Emergency medicine clerkship goes online: Evaluation of a telesimulation programme
Submitted: 30 August 2020
Accepted: 9 December 2020
Published online: 13 July, TAPS 2021, 6(3), 56-66
https://doi.org/10.29060/TAPS.2021-6-3/OA2440
Gayathri Devi Nadarajan1, Kirsty J Freeman2, Paul Weng Wan1, Jia Hao Lim1, Abegail Resus Fernandez2 & Evelyn Wong1
1Department of Emergency Medicine, Singapore General Hospital, Singapore; 2Office of Education, Duke-NUS Medical School, Singapore
Abstract
Introduction: COVID-19 challenged a graduate medical student Emergency Medicine Clinical Clerkship to transform a 160-hour face-to-face clinical syllabus to a remotely delivered e-learning programme comprising of live streamed lectures, case-based discussions, and telesimulation experiences. This paper outlines the evaluation of the telesimulation component of a programme that was designed as a solution to COVID-19 restriction.
Methods: A mixed methods approach was used to evaluate the telesimulation educational activities. Via a post-course online survey student were asked to rate the pre-simulation preparation, level of engagement, confidence in recognising and responding to the four clinical presentations and to evaluate telesimulation as a tool to prepare for working in the clinical environment. Students responded to open-ended questions describing their experience in greater depth.
Results: Forty-two (72.4%) out of 58 students responded. 97.62% agreed that participating in the simulation was interesting and useful and 90.48% felt that this will provide a good grounding prior to clinical work. Four key themes were identified: Fidelity, Realism, Engagement and Knowledge, Skills and Attitudes Outcomes. Limitations of telesimulation included the inability to examine patients, perform procedures and experience non-verbal cues of team members and patients; but this emphasised importance of non-verbal cues and close looped communication. Additionally, designing the telesimulation according to defined objectives and scheduling it after the theory teaching contributed to successful execution.
Conclusion: Telesimulation is an effective alternative when in-person teaching is not possible and if used correctly, can sharpen non-tactile aspects of clinical care such as history taking, executing treatment algorithms and team communication.
Keywords: Telesimulation, COVID-19, Emergency Medicine, Programme Evaluation
Practice Highlights
- Telesimulation doesn’t replace but can be an effective alternative when in-person teaching is not possible.
- When implemented correctly, it can sharpen non-tactile aspects of clinical care.
- It is possible to achieve a level of fidelity and realism in a telesimulation environment.
- Simulation faculty needs to be skilled in debriefing techniques that enable the learner to reflect.
- Limitations of telesimulation can be reframed as learning opportunities.
I. INTRODUCTION
COVID-19 brought about unexpected challenges to medical education, especially to student clinical clerkships where medical students would spend time within a clinical discipline, interacting with clinicians and learning from patients. Healthcare institutions restricted student movement within clinical environments and barred students from entering the high-risk frontline areas to reduce exposure risk.
Prior to COVID-19, students undertaking an Emergency Medicine (EM) Clinical Clerkship, would have the opportunity to manage and deliver care to high acuity patients, with bedside teaching, small group tutorials, problem-based learning and simulation modalities. With COVID-19, students were not permitted into the Emergency Department (ED) and face-to-face teaching activities were halted. Hence this clerkship had to be conducted remotely. The EM clerkship was transformed from a 160-hour clinical programme to a remotely administered programme comprising 40 hours of e-learning, 40 hours of interactive live online session and 15 hours of telesimulation. As part of this programme, we decided to utilise telesimulation to help students achieve some of the objectives of a clinical clerkship.
Telesimulation is defined as the “Process by which telecommunication and simulation resources are utilised to provide education, training and/or assessment to learners at an off-site location” (McCoy et al., 2017). By allowing simulation to be conducted through devices such as the computer and phone, it mitigates the problem of physical proximity. Though telesimulation has existed for about a decade, its utilisation appears limited to the rural settings and studies mainly describe its usage for learning skills (Mikrogianakis et al., 2011; Naik et al., 2020; Okrainec et al., 2010) rather than for emergency management of patients. With the need to adapt teaching to remote experiences, telesimulation is gaining popularity (Sa-Couto & Nicolau, 2020).
A. Programme Overview
This remote learning programme was developed in a tertiary ED in Singapore which receives both undergraduate and postgraduate medical students for their EM clerkship. There were 58 postgraduate medical students undertaking their 4-week EM clerkship in June 2020. The EM core clinical training curriculum was taught by EM faculty via online modules and interactive classroom sessions delivered via the video conferencing platform, Zoom. The learners spent the mornings in interactive online sessions with faculty, and afternoons in self-study as part of a flipped classroom learning, using provided learning materials. The telesimulation session was scheduled in the last week, over five days. The students were split into ten groups each comprising of five to six students, where two groups participated in one telesimulation session each day.
