009). Educational gaming in the health sciences: Systematic review. Journal of Advanced Nursing, 65(2), 259–269. https://doi.org/10.1111/j.1365-2648.2008.04843.x
Bonilla–Escobar, F. J., Bonilla–Velez, J., Tobón–García, D., & Ángel–Isaza, A. M. (2017). Medical student researchers in Colombia and associated factors with publication: A cross–sectional study. BMC Medical Education, 17(1), Article 254. https://doi.org/10.1186/s12909–017–1087–9
Bosnjak, M., Ajzen, I., & Schmidt, P. (2020). The theory of planned behavior: Selected recent advances and applications. Europe’s Journal of Psychology, 16(3), 352–356. https://doi.org/10.5964/ejop.v16i3.3107
Carberry, C., McCombe, G., Tobin, H., Stokes, D., Last, J., Bury, G., & Cullen, W. (2021). Curriculum initiatives to enhance research skills acquisition by medical students: A scoping review. BMC Medical Education, 21(1), Article 312. https://doi.org/10.1186/s12909–021–02754–0
Dange, J. K. (2016). Perception, passion and obsession: The three elements of theory of success. International Journal of Advanced Education and Research, 1(7), 1–3.
Davila, J. R. (2016). The physician–scientist: Past trends and future directions. Michigan Journal of Medicine, 1(1), 66-73. https://doi.org/10.3998/mjm.13761231.0001.112
Deci, E. L., Koestner, R., & Ryan, R. M. (1999). A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychological Bulletin, 125(6), 627–668. https://doi.org/10.1037/0033-2909.125.6.627
Dorrance, K. A., Denton, G. D., Proemba, J., La Rochelle, J., Nasir, J., Argyros, G., & Durning, S. J. (2008). An internal medicine interest group research program can improve scholarly productivity of medical students and foster mentoring relationships with internists. Teaching and Learning in Medicine,20(2), 163–167. https://doi.org/10.1080/10401330801991857
El Achi, D., Al Hakim, L., Makki, M., Mokaddem, M., Khalil, P. A., Kaafarani, B. R., & Tamim, H. (2020). Perception, attitude, practice and barriers towards medical research among undergraduate students. BMC Medical Education, 20(1), Article 195. https://doi.org/10.1186/s12909–020–02104–6
Funston, G., Piper, R. J., Connell, C., Foden, P., Young, A. M. H., & O’Neill, P. (2016). Medical student perceptions of research and research–orientated careers: An international questionnaire study. Medical Teacher, 38(10), 1041–1048. https://doi.org/10.3109/0142159X.2016.1150981
Habineza, H., Nsanzabaganwa, C., Nyirimanzi, N., Umuhoza, C., Cartledge, K., Conard, C., & Cartledge, P. (2019). Perceived attitudes of the importance and barriers to research amongst Rwandan interns and pediatric residents – A cross–sectional study. BMC Medical Education, 19(1), Article 4. https://doi.org/10.1186/s12909–018–1425–6
Ichsan, I., Wahyuniati, N., McKee, R., Lobo, L., Lancaster, K., & Redwood–Campbell, L. (2018). Attitudes, barriers, and enablers towards conducting primary care research in Banda Aceh, Indonesia: A qualitative research study. Asia Pacific Family Medicine, 17(1), Article 8. https://doi.org/10.1186/s12930–018–0045–y
Kamwendo, K. (2002). What do Swedish physiotherapists feel about research? A survey of perceptions, attitudes, intentions and engagement. Physiotherapy Research International, 7(1), 23–34. https://doi.org/10.1002/pri.238
Laidlaw, A., Aiton, J., Struthers, J., & Guild, S. (2012). Developing research skills in medical students: AMEE Guide No. 69. Medical Teacher, 34(9), 754–771. https://doi.org/10.3109/0142159X.2012.704438
Lev, E. L., Kolassa, J., & Bakken, L. L. (2010). Faculty mentors’ and students’ perceptions of students’ research self-efficacy. Nurse Education Today, 30(2), 169–174. https://doi.org/10.1016/j.nedt.2009.07.007
Lyons, O., George, R., Galante, J. R., Mafi, A., Fordwoh, T., Frich, J., & Geerts, J. M. (2021). Evidence–based medical leadership development: A systematic review. BMJ Leader, 5(3), 206–213. https://doi.org/10.1136/leader–2020–000360
Ma, X., & Xu, J. (2004). Determining the causal ordering between attitude toward mathematics and achievement in mathematics. American Journal of Education, 110(3), 256–280. https://doi.org/10.1086/383074
Memarpour, M., Fard, A. P., & Ghasemi, R. (2015). Evaluation of attitude to, knowledge of and barriers toward research among medical science students. Asia Pacific Family Medicine, 14(1), Article 1. https://doi.org/10.1186/s12930–015–0019–2
Northouse, P. G. (2021). Leadership: Theory and practice (9th ed.). SAGE publications.
Okoduwa, S. I. R., Abe, J. O., Samuel, B. I., Chris, A. O., Oladimeji, R. A., Idowu, O. O., & Okoduwa, U. J. (2018). Attitudes, perceptions, and barriers to research and publishing among research and teaching staff in a Nigerian research institute. Frontiers in Research Metrics and Analytics, 3, Article 26. https://doi.org/10.3389/frma.2018.00026
Osman, T. (2016). Medical students’ perceptions towards research at a Sudanese University. BMC Medical Education, 16(1), Article 253. https://doi.org/10.1186/s12909–016–0776–0
Özer, S. (2020). The predictiveness of attitude and motivation on achievement in ESP: The mediating role of anxiety. International Journal of Curriculum and Instruction, 12(2), 25-41.
Pallamparthy, S., & Basavareddy, A. (2019). Knowledge, attitude, practice, and barriers toward research among medical students: A cross–sectional questionnaire–based survey. Perspectives in Clinical Research, 10(2), 73.
Parker, S. M., Vona-Davis, L. C., & Mattes, M. D. (2021). Factors predictive of publication among medical students participating in school-sponsored research programs. Cureus, 13(9), e18176. https://doi.org/10.7759/cureus.18176
Peifer, C., Schönfeld, P., Wolters, G., Aust, F., & Margraf, J. (2020). Well done! Effects of positive feedback on perceived self-efficacy, flow and performance in a mental arithmetic task. Frontiers in Psychology,11, Article 1008. https://doi.org/10.3389/fpsyg.2020.01008
Pengpid, S., Peltzer, K., Puckpinyo, A., Tiraphat, S., Viripiromgool, S., Apidechkul, T., Sathirapanya, C., Leethongdee, S., Chompikul, J., & Mongkolchati, A. (2016). Knowledge, attitudes, and practices about tuberculosis and choice of communication channels in Thailand. Journal of Infection in Developing Countries, 10(7), 694-703. https://doi.org/10.3855/jidc.6963
Puljak, L. (2007). An overlooked source of physician–scientists. Journal of Investigative Medicine, 55(8), 402–405. https://doi.org/10.2310/6650.2007.00029
Rollnick, S., Butler, C. C., Kinnersley, P., Gregory, J., & Mash, B. (2010). Motivational interviewing. BMJ, 340, c1900. https://doi.org/10.1136/bmj.c1900
Rosenkranz, S. K., Wang, S., & Hu, W. (2015). Motivating medical students to do research: A mixed methods study using self-determination theory. BMC Medical Education, 15, Article 95. https://doi.org/10.1186/s12909-015-0379-1
Saini, M., Kumar, A., & Kaur, G. (2020). Research perception, motivation and attitude among undergraduate students: A factor analysis approach. Procedia Computer Science, 167, 185–192. https://doi.org/10.1016/j.procs.2020.03.210
Schellenberg, B. J. I., Gaudreau, P., & Bailis, D. S. (2022). Lay theories of obsessive passion and performance: It all depends on the bottom line. Personality and Individual Differences, 190, Article 111528. https://doi.org/10.1016/j.paid.2022.111528
Seitz, R. J., Paloutzian, R. F., & Angel, H.-F. (2017). Processes of believing: Where do they come from? What are they good for? F1000Research, 5, Article 2573. https://doi.org/10.12688/f1000research.9773.2
Simpson, R. D., & Oliver, J. S. (1990). A summary of major influences on attitude toward and achievement in science among adolescent students. Science Education, 74(1), 1–18. https://doi.org/10.1002/sce.3730740102
Sobczuk, P., Dziedziak, J., Bierezowicz, N., Kiziak, M., Znajdek, Z., Puchalska, L., Mirowska–Guzel, D., & Cudnoch–Jędrzejewska, A. (2022). Are medical students interested in research? – Students’ attitudes towards research. Annals of Medicine, 54(1), 1538–1547. https://doi.org/10.1080/07853890.2022.2076900
Taylor, D. C. M., & Hamdy, H. (2013). Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Medical Teacher, 35(11), e1561–e1572. https://doi.org/10.3109/0142159X.2013.828153
Tober, G. (2013). Motivational interviewing: Helping people change. Alcohol and Alcoholism, 48(3), 376–377. https://doi.org/10.1093/alcalc/agt010
Turner, J. E., Li, B., & Wei, M. (2021). Exploring effects of culture on students’ achievement motives and goals, self–efficacy, and willingness for public performances: The case of Chinese students’ speaking English in class. Learning and Individual Differences, 85, Article 101943. https://doi.org/10.1016/j.lindif.2020.101943
Valladares–Garrido, M. J., Mejia, C. R., Rojas–Alvarado, A. B., Araujo–Chumacero, M. M., Córdova–Agurto, J. S., Fiestas, J., Rojas–Vilar, F. J., & Culquichicón, C. (2022). Factors associated with producing a scientific publication during medical training: Evidence from a cross–sectional study of 40 medical schools in Latin America. F1000Research, 9, Article 1365. https://doi.org/10.12688/f1000research.26596.2
Wolf, E. J., Harrington, K. M., Clark, S. L., & Miller, M. W. (2013). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educational and Psychological Measurement, 76(6), 913–934. https://doi.org/10.1177/0013164413495237
Zhang, G., Wu, H., Xie, A., & Cheng, H. (2022). The association between medical student research engagement with learning outcomes. Medical Education Online, 27(1), Article 2100039. https://doi.org/10.1080/10872981.2022.2100039
*Anupong Kantiwong
317 Ratchawithi Rd,
Thung Phaya Thai,
Ratchathewi, Bangkok 10400
+66909838338
E-mail: anupongpcm31@gmail.com
Submitted: 2 December 2022
Accepted: 24 July 2023
Published online: 3 October, TAPS 2023, 8(4), 13-22
https://doi.org/10.29060/TAPS.2023-8-4/OA3093
Julie Yun Chen1,2, Tai Pong Lam1, Ivan Fan Ngai Hung3, Albert Chi Yan Chan4, Weng-Yee Chin1, Christopher See5 & Joyce Pui Yan Tsang1
1Department of Family Medicine and Primary Care, University of Hong Kong, Hong Kong; 2Bau Institute of Medical and Health Sciences Education, University of Hong Kong, Hong Kong; 3Department of Medicine, University of Hong Kong, Hong Kong; 4Department of Surgery, University of Hong Kong, Hong Kong; 5School of Biomedical Sciences, The Chinese University of Hong Kong, Hong Kong
Abstract
Introduction: Medical students have long provided informal, structured academic support for their peers in parallel with the institution’s formal curriculum, demonstrating a high degree of motivation and engagement for peer teaching. This qualitative descriptive study aimed to examine the perspectives of participants in a pilot peer teaching programme on the effectiveness and feasibility of adapting existing student-initiated peer bedside teaching into formal bedside teaching.
Methods: Study participants were senior medical students who were already providing self-initiated peer-led bedside clinical teaching, clinicians who co-taught bedside clinical skills teaching sessions with the peer teachers and junior students allocated to the bedside teaching sessions led by peer teachers. Qualitative data were gathered via evaluation form, peer teacher and clinician interviews, as well as the observational field notes made by the research assistant who attended the teaching sessions as an independent observer. Additionally, a single Likert-scale question on the evaluation form was used to rate teaching effectiveness.
Results: All three peer teachers, three clinicians and 12 students completed the interviews and/or questionnaires. The main themes identified were teaching effectiveness, teaching competency and feasibility. Teaching effectiveness related to the creation of a positive learning environment and a tailored approach. Teaching competency reflected confidence or doubts about peer-teaching, and feasibility subthemes comprised barriers and facilitators.
Conclusion: Students perceived peer teaching effectiveness to be comparable to clinicians’ teaching. Clinical peer teaching in the formal curriculum may be most feasible in a hybrid curriculum that includes both peer teaching and clinician-led teaching with structured training and coordinated timetabling.
Keywords: Peer Teaching, Undergraduate Medical Education, Bedside Teaching, Medical Students
Practice Highlights
- Peer-led teaching environment facilitates questions and answers from learners to strengthen learning.
- Training on specific skills and pre-case preparation can help improve peer teacher effectiveness.
- Clear understanding of the logistics and expectations is necessary to optimise the process.
- Formal peer teacher training may help quality assurance and encourage more participation.
I. INTRODUCTION
In accordance with the longstanding apprenticeship model of medical training, senior doctors and trainees have been responsible for teaching their junior colleagues across the continuum of medical education. Despite this accepted practice, peer teaching has not become widely formalised in undergraduate medical curricula.
Peer teaching has been shown to be beneficial at multiple levels. For students who are being taught by peers, learning is enabled by social and cognitive congruence because of the near-peer demographic which allows for a more comfortable learning environment for free flow of discussion and better understanding of the learner’s challenges including awareness of the primacy for exam success (Benè & Bergus, 2014; Rees et al., 2016). The peer teacher develops and hones teaching skills that will be useful in internship (Haber et al., 2006) and through teaching, develops higher motivation and deeper understanding of concepts and perhaps also improve their own exam performance (Burgess et al., 2014). The institution derives some practical benefit from the supplementary manpower (Tayler et al., 2015) due to the comparable effectiveness of peer teachers in teaching in certain areas such as physical examination and communication skills (Rees et al., 2016) but perhaps most importantly, it benefits from building a collaborative relationship with students in their learning process. Though the benefits of peer teaching have been noted, students remain an untapped resource as training provided for students to serve as teachers is inconsistent (Soriano et al., 2010).
