Eight tips for inclusion of persons with disabilities as standardised patients
Published online: 5 May, TAPS 2020, 5(2), 41-44
https://doi.org/10.29060/TAPS.2020-5-2/SC2134
Sok Mui May Lim1,2, Zi An Galvyn Goh2 & Bhing Leet Tan1
1Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore; 2Centre for Learning Environment and Assessment Development (CoLEAD), Singapore Institute of Technology, Singapore
Abstract
The use of standardised patients has become integral in the contemporary healthcare and medical education sector, with ongoing discussion on exploring ways to improve existing standardised patient programs. One potentially untapped group in society that may contribute to such programs are persons with disabilities. Persons with disabilities have journeyed through the healthcare system, from injury to post-rehabilitation, and can provide inputs based on their experiences beyond their conditions. This paper draws on our experiences gained from a two-phase experiential learning research project that involved occupational therapy students learning from persons with disabilities. This paper aims to provide eight highly feasible, systematic tips to involve persons with disabilities as standardised patients for assessments and practical lessons. We highlight the importance of considering persons with disabilities when they are in their role of standardised patients as paid co-workers rather than volunteers or patients. This partnership between persons with disabilities and educators should be viewed as a reciprocally beneficial one whereby the university and the disability community learn from one another.
Keywords: Standardised Patients, Objective Structured Clinical Examination (OSCE), Persons with Disabilities, Inclusion, Role-play, Script, Practical Lessons
I. INTRODUCTION
The use of standardised patients (SPs) has become integral to the contemporary healthcare and medical education sector. While an SP is commonly defined as a person trained to portray a scenario, an SP can also be an actual patient using his or her own history and physical exam findings (Kowitlawakul, Chow, Salam, & Ignacio, 2015). Presently, persons with disability (PWDs) have participated in SP programs, albeit less frequently and on a smaller scale (Long-Bellil et al., 2011; Minihan et al., 2004; Wells, Byron, McMullen, & Birchall, 2002). SPs with disabilities have also been used in Singapore hospitals, but mainly as patients to be examined for their own medical conditions. PWDs have a lot to offer in clinical education beyond sharing about their conditions.
A. Why Incorporate Persons with Disabilities into SP Programs?
There are many benefits in involving PWDs in SP programs. PWDs may be able to impart knowledge that ‘goes beyond the textbook’, due to their experiences of receiving services from various healthcare professionals – from the time the disability occurred to the post-rehabilitation phase of living independently in society. The input given based on their individual experiences would, therefore, be authentic (Wells et al., 2002). Students can get practice working with real PWDs in a safe setting where they can make mistakes and receive feedback before going for their clinical placements and meeting with real patients (Minihan et al., 2004). This can nurture a new generation of healthcare professionals who may be more proficient in treating PWDs, thereby raising the service delivery standard for the entire sector.
B. Perspectives Gained From Previous Experiential Learning Project
This paper is based on our experiences gained from a previous experiential learning research project. PWDs participated in a two-phase experiential learning research project that spanned two years (Lim, Tan, Lim, & Goh, 2018). In phase one, the PWDs acted as community teachers to occupational therapy student groups, interacting with them in the community while performing their daily activities. This paper draws from our experiences in Phase Two of the study, in which a group of PWDs were trained to and worked as SPs in practical classes and Objective Structured Clinical Examinations (OSCEs). Upon the conclusion of the research project, PWDs continue to be part of the degree programme contributing as community teachers and SPs. The paper aims to provide practical helpful tips in bringing PWDs onboard as SPs.
II. DISCUSSION
A. Tip 1 – Interviewing and Selecting PWDs Who Are Suitable for Acting
PWDs were selected based on six criteria determined by faculty members in the health profession who have prior experience working with SPs. First, the PWD has an interest in healthcare education and wants to work with students for the purpose of educating them as future healthcare professionals. Second, the PWD should have come to terms and accepted their disability. It is very difficult for them to talk about their disability or role-play as a patient when they are still struggling emotionally with their own conditions. Third, the PWD does not have cognitive impairment and is able to understand and remember the script for role-playing. Fourth, he/she must be able to communicate clearly and coherently. Fifth, the PWD should be willing to learn the basics of acting or role-playing. Sixth, he/she must understand the objectives of the training or assessment, such as being impartial to all students and being honest in giving feedback when required.
