Harnessing the potential of AI in lifelong learning for medical undergraduates
Submitted: 24 September 2024
Accepted: 3 June 2025
Published online: 7 October, TAPS 2025, 10(4), 81-83
https://doi.org/10.29060/TAPS.2025-10-4/II3527
Nathasha Luke, Shing Chuan Hooi & Celestial T. Yap
Department of Physiology, Yong Loo Ling School of Medicine, National University of Singapore, Singapore
I. INTRODUCTION
Lifelong learning is an essential skill for a successful medical practitioner to keep pace with rapidly advancing medical knowledge and technologies. Artificial intelligence(AI) has a potential in developing and promoting the skill of lifelong learning among medical undergraduates. AI can facilitate adaptive learning, collaborative learning, coaching, and incorporating evidence-based learning in undergraduate education as measures promoting lifelong learning. Users should be aware of the capabilities and limitations of the technology to promote effective incorporation in education. Medical undergraduates should receive a basic AI education to harness its’ potential in the best possible ways in lifelong learning.
Modern-day medical practice is rapidly revolutionising. The increasing content and complexity of medical knowledge are often beyond the human capacity to process and synthesise. A study in 2019 revealed there was an overall 2620% increase in the number of knowledge syntheses published over 20 years, from 1999 to 2019 (Maggio et al., 2020). Medical students and doctors struggle to stay updated with the expanding knowledge and find it difficult to cope with information overload. A successful practitioner should have excellent foundational knowledge, be up-to-date, know when and where to seek additional information, and understand optimal practices in the work environment. Such practitioners will adopt technologies to make their lifelong learning more effective and targeted toward improving patient care.
Artificial intelligence (AI) is at exponential growth, particularly in the field of medicine. AI inventions span across multiple dimensions such as AI-aided diagnostic systems, image interpretation, medical records, patient communication, and community-based care. Future practice environments are likely to be heavily AI-integrated. AI-based knowledge management systems and search engines will streamline the process of practitioners keeping themselves up to date with evolving medicine.
Developing lifelong learning among students is an important domain of medical education, that will them to keep abreast of rapid advances in medicine. Medical schools foster the development of lifelong learning habits through strategies such as (1) adaptive learning (2) collaborative learning (3) coaching and (4) incorporating evidence-based learning into the curriculum. This article focuses on how AI could be harnessed to facilitate and enhance these strategies to inculcate lifelong learning among medical undergraduates.
II. HOW COULD AI ENHANCE THE PROCESS OF ADAPTIVE LEARNING?
Adaptive learning is a process that customises individual learning experiences by determining an individual’s strengths and weaknesses and specifically addressing them. The concept of adaptive learning has become popular in recent years. However, this concept was originally highlighted more than a century ago. In 1912, Edward Thorndike introduced the idea of the learning machine, where the machine could ask questions from the learner and suggest areas that need improvement. With the rise of Generative AI, this concept is coming to reality. Generative AI, which produced content like text, videos and music in response to user prompts, powers adaptive learning tools that assess student knowledge, offer personalised feedback, and pinpoint areas for improvement to help guide their learning process toward mastery (Luke & Hooi, 2024).
Rapid advancements in generative AI have made this technology accessible to many users, allowing learning institutions to customise adaptive AI platforms at a relatively lower cost. Such tools may not only facilitate the learning journey of medical students but also make them strive for continuous feedback-driven improvement as practitioners. In the future, AI-driven adaptive learning may revolutionise continuous professional development (CPD) to pinpoint and address learning gaps, allowing efficient and relevant learning for busy clinicians.
III. WILL AI-DRIVEN LEARNING ENVIRONMENTS PROMOTE COLLABORATION?
Collaboration is defined as the mutual engagement of participants in a coordinated effort to solve the problem together (Roschelle & Teasley, 1995). Collaborative learning by means of peer learning, interdisciplinary learning, and interprofessional learning should be promoted to ensure students develop the skills and confidence to collaborate as clinicians in the future. In clinical environments, doctors learn from each other in both formal and informal ways. This type of learning is particularly important in learning new skills and encourages self-learning behaviours in individuals. In medical school, collaborative learning skills are enhanced through group work, simulations, and collaborative activities among students from different related streams such as medicine, nursing, and pharmacy. These approaches strengthen interprofessional communication, knowledge sharing, and enhance learning.
AI-based virtual reality simulated clinical environments are adopted by multiple medical schools to promote experiential learning. Promoting collaboration should be incorporated as a learning outcome when possible into such simulations. For example, simulations can focus on students’ decision-making skills as what team members are to be activated in a simulated encounter and developing communication skills for effective collaboration. In addition, in the future, AI-based platforms may allow more widespread collaboration crossing boundaries, such as enabling clinicians to find the ‘expert’ to seek opinions on a particular condition, where AI-based systems can facilitate collaboration.
IV. COACHING FOR LIFE-LONG LEARNING – CAN AI DO THIS?
Coaching is a development process that enables a person to identify and enhance their own capabilities to reach personal and professional goals. This process has been demonstrated to be beneficial for students in educational settings (Breslin et al., 2023). How does coaching promote lifelong learning? Coaching, which allows the person to learn about self, enables one to identify own impediments towards learning. This will enhance behaviours facilitating learning. AI coaching or virtual coaching is now being explored. The advantages of AI coaching are accessibility, lack of bias, and convenience. Human coaching is still believed to be superior due to the aspects of the ability to express empathy, pick up non-verbal cues during conversation, and be more adaptive. Though the current technology of AI is unable to surpass an experienced human coach (Terblanche et al., 2022), these hurdles may be overcome with future advancements of the technology.
V. EMPHASISE EVIDENCE-BASED APPROACHES WITHIN THE CURRICULUM
Reading journals, critically appraising relevant publications, and adopting them in one’s own practice are essential elements of the lifelong learning process for doctors, which should be developed from undergraduate days themselves. The main hurdle for such incorporations is the tight schedule within the curriculum and the content load. Despite traditional teaching being replaced by integrated teaching, the content load covered within the curriculum remains substantial. The depth and breadth of the content taught in medical school have not proportionately evolved over the years, despite major changes happening in clinical environments with AI integration. AI acts as an instant source of knowledge, aiding clinical decision-making and patient care. Bearing this in mind, educators should revise their curricula to reduce the depth of certain elements that could be easily retrieved digitally. However, students should have a sound knowledge on foundational principles on which advanced concepts can build on.
Re-evaluating the curriculum to reduce the content load would free more time in the schedule to promote critical appraisal of scientific literature, enabling students to wisely use scientific literature to stay up to date. A thoughtful and pragmatic approach to curriculum revaluation for lifelong learning involves embedding core competencies such as critical thinking, adaptability, self-directed learning, and interdisciplinary collaboration instead of overloading content.
VI. EQUIP UNDERGRADUATES WITH BASIC AI KNOWLEDGE AND SKILLS
Some medical schools, including NUS Medicine, have incorporated AI into the curricula. Exposing medical undergraduates to the foundations of AI technology can help them foresee the revolutionisation of future practice and equip themselves to embrace the technology. In addition, this will enable them to pursue new career pathways combining AI and Medicine. With regards to lifelong learning, clinicians may be equipped with AI-based tools to learn from real-time patient data for clinical decision-making, rather than waiting for prospective clinical trials or research. For example, students with foundational knowledge of AI will be able to use AI analytical skills to draw conclusions based on real-time and latest clinical data, as well as to detect trends of emerging diseases and antibiotic resistance, promoting early intervention.
Equipping future generations with AI knowledge will improve the quality of care and reduce diagnostic errors. Also, AI knowledge will guide practitioners to remain vigilant about data privacy and algorithmic bias when using AI. A future-ready curriculum will not only prepare students to use AI responsibly but also to question and enhance the tools.
AI comes with challenges and opportunities. The risk of bias, data quality and security issues, risk of over-reliance, AI relying on historical rather than real-time data, and lack of transparency in decision-making processes are some of the limitations. Still, AI has a vast potential to augment healthcare and health professions’ education as discussed above. AI should augment clinical decision making, and not replace. Ethical considerations, including patient consent, data security, and accountability, must remain central to any AI integration in healthcare practice.
In summary, AI has huge potential to enhance the strategies implemented in medical education to promote lifelong learning in medical undergraduates. The users should be aware of the limitations of the technology, and incorporate it cautiously to harness the maximum benefit of the technology in the process of transforming our undergraduates to better clinicians and lifelong learners.
Notes on Contributors
NL conceptualised the article, created the first draft, and revised subsequent versions. In addition, approved the final version of the article for submission.
HSC conceptualised the article, revised the draft versions, and approved the final version of the article for submission.
CTY conceptualised the article, revised the draft versions, and approved the final version of the article for submission.
Funding
We did not receive any funding for this publication.
Declaration of Interest
We do not have any conflicts of interest, including financial, consultant, institutional, or other relationships that might lead to bias or a conflict of interest.
References
Luke, W. N. V., & Hooi, S. C. (2024). The role of artificial intelligence in knowledge management for medical students and doctors. Medical Teacher, 1–2. https://doi.org/10.1080/0142159x.2024.2336065
Maggio, L. A., Costello, J. A., Norton, C., Driessen, E. W., & Artino, A. R., Jr. (2020). Knowledge syntheses in medical education: A bibliometric analysis. Perspectives on Medical Education, 10(2), 79–87. https://doi.org/10.1007/s40037-020-00626-9
Roschelle, J., & Teasley, S. D. (1995). The construction of shared knowledge in collaborative problem solving (pp. 69–97). Springer eBooks. https://doi.org/10.1007/978-3-642-85098-1_5
Terblanche, N., Molyn, J., De Haan, E., & Nilsson, V. O. (2022). Comparing artificial intelligence and human coaching goal attainment efficacy. PLoS ONE, 17(6), e0270255. https://doi.org/10.1371/journal.pone.0270255
*Nathasha Luke
2 Medical Drive, MD 9,
National University of Singapore, 117593
+6596204104, +6566013506
Email: nathasha@nus.edu.sg
Submitted: 6 February 2025
Accepted: 14 May 2025
Published online: 7 October, TAPS 2025, 10(4), 94-96
https://doi.org/10.29060/TAPS.2025-10-4/II3664
Charlene Tan1 & Ruth Neo2
1College of Arts, Humanities and Languages, Life University, Cambodia; 2UNSW Medicine & Health, University of New South Wales, Australia
I. INTRODUCTION
This article proposes a Chinese philosophical approach to well-being for medical education by drawing on the thought of Mencius (372-289 B.C.E.). As it is not possible to cover all areas of Mencius’ philosophy within this short essay, our focus is on Mencius’ idea of interpersonal joy, as recorded in the classic Mengzi. This paper shall explain how interpersonal joy, from a Mencian perspective, centres on the shared delight from benefiting others while cultivating personal virtue.
II. MENCIUS ON WELL-BEING AND INTERPERSONAL JOY
Well-being is used synonymously or in conjunction with related terms such as welfare, happiness, prudential value, the good life, prudential good life, quality of life, flourishing, self-interest, fulfilment, utility and pastoral care (Fletcher, 2016). Mencius’ approach to well-being is encapsulated in his idea of interpersonal joy, which harmonises personal and communal delight. A representative passage is 7A20.1 in the Mengzi:
Mengzi said, “An exemplary person [Junzi] takes joy in three things, and being King of the world is not one of them. The person’s first joy is that one’s parents are both alive and one’s siblings have no difficulties. The second joy is that looking up one is not disgraced before Heaven, and looking down on one is not ashamed before humans. The third joy is getting assistance and cultivating the brave and talented people of the world. An exemplary person takes joy in three things, and being King of the world is not one of them (Van Norden, 2008, p. 176).
This passage is about a Junzi which literally means ‘son of a noble’. Confucius appropriated this historical term and infused it with moral import, thereby changing its meaning to denote an exemplary person. That the exemplary person embodies Confucian well-being is evidenced by passages in the Mengzi that describe such a person as having “no anxieties” (4B28.7) and experiencing “joy” (7A20.1, 7A21.2).
With respect to 7A20.1, the passage begins by stating that an exemplary person does not derive joy from being King of the world. Mencius is not asserting that holding political power is wrong or detrimental to one’s well-being. On the contrary, he acknowledges in the next passage that an exemplary person, like all rulers, “desires a large territory and numerous people” (7A21.1). Mencius’ point is that Kingship, in itself, does not give satisfaction to an exemplary person; instead, such a person “takes joy in taking one’s place in the middle of the world and making all the people within the Four Seas settled” (7A21.1) (Van Norden, 2008, p. 176). We see here how an exemplary person obtains personal joy by bringing joy to others (“making all the people within the Four Seas settled”).
All people can become exemplary people by developing the four sprouts within them, namely the mind-and-heart of compassion, the shame of evil in oneself and hatred of evil in others, humility and deference, and right and wrong (2A.6). These four sprouts, when consistently cultivated, will grow into the virtues of benevolence, propriety, righteousness and wisdom, all of which contribute to interpersonal joy. Retuning to 7A20.1, Mencius’ message is that an exemplary person does not obtain pleasures and life satisfaction from prudential desires, which are manifested in egoistic ambitions with little regard for others. Instead, joy is felt when a person immerses oneself in social interactions and builds strong connections with others. An exemplary person also derives delight by treating others well and developing their potential for the common good. The end result is “making all the people within the Four Seas settled” (7A21.1) (Van Norden, 2008, p. 176).
To sum up, Mencian well-being is indicated by interpersonal joy which integrates individual and collective happiness, as demonstrated by the exemplary person. Communal joy engenders collective well-being, illustrated by the King “sharing the same delight as the people” (1B1.4) (Van Norden, 2008, p. 16).
III. RECOMMENDATIONS FOR MEDICAL EDUCATION
A major implication of Mencian well-being is for medical schools to promote interpersonal joy in the curriculum and assessment. Two suggestions are elaborated in this section: a shift from summative assessment and competition to formative assessment and collaboration; and the introduction of a wellness curriculum that pivots on interpersonal joy.
First, medical schools need to review their curriculum and assessment so as to remove any hindrances to the realisation of interpersonal joy in their students. A specific recommendation is to replace summative assessment and competition with formative assessment and collaboration. Mencius’ call for collective well-being is difficult to achieve if students are fixated with outperforming one another due to the pressures of high-stakes exams. Kachel et al. (2020) report that “during medical school interpersonal skills linked to being an active member of an institution are underrepresented in curricula” (p. 11). It is a challenge for medical students to care for the well-being of others and be open about their mental health needs if they are circumscribed by a culture of competition, distrust and judgement (Canadian Federation of Medical Students, 2021). Cooperation and interdependence can be enhanced by reducing or removing pen-and-paper examination and norm-referenced assessments, and introducing (more) collaborative projects and criterion-referenced assessments. The assessment mode for the cultivation of interpersonal joy should be formative, where students are given continuous feedback and find enjoyment in learning and sharing.
A pedagogical approach to foster interpersonal joy is group projects, where students collaborate for shared success. Anchored upon the principles of cooperation and harmony, group projects foreground interpersonal joy and competencies that are underrepresented in the curricula (Kachel et al., 2020). Termly group projects nurture communication and teamwork skills, spanning a wide range of topics from the basic clinical sciences to medical ethics and public health. The group projects can be evaluated via negotiated assignment, where students develop their own research questions and set their own assessment criteria that are aligned with the course themes. The goal is to foster student-driven learning that gives students the opportunity to explore common topics of interest beyond the confines of standard, end-of-course examinations. A related pedagogical approach is encouraging students to participate in service learning, community involvement as well as local and overseas volunteer projects, so as to generate communal interactions and bonding. By serving others, the students’ sprout of compassion is cultivated and manifested through empathy, beneficence and concern for others (Van Norden, 2008).
The second recommendation is for medical schools to enact a wellness curriculum that pivots on interpersonal joy. Medical schools could adapt the wellness curriculum for medical students in a Canadian university; students there were asked to “define their core values and beliefs while respecting those of others, and apply them in the context of their developing physician identity and that of the medical profession” (Canadian Federation of Medical Students, 2021, p. 22). Mencian ideas can be integrated into the before-mentioned wellness curriculum through reflective questions such as: What does an exemplary person (junzi) mean to me? How can Mencian interpersonal joy be part of my core values as a medical professional? How can I obtain interpersonal joy through interacting with and serving others? The self-reflection activity can be undertaken in various formats such as group discussions, journalling and multi-media presentations.
Mencian ideas of well-being and related suggestions may face challenges in medical schools where individualism and competition are often culturally entrenched. In this regard, Mencian well-being may be more appropriate for medical education in Confucian heritage cultures. Significantly, studies have shown that Asian adolescents experience a strong sense of well-being when they partake in collective activities; in contrast, adolescents in Anglo-American societies typically enjoy higher well-being when they engage in more individualistic activities (Chue, 2023). Relatedly, Mencian well-being’s focus on moral cultivation sets it apart from two dominant models in Anglophone societies, namely Seligman’s PERMA (Positive emotions, Engagement, Relationships, Meaning & Accomplishment) and Ryff’s six aspects of psychological well-being, which are autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self-acceptance. As noted earlier, Mencius advocates for the development of our innate goodness in the form of the four sprouts, which in turn contributes to interpersonal joy. In contrast, the theories of Seligman and Ryff generally de-emphasise moral education.
In individualistic societies, interpersonal joy can complement the existing wellness frameworks by underscoring collaborative learning, such as group projects and service learning (Bourcier et al., 2021). Staff development is also critical, where faculty members are introduced to Mencian principles and practical ways to promote them, such as organising service learning and designing wellness curricula. Ultimately, the successful implementation of interpersonal joy necessitates faculty development, which should be strategically incorporated into the staff training programmes (Canadian Federation of Medical Students, 2021).
IV. CONCLUSION
Mencius’ approach to well-being is encapsulated in his idea of interpersonal joy, which harmonises personal and communal delight. Mencian well-being supports collective well-being by twinning self-interests and other interests. This paper has also suggested that medical schools revamp the curriculum and assessment modes to shift from summative assessment and competition to formative assessment and collaboration. Medical schools should also explore pedagogical methods that incorporate Mencian idea of interpersonal joy into the curriculum.
Notes on Contributors
Charlene Tan conceptualised the topic, provided philosophical ideas and drafted the manuscript. Ruth Neo gave inputs that pertained to medical student well-being and co-drafted the manuscript.
Ethical Approval
Ethical approval is not relevant as this is a conceptual paper that does not involve human participants and/or animals.
Acknowledgement
The authors thank the anonymous reviewers for valuable suggestions to earlier drafts.
Funding
The authors did not receive support from any organisation for the submitted work.
Declaration of Interest
No potential competing interest was reported by the authors. The authors have no relevant financial or non-financial interests to disclose.
References
Canadian Federation of Medical Students. (2021). Canadian federation of medical students wellness curriculum framework. https://www.cfms.org/files/wellness-resources/CFMS-Wellness-Curriculum-Framework_FINAL.pdf
Chue, K. L. (2023). Cultural issues in measuring flourishing of adolescents. In R. B. King, I. S. Caleon, & A. B. I. Bernardo (Eds.), Positive psychology and positive education in Asia: Understanding and fostering well-being in schools (pp. 329-342). Springer.
Fletcher, G. (Ed.). (2016). The Routledge handbook of philosophy of well-being. Routledge.
Kachel, T., Huber, A., Strecker, C., Höge, T., & Höfer, S. (2020). Development of cynicism in medical students: Exploring the role of signature character strengths and well-being. Frontiers in Psychology, 11(328), 1-16. https://doi.org/10.3389/fpsyg.2020.00328
Van Norden, B. W. (2008). Mengzi. With selections from traditional commentaries. Hackett Publishing Company, Inc.
*Charlene Tan
Life University, Phreah Sihanouk,
Sihanoukville, Cambodia
Email: chptan@u.nus.edu
Submitted: 18 November 2024
Accepted: 14 May 2025
Published online: 7 October, TAPS 2025, 10(4), 5-25
https://doi.org/10.29060/TAPS.2025-10-4/RA3572
Matthew Jian Wen Low1, Han Ting Jillian Yeo2, Dujeepa D. Samarasekera2, Gene Wai Han Chan1 & Lee Shuh Shing2
1Department of Emergency Medicine, National University Hospital, Singapore; 2Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Abstract
Introduction: Effective and actionable instructional design features improve return on investment in Technology enhanced simulation (TES). Previous reviews on instructional design features for TES that improve clinical outcomes covered studies up to 2011, but updated, consolidated guidance has been lacking since then. This review aims to provide such updated guidance to inform educators and researchers.
Methods: A narrative review was conducted on instructional design features in TES in medical education. Original research articles published between 2011 to 2022 that examined outcomes at Kirkpatrick level three and above were included.
Results: A total of 30,491 citations were identified. After screening, 31 articles were included in this review. Most instructional design features had a limited evidence base with only one to four studies each, except 11 studies for simulator modality. Improved outcomes were observed with error management training, distributed practice, dyad training, and in situ training. Mixed results were seen with different simulation modalities, isolated components of mastery learning, just-in-time training, and part versus whole task practice.
Conclusion: There is limited evidence for instructional design features in TES that improve clinical outcomes. Within these limits, error management training, distributed practice, dyad training, and in situ training appear beneficial. Further research is needed to assess the effectiveness and generalisability of these features.
Keywords: Simulation, Instructional Design, Clinical Outcomes, Review
Practice Highlights
- This review pinpoints additional beneficial instructional design features emerging since 2011.
- These include error management training, distributed practice, dyad training, and in situ training.
- Further evidence from diverse task and learner contexts is needed to establish generalisability.
- Current evidence continues to suggest no clear superiority of one simulator modality over the other.
I. INTRODUCTION
Technology enhanced simulation (TES) training has been shown to be effective for skills, behaviour, and patient-related outcomes (Cook et al., 2011; McGaghie et al., 2011). Instructional design features in simulation refer to variations in aspects of simulation design that act as active ingredients or mechanisms that make simulation effective, with examples including distributed practice, mastery learning, and range of difficulty (Cook, Hamstra, et al., 2013). Effective instructional design features for TES are actionable for educators because they offer specific, implementable guidance, and an area of research interest (Issenberg et al., 2005; Nestel et al., 2011; Schaefer et al., 2011), including those that lead to transfer to authentic clinical practice (Frerejean et al., 2023; Zendejas et al., 2013).
While it is acknowledged that conducting a study to establish a causal relationship between an educational intervention and subsequent patient and clinical process outcomes is challenging (Cook & West, 2013), such studies become particularly valuable when appropriately executed (Dauphinee, 2012). These studies represent the apex of impact in Kirkpatrick’s model for program evaluation (Kirkpatrick & Kirkpatrick, 2006), holding the highest clinical significance and representing the ultimate goal of health professions education which is to enhance patient outcomes by equipping the healthcare workforce to effectively address societal needs (Carraccio et al., 2016). Additionally, the examination of clinical outcomes, when coupled with a consideration of costs, contributes to the informed allocation of limited institutional resources to such educational approaches (Lin et al., 2018).
In prior reviews of TES including studies up to 2011, the vast majority of studies examined outcomes at the levels of reaction and learning demonstrated in written or simulation tests, with only a small body of evidence studying outcomes in workplace contexts (Cook, Hamstra, et al., 2013; Nestel et al., 2011; Zendejas et al., 2013) suggesting that clinical variation, multiple learning strategies, and increased time learning are beneficial variations. This limited evidence base for transfer to workplace contexts hinders educators in fully harnessing the potential of TES to improve patient and system outcomes and obtain the best returns on investments in simulation technology. Given the time interval since these prior reviews, further evidence would have accrued regarding these and other instructional design features.
Given the time elapsed since the last comprehensive review of TES instructional design features, the scarcity of prior studies on clinical outcomes, and the importance of these outcomes, we conducted this narrative review. The objective was to provide an updated understanding of the instructional design features in TES that are associated with enhanced clinical outcomes, thereby addressing a significant gap in the existing literature, to guide educators seeking to optimise instructional design, and provide researchers with an overview of the current state of this literature and guide further inquiry.
II. METHODS
We conducted a narrative review based on the framework proposed by Ferrari (2015). We searched MEDLINE, ERIC, Embase, Scopus and Web of Science databases for articles published from 2012 January 01 to 2022 December 06. We translated abstracts and articles not in English into English using Google Translate.
The following search terms were used: (Medical education) AND (Simulation OR Cadaver OR Simulator OR Augmented Reality OR Virtual reality OR Mixed reality).
Studies were included if they were original research articles examining instructional design variations in TES with at least one outcome at Kirkpatrick levels three or above, as described and utilised by the Best Evidence Medical Education Collaboration (Steinert et al., 2006). We included a broad range of TES modalities, such as computer based virtual reality simulators, high fidelity and static mannequins, plastic models, live animals, inert animal products, and human cadavers as stipulated in the review by Cook et al. (2011). We included augmented reality and mixed reality as they satisfied the prior definition of “materials and devices created or adapted to solve practical problems” in simulation established by Cook et al (2011). Studies where TES was utilised together with human patient actors were included. We included studies with observational, experimental, and qualitative designs.
Studies were excluded if they involved only human patient actors as the sole modality of simulation, used simulation outside of health professions education, used simulation for noneducation purposes such as procedural planning or patient education, or only compared simulation with no simulation. We excluded studies involving only nurses given that there are recent and ongoing reviews addressing a similar research question (El Hussein & Cuncannon, 2022; Jackson et al., 2022), but included interprofessional studies. Figure 1 shows the flow of studies through the review and selection process.
Three researchers (MJWL, SSL, JHTY) independently read the full text of articles that met the inclusion criteria and extracted study information including geographical origin, specialty context, type of skill studied, level of the learner, simulation modalities used, instructional design variations studied, and outcomes categorised into the highest Kirkpatrick level studied. Any differences were resolved by a discussion among researchers to arrive at a consensus.
III. RESULTS
A total of 30,491 records were identified using the search strategy. From these, 31 eligible studies were identified and reviewed (Figure 1 and Table 1). Figure 2 summarises basic information on these studies. The number of studies from each geographic region were 13 from North America (42%), 11 from Europe (35%), three from Asia (10%), two from Africa (6%), and one from South America (3%). One study did not clearly state the countries involved.
28 out of 31 (90%) of the studies adopted a quantitative research design focusing on experimental design. Most simulation interventions were conducted among residents/fellows/interns, followed by medical students.
The results reported in the studies are divided into two groups:
- Evidence suggests improved outcomes
- Evidence shows mixed results
A. Improved Outcomes
Error management training was associated with improved obstetric ultrasound skills compared to error avoidance training in novices (Dyre et al., 2017). Frequent brief on-site simulation, at 40 minutes a month and three minutes a week, was associated with reduced infant mortality compared to a single day course (Mduma et al., 2015). Integrating non-technical skills (NTS) training into a colonoscopy skills curriculum with TES, without increasing time spent teaching, improved observed performance during colonoscopies on real patients, although it was unclear whether this was driven by changes in observed NTS only, or both NTS and technical skills (Walsh et al., 2020).