Undergraduate medical curricula aim to provide a foundation for future training and the framework for such curricula are guided by the recognition that medical students must achieve certain outcomes, including being able to teach, to be prepared for future practice. Well-accepted frameworks such as the ‘Outcomes for Graduates’, from the UK General Medical Council (2015) and the ‘CanMEDS Framework’ from the Royal College of Physicians and Surgeons of Canada (2015) expect medical graduate to teach others. In Hong Kong, similar guidance is provided in the document ‘Hong Kong Doctors’ published by the Medical Council of Hong Kong, which states that undergraduate medical education must prepare graduates to fulfil the roles of ‘medical practitioner, communicator, educator…’ (Medical Council of Hong Kong, 2017).
It is common in medical schools to have informal peer teaching, where senior students coach junior students on an ad hoc basis or organise revision sessions before exams. Zhang et al. (2011) revealed that a majority of medical students believed that informal learning approaches, including the use of past student notes, and participation in self-organised study groups and peer-led tutorials, helped them pass examinations and be a good doctor. Similarly, in our institution, these kinds of informal peer teaching are popular among students and include sharing sessions on study and exam tips, bedside sessions, and sharing of organised study notes. These activities are not subject to any formal oversight.
With the documented benefits of peer teaching, the availability of enthusiastic senior students who are willing to coach their junior peers, and the demand from junior students to learn from their seniors, there is an opportunity to harness the potential peer teaching that is already taking place. This pilot project is important as it aimed to adapt existing student-initiated peer bedside teaching into the formal bedside teaching curriculum and to examine the perspectives of participants on the effectiveness and feasibility of this initiative. It will be helpful to understand the benefits and drawbacks of formal peer bedside teaching in order to further develop this pedagogical approach in medical education.
II. METHODS
This was a descriptive qualitative study of participants in a pilot peer-teaching initiative for bedside teaching implemented in the first clinical year of study for medical students.
A. Setting
1) Small group bedside teaching for Year 4 medical students in the Clinical Foundation Block: The 11-week Clinical Foundation Block (CFB) of the MBBS Year 4 curriculum at The University of Hong Kong runs from August to October and is the first block of the first clinical year of study. It serves to prepare students for the ward- and clinic-based teaching to follow in the clinical clerkships (Figure 1). Year 4 medical students were selected for the study because it is the first clinical year of study when clinical bedside teaching begins. In addition, as the most junior clinical students, they would benefit most from learning from their senior peers. During the CFB, all Year 4 students learn basic history taking, physical examination and clinical skills as well as common clinical problems of 10 key specialty disciplines. In internal medicine, students attend whole class sessions in which the proper clinical examination of each body system is demonstrated followed by seven small group sessions at the bedside for hands-on practice led by a clinician.
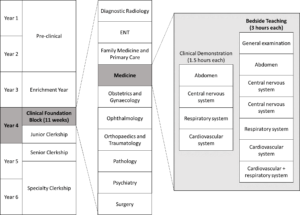
Figure 1. Teaching activities under Medicine within the Clinical Foundation Block in the medical curriculum
Each small group bedside teaching session is comprised of six to eight CFB students who follow the same clinical teacher to examine 3 pre-selected ward patients over a two-hour period. In this pilot study, a peer teacher joined the clinical teacher for the bedside teaching with the first patient case taught by the clinician, the second case taught by the peer teacher under the supervision of the clinician and the final case taught by the peer teacher alone.
2) Peer teaching recruitment and training: Over the years, medical students have been organising bedside peer-teaching on their own and we identified these peer-teaching leaders to help recruit peer teachers for this initiative. Peer teachers recruited in July 2018 and comprised Year 5 students in Senior Clerkship, who were enthusiastic in teaching, and were available to join the training tutorial and take up a subsequent Year 4 CFB bedside teaching session. During the 2.5-hour tutorial, the CFB Coordinator explained the project, and three clinicians then provided a briefing on cardiovascular, neurological, respiratory and abdominal physical examination, common pitfalls, and how to give feedback. There was also time for students to raise questions both on the project and bedside teaching techniques.
B. Participants
The target participants included the three peer teachers who were recruited for this study, together with the three clinician partners and the 24 CFB students in the corresponding three bedside teaching groups. Written informed consent was obtained from all participants before data collection.
C. Data Collection
The qualitative data were collected using a dual subjective (peer teachers, clinicians and students) and objective (independent observer) approach was taken to provide a more holistic perspective of the peer teaching experience. A research assistant not involved in the teaching followed one (of the three) peer teachers as the independent observer. All peer teachers and clinicians were interviewed in-person, by phone or by email, using an interview guide (Appendix 1) by the research assistant after the session where field notes were taken and transcribed. CFB students were invited to complete an evaluation form comprised of open-ended questions and a single Likert-scale question (Appendix 2) immediately after the bedside session, to rate effectiveness and to give general feedback about the peer teaching session.
D. Data Analysis
The qualitative data comprising interview field notes, interview transcripts, email transcripts and open-ended questions from the evaluation form collected from CFB students were analysed thematically by the authors JC and JPYT. The Likert-scale question from the evaluation form was analysed using descriptive statistics. All data were anonymised.
III. RESULTS
All three peer teachers and three clinicians who participated in the pilot peer teaching sessions were interviewed. Eighteen out of 24 CFB students consented to participate and 12 completed questionnaires were collected. Three main themes were identified with two corresponding subthemes for each.
A. Teaching Effectiveness
Peer teachers were rated favourably in terms of their teaching effectiveness. From the evaluation form completed by CFB students, the mean peer teaching effectiveness rating was 4.5/5. While a few students felt the teaching effectiveness of clinicians and peer teachers was comparable, many of them felt less intimidated being taught by the peer teachers. Students also appreciated that the peer teachers understood their current level of understanding and therefore were able to make the teaching more effective by tailoring it to their needs. Students found the experience-sharing by the peer teachers an added-value as shown in Table 1 (Item 1-4). All clinicians agreed that the CFB students appeared more relaxed while the peer teachers were teaching, and the peer teachers met their standard of professionalism as shown in Table 1 (Item 3).
|
Subtheme: Learning environment |
|
1. ‘I was more willing to ask questions.’ – CFB Student 8 |
|
2. ‘I felt more comfortable and less intimidate[ed] with the peer teacher.’ – CFB Student 12 |
|
3.‘I think it is pretty well received among the CFB students – they looked like they are more comfortable and less stressed.’ – Clinician B |
|
Subtheme: Tailoring to needs |
|
4.‘We were told her past experience.’ – CFB Student 9 |
|
5.‘More exam advice from peer tutor.’ – CFB student 10 |
Table 1. Exemplar quotes from participants on teaching effectiveness
These comments were congruent with the observations of the independent observer. When the clinician was teaching, students appeared to be cautious when performing physical examination and answering questions from the clinician. On the other hand, when the peer teacher was teaching, students were asking for reassurance while performing physical examination, and appeared less hesitant when attempting to answer the questions. The peer teacher sometimes also asked the students how they would do a certain examination before they actually performed it. He also shared his own bedside experience. After the clinician ended the bedside session and left, the peer teachers stayed behind and answered further questions from the students regarding physical examination skills and examination tips.
B. Teaching Competence
For students, the teaching on physical examination skills by peer teacher appeared to be comparable to that by clinicians, with the perceived benefit of tailored instructions to student’s current level, and additional personal experience sharing as shown in Table 2 (Item 1-2).
After co-teaching with the peer teacher, clinicians had different opinions about the competency of an undergraduate student as a formal peer teacher. Two stated that it was more appropriate for senior students to do sharing instead of teaching, while the other was satisfied with the ability of the peer teachers to teach, and appreciate the opportunity to exchange ideas with peer teachers. One clinician also suggested that peer teachers might need more practice on teaching to build up confidence as shown in Table 2 (Item 3, 6 and 7).
On the other hand, all the peer teachers expressed that they felt stressed being observed by the clinicians. Two of them felt confident to teach, while one was less confident and prefer to co-teach with a clinician as shown in Table 2 (Item 4, 5 and 8).
The peer teachers also questioned their role as a peer teacher in the regular curriculum. They were unsure to teach in place of clinicians in the regular bedside sessions for the CFB students, yet were more comfortable to co-teach with the clinicians, or to teach in unofficial or supplementary peer-led sessions as shown in Table 2 (Item 4, 8 and 9).
|
Subtheme: Confidence in teaching competence |
|
1. ‘Very comprehensive teaching; detailed explanation on how to report findings.’ – CFB Student 1 |
|
2. ‘Senior students know what we need to know and what we don’t know at this stage.’ – CFB Student 5 |
|
3. ‘The peer teacher was sufficiently prepared on content knowledge and teaching skills.’ – Clinician A |
|
4. ‘I am confident with my knowledge and teaching skills. The CFB cases were easy enough for me to handle. I have been teaching student-initiated sessions anyway.’ – Peer Teacher A |
|
5. ‘Are we going to replace the clinicians? The student-initiated sessions worked just fine.’ – Peer Teacher B |
|
Subtheme: Doubts on teaching competence |
|
1. ‘It is too early for the current peer teachers to teach as they lack competency and confidence in teaching.’ – Clinician B |
|
2. ‘Tutors should be at least medical graduates who have shown evidence of proficiency and knowledge in the areas that they teach. Senior students can share their experience of learning, but not to teach.’ – Clinician C |
|
3. ‘The clinicians are definitely better at teaching and has better skills… It would work better if I was to co-teach with a clinician but not to teach solo.’ – Peer Teacher C |
|
4. ‘It isn’t appropriate to take away the proper learning opportunity to be taught by clinicians from the students.’ – Peer Teacher C |
Table 2. Exemplar quotes from participants on teaching competency
C. Feasibility
1) Barriers: One of the peer teachers was disappointed that the session did not go as planned. He suspected that the clinicians may not truly understand the purpose and the plan for the project, and hence sometimes took the lead when the peer teachers were supposed to be teaching as shown in Table 3 (Item 1).
They also mentioned that timetabling conflicts between CFB and Senior Clerkship were also an issue. For all groups, the session overran and resulted in peer teachers missing their own class, which was scheduled immediately following the intended finishing time of this bedside session.
Peer teachers also commented that there was no concrete incentive for them to join the project. With the added pressure of being observed by clinicians, most peer teachers were hesitant to volunteer again.
2) Facilitators: One peer teacher considered it as an extra learning opportunity as shown in Table 3 (Item 2). Clinicians also believed that the peer teachers could benefit since these were essentially extra tutorials and bedside exposure for them outside of the regular curriculum although students thought that the cases used for CFB were too easy for them to learn anything new. Both peer teachers and clinicians agreed that more practical training on physical examination would be beneficial to boost the confidence and competence of the peer teachers in teaching. Peer teachers suggested that to make the session more efficient, they would prefer to clerk the case themselves before the session, to be better prepared to recognise abnormal physical signs shown in Table 3 (Item 3). A pre-meeting between the peer teacher and the partner clinician would be helpful to clarify expectations and understanding of the process since the training tutorial was conducted by a different clinician. A clinician pointed out that an open call should be made for the recruitment to allow all interested students to participate.
|
Barriers |
|
1. ‘I felt like the clinician did not want to let me teach solo. Maybe he did not understand the project.’ – Peer Teacher A |
|
Facilitators |
|
2. ‘The organisation of the curriculum is weird – there were a lot to learn in the Medicine Block of the Junior Clerkship, but not much in that of Senior Clerkship. There was also a large gap of time where there was no supervised physical examination at bedside. This is a good refresher session for me.’ – Peer Teacher C |
|
3. The students and I all saw the case for the first time during the session. I felt a bit unprepared and can only comment on the physical examination skills of the students. There is no way to tell if they reported the correct findings. It would help if the peer tutors can clerk the case before the session.’ – Peer Teacher C |
Table 3. Exemplar quotes from participants on barriers and facilitators
IV. DISCUSSION
This pilot project aimed to examine the effectiveness and feasibility of adapting peer bedside teaching into the formal curriculum. Student rating has been used as the primary measure of teaching effectiveness in many schools (Chen & Hoshower, 2003). In this project, we triangulated student ratings with clinician viewpoint and also that of an independent observer to assess teaching effectiveness. All found the teaching by the peer teachers was professional and comparable to clinicians.
Their views were also congruent to the observation that peer teaching provided a more relaxed learning environment as cited in the literature (Tai et al., 2016). This is reflected in a study on problem-based learning (PBL) that showed student tutor-led tutorials were rated more highly in group functioning and supportive atmosphere, compared with faculty-led sessions (Kassab et al., 2005).
Sharing from peer teachers was also identified as a bonus feature of bedside peer teaching in our study. Sharing from senior students not only provide junior student with practical exam and ward survival tips, but also served as inspiration and motivation for students to learn. Again this has also been observed in other studies such as one in which students whose peer teachers shared real life experiences performed better in a post-training CPR knowledge test, and demonstrated more confidence and learning motivation (Souza et al., 2022).