Our objectives for this telesimulation programme was to ensure that the students could take a focused clinical history from the simulated patients, communicate with them, construct a list of differentials and manage them accordingly in the emergency setting. The secondary objectives were to train them to prioritise the investigations and management of critically ill patients and to communicate and work effectively within a team. Using Kern’s six step approach, the team of simulation and clinical educators’ planned and implemented the telesimulation activity to achieve these outcomes (Harden et al., 1999; Smith & Dollase, 1999) during their EM clerkship.
As medical students, the learners are at a novice stage according to The Dreyfus Model of Skill Acquisition (Benner, 2004; Dreyfuss & Dreyfus, 1980). Hence, the deliberate attempt not to assess skills such as intubation or defibrillation through telesimulation as it may create unnecessary anxiety and feelings of incompetence (Papanagnou, 2017). Furthermore, it was deemed challenging to conduct procedural skill teaching through this modality. Instead, the focus was on clinical reasoning and patient management. The clinical students fall under the category of “show how” within the Miller’s pyramid, with regards to history taking, clinical reasoning and management. As adult learners, a problem centred (Knowles, 1990), experiential learning approach (Kolb, 1984) would be more valuable. Hence telesimulation was an appropriate modality.
Each telesimulation session was conducted by two simulation and one physician faculty. There was a total of four scenarios for each session, where one group, consisting of five to six students, will participate in the scenario, while the other group observes, before switching. This allowed each group of students to participate in two clinical scenarios. The topics chosen for telesimulation were Anaphylaxis, Cardiac Arrest, Meningitis, and Syncope where the theory was covered in the core topics in the preceding weeks. Each of these scenarios began with the students taking a history from the simulated patient, before the patient progressively deteriorated and required resuscitation. Figure 1 shows a summary of the scenarios. The scenarios were selected as they did not require much procedure-based interventions (e.g. chest tube insertion in a poly trauma victim) which would be difficult to assess via Zoom.
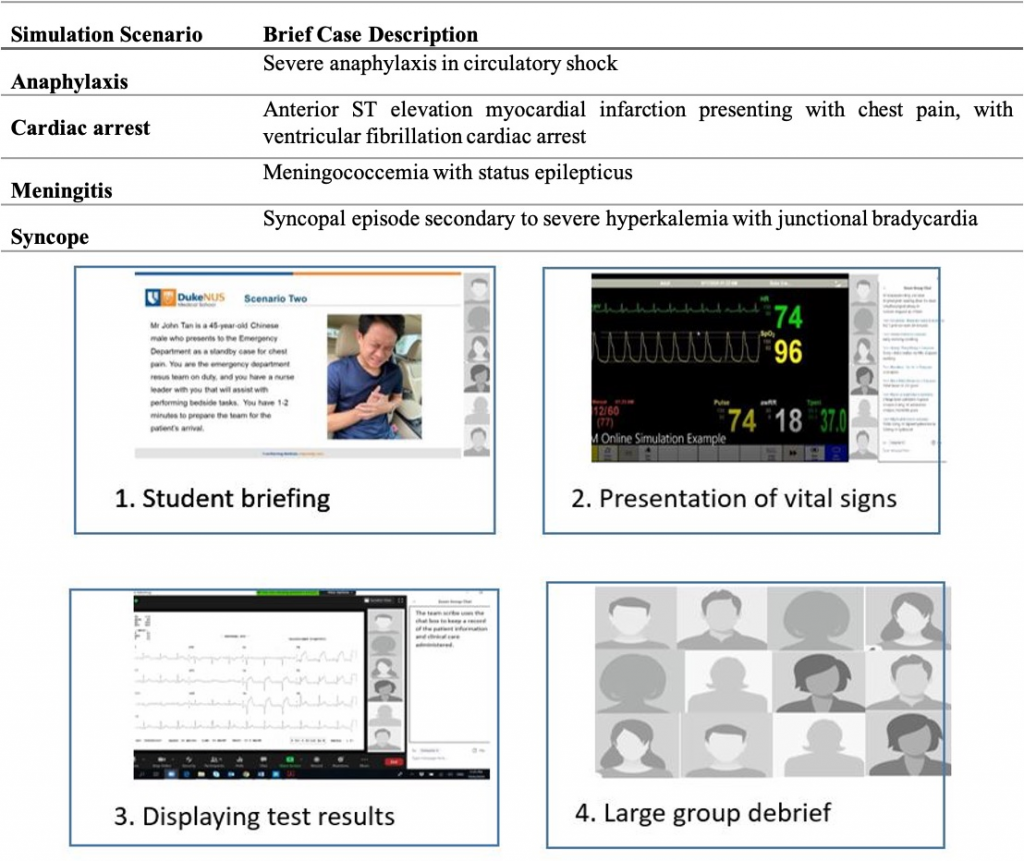
Figure 1. Brief case description of simulation scenarios and visual presentation of the flow of the telesimulation experience
The sessions commenced with a briefing where the students were orientated to the online environment, including the use of video and microphones. As depicted in Figure 1, using the share screen feature, the simulation technician switched between different views. The briefing included a photo of the patient as a visual cue, along with the text of the presenting case. One of the simulation faculty played the circulating nurse, providing prompts to aid students’ engagement and asking participants to clarify their statements or orders as the scenario progressed. Using existing mannequin software and ensuring sharing of screen sounds, real-time patient monitoring was provided to the learners when requested. Upon request, additional visual cues of investigation results would be displayed, reverting back to either a picture of the patient or the patient monitoring. With their video off, the clinical faculty voiced the patient. At the conclusion of the scenario, all participants and faculty turned their video and microphones back on to participate in the large group debrief before proceeding on to the next scenario.
