In situ simulation in a time of pandemic
Submitted: 16 July 2020
Accepted: 16 September 2020
Published online: 13 July, TAPS 2021, 6(3), 95-98
https://doi.org/10.29060/TAPS.2021-6-3/SC2342
Shin Ying Thng, Bao Yu Geraldine Leong, Guat Keng Yvonne Goh, Ching Ching Elaine Tan, Jimmy Kock Keng Goh & Kaibin Kelvin Kuan
Emergency Department, Changi General Hospital, Singapore
Abstract
Introduction: Singapore was one of the earliest countries affected by the COVID-19 outbreak, requiring our emergency department to respond urgently to this surge. A designated Fever Area (FA) with a resuscitation room was rapidly set up to manage patients at risk of COVID-19. Our paper describes measures put into this new area to optimise safety outcomes of these patients.
Methods: Plan-Do-Study-Act (PDSA) cycles incorporating in-situ simulation in the FA resuscitation room were conducted. Using varied resuscitation scenarios and facilitated debriefing, we identified safety gaps and took immediate steps to rectify them in a collaborative manner involving various respective stakeholders.
Results: Following reflective debriefing and studying of work processes, latent safety threats were identified resulting in successful improvements and modifications to protocols, equipment, staffing and processes in the FA resuscitation area.
Conclusion: PDSA cycles involving in-situ simulation helped to identify safety threats and refine work processes in a newly set up FA facility. As a result, our healthcare team was more prepared to manage the complexities of COVID-19 patients in a high-risk environment.
Keywords: Simulation, COVID-19, Medical Education
I. INTRODUCTION
Singapore was one of the first countries to be affected by the COVID-19 pandemic and has the highest number of Covid-19 cases in South East Asia to date. When the COVID-19 outbreak first reached Singapore, healthcare facilities had to prepare for a surge of patients with suspected or confirmed COVID-19. Our Emergency Department (ED) serves a 1006 bed hospital and sees an average of 400 patients daily pre-COVID-19. We were required to quickly reconfigure our space, equipment and staff. There was a need to segregate high risk or suspect COVID cases to be seen in a separate area in order to minimise cross-infection risks to our vulnerable patients. There was also a need to limit exposure of high-risk patients to a designated team of doctors and healthcare professionals in order to ensure continuity of services.
An area comprising the original admission transit area (with three isolation negative pressure rooms) and unused outpatient clinics next to the main ED underwent reconfiguration to become the new designated Fever Area (FA). This was to allow easy access to shared ED resources. The new FA had a combined capacity of 58 patients. Two FA resuscitation rooms were set up to cater for rapidly deteriorating patients that will require endotracheal intubation and resuscitation, both for COVID related complications as well as non-infectious related medical emergencies, such as an acute myocardial infarction or an acute surgical abdomen. Adequate resuscitation and stabilisation facilities in the FA were needed to minimise unnecessary movements of these infectious critically ill patients to the resuscitation area in the main ED, thus, decreasing the risk of cross-infection in other personnel.
The first few patient resuscitations conducted in the FA were challenging. There were many issues raised by the healthcare team concerning resuscitating and performing high-risk procedures in an unfamiliar environment. The FA team recognised an urgent need to improve system workflow competence in the FA resuscitation area. The healthcare team had to be shown that the improved FA resuscitation rooms were as well equipped as the main ED resuscitation area to handle critically ill patients and that such patients can be stabilized effectively there.
II. METHODS
In-situ simulation was the chosen modality as many of the difficulties encountered were systemic issues related to acute care in the unfamiliar FA resuscitation rooms and appropriate usage of Personal Protective Equipment (PPE) in such a scenario. In-situ simulation occurs where the case scenario is simulated in the actual clinical care area with real inter-professional teams instead of in an artificial setting in the simulation centre. By carrying out in-situ simulation, the team hoped to be able to recognise and remedy potential active failures and latent threats (Couto et al., 2018) present in the FA resuscitation rooms before any real-life adverse outcomes (Raemer et al., 2018) can occur.
Four emergency physicians and two nurse clinicians experienced in simulation design and debriefing conducted four in-situ simulation sessions with a high-fidelity mannequin in the FA (Dieckmann et al., 2020). Safety of all faculty, staff and patients were a priority and careful measures were taken to ensure participants and patients were not put at risk by simulating in-situ (Knight et al., 2018). Simulation sessions were conducted at the time of lowest patient load and all participants were outfitted in full PPE. They were also educated prior on potential safety hazards of in-situ simulation. Participant numbers for each simulation session were kept small at five to six with two facilitators.
The simulation scenarios, comprising of COVID-19 patients deteriorating from acute myocardial infarction, respiratory failure and cardiac arrest, were designed to challenge the complexities of adapting clinical management, manpower and equipment requirement and existing workflows to an infectious setting.