In the next incarnation of peer teaching the barriers and facilitators noted by stakeholders need to be addressed. The difficulty in scheduling can be overcome by engaging senior students who are already on the ward to teach by embedding this requirement as part of their usual work. A clinical peer-assisted learning programme by Nikendei, et al. (Nikendei et al., 2009) had demonstrated a successful peer teaching programme at the bedside with final year medical students who were working in the wards as tutors. The comment among peer teachers that there is no ‘concrete incentive’ to being a peer teacher may be due a lack of awareness of the appreciation from peer learners as well as from faculty teachers. More regular and deliberate sharing of learner feedback and role modelling the enjoyment of teaching by teachers and experienced peer teachers can help. Reflecting on the benefits of the learning process undertaken through the preparation and ‘paying forward’ the efforts from other teachers are also less tangible (but important!) factors to emphasise to encourage future students to undertake peer-teaching.
Peer teachers and clinicians should meet before the teaching session to clarify aims and logistics, and match their expectations. To improve peer teacher confidence and to alleviate clinician concern about their competency to teach, more extensive and formal training can be provided to peer teachers, including both theoretical and practical training on physical examination, and on teaching skills. Burgess et al. (2017) had developed and implemented an interprofessional Peer Teaching Training (PTT) programme for medicine, pharmacy and health sciences students, which aimed to develop students’ skills in teaching, assessment and feedback for peer assisted learning and future practice. The PTT course design was adapted by Karia et al. (Karia et al., 2020) for medical students only. Both programmes were shown to be effective in improving students’ confidence and competence in peer teaching, and increasing intention to participate in teaching. This is encouraging and we are also developing a structured peer teaching training programme to fill this gap. Nevertheless, when attempting to include peer teachers in the formal curriculum as a complement to formal teaching by the faculty care must be taken to not over-formalise the process which may undermine the unique benefits of peer teaching (Tong & See, 2020).
A. Strengths and Limitations
This was a small-scale pilot study and the evaluation of the impact was limited to perceptions and feedback from stakeholders and did not include tangible outcomes such as academic performance and clinical competency of participants. However, the objective contemporaneous observations made during the teaching sessions by a third-party researcher strengthened the trustworthiness of the data. A 360-degree evaluation including feedback from patients and ward staff could also provide a more comprehensive evaluation.
V. CONCLUSION
This study examined the perspectives of clinicians, peer teachers and students on the effectiveness and feasibility of peer-led bedside teaching in the formal curriculum and the benefits are encouraging. Peer teaching effectiveness was comparable to clinicians with the added benefit that peer-teachers are better able to understand and meet students’ needs while creating a friendlier environment conducive to constructive learning. Concerns about peer teaching competency were expressed by clinicians and peer-teachers and all participants did not wish to have peer-teaching replace clinician-led teaching. Clinical peer teaching in the formal curriculum may be most feasible in a hybrid curriculum that includes both peer teaching and clinician-led teaching. It can be accomplished with more structured training and overcoming practical barriers of timetabling and preparation. The benefits of peer teaching and promising responses from all stakeholders support further initiatives in clinical peer teaching.
Notes on Contributors
JY Chen designed the study, performed data collection and data analysis, drafted the manuscript and approved the final manuscript.
TP Lam designed the study, gave critical feedback, read and approved the final manuscript.
IFN Hung designed the study, gave critical feedback, read and approved the final manuscript.
ACY Chan designed the study, gave critical feedback, read and approved the final manuscript.
WY Chin designed the study, gave critical feedback, read and approved the final manuscript.
JPY Tsang performed data collection and data analysis, drafted the manuscript and approved the final manuscript.
C See designed the study, gave critical feedback, read and approved the final manuscript.
Ethical Approval
This study was approved by the Institutional Review Board of the University of Hong Kong/ Hospital Authority Hong Kong West Cluster (Reference number: UW 18-439).
Data Availability
The data of this qualitative study are not publicly available due to confidentiality agreements with the participants.
Acknowledgement
We would like to thank the peer teachers, students and clinicians of HKUMed for participating in the study.
Funding
This work was supported by a Teaching Development Grant funded by The University of Hong Kong (Ref No:. N/A).
Declaration of Interest
The authors declare that there is no conflict of interest.
References
Benè, K. L., & Bergus, G. (2014). When learners become teachers: A review of peer teaching in medical student education. Family Medicine, 46(10), 783-787.
Burgess, A., McGregor, D., & Mellis, C. (2014). Medical students as peer tutors: A systematic review. BMC Medical Education, 14(1), 115.
Burgess, A., Roberts, C., van Diggele, C., & Mellis, C. (2017). Peer teacher training (PTT) program for health professional students: Interprofessional and flipped learning. BMC Medical Education, 17(1), Article 239.
Chen, Y., & Hoshower, L. B. (2003). Student evaluation of teaching effectiveness: An assessment of student perception and motivation. Assessment Evaluation in Higher Education, 28(1), 71-88.
General Medical Council. (2015). Outcomes for graduates (Tomorrow’s Doctors). Retrieved July 18, 2022 from https://www.gmc-uk.org/-/media/documents/Outcomes_for_graduates_jul_15_1216.pdf_61408029.pdf
Haber, R. J., Bardach, N. S., Vedanthan, R., Gillum, L. A., Haber, L. A., & Dhaliwal, G. S. (2006). Preparing fourth‐year medical students to teach during internship. Journal of General Internal Medicine, 21(5), 518-520. https://doi.org/10.1111/j.1525-1497. 2006.00441.x
Karia, C., Anderson, E., Hughes, A., West, J., Lakhani, D., Kirtley, J., Burgess, A., & Carr, S. (2020). Peer teacher training (PTT) in action. Clinical Teacher, 17(5), 531-537.
Kassab, S., Abu-Hijleh, M. F., Al-Shboul, Q., & Hamdy, H. (2005). Student-led tutorials in problem-based learning: Educational outcomes and students’ perceptions. Medical Teacher, 27(6), 521-526.
Medical Council of Hong Kong. (2017). Hong Kong Doctors. Retrieved July 18, 2022 from https://www.mchk.org.hk/english/publications/hk_doctors.html
Nikendei, C., Andreesen, S., Hoffmann, K., & Jünger, J. (2009). Cross-year peer tutoring on internal medicine wards: Effects on self-assessed clinical competencies–A group control design study. Medical Teacher, 31(2), e32-e35.
Rees, E. L., Quinn, P. J., Davies, B., & Fotheringham, V. (2016). How does peer teaching compare to faculty teaching? A systematic review and meta-analysis. Medical Teacher, 38(8), 829-837.
Royal College of Physicians and Surgeons of Canada. (2015). CanMEDS Framework. Retrieved July 18, 2022 from http://www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e
Soriano, R. P., Blatt, B., Coplit, L., CichoskiKelly, E., Kosowicz, L., Newman, L., Pasquale, S. J., Pretorius, R., Rosen, J. M., & Saks, N. S. (2010). Teaching medical students how to teach: a national survey of students-as-teachers programs in US medical schools. Academic Medicine, 85(11), 1725-1731.
Souza, A. D., Punja, D., Prabhath, S., & Pandey, A. K. (2022). Influence of pretesting and a near peer sharing real life experiences on CPR training outcomes in first year medical students: A non-randomized quasi-experimental study. BMC Medical Education, 22(1), 1-11.
Tai, J., Molloy, E., Haines, T., & Canny, B. (2016). Same‐level peer‐assisted learning in medical clinical placements: A narrative systematic review. Medical Education, 50(4), 469-484.
Tayler, N., Hall, S., Carr, N. J., Stephens, J. R., & Border, S. (2015). Near peer teaching in medical curricula: Integrating student teachers in pathology tutorials. Medical Education Online, 20(1), 27921.
Tong, A. H. K., & See, C. (2020). Informal and formal peer teaching in the medical school ecosystem: Perspectives from a student-teacher team. JMIR Medical Education, 6(2), e21869.
Zhang, J., Peterson, R. F., & Ozolins, I. Z. (2011). Student approaches for learning in medicine: What does it tell us about the informal curriculum? BMC Medical Education, 11(1), Article 87.
*Julie Chen
4/F William MW Mong Block
Faculty of Medicine Building
21 Sassoon RoadMarrakesh, Marrakesh-Safi,
Pokfulam, Hong Kong
Email address: juliechen@hku.hk
Submitted: 28 September 2022
Accepted: 2 March 2023
Published online: 3 October, TAPS 2023, 8(4), 5-12
https://doi.org/10.29060/TAPS.2023-8-4/OA2883
Soumia Merrou1, Abdellah Idrissi Jouicha2, Abdelmounaim Baslam3, Zakaria Ouhaz3 & Ahmed Rhassane El Adib1
1Health Sciences Research Centre (HSRC), Faculty of Medicine and Pharmacy of Marrakech, Cadi Ayyad University, Morocco; 2Health Sciences Research Centre (HSRC), Faculty of Science Semlalia, Cadi Ayyad University, Morocco; 3Pharmacology, neurobiology and behaviour Lab, Faculty of Science Semlalia, Cadi Ayyad University, Morocco
Abstract
Introduction: A deep understanding of physiology, physiopathology, pharmacology, and the management of pain is crucial for nurse anaesthetists to ensure the well-being of their patients. Thus, the teaching strategies should enhance the transition from acquiring the fundamental pain phenomena, to developing translational and critical thinking. The aim of the study is to determine if the flipped classroom that is considered an active learning approach is most effective compared to the traditional method in teaching pain management and if it improves students’ academic performance.
Methods: This study was quasi experimental, at a higher institute of nursing professions, among third-year anaesthesia resuscitation nursing students. participants were randomly allocated into either: the flipped classroom group where PBL was used (FG, n = 19), or the traditional lecture-based classroom group (TG, n = 19). The results and impact of the above approach were appreciated via the analysis of the summative assessment of the class group and from the questionnaire submitted to students.
Results: The present study revealed that in the midterm exam, the mean score of the flipped classroom group (14.0) which is significantly higher (p<0.01) than the traditional lecture group (11.9). Moreover, the standard deviation of this latter is slightly higher (2.41) which indicates scores far from the average. Also, a significant difference between the averages of the two approaches in favor of flipped classroom Group was revealed (p<0.01).
Conclusion: The assessment of student’s grades and their appreciation of both teaching approaches showed a preference for the PBL.
Keywords: Flipped Classroom, Nursing Education, Pain Management, Problem-Based Learning
Practice Highlights
- Flipped classroom showed advantageous results on nursing students’ grades.
- Flipped classroom endorsed positive results on course comprehension by nursing students.
- Flipped classroom has shown to effectively support content learning.
I. INTRODUCTION
Flipped classroom is a pedagogical approach defined as: “What was previously completed as homework is now finished in class, and what was previously completed in class is now completed at home” (Dong, 2016). Using this approach, traditional classroom time is spent on active learning strategies such as problem-based learning, games, or practice questions to allow teachers to guide students in developing strategies. critical thinking (Dong, 2016). Flipped classrooms are used as the main teaching method in the courses of health professions such as nursing theory, statistics and pharmacology (Hanson, 2016; Immekus, 2019; Peisachovich et al., 2016). In fact, there is evidence that students’ academic performance improved in midterm exams while using flipped classroom approach (Geist et al., 2015).
Despite feeling that this method increased their knowledge, nursing students said they preferred traditional lectures to the use of a flipped classroom (Hanson, 2016). It is not uncommon for students to prefer lectures to the flipped classroom method, which may be related to how much work they feel they have to do or insecurity of exam preparation or both of them (Dong, 2016; Tune et al., 2013). The use of the flipped classroom in nursing was supported by evidence that showed lecturers were enthusiastic about this method. The most effective method for implementing and assessing this strategy in nursing education, though, is not consistently supported by the available data (Barranquero-Herbosa et al., 2022; Dong, 2016; Njie-Carr et al., 2017).
Contextual learning can encourage the growth of critical reasoning, which enables students to pick out the top nursing concerns for patients from a long list of problems, ultimately fostering the development of problem-based nursing analysis in line with Benner’s model (Dong, 2016). Problem-based learning (PBL) uses problem scenarios to develop knowledge and understanding learning objectives (Wood, 2003). Among the strategies used in a flipped classroom, the PBL has been used in nursing education, in courses such as pharmacology, mental health nursing and critical care nursing (Alton, 2016; Gholami et al., 2016). Any teaching strategy that involves students in the learning process is considered to be an active learning strategy, which includes PBL (Peisachovich et al., 2016).
Despite the introduction of pain management in health professions education, pain is still undertreated. It affects 80%-90% of patients in medicine, surgery, and cancer units (Gerbershagen et al., 2009; Gianni et al., 2010). Previous research also highlighted that 43% to 51% of patients received inadequate or insufficient analgesic treatment and only 14% of patients who received analgesia benefit from reassessment (Deandrea et al., 2008; Manias et al., 2005). To effectively manage pain, nurses are crucial. Therefore, it is crucial that they receive effective training to ensure better pain management (Teike Lüthi et al., 2015).
In this direction, in order to encourage students’ acquisition strategies, nursing science professors must implement effective teaching techniques. Training typically aims to increase knowledge, which is insufficient in this case; as a result, skills development is a top priority (Kerner et al., 2013). While prior research emphasised the value of nurse-patient interactions in pain management, it undervalued the impact of nurses’ scientific knowledge of pain mechanisms and pharmacology. It is interesting to note that a recent study highlighted the significance of the classroom setting and instructional methods in approaching pain management in a novel manner (Teike Lüthi et al., 2015).
However, a need for a rigorous evaluation of learning strategies is crucial for best practices in nursing education (Barranquero-Herbosa et al., 2022; Njie-Carr et al., 2017). The present study provides an assessment of PBL as a model of applied learning in a flipped classroom of anesthesia nursing students in the context of a pain management course.
The main purpose of the study was to determine if the flipped classroom is more effective than traditional learning in teaching pain management by assessing students’ academic performance and determine their perceptions about the flipped classroom approach. In that capacity, the research questions of the study are:
- Is there a significant difference in students’ academic performance between the traditional and flipped classroom approaches on declarative knowledge?
- Is there a significant difference in students’ academic performance between the traditional and flipped classroom approaches on conditional knowledge?