The objective of this paper is to describe the students’ experience of telesimulation as part of an online clerkship programme and how such techniques can be used to meet learning outcomes (Harden et al., 1999) in various settings. At the time of writing, there is no literature describing evaluation of the use of a telesimulation programme within the ED for medical student education, with this paper aiming to address this gap.
II. METHODS
A mixed methods approach was used to evaluate the introduction of telesimulation to the EM online clerkship, and to gain students’ perspective on learning through telesimulation. Programme evaluation research aligns with a mixed methods approach as the collection of both quantitative and qualitative data provide a deeper understanding of the student experience (Cohen et al., 2011).
A. Participants, Data Collection and Analysis
58 final year medical students who participated in the EM Online Clerkship programme were invited to participate in a post-telesimulation activity evaluation survey. Using a 5-point Likert scale, students were asked to indicate their agreement on 11 items addressing pre-simulation preparation, their level of engagement, confidence in recognising and responding to the four clinical presentations and telesimulation as a tool to prepare for working in the clinical environment. Seven open-ended questions were asked to enable the students to describe their experience in greater depth. 24hrs after completing the telesimulation session, students received an email with a link to the survey. Qualtrics online survey software was used to build, distribute and collect the survey responses. Voluntary consent was assumed by participation in the anonymised online evaluation. A statement outlining the purpose of the survey was included at the start of the survey and require an agreement before the survey could be commenced. Completion of the survey therefore implied consent. The survey took between three and five minutes to complete, all responses were anonymous, with no identifiable data collected.
Descriptive statistics was used to analyse the responses to the Likert scale questions, with thematic analysis of the open-ended survey questions. Author one (GN) and author two (KF) reviewed the transcripts separately, making note of key phrases, outline possible categories or themes. Both authors then jointly rearranged and renamed the codes, developing higher order themes. NVivo 12™ was used to store, code and manage the qualitative data.
III. RESULTS
Of the 58 students who were invited to participate in the survey, 42 complete responses were received, a response rate of 72.4%. As seen in table 2, the results demonstrated that 97.62% of respondents agreed/strongly agreed that participating in the telesimulation session was interesting and useful to their learning. In relation to the use of visual and auditory cues, 93% of respondents felt that these helped them engage in the simulation. In relation to their level of preparedness to participate in the telesimulation experience, nearly 17% of respondents reported that the pre-session handout did not adequately preparing them for what to expect in the session.
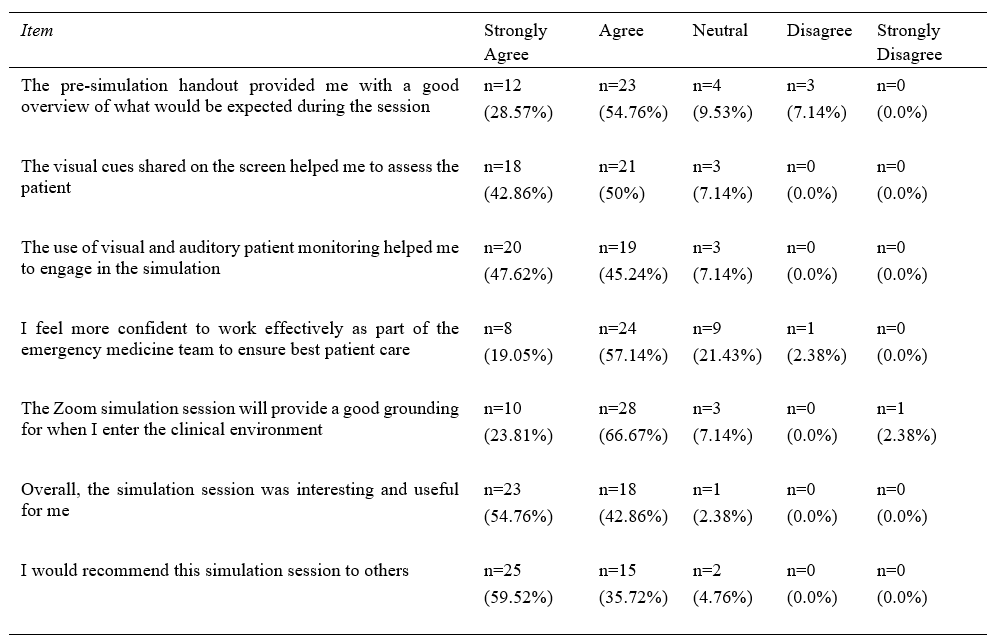
Table 1. Results of the student responses to the Likert scale items
When asked to rate if they felt more confident recognising and responding to the four clinical presentations (anaphylaxis, cardiac arrest, meningitis, and syncope), between 90% and 93% agreed/strongly agreed that participating in the telesimulation sessions resulted in them feeling more confident in recognising and responding to the specific clinical presentations (Figure 2).