One qualitative study found that in situ training had greater organisational impact and provided more information for practical organisational changes (Sørensen et al., 2015). One qualitative study found that multi-professional training led to improved communication, leadership, and clinical management of post-partum haemorrhage (Egenberg et al., 2017).
1. Dyad Training
In one study of obstetric ultrasound skills (Tolsgaard et al., 2015) a larger proportion of the dyad training group (71%) scored above the criterion referenced pass fail level than the individual training group (30%) on the objective structured assessment of ultrasound skills, though the difference in mean scores on did not reach statistical significance. Other benefits included increased efficiency from greater faculty to learner ratios.
2. Complex Bundles
Three studies found improvements with complex bundles comprising multiple instructional design variations.
Medical students performed the correct sequence of steps for endotracheal intubation measured by a checklist more often when practice with a mannequin was augmented by a 10-question pre-test, hand held tablets containing scenarios, checklists, and learning algorithms, 24-hour access to the simulation laboratory, and remote review of practice recordings with feedback from teachers via email (Mankute et al., 2022).
Residents had improved observed performance in laparoscopic salpingectomy with lectures, videos, reading materials, a box trainer with pre-set proficiency benchmarks, a VR simulator for technical skills, and non-technical skills training with scripted confederates, compared to a conventional curriculum including simulation with minimal further description (Shore et al., 2016).
In one qualitative study of obstetric residents, there was improved transfer of communication and team work skills and situational awareness with simulation aligned to multiple principles including authenticity, psychological fidelity, engineering fidelity, Paivio’s dual coding, feedback, variability, and increasing complexity (de Melo et al., 2018).
B. Mixed Results
1. Simulation Modality
Eleven studies examined whether outcomes differed when different simulation modalities were used. Examples include higher versus lower technological complexity in a physical simulator (DeStephano et al., 2015; Sharara-Chami et al., 2014), cadaveric versus synthetic models (Lal et al., 2022; Tan et al., 2018; Tchorz et al., 2015), virtual reality (VR) versus physical simulators (Daly et al., 2013; Gomez et al., 2015; Orzech et al., 2012; O’Sullivan et al., 2014), and a computer based versus physical simulated operating room for student orientation (Patel et al., 2012).
Overall, there no clear pattern of superiority of a particular type of simulator. Most studies found no difference, with three exceptions: Gomez et al (2012) found that VR alone, and VR with physical simulator, led to superior performance in observed colonoscopic skills in real patients, compared to physical simulator alone; Chunharas et al (2013) found that adding practice on fellow students on top of mannequin practice improved observed performance in subcutaneous and intramuscular injection skills; Patel et al (2012) found that using a physical simulated operating room was superior to an online computer based operating room for training novice medical students in appropriate behaviour in the operating room.
To view Table 1 click here.
Abbreviations. ACS/APDS: American College of Surgeons / Association of Program Directors in Surgery; EAT: Error avoidance training; EMT: Error management training; GAGES-C: Global Assessment of Gastrointestinal Endoscopic Skills-Colonoscopy; GOALS: Global Operative Assessment of Laparoscopic Skills; ISS: In situ simulation; JAG DOPS: Joint Advisory Group Direct Observation of Procedural Skills; JIT: Just in time; OSA-LS: objective structured assessment of laparoscopic salpingectomy; NTS: Non-technical skills. OSAUS: objective structured assessment of ultrasound; OSS: Off-site simulation; PGY: Post graduate year; UK: United Kingdom; USA: United States of America; VR: Virtual reality.
Kirkpatrick levels. 1: Reaction e.g. participants’ views on learning experience; 2a: Learning – Change in attitudes; 2b: Learning – Modification of knowledge or skills; 3: Behaviour – Change in behaviours; 4a: Results – Change in the system/organisational practice; 4b: Results – Change in patient outcomes.
Table 1. List of included studies and skills, instructional design variations and outcomes examined
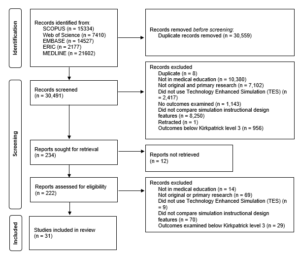
Figure 1. Flow of studies through identification process
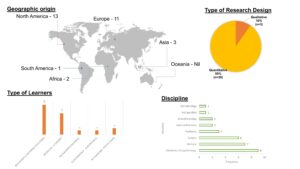
Figure 2. Summary of geographical origin, type of research, type of learners and disciplines studied
2. Components of Mastery Learning
Four studies examined components of mastery learning, such as progressive task difficulty and proficiency-based progression. Progressive task difficulty for TES was associated with improved rater observed colonoscopic performance on real patients (Grover et al., 2017), while the evidence was mixed for proficiency-based progression for TES, with studies finding reduced epidural failure rates (Srinivasan et al., 2018) and fewer adverse events in laparoscopic cholecystectomy (De Win et al., 2016), while another found no difference in operative performance for bowel anastomosis in real patients (Naples et al., 2022).
3. Part Versus Whole Task
Two studies compared part versus whole task training. Both found no difference, in rater observed performance in laparoscopic inguinal hernia repair (Hernández-Irizarry et al., 2016), and intraoperative camera navigation skills (Nilsson et al., 2017), though randomised part task training led to faster skills mastery with greater cost effectiveness compared to whole task training.
4. Increased Time Spent in Simulation Training
Two studies examined amount of time spent in simulation training. One study showed reduced incidence of malpractice claims (Schaffer et al., 2021), while another study found no difference in successful deep biliary cannulation during endoscopic retrograde cholangiopancreatography (Liao et al., 2013).
5. Just in Time (JIT) Training
Overall, there was mostly no benefit seen with JIT training with TES, across three studies. One study examined the addition of JIT video after prior TES (Todsen et al., 2013), and one study compared JIT practice alone, JIT practice with feedback from this practice, and feedback alone derived from baseline testing (Kroft et al., 2017). JIT and just-in-place physical simulator training did not improve first pass lumbar puncture success, but improved mean number of attempts and process measures such as early stylet removal (Kessler et al., 2015).
IV. DISCUSSION
We sought to provide an updated synthesis on effective instructional design features in simulation in medical education, focusing on those that produce higher level outcomes at Kirkpatrick levels three and above. A prior review searching until 2011 identified only 18 studies that examined outcomes at Kirkpatrick level three and above, out of their pool of 10,297 studies. Our review reveals a notable rise in the number of studies over the past ten years, exploring instructional design and clinical outcomes. In the discussion that follows, we synthesise the findings with existing literature and theory to extract valuable insights for medical educators.
A. Implications for Current Practice
This review underscores the necessity of directing resources towards effective instructional design features, emphasising that these need not be strictly tied to specific simulator types, as advocated by Norman. Despite the ongoing evolution and incorporation of an expanding array of TES modalities, including Virtual Reality (VR) in this review, we observed mixed results concerning simulation modality as an instructional design variation. Upon closer examination of interventions outlined in studies comparing simulation modalities, it becomes evident that confounding factors may arise due to variations in the application of training to proficiency criteria (a characteristic of mastery learning) or differences in the quality of measurement.
In the study conducted by Gomez et al (2015), training to proficiency criteria was incorporated in study arms demonstrating benefit (VR and VR plus physical simulator) and not incorporated in the remaining arm (physical simulator alone). Similarly, in the study by Orzech et al (2012) where training until proficiency criteria were reached was a shared feature of both arms, no significant difference between groups was observed. It remains unclear whether observed differences were attributable to the application of training until proficiency criteria were met or to the varied simulation modalities.
Chunharas et al (2013) and Patel et al (2012) also noted outcome differences when comparing different simulation modalities. However, the robustness of these findings is constrained using a checklist observation scale developed for individual studies with minimal validity evidence. Clinical and task variations, recognised as beneficial in prior reviews (Zendejas et al., 2013), may elucidate the advantages identified by Chunharas et al and the VR plus physical simulator arm in the study by Gomez et al.
Components of mastery learning appear mostly effective, although isolated implementation of a component without the whole may erode effectiveness. The inconsistent evidence for effectiveness of components of mastery learning in this review is surprising, given prior evidence for the effectiveness of mastery learning for translational outcomes (Griswold-Theodorson et al., 2015). The difference may lie in piecemeal rather than holistic implementation of mastery learning as a complex intervention, with seven complementary components working together (McGaghie, 2015).
Another difference is that our review only included studies comparing different TES interventions, while the review by Griswold-Theodorson et al included studies that compared mastery learning with a wider range of comparators, including no TES. Notably, a separate systematic review and meta-analysis of mastery learning found only three studies from 1984-2010 comparing mastery learning to other TES interventions for patient outcomes, with no statistically significant benefit overall and substantial heterogeneity (Cook, Brydges, et al., 2013).
Methodological issues may be another contributory factor. Naples et al (2022) postulate in their study the reasons for the lack of observed difference, including a long duration between intervention and outcome assessment, which was longer in the intervention group than the control group, biasing towards the null, and surprisingly high baseline performance with an insufficiently sensitive rater observation tool. This study had only nine participants, limiting statistical power. These represent important methodological considerations for researchers designing educational intervention studies.
The effectiveness of increased time spent in simulation training is associated with incorporation of learning conversations. Discrepancies in outcomes between the two studies assessing the impact of time spent in simulation training may be attributed to the presence of debriefing in the study conducted by Schaffer et al (2021), as opposed to un-coached practice without feedback in the study by Liao et al (2013). It is crucial to note that the advantages derived from extended training periods are not solely attributed to prolonged duration but are also influenced by the integration of learning conversations. These conversations encompass both debriefing and feedback (Tavares et al., 2020), both of which have demonstrated efficacy, as supported by existing research (Cheng et al., 2014; Hattie & Timperley, 2007).
In a systematic review by Hatala and colleagues (Hatala et al., 2014), feedback emerged as moderately effective for procedural skills simulation training. Notably, feedback from multiple sources, including instructors, proved more effective than feedback from a single source.
Distributed practice is preferred over blocked practice for TES. Frequent brief simulation (Mduma et al., 2015) essentially describes distributed rather than blocked practice. The increased effectiveness seen with distributed practice here is consistent with existing literature within (Cecilio-Fernandes et al., 2023) and outside (Dunlosky et al., 2013) of health professions education.
Dyad training is notable for being efficient with similar or better outcomes, and is consistent with existing literature on motor skills learning (Wulf et al., 2010). The optimal group size has not been clearly determined, beyond single versus dyad, and would be a productive avenue of inquiry for evidence-based determination of learner to faculty ratios, accounting for contextual factors such as task complexity and stage of learner’s development.
In situ simulation may be beneficial in generating participant insights that feed into systems-based improvements through quality improvement mechanisms (Calhoun et al., 2024; Nickson et al., 2021). This combines multiple mechanisms by which TES can produce meaningful impact: through changing individual learner behaviour and changing systems processes.
Error management training appears beneficial for transfer outcomes in novices. This is congruent with literature outside of medical education (Keith & Frese, 2008). The limited evidence base within medical education makes this ripe for further study across task and learner types.
In summary, the features mentioned above are predominantly drawn from previous studies, primarily conducted at Kirkpatrick level two. This review contributes by offering an updated synthesis of evidence, outlining the extent to which this evidence can be extrapolated to higher Kirkpatrick levels, and highlighting features that were previously unexplored at clinical process and outcome levels. Collectively, evidence spanning these levels serves as a guide for those designing TES with the goal of achieving educational and clinical impact.
B. Limitations and Implications for Future Research
Studies that examine Kirkpatrick levels three and above continue to constitute a relatively small fraction of the overall research landscape. Furthermore, this limited body of research is dispersed among various instructional design features, with only a small number of studies investigating each specific feature. Consequently, drawing definitive conclusions about effectiveness becomes challenging, representing a primary constraint of this review. Despite these limitations, we have tried to extract valuable insights for health professions educators by synthesising the findings with existing literature and theory.
The limited evidence bases for most individual instructional design features, especially those demonstrating benefits at Kirkpatrick levels three and four, limits the strength of conclusions that can be drawn about their effectiveness. Further studies replicating these results would strengthen the argument that a particular instructional design feature is able to achieve clinical impact. The evidence base is also limited in the variety of task and learner contexts studied for each individual instructional design feature. Determining the generalisability of these findings requires further research applying these features across diverse TES contexts with different skills and learner groups. Future research should also continue to explore novel and promising instructional design features, such as hybrid simulations where mannequins are overlayed with animal tissue or gel-based phantoms (Balakrishnan et al., 2025).
V. CONCLUSION
There is limited evidence for instructional design features in TES that translate to improved clinical outcomes. Within these limits, error management training, distributed practice, dyad training, and in situ training appear beneficial. Given the limited evidence base for these individual features, definitive determination of effectiveness and generalisability requires further research applying promising target features across different task and learner contexts.
Notes on Contributors
Matthew Low is an emergency physician at National University Hospital, Singapore, and adjunct assistant professor at the Yong Loo Lin School of Medicine, National University of Singapore.
Jillian Yeo is a medical educationalist at the Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore.
Dujeepa Samarasekera is senior director at the Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore.
Gene Chan is an emergency physician at National University Hospital, Singapore, and adjunct assistant professor at the Yong Loo Lin School of Medicine, National University of Singapore.
Shuh Shing Lee is a medical educationalist at the Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore.
Matthew Low, Jillian Yeo and Shuh Shing Lee conceived of the work, collected and analysed data, and drafted the work. Gene Chan and Dujeepa Samarasekera conceived of the work and reviewed it critically for important intellectual content. All contributors gave final approval of the version to be published and are agreeable to be accountable for all aspects of the work.
Ethical Approval
Ethical approval was not applicable as this is a review paper.
Funding
There was no funding for this paper.
Declaration of Interest
The authors report no conflicts of interest.
References
Balakrishnan, A., Law, L. S.-C., Areti, A., Burckett-St Laurent, D., Zuercher, R. O., Chin, K.-J., & Ramlogan, R. (2025). Educational outcomes of simulation-based training in regional anaesthesia: A scoping review. British Journal of Anaesthesia, 134(2), 523–534. https://doi.org/10.1016/j.bja.2024.07.037
Calhoun, A. W., Cook, D. A., Genova, G., Motamedi, S. M. K., Waseem, M., Carey, R., Hanson, A., Chan, J. C. K., Camacho, C., Harwayne-Gidansky, I., Walsh, B., White, M., Geis, G., Monachino, A. M., Maa, T., Posner, G., Li, D. L., & Lin, Y. (2024). Educational and patient care impacts of in situ simulation in healthcare: A systematic review. Simulation in Healthcare, 19(1S), S23–S31. https://doi.org/10.1097/SIH.0000000000000773
Carraccio, C., Englander, R., Van Melle, E., Ten Cate, O., Lockyer, J., Chan, M.-K., Frank, J. R., Snell, L. S., & International Competency-Based Medical Education Collaborators. (2016). Advancing competency-based medical education: A charter for clinician-educators. Academic Medicine, 91(5), 645–649. https://doi.org/10.1097/ACM.0000000000001048
Cecilio-Fernandes, D., Patel, R., & Sandars, J. (2023). Using insights from cognitive science for the teaching of clinical skills: AMEE Guide No. 155. Medical Teacher, 45(11), 1214–1223. https://doi.org/10.1080/0142159X.2023.2168528
Cheng, A., Eppich, W., Grant, V., Sherbino, J., Zendejas, B., & Cook, D. A. (2014). Debriefing for technology-enhanced simulation: A systematic review and meta-analysis. Medical Education, 48(7), 657–666. https://doi.org/10.1111/medu.12432
Chunharas, A., Hetrakul, P., Boonyobol, R., Udomkitti, T., Tassanapitikul, T., & Wattanasirichaigoon, D. (2013). Medical students themselves as surrogate patients increased satisfaction, confidence, and performance in practicing injection skill. Medical Teacher, 35(4), 308–313. https://doi.org/10.3109/0142159X.2012.746453
Cook, D. A., Brydges, R., Zendejas, B., Hamstra, S. J., & Hatala, R. (2013). Mastery learning for health professionals using technology-enhanced simulation: A systematic review and meta-analysis. Academic Medicine, 88(8), 1178–1186. https://doi.org/10.1097/ACM.0b013e31829a365d
Cook, D. A., Hamstra, S. J., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., Erwin, P. J., & Hatala, R. (2013). Comparative effectiveness of instructional design features in simulation-based education: Systematic review and meta-analysis. Medical Teacher, 35(1), e867-898. https://doi.org/10.3109/0142159X.2012.714886
Cook, D. A., Hatala, R., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., Erwin, P. J., & Hamstra, S. J. (2011). Technology-enhanced simulation for health professions education: A systematic review and meta-analysis. JAMA, 306(9), 978–988. https://doi.org/10.1001/jama.2011.1234
Cook, D. A., & West, C. P. (2013). Perspective: Reconsidering the focus on “outcomes research” in medical education: A cautionary note. Academic Medicine, 88(2), 162–167. https://doi.org/10.1097/ACM.0b013e31827c3d78
Daly, M. K., Gonzalez, E., Siracuse-Lee, D., & Legutko, P. A. (2013). Efficacy of surgical simulator training versus traditional wet-lab training on operating room performance of ophthalmology residents during the capsulorhexis in cataract surgery. Journal of Cataract and Refractive Surgery, 39(11), 1734–1741. https://doi.org/10.1016/j.jcrs.2013.05.044
Dauphinee, W. D. (2012). Educators must consider patient outcomes when assessing the impact of clinical training. Medical Education, 46(1), 13–20. https://doi.org/10.1111/j.1365-2923.2011.04144.x
de Melo, B. C. P., Rodrigues Falbo, A., Sorensen, J. L., van Merriënboer, J. J. G., & van der Vleuten, C. (2018). Self-perceived long-term transfer of learning after postpartum haemorrhage simulation training. International Journal of Gynaecology and Obstetrics, 141(2), 261–267. https://doi.org/10.1002/ijgo.12442
De Win, G., Van Bruwaene, S., Kulkarni, J., Van Calster, B., Aggarwal, R., Allen, C., Lissens, A., De Ridder, D., & Miserez, M. (2016). An evidence-based laparoscopic simulation curriculum shortens the clinical learning curve and reduces surgical adverse events. Advances in Medical Education and Practice, 7, 357–370. https://doi.org/10.2147/AMEP.S102000
DeStephano, C. C., Chou, B., Patel, S., Slattery, R., & Hueppchen, N. (2015). A randomized controlled trial of birth simulation for medical students. American Journal of Obstetrics and Gynaecology, 213(1), 91.e1-91.e7. https://doi.org/10.1016/j.ajog.2015.03.024
Dunlosky, J., Rawson, K. A., Marsh, E. J., Nathan, M. J., & Willingham, D. T. (2013). Improving students’ learning with effective learning techniques: Promising directions from cognitive and educational psychology. Psychological Science in the Public Interest, 14(1), 4–58. https://doi.org/10.1177/1529100612453266
Dyre, L., Tabor, A., Ringsted, C., & Tolsgaard, M. G. (2017). Imperfect practice makes perfect: Error management training improves transfer of learning. Medical Education, 51(2), 196–206. https://doi.org/10.1111/medu.13208
Egenberg, S., Karlsen, B., Massay, D., Kimaro, H., & Bru, L. E. (2017). “No patient should die of PPH just for the lack of training!” Experiences from multi-professional simulation training on postpartum haemorrhage in northern Tanzania: A qualitative study. BMC Medical Education, 17(1), 119. https://doi.org/10.1186/s12909-017-0957-5
El Hussein, M. T., & Cuncannon, A. (2022). Nursing students’ transfer of learning from simulated clinical experiences into clinical practice: A scoping review. Nurse Education Today, 116, 105449. https://doi.org/10.1016/j.nedt.2022.105449
Ferrari, R. (2015). Writing narrative style literature reviews. Medical Writing, 24(4), 230–235. https://doi.org/10.1179/2047480615Z.000000000329
Frerejean, J., van Merriënboer, J. J. G., Condron, C., Strauch, U., & Eppich, W. (2023). Critical design choices in healthcare simulation education: A 4C/ID perspective on design that leads to transfer. Advances in Simulation (London, England), 8(1), 5. https://doi.org/10.1186/s41077-023-00242-7
Gomez, P. P., Willis, R. E., & Van Sickle, K. (2015). Evaluation of two flexible colonoscopy simulators and transfer of skills into clinical practice. Journal of Surgical Education, 72(2), 220–227. https://doi.org/10.1016/j.jsurg.2014.08.010
Griswold-Theodorson, S., Ponnuru, S., Dong, C., Szyld, D., Reed, T., & McGaghie, W. C. (2015). Beyond the simulation laboratory: A realist synthesis review of clinical outcomes of simulation-based mastery learning. Academic Medicine, 90(11), 1553–1560. https://doi.org/10.1097/ACM.0000000000000938
Grover, S. C., Scaffidi, M. A., Khan, R., Garg, A., Al-Mazroui, A., Alomani, T., Yu, J. J., Plener, I. S., Al-Awamy, M., Yong, E. L., Cino, M., Ravindran, N. C., Zasowski, M., Grantcharov, T. P., & Walsh, C. M. (2017). Progressive learning in endoscopy simulation training improves clinical performance: A blinded randomized trial. Gastrointestinal Endoscopy, 86(5), 881–889. https://doi.org/10.1016/j.gie.2017.03.1529
Hatala, R., Cook, D. A., Zendejas, B., Hamstra, S. J., & Brydges, R. (2014). Feedback for simulation-based procedural skills training: A meta-analysis and critical narrative synthesis. Advances in Health Sciences Education, 19(2), 251–272. https://doi.org/10.1007/s10459-013-9462-8
Hattie, J., & Timperley, H. (2007). The power of feedback. Review of Educational Research, 77(1), 81–112. https://doi.org/10.3102/003465430298487
Hernández-Irizarry, R., Zendejas, B., Ali, S. M., & Farley, D. R. (2016). Optimizing training cost-effectiveness of simulation-based laparoscopic inguinal hernia repairs. American Journal of Surgery, 211(2), 326–335. https://doi.org/10.1016/j.amjsurg.2015.07.027
Issenberg, S. B., McGaghie, W. C., Petrusa, E. R., Lee Gordon, D., & Scalese, R. J. (2005). Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Medical Teacher, 27(1), 10–28. https://doi.org/10.1080/01421590500046924
Jackson, M., McTier, L., Brooks, L. A., & Wynne, R. (2022). The impact of design elements on undergraduate nursing students’ educational outcomes in simulation education: Protocol for a systematic review. Systematic Reviews, 11(1), 52. https://doi.org/10.1186/s13643-022-01926-3
Keith, N., & Frese, M. (2008). Effectiveness of error management training: A meta-analysis. Journal of Applied Psychology, 93(1), 59–69. https://doi.org/10.1037/0021-9010.93.1.59
Kessler, D., Pusic, M., Chang, T. P., Fein, D. M., Grossman, D., Mehta, R., White, M., Jang, J., Whitfill, T., Auerbach, M., & INSPIRE LP investigators. (2015). Impact of just-in-time and just-in-place simulation on intern success with infant lumbar puncture. Pediatrics, 135(5), e1237-1246. https://doi.org/10.1542/peds.2014 -1911
Kirkpatrick, D., & Kirkpatrick, J. (2006). Evaluating training programs: The four levels. Berrett-Koehler Publishers.
Kroft, J., Ordon, M., Po, L., Zwingerman, N., Waters, K., Lee, J. Y., & Pittini, R. (2017). Preoperative practice paired with instructor feedback may not improve obstetrics-gynaecology residents’ operative performance. Journal of Graduate Medical Education, 9(2), 190–194. https://doi.org/10.4300/JGME-D-16-00238.1
Lal, B. K., Cambria, R., Moore, W., Mayorga-Carlin, M., Shutze, W., Stout, C. L., Broussard, H., Garrett, H. E., Nelson, W., Titus, J. M., Macdonald, S., Lake, R., & Sorkin, J. D. (2022). Evaluating the optimal training paradigm for transcarotid artery revascularization based on worldwide experience. Journal of Vascular Surgery, 75(2), 581-589.e1. https://doi.org/10.1016/j.jvs.2021.08.085
Liao, W.-C., Leung, J. W., Wang, H.-P., Chang, W.-H., Chu, C.-H., Lin, J.-T., Wilson, R. E., Lim, B. S., & Leung, F. W. (2013). Coached practice using ERCP mechanical simulator improves trainees’ ERCP performance: A randomized controlled trial. Endoscopy, 45(10), 799–805. https://doi.org/10.1055/s-0033-1344224
Lin, Y., Cheng, A., Hecker, K., Grant, V., & Currie, G. R. (2018). Implementing economic evaluation in simulation-based medical education: Challenges and opportunities. Medical Education, 52(2), 150–160. https://doi.org/10.1111/medu.13411
Mankute, A., Juozapaviciene, L., Stucinskas, J., Dambrauskas, Z., Dobozinskas, P., Sinz, E., Rodgers, D. L., Giedraitis, M., & Vaitkaitis, D. (2022). A novel algorithm-driven hybrid simulation learning method to improve acquisition of endotracheal intubation skills: A randomized controlled study. BMC Anaesthesiology, 22(1), 42. https://doi.org/10.1186/s12871-021-01557-6
McGaghie, W. C. (2015). Mastery learning: It is time for medical education to join the 21st century. Academic Medicine, 90(11), 1438–1441. https://doi.org/10.1097/ACM.0000000000000911
McGaghie, W. C., Issenberg, S. B., Cohen, E. R., Barsuk, J. H., & Wayne, D. B. (2011). Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Academic Medicine, 86(6), 706–711. https://doi.org/10.1097/ACM.0b013e318217e119
Mduma, E., Ersdal, H., Svensen, E., Kidanto, H., Auestad, B., & Perlman, J. (2015). Frequent brief on-site simulation training and reduction in 24-h neonatal mortality—An educational intervention study. Resuscitation, 93, 1–7. https://doi.org/10.1016/j.resuscitation.2015.04.019
Naples, R., French, J. C., Han, A. Y., Lipman, J. M., & Awad, M. M. (2022). The impact of simulation training on operative performance in general surgery: Lessons learned from a prospective randomized trial. Journal of Surgical Research, 270, 513–521. https://doi.org/10.1016/j.jss.2021.10.003
Nestel, D., Groom, J., Eikeland-Husebø, S., & O’Donnell, J. M. (2011). Simulation for learning and teaching procedural skills: The state of the science. Simulation in Healthcare, 6 Suppl, S10-13. https://doi.org/10.1097/SIH.0b013e318227ce96
Nickson, C. P., Petrosoniak, A., Barwick, S., & Brazil, V. (2021). Translational simulation: From description to action. Advances in Simulation (London, England), 6(1), 6. https://doi.org/10.1186/s41077-021-00160-6
Nilsson, C., Sorensen, J. L., Konge, L., Westen, M., Stadeager, M., Ottesen, B., & Bjerrum, F. (2017). Simulation-based camera navigation training in laparoscopy—A randomized trial. Surgical Endoscopy, 31(5), 2131–2139. https://doi.org/10.1007/s00464-016-5210-5
Orzech, N., Palter, V. N., Reznick, R. K., Aggarwal, R., & Grantcharov, T. P. (2012). A comparison of 2 ex vivo training curricula for advanced laparoscopic skills: A randomized controlled trial. Annals of Surgery, 255(5), 833–839. https://doi.org/10.1097/SLA.0b013e31824aca09
O’Sullivan, O., Iohom, G., O’Donnell, B. D., & Shorten, G. D. (2014). The effect of simulation-based training on initial performance of ultrasound-guided axillary brachial plexus blockade in a clinical setting—A pilot study. BMC Anaesthesiology, 14, 110. https://doi.org/10.1186/1471-2253-14-110
Patel, V., Aggarwal, R., Osinibi, E., Taylor, D., Arora, S., & Darzi, A. (2012). Operating room introduction for the novice. American Journal of Surgery, 203(2), 266–275. https://doi.org/10.1016/j.amjsurg.2011.03.003
Schaefer, J. J., Vanderbilt, A. A., Cason, C. L., Bauman, E. B., Glavin, R. J., Lee, F. W., & Navedo, D. D. (2011). Literature review: Instructional design and pedagogy science in healthcare simulation. Simulation in Healthcare, 6 Suppl, S30-41. https://doi.org/10.1097/SIH.0b013e31822237b4
Schaffer, A. C., Babayan, A., Einbinder, J. S., Sato, L., & Gardner, R. (2021). Association of simulation training with rates of medical malpractice claims among obstetrician-gynaecologists. Obstetrics and Gynaecology, 138(2), 246–252. https://doi.org/10.1097/AOG.0000000000004464
Sharara-Chami, R., Taher, S., Kaddoum, R., Tamim, H., & Charafeddine, L. (2014). Simulation training in endotracheal intubation in a paediatric residency. Middle East Journal of Anaesthesiology, 22(5), 477–485.
