Defining undergraduate medical students’ physician identity: Learning from Indonesian experience
Submitted: 16 July 2023
Accepted: 21 December 2023
Published online: 2 April, TAPS 2024, 9(2), 18-27
https://doi.org/10.29060/TAPS.2024-9-2/OA3098
Natalia Puspadewi
Medical Education Unit, School of Medicine and Health Sciences, Atma Jaya Catholic University of Indonesia, Indonesia
Abstract
Introduction: Developing a professional identity involves understanding what it means to be a professional in a certain sociocultural context. Hence, defining the characteristics and/or attributes of a professional (ideal) physician is an important step in developing educational strategies that support professional identity formation. To date, there are still limited studies that explore undergraduate medical students’ professional identity. This study aimed to define the characteristics and/or attributes of an ideal physician from five first-year and three fourth-year undergraduate medical students.
Methods: Qualitative case studies were conducted with eight undergraduate medical students from a private Catholic medical school in Jakarta, Indonesia. The study findings were generated from participants’ in-depth interviews using in vivo coding and thematic analysis. Findings were triangulated with supporting evidence obtained from classroom observations and faculty interviews.
Results: First-year participants modeled their professional identities based on their memorable prior interactions with one or more physicians. They mainly cited humanistic attributes as a part of their professional identity. Fourth-year participants emphasised clinical competence and excellence as a major part of their professional identities, while maintaining humanistic and social responsibilities as supporting attributes. Several characteristics unique to Indonesian’s physician identity were ‘Pengayom’ and ‘Jiwa Sosial’.
Conclusion: Study participants defined their professional identities based on Indonesian societal perceptions of physicians, prior interactions with healthcare, and interactions with medical educators during formal and informal learning activities.
Keywords: Professional Identity Formation, Indonesia Undergraduate Medical Students, Physician Identity
Practice Highlights
- Defining the attributes of ideal physicians is important for developing strategies that support PI.
- Prior interactions with healthcare and formal/informal learning activities influence PI definition.
I. INTRODUCTION
Supporting the (trans)formation of a medical student’s identity, from a layperson to a professional, is an important process in preparing future physicians (Cruess et al., 2014; Goldie, 2012; Wald, 2015). This process includes professional identity formation (PIF) throughout their medical education continuum. Professional identity (PI) refers to how someone represents their profession’s characteristics, values, and attributes through thoughts, actions, and behaviors (Cruess et al., 2014; Gee, 2003; Luehmann, 2011). It is highly related to professionalism, which influences and shapes one’s identity in a professional context (Forouzadeh et al., 2018). The formation of PI involves developing one’s understanding of their professional roles, responsibilities, and expectations that are socio-culturally dependent (Siebert & Siebert, 2007). Therefore, the process of forming one’s PI also involves developing one’s cultural identity (Forouzadeh et al., 2018).
Studies on PI formation in medical education tend to focus on educational strategies that support PI formation during medical training (Adema et al., 2019; Ahmad et al., 2018; Cruess et al., 2015; Foster & Roberts, 2016). These studies provide insights on how to support PI formation without really addressing what needs to be taught to support medical students’ PI formation. Several theories on identity and PI formation suggest that one’s identity is formed through dialectical conversations that facilitate the acceptance, rejection, or modification of the profession’s characteristics and/or attributes into one’s core identity (Cruess et al., 2015; Gee, 2003; Siebert & Siebert, 2007; Stets & Burke, 2000). These characteristics and/or attributes are usually context-dependent (Cruess et al., 2014). Thus, defining and understanding what it means to be a professional physician in a certain socio-cultural context is as important as finding out how best to facilitate its formation in an educational setting (Wacquant, 2013).
Altruism and humanism are the two most cited values expected from a physician, along with integrity and accountability, honesty, and morality (Cruess et al., 2014; Edgar et al., 2020; Hall, 2021). Additionally, care providers, researchers, and teachers are some professional roles of physicians often mentioned in the literature (Ahmad et al., 2018; Branch & Frankel, 2016; Carlberg-Racich et al., 2018; Hatem & Halpin, 2019). Nevertheless, there might be other roles and characteristics that have yet to be fully elucidated, especially considering that the current literature on PI formation is mainly dominated by the Western representation of the medical profession.
This study aimed to describe the characteristics and/or attributes of ideal (professional) physicians in Indonesia as defined by undergraduate medical students. Undergraduate medical students are unique as they have limited opportunities to interact with real patients in a real workplace. Through this study, we hope to gain new insights from undergraduate medical students on what it means to be a professional physician.
II. METHODS
This was a qualitative phenomenology research using case studies design at a private Catholic medical school in Jakarta, Indonesia. Participants were recruited using a purposive sampling method. Transitional phases in one’s life are often associated with identity renegotiation as they are exposed to changes in their roles, responsibilities, and expectations (Kay et al., 2019). Therefore, we sought to explore how Indonesian undergraduate medical students defined their professional identity at the beginning (first-year) and end (fourth-year) of their preclinical years. Ethical clearance was obtained from the school’s Research Ethics Committee prior to the study.
We set a quota of 5 participants for each study year (with a total of 10 study participants) to account for any possible socioeconomic status, ethnicity, religion, and gender variations. We recruited five first-year and five fourth-year preclinical students at the beginning of the study; however, two of the fourth-year participants dropped out during data collection; hence, only eight case studies constructed to depict the characteristics and/or attributes of an ideal Indonesian physician.
Each case study participant was interviewed twice using semi-structured interviews. The first interview was conducted at the beginning of school semester (August 2021) and the follow up interview was conducted one month after. The purpose of the first interview was to determined participants’ current understanding and views of what it meant to be a physician, while the second interview aimed to determine if there were any changes in their understanding or views and what precipitated the changes. Interview questions include: What kind of physician do you aspire to be? Was there one or more specific moment that prompted you to become a physician (if so, please describe it)? What characteristics and/or attributes should an ideal physician possess? Please explain. At the follow-up interviews, participants were asked to re-describe the characteristics and/or attributes of physicians that they aspired to be and what prompted the changes. Furthermore, participants were also asked to describe any specific learning moments that might influence their understanding of what it means to be a professional physician. Because of the COVID-19 physical distancing policy during the data collection phase, all data were obtained virtually or through electronic exchange via secured online platforms. All interviews were transcribed verbatim and analysed in vivo using abductive thematic analysis with Atlas.Ti 8
In addition to from the interviews, we also conducted several classroom observations. We observed the first- and fourth-year’s large classroom lecture, problem-based learning, and skills laboratory session once, focusing on the teacher-student interactions and made note on how, if any, the faculty member facilitated students’ PI formation in the classroom. We also interviewed several faculty members who interacted with the participants in teaching capacity during the data collection phase. Faculty members were asked to describe what kind of physicians they wanted their students to be based on institutional values and their own beliefs about what constitutes an ideal physician. They were also asked to elaborate on their efforts to facilitate those characteristics and/or attributes in the formal and informal curriculum.
Data obtained from classroom observation and faculty interviews were used to triangulate the findings from the participants’ interviews. Permission was obtained from all related parties to record and use the interviews and classroom interactions in the data analysis. Individual case study reports were generated by combining the data obtained from interviews and field notes. These case study reports were then cross-analysed to find commonalities across the case studies to define the characteristics and/or attributes of an ideal physician that the participants aspired to be at their current stage of education.
III. RESULTS
The majority of participants were either Chinese or of Chinese descent. Five participants were Christian Protestants, one was a Buddhist, and two refused to disclose their ethnicity and religion. Note that the names used in these case studies are pseudonyms.
A. Case Study #1: Celine (First-year Student)
Celine, a female of Chinese-Betawi descent from West Java, was raised in a devout Christian-Protestant family. Being a physician was not her childhood aspiration. Initially, she thought physicians tended to be “rude, bossy, had too much pride, unwilling to listen to suggestions” (Celine, Interview 1, Line 42-43), which contradicted her personal values to being humble and helping others as a form of service and manifestation of her faith. Nevertheless, she developed a new appreciation toward physicians when she found out that there were physicians who gave back to the surrounding community by providing free healthcare (see Appendix No. 1).
Humility, and self-reflectiveness—which Celine called “openness to criticism” (Celine, Interview 1, Line 39-44) were the characteristics she deemed important as a physician. She believed that a physician should engage in social actions and put the patient first. Furthermore, a physician should consider the patient’s personal circumstances while providing individualised healthcare based on the patient’s needs. A good physician should also believe that their most important role is to provide credible health information and educate the community to improve their health and well-being. Good communication skills, including active listening, empathy, building trust, and the ability to break bad news, were essential in supporting this role (see Appendix No. 2).
B. Case Study #2: Dimitri (First-year Student)
Dimitri, a Christian-Protestant female of Chinese descent, was quite familiar with medicine and the medical profession as she was surrounded by people who either worked as or studied to become a physician. Additionally, she helped caring for her visually impaired sibling since she was young, which gave her opportunities to interact with various care providers as she accompanied her sibling for treatment. Being a physician naturally became her aspiration since childhood. Dimitri was appointed as a ‘Dokter Kecil’ (or, ‘little doctor’) in elementary school, assigned to provide first aid treatment to fellow students and promote health efforts conducted by the school. Before entering medical school, Dimitri’s grandfather fell critically ill; therefore, she helped her family to care for him in the hospital. There, she met a cardiologist whom she respected. She recalled that she appreciated the way this cardiologist relayed which information could be shared with her grandfather to keep his spirit up and which information should be disclosed to her family to prepare for the worst possible outcome. She mentioned that her grandfather looked “calm and comfortable” in his last days, which helped the family to accept his departure peacefully (Dimitri, Interview 1, Line 77-80).
Dimitri highlighted a physician’s ability to handle the distribution of information as an important part of her ideal physician identity (See Appendix No. 3). She believed that it was acceptable for a physician to keep certain information from the patient if that information could add unnecessary stress or cause them to stop following the treatment (Dimitri, Interview 1, Line 90-98). Regardless, the physician should disclose all information to the patient’s relatives as the patient’s decision-maker. Dimitri aspired to be a caring and compassionate physician with good communication skills who can be held accountable for her actions. Aside from being a care provider, Dimitri believed that a physician should take on a role as ‘Pengayom’ (protector). She believed that patients were in vulnerable positions due to their health issues, and therefore the physician was responsible for protecting them like a parent would when their child was sick. Implied in the Pengayom role was the leader whose responsibility was to make the best decision for the patient’s health and well-being (See Appendix No. 4).
C. Case Study #3: Faustine (First-year Student)
Faustine, a Christian-Protestant female of Chinese descent, was born and raised in a remote area in Riau province, in the southern part of Sumatra Island. Her interest in biology and life sciences prompted her to browse online videos related to healthcare since she was young. She tended to feel sad if the people closest to her were suffering and she could not do anything to help. She made up her mind to study medicine when one of her high school friends was forced to seek treatment abroad because of limited healthcare access in her region. Prior to this, her father was misdiagnosed with a malignant tumor, which caused tremendous distress for her family. These incidents drove her to be a physician who could provide good quality care, especially to those closest to her (See Appendix No. 5).
Faustine aspired to be an empathetic physician, taking patients’ mental or psychological state into consideration when planning for their treatment. She did not want to be a physician who focused on financial gain at the cost of the patient’s wellbeing. Being aware of her limitations in providing care and continuously updating her knowledge and skills were characteristics she hoped to develop once she became a physician (Faustine, Interview 1, Line 103-115). Faustine also mentioned that a physician was responsible for being a reliable source of information and improving community wellbeing through education (See Appendix No. 6).
D. Case Study #4: Jasmine (First-year Student)
Jasmine originated from Rembang, a small regency on the northeast coast of Central Java. Being a physician had always been her childhood aspiration because she loved helping people and interacting with others. Jasmine tended to her grandmother’s health needs during middle school. This event confirmed her passion and desire to serve others. Putting others’ needs above herself was a value instilled by her father since she was young. She wanted to be a physician who focused on social services, and was driven to help others sincerely without expecting anything in return.
As Jasmine mentioned, an ideal physician should be honest, disciplined, possess high ‘Jiwa Sosial’ (an attitude that shows concern to perform actions that are beneficial for humanity and social community), and always put the patient’s needs first (Jasmine, Interview 1, Line 50-53). Jasmine viewed her work as an extension of her faith, and she wanted to reflect Christian values, particularly the value of servitude, in her professional life (See Appendix No. 7-8).
E. Case Study #5: Rose (First-year Student)
Rose, a Christian-Protestant female of Chinese descent, was born and raised in Ambon city, Maluku province, Eastern Indonesia. She was the oldest child in her family. Rose became interested in medicine when her mother was diagnosed with a serious illness and could not receive appropriate treatment. She disclosed that her mother ignored the early signs and symptoms of her illness until her condition became so severe that she could not be treated fully. From this experience, Rose was motivated to become a physician so that she could take better care of her family (See Appendix No. 9).
Growing up, Rose heard several stories in which a patient did not receive appropriate healthcare due to their socioeconomic status. She aspired to be a competent and non-discriminative physician. Putting the patient’s needs first, being responsible, helpful, patient, disciplined, and continuously improving her knowledge and skills were the characteristics that she hoped to develop by the time she became a physician. Aside from being a care provider, Rose believed that a physician was responsible for improving the wellbeing of the community through education (See Appendix No. 10).
F. Case Study #6: *Anton (Fourth-year Student)
*Anton, a Christian-Protestant male of Chinese-descent, had an interest in biology since childhood. He was dissatisfied with Indonesian healthcare services, particularly with the healthcare workers’ communication skills when treating his father. This incident occurred when he was in middle school. *Anton observed a power imbalance between the patients and physicians, where the healthcare providers held more power over their patients. As a patient, he felt disadvantaged because he could not demand a better quality of care nor asked for a lower cost of the care he received (See Appendix No. 11). He described the two roles of physicians: as a healthcare provider and educator. As a healthcare provider, one should be able to help patients understand what is best for them while still respecting their autonomy. As educators, physicians have the responsibility to provide valid evidence-based information for patients.
For *Anton, an ideal physician’s fundamental values and skills included providing good quality care that kept the patients’ best interest, respecting patients’ autonomy, doing no harm, having all necessary medical competencies as listed in the Competence Standards of Indonesian Physician, the drive to learn for a lifetime, patience, humility, competence, and the ability to engage in interprofessional collaboration (See Appendix No. 12).
G. Case Study #7: *R (Fourth-year Student)
*R is a Chinese Buddhist female from Sintang, central Indonesia. *R wanted to pursue medicine because physician was portrayed as a noble profession in Indonesia and as a ‘role model’ in her family. She wanted to serve marginalised areas in East Indonesia after hearing about the poor health situation in those areas from several alumni and fellow students who served there in various capacities. This experience, along with her formal learning experiences, shaped her ideal physician image, which included being detail-oriented, confident, honest, thorough, and caring. She believed that physicians should be able to fulfill the roles and responsibilities of a healthcare provider, which required good proficiency in medical competencies, based on several fundamental values such as honesty, willingness to serve marginalised and under-served communities, and being sensitive to patients’ needs (See Appendix No. 13).
H. Case Study #8: *Anastasia (Fourth-year Student)
*Anastasia, who identified as a female, wanted to be a physician since elementary school. She did not have a specific motivation to enter a medical school when she first started. Nevertheless, there were several past experiences that she claimed to have influenced her image of ideal physicians. She mentioned feeling comfortable being examined by her pediatrician during her childhood. This made her consider the pediatrician as her role model. She also followed several healthcare professionals’ whom she admired on their social media accounts. She claimed that these figures influenced her to be selfless and put the patients’ needs above her own. She acknowledged the importance of entrepreneurial skills in aiding her goal of being selfless yet still able to make a living for herself. Her ideal physician image is someone who has good communication skills, clinical competence, and willingness to learn continuously. She identified healthcare provider as the essential role of a physician, who was responsible for providing physical and mental healthcare, as well as participating in preventive and promotive healthcare. She particularly considered female medical teachers at her school as her role models because she admired the way these figures divide their time and energy to work professionally–both as healthcare practitioners and teachers–and keeping up with their personal and family time. She aspired to be someone who could divide her focus like these figures once she graduated (See Appendix No. 14).
IV. CROSS-CASE ANALYSIS AND DISCUSSION
Cross-case analysis revealed four major attributes of physician identity as defined by the first- and fourth-year participants (indicated by * behind their pseudonyms), including characteristics, values, roles and responsibilities, and skills. First-year participants drew their ideal image of a physician based on their interactions with one or more healthcare provider whom they met in their earlier lives. These interactions left a significant impression that further strengthened their motivation to study medicine and influenced the kind of values or other things that they held important and were willing to stand for as future physicians.
First-year participants mainly mentioned humanistic and altruistic values as the characteristics and/or attributes that define their professional identity. Honesty, humbleness/humility, accountability, patience, jiwa social, prioritising patients’ needs, empathy, care, and compassion are some of the characteristics mentioned by the first-year participants as characteristics of an ideal physician. These characteristics correspond to society’s expectations of professional physicians to put patient’s interest above all else, which is then further translated into medical professionalism and professional responsibilities (Alrumayyan et al., 2017; Elaine Saraiva Feitosa et al., 2019).
Different from their counterparts, fourth-year participants focused on clinical excellence and competence when citing the ideal characteristics and/or attributes of an ideal physician based on the national Competence Standards for Indonesian Physician. This indicates that fourth-year participants were aware of the standards as well as the ethical principles and physician’s code of conduct that were being enforced in Indonesia (See Appendix 15-16).
The way fourth-year participants described their physician identity aligned with the image of a professional physician painted by the school’s teaching faculty. According to interviews with several key faculty members, meeting the minimal standard of competence, being aware of one’s limitations, practicing evidence-based medicine, honesty, and discipline were some of the fundamental physician attributes/values/characteristics that they tried to instill in their students during education. These institutional values were most notably found in the way first-year participants described their physician identity during their second interview (See Appendix No. 17-18).
The attributes of Indonesian physicians mentioned by all case studies participants closely resemble China’s framework of professionalism, where they emphasise altruism, integrity and accountability, excellence, and religion/moral values (Al-Rumayyan et al., 2017). Possessing jiwa sosial (inherent sense of social responsibility, empathy, and engagement) and being a pengayom (mentor/guardian/protector) are two unique attributes that represent the Indonesian ideal physician.
There were minimal overlaps between the first- and fourth-year participants’ ideal physician images. First-year participants placed humanism/altruism and social responsibility as the focal points of their physician identity, whereas fourth-year participants chose clinical excellence and competence to represent their physician identities. Social interactions play a major role in identity formation (Thomas et al., 2016). This may explain the shift in the first- and fourth-year participants’ definition of an ideal physician. First-year participants modeled their ideal physician identity after their memorable interactions with physicians who provided care for them or their family members. Positive past interactions with healthcare providers shaped the characteristics and/or attributes that participants aspired to be, whereas negative past interactions motivated them to develop the opposite of observed characteristics and/or attributes. Fourth-year participants also integrated the characteristics and/or attributes they identified from the formal and informal learning experiences with their evolving understanding of an ideal physician. In these case studies, fourth-year participants cited clinical competencies and excellence, as well as discipline and honesty—which were emphasised by the teachers during their undergraduate medical training—as the major characteristics and/or attributes that defined their physician identity.
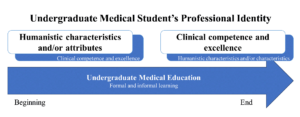
Figure 1. Shift in First-Year and Fourth-Year Participants’ Definition of Physician Identity
The first year of the medical curriculum was indicated to be an important transition point that shaped all participants’ PI. In particular, all participants mentioned the school orientation as one of the learning moments that triggered their identity negotiation. Participants were introduced to the school’s expectations of them as medical students and future physicians. These expectations include the characteristics of self-regulated and life-long learners and those of professional physicians (See Appendix No. 19-20). For example, Jasmine “learned to be disciplined and responsible and she believed that the school orientation “helped shape [her] basic personality as a physician [who needs] to be disciplined and responsible [as well as] trustworthy.” (Jasmine, Interview 1, Line 115-118).
The shifts in participants’ physician identity definition indicated that participants engaged in a dialectical conversation that stimulated them to merge their core or personal identity with the institution’s perception of ideal physicians (“virtual/ideal identity) as interpreted in their curriculum, which was a part of one’s identity negotiation process (Gee, 2003). In the cross-case analysis, we found that participants’ reactions toward the values, characteristics, and attributes instilled by the faculty varied. For example, some participants saw the importance of being on time (‘discipline’) as well as being academically honest by avoiding plagiarism and cheating during exams (‘honesty’), which they accepted as a part of their physician identity. On the other hand, other participants struggled to understand the relevance of being on time and academically honest with their future physician roles or aspirations. This became a major challenge for these participants in incorporating those values into their physician identity. Nevertheless, no participants rejected any characteristics/attributes instilled by the institution even if those characteristics/attributes were distinctly different from their personal beliefs system (See Appendix No. 21-23).
Any new or contradictory characteristics or attributes to one’s core identity pose a professional dilemma that triggers an identity negotiation (Spencer et al., 1997). During this identity negotiation process, the study participants tried to merge their core identity, which was represented by their definition of the ideal physician that they aspired to be, either by accepting, rejecting, or integrating the new characteristics/attributes into their core identity (Cruess et al., 2015).
The acceptance of new characteristics/attributes into one’s physician identity will be easier if it is consistent with one’s core identity; however, it is still possible to instill characteristics/attributes that contradict one’s core identity if they are provided with the long-term benefit of accepting those characteristics/attributes (Guillemot et al., 2022). This underlined the importance of providing students with the relevancy of developing certain characteristics/attributes desired from a professional physician during their educational phase to support their PIF.
V. CONCLUSION
This case study found that first-year participants prioritised humanistic characteristics as the foreground of their professional identity, and medical professionalism as their background. Meanwhile, fourth-year participants developed a projected identity that embodied the general values of the medical profession and those promoted by their institution. The perceived image of ideal physicians as constructed by the Indonesian society’s ideal image of a physician, prior interactions with Indonesian physicians that influenced their decisions to study medicine, and interactions with the medical teachers during formal and informal learning activities influenced the way participants defined their professional identity.
Notes on Contributors
Natalia Puspadewi contributed to the work’s conception and design by developing the study proposal, protocols and instruments, data collection, analysis, and interpretation. Further, Natalia also drafted and revised the manuscript and ensured that all aspects of the work were accountable, and followed all procedures to ensure data security and anonymity.
Ethical Approval
This study was a part of a doctoral dissertation. The University of Rochester acted as the author’s host institution, and Atma Jaya Catholic University of Indonesia, School of Medicine and Health Sciences, was the research site. Ethical approval was provided by the University of Rochester RSRB (a letter of exempt determination was obtained on July 8th, 2021 for Study ID 00006273) and the Atma Jaya Catholic University of Indonesia, School of Medicine and Health Sciences Ethics Committee (ethical clearance certificate No. 08/07/KEP-FKUAJ/2021).
Data Availability
The data supporting the findings of this study are openly available in the Figshare repository
https://doi.org/10.6084/m9.figshare.23684235. The data were not translated into English to preserve the Indonesian sociocultural nuances captured in the interviews. All data were coded and analysed in vivo in Bahasa Indonesia before being translated into English for presentation in this manuscript.