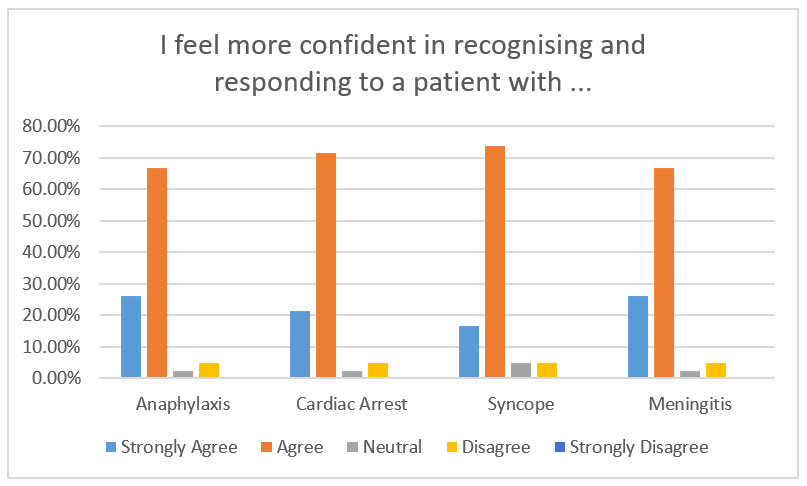
Figure 2. Student rating to the question “I feel more confident in recognising and responding to a patient with …”
Four key themes were identified following the data analysis of the open-ended survey questions, describing around the telesimulation experience of the respondents: 1) Fidelity; 2) Realism; 3) Engagement; and 4) Outcomes. As demonstrated in Figure 3, the themes do not exist in isolation, but intersect as they describe the telesimulation experience that the students had. The students feedback reflected the benefits and limitations which fall under these main themes.
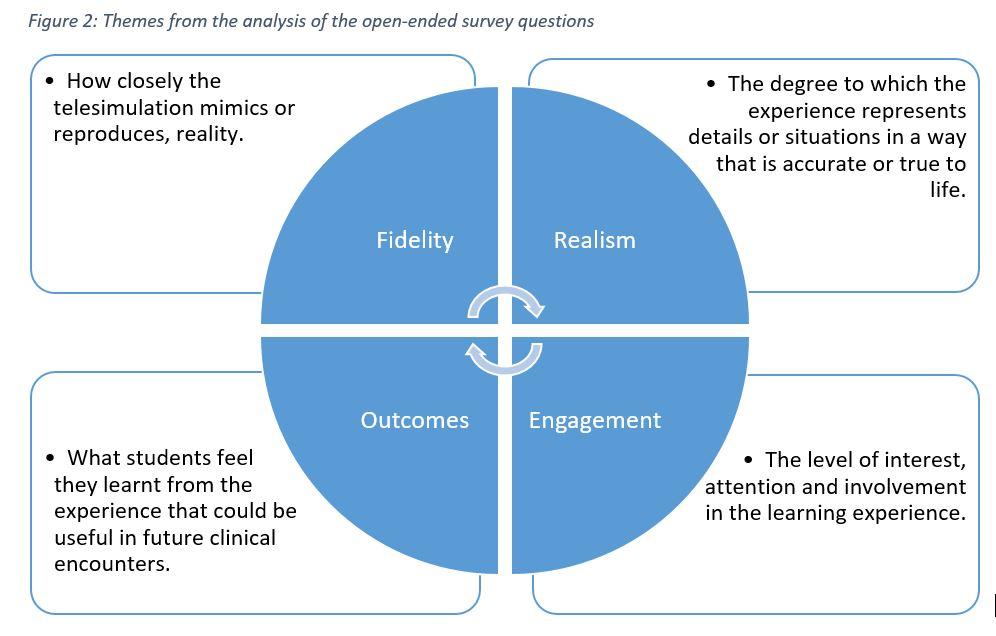
Figure 3. Themes reflecting the students experience with telesimulation
A. Fidelity – Physical, Psychological and Conceptual
The theme Fidelity reflects how closely the telesimulation mimics or reproduces, reality. Subthemes of conceptual, physical and psychological fidelity were also reflected. The students’ feedback reflected limitations in physical fidelity while conceptual and psychological fidelity was present mostly.
They reported that the auditory and visual stimulus from the dynamic display of investigations and real-time vital signs monitoring, provided a high level of physical fidelity.
“Auditory and visual information on patients’ vitals and results were really helpful in generating the differential list.”