Shore, E. M., Grantcharov, T. P., Husslein, H., Shirreff, L., Dedy, N. J., McDermott, C. D., & Lefebvre, G. G. (2016). Validating a standardized laparoscopy curriculum for gynaecology residents: A randomized controlled trial. American Journal of Obstetrics and Gynaecology, 215(2), 204.e1-204.e11. https://doi.org/10.1016/j.ajog.2016.04.037
Sørensen, J. L., Navne, L. E., Martin, H. M., Ottesen, B., Albrecthsen, C. K., Pedersen, B. W., Kjærgaard, H., & van der Vleuten, C. (2015). Clarifying the learning experiences of healthcare professionals with in situ and off-site simulation-based medical education: A qualitative study. BMJ Open, 5(10), e008345. https://doi.org/10.1136/bmjopen-2015-008345
Srinivasan, K. K., Gallagher, A., O’Brien, N., Sudir, V., Barrett, N., O’Connor, R., Holt, F., Lee, P., O’Donnell, B., & Shorten, G. (2018). Proficiency-based progression training: An “end to end” model for decreasing error applied to achievement of effective epidural analgesia during labour: A randomised control study. BMJ Open, 8(10), e020099. https://doi.org/10.1136/bmjopen-2017-020099
Steinert, Y., Mann, K., Centeno, A., Dolmans, D., Spencer, J., Gelula, M., & Prideaux, D. (2006). A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Medical Teacher, 28(6), 497–526. https://doi.org/10.1080/01421590600902976
Tan, T. X., Buchanan, P., & Quattromani, E. (2018). Teaching residents chest tubes: Simulation task trainer or cadaver model? Emergency Medicine International, 2018, 9179042. https://doi.org/10.1155/2018/9179042
Tavares, W., Eppich, W., Cheng, A., Miller, S., Teunissen, P. W., Watling, C. J., & Sargeant, J. (2020). Learning conversations: An analysis of the theoretical roots and their manifestations of feedback and debriefing in medical education. Academic Medicine, 95(7), 1020–1025. https://doi.org/10.1097/ACM.0000000000002932
Tchorz, J. P., Brandl, M., Ganter, P. A., Karygianni, L., Polydorou, O., Vach, K., Hellwig, E., & Altenburger, M. J. (2015). Pre-clinical endodontic training with artificial instead of extracted human teeth: Does the type of exercise have an influence on clinical endodontic outcomes? International Endodontic Journal, 48(9), 888–893. https://doi.org/10.1111/iej.12385
Todsen, T., Henriksen, M. V., Kromann, C. B., Konge, L., Eldrup, J., & Ringsted, C. (2013). Short- and long-term transfer of urethral catheterization skills from simulation training to performance on patients. BMC Medical Education, 13, 29. https://doi.org/10.1186/1472-6920-13-29
Tolsgaard, M. G., Madsen, M. E., Ringsted, C., Oxlund, B. S., Oldenburg, A., Sorensen, J. L., Ottesen, B., & Tabor, A. (2015). The effect of dyad versus individual simulation-based ultrasound training on skills transfer. Medical Education, 49(3), 286–295. https://doi.org/10.1111/medu.12624
Walsh, C. M., Scaffidi, M. A., Khan, R., Arora, A., Gimpaya, N., Lin, P., Satchwell, J., Al-Mazroui, A., Zarghom, O., Sharma, S., Kamani, A., Genis, S., Kalaichandran, R., & Grover, S. C. (2020). Non-technical skills curriculum incorporating simulation-based training improves performance in colonoscopy among novice endoscopists: Randomized controlled trial. Digestive Endoscopy, 32(6), 940–948. https://doi.org/10.1111/den.13623
Wulf, G., Shea, C., & Lewthwaite, R. (2010). Motor skill learning and performance: A review of influential factors. Medical Education, 44(1), 75–84. https://doi.org/10.1111/j.1365-2923.2009.03421.x
Zendejas, B., Brydges, R., Wang, A. T., & Cook, D. A. (2013). Patient outcomes in simulation-based medical education: A systematic review. Journal of General Internal Medicine, 28(8), 1078–1089. https://doi.org/10.1007/s11606-012-2264-5
*Matthew Low
Emergency Medicine Department,
National University Hospital
9 Lower Kent Ridge Road, Level 4,
Singapore 119085
Email: mlow@nus.edu.sg
Submitted: 24 October 2024
Accepted: 5 July 2025
Published online: 7 October, TAPS 2025, 10(4), 26-34
https://doi.org/10.29060/TAPS.2025-10-4/OA3552
Shoko Horita1,2, Masashi Izumiya2, Satoshi Kondo2,3,4, Junki Mizumoto2,5,6, Hiroko Mori6,7 & Masato Eto2
1Department of Medical Education, School of Medicine, Teikyo University, Itabashi-ku, Tokyo, Japan; 2Department of Medical Education Studies, International Research Centre for Medical Education, Graduate School of Medicine, The University of Tokyo, Bunkyo-ku, Tokyo, Japan; 3Department of Medical Education, Graduate School of Medicine, University of Toyama, Toyama, Japan; 4Center for Medical Education and Career Development, Graduate School of Medicine, University of Toyama, Toyama, Japan; 5Department of Family Practice, Ehime Seikyo Hospital, Matsuyama, Ehime, Japan; 6Center for General Medicine Education, School of Medicine, Keio University, Shinjuku, Tokyo, Japan; 7Professional Development Centre, The University of Tokyo Hospital, Bunkyo-ku, Tokyo, Japan
Abstract
Introduction: Conventionally, face-to-face education has been prevalent in medical education because it can help medical students learn interpersonal skills, including medical interviews and physical examination. However, because of the coronavirus disease 2019 pandemic, face-to-face education was suspended to prevent the spread of the infection. As face-to-face classes in Japan were discontinued when the pandemic began in the spring of 2020, we developed an online education program to develop medical interview skills. We were interested in determining the educational outcomes between face-to-face and online medical interview classes. Therefore, we compared them before and after the pandemic.
Methods: Fourth-year students of the University of Tokyo Medical School took medical interview classes. Under consent, the score of the medical interview area of the preclinical clerkship, Objective Structured Clinical Examination (OSCE), as a high-stakes examination, which falls at the top level of the Kirkpatrick’s model, was compared by year or before and after the pandemic.
Results: The online group showed higher item-wise scores of the medical interview of the preclinical clerkship OSCE than the face-to-face group. In terms of the global score, no significant difference was observed. In the computer-based test (CBT), the online group had higher scores compared with the face-to-face group.
Conclusion: The educational outcomes of online medical interview classes were not inferior to those of conventional face-to-face classes, as revealed by high-stakes examination preclinical clerkship OSCE. Similar to face-to-face education, online education is a viable option for developing interpersonal skills.
Keywords: COVID-19 Pandemic, Medical Interview, OSCE, Educational Outcome, Online Education, Interpersonal Skills, Communication Skills
Practice Highlights
- Due to the COVID-19 pandemic, we shifted medical interview classes from face-to-face to online.
- The online group had interview global OSCE scores non-inferior to those of the face-to-face group.
- The online group had higher interview elementary OSCE scores than the face-to-face group.
I. INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic severely restricted face-to-face teaching and affected almost all levels and fields of education, including undergraduate preclinical medical education (Bastos et al., 2022; Crawford et al., 2020). Moreover, it resulted in drastic changes in medical education. Globally, face-to-face learning was forcibly discontinued as part of infection control. Thus, to continue medical education, online or remote learning was rapidly introduced (Daniel et al., 2021; Gordon et al., 2020). Various instrumental trans communication devices, including video conferencing tools, simulation, virtual reality, and augmented reality, were used to facilitate online learning. However, this rather hasty shift from face-to-face to online learning brought some confusion into the field of medical education. In the UK, Dost et al. (2020) reported that medical students were unsatisfied with online classes compared with face-to-face classes.
Globally, tele-education is increasingly being encouraged around the world (American Medical Association, 2016). In the field of medical interview (Budakoğlu et al., 2021; Hammersley et al., 2019; Zaccariah et al., 2022), telemedicine is gradually becoming common, showing favourable results. However, because of technical problems, tele-education did not spread smoothly (Zaccariah et al., 2022). Additionally, the educational outcomes of both strategies have not been satisfactorily studied (Khamees et al., 2022). Recently, some reports showing that the educational outcome of online classes are equal or more effective than traditional face-to-face education, however, they are restricted mainly in knowledge-based education (Alshaibani et al., 2023; Basuodan, 2024; Saad et al., 2023). Furthermore, few studies have compared high-stakes examination, including the Objective Structured Clinical Examination (OSCE), and no study has compared the educational results between face-to-face classes and tele-education (online) using the top level of Kirkpatrick’s model (Kirkpatrick, 1996).
The OSCE (Harden et al., 1975) has been widely accepted as a form to assess clinical performance in medical education. Currently, OSCEs are used worldwide to appraise medical students’ communication and clinical skills. Various educational methods have been evaluated using OSCE as one of the indicators of educational outcomes (Guetterman et al., 2019). In Japan, passing the preclinical clerkship (pre-CC) OSCE has become legally obligatory as one of the elements for promotion to the CC course since the spring of 2023. In 2023, the pre-CC OSCE in Japan is conducted in at least eight areas, which are medical interview, “Basic Clinical Procedure”, “Basic Life Support”, and physical examinations of “head and neck”, “chest”, “vital signs”, “abdomen”, and “neurological examinations”.
In the present study, we aimed to determine the educational outcomes between face-to-face and online medical interview classes. We provided medical interview classes to fourth-year medical students before taking the pre-CC OSCE, face-to-face classes before 2019, and tele-education (online) after 2020. We decided to conduct research in medical interview, other than the other areas of the pre-CC OSCE, because of the importance of the medical interview as the basis of medical practice. Moreover, it was inevitable that the medical interview classes had to be implemented as online classes to protect the simulated patients form the risk of infection, which was another main reason for selecting medical interview for this research. In another point of view, medical interview classes were able to implement via online. As mentioned above, no prior studies have compared face-to-face and online medical interview training using both high-stakes OSCE score and Kirkpatrick’s top-level outcomes, our study would have significant importance.
II. METHOD
A. Participants
This study was approved in 2021 by the ethics committee of the University of Tokyo (UTokyo) Faculty of Medicine (Approval No. 2021005NI). All methods were performed in accordance with the relevant guidelines and regulations. Moreover, the data of students who provided consent for the secondary use of their data (Approval No. 11763) in another research approved in 2017 were included.
B. Sample Population
Students in the UTokyo Faculty of Medicine were asked if they were willing to participate in “A Study of the Educational Effectiveness of Online “Medical interviewing Practice” in the post-class reflection questionnaire of the “Online medical interview classes or the waiting period after the pre-CC OSCE. Out of 229 students (2021 and 2022), 87 students participated in this study. A summary of the annual participants is shown in Appendix 1. In early 2020 almost all the classes in UTokyo were stopped due to the COVID-19 pandemic, which made it difficult to contact students face-to-face and to obtain participants in the previous research (Approval No. 11763); and as this research started in 2021, it was practically difficult to obtain consent to participate in this study in 2020. In 2020 the online medical interview classes have just been launched, which significantly improved in 2021. Hence, we thought that it would be better to exclude the small participants of 2020 from the analysis to keep the validity of this study.
C. Details of Medical Interview Classes
Before 2019, the medical interview classes were performed as follows: Early in their fourth year, students joined classes introducing the outline of medical interview. A few days before the class, students watched an instructional video of a medical interview performed by the Common Achievement Tests Organization (CATO) (2005) in Japan. Afterward, students in a group of eight to nine faced the simulated patient in a classroom in the UTokyo and performed a medical interview roleplay. Thereafter, feedback about the technical factor of the medical interview as well as rapport status and nonverbal communications such as faces and gesture was provided by the students themselves, other students, simulated patients, and teachers. Since 2020, most face-to-face classrooms, including those in the present study, were closed because of the COVID-19 pandemic and were replaced with online classes. The present face-to-face class was also held online with the simulated patients and teachers using Zoom(R). Using the “Close-Up” function of Zoom(R), the simulated patient and student were faced with each other, whereas other participants (e.g., other students, other simulated patients, and the teacher) were not on the television (Appendix 2). After the roleplay was over, all students and the teacher came back on the television and provided feedback to the student, similar to face-to-face classes. Moreover, the class was recorded using the function of Zoom(R) and provided to students exclusively for review. After the class students reflected on the reflection sheet (until 2019) or the Learning Management System (from 2020) which was reviewed and commented on by teachers. The contents of the reflections were used for this study to investigate the impressions of the students.
D. Pre-CC OSCE and Computer-Based Test (CBT)
In Japan, medical students usually take the pre-CC OSCE in the fourth year, prior to the two-year CC course. Before 2022, the minimum assessment factors were medical interview, physical examinations (including head and neck, chest, abdomen, neurological examinations), basic clinical procedure, and basic life support. The examinations were administered by CATO. The evaluation criteria are not publicly available because of CATO policy. Two scores are used in the evaluation: global score (GS) which means the evaluation as a total performance and item-wise score (IS) which means scores by checklist. Before 2023, the borderline was set by each institute. At least one certified evaluator per area was responsible, and each evaluator was a faculty member. Moreover, CATO sent at least one external evaluator per area and an external supervisor. After each performance, each examinee was evaluated by two or three evaluators per room. The pre-CC OSCE is one of the examinations that students must pass to proceed to the CC course.
Aside from the pre-CC OSCE, students must also pass the CBT. The CBT corresponds to the assessment of medical knowledge prior to the CC (Horita et al., 2021). In 2023, the pre-CC OSCE and CBT have been made official, and students must pass both examinations before they can take the national board examination in Japan.
E. Data Analysis
The pre-CC OSCE scores were analysed using R, Rstudio, JMP version17.0 (SAS Institute, N.C., USA) and Microsoft Excel (Microsoft Corporation, W.A., USA). Non-paired T test, Mann-Whitney U test, and Steel-Dwass test were used respectively, for parametric or non-parametric comparisons.
III. RESULTS
A. Year-to-Year Comparison of the Pre-CC OSCE Results in the Medical Interview area and CBT Results
First, we compared the year-to-year results of the pre-CC OSCE in the medical interview area. Table 1 and Figure 1 shows a statistical summary of the pre-CC OSCE scores in 2022, 2021, 2019, and 2018. The results of non-parametric tests revealed that the p-values in the IS between 2022 and 2019, 2022 and 2018, and 2021 and 2018 were below 0.05, whereas no significant difference was observed in the GS.
|
Year |
IS/GS |
Average |
SD |
SE |
Bottom 95 |
Upper 95 |
|
2022 |
IS |
85.67 |
9.19 |
1.18 |
83.32 |
88.02 |
|
GS |
4.41 |
0.68 |
0.09 |
4.24 |
4.58 |
|
|
2021 |
IS |
82.69 |
9.71 |
1.90 |
78.77 |
86.61 |
|
GS |
4.62 |
0.75 |
0.15 |
4.31 |
4.92 |
|
|
2019 |
IS |
79.04 |
10.19 |
1.07 |
76.92 |
81.16 |
|
GS |
4.33 |
0.89 |
0.09 |
4.14 |
4.51 |
|
|
2018 |
IS |
73.63 |
9.94 |
1.10 |
71.43 |
75.83 |
|
GS |
4.26 |
0.79 |
0.09 |
4.09 |
4.44 |
Table 1. Averages of IS and GS of the medical interview area per the pre-CC OSCE implementation year. IS, item-wise score; GS, global score; SD, standard deviation; SE, standard error
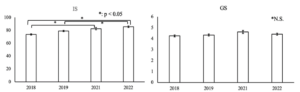
Figure 1. Average of IS and GS. The error bar shows standard error
|
Year |
Average |
SD |
SE |
Bottom 95 |
Upper 95 |
|
2022 |
566.62 |
121.03 |
15.50 |
535.63 |
597.62 |
|
2021 |
576.07 |
106.64 |
20.52 |
533.89 |
618.26 |
|
2019 |
565.02 |
119.91 |
12.71 |
539.76 |
590.28 |
|
2018 |
529.72 |
116.34 |
12.93 |
503.99 |
555.44 |
Table 2. Year-by-year score distribution of CBT (IRT score)
B. Comparison Before and After the Pandemic
The medical interview classes were held face-to-face before the pandemic (2018 and 2019) and online after the pandemic (2021 and 2022). We compared the results of pre-CC OSCE medical interview and CBT before and after the pandemic. A summary of the results is shown in Table 3 and Figure 2. The results of statistical analyses revealed a significant difference in the medical interview IS and CBT between the face-to-face group and the online group (p < 0.001 and 0.032 respectively). However, no significant difference in GS was observed.
|
|
Group |
Number |
Average |
SE |
Bottom 95 |
Upper 95 |
|
OSCE (medical interview) IS |
F-to-F |
164 |
76.18 |
0.79 |
74.62 |
77.74 |
|
online |
85 |
84.71 |
1.10 |
82.54 |
86.87 |
|
|
OSCE (medical interview) GS |
F-to-F |
164 |
4.28 |
0.06 |
4.15 |
4.40 |
|
online |
85 |
4.47 |
0.09 |
4.30 |
4.64 |
|
|
CBT (IRT score) |
F-to-F |
162 |
546.5 |
9.39 |
528.1 |
565.0 |
|
online |
86 |
569.7 |
12.9 |
544.3 |
595.1 |
Table 3. Comparison of pre-CC OSCE (IS and GS respectively) and CBT results between the face-to-face (F-to-F) group and the online group

Figure 2. Comparison of pre-CC OSCE (IS and GS respectively) and CBT results between the face-to-face (F-to-F) group and the online group. The error bar shows standard error.
IV. DISCUSSION
We found no significant negative effects in some of the important educational outcomes in medical students’ scores of the medical interview due to online education caused by the COVID-19 pandemic. The quality of the medical interview after the emergence of the pandemic was no less than that before the pandemic. The same could be said for other indicators, including the CBT and other areas of the OSCE (data not shown).
One of the reasons why the scores of the online classes were not inferior to those of face-to-face classes might be because of the availability of each student to review the video recordings. We provided each student with a recording of their own performance in the class for self-review, which was not always provided in face-to-face classes. We also provided students with feedback from the teacher and other students during online classes. This is consistent with the findings of a previous study, which found that video reviewing of the OSCE performance is effective (Mookherjee et al., 2019). Moreover, the students accepted online classes well, and their motivation for learning was not affected despite the lack of face-to-face communication with simulated patients. During the reflection, some students noted that “I learned a lot in this class, though the class was held online” and that “I thought that online classes are not so bad” (data not shown). There were almost no complaints regarding online classes. We guess that in the environment that the face-to-face classes were restricted and the students experienced suspended classes the students felt satisfied for joining the classes even online. Further investigation will be needed regarding this point.
Recently, Khamees et al. (2022) pointed out the lack of control groups and poor transferability in numerous publications due to singularity of institution, department, and program. In the present study, the marks of students on high-stakes examinations before the pandemic were used as a comparison between face-to-face and online classes. Some studies have revealed that there are no significant differences in educational outcomes between face-to-face and online classes in basic medicine (Omole et al., 2023), and pharmacological education (Aoe et al., 2023). However, when it comes to high-stakes examinations, it remains unclear whether online education is not inferior to face-to-face education. Saad et al (2023) have showed that in some areas (clinical reasoning and history taking) of pre-clinical OSCE, students showed no less than comparable results, arguing that these skills are amenable to online learning in a medical school in Australia. Their results in some areas like medical interview in Japanese OSCE support our results. However, in their study, it is not clear about the details of the OSCE assessment, whether the assessment is by item-wise or global. In recent years, the pre-CC OSCE results have been recognized as an important educational outcome also for educational institutions (Hirsh et al., 2012). Our result, the educational outcome in the high-stakes examination, can be considered to fall in the top tier, the result, in the Kirkpatrick’s four-level model (Kirkpatrick, 1996). Moreover, our research is unique and important as few studies have directly compared the educational outcomes between face-to-face classes and online classes in high-stakes examination.
In Japan, the Medical Practitioners Act was revised in 2023, allowing medical students to perform some medical procedures under the supervision of a teaching physician after passing the pre-CC OSCE and CBT. This change also made the pre-CC OSCE a requirement for the national board examination. Hence, the pre-CC OSCE in Japan has become even more important, as much the responsibility for the education even greater. Our results show that online classes can contribute to the practice of “Medical interviews”.
It must be noted that online classes are not a complete alternative to face-to-face classes. Many studies have indicated that online education has some negative aspects (e.g., the need for infrastructure and devices, high cost, lack of personal interaction, etc.) (Arja et al., 2022; Mortazavi et al., 2021; Shaiba et al., 2023). One of the most significant elements that are difficult to teach in online classes is nonverbal communication. However, as Ishikawa et al. (2010) reported, although students are capable of understanding nonverbal communication despite struggling to change their performance through educational intervention, it is well recognized that nonverbal communication is difficult to teach even in face-to-face classes. Additionally, when it comes to procedural skills such as venipuncture, the educational outcomes in the online learning group were inferior to that of face-to-face learning group and students also felt that they were not taught satisfactorily (Dost et al., 2020; Saad et al., 2023). We should keep in mind that online education does not fully replace face-to-face education.
We saw a lack of significant differences in GS, both in year-by-year comparison and comparison between face-to-face and online groups. Although the tasks allocated to each university by CATO differ every year, the checkpoints are essentially common in quite a few areas; so, a comparison was made for both year by year and before and after the pandemic. GS usually reflects holistic assessment, which is difficult to produce results via technical education, whereas it might be easier for learners and teachers to deal with item-wise assessment (Govaerts et al., 2011; Jonsson & Svingby, 2007; Sadler, 2009). Moreover, in online classes, we used a checklist of the students’ performance (not shown to the students, but comments were given according to the checklist), which might have contributed to the improvement of IS. As to CBT, it is standardized by the accumulated examinations and the Item Response Theory and is assessed basically by knowledge base. The educational strategies that mainly should impact on the assessment of CBT, based on the lecture, have not changed before and after the pandemic, in the face-to-face classes or online classes. During the pandemic, the extra-curricular activities of the students were restricted, and several articles argue that self-studying time of the students increased (Barton et al., 2021; Guluma & Brandl, 2023). These might have contributed to the smaller elevation of CBT-IRT than the IS of pre-CC OSCE.
We need to take into consideration the confounding of several factors such as the curriculum changes, instructor training, student characteristics and students’ self-study time. While online classes have been a change in the curriculum, the rest remains unchanged. The instructors and students needed to become familiar with online classes, but there was no change in the educational goals of the class itself. Additionally, in the first year of the pandemic in 2020, we were unable to get enough data and the online class itself was implemented as “being built”. By 2021 and 2022, the class was almost stable. However, getting used to online classes of the instructors and students could be a confounding factor. The class tool (Zoom®) was continuously improved, which might be a minor confounding factor. Additionally, the students might have had excellent ITC skills, which might also be a confounding factor.
Some frameworks describing the evidence of online medical education outcome might contribute to generalizing our results (Martinengo et al., 2024; McGee et al., 2024; Wilcha, 2020). Needless to say, there are confrontations regarding the limitations of these generalizations, pointing out the context-depending factors, high heterogeneity among studies and “The Covid-19 Effects” (Abdull Mutalib et al., 2022; Liu et al., 2016; Martinengo et al., 2024; McGee et al., 2024). However, these frameworks will be applicable in generalizing our results; although there are some potential confounding factors such as the students, the instructors, the educational resources and the “pandemic era” itself, the online medical interview education could be an effective educational curriculum for educating medical interview skills as well as some interpersonal skills.
A. Limitations
One of the limitations of this study is that it was performed in a single institution. Hence, the generalizability of this study may be lower than that of multi-institutional studies. However, not much variation exists in the nature of students and in the educational curriculum they experience. Of course, to make the evidence more robust and further validate, multi-centred or multi-institutional studies are still needed. At the same time, these factors should not be too disparate as it is very difficult to find a suitable population for these factors. In this regard, our participants and classes can be considered as a reasonable population.
Another limitation of this study is the number of participants. In 2020, we could not obtain enough participants because of the pandemic. After the pandemic, our students and staff shifted to online classes, and the number of face-to-face classes decreased. In 2021 and 2022, we decided to obtain consent for participation in this study in the waiting time after face-to-face OSCE examination as it was difficult to obtain consent only during online classes. In this context, the participants may have a positive view of various aspects of student life including studies, which may be a potential bias of sample population. Additionally, the waiting time after the OSCE examination was short for some students, which might have made it difficult to think about understanding the concept of this research and whether consent should be given.
In this study, qualitative analyses investigating if the students were positive about the classes are limited to some extent. During the pandemic, the psychological situation and the learning behaviour of the students might have differed from that of before the pandemic. To investigate this aspect, qualitative studies will be needed.
Moreover, the evaluation criteria of the pre-CC OSCE are not open to the public due to CATO policy. This probably leads to a lack of transparency of the evaluation, causing another limitation of this study. However, Japanese OSCE evaluation criteria is similar to CANMED’s OSCE checklist (Kassam et al., 2016), which will support the validity of the results of Japanese OSCE and our results.