Acknowledgement
We would like to express our gratitude to those who have contributed to this study and article development: Dr. Rafaella Borasi as the head of the dissertation committee and advisor, Dr. Sarah Peyre as dissertation committee member, and Gracia Amanta, MD and Cristopher David, MD who helped with manuscript organisation and layouts.
Funding
This study was funded by the Atma Jaya Catholic University of Indonesia and American Indonesian Cultural and Education Foundation.
Declaration of Interest
The author has no conflicts of interest to disclose.
References
Adema, M., Dolmans, D., Raat, J. a. N., Scheele, F., Jaarsma, D., & Helmich, E. (2019). Social interactions of clerks: The role of engagement, imagination, and alignment as sources for professional identity formation. Academic Medicine, 94(10), 1567. https://doi.org/10.1097/ACM.0000000000002781
Ahmad, A., Yusoff, M. S. B., Mohammad, W. M. Z. W., & Nor, M. Z. M. (2018). Nurturing professional identity through a community based education program: Medical students experience. Journal of Taibah University Medical Sciences, 13(2), 113–122. https://doi.org/10.1016/j.jtumed.2017.12.001
Alrumayyan, A., Van Mook, W. N. K. A., Magzoub, M., Al-Eraky, M. M., Ferwana, M., Khan, M. A., & Dolmans, D. (2017). Medical professionalism frameworks across non-Western cultures: A narrative overview. Medical Teacher, 39(sup1), S8–S14. https://doi.org/10.1080/0142159X.2016.1254740
Branch, W. T., & Frankel, R. M. (2016). Not all stories of professional identity formation are equal: An analysis of formation narratives of highly humanistic physicians. Patient Education and Counseling, 99(8), 1394–1399. https://doi.org/10.1016/j.pec.2016 .03.018
Carlberg-Racich, S., Wagner, C. M. J., Alabduljabbar, S. A., Rivero, R., Hasnain, M., Sherer, R., & Linsk, N. L. (2018). Professional identity formation in HIV care: Development of clinician scholars in a longitudinal, mentored training program. Journal of Continuing Education in the Health Professions, 38(3), 158–164. https://doi.org/10.1097/CEH.0000000000000214
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2014). Reframing medical education to support professional identity formation. Academic Medicine, 89(11), 1446-1451. https://doi.org/10.1097/ACM.0000000000000427
Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2015). A schematic representation of the professional identity formation and socialisation of medical students and residents: A guide for medical educators. Academic Medicine, 90(6), 718-725. https://doi.org/10.1097/ACM.0000000000000700
Edgar, L., McLean, S., Hogan, S. O., Hamstra, S., & Holmboe, E. S. (2020). The milestones guidebook. Accreditation Council for Graduate Medical Education (ACGME).
Feitosa, E. S., Brilhante, A. V. M., De Melo Cunha, S., Sá, R. B., Nunes, R. R., Carneiro, M. A., De Sousa Araújo Santos, Z. M., & Catrib, A. M. F. (2019). Professionalism in the training of medical specialists: An integrative literature review. Revista Brasileira De Educação Médica, 43(1), 692–699. https://doi.org/10.1590/1981-5271v43suplemento1-20190143.ING
Forouzadeh, M., Kiani, M., & Bazmi, S. (2018). Professionalism and its role in the formation of medical professional identity. Medical Journal of the Islamic Republic of Iran, 32(1), 765–768. https://doi.org/10.14196/mjiri.32.130
Foster, K., & Roberts, C. (2016). The heroic and the villainous: A qualitative study characterising the role models that shaped senior doctors’ professional identity. BMC Medical Education, 16(1), 206. https://doi.org/10.1186/s12909-016-0731-0
Gee, J. P. (2003). What video games have to teach us about learning and literacy. Computers in Entertainment, 1(1), 20. https://doi.org/10.1145/950566.950595
Goldie, J. (2012). The formation of professional identity in medical students: Considerations for educators. Medical Teacher, 34(9), e641–e648. https://doi.org/10.3109/0142159X.2012.687476
Guillemot, S., Dyen, M., & Tamaro, A. (2022). Vital service captivity: Coping strategies and identity negotiation. Journal of Service Research, 25(1), 66–85. https://doi.org/10.1177/10946705 211044838
Hall, C. (2021). Professional identity in nursing. In R. Ellis & E. Hogard (Eds.), Professional identity in the caring professions: Meaning, measurement and mastery. Routledge. https://www.taylorfrancis.com/books/9781003025610
Hatem, D. S., & Halpin, T. (2019). Becoming doctors: Examining student narratives to understand the process of professional identity formation within a learning community. Journal of Medical Education and Curricular Development, 6. https://doi.org/10.1177/2382120519834546
Kay, D., Berry, A., & Coles, N. A. (2019). What experiences in medical school trigger professional identity development? Teaching and Learning in Medicine, 31(1), 17–25. https://doi.org/10.1080/10401334.2018.1444487
Luehmann, A. (2011). The lens through which we looked. In A. Luehmann & R. Borasi (Eds.), Blogging as change: Transforming science & math education through new media literacies. Peter Lang Inc.
Siebert, D. C., & Siebert, C. F. (2007). Help seeking among helping professionals: A role identity perspective. American Journal of Orthopsychiatry, 77(1), 49–55. https://doi.org/10.1037/0002-9432 .77.1.49
Spencer, M. B., Dupree, D., & Hartmann, T. (1997). A Phenomenological Variant of Ecological Systems Theory (PVEST): A self-organisation perspective in context. Development and Psychopathology, 9(4), 817–833. https://doi.org/10.1017/S0954579497001454
Stets, J. E., & Burke, P. J. (2000). Identity theory and social identity theory. Social Psychology Quarterly, 63(3), 224–237. https://doi.org/10.2307/2695870
Thomas, E. F., McGarty, C., & Mavor, K. (2016). Group interaction as the crucible of social identity formation: A glimpse at the foundations of social identities for collective action. Group Processes & Intergroup Relations, 19(2), 137–151. https://doi.org/10.1177/1368430215612217
Wacquant, L. (2013). Homines in extremis: What fighting scholars teach us about habitus. Body & Society, 20(2), 3-17. https://doi.org/10.1177/1357034X13501348
Wald, H. S. (2015). Professional identity (trans)formation in medical education: Reflection, relationship, resilience. Academic Medicine, 90(6), 701. https://doi.org/10.1097/ACM.00000000000 00731
*Natalia Puspadewi
School of Medicine and Health Sciences,
Atma Jaya Catholic University of Indonesia,
Jl. Pluit Selatan Raya No. 19, Penjaringan,
Jakarta Utara, 14440
Email: natalia.puspadewi@atmajaya.ac.id
Submitted: 1 May 2023
Accepted: 21 December 2023
Published online: 2 April, TAPS 2024, 9(2), 5-17
https://doi.org/10.29060/TAPS.2024-9-2/OA3053
WCD Karunaratne1, Madawa Chandratilake2, Kosala Marambe3
1Centre for Medical Education, School of Medicine, University of Dundee, United Kingdom; 2Department of Medical Education, Faculty of Medicine, University of Kelaniya, Sri Lanka; 3Department of Medical Education, University of Peradeniya, Sri Lanka
Abstract
Introduction: The literature confirms the challenges of learning clinical reasoning experienced by junior doctors during their transition into the workplace. This study was conducted to explore junior doctors’ experiences of clinical reasoning development and recognise the necessary adjustments required to improve the development of clinical reasoning skills.
Methods: A hermeneutic phenomenological study was conducted using multiple methods of data collection, including semi-structured and narrative interviews (n=18) and post-consultation discussions (n=48). All interviews and post-consultation discussions were analysed to generate themes and identify patterns and associations to explain the dataset.
Results: During the transition, junior doctors’ approach to clinical reasoning changed from a ‘disease-oriented’ to a ‘practice-oriented’ approach, giving rise to the ‘Practice-oriented clinical skills development framework’ helpful in developing clinical reasoning skills. The freedom to reason within a supportive work environment, the trainees’ emotional commitment to patient care, and their early integration into the healthcare team were identified as particularly supportive. The service-oriented nature of the internship, the interrupted supervisory relationships, and early exposure to acute care settings posed challenges for learning clinical reasoning. These findings highlighted the clinical teachers’ role, possible teaching strategies, and the specific changes required at the system level to develop clinical reasoning skills among junior doctors.
Conclusion: The ‘Practice-oriented clinical skills development framework’ is a valuable reference point for clinical teachers to facilitate the development of clinical reasoning skills among junior doctors. In addition, this research has provided insights into the responsibilities of clinical teachers, teaching strategies, and the system-related changes that may be necessary to facilitate this process.
Keywords: Clinical Reasoning, Medical Decision Making, Medical Graduates, Junior Doctor Transition, Hermeneutic Phenomenology, Qualitative Research
Practice Highlights
- A safe environment and early healthcare team integration facilitate learning clinical reasoning.
- Adopting a comprehensive approach to reasoning can overcome specialty-specific reasoning challenges.
- Trainees’ emotional commitment toward patients could help them learn clinical reasoning skills.
- Interrupted supervisory relationships and early acute care exposure can hamper learning reasoning.
- Ensuring junior doctor training is both service and learning oriented is of paramount importance.
I. INTRODUCTION
Clinical reasoning is composed of cognitive processes, metacognitive processors, and behaviour during the application of critical thinking to a clinical situation and is heavily influenced by numerous contextual factors related to the doctor, patient, and the clinical environment (Durning et al., 2011; Durning et al., 2013; Norman, 2005).
The clinical reasoning of learners evolves along the continuum of medical education with unique challenges associated with major transition phases, the progression from non-clinical to clinical stage, medical graduate to junior doctor, and specialist trainee to medical specialist (Teunissen & Westerman, 2011). Notably, the medical graduate to junior doctor transition presents more pronounced difficulties (Brennan et al., 2010), primarily due to changing roles and responsibilities towards patient care, limited experience in navigating clinical uncertainties, and the need to work within multi-professional teams with limited support. Consequently, these factors have contributed to a steep learning curve for developing clinical reasoning skills (Brennan et al., 2010; Lempp et al., 2005; Prince et al., 2004; Tallentire et al., 2017). The challenges in developing reasoning skills are associated with the reduced applicability of undergraduate training in clinical practice (Cave et al., 2009; Monrouxe et al., 2017), coordinating and organising clinical and administrative responsibilities (Cameron et al., 2014; Teunissen & Westerman, 2011), and dealing with diverse contextual factors in practice. These factors encompass navigating hierarchical relationships and meeting the expectations of seniors, difficulties in recognising disease severity, uncertainty regarding their role, and tension in interpersonal relationships with team members (Cameron et al., 2014; Tallentire et al., 2011, 2017). When these challenges are not resolved, they could boil down to deficits in clinical reasoning and diagnostic error leading to adverse patient outcomes (Graber et al., 2005; Huckman & Barro, 2005; Jen et al., 2009).
The challenging nature of the junior doctor transition is shared across many similar contexts globally (Prince et al., 2000; Teunissen & Westerman, 2011) calling for a coherent approach to facilitate learning clinical reasoning. Concerns around clinical reasoning deficits of doctors continue to soar even today in resourceful developed countries (Health Services Safety Investigation Body, 2022; Huckman & Barro, 2005; Jen et al., 2009), emphasising the need for faculty to take decisive actions to resolve it! Unless for the limited research on clinical reasoning outside the western region (Lee et al., 2021), the situation could have been the same elsewhere.
There is ample evidence of numerous factors that may improve the development of clinical reasoning skills. Accordingly, work experience (Ericsson, 2004; Norman, 2005; Norman et al., 2007), a strong foundation on basic biomedical concepts (Woods, 2007), reflective practice (Mamede et al., 2008, 2012), feedback (Hattie & Timperley, 2007), learning from others during practice, and conducive organisational context for learning (Goldacre et al., 2003; Hattie & Timperley, 2007; Lempp et al., 2005) are found to be central in learning clinical reasoning. This evidence, however, is not specific to junior doctors. The learning needs of junior doctors in transition may vary from other trainee doctors and other health professions staff. Therefore, it has become critical that the clinical reasoning experiences, challenges, and practices of junior doctors as a vulnerable group of trainees are understood well to be able to better support their development of clinical reasoning.
When exploring this period of transition, the five-stage model of adult skill acquisition from novice to expert (Dreyfus, 2004), can help understand how junior doctors progress in relation to these stages. The situated learning theory (S. J. Durning & Artino, 2011; Lave, 1991) can provide the basis for understanding the social nature of learning clinical reasoning. The influence of contextual factors on mediating internal motivation for learning clinical reasoning can be understood through the self-determination theory (Ryan & Deci, 2000; Taylor & Hamdy, 2013). Therefore, to gain a better understanding of the transition experiences from medical graduates to junior doctors, a longitudinal study was designed using the above theoretical models as the conceptual framework to explore the following research questions:
(1) How do junior doctors evaluate their learning experiences of clinical reasoning development?
(2) What adjustments in the application of different educational means into the learning environment are necessary to improve the development of clinical reasoning skills?
II. METHODS
A. Methodology
The methodological approach of hermeneutic phenomenology (Crotty, 1998; Laverty, 2003) was employed in this study (Kafle, 2011; Laverty, 2003). Such an approach to clinical reasoning was adopted by other researchers exploring clinical reasoning (Ajjawi & Higgs, 2007; Langridge et al., 2015; Robertson, 2012).
B. Study Setting
The study was conducted at the North Colombo Teaching Hospital, Ragama, Sri Lanka with ethical clearance (P/11/01/16) from the Faculty of Medicine, University of Kelaniya.
In Sri Lanka, medical undergraduate training is a five-year programme with two pre-clinical and three clinical years. After graduation, medical graduates follow a 12-month internship where they work under a consultant for six months each in any of the two main clinical specialities, namely, Medicine, Surgery, Paediatrics, and Gynaecology & Obstetrics before obtaining full registration as a medical doctor.
C. Study Design and Sampling
The study participants were junior doctors during the 12 months of internship following graduation. Maximum variation sampling (Cohen et al., 2017), which enabled purposefully selecting the widest range of variation on dimensions of interest relevant to learning and practicing clinical reasoning was employed. The concept of ‘information power’ which sought not theoretical saturation but sufficient information to address the research questions informed the sample size (Malterud et al., 2016; Varpio et al., 2017). Hence, junior doctors working in the four main clinical specialties, in both university clinical wards staffed by university clinical academics and other clinical wards composed of medical consultants under the Ministry of Health and according to gender were enrolled in the study following informed consent.
Accordingly, eighteen junior doctors (n=18, males=8, females=10) from the four main clinical specialities (Medicine-4, Surgery-5, Paediatrics-4, Obstetrics and Gynaecology-5) were enrolled in the first stage of the study. The second stage of the study imposed heavy demands on the study participants because it involved recording multiple doctor-patient encounters and subsequent discussions based on stimulated recall. Therefore, out of the initially recruited participants, only the well-articulated consenting participants (n=8), who could proficiently express their thoughts and reasoning to obtain a good insight into the nature of practicing clinical reasoning were enrolled in this stage.
D. Data Collection
The data collection proceeded in two stages.
During the first stage, a combination of individual semi-structured interviews with narrative interviews were conducted. Semi-structured interviews allowed probing where necessary (Cohen et al., 2017), while the narratives allowed participants to tell their stories of clinical reasoning (Muylaert et al., 2014). Each lasted for 45-50 minutes.
The second stage included audio-recording the patient consultations of the selected participants on predefined dates during the first and second six months of their internship. The consultations were replayed, and post-consultation discussions were conducted soon afterward by employing a stimulated recall method, to account for a total of 48 post-consultation discussions. As clinical reasoning is a concept revealed only in action (Charlin et al., 2000), employing such an approach was considered essential during this study.
E. Data Analysis
All interviews and discussions were transcribed verbatim. The data analysis followed phenomenological and hermeneutic strategies, which required a thorough description of lived experiences (Ajjawi & Higgs, 2007) and employing a hermeneutic circle for data interpretation by moving back and forth between the parts and the whole of the experience to reach a deeper understanding of the experience (Laverty, 2003).
Thematic data analysis (Braun & Clarke, 2012) was conducted to generate themes explaining the data set as a whole.
The principal researcher developed two thematic frameworks for the two stages of the study. The two supervisors of the project re-coded selected transcripts from each stage. These independently derived frameworks were discussed, themes refined, and new themes identified until an agreement was reached. The finalised thematic framework was employed to code all the transcripts using the Atlas.ti qualitative data analysis tool.
III. RESULTS
A total of 18 individual interviews and 48 post-consultation discussions were analysed giving rise to seven themes. During analysis, it was noted that the factors that inform the development of clinical reasoning could be condensed together as a model. This is presented later in the text.
Each theme is elaborated below with quotations. When more than one quotation is required to describe a theme, these are presented within a table. Additional supportive quotations are openly available in Figshare at https://doi.org/10.6084/m9.figshare.23536548.v2 (Karunaratne et al., 2023).
A. A Safe and Supportive Working Environment Empowers Junior Doctors to Develop Clinical Reasoning Skills
It was the collective view that a ‘safe’ work environment is characterised by easy access to more experienced doctors, and the presence of a safety net of seniors who review junior doctors’ work and understand their reasoning challenges. It provided junior doctors the opportunity and freedom to practice clinical reasoning independently, learn from errors, and arrive at their own reasoning decisions.
Such a conducive work environment also provided them with opportunities to emulate seniors and receive real-time feedback while actively participating in authentic tasks and applying knowledge and skills acquired during their undergraduate training.
“I’m working in a unit where each admission is clerked by the registrar. So, in that case, we are always in feedback…What I usually do is sometimes I clerk the patients first, and after that, I compare it with the registrar’s clerking. So, in that case, we can easily adapt their clerking.”
(MP3, Medicine, Male, Phase-1)
B. Learning to Reason with Clinical Problems is Situated and Facilitated by Work Experience
Work experience provided the opportunity to learn from repeated exposure to clinical presentations and their variations, learn from seniors, and lapses of reasoning. However, work experience alone is not solely sufficient, and it is the collective influence of many other factors that help learn clinical reasoning. These factors are captured by the model developed from this study.
With work experience, junior doctors’ approach to reasoning changed from a ‘disease-oriented approach’ developed through undergraduate education to a ‘practice-oriented approach’. In the practice-oriented approach, junior doctors actively analyse clinical problems instead of matching them with memorised configurations of disease presentations.
They also developed ‘instincts’ for swift decision-making, sharpened through experience in recognising contextual factors in patient presentations. This was especially valuable for identifying acute cases requiring urgent care. In addition, they recognised the impact of the previous disease burden in formulating differential diagnoses, leading to a broader approach in their clinical reasoning.
Table 1 illustrates participant quotations that shed light on the role of work experience in learning clinical reasoning skills.
|
“…This approach in the ward is always problem-based. We’re dealing with problems. We try to solve the problems. That approach as a student was trying to fit the history into one of the long cases we have studied…Now we are not worried about that broad category. We will instead deal with the different problems that they have.” (MP2, Medicine, Male, Phase-1) |
|
“I think it’s just being with the patients. You realise that … it’s not just what’s written in the book…I mean now, if you’re just walking past a patient, you realise that this patient is not well. Whereas initially, you would have to go through the ward round and… go through the records, and then only you’ll see it. I don’t know how you get that but…” (MP2, Medicine, Male, Phase-1) |
|
“…Once a child with hypovolemic shock came to the ward. I was in the ward alone. I was very afraid at that time as I was in my first week of internship. So, nothing was on my mind, and I called my senior and he asked me to give (fluid) boluses until he came…. (There was another emergency at the same time). An Angioedema child came to the ward. I thought of (laughing)… running away from the ward. Because it was the initial period, it was very difficult, and our clinical knowledge was also poor. But now, we can manage any emergencies until the senior comes.” (PP, Paediatrics, Female, Phase-1) |
|
(When enquired on the reasons for commencing consultations with comorbidities?) “… Even the presenting complaint may be related to past medical conditions as well…and even this patient has diabetes… so, they can present in various ways… As an intern, I developed that. As an undergraduate, we are asking for name, age, where are you from, and then go on to take the history first…” (MP4, Medicine, Female, Phase-2) |
Table 1. Quotes illuminating that learning clinical reasoning is situated and facilitated by work experience
C. Internal Motivation and the Ability to Reflect and Employ Self-directed Learning are Powerful Tools for Developing Clinical Reasoning Skills
Learning clinical reasoning necessitated junior doctors to be internally driven for learning. Such internal motivation made them willing to learn from any source and be self-directed in their own learning. These individuals progressed rapidly in learning to reason with clinical problems compared to others who were not internally motivated.
Maintenance of internal motivation throughout the internship necessitated external encouragement even for the motivated particularly from the senior staff. There was a similar effect when the work environment fostered a culture of learning with the inclusion and recognition of junior doctors as a group of learners.
Table 2 presents participant quotations that highlight the significance of internal motivation in developing clinical reasoning skills.
|
“(reasoning with a complicated presentation) …With this kind of patient, it’ll refresh our memory. Going through how to take the history, how to use the basics, and how you investigate and manage…It is not like people coming with gastritis, or headache. Those are just simple things. (MP3, Medicine, Male, Phase-2) |
|
“I think you don’t need people who are good at what they do, I mean, you need people who are competent, but er…, you need a pleasant environment. Even if, there are, like 50 patients, if the people you work with are good, you can go through it. But then, if someone is really unpleasant, then that day is ruined.” (MP1, Medicine, Female, Phase-1) |
Table 2. Quotes illuminating internal motivation, reflective practice, and being self-directed as central to learning clinical reasoning skills
D. Caring and Compassionate Attitudes towards Patients Facilitate Developing Clinical Reasoning Skills
The individual caring and compassionate attitudes towards patients and the positive role modeling of senior doctors motivated junior doctors to learn clinical reasoning. Work experience nurtured these attitudes irrespective of gender, reflecting the potential to learn them during practice. However, a heavy workload and orientation towards efficiency in practice hindered the development of such attitudes among junior doctors.
“We’ve realised that although we’re members of a team, even individually, we can always do something for the patients. So, we always try to do something at our level. But we’re always willing to take the feeling from everyone above us to help.”
(MP1, Medicine, Female, Phase-1)
E. Collaborating within a Healthcare Team and Engaging in Ward Activities and Procedures Help Expedite the Development of Clinical Reasoning Skills
Junior doctors learn mostly from registrars, who are the immediate seniors and near-peers. In addition, peers and other healthcare staff contribute to their learning by timely sharing of information and working as a team. Patients’ unique characteristics which demand variation in reasoning also provide learning opportunities.
“I think the main influence is probably the registrars. Because we’re mostly in contact with them…So, in a way through working with them, I think I have learned quite a lot. Different ones will teach you different skills. Some are good at acute medicine and how to do that, and some are very willing to teach us how to do a pleural tap… So, from different people, we have learned different things.”
(MP2, Medicine, Male, Phase-1)
F. The Increasing Recognition of Professional Responsibility and Accountability towards Patient Care Drives Learning Clinical Reasoning
This was a strong theme commonly experienced by all junior doctors. During this transition, junior doctors recognised the patient care responsibilities vested in them and experienced a change of role from an undergraduate to a medical doctor. This led them to internalise their role and work towards meeting these expectations, whilst learning from all opportunities.