Student 37
“The noise and sights is a good proxy for real life cases in a virtual environment.”
Student 4
“Seeing the vitals of the patient in real-time allows us to experience the importance of time in managing critically ill patients”
Student 20
However, aspects of physical fidelity, particularly related to the patient assessment, were reported as challenging via telesimulation. With the patient represented as a static picture, voiced by the clinical faculty, students shared how the lack of non-verbal and visual cues from the patient impacted their ability to perform a physical assessment of their patient.
“….we don’t get to observe the body language of the patient as much as we would like”
Student 12
“More difficult than in real life. Seeing and hearing a real patient gives much information”
Student 15
“I think what is lacking is being able to visually evaluate the patient”
Student 21
In terms of the level of psychological fidelity, the auditory cues from the ‘patient’ and the real-time vital signs monitoring simulated the ED resuscitation room, which appears to have instilled a similar sense the stress and the need to think under pressure, as reflected by the students’ feedback.
“Have to work around the distractions of beeping monitors, seizing patient, teammates asking questions/suggestions.”
Student 33
“It’s dynamic and gives us the opportunity to think under pressure.”
Student 13
“Stressful but probably close to reality?”
Student 35
The students’ statements reflected the subtheme of conceptual fidelity, where they felt the context and sequence was similar to what they would encounter in the ED, where they are required to deliver timely and lifesaving treatment. This was possibly because the faculty made deliberate attempts to ensure that events during the simulation would unfold as it usually would in the ED room, based on the learners’ actions.
“It simulates a clinical environment with real time updates of vitals and test results in addition to the history and communications.”
Student 5
What the students did report struggling with however, was the limitations of the platform in terms of multiple actions occurring simultaneously. Unlike in real life, multiple tasks could not be performed at the same time over the online platform, and this impeded the conceptual fidelity.
“In reality, multiple interventions would be carried out in tandem.”
Student 35
“More challenging to perform tasks concurrently over Zoom.”
Student 36
“…many things cannot occur concurrently.”
Student 2
B. Realism
The theme Realism captures the degree to which the experience represented details or situations in a way that is accurate or true to life. Students reported that aspects of the telesimulation experience represented what they thought an actual ED encounter would be like.
“I think the process is similar to the actual clinical environment, it is difficult, especially when the patient is deteriorating in front of you, and your team are waiting for you to make the decisions.”
Student 41
“The pictures/videos and the beeping of the monitor, they make it more real”.
Student 42
“It was realistic as getting the differentials was time sensitive”.
Student 13
The students also acknowledged the limitations in achieving realism presented by telesimulation as the various team members could not perform tasks simultaneously and take in cues from the patient to assess the outcome of their actions.
“Harder to communicate with my teammates compared to real life because only one person could speak at a time while in real life, multiple conversations could be occurring”
Student 3
“More difficult than taking a history in real life – more technical issues (can’t hear properly), Can’t see the patient”
Student 8
C. Engagement
The theme Engagement relates to the level of interest, attention and involvement in the learning experience. The level of fidelity and realism impacts the level of engagement of the learners. Most students were able to immerse themselves and fully engage in the scenarios, possibly because aspects of fidelity and realism were deliberately given close attention during the preparation phase.
“I actually forgot that the patient was being voiced by the clinical tutor”
Student 41
“My heart was racing doing the simulation – what will I be like when I am there for real?”
Student 41
However, on the downside, without being together in the same place, some felt that the scenario was too “messy” and “chaotic” and found it difficult to follow.
“It was a little hectic with the many other ongoing tasks in the background”
Student 6
“Easier to detach oneself from the patient (less affected by patient’s appearance, tone of voice, blood, gore, suffering etc.)”
Student 28
At the same time, some students faced technical difficulties, such as small or flickering screen, poor internet connection or poor audio, which were barriers to their engagement.
“…there were some issues hearing the faculty clearly which may affect the quality of learning.”
Student 6
By addressing the concepts of realism and fidelity, the students reported increased levels of engagement, although it appears that technical barriers unique to telesimulation provide challenges for some students achieving a greater level of engagement.
D. Outcomes- Knowledge, Skills and Attitudes
The theme Outcomes encompasses what students feel they learnt from the experience that could be useful in future clinical encounters. Under outcomes, there were sub-themes of knowledge, skills and attitudes. From a knowledge perspective, students reported that the telesimulation reinforced their clinical reasoning to arrive at a differential list.
“It was very useful and helped with our clinical reasoning. It was also useful in learning how to generate differential diagnoses as a team and going down the path of a working differential diagnosis while keeping others in mind.”
Student 32
Whilst the lack of hands-on practice was acknowledged, the telesimulation environment required them to practice the skills of prioritisation, leadership, teamwork and effective, close loop communication to manage the patient and this accounted for their skills gained.