- What are anesthesia and resuscitation nursing students’ perceptions of PBL impact on the acquisition and application of pain management knowledge?
- What are anesthesia and resuscitation nursing students’ perceptions of PBL as a model for learning in pain management?
II. METHODS
A. Research Design and Samples
This study is quasi experimental, and was conducted from September at a higher institute of nursing professions. The participants are third-year anaesthesia resuscitation nursing students. Participation in the study was voluntary and anonymous. Oral consent of all participants was obtained. These participants were randomly allocated into either: The flipped classroom group where PBL was used (FG, n = 19), or the traditional lecture-based classroom group (TG, n = 19). Both classroom groups had the same professor.
B. Curriculum Description
The “pain management” course (50h) is taught during the third year of nursing studies in the institute. It is composed of three parts: the pathophysiology of pain; the evaluation of pain, and the pain management.
C. Problem Based Learning on Flipped Classroom Approach
The problem-based template was designed by the professor who teaches the course, by using small groups of 5 to 6 students. The students were the facilitators of the discussion; they meet in group work to discuss a case for an hour. The objective is to identify the type of pain or to choose the best pain assessment tool for the case. The group must then suggest a drug treatment protocol and design appropriate nursing interventions. The role of the professor was to provide immediate and specific feedback during the discussion.
All cases were written by the professor. The objectives were the acquisition of knowledge and the development of clinical reasoning. Each case contained 300 words and included key patient data. Each of these cases included information that could be analysed to provide priority elements to the discussed case.
D. Data Collection and Statistical Analyses
The results and impact of the above approach were extracted via an analysis of the summative assessment of the class group and from the questionnaire submitted to students.
1) Summative assessment (exam):
Students in both groups went through two exams: midterm exam (ME) which took place in the middle of the course in the 6th week in order to assess the students’ declarative knowledge, and a final exam (FE) which took place at the end of the course, to assess conditional knowledge. The tests were graded from zero to twenty. The final score (FS) was obtained by the following equation:
FS=(ME+FE)/2
2) Questionnaire:
At the end of the course, the FG students were asked to fill out an anonymous questionnaire divided into two sections. The questions were developed in the first section of the questionnaire to determine students’ perceptions of knowledge acquisition. Elements evoked in the questionnaire were created with a language that demonstrates perceived ability and related to self-efficacy (Tune et al., 2013). The second set of items was created to determine students’ perceptions of the cases used in the course. The statements began, for example, with “Participating in the group discussions made me more confident for…”. Likert scale was used to measure the responses. The scale is presented as follows:
1 = Strongly disagree, 2 = Disagree, 3 = Neither agree nor disagree, 4 = Agree, and 5 = Strongly agree.
3) Statistical analyses:
Data analysis was performed using MS Excel (21), background variables of the study participants were calculated, and the results are presented as frequency distribution, percentages, mean, and standard deviation, statistical significance when p <0.05.
III. RESULTS
The data that support the findings of this RCT study are openly available at https://doi.org/10.6084/m9.figshare.22639279 (Merrou et al., 2023).
A. Demographics
The number of participants in the study was 38 students, 19 per group. Female students represented 79% of the study participants, whereas 21% were male.
B. Students’ Grades
Based on the data obtained, statistical analysis was done to analyse the influence of the teaching approach and the type of examination on learners’ results. The obtained findings have been presented in Tables 1 and 2. They indicate the average performance of learners in both exams: midterm (ME) and final exam (FE) where conditional knowledge is measured for both teaching approaches.
|
Type of exam |
Teaching approach |
M |
Sd |
Inf born |
Sup born |
P value |
|
ME |
TG |
11.9 |
2.41 |
7.38 |
16.1 |
<0.01 |
|
FG |
14.0 |
1.94 |
9.0 |
16.5 |
||
|
FE |
TG |
11.9 |
3.28 |
6.09 |
16 |
<0.01 |
|
FG |
14.1 |
1.96 |
10 |
16 |
Table 1. Descriptive statistics by exam type for each teaching approach.
According to Table 1, it is noted that in the midterm exam (ME), the mean score is significantly higher (p<0.01) in the FG (14.0) compared to the TG (11.9), also, with this latter, there is a slightly high standard deviation of 2.41 which indicates scores far from the average. FG, on the other hand, dressed a lower standard deviation (1.94) which indicates that the scores are more grouped around the mean (14.0). The application of the PBL on flipped classroom approach has, as it appears, improved the grades and reduced the gap between them.
For the final exam, with the traditional approach, the dispersion increased (Sd=3.28). On the other hand, PBL approach has improved student outcomes and widened the gap between them compared to TG (p<0.01). Figure 1 highlights the dispersion of the continuous and final control data (before for the traditional approach and after for PBL).
Figure 1. Students’ performance during the midterm exam (ME) and final exam (FE)
The ME grades were improved using PBL. As the number of compared participants is limited, a nonparametric test was carried out (Paired Mann-Whitney test) which revealed that the average grade of MEs is significantly different (p <0.01), between the traditional approach and the PBL. Similarly, an improvement in FE grades is observed when using the PBL approach. This approach allowed an improvement in the means as well as the dispersion. This leads us to state that the teaching approach based on case studies in the context of a flipped classroom (PBL), may improve both declarative and conditional knowledge on students’ outcomes.
|
Teaching approach |
N |
M |
Standard deviation |
Δ mean |
p |
|
TG |
19 |
11.9 |
3.30 |
2.21
|
0.01
|
|
FG |
19 |
14.1 |
1.95 |
Table 2: Descriptive statistics by teaching approach for the different types of controls.
From Table 2, there is a difference between the averages of the two approaches in favor of FG (p<0.01). This means that students who have taken the PBL approach had increased grades compared to those who have taken the traditional approach. To check if these differences are significant, a Paired Mann-Whitney test was used. This one demonstrated that the average rank of the grades is significantly different between the two studied approaches (p = 0.01).
The mean score and the standard deviation for each question in the questionnaire was determined. Average responses to the 12 items that referred to acquisition and application of knowledge related to the pain management ranged from 3.8 to 4.5 (See Table 3).
|
Statements |
Average score (Sd) |
|
1. I am confident in my ability to read a case and select the patient’s key factors that may impact their care. |
4.3 (0.7) |
|
2. I am confident in my ability to identify the presence of pain in a given patient. |
4.1 (0.6) |
|
3. I feel confident in determining the type of pain from the etiology involved. |
4.2 (0.6) |
|
4. I feel confident in determining the type of pain from the descriptive semiology used by a patient. |
4.2 (0.7) |
|
5. I am confident in my ability to choose the right pain assessment test for a given patient. |
4.5 (0.5) |
|
6. I am confident in my ability to use pain assessment tests with a given patient. |
4.3 (0.6) |
|
7. I am confident in my ability to understand the mechanism of action of an analgesic according to its pharmacological class. |
4.1 (0.6) |
|
8. I feel confident in my ability to relate the therapeutic benefit of a drug to its mechanism of action. |
4.1 (0.5) |
|
9. I am confident in my ability to determine the oxidative, supra-additive, or sub-additive effects of painkillers. |
4.1 (0.8) |
|
10. I feel more sensitive to the importance of pain management. |
4 (0.7) |
|
11. I feel better prepared at the clinic after participating in clinical case discussions as part of the flipped classroom. |
4.1 (0.5) |
|
12. I feel better prepared to act as an advocate for my patient’s interests to ensure comfort. |
3.8 (0.8) |
Table 3. Acquisition and application of knowledge
The statement “I feel better prepared to act as an advocate for my patient’s interests to ensure comfort” received a response rate of 3.8. This statement has the least satisfaction rate compared to all statements in the corresponding section.
|
Statements |
Average score (Sd) |
P value |
|
1. The cases were relevant and interesting. |
4.7 (0.4) |
Ns* |
|
2. I was nervous at the beginning of the module, but I gained confidence in myself as the course progressed. |
4.3 (0.8) |
|
|
3. Participating in the group discussions made me more confident in analysing key pain-related data. |
4.1 (0.9) |
|
|
4. I find that discussions have helped me learn more effectively than lectures. |
4.5 (0.6) |
|
|
5. I found that the group discussions helped my learning more effectively than the manual (handout). |
4.6 (0.7) |
|
|
6. I would recommend case-based seminar discussions as a tool for other courses. |
4 (0.9) |
*mean comparison of each item
Table 4. Perception of LPLs as a teaching/learning model
Average responses to the six questionnaire items that referred to cases as a learning model ranged from 4 to 4.7. None of the average responses differed significantly (p>0.05) from the other responses in this section of the questionnaire. The average response to the question “Were the cases relevant and interesting?” was 4.7, which was higher than all other answers. The statement “I would recommend the PBL format (no lectures, only case studies with assigned readings) as a tool for other courses” has a response average of 4, which is lower than all other responses in the corresponding category.
IV. DISCUSSION
Nursing students must grasp intricate concepts of basic physiology, pathophysiology, pharmacology, and more. Employing effective teaching methods with active learning can foster critical thinking abilities and uphold patient safety in complex care scenarios (Dong, 2016; Forsgren et al., 2014; Wood, 2003). Nowadays, nursing education has embraced the use of the flipped classroom as it offers a rich learning environment (Dong, 2016; Hanson, 2016; Immekus, 2019; Missildine et al., 2013; Ndosi & Newell, 2009; Peisachovich et al., 2016; Wood, 2003). Problem-based learning (PBL) is a frequently employed active learning approach in flipped classroom scenarios (Dong, 2016; Geist et al., 2015). PBL has been demonstrated to enhance the capacity of nursing students to evaluate patient information and arrive at more contemplative clinical judgments (Forsgren et al., 2014; Njie-Carr et al., 2017). When nursing students engage in discussions within small groups, they open themselves up to a wealth of interactive learning opportunities that are guided by their professor. This active learning situation is far more advantageous than the traditional lecture format as it promotes critical thinking skills and fosters independent learning. By participating in small group discussions, nursing students are able to delve deeper into the subject matter, ask questions, and engage in meaningful dialogue with their peers and instructor. This type of collaborative learning environment encourages students to take ownership of their education and empowers them to become more confident and competent healthcare professionals. Therefore, it is crucial that nursing programs prioritise small group discussions as a key component of their curriculum (Bailey, 2017; Carvalho et al., 2017; Kong et al., 2014; Teike Lüthi et al., 2015; Wood, 2003). High-level thinking and independent learning are enhanced with the use of interactive small groups (Alton, 2016; Gholami et al., 2016). We note from a review of the literature that a limited number of studies have examined the use of PBL in nursing (Bailey, 2017; Forsgren et al., 2014).
The current study revealed that regardless of the nature of the exam, student learning outcomes significantly improved with the flipped classroom method. Furthermore, the students participating in this study consider this method as a useful model to improve their learning and be more engaging. In fact, active learning allows effective knowledge acquisition (Arrue et al., 2017) and the development of critical thinking skills on nursing students as well as the improvement of metacognitive skills (Bailey, 2017; Carvalho et al., 2017; Domínguez, 2012). Furthermore, the students participating in this study consider this method as a useful model to improve their learning and be more engaging (Schlairet et al., 2014). Consequently, alternating between lectures and PBL approach may be a better option for health science courses (Alexandre & Wright, 2013). Greater confidence is demonstrated in acquiring and applying knowledge (practice) related to pain management.
Participation in this approach was considered a positive learning strategy, regardless of course content, the flipped classroom has shown to effectively support content learning (Hanson, 2016). When students were asked to consider whether it helped them learn more effectively than lectures, a higher response was obtained, and the response was very positive. This conclusion is in line with one from a study conducted in Portugal, which found that using this method in a second-year pathophysiology course led to higher levels of student satisfaction (Marques & Correia, 2017). Although some discomfort may be reported students are uncertain about the content and will attend classes on the assumption that it will help them understand exactly what they need to do and what they hope to achieve. This result confirms that student satisfaction does not always accurately reflect their learning (Dong, 2016). Further evaluation of this strategy and other learning tools is needed to establish best practices in nursing education (Barranquero-Herbosa et al., 2022; Njie-Carr et al., 2017).
A. Limitations
The small number of participants may affect the validity of the study. The results of this study cannot be generalised because participants belonged to one track only, so they are not representative to all nursing students. In addition, the small sample size of the study participants and the small number of available academic levels covered by the study.
B. Implications for Teaching and Future Research
Future studies could be considered to compare different learning strategies (e.g., games, medication card design, and practice problems) to determine the best practices for active learning strategies that support learning in a professional education setting and support flipped classroom learnings in nursing education.
V. CONCLUSION
Nursing education is about the development of professional skills; hence it is important to adopt active teaching strategies that promote critical thinking and knowledge transfer. However, the time constraint often pushes teachers to adopt the magistral lectures, the traditional form of knowledge delivery which mostly lacks the element of interactivity which is an issue recognised among many researchers worldwide.
The flipped classroom, in our case, is a solution to the time management problem. It allowed us to free up time in class which was beneficial to give space for interactive activities and active animation techniques such as case studies. In addition, in this study, we were able to compare the impact of the flipped classroom with the traditional model on two groups of students enrolled to the same course: pain management. The comparison results were mainly based on the acquisition of knowledge by students. We also measured students’ satisfaction with the proposed model as well as their sense of self-efficacy.
Students’ grades were clearly in favour of the PBL model in the flipped classroom. The students were also mostly satisfied with the proposed model and confirmed the development of their sense of self-efficacy regarding the pain management course.
Our perspective is the improvement of our teaching which, in our opinion, must be constantly corrected and enriched to face new conditions and situations. In this direction, the present study could constitute a roadmap for further in-depth studies to bring more to the PBL-based teaching model in the flipped classroom.
Notes on Contributors
Soumia Merrou is involved in the conceptualisation, methodology, data curation, writing and original draft preparation.
Abdellah Idrissi Jouicha helped in the methodology, participated in data curation and software, helped in writing – reviewing and editing.