“We realise that somehow, we’ve got to do something. It wasn’t like that as students. (Now, as doctors) If we can’t take an ABG (Arterial Blood Gas) once, we will try ten times and somehow take the ABG. We realise- we have that ownership, “This is my patient. I will do something for her.” So, I think that’s a good thing. We didn’t have that as students.”
(MP1, Medicine, Female, Phase-1)
Parallel to the change of role, they were accepted as members of a community of doctors actively involved in providing patient care, which gave them a sense of inclusion and prestige and they worked hard towards meeting the expectations, which in turn helped them learn clinical reasoning.
G. Diversity of Personal, Interpersonal, and Contextual Factors Impede the Development of Clinical Reasoning Skills
Several negative influences on learning clinical reasoning exist.
The personal factors that can diminish learning clinical reasoning are related to a lack of internal motivation to learn and limited use of reflective practice.
In addition, external factors such as lack of encouragement and limited recognition of their contribution as doctors further demotivate junior doctors. Settings supervised by several senior clinicians provide better learning opportunities, but they also expose them to experience individual variations of reasoning due to staff working patterns and hinder their ability to appreciate the continuity of care.
Moreover, as junior doctors, they handle a heavy workload and work under time constraints, which gives them limited opportunity to reflect and learn from experience. Junior doctors also experience the presence of a power gap between juniors and seniors within the healthcare team and maintenance of this hierarchy is a barrier to learning during practice.
Table 3 presents participant quotes highlighting the diversity of contextual factors that hinder learning clinical reasoning skills.
|
“…usually hiccups occur with failures of… all types of failures… I do not have much knowledge about those things. Actually, I got to know that hiccups occur due to organ failure also, after this patient… (laughs)” (no intentions to learn more expressed) (SP2, Medicine, Male, Phase-2) |
|
“…here I think, in our unit, because the consultant changes daily, I think that is a negative point. The fact that you don’t have that connection with one person, and the fact that there is no continuity in care…” (MP1, Medicine, Female, Phase-1) |
|
“…I mean, there are too many admissions some days and you’re just trying to get through from one patient to the next one. So, you don’t really have that much time to analyse the problem as such. I mean, when the ward is less heavy, I’m trying to figure out what’s wrong but some days it’s a little bit… like going through.” (MP2, Medicine, Male) |
Table 3. Quotes illuminating contextual factors that impede the development of clinical reasoning skills
In addition, the discussions with junior doctors revealed that their main goal during the internship was to arrive at a diagnosis and/or manage patients’ clinical problems. No learning-related goals were readily verbalised.
(When enquired about the goals of reasoning during the internship)
“That…..err…is… coming to a final diagnosis and starting the treatment…Basically, we are supposed to recognise life-threatening conditions and treat them.”
(MP3, Medicine, Male, Phase-2)
Similarly, the informal discussions with senior clinicians revealed their limited expectations of the contribution of the internship towards facilitating the development of clinical reasoning skills among juniors. This could be due to the service orientation of the internship leaving ‘learning to happen’ concurrently without being actively encouraged. This is not conducive to learning clinical reasoning.
H. The Construction of the ‘practice-oriented clinical reasoning skills development framework’
Embedded within the seven themes were a multitude of factors that could be clearly categorised as ‘Facilitators’, ‘Drivers’, ‘Sources’, and ‘Challenges’ of developing clinical reasoning skills. These factors helped junior doctors to migrate from a disease-oriented to a practice-oriented approach to clinical reasoning (Figure 1).
The categorisation was informed by how these factors influenced the development of clinical reasoning skills. ‘Facilitators’ actively support learning, while ‘drivers’ exert strong internal pressure to motivate learning clinical reasoning. A ‘source’ is an individual or an activity, that helps learn clinical reasoning through interacting with them. ‘Challenges’ are either internal or external to an individual and negatively influence the development of clinical reasoning skills.
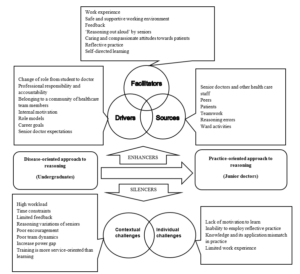
Figure 1. ‘Practice-oriented clinical reasoning skills development framework’ highlighting the factors that influence the development of clinical reasoning skills during the transition from medical graduates to junior doctors
IV. DISCUSSION
Aligned with existing literature (Brennan et al., 2010; Lempp et al., 2005; Prince et al., 2000; Teunissen & Westerman, 2011), this study identified a steep learning curve for junior doctors in developing clinical reasoning skills upon commencing the internship. A ‘disjunction’ (Koufidis et al., 2020) was evident between knowledge acquired during medical undergraduate education and the demands of effective reasoning in clinical practice (Cave et al., 2009; Monrouxe et al., 2017). The ‘practice-oriented clinical reasoning skills development framework’ derived from this study shed light on the factors serving as ‘enhancers’ and ‘silencers’ of learning clinical reasoning skills during this critical period. This classification helps consolidate existing knowledge specific to this period and offers insights for addressing disconnections and facilitating the development of clinical reasoning skills.
In this study, novice doctors initially faced clinical reasoning challenges due to limited contextual understanding and reliance on rule-based reasoning comparable to the Dreyfus model of adult skill acquisition (2004). With increased work experience, they were able to promptly recognise contextual features distinguishing acute from non-acute presentations requiring urgent care. Additionally, they acknowledged the significance of the patient’s past medical history in forming a broader approach to reasoning. Some even acquired instincts for prompt clinical decision-making, a form of non-analytic reasoning identified by clinical experts (Norman et al., 2007) and blending non-analytic reasoning with occasional rule-based confirmation (analytic reasoning). This dual-process approach (Croskerry, 2009; Eva, 2004; Pelaccia et al., 2011), incorporating both analytic and non-analytic reasoning is recognised to overcome challenges associated with each approach. Such development of clinical reasoning skills with work experience is reflective of the advancement of reasoning skills along the first four stages of the Dreyfus model, from novice to proficiency stages. This contrasts with the limited value placed on the internship for developing clinical reasoning skills among some clinical supervisors and needs addressing during staff development initiatives.
It was also noted that junior doctors revert to the novice stage using more analytical rule-based reasoning with uncommon presentations or at the start of a new rotation in another specialty (Groves, 2012). This highlights the complexity of developing clinical reasoning skills, varying with the nature of the presentation and the clinical specialty, requiring more support for its development. This aligns with the ‘context-specific nature’ of clinical reasoning (Eva et al., 1998), the variation of reasoning outcomes of an individual due to contextual factors unique to clinical situations. The study revealed a clear influence of clinical specialty on reasoning, confining the development of clinical reasoning to a few focused clinical problems common to a particular specialty. This limits the overall development of clinical reasoning and hinders the momentum of clinical reasoning development entering a new clinical specialty. Therefore, clinical teachers should promote a comprehensive approach, considering differential diagnoses beyond a single specialty. Given the need for promptly recognising contextual features of disease severity in acute care settings coupled with early internship challenges, delaying trainees’ placement in acute care settings until later in a clinical rotation is a reasonable approach, contrary to current clinical practice.
Work experience was central to developing clinical reasoning skills (Charlin et al., 2007; Schmidt & Rikers, 2007; Schmidt & Boshuizen, 1993), but benefiting from experience required junior doctors to be internally motivated. According to the self-determination theory, when an individual experiences a feeling of being able to do something successfully (competence), when their actions are controlled internally or self-determined (autonomy), and when there is a sense of safety, belonging, and supportive relationships (relatedness), it enhances the intrinsic motivation of an individual (Ryan & Deci, 2000) and this was clearly noted during this study. The ‘drivers’, ‘facilitators’, and ‘sources’ of learning clinical reasoning identified during this study enabled fulfilling these three basic psychological needs required to be motivated to learn clinical reasoning. Hence, the ‘practice-oriented clinical skills development framework’ could serve as a valuable reference for clinical teachers supporting junior doctors in developing clinical reasoning skills during their transition to the workplace.
Echoing the evidence in the field (Ajjawi & Higgs, 2008; Gruppetta & Mallia, 2020), junior doctors recognised the change in their role from student to medical doctor and subsequent absorption into the healthcare team which made them internalise their responsibility and accountability towards patient care. Their engagement in patient care gradually increased to finally becoming valued members of this community, collaborating with other like-minded colleagues to develop a more deliberate understanding of reasoning and methods of using it. This aligns with the principles of legitimate peripheral participation and community of practice of the Situated Learning Theory (O’Brien & Battista, 2020). The community of practice created a safe learning environment, motivating junior doctors to learn clinical reasoning actively. This emphasises the significance of early integration of junior doctors as valued members of the healthcare team. A team-oriented approach to patient care, acknowledging every team member’s contribution, proves more beneficial here than an individual-focused hierarchical approach.
The junior doctors of this study learned through their interactions with senior doctors, peers, and other healthcare staff, as well as by actively participating in ward activities, revealing learning as a dynamic social act. The opportunity to observe, listen to, and emulate senior colleagues as they engaged in clinical reasoning with authentic patient presentations, followed by the application of the newly acquired skills, significantly influenced the development of their clinical reasoning skills. This highlights the continued relevance of apprenticeship as a pedagogical tool today (Dornan, 2005), facilitating the ongoing development of clinical reasoning skills among junior doctors. It also provides a unique opportunity to witness firsthand the decision-making processes of junior doctors operating independently in clinical practice, aligning with the highest level of clinical skills assessment in Miller’s pyramid (Miller, 1990). This presents a potential opening for formative assessment of clinical reasoning, whether conducted formally or informally, as part of junior doctor training.
Junior doctors also constructed knowledge through interpersonal interactions in the workplace by engaging in an iterative process of learning, application, and consolidation of knowledge with each experience contributing to the refinement of their clinical reasoning skills. Learning from these experiences required them to reflect on these experiences and arrive at new understandings by integrating and building on previous knowledge. This is aligned with the principles of experiential learning theory (Morris, 2020; Yardley et al., 2012) and the constructivism learning theory (Olusegun, 2015). This highlights the importance of encouraging reflection by proactively including junior doctors in all pertinent patient-related discussions. Also, the value of implementing a reflective portfolio to acknowledge junior doctors’ learning needs at the outset of the internship, with formative assessments conducted midway and at its conclusion by clinical supervisors. This could also introduce a learning orientation to the already service-focused internship placement.
Junior doctors found collaborative learning, including referrals to other specialties and engaging in those discussions or working in partnerships with peers, beneficial for developing clinical reasoning (Laal & Laal, 2012; Tolsgaard et al., 2016). This highlights the value of involving junior doctors in collaborative work within or across disciplines. Simulation-based training (Khan et al., 2011) offers similar opportunities for collaborative learning within a safe environment, without compromising patient safety. Integrating simulation-based training for junior doctors immediately after graduation or before the internship can equip them with reasoning skills for authentic practice, addressing challenges during their transition to the workplace.
The caring and compassionate attitudes instilled in junior doctors by their seniors and further nurtured through close patient interactions, served as indirect motivators for learning clinical reasoning skills. This is an area not widely discussed in literature. While there is acknowledgment of the potential influence of clinicians’ emotions on clinical reasoning (Kozlowski et al., 2017), the specific impact of emotional closeness in patient care, and whether it aligns with the conventions of a more objective, rule-based healthcare delivery system, remains an area that merits more comprehensive investigation (Dreyfus, 2004). However, the study findings support that the more emotionally closer the junior doctors are to their patients, the more they are invested in learning clinical reasoning to ensure healthier outcomes for their patients. Clinical teachers could nurture such attitudes through role modeling as noted in this study.
The interrupted supervisory relationships due to work rotations of the senior staff challenged learning clinical reasoning. Such system-related factors deprived junior doctors of learning by emulating senior practice. It also hampered their ability to appreciate the continuity of patient care due to individual variations of reasoning among senior staff and prevented developing closer relationships with seniors, which could have been more emotionally satisfying (Ryan & Deci, 2000). This underlines the need to take necessary steps to prevent any adverse effects of staff working patterns on trainee doctors, while simultaneously ensuring extended periods of supervision within a consistent healthcare team.
The collective findings of this study not only confirm but also add valuable insights to the clinical reasoning pathway for teaching clinical reasoning skills (Linn et al., 2012). According to this framework, the teaching of clinical reasoning occurs in three stages through three consultations. Stage 1- Demonstration and deconstruction, Stage 2- Comprehension, and Stage 3- Performance. The transition in focus from the teacher’s approach to the student’s performance occurs in the last stage. In junior doctor training, this framework is ideally applied within a team context during daily clinical ward rounds focusing on selected patient presentations as afforded by the time constraints. The three stages of the framework can be combined, and the reasoning discussions can be brief and can take place within the ward round after the selected presentations with increasing junior doctors’ involvement as they gain experience. This could allow junior doctors to learn from verbalised reasoning from the team, reflect and actively contribute to the discussion, and feel valued as team members. They can apply newly acquired reasoning skills in subsequent patient consultations independently, in addition to the opportunity to demonstrate these during the ward rounds. Based on the study findings, additional considerations for analysing patient presentations could be proposed as enhancements to the clinical reasoning pathway (Linn et al., 2012). These aspects are detailed within the overall structure of this framework in Figure 2.
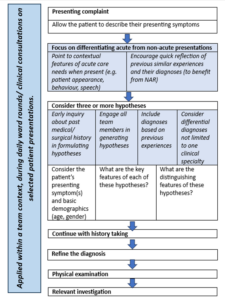
Figure 2. Proposed additions to the deconstructed consultation according to the clinical reasoning pathway (Linn et al., 2012) for teaching clinical reasoning to junior doctors as part of daily clinical ward rounds
Additions are presented in italics and highlighted. (NAR- non-analytic reasoning)
V. CONCLUSION
The ‘practice-oriented clinical skills development framework’ has brought together factors that act as ‘enhancers’ and ‘silencers’ of learning clinical reasoning specific to this period of transition from medical graduates to junior doctors. These findings offer practical insights that can prove invaluable for clinical educators in their teaching practices to facilitate the development of clinical reasoning skills.
This research also offers insights into the responsibilities of clinical teachers in supporting the development of clinical reasoning skills among junior doctors during their internship. It provides suggestions for teaching these skills in practice and highlights potential system-related changes needed to facilitate this process.
A. Limitations of the Study
The reader needs to determine the applicability of the findings to their context to overcome the limitations of qualitative research. To facilitate this process, the methodology and the data analysis are appropriately detailed.
The study focused on immediate medical graduates, and therefore, it did not delve into the clinical reasoning experiences of junior doctors at different levels of seniority and training, although this could have added to our understanding. This lack of comparative analysis is another limitation of this study.
Notes on Contributors
Dr WCD Karunaratne conceptualised the study, prepared the study proposal, conducted all interviews, analysed them and developed the manuscript for this submission.
Professor Madawa Chandratilake was a supervisor of this study and he contributed to the study design, guided initial interviews, and analysed selected transcripts to finalise the final coding framework for the study. He also reviewed and provided feedback on different versions of the manuscript.
Professor Kosala Marambe was also a supervisor of the study. She contributed to the study design and analysis of selected transcripts to finalise the final coding framework for the study and provided feedback on different versions of the manuscript.
Ethical Approval
Ethical clearance (P/11/01/16) was obtained from the Faculty of Medicine, University of Kelaniya, Sri Lanka.
Data Availability
Institutional ethical clearance was given to maintain the data in the secure storage of the principal investigator of the study. However, additional supportive quotations are deposited in the repository (Karunaratne et al., 2023) and are available from this URL – https://doi.org/10.6084/m9.figshare.23536548.v2.
Readers may contact the principal researcher for additional data and details if required.
Acknowledgement
We would like to acknowledge Dr Pavithra Godamunne (Faculty of Medicine, University of Kelaniya, Sri Lanka) who applied and secured funding for the project and Dr Paul Crampton (Hull York Medical School, UK) who reviewed the manuscript and provided constructive comments.
Funding
University of Kelaniya, Sri Lanka funded this research study (No. RP/03/04/17/01/16).
Declaration of Interest
The authors have no conflicts of interest to disclose.
References
Ajjawi, R., & Higgs, J. (2007). Using hermeneutic phenomenology to investigate how experienced practitioners learn to communicate clinical reasoning. The Qualitative Report, 12(4), 612–638. https://doi.org/10.46743/2160-3715/2007.1616
Ajjawi, R., & Higgs, J. (2008). Learning to reason: A journey of professional socialisation. Advances in Health Sciences Education, 13, 133–150. https://doi.org/10.1007/s10459-006-9032-4
Braun, V., & Clarke, V. (2012). Thematic Analysis. In APA Handbook of Research Methods in Psychology, 2, 57-71. https://doi.org/10.1037/13620-004
Brennan, N., Corrigan, O., Allard, J., Archer, J., Barnes, R., Bleakley, A., Collett, T., & De Bere, S. R. (2010). The transition from medical student to junior doctor: Today’s experiences of tomorrow’s doctors. Medical Education, 44(5), 449–458. https://doi.org/10.1111/j.1365-2923.2009.03604.x
Cameron, A., Millar, J., Szmidt, N., Hanlon, K., & Cleland, J. (2014). Can new doctors be prepared for practice? A review. Clinical Teacher, 11(3), 188–192. https://doi.org/10.1111/tct.12127
Cave, J., Woolf, K., Jones, A., & Dacre, J. (2009). Easing the transition from student to doctor: How can medical schools help prepare their graduates for starting work? Medical Teacher, 31(5), 403–408. https://doi.org/10.1080/01421590802348127
Charlin, B., Boshuizen, H. P. A., Custers, E. J., & Feltovich, P. J. (2007). Scripts and clinical reasoning. Medical Education, 41(12), 1178–1184. https://doi.org/10.1111/j.1365-2923.2007.02924.x
Charlin, B., Tardif, J., & Boshuizen, H. P. A. (2000). Scripts and medical diagnostic knowledge: Theory and applications for clinical reasoning instruction and research. Academic Medicine, 75(2), 182–190. https://doi.org/10.1097/00001888-200002000-00020
Cohen, L., Manion, L., & Morrison, K. (2017). Research methods in education (8th ed.). Routledge. https://doi.org/10.4324/9781315456539
Croskerry, P. (2009). A universal model of diagnostic reasoning. Academic Medicine, 84(8), 1022–1028. https://doi.org/10.1097/ACM.0b013e3181ace703
Crotty, M. (1998). Foundations of social research: Meaning and perspective in the research process (1st ed.). Routledge. https://doi.org/10.4324/9781003115700
Dornan, T. (2005). Osler, Flexner, apprenticeship and “the new medical education.” Journal of the Royal Society of Medicine, 98(3), 91–95. https://doi.org/10.1177/014107680509800302
Dreyfus, S. E. (2004). The five-stage model of adult skill acquisition. Bulletin of Science, Technology and Society, 24(3), 177–181. https://doi.org/10.1177/0270467604264992
Durning, S., Artino, A. R., Jr., Pangaro, L., van der Vleuten, C. P. M., & Schuwirth, L. (2011). Context and clinical reasoning: Understanding the perspective of the expert’s voice. Medical Education, 45(9), 927–938. https://doi.org/10.1111/j.1365-2923.2011.04053.x
Durning, S. J., & Artino, A. R. (2011). Situativity theory: A perspective on how participants and the environment can interact: AMEE guide no. 52. Medical Teacher, 33(3), 188-199. https://doi.org/10.3109/0142159x.2011.550965
Durning, S. J., Artino, A. R., Jr., Schuwirth, L., & van der Vleuten, C. (2013). Clarifying assumptions to enhance our understanding and assessment of clinical reasoning. Academic Medicine, 88(4), 442-448. https://doi.org/10.1097/acm.0b013e3182851b5b
Ericsson, K. A. (2004). Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine, 79(10 Suppl), S70–S81. https://doi.org/10.1097/00001888-200410001-00022
Eva, K., Neville, J., & Norman, G. (1998). Exploring the etiology of content specificity: Factors influencing analogic transfer and problem solving. Academic medicine, 73(10), S1-S5. https://doi.org/10.1097/00001888-199810000-00028
Eva, K. W. (2004). What every teacher needs to know about clinical reasoning. Medical Education, 39(1), 98–106. https://doi.org/10.1111/j.1365-2929.2004.01972.x
Goldacre, M. J., Davidson, J. M., & Lambert, T. W. (2003). Doctors’ views of their first year of medical work and postgraduate training in the UK: Questionnaire surveys. Medical Education, 37(9), 802–808. https://doi.org/10.1046/j.1365-2923.2003.01611.x
Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165(13), 1493–1499. https://doi.org/10.1001/archinte.165.13.1493
Groves, M. (2012). Understanding clinical reasoning: The next step in working out how it really works. Medical Education, 46(5), 444–446. https://doi.org/10.1111/j.1365-2923.2012.04244.x
Gruppetta, M., & Mallia, M. (2020). Clinical reasoning: Exploring its characteristics and enhancing its learning. British Journal of Hospital Medicine, 81(10), 1–9. https://doi.org/10.12968/hmed.2020.0227
Hattie, J., & Timperley, H. (2007). The power of feedback. Review of Educational Research, 77(1), 81–112. https://doi.org/10.3102/003465430298487
Health Services Safety Investigation Body. (2022). Investigation report: Clinical decision making- diagnosis and treatment of pulmonary embolism in emergency departments. Retrieved from https://www.hssib.org.uk/patient-safety-investigations/clinical-decision-making-diagnosis-of-pulmonary-embolism-in-emergency-departments/investigation-report/
Huckman, R. S., & Barro, J. R. (2005). NBER working paper series cohort turnover and productivity: The July phenomenon in teaching hospitals. Retrieved from http://www.nber.org/papers/ w11182
Jen, M. H., Bottle, A., Majeed, A., Bell, D., & Aylin, P. (2009). Early in-hospital mortality following trainee doctors’ first day at work. PLoS ONE, 4(9), Article e7103. https://doi.org/10.1371/jo urnal.pone.0007103
Kafle, N. P. (2011). Hermeneutic phenomenological research method simplified. Bodhi: An Interdisciplinary Journal, 5(1), 181–200. https://doi.org/10.3126/bodhi.v5i1.8053
Karunaratne, D., Chandratilake, M., & Marambe, K. (2023). Annexure-1 Additional supportive quotations (Version 2). [Data set]. Figshare. https://doi.org/10.6084/m9.figshare.23536548.v2
Khan, K., Pattison, T., & Sherwood, M. (2011). Simulation in medical education. Medical Teacher 33(1), 1-3. https://doi.org/10.3109/0142159X.2010.519412
Koufidis, C., Manninen, K., Nieminen, J., Wohlin, M., & Silén, C. (2020). Grounding judgement in context: A conceptual learning model of clinical reasoning. Medical Education, 54(11), 1019–1028. https://doi.org/10.1111/medu.14222
Kozlowski, D., Hutchinson, M., Hurley, J., Rowley, J., & Sutherland, J. (2017). The role of emotion in clinical decision making: An integrative literature review. BMC Medical Education, 17(1), Article 255. https://doi.org/10.1186/s12909-017-1089-7
Laal, M., & Laal, M. (2012). Collaborative learning: What is it? Procedia Social and Behavioral Sciences, 31, 491–495. https://doi.org/10.1016/j.sbspro.2011.12.092
Langridge, N., Roberts, L., & Pope, C. (2015). The clinical reasoning processes of extended scope physiotherapists assessing patients with low back pain. Manual Therapy, 20(6), 745-750. https://doi.org/10.1016/j.math.2015.01.005
Lave, J. (1991). Situating learning in communities of practice. In L. B. Resnick, J. M. Levine, & S. D. Teasley (Eds.), Perspectives on socially shared cognition (pp. 63–82). American Psychological Association. https://doi.org/10.1037/10096-003
Laverty, S. M. (2003). Hermeneutic phenomenology and phenomenology: A comparison of historical and methodological considerations. International Journal of Qualitative Methods, 2(3), 21–35. https://doi.org/10.1177/160940690300200303
Lee, C. Y., Jenq, C. C., Chandratilake, M., Chen, J., Chen, M. M., Nishigori, H., Wajid, G., Yang, P. H., Yusoff, M. S. B., & Monrouxe, L. (2021). A scoping review of clinical reasoning research with Asian healthcare professionals. Advances in Health Sciences Education, 26(5), 1555–1579. https://doi.org/10.1007/s10459-021-10060-z
Lempp, H., Seabrook, M., Cochrane, M., & Rees, J. (2005). The transition from medical student to doctor: Perceptions of final year students and preregistration house officers related to expected learning outcomes. International Journal of Clinical Practice, 59(3), 324–329. https://doi.org/10.1111/j.1742-1241.2005.00 438. x
Linn, A., Khaw, C., Kildea, H., & Tonkin, A. (2012). Clinical reasoning: A guide to improving teaching and practice. Australian Family Physician, 41(1), 18–20. https://search.informit.org/doi/10. 3316/informit.875577247352301
Malterud, K., Siersma, V. D., & Guassora, A. D. (2016). Sample size in qualitative interview studies: Guided by information power. Qualitative Health Research, 26(13), 1753-1760. https://doi.org/10.1177/1049732315617444
Mamede, S., Schmidt, H. G., & Penaforte, J. C. (2008). Effects of reflective practice on the accuracy of medical diagnoses. Medical Education, 42(5), 468–475. https://doi.org/10.1111/j.1365-2923. 2008.03030.x
Mamede, S., van Gog, T., Moura, A. S., de Faria, R. M. D., Peixoto, J. M., Rikers, R. M. J. P., & Schmidt, H. G. (2012). Reflection as a strategy to foster medical students’ acquisition of diagnostic competence. Medical Education, 46(5), 464–472. https://doi.org/10.1111/j.1365-2923.2012.04217.x
Miller, G. (1990). The assessment of clinical skills/competence/performance. Academic Medicine, 65(9), S63–S67. https://doi.org/10.1097/00001888-199009000-00045
Monrouxe, L. V., Grundy, L., Mann, M., John, Z., Panagoulas, E., Bullock, A., & Mattick, K. (2017). How prepared are UK medical graduates for practice? A rapid review of the literature 2009-2014. British Medical Journal Open, 7, Article e013656. https://doi.org/10.1136/bmjopen-2016-013656
Morris, T. H. (2020). Experiential learning – A systematic review and revision of Kolb’s model. Interactive Learning Environments, 28(8), 1064–1077. https://doi.org/10.1080/10494820.2019.15702 79
Muylaert, C. J., Sarubbi, V., Jr., Gallo, P. R., Neto, M. L. R., & Reis, A. O. A. (2014). Narrative interviews: An important resource in qualitative research. Revista Da Escola de Enfermagem Da USP, 48, 184–189. https://doi.org/10.1590/s0080-623420140000800027
Norman, G. (2005). Research in clinical reasoning: Past history and current trends. Medical Education, 39(4), 418–427. https://doi.org/10.1111/j.1365-2929.2005.02127.x
Norman, G., Young, M., & Brooks, L. (2007). Non-analytical models of clinical reasoning: The role of experience. Medical Education, 41(12), 1140–1145. https://doi.org/10.1111/j.1365-292 3.2007.02914.x
O’Brien, B. C., & Battista, A. (2020). Situated learning theory in health professions education research: A scoping review. Advances in Health Sciences Education, 25(2), 483–509. https://doi.org/10.1007/s10459-019-09900-w
Olusegun, S. (2015). Constructivism learning theory: A paradigm for teaching and learning. IOSR Journal of Research & Medical Edication, 5(6), 66–70.