“I will be able to apply the concept of teamwork, thinking on my feet, thinking broad, and constant reassessment of the unstable patient in my clinical training over the next few months”
Student 6
“Stay calm, go back to first principles, have the approach at your fingertips, make an effort to remember drug doses and administration route”
Student 2
IV. DISCUSSION
In relation to Kirkpatrick’s model for evaluating educational outcomes, the results of this study (table 1) demonstrate achievement of both level one (reactions) and level two (learning) outcomes (Kirkpatrick & Kirkpatrick, 2009). Whilst these findings may not determine the effectiveness of telesimulation, it does however provide insight into the learners’ experience that have highlighted the strengths and limitations of telesimulation, which the authors of this paper believe provides a foundation upon which others can build.
It is well documented in the simulation literature that fidelity and realism are important concepts that need to be considered when planning simulation-based education (Oliver, 2002). And this was an initial concern by the educators. The lack of a physical ‘patient’ on which to carry out procedures and physical examination could limit the effectiveness of the telesimulation experience. To address this limitation, faculty briefed the learners about the limitations and the strategies, such as the use of a ‘nurse confederate’ to provide clinical information, as well as having visual cues such as pictures and videos to trigger their actions. Interestingly, the feedback suggests that the lack of a physical ‘patient’ to examine, resulted in more emphasis being placed on the audio and visual cues during the session. This allowed the learners to proactively compensate for the lack of tactile cues with audio and visual ones, reinforcing the importance of clinical alerts and alarms. The inability to perform a physical examination provided an opportunity for the debriefer to emphasise the importance of the skill in clinical care.
There was a deliberate attempt to create scenarios that were commonly seen in the ED in as much details as possible to achieve realism in the virtual space. This limited the scenarios that could be used as we had to use ensure procedures were not required for the patient management to progress (for example, trauma was deemed inappropriate). The faculty feel that the typical, non-complex ED scenarios compounded with the sequence of events as it would occur in real life possibly contributed to the student’s perception of realism during the telesimulation.
Instructional scaffolding was key to student engagement. The faculty configured the telesimulation session to be held after three weeks of interactive and didactic sessions on Zoom. This allows the learners to acquire essential knowledge which they can then apply during the telesimulation session. With the background baseline knowledge, the telesimulation setup and audio and visual prompts of a real ED environment, the faculty felt that they were able to immerse the students within the scenario rather than conducting it as an online Problem-Based-Learning session. This may have contributed to their engagement.
Communication skills were a common thread reported by the students, both positively and negatively in many of their statements. They described the shortcomings of communication over Zoom and felt that the session highlighted how non-verbal cues and the physical presence influences the way one communicates. At the same time, the absence of visual and tactile stimuli forced them to practice good communication to get their points across when managing the patients.
Interestingly, though many students scored high on the Likert scale about feeling confident in managing emergencies, with the open-ended questions, they reflected feelings of nervousness, fear and a lack of confidence to working in the ED, showing that perhaps this cannot replace patient contact.
Cognisant of the limitations of telesimulation, most of the learners enjoyed the session. This may have been due to the novelty of it and ED room mimics such as the beeping of the monitors and the realistic scenarios. Faculty also realise that the limitations of telesimulation and used them as discussion points to highlight elements that one may take for granted during their patient encounters, such as the non-verbal cues and the tactile stimuli.
Key to this successful telesimulation session was establishing realistic and focused objectives (Harden et al., 1999). Failing to recognise that telesimulation differs from conventional simulation and therefore emphasising on tactile skills such as procedures and physical examination will minimise the effectiveness of the session. Knowing the inherent limitations helped faculty to prepare holistically for the session. Learning objectives focused on non-tactile aspects, such as history taking and executing treatment algorithms. In addition, as tactile cues are limited in the telesimulation setting, all other cues such as visual and audio were optimised.
Debriefing during the telesimulation sessions has an even more vital role in student learning compared to conventional simulation sessions (Fanning & Gaba, 2007). The debriefer not only has to highlight salient clinical points regarding the case, but also probe learners to think about limitations of the telesimulation modality. Therein, understanding the importance of highlighting tactile and visual feedback. For example, one learner recognised that he was “unable to visually observe and direct the teammate”; another came to the conclusion that “being able to see the patient and physical expression of fellow doctors/nurses is crucial”. This allows the educator to discuss the importance of situational awareness and non-verbal cues in enhancing team dynamics. However, if the debriefer fails to address this limitation, the learners may leave the session feeling dissatisfied or inadequate with their performance at the session. The uniqueness of telesimulation adds another facet to debriefing where the debriefer needs to be able to address the limitations of telesimulation and relate it back to clinical relevance. Therefore, there might be a need to provide additional training for educators in debriefing telesimulation sessions.
Simulation-based training is an effective modality to teach procedural skills, put into practice treatment algorithms and hone soft-skill relevant to team dynamics. (Lateef, 2010; Sirimanna & Aggarwal, 2014). As demonstrated through this innovative programme, it has an important role to play in medical education during such a pandemic where it might be used to mitigate the negative educational impact of no patient contact, team-based training and protocol development and testing (Chaplin et al., 2020; Dieckmann et al., 2020). All this is done within a psychologically and physically safe environment.