Baslam Abdelmounaim participated in writing the original draft preparation, performed statistical analyses, helped in reviewing and editing corrections.
Zakaria Ouhaz was involved in visualisation, participated in data collection, helped writing and reviewed the manuscript.
Ahmed Rhassane El Adib was central to the conceptualisation and methodology, validated the design study, and supervised work progress. All authors have read and approved the final manuscript.
Ethical Approval
Participation in the study was voluntary and anonymous. Oral consent of all participants was obtained and the research was approved by the Institutional Ethical committee (CCBE-FSA Ref. No: ER-CS-10/2022-000).
Data Availability
The data that support the findings of this study are openly available in Figshare repository, https://doi.org/10.6084/m9.figshare.21385446.
Acknowledgement
We acknowledge the efforts of both professor and participants.
Funding
The study received no funding.
Declaration of Interest
The authors declare that they have no conflict of interest.
References
Alexandre, M. S., & Wright, R. R. (2013). Flipping the classroom for student engagement. International Journal of Nursing Care, 1(2), 100.
Alton, S. (2016). Learning how to learn: Meta-learning strategies for the challenges of learning pharmacology. Nurse Education Today, 38, 2–4. https://doi.org/10.1016/j.nedt.2016.01.003
Arrue, M., Ruiz de Alegría, B., Zarandona, J., & Hoyos Cillero, I. (2017). Effect of a PBL teaching method on learning about nursing care for patients with depression. Nurse Education Today, 52, 109–115. https://doi.org/10.1016/j.nedt.2017.02.016
Bailey, L. A. (2017). Adaptation of know, want to know, and learned chart for problem-based learning. Journal of Nursing Education, 56(8), 506–508. https://doi.org/10.3928/01484834-20170712-11
Barranquero-Herbosa, M., Abajas-Bustillo, R., & Ortego-Maté, C. (2022). Effectiveness of flipped classroom in nursing education: A systematic review of systematic and integrative reviews. International Journal of Nursing Studies, 105, Article 104327. https://doi.org/10.1016/j.ijnurstu.2022.104327
Carvalho, D. P. S. R. P., Azevedo, I. C., Cruz, G. K. P., Mafra, G. A. C., Rego, A. L. C., Vitor, A. F., Santos, V. E. P., Cogo, A. L. P., & Ferreira Júnior, M. A. (2017). Strategies used for the promotion of critical thinking in nursing undergraduate education: A systematic review. Nurse Education Today, 57, 103–107. https://doi.org/10.1016/j.nedt.2017.07.010
Deandrea, S., Montanari, M., Moja, L., & Apolone, G. (2008). Prevalence of undertreatment in cancer pain. A review of published literature. Annals of Oncology, 19(12), 1985–1991. https://doi.org/10.1093/annonc/mdn419
Domínguez, R. G. (2012). Participatory Learning. In N. M. Seel (Ed.), Encyclopedia of the Sciences of Learning (pp. 2556–2560). Springer.
Dong, X. (2016). Application of flipped classroom in college english teaching. Creative Education, 7(9), 1335–1339. https://doi.org/10.4236/ce.2016.79138
Forsgren, S., Christensen, T., & Hedemalm, A. (2014). Evaluation of the case method in nursing education. Nurse Education in Practice, 14(2), 164–169. https://doi.org/10.1016/j.nepr.2013.08.003
Geist, M. J., Larimore, D., Rawiszer, H., & Al Sager, A. W. (2015). Flipped versus traditional instruction and achievement in a baccalaureate nursing pharmacology course. Nursing Education Perspectives, 36(2), 114-115. https://doi.org/10.5480/13-1292
Gerbershagen, K., Gerbershagen, H. J., Lutz, J., Cooper-Mahkorn, D., Wappler, F., Limmroth, V., & Gerbershagen, M. (2009). Pain prevalence and risk distribution among inpatients in a German teaching hospital. The Clinical Journal of Pain, 25(5), 431–437.
Gholami, M., Moghadam, P. K., Mohammadipoor, F., Tarahi, M. J., Sak, M., Toulabi, T., & Pour, A. H. H. (2016). Comparing the effects of problem-based learning and the traditional lecture method on critical thinking skills and metacognitive awareness in nursing students in a critical care nursing course. Nurse Education Today, 45, 16–21. https://doi.org/10.1016/j.nedt.2016.06.007
Gianni, W., Madaio, R., Cioccio, L., D’Amico, F., Policicchio, D., Postacchini, D., Franchi, F., Ceci, M., Benincasa, E., Gentili, M., & Zuccaro, S. (2010). Prevalence of pain in elderly hospitalized patients. Archives of Gerontology and Geriatrics, 51(3), 273-276. https://doi.org/10.1016/j.archger.2009.11.016
Hanson, J. (2016). Surveying the experiences and perceptions of undergraduate nursing students of a flipped classroom approach to increase understanding of drug science and its application to clinical practice. Nurse Education in Practice, 16(1), 79–85. https://doi.org/10.1016/j.nepr.2015.09.001
Immekus, J. C. (2019). Flipping statistics courses in graduate education: Integration of cognitive psychology and technology. Journal of Statistics Education, 27(2), 79–89. https://doi.org/10.1080/10691898.2019.1629852
Kerner, Y., Plakht, Y., Shiyovich, A., & Schlaeffer, P. (2013). Adherence to guidelines of pain assessment and intervention in internal medicine wards. Pain Management Nursing, 14(4), 302–309. https://doi.org/10.1016/j.pmn.2011.06.005
Kong, L.-N., Qin, B., Zhou, Y., Mou, S., & Gao, H.-M. (2014). The effectiveness of problem-based learning on development of nursing students’ critical thinking: A systematic review and meta-analysis. International Journal of Nursing Studies, 51(3), 458–469. https://doi.org/10.1016/j.ijnurstu.2013.06.009
Manias, E., Bucknall, T., & Botti, M. (2005). Nurses’ strategies for managing pain in the postoperative setting. Pain Management Nursing: Official Journal of the American Society of Pain Management Nurses, 6(1), 18–29. https://doi.org/10.1016/j.pmn.2004.12.004
Marques, P. A. O., & Correia, N. C. M. (2017). Nursing education based on “hybrid” problem-based learning: The impact of PBL-based clinical cases on a pathophysiology course. Journal of Nursing Education, 56(1), 60. https://doi.org/10.3928/01484834-20161219-12
Merrou, S., Jouicha, A. I., Baslam, A., Ouhaz, Z., & El Adib, A. R. (2023). Problem-based learning method in the context of a flipped classroom: Outcomes on pain management course acquisition [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.22639279
Missildine, K., Fountain, R., Summers, L., & Gosselin, K. (2013). Flipping the classroom to improve student performance and satisfaction. Journal of Nursing Education, 52(10), 597-599.
Ndosi, M. E., & Newell, R. (2009). Nurses’ knowledge of pharmacology behind drugs they commonly administer. Journal of Clinical Nursing, 18(4), 570–580. https://doi.org/10.1111/j.1365-2702.2008.02290.x
Njie-Carr, V. P. S., Ludeman, E., Lee, M. C., Dordunoo, D., Trocky, N. M., & Jenkins, L. S. (2017). An integrative review of flipped classroom teaching models in nursing education. Journal of Professional Nursing, 33(2), 133–144. https://doi.org/10.1016/j.profnurs.2016.07.001
Peisachovich, E. H., Murtha, S., Phillips, A., & Messinger, G. (2016). Flipping the classroom: a pedagogical approach to applying clinical judgment by engaging, interacting, and collaborating with nursing students. International Journal of Higher Education, 5(4), 114. https://doi.org/10.5430/ijhe.v5n4p114
Schlairet, M. C., Green, R., & Benton, M. J. (2014). The flipped classroom. Nurse Educator, 39(6), 321–325. https://doi.org/10.1097/nne.0000000000000096
Teike Lüthi, F., Gueniat, C., Nicolas, F., Thomas, P., & Ramelet, A.-S. (2015). Les obstacles à la gestion de la douleur perçus par les infirmières: Étude descriptive au sein d’un hôpital universitaire Suisse. [Barriers to pain management as perceived by nurses: A descriptive study in a Swiss University Hospital.] Douleur et Analgesie [Douleur & Analgésie], 28, 93-99. https://doi.org/10.1007/s11724-015-0414-3
Tune, J. D., Sturek, M., & Basile, D. P. (2013). Flipped classroom model improves graduate student performance in cardiovascular, respiratory, and renal physiology. Advances in Physiology Education, 37(4), 316–320. https://doi.org/10.1152/advan.00091.2013
Wood, D. (2003). Problem based learning. British Medical Journal, 326, 328–330. https://doi.org/10.1136/bmj.326.7384.328
*Abdellah Idrissi Jouicha
Marrakesh, Marrakesh-Safi,
40000, Morocco
Email: abdellah.idrissi@ced.uca.ac.ma
Submitted: 6 September 2022
Accepted: 1 March 2023
Published online: 3 October, TAPS 2023, 8(4), 1-4
https://doi.org/10.29060/TAPS.2023-8-4/GP2878
Saroj Jayasinghe1, Santhushya Fernando2
1Department of Clinical Medicine, Faculty of Medicine, University of Colombo, Sri Lanka; 2Department of Medical Humanities, Faculty of Medicine, University of Colombo, Sri Lanka
Abstract
Introduction: Medical Humanities is the interface of health sciences and humanities and an emerging field of interest. Several papers have outlined the status of this field in the Asian region where a diversity of teaching and learning approaches have been used. We share developments initiated in a Sri Lankan medical school and discuss its relevance to the southern Asian region, especially in using arts in medical humanities.
Methods: Historical records, narratives, grey literature, and published resources were collated to describe the initiative in the Faculty of Medicine, University of Colombo. The data was collected, synthesized and described especially in the context of the region.
Results: We observe a structured development of medical humanities in the curriculum. The novelty of the curriculum is that it evolving to include wider experiences from the visual and performance arts, in order to achieve the goal of promoting humaneness. The contents were locally developed, based on needs with an indigenous cultural bias giving rise to a unique southern Asian perspective of medical humanities.
Conclusion: There are diverse experiences and initiatives in medical humanities in Asian, and some are not captured in published literature. It is challenging to follow these diverse trends in different locations, share experiences and learn from each other, and place medical humanities in the regional and global maps of health professional education.
Practice Highlights
- Asia has seen several developments in the field of medical humanities.
- Sri Lanka has made significant progress and introduced it to medical education.
- One key innovation is the integration of arts to its teaching-learning.
- Southern Asia has rich and diverse religious, cultural and artistic traditions.
- The region could give a unique perspective to medical humanities.
I. INTRODUCTION
A recent scoping review traced the history of developments in the teaching / learning of humane care and recognition of its importance in medical training (Zhu et al., 2021). This paper also outlined the need to develop culturally relevant, effective, and integrative curricula that would promote humanistic attitudes and behaviours among medical students and physicians in Asia. There were developments of this field in Nepal that were shared in a subsequent correspondence (Shankar, 2022). These papers and several other publications have highlighted the developments in the field with a diversity of experiences.
We share a few developments from Sri Lanka that demonstrate a widening interest in the field in southern Asia and opportunities to use its unique heritage to move forward.
II. SCOPE AND BACKGROUND INFORMATION
The Faculty of Medicine, University of Colombo is one of the oldest continuously functioning medical schools in Asia (from 1870). It has the distinction of pioneering an integrated curriculum in the country in 1995 and establishing the first Department of Medical Humanities in 2016.
For decades, the curriculum was based on Flexner’s structures and was a conventional discipline-based curriculum with little inputs from the humanities. The reforms in 1995 led to a more integrated modular system with a longitudinal input from Behavioural Sciences (BS). The BS program had modules that focused on teaching / learning in topics related to personal development, communication skills, medical ethics, health management and professionalism (Jayasinghe, 2017). It was organized by appointing a group of academics to a Behavioural Science Stream (BSS) to coordinate the teaching / learning programs through the 5-year MBBS course.
However, inputs from the arts were minimal though it flourished outside the formal curriculum in the form of concerts, art festivals, photography exhibitions and musical events organized by the student body. These activities were heavily influenced by the urbanized Western culture and activities such as ball-room dancing, predominantly British literature, and Western models of theatre played a predominant role.
A qualitative change in the range of activities was observed around 1974 with the establishment of an Arts Circle in the Faculty of Medicine that promoted infusion of local culture. Interestingly, this coincided with changes in the admission criteria to universities that resulted in student intakes from diverse of social groups and a significant increase in entry from a wider range of districts and more rural schools.
In 2011, the BSS began to organize internal workshops to review its curriculum and propose future developments. During these discussions, participants expressed the need to promote more humaneness, empathy and compassion among students (Jayasinghe, 2017). This led to discussions on the potential role of the arts to meet these needs. The first lecture on “Illness from the perspective of humanities” was introduced in 2012. Soon a consensus view emerged to establish a Department of Medical Humanities in order to deliver a heavier educational input from humanities and thereby promote humane values in students. In August 2016, the Faculty of Medicine, University of Colombo, formally established the first Department of Medical Humanities in the country. In 2020 the BSS was renamed Humanities, Society and Professionalism Stream (HSPS) to reflect the introduction of new content to the curriculum.
III. EDUCATIONAL STRATEGIES
In order to identify contents for its new curriculum, the Department organized a series of invited lectures and discussions targeting the academic staff. It was titled “Exploring the Role of Humanities in Health”. The resource persons were experts on medical humanities and a diverse range of topics included “Role of Arts in Medicine”; “Approaches to teaching humanities to medical students”; “Medical narratives”; “Using poetry to inculcate attitudes”; and “Humanities in medicine: The Ruhuna Experiment”. Other opportunities, such as invitations to deliver guest lectures in conferences, were used by the authors to stimulate discussions on the potential role of the arts in health professional education (Jayasinghe, 2018).