Pelaccia, T., Tardif, J., Triby, E., & Charlin, B. (2011). An analysis of clinical reasoning through a recent and comprehensive approach: The dual-process theory. Medical Education Online, 16(1), Article 5890. https://doi.org/10.3402/meo.v16i0.5890
Prince, K. J. A. H., Van de Wiel, M. W. J., Scherpbier, A. J. J. A., Van der Vleuten, C. P. M., & Boshuizen, H. P. A. (2000). A qualitative analysis of the transition from theory to practice in undergraduate training in a PBL-medical school. Advances in Health Sciences Education, 5, 105–116. https://doi.org/10.1023/a:1009873003677
Prince, K. J. A. H., Van de Wiel, M. W. J., Van der Vleuten, C. P. M., Boshuizen, H. P. A., & Scherpbier, A. J. J. A. (2004). Junior doctors’ opinions about the transition from medical school to clinical practice: A change of environment. Education for Health, 17(3), 323–331. https://doi.org/10.1080/13576280400002510
Robertson, D. (2012). Critical thinking and clinical reasoning in new graduate Occupational therapists: A phenomenological study. [Doctoral Dissertation, Robert Gordan University]. OpenAIR@RGU. http://hdl.handle.net/10059/792
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68–78. https://doi.org/10.1037/0003-066X.55.1.68
Schmidt, H., & Rikers, R. (2007). How expertise develops in medicine: Knowledge encapsulation and illness script formation. Medical Education, 41(12), 1133–1139. https://doi.org/10.1111/j. 1365-2923.2007.02915.x
Schmidt, H. G., & Boshuizen, H. P. A. (1993). On acquiring expertise in medicine. Educational Psychology Review, 5(3), 205–221. https://doi.org/10.1007/BF01323044
Tallentire, V. R., Smith, S. E., Facey, A. D., & Rotstein, L. (2017). Exploring newly qualified doctors’ workplace stressors: An interview study from Australia. British Medical Journal Open, 7, e015890. https://doi.org/10.1136/bmjopen-2017-015890
Tallentire, V. R., Smith, S. E., Skinner, J., & Cameron, H. S. (2011). Understanding the behaviour of newly qualified doctors in acute care contexts. Medical Education, 45(10), 995–1005. https://doi.org/10.1111/j.1365-2923.2011.04024.x
Taylor, D. C. M., & Hamdy, H. (2013). Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Medical Teacher, 35(11), e1561–e1572. https://doi.org/10.3109/0142159X.2013.828153
Teunissen, P. W., & Westerman, M. (2011). Opportunity or threat: The ambiguity of the consequences of transitions in medical education. Medical Education, 45(1), 51–59. https://doi.org/10.1111/j.1365-2923.2010.03755.x
Tolsgaard, M. G., Kulasegaram, K. M., & Ringsted, C. V. (2016). Collaborative learning of clinical skills in health professions education: The why, how, when and for whom. Medical Education, 50(1), 69–78. https://doi.org/10.1111/medu.12814
Varpio, L., Ajjawi, R., Monrouxe, L. V., O’Brien, B. C., & Rees, C. E. (2017). Shedding the cobra effect: Problematising thematic emergence, triangulation, saturation and member checking. Medical Education, 51, 40–50. https://doi.org/10.1111/medu.13124
Woods, N. N. (2007). Science is fundamental: The role of biomedical knowledge in clinical reasoning. Medical Education, 41(12), 1173–1177. https://doi.org/10.1111/j.1365-2923.2007.029 11.x
Yardley, S., Teunissen, P. W., & Dornan, T. (2012). Experiential learning: AMEE Guide No. 63. Medical Teacher, 34(2), e102–e115. https://doi.org/10.3109/0142159X.2012.650741
*WCD Karunaratne
Centre for Medical Education,
University of Dundee
Scotland, DD2 4BF
+44 7594 504928
Email: dilminikarunaratne@gmail.com / Wkarunaratne001@dundee.ac.uk
Submitted: 8 July 2023
Accepted: 21 September 2023
Published online: 2 April, TAPS 2024, 9(2), 1-4
https://doi.org/10.29060/TAPS.2024-9-2/GP3089
Lamiaa Mohsen1, Marwa Shabrawy1, Waleed Hassan1, Zakia Arfeen2 & Mohammed Ahmed Rashid2
1School of Medicine, Newgiza University, Cairo, Egypt; 2UCL Medical School, Faculty of Medical Sciences, University College London, London, United Kingdom
Abstract
Introduction: In 2016, a new university opened in Egypt that sought to ‘challenge the ordinary’ in a country with a long and rich heritage of knowledge production. Newgiza University (NGU), located adjacent to the ancient pyramids of Giza outside Cairo, launched with a foundational focus on health sciences, through undergraduate courses in medicine, dentistry, and pharmacy. Each programme was co-developed through an academic collaboration with University College London (UCL), a high-ranking, research-intensive, UK university.
Methods: As the collaboration passes a key juncture of graduating the first cohorts of doctors, dentists, and pharmacists from these courses who embark on their professional careers, we examine and reflect on the journey to date. In particular, this article reviews the growing academic literature about international partnerships in medical education, describes how curricula, assessments, and management structures in the three NGU healthcare courses were adapted and finessed to fit the Egyptian context, and shares the lessons learnt by the academic leadership teams responsible for this challenging but stimulating collaboration project.
Results: The collaboration between NGU and UCL is an example of an international education partnership approach that seems to be growing in popularity globally. The overriding importance of building trust and respect between partners was clear in this collaboration, as was the need for clear communication channels to guide the necessarily complex decision-making that underpinned it.
Conclusion: Given inevitable power imbalances in such collaborations, critical examinations of their impacts on organisations, staff, and students are an important research priority in the future.
Practice Highlights
- International education partnerships are growing in popularity and there is a growing academic literature exploring different collaboration models.
- Co-development of healthcare professions education curricula across national borders requires attention to relational factors including trust and respect.
- Power differentials make it crucial to evaluate such partnerships using a critical lens.
I. INTRODUCTION
Egypt has a long and rich intellectual and cultural heritage dating back millennia. In the last century, Egyptian higher education sector has been shaped both by globalisation and a series of governmental policies (Reid, 2002). Against this backdrop, a new university was conceptualised that would ‘challenge the ordinary’ by creating a diverse community of staff and students to spearhead academic and scientific advancement in Egypt and beyond. Endorsed by Presidential Decree as a non-profit, private university in April 2010, Newgiza University (NGU) officially opened in 2016 with an initial focus on healthcare sciences, launching schools in Medicine, Dentistry, and Pharmacy.
As part of its mission to create an exciting learning environment that is filled with energy, talent, and cultural diversity to redefine the future of Egypt, NGU had a strategic objective to partner with a leading overseas university with a strong track-record in health professions education (HPE) to co-develop these new programmes. After briefly considering the literature on international education partnerships, this article will describe the experiences of an academic collaboration between NGU and University College London (UCL) to co-develop new undergraduate programmes in Medicine, Dentistry, and Pharmacy, that graduated their first cohorts in early 2023.
An emerging phenomenon in recent decades has been the delivery of curricula outside of the country in which they were developed. A variety of terms have been used to describe such arrangements, including ‘offshore education’, ‘transnational education’, and ‘crossborder curriculum partnerships’. The purpose of these partnerships is to provide comparable educational experiences in both institutions and can be attractive for students who are seeking a foreign qualification but do not wish to move overseas.
A literature review on international curriculum partnerships noted that almost all identified articles were about early-stage developments, reflecting that this is a growing and evolving topic (Waterval et al., 2015). It found that the most common reason for partnerships to deteriorate is mistrust and ‘disturbed relationships’, going on to conclude that there are no quick fixes to resolve cultural differences and that personal collaborations at all levels should be prioritised. As was noted in a subsequent systematic review, the academic literature is currently dominated by single case studies and there are many possible directions for future research (Kosmützky et al., 2016). Within HPE, Hodges et al. (2009) observed the growing trend of international education partnerships within a rapidly evolving globalisation discourse within the field more broadly. A later study that focussed on challenges and solutions in the context of international education partnerships in medicine suggested that there are both financial and academic advantages to both institutions (Waterval et al., 2016).
II. METHODS
From its inception, the stated vision of NGU has been to establish healthcare programmes that inspire and educate a new generation of clinicians by moving away from structures and practices of traditional universities in the region that limit effective learning. The NGU leadership team sought to reduce class sizes, focus on innovation and leadership, and move away from didactic and theoretical teaching, and towards a more patient-centred and practice-focused model of education. University College London (UCL) is based in the heart of London in the UK and is consistently ranked as one of the world’s best universities. It has schools of medicine, dentistry, and pharmacy, which each focuses on providing integrated and patient-focused education.
The underlying ethos of this collaboration has been of respectful co-development, with each team mindful of what they bring ‘to the table’ by way of expertise and experience. As such, a paradoxical success of this collaboration has been that it has shrunk and scaled back since the outset, as NGU academic, managerial, and administrative teams have taken on increasing levels of independent responsibility and their counterpart UCL teams have evolved to play roles of advisor and mentor accordingly. Although UCL curricula, assessments, and policies have been the basis for the corresponding NGU programmes in each of the three disciplines, these have gradually been adapted and contextualised to fit with the vision and operating environment of NGU.
The collaboration was structured around a three-phase approach. Phase one involved an exercise to clarify the vision and high-level structure for the three programmes and agree the legal and academic basis for the collaboration project. Phase two involved the detailed co-design and implementation of curricula and assessments across the three programmes to support their launch and delivery. Phase three, which is currently in progress, involves the ongoing operationalisation and continuous improvement of the programmes and the further development of the schools in other domains, including postgraduate education and research. These three phases are underpinned by a service contract between the two universities that takes the shape of work packages, which set the parameters and arrangements for each aspect of the collaboration.
III. RESULTS
Although geopolitical unrest was identified as a risk by both parties at the outset, this has not affected the project thus far. Instead, it has been a pandemic, COVID-19, that has proved to be the greatest disruption. Restrictions to air travel and international movement meant that for almost two years, the UCL-NGU collaboration shifted to an entirely virtual format.
This period of physical distance between the respective teams illuminated the importance of in-person visits. Seeing each other’s campuses and witnessing the contexts in which the two universities function was undoubtedly an important part of strengthening the relationship. That the project had been established for four years at the time of the onset of the pandemic meant that this was fortunately already well developed. As well as the important contextual understanding that these visits provided, it also allowed teams to socialise together and rich conversations over coffee breaks and meals often blurred the boundaries between professional and personal relationships. Indeed, close relationships between NGU and UCL counterparts was central to the success of the collaboration.
A particularly intellectually engaging aspect of this collaboration has been the adaptation of curricula content for a context that differs in social, political, cultural, epidemiological, and clinical domains. Whilst many scientific and technical aspects of HPE curricula seemingly transfer across countries readily, collaborators on both sides were surprised by the extent to which they required modification. For example, the many epidemiological and health system differences between the UK and Egypt meant there were important differences in disease patterns, drug availability, and technical equipment that need to be reflected in curricula to prepare students adequately for clinical practice. Likewise, significant areas of each curricula focus on topics linked to professional practice, including communication, healthcare ethics and law, and patient safety and clinical governance. These topic areas required significant adaptation to align with Egyptian legal and social practices, often prompting stimulating discussions and several iterative stages of development to contextualise individual teaching resources.
As well as drawing on UCL curricula structure and teaching resources to establish the new courses across the three healthcare schools, NGU also utilised UCL assessment policies and items to develop NGU assessments in each of the schools. There were, though, important adaptations. For example, the regulatory context in Egyptian higher education meant that a greater proportion of assessment weighting had to be given to ‘in semester’ assessment, necessitating a shift in emphasis from the UCL approach. Rather than using UCL assessment items directly in summative exams, the approach from the NGU schools was instead to use these to help their own faculty recognise the characteristics of high-quality items as they developed their own items. This was supplemented by many assessment writing workshops, which were often cross-disciplinary in the early phases of the collaboration as each faculty grew in size. Assessment tools used at UCL, including objective structured clinical examinations and workplace-based assessments, are not widely used in undergraduate education in Egypt and took time to embed.
One of the benefits of designing three undergraduate healthcare programmes together, launching simultaneously on a purpose-built modern campus, was the opportunity to maximise interprofessional education opportunities. This was realised through an ambitious introductory module for students from all three programmes. Not only did this provide an opportunity for students from all three NGU healthcare courses to learn together and from each other, it also embedded an inter-disciplinary approach across the three NGU schools, with faculty members from different schools often co-leading particular sessions or components of the module. On top of these benefits, it also enabled the three UCL schools to work much more closely and ensure alignment across all of their approaches. This interprofessional collaboration helped to foster closer working between schools at both NGU and UCL in other domains, which was an unexpected but pleasing consequence of this collaboration.
IV. DISCUSSION
A striking finding for teams from both universities was the central importance of human and relational factors to the collaboration. The formation of a new university creates distinct requirements in terms of leadership and culture, which can be challenging for any education leader or team. The additional layer of complexity of managing an international partner heightens this challenge, and meant the NGU leadership teams had to manage many more stakeholders than one might ordinarily have to contend with. This was especially so given the history and prestige associated with UCL, being from a high-income country with a reputation for academic excellence. The history of the UK as a former colonising country and Egypt as a former colonised country can also not be ignored. Together, these power imbalances and perceived knowledge hierarchies inevitably created a context that can easily slip to being unequal and exploitative.
By recognising the tensions faced by the NGU leadership and the potentially problematic power structures inherent to this collaboration, the teams in this collaboration acutely recognised the need for flexibility and understanding. The principle of respect and friendship was of overriding importance as it framed this collaboration not as one underpinned by ‘neutrality’, as such a thing does not exist, but rather through an outlook of deeply caring about the experiences and success of your partner team. Throughout the operational and academic aspects of the collaboration, this overriding focus on co-development and respect allowed both partners to ensure they were holding themselves and one another to account for the sake of the project mission.
Another crucial area of learning for both teams has been a sense of regret at the lack of formal scholarship and research that has been embedded in this collaboration. From the outset, the unwavering focus has been to help NGU achieve high-quality education programmes and to ensure that NGU students have an excellent student experience. This relentless focus on educational delivery, assessment, and quality management of the programmes left little time to focus on scholarship, despite a clear desire from both sides to do so. In particular, both teams recognise the many avenues of research that could have been explored through the collaboration thus far, including psychometric analyses comparing assessment performance between NGU and UCL cohorts all the way through to in-depth work using theories that help understand the complex relational factors through lenses of power and globalisation, and much between. Fortunately, this has become a priority as the collaboration moves to its next stage.
V. CONCLUSION
As the first student cohorts from its three healthcare courses graduate, NGU will enter a new stage of its development, and plans are underway to extend and deepen the collaboration with UCL across these schools. This article has summarised the dearth of academic literature on international partnerships in HPE and juxtaposed this with a complex and rich story that highlights the many different insights that can emerge from a single multi-professional collaboration. In our increasingly globalised world, the cross-cultural and relational issues raised through these partnerships have the potential to have wide-ranging and beneficial findings that extend beyond those communities working specifically on international partnerships. The importance of embedding scholarship into international HPE collaborations is clear to the academic teams on both sides of the UCL-NGU collaboration. As we plan for this in the next stages of our work together, we encourage others involved in international education partnerships to do the same and contribute to a scholarly area of growing importance in the field.
Notes on Contributors
LM led the collaboration on behalf of the NGU school of medicine, conceptualised the study, analysed the literature, and co-wrote the manuscript.
MS co-ordinated the collaboration on behalf of NGU, conceptualised the study, and developed the manuscript.
WH managed the collaboration on behalf of the NGU school of medicine, conceptualised the study, and developed the manuscript.
ZA co-ordinated the collaboration on behalf of UCL medical school, conceptualised the study, and developed the manuscript.
MAR led the collaboration on behalf of UCL medical school, reviewed the literature, conceptualised the study, and co-wrote the manuscript.
Funding
No funding was received.
Declaration of Interest
All authors were engaged in the academic collaboration described in this article.
References
Hodges, B. D., Maniate, J. M., Martimianakis, M. A., Alsuwaidan, M., & Segouin, C. (2009). Cracks and crevices: Globalization discourse and medical education. Medical teacher, 31(10), 910-917.
Kosmützky, A., & Putty, R. (2016). Transcending borders and traversing boundaries: A systematic review of the literature on transnational, offshore, cross-border, and borderless higher education. Journal of Studies in International Education, 20(1), 8-33.
Reid, D. M. (2002). Cairo University and the making of modern Egypt (Vol. 23). Cambridge University Press.
Waterval, D. G., Frambach, J. M., Driessen, E. W., & Scherpbier, A. J. (2015). Copy but not paste: A literature review of crossborder curriculum partnerships. Journal of Studies in International Education, 19(1), 65-85.
Waterval, D. G., Frambach, J. M., Oudkerk Pool, A., Driessen, E. W., & Scherpbier, A. J. (2016). An exploration of crossborder medical curriculum partnerships: Balancing curriculum equiva- lence and local adaptation. Medical teacher, 38(3), 255-262.
*Mohammed Ahmed Rashid
University College London,
Gower Street, London,
WC1E 6AE, United Kingdom
Email: ahmed.rashid@ucl.ac.uk
Submitted: 27 April 2023
Accepted: 17 August 2023
Published online: 2 January, TAPS 2024, 9(1), 36-41
https://doi.org/10.29060/TAPS.2024-9-1/OA3051
Mae Yue Tan1,2, Zong Jie Koh1,3, Shoban Krishna Kumar4, Rui Min Foo5, Rou An Tan6, Nisha Suyien Chandran7,8 Jeremy Bingyuan Lin1,2, Malcolm Mahadevan9 & Eng Loon Tng5
1Department of Paediatrics, Khoo Teck Puat – National University Children’s Medical Institute, National University Health System, Singapore; 2Department of Paediatrics & 8Department of Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 3Department of General Surgery, University Surgical Cluster, National University Health System, Singapore; 4Division of Advanced Internal Medicine, Department of Medicine, National University Hospital, National University Health System, Singapore; 5Department of Medicine & 6Department of Intensive Care Medicine, Ng Teng Fong General Hospital, National University Health System, Singapore; 7Division of Dermatology, Department of Medicine, National University Hospital, National University Health System, Singapore; 9Emergency Medicine Department, National University Hospital, National University Health System, Singapore
Abstract
Introduction: The night float (NF) system has been instituted in some hospitals in Singapore to improve the working hours and wellbeing of junior doctors. There have been concerns of compromised learning and patient safety with NF. The objective of this study is to compare clinical competency outcomes, based on existing assessment framework, between post-graduate year 1 (PGY1) doctors working on NF versus traditional call (TC) systems. The secondary aim was to explore patient safety outcomes between these groups of PGY1s.
Methods: Data on the formal assessments of PGY1s using the Entrustable Professional Activities (EPAs) and medical errors were prospectively collected between May 2021 and April 2022 from two hospitals that employed different on-call systems. Data was analysed descriptively. Categorical data was analysed using the Chi-square test or Fisher’s exact test where appropriate.