A multidisciplinary team comprising of eight nurses, six doctors and two radiographers involved in patient care at the FA participated in four simulation sessions held over two months. Verbal informed consent was taken from participants prior to simulation and confidentiality of participants was ensured. Centralised Institution Review Board (CIRB) review was submitted and waiver of consent was obtained. After each simulation scenario, formalised debriefing was carried out immediately, focusing on work process issues, communication failures and latent threats identified within the FA. Questions were crafted to guide participants to attain dialogical reflection and to move past a description of errors. They were encouraged to consider the implications of observations and come up with solutions for change using Fleck’s framework of reflection levels (Kihlgren et al., 2015).
The list of ideas generated was gathered and studied for common themes. A separate session was held where clinical, operational and administrative representatives brainstormed to find feasible and practical solutions to each problem identified. Immediate steps were taken to implement improvements and modifications to clinical protocols, equipment, staffing and workflows. Plan-Do-Study-Act (PDSA) quality improvement cycles were used to evaluate the improvements instituted after each simulation. This was carried out by a multidisciplinary team, comprising of medical, nursing and allied health staff.
III. RESULTS
The latent safety threats that surfaced were broadly categorised into five descriptive categories: Equipment, Organization, Staffing, Communication and Protocol (Refer to Table 1).
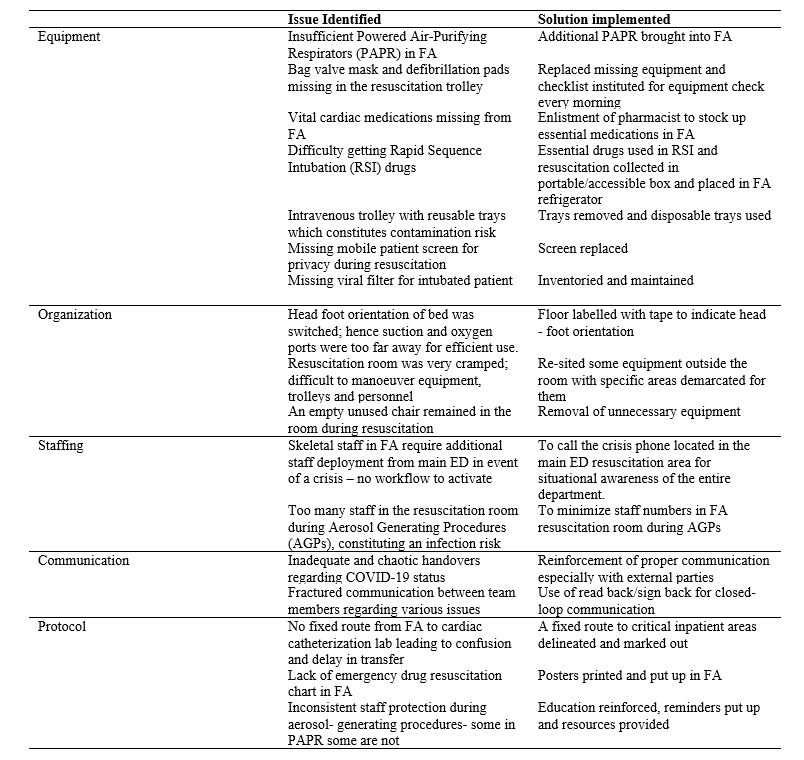
Table 1: Results
In-situ simulation uncovered the problems of insufficient Powered-Air Purifying Respirators (PAPR) and viral filters, as well as, missing defibrillator pads and bag valve masks from resuscitation trolleys. A checklist of essential equipment and medications was created with mandatory checks and re-stocking carried out by the FA nurses every morning. Medications vital for resuscitation were also found to be inadequate. A pharmacist was recruited to draw up and stock an essential list of drugs in the FA. Medications, which required refrigeration, were packed in a portable box so they could be easily brought to the FA resuscitation room from the fridge when required. Drug and resuscitation charts were put up as reminders and easy reference to improve patient safety.
Workspace organization issues that surfaced from in-situ simulation included the need to maintain patient privacy with mobile screens during resuscitation. Confusion over the head-foot orientation of the trolley bed resulted in suction and oxygen ports being too far for efficient use when it was placed in the wrong configuration. To correct this, the FA resuscitation room floor was labelled with tape indicating the proper orientation. The small FA resuscitation room area made manoeuvring equipment, trolleys and personnel difficult. Efforts were taken to re-site equipment to specific demarcated areas outside the FA resuscitation room, with the added benefit of reducing equipment contamination. A crisis phone was set up so that existing staff in FA could quickly call for additional staff deployment in event of a surge, thus improving communication and increasing situational awareness of the entire department to emergent needs at the FA.
Protocols were also adapted to the needs of the FA. During a resuscitation scenario, too many healthcare workers crowded into the room, raising a safety concern. It was protocolised that staff numbers should be minimized in the FA resuscitation room, especially during Aerosol Generating Procedures (AGP). PPE use was a barrier to communications, with “handovers” and “read back” being disrupted or unclear. The importance of adhering to these communication tools was reinforced. There was no fixed route identified for the transport of infectious patients to critical inpatient areas, thus, these were delineated so as to minimize confusion and decrease the infectious footprint, and risk of cross-infection to others. Staff protection during AGP was found to be inconsistent; hence PPE education was reinforced and educational resources provided to staff.