The series of lectures culminated in the First International Conference on Medical Humanities held in 2018, on the theme “Learning to be more humane: The role of Medical Humanities” (Colombo Medical Humanities News, 2019). It included a half-day workshop on “Arts in Health Professional Education”. There was wide participation by experts in the field and the conference and workshop were used to refine the curriculum on medical humanities, especially on how to effectively introduce the arts to health professional education. This issue was further debated and discussed during seminars on Medical Humanities at the Colombo Medical Congress (in 2020) and orations dedicated to Medical Humanities (from 2021).
The knowledge gained from the above activities, were used to design an innovative curriculum that included a wider infusion from the arts and narrative-based learning. The main goals of the latter were to promote humaneness, encourage learners to develop a person-centred approach to clinical practice, and appreciate patient perspectives of illness. A range of educational strategies were used: assignment on appreciation of the arts and its relevance to empathy in care; student seminar to reflect on personal experiences of kind and unkind health professional behaviours, obtaining narratives from patients to highlight the humane and person-centered issues of illness; large-group lectures on topics such as “The Arts in Health and Illness” and “Empathy and Compassion”. The latter focused on research evidence from neurophysiology to demonstrate links between art appreciation and traits such as compassion and empathy.
In 2021, during the COVID pandemic, the HSPS and the Department of Medical Humanities introduced an innovative programme aimed at the students. A series of interactive multi-disciplinary webinars termed Humanitas were organied to explore contemporary issues connected to health and have continued as part of the teaching-learning programme. They have been held approximately at bi-monthly intervals and addressed a wide range of issues: life-experiences amidst environmental disasters, linguicism and decolonizing tertiary education, the world of animal welfare, lives of workers in the apparel industry, social and psychological issues faced by those with different sexual identities and orientations, and the emotional journey of a parent who lost her child to cancer.
Interviews from affected groups of people, artists, academics and intellectuals were creatively juxtaposed with short films, extracts from movies, selected musical scores. Examples of the latter included songs of peace sung during non-violent protests organised by Mahatma Gandhi and Martin Luther King Sr., and extracts of poetry and literature that drew attention to contemporary issues such as the plight of garment factory workers. Contributions were predominantly from Sri Lankan commentators reflecting our own historical and cultural context and local experiences.
Since the pandemic ended, Humanitas will be conducted in-person. The first for 2023 was titled ‘Dance and Life’, featuring live Indian and traditional Sri Lankan dance recitals by professional dancers. These performances were accompanied by commentaries by dancers on the emotions they felt while dancing, and the mechanisms of evoking feelings in the audience described by medical experts. These emotions and feelings were in turn linked to the ability of certain dances to generate compassion and empathy. The session ended with an expert dancer performing and describing how certain traditional dances of the Sinhalese (e.g. ‘Thovil’) were used as therapy for a diversity of illnesses.
The second recent innovation relates to activities on medical humanities organized for the 3rd Colombo Medical Congress in November 2022, an annual event in the University calendar and open to students. We organised a symposium exploring the neurophysiological correlates of music, poetry, and dance and complemented the academic program with a series of activities throughout the conference: free exhibitions of art, sculptures and photography, open-air musical events by students, and live sculpture and portrait sessions by professional artists. The latter live sessions enabled students and attendees to experience and interact with the process of artistic creations.
IV. DISCUSSION
Medical Humanities is an emerging field of interest in the interface of health sciences and humanities. The diversity of experiences in the Asian region has led to several initiatives. The initiative in Colombo used contemporary topics with contributions mainly from Sri Lankan commentators reflecting on our own historical and cultural contexts. We believe this enriched a field that is dominated by an allopathic or modern medical system that are predominantly Eurocentric and based on ‘Western’ values and culture.
We hope our experiences would diffuse in the Asian region. Southern Asia has a rich, historical and cultural heritage based predominantly from the Indian religions and include Hinduism, Sikhism, Jainism, Buddhism, and Islam that came from the Middle East and spread to the Indian sub-continent. The philosophical, cultural and religious foundations of this region give us a unique opportunity to give a novel perspective to the field. This will require a process of decolonizing our values and beliefs, and reconnecting to our own cultures and heritages. We also need to follow these trends in different locations, share experiences and learn from each other, often a difficult task because these initiatives may fail to reach mainstream journals or remain unpublished.
V. CONCLUSION
The paper highlights the need to have more collaborations within the southern Asian region and share knowledge that would be mutually beneficial. Southern Asia has a rich historical and cultural heritage. These roots could help develop a unique southern Asian version of Medical Humanities and place our version of medical humanities in the global maps of health professional education.
Notes on Contributors
Saroj Jayasinghe conceptualised and wrote the initial draft.
It was revised and expanded by Santhushya Fernando.
Both authors read and approved the manuscript.
Funding
The study was funded by personal funds.
Declaration of Interest
The authors have no conflicts of interest, including financial, consultant, institutional and other relationships that might lead to bias.
References
Our beginnings. (2019). Colombo Medical Humanities News, 1(1). https://med.cmb.ac.lk/medical-humanities/
Jayasinghe, S. (2017). Of course! We must look at the Arts… in its widest sense! Journal of the Ruhunu Clinical Society, 22(1), 4-5. http://doi.org/10.4038/jrcs.v22i1.26
Jayasinghe, S. (2018). Can the arts promote more humane health professionals? Exploring evidence from the neurosciences. Ceylon Journal of Medical Science, 55(1), 1-2. http://doi.org/10.4038/cjms.v55i1.4938
Shankar, P. R. (2022). Learning humanistic values in Nepal. The Asia Pacific Scholar, 7(3), 63-64. https://doi.org/10.29060/TAPS.2022-7-3/LE2777
Zhu, C. S., Yap, R. K. F., Lim, S. Y. S., Toh, Y. P., & Loh, V. W. K. (2021). Humanism in Asian medical education – A scoping review. The Asia Pacific Scholar, 7(1), 9-20. https://doi.org/10.29060/TAPS.2022-7-1/RA2460
*Saroj Jayasinghe
Faculty of Medicine,
University of Colombo,
No 25, Kinsey Road,
Colombo 8, Sri Lanka
+94718619331
Email: saroj@clinmed.cmb.ac.lk
Submitted: 19 August 2022
Accepted: 1 February 2023
Published online: 4 July, TAPS 2023, 8(3), 72
https://doi.org/10.29060/TAPS.2023-8-3/MA1603
Christopher See1*, Cynthia Sin Nga Lam2* & Yalsin Yik Sum Li2
1School of Biomedical Sciences, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong; 2Hospital Authority, Hong Kong
*Authors contributed equally
References
Chang, C. Y., Hwang, G. J., & Gau, M. L. (2022). Promoting students’ learning achievement and self‐efficacy: A mobile chatbot approach for nursing training. British Journal of Educational Technology, 53(1), 171-188. https://doi.org/10.1111/bjet.13158
Huang, W., Hew, K. F., & Gonda, D. E. (2019). Designing and evaluating three chatbot-enhanced activities for a flipped graduate course. International Journal of Mechanical Engineering and Robotics Research, 8(5), 813-818. https://doi.org/10.18178/ijmerr.8.5.813-818
Inkster, B., Sarda, S., & Subramanian, V. (2018). An empathy-driven, conversational artificial intelligence agent (Wysa) for digital mental well-being: Real-world data evaluation mixed-methods study. JMIR mHealth and uHealth, 6(11), e12106. http://doi.org/10.2196/12106
Lam, C. S. N., Li, Y. S., Chan, L. K., & See, C. (2019, November 11). Can the A.I.natomy chatbot teach anatomy? [Poster presentation]. 2nd Korea University International Medical Student Conference, Korea University, Seoul, Korea.
Li, C., Zhang, X., Chrysostomou, D., & Yang, H. (2022). ToD4IR: A humanised task-oriented dialogue system for industrial robots. IEEE Access, 10, 91631-91649. https://doi.org/10.1109/ACCESS.2022.3202554
Schlögl, S., Doherty, G., & Luz, S. (2015). Wizard of Oz experimentation for language technology applications: Challenges and tools. Interacting with Computers, 27(6), 592-615. https://doi.org/10.1093/iwc/iwu016
See, C., Lam, C. S. N., Li, Y. S., & Chan, L. K. (2019, May 31). Methods for training an AI for Higher Education [Poster presentation]. Centre for Information Technology in Education Research Symposium 2019, Faculty of Education, the University of Hong Kong, Hong Kong.
Suleman, R. M., Mizoguchi, R., & Ikeda, M. (2016). A new perspective of negotiation-based dialog to enhance metacognitive skills in the context of open learner models. International Journal of Artificial Intelligence in Education, 26, 1069-1115. https://doi.org/10.1007/s40593-016-0118-8
Kron, F. W., Fetters, M. D., Scerbo, M. W., White, C. B., Lypson, M. L., Padilla, M. A., Gliva-McConvey, G. A., Belfore II, L. A., West, T., Wallace, A.M., Guetterman, T. C., Schleicher, L. S., Kennedy, R. A., Mangrulkar, R. S., Cleary, J. F., Marsella, S. C., Becker, D. M. (2017). Using a computer simulation for teaching communication skills: A blinded multisite mixed methods randomized controlled trial. Patient Education and Counseling, 100(4), 748-759. https://doi.org/10.1016/j.pec.2016.10.024
Ward, T., Falconer, L., Frutos-Perez, M., Williams, B., Johns, J., & Harold, S. (2016). Using virtual online simulations in Second Life® to engage undergraduate psychology students with employability issues. British Journal of Educational Technology, 47(5), 918-931. https://doi.org/10.1111/bjet.12307
Weizenbaum, J. (1966). ELIZA – A computer program for the study of natural language communication between man and machine. Communications of the ACM, 9(1), 36-45.
*Christopher See
Rm 610S, 6/F, Choh-Ming Li Basic Medical Sciences Building,
The Chinese University of Hong Kong, Shatin, New Territories,
Hong Kong Special Administrative Region, China
+852 3943 0465
Email: christophersee@cuhk.edu.hk
Submitted: 16 December 2022
Accepted: 3 January 2023
Published online: 4 July, TAPS 2023, 8(3), 68-69
https://doi.org/10.29060/TAPS.2023-8-3/LE2930
David Mathew
Department of Anaesthesia, Khoo Teck Puat Hospital, Singapore
Dear Editor,
I read with great interest the article entitled “The associates of Emotional Intelligence in medical students: A systematic review” (Edussuriya et al., 2022) in your journal published in October 2022. The association of Emotional Intelligence (EI) with wellbeing cannot be underestimated, especially with the plethora of positive effects it has on mental health and academic performance. In fact, I think this can be extended beyond students, to all healthcare professionals.
In my opinion, humanities in medicine provide a potentially novel way of improving emotional intelligence. The writer of a piece acknowledges the scientific experience that has moved him/her, and subsequently reflects on the entire experience through the arts and writing. The process of writing can be cathartic as it presents an avenue for the writer to release emotions that might have been pent-up or hidden as we provide a brave front to our patients. Once written, the piece can be shared, and reach out to other healthcare professionals who might have encountered similar experiences. Some may find comfort in reading such pieces, as they realise they are not alone in experiencing the roller-coaster of emotions in their daily lives.
I have appended a piece I wrote regarding my experience with an obstetrics patient and how sometimes the lesser said, the more it means. The process of writing and sharing this piece helped me better understand and appreciate what I went through and I hope it can do the same for fellow readers.
Cry
The day I saw her cry
was when her baby’s heart
slowed.
She needed the Caesarean
quickly.
Her eyes conceived tears
crawling down her cheeks
shaping into an anxious cry.
I counted the tears
and spoke more words
comforting, reassuring.
I saw her cry
one week later,
this time her littlest bundle
the greatest joy.
Tears of happiness
dancing muted screams of relief
I counted the tears
but spoke nothing
comforting, reassuring.
Tears
instead of words,
won wars of emotions.
And staying silent
might be the most reassuring cry
of comfort.
Note on Contributor
DM came up with the concept of the manuscript, and wrote the entirety of its contents.
Funding
There was no funding for this paper.
Declaration of Interest
There is no conflict of interest declared.
References
Edussuriya, D., Perera, S., Marambe, K., Wijesiriwardena, Y., & Ekanayake, K. (2022). The associates of Emotional Intelligence in medical students: A systematic review. The Asia Pacific Scholar, 7(4), 59–70. https://doi.org/10.29060/taps.2022-7-4/oa2714
*David Mathew
Khoo Teck Puat Hospital,
90 Yishun Central, Singapore
Email: davidmathew3142@gmail.com
Submitted: 20 October 2022
Accepted: 3 January 2023
Published online: 4 July, TAPS 2023, 8(3), 65-67
https://doi.org/10.29060/TAPS.2023-8-3/CS2906
Hiroshi Kawahira1, Yoshitaka Maeda1, Yoshihiko Suzuki1, Yuji Kaneda1, Yoshikazu Asada2, Yasushi Matsuyama2, Alan Kawarai Lefor3 & Naohiro Sata3
1Medical Simulation Center, Jichi Medical University, Japan; 2Medical Education Center, Jichi Medical University, Japan; 3Department of Surgery, Jichi Medical University, Japan
I. INTRODUCTION
The ongoing COVID-19 pandemic has a significant impact on medical education, forcing changes in the curriculum (Rose, 2020). Since the COVID-19 pandemic began, governments and authorities in many countries have imposed online learning on medical students and in many institutions, medical students were not permitted to participate in in-person clinical clerkships or other practical training at university hospitals (Mian & Khan, 2020). Although the surgical clerkship is an important contributing factor to nurture student interest in a surgical career (Khan & Mian, 2020), medical students were excluded from the operating room due to lack of personal protective equipment, and participation in ward duties and training facilities were restricted (Calhoun, et al., 2020).