Results: One hundred and ninety-three PGY1s consented to the study. There was no statistically significant difference in the clinical competency of PGY1s in both groups. The number of PGY1s who had ‘needs improvement’ scores in a detailed EPA was not significantly different (9.0% in the NF group versus vs 3.7% in the TC group (p = 0.14)). They nonetheless passed the overall core EPA and no PGY1 failed their postings. No serious reportable medical errors occurred in either group.
Conclusion: PGY1s who worked on NF are equally competent compared to those who worked on TC based on the EPA assessment matrix. Patient safety is not compromised by PGY1s working on NF.
Keywords: Clinical competence, Float, Junior doctor, Patient safety, Wellbeing
Practice Highlights
- Night float did not affect competency of post-graduate Year 1 doctors on current assessments.
- Night float did not lead to compromised patient safety.
- We provide objective data in consideration of restructuring working hours for junior doctors.
I. INTRODUCTION
Post graduate year 1 (PGY1) doctors are fresh graduates who are in their transitional year where they learn clinical decision-making skills and how to perform simple medical procedures independently. In Singapore, following the Medical Registration Act, PGY1s are required to complete 4 months of Internal Medicine and 4 months of General Surgery or Orthopaedic Surgery, with another 4-month posting of their choice in their 12 months as a PGY1 (Ministry of Health Holdings Pte Ltd, 2018). As part of the national PGY1 training framework (Ministry of Health, 2019), each hospital is required to provide training (teaching activities) to allow PGY1s to achieve their learning and competency outcomes. PGY1s are assessed via a standardized matrix which is used across all hospital rotations and institutions. They are expected to achieve competency in situations where senior supervision is less readily available, for example, while working on-call. PGY1 duties are similar regardless of discipline as they focus on core medical competencies common to general medical practice.
In Singapore, some hospitals have instituted the night float (NF) system as a service model where a dedicated team of doctors, including PGY1s, take over the care of patients for consecutive nights in a week. A different team of doctors will resume care of patients the following day. This facilitates timely handovers of patient management, eliminates the need for prolonged post-night call working hours and provides junior doctors with adequate rest, avoiding sleep deprivation. Conversely, in the traditional call (TC) system, junior doctors commence night duties immediately after their daytime routines. Frequently, at the end of their night calls, PGY1s continue with daytime work till mid-day or later, resulting in shifts of up to 36 hours.
The Accreditation Council for Graduate Medical Education (ACGME) guidelines recommended a maximum of 80 hours of duties per week based on extant literature on the impact of prolonged duty hours on burnout and fatigue (Singapore Medical Council, 2017), medical errors and adverse events (Barger et al., 2006; Landrigan et al., 2004; Trockel et al., 2020). Departments that have instituted the NF system have significantly improved their compliance to duty hour recommendations. However, concerns were raised regarding reduced training opportunities, specifically during the after-office hour period due to the reduced working hours with NF as well as potential compromises in patient safety arising from communication lapses associated with frequent handovers (Desai et al., 2013; Sun et al., 2016). These concerns have prevented widespread adoption of NF in Singapore hospital systems.
Two studies in Singapore have shown that residents who worked on NF felt that it did not affect their learning outcomes or compromise patient safety (Loo et al., 2020; Tan et al., 2019). However, these studies assessed the perceptions of junior doctors and provided no objective data for comparison of NF against TC. We thus aimed to compare clinical competency outcomes between PGY1s who worked on NF and those who worked on TC, across similar specialties. The secondary aim was to explore any differences in patient safety and medical errors between these two groups. We chose the PGY1 group for this study for the following reasons. Firstly, PGY1 training outcomes and assessments are standardized nationwide thus allowing for direct comparisons across institutions. Additionally, any policy implementation or change would impact all PGY1s across the board equally. In contrast, physicians in their later years of training (PGY2 and above) are a heterogenous group with their training assessment frameworks dependent on the relevant speciality programmes. Secondly, PGY1s are considered to have the one of the highest risks of burnout among physicians and are likely to benefit most from well-being initiatives. Lastly, the PGY1 year is a compulsory year of formative training with PGY1s subsequently graduating as fully licensed physicians. This decisive and important transitional year from medical training to clinical practice underscores the importance of considerations for their training and competency.
II. METHODS
This study was conducted over three rotations (each PGY1 rotation spans 4 months) from May 2021 to April 2022. PGY1s working in National University Health System cluster (either in National University Hospital where NF is the structure for PGY1s rotating through General Surgery, Internal Medicine, and Orthopaedics (since January 2022), or Ng Teng Fong General Hospital where TC is practiced) were invited to participate via emails. PGY1s could opt out of the study. Ethics approval was obtained [National Healthcare Group Domain Specific Review Board (NHG DSRB), Singapore; Reference No.: 2021/00536].
Prospective data was collected from formal educational and workplace-based assessments. Currently, the Entrustable Professional Activities (EPAs) framework, which describes professional activities that a trainee can be entrusted to perform at varying levels of supervision, is used for this purpose. EPAs are established milestones in post graduate medical education to gauge whether trainees have achieved necessary skill sets that are appropriate for their level of training. In its current form, the local EPA framework for PGY1s includes 7 ‘core EPA’ groups. Each ‘core EPA’ group further encompasses a list of ‘detailed EPAs’. An example of a ‘core EPA’ and its ‘detailed EPAs’ is shown in Table 1. At the end of a rotation during their final evaluation, PGY1s are evaluated by their supervisors for each ‘detailed EPA’ as part of their ‘Learning Needs’. A grading of ‘needs improvement’ for a detailed EPA indicates that the PGY1 has not demonstrated sufficient competence in that specific activity. No input is required if a PGY1 is deemed to have met expectations for the detailed EPA. In performing this evaluation, the supervisor is expected to canvass feedback from other team and faculty members who have worked with the PGY1. At the end of the rotation, should all EPAs (core and detailed) be assessed as competent, the supervisor would grade the posting outcome as a pass, with the opportunity to nominate the PGY1 for the national outstanding PGY1 award.
|
Core Entrustable Professional Activity (EPA) |
Detailed EPAs |
|
Manage patients by obtaining a detailed history, performing appropriate physical examination, requesting & follow-through relevant diagnostic evaluation & therapeutic interventions. |
|
Table 1. Example of an Entrustable Professional Activity (EPA), with detailed EPAs within the core EPA
Data on medical errors or patient safety issues involving PGY1s, including near-miss events, were also collected from the medical error reporting systems of both hospitals. All data were anonymized prior to data analysis. Data was analysed descriptively and with comparative statistics. Chi-square test or Fisher’s exact test were used for analysis of categorical data where appropriate.
III. RESULTS
A total of 193 PGY1s consented to this study with no opt-outs. There was no statistically significant difference in the proportion of PGY1s with ‘needs improvement’ between the 2 groups: 9.0% of PGY1s in the NF group compared to 3.7% in the TC group had ‘needs improvement’ in any of the ‘detailed EPAs’ (p = 0.16) (Table 2). All PGY1s with ‘needs improvement’ were deemed competent in the ‘core EPA’. Notably, three PGY1s in the NF group who had ‘needs improvement’ in the ‘detailed EPAs’ were nominated for the Outstanding PGY1 Award by the Ministry of Health. All PGY1s in this study passed their postings satisfactorily.
|
|
Night Float (NF) |
Traditional On-Call (TC) |
P-value |
|
Total number of PGY1s who had ‘needs improvement’ for a detailed EPA / total number of PGY1s (%) |
10 / 111 (9.0) |
3 / 82 (3.7) |
0.16 |
|
1st rotation (%) |
3 / 36 (8.3) |
2 / 29 (6.9) |
0.99 |
|
2nd rotation (%) |
2a / 32 (6.3) |
0 / 22 (0.0) |
0.51 |
|
3rd rotation (%) |
5b /43 (11.6) |
1 / 31 (3.2) |
0.39 |
Table 2. Proportion of post graduate year 1 (PGY1) doctors who had detailed EPAs that were marked as ‘needs improvement’
aBoth these PGY1s were nominated for the outstanding PGY1 award.
bOne PGY1 was nominated for the outstanding PGY1 award.
In terms of medical errors, there were 25 reported events in the NF group and 12 in the TC group. To account for the difference in number of PGY1s between both groups, we reported the average event rate per PGY1, i.e. event rate over the number of PGY1s in the rotation. There was no statistically significant difference in the average event rate per PGY1 between the two groups (0.23 vs 0.15, p = 0.20) (Table 3). There was also no statistically significant difference between the two groups when comparison was made for each rotation. All reported errors regardless of NF or TC, were in the ‘No Harm’, or ‘Minor Harm’ categories with no serious reportable events: 24.3% of all errors were needle stick-related events while 24.3% were for wrongly labelled blood tubes.
|
|
Night Float (NF) |
Traditional On-Call (TC) |
P-value |
|
Average event rate per PGY1 |
0.23 |
0.15 |
0.20 |
|
1st rotation |
0.11 |
0.14 |
0.99 |
|
2nd rotation |
0.25 |
0.14 |
0.49 |
|
3rd rotation |
0.30 |
0.16 |
0.18 |
Table 3. Event rates for reported events (either medical errors or patient safety issues) in post graduate year 1 (PGY1) doctors over the study period.
IV. DISCUSSION
Our study revealed insights on the effects of the NF system on the clinical training of PGY1s and impact on patient safety. There was no statistically significant difference in objective clinical competency between PGY1s working on NF or TC. This refutes the concern of inadequate training opportunities arising from shorter working hours during after-office-hours shifts. These objective findings are in line with the subjective evaluation and perceptions of junior doctors on the impact of the local night float system on their training (Loo et al., 2020; Tan et al., 2019).
Though the time spent for emergency-related work or ‘on-call’ situations where senior supervision is less readily is reduced on the NF compared to the TC groups, the training outcomes were similar and not compromised. We postulate that this is because of the robust formal training programme during the daytime which is consistent across hospitals given the national framework guidelines. In addition, the high number of emergency cases being admitted after office hours in both the NF and TC groups provide ample learning opportunities for the PGY1s. Regardless of which service model the PGY1s practice in, formal training during daytime work is consistent across hospitals given the national framework guidelines. PGY1s have protected teaching time each week and they are able to catch up with the teaching topics through e-learning modules when they are post call. As such, the NF system does not negatively affect their learning through the formal teaching program. While hours spent on training activities are important, it is just one component that contributes to learning outcomes. Previous literature has shown that shorter training hours can also optimize learning as it allows between-session and post-training learning to occur (Molloy et al., 2012).
Though not statistically significant, the NF group did have a higher number of PGY1s who were flagged for ‘needs improvement’ in their ‘detailed EPA’ as compared to the TC group (9.0% vs 3.7%, p = 0.16). We believe this was a result of the limitations with the EPA assessment matrix rather than poor clinical training in the PGY1s in the NF group. The standardized assessment matrix in the overall evaluation form provides only two options in the grading of each ‘detailed EPA’; PGY1s who are deemed to have failed the task should be graded as ‘needs improvement’ whilst the section is left blank by the supervisors for PGY1s who are deemed to be competent in the task. Thus, the grade of ‘needs improvement’ is in reality that of failure, but is commonly misconstrued as having room for improvement in an already competent PGY1. Hence, supervisors may mistakenly grade the ‘detailed EPA’ domains as ‘needs improvement’ without any intent that the PGY1 is in any way incompetent. Supervisors may even grade the PGY1s as ‘needs improvement’ in an effort to spur them to greater heights, and we suspect this to be the case as seen in the 3 PGY1s who were nominated for the Outstanding Award on their overall assessment despite having a “needs improvement” grade for a detailed EPA. Additionally, as with any assessment matrix, the utility and accuracy of EPAs in reflecting competency is heavily dependent on how well it is used by the supervisor and PGY1, and its refinement and standardization continue to be work in progress.
Our study showed that the NF system does not affect patient safety adversely. There were no major clinical errors or adverse patient events in both groups. There were also no statistically significant differences in the minor clinical errors, categorized as ‘No Harm’ and ‘Minor Harm’, that were made by PGY1s between the two groups (0.23 vs 0.15, p = 0.20). Given the anonymity of data on the medical error reporting systems, we were unable to discern whether errors were made while on call or if certain PGY1s were making repeated errors. As these numbers are small, comparative analysis is not meaningful and thus not performed. There were no medical errors arising from miscommunications because of increased handovers in our study. We believe that PGY1s were able to provide better quality handovers in a timelier fashion due to the structured work-hour cycles in NF. NF reduces PGY1 fatigue and the associations between fatigue and its impact on judgement, competency and risk of mistakes has been demonstrated (Trockel et al., 2020).
V. CONCLUSION
In conclusion, our study supports existing evidence that the NF system does not compromise clinical training for PGY1s or patient safety. The NF system emphasizes the importance of training quality over quantity and enhances PGY1 wellbeing. We believe our study provides objective data for the medical fraternity for consideration in the restructuring of working hours for junior doctors (Abu Baker, 2022).
Notes on Contributors
MYT contributed to design and conception of the work, data analysis and interpretation, drafted the article and revised it critically for important intellectual content. ZJK contributed to design and conception of the work, data analysis and interpretation, drafted the article and revised it critically for important intellectual content. SKK contributed to design and conception of the work, data analysis and interpretation, drafted the article and revised it critically for important intellectual content. RMF contributed to data acquisition and revised the article critically for important intellectual content. RAT contributed to data acquisition and revised the article critically for important intellectual content. NSC contributed to study conception, data interpretation and revised the article critically for important intellectual content. JBL contributed to design and conception of the work and revised the article critically for important intellectual content. MM contributed to conception of work, data interpretation and revised the article critically for important intellectual content. ELT contributed design and conception of the work, data acquisition and revised the article critically for important intellectual content. All authors read and approved the final version, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethical Approval
This study was performed in line with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Ethics approval for the study was obtained from the National Healthcare Group Domain Specific Review Board (NHG DSRB), Singapore; Reference No.: 2021/00536.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgement
The authors would like to thank the Ministry of Health, Singapore, for supporting the implementation of the night float call system for junior doctors in our institution. We would also like to thank our PGY1s for consenting to this study, and our program coordinators for providing administrative assistance for this project. Lastly, we would like to thank Ms Sheena Nishanti Ramasamy for her assistance in editing and formatting the manuscript for submission.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of Interest
The authors declare no relevant financial or non-financial competing interests with respect to the research, authorship and/or publication of this article.
References
Abu Baker, J. (2022, March 9). Review of junior doctors’ work hours among steps to improve healthcare workers’ well-being. Channel News Asia. https://www.channelnewsasia.com/singapore /review-junior-doctors-work-hours-among-steps-improve-healthcare-workers-well-being-2551376
Barger, L. K., Ayas, N. T., Cade, B. E., Cronin, J. W., Rosner, B., Speizer, F. E., & Czeisler, C. A. (2006). Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Medicine, 3(12), Article e487. https://doi.org/10.1371/journal.pmed.0030487
Desai, S. V., Feldman, L., Brown, L., Dezube, R., Yeh, H. C., Punjabi, N., Afshar, K., Grunwald, M. R., Harrington, C., Naik, R., & Cofrancesco, J., Jr (2013). Effect of the 2011 vs 2003 duty hour regulation-compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: A randomized trial. JAMA Internal Medicine, 173(8), 649–655. https://doi.org/10.1001/jamainternmed.2013.2973
Landrigan, C. P., Rothschild, J. M., Cronin, J. W., Kaushal, R., Burdick, E., Katz, J. T., Lilly, C. M., Stone, P. H., Lockley, S. W., Bates, D. W., & Czeisler, C. A. (2004). Effect of reducing interns’ work hours on serious medical errors in intensive care units. The New England Journal of Medicine, 351(18), 1838–1848. https://doi.org/10.1056/NEJMoa041406
Loo, B. K. G., Ng, C. L., Chin, R. T., Davies, L. J., Yong, J., Ang, A. E. L., Chong, Y. W., & Tambyah, P. A. (2020). Nationwide survey comparing residents’ perceptions of overnight duty systems in Singapore: Night float versus full overnight call. Singapore Medical Journal, 61(10), 559–562. https://doi.org/10.11622/sme dj.2020149
Ministry of Health Holdings Pte Ltd. (2018). Medical service career path. https://www.physician.mohh.com.sg/medicine/medi cal-service-career-path
Ministry of Health Singapore. (2019, January 16). The national PGY1 training and assessment framework. https://www.moh.gov.sg/hpp/all-healthcareprofessionals/news/NewsArticleDetails/nationalpgy1_training_assessment_framework
Molloy, K., Moore, D. R., Sohoglu, E., & Amitay, S. (2012). Less is more: Latent learning is maximized by shorter training sessions in auditory perceptual learning. PloS One, 7(5), Article e36929. https://doi.org/10.1371/journal.pone.0036929
Singapore Medical Council. (2017). SMC circular – Guidelines on Postgraduate Year 1 (PGY1) training and postings for the accreditation of PGY1 training posts.
Sun, N. Z., Gan, R., Snell, L., & Dolmans, D. (2016). Use of a night float system to comply with resident duty hours restrictions: Perceptions of workplace changes and their effects on professionalism. Academic Medicine: Journal of the Association of American Medical Colleges, 91(3), 401–408. https://doi.org/10.1097/ACM.0000000000000949
Tan, B. Y., Ngiam, N. J., Chang, Z. Y., Tan, S. M. Y., Shen, X., Mok, S. F., Subramanian, S., Ooi, S. B. S., & Kee, A. C. (2019). Perceptions of a night float system for intern doctors in an internal medicine program: An Asian perspective. Korean Journal of Medical Education, 31(3), 271–276. https://doi.org/10.3946/kjme.2019.137
Trockel, M. T., Menon, N. K., Rowe, S. G., Stewart, M. T., Smith, R., Lu, M., Kim, P. K., Quinn, M. A., Lawrence, E., Marchalik, D., Farley, H., Normand, P., Felder, M., Dudley, J. C., & Shanafelt, T. D. (2020). Assessment of physician sleep and wellness, burnout, and clinically significant medical errors. JAMA Network Open, 3(12), Article e2028111. https://doi.org/10.1001/jamanet work open.2020.28111
*Dr Mae Yue TAN
Department of Paediatrics,
Khoo Teck Puat-National University
Children’s Medical Institute,
National University Health System, Singapore
Department of Paediatrics,
Yong Loo Lin School of Medicine,
National University of Singapore, Singapore
NUHS Tower Block Level 12,
1E Kent Ridge Rd, Singapore 119228
Email: mae_yue_tan@nuhs.edu.sg
Submitted: 28 January 2023
Accepted: 17 August 2023
Published online: 2 January, TAPS 2024, 9(1), 3-19
https://doi.org/10.29060/TAPS.2024-9-1/OA2947
Thun How Ong1, Hwee Kuan Ong2, Adrian Chan1, Dujeepa D. Samarasekera3 & Cees Van der Vleuten4
1Department of Respiratory and Critical Care Medicine, Singapore General Hospital, Duke-NUS Medical School, Singapore; 2Department of Physiotherapy, Singapore General Hospital; 3Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 4Department of Educational Development and Research, Maastricht University, Maastricht, The Netherlands
Abstract
Introduction: The mini-Clinical Evaluation Exercise (CEX) is meant to provide on the spot feedback to trainees. We hypothesised that an ultra-short assessment tool with just one global entrustment scale (micro-CEX) would encourage faculty to provide better feedback compared to the traditional multiple domain mini-CEX.
Methods: 59 pairs of faculty and trainees from internal medicine completed both the 7-item mini-CEX and a micro-CEX and were surveyed regarding their perceptions of the 2 forms. Wordcount and specificity of the feedback was assessed. Participants were subsequently interviewed to elicit their views on factors affecting the utility of the CEX.
Results: Quantity and quality of feedback increased with the micro-CEX compared to the mini-CEX. Wordcount increased from 9.5 to 17.5 words, and specificity increased from 1.6 to 2.3 on a 4-point scale, p < 0.05 in both cases. Faculty and residents both felt the micro-CEX provided better assessment and feedback. The micro-CEX, but not the mini-CEX, was able to discriminate between residents in different years of training. The mini-CEX showed a strong halo effect between different domains of scoring. In interviews, ease of administration, immediacy of assessment, clarity of purpose, structuring of desired feedback, assessor-trainee pairing and alignment with trainee learning goals were identified as important features to optimize utility of the (mini or micro or both) CEX.
Conclusions: Simplifying the assessment component of the CEX frees faculty to concentrate on feedback and this improves both quantity and quality of feedback. How the form is administered on the ground impacts its practical utility.
Keywords: Workplace Based Assessment, Mini-CEX, Micro-CEX, Feedback, Assessment
Practice Highlights
- Simplifying the assessment component of the CEX frees faculty to concentrate on feedback.
- A simpler form can result in better and more feedback.
- Making it easy for faculty to use the form is important and increases its utility in providing feedback and assessment.
I. INTRODUCTION
The Mini-CEX is one of the most widely used work-placed based assessment (WBA) tools and is supported by a large body of theoretical and empirical evidence which have shown that when used in the context of repeated sampling, it is both a valid assessment tool and is also an effective education tool in giving feedback to the trainee (Hawkins et al., 2010; Norcini et al., 2003). However, in practice, the educational value of the mini-CEX, as measured chiefly by trainee and faculty perceptions and satisfaction, varied significantly (Lorwald et al., 2018). Factors affecting the educational value have been described by Lorwald et al. and categorised into context of usage, and user, implementation and outcome factors (Lorwald et al., 2018).
Context refers to the situation in which the mini-CEX is executed, and factors which impact its actual usage, such as time needed for conducting the Mini-CEX, or the usability of the tool. Time constraint on the part of both the residents and the assessors is an especially frequent issue across multiple studies (Bindal et al., 2011; Brazil et al., 2012; Castanelli et al., 2016; Lörwald et al., 2018; Morris et al., 2006; Nair et al., 2008; Yanting et al., 2016). The mini-CEX was conceived as a 30-minute exercise of directly observed assessment, and there are 6 or 7 domains which faculty are expected to assess (Norcini et al., 2003). In a busy clinical environment however, what actually occurs is often a brief clinical encounter of 10-15 minutes or even less where only a few of the mini-CEX’s domains were assessed (Berendonk et al., 2018).
User factors refers to trainee and faculty knowledge of the mini-CEX and their perceptions of its use. Studies have found that the mini-CEX is frequently regarded as a check box exercise (Bindal et al., 2011; Sabey & Harris, 2011). Assessor’s and trainee’s training and attitudes, or unfamiliarity with the WBA tools also negatively impact the educational value of the mini-CEX (Lörwald et al., 2018). Reports have shown that educating faculty on the formative intent of mini-CEX can improve feedback provided (Liao et al., 2013).
Implementation factors refer to how the mini-CEX is actually executed on the ground. Some studies have reported that the mini-CEX often occurs without actual direct observation (Lörwald et al., 2018) or feedback provided (Weston & Smith, 2014). Implementation in turn affected outcome, which refers to the trainees appraisal of the feedback received (Lörwald et al., 2018).