Finally, this study retrospectively compared the educational effect between students before and after the pandemic, which may limit the causal inferences of educational outcome effects of face-to-face versus online in medical interview OSCE. A randomized controlled trial will be needed to verify the results obtained in this study.
V. CONCLUSION
Because of the COVID-19 pandemic, we were forced to change our medical interview classes from face-to-face to be online. However, in high-stakes examinations such as the pre-CC OSCE and CBT, the results of the online group were not inferior to those of the face-to-face group. We consider this result extremely important because we directly compared the educational outcomes of high-stakes examinations between online and face-to-face groups who took the same medical interview classes, and because this evaluation falls in the top level of Kirkpatrick’s model. Our results suggest that online education provides a viable option in teaching interpersonal skills and support the integration of online medical interview training into preclinical curricula, particularly in resource-constrained settings. Randomized controlled trials and multi-institutional studies are needed to further validate our results.
Notes on Contributors
SH and ME conducted the whole research.
SH, MI, SK, JM, HM, and ME performed the classes and collected the data.
SH performed data analyses.
SH, MI, SK, JM, HM, and ME contributed to writing the manuscript.
Ethical Approval
This study was approved by the ethics committee of the UTokyo Faculty of Medicine (Approval No. 2021005NI). All methods were performed in accordance with the relevant guidelines and regulations. Moreover, the data of students who provided consent to the secondary use of their data in another research, given by the ethics committee of the UTokyo Faculty of Medicine (Approval No. 11763), were included.
Data Availability
The data in this study are not publicly available because of confidentiality agreements with the participants, conditions obligating CATO, and confidential nature of the data.
Acknowledgement
We thank the students of the UTokyo Medical School who participated in this study. We also thank the UTokyo Staff for their cooperation.
Funding
This study was funded by JSPS KAKENHI Grant Number 24K06092 and ACRO incubation grants of Teikyo University.
Declaration of Interest
The authors have no potential conflicts to disclose.
References
Abdull Mutalib, A. A., Md. Akim, A., & Jaafar, M. H. (2022). A systematic review of health sciences students’ online learning during the COVID-19 pandemic. BMC Medical Education, 22(1), 524. https://doi.org/10.1186/s12909-022-03579-1
Alshaibani, T., Almarabheh, A., Jaradat, A., & Deifalla, A. (2023). Comparing online and face-to-face performance in scientific courses: A retrospective comparative gender study of Year-1 students. Advances in Medical Education and Practice, 14, 1119–1127. https://doi.org/10.2147/amep.s408791
American Medical Association. (2016, June 15). AMA encourages telemedicine training for medical students, residents. AMA Press Releases.
Aoe, M., Esaki, S., Ikejiri, M., Ito, T., Nagai, K., Hatsuda, Y., Hirokawa, Y., Yasuhara, T., Kenzaka, T., & Nishinaka, T. (2023). Impact of different attitudes toward face-to-face and online classes on learning outcomes in Japan. Pharmacy, 11(1), 16. https://doi.org/10.3390/pharmacy11010016
Arja, S. B., Fatteh, S., Nandennagari, S., Pemma, S. S. K., Ponnusamy, K., & Arja, S. B. (2022). Is emergency remote (online) teaching in the first two years of medical school during the COVID-19 pandemic serving the purpose? Advances in Medical Education and Practice, 13, 199–211. https://doi.org/10.2147/amep.s352599
Barton, J., Rallis, K. S., Corrigan, A. E., Hubbard, E., Round, A., Portone, G., Kuri, A., Tran, T., Phuah, Y. Z., Knight, K., & Round, J. (2021). Medical students’ pattern of self-directed learning prior to and during the coronavirus disease 2019 pandemic period and its implications for Free Open Access Meducation within the United Kingdom. Journal of Educational Evaluation for Health Professions, 18, 5. https://doi.org/10.3352/jeehp.2021.18.5
Bastos, R. A., Carvalho, D. R. D. S., Brandão, C. F. S., Bergamasco, E. C., Sandars, J., & Cecilio-Fernandes, D. (2021). Solutions, enablers and barriers to online learning in clinical medical education during the first year of the COVID-19 pandemic: A rapid review. Medical Teacher, 44(2), 187–195. https://doi.org/10.1080/0142159x.2021.1973979
Basuodan, R. (2024). Comparisons of the academic performance of Medical and Health-Sciences students related to three learning methods: A cross-sectional study. Advances in Medical Education and Practice, 15, 1339–1347. https://doi.org/10.2147/amep.s493782
Budakoğlu, I. İ., Sayılır, M. Ü., Kıyak, Y. S., Coşkun, Ö., & Kula, S. (2021). Telemedicine curriculum in undergraduate medical education: a systematic search and review. Health and Technology, 11(4), 773–781. https://doi.org/10.1007/s12553-021-00559-1
Common Achievement Tests Organization (CATO). (2005). Common Achievement Tests Organization. https://www.cato.or.jp/index.html
Crawford, J., Butler-Henderson, K., Rudolph, J., Malkawi, B., Glowatz, M., Burton, R., Magni, P. A., & Lam, S. (2020). COVID-19: 20 countries’ higher education intra-period digital pedagogy responses. Journal of Applied Learning & Teaching, 3(1). https://doi.org/10.37074/jalt.2020.3.1.7
Daniel, M., Gordon, M., Patricio, M., Hider, A., Pawlik, C., Bhagdev, R., Ahmad, S., Alston, S., Park, S., Pawlikowska, T., Rees, E., Doyle, A. J., Pammi, M., Thammasitboon, S., Haas, M., Peterson, W., Lew, M., Khamees, D., Spadafore, M., … Stojan, J. (2021). An update on developments in medical education in response to the COVID-19 pandemic: A BEME scoping review: BEME Guide No. 64. Medical Teacher, 43(3), 253–271. https://doi.org/10.1080/0142159x.2020.1864310
Dost, S., Hossain, A., Shehab, M., Abdelwahed, A., & Al-Nusair, L. (2020). Perceptions of medical students towards online teaching during the COVID-19 pandemic: A national cross-sectional survey of 2721 UK medical students. BMJ Open, 10(11), e042378. https://doi.org/10.1136/bmjopen-2020-042378
Gordon, M., Patricio, M., Horne, L., Muston, A., Alston, S. R., Pammi, M., Thammasitboon, S., Park, S., Pawlikowska, T., Rees, E. L., Doyle, A. J., & Daniel, M. (2020). Developments in medical education in response to the COVID-19 pandemic: A rapid BEME systematic review: BEME Guide No. 63. Medical Teacher, 42(11), 1202–1215. https://doi.org/10.1080/0142159x.2020.1807484
Govaerts, M. J. B., Schuwirth, L. W. T., Van Der Vleuten, C. P. M., & Muijtjens, A. M. M. (2010). Workplace-based assessment: Effects of rater expertise. Advances in Health Sciences Education, 16(2), 151–165. https://doi.org/10.1007/s10459-010-9250-7
Guetterman, T. C., Sakakibara, R., Baireddy, S., Kron, F. W., Scerbo, M. W., Cleary, J. F., & Fetters, M. D. (2019). Medical students’ experiences and outcomes using a virtual human simulation to improve communication skills: Mixed methods study. Journal of Medical Internet Research, 21(11), e15459. https://doi.org/10.2196/15459
Guluma, K. Z., & Brandl, K. (2022). Virtual learning allows for adaptation of study strategies in a cohort of U.S. medical students. Medical Teacher, 45(1), 89–96. https://doi.org/10.1080/0142159x.2022.2105690
Hammersley, V., Donaghy, E., Parker, R., McNeilly, H., Atherton, H., Bikker, A., Campbell, J., & McKinstry, B. (2019). Comparing the content and quality of video, telephone, and face-to-face consultations: A non-randomised, quasi-experimental, exploratory study in UK primary care. British Journal of General Practice, 69(686), e595–e604. https://doi.org/10.3399/bjgp19x704573
Harden, R. M., Stevenson, M., Downie, W. W., & Wilson, G. M. (1975). Assessment of clinical competence using objective structured examination. BMJ, 1(5955), 447–451. https://doi.org/10.1136/bmj.1.5955.447
Hirsh, D., Gaufberg, E., Ogur, B., Cohen, P., Krupat, E., Cox, M., Pelletier, S., & Bor, D. (2012). Educational outcomes of the Harvard Medical School–Cambridge integrated clerkship. Academic Medicine, 87(5), 643–650. https://doi.org/10.1097/acm.0b013e31824d9821
Horita, S., Park, Y., Son, D., & Eto, M. (2021). Computer-based test (CBT) and OSCE scores predict residency matching and National Board assessment results in Japan. BMC Medical Education, 21(1). https://doi.org/10.1186/s12909-021-02520-2
Ishikawa, H., Hashimoto, H., Kinoshita, M., & Yano, E. (2010). Can nonverbal communication skills be taught? Medical Teacher, 32(10), 860–863. https://doi.org/10.3109/01421591003728211
Jonsson, A., & Svingby, G. (2007). The use of scoring rubrics: Reliability, validity, and educational consequences. Educational Research Review, 2(2), 130–144. https://doi.org/10.1016/j.edurev.2007.05.002
Kassam, A., Cowan, M., & Donnon, T. (2016). An objective structured clinical exam to measure intrinsic CanMEDS roles. Medical Education Online, 21(1), 31085. https://doi.org/10.3402/meo.v21.31085
Khamees, D., Peterson, W., Patricio, M., Pawlikowska, T., Commissaris, C., Austin, A., Davis, M., Spadafore, M., Griffith, M., Hider, A., Pawlik, C., Stojan, J., Grafton-Clarke, C., Uraiby, H., Thammasitboon, S., Gordon, M., & Daniel, M. (2022). Remote learning developments in postgraduate medical education in response to the COVID-19 pandemic: A BEME systematic review: BEME Guide No. 71. Medical Teacher, 44(5), 466–485. https://doi.org/10.1080/0142159x.2022.2040732
Kirkpatrick, D. (1996). Great ideas revisited. Techniques for evaluating training programs. Revisiting Kirkpatrick’s Four-Level model. Training & Development, 50(1), 54–59. https://eric.ed.gov/?id=EJ515660
Liu, Q., Peng, W., Zhang, F., Hu, R., Li, Y., & Yan, W. (2016). The effectiveness of blended learning in health professions: Systematic review and meta-analysis. Journal of Medical Internet Research, 18(1), e2. https://doi.org/10.2196/jmir.4807
Martinengo, L., Ng, M. S. P., De Rong Ng, T., Ang, Y., Jabir, A. I., Kyaw, B. M., & Car, L. T. (2024). Spaced digital education for health professionals: A systematic review and meta-analysis (Preprint). Journal of Medical Internet Research, 26, e57760. https://doi.org/10.2196/57760
McGee, R. G., Wark, S., Mwangi, F., Drovandi, A., Alele, F., & Malau-Aduli, B. S. (2024). Digital learning of clinical skills and its impact on medical students’ academic performance: A systematic review. BMC Medical Education, 24(1). https://doi.org/10.1186/s12909-024-06471-2
Mookherjee, S., Strujik, J., Cunningham, M., Kaplan, E., & Çoruh, B. (2018). Independent and mentored video review of OSCEs. The Clinical Teacher, 16(1), 23–29. https://doi.org/10.1111/tct.12755
Mortazavi, F., Salehabadi, R., Sharifzadeh, M., & Ghardashi, F. (2021). Students’ perspectives on the virtual teaching challenges in the COVID-19 pandemic. Journal of Education and Health Promotion, 10(1), 59. https://doi.org/10.4103/jehp.jehp_861_20
Omole, A. E., Villamil, M. E., & Amiralli, H. (2023). Medical education during COVID-19 pandemic: A comparative effectiveness study of face-to-face traditional learning versus online digital education of basic sciences for medical students. Cureus. https://doi.org/10.7759/cureus.35837
Saad, S., Richmond, C., King, D., Jones, C., & Malau-Aduli, B. (2023). The impact of pandemic disruptions on clinical skills learning for pre-clinical medical students: Implications for future educational designs. BMC Medical Education, 23(1). https://doi.org/10.1186/s12909-023-04351-9
Sadler, D. R. (2008). Indeterminacy in the use of preset criteria for assessment and grading. Assessment & Evaluation in Higher Education, 34(2), 159–179. https://doi.org/10.1080/02602930801956059
Shaiba, H., John, M., & Meshoul, S. (2022). Female Saudi College students’ e-learning experience amidst COVID-19 pandemic: An investigation and analysis. Heliyon, 9(1), e12768. https://doi.org/10.1016/j.heliyon.2022.e12768
Wilcha, R. (2020). Effectiveness of virtual medical teaching during the COVID-19 Crisis: Systematic review. JMIR Medical Education, 6(2), e20963. https://doi.org/10.2196/20963
Zaccariah, Z. R., Irvine, A. W., & Lefroy, J. E. (2022). Feasibility study of student telehealth interviews. The Clinical Teacher, 19(4), 308–315. https://doi.org/10.1111/tct.13490
*Shoko Horita
2-11-1, Kaga, Itabashi-ku,
Tokyo 173-8605, Japan
Email: horitas-tky@umin.ac.jp
Submitted: 19 February 2025
Accepted: 14 May 2025
Published online: 7 October, TAPS 2025, 10(4), 73-76
https://doi.org/10.29060/TAPS.2025-10-4/SC3672
Astrid Pratidina Susilo1, Lucia Pudyastuti Retnaningtyas1, Lisa Aditama2 & Karunia Wijayanti3
1Faculty of Medicine, Universitas Surabaya, Indonesia; 2Faculty of Pharmacy, Universitas Surabaya, Indonesia; 3Faculty of Medicine, Universitas Negeri Surabaya, Indonesia
Abstract
Introduction: Healthcare professionals need to advocate for mothers and understand breastfeeding challenges, especially in a community-based culture. We developed a breastfeeding management course for healthcare professionals and students in health-related majors on an online platform at our university. This study aimed to explore what participants learned from an experiential learning assignment to interview mothers regarding their breastfeeding challenges, and write a reflection on it.
Methods: In this qualitative study, we analysed the written reflections of 56 participants after they interviewed mothers regarding their breastfeeding challenges. Thematic analysis and triangulation among the researchers were conducted to obtain themes.
Results: Four themes were identified: (1) differences in knowledge and beliefs about breastfeeding among mothers and their families, (2) breastfeeding challenges that can be a threat to breastfeeding, (3) healthcare professionals’ central role in providing education and advocating for breastfeeding, and (4) involvement of the family and community in breastfeeding education.
Conclusion: This interview and reflective writing assignment strengthened the participants’ awareness of how to advocate for breastfeeding mothers, including considering the influence of the community context.
Keywords: Breastfeeding, Communal Culture, Experiential Learning, Reflective Writing
I. INTRODUCTION
Breastfeeding is a natural method of providing the best nutritional intake for babies’ growth and development, and strengthening the emotional bond between the mother and the baby. The low rate of breastfeeding is a global problem because only less than half of babies under six months of age are exclusively breastfed (Balogun et al., 2015).
Several factors influence breastfeeding, including stigma and support from people closest to the mother. These factors are prominent in communal cultures where the influence of family and community is strong (Susilo et al., 2019). Healthcare professionals can encourage the success of breastfeeding programs by providing education to mothers and their families. Therefore, they need to learn about breastfeeding management and strategies to increase public knowledge. Apropos this, mother-centred advocacy tailored to mothers’ needs can be offered by healthcare professional (Mulcahy et al., 2022).
We developed a breastfeeding management training program for healthcare professionals and students through an online course platform. One of the assignments in this course was to interview breastfeeding mothers and write reflections on their experiences. According to Kolb’s Experiential Learning Theory, this learning activity can help learners conceptualise the essential principles they must master (Yardley et al., 2012). Such a learning activity is innovative and scarcely reported in the existing literature. Additionally, this assignment is novel in the field of breastfeeding-related education. A systematic review of breastfeeding training reported that only one breastfeeding training program used reflective writing (Mulcahy et al., 2022). This study aimed to explore what participants learned from an experiential learning assignment of interviewing mothers on their breastfeeding challenges and writing reflections afterwards.
II. METHODS
This qualitative study used an interpretive descriptive approach to identify themes and patterns among subjective perspectives based on the reflections of breastfeeding management training participants. The training was conducted online through our university’s open online course platform Ubaya Global Academy (UGA). This online course consisted of six sessions and targeted healthcare professionals and students from different domains (medicine, pharmacy, and midwifery). The six sessions were basic science of breastfeeding, common challenges in breastfeeding for healthy mothers (part 1), common challenges in breastfeeding for healthy mothers (part 2), supporting breastfeeding in mothers with specific health issues (non-communicable disease), supporting breastfeeding in mothers with specific health issues (communicable disease), and essential principles in breastfeeding (wrap up and reflection). Students should have completed their first year of education to have basic exposure to health sciences. We invited all participants who had attended the training to participate in this study. At the beginning of the second session, each participant interviewed a mother who had breastfeeding experience, following which, they wrote a reflective writing of 200-500 words.
|
No |
Question |
|
1 |
Why did mothers choose to provide breast milk for babies? |
|
2 |
What were the challenges in the breastfeeding process, and how can they be overcome? |
|
3 |
What food, medicines, or activities do they believe facilitate or inhibit breast milk production (examples of beliefs: eating katuk leaves and breast massage can facilitate breastfeeding)? Where did the mother or partner get this information about food, medicine, and activities? |
Table 1. Interview Questions
We analysed the data using a thematic analysis approach by reading and re-reading the reflective writings, selecting relevant ideas, coding and grouping them according to their similarities, and organising them into themes and subthemes based on the results of interviews and participants’ reflections. Atlas.ti version 24 was used to manage the data. Data triangulation was conducted between researchers by discussing themes and differences until a consensus was reached.
III. RESULTS
Fifty-six participants agreed to participate in the study and completed the interviews. Forty-five of them were from medicine, eight from pharmacy, and three from midwifery. There were variations in participants’ reflective writing, and the following four themes emerged:
A. Differences in Knowledge and Beliefs about Breastfeeding among Mothers and Their Families
Participants reflected that mothers’ knowledge and beliefs about breastfeeding varied depending on the information they received from their surroundings. Family members were their main sources of information on ways to overcome breastfeeding challenges.
‘The mother tried to commit to breastfeeding for six months. But when she fell ill and was weak, she had to give formula milk to the child on the advice of her mother-in-law, but after that, the child did not want to drink breast milk.’ (P24)
B. Breastfeeding Challenges that can be a Threat to Breastfeeding
Participants indicated that mothers faced various obstacles in breastfeeding, such as the pain experienced by them during breastfeeding, which may force them to switch to formula milk. Problems that triggered pain included low milk production, swelling of the breasts, and sore nipples. Mother’s health was also a reason for the people around her to support breastfeeding cessation. Another challenge in breastfeeding was mother’s readiness to breastfeed, particularly for working mothers to manage their time for breastfeeding. Therefore, healthcare professionals should explore the challenges of breastfeeding before providing appropriate advice.
‘In the Integrated Services Post (Posyandu), midwives or health workers can open a special session on questions about breastfeeding.’ (P28)
C. Healthcare Professionals’ Central Role in Providing Education and Advocating for Breastfeeding
Healthcare professionals should have adequate knowledge of breastfeeding management, good communication skills, ability to demonstrate breastfeeding techniques, and educational strategies to the public. They should also involve community leaders and use social media platforms to promote breastfeeding.
‘It is essential for healthcare workers to provide proper education, not endorse and recommend products such as breast milk supplements, whose ingredients and side effects are unknown. Instead, they must teach and provide education on benefits of breastmilk, breast massages which can facilitate mother’s breast milk production, and on managing stress which can impact breast milk production.’ (P48)
D. Involvement of the Family and Community in Breastfeeding Education
Participants reflected that breastfeeding is influenced by cultural aspects; if the mother does not have prior breastfeeding experience, she is likely to believe information provided by the people around her. Hence, apart from the mothers, breastfeeding education must also be extended to companions and families. Such education must include factors to support breastfeeding such as preparation and methods for giving breast milk, and appropriate information about lactation.
‘We as healthcare workers must pick up the ball by providing mass education to the community, especially to family members who are “always” supposed to be listened to. Breastfeeding education will be in vain if we do not educate the public. We are also responsible for the health and quality of the nation’s future generations.’ (P25)
IV. DISCUSSION
Healthcare professionals must possess mother-centred advocacy skills to promote breastfeeding. Increasing their understanding through educational measures is a commitment to achieving better breastfeeding coverage and improving maternal and child health (Mulcahy et al., 2022). In line with the principles of Kolb’s Experiential Learning Theory, the interviews provided authentic exposure to the participants where they could practice skills to explore mothers’ beliefs and knowledge, and develop an empathetic attitude towards mothers’ challenges. The reflection process also enabled them to strengthen their understanding and conceptualise their interpersonal skills and professional development (Yardley et al., 2012).
Participants reflected that knowledge and beliefs of mothers are essential factors in sustaining breastfeeding. Mothers’ lack of independence from family influence and low self-confidence in overcoming challenges are considered to be related to short duration of breastfeeding (Balogun et al., 2015). The communal culture often affects mothers’ decision-making regarding breastfeeding as they are dependent on informal information from the surrounding people. Though this information may help them overcome breastfeeding-related problems, it may not necessarily be evidence-based (Susilo et al., 2019).
Hence, participants were aware of the urgency with which healthcare professionals must act to provide appropriate breastfeeding counselling. This assignment helped them critically think about mothers’ perceptions of challenges in breastfeeding and their own future actions to support breastfeeding. This comprehensive understanding will help promote breastfeeding, by providing mother-centred advocacy and breastfeeding counselling with appropriate advice and anticipatory steps to overcome breastfeeding obstacles (Radzyminski & Callister, 2015).
Our study showed that the participants were motivated to play a central role in supporting breastfeeding mothers. This assignment served as a strong trigger to motivate participants to improve the knowledge about breastfeeding management they would obtain throughout the course.
This study has two limitations. First, the analysis of participants’ awareness was based on their reflective writing skills, which may be diverse as they have not been consistently introduced in academic institutions in Indonesia. This may have influenced how the participants expressed their understanding in their reflective writing. Oral reflections can yield different themes. Second, this study focused only on the interviews and reflective writing assignments of the course, as we believe that an intensive look at these would provide valuable lessons. Triangulation with other data is necessary to determine the effectiveness of the entire course.
V. CONCLUSION
An assignment based on experiential learning principles made participants aware of the diversity of knowledge and beliefs of breastfeeding mothers in a communal culture and the potential challenges for mothers deciding to stop breastfeeding. The reflection process motivated them to learn about mother-centred advocacy for breastfeeding mothers and their surroundings.
Notes on Contributors
Astrid Pratidina Susilo designed the study, conducted the data collection and analysis, and drafted the manuscript.
Lucia Pudyastuti Retnaningtyas designed the study, conducted the data collection and analysis, and reviewed the manuscript.
Lisa Aditama designed the study, conducted the data collection, and reviewed the manuscript.
Karunia Wijayanti designed the study, conducted the data analysis, and drafted the manuscript.
Ethical Approval
This study was approved by the institutional ethics committee of Universitas Surabaya (No. 179/KE/VII/2023). All the participants provided written informed consent.
Data Availability
We do not share the raw data as the reflective writing assignments were in Indonesian. Readers who are interested in accessing the data can contact the author.
Acknowledgement
We are grateful to the Ubaya Global Academy (UGA) management team for supporting the development and implementation of this online course. We also thank Santi Desi, Denny Herliana, and Laurentia Audi Agatha for their administrative support for this study. This study was presented at the International Conference of the AMEE 2024.
Funding
This research was supported by the Ministry of Education, Culture, Research, and Technology of Indonesia (Grant Number 109/E5/PG.02.00.PL/2024).
Declaration of Interest
No potential conflicts of interest are relevant to this article.
References
Balogun, O. O., Dagvadorj, A., Anigo, K. M., Ota, E., & Sasaki, S. (2015). Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: A quantitative and qualitative systematic review. Maternal & Child Nutrition, 11(4), 433-451. https://doi.org/10.1111/mcn.12180
Mulcahy, H., Philpott, L. F., O’Driscoll, M., Bradley, R., & Leahy-Warren, P. (2022). Breastfeeding skills training for health care professionals: A systematic review. Heliyon, 8(11). https://doi.org/10.1016/j.heliyon.2022.e11747
Radzyminski, S., & Callister, L. C. (2015). Health professionals’ attitudes and beliefs about breastfeeding. The Journal of Perinatal Education, 24(2), 102-109. https://doi.org/10.1891/1058-1243.24.2.102
Susilo, A. P., Marjadi, B., Dalen, J. V., & Scherpbier, A. (2019). Patients decision-making in the informed consent process in a hierarchical and communal culture. The Asia Pacific Scholar, 4(3), 57-66. https://doi.org/10.29060/TAPS.2019-4-3/OA2085
Yardley, S., Teunissen, P. W., & Dornan, T. (2012). Experiential learning: AMEE guide No. 63. Medical Teacher, 34(2), e102-e115. https://doi.org/10.3109/0142159X.2012.650741
*Lucia Pudyastuti Retnaningtyas
Faculty of Medicine, University Surabaya, Indonesia
Jl. Raya Kalirungkut, Surabaya 60293
+628113113338
Email: luciaretnaningtyas@staff.ubaya.ac.id
Submitted: 9 October 2024
Accepted: 25 July 2025
Published online: 7 October, TAPS 2025, 10(4), 90-93
https://doi.org/10.29060/TAPS.2025-10-4/II3539
Shigeki Matsubara
Department of Obstetrics and Gynaecology, Jichi Medical University, Japan; Department of Obstetrics and Gynaecology, Koga Red Cross Hospital, Japan; Medical Examination Centre, Ibaraki Western Medical Centre, Japan
I. INTRODUCTION
The concept of “gamification” has been introduced to medical education: game elements employed for education enhance learning outcomes by making the educational process more interactive and engaging (Lee et al., 2025). Various games have been introduced—serious games, escape rooms, simulation games, and others. Although the theoretical underpinnings of why “gamification” improves educational outcomes are not yet fully clarified, incorporating game mechanics into medical education appears to enhance learner motivation, engagement, and performance, particularly in teaching clinical reasoning and collaborative decision-making (Lee et al., 2025).
In this manuscript, I wish to introduce the application of “gamification” to medical meetings, especially from the viewpoint of the audience. More accurately, I have been practicing it for 30 years—long before the term “gamification” became widely recognised. Here, “gamification” does not refer to a systematic process involving meeting stakeholders, but rather to the individual audience member’s attitude toward how to attend. I believe that “gamification” activates attendees and benefits them: it helps them remain well informed in the face of ever-expanding knowledge.