The purpose of this study is to analyse how the lack of in-person surgical experience and ward duties (online clerkship), among the most important components of a surgical clerkship, affected student interest in a career in surgery. The impact on student perceptions of surgery comparing online learning and onsite clinical clerkship (typical in-person clerkship) was assessed by comparing student satisfaction with the surgical clerkship, changes in interest in a career in surgery, and changes in the image of surgery at the beginning and end of rotations for online and onsite training groups.
II. METHODS
This study was reviewed by the Ethical Review Committee of Jichi Medical University, and no ethical review was required (Reference No. 20-186). A total of 133 fifth-year medical students, all in the same academic year, participated in surgery clerkships from April 2020 to February 2021. All 133 medical students completed clerkships in internal medicine during the previous academic year. The 133 students were divided into eight groups, with 16 or 17 students per group, rotating in surgery every three weeks. The first five groups of that academic year had online lectures only and the last three groups had onsite practice (typical clerkship experience).
Of the 133 students, 124 who provided consent were included in this study. Of these, 79 received online training from April through September 2020, and 45 received onsite clerkship training from October 2020 through February 2021. Moodle, an online learning management system, was used as the platform for online learning, and designed content to be studied on demand. An orientation and lecture with a comprehensive explanation of each aspect of surgical training were synchronous, and online communication with individual students was also conducted. Faculty also communicated online with individual students using Moodle, and individual questions were answered via email as appropriate.
Questionnaires for students in the clerkship were administered using the Moodle platform regardless of whether the clerkship was onsite or online. Questionnaire items addressed: 1. anxiety about surgery, 2. Opinion about difficulty of surgery compared to internal medicine, and 3. interest in surgery. Responses were given as a single choice and were scored using a four-point scale: 1: disagree, 2: somewhat disagree, 3: somewhat agree, and 4: agree.
Comparisons between responses at the beginning and end of the three-week clerkship for all participants were made with the Wilcoxon signed rank test. After calculating differences between the beginning and end of the clerkship, the online and onsite groups were compared using the Mann-Whitney U test. A p < 0.05 was considered statistically significant. Cohen’s d was used as an index of effect size, with 0.2 as a small effect size, 0.5 as a medium effect size, and 0.8 as a large effect size. The statistical software used was R 3.6.1 with GUI 1.70 (The R Project for Statistical Computing, Vienna).
III. RESULTS
The results for the 124 students enrolled in this study showed that after three weeks of practice compared to the beginning of the study, they were less anxious about surgery (p<0.00001, effect size 0.43), less likely to find surgery difficult compared to study in other departments (p<0.00001, effect size 0.57), and were more interested in surgery as a career (p<0.0001 and effect size 0.38) (See Table 1).
The onsite clinical clerkship resulted in less anxiety about surgery (p = 0.017, effect size 0.41) compared with the online clerkship. There was no significant difference in change of the image of surgery as hard compared to other departments (p = 0.293, effect size 0.21) or change of interest in surgery (p = 0.407, effect size 0.09) in comparing the onsite and the online groups, and the effect size on change of image and interest were also small (See Table 1).
|
|
|
Average |
p* |
p# |
Cohen’s d |
||
|
|
|
Beginning |
Ending |
Beginning – End |
|||
|
How anxious are you about the surgery rotation? |
Total (n=124) |
3.31 |
2.99 |
– |
< 0.00001 |
– |
0.43 |
|
online clerkship (n=79) |
3.38 |
3.19 |
0.19 |
– |
0.017 |
0.41 |
|
|
onsite clerkship (n=45) |
3.20 |
2.64 |
0.56 |
||||
|
How difficult is the surgery rotation compared to other departments? |
Total (n=124) |
3.40 |
2.99 |
– |
< 0.00001 |
– |
0.57 |
|
online clerkship (n=79) |
3.62 |
2.99 |
0.63 |
– |
0.293 |
0.21 |
|
|
onsite clerkship (n=45) |
3.53 |
3.00 |
0.53 |
||||
|
How interested do you feel in surgery as a career? |
Total (n=124) |
3.06 |
3.32 |
– |
< 0.0001 |
– |
0.38 |
|
online clerkship (n=79) |
3.00 |
3.29 |
-0.29 |
– |
0.407 |
0.09 |
|
|
onsite clerkship (n=45) |
3.16 |
3.38 |
-0.22 |
||||
Table 1. Changes in the results of responses at the beginning and end of online and onsite clerkships
p*: Wilcoxon signed rank test, p#: Mann-Whitney U test
IV. DISCUSSION
During the COVID-19 pandemic, medical schools have established integrating digital technology and novel pedagogy (Tan, et al., 2022). Regardless of the clerkship format, three weeks of surgical clinical clerkship resulted in less anxiety about surgery than initially felt, a less daunting image of surgery in comparison to other departments, and significantly higher interest in surgery. However, the effect sizes were moderate (0.43, 0.57, and 0.38), suggesting a positive change in the image of surgery, especially in comparison with other departments. The onsite clinical clerkship group showed a greater decrease in change in anxiety about surgery than the online clinical clerkship at the end of the surgical clinical clerkship (effect size 0.41). The effect size was moderate, suggesting the effectiveness of the onsite clinical clerkship. This study also shows that there were no statistical differences in the feeling of difficulty or interest in a surgical career between the onsite and the online groups. We believe that online content via Moodle was attractive for medical students. Also, medical students could feel the realism of the surgical workplace using Moodle.
V. CONCLUSION
Face-to-face communications with senior physicians are essential to foster an image of the role of physicians to medical students. It is desirable to develop a hybrid type of clinical clerkship that takes advantage of the advantages of the realism of surgery provided by an onsite clinical clerkship and the easy accessibility of educational content of an online clinical clerkship.
Notes on Contributors
Kawahira, Maeda and Suzuki designed the study. Asada and Kawahira constructed the Moodle platform. Kaneda, Lefor and Sata conducted surgical clinical practice. Kawahira and Maeda analyzed data. Kawahira and Lefor wrote the manuscript.
Acknowledgement
The authors would like to acknowledge Ms. Yasuko Saikai who did the administrative contact for the students, and all the staffs and surgeons of the Department of Surgery for instructing the students on the clinical clerkship.
Funding
This research was funded by the education and research expenses from Jichi Medical University.
Declaration of Interest
The authors declare that they have no competing interests.
References
Rose, S. (2020). Medical student education in the time of COVID-19. JAMA, 323(21), 2131-2132. https://doi.org/10.1001/jama.2020.5227
Mian, A., & Khan, S. (2020). Medical education during pandemics: a UK perspective. BMC Medicine, 18, Article 100. https://doi.org/10.1186/s12916-020-01577-y
Khan, S., & Mian, A. (2020). Medical education: COVID-19 and surgery. British Journal of Surgery, 107(8), Article e269. https://doi.org/10.1002/bjs.11740
Calhoun, K. E., Yale, L. A., Whipple, M. E., Allen, S. M., Wood, D. E., & Tatum, R. P. (2020). The impact of COVID-19 on medical student surgical education: Implementing extreme pandemic response measures in a widely distributed surgical clerkship experience. American Journal of Surgery, 220(1), 44-47. https://doi.org/10.1016/j.amjsurg.2020.04.024
Tan, C. J., Cai, C., Ithnin, F., & Eileen, L. (2022). Challenges and innovations in undergraduate medical education during the COVID-19 pandemic – A systematic review. The Asia Pacific Scholar, 7(3), 1-9. https://doi.org/10.29060/TAPS.2022-7-3/OA2722
*Hiroshi Kawahira
Medical Simulation Center
Jichi Medical University
3311-1 Yakushiji, Shimotsuke, Tochigi
Japan 329-0498
Email: kawahira@jichi.ac.jp
Submitted: 14 December 2022
Accepted: 22 March 2023
Published online: 4 July, TAPS 2023, 8(3), 62-64
https://doi.org/10.29060/TAPS.2023-8-3/PV2926
Sachiko Kasamo, Satoshi Ozeki, Hiroyasu Inoue & Seiji Matsumoto
Institutional Research Office, Asahikawa Medical University, Japan
I. INTRODUCTION
There is growing interest in social responsibility around the world in order to accomplish a sustainable society. Indeed, modern universities cannot be ivory towers unrelated to society. It would not be an overstatement to say that without interaction and contribution to society, the university’s survival and development are unlikely.
It is frequently said that the university fulfils three different missions: education, research, and social contribution. J. A. Perkins, the eminent theoretician of higher education in the 1960s, proposed there are three aspects of knowledge that must be understood as they have their institutional reflections in the university’s three missions (Perkins, 2016). For knowledge itself to have significant power, there must be communication and interaction between the newly acquired knowledge, its transmission, and its application. The above concept began in the United States and has since been widely adopted as three major missions in many universities worldwide. Despite these three missions, however, depending on the university’s expertise and readiness, and the resources and support received from external organisations and individuals, the university may be more active on some missions and less active on others.
Some with a conventional conception of “social contribution” may wonder “why now?”, as the results of both “education and research” are ultimately returned to society. However, the major difference is that while the conventional efforts of the university were at the level of individual responses by faculty members and others, the current “social contribution” is positioned as the essential function of the university. Expectations for universities have changed significantly, and universities have changed in a variety of ways; universities are now required to use knowledge for society from various perspectives. The greater the need to contribute to society and the greater its role, the more we need to question the meaning of “social contribution” in relation to the traditional roles of “education and research” in the university.
II. GLOBAL CONCEPTS OF SOCIAL ACCOUNTABILITY IN MEDICAL SCHOOLS
The concept of social contribution is embedded in the social accountability of medical schools. The World Health Organization defined it as “the obligation to direct their education, research and service activities towards addressing the priority health concerns of the community, region, and/or nation they have a mandate to serve” (Boelen & Heck, 1995). Following this, the Global Consensus for Social Accountability of Medical Schools defined a socially accountable medical school as one that “responds to current and future health needs and challenges in society, re-orientates its education, research and service priorities accordingly, strengthens governance and partnerships with other stakeholders and use evaluation and accreditation to assess their performance and impact” (Global Consensus for Social Accountability of Medical Schools [GCSA], 2010). This document also emphasised the significance of enhancing medical schools’ ability to address the demands and difficulties of providing healthcare for citizens and society at large, in accordance with the fundamental principles of quality, equity, relevance, and effectiveness. In addition, the criteria for ASPIRE-to-Excellence Award for Social Accountability by Association for Medical Education in Europe provide a practical framework for medical schools to consider when examining their own social contribution. This award itself gives schools the opportunity to be acknowledged globally for their excellence in education, which also covers social accountability (Mori et al., 2022). These internationally accepted concepts should always be kept in mind when promoting social contribution activities in medical schools.
III. SOCIAL CONTRIBUTIONS IN JAPANESE MEDICAL SCHOOLS
Japan might be one of the unique countries to set clear objectives regarding the university’s social contribution in legislation. There are two revisions that have pushed the idea of social contribution forward as a fundamental function of the university (Hosono, 2014). First, the 2006 Revision of Basic Act on Education, Article 7 stated, “Universities, as the core of scholarly activities, are to contribute to the development of society by cultivating advanced knowledge and specialised skills, inquiring deeply into the truth to create new knowledge, and broadly offering the fruits of these endeavours to society.” Second, 2007 Revision of School Education Act, Article 83(2) stated, “Universities shall contribute to the development of society by conducting education and research to achieve their objectives and by providing the results widely to the society.” In light of these key statement revisions, the mission of the universities has changed along with the social trends, and more direct social contributions are being sought.
The importance of social contribution is also emphasised by Japanese medical schools. The recent study has analysed the Japan Accreditation Council for Medical Education accreditation documents of 45 medical schools against a global framework, and revealed that social contribution is identified to be one of the key components in the main category of “issues in society” for social accountability (Mori et al., 2022). As an essential aspect of social contribution, the need for an individual’s lifelong learning has increased by an accumulation of factors, such as disaster-related disruptions, pandemics, and the ageing population with longevity. Medical schools can certainly use their strengths as health experts to assist in health literacy and well-being for the members of communities. In addition, the government has long been prioritising, promoting, and advancing lifelong learning in Japan, in recognition of global challenges and social changes. Therefore, social contribution activities by medical schools can come into play to satisfy the need of individuals, society, and the country.
IV. SOCIAL CONTRIBUTION THROUGH COMMUNITY LECTURES: A CASE FROM A REGIONAL MEDICAL UNIVERSITY
Here, we share an example of ongoing direct social contribution activity at our university. The university positions social contribution as a significant role and mission in Educational Philosophy, and our “Community Lectures (haken kouza)” constitutes one of the essential elements in this role. This activity began in 2002 to meet the local community’s lifelong learning needs, and the university’s members have been giving lectures at the request of local public organisations. There are over 350 different topics offered to date. The lecture themes are not limited to medical and nursing topics, but also include educational and cultural topics. Between 2016 and 2019, we provided over 600 lectures to the local and regional communities. As the northernmost medical university in Japan, it is necessary to devise something unique to the region that makes the best use of the regional characteristics, and we firmly believe that there is a stage for the university to play an active role.
V. WHAT, THEN, IS THE SOCIAL CONTRIBUTION OF UNIVERSITIES
We acknowledge that the above Community Lecture is just one example, and in fact, social contribution can take many forms and shapes and be offered at various levels. The social contribution made by universities must not be merely the provision of free labour or lending facilities, but should fully utilise the characteristics of the university as the base for intellectual creative activities. In other words, the knowledge acquired and transmitted through the university’s education and research activities should be returned to the local community by the mechanism of social contribution with the aim of improving the lives and welfare of the local population. The ideal relationship between the university and the community should not be a one-way relationship but should be a reciprocal one; where the community benefits from the intellectual and human resources of the university through community cooperation, and the university makes effective use of the region as part of its education and research.