B. Tip 2 – Training Should Be Conducted in Gradual Phases
Training PWDs as SPs can be carried out in a gradual phase as outlined in details in Figure 1. In the first phase, novice PWD SPs are taught the basics of role-play by faculty and experienced SPs. In the second phase, the entire group goes through a common script. Novice PWD SPs observe the faculty and experienced SPs enact the script. Then, the novice PWD SPs practice amongst themselves and receive feedback.
After the training, faculty should speak to the PWDs individually to determine if they are comfortable with role-playing and address any queries that they may have. It is only after they attempt the role of an SP that they can personally assess their comfort level and confidence. This can ensure that the PWDs who participate are comfortable with their roles and feel engaged and respected by the institution.
In the third phase, PWD SPs can progress to non-graded practical lessons with students, which are less stressful for both students and PWD SPs. In subsequent phases, the faculty can then decide to select PWD SPs whom they deem are ready for summative assessments such as the OSCE.
C. Tip 3 – Start Novice PWD SPs with Simple and Suitable Scripts
Initial scripts should be simple and should not require complex acting skills. It takes time to gain confidence in memorising required lines, maintaining their roles as well as acting in scenarios which require more expression of emotions. Scripts that involve more sophisticated acting skills (e.g., maintenance of strong emotions) should be reserved for SPs who are experienced and confident with acting. The PWD SPs should be matched to suitable scripts that do not conflict with their disability. For example, a PWD SP who uses a wheelchair cannot be paired with a script that involves walking. The combination of progressing gradually and usage of suitable scripts allows for PWD SPs to refine their skills and ensure that their acting skills do not compromise the students’ learning experience.
D. Tip 4 – Prepare Students Not to Be Surprised By Real Disability
Prior to the interaction session, students should be pre-empted by the faculty that they would be working with PWDs who may have a range of disabilities. This is to prevent unnecessary surprise. In addition, students should be reminded that the disability may or may not be the focus of the scenario, depending on the instruction given to the student. For example, in an OSCE scenario, students may be tasked to explain a medical error or demonstrate a procedural skill instead of addressing the disability of the SP. This pre-empting can be complemented with teaching communication skills geared towards interacting with PWDs.
E. Tip 5 – Checking Accessibility – Within and Outside of the Venue
Ensuring accessibility prior to the session is important. This includes the route from the nearest public transport node (e.g., train station) to the venue. Things to take note of are the availability of ramps and lifts for wheelchair users and the presence of accessible parking lots. In addition, the venue where the lesson or assessment is going to take place needs to be inspected to ensure that the entrances and exits are wide enough for wheelchairs access.
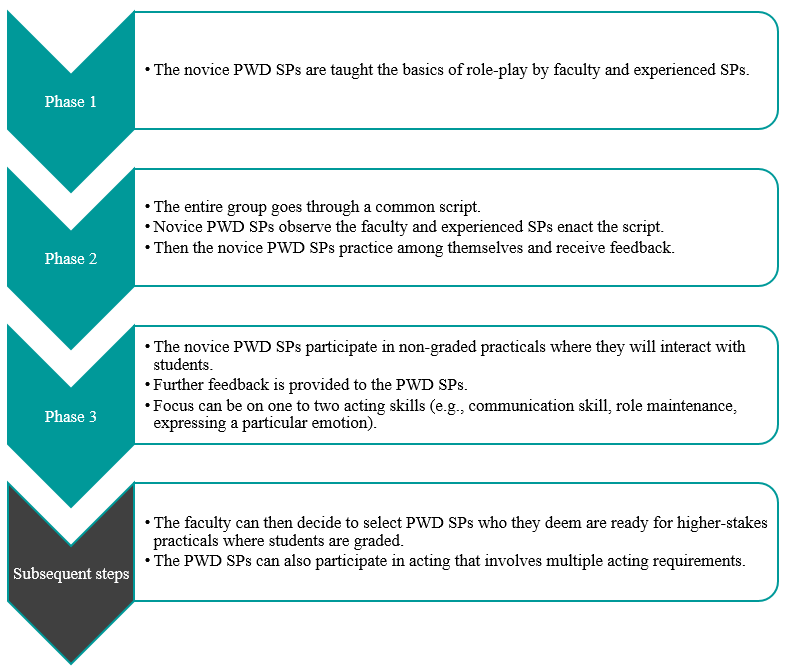
Figure 1. Diagram to outline general recommended steps for training PWD SPs
F. Tip 6 – Pay PWDs at Market Rates and Accord Them Identical Contractual Rights
PWD SPs should be remunerated at market rates that are equal to SPs without disability. They also sign the same SP contract and fulfil the same legal obligations. In performing the role of the SP, they are treated as co-workers of the university, not volunteers or patients. This reflects the principles of equality and diversity, as well as the seriousness of their roles as active members of the healthcare and medical education system. If there are certain risks involved in their interaction with students, such risks should be made clear to the PWD SPs, so they can make an informed decision on accepting the job.