Medical meetings consist of the audience, presenter, chairperson, and organizers. While some publications focus on how to deliver an effective presentation (Nundy et al., 2022), it is crucial to recognize that the top priority should be the audience (Matsubara & Matsubara, 2024a). A previous report suggested that presenters and chairpersons could activate audience-friendly meetings (Matsubara & Matsubara, 2024a). However, practical suggestions for the audience remain relatively scarce. Some literature merely advises: “Be an active learner; ask questions” (Fisher & Trautner, 2022). To my knowledge, there is limited evidence on whether “active learning and active asking” are truly lacking in real-world settings, and if so, what barriers may underlie this. If the absence of “gamification” factors partly contributes to these barriers, then the present proposal may become more reasonable and persuasive. That said, this proposal is not primarily based on such reasoning. But indeed, publications on active learning and active asking from the viewpoint of “gamification” are lacking, and senior staff are less likely to provide practical advice. Thus, audience members, especially younger generations, may receive little guidance on how to participate effectively in scientific meetings.
I propose a new way of how audiences actively participate in medical meetings. Based on my decade-long experience, I focus on two elements: “listening” and “asking”. These two actions are, I believe, the essence of audience participation. My proposal is to incorporate the concept of “gamification” into personal “listening and asking” activity.
II. “LISTENING”: EFFECTIVE KNOWLEDGE ACQUISITION AT MEDICAL MEETINGS
When I was younger, I took notes on everything and tried to memorise the data presented. For example, I wrote down, “Methotrexate 50 mg cured ectopic pregnancy”. While this approach might work for some, I found that for me, this classroom-like method was neither effective nor reliable. It exhausted my physical and mental energy, sometimes leading to the retention of inaccurate information.
Around 30 years ago, I changed my style. I began to approach meetings as if they were a “game”, the concept now acknowledged as “gamification”. The night before the scientific or medical meetings, I quickly glanced through the program listing titles of the presentations (and abstracts, if available) to form a rough idea of the topics, ignoring details. Before the session starts, I read the presentation titles, for example, “Methotrexate for ectopic pregnancy,” and came up with some likely scenarios (A, B, or C) that the presenter might discuss, akin to forming a hypothesis. If the presenter confirmed scenario A, I thought, “Got it!”. After the presentation, I created a one-line conclusion based on my interpretation, which might align with or differ from the presenter’s. Importantly, this conclusion should always be in my own words (Tip 1 and Additional Notes in the Appendix).
I always did this and made it a routine for medical or scientific meetings. It was useful to skim the titles or abstracts beforehand to become familiar with the field. This enabled me to predict what the presenter might say. Afterwards, I summarised the presentation in my own words. This process mirrors manuscript writing, where I gather general knowledge, form a hypothesis, and craft a key message—essential steps for completing a successful paper (Matsubara & Matsubara, 2024b). Thus, listening to presentations served as practice for writing manuscripts. This procedure changed my attitude toward scientific meetings, and even improved my paper productivity. I began to look forward to the next meeting, anticipating the new ideas I might encounter. I became an active audience member. The one-line conclusion made me continue contemplating whether my interpretation was correct. Even after the meetings, I repeatedly glanced at it, and sometimes a new idea or concept emerged from that single line, which triggered me to write some papers. Thus, this “gamification” concept in listening was effective not only during the scientific meeting but also afterwards. As described, “gamification” has now been widely discussed as an effective measure in medical education (Lee et al., 2025). Here, I propose that involving the concept of “gamification” at a personal level may enhance active participation in scientific meetings, and thereby support life-long learning.
Why not view medical meetings as a “game” rather than a mere duty? This perspective helped me stay relaxed and engaged throughout the session. It renewed my knowledge base and offered a chance for manuscript-writing practice.
III. VALUABLE QUESTIONS AND COMMENTS TO ACTIVATE MEETINGS
Asking questions not only deepens one’s understanding, but also helps activate the meeting itself. The following suggestions may be particularly useful for senior attendants, including meeting leaders, but they are equally relevant to the general audience, including the younger generation.
Valuable questions can:
- help clarify knowledge for the audience and enhance their understanding,
- increase the significance of the study being discussed. Here, “questions” can also refer to general remarks about the presentation.
Some studies present an incorrect message regarding treatment recommendations, which less-experienced doctors may apply without question. Ask questions to clarify. Some presenters may refrain from stating a clear conclusion. Ask for a tentative conclusion. These kinds of questions may also be considered, in a broader sense, a form of “gamification”: such questions can open further discussion and, in that sense, the questioner could act as a “game changer”.
Questions often increase the significance of a study. For example, ask if there’s another relevant interpretation of the data, if similar studies exist that the presenter might not be aware of, or if there are historical perspectives on the issue. Cross-disciplinary perspectives are often useful. For example, perspectives from fields like neurosurgery, gastroenterology, or urology can activate discussions in psychiatry, endoscopy, or nephrology meetings, respectively. Please focus on asking questions that relate to the study’s significance, rather than those solely of personal interest. This approach is akin to how a chairperson should handle the question-answer sessions (Matsubara & Matsubara, 2024a) (Tip 2 and Additional Notes in the Appendix).
Questions can complement presentations much like correspondences enrich published articles by offering additional perspectives. Good questions prompt the presenter and audience to recognise further significance in the presentation. This benefits everyone—the questioner, the presenter, and the general audience. This situation mirrors how good correspondence enriches all parties involved in the academic discussion.
IV. CONCLUSION: PASSING ON THE EXPERIENCE TO THE NEXT GENERATION
I propose a change in perspective: learning at scientific meetings should be viewed as a game. “Listening” and “asking” share similarities with writing a paper. Having a bird’s-eye view, crafting a hypothesis, and forming a key message are essential for both “effective attendance to meetings” and paper writing (Matsubara & Matsubara, 2024b). A good question is like a brief, insightful correspondence. Thus, making an effort to be a good audience also nurtures good researchers and writers.
Finally, I would like to add that, medical meetings provide opportunities not only to gain knowledge, but also to engage in face-to-face communication. Making acquaintances there may broaden future research opportunities, which is especially important for younger physicians. A positive meeting atmosphere encourages such communication. I believe that good “listening” and thoughtful “asking” contribute to this. Active listening and well-considered questions benefit all participants in three ways: deepening understanding for those who ask, helping everyone grasp the presentation’s significance, and fostering a welcoming atmosphere.
Having participated in numerous meetings, I’ve developed this perspective. It’s unclear whether some hierarchical or systemic influences hinder “natural” listening and asking, especially among younger generations. If so, how best to address them should be studied. Regardless, we, as meeting participants, should cultivate the sensitivity to recognise a question that sparks a game-changing moment. I believe the present description offers a way to fully engage in medical and scientific meetings by viewing them as a “game”. This approach has helped me grow as a researcher-physician, contributing to the publication of over 600 PubMed-indexed papers. Thus, for me, this method is time-tested. I believe seasoned doctors like myself have a responsibility to pass on their experiences to the next generation. I invite you to try my perspective, and hope that it serves as a platform for further discussion.
Notes on Contributors
Shigeki Matsubara reviewed the literature, made the concept, wrote and edited the manuscript.
Acknowledgement
I thank Professor Shinya Ito (University of Toronto, Canada), Professor Yasushi Matsuyama (Jichi Medical Univeristy, Japan), and Teppei Matsubara (Harvard Medical School, USA), for their critical reading of this manuscript.
Funding
There are no funding sources for this paper.
Declaration of Interest
Shigeki Matsubara has no conflict of interest to declare.
References
Fisher, J.W. & Trautner, B.W. (2022). Maximizing the academic conference experience: Tips for your career toolkit. Journal of Graduate Medical Education, 14(2), 144-148. https://doi.org/10.4300/jgme-d-21-00943.1
Lee, C.Y., Lee, C.H., Lai, H.Y., Chen, P.J., Chen, M.M., & Yau, S.Y. (2025). Emerging trends in gamification for clinical reasoning education: A scoping review. BMC Medical Education, 25(1), 435. https://doi.org/10.1186/s12909-025-07044-7
Matsubara, S., & Matsubara, D. (2024a). An audience-friendly medical meeting: A good presentation and chairpersonship. JMA journal, 7(3), 406-409. https://doi.org/10.31662/jmaj.2023-0219
Matsubara, S., & Matsubara, D. (2024b). A checklist confirming whether a manuscript for submission adheres to the fundamentals of academic writing: A proposal. JMA journal, 7(2), 276-278. https://doi.org/10.31662/jmaj.2023-0201
Nundy, S., Kakar, A., & Bhutta, Z.A. (2022). How to give an oral presentation? In Nundy S., Kakar A., & Bhutta Z.A. (Eds.), How to practice academic medicine and publish from developing countries?: A practical guide (pp. 357-366). Springer Nature. https://doi.org/10.1007/978-981-16-5248-6
*Shigeki Matsubara
Department of Obstetrics and Gynaecology,
Jichi Medical University
3311-1 Yakushiji, Shimotsuke, Tochigi 329-0498, Japan
Email: matsushi@jichi.ac.jp
Submitted: 30 December 2024
Accepted: 5 July 2025
Published online: 7 October, TAPS 2025, 10(4), 63-72
https://doi.org/10.29060/TAPS.2025-10-4/OA3777
Chollada Sorasak1, Worayuth Nak-Ai2, Choosak Yuennan3 & Mansuang Wongsapai1
1Intercountry Centre for Oral Health, Department of Health, Thailand; 2Sirindhorn College of Public Health Chonburi, Praboromarajchanok Institute, Thailand; 3Boromarajonani College of Nursing Chiang Mai, Praboromarajchanok Institute, Thailand
Abstract
Introduction: Nutrition literacy represents a critical determinant of oral health outcomes. Guided by Social Cognitive Theory and the Nutrition Literacy Skills Framework, this study evaluated the implementation and effectiveness of a nutrition literacy programme for oral health promotion among village health volunteers (VHVs), key implementers in Thailand’s healthcare system, during January to December 2024.
Methods: A convergent parallel mixed-methods design was employed to address existing methodological gaps in nutrition literacy research. The quantitative component comprised a cross-sectional survey (N=60 VHVs trained in January 2024) and clinical outcome monitoring via electronic health records. The qualitative strand involved a multi-case study approach with purposive sampling (n=20) through in-depth interviews. Data collection occurred at 6-month post-implementation (July 2024), with clinical monitoring through December 2024. Analysis integrated descriptive and inferential statistics with thematic analysis.
Results: Post-implementation analysis revealed significantly enhanced nutrition literacy skills (M=4.14, SD=0.414), with notable improvements in communication (M=4.74, SD=0.511) and implementation (M=4.21, SD=0.440). All six nutrition literacy domains showed strong correlations (r=0.712-0.868, p<.01), supporting the framework’s interconnected nature. Clinical outcomes improved significantly: oral health check-up rates increased from 1.41% to 2.61% (p<.05), and functional teeth retention rose from 87.36% to 92.72% (p<.01). Qualitative findings revealed adaptive knowledge transfer methods and context-specific implementation strategies influenced by community readiness.
Conclusion: Through comprehensive mixed-methods evaluation, the 12-month implementation data demonstrated significant improvements in both VHVs’ nutrition literacy skills and clinical oral health outcomes. Success factors included theoretically-grounded implementation strategies and stakeholder engagement in resource-limited settings.
Keywords: Convergent Parallel, Health Literacy, Mixed Methods, Nutrition, Oral Health, Thailand, Village Health Volunteer
Practice Highlights
- Nutrition literacy among VHVs significantly improved across all six key domains.
- Oral health check-up rates increased from 41% to 2.61% post-programme implementation.
- Functional teeth retention rose from 36% to 92.72% over the 12-month period.
- VHVs used context-specific strategies for community-based nutrition education.
I. INTRODUCTION
Oral health is fundamentally linked to nutrition and dietary behaviours, yet nutritional factors affecting oral health remain a significant public health challenge worldwide, particularly in low- and middle-income countries (Peres et al., 2019; Watt et al., 2019). In Thailand, the high prevalence of dental caries and periodontal diseases related to dietary habits (Chaianant et al., 2022), underscores the urgent need for effective nutrition education strategies for oral health promotion.
Understanding the relationship between nutrition literacy and oral health behaviours requires consideration of multiple theoretical perspectives. Social Cognitive Theory (Bandura, 2004) highlights how personal factors, dietary patterns, and environments interact to shape oral health behaviours, particularly relevant in Thailand’s family-based eating culture. The nutrition literacy skills Framework (Squiers et al., 2012) outlines how individuals develop and apply nutrition literacy competencies through interactions between dietary knowledge and social environments. Additionally, Ecological Systems Theory (Bronfenbrenner, 1979) demonstrates how family and societal systems influence health behaviours and programme implementation.
Within this theoretical context, nutrition literacy for oral health emerges as a critical determinant of oral health outcomes. While health literacy encompasses capacities for accessing and using health information (Sørensen et al., 2012), nutrition literacy for oral health specifically focuses on these competencies in oral healthcare. Evidence consistently shows that individuals with low nutrition literacy tend to exhibit poor oral health behaviours and outcomes (Berkman et al., 2011; Kickbusch et al., 2013). This relationship is particularly significant in reducing oral health disparities (Horowitz & Kleinman, 2012), with higher nutrition literacy correlating with improved oral hygiene practices and health outcomes (Baskaradoss, 2018).
Recent advances in nutrition literacy programmes for oral health promotion have revealed that culturally tailored, context-specific interventions can significantly enhance service accessibility and oral healthcare engagement (Macek et al., 2016). Various programme modalities have emerged, encompassing educational initiatives, community-based activities, and digital media interventions (Dickson-Swift et al., 2014). These approaches align well with Thailand’s dental public health policy, which emphasises proactive oral health promotion and community participation. Systematic review (Firmino et al., 2017) identified several critical gaps in existing research: the absence of mixed-methods studies examining both programme effectiveness and change processes, limited analysis of community-level behavioural change mechanisms, and insufficient research in resource-constrained developing countries where success factors may differ substantially from developed nations.
To address these research gaps, this study aims to evaluate the effectiveness of a nutrition literacy programme for oral health promotion in Thailand’s context. Of particular interest is the role of VHVs as key implementation agents, given their established position in community health promotion (Kowitt et al., 2015). While previous research has demonstrated VHVs’ capacity to utilise technology for expanding health service coverage (Jandee et al., 2015), empirical evidence regarding their role in promoting nutrition literacy for oral health remains limited.
Guided by our theoretical framework, we employed a Convergent Parallel Mixed Methods design (Creswell & Plano Clark, 2017), enabling comprehensive assessment of both quantitative programme effectiveness and qualitative change mechanisms. This approach examines how social modelling, nutrition literacy skill development related to oral health, and environmental factors interact to influence programme outcomes. Ultimately, this study’s findings will contribute to developing contextually appropriate nutrition literacy strategies for oral health promotion in developing countries while aligning with Thailand’s dental public health policies.
II. METHODS
A. Study Design
This study employed a convergent parallel mixed methods design (Creswell & Plano Clark, 2017) to comprehensively evaluate the implementation and effectiveness of a nutrition literacy programme for oral health promotion. The design integrated quantitative outcomes with qualitative insights to achieve deeper understanding than single-method approaches. The quantitative component utilised a cross-sectional survey to assess nutrition literacy skills and clinical outcomes, while the qualitative component employed a multi-case study approach (Yin, 2018) to explore implementation experiences and contextual factors.
B. Population and Sampling
The quantitative phase included all VHVs who completed nutrition literacy training (N=60) in January 2024, with data collection occurring in July 2024. For the qualitative component, 20 VHVs were purposively selected using intensity sampling (Miles et al., 2013) based on four criteria: programme implementation experience exceeding six months, strong communication abilities, representation from varied performance areas, and voluntary informed consent. This sample size achieved theoretical saturation (Creswell, 2013; Guest et al., 2006). Gender distribution differed between samples (quantitative: 98.3% female; qualitative: 70% female) due to purposive sampling for diverse leadership perspectives. Sensitivity analysis confirmed no significant gender-based differences in primary outcomes (p > .05). The six-month assessment period aligned with established behaviour change evaluation timeframes (Glasgow et al., 2019), while monitoring through December 2024 captured seasonal variations and sustainability data.
C. Research Instruments
Two complementary instruments were developed and validated through pilot testing with 30 VHVs sharing similar characteristics with the target population, but excluded from the final sample. The questionnaire was designed according to Nutbeam’s health literacy framework (Nutbeam, 2000), operationalizing three literacy levels into six nutrition literacy components relevant to oral health promotion. Items utilised a five-point Likert scale (1 = “not confident at all” to 5 = “very confident”) for self-assessment of perceived competencies. A panel of five experts including community dentistry, nutrition, public health, health literacy, and health communication specialists assessed content validity, achieving a high IOC index of 0.96, while internal consistency demonstrated excellent reliability (Cronbach’s alpha = 0.929).
The structured interview guide explored knowledge application, teaching methods, implementation challenges, outcomes, and recommendations following established qualitative research principles (Jacob & Furgerson, 2012). Qualitative trustworthiness was ensured through member checking at two stages: during interviews for immediate verification and after preliminary analysis with eight selected participants for validation and refinement.
D. Data Collection
Baseline data was collected prior to programme implementation in January 2024, establishing pre-intervention metrics through public health service records. Following six-month implementation, parallel quantitative and qualitative assessments were conducted in July 2024. Self-assessment questionnaires were administered to all VHVs, followed by in-depth interviews (45-60 minutes) with 20 purposively selected participants until data saturation was achieved (Guest et al., 2006). In accordance with Consolidated Criteria for Reporting Qualitative Studies (COREQ) guidelines (Zachariah et al., 2024), participant confidentiality was maintained throughout the study, with written informed consent obtained after comprehensive briefing on study objectives and participant rights. Monthly data extraction from the Health Data Centre continued through December 2024 to capture sustained programme effects, with systematic collection on the 5th of each month ensuring complete and timely data acquisition.
E. Data Analysis
The analytical approach integrated multiple complementary methods for comprehensive understanding. Quantitative analysis included descriptive statistics (frequencies, percentages, means, standard deviations) with Shapiro-Wilk normality testing. Inferential analyses comprised paired t-tests for pre-post comparisons (α = 0.05), chi-square tests for categorical outcomes, and Pearson’s correlation coefficients examining relationships between nutrition literacy domains. Effect sizes were reported using Cohen’s d with bootstrap confidence intervals (1,000 resamples). Statistical analyses utilised IBM’s Statistical Package for the Social Sciences (SPSS) Statistics software. Missing data patterns were examined using Little’s Missing Completely at Random (MCAR) test, with multiple imputation (5 datasets) addressing missing values following Rubin’s guidelines (2004). Sensitivity analyses compared complete-case and imputed datasets (van Buuren, 2018).
Qualitative data underwent thematic analysis following established frameworks (Braun & Clarke, 2006), involving verbatim transcription, independent coding by two researchers, and iterative thematic framework development through consensus meetings. ATLAS.ti software facilitated systematic organisation and analysis. Quality assurance included investigator triangulation, member checking with eight participants, audit trail documentation, and researcher reflexivity journals.
F. Data Integration
A comprehensive integration strategy synthesised quantitative and qualitative findings through three interconnected phases (Cano & Lomibao, 2023). Joint displays facilitated systematic comparison of results, enabling identification of convergent and divergent patterns. Meta-inferences were constructed through iterative cross-method analysis, with attention to complementary insights. Pattern matching techniques examined alignments between quantitative outcomes and qualitative themes, developing integrated theoretical understandings. Conflicting findings were reconciled by contextualising quantitative results with qualitative explanations, while complementary data enriched overall interpretation, enhancing study rigor and validity.
III. RESULTS
All participants (N=60) completed quantitative assessments at baseline and a 6-month follow-up, with 20 VHVs participating in qualitative interviews. Clinical outcomes were monitored through December 2024 using complete Health Data Centre monthly data. Following convergent parallel design, quantitative and qualitative data streams were systematically merged to achieve comprehensive understanding of programme implementation and outcomes. The integrated analysis revealed that communication skills improvements were explained through qualitative evidence of adaptive teaching strategies, while regional outcome variations were illuminated by implementation challenges identified through qualitative inquiry. This systematic data merging approach provided richer insights than either quantitative or qualitative methods could offer independently.
A. Baseline Characteristics
1. Qualitative Sample (n = 20)
The qualitative sample achieved a full response rate (100%). Participants were predominantly female (70%), with males comprising 30%. The age distribution showed that 70% were between 50–60 years, while 15% each were aged 30–39 and 40–49 years. No participants were over 60. In terms of role, 65% served as Village Health Volunteers (VHVs), and 35% were Caregivers. None held dual roles.
2. Quantitative Sample (n = 60)
The quantitative sample also achieved a 100% response rate. Females constituted the vast majority (98.3%), with only one male respondent (1.7%). Most participants (70%) were aged 50–60 years, with smaller proportions aged 30–39 (11.7%), 40–49 (16.7%), and over 60 (1.7%). Regarding position, 85% were VHVs, 13.3% were Caregivers, and 1.7% held both roles.
B. Programme Implementation and Nutrition Literacy Skills for Oral Health
The intervention (Table 1) demonstrated significant improvements across all six nutrition literacy domains (p< 0.001) with large effect sizes. Communication skills showed the greatest improvement (d = 1.64, mean difference: 0.84 points, 95% CI: 0.66-1.02), followed by Decision Making (d = 0.90), Critical Inquiry (d = 0.88), Understanding (d = 0.85), Application (d = 0.77), and Access (d = 0.74). Other domains improved by 0.36-0.41 points.
C. Clinical Outcomes and Programme Effectiveness
Clinical outcomes significantly improved. Dental check-up rates increased from 1.41% to 2.61% (difference: 1.20 percentage points, 95% CI: 0.90-1.50, p=0.032). Participants with ≥20 functional teeth rose from 87.36% to 92.72% (difference: 5.36 percentage points, 95% CI: 3.38-7.34, p< 0.001), indicating substantial improvements in both knowledge and oral health behaviour.
|
Outcomes |
Baseline (mean±SD) |
6-month (mean±SD) |
Mean difference (95% CI) |
p-value |
|
Nutrition Literacy Skills |
||||
|
Access |
3.80±0.50 |
4.16±0.47 |
0.36 (0.19, 0.53) |
<0.001† |
|
Understanding |
3.75±0.48 |
4.15±0.46 |
0.40 (0.23, 0.57) |
<0.001† |
|
Critical Inquiry |
3.70±0.47 |
4.11±0.46 |
0.41 (0.24, 0.58) |
<0.001† |
|
Decision Making |
3.72±0.46 |
4.13±0.45 |
0.41 (0.25, 0.57) |
<0.001† |
|
Application |
3.85±0.49 |
4.21±0.44 |
0.36 (0.19, 0.53) |
<0.001† |
|
Communication |
3.90±0.52 |
4.74±0.51 |
0.84 (0.66, 1.02) |
<0.001† |
|
Clinical Outcomes |
||||
|
Dental check-up rate (%) |
1.41 |
2.61 |
1.20 (0.90, 1.50) |
0.032‡ |
|
Functional teeth (%) * |
87.36 |
92.72 |
5.36 (3.38, 7.34) |
<0.001‡ |
Note: *Defined as having ≥20 functional natural teeth
†Statistically significant at p< 0.001, Paired t-test
‡Statistically significant at p< .05 for dental check-up rate and p< 0.001 for functional teeth, Chi-square test
Data were retrieved from the Health Data Centre database (Ministry of Public Health, 2024).
Table 1. Changes in Nutrition Literacy Skills Related to Oral Health and Clinical Outcomes After a 6-Month Training Programme (N=60)
|
Health Literacy Domain |
1. Access |
2. |
3. |
4. |
5. Application |
6. Communication |
|
1. |
1 |
|||||
|
2. |
.858** |
1 |
||||
|
3. |
.753** |
.712** |
1 |
|||
|
4. |
.775** |
.817** |
.834** |
1 |
||
|
5. |
.724** |
.770** |
.797** |
.797** |
1 |
|
|
6. |
.812** |
.820** |
.822** |
.868** |
.799** |
1 |
Note: N = 60; **p < .01 (2-tailed) Pearson correlation coefficients are shown.
Table 2. Correlation Analysis of Nutrition Literacy Domains Related to Oral Health
Regional variations in dental check-up rates were substantial, ranging from 0.07% to 38.18% (p < 0.001) across participating health centres, suggesting the need to investigate factors contributing to different implementation outcomes despite similar geographical and healthcare delivery contexts.
The findings support overall programme effectiveness, though the cross-sectional design indicates the need for longitudinal research to confirm long-term impacts. Future nutrition literacy programmes for oral health promotion should emphasize communication skills and context-specific implementation approaches. The qualitative analysis of 20 VHV interviews yielded four main themes (Figure 1).

Figure 1. Qualitative final thematic map
D. Implementation Process and Contextual Factors
1. Knowledge Transfer Patterns
VHVs utilised multiple communication channels and diverse pedagogical approaches. Individual consultations involved direct problem assessment, with participants noting “Face-to-face, asking what problems they have, like sensitive teeth” (P15). Digital platforms expanded reach through “Online communication and inviting others to join our Line group” (P5). Teaching methods included demonstrations, mnemonics, and hands-on practice.
2. Audience Diversity
VHVs encountered heterogeneous learning populations with varying engagement levels. Successful interactions were characterised by high comprehension rates: “Everyone understood and could practice, no problems as they all understood well” (P19). However, engagement challenges persisted, with some noting “One person at home is not very interested” (P16).
3. Implementation Challenges
Communication barriers emerged as significant obstacles. VHVs identified hearing difficulties: “The listener’s hearing, they can’t hear well” (P1), language barriers: “Don’t use too many English terms, some words are not understood” (P10), and content complexity issues: “Some content is difficult to understand, takes a long time and repeated study” (P14).
4. Development Approaches
VHVs suggested practical improvements emphasising “Should practice more than theory” (P1). They recommended age-appropriate strategies: “Elderly may have difficulty learning, but if we can make content easy to understand, they will gain knowledge too” (P15), and streamlined delivery: “Shorter courses might attract more participants” (P5).
E. Integrated Results
The convergent parallel design employed a merging data integration approach to synthesise quantitative and qualitative findings systematically, providing comprehensive understanding of programme effectiveness., as presented in Table 3.
|
Major Themes |
Quantitative |
Qualitative |
Meta-inference |
|
Nutrition Literacy Skills Performance Related to Oral Health |
Overall implementation: M=4.14±0.41, p< 0.001; Highest in communication (M=4.74±0.51); Strong inter-skill correlations (r=.712-.868, p< 0.001) |
Demonstrated multiple teaching approaches: individual counselling, memory techniques, continuous monitoring |
Quantitative high scores validated by qualitative evidence of practical skill application |
|
Clinical Outcome Changes |
Dental check-up: 1.41% to 2.61% (p< .01); Functional teeth: 87.36% to 92.72% (p< .01); Regional variation: 0.07-38.18% |
Implementation variations: successful behaviour adoption, mixed community readiness, diverse response levels |
Outcome improvements linked to implementation quality and community readiness |
|
Implementation Challenges |
Highest in self-monitoring (M=4.25±0.44); Significant regional differences (p< .01) |
Identified barriers: technical language, age-related learning, practice compliance |
Statistical variations explained by specific implementation challenges identified qualitatively |
|
Support Systems |
Strong correlations between: decision-making and communication (r=.868); access and understanding (r=.858); all p< 0.001 |
Multiple support channels: digital platforms, family networks, community groups |
Integrated support systems crucial for programme effectiveness |
Table 3. Integrated Analysis of Mixed Methods Results
The systematic merging of quantitative and qualitative data through meta-inference analysis revealed four key dimensions of programme implementation and outcomes.