One way of improving the educational value of the mini-CEX then might be to improve the context of its usage, by redesigning the mini-CEX to better fit the realities of the clinical workplace. In different clinical encounters, specific domains of performance are more easily and obviously observed and assessed than others (Crossley & Jolly, 2012). Reducing the number of dimensions the assessors are asked to rate was shown to decrease measured cognitive load and improved interobserver reliability (Tavares et al., 2016). It has also been shown that using rating scales that align with the clinician’s cognitive schema perform better, for instance, scales that ask the clinician assessors about the trainees ability to practice safely with decreasing levels of supervision (i.e. entrustability) showed better discrimination and higher reliability (Weller et al., 2014). Compared to multidimension rating scales, global rating scales have greater reliability and validity in assessing candidates in OSCE examinations (Regehr et al., 1998), assessing technical competence in procedures (Walzak et al., 2015) and in simulation-based training (Ilgen et al., 2015).
We proposed therefore to replace the multiple domains with a single rating asking faculty what level of supervision the resident would require in performing a similar task, i.e. a global entrustment scale. The shorter assessment task should refocus the faculty on the feedback component, whilst still retaining the ability to identify trainee progression. One such form has been proposed by Kogan and Holmboe (2018), and we designated this the micro-CEX.
We hypothesised that these changes would improve the usability (“context” as described by Lorwald et al.) and hence improve the educational value of the assessment, measured in this study by the specificity and quality of the feedback given by faculty.
Our study aims to show therefore that the shorter micro-CEX can provide better feedback than the usual mini-CEX. We also sought to find out, from the perspective of the end-users, what other adjustments to the implementation and design of the mini or micro-CEX can be made to improve its acceptability, educational value and validity.
The study focussed on the following questions:
Does the micro-CEX stimulate faculty to provide more specific and actionable feedback compared to the mini-CEX?
Can the micro-CEX provide discriminatory assessment for residents across different years of practice?
What are the perceptions of the faculty and residents regarding the factors affecting utility of the assessment instrument in providing feedback and assessment?
II. METHODS
A. Setting and Subjects
The study was conducted in the division of Internal Medicine in a 1700 bed hospital in Singapore between September and December 2018. All faculty and residents rotating through internal medicine were invited to participate via e-mail, and agreeable faculty and residents paired up. In usual practice, residents must complete at least 2 mini-CEX covering standard inpatient or outpatient encounters during each three-month internal medicine posting, hence both residents and faculty are familiar with the usual mini-CEX.
B. Design
In order to evaluate for any participant reactivity affecting the CEX data (i.e. a Hawthorne effect) (Paradis & Sutkin, 2017), a baseline sample of 30 of the usual mini-CEX performed in the 3 months prior to the study was randomly selected and deidentified (from June to August 2018) . The quantity and specificity of feedback in these was evaluated as detailed below.
For the study itself, faculty and residents used the usual mini-CEX as the first assessment in the first 2 weeks of the month, followed by a second assessment using the micro-CEX in the next 2 weeks. This sequence was chosen as performing the micro-CEX first might affect how the subsequent mini-CEX was performed. Cases chosen for the mini-CEX and micro-CEX were inpatient or outpatient internal medicine encounters, and faculty were simply instructed to choose cases that represented typical cases of average difficulty with no restrictions on the exact cases to be chosen.
Faculty and residents completed an anonymised survey on their experiences at the end of the study and were invited to participate in a semi-structured group interview to elicit their views regarding which aspects of the mini-CEX exercise influenced feedback and assessment (Appendix 2). Both faculty and residents were informed that the survey and interviews were part of this study and participation in either was taken to be implied consent. The workflow of the study is seen in Figure 1.
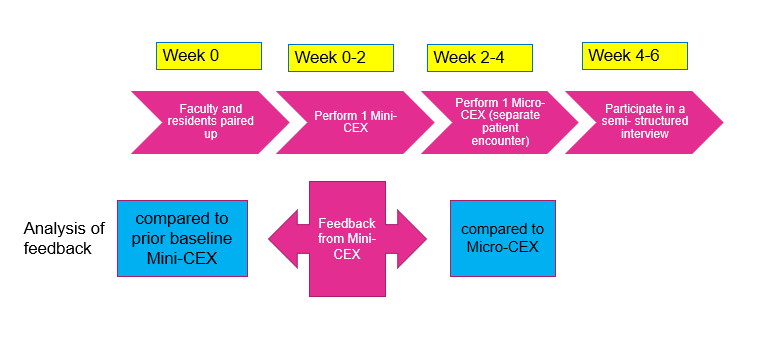
Figure 1. Study workflow
C. Instruments
The mini-CEX used in the program is based on the one described by Norcini (Norcini et al., 2003).This form was hosted on the internet ( New Innovations, Ohio, USA) and could be accessed by faculty from their mobile devices or their email. The micro- CEX was hosted on an opensource online survey tool (LimeSurvey GmbH, Hamburg, Germany) and can be accessed from mobile devices. A copy of both forms is available in Appendix 1.
D. Analysis of Feedback
The quality of feedback was assessed firstly by a word count, and then by grading the specificity of the feedback on a three-point scale (Pelgrim et al., 2012) (Appendix 3) and finally by the presence or absence of an actionable plan for improvement. In order to avoid rater bias, the assessor for the specificity of the feedback was blinded to the source of feedback (mini or Micro CEX). The first 20 forms were independently graded by two separate assessors (OTH and AC) using the above criteria, achieving a kappa coefficient of 0.852; all subsequent forms were graded by OTH, with any uncertainty resolved by discussion between AC and OTH. Word count and specificity, as well as faculty and resident preferences between the forms, were analysed using paired samples T-test. Proportion of Feedback which showed an actionable plan was compared using a Chi-Square test.
E. Semi-structured Interviews
Faculty and residents were interviewed separately. 21 residents and 6 faculty were interviewed over 8 sessions lasting between 20 to 30 minutes each. Interviews were conducted by the investigator (OTH). The interviews were audiotaped and transcribed verbatim. Data collection ended when saturation was reached. Member checking of the transcripts was carried out.
The inductive template analysis as described by Nigel King was used to analyse the interview transcripts (King, 2012). Two transcripts were studied and coded separately by the investigator (OTH) and a collaborator (OHK). A priori themes of assessment, feedback and administration were used to structure the data so that the research question could be answered. Codes were discussed between OTH and OHK until a consensus was reached, and a codebook was created. The subsequent transcripts were coded by OTH. OHK, AC and OTH subsequently met to discuss the categories and emerging themes. NVivo 12 was used to store and manage the codes and transcripts. Results were triangulated with data from the quantitative surveys.
For all quantitative data, an alpha of 0.05 was used as the cut-off for significance. IBM SPSS 25 (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY) was used for calculations.
III. RESULTS
The data that support the findings of this study are openly available in Figshare repository, at https://doi.org/10.60 84/m9.figshare.21862068.v1 (Ong, 2023).
There were 33 internal medicine residents during the study period and 32 (97%) participated in the study; one resident declined to participate. They were paired with 39 different faculty over the three months of the study. 59 unique faculty- resident pairs completed both sets of CEX. 30.5% of the residents were in their first year of residency (R1), 47.9% in second year (R2), and 22.0% were in their third year (R3). The residents completed an average of 1.96 pairs of mini and micro CEX each. Time taken to complete the assessments was estimated by faculty to be 11.33 +/- 6.56 min for mini-CEX vs 9.42 +/-5.51 min for the micro-CEX (p = 0.02).
A. Evaluation of Feedback in the Mini-CEX: Baseline and During Study
30 de-identified mini-CEX were extracted randomly from the 3 months preceding the initiation of the study. These served as a baseline control and were compared to the feedback from the first, traditional mini-CEX done during the study (Table 1). During the period of the study, faculty using the same mini-CEX provided feedback that was more specific. Proportion of actionable feedback provided was much more in the mini-CEX done as part of the study compared to baseline controls (Table 1: 3.3% controls vs 28% study mini-CEX, p = 0.005).
|
|
Mini-CEX vs prior baseline control |
Mini-CEX vs Micro-CEX |
||||
|
Prior baseline control mini-CEX (mean+/-SD) |
Study Mini-CEX (mean +/- SD) |
p value |
Mini-CEX (mean +SD) |
Micro CEX (mean +SD) |
p value |
|
|
Q1 in which areas did the resident do well |
|
|||||
|
Word count |
12.1 +/-14.1 |
9.5 +/- 7.0 |
0.93 |
9.5 +/- 7.0 |
17.5 +/- 10.3 |
<0.001 |
|
Specificity* |
1.2 +/- 1.0 |
1.6 +/- 0.90 |
0.08 |
1.6+/- 0.9 |
2.3 +/- 0.7 |
<0.001 |
|
Q2/3 Areas needing improvement/ recommendations for future improvement |
||||||
|
Word count |
3.8 +/- 6.8 |
5.7 +/- 7.3 |
0.06 |
5.7 +/- 7.3 |
19.3 +/- 15.1 |
<0.001 |
|
Specificity* |
0.5 +/- 0.7 |
1.1 +/-1.1 |
0.01 |
1.1 +/- 1.0 |
1.8 +/- 0.9 |
<0.001 |
|
Actionable |
1/30 (3.3%) |
17/59(28.8%) |
0.005 |
17/59 (28.8%) |
18/59(30.5%) |
0.84 |
Table 1. Quality and quantity of feedback in prior baseline control vs study mini-CEX, and in mini vs Micro-CEX
B. Evaluation of Feedback in the Micro and Mini-CEX During Study
Comparison of the feedback given in the mini and micro-CEX during the study is shown in Table 1. Feedback wordcount increased and was more specific with micro-CEX compared to the contemporaneous mini-CEX done by the same pair. However, there were no differences in the proportion of actionable feedback given in both forms.
C. Discrimination Between Residents in Different Years of Training
The micro-CEX was able to show progression between the years of training, with a significant rise in the resident’s mean score across the three years of training. On a 4 point score the mean entrustment score increased from 2.45 in the first year of training to 3.30 by the third year (p<0.05). (Figure 2)
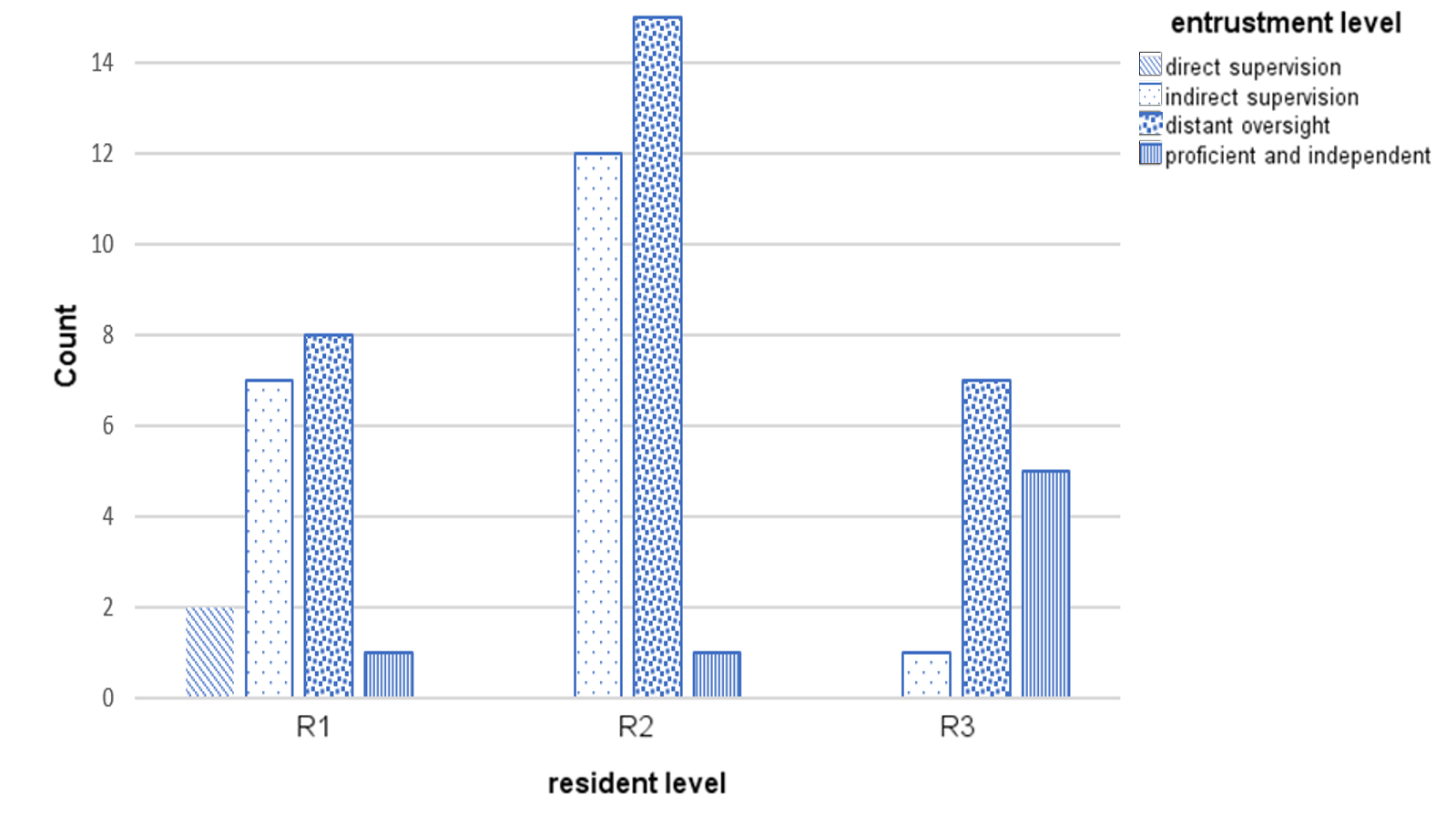
Figure 2. Level of entrustment vs Year of training
Correlation of residents’ year of training and grading of the mini-CEX domains was moderate (kappa 0.39 to 0.60). There was high correlation between all seven questions in the mini-CEX (kappa 0.7 to 0.8) (see appendix 4), implying that the resident’s score in one domain heavily influenced the score in other domains i.e. a halo effect.
D. Faculty and Resident Preferences
21 (out of total 32 participating residents, 65% response rate) residents and 25 (out of total 39 participating faculty, 64.9% response rate) responded to the survey. Faculty and residents felt that the Micro -CEX had better value for both assessment and feedback compared to the Mini-CEX (Table 2).
|
|
Mini-CEX Mean + SD |
Micro CEX Mean + SD |
p value |
t-Stats |
Cohen’s d |
|
Usefulness for assessment |
|||||
|
Faculty |
6.04 +/- 1.34 |
6.57 +/- 0.95 |
0.04 |
2.23 |
0.46 |
|
Residents |
6.00 +/- 1.62 |
6.9 +/- 0.91 |
0.03 |
-2.31 |
0.52 |
|
Usefulness for feedback |
|||||
|
Faculty |
6.00 +/- 1.35 |
6.87 +/- 1.10 |
0.01 |
-3.07 |
0.64 |
|
Residents |
5.43 +/- 1.40 |
6.81 +/- 1.57 |
0.09 |
-3.82 |
0.83 |
Table 2. Perceptions of faculty and residents regarding usefulness of mini and micro-CEX for assessment and feedback
*Scoring is on a 9-point Likert scale, with 1 = not useful at all …. 9 = very useful
E. Qualitative Data
Qualitative data from the semi-structured interviews was analysed to better understand what the features of the micro-CEX driving this preference were, and to look for helpful features in the CEX. Themes from the semi-structured interviews were distilled into 6 themes (Table 3):
1) Make it easy: A recurrent theme was that the micro-CEX was easier to use and the short form could be used by the bedside, on resident or faculty mobile devices.
2) Immediacy is important: Faculty and residents both prized the ability to integrate the assessment into their daily routines, and this immediacy was very important in enhancing the value of the feedback.
3) Tell us what it’s for: Faculty and residents both expressed that the intended purpose of the forms needed to be explicit. Uncertainty in purpose of the form resulted in a perception of redundancy with the other assessments, and confusion about summative vs formative intent of the assessment inhibited honest feedback and assessment.
4) Structure the form so we know what you want: Structuring the form with specific areas to remind them to provide narrative feedback, and what specific areas to provide feedback in, was useful. Faculty and residents both felt that the micro-CEX had better learning value than the mini-CEX.
5) Choice of assessor matters depending on objective of the tool: Faculty and residents agreed that assessments were frequently affected by the prior experiences between the two, impacting the objectivity of assessments via both the micro-and mini- CEX. Prior engagement with the resident facilitated provision of feedback. However, for assessment purposes, residents felt that a faculty with no prior knowledge of the trainee might be more objective.
6) Align assessment with learning goals: Many of the residents were preparing for their postgraduate medical examinations, and they found the mini-CEX exercise especially useful if it was conducted in a way similar to their examinations (the Royal College of Physicians PACES exam) – in other words, the utility of the exercise increased greatly when the assessment was aligned with the residents’ own learning goals.
|
S/N |
Themes |
Quotations |
|
1. |
Make it easy to do |
The micro-CEX was “more succinct. So, it’s, it’s much easier to administer” -F
“If it’s a shorter form, even though the quantity may be less maybe the fact that the quality of whatever feedback we’re given is better because they’re really giving the one or two points that really stood out to them that we need to improve on or the one or two things that we really did well” -R
(Regarding the mini-CEX) “The fact that it’s more detailed actually maybe reduces the quality of the feedback because … if you ask me for additional remarks for every single domain, then they just put nil, nil, nil because there’s no time” -F
|
|
2. |
Immediacy is important |
“Memory is also fresh because you’ve just done the case and so I think the learning value’s a lot better” -R
“I think looking at it in terms of like a learning experience also, um, when we have that micro-CEX on the spot, ah, not only can we address, like all the points immediately, like what the resident should, um, but at the same time, ah, you can kinda go through certain topics at the same setting as well” -F
|
|
3. |
What is this for |
“I think we need clear goals as to why we do these, rather than to simply check boxes.” -R
“The form should come with what is the expectation of this, uh, assessment, whether it’s for assessing, or it’s for a feedback, or it’s …. whether this person can work as a HO. I mean, the intention will drive how I assess” -R
“We have a lot of forms, the 360 and the mini-cex and all. Sometimes maybe I personally don’t really see what the difference is sometimes or how it can help to change assessment. I think it’s just extra admin for everyone and everyone just gets fed up doing it” -R
“I think the assessor, sometimes they’re very nice, they know it affects your, your grading or your, your overall performance in the residency, so they try not to be too strict” -R
|
|
4. |
Be specific about what you want to know |
The micro-CEX had “I think several features currently that are really quite useful. Number one is that there is the mandatory open-ended field, um, for areas that need improvement and areas that need to be reinforced” -F
“I find the comments, uh, quite useful. Maybe not the grades itself, because usually people would just give, like, mod- middle-grade. But, the written comments are actually quite useful” -R
|
|
5. |
Choice of assessor matters depending on objective for the tool |
“It’s quite easy for me to, to, to, remember each of them and give them dedicated feedback” -F
“It should be someone that you don’t really know, but maybe in the same department. So, that it can be like, really, like a proper case scenario, yeah. Instead of grading you based on what their other impressions are” -R
|
|
6. |
Align assessment with learning goals |
“So I had this one particular case, that was a very good PACES case, that I clerked in the morning, and, we impromptu made it into a mini-CEX kind of session and, and we went in quite in depth into the discussion, and PACES that sort of stuff, and I thought that was very useful.” -R
|
Table 3. Themes with supporting quotations
*1 PACES = Membership of Royal Collage Physicians clinical examination, a required exit certification for the residents.
IV. DISCUSSION
The most striking result from this study is that even without specific faculty training or other intervention, simplifying the assessment task alone led faculty to write longer, and more specific feedback. Faculty and residents also perceived that the feedback was better. By simplifying the assessment, the faculty’s attention was shifted from grading the resident in multiple domains toward qualitatively identifying good and bad points in the encounter, providing feedback for the residents.
Proportion of actual actionable feedback in the two forms, however, was not different. This is perhaps because there was no specific faculty training for the study as we felt that the additional training itself would impact results. Specific faculty training may be needed to improve this aspect.
A Hawthorne effect was noticed in the study (Adair, 1984). The proportion of actionable feedback provided was much more in the mini-CEX done as part of the study compared to baseline controls (Table 1: 3.3% controls vs 28% study mini-CEX, p = 0.005). Word count and specificity also increased. However, despite this, we were still able to show that the micro-CEX induced faculty to provide more and better feedback.
From the global entrustment scale used in the micro-CEX, it was possible to demonstrate progression from first year to third year of residency (Figure 2). One potential concern is loss of granularity in assessment of different domains, i.e., that we might lose the ability to identify the specific domain in which the resident is weak if we do not ask faculty to score physical examination, history taking, management etc. separately. However, we found a high correlation between the scores in all domains in the mini-CEX (kappa ranged from 0.7 to 0.8, see appendix 4), indicating a strong halo effect. This suggests that in practice, faculty are making a global assessment anyway rather than a separate assessment of separate domains. Faculty and residents perceived that the single global assessment with the micro-CEX provided better assessment.
The messages from faculty and residents about what they perceive to be important in making the CEX work for them speak for themselves. The importance of making the form easy to administer is very intuitive; the bureaucratic impracticality of paper portfolios was pointed out long ago and e-portfolios were touted as the preferred solution (Van Tartwijk & Driessen, 2009) but the message here is that administrative details have significant impact on the utility of the CEX – many of the issues cited such as the number of assessments an individual assessor has to make, whether the assessor is equipped to do the assessment on the spot, or whether the assessor has prior exposure to the resident or not – are administrative and educational design details that faculty training alone cannot solve.
Our study had several limitations. Variations in the clinical environment such as ward vs ambulatory clinic, variable workload or competing responsibilities of the faculty and residents might have affected how the CEX was administered. However, distractions in the ward do affect the performance of CEX in real life as well.
We also note that in this study design, the mini-CEX was performed before the micro-CEX. This was deliberate as the residents and faculty were used to doing the mini-CEX on an ongoing basis so the first mini-CEX would be a “usual” assessment followed by the new assessment. Performing the micro-CEX first might affect how the subsequent mini-CEX was performed.
In this study, we did not attempt to make judgements about reliability and validity of the micro-CEX as only one specific data point was obtained for each trainee. The mini-CEX is validated to be reliable mainly in the context of repeated tests , and preferably in the context of a coherent program of assessment (van der Vleuten & Schuwirth, 2005). Whether the micro-CEX is able to provide equivalent robust and valid assessment compared to the mini-CEX depends on how it is used and is an area ripe for future study.
V. CONCLUSION
Our study demonstrated that the micro-CEX has a high rate of acceptability amongst faculty and residents, as well as a measurable improvement in feedback characteristics compared to the usual mini-CEX. The context in which the form is administered in actual practice has significant impact on its utility for feedback and assessment.
Ethical Approval
The study protocol was reviewed by the hospital Institutional Review Board, who deemed this as an educational quality improvement project which did not require IRB approval (Singhealth CIRB Ref: 2018/2696).
Notes on Contributors
Thun How Ong conceptualised and designed the study, administered the interviews, analysed the data and wrote the manuscript.
Hwee Kuan Ong participated in data analysis and coding of the qualitative data.
Adrian Chan participated in data analysis and in grading of the feedback specificity.
Dujeepa D. Samarasekera provided input on initial study design and reviewed the manuscript.
C. P. M. van der Vleuten provided guidance and input at all stages of the study, from initial study design to data analysis and manuscript writing.