G. Tip 7 – Provide Opportunity for PWDs to Give Feedback
PWDs can be a valuable resource in providing feedback to faculty, scenario developers and other SPs. Similarly, they may be able to give insightful feedback to students. It is important to train the PWD SPs on the methods of providing feedback to students. Given their lived experience, they can provide insight into how real patients would respond and react while suggesting ways for trainee healthcare professionals to respond in a more patient-centred manner.
H. Tip 8 – Reflect and Improve
Carrying out an evaluation with the respective stakeholders, whether they are PWD SPs, faculty, or students, is key to the success of an inclusive SP program. This can also ensure quality assurance of the program. The following are several broad questions which can be considered in the evaluation. Firstly, whether the stakeholder faced any challenges during the session. Secondly, whether the scenarios or scripts worked well for PWD SPs to interact with students. Thirdly, whether there are any other ways that the learning experience can be improved. This can provide rich data for the SP program developers to reflect and improve upon the pedagogy. We have received positive feedback from both students and PWDs in this project.
III. CONCLUSION
It is important to empower PWDs and create a dynamic relationship between them and healthcare professionals/
educators. For an inclusive SP program to be effective, educators must change their own mindset about PWDs. We have to switch the lens from viewing them as patients to co-workers. This partnership should be viewed as a reciprocally beneficial one whereby the university and the disability community learn from one another. Through the process of engagement, both educators and students learn from PWD SPs about knowledge that goes beyond the textbook, and the factors that enhance or diminish the quality of healthcare/medical service delivery from individuals who have experienced going through the healthcare/medical system. With time and with more training institutions engaging PWDs as SPs, this can be a potentially viable employment option for PWDs.
Notes on Contributors
Associate Professor May Lim is the Director of the Centre for Learning Environment and Assessment Development (CoLEAD) at the Singapore Institute of Technology, and a faculty in the Health and Social Sciences Cluster teaching occupational therapy.
At the time when this work was done, Mr Goh Zi An Galvyn was a research assistant in the Centre for Learning Environment and Assessment Development (CoLEAD) at the Singapore Institute of Technology.
Associate Professor Tan Bhing Leet is the Deputy Cluster Director (Applied Learning) of the Health and Social Sciences Cluster, and Programme Director of the Bachelor of Science in Occupational Therapy degree programme at the Singapore Institute of Technology.
Ethical Approval
Ethics approval was granted by the Singapore Institute of Technology Institutional Review Board for this project (IRB number: 20150002).
Acknowledgements
The authors thank all faculty, students, PWD and non-PWD standardised patients who were involved in the Singapore Institute of Technology Bachelor of Science in Occupational Therapy degree programme. In addition, we would like to extend our deepest gratitude to Associate Professor Tham Kum Ying, Education Director of Tan Tock Seng Hospital Pre-Professional Education Office and senior lecturers Miss Heidi Tan and Mr Lim Hua Beng from the Singapore Institute of Technology.
Funding
Funding was provided from the Singapore Ministry of Education (MOE Tertiary Education Research Fund grant: R-MOE-A203-A002).