Based on the feedback collected, a conceptual framework below (Figure 4) was drawn, showing the relationship between the concepts of fidelity and realism in the telesimulation experience to the level of engagement and therefore outcomes perceived by the learners. This is supported by the objectives, experiential learning and a safe learning environment.
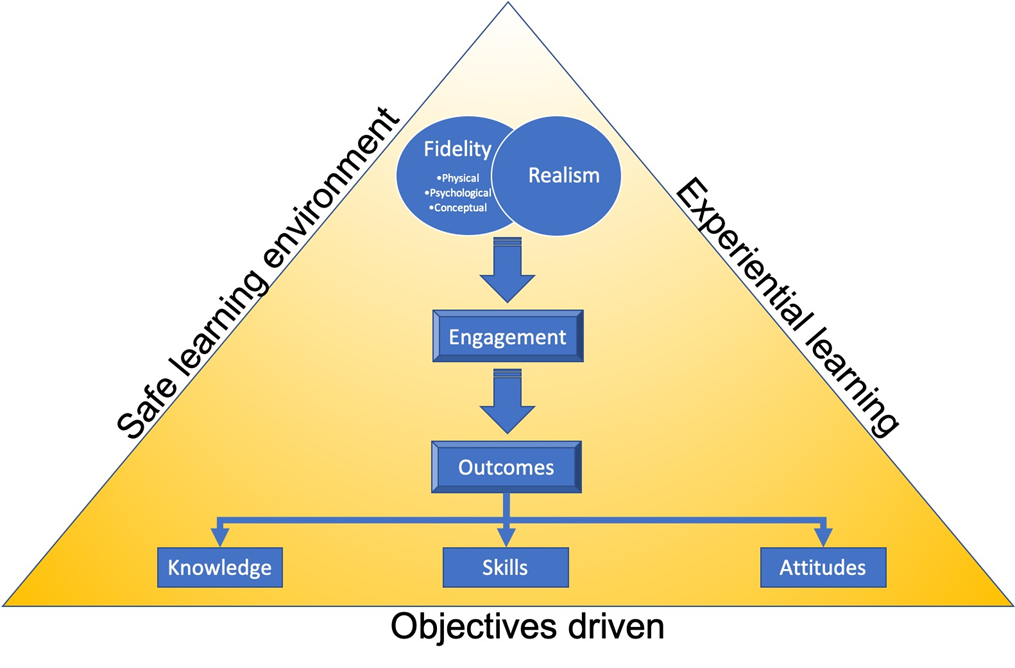
Figure 4. Conceptual framework
V. CONCLUSION
The role of face-to-face interactions with patients and immersing oneself in the acute care environment in bridging the theory to practice gap experienced by all healthcare students is essential to their clinical training. The restrictions encountered due to COVID-19 have required clinical educators to be agile and innovative in their approach the clinical clerkships. The EM clerkship telesimulation programme set out to provide an avenue for medical students to hone their clinical skills (history taking) and clinical reasoning (deriving differential diagnosis) in a safe environment. The evaluation of this programme has highlighted key areas of telesimulation which educators need to consider when planning to use it. The feedback from the students is promising and it highlights certain teaching points which may not be reflected upon during in-person simulation. Educators who wish to implement a telesimulation programme should pay particular attention to the learning objectives and debriefing methods. Whilst this paper has outlined how telesimulation can be implemented during a pandemic, it is envisaged that educators from other healthcare disciplines could use these findings to support the adoption of telesimulation in a variety of educational contexts. Telesimulation is a good alternative in settings such as this pandemic or during distance training programmes and may be a convenient way to hone history taking, clinical reasoning and communication skills without the use of an expensive simulation laboratory. The modality needs to meet the learning objectives and the debriefing should be adopted for telesimulation. However, the authors/faculty feel it cannot replace the full benefits of in-person simulation or learning from direct patient contact.
Notes on Contributors
Gayathri Devi Nadarajan and Kirsty J Freeman conceptualised the article, undertook the thematic analysis, contributed to article sections, and reviewed and revised manuscript based on suggestions from the other authors.
Lim Jia Hao, Wan Paul Weng and WONG Evelyn contributed to the conceptualisation of the paper, contributed to the article sections, reviewed and revised drafts.
Abegail Resus Fernandez undertook the quantitative analysis, and reviewed drafts.
All authors were involved in the development and delivery of the EM Clerkship Telesimulation Programme. All the authors have read and approved the final manuscript.
Ethical Approval
The SingHealth Centralised Institutional Review Board (CIRB) granted an exemption, CIRB Ref. No.: 2020/2719, as this study was assessed as a quality improvement project.
Data Availability
All relevant data are within the manuscript.
Acknowledgement
We would like to thanks the students who participated in this unit and their willingness to adapt to the online platform with grace and enthusiasm.
Funding
This work has not received any external funding.