In addition, activities such as international collaboration, regional collaboration, industry-academia-government collaboration, and training programs are all solid initiatives aimed at giving back to society in a more direct way. The university faculty and staff have been independently engaged in these activities as experts in their respective fields. These include serving on committees of administrative agencies, supporting science education in schools, joint research with industries, and public lectures for non-students. They voluntarily carry out these social contribution activities (without even recognising them as such) alongside their busy daily clinical duties, teaching and research. However, these activities are often missed or not subject to systematic evaluation by the universities. In the future, these activities should be highlighted and evaluated as important activities that play a role in the functions of universities. We hope this article will stimulate interest in expanding social contribution in the university context. For future work, we plan to review other areas of social contribution activities conducted at the university.
Notes on Contributors
Sachiko Kasamo reviewed the literature, conceptualised and took the lead in writing and editing the manuscript.
Satoshi Ozeki contributed to the conception and revision of the manuscript critically.
Hiroyasu Inoue contributed to the conception and theoretical ideas of the manuscript.
Seiji Matsumoto supervised and gave critical feedback on the intellectual content of the manuscript.
All the authors have read and approved the final manuscript.
Acknowledgement
We sincerely thank Ms Misako Sato (Institutional Research Office’s administrative staff) and the Research Support Section of Asahikawa Medical University for their support.
Funding
There is no funding source required for this study.
Declaration of Interest
All authors have no conflicts of interest to disclose.
References
Boelen, C., & Heck, J. E. (1995). Defining and measuring the social accountability of medical schools. Geneva: World Health Organization.
Global Consensus for Social Accountability of Medical Schools (GCSA). (2010). Global census for social accountability of medical schools. https://healthsocialaccountability.sites.olt.ubc.ca/files/2011/06/11-06-07-GCSA-English-pdf-style.pdf
Hosono, M. (2014). Kokuritsu daigaku niokeru syakaikoukenkatsudouno genjyou to kadai. [Current Status and Issues of Social Contribution Activities at National Universities]. The Journal of Science Policy and Research Management, 29(1), 44-49. https://doi.org/10.20801/jsrpim.29.1_44
Mori, H., Izumiya, M., Hayashi, M., & Eto, M. (2022). Current perception of social accountability of medical schools in Japan: A qualitative content analysis. Medical Teacher, 1-8. https://doi.org/10.1080/0142159X.2022.2140033
Perkins, J. A. (2016). The university in transition. Princeton University Press.
*Seiji Matsumoto
Institutional Research Office,
Asahikawa Medical University,
2-1-1-1, Midorigaoka-Higashi,
Asahikawa, Hokkaido,
078-8510, Japan
Email: matsums@asahikawa-med.ac.jp
Submitted: 11 September 2021
Accepted: 22 March 2023
Published online: 4 July, TAPS 2023, 8(3), 58-61
https://doi.org/10.29060/TAPS.2023-8-3/SC2694
Maria Isabel Atienza & Noel Atienza
San Beda University College of Medicine, Philippines
Abstract
Introduction: An evaluation of the online medical course was conducted to assess student readiness, engagement, and satisfaction at the San Beda University College of Medicine in Manila during the COVID-19 pandemic.
Methodology: A convergent mixed methods approach was done with a quantitative online survey and a qualitative thematic analysis of focus group discussions (FGD) with medical students. A total of 440 students participated in the survey while 20 students participated in the FGDs.
Results: The medical students were sufficiently equipped with computers and internet connections that allowed them to access the online medical course from their homes. The 5 themes identified during the study that were relevant to education were: Student readiness for online learning, Learning Management System (LMS) and internet connectivity, teaching and learning activities, the value of engagements, and teaching effectiveness of the faculty. The combined quantitative and qualitative analysis revealed vital issues that affect student learning. This included the need for students to interact with fellow students and to be engaged with their faculty. The issues that affect teaching included the need for continuing faculty training and management skills in delivering the full online course.
Conclusion: The success of online education rests heavily on the interactions of the students, the teachers, and the knowledge. Student interactions, managerial and skills training for the faculty, and providing students with a mix of synchronous and asynchronous activities are the most effective means to ensure the effective delivery of online medical courses.
Keywords: Medical Curricular Revision, Formative Evaluation, Student Engagement, Synchronous and Asynchronous Online Learning, Cognitive Overload
I. INTRODUCTION
The COVID-19 pandemic necessitated a shift to online teaching and a revision of the medical curriculum with synchronous and asynchronous online activities. Medical schools worldwide adapted teaching strategies utilising Video Conferencing and Learning Management Systems.
This program evaluation of the online medical course aimed to evaluate the effectiveness of instruction using the various components of online learning. The study centered on the perspectives of students using a mixed methods design (Fitzpatrick et al., 2011). The study focused on the interplay of digital capabilities, students’ perceptions and satisfaction with the interactions and engagements during the online course.
II. METHODS
The mixed methods research protocol was approved by the Institutional Ethics Board of San Beda University. The study utilised a convergent mixed method design with a quantitative online survey that was conducted on 440 respondent students representing each of the four-year levels of the medical school. Six focus group discussion (FGD) sessions were conducted on 20 students. All student participants provided a signed informed consent form to participate in the survey and in the FGDs. The 25-item online survey questionnaire included a 5-point Likert scale for items on readiness for the online course, overall satisfaction, and engagement. The online FGD sessions were conducted using an open-ended questionnaire guide on student capabilities for the online course, student satisfaction, and student engagement.
The FGD recordings were transcribed and subjected to thematic analysis to identify major themes. Quantitative and qualitative data were analysed simultaneously through a joint display of the two sets of results. A joint display using pillar integration was done to demonstrate the themes where the data corroborated or validated each other. The conceptual framework, data collection tools, the data results, and the pillar integration table are posted in a data repository file for this study can be accessed through a repository at: https://doi.org/10.6084/m9.figshare.16682569.v2 (Atienza & Atienza, 2021).
III. RESULTS
The survey revealed that students were adequately equipped with the necessary computers and smartphones needed to access the online course. Only 50% of the students were taking the online course from their homes within the same city as the medical school. While 72% encountered internet connectivity problems, 88% of students were successful in the use of the LMS and the videoconferencing platform to access the course and take online examinations.
Seventy-eight percent of students found online student-to-student and faculty-to-class interactions to be beneficial to student learning. Among the synchronous activities, 63% of students preferred live online lectures. Among the asynchronous activities, 52% of students preferred uploaded video lectures. Overall, around 52% of students experienced being overloaded with study requirements while 48% of students felt there was sufficient time for independent study.
The results of the survey and the thematic analysis of the FGDs were organised into themes and subthemes. These themes were generated from the integration of the quantitative and qualitative data. The schematic diagram (Figure 1) demonstrates how the themes are related to the effectiveness of learning based on the perspective of the students.
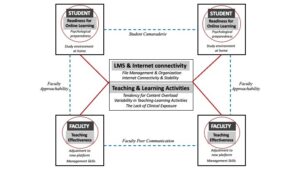
Figure 1. Schematic diagram of themes and subthemes identified in a mixed methods analysis of a fully online medical course at SBU-COM during the COVID pandemic
A. Student Readiness
The first theme that surfaced from the results was Student Readiness to engage in online learning. Students found their readiness to be dependent on two subthemes:
1) Study environment at home: Students expressed that the sudden shift to studying from home required that they designate sufficient time and space for studying. Students recognised that responsibilities at home and to the family could be distractions if not managed properly.
2) Psychological preparedness: The students also expressed the value of psychological preparedness as essential in dealing with stress and fatigue resulting from the unexpected shift to the online learning mode.
B. LMS and Internet Connectivity
The second theme highlights the importance of having computers and a stable internet connection as major determinants of student satisfaction with the online course. The introduction of an LMS for the medical course required immediate training for both the students and the faculty. While 81% of the students had the necessary gadgets and a good internet signal, 17% experienced major connection problems that disrupted up to 50% of live lectures and offline recorded videos. Student satisfaction with online learning was dependent on how timely and how organised the learning materials were uploaded into the LMS.
C. Teaching and Learning Activities
The third theme refers to the blend of online and offline activities for the different courses. The major subthemes included cognitive overload, variability of teaching and learning activities across courses, and the lack of clinical exposure.
1) Cognitive overload: Students had a perception of being overloaded by the volume of information delivered through the online course. The introduction of new forms of assessments such as video assignments, group reports, and research outputs contributed to the perceived cognitive overload.
2) Variability of teaching and learning activities: The variability in the blend of online and offline activities across the different courses required varying degrees of adjustments from the students. The students expressed their preference for live or recorded lectures over small group discussions and live laboratory demonstrations.
3) Lack of clinical exposure: Students in the 3rd and 4th year levels were apprehensive about the lack of clinical exposure in the actual medical environment due to the restrictions brought about by the pandemic. They recognise that they may not have the necessary skills training needed for internship.
D. The Value of Engagements
Unexpectedly, the fourth theme that students found important in the shift to online learning was the value of engagements.
1) Student-to-student online interactions: Up to 78% of students found support through interactions with other students. These interactions were useful not only for sharing the academic workload but also for mental and emotional support highlighting the value of student camaraderie despite being limited to virtual interactions.
2) Faculty-to-class interactions: Up to 80% of students expressed appreciation for the efforts of the faculty to get student feedback, answer clarificatory questions, and provide explanations when necessary. The students also expressed greater satisfaction with courses delivered online. Both faculty interactions with the class and with individual students were recognised as faculty approachability.
E. Teaching Effectiveness of The Faculty
The fifth theme Teaching pertains to the ability of the faculty to manage the online platform for teaching.
1) Faculty management skills: Teaching effectiveness is facilitated by the ease by which the faculty manages virtual teaching.
2) Faculty peer communication: Students recommend that the faculty within and across different courses coordinate their activities so that students can more easily manage their time and learning.
IV. DISCUSSION
The experience of delivering the medical course online has been very limited in the past. The teaching and learning strategies for medical courses to be delivered fully online require extensive preparation of the three main points in the transaction of learning: the learners, the teachers, and the course content. Learner readiness entails a clear delineation of the study environment in terms of time and space for study. Proper orientation to the online learning environment and psychological support should be made available to the students before the course begins. An inventory of the students’ computers and internet connectivity should also be done to ensure readiness for the course.
Delivering the course online necessitates faculty training on teaching and learning strategies for synchronous and asynchronous delivery as well as the proper navigation of the LMS and its available features. The faculty must maximise the benefits of technology as well as pedagogy in the online learning environment.
This study showed that in the shift of medical education to an online mode during the pandemic, student learning relies heavily on interactions between the learners, the teachers, and the course content. In an online course that relies so much on technology as a means of course delivery and integration, teaching and learning success depends on how well the interactions are established among these three points (Ifinedo & Rikala, 2019).
The design of courses must facilitate student-to-student interactions while faculty-to-class interactions using both synchronous and asynchronous activities would provide a good learning experience for students (Rhim & Han, 2020; Seymour-Walsh et al., 2020).
V. CONCLUSION
To succeed in the delivery of the online medical course, sufficient time must be given for faculty-to-student interactions during synchronous sessions and after the online classes. The faculty must demonstrate approachability by being open to continuing interactions with students outside the synchronous sessions. The coordination of faculty members within and across different courses must be enhanced to reflect efficiency in delivering their respective courses.
This study was performed during the early phase after the shift to full online delivery of the medical course. While the study is based on the perceptions of the students, the results of this study may be valuable in planning for continuing the online delivery of the medical course. The results of this study may be more robust with the inclusion of faculty perceptions and indicators of student academic performance.
Notes on Contributors
Dr. Maria Isabel Atienza conceptualised, designed, and implemented this study. She conducted the focus group discussions, prepared the thematic analysis, and wrote the manuscript for this study.
Dr. Noel Atienza helped in the design and conduct of the online survey and was involved in the data processing and data analysis of the survey. He was also involved in the preparation and editing of the final manuscript.
Ethical Approval
The research protocol SBU-REB # 2020-028 for this study was reviewed and approved by the San Beda University Research Ethics Board on November 28, 2020.
Data Availability
Data collection tools and research data are available and can be accessed by any interested reader through a repository at: https://doi.org/10.6084/m9.figshare.16682569.v2. The data in the repository may not be copied or cited without written permission from the authors.
Acknowledgment
The authors would like to acknowledge the support provided by the Alumni of San Beda and their commitment to promoting faculty research activities.
Funding
This study was funded by the Jesus P. Francisco Distinguished Professorial Chair Research Grant from the San Beda College Alumni Foundation, Inc.
Declaration of Interest
There are no conflicts of interest in this study.
References
Atienza, M., & Atienza, N. (2021). An online medical course during the COVID-19 pandemic: A mixed methods analysis. [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.16682569.v2
Fitzpatrick, J., Sanders, J., & Worthen, B. (2011). Program evaluation: Alternative approaches and practical guidelines 4th Edition. Pearson Education, Inc.
Ifinedo, E., & Rikala, J. (2019). TPACK and educational interactions: Pillars of successful technology integration. World Conference on E-Learning. Association for the Advancement of Computing in Education, 295-305. https://www.learntechlib.org/primary/p/211094/
Rhim, H., & Han, H. (2020). Teaching online: Foundational concepts of online learning and practical guidelines. Korean Journal of Medical Education, 32(3), 175-183. https://doi.org/10.3946/kjme.2020.171
Seymour-Walsh, A., Bell, A., Weber, A., & Smith, T. (2020). Adapting to a new reality: COVID-19 coronavirus and online education in the health professions. Rural and Remote Health, 20, 6000. https://doi.org/10.22605/RRH6000
*Maria Isabel Maniego Atienza
San Beda University, Mendiola Street,
Barangay San Miguel,
City of Manila, Philippines
+639178668751
Email: mimatienza@yahoo.com
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