1. Nutrition Literacy Skills and Clinical Outcomes
Quantitative findings demonstrated high overall implementation levels (M=4.14±0.41, p< 0.001), with communication skills showing exceptional improvement (M=4.74±0.51). The strong correlation between communication and decision-making skills (r=.868, p< 0.001) was validated through qualitative evidence: “We adapted communication methods based on audience needs” (P15).
Dental check-up rates increased significantly from 1.41% to 2.61% (p< .01), while functional dentition improved from 87.36% to 92.72% (p< .01). Qualitative insights revealed implementation quality influences: “Regular follow-ups and practical demonstrations helped maintain behaviour changes” (P8). Regional outcome variations (0.07-38.18%) aligned with identified barriers and facilitators.
2. Implementation Dynamics and Support Systems
Strong correlations between access and understanding (r=.858, p< 0.001) were complemented by contextual adaptation findings. VHVs balanced cultural factors: “We needed to balance traditional beliefs with modern dental care practices” (P13). Statistical associations among nutrition literacy domains (r=.712-.868, all p< 0.001) were substantiated by interconnected support mechanisms: “The combination of in-person support and online reminders helped maintain engagement” (P5).
The meta-inference demonstrates programme effectiveness through synergy of enhanced nutrition literacy skills and context-sensitive implementation strategies, emerging through systematic integration of quantitative measurements with qualitative insights.
IV. DISCUSSION
A. Programme Effectiveness and Theoretical Framework
This study demonstrates the effectiveness of a Village Health Volunteers (VHVs)-led nutrition literacy programme for oral health promotion in significantly improving nutrition literacy skills and clinical outcomes. The findings align with established empirical evidence at regional and international levels regarding healthcare personnel capacity development and relationships between nutrition literacy for oral health, oral health behaviours, and preventive service utilisation (Baskaradoss, 2018; Nutbeam, 2008; Samarasekera et al., 2024; Batista et al., 2017; Baskaradoss, 2016).
The strong correlation between nutrition literacy components, particularly communication and decision-making (r = .868), reflects their interconnected nature and underscores comprehensive skill development importance (Kunathum, 2023). This finding aligns with Social Cognitive Theory (Bandura, 2004), emphasising behavioural, personal, and environmental factor interdependence in health promotion. Results support the Nutrition Literacy Skills Framework (Squiers et al., 2012), positioning communication and decision-making as essential mediators between nutrition literacy and oral health behavioural outcomes in diverse cultural contexts.
B. Clinical Outcomes and Community Engagement
The increase in dental check-up rates from 1.41% to 2.61%, while statistically significant, represents modest absolute change. However, within rural communities where oral health service access is severely limited and baseline utilisation extremely low, even small improvements may represent important community health engagement shifts (Petersen, 2009). This suggests early evidence of improved health literacy and behaviour change among participants, particularly VHVs who played critical implementation roles.
Future interventions could incorporate community-based incentives, outreach dental services, and proactive VHV follow-up to reinforce preventive behaviours. Evidence demonstrates that community mobilisation and culturally tailored interventions effectively improve oral health behaviours in low-resource settings (Fisher-Owens et al., 2013; Watt, 2007).
C. Domain-Specific Performance and Regional Variations
Communication and skill application emerged as key behavioural change drivers in nutrition literacy for oral health (M = 4.74, SD = 0.51 and M = 4.21, SD = 0.44 respectively). The relatively lower scores in critical inquiry (M = 4.11, SD = 0.46) and decision-making (M = 4.13, SD = 0.45) skills align with identified community health worker limitations (Gall et al., 2023) and indicate the necessity of incorporating hybrid learning approaches to strengthen advanced nutrition literacy competencies (Lin et al., 2024).
Regional analysis revealed significant outcome variations across implementation areas (0.07% to 38.18%, p < .01) (Watt et al., 2019), with stronger outcomes in communities with higher social capital. This pattern aligns with systematic reviews from low- and middle-income countries (Haldane et al., 2019) and documented disparities in Thailand’s healthcare systems (Chaianant et al., 2022). These findings support Asset-Based Community Development theory (Kretzmann & McKnight, 1993), emphasising the importance of leveraging existing community strengths for sustainable oral health improvements.
D. Social Support Systems and Cultural Context
Social support systems proved crucial for programme success, particularly in developing countries where social networks, family support systems, and community resources serve as primary health determinants (Kowitt et al., 2015). The strong correlation between communication and community participation (r = .799, p < .01) reflects these interconnections, aligning with Ecological Systems Theory (Bronfenbrenner, 1979), which emphasises how multiple environmental layers influence nutrition-related oral health behaviours in developing countries where community and cultural contexts play crucial roles.
E. Gender Considerations and Methodological Considerations
The quantitative sample exhibited significant gender imbalance (98.3% female participants), potentially influencing generalisability. In Northern Thailand, approximately 83% of VHVs are female, reflecting traditional social roles where women are often a group highly motivated to engage in volunteer work aimed at assisting others. Furthermore, women’s volunteer roles frequently involve healthcare and activities related to building community resilience (Sukhampha et al., 2023). Women typically exhibit higher health awareness and more proactive health behaviours than men, which may partly explain observed positive outcomes (Tan et al., 2021).
The notably high correlations between nutrition literacy domains (r=0.712-0.868) reflect comprehensive skill development influenced by the holistic training programme and Thai VHVs’ cultural context where integrated health communication is traditionally emphasised. This finding aligns with studies in Asian contexts (Leung et al., 2020; Oh et al., 2022) suggesting important cultural influences on health literacy skill development.
F. Study Strengths and Limitations
This study demonstrates methodological strengths through its convergent parallel mixed-methods design with systematic data integration, enhancing understanding through integrated quantitative and qualitative insights. The qualitative component achieved theoretical saturation (Guest et al., 2006), while community-based implementation aligned with established nutrition literacy research practices (Kowitt et al., 2015).
Key limitations include absence of factor analysis despite high internal consistency (Cronbach’s α = 0.929), pronounced gender imbalance restricting applicability, six-month follow-up potentially inadequate for capturing long-term changes (Baskaradoss, 2018), self-reported data risks and social desirability bias (Althubaiti, 2016), geographical specificity limiting generalisability given Thailand’s varied healthcare systems (Chaianant et al., 2022), and resource constraints precluding randomised controlled design. While the dental check-up rate increase was statistically significant (p=0.032), the modest improvement suggests need for more intensive interventions.
V. CONCLUSION
The VHVs-led nutrition literacy programme for oral health promotion demonstrates clear effectiveness through significant behavioural and clinical changes. Key success factors include local context adaptation and community engagement. For broader implementation, three policy directions are suggested: (1) integration with national health promotion policies, (2) inclusion of nutrition literacy indicators related to oral health in monitoring systems, and (3) development of standardised guidelines allowing local adaptation. Long-term VHVs capacity development should incorporate continuous professional development through structured mentoring programmes, nutrition literacy skill enhancement workshops for oral health promotion, and recognition systems for advanced competencies. Digital health integration should focus on mobile learning platforms, telemedicine support, and electronic health records, while sustainable monitoring mechanisms should include automated data collection, regular feedback loops, and community-based evaluations.
Future studies should have follow-up periods of at least one year to confirm sustainability of nutrition-related oral health behaviour changes (Baskaradoss, 2018). Research priorities should analyse regional variations, conduct economic evaluations, and develop sustainability indicators while integrating diverse learning approaches to enhance effectiveness (Lin et al., 2024). This study confirms the programme’s effectiveness and provides insights into change mechanisms and success factors for future nutrition literacy programmes focused on oral health promotion and public health policy. A phased scaling approach with diverse pilot programmes is recommended to optimise outcomes through cross-regional learning and experience sharing.
Notes on Contributors
Chollada Sorasak led the research design, developed methodology, conducted formal analysis and investigation. She was responsible for writing the original manuscript draft and managing the revision process.
Worayuth Nak-Ai provided expertise in validating the research design, research methodology and supervised the overall research implementation process. He was responsible for proof the original manuscript draft and managing the revision process.
Choosak Yuennan managed the data curation process and provided supervision for data collection and analysis procedures.
Mansuang Wongsapai coordinated resource allocation and managed project administration tasks throughout the study period.
Ethical Approval
This study was approved by the Human Research Ethics Committee of Sirindhorn College of Public Health, Chonburi (COA No. 2023/T07, dated 21 August 2023).
Data Availability
The data supporting the findings of this study, including four tables and one figure used in the analysis, are openly available in Figshare at http://dx.doi.org/10.6084/m9.figshare.28105718.
The dataset includes the complete quantitative and qualitative analysis results, tables, and figures used in this study and can be accessed without restrictions for research purposes.
Acknowledgement
We express our gratitude to Dr. Kwanmuang Kaewdamkoeng, Mr. Songkat Duangkhamsawat, Ms. Jariyakorn Ditjinda, and Ms. Wilawan Tangsattayatistan for their expertise in health literacy. We thank Dr. Chalermpol Kongchit, Ms. Waenkaew Chaiararm from Chiang Mai University for communications guidance, and Ms. Umaporn Nimtrakul and the Health Centre Region 1 Chiang Mai team for networking support. We also acknowledge the institutional support from the Intercountry Centre for Oral Health, Department of Health, Thailand, Sirindhorn College of Public Health Chonburi, and Boromarajonani College of Nursing.
Funding
This research received no external funding. The Intercountry Centre for Oral Health, Department of Health provided in-kind support through equipment, materials, and transportation for data collection. The remaining expenses were self-funded by the corresponding author.
Declaration of Interest
The authors declare no conflicts of interest, financial, consultant, institutional or other relationships that might lead to bias or a conflict of interest.
References
Althubaiti, A. (2016). Information bias in health research: Definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare, 9, 211–217. https://doi.org/10.2147/JMDH.S104807
Bandura, A. (2004). Health promotion by social cognitive means. Health Education & Behaviour, 31(2), 143–164. https://doi.org/10.1177/1090198104263660
Baskaradoss, J. K. (2016). The association between oral health literacy and missed dental appointments. Journal of the American Dental Association, 147(11), 867–874. https://doi.org/10.1016/j.adaj.2016.05.011
Baskaradoss, J. K. (2018). Relationship between oral health literacy and oral health status. BMC Oral Health, 18(1), 172. https://doi.org/10.1186/s12903-018-0640-1
Batista, M. J., Lawrence, H. P., & Sousa, M. D. L. R. D. (2017). Oral health literacy and oral health outcomes in an adult population in Brazil. BMC Public Health, 18, 60. https://doi.org/10.1186/s12889-017-4443-0
Berkman, N. D., Sheridan, S. L., Donahue, K. E., Halpern, D. J., & Crotty, K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155(2), 97–107. https://doi.org/10.7326/0003-4819-155-2-201107190-00005
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press.
Cano, J. C., & Lomibao, L. S. (2023). A mixed methods study of the influence of phenomenon-based learning videos on students’ mathematics self-efficacy, problem-solving and reasoning skills, and mathematics achievement. American Journal of Educational Research, 11(3), 97–115.
Chaianant, N., Tussanapirom, T., Niyomsilp, K., & Gaewkhiew, P. (2022). Factors associated with oral health check-up in working adults: The 8th Thai National Oral Health Survey 2017. Thai Dental Public Health Journal, 27(2), 112–123.
Creswell, J. W. (2013). Qualitative inquiry and research design: Choosing among five approaches (3rd ed.). SAGE Publications, Inc.
Creswell, J. W., & Plano Clark, V. L. (2017). Designing and conducting mixed methods research (3rd ed.). SAGE Publications, Inc.
Dickson-Swift, V., Kenny, A., Farmer, J., Gussy, M., & Larkins, S. (2014). Measuring oral health literacy: A scoping review of existing tools. BMC Oral Health, 14, Article 148. https://doi.org/10.1186/1472-6831-14-148
Duijster, D., Monse, B., Dimaisip-Nabuab, J., Djuharnoko, P., Heinrich-Weltzien, R., Hobdell, M., Kromeyer-Hauschild, K., Kunthearith, Y., Mijares-Majini, M. C., Siegmund, N., Soukhanouvong, P., & Benzian, H. (2017). “Fit for School” – A school-based water, sanitation and hygiene programme to improve child health: Results from a longitudinal study in Cambodia, Indonesia and Lao PDR. BMC Public Health, 17, Article 302. https://doi.org/10.1186/s12889-017-4203-1
Firmino, R. T., Ferreira, F. M., Paiva, S. M., Granville-Garcia, A. F., Fraiz, F. C., & Martins, C. C. (2017). Oral health literacy and associated oral conditions: A systematic review. Journal of the American Dental Association, 148(8), 604–613. https://doi.org/10.1016/j.adaj.2017.04.012
Fisher-Owens, S. A., Isong, I. A., Soobader, M. J., Gansky, S. A., Weintraub, J. A., Platt, L. J., & Newacheck, P. W. (2013). An examination of racial/ethnic disparities in children’s oral health in the United States. Journal of Public Health Dentistry, 73(2), 166–174. https://doi.org/10.1111/j.1752-7325.2012.00367.x
Gall, M., Schroeder, F., & Heise, G. (2023). Community health worker use of smart devices for health promotion: Scoping review. JMIR mHealth and uHealth, 11(1), e42023. https://doi.org/10.2196/42023
Gholami, M., Pakdaman, A., Montazeri, A., Jafari, A., & Virtanen, J. I. (2014). Assessment of periodontal knowledge following a mass media oral health promotion campaign: A population-based study. BMC Oral Health, 14, Article 31. https://doi.org/10.1186/1472-6831-14-31
Glasgow, R. E., Harden, S. M., Gaglio, B., Rabin, B., Smith, M. L., Porter, G. C., Ory, M. G., & Estabrooks, P. A. (2019). RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. Frontiers in Public Health, 7, 64. https://doi.org/10.3389/fpubh.2019.00064
Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
Haldane, V., Chuah, F. L. H., Srivastava, A., Singh, S. R., Koh, G. C. H., Seng, C. K., & Legido-Quigley, H. (2019). Community participation in health services development, implementation, and evaluation: A systematic review of empowerment, health, community, and process outcomes. PLOS ONE, 14(5), e0216112. https://doi.org/10.1371/journal.pone.0216112
Horowitz, A. M., & Kleinman, D. V. (2012). Oral health literacy: A pathway to reducing oral health disparities in Maryland. Journal of Public Health Dentistry, 72(s1), S26–S30. https://doi.org/10.1111/j.1752-7325.2012.00316.x
Jacob, S. A., & Furgerson, S. P. (2012). Writing interview protocols and conducting interviews: Tips for students new to the field of qualitative research. The Qualitative Report, 17, 1–10.
Jandee, K., Kaewkungwal, J., Khamsiriwatchara, A., Lawpoolsri, S., Wongwit, W., & Wansatid, P. (2015). Effectiveness of using mobile phone image capture for collecting secondary data: A case study on immunization history data among children in remote areas of Thailand. JMIR mHealth and uHealth, 3(3), e75. https://doi.org/10.2196/mhealth.4183
Kickbusch, I., Pelikan, J. M., Apfel, F., & Tsouros, A. D. (2013). Health literacy: The solid facts. World Health Organization Regional Office for Europe. https://apps.who.int/iris/handle/10665/128703
Kowitt, S. D., Emmerling, D., Fisher, E. B., & Tanasugarn, C. J. (2015). Community health workers as agents of health promotion: Analysing Thailand’s Village Health Volunteer Programme. Journal of Community Health, 40(4), 780–788. https://doi.org/10.1007/s10900-015-9999-y
Kretzmann, J. P., & McKnight, J. L. (1993). Building communities from the inside out: A path toward finding and mobilizing a community’s assets. ACTA Publications.
Kunathum, W. (2023). The relationship between health literacy and roles in chronic disease prevention among village health volunteers. Public Health Policy and Laws Journal, 9(3), 431–444.
Leung, A. Y. M., Chau, P. H., & Leung, I. S. H. (2020). Health literacy experiences of multi‐ethnic patients and their health‐care providers in the management of type 2 diabetes in Malaysia. Health Expectations, 23(6), 1442–1452. https://doi.org/10.1111/hex.13095
Lin, G. S. S., Tan, W. W., Ng, Y. S., & Afrashtehfar, K. I. (2024). Enhancing students’ academic performance through hybrid team-based case-based learning. The Asia Pacific Scholar, 9(3), 67–69. https://doi.org/10.29060/TAPS.2024-9-3/CS3189
Macek, M. D., Atchison, K. A., Watson, M. R., Holtzman, J., Wells, W., Braun, B., … Richards, J. (2016). Assessing health literacy and oral health: Preliminary results of a multi-site investigation. Journal of Public Health Dentistry, 76(4), 303–313. https://doi.org/10.1111/jphd.12156
McKinnon, M. A., Odoh, O., Taylor, P., Charlie, D., Morry, J., Mathu-Muju, K., & Donnelly, L. (2022). Developing a land-based oral health promotion project with an Indigenous community in northern British Columbia, Canada. Canadian Journal of Dental Hygiene, 56(3), 172–176.
Miles, M. B., Huberman, A. M., & Saldaña, J. (2013). Qualitative data analysis: A methods sourcebook (3rd ed.). SAGE Publications, Inc.
Ministry of Public Health. (2024). Health Data Centre Service [Dashboard].
Nutbeam, D. (2000). Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15(3), 259–267. https://doi.org/10.1093/heapro/15.3.259
Nutbeam, D. (2008). The evolving concept of health literacy. Social Science & Medicine, 67(12), 2072–2078. https://doi.org/10.1016/j.socscimed.2008.09.050
Oh, K. M., An, K., Lee, M., & Kreps, G. L. (2022). Cultural factors influencing health literacy, health care access, and health behaviours among Korean-Americans. Health Literacy Research and Practice, 6(2), e89–e97. https://doi.org/10.4324/9781003230243-2
Peres, M. A., Macpherson, L. M. D., Weyant, R. J., Daly, B., Venturelli, R., Mathur, M. R., Listl, S., Celeste, R. K., Guarnizo-Herreño, C. C., Kearns, C., Benzian, H., Allison, P., & Watt, R. G. (2019). Oral diseases: A global public health challenge. The Lancet, 394(10194), 249–260. https://doi.org/10.1016/S0140-6736(19)31146-8
Petersen, P. E. (2009). Global policy for improvement of oral health in the 21st century – Implications to oral health research of World Health Assembly 2007, World Health Organisation. Community Dentistry and Oral Epidemiology, 37(1), 1–8. https://doi.org/10.1111/j.1600-0528.2008.00448.x
Rubin, D. B. (2004). Multiple imputation for nonresponse in surveys (Vol. 81). Wiley.
Samarasekera, D. D., Lee, S. S., Yeo, S. P., Chen, J., Findyartini, A., Greviana, N., & Sherman, L. (2024). The state of continuing professional development in East and Southeast Asia among medical practitioners. The Asia Pacific Scholar, 9(3), 1–14. https://doi.org/10.29060/TAPS.2024-9-3/OA3045
Sørensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand, H. (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12, 80. https://doi.org/10.1186/1471-2458-12-80
Squiers, L., Peinado, S., Berkman, N., Boudewyns, V., & McCormack, L. (2012). The health literacy skills framework. Journal of Health Communication, 17(suppl 3), 30–54. https://doi.org/10.1080/10810730.2012.713442
Sukhampha, R., Khwanriang, P., & Vaisamruat, K. (2023). Women on the frontline of COVID-19: Understanding local women village health volunteers in the northern province of Thailand. BMC Health Services Research, 23, Article 9305. https://doi.org/10.1186/s12913-023-09305-x
Tan, J., Yoshida, Y., Ma, S.-K., & Mauvais-Jarvis, F. (2021). Gender differences in health protective behaviours during the COVID-19 pandemic in Taiwan: An empirical study. medRxiv [Preprint]. https://doi.org/10.1101/2021.04.14.21255448
Tay, R. S. C., Wegner, D. R., Lim, L. S., Ting, J., & Ong, S. T. (2024). Enhancing teaching and learning of evidence-based practice via game-based learning. The Asia Pacific Scholar, 9(3), 41–49. https://doi.org/10.29060/TAPS.2024-9-3/SC3111
van Buuren, S. (2018). Flexible imputation of missing data (2nd ed.). Chapman and Hall/CRC. https://doi.org/10.1201/9780429492259
Walker, D., Tynan, A., Tucker, T., Fisher, B., & Fisher, T. (2023). Engaging with a rural Aboriginal community to identify strategies to improve oral health within their community. Australian Journal of Primary Health, 29(1), 38–46. https://doi.org/10.1071/PY22215
Watt, R. G. (2007). From victim blaming to upstream action: Tackling the social determinants of oral health inequalities. Community Dentistry and Oral Epidemiology, 35(1), 1–11. https://doi.org/10.1111/j.1600-0528.2007.00348.x
Watt, R. G., Daly, B., Allison, P., Macpherson, L. M. D., Venturelli, R., & Benzian, H. (2019). Ending the neglect of global oral health: Time for radical action. The Lancet, 394(10194), 261–272. https://doi.org/10.1016/S0140-6736(19)31133-X
Yin, R. K. (2018). Case study research and applications: Design and methods. SAGE Publications, Inc.
Zachariah, R., Kumar, A. M. V., Isaakidis, P., Sreenivas, A., Bissell, K., Van den Bergh, R., Satyanarayana, S., Van Henten, S., & Reid, A. J. (2024). Reporting guideline for global health qualitative research methods. Global Health Action, 17(1), 2350585. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11353496/
*Worayuth Nak-Ai
Praboromarajchanok Institute, Thailand
668-3570-5859
Email: worayuth@scphc.ac.th
Submitted: 28 October 2024
Accepted: 16 June 2025
Published online: 7 October, TAPS 2025, 10(4), 35-43
https://doi.org/10.29060/TAPS.2025-10-4/OA3559
Reshma Mohamed Ansari1,2, Chan Choong Foong3, Hidayah Mohd Fadzil4 & Mohamad Nabil Mohd Noor3
1Institute for Advanced Studies, Universiti Malaya, Malaysia; 2Department of Medical Education, International Medical School, Management and Science University, Malaysia; 3Medical Education and Research Development Unit (MERDU), Faculty of Medicine, Universiti Malaya, Malaysia; 4Department of Mathematics and Science Education, Faculty of Education, Universiti Malaya, Malaysia
Abstract
Introduction: Self-care agency, a core concept that helps alleviate the stressors of medical training, is postulated to be practiced by medical students who exhibit a growth mindset. Hence, this pilot study was designed to measure, compare, and correlate the self-care agency and mindsets of undergraduate medical students to assess the potential for scaling to a national survey.
Methods: This cross-sectional study was conducted at one public and one private medical university using a revised version of the Appraisal of Self-Care Agency Scale to measure self-care agency and the Implicit Theories of Intelligence Scale to measure participants’ mindset. Data was analysed using IBM SPSS.
Results: In total, 329 complete responses were obtained. Among the self-care domains, a higher capacity for self-care and a developing capacity for self-care, with a lower ability to indulge in self-care, were reported. Self-care agency showed a significant difference between pre-clinical and clinical students (p = .027; Cohen’s d = .2). Mindset measurements revealed a higher growth than a fixed mindset. The Pearson correlation coefficient showed a weak positive correlation, (r = 0.19) between the means of self-care agency and a growth mindset. Clinical students showed a higher tendency toward self-care than their pre-clinical counterparts in an independent-samples t-test, with no differences between genders and universities.
Conclusion: This pilot study found a positive correlation between self-care agency and growth mindset among undergraduate medical students. Although limited by two prototype universities and response bias, this study provides a solid foundation for future nationwide or cross-country studies.
Keywords: Self-care Agency, Growth Mindset, Fixed Mindset, Medical Education, Undergraduate Medical Students, Pilot Study
Practice Highlights
- Undergraduate medical students acknowledge importance of self-care agency and growth mindset.
- Growth mindset correlates with self-care agency necessitating inculcation of both.
- Growth mindset combats the stressors of medical training by indulging in proactive self-care.
I. INTRODUCTION
Orem et al. (1995, p. 19) defined self-care as the “practice of activities that individuals start and perform for their benefit, for the maintenance of life, health, and well-being”. Self-care agency, a component of the self-care deficit nursing theory, is “the acquired, complex capacity to meet the requirements to take care of oneself, regulating life processes, maintaining or promoting integrity, structure, and functioning, as well as one’s development and promotion of well-being” (Oliveira et al., 2022, p. 20; Orem et al., 1995). Research has elucidated that the stressors of medical training, which can cause high rates of burnout, anxiety, depression and poor physical health in students (Ayala et al., 2017; Bostock et al., 2018), could be alleviated through self-care (Ayala et al., 2018).
However, during medical training, students find little to no time to engage in self-care; factors such as increased pressure, poor time management, and a negative environment often acting as barriers (Ayala et al., 2017; Ayala et al., 2018). Guldner et al. (2020) suggested that mindset is a predictor of depression and burnout among medical residents, highlighting the relationship between mindset and poor psychological well-being, alleviated by self-care practices (Carter et al., 2025).
Carol Dweck coined the terms “growth mindset” and “fixed mindset” as part of the implicit theories of intelligence, in which individuals could view intelligence as fixed (entity theory) or as a dimension that can be improved with effort (incremental theory) (Cook et al., 2018; Dweck, 2013). The mindset theory, when applied to the medical education context, suggests that a growth mindset views effort as a means to develop abilities (Theard et al., 2021). In contrast, a fixed mindset could lead to poorer outcomes in a high-pressure educational environment (Bostock et al., 2018) and resultant poor psychological well-being (Root Kustritz, 2017).
Studies have measured participants’ mindsets and correlated them with scales measuring anxiety or overall well-being (Guldner et al., 2020; Root Kustritz, 2017; Wolcott et al., 2021). One of the reasons for a growth mindset to aid students’ well-being is by allowing them to place greater value on health and fitness and exhibit health-seeking behaviours (Orvidas et al., 2018; Thomas et al., 2019).
Adding on, identification of stressors, the burnout caused by them, mental health issues, active self-care seeking behaviours including coping strategies are associated with a growth mindset (Burnette et al., 2020). Nursing students who were exposed to structured activities fostering a growth mindset, reported indulging in student-preferred strategies such as viewing obstacles from a newer perspective, working for competency, and indulging in self-care practices, thus directly relating a growth mindset to better self-care agency (Carter et al., 2025).