Declaration of Interest
All authors declare that there are no conflicts of interest.
References
Benner, P. (2004). Using the dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bulletin of Science, Technology and Society, 24(3), 188–199. https://doi.org/10.1177/0270467604265061
Chaplin, T., McColl, T., Petrosoniak, A., & Hall, A. K. (2020). Building the plane as you fly: Simulation during the COVID-19 pandemic. Canadian Journal of Emergency Medicine, 22(5), 576–578. https://doi.org/10.1017/cem.2020.398
Cohen, L., Manion, L., & Morrison, K. (2011). Research methods in education. Routledge. https://doi.org/10.4324/9780203720967
Dieckmann, P., Torgeirsen, K., Qvindesland, S. A., Thomas, L., Bushell, V., & Langli Ersdal, H. (2020). The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: Practical tips and resources from Norway, Denmark, and the UK. Advances in Simulation, 5(1), 1–10. https://doi.org/10.1186/s41077-020-00121-5
Dreyfuss, S. E., & Dreyfus, H. L. (1980). A five-stage model of the mental activities involved in directed skill acquisition. Berkeley. https://apps.dtic.mil/dtic/tr/fulltext/u2/a084551.pdf
Fanning, R. M., & Gaba, D. M. (2007). The role of debriefing in simulation-based learning. Simulation in Healthcare, 2(2), 115–125. https://doi.org/10.1097/SIH.0b013e3180315539
Harden, R. M., Crosby, J. R., & Davis, M. H. (1999). AMEE Guide No. 14: Outcome-based education: Part 1 – An introduction to outcome-based education. Medical Teacher, 21(1), 7–14. https://doi.org/10.1080/01421599979969
Kirkpatrick, D. L., & Kirkpatrick, J. D. (2009). Evaluating: Part of a ten-step process. In evaluating training programs. Berrett-Koehler Publishers.
Knowles, M. S. (1990). The adult learner: A neglected species. Gulf Publishing Co.
Kolb, D. A. (1984). The process of experiential learning. Experiential learning: Experience as the source of learning and development (pp. 20-38). Prentice Hall.
Lateef, F. (2010). Simulation-based learning: Just like the real thing. Journal of Emergencies, Trauma, and Shock, 3(4), 348. https://doi.org/10.4103/0974-2700.70743
McCoy, C. E., Sayegh, J., Alrabah, R., & Yarris, L. M. (2017). Telesimulation: An innovative tool for health professions education. Academic Emergency Medicine Education and Training, 1(2), 132–136. https://doi.org/10.1002/aet2.10015
Mikrogianakis, A., Kam, A., Silver, S., Bakanisi, B., Henao, O., Okrainec, A., & Azzie, G. (2011). Telesimulation: An innovative and effective tool for teaching novel intraosseous insertion techniques in developing countries. Academic Emergency Medicine, 18(4), 420–427. https://doi.org/10.1111/j.1553-2712.2011.01038.x
Naik, N., Finkelstein, R. A., Howell, J., Rajwani, K., & Ching, K. (2020). Telesimulation for COVID-19 Ventilator management training with social-distancing restrictions during the coronavirus pandemic. Simulation and Gaming, 51(4), 571–577. https://doi.org/10.1177/1046878120926561
Okrainec, A., Henao, O., & Azzie, G. (2010). Telesimulation: An effective method for teaching the fundamentals of laparoscopic surgery in resource-restricted countries. Surgical Endoscopy, 24(2), 417–422. https://doi.org/10.1007/s00464-009-0572-6
Oliver, R. G. (2002). Simulation-based medical education. In R. M. Harden & J. A. Dent (Eds.), A practical guide for medical teachers (4th ed., Vol. 29, Issue 2, pp. 226–233). Churchill Livingstone.
Papanagnou, D. (2017). Telesimulation: A paradigm shift for simulation education. Academic Emergency Medicine Education and Training, 1(2), 137–139. https://doi.org/10.1002/aet2.10032
Sa-Couto, C., & Nicolau, A. (2020). How to use telesimulation to reduce COVID-19 training challenges: A recipe with free online tools and a bit of imagination. MedEdPublish, 9(1), 1–7. https://doi.org/10.15694/mep.2020.000129.1
Sirimanna, P. V., & Aggarwal, R. (2014). Patient safety. In Levine, A., DeMaria, S., Jr., Schwartz, A. D., & Sim. A. J. (Eds.). The comprehensive textbook of healthcare simulation. Springer.
Smith, S. R., & Dollase, R. (1999). AMEE guide No. 14: Outcome-based education: Part 2 – Planning, implementing and evaluating a competency-based curriculum. Medical Teacher, 21(1), 15–22. https://doi.org/10.1080/01421599979978
*Gayathri Devi Nadarajan
Department of Emergency Medicine
Singapore General Hospital
1 Outram Road, Singapore 169608
Tel: +65 96804724
Email: gayathri.devi.nadarajan@singhealth.com.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