Data Availability
The data that support the findings of this study are openly available in Figshare repository, at
https://doi.org/10.6084/m9.figshare.21862068.v1
Acknowledgement
The authors would like to acknowledge the contributions of the following:
Tan Shi Hwee and Nur Suhaila who provided the administrative support that made the whole project feasible.
The Faculty and Residents who were willing to do the extra CEX and the interviews, and who labour daily in pursuit of the ultimate goal of providing better care for our patients.
Funding
No funding was obtained for this study.
Declaration of Interest
All authors have no declaration of interest.
References
Adair, J. G. (1984). The Hawthorne effect: A reconsideration of the methodological artifact. Journal of Applied Psychology, 69(2), 334-345. https://doi.org/10.1037/0021-9010.69.2.334
Berendonk, C., Rogausch, A., Gemperli, A., & Himmel, W. (2018). Variability and dimensionality of students’ and supervisors’ mini-CEX scores in undergraduate medical clerkships – A multilevel factor analysis. BMC Medical Education, 18(1), 100. https://doi.org/10.1186/s12909-018-1207-1
Bindal, T., Wall, D., & Goodyear, H. M. (2011). Trainee doctors’ views on workplace-based assessments: Are they just a tick box exercise? Medical Teacher, 33(11), 919-927. https://doi.org/10.3109/0142159X.2011.558140
Brazil, V., Ratcliffe, L., Zhang, J., & Davin, L. (2012). Mini-CEX as a workplace-based assessment tool for interns in an emergency department – Does cost outweigh value? Medical Teacher, 34(12), 1017-1023. https://doi.org/10.3109/0142159X.2012.719653
Castanelli, D. J., Jowsey, T., Chen, Y., & Weller, J. M. (2016). Perceptions of purpose, value, and process of the mini-Clinical Evaluation Exercise in anesthesia training. Canadian Journal of Anaesthesia, 63(12), 1345-1356. https://doi.org/10.1007/s12630-016-0740-9
Crossley, J., & Jolly, B. (2012). Making sense of work-based assessment: Ask the right questions, in the right way, about the right things, of the right people. Medical Education, 46(1), 28-37. https://doi.org/10.1111/j.1365-2923.2011.04166.x
Hawkins, R. E., Margolis, M. J., Durning, S. J., & Norcini, J. J. (2010). Constructing a validity argument for the mini-Clinical Evaluation Exercise: A review of the research. Academic Medicine, 85(9), 1453-1461. https://doi.org/10.1097/ACM.0b013 e3181eac 3e6
Ilgen, J. S., Ma, I. W., Hatala, R., & Cook, D. A. (2015). A systematic review of validity evidence for checklists versus global rating scales in simulation-based assessment. Medical Education, 49(2), 161-173. https://doi.org/10.1111/medu.12621
King, N. (2012). Doing template analysis. Sage Knowledge, 426-450. https://doi.org/10.4135/9781526435620.n24
Kogan, J. R., & Holmboe, E. (2018). Practical guide to the evaluation of clinical competence appendix 4.6 (2nd ed.). Elsevier.
Liao, K. C., Pu, S. J., Liu, M. S., Yang, C. W., & Kuo, H. P. (2013). Development and implementation of a mini-Clinical Evaluation Exercise (mini-CEX) program to assess the clinical competencies of internal medicine residents: From faculty development to curriculum evaluation. BMC Medical Education, 13, 31-31. https://doi.org/10.1186/1472-6920-13-31
Lörwald, A. C., Lahner, F. M., Greif, R., Berendonk, C., Norcini, J., & Huwendiek, S. (2018). Factors influencing the educational impact of Mini-CEX and DOPS: A qualitative synthesis. Medical Teacher, 40(4), 414-420. https://doi.org/10.1080/0142159X.2017 .1408901
Lorwald, A. C., Lahner, F. M., Nouns, Z. M., Berendonk, C., Norcini, J., Greif, R., & Huwendiek, S. (2018). The educational impact of mini-Clinical Evaluation Exercise (mini-CEX) and Direct Observation of Procedural Skills (DOPS) and its association with implementation: A systematic review and meta-analysis. PLoS One, 13(6), Article e0198009. https://doi.org/10.1371/jour nal.pone.0198009
Morris, A., Hewitt, J., & Roberts, C. M. (2006). Practical experience of using directly observed procedures, mini Clinical Evaluation Examinations, and peer observation in pre-registration house officer (FY1) trainees. Postgraduate Medical Journal, 82(966), 285-288. https://doi.org/10.1136/pgmj.2005.040477
Nair, B. R., Alexander, H. G., McGrath, B. P., Parvathy, M. S., Kilsby, E. C., Wenzel, J., Frank, I. B., Pachev, G. S., & Page, G. G. (2008). The mini clinical evaluation exercise (mini-CEX) for assessing clinical performance of international medical graduates. Medical Journal of Australia, 189(3), 159-161.
Norcini, J. J., Blank, L. L., Duffy, F. D., & Fortna, G. S. (2003). The mini-CEX: A method for assessing clinical skills. Annals Internal Medicine, 138(6), 476-481.
Ong, T. H., Ong, H. K., Chan, A., Samarasekera, D. D., van der Vleuten, C. (2023). Micro CEX vs Mini CEX: Less can be more [Dataset]. Figshare. https://doi.org/https://doi.org/10.6084/m9.Fig share.21862068.v3
Paradis, E., & Sutkin, G. (2017). Beyond a good story: From Hawthorne Effect to reactivity in health professions education research. Medical Education, 51(1), 31-39. https://doi.org/10.1111/medu.13122
Pelgrim, E. A. M., Kramer, A. W. M., & Van der Vleuten, P. M. (2012). Quality of written narrative feedback and reflection in a modified mini-Clinical Evaluation Exercise: An observational study. BMC Medical Education, 12(1), 97. https://doi.org/10.1186/1472-6920-12-97
Regehr, G., MacRae, H., Reznick, R. K., & Szalay, D. (1998). Comparing the psychometric properties of checklists and global rating scales for assessing performance on an OSCE-format examination. Academic Medicine, 73(9), 993-997.
Sabey, A., & Harris, M. (2011). Training in hospitals: What do GP specialist trainees think of workplace-based assessments? Education for Primary Care, 22(2), 90-99.
Tavares, W., Ginsburg, S., & Eva, K. W. (2016). Selecting and simplifying: Rater performance and behavior when considering multiple competencies. Teaching and Learning in Medicine, 28(1), 41-51. https://doi.org/10.1080/10401334.2015.1107489
van der Vleuten, C. P., & Schuwirth, L. W. (2005). Assessing professional competence: From methods to programmes. Medical Education, 39(3), 309-317. https://doi.org/10.1111/j.1365-2929. 2005.02094.x
Van Tartwijk, J., & Driessen, E. W. (2009). Portfolios for assessment and learning: AMEE Guide no. 45. Medical Teacher, 31(9), 790-801. https://doi.org/10.1080/01421590903139201
Walzak, A., Bacchus, M., Schaefer, J. P., Zarnke, K., Glow, J., Brass, C., McLaughlin, K., & Ma, I. W. (2015). Diagnosing technical competence in six bedside procedures: Comparing checklists and a global rating scale in the assessment of resident performance. Academic Medicine, 90(8), 1100-1108. https://doi.org/10.1097/acm.0000000000000704
Weller, J. M., Misur, M., Nicolson, S., Morris, J., Ure, S., Crossley, J., & Jolly, B. (2014). Can I leave the theatre? A key to more reliable workplace-based assessment. British Journal of Anaesthesia, 112(6), 1083-1091. https://doi.org/10.1093/bja/aeu052
Weston, P. S. J., & Smith, C. A. (2014). The use of mini-CEX in UK foundation training six years following its introduction: Lessons still to be learned and the benefit of formal teaching regarding its utility. Medical Teacher, 36(2), 155-163. https://doi.org/10.3109/0142159X.2013.836267
Yanting, S. L., Sinnathamby, A., Wang, D., Heng, M. T. M., Hao, J. L. W., Lee, S. S., Yeo, S. P., & Samarasekera, D. D. (2016). Conceptualizing workplace-based assessment in Singapore: Undergraduate mini-Clinical Evaluation Exercise experiences of students and teachers. Tzu-Chi Medical Journal, 28(3), 113-120. https://doi.org/10.1016/j.tcmj.2016.06.001
*Ong Thun How
Academia, 20 College Road,
Singapore 168609
97100638
Email: ong.thun.how@singhealth.com.sg
Published online: 2 January, TAPS 2024, 9(1), 1-2
https://doi.org/10.29060/TAPS.2024-9-1/EV9N1
The practice of medicine and provision of healthcare is evolving rapidly, driven not just by advancements in new treatment modalities but also by the integration of modern technologies in providing precision care to our patients. It is important to understand and embrace, where appropriate, innovative technologies to respond effectively to the evolving needs of a modern society. What will be seen in this transformative wave is how Artificial Intelligence (AI) has the potential to revolutionise various sectors in medicine and healthcare (Yu et al., 2018).
Focusing on health professions education, AI emerges as a pivotal force in training the future healthcare practitioners and preparing them for the multifaceted challenges of the modern medical landscape (Paranjape et al., 2019). There are 3 distinct uses of AI in education which was reported by Baker et al. (2019): Learner-oriented AI, Instructor-oriented AI and Institution-oriented AI. Let’s focus on some of these areas:
A. Enriched Learning Experiences
One of the most significant advantages of integrating AI into health professions education is the enhancement of learning experiences. AI-powered platforms can provide personalised, adaptive learning modules tailored to individual students’ needs and learning paces (Kong et al., 2021). This personalisation not only accelerates the learning process but also ensures that students grasp complex concepts thoroughly, laying a robust foundation for their future careers. Furthermore, AI provides the opportunity for the students as well as for the trainers to use and adapt the best materials from multiple sources. It also enhances their networking through AI search capabilities and the ability to link up with other experts in the field or learning communities (Luke et al., 2021).
B. Simulation and Practical Training
AI-driven simulations are revolutionising practical training in healthcare education. Medical students can now practice patient safety, surgical procedures, diagnose illnesses, and interact with virtual patients in a risk-free environment. These simulations not only refine their technical skills but also improve their decision-making and inter-professional teamwork abilities. By repeatedly engaging in realistic scenarios, students can hone their expertise, fostering confidence and competence before they enter real-world clinical settings, a critical step to ensure patient safety and ethical practice of medicine.
C. Data-Driven Insights
AI’s ability to analyse large amounts of data quickly and efficiently provide an excellent platform to improve systems and processes (American Medical Association [AMA], 2016). In the context of health professions education, this capability translates into valuable insights. Educational institutions can collect data on students’ performance, identify areas where they struggle, and provide targeted interventions. Educators can adapt their teaching methods based on this data, ensuring that their teaching-learning approaches are appropriate and leading to good outcomes. Moreover, AI can predict trends in learning, enabling institutions to proactively address challenges and optimise their curricula. Funding and resource allocations can also be done where it is needed most or areas of future needs to build capacity and relevance of programs.
D. Fostering Research and Innovation
AI-powered tools are accelerating Scholarship of Teaching and Learning in the areas of research and innovation. AI algorithms help to analyse large amounts of data quickly and identify patterns that researchers could potentially miss. This could help us better understand the complex datasets, find relationships between variables faster, and draw appropriate conclusions and recommendations. AI has also reduced the time required to conduct literature review by analysing large amounts of scientific articles, identifying relevant research, and summarising the content in seconds.
E. Addressing Global Health Disparities
Focusing on medical and health professions education, we believe that this is another area AI could assist and enhance the training of healthcare practitioners in resource poor settings. Unbundling of curricula and connecting with the best training materials as well as experts are key advantages of AI capable training environments could support the resource poor settings.
Another area that AI driven knowledge and skills sharing could be addressing the present shortage of skilled healthcare professionals, leading to significant disparities in healthcare access. AI-based education has the potential to bridge this gap. Online platforms and mobile applications powered by AI can deliver high-quality continuous professional development to remote and underserved communities, reaching out to healthcare professionals irrespective of their geographical location. With this unbundling, the present set programs or training, we believe has the potential to significantly reduce global healthcare disparities.
F. Ethical Considerations and Collaboration
While the potential of AI in health professions education is immense, it is crucial to navigate ethical challenges. In the process of developing AI capable environments, we must ensure that the systems are transparent, unbiased and fair. However, we do not see in any medical school or a healthcare training site developing or having conversations on the use of guidelines/protocols on ethical use of AI in health professional education. Educators, policymakers, and technology developers must collaborate to establish ethical guidelines that ensure the responsible use of AI. This collaboration should prioritise transparency, fairness, and equity, safeguarding the integrity of healthcare education and the welfare of future patients (Chan & Zary, 2019).
Artificial Intelligence provides huge benefits to health professions education in many ways. By embracing AI-powered tools and methodologies, educational institutions can produce a generation of healthcare professionals who are not only adept at leveraging advanced technologies, but also compassionate and skilled in delivering patient-centred care. As we advance and evolve, it is clear that we need to channel our efforts into the investment of AI capabilities, aiming to elevate the learning experiences of our students and residents, propel educational scholarship and research forward, and foster enhanced collaboration. This strategic commitment is essential to maximising the potential advantages of this technology, with a primary objective of ultimately enhancing the health and well-being of patients within both local and global communities. The achievement of success in this pursuit necessitates a united front, where educators, institutions, and policymakers collaborate seamlessly. Only through such concerted efforts can we guarantee that AI not only benefits current learners but also ensures future positive impact on the well-being of the patients they will serve.
Dujeepa D. Samarasekera, Shuh Shing Lee & Han Ting Jillian Yeo
Centre for Medical Education (CenMED), NUS Yong Loo Lin School of Medicine,
National University Health System, Singapore
American Medical Association. (2016). Digital Health Study Physicians’ motivations and requirements for adopting digital clinical tools. https://www.ama-assn.org/practice-management/digital
Baker, T., Smith, L., & Anissa, N. (2019). Educ-AI-tion Rebooted? Exploring the future of artificial intelligence in schools and colleges. Nesta. https://www.nesta.org.uk/report/education-rebooted/
Chan, K. S., & Zary, N. (2019). Applications and challenges of implementing artificial intelligence in medical education: Integrative review. JMIR Medical Education, 5(1), Article e13930. https://doi.org/10.2196/13930
Luke, N., Taneja, R., Ban, K., Samarasekera, D., & Yap, C. T. (2021). Large language models (ChatGPT) in medical education: Embrace or abjure? The Asia Pacific Scholar, 8(4), 50-52. https://doi.org/10.29060/TAPS.2023-8-4/PV3007
Paranjape, K., Schinkel, M., Nannan Panday, R., Car, J., & Nanayakkara, P. (2019). Introducing artificial intelligence training in medical education. JMIR Medical Education, 5(2), Article e16048. https://doi.org/10.2196/16048
Yu, K. H., Beam, A. L., & Kohane, I. S. (2018). Artificial intelligence in healthcare. Nature Biomedical Engineering, 2(10), 719-731. https://doi.org/10.1038/s41551-018-0305-z
Submitted: 11 August 2023
Accepted: 23 August 2023
Published online: 2 January, TAPS 2024, 9(1), 64-65
https://doi.org/10.29060/TAPS.2024-9-1/LE3109
Mildred Lopez
Tecnologico de Monterrey, Escuela de Medicina y Ciencias de la Salud, Mexico
Artificial intelligence (AI) in education has raised several ethical questions regarding academic integrity, privacy, and bias in language algorithms (Master, 2023). These concerns have yielded to distrust to the point that several institutions banned chatbots at Campus locations. Still, the discussion should not be about whether we should use them but how fast we can leverage the data-crunching possibilities to address the biggest challenges of medical education. To do so, educators have the task of transforming the generic use of generative AI to a specific task, such as designing an educational case, a grading rubric, or an exam. However, the quality of the designs depends heavily on the clarity of the educational intent and the technological savviness of the user to provide clear instructions for the algorithm to process.
Early experimentation of educators with generative AI, such as ChatGPT, could be an opportunity to refine the technological savviness and the specificity of prompts we supply to make the algorithm produce more effectively. Recently, Rospigliosi (2023) discussed that the challenge is to define what to ask of ChatGPT, as the quality of the prompt makes the quality of the response. In this ideation and creation stage, where early adopters are piloting small-scale interventions and experimenting with the tool’s limits, educators must work collaboratively across continents and among fields to define guidelines and identify effective strategies for large-scale implementations. While doing so, we speed up the developing process of learning resources in medical education and aspire to have more updated content in the curriculum.
Nevertheless, once a recipe to generate a learning resource has been implemented, the quality of the produced content should be assessed by specialists in the field. The definition of that quality level is also a field for discussion but should be closely aligned with the educational intent. In the future, not so far away, we could even have an AI tool to assess the quality of the content that the generative AI created. Then the question remains: What AI prompt would be the best to do what I, as an educator, need to work on?
Notes on Contributors
ML wrote the manuscript and edited it.
Funding
No funding was received for writing this paper.
Declaration of Interest
The author declares that there is no conflict of interest to disclose.
References
Masters, K. (2023). Ethical use of Artificial Intelligence in Health Professions Education: AMEE Guide No. 158, Medical Teacher, 45(6), 574-584. https://doi.org/10.1080/0142159X.2023.2186203
Rospigliosi, P. (2023). Artificial intelligence in teaching and learning: What questions should we ask of ChatGPT? Interactive Learning Environments, 31(1), 1-3. https://doi.org/10.1080/10448 20.2023.2180191
*Mildred Lopez
Ave. Eugenio Garza Sada 2501 Sur. Col Tecnologico,
64710
Monterrey, Mexico
Email: mildredlopez@tec.mx
Submitted: 25 May 2023
Accepted: 27 July 2023
Published online: 2 January, TAPS 2024, 9(1), 61-63
https://doi.org/10.29060/TAPS.2024-9-1/CS3061
Veranja Liyanapathirana
Department of Microbiology, Faculty of Medicine, University of Peradeniya, Sri Lanka
I. INTRODUCTION
Antimicrobial resistance has been considered a “silent” global pandemic of magnitudes similar to climate change. However, just as climate change, awareness and understanding of the public on this needs to be increased. Recent work from Sri Lanka indicates the same (Gunasekera et al., 2022). World Health Organisation (WHO) also recommends that awareness should be increased among those involved in antibiotic prescription as well as consumers and that this should be made part of the core curriculum in professional training (World Health Organisation, 2023). Those studying in health-science related streams and other biology related streams tend to take knowledge on concepts like “microorganisms”, “infectious diseases” and “antibiotics” as granted. As they are taught these concepts, or they revise what they learnt in school once again in the university, they assume that the others may also have an acceptable level of understanding on these key concepts. This leads to a communication gap between the two groups of people, the ones who have formal education on concepts like “microorganisms”, “infectious diseases” and “antibiotics” and the ones who do not have such education. Therefore, we find that health education materials are not targeted to the level of simplicity that is required by the general public.
The target audience for the assignment in this particular course were from a general biology background, with no training in health-sciences in the university. For these students, a course on “Bacteria of Medical Importance” was commenced in the first semester of the third year. This included introductory lectures on antibiotics, antibiotic sensitivity testing and antimicrobial resistance. The course was conducted by the staff of the Department of Microbiology, Faculty of Medicine, University of Peradeniya, Sri Lanka and the given assignment was designed and conducted by the author.
This activity was planned as an assignment with a reflective component, so that the undergraduates who follow the course would get a first-hand experience in the extent of ignorance that is there regarding antibiotics and their use in the community.
II. METHODS
The assignment being described was developed aiming at increasing the awareness among the participants on the ground reality about the public perceptions on antibiotic use and resistance. At the same time, the activity also aimed to develop reflective practices among the students.
The assignment included the following simple instructions as shown in Table 1. Students were given a period of two weeks to complete the task and upload the content to the learner management system. Students were requested to inform the interviewee they had chosen that the assignment was part of their course work and were requested to get verbal consent for participation.
Once the assignments were submitted, evaluation was conducted and students were given feedback on their reflective write up. For this paper, their reflective write ups were coded and thematically analysed.
|
Talk to a family member/friend who has had no formal teaching on microbiology or health sciences and ask the following questions in English or in the language you converse in. Document the answers you get, translate to English. The last two questions are for you to answer.
• Age of the person spoken to • Highest educational qualification of the person you spoke to • Occupation of the person you spoke to (if a university student, state the course) 1.What is an antibiotic (open ended question)? 2.When did you last take an antibiotic?
3. How did you get that antibiotic?
4. What was the antibiotic you took?
5. Name two other antibiotics you know of.
6. Have you ever taken antibiotics when you have had a cold?
7. What group of micro-organisms cause common cold?
8. 8.1 Do you think it is correct to take antibiotics for common cold?
8.2 Why? (Open ended question): ……………………….. •State one more question you would have liked to ask the participant (just state this without asking your informant): ……………………………. •Your reflection on the answers you got in relation to combatting antimicrobial resistance (500 words): …………………………………………….. |
Table 1: The assignment
III. RESULTS
There were 11 students who took the said course and all of them submitted the assignment on time. The common themes and the narrative that emerged from the analysis of the reflections given by the participants follows.
The subjects interviewed by students were from varying backgrounds. And while some knew that viruses cause common cold other did not know or thought it was caused by bacteria. Nine of the eleven participants interviewed had stated that taking antibiotics for common cold was correct. The reasons given by the subjects interviewed were that doctors prescribe; therefore, antibiotics are indicated in common cold, antibiotics are more potent than pain killers, they give faster cure and boost immunity. Students reflected that the knowledge on antibiotics was poor among the subjects interviewed. Students identified that there is a need for education on this among the general public. There was a theme that emerged which queried the reason for medical officers continue to prescribe antibiotics for common cold as they have been equipped for the necessary knowledge.
IV. DISCUSSION
Reflection is a learned skill. This is not formally taught in many undergraduate courses in Sri Lanka or during secondary education. Therefore, some of the students in the course had written accounts on what is correct and incorrect in relation to antibiotic use or accounts on antibiotic resistance instead of writing a reflection as instructed. Some students did write reflections, still their reflections were mostly not in relation to the possible implications on combatting antimicrobial resistance, but on the answers given in general. Students were given feedback on their reflections.
However, from the reflections provided, a narrative could be derived as stated in the results section, which shows that collectively, their reflections do generate a narrative that is useful. Therefore, from the next batch onwards, we plan to get the students to construct a narrative from their collective reflections.
This was the first time this assignment was used. We chose the questions used as in the local context, antibiotic misuse for upper respiratory tract infections is the commonest reason for antibiotic prescription as well as irrational use (Tillekeratne et al., 2017). But, globally too, upper respiratory tract infections are one of the commonest reasons for antibiotic prescriptions.
We plan to modify this assignment slightly and use it on other undergraduates or postgraduates who are following courses on antibiotics and antimicrobial resistance. As pre-activity exercise, we would like to conduct a briefing session on reflective writing, before the assignment is given to the students.
V. CONCLUSION
The given assignment can be modified and used to increase awareness on the ground realities about the understanding on antibiotics among students who are being educated on antibiotics and antibiotic resistance.
Notes on Contributors
The author conceptualised, conducted and evaluated the assignment and drafted the paper.
Acknowledgement
The author would like to acknowledge all the students of the class and the participants they interviewed.
Funding
No funding was received for the activity.
Declaration of Interest
The author does not have any conflict of interest to declare.