Medical students in Malaysia, akin to their global counterparts have reported increased levels of stress and psychological distress (Masilamani et al., 2020), due to stringent admission processes, higher cognitive load, and an assessment-based curriculum (Yusoff et al., 2013). Studies across four public medical schools in Malaysia have shown that students tend to alleviate stress through religious activities, active coping strategies, positive reinterpretation, acceptance, and planning (Yusoff et al., 2011), which could be viewed as a subtle expression of a growth mindset. Despite the postulation that a growth mindset accentuates self-care agency, there is a dearth of studies on the self-care agency of Malaysian medical students and its correlation with mindset.
Hence, this pilot study was conducted with the objective of measuring, comparing, and correlating self-care agency and the mindsets of Malaysian undergraduate medical students to gauge the feasibility of a nationwide survey (Lowe, 2019).
II. METHODS
This cross-sectional pilot study was conducted at a public and a private medical university in Malaysia. which were accessible to researchers. The selected public university is a prototype of Malaysian public universities characterised by highly qualified students with excellent examination results paying subsidised fees, as the operation of the university is funded by the government (Wan, 2007). The selected private university is representative of Malaysian private universities, which primarily provide an alternate pathway for the high school students who are not placed in public universities. Being self-funded, the fees are relatively higher, and the students are typically of paying capacity (Wan, 2007).
Permission to conduct this study was obtained from the ethics committees of both the public and private universities (UM.TNC2/UMREC_2872 and RMC/SEP/2023/EC02, respectively). Generally, although every medical school in Malaysia is homegrown and has variations in its curriculum, both the universities chosen for this study had a similar integrated curriculum spanning over five years for the Bachelor of Medicine, Bachelor of Surgery (MBBS) program, with two years of pre-clinical and three years of clinical studies.
The study instrument consisted of three sections. Data collection was anonymous, and the first section recorded the details of the participants’ age, gender, institution of study, and year of study. Section two included the revised version of the Appraisal of Self-care Agency Scale (ASAS-R), used to measure self-care agency (Oliveira et al., 2022). The ASAS is a 24-item scale developed by Evers et al. in 1986 (Evers, 1989) and modified by Sousa et al. (2010) into a 15-item scale that can be applied to adults aged over 18 years.
The three domains of ASAS-R holistically measure the three types of personal trait components that characterise the concept of self-care agency (Oliveira et al., 2022). The responses were ranked on a 5-point Likert scale (1 = totally disagree; 5 = totally agree). The total scores ranged from 15 to 75, with higher scores indicating greater self-care agency (Oliveira et al., 2022).
Sousa et al. (2010) divided the items into the following domains: Domain I: having the capacity for self-care (items 1, 2, 3, 5, 6, and 10; maximum domain score = 30); Domain II: developing the capacity to self-care (items 7, 8, 9, 12, and 13; maximum domain score = 25); and Domain III: inability to self-care (items 4, 11, 14, and 15; maximum domain score = 20), with acceptable Cronbach’s alpha values of 0.86, 0.83, and 0.79, respectively. The instrument has been validated among the general population in countries such as China, Spain, and Brazil, and among medical students in Portugal (Alhambra-Borrás et al., 2017; Guo et al., 2017; Oliveira et al., 2022; Yuan et al., 2021).
Section three consisted of the Implicit Theories of Intelligence Scale (ITIS), adopted from the published version of the ITIS by Cook et al. (2017), to measure the mindset of medical students. The ITIS is an eight-item instrument with four items related to incremental beliefs (1, 2, 3, and 4) and four items related to entity beliefs (5, 6, 7, and 8) regarding intelligence and ability. Responses were based on a 6-point Likert scale (1 = strongly disagree; 6 = strongly agree) (Cook et al., 2017). For each domain, the scores ranged from 4 to 24.
A confirmatory factor analysis of the ITIS scores demonstrated an overall acceptable model fit; an exploratory factor analysis confirmed a two-factor structure (Cook et al., 2017), with the Cronbach’s alpha ≥ 0.77 for each domain (Cook et al., 2018).
The sample size of the study was calculated using Raosoft online software (http://www.raosoft.com/samplesize.html).
With an approximate total population of 1300 (public university = approximately 900; private university = approximately 400), based on a confidence level of 95%, a response distribution of 50%, and a margin of error of 5%, the sample size was determined to be 297. A quota sampling technique was applied to ensure adequate sample representation for each university: 204 from the public university and 93 from the private university.
The questionnaire items were entered into a Google Form, and the link was distributed to all the students of both the universities where they were asked to answer the questionnaire after reading the participant information sheet and providing informed consent.
The data were collected over four weeks, starting on November 1 – November 30, 2023, which was two months from the start of the new semester (September 2023) in both universities which gives ample time for the students to experience the learning environment and respond to the questionnaire. A reminder was provided two weeks after the start of data collection, and data collection ended two weeks after the reminder. The students were informed of the closure of data collection.
The data were analysed using the IBM Statistical Package for Social Sciences (SPSS) v.26 via descriptive and inferential tests. The normality of the data distribution was screened. Pearson’s product-moment correlation was used to analyse the relationship between self-care agency and mindset, whereas independent-samples t-tests were used for comparative analyses between gender and years of study.
III. RESULTS
A. Participants’ Characteristics
A total of 329 valid responses were received. The participants’ demographic characteristics are presented in Table 1.
The distribution of the participants according to their year of study followed the same pattern in both universities, with more female than male respondents and more pre-clinical than clinical students, implying that the sample was representative of the population.
|
Age |
Range (years) |
Mean |
|
|||
|
|
18–28 |
20.8 |
|
|||
|
Year of study |
Private university n (%) |
n=118 (35%) |
Pre-clinical n (%) |
68 57.63% |
Year 1 n (%) |
n=31 45.5% |
|
Year 2 n (%) |
n=37 54.5% |
|||||
|
Clinical n (%) |
50 42.37% |
Year 3 n (%) |
n=28 56% |
|||
|
Year 4 n (%) |
n=12 24% |
|||||
|
Year 5 n (%) |
n=10 20% |
|||||
|
Public university n (%) |
n=211 (65%) |
Pre-clinical n (%) |
127 60.2% |
Year 1 n (%) |
n=78 61.4% |
|
|
Year 2 n (%) |
n=49 38.6% |
|||||
|
Clinical n (%) |
84 39.8% |
Year 3 n (%) |
n=20 23.8% |
|||
|
Year 4 n (%) |
n=8 9.5% |
|||||
|
Year 5 n (%) |
n=56 66.7% |
|||||
|
Gender |
Male n (%) |
n=112 34.1%
|
Private university n (%) |
n=38 33.9% |
|
|
|
Public university n (%) |
n=74 66.1% |
|||||
|
Female n (%)
|
n=217 65.9% |
Private university n (%) |
n=80 36.9% |
|||
|
Public university n (%) |
n=137 63.1% |
|||||
Table 1. Participants’ demographic characteristics (N = 329)
B. Descriptive Statistics
The key descriptive statistics and reliability indices of the ASAS-R are presented in Table 2.
|
Item No. |
Itemsa |
Minimum |
Maximum |
Mean (SD) |
|
|
|
ASAS-R Cronbach’s alpha |
.841 |
|||||
|
ASAS-R total score Mean (SD) |
55.74 (8.10) |
|||||
|
Domain I: Having the capacity for self-care (items 1, 2, 3, 5, 6 & 10 of ASAS-R) |
||||||
|
|
Domain total score (SD) |
|
|
|
24.14 (4.17) |
|
|
|
Domain Cronbach’s alpha |
|
|
|
.875 |
|
|
Domain II: Developing the capacity for self-care (items 7, 8, 9, 12 & 13 of ASAS-R) |
||||||
|
|
Domain total score (SD) |
|
|
|
19.69 (3.61) |
|
|
|
Domain Cronbach’s alpha |
|
|
|
.762 |
|
|
Domain III: Inability to self-care (items 4, 11, 14 & 15 of ASAS-R) |
||||||
|
4 |
* I often lack energy to care for myself in the way that I know I should. |
1.00 |
5.00 |
3.09 (1.18) |
|
|
|
11 |
* In my daily activities I seldom take time to care for myself. |
1.00 |
5.00 |
2.82 (1.19) |
||
|
14 |
* I seldom have time for myself. |
1.00 |
5.00 |
2.82 (1.18) |
||
|
15 |
* I am not always able to care for myself in a way I would like. |
1.00 |
5.00 |
3.15 (1.20) |
||
|
Domain total score (SD) |
11.90 (3.63) |
|||||
|
Domain Cronbach’s alpha |
.761 |
|||||
*Negatively worded items; the answers were reversely scored.
a5-point Likert scale: 1 (totally disagree) to 5 (totally agree).
Table 2. ASAS-R and its scores
The domain scores for Domains I (M = 24.14, SD = 4.17) and II (M = 19.69, SD = 3.61; maximum scores = 30 and 25, respectively) were higher than those for Domain III (M = 11.90, SD = 3.63; maximum score = 20). The items of Domains I and II showed mean scores varying from 3.7 to 4.1, indicating global positive scores for one’s self-perception of having and developing self-care abilities. The mean scores of the items of Domain III varied from 2.8 to 3.15, suggesting that the students acknowledged a lack of means to self-care (all four items were reversely worded) (Damásio & Koller, 2013).
Table 3 presents the key descriptive statistics and reliability indices of the ITIS questionnaire. The maximum score for each domain was 24. The score for the incremental domain (Min: 1.00 and Max: 6.00; M = 18.49, SD = 4.13) was higher than that for the entity domain (Min: 1.00 and Max: 6.00; M = 12.33, SD = 5.24), indicating that the students were more aligned toward a growth mindset than a fixed mindset (Sun et al., 2021). The mean of the items indicating a fixed mindset (entity domain) showed a range of 2.8 to 3.3, compared with the mean of the items indicating a growth mindset (incremental domain), which showed a range of 4.5 to 4.7 (Hong et al., 1999).
|
ITIS Cronbach’ alphaa |
.724 |
|
Domain: Entity (items 1, 2 3 & 4 of ITIS) |
|
|
Domain total score Mean (SD) |
12.33 (5.24) |
|
Domain Cronbach’s alpha |
.930 |
|
Domain: Incremental (items 5, 6, 7 & 8 of ITIS) |
|
|
Domain total score Mean (SD) |
18.49 (4.13) |
|
Domain Cronbach’s alpha |
.907 |
a6-point Likert scale: 1 (strongly disagree) to 6 (strongly agree).
Table 3. ITIS and its scores
C. Correlational Analysis
For inferential statistics, the total score of self-care agency and the mindset domains were subjected to tests of normality using the applied statistical methods of skewness and kurtosis; z-values were not considered as the sample size was greater than 300 (Kim, 2013). The resultant absolute skew values were less than 2, and the absolute kurtosis values were less than 7. Hence, the data were considered to be normally distributed, and parametric tests were applied (Hair et al., 2006; Kim, 2013). All values were considered significant if the p value was less than 0.05.
The relationship between self-care agency (total score) and growth mindset (domain score) was investigated using Pearson’s product-moment correlation coefficient. There was a significant positive correlation between the two variables (r = .19, n = 329, p < .01 (two-tailed)), indicating that self-care agency behaviour is associated with a growth mindset. In contrast, the Pearson correlation between self-care agency (total score) and a fixed mindset (domain score) was not significant (r = .060, n = 329, p = .278 (two-tailed)). Pearson’s correlation did not show significant correlations between the domains of growth and a fixed mindset with the individual domains of capacity for self-care, developing capacity for self-care, and inability to perform self-care.
D. Comparative Analysis
An independent-samples t-test was performed to compare the self-care agency (total score) between pre-clinical and clinical students. The analysis showed a significant difference in the total scores of pre-clinical (M = 54.92, SD = 8.86) and clinical students (M = 56.93, SD = 6.71; t (329) = -2.22, p = .027, two-tailed). Though the magnitude of the differences in the means (mean difference = -2.00, 95% CI: -3.78 to -.23) was small (Cohen’s d = .2), it implicates that the factors that hinder self-care could be further explored and mindset interventions could be targeted for pre-clinical students. However, the independent-samples t-test performed to compare the domain scores of fixed and growth mindsets did not show any significant difference between pre-clinical and clinical students (t (329) = -1.668, p = .096, two-tailed) and (t (329) = .216, p = .829, two-tailed), indicating that their mindsets did not differ in this population.
An independent-samples t-test performed to compare the means of self-care agency, fixed mindset, and growth mindset among private and public university students exhibited no significant differences (t (329) = .772, p = .441, two-tailed), (t (329) = -.916, p = .360, two-tailed), (t (329) = -.252, p = .801, two-tailed) indicating that similar stressors and barriers to self-care agency existed in both types of institutions.
An independent-samples t-test was performed to compare the means of self-care agency, fixed mindset, and growth mindset among genders; no significant differences were found (t (329) = -.58, p = .954 two-tailed), (t (329) = .936, p = .350, two-tailed), (t (329) = .052, p = .959, two-tailed) suggesting that both the genders had similar views on the problems encountered in medical schools which could hinder self-care despite possessing a growth mindset. A one-way ANOVA was performed to compare the means of self-care agency, growth mindset, and fixed mindset with respect to the year of study (Year 1–Year 5). The post-hoc Tukey test also did not reveal any significant differences.
IV. DISCUSSION
The total ASAS-R score in this pilot study is comparable to Guo et al.’s (2017) study of older Chinese individuals (55.29 ± 5.22) and Schönenberg et al.’s (2022) study of adults with at least one chronic disorder (52.81 ± 8.39). A study conducted in Brazil among fibromyalgia patients showed similar baseline total scores of 51.9 ± 9.7 and 53.5 ± 11.0 in two samples (Yuan et al., 2021). Oliveira et al. (2022) did not report the total ASAS-R score among Portuguese medical students, but the higher means of Domains I and II and the lower mean of Domain III in this pilot study resonated with their findings which could be further explored by qualitative research. Despite that, Portuguese medical students reported higher mean with Domain II rather than Domain I unlike participants of the current pilot study. This indicates that Portuguese students though lack self-care currently, are positive to be able develop self-care abilities in future. On the other hand, Malaysian students are quite satisfied with their current self-care abilities rather than develop the abilities (Oliveira et al., 2022). The factors for this difference of opinion could be that the Portuguese respondents were of higher age (Mean = 22) and possible cultural factors which could be explored by research as well.
Two items in Domain III (items 11 and 14) scored the lowest in this pilot study and can be likened to the study by Guo et al. (2017) who reported that item number 15 in Domain III “I am not always able to care for myself in the way I would like” scored the lowest (2.83 ± 0.93). The opinion that our students also agree that they lack time and energy for self-care are similar to a study conducted at Yale University, and in the United States of America (USA), where medical students neglected self-care and attributed it to lack of time and high stress levels in their academic journey (Ayala et al., 2018; Gold et al., 2015). Similar factors including organisation for self-care, attributable to an intense medical curriculum were voiced out by Portuguese and Malaysian medical students alike (Oliveira et al., 2022; Yusoff et al., 2013). A worldwide analogous opinion among medical students should be taken into account by medical educators to act on easing the academic journey through early detection and targeted interventions.
In this pilot study, there was no difference in gender in the self-care agency domain, which differs from a study conducted by Ayala et al. (2018), who reported higher stress and self-care activities among female students. However, nursing students in Turkey reported a more optimistic approach to stress management by male students, which correlated with self-care agency among them as well (Komser & Özakgül, 2023). The difference in study results pertaining to gender necessitates a multi-institutional future study with a robust sample size to yield comparable outcomes. Higher self-care agency among clinical students reported in this study is similar to another Malaysian study by Aida et al (2014). Clinical students initially sought predominantly informal ways (peers, friends, and parents) for health seeking rather than formal channels (counselling and psychiatrists) (Aida et al., 2014). Active coping strategies, reframing (focusing on the process not results, viewing failures as opportunities) and planning as means of self-care was also reported by clinical students (Masilamani et al., 2020). Students have reported struggle in self-care behaviours within the first 12 weeks of medical school training regardless of their gender in USA as they struggle with poor sleep and physical activity (Boyd et al., 2023). Though it can be hypothesised that older students with more experience and maturity learn self-care behaviours along their student journey, it is still open to research. Since there is no difference in self-care agency between public and private universities similar to other studies, (Ayala et al. 2018), we can deduce that the factors for poor self-care are alike across different institutions.
In this pilot study, more medical students were found to exhibit a growth mindset rather than a fixed mindset with comparable means with a study among international students in USA, where the growth mindset score was 19.51 ± 1.362, and the fixed mindset score was 14.34 ± 1.557 (Winfrey, 2020) comparable to clinical veterinary students (Guldner et al., 2020; Whittington et al., 2017). There was no difference between fixed and growth mindsets between genders in this pilot study. However, Bostock et al. (2018) reported that more females had a fixed mindset and poorer mental health than their male counterparts. There was no difference in mindset among the students of different years of study in this pilot study. This finding differs from the results of Root Kustritz (2017), who reported that year–two veterinary students showed a more growth-oriented mindset, while Bostock et al. (2018) reported that year–four students had a higher growth-oriented mindset.
Studies that establish a link between psychological distress and mindset predict overall psychological well-being and better mental health in people with a growth mindset due to their adjustment skills (Whittington et al., 2017). Although there have been limited studies directly correlating growth mindsets and self-care, Orvidas et al. (2018) reported that mindsets lead to self-regulatory actions to help people engage in exercise and healthy eating habits, which are attributed to two of the ten domains of self-care by Ayala et al. (2017). This is due to the fact that growth mindsets are important for increasing the capacity to engage in activities even when challenges arise, as it enables understanding of the value and self-relevance of such activities (Ayala et al., 2017).
Individuals with a growth mindset have intrinsic motivation and show resilience, which translates into self-care abilities during periods of distress (Alatorre et al., 2020; Root Kustritz, 2017). Additionally, growth-mindset individuals value personal growth, autonomy, purpose in life, and self-acceptance, which could explain their self-care abilities and psychological well-being (Whittington et al., 2017). Individuals with a fixed mindset are more prone to stress and unhealthy perfectionism, which are linked to suicidal behaviours (Dweck, 2013). A fixed mindset does not believe in change, and self-care to bring about positive change may not be appreciated (Root Kustritz, 2017). A meta-analysis conducted by Burnette et al. (2020) concluded that there is a negative relationship between growth mindset and psychological distress, but a positive correlation with active coping and treatment values, indicating that a growth mindset places value on self-care (Burnette et al., 2020).
Selection, complexity, reliability and generalisability biases could occur with quota sampling employed in this study. Selection bias was mitigated by calculating the sample size based on the population in the respective medical schools and complexity was avoided by including two protype schools only. The alpha values for the data ensured reliability. Since this was a pilot study the findings were not generalised but were intended to gauge the logistic and statistical feasibility of a nationwide study. Although respondents were informed of their anonymity prior to answering the questionnaire to minimise bias, some respondents might have wanted to demonstrate their positive side and, therefore, present themselves as having self-care abilities and a growth mindset, giving rise to response bias.
V. CONCLUSION
The findings of this pilot study indicate that although students are in favour of self-care capacity and its development, they lack of self-care ability in practice, factors of which could be explored qualitatively in future research. The positive correlation between a growth mindset and self-care ability could be utilised in medical curricula by integrating mindset training to enhance self-care capacity among the students. This pilot study also provides justification for a nationwide, multi-institutional global research.
Notes on Contributors
RMA was involved in literature search, data acquisition and analysis, manuscript preparation and revision.
FCC was involved in the study conception and design, data analysis, manuscript editing, and review.
HMF was involved in the study conception and design and manuscript review.
MNMN was involved in data acquisition and manuscript revision.
All the authors approved the final version of the manuscript and its revised versions.
Ethical Approval
Ethical approval was obtained from the research ethics committees of both the public and private universities, (UM.TNC2/UMREC_2872 and RMC/SEP/2023/EC02, respectively) in accordance with the Declaration of Helsinki.
Data Availability
As per the requirements of the local ethics committees, data will be stored in an enclosed and dedicated facility in the faculty building. The datasets used and/or analysed in the current study are available from the corresponding author upon reasonable request.
Acknowledgement
The authors express their sincere gratitude to all the students who participated in this study.
Funding
The authors declare no sources of funding.
Declaration of Interest
The authors declare that they have no competing interests.
References
Aida, J., Hizlinda, T., Siti Fatimah, S., Mohd Muhaimin, A., Chai, S. Y., Sahrina, W., & Teo, B. H. (2014). Psychological disorders and help seeking behaviour among Malaysian medical students in their clinical years. Medicine & Health, 9(2), 114–23. https://www.researchgate.net/publication/272093951
Alatorre, A. I., DePaola, R. V., & Haeffel, G. J. (2020). Academic achievement and depressive symptoms: Are fixed mindsets distinct from negative attributional style? Learning and Individual Differences, 77, 101811. https://doi.org/10.1016/j.lindif.2019.101811
Alhambra-Borrás, T., Durá-Ferrandis, E., Garcés-Ferrer, J., & Sánchez-García, J. (2017). The Appraisal of Self-Care Agency Scale – Revised (ASA-R): Adaptation and validation in a sample of Spanish older adults. The Spanish Journal of Psychology, 20, E48. https://doi.org/10.1017/sjp.2017.52
Ayala, E. E., Omorodion, A. M., Nmecha, D., Winseman, J. S., & Mason, H. R. C. (2017). What do medical students do for self-care? A student-centered approach to well-being. Teaching and Learning in Medicine, 29(3), 237–246. https://doi.org/10.1080/10401334.2016.1271334
Ayala, E. E., Winseman, J. S., Johnsen, R. D., & Mason, H. R. C. (2018). U.S. medical students who engage in self-care report less stress and higher quality of life. BMC Medical Education, 18(1), 189. https://doi.org/10.1186/s12909-018-1296-x
Bostock, R., Kinnison, T., & May, S. A. (2018). Mindset and its relationship to anxiety in clinical veterinary students. Veterinary Record, 183(20), 623–623. https://doi.org/10.1136/vr.104621
Boyd, A., Mealand, K., Briggs Early, K., & Oestreich, E. (2023). Perceived stress, grit, and self-care behaviours in first-year medical students. American Journal of Lifestyle Medicine, 17(6), 803-812. https://doi.org/10.1177/15598276221124576
Burnette, J. L., Knouse, L. E., Vavra, D. T., O’Boyle, E., & Brooks, M. A. (2020). Growth mindsets and psychological distress: A meta-analysis. Clinical Psychology Review, 77, 101816. https://doi.org/10.1016/j.cpr.2020.101816
Carter, A. N., Evans, J., Seibert, S. A., & Weir, S. (2025). Growth mindset enhancement for new nursing students. Teaching and Learning in Nursing, 20(1), e258-e262. https://doi.org/10.1016/j.teln.2024.10.023
Cook, D. A., Castillo, R. M., Gas, B., & Artino Jr., A. R. (2017). Measuring achievement goal motivation, mindsets and cognitive load: Validation of three instruments’ scores. Medical Education, 51(10), 1061–1074. https://doi.org/10.1111/medu.13405
Cook, D. A., Gas, B. L., & Artino, Jr., A. R. (2018). Measuring mindsets and achievement goal motivation: A validation study of three instruments. Academic Medicine, 93(9), 1391–1399. https://doi.org/10.1097/ACM.0000000000002290
Damásio, B. F., & Koller, S. H. (2013). The Appraisal of Self-Care Agency Scale – Revised (ASAS-R): Adaptation and construct validity in the Brazilian context. Cadernos de Saúde Pública, 29(10), 2071–2082. https://doi.org/10.1590/0102-311X00165312
Dweck, C. S. (2013). Self-theories: Their role in motivation, personality, and development. Psychology Press.
Evers, G. C. (1989). Appraisal of Self-Care Agency ASA-scale: Reliability and validity testing of the Dutch version of the ASA-scale measuring Orem’s concept’ Self-Care Agency’. [Doctoral thesis, Maastricht University]. https://doi.org/10.26481/dis.19890629ge
Gold, J. A., Johnson, B., Leydon, G., Rohrbaugh, R. M., & Wilkins, K. M. (2015). Mental health self-care in medical students: A comprehensive look at help-seeking. Academic Psychiatry, 39(1), 37–46. https://doi.org/10.1007/s40596-014-0202-z
Guldner, G., Siegel, J., Ellis, B., & Brafford, A. (2020, February 27–29). The role of mindset, impostorism, and irrational beliefs in resident wellness: Results from the HCA Nationwide Longitudinal Resident Wellness Study [Poster presentation]. ACGME 2020 Annual Educational Conference, San Diego, CA. https://scholarlycommons.hcahealthcare.com/teaching-learning/5/
Guo, L., Zauszniewski, J. A., Ding, X., Zhang, L., Gao, H., Guo, Q., & Liu, K. (2017). The Appraisal of Self-Care Agency Scale – Revised (ASAS-R): Reliability and validity among older Chinese people. Western Journal of Nursing Research, 39(11), 1459–1476. https://doi.org/10.1177/0193945916672821
Hair, J. F., Black, W. C., Babin, B. J., Anderson, R. E., & Tatham, R. L. (2006). Multivariate data analysis (6th ed.). Pearson Prentice Hall.
Hong, Y. Y., Chiu, C. Y., Dweck, C. S., Lin, D. M. S., & Wan, W. (1999). Implicit theories, attributions, and coping: A meaning system approach. Journal of Personality and Social Psychology, 77(3), 588–599. https://doi.org/10.1037/0022-3514.77.3.588
Kim, H. Y. (2013). Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restorative Dentistry & Endodontics, 38(1), 52–54. https://doi.org/10.5395/rde.2013.38.1.52
Komser, N., & Özakgül, A. (2023). Attitudes of coping with stress and self-care agency levels of nursing students. Journal of Education and Research in Nursing, 20(1), 28–34. https://doi.org/10.5152/jern.2023.21004
Lowe, N. K. (2019). What is a pilot study? Journal of Obstetric, Gynecologic & Neonatal Nursing, 48(2), 117–118. https://doi.org/10.1016/j.jogn.2019.01.005
Masilamani, R., Jabbar, M. A., Liang, C. S., You, H. L. S., Jonathan, L. J. K., Pei-Suen, W., Yuan, Y.X. & Ling, Y. M. (2020). Stress, stressors, and coping strategies between pre-clinical and clinical medical students at Universiti Tunku Abdul Rahman. Malaysian Journal of Public Health Medicine, 20(1), 175-183. https://doi.org/10.37268/mjphm/vol.20/no.1/art.503
Oliveira, L., Teixeira, A., & Duarte, I. (2022). The Appraisal of Self-Care Agency Scale – Revised (ASAS-R): Reliability and validity among Portuguese medical students. International Journal of Environmental Research and Public Health, 19(17), 10848. https://doi.org/10.3390/ijerph191710848
Orem, D. E., Taylor, S. G., & Renpenning, K. M. (1995). Nursing: Concepts of practice. Mosby.