Declaration of Interest
The authors declare no conflict of interest concerning any aspect of this research.
References
Kowitlawakul, Y., Chow, Y., Salam, Z., & Ignacio, J. (2015). Exploring the use of standardized patients for simulation-based learning in preparing advanced practice nurses. Nurse Education Today, 35(7), 894-899. https://doi.org/10.1016/j.nedt.2015.03.004
Lim, S. M., Tan, B. L., Lim, H. B., & Goh, Z. A. G. (2018). Engaging persons with disabilities as community teachers for experiential learning in occupational therapy education. Hong Kong Journal of Occupational Therapy, 31(1), 36-45. https://doi.org/10.1177/1569186118783877
Long-Bellil, L. M., Robey, K. L., Graham, C. L., Minihan, P. M., Smeltzer, S. C., Kahn, P., & Alliance for Disability in Health Care Education. (2011). Teaching medical students about disability: The use of standardized patients. Academic Medicine, 86(9), 1163-1170. https://doi.org/10.1097/ACM.0b013e318226b5dc
Minihan, P. M., Bradshaw, Y. S., Long, L. M., Altman, W., Perduta-Fulginiti, S., Ector, J., … Sneirson, R. (2004). Teaching about disability: Involving patients with disabilities as medical educators. Disability Studies Quarterly, 24(4). https://doi.org/10.18061/dsq.v24i4.883
Wells, T. P. E., Byron, M. A., McMullen, S. H. P., & Birchall, M. A. (2002). Disability teaching for medical students: Disabled people contribute to curriculum development. Medical Education, 36(8), 788-790. https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1365-2923.2002.01264_1.x
*Lim Sok Mui
Singapore Institute of Technology,
SIT@Dover, 10 Dover Drive,
Singapore 138683
Email: may.lim@singaporetech.edu.sg
Announcements
- Best Reviewer Awards 2025
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2025.
Refer here for the list of recipients. - Most Accessed Article 2025
The Most Accessed Article of 2025 goes to Analyses of self-care agency and mindset: A pilot study on Malaysian undergraduate medical students.
Congratulations, Dr Reshma Mohamed Ansari and co-authors! - Best Article Award 2025
The Best Article Award of 2025 goes to From disparity to inclusivity: Narrative review of strategies in medical education to bridge gender inequality.
Congratulations, Dr Han Ting Jillian Yeo and co-authors! - Best Reviewer Awards 2024
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2024.
Refer here for the list of recipients. - Most Accessed Article 2024
The Most Accessed Article of 2024 goes to Persons with Disabilities (PWD) as patient educators: Effects on medical student attitudes.
Congratulations, Dr Vivien Lee and co-authors! - Best Article Award 2024
The Best Article Award of 2024 goes to Achieving Competency for Year 1 Doctors in Singapore: Comparing Night Float or Traditional Call.
Congratulations, Dr Tan Mae Yue and co-authors! - Best Reviewer Awards 2023
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2023.
Refer here for the list of recipients. - Most Accessed Article 2023
The Most Accessed Article of 2023 goes to Small, sustainable, steps to success as a scholar in Health Professions Education – Micro (macro and meta) matters.
Congratulations, A/Prof Goh Poh-Sun & Dr Elisabeth Schlegel! - Best Article Award 2023
The Best Article Award of 2023 goes to Increasing the value of Community-Based Education through Interprofessional Education.
Congratulations, Dr Tri Nur Kristina and co-authors! - Best Reviewer Awards 2022
TAPS would like to express gratitude and thanks to an extraordinary group of reviewers who are awarded the Best Reviewer Awards for 2022.
Refer here for the list of recipients. - Most Accessed Article 2022
The Most Accessed Article of 2022 goes to An urgent need to teach complexity science to health science students.
Congratulations, Dr Bhuvan KC and Dr Ravi Shankar. - Best Article Award 2022
The Best Article Award of 2022 goes to From clinician to educator: A scoping review of professional identity and the influence of impostor phenomenon.
Congratulations, Ms Freeman and co-authors.