References
Gunasekera, Y. D., Kinnison, T., Kottawatta, S. A., Silva-Fletcher, A., & Kalupahana, R. S. (2022). Misconceptions of antibiotics as a potential explanation for their misuse. A survey of the general public in a rural and urban community in Sri Lanka. Antibiotics, 11(4), 454. https://doi.org/10.3390/antibiotics11040454
Tillekeratne, L. G., Bodinayake, C. K., Dabrera, T., Nagahawatte, A., Arachchi, W. K., Sooriyaarachchi, A., Stewart, K., Watt, M., Østbye, T., & Woods, C. W. (2017). Antibiotic overuse for acute respiratory tract infections in Sri Lanka: A qualitative study of outpatients and their physicians. BMC Family Practice, 18(1), Article 37. https://doi.org/10.1186/s12875-017-0619-z
World Health Organisation. (2023, June) Raising awareness and educating on antimicrobial resistance. https://www.who.int/activities/raising-awareness-and-educating-on-antimicrobial-resistance
*Veranja Liyanapathirana
Department of Microbiology,
Faculty of Medicine,
University of Peradeniya,
Galaha Rd, Peradeniya 20400,
Sri Lanka
+94777060887
Email: veranja.liyanapathirana@med.pdn.ac.lk
Submitted: 12 June 2023
Accepted: 2 August 2023
Published online: 2 January, TAPS 2024, 9(1), 58-60
https://doi.org/10.29060/TAPS.2024-9-1/PV3064
Rintaro Imafuku, Chihiro Kwakami, Kaho Hayakawa & Takuya Saiki
Medical Education Development Center, Gifu University, Japan
I. GLOBALISATION IN EAST ASIA
Globalisation, a complex and multifaceted phenomenon, encompasses not merely an increasing people’s mobility and economical trades, but sometimes, their political and ideological struggles, and cultural identity formation issues, too. While North American and European countries have had a long history of accepting a large number of immigrants, while Asia experienced 74% growth of hosting international migrants from 2000 to 2020, which was most remarkable (McAuliffe & Triandafyllidou, 2021). For example, Japan’s proportion of immigrant population increased from 1.3% in 2000 to 2.2% in 2021, with Chinese migrants constituting the largest group, followed by Vietnamese, Koreans, Filipinos, and Brazilians. Similarly, in 2021, immigrants accounted for 3.4% of Korea’s total population in 2021, compared to 0.5% in 2000. These immigrants came from China, Vietnam, Thailand, Uzbekistan and other countries (McAuliffe & Triandafyllidou, 2021).
These changes in culture and population dynamics have significantly impacted on people’s health and healthcare in East Asia. One of the most challenging issues in such globalised Asian societies is managing intercultural communication between health professionals and migrant patients. Given this context, as languages become a key issue, health professionals are expected to accommodate patients’ communication needs. Moreover, while responding to the rapid internationalisation, health professionals in Asia need to embrace the belief that individuals are members of multiple, diverse, local and non-local networks, thus promoting global citizenship. In fact, the question is: How should Asian health professionals address the intercultural communication situations in healthcare?
II. COMMUNICATION STRATEGIES IN INTERCULTURAL SETTINGS
Many previous linguistic studies have discussed that in Asia, English serves as the lingua franca – a common language adopted among people who do not share a native language. Singaporeans, for instance, use English as an intra-national communication medium, while in East Asian countries, somewhat different contexts would have existed, particularly in relatively ‘monolingual’ speech communities. Given that, most immigrants in East Asia are not native English speakers, in many cases where English does not function as their medium of communication for them. In other words, English is not the sole solution for intercultural communication issues, particularly in East Asian countries. However, some health professionals in Japan viewed English as the panacea for intercultural communication issues, regardless of the patients’ native language, which highlighted the need to consider another communication management strategy in an intercultural setting (Imafuku et al., 2022).
A host country’s plain language, which is defined as clear and concise language accommodation, can be an effective medium of communication (Imafuku et al., 2022). For example, a national survey in Japan demonstrated that many immigrants could understand simple Japanese in daily life, even though their proficiency was limited. Assuming that the speakers tailor their communication to the interlocutors’ language proficiency levels and cultural backgrounds, plain language in spoken communication can be achieved by using short and simple sentences, active voice which emphasises the doer of an action, and personal pronouns which makes it easier for the listeners to picture themselves in the message. Furthermore, speakers must avoid ambiguous expressions and fillers that fill pauses with words, such as “um”, “ah”, “er” and so forth. Visual aids, such as charts, pictures and writing down messages, are also helpful for listeners to process the information in conversations.
Language translation devices, application software, and artificial intelligence (AI) technologies can be useful resources for managing intercultural communication in healthcare. For example, ChatGPT has the potential to assist and enhance health communication in hospitals. In particular, as these AI tools rely on patterns in huge amounts of existing text data, they excel at automating routine tasks, generating document summaries and translating simple texts of factual information. However, the users also need to be aware of the potential drawbacks of these tools, which may lack the ability to interpret patients’ communication signals by patients, such as tone, prosody, and non-verbal cues, potentially resulting in misunderstandings and miscommunications, especially with immigrant patients. This absence of human interaction, including the consideration of patients’ thoughts, emotions, patience, and empathy, emphasises the need for health professionals to critically evaluate and appraise the use of these AI tools for use in intercultural communication (Santandreu-Calonge et al., 2023).
In addition to the linguistic and sociolinguistic aspects, different cultural values and religious beliefs may create barriers in intercultural communication between providers and patients (Zhao, 2023). For example, patients may have diverse perspectives on confidentiality, gender, trust in health professionals and privacy concerns, which greatly impact on interactions in healthcare. Zhao (2023) suggests that patients with certain cultural backgrounds view the family as a collective unit, and would trade off their privacy for family support. However, sharing patients’ information with their family members can pose an issue of confidentiality issues for health professionals. In this case, the patients’ beliefs about family support and ties are closely intertwined with confidentiality in healthcare. In other words, effective intercultural communications will be enhanced by health professionals gaining a better socio-cultural understanding of immigrant patients.
III. MOVING FORWARD: EDUCATIONAL DEVELOPMENT
Educational development is key to effectively addressing the challenges faced by health professionals in East Asia’s globalisation wave. English has been taught as an ‘international academic language’ in Asian medical schools and serves as the medium of instruction in certain countries and Asian institutions. In other words, English can be a means of facilitating intercultural communication in Asian healthcare, particularly for foreign visitors from Western countries.
Additionally, for more successful language accommodation, plain language should be systematically taught in health communication courses in East Asia’s medical education. A growing body of evidence from Western countries indicates that incorporating plain language training into medical education has positive implications for oral and written communication skills. By using the host country’s plain language for practical training of intercultural communication in the curriculum, medical students in East Asia should be given more opportunities to interact with migrant citizens with different cultural backgrounds.
In addition to the effective use of plain language as an option of communication management strategies, this opportunity will also broaden the students’ worldviews and cultural understanding in the current globalised societies. Specifically, our institution, Gifu University, has incorporated learning opportunities through interactions with migrant citizens from Vietnam, Philippines and Brazil into first year medical education. This can serve as a springboard to cultivate the medical students’ global citizenship by learning diverse cultural values through conversations with the migrants in Japan.
Translation software and AI technologies are increasingly being utilised in the intercultural communication settings. Although these devices and tools are helpful, they can also be a double-edged sword for healthcare professionals as communicators. Health professionals and educators should recognise that human interaction is the foundation of communication. Relying excessively on such tools without critical evaluation may cause serious communication problems with migrant patients and their family members. In Japan, information technology has been newly set as a learning objective in the 2022 revision of the Model Core Curriculum for Medical Education (Medical Education Model Core Curriculum Expert Research Committee, 2022). Further educational development is necessary to train health professionals to fully understand the principles of the information science and technology, and effectively apply them in clinical practice. Specifically, in the field of health communication education, the educators must address the challenges posed by rapid globalisation by developing programs that enable learners to understand the advantages and disadvantages of AI-mediated communications and effectively utilise the information technologies in the intercultural settings.
Finally, from the perspective of medical education research, more internationally published research on intercultural health communication from Asian countries is necessary. The rich descriptions and analysis of the interactions between healthcare providers and migrant patients in the current globalised Asian countries can offer different perspectives on medical education for an international readership. Additionally, for further educational development, it would be worthwhile to explore AI-mediated communication in intercultural situations, as this is a relatively new research area.
Notes on Contributors
Rintaro Imafuku contributed to this manuscript’s conceptualisation, wrote its first draft, and revised its subsequent draft. Chihiro Kawakami, Kaho Hayakawa and Takuya Saiki contributed to the conceptualisation and critically revised the first draft. All the authors discussed and contributed to the final manuscript.
Funding
This study was supported by the JSPS KAKENHI [Grant number: 20K10374].
Declaration of Interest
The authors declare no competing interests.
References
Imafuku, R., Nagatani, Y., & Shoji, M. (2022). Communication management processes of dentists providing healthcare for migrants with limited Japanese proficiency. International Journal of Environmental Research and Public Health, 19(22), Article 22. https://doi.org/10.3390/ijerph192214672
McAuliffe, M., & Triandafyllidou, A. (2021). World migration report 2022. International Organization for Migration (IOM). https://publications.iom.int/books/world-migration-report-2022
Medical Education Model Core Curriculum Expert Research Committee. (2022). Model core curriculum for medical education in Japan 2022. Ministry of Education, Culture, Sports, Science and Technology. https://www.mext.go.jp/content/20230315-mxtigaku -000026049_00003.pdf
Santandreu-Calonge, D., Medina-Aguerrebere, P., Hultberg, P., & Shah, M.A. (2023). Can ChatGPT improve communication in hospitals? Profesional de la información, 32(2), Article e320219. https://doi.org/10.3145/epi.2023.mar.19
Zhao, X. (2023). Challenges and barriers in intercultural communication between patients with immigration backgrounds and health professionals: A systematic literature review. Health Communication, 38(4), 824–833. https://doi.org/10.1080/10410236.2021.1980188
*Rintaro Imafuku
1-1 Yanagido Gifu, Gifu, Japan
+81-58-230-6469
Email: imafuku.rintaro.f9@f.gifu-u.ac.jp
Submitted: 20 April 2023
Accepted: 23 August 2023
Published online: 2 January, TAPS 2024, 9(1), 54-57
https://doi.org/10.29060/TAPS.2024-9-1/SC3048
Atul Kumar1, Amol Gawande1, Meghana Bhilare2, Vishal Wadajkar2, Indrajit Ghoshal3 & Shirish Raibagkar4
1Dr.D.Y. Patil B-School, Pune, India; 2Dr.D.Y. Patil Institute of Management and Research, Pune, India; 3Faculty of Computer Science and Engineering, Poornima University, Jaipur, India; 4Savitribai Phule Pune University, Pune, India
Abstract
Introduction: The purpose of this study is to carry out a comparative analysis of the job satisfaction of nurses working in India based on the different types of the hospital they are working with. The study tests the null hypothesis that the job satisfaction of nurses from India across different types of hospitals is the same.
Methods: Four hundred nurses divided into 100 each for four popular types of hospitals – (1) Educational; (2) Government; (3) Charitable Trust; and (4) Private, from all over India were surveyed. Two ANOVA tests were performed. The first one was performed, taking overall job satisfaction as the dependent variable. The second ANOVA was performed by taking the monetary and compensation factors, work environment and management support, and job-related factors as the dependent variables.
Results: The overall mean of job satisfaction was -0.73 (SD 0.60). Overall, 65 percent of the variability of the dependent variable, job satisfaction, is explained by the type of hospital and is statistically significant (p<0.0001).
Conclusion: Monetary and compensation factors, work environment and management support, and job-related factors impact nurses’ job satisfaction. These factors vary with the type of hospital, and hence it can be concluded that due to variation in these factors depending on the type of hospital, the job satisfaction of nurses varies. Implications of our study are for the educational, government, and charitable trust hospitals to improve their work culture, management, and work environment so that nurses will have higher job satisfaction.
Keywords: Nurses, Job Satisfaction, India, Hospitals, Government, Private, Charitable Trust, Educational
I. INTRODUCTION
India’s ratio of nurses per 1000 population is only 1.96 as against the WHO norm of 3 per 1000 population. Another 4.3 million more nurses are required by India by the year 2024 to meet the World Health Organization (WHO) standard of 3 nurses per 1000 population (Business Standard, 2021). Job satisfaction of nurses assumes significance given the huge gap between its current ratio of nurses per 1000 and the WHO norm. But studies investigating linkages between types of hospitals (legal structure of the hospital) and their impact on the job satisfaction of nurses are relatively low. Different types of hospitals can be found in India – Educational, Government, Charitable Trust, Private, Military, Missionary, Railway, and a few more. A sizable amount of literature is available which suggests that factors like organisational culture matters in the job satisfaction of nurses (Rahnavard et al., 2018). But there are few studies correlating these factors with the type of hospital. The association between the factors and the type of hospital remains unexplored. This research attempts to provide empirical evidence supporting the association of the factors influencing job satisfaction and the type of hospitals. The study expects to generate valuable insights for nurses and their employers of different types. It is based on a survey of 100 nurses each from the four most popular types of hospitals – (1) Educational; (2) Government; (3) Charitable Trust; and (4) Private owned.
II. METHODS
The size of the Indian population of nurses is more than 3 million. At a 95 percent confidence interval, the sample size for this population works out to 384, which we rounded off to 400, giving an equal representation of 100 nurses each from the four types of hospitals – educational, government, charitable trust, and private owned. The task of collecting 100 responses for each type of hospital was distributed among the authors. Convenience and purposive sampling method were used. However, to make the study group more inclusive, the sample included nurses from all regions and parts of India – urban, semi-urban, and rural. The questionnaire was administered through Google Forms. The survey was conducted in March 2023. Express written consent for participation was obtained from each respondent.
The study got ethics committee approval number DYP202301, from the Dr.D Y Patil (Deemed to be) University, Pune, India, and Dr.Ajeenkya D Y Patil University, Pune, India.
A scale developed by Chang et al. (2017) to measure the job satisfaction of healthcare workers was largely referred to while designing our scale, which was duly tested for validity and reliability (Cronbach Alpha 0.96). We spoke to a few senior nurses who advised us to consider monetary and compensation factors while assessing the job satisfaction of nurses. Monetary benefits are important for any working human in any part of the world. Studies on job satisfaction (conducted in developed, developing, and underdeveloped countries) include monetary benefits as a parameter. Based on our discussion with the senior nurses and the existing literature, we identified three main factors as determinants of job satisfaction for Indian nurses – monetary and compensation factors, work environment and management support, and job-related factors. monetary and compensation Factors included items like “The salary pay-scales are satisfactory”, “Benefits like provident fund, and gratuity are duly given”, and others. work environment and management support included items like “The management of this organization is supportive of me”, “The management makes changes based on my suggestions and feedback”, and others. job-related factors included items like “I receive the right amount of support and guidance from my direct supervisor”, “I am provided with all trainings necessary for me to perform my job”, and others.
III. RESULTS
Some of the distinctive features of the profile information include a relatively high concentration of respondents in the work experience groups of 10-15 years (158 respondents representing 40 percent of the sample), very low representation of postgraduate educational qualification (10 respondents representing 3 percent of the sample); very low representation of hospitals with a standing of <10 years (11 respondents representing 3 percent of the sample). All these 11 hospitals with a standing of <10 years were private hospitals. The data that support the findings of this study are openly available at https://www.openicpsr.org/ openicpsr/project/190042/version/V1/view (Bhilare, 2023).
A. Descriptive Statistics
Table 1 shows descriptive statistics of the sample.
|
Type |
Total |
Monetary |
Work Env. |
Job related |
||||
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
|
Educational |
-0.22 |
0.86 |
-0.21 |
0.87 |
-0.27 |
0.89 |
-0.19 |
0.90 |
|
Govt. |
-1.55 |
0.40 |
-1.53 |
0.39 |
-1.60 |
0.47 |
-1.54 |
0.44 |
|
Trust |
-1.57 |
0.46 |
-1.51 |
0.47 |
-1.65 |
0.50 |
-1.53 |
0.50 |
|
Private |
0.42 |
0.68 |
0.39 |
0.74 |
0.39 |
0.68 |
0.48 |
0.71 |
|
Total |
-0.73 |
0.60 |
-0.71 |
1.05 |
-0.78 |
1.09 |
-0.70 |
1.09 |
Table 1. Descriptive statistics of the sample
The overall job satisfaction mean scores of the hospitals were -0.22 (0.86) for educational hospitals, -1.55 (0.40) for Government hospitals, -1.57 (0.46) for Trust hospitals, and 0.42 (0.68) for private hospitals. For all the 400 respondents taken together, the mean job satisfaction score was -0.73 (SD 0.60).
In the case of educational hospitals, all three factors of job satisfaction were negative – monetary and compensation factors (M= -0.21, SD 0.87), work environment and management support (M= -0.27, SD 0.89), and Job-related factors (M= -0.19, SD 0.90). The same was the case with government hospitals which reported negative job satisfaction for all three factors – monetary and compensation factors (M= -1.53, SD 0.39), work environment and management support (M= -1.60, SD 0.47), and Job-related factors (M= -1.54, SD 0.44).
Further, charitable trust hospitals too reported negative job satisfaction for all three factors – monetary and compensation factors (M= -1.51, SD 0.47), work environment and management support (M= -1.65, SD 0.50), and job-related factors (M= -1.53, SD 0.50). However, private hospitals were the only type of hospitals that reported positive job satisfaction for all three factors – monetary and compensation factors (M= 0.39, SD 0.74), Work environment and management support (M= 0.39, SD 0.68), and job-related factors (M= 0.48, SD 0.71).
B. Testing of the Hypotheses
Two ANOVA tests were performed. The first one was performed, taking overall job satisfaction as the dependent variable (R2 0.65, p<0.0001). The second ANOVA was performed by taking the monetary and compensation factors (R2 0.62, p<0.0001), work environment and management support (R2 0.64, p<0.0001), and job-related factors (R2 0.64, p<0.0001) as the dependent variables.
IV. DISCUSSION
The overall job satisfaction score of the entire sample size of 400 respondents is -0.73 (SD 0.60), which is close to -1, indicating somewhat dissatisfied. Thus, on an overall basis, Indian nurses have reported job dissatisfaction. An important reason for this is the mismatch between the guidelines of the Nursing Council about the working conditions and the actual working conditions at the various hospitals. The analysis shows that for all the three factors, namely, the Monetary and compensation factors, the work environment and management support factors, and job-related factors the scores are range-bound. This indicates a close relationship between these three factors.
However, when we look at the analysis by the type of hospitals, major variations are seen. Three out of the four types: educational hospitals, government hospitals, and charitable trust hospitals, show negative job satisfaction, whereas only one type, the private owned hospitals, show positive job satisfaction. This is because private hospitals offer a much better and more professional work culture leading to higher job satisfaction among the nurses (Srimulyani & Hermanto, 2022). Interestingly, there is not much difference between the job satisfaction scores of government hospitals and charitable trust hospitals. The standard deviations associated with these two high negative scores are also similar. Scores of government hospitals and charitable trust hospitals can be taken as lying between somewhat dissatisfied and strongly dissatisfied ratings, pointing out a big gap between the prescribed norms of working conditions and the actual working conditions. The score of -0.22 indicates relatively much lesser job dissatisfaction in the case of educational hospitals (as compared to government and charitable trusts). It indicates that the control over educational hospitals is better as compared to the other two types of hospitals. The positive score of 0.42 in the case of private hospitals lies between neutral and somewhat satisfactory pointing a positive and professional work culture.
An important observation that emerges from the analysis is that for each of the four types of hospitals, there is little variation in the three factors of job satisfaction or dissatisfaction. This is because the three factors are closely related to each other.
V. CONCLUSION
Indian nurses, on an overall basis, are somewhat dissatisfied with their jobs. However, when we look into different types of hospitals, it is concluded that nurses working in private hospitals are moderately satisfied, those working in educational hospitals are moderately dissatisfied, and those working in government and charitable trust hospitals are highly dissatisfied. monetary and compensation factors, work environment and management support, and job-related factors impact nurses’ job satisfaction. These factors vary with the type of hospital, and hence it can be concluded that due to variation in these factors depending on the type of hospital, the job satisfaction of nurses varies. This impact is strong on an overall basis, as well as for the three factors (monetary and compensation Factors, work environment and management support, and job-related factors) separately. Interestingly there is a strong correlation among the three factors that we have used for measuring the job satisfaction of nurses. We conclude that positive and relatively higher job satisfaction among nurses working in private hospitals (Srimulyani & Hermanto, 2022) can be attributed to professional working culture, better monetary and compensation factors, better co-worker relationships, and other factors.
Notes on Contributors
Dr. Atul Kumar contributed to the conceptualization of the entire study. Dr. Amol Gawande contributed in designing methods for the study. Dr. Meghana Bhilare contributed to data collection. Dr. Vishal Wadajkar contributed to data analysis. Dr. lndrajit Ghoshal contributed in deducing findings and writing the discussion. Dr. S S Raibagkar contributed in writing the full paper including the conclusion. All the authors have read and approved the final manuscript.
Ethical Approval
The study got ethics committee approval number DYP202301, from the Institutional Review Boards of Dr.D Y Patil (Deemed to be) University, Pune, India, and Dr.Ajeenkya D Y Patil University, Pune, India.
Data Availability
All 400 responses were collated in a data set that has been deposited in a repository and can be accessed at https://www.openicpsr.org/openicpsr/project/190042/version/V1/view
Funding
No external funding was used for the study.
Declaration of Interest
We declare that there is no conflict of interest or competing interest of any sort with any individual or organization.
References
Bhilare, M. (2023). Data set Nurses Job Satisfaction (ICPSR 190042; Version V1) [Data set]. ICPSR. https://www.openicpsr.org/openicpsr/project/190042/version/V1/view
Business Standard. (2021, September 2). India in need of 4.3 mn more nurses by 2024 to meet who norms: Nurse org. Retrieved March 29, 2023, from https://www.business-standard.com/article/ current-affairs/india-in-need-of-4-3-mn-more-nurses-by-2024-to-meet-who-norms-nurse-org-121090201448_1.html
Chang, E., Cohen, J., Koethe, B., Smith, K., & Bir, A. (2017). Measuring job satisfaction among healthcare staff in the United States: a confirmatory factor analysis of the Satisfaction of Employees in Health Care (SEHC) survey. International Journal for Quality in Health Care, 29(2), 262-268. https://doi.org/10.1093/intqhc/mzx012
Rahnavard, F., Sadati, A. K., Hemmati, S., Ebrahimzade, N., Sarikhani, Y., Heydari, S. T., & Lankarani, K. B. (2018). The impact of environmental and demographic factors on nursing job satisfaction. Electronic Physician, 10(4), 6712. https://doi.org/10.19082%2F6712
Srimulyani, V. A., & Hermanto, Y. B. (2022). Organizational culture as a mediator of credible leadership influence on work engagement: empirical studies in private hospitals in East Java, Indonesia. Humanities and Social Sciences Communications, 9(1), Article 274. https://doi.org/10.1057/s41599-022-01289-z
*Shirish S Raibagkar
Savitribai Phule Pune University,
Ganeshkhind, Pune, India
Email: ssrssr696@gmail.com
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