Orvidas, K., Burnette, J. L., & Russell, V. M. (2018). Mindsets applied to fitness: Growth beliefs predict exercise efficacy, value and frequency. Psychology of Sport and Exercise, 36, 156–161. https://doi.org/10.1016/j.psychsport.2018.02.006
Root Kustritz, M. V. (2017). Pilot study of veterinary student mindset and association with academic performance and perceived stress. Journal of Veterinary Medical Education, 44(1), 141–146. https://doi.org/10.3138/jvme.1115-181R1
Schönenberg, A., Teschner, U., Prell, T., & Mühlhammer, H. M. (2022). Validation and psychometric analysis of the German translation of the appraisal of self-care agency scale-revised. Healthcare, 10(9), 1785. https://doi.org/10.3390/healthcare10091785
Sousa, V. D., Zauszniewski, J. A., Bergquist-Beringer, S., Musil, C. M., Neese, J. B., & Jaber, A. F. (2010). Reliability, validity and factor structure of the Appraisal of Self‐Care Agency Scale – Revised (ASAS‐R). Journal of Evaluation in Clinical Practice, 16(6), 1031–1040. https://doi.org/10.1111/j.1365-2753.2009.01242.x
Sun, X., Nancekivell, S., Gelman, S. A., & Shah, P. (2021). Growth mindset and academic outcomes: A comparison of US and Chinese students. NPJ Science of Learning, 6(1), 21. https://doi.org/10.1038/s41539-021-00100-z
Theard, M. A., Marr, M. C., & Harrison, R. (2021). The growth mindset for changing medical education culture. eClinicalMedicine, 37, 100972. https://doi.org/10.1016/j.eclinm.2021.100972
Thomas, F. N., Burnette, J. L., & Hoyt, C. L. (2019). Mindsets of health and healthy eating intentions. Journal of Applied Social Psychology, 49(6), 372–380. https://doi.org/10.1111/jasp.12589
Wan, C. D. (2007). Public and private higher education institutions in Malaysia: Competing, complementary or crossbreed as education providers. Kajian Malaysia, 25(1), 1–14. https://www.researchgate.net/publication/49583836
Whittington, R. E., Rhind, S., Loads, D., & Handel, I. (2017). Exploring the link between mindset and psychological well-being among veterinary students. Journal of Veterinary Medical Education, 44(1), 134–140. https://doi.org/10.3138/jvme.1215-192R
Winfrey, S. E. (2020). Validating the mindset scale for use with international students attending college in the United States [Doctoral dissertation, North Dakota State University]. https://hdl.handle.net/10365/32293
Wolcott, M. D., McLaughlin, J. E., Hann, A., Miklavec, A., Beck Dallaghan, G. L., Rhoney, D. H., & Zomorodi, M. (2021). A review to characterise and map the growth mindset theory in health professions education. Medical Education, 55(4), 430–440. https://doi.org/10.1111/medu.14381
Yuan, S. L. K., Couto, L. A., & Marques, A. P. (2021). Effects of a six-week mobile app versus paper book intervention on quality of life, symptoms, and self-care in patients with fibromyalgia: A randomized parallel trial. Brazilian Journal of Physical Therapy, 25(4), 428–436. https://doi.org/10.1016/j.bjpt.2020.10.003
Yusoff, M. S. B., Abdul Rahim, A. F., Baba, A. A., Ismail, S. B., Mat Pa, M. N., & Esa, A. R. (2013). The impact of medical education on psychological health of students: A cohort study. Psychology, Health & Medicine, 18(4), 420–430. https://doi.org/10.1080/13548506.2012.740162
Yusoff, M. S. B., Yee, L. Y., Wei, L. H., Meng, L. H., Bin, L. X., Siong, T. C., & Rahim, A. F. A. (2011). A study on stress, stressors and coping strategies among Malaysian medical students. International Journal of Students’ Research, 1(2), 45–50. https://www.researchgate.net/publication/50944546_A_study_on_stress_stressors_and_coping_strategies_among_Malaysian_medical_students
*Foong Chan Choong
Medical Education and Research Development Unit,
Faculty of Medicine, Universiti Malaya, Malaysia
+0060 12-419 1248
Email: foongchanchoong@um.edu.my
Submitted: 24 September 2024
Accepted: 14 May 2025
Published online: 7 October, TAPS 2025, 10(4), 84-89
https://doi.org/10.29060/TAPS.2025-10-4/II3528
Seema Tanaji Methre1, Ramya Jayakumar1, Sugata Sunil Jadhav1, Chhaya Anil Saraf 2, Rajkumar Sansarchand Sood1 & Ashwini Namdeorao Patil3
1Department of Physiology, Dr. D. Y. Patil Medical College, Hospital & Research Centre, India; 2Department of Physiology, Vydehi Institute of Medical Sciences and Research Centre, India; 3Department of Physiology, Symbiosis Medical College for Women, Symbiosis (International) (Deemed University), India
I. INTRODUCTION
Soft skills help a person to boost his or her own performance. They are necessary for professional development. Effective communication and decision making are an integral part of good clinical care. Introduction to soft skills during undergraduate training helps students to appreciate and learn effective interpersonal communication with patients and their families. Soft skills training was not a part of academic curriculum in formal traditional medical training. (Sancho-Cantus et al., 2023).
However, since 2019, AETCOM module was added in medical profession in India, in which students need to learn attitude, ethics and communication (Medical Council of India [MCI], 2018). In addition to verbal communication, non-verbal communication including body language, eye contact, facial expression, touch and gestures are equally important in building trust in doctor-patient relationships. In order to inculcate these soft skills in their future profession, students need to practice these skills again and again.
Various professional bodies and medical students have revealed the need for soft skills training in the curriculum (Modi et al., 2016). Integrating these soft skills with clinical skills training is a big challenge. The concept of role play has been widely used to introduce soft skills in medical profession. Role play promotes active learning among the students and motivates them to work as a team. In contrast to lectures, students get completely involved while performing the act during the role play. This enables them to retain and remember the concepts for longer duration. Role play helps the students to have an in-depth understanding of the topic at hand as they are made to think, script and act out the complete scenario on their own. (Goothy et al., 2019). Role play promotes better understanding and leaves an impact not only amongst the participating students but also in peers who are observing them (Rønning & Bjørkly, 2019). The current study aimed to evaluate effectiveness of role play in nourishing various soft skills in the first-year medical students.
II. METHODS
An interventional study was conducted at a teaching medical institute in Western Maharashtra, India. Ethics clearance from the Institutional Ethical Committee was taken before the commencement of the study (Reference Code: I.E.S.C./159/2022). Selection of participants was purely on a voluntary basis.
A. Pre-Role-Play Self-Assessment of Skills
Topics for role play were given 15 days prior to role play. Five students gave verbal consent for this study. The study procedure was explained to the participants. Topics were given as shown in Appendix 2. They wrote their own script for the role play. Pre-test was conducted through Google form which included following types of questions related to various skills like communication, interpersonal, intellectual, self-management and learning. Pre-validated questionnaire was adapted from the website of College of Physiotherapists of Ontario which was modified and rectified by senior faculties as per the need of our study.
This questionnaire allows students to self-assess their own skills so that they know where they may need to improve. Each question has 3 columns as A, B & C. Each column should be filled per the instructions given below as shown in supplementary table (Appendix 1).
1. Column A
How important is the skill for the participant that he/she thinks should possess/acquire? Need to write the number as per the scale given below:
6 – very important
5 – important
4 – slightly important
3 – slightly unimportant
2 – unimportant
1 – very unimportant
2. Column B
Where does participant see himself/herself in already possessing the following skills (i.e., his/her self-assessment of present skill level)? Need to write the number as per scale given below:
6 – Expert, no need for further training
5 – Expert, needs self-training
4 – Good, needs occasional training from experts
3 – Average, needs frequent training
2 – Poor, needs regular training
1 – Bad, needs handholding and training
3. Column C
Participants need to subtract column B number from column A number (column A – column B). The highest number in this column C shows a major disparity between what he/she thinks about the importance of a particular skill and its current expertise level. These are the skills where participants need to improve whenever she gets opportunity in future.
B. Role Play Enactment Sessions (Intervention)
A total of 3 role plays were enacted by the participants focusing on-bad followed by good 1) attitude, 2) behavior and 3) communication of doctor with patients as per topics given to them (Appendix 2).
C. Post-Role-Play Self-Assessment of Skills
Post-test was conducted for participants using the same questionnaire.
1. Statistical Analysis
Scores of pre-test and post-test were copied into excel sheet and data was analysed by paired t -test using Primer of Biostatistics software, version 7.0.
III. RESULTS
Mean score of post-tests in communication skill (0.35±0.14) was highly reduced compared to pretest (2.64±0.36) and was statistically significant (p<0.0001***).
Mean score of post-tests in interpersonal skill (0.5±0.20) was highly reduced compared to pretest (2.55±0.19) and was statistically significant (p<0.0001***).
Mean score of post-tests in self-management skill (0.54±0.25) was highly reduced compared to pretest (1.33±0.21) and was statistically significant (p<0.0001***.
Mean score of post-tests in intellectual skill (0.67±0.39) was also reduced compared to pretest (2.73±0.46) and was statistically significant (p=0.002**).
Mean score of post-tests in learning skills (0.5±0.31) was also reduced compared to pretest (1.32±0.30) and was statistically significant (p=0.002**). Self-assessed improvement of communication skills, interpersonal skills and self-management skills by the participants in role play showed highly significant results (Table 1).
|
Sl No |
Skill |
Mean (SD) |
SEM |
95% Confidence Interval |
t |
dF |
p |
||
|
Upper Limit |
Lower Limit |
|
|
|
|||||
|
1 |
Communication (Q1 – Q5) |
Pre-test |
2.64 (0.36) |
0.16 |
1.99 |
2.59 |
21.5 |
4 |
<0.0001*** |
|
Post-test |
0.35 (0.14) |
0.06 |
|||||||
|
2 |
Interpersonal skills (Q6-Q9)
|
Pre-test |
2.55 (0.19) |
0.09 |
1.88 |
2.22 |
37.9 |
3 |
<0.0001*** |
|
Post-test |
0.5 (0.20) |
0.10 |
|||||||
|
3 |
Intellectual skills (Q10-Q12) |
Pre-test |
2.73 (0.46) |
0.27 |
1.67 |
2.47 |
22.2 |
2 |
0.002** |
|
Post-test |
0.67 (0.39) |
0.22 |
|||||||
|
4 |
Self-Management Skill (Q13-Q18) |
Pre-test |
1.33 (0.21) |
0.08 |
0.59 |
0.99
|
10.1 |
5 |
<0.0001*** |
|
Post-test |
0.54 (0.25) |
0.1 |
|||||||
|
5 |
Learning skills (Q19-Q23) |
Pre-test |
1.32 (0.30) |
0.14 |
0.51 |
1.13 |
7.4 |
4 |
0.002** |
Data presented as mean of scores ± SD, p- value calculated by paired t-test, p*** – highly significant & p** – significant
Table 1. Self-assessed improvement of various skills by the participants in role play
IV. DISCUSSION
Present study showed self-assessed improvement in communication skills, interpersonal skills and self–management skills due to role play in the participants which was highly significant. Intellectual skills and learning skills also improved significantly in this study. Role play promotes active learning. Participants write scripts on their own, think about the characters, plan for acting and do rehearsal also. Role play helps to build leadership qualities and teamwork amongst participants (Goothy et al., 2019). In order to provide good quality health care, soft skills training is necessary to strengthen these skills in professional training. Improvement in soft skills like communication, interpersonal, intellectual, self-management & learning skills enhances academic performance as well as overall professional development of the student (Sancho-Cantus et al., 2023). Cognitive and psychomotor skills are also enhanced through such activities (Goothy et al., 2019). Such soft skill training also improves coping abilities during disturbances as seen in COVID 19 pandemic and also reduces the incidence of anxiety and depression (Sancho-Cantus et al., 2023).
Only five students volunteered to participate in this study. Improvement in these skills was based on self-assessment. Due to small sample size, social desirability bias and self-report bias, statistical significance may vary and might affect the generalisation of the findings. But this pilot study can be extended with large sample size for getting more appropriate results. Focus group discussions, direct observations and reflective essays might give more in-depth information in future studies.
V. CONCLUSION
Soft skills like communication skills, interpersonal skills and self–management skill may be improved along with Intellectual skills and learning skills by the role play in students of medical profession. Role play can be used as an effective tool to enhance soft skills in the students. Such studies should be facilitated in larger population.
Notes on Contributors
Seema Tanaji Methre was involved in conceptualisation, methodology, project administration and supervision, data analysis and writing (original draft and editing).
Ramya Jayakumar was involved in conceptualisation, methodology, project administration and supervision, data analysis and writing (editing).
Sugata Sunil Jadhav was involved in methodology, project administration and supervision, data analysis and writing (editing).
Chhaya Anil Saraf was involved in project administration and supervision.
Rajkumar Sansarchand Sood was involved in conceptualisation, methodology and writing (editing).
Ashwini Namdeorao Patil was involved in conceptualisation, methodology, data analysis and writing (editing).
Ethical Approval
This study was reviewed by the Institutional Ethics Sub-Committee Committee from the Dr. D. Y. Patil Vidyapeeth, Pune (Deemed to be University), Dr. D. Y. Patil Medical College, Hospital & Research Centre, Pimpri, Pune with an exemption from IRB review and the approval to conduct research at institute (Reference Code: I.E.S.C./159/2022).
Acknowledgement
We would like to acknowledge our participants whose efforts were truly appreciable in this study.
Funding
This study was self-funded.
Declaration of Interest
The authors declare no conflicts of interest.
References
Goothy, S. K., Sirisha, D., & Movva, S. (2019). Effectiveness of academic role-play in understanding the clinical concepts in medical education. International Journal of Research in Pharmaceutical Sciences, 10(2), 1205-1208. https://www.researchgate.net/publication/332734016_Effectiveness_of_Academic_Role-play_in_Understanding_the_Clinical_Concepts_in_Medical_Education
Medical Council of India. (2018). Attitude, Ethics and Communication (AETCOM) competencies for the Indian Medical. https://www.nmc.org.in/wpcontent/uploads/2020/01/AETCOM_book.pdf
Modi, J. N., Chhatwal, A. J., Gupta, P., & Singh, T. (2016). Teaching and assessing communication skills in medical undergraduate training. Indian Pediatrics, 53(15), 497-504. https://www.indianpediatrics.net/june2016/497.pdf
Rønning, S. B., & Bjørkly, S. (2019). The use of clinical role-play and reflection in learning therapeutic communication skills in mental health education: An integrative review. Advances in Medical Education and Practice, 10, 415-425. http://doi.org/10.2147/AMEP.S202115
Sancho-Cantus, D., Cubero-Plazas, L., Botella Navas, M., Castellano-Rioja, E., & Cañabate Ros, M. (2023). Importance of soft skills in health sciences students and their repercussion after the COVID-19 epidemic: Scoping review. International Journal of Environmental Research and Public Health, 20(4901), 1-10. https://doi.org/10.3390/ijerph20064901
*Ramya Jayakumar
Department of Physiology,
Dr. D. Y. Patil Medical College, Hospital & Research Centre,
Dr D. Y. Patil Vidyapeeth, Sant Tukaram Nagar, Pimpri,
Pune. Maharashtra – 411018
8446428137
Email: ramyajksk@gmail.com
Submitted: 19 August 2025
Accepted: 30 September 2025
Published online: 7 October, TAPS 2025, 10(4), 1-4
https://doi.org/10.29060/TAPS.2025-10-4/GP3858
Dujeepa D. Samarasekera1, Gominda Ponnamperuma2, Lee Shuh Shing1 & Han Ting Jillian Yeo1
1Centre for Medical Education (CenMED), Yong Loo Lin School of Medicine, National University of Singapore, Singapore; 2Faculty of Medicine, University of Colombo, Sri Lanka
Abstract
Introduction: Medical education aims to produce healthcare professionals who are not only competent, but also able to perform effectively in clinical practice settings. Assessment systems are critical to achieving this by guiding learning, ensuring competence, and certifying readiness for independent practice. This article proposes a staged assessment approach that integrates both competence and performance to ensure safe and empathetic healthcare practice.
Methods: First, we analysed the strengths and limitations of the existing assessment methods and their roles in medical education. Then, we explored strategies to integrate diverse assessment tools into a cohesive assessment system capable of effectively and reliably evaluating the competencies required for developing holistic practitioners.
Results: Competence is assessed via structured assessment tools such as written assessments. Clinical performance in real-world settings relies on Supervised in-practice assessments (SuPs), including tools like Direct Observation of Procedural Skills (DOPS) and Mini-Clinical Evaluation Exercises (mini-CEXs). Assessment tools used to evaluate performance rely on expert judgement, which, although subjective, is essential for evaluating non-cognitive skills such as empathy and professionalism.
Conclusion: This article outlines the design of a progressive assessment system, transitioning from objective assessment methods such as Multiple-Choice Questions (MCQs) to performance-focused methods, anchored by Entrustable Professional Activities (EPAs), using Workplace-Based Assessment tools and portfolios. The progression from early objective assessment tools to those which leverage expert judgement and situational specificity are highlighted as essential for preparing safe, effective, and empathetic healthcare practitioners.
Practice Highlights
- Modern assessment systems focus on both competence in non-practice settings and performance in authentic clinical practice settings.
- A combination of tools is required to assess from “knows” to “is” level of clinical performance.
- Expert evaluations provide qualitative insights into candidate performance.
I. INTRODUCTION
Traditionally, assessments in clinical education strived for standardisation, structuredness and objectivity. A single quantitative method, such as paper-based Multiple-Choice Questions (MCQs), was often used to assess a student’s competence in knowledge. Similarly, the Objective Structured Clinical Examinations (OSCEs) or long/short clinical cases were used for assessing psychomotor and affective domains related to clinical skills. To deliver healthcare effectively and empathetically, a broad range of skills must be cultivated. Over the years, there has been a gradual yet noteworthy transition from exclusively focusing on the development and assessment of one’s competence in clinical skills to placing greater emphasis on enhancing clinical performance within specific clinical contexts (Hays et al,2024).
Miller’s Pyramid (1990) of Clinical Competence illustrates this progression: from “knows” to “knows how”, “shows how”, and finally “is” as proposed by Cruess et al. (2016). At present, medical and health professional training programs judiciously select a combination of assessment methods to ensure learners are task-ready, empathetic, and safe for clinical practice. This article proposes and elaborates on the use of a staged assessment approach in health professional training, progressing from the development of competence to the refinement of clinical performance within specific practice contexts. The core idea is that competence alone does not ensure effective clinical practice. Both competence and performance must be developed to ensure safe and compassionate care.

Figure 1: The diagram adapted from Cruess et al (2016) article on “Amending Miller’s Pyramid to Include Professional Identity Formation”, to illustrate a shift in focus as trainees progress to the later stages of training from assessment of competence to assessment of performance.
II. COMPETENCE AND ITS ASSESSMENT
As illustrated in Figure 1, competence or “Readiness to Practice” refers to an individual’s “ability”, encompassing knowledge, psychomotor or clinical skills, and attitudes, which together form the foundation of medical practice. Knowledge-based skills include problem-solving and clinical reasoning, psychomotor skills involve physical examinations and procedural techniques, while affective skills pertain to empathetic communication. Historically, our assessments have primarily focused on evaluating competence, employing a range of assessment tools as the following.
Written assessments, such as MCQs and Modified Essay Questions (MEQs), are designed to evaluate the “knows” and “knows how” levels of Miller’s Pyramid. These assessments primarily focus on theoretical knowledge, including understanding disease pathophysiology, as well as the procedural steps involved in performing clinical skills and managing medical conditions.
In contrast, practical and competence-based assessments, such as OSCEs, evaluate psychomotor and affective competencies, including procedural skills, diagnostic reasoning, patient interaction and communication in a controlled environment. Long and short cases, on the other hand, assess the same abilities within semi-controlled environments. These assessment formats target the “shows” level of Miller’s Pyramid, emphasising the development and demonstration of clinical skills in structured, controlled testing settings.
The feature of “shows” assessment methods is that they promote standardisation and assessment based on a rubric. Hence, they are “objective” and fairly reliable for assessing specific aspects of competence.
III. PERFORMANCE AND THE ROLE OF SUPERVISED IN-PRACTICE ASSESSMENTS (SuPs)
As illustrated in Figure 1, as learners progressed from early stages to later or final stages of learning, the focus shifts from assessment of competence to assessment of performance. While the assessment of knowledge continues to play an important role, the focus increasingly shifts towards ensuring that graduates are ready for clinical practice. Performance or “Quality in Practice” requires learners to apply their competence in dynamic, high-pressure clinical settings. These situations are both context-specific and situation-specific. In modern medical education, Entrustable Professional Activities (EPAs) anchor these authentic clinical tasks. EPAs focus on specific professional responsibilities, such as managing acute care or conducting patient handovers. These tasks are assessed by an “expert” using professional judgement. Entrustment decisions are based on evaluations from multiple experts (Cate & Schumacher, 2022).
Common tools used during SuPs include Direct Observation of Procedural Skills (DOPS), Case-Based Discussions (CBDs), multi-rater or 360 assessments, and Mini-Clinical Evaluation Exercises (mini-CEXs). These tools provide real-time feedback on a student’s or resident’s clinical performance in specific contexts. Collectively, they are also known as Workplace-Based Assessment tools (WBAs).
As students’ progress through clinical rotations or clerkships, these SuPs are compiled into an assessment portfolio. This portfolio includes case logs, feedback from supervisors and learner reflections. Together, these elements document the student’s longitudinal development. At certain time points, the portfolio is assessed by a Committee of Experts (CoE), and an Entrustment Decision is given. SuP assessments immerse learners in authentic clinical environments, enabling them to demonstrate how they apply competence gained in clinical practice. Final judgement of a student or a trainee’s performance and fitness for clinical practice then should be based on the CoE’s value judgement based on the portfolio.
IV. ADVOCATING FOR EXPERT JUDGEMENT: HOLISTIC EVALUATION OF A LEARNER
Expert judgement by assessors when conducting SuP assessments is commonly perceived to be subjective and bias-laden as it shifts away from quantitative to qualitative measures. However, we offer a different insight on how SuP assessments can triangulate with other more “objective” assessment tools to formulate a complete evaluation of a learner.
Expert judgement made by assessors can synthesise multiple facets of performance of a task such as that involving clinical reasoning, empathy and professionalism, in a specific context, into an interconnected evaluation, something that an objective assessment is unable to measure authentically. Multiple ‘subjective’ evaluations by many experts often provide richer, more personalised feedback that helps learners understand their strengths and areas for improvement, promoting deeper learning and growth. At the same time, in WBA, if multiple cases (i.e., patients with varying disease conditions) in many situations/contexts are assessed by multiple expert assessors, both validity and reliability of such assessment are not compromised.
Expert judgement is essential for performance assessments. While often viewed as subjective, expert judgement is vital for evaluating attributes like clinical reasoning, empathy, and professionalism. For example, in EPA-based assessments, experts determine whether learners can perform specific tasks independently, considering not just technical skills but also communication, prioritisation, and adaptability (Cate & Regehr, 2018). To ensure consistency, assessors require thorough calibration through training. Standardised tools, rating scales, and regular discussions among assessors enhance reliability and minimise bias.
Non-cognitive skills such as empathy and professionalism are essential for safe practice but challenging to assess. Portfolios which incorporate Multi-Source Feedback (MSF) provide avenues to evaluate these qualities, incorporating input from patients, peers, and supervisors. Reflective exercises encourage learners to explore biases, communication styles, and values, fostering self-awareness and empathy, and continued learning.
V. PRACTICAL CONSIDERATIONS
A. Balancing Objectivity and Subjectivity
The challenge lies in balancing “objective” assessments with “subjective” evaluations of performance. While MCQs and OSCEs provide standardised measures, expert judgement is crucial for situational assessments. Safeguards need to be in place to maximise the value of subjectivity while ensuring fairness and reliability. These include developing a structured rating scale, calibrating assessors on the scale through vocalising their thought process, discussion on biases, and using judgements from many assessors and contexts before an assessment decision is made.
B. Resource Allocations
SuP assessments demand significant resources, including trained assessors, robust documentation systems, and protected time for feedback as well as the transience of the judgement. Institutions must prioritise these investments to sustain an effective assessment system.
C. Prioritising Transparency
Ensuring transparency of expectations and standards for all assessment tools for educators and learners is important. This involves clearly defining and effectively communicating the criteria for both “objective and subjective” components of the assessment process. Judgements should be documented and explained, with a clear linkage to observable behaviours or outcomes, to foster understanding and trust in the assessment process.
VI. COMPETENCE AND ITS ASSESSMENT
Designing an assessment system to develop a safe, effective, and empathetic practitioners requires a staged, integrated approach. Competency-based assessments build foundational skills, while SuP assessments evaluate task-specific performance through expert judgement. The gradual shift from competence to performance ensures learners are prepared for the complexities of clinical practice. By incorporating EPAs, expert feedback and portfolios, the system prepares graduates to deliver patient-centred, professional, and safe care.
Future innovations like simulation-based assessments, AI-driven capture of assessor comments and feedback systems hold promise for further improving the credibility, transferability, dependability and confirmability of assessments processes for health professional programmes. The ultimate goal is to prepare practitioners for high-quality, empathetic care in an evolving healthcare landscape.
Notes on Contributors
Dujeepa Samarasekera contributed to the concept and writing of the manuscript.
Lee Shuh Shing and Han Ting Jillian Yeo contributed to writing and editing the manuscript.
Gominda Ponnamperuma contributed to reviewing the manuscript.
Funding
This study has not received any funding.
Declaration of Interest
There are no conflicts of interests related to the content presented in the paper.
References
Cate, O. T., & Regehr, G. (2018). The power of subjectivity in the assessment of medical trainees. Academic Medicine, 94(3), 333–337. https://doi.org/10.1097/ACM.0000000000002495
Cate, O. T., & Schumacher, D. J. (2022). Entrustable professional activities versus competencies and skills: Exploring why different concepts are often conflated. Advances in Health Sciences Education, 27(2), 491–499. https://doi.org/10.1007/s10459-022-10098-7
Cruess, R. L., Cruess, S. R., & Steinert, Y. (2016). Amending Miller’s Pyramid to Include Professional Identity Formation. Academic medicine: Journal of the Association of American Medical Colleges, 91(2), 180–185. https://doi.org/10.1097/ACM.0000000000000913
Hays, R.B., Wilkinson, T., Green-Thompson, L., McCrorie, P., Bollela, V., Nadarajah, V.D., Anderson, M.B., Norcini, J., Samarasekera, D.D., Boursicot, K. and Malau-Aduli, B.S. (2024). Managing assessment during curriculum change: Ottawa consensus statement. Medical Teacher, 1-11. https://doi.org/10.1080/0142159X.2024.2350522
Miller, G. E. (1990). The assessment of clinical skills/competence/performance. Academic Medicine, 65(9), S63-7. https://doi.org/10.1097/00001888-199009000-00045
*Dujeepa D. Samarasekera
Yong Loo Lin School of Medicine,
National University of Singapore,
Block MD 11, #01-11,
Clinical Research Centre 10 Medical Drive,
Singapore 117597
Email: dujeepa@nus.edu.sg
Announcements
- Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