IV. CONCLUSION
Many issues were surfaced and lessons learnt via in-situ simulation, which allowed immediate risk mitigation to be carried out. Simple, immediate changes were made in FA with the available resources, resulting in improved patient and staff safety—which is especially important during surges due to the COVID-19 pandemic. We have successfully used in situ simulation with PDSA cycles to test and develop new facilities and protocols whilst managing the demands of a pandemic. Similar outcomes had also been demonstrated in other in-situ simulation studies. Using this modality to test pre-existing protocols and equipment in the FA resuscitation rooms offered an opportunity for the identification of potential threats and service gaps that would otherwise not have been detected as efficiently via conventional reporting systems (Knight et al., 2018). This method of PDSA testing is useful in the rapidly evolving COVID-19 situation, and may be replicated in other hospitals and regions safely when required. It ensures the safety of healthcare workers and actively improves patient safety despite the limitations of the pandemic.
A follow-up study to look at the usage of the FA resuscitation area, number of critically ill patients in the FA being transferred into the main ED resuscitation room, and patient morbidity and mortality data would be necessary to further determine the success of our intervention at a higher Kirkpatrick level of behavioural change to improve patient outcomes in the FA.
Notes on Contributors
Dr Elaine Tan carried out the literature search and instituted the changes. Dr Geraldine Leong ran the simulation, wrote the manuscript and instituted the changes. Dr Jimmy Goh set up the fever area, advised regarding the manuscript and instituted the changes. Dr Kelvin Kuan ran the simulation, wrote the manuscript and instituted the changes. Dr Thng Shin Ying designed the simulation, ran the simulation, and wrote the manuscript. Dr Yvonne Goh designed the simulation, ran the simulation and wrote the manuscript.
Ethical Approval
This study was exempted from CIRB review- 2020/2640.
Acknowledgements
The authors would like to acknowledge the staff of Changi Simulation Institute for their technical help and assistance with this project. We would also like to thank Dr Syahid Hassan for providing his expertise in the methodology of this project.
Funding
No funding was required.
Declaration of Interest
The authors state no conflict of interest.
References
Couto, T. B., Barreto, J. K. S., Marcon, F. C., Mafra, A. C. C. N., & Accorsi, T. A. D. (2018). Detecting latent safety threats in an interprofessional training that combines in situ simulation with task training in an emergency department. Advances in Simulation, 3(1), 23. https://doi.org/10.1186/s41077-018-0083-4
Dieckmann, P., Torgeirsen, K., Qvindesland, S. A., Thomas, L., Bushell, V., & Langli Ersdal, H. (2020). The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: Practical tips and resources from Norway, Denmark, and the UK. Advances in Simulation, 5, 3. https://doi.org/10.1186/s41077-020-00121-5
Kihlgren, P., Spanager, L., & Dieckmann, P. (2015). Investigating novice doctors’ reflections in debriefings after simulation scenarios. Medical Teacher, 37(5), 437-443. https://doi.org/10.3109/0142159X.2014.956054
Knight, P., MacGloin, H., Lane, M., Lofton, L., Desai, A., Haxby, E., Macrae, D., Korb, C., Mortimer, P., & Burmester, M. (2018). Mitigating latent threats identified through an embedded in situ simulation program and their comparison to patient safety incidents: A retrospective review. Frontiers in Pediatrics, 5, 281. https://doi.org/10.3389/fped.2017.00281
Raemer, D., Hannenberg, A., & Mullen, A. (2018). Simulation safety first: An imperative. Simulation in Healthcare, 13, 373-375. https://doi.org/10.1097/SIH.0000000000000341
*Thng Shin Ying
Changi General Hospital
2 Simei Street 3
Singapore, 529889
Email: thng.shin.ying@singhealth.com.sg
Announcements
- Fourth Thematic Issue: Call for Submissions
The Asia Pacific Scholar is now calling for submissions for its Fourth Thematic Publication on “Developing a Holistic Healthcare Practitioner for a Sustainable Future”!
The Guest Editors for this Thematic Issue are A/Prof Marcus Henning and Adj A/Prof Mabel Yap. For more information on paper submissions, check out here! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Volume 9 Number 1 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors. - Volume 8 Number 3 of TAPS is out now! Click on the Current Issue to view our digital edition.

- Best Reviewer Awards 2021
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2021.
Refer here for the list of recipients. - Most Accessed Article 2021
The Most Accessed Article of 2021 goes to Professional identity formation-oriented mentoring technique as a method to improve self-regulated learning: A mixed-method study.
Congratulations, Assoc/Prof Matsuyama and co-authors. - Best Reviewer Awards 2020
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2020.
Refer here for the list of recipients. - Most Accessed Article 2020
The Most Accessed Article of 2020 goes to Inter-related issues that impact motivation in biomedical sciences graduate education. Congratulations, Dr Chen Zhi Xiong and co-authors.









